Abstract
Introduction and importance
Ascariasis is one of the most common parasitic infections worldwide, especially in tropical and subtropical developing countries with poor personal hygiene and sanitation. This condition is a staggering worldwide public health problem with high morbidity and mortality. Intestinal obstruction is an acute presentation that occurs in cases where clumps of worms form, causing partial or complete obstruction of the intestinal lumen.
Case presentation
We report a case of a 5-year-old boy with total intestinal obstruction due to Ascaris lumbricoides, who underwent exploratory laparotomy and enterotomy to remove the worm masses.
Clinical discussion
Infestation with roundworms is widespread in developing countries. While the majority of the intestinal obstruction they cause may be treated conservatively, in some circumstances, surgery may be required.
Conclusion
Infestation with roundworms is widespread in developing countries, and although the majority of the intestinal obstruction they cause may be treated conservatively, in some circumstances, surgery may be required.
Keywords: Intestinal obstruction, Roundworms, Ascaris lumbricoides
Highlights
-
•
Infestation with roundworms is widespread in developing countries.
-
•
Most intestinal obstruction due to ascariasis may be treated conservatively.
-
•
In some circumstances, surgery may be required.
-
•
Hygiene, anthelmintic medication, and education are critical for prevention.
1. Introduction
Ascariasis is one of the worm infestations often found in the human body, located around 25 % of the world's human population and reaching at least 807 million to 1121 billion cases [1]. It has a mortality rate of 60,000 per year, mainly among cases that cause intestinal obstruction [2], [3].
Worms that cause intestinal disorders in children are common at 1–14 years of age [1], [4]. This occurs mainly in developing tropical and subtropical countries where personal hygiene and sanitation are poor [1]. We report this case according to the Updating Consensus Surgical CAse REport (SCARE) 2020 guidelines [5].
2. Presentation of case
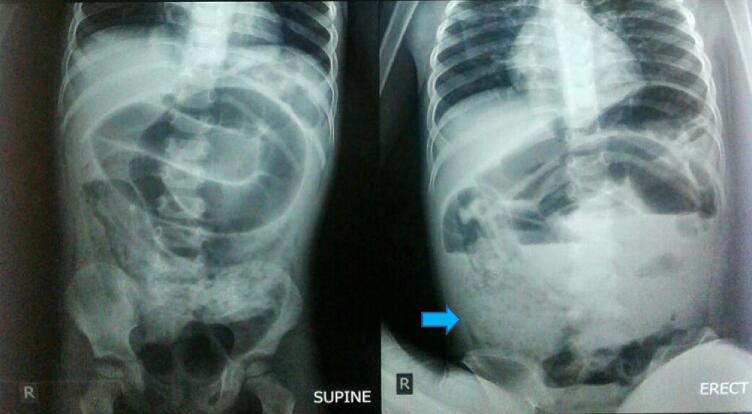
A 5-year-old boy was admitted to the emergency department with complaints of worsening abdominal pain over the previous 2 days. He had not passed urine or flatus for 3 days, accompanied by complaints of vomiting. For two weeks previously, he had abdominal pain, and the patient had a history of diarrhea. On examination, the child was thin, with symptoms and signs of malnutrition. The WHO performance status was 2, accompanied by moderate dehydration with a heart rate of 96 beats/min, respiration 22 times/min, and a temperature of 37.9 °C. On physical examination, the abdomen appeared to have a dark contour, which was painful when pressed, especially at the right hypochondrium, and a palpable mass was visible at the right hypochondrium. Other head-to-toe assessments were within normal limits. Laboratory examinations were within normal limits. An abdominal X-ray examination showed intestinal obstruction and the lower right area showed a view of a mass “whirlpool image,” with air-fluid level and no free air under the right hemidiaphragm (Fig. 1). Based on these examinations, the patient was diagnosed with total intestinal obstruction as high as the ileum due to suspected periappendicular infiltrates.
Fig. 1.
Abdominal X-ray examination showed dilated loops of the small intestine, with air-fluid levels, no free air under the right hemidiaphragm, and the right hypochondrium region showing a mass “whirlpool image” (arrow).
An exploratory laparotomy was performed, and intraoperatively it transpired that the appendix was only slightly hyperemic. Further identified in the terminal ileum to 20 cm distal to the cecum was an intraluminal mass as a bolus of ascariasis, and no other intra-abdominal organ abnormalities were found. Enterotomy was made 30 cm distal cecum (colon ascendens), milking from the ileum to the distal cecum to remove 540 g of the ascaric mass (Fig. 2). Postoperatively, the patient was given intravenous antibiotics for 7 days and a single dose of an anthelmintic drug by a pediatric doctor based on the results of a stool analysis. The patient went home on the 12th day.
Fig. 2.
Extraction of the worms during an enterotomy.
3. Discussion
In developing countries in Asia, Latin America, and Africa with poor sanitation, low educational standards, and personal hygiene, ascariasis is still a common parasite infection [6]. In south Asia and southeast Asia, the most prevalent soil-transmitted helminth discovered was Ascaris, with a prevalence of 18 %, followed by Trichuris 14 %, and hookworm 12 %. Cambodia, Vietnam, and Laos had the highest hookworm prevalence [7].
The infection caused by A. lumbricoides is frequently asymptomatic or produces mild, nonspecific symptoms. The phase of the parasite's life cycle and the severity of the infection influence symptoms in those seeking medical attention. At 10–14 days after infection, eosinophilic pneumonia (Loeffler syndrome) may develop as a result of a normally self-limiting inflammatory response to larvae migrating through pulmonary tissue [8]. In addition to coughing, urticaria, hemoptysis, and dyspnea, patients may also present with abnormal auscultatory breath sounds [8], [9]. Adult ascaris infections can cause acute abdomens, such as small bowel obstruction, upper gastrointestinal bleeding, intussusception and volvulus, peritonitis, and even gastric ascariasis with perforation. Acute cholecystitis, acute cholangitis, biliary colic, hepatic abscess, and acute pancreatitis are the five major clinical syndromes caused by hepatobiliary and pancreatic ascariasis. Intestinal ascariasis is frequently accompanied by diarrhea, loss of appetite, asthenia or stomach pain, other changes in bowel habits, and weight loss. Increased bowel sounds, abdominal discomfort, and distension are signs of intestinal obstruction, as is occult or fresh fecal blood, and anemia is typical with mucosal bleeding [9]. Many patients have a history of ascaris extrusion through the mouth or rectum [6].
The physical examination may reveal bloating, abdominal mass, abdominal tenderness, or abdominal pain [6]. Massive worm populations, coiled-up and interlaced behavior, neurotoxic release, and peristaltic contraction are the causes of intestinal blockages [10]. In the digestive tract, worms may produce an obstructive bolus when the load is massive. Though they can also be seen in large numbers in the jejunum, worms typically congregate in the terminal ileum [6], [11], [12].
The main causes of ascaris-related intestinal obstruction are that worms can form a large bolus that causes mechanical obstruction of the bowel lumen; the worm bolus may serve as a lead point in intussusception or a pivot in small-bowel volvulus; ascaris worms may be localized on the ileocecal valve, where their release of neurotoxins causes the contraction of the small intestine and can obstruct the intestine; and the inflammatory response brought on by the worms' anaphylatoxins, hemolysins, and endocrinolysins can result in obstruction of the intestinal lumen [6].
An abdominal x-ray that shows the levels and multiple linear images of Ascaris lumbricoides in dilated intestinal loops [10], with a “whirlpool” image in some cases, supports the diagnosis of roundworm obstruction, which is suspected based on the patient's medical history and symptoms of intestinal obstruction [10], [13]. The ultrasound examination will help detect thick echogenic strips with a central anechoic tube, several linear or curved echogenic strips without acoustic shadowing, “three-line” or “four-line” signs, and “bull's eye” appearances or “railway track” signs on transverse scans [13].
If the patient presents with intestinal subocclusion, medical procedures such as nasogastric drainage, broad-spectrum antibiotics, and intravenous fluids and electrolytes must be used. However, patients with total obstruction are candidates for surgical intervention after initial resuscitation and antimicrobial therapy. One strong dose of an anthelmintic may cause a fully developed intestinal blockage and be indicated to prevent the spontaneous resolution of the entangled bolus [13].
Surgical treatment includes performing milking of the worms distantly in the intestine, an enterotomy to remove the worms from the colon, or an intestinal resection with an entero–entero anastomosis in cases of necrosis [13]. If the obstruction is at the ileal level, the worms may be delicately milked to the cecum without damaging the bowel wall. Enterotomy must be performed if the obstruction is at the jejunum level since milking the bolus to the ileocecal valve could injure the bowel wall [6], [12].
An ileum enterotomy was performed in our case because the extent of the infestation prevented milking all Ascaris lumbricoides to the large bowel and could have damaged the intestinal wall. This allowed the majority of the roundworms to be removed, with the remainder requiring medical treatment with albendazole once intestinal transit had resumed. After taking the history of the present illness, the patient's parents did not know that their child previously had intestinal worms, except for a history of diarrhea and vomiting several times.
Due to the possibility of residual worms developing a worm bolus and spastic paralysis, anthelmintic therapy should be started 3 to 5 days following surgery, after the first bowel movement [6].To eliminate any worms, mebendazole or albendazole 100 mg twice daily for 3 days must be started following resolution and repeated 6 weeks later [13]. Resolution is defined as the occurrence of any two of the following criteria: beginning of defecation, removal of colicky discomfort, and disappearance of air-fluid levels [13].
A delay in therapy can cause intestinal perforation, intestinal gangrene, and worm spillover into the abdominal cavity [14], [15]. In children aged under 10 years, the mortality rate from ascaris intestinal blockage is 5.7 % [16].
4. Conclusion
Infestation with roundworms is widespread in developing countries, and although the majority of the intestinal obstruction they cause may be treated conservatively, in some circumstances, surgery may be required. The author would like to make some key recommendations to highlight the importance of population sanitary hygienic education (especially for risk groups), implementation of anti-helminthic medication programs, and educating authorities and leaders about intestinal parasitism because prevention is the most crucial aspect of this disease.
Patient consent
Written informed consent was obtained from the child's parents or guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Ethical approval was waived by the authors institution.
Funding
N/A.
Guarantor
Sulmiati and Muhammad Faruk.
Research registration number
N/A.
CRediT authorship contribution statement
Sulmiati, Farid Nurmantu, Ahmadwirawan, Nita Mariana, and Tommy R. Habar: study concept, surgical therapy for this patient. Sulmiati, and Muhammad Faruk: Data collection, Writing-Original draft preparation. Sulmiati, and Muhammad Faruk: Editing, Writing. All authors read and approved the final manuscript.
Conflicts of interest
N/A.
Acknowledgment
None.
References
- 1.Asai T., Còrdova Vidal C., Strauss W., Ikoma T., Endoh K., Yamamoto M. Effect of mass stool examination and mass treatment for decreasing intestinal helminth and protozoan infection rates in Bolivian children: a cross-sectional study. PLoS Negl. Trop. Dis. 2016;10 doi: 10.1371/journal.pntd.0005147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Tameemi K., Kabakli R. Ascaris lumbricoides: epidemiology, diagnosis, treatment, and control. Asian J. Pharm Clin. Res. 2020:8–11. doi: 10.22159/ajpcr.2020.v13i4.36930. [DOI] [Google Scholar]
- 3.J. Shah A. Shahidullah , Ascaris lumbricoides: a startling discovery during screening colonoscopy., Case Rep. Gastroenterol. 12 (n.d.) 224–229. doi:10.1159/000489486. [DOI] [PMC free article] [PubMed]
- 4.Khan W., Rahman H., Rafiq N., Kabir M., Ahmed M.S., Escalante P.D.L.R. Risk factors associated with intestinal pathogenic parasites in schoolchildren. Saudi J. Biol. Sci. 2022;29:2782–2786.. doi: 10.1016/j.sjbs.2021.12.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Stojanovic M., Slavkovic A., Stojanovic M., Marjanovic Z., Bojanovic M. A rare case of intestinal obstruction due to ascariasis in Niš, South Serbia. Open Med. 2011;6:390–394. doi: 10.2478/s11536-011-0028-y. [DOI] [Google Scholar]
- 7.Silver Z.A., Kaliappan S.P., Samuel P., Venugopal S., Kang G., Sarkar R., Ajjampur S.S.R. Geographical distribution of soil transmitted helminths and the effects of community type in South Asia and South East Asia - a systematic review. PLoS Negl. Trop. Dis. 2018;12 doi: 10.1371/journal.pntd.0006153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lal C., Huggins J.T., Sahn S.A. Parasitic diseases of the pleura. Am J Med Sci. 2013;345:385–389. doi: 10.1097/MAJ.0b013e318266e984. [DOI] [PubMed] [Google Scholar]
- 9.Jourdan P.M., Lamberton P.H.L., Fenwick A., Addiss D.G. Soil-transmitted helminth infections. Lancet. 2018;391:252–265. doi: 10.1016/S0140-6736(17)31930-X. [DOI] [PubMed] [Google Scholar]
- 10.Bhatt P.N. Acute intestinal obstruction due to ascaris. Med. Phoenix. 2017;1:39–40. doi: 10.3126/medphoenix.v1i1.17887. [DOI] [Google Scholar]
- 11.Wani I., Rather M., Naikoo G., Amin A., Mushtaq S., Nazir M. Intestinal ascariasis in children. World J. Surg. 2010;34:963–968. doi: 10.1007/s00268-010-0450-3. [DOI] [PubMed] [Google Scholar]
- 12.Hefny A.F., Saadeldin Y.A., Abu-Zidan F.M. Management algorithm for intestinal obstruction due to ascariasis: a case report and review of the literature. Ulus. Travma Acil Cerrahi Derg. 2009;15:301–305. http://www.ncbi.nlm.nih.gov/pubmed/19562557 [PubMed] [Google Scholar]
- 13.Andrade A.M., Perez Y., Lopez C., Collazos S.S., Andrade A.M., Ramirez G.O., Andrade L.M. Intestinal obstruction in a 3-year-old girl by Ascaris lumbricoides infestation: case report and review of the literature. Medicine (Baltimore) 2015;94 doi: 10.1097/MD.0000000000000655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta S., Kumar S., Satapathy A., Ray U., Chatterjee S., Choudhury T.K. Ascaris lumbricoides: an unusual aetiology of gastric perforation. J. Surg. Case Rep. 2012;2012 doi: 10.1093/jscr/rjs008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Romano G., Pepe P., Cavallero S., Cociancic P., Di Libero L., Grande G., Cringoli G., D’Amelio S., Rinaldi L. Ascariasis in a 75-year-old man with small bowel volvulus: a case report. BMC Infect. Dis. 2021;21:1045. doi: 10.1186/s12879-021-06718-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Darlington C.D., Anitha G.F.S. Ascaridial volvulus: an uncommon cause of ileal perforation. Iran. J. Med. Sci. 2018;43:432–435. http://www.ncbi.nlm.nih.gov/pubmed/30046214 [PMC free article] [PubMed] [Google Scholar]