Abstract
Background
Nicotine is a psychostimulant drug with purported use in sports environments, though the use of nicotine among athletes has not been studied extensively.
Objective
The aim of this study was to assess the nicotine positivity rate in 60,802 anti-doping urine samples from 2012 to 2020.
Methods
Urine samples obtained in-competition at different national and international sports events held in Italy during the period 2012–2020 were analysed. All samples were from anonymous athletes that were collected and analysed at the WADA-accredited antidoping laboratory in Rome, Italy. Samples were analysed by gas chromatography coupled with mass spectrometry, with a cut-off concentration for nicotine of > 50 ng/mL. Results were stratified by year, sport and sex.
Results
An overall mean of 22.7% of the samples (n = 13,804; males: n = 11,099; females: n = 2705) showed nicotine intake, with male samples also displaying higher positivity rates than female (24.1% vs 18.5%). Sample positivity was higher during 2012–2014 (25–33%) than 2015–2020 (15–20%). Samples from team sports displayed a higher positivity rate than those from individual sports (31.4 vs 14.1%).
Conclusions
The current data demonstrates that one in five samples from a range of 90 sports test positive for nicotine in-competition. There is a lower positivity rate in endurance versus power/strength athletes and higher positivity rate in team versus individual sports, probably accounted for by differences in physiological and psychological demands and the desire for socialisation. WADA, international and national sports federations should consider these findings with concern, proactively investigate this phenomenon and act in order to protect the health and welfare of its athletes.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40279-023-01819-y.
Key Points
| WADA currently has nicotine on its Monitoring Program due to high use in winter sports, although current research evidence does not support a clear ergogenic effect. |
| This study highlights that one in five samples from a range of 90 sports test positive for nicotine in-competition, with use amongst aerobic/endurance athletes greatest, followed by team sports. |
| International and national sports federations should proactively investigate this phenomenon and act in order to protect the health and welfare of its athletes. |
| WADA should continue to monitor nicotine use and support research that further determines user trends to understand why and how athletes use nicotine. |
Introduction
After caffeine, nicotine is the most widely consumed psychoactive substance in the world [1], with a prevalence of consumption in excess of 20% for the global population [2] in the form of smoked and smokeless tobacco, and a range of products marketed as nicotine replacement therapies. In the sporting domain, whilst nicotine consumption through the use of chewing tobacco became synonymous with professional baseball [3], it was the discovery of its high use amongst winter sports [4, 5] that led to the World Anti-Doping Agency (WADA) placing nicotine on its Monitoring Program in 2012 [6]. This signalled that WADA wanted to detect patterns of (mis)use to determine whether nicotine could enhance sport performance or increase the health risk to an athlete that would see it upgraded to the List of Prohibited Substances.
Athletes believe the consumption of nicotine (or related substances) to be beneficial by preventing a dry mouth through increased saliva secretion, stimulating satiety to control body weight, improving concentration and reaction time, and helping relaxation to achieve a desirable arousal-attention (for review, see [3]). Despite exerting physiological and psychological effects that should be ergogenic and nootropic, the current evidence base does not support this [3]. However, long-term exposure to nicotine (i.e. chronic users) could lead to addiction that develops tolerance, withdrawal and dependence [7], whereby nicotine use in this cohort has been shown to improve exercise performance when nicotine-abstinent compared with -satiated [8].
Given the health risks to athletes posed by long-term use of nicotine directly, and indirectly through tobacco [9], and that research on this topic has not been forthcoming in recent years, the purpose of this paper was to describe the positivity rate of nicotine use in athletes and determine any temporal and user trends from a sample of 60,802 doping control tests from 2012 to 2020.
Materials and Methods
Sample Collection
All urine samples were collected from national and international in-competition (IC) doping control tests that took place in Italy between 2012 and 2020. Note, sample collection (and analyses) for 2020 were adversely affected by the emergence of COVID-19. Samples were anonymously analysed as part of the WADA Monitoring Program at the WADA-accredited antidoping laboratory in Rome, Italy. The sample was composed of national and international athletes that were tested during sports competitions held in Italy. According to the WADA Code, we analysed urine samples collected from participants that were regularly enrolled in the national and international sports federations of each discipline (elite and amateur levels and paralympic sports).
Sample Analysis
Concerning the techniques employed in the analysis of the samples, we used gas chromatography (GC) coupled with mass spectrometry (GS/MS) with electronic ionisation and acquisition in selected ion monitoring. The GC/MS system was a GC 7890 from Agilent Technologies interfaced with an Agilent 5975 MS, with an HP5 column (17 m × 0.2 mm × 0.33 μm). The parameters for GC were the following: oven programme – 85 °C (1 min), 15 °C/min to 270 °C, 50 °C/min to 310 °C (3.5 min); injection – 1 µL, pulsed splitless; injector temperature – 270 °C. We followed the protocol that is normally used for narcotics and stimulants [10]. The urine samples were alkalinised with NaOH and NaCl was added for a salting out effect. The samples were extracted with tert-butyl methyl ether. The organic extracts were then taken to dryness under a reduced nitrogen flow at room temperature and reconstituted with an extraction solvent before GC/MS analysis. Diphenylamine was added as an internal standard (ISTD).
The estimated nicotine concentration was > 50 ng/mL according to the WADA monitoring program, which is based on allowing for the lower limit of quantification and a conservative concentration limit for active consumption [4]. The advantage of this conservative limit is that active consumption is clearly distinct from passive exposure (e.g. tobacco smoke) and trace amounts through diet (e.g. potatoes, cauliflower) in ‘tobacco-free’ individuals, as well as abstinent nicotine users [3, 4]. However, a disadvantage is a potential under-estimation of true positivity.
Data Analysis and Statistics
Data were presented as number of urine samples, number of nicotine (positive) samples and stratified by biological sex using positivity rate (percentage). We further stratified positivity (percentage) by year and for team and individual sports. All data management and analyses were performed using GraphPad Prism (GraphPad Software, Inc., CA, USA).
Results
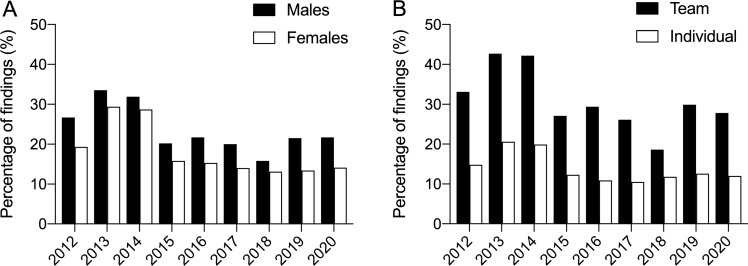
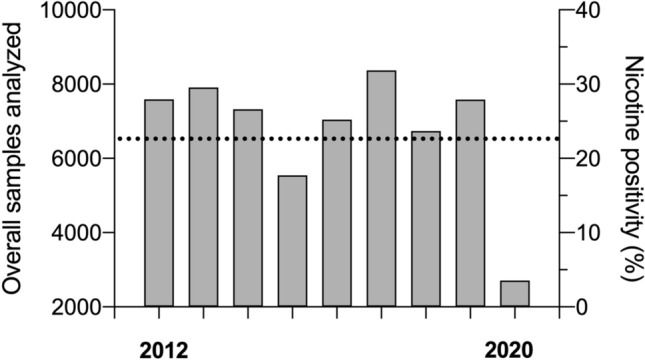
Figure 1 displays that 13,804 samples showed nicotine intake (males = 11,099 [overall mean 24.1%]; females = 2705 [overall mean 18.5%]), equating to an overall mean positivity of 22.7%. As can be seen in Fig. 1 and Table 1, there was a decline in positivity rate in 2015 that was maintained until 2020. Of 90 sports, 83 (92.2%) showed at least one sample that contained nicotine (Supplementary Table 1, see electronic supplementary material [ESM]). The most represented sport was association football (soccer) with 20,454 tests, with overall nicotine positivity at 29% (range from 18 to 40% depending on year). Figure 2A displays trends for positivity in male and female samples, while Fig. 2B shows team (overall mean 31.4%) and individual (overall mean 14.1%) sports. Table 2 further details sports above the sample median per year, and shows that 90.1% (73/81) of team sports compared with 39.9% of individual sports (69/173) exhibited nicotine use greater than the 20% global consumption in the general population. Table 2 also shows that athletes in endurance events/sports displayed a lower rate of positivity than those engaged in power and strength sports/disciplines. This is highlighted particularly well by the results from athletics (Supplementary Table 2, see ESM), the third most represented sport.
Fig. 1.
Total samples in competition by year with detected nicotine positivity (%). Bars represent total sample for each year; horizontal black dashed line represents the overall mean for nicotine positivity (22.7%)
Table 1.
Nicotine positivity rate in all samples analysed
| Year | Urine samples | Nicotine positive samples | Nicotine positivity % |
||||
|---|---|---|---|---|---|---|---|
| Total (N) | Males (N) | Females (N) | Total (N) | Males (N) | Females (N) | ||
| 2012 | 7591 | 5898 | 1693 | 1901 | 1575 | 326 | 25.0 |
| 2013 | 7909 | 6034 | 1875 | 2574 | 2022 | 552 | 32.5 |
| 2014 | 7321 | 5555 | 1766 | 2277 | 1771 | 506 | 31.1 |
| 2015 | 5540 | 4346 | 1194 | 1069 | 880 | 189 | 19.3 |
| 2016 | 7042 | 5357 | 1685 | 1421 | 1164 | 257 | 20.2 |
| 2017 | 8368 | 6330 | 2038 | 1550 | 1265 | 285 | 18.5 |
| 2018 | 6737 | 5180 | 1557 | 1023 | 819 | 204 | 15.2 |
| 2019 | 7582 | 5376 | 2206 | 1450 | 1154 | 296 | 19.1 |
| 2020 | 2712 | 2073 | 639 | 539 | 449 | 90 | 19.9 |
Fig. 2.
Positivity rate (%) of nicotine for males and females (A) and team and individual sports (B)
Table 2.
Nicotine positivity collected in-competition from 2012 to 2020 by sport
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | |
| Team sports | ||||||||||||||||||
| American football | 41.7 | 36 | 41.7 | 36 | 41.8 | 55 | ||||||||||||
| Baseball | 74.7 | 75 | 65.0 | 60 | 85.5 | 55 | 47.8 | 46 | 47.1 | 51 | 55.8 | 43 | 66.7 | 72 | ||||
| Basketball | 37.2 | 309 | 40.4 | 230 | 47.0 | 304 | 32.1 | 190 | 27.2 | 393 | 22.5 | 396 | 16.6 | 308 | 24.6 | 289 | 17.6 | 85 |
| Handball | 47.5 | 80 | 61.3 | 142 | 71.1 | 54 | 46.3 | 54 | 38.9 | 131 | 29.7 | 155 | 18.9 | 74 | 29.5 | 61 | 23.3 | 30 |
| Hockey (field) | 37.7 | 61 | 51.9 | 27 | 45.5 | 33 | 28.7 | 101 | 10.0 | 40 | ||||||||
| Hockey (ice) | 46.3 | 82 | 61.3 | 88 | 53.8 | 80 | 34.3 | 70 | 18.1 | 72 | 39.3 | 56 | 44.4 | 36 | ||||
| Hockey (indoor) | 30.0 | 40 | 35.2 | 37 | 40.0 | 30 | 48.5 | 132 | 33.7 | 95 | ||||||||
| Rugby | 38.0 | 184 | 46.8 | 109 | 45.5 | 99 | 17.7 | 175 | 32.1 | 187 | 30.5 | 174 | 17.4 | 201 | 34.8 | 282 | 25.0 | 60 |
| Soccer | 31.3 | 3003 | 40.4 | 3078 | 39.0 | 2551 | 26.0 | 1943 | 26.2 | 1926 | 25.1 | 2879 | 18.4 | 2325 | 27.3 | 1623 | 26.1 | 1126 |
| Volleyball | 32.1 | 249 | 53.6 | 248 | 46.4 | 265 | 31.7 | 145 | 33.9 | 274 | 27.0 | 237 | 23.8 | 261 | 37.4 | 222 | 39.5 | 124 |
| Water polo | 21.5 | 191 | 38.5 | 252 | 40.2 | 209 | 23.6 | 140 | 21.5 | 261 | 25.9 | 239 | 21.5 | 135 | 21.4 | 187 | 34.6 | 26 |
| Individual sports | ||||||||||||||||||
| Archery | 30.6 | 49 | 68.1 | 47 | 27.9 | 37 | 27.6 | 86 | 8.7 | 46 | 29.0 | 62 | 52.6 | 19 | ||||
| Athletics | 9.9 | 476 | 15.8 | 704 | 12.4 | 676 | 5.7 | 488 | 7.2 | 636 | 6.1 | 865 | 12.6 | 540 | 6.8 | 851 | 3.7 | 216 |
| Biathlon | 8.3 | 48 | ||||||||||||||||
| Body building | 20.8 | 72 | ||||||||||||||||
| Boxing | 15.0 | 160 | 32.3 | 124 | 36.3 | 135 | 13.5 | 133 | 6.7 | 90 | 10.8 | 93 | 9.0 | 111 | 18.6 | 156 | 14.5 | 62 |
| Canoe | 4.5 | 44 | 8.3 | 48 | 11.4 | 79 | 6.3 | 63 | 4.9 | 82 | 11.8 | 85 | ||||||
| Climbing | 13.5 | 37 | 7.4 | 27 | 12.7 | 72 | ||||||||||||
| Cycling | 5.6 | 948 | 8.2 | 1067 | 8.5 | 1135 | 4.9 | 896 | 4.0 | 1048 | 5.2 | 1052 | 9.3 | 783 | 4.6 | 862 | 2.3 | 260 |
| Dance sports | 57.1 | 42 | 25.0 | 16 | ||||||||||||||
| Diving | 34.4 | 32 | 43.1 | 51 | 43.6 | 39 | 34.5 | 58 | 25.5 | 55 | 26.2 | 65 | ||||||
| Equestrian | 56.7 | 30 | 23.6 | 55 | 47.1 | 17 | ||||||||||||
| Fencing | 42.1 | 159 | 47.1 | 121 | 43.3 | 120 | 27.3 | 55 | 44.9 | 49 | 21.6 | 116 | 15.7 | 108 | 26.2 | 122 | ||
| Golf | 34.8 | 46 | 50.0 | 36 | ||||||||||||||
| Gymnastics | 22.4 | 58 | 20.4 | 54 | 25.8 | 62 | 26.0 | 50 | 20.9 | 43 | 4.9 | 81 | 22.8 | 57 | 26.0 | 131 | 28.1 | 32 |
| Judo | 7.7 | 65 | 18.4 | 38 | 18.4 | 38 | 11.9 | 59 | 15.7 | 51 | 17.9 | 140 | ||||||
| Karate | 31.3 | 16 | ||||||||||||||||
| Kickboxing | 10.8 | 51 | ||||||||||||||||
| Lifesaving | 8.2 | 61 | 6.7 | 45 | ||||||||||||||
| Motorcycling racing | 15.8 | 19 | ||||||||||||||||
| Powerlifting | 25.0 | 24 | ||||||||||||||||
| Roller sports | 8.9 | 45 | 15.2 | 66 | 6.3 | 16 | ||||||||||||
| Rowing | 9.0 | 67 | 8.3 | 96 | 3.2 | 63 | 8.0 | 75 | 7.3 | 110 | 3.6 | 56 | 6.3 | 143 | ||||
| Sailing | 17.2 | 29 | ||||||||||||||||
| Shooting | 34.3 | 108 | 42.9 | 28 | 33.3 | 69 | 40.0 | 55 | 26.0 | 96 | 28.6 | 42 | 28.2 | 163 | 38.9 | 18 | ||
| Skating (artistic) | 33.3 | 36 | ||||||||||||||||
| Skating (speed) | 27.3 | 161 | 3.6 | 28 | 14.3 | 35 | 10.6 | 104 | 9.6 | 157 | ||||||||
| Skiing (alpine) | 5.4 | 93 | 58.3 | 65 | 57.8 | 64 | 25.4 | 106 | 27.8 | 54 | 16.6 | 73 | 16.5 | 97 | 12.5 | 24 | ||
| Skiing (cross c.) | 15.3 | 72 | 23.3 | 90 | 33.9 | 56 | 13.3 | 60 | 10.2 | 49 | 14.0 | 86 | ||||||
| Skiing (mountaineer) | 19.6 | 46 | 25.0 | 32 | ||||||||||||||
| Swimming | 10.1 | 149 | 10.8 | 158 | 16.7 | 239 | 14.2 | 219 | 6.4 | 362 | 2.5 | 322 | 9.1 | 350 | 5.7 | 420 | 1.9 | 106 |
| Taekwondo | 33.3 | 27 | 17.7 | 62 | ||||||||||||||
| Tennis | 29.2 | 106 | 32.8 | 64 | 18.2 | 77 | 23.4 | 64 | 14.3 | 91 | 13.3 | 75 | 15.4 | 65 | ||||
| Tennis (table) | 14.0 | 43 | 40.0 | 45 | ||||||||||||||
| Triathlon | 6.3 | 79 | 3.3 | 60 | 3.6 | 83 | 3.6 | 84 | 5.7 | 88 | 7.8 | 115 | 1.7 | 181 | ||||
| Underwater sports | 5.3 | 38 | 22.2 | 27 | 22.6 | 53 | 6.8 | 103 | 13.6 | 66 | 10.3 | 58 | ||||||
| Weightlifting | 47.4 | 38 | 60.0 | 50 | 56.7 | 30 | 40.3 | 67 | 38.6 | 83 | 19.8 | 121 | 39.4 | 66 | ||||
| Wrestling | 31.0 | 29 | 45.2 | 31 | 10.8 | 83 | 15.5 | 84 | 12.5 | 72 | ||||||||
Data are presented as positivity rate of nicotine (> 50 ng/ml) present in urine samples in percentage values (%) and number of samples analysed (n) in competitions stratified by team sports and individual sports. The sample cut-off is the median for each year (2012: 36; 2013: 27; 2014: 27; 2015: 27; 2016: 39; 2017: 40; 2018: 40; 2019: 55; 2020: 16)
Discussion
The novel and important results of this investigation are that (i) one in five samples from a range of 90 sports contained nicotine in-competition, (ii) there is a trend of declining consumption across the nine years of anti-doping urinalysis, (iii) samples from team sports displayed approximately twice the positivity than those from individual sports, and (iv) one in four male and one in five female samples showed nicotine positivity. The current data supports previous doping control reports [4, 5] in demonstrating a high positivity rate of active nicotine use by athletes in-competition that is sustained temporally and across many sports.
Strong User Trends are Demonstrated for Nicotine Use
We observed a clear difference in nicotine use between different sports. Table 2 highlights that in general, athletes requiring high aerobic capacity (endurance, e.g. cycling, athletics, triathlon, rowing, swimming) displayed much lower nicotine use than those more reliant on strength and power (e.g. American football, baseball, weightlifting) and skill and tactics (e.g. golf, fencing, shooting). This observation is similar to previous reports from athletes [11, 12] and is best explained by the fact that tobacco use could reduce aerobic and muscular performance, which would lead to lower consumption [3], and/or that endurance athletes have greater health awareness of the long-term use of nicotine/tobacco [9]. Future research could include more detailed analysis around this matter by using, for example, a standardised framework that provides quantitative assessment of the demands across different sports that are comparable in their athletic variables (i.e. bioenergetic, neuromuscular, psychomotor and biomechanical factors) to group sports as strength and power, muscular endurance, aerobic endurance, movement agility, reaction time, psychomotor skill and accuracy [13].
It was surprising to observe a high positivity in sports with high overall metabolic demand such as basketball, handball, hockey, association (soccer) and rugby football, and volleyball (Table 2). As suggested by McDuff et al. [14], such use is more likely a result of the social environment and/or reflects patterns of use that are explained not by a drive for performance-enhancement but by the need for relaxation and/or recovery. For example, an investigation into snus use by footballers in the UK revealed an alarming and increasing trend [15]. One high-profile player, Jamie Vardy, admitted snus “…helped me chill out…” [15], something that is corroborated by practitioners who claim widespread practice, with players using and sharing products openly [16]. This type of use may be explained by the fact that at high doses nicotine exerts a depressant or relaxant effect through the activation of endogenous opioid pathways [17], whilst nicotine could increase the pain threshold by exerting antinociceptive effects [18, 19]. Data from winter sports indicate that in addition to high use [4, 5], regular smokeless tobacco use induces greater satisfaction and psychological reward, similar to the effects of smoking tobacco [20]. A recent study showed that athletes who practiced high-intensity sports were less likely to smoke cigarettes compared with low-intensity sport athletes. Moreover, those practicing an individual sport are less likely to use smokeless tobacco and more likely to vape compared with those practicing team sports [21]. Team sports were also associated with increased use of smokeless and smoked tobacco compared with no participation in team sports [22], confirming, as in our sample, that socialisation could be fundamental in this type of behaviour. Notably, our data supports an increased use in team compared with individual sports (Fig. 2B). However, this is likely secondary to aerobic demand, as discussed above, as some individual sports (e.g., archery, diving, fencing, shooting, weightlifting) consistently displayed high use (Table 2).
Research and Policy Implications
Let us use association football (soccer) as an example, as this represented the largest cohort within our sample (Table 2; n = 20,454 or 34%). Overall positivity of nicotine amongst this cohort was 29% (yearly range 18–40%) with the high-profile investigation noted above uncovering the extent of this problem. Professional football players display elevated levels of supplement use—some without seeking advice—but low levels of knowledge about doping, with a majority not expecting to be tested for drugs [23, 24]. This type of behaviour makes it imperative that national and international governing bodies proactively investigate this concerning issue and act to protect the health and welfare of its athletes, for example with anti-doping prevention and education programmes [24]. Additionally, results from the current study and previous doping control reports [4, 5] should convince WADA to maintain nicotine’s inclusion in its monitoring programme to further determine patterns of use amongst athletes that would afford a better understanding of why and how athletes use nicotine; this could inform policy or interventions to reduce consumption and minimise harm.
Nicotine is highly addictive and poses health risks to athletes, especially through long-term use, whether caused by nicotine directly or indirectly through tobacco [9]. The current data indicate that since 2012, nicotine use amongst athletes has declined, although Fig. 1 shows that since 2015 positivity has been sustained. This mirrors declining global trends in tobacco use, for both males and females, because of tobacco control measures [25]. Nevertheless, there is still cause for concern given that for young adults and youths, > 70% of nicotine consumption is attributable to vaping [26]. There is a distinction between risk reduction from tobacco cessation and potential harm from nicotine dependence and the gateway effect, whereby nicotine replacement therapies occupy a lower place on the harm continuum than tobacco; they are not harmless or risk-free [26–28]!
Limitations
The current data set is taken from one country only, and therefore may not be representative of other countries or regions. However, as an example, trends for tobacco use in Italy mirror those globally, both in terms of prevalence and declining rate [25, 29]. Further, the current larger data set is not dissimilar to that reported from the Swiss Laboratory for Doping Analyses 2010–11 [5]. Adopting a conservative concentration limit for the presence of urinary nicotine may underestimate true positivity but allows determination of active consumption (cf. passive smoking). However, anti-doping analyses such as this do not allow the route of nicotine consumption to be identified (i.e. smoked vs smokeless tobacco vs nicotine replacement products [electronic cigarettes]). Such information is necessary in order to understand why and how athletes use nicotine, in an attempt to reduce consumption and minimise harm. Finally, it was not possible to calculate (period) prevalence with the current data set due to the following: no baseline data, knowledge of true random testing, unique versus duplicate athlete sampling, the wider population (i.e. Italian vs international athletes). However, the fact that our positivity rates are in line with previous research [4, 5, 11, 12, 21, 22] provides confidence.
Conclusion
The finding of 22.7% nicotine positivity among samples is alarming and should not be underestimated. Our findings should be considered with concern by stakeholders in the sports environment. They should further investigate this phenomenon and act in order to protect the health and welfare of their athletes.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Conflicts of Interest
TM has received funding from WADA for research into nicotine (project support only).
Availability of data and material
All data that support the findings of this study are shown in the Supplementary Material Table 1 (see electronic supplementary material).
Ethics approval
The WADA-approved laboratory (as Rome Antidoping Lab) follows the 1964 Declaration of Helsinki and any applicable national standards as they relate to the involvement of human subjects in research. There is no need for an ethical approval for antidoping samples where the analysis is targeted to a substance that is in the WADA list or in the WADA monitoring program: the athletes approve this when they are ‘enrolled’ within the rules of the sport federations. The Director of the WADA-accredited laboratory that analysed the data provided the Code of Ethics to all employees and ensured their understanding and compliance with all aspects of the Code. All employees of laboratories and WADA-approved laboratories shall strictly respect the confidentiality of analytical testing results, as well as that of all other laboratory or testing authority information, including information provided by WADA under confidentiality. The laboratory implemented and complied with the provision(s) of the WADA Code of Ethics to ensure the strict anonymity of individual athletes. The laboratories are expected to comply with the relevant and applicable national laws regarding the handling, storage and discarding of controlled (illegal) substances.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Author contributions
TZ and TM drafted the manuscript and interpreted the data. FB and MGA analysed the data. All authors critically reviewed the manuscript, provided significant input and approved the final version.
References
- 1.Boutrel B, Koob GF. What keeps us awake: the neuropharmacology of stimulants and wakefulness-promoting medications. Sleep. 2004;27(6):1181–1194. doi: 10.1093/sleep/27.6.1181. [DOI] [PubMed] [Google Scholar]
- 2.Reitsma MB, Kendrick PJ, Ababneh E, Abbafati C, Abbasi-Kangevari M, Abdoli A, Abedi A, Abhilash ES, Abila DB, Aboyans V, Abu-Rmeileh NM. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. The Lancet. 2021;397(10292):2337–2360. doi: 10.1016/S0140-6736(21)01169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mündel T. Nicotine: sporting friend or foe? a review of athlete use, performance consequences and other considerations. Sports Med. 2017;47(12):2497–2506. doi: 10.1007/s40279-017-0764-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marclay F, Saugy M. Determination of nicotine and nicotine metabolites in urine by hydrophilic interaction chromatography-tandem mass spectrometry: Potential use of smokeless tobacco products by ice hockey players. J Chromatogr A. 2010;1217(48):7528–7538. doi: 10.1016/j.chroma.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Marclay F, Grata E, Perrenoud L, Saugy M. A one-year monitoring of nicotine use in sport: Frontier between potential performance enhancement and addiction issues. Forensic Sci Int. 2011;213(1–3):73–84. doi: 10.1016/j.forsciint.2011.05.026. [DOI] [PubMed] [Google Scholar]
- 6.World Anti-Doping Agency (WADA). The 2012 Monitoring Program, Montreal. www.wada-ama.org/sites/default/files/resources/files/WADA_Monitoring_Program_2012_EN.pdf. Accessed 9 Sept 2022.
- 7.Zandonai T, Chiamulera C, Mancabelli A, Falconieri D, Diana M. A preliminary investigation on smokeless tobacco use and its cognitive effects among athletes. Front Pharmacol. 2018;9:216. doi: 10.3389/fphar.2018.00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zandonai T, Tam E, Bruseghini P, Capelli C, Baraldo M, Chiamulera C. Exercise performance increase in smokeless tobacco-user athletes after overnight nicotine abstinence. Scand J Med Sci Sports. 2019;29(3):430–439. doi: 10.1111/sms.13333. [DOI] [PubMed] [Google Scholar]
- 9.Benowitz NL. Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annu Rev Pharmacol Toxicol. 2009;49:57–71. doi: 10.1146/annurev.pharmtox.48.113006.094742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strano Rossi S, de la Torre X, Botrè F. A fast gas chromatography/mass spectrometry method for the determination of stimulants and narcotics in urine. Rapid Commun Mass Spectrom. 2010;24(10):1475–1480. doi: 10.1002/rcm.4542. [DOI] [PubMed] [Google Scholar]
- 11.Alaranta A, Alaranta H, Patja K, Palmu P, Prättälä R, Martelin T, Helenius I. Snuff use and smoking in Finnish Olympic athletes. Int J Sports Med. 2006;27:581–586. doi: 10.1055/s-2005-865826. [DOI] [PubMed] [Google Scholar]
- 12.Martinsen M, Sundgot-Borgen J. Adolescent elite athletes’ cigarette smoking, use of snus, and alcohol. Scand J Med Sci Sports. 2014;24(2):439–446. doi: 10.1111/j.1600-0838.2012.01505.x. [DOI] [PubMed] [Google Scholar]
- 13.Hayward G, Gaborini L, Sims D, Schumacher YO, Millet GP, Rhumorbarbe D, Coquet R, Robinson N. The athletic characteristics of Olympic sports to assist anti-doping strategies. Drug Test Anal. 2022;14(9):1599–1613. doi: 10.1002/dta.3329. [DOI] [PubMed] [Google Scholar]
- 14.McDuff D, Stull T, Castaldelli-Maia JM, Hitchcock ME, Hainline B, Reardon CL. Recreational and ergogenic substance use and substance use disorders in elite athletes: a narrative review. Br J Sports Med. 2019;53:754–760. doi: 10.1136/bjsports-2019-100669. [DOI] [PubMed] [Google Scholar]
- 15.Keegan M. The drug that is swamping football: Sportsmail’s investigation reveals use of banned stimulant ‘snus’ prevalent in the sport… with some players using drug during matches. Daily Mirror UK. https://www.dailymail.co.uk/sport/football/article-5559923/THE-DRUG-SWAMPING-FOOTBALL-Sportsmail-investigation-reveals-use-banned-stimulant-snus.html. Accessed 19 Sept 2022.
- 16.Kasper AM, Close GL. Practitioner observations of oral nicotine use in elite sport: You snus you lose. Eur J Sport Sci. 2021;21(12):1693–1698. doi: 10.1080/17461391.2020.1859621. [DOI] [PubMed] [Google Scholar]
- 17.Silvette H, Hoff EC, Larson PS, Haag HB. The actions of nicotine on central nervous system functions. Pharmacol Rev. 1962;14:137–173. [PubMed] [Google Scholar]
- 18.Jamner LD, Girdler SS, Shapiro D, Jarvik ME. Pain inhibition, nicotine, and gender. Exp Clin Psychopharmacol. 1998;6(1):96–106. doi: 10.1037/1064-1297.6.1.96. [DOI] [PubMed] [Google Scholar]
- 19.LaRowe LR, Ditre JW. Pain, nicotine, and tobacco smoking: current state of the science. Pain. 2020;161(8):1688–1693. doi: 10.1097/j.pain.0000000000001874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zandonai T, Chiamulera C. The importance of nicotine use among winter sports athletes, especially in skiers. J Sci Med Sport. 2019;22(10):1072. doi: 10.1016/j.jsams.2019.05.022. [DOI] [PubMed] [Google Scholar]
- 21.Gossin M, Gmel G, Studer J, Saubade M, Clair C. The association between type and intensity of sport and tobacco or nicotine use—a cross-sectional study among young Swiss men. Int J Environ Res Public Health. 2020;17(22):8299. doi: 10.3390/ijerph17228299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mattila VM, Raisamo S, Pihlajamäki H, Mäntysaari M, Rimpelä A. Sports activity and the use of cigarettes and snus among young males in Finland in 1999–2010. BMC Public Health. 2012;12(1):1–7. doi: 10.1186/1471-2458-12-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Waddington I, Malcolm D, Roderick M, Naik R. Drug use in English professional football. Br J Sports Med. 2005;39(4):e18. doi: 10.1136/bjsm.2004.012468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morente-Sánchez J, Zandonai T, Zabala DM. Attitudes, beliefs and knowledge related to doping in different categories of football players. J Sci Med Sport. 2019;22(9):981–986. doi: 10.1016/j.jsams.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization . WHO global report on trends in prevalence of tobacco smoking 2000–2025. 4. Geneva: World Health Organization; 2021. [Google Scholar]
- 26.National Institute on Drugs Abuse (NIDA). Tobacco, Nicotine, and E-Cigarettes Research Report. https://nida.nih.gov/publications/research-reports/tobacco-nicotine-e-cigarettes/introduction. Accessed 19 Sept 2022.
- 27.Abrams DB, Glasser AM, Villanti AC, Pearson JL, Rose S, Niaura RS. Managing nicotine without smoke to save lives now: evidence for harm minimization. Prev Med. 2018;117:88–97. doi: 10.1016/j.ypmed.2018.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beaglehole R, Bates C, Youdan B, Bonita R. Nicotine without smoke: fighting the tobacco epidemic with harm reduction. Lancet. 2019;394(10200):718–720. doi: 10.1016/S0140-6736(19)31884-7. [DOI] [PubMed] [Google Scholar]
- 29.Istituto Superiore di Sanità (ISS). Comunicato Stampa N°39/2022-Fumo: in Italia circa 800mila fumatori in più rispetto al 2019. Triplicato il consumo di sigarette a tabacco riscaldato. https://www.iss.it/web/guest/primo-piano/-/asset_publisher/3f4alMwzN1Z7/content/id/7146126. Accessed 19 Sept 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.