Abstract
Conjunctival nevi are benign, heterogenous tumors that uncommonly arise from the lacrimal caruncle and plica semilunaris. We present a case of a patient diagnosed and managed for an unusual, pigmented nevus of the left caruncle involving the plica. An 84-year-old woman presented with a rapidly growing, pigmented lesion in her left nasal canthus. Examination demonstrated a raised, dark, pigmented area arising from the left caruncle and seeming to involve the plica semilunaris without scleral extension. The lesion was completely excised for histopathology, which confirmed the diagnosis of a compound nevus with pigment incontinence. Given the unfavorable anatomical position and prognostic significance in the case of malignancy, pigmented caruncular lesions should be thoroughly investigated with a low threshold for surgical removal.
Keywords: Lacrimal caruncle, Plica semilunaris, Benign pigmented nevus, Case report
Introduction
Nevi arising from the lacrimal caruncle and plica semilunaris are uncommon and sparsely reported in the literature [1–3]. Clinically, they can be difficult to distinguish from melanoma, which has important prognostic implications [1, 4]. This report overviews the diagnosis and management of a patient presenting with an unusual compound pigmented nevus.
Case Presentation
An 84-year-old woman presented with an expanding, pigmented lesion in the left nasal canthus, which had grown rapidly over 5 months. It had been discovered incidentally during a routine optometry assessment 14 months previously and has since shown no morphological change other than the recent size variation. She did not report any vision loss, eye pain, redness, or foreign body sensation, and there was no history of discharge or bleeding from the lesion. Her past ocular history was notable only for bilateral cataract surgeries 13 years before, with no history of trauma, eye disease, malignancy, chemotherapy use, occupational exposures, or use of industrial chemicals. Her medical conditions included type 2 diabetes mellitus, hypertension, and cardiac arrhythmia that were medically controlled, and her family history was unremarkable.
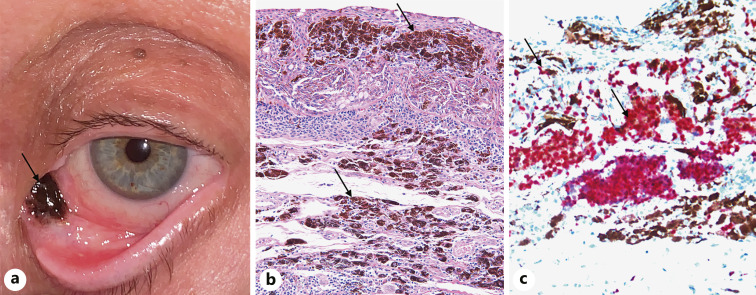
Visual acuity was 6/6 and 6/6-2 in her right and left eyes, respectively. Intraocular pressure was 8 mm Hg in the right and 8 mm Hg in the left eye. Anterior segment examination showed a raised, homogenous, pigmented region overlying her left caruncle and clinically involving the plica semilunaris but without scleral extension (shown in Fig. 1). Dilated ophthalmoscopy showed no abnormalities. Examination of the right eye was also unremarkable.
Fig. 1.
Compound nevus with pigment incontinence. a Clinical photograph demonstrating the lesion occupying the left caruncle and involving the plica semilunaris; the surrounding tissue appears healthy. There are no additional features including hairs, feeder vessels, cysts, or satellite lesions. b Excisional biopsy histology (H&E, ×100) demonstrating heavily pigmented spindle melanocytes arranged at the epithelial-stromal junction and mature epithelioid nevus cells in the underlying stroma that are associated with abundant melanin-laden macrophages. c Nevus cells stain red with Sox 10 (Sox 10, ×200).
Given the tumor’s recent expansion and its unusual anatomical position, the decision was made to proceed with complete surgical removal. Excisional biopsy showed, in a 5 × 3 mm piece, a 5 mm proliferation of heavily pigmented melanocytes arranged at the epithelial-stromal junction, mature nevus cells, and abundant melanin-laden macrophages in the underlying stroma with no evidence of pagetoid spread or dysplasia, confirming a compound nevus (shown in Fig. 1). Given these findings, no further investigations were performed including cytogenetic analysis. The patient had an uncomplicated postoperative course and will continue to be reviewed regularly for recurrence.
Conclusion
The lacrimal caruncle and plica semilunaris are modified structures of the bulbar conjunctiva, located within the nasal canthus [5]. Conjunctival nevi comprise more than 50% of all conjunctival tumors; however, they uncommonly arise at this site, and although they are benign, the risk of local recurrence is unclear and malignant transformation can occur [2, 3].
Conjunctival nevi have a wide spectrum of clinical and histological features with a broad list of differentials [1–3]. They can present either during infancy (congenital) or are acquired later in life, as was the case in this report [6]. They most commonly occur in Caucasian patients, although other racial groups are affected [2]. The epibulbar conjunctiva is the most common site, whereas the plica is the least common [2]. Patients often notice a new lesion and may report other symptoms including pain and inflammation; however, these symptoms are uncommon [2]. Unlike this case, nevi may begin as nonpigmented and then progressively darken over time, particularly during puberty and pregnancy, and this can be misinterpreted as tumor growth [7]. Clinically, pigmented nevi are typically raised, circumscribed, brown/tan lesions that may appear cystic, with possible vascularization or chronic inflammatory changes [1, 2].
Amelanotic nevi should be distinguished from other conditions with similar features such as inflamed pingueculum, allergic conjunctivitis, or lymphangioma, which have different management implications [2]. Typical pigmented nevi can often be diagnosed clinically, managed with 6-monthly or annual reviews, and documented with clinical photography [7]. However, there might be risk factors and/or clinical features that are concerning for malignancy including older patient age at the time of presentation, a history of cutaneous melanoma or dysplastic nevus syndrome, atypical location, color change, lack of intrinsic cysts, prominent feeder vessels, and rapid growth over weeks to months [2, 3, 7]. In such cases or where there is diagnostic uncertainty, complete excision for histological visualization is advised [2, 7]. Other reasons for removal include patient concerns about possible malignancy and cosmetic purposes [2]. In this report, it was rapid tumor growth and the unusual location that prompted an urgent biopsy.
As with other conjunctival nevi, a compound growth pattern with stromal and junctional melanocytes is the most common histology, followed by subepithelial and junctional forms [2]. A broad list of differential diagnoses has been reported and includes inflammatory conditions, acquired melanosis, seborrheic and solar keratoses, papilloma, in situ or invasive carcinoma, and melanoma; nevi are the most prevalent [1]. Although cases of melanoma are isolated [8], the plica and caruncle are regarded as unfavorable locations for conjunctival melanoma with an associated higher risk of recurrence and disease mortality [1]. Therefore, pigmented lesions at this site should be treated with a higher degree of concern, and clinicians should have a lower threshold for surgical intervention.
The patient’s written informed consent was obtained for the publication of this case report and any accompanying images. The CARE Checklist has been completed by the authors for this case report, attached as online supplementary material (for all online suppl. material, see www.karger.com/doi/10.1159/000529421).
Statement of Ethics
This retrospective review of patient data did not require ethical approval in accordance with local/national guidelines. All data that support the findings of this study are included in this article. The patient’s written informed consent was provided for this report including for the publication of medical details and accompanying images. All identifiable patient information is kept strictly confidential and not reported.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding was received for this report.
Author Contributions
Mr Joshua Meyerov: corresponding author, responsible for performing the literature review, writing the manuscript, and preparing the final version for submission. Dr Lewis Levitz: the consultant ophthalmic surgeon for this case, responsible for overseeing the research team, assisted with the writing of the manuscript, and approved the final version for submission. Dr Afaf Haddad: the lead pathologist for this case, assisted with image collection, the interpretation of histology, and the writing of the report.
Funding Statement
No funding was received for this report.
Data Availability Statement
All data generated or analyzed during this study are included in this article and its online supplementary material. Further inquiries can be directed to the corresponding author.
Supplementary Material
References
- 1. Levy J, Ilsar M, Deckel Y, Maly A, Pe’er J. Lesions of the caruncle: a description of 42 cases and a review of the literature. Eye. 2009;23(5):1004–18. 10.1038/eye.2008.316. [DOI] [PubMed] [Google Scholar]
- 2. Shields CL, Fasiuddin AF, Mashayekhi A, Shields JA. Conjunctival nevi: clinical features and natural course in 410 consecutive patients. Arch Ophthalmol. 2006 Feb;122(22):167–75. 10.1001/archopht.122.2.167. [DOI] [PubMed] [Google Scholar]
- 3. Shields CL, Chien JL, Surakiatchanukul T, Sioufi K, Lally SE, Shields JA. Conjunctival tumors: review of clinical features, risks, biomarkers, and outcomes–the 2017 J. Donald M. Gass lecture. Asia Pac J Ophthalmol. 2017;6(2):109–20. 10.22608/APO.201710. [DOI] [PubMed] [Google Scholar]
- 4. Paridaens AD, Minassian DC, McCartney AC, Hungerford JL. Prognostic factors in primary malignant melanoma of the conjunctiva: a clinicopathological study of 256 cases. Br J Ophthalmol. 1994;78(4):252–9. 10.1136/bjo.78.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Forrester JV, Dick AD, McMenamin PG, Roberts F, Pearlman E. The eye: basic sciences in practice. 4th ed.Edinburgh UK: Elsevier; 2016. p. 85–6. [Google Scholar]
- 6. Alkatan HM, Al-Arfaj KM, Maktabi A. Conjunctival nevi: clinical and histopathologic features in a Saudi population. Ann Saudi Med. 2010;30(4):306–12. 10.4103/0256-4947.65265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. American Academy of Ophthalmology . Conjunctival pigmented lesions: diagnosis and management. [cited 2022 Oct 10]. Available from: https://www.aao.org/eyenet/article/conjunctival-pigmented-lesions-diagnosis-managemen. [Google Scholar]
- 8. Jain S, Chandravanshi SL, Rathore MK, Goyal P, Jain SC. Huge malignant melanoma of caruncle with extensive involvement of conjunctiva. J Indian Med Assoc. 2012;110(2):115–7. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this article and its online supplementary material. Further inquiries can be directed to the corresponding author.