Abstract
Upon the COVID-19 pandemic onset in Ireland, cancer service disruptions occurred due to prioritisation of COVID-19 related care, redeployment of staff, initial pausing of screening, diagnostic, medical and surgical oncology procedures, staff shortages due to COVID-19 infection and impacts on the physical and mental health of cancer healthcare workers. This was coupled with reluctance among people with symptoms suspicious for cancer to attend for clinical evaluation, due to concerns of contracting the virus. This was further compounded by a cyber-attack on national health service IT systems on May 14th 2021. The Irish Cancer Society, a national cancer charity with a role in advocacy, research and patient supports, convened a multi-disciplinary stakeholder group (COVID-19 and Cancer Working Group) to reflect on and understand the impact of the pandemic on cancer patients and services in Ireland, and discuss potential mitigation strategies. Perspectives on experiences were gathered across domains including timeliness of data acquisition and its conversion into intelligence, and the resourcing of cancer care to address cancer service impacts. The group highlighted aspects for future research to understand the long-term pandemic impact on cancer outcomes, while also highlighting potential strategies to support cancer services, build resilience and address delayed diagnosis. Additional measures include the need for cancer workforce recruitment and retention, increased mental health supports for both patients and oncology professionals, improvements to public health messaging, a near real-time multimodal national cancer database, and robust digital and physical infrastructure to mitigate impacts of the current pandemic and future challenges to cancer care systems.
Keywords: COVID-19, Cancer care, Healthcare, Ireland
1. Introduction
The first COVID-19 case on the island of Ireland was reported on 26th February 2020 [1]. In the Republic of Ireland, significant public health measures and restrictions were implemented in March 2020 in order to mitigate the impact of the pandemic. These included prioritisation of COVID-19 care, redeployment of staff, initial pausing of screening, diagnostic, medical and surgical oncology procedures, staff shortages due to COVID-19 infection, which collectively hampered cancer-related care, including screening [2], [3], [4], [5]. This was coupled with reluctance among people with symptoms suspicious for cancer to attend for clinical evaluation, due to their concerns of contracting the virus. The impact of the pandemic waves was further exacerbated by a system-wide cyber-attack on national health IT systems on May 14th 2021 [6], [7].
By October 2022, the Republic of Ireland had recorded almost 1.7 million PCR confirmed cases, nearly 8000 COVID-related deaths, and over 7.9 million vaccine doses administered [8], [9]. The novel evolution of potential new COVID-19 variants suggest that COVID-19 infection may remain a significant health challenge for the foreseeable future.
Though much progress has yet to be made, cancer survival statistics have shown improvements nationally in the last decade, such as a 15 % reduction in premature cancer deaths [10]. These developments have been driven by diverse factors including national cancer strategies, national screening programmes, centralisation of treatment expertise, multidisciplinary improvements in treatment and care and translation of research to clinical practice. The incidence of cancer nationally is projected to double between 2015 and 2045, compounding the impact of the pandemic on cancer care [11], [10]. The Irish Cancer Society (www.irishcancersociety.ie), a major national cancer charity, convened a multi-disciplinary stakeholder group (COVID-19 and Cancer Working Group) to reflect on and understand the impact of the pandemic on cancer services in Ireland. Given that public health measures and healthcare services in Northern Ireland are under a separate jurisdiction, this paper focused on the Republic of Ireland. The group also discussed measures to build greater resilience in patient care pathways to mitigate the impact of the pandemic and other disruptions to cancer care. The group also sought testimonies from patient advocates and healthcare workers to illustrate the personal impact of this period.
1.1. The COVID-19 pandemic and cancer patients
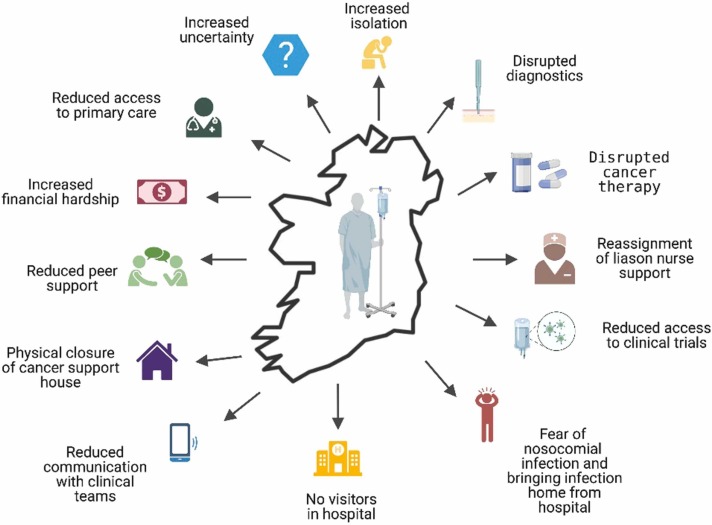
The extensive short and long-term impacts of the COVID-19 pandemic on patients with cancer have yet to be fully determined. A snapshot and insight into the individual experiences and perspectives of those directly affected by both cancer and COVID-19 is provided in Box 1 and Fig. 1. Though research continues to examine the impact [12], more studies are warranted to determine and quantify the long-term physical, social, and psychological impact of key factors including those highlighted in Fig. 1.
Box 1. Testimonies sought from two patients providing their insight into the impact of the COVID-19 pandemic.
Testimony from a patient with early stage breast cancer.
“I was initially diagnosed with early-stage breast cancer just before the pandemic. COVID-19 related restructuring meant that I had surgery in a private hospital and follow-up in the referring public hospital. However, it was difficult to provide seamless supportive care between two hospitals, one of which was contracted to provide a service to the other for a finite period of time and the infrastructures between the two are not integrated. Therefore, every interaction was more complex and layered with interruptions across every stage. One such example was challenges around post-surgical review. When it came to complications with wound healing and referrals to community services, there were no home visits from public health nurses which resulted in acutely unwell patients having to travel to local primary care centres or attend hospital for dressings and wound reviews. In my case, this led to a delay in commencement of chemotherapy due to these unresolved post-operative complications.
When chemotherapy started, there was a focus on minimising contact interactions with acute hospitals, leading to fewer opportunities for education on treatments and their side effects. I experienced long delays in chemotherapy due to the change in capacity on the day-ward as a result of social distancing. There was nowhere to go during these delays as all rest areas were closed. This experience was compounded by delays in admission to specialist units due to constant changes in COVID-19 protocols and the need to isolate while clarification was sought on access to treatment for chemotherapy complications. Subsequent adjuvant radiotherapy was noteworthy for delays in appointments due to staff absences and an increase in remote review appointments. At present, my treatment is completed but I am anxious to have reconstructive surgery to move beyond cancer. The usual 2 years wait time for this has now increased to at least 4 years, further delaying my recovery.”
Testimony from a patient with advanced stage breast cancer patient.
"I was diagnosed with primary breast cancer in 2014. I saw my family doctor on a Monday, had biopsies on a Thursday and was given a hormone-positive breast cancer diagnosis a week later. I had never felt healthier, so it was a huge shock. I was working as a Paediatric Nurse, so I had faith in the system. My husband and I knew we had a rough road ahead, but it helped that we were being looked after by good people. My metastatic diagnosis came in 2018 after a long process of scans, lung surgery and multidisciplinary decisions re my plan of care. I certainly didn’t feel lucky at the time, but had I known that we were facing into a pandemic within two years I may have been more appreciative of receiving a diagnosis. At least this way we had a plan for my cancer unlike many patients throughout the pandemic who lived in fear of cancer ripping through their bodies due to delayed diagnostics. My diagnosis, whilst grim, has treatment options and the chance of good quality of life for some years. Once I eventually came to terms with having a slim chance of growing old, I learnt to appreciate fully the life I have now.
The arrival of COVID-19 created panic for cancer patients. I feel like I have been dodging bullets for the last two years, knowing my treatment was essential but making me vulnerable to the detrimental effects of the virus. Thankfully, my husband was able to work from home and our 3 kids adapted amazingly to lockdown so being at home felt safe. Bigger challenges came when lockdowns were lifted, and the kids needed to return to school not just for academic reasons but for their mental wellbeing. It was hard on them knowing the damage COVID-19 could do if brought home. No child should ever have to carry that burden. Our first COVID-19 scare was the hardest as it was our youngest who was only 8 years old at the time. He was petrified and the hardest thing for me was not being able to hug him when he needed it most. Thankfully, that time his test was negative so we were able to hug him again 48 h later.
Radiology and radiotherapy access was taken for granted before the complications of the pandemic. I had a course of stereotactic radiotherapy to my rib just before COVID-19 emerged. Months later pain during a “star jump” on a trampoline stopped me in my tracks and the fear that it was likely due to progression was nearly as debilitating as the injury. Up to that I had been delighted with myself doing my exercise programme and bouncing on my trampoline. In hindsight, probably not the best choices of exercise for me but exercise options were limited during lockdown. Knowing what to report or worry about with metastatic cancer can be hard and even harder during a pandemic. Many oncology liaison nurses were redeployed, and staff shortage meant opportunities to discuss concerns were few and far between. Consultant appointments were sometimes over the phone or online. Months later, progression was confirmed so my medications were changed, and bone infusions were commenced to help strengthen my bones due to bone metastasis. Throughout the pandemic I changed medications twice. Over the two years, I experienced scan and multidisciplinary decision delays. My treatments had to be postponed a couple of times while waiting for a viral test result due to being a close contact. This increased stress levels and knocked my confidence of being in safe hands at times until at least vaccinations brought some level of security. Thankfully, I have managed so far to avoid catching COVID-19 and my online mindfulness classes through community cancer support services kept me sane throughout the pandemic. Despite living with cancer, I, like any other mum/wife, still have an active role in running the household, so the threat of COVID-19 wiping me out in a matter of weeks was unimaginable. I cannot control what is written in the stars for me, but I would like to think that the course of my illness will stretch as far as medicine can take me and when the time comes, we will know we did everything we could. No regrets, no unspoken words, and an appreciation that life and time are precious gifts."
* Testimonies were directly sought from two patient advocates to reflect on the individual pandemic impact.
Fig. 1.
Summary illustration of the working group discussions of the impact of the pandemic on new and existing cancer patients.
1.2. The COVID-19 pandemic and cancer services – from primary to palliative care
1.2.1. Perspectives from primary care and primary prevention
Primary care operates across the cancer continuum from prevention to end-of-life care. It played a key role in the prevention, triage, diagnosis and management of patients with COVID-19 in the community [13]. General Practitioners (GPs) were involved in the identification of patients classed as clinically vulnerable, as well as delivering vaccinations. Similar to other countries, the pandemic necessitated a rapid transition to remote consultations in primary care (telephone, email, and video consultations) [14], [15], [16]. This change in care delivery had a particular impact on end-of-life care for people in the community. Patient hesitancy (due to fear of contracting COVID-19) when it came to attending clinical appointments in-person, affected the care of chronic conditions including cancer [17], [18], [19], [20].
Impacts on wider determinants of cancer have also been observed during the pandemic, with negative impacts on health behaviours [21], [22]. The Healthy Ireland Survey 2021 found that 51 % of respondents reported that they drank more, smoked more, had gained weight or reported a worsening in their mental health over the course of the COVID-19 pandemic. Furthermore, 30.5 % of smokers and 22.2 % of drinkers reported increased consumption of cigarettes/alcohol in the Central Statistics Office Social Impact Survey collected during the first implementation period of restrictions [23]. Additional understanding of the distribution of these determinants across the population will be important in planning for and managing the burden of cancer into the future.
1.3. Perspectives from diagnostics including pathology
Following on from publications from the UK experience of the negative impact of COVID-19 on cancer services and cancer patients, two collaborative reports led by the Faculty of Pathology at the Royal College of Physicians of Ireland (RCPI) were published in December 2020 and 2021 respectively and aimed to understand more completely the nature of the pandemic impact on cancer-related services [24], [25]. The reports noted that the reduction in cancer services activity, affecting presentation, diagnosis, and treatment were most marked upon the first wave of the pandemic, as compared with the same months in 2019 [24]. For example, the second report found that in 2020, diagnostic biopsies were 86 % of 2019 levels, gut endoscopic biopsies were 80 % of 2019 and non-gynaecological cytological evaluations were 80 % of 2019 levels. These reductions were attributed to the comprehensive COVID-19 risk-reducing measures that were introduced to manage the novel viral pathogen, involving a pausing of many diagnostic procedures, coupled with symptomatic patient hesitancy to attend for clinical evaluation. Variable recovery was identified from June 2020 onwards with initial data from January to March 2021, although incomplete at the time of publication of the RCPI reports, suggesting continued resilience and recovery into 2021. As noted by the reports, engagement across many services including acute services, primary care, the voluntary and private sector along with cancer support services, was key in this recovery [24], [25]. Both reports highlighted how the absence of near real-time, complete data (as had been established for COVID-19 monitoring) and integrated electronic health records across the health care system presented challenges to compiling those reports, affecting the ability to obtain a holistic comprehensive view of overall cancer related activity in Ireland at the time. Despite this, the reports demonstrated the benefits of collating such data and provides additional rationale for how such a comprehensive cancer data network, encompassing both public and private healthcare systems, would be hugely beneficial for dealing with the healthcare challenges that a pandemic or other disruptions to a health system can lead to.
1.4. Perspectives from cancer screening
In Ireland, the National Screening Service provides population-based colorectal, breast and cervical cancer screening. Similar to most international cancer screening programmes, all of these services were paused following the pandemic onset. Screening staff were redeployed to support the continuation of symptomatic cancer services and to support the national public health response to COVID-19. This pause led to a reduction in screening across programmes in the early stages of the pandemic period [26]. Upon resumption, screening numbers in January to September 2021 demonstrated the phased return of cancer screening to pre-pandemic levels, with a catch up programme in cervical cancer screening only. In Ireland, screening accounts for just under 7 % of all cancers detected annually; thus delays in screening will have a small but defined impact on cancer detection rates.
1.5. Perspectives from surgical oncology
In the first three months of the COVID-19 pandemic, an estimated 28 million surgical procedures were delayed worldwide [27]. In Ireland, there were reductions in certain surgical oncology procedures of up to 39 % [27], [28]. The initial marked reductions in activities observed following the onset of the first pandemic wave however were not replicated during the subsequent 2nd wave. The establishment of COVID-19 protected pathways at separate elective hospital sites was essential for continuing to deliver standard-of-care treatment to surgical oncology patients [29], [30]. The takeover of private hospitals by the State for 6 months at the onset of the pandemic to secure additional capacity also allowed separation of COVID-19 and non-COVID-19 related care, including cancer surgery. This was also likely coupled with behavioural changes among patients, who may have presented for surgery more readily as knowledge and information around COVID-19 accumulated and the healthcare system adapted to the challenges of the pandemic. The European experience has been that even in the most challenged circumstances, surgical oncology treatment can be delivered while minimising risks [31], [32], [33]. For avoiding future disruptions within the surgical oncology setting, improved operational infrastructure, along with protected physical infrastructure (e.g., theatre access, increased beds) with the necessary supporting oncology staff, will be critical to maintaining scheduled surgical oncology activity. The lack of harmonised diagnostic platforms and electronic patient records in Ireland limited the potential of inter-hospital transfer of care to maximise surgical resource availability. Furthermore, the redeployment of theatre staff away from essential surgical oncology care and time-critical surgery must be avoided, and undergraduate and postgraduate training in surgical oncology (and training in other specialties) must be maintained.
1.6. Perspectives from medical oncology
Within the medical oncology setting, concerns about the vulnerability of cancer patients in healthcare environments led to de-escalation or deferral in chemotherapy treatments, in keeping with international guidelines [34], [35]. Screening for COVID-19 was instigated prior to attendance for outpatient chemotherapy [36]. As with primary care, clinic visits were supplemented with telemedicine, and infusional chemotherapy units in two centres were moved away from COVID-19 treating facilities [37]. A weekly call with the National Cancer Control Programme (NCCP) among medical oncologists nationally facilitated information sharing [38]. Such measures were necessary, particularly as studies in Ireland [39], and elsewhere [40], demonstrated increased mortality in patients with cancer who developed COVID-19 infection.
1.7. Perspectives from radiation oncology
Radiotherapy services in Ireland also suffered an abrupt impact following the onset of the pandemic. Shorter, more accelerated fractionation and delivery schedules were rapidly adopted to minimise the number of treatment visits for individual patients [41]. Guidance documents published by the NCCP provided an initial framework for services in November 2021, and subsequently through a risk-adapted strategy based on treatment capacity in February 2022. Prioritisation of service provision shifted rapidly to focus on the delivery of radiation to patients treated with curative intent and those in need of emergency treatment [42]. International tumour site-specific guidelines were rapidly published with consensus recommendations on how to modify schedules and prioritise treatment delivery in the COVID-19 era [43]. Data on cancer-specific impacts in Ireland are lacking. However, a UK study showed that radiotherapy treatments for prostate and non-melanoma skin cancer fell but radiotherapy courses for bladder, oesophageal and bowel cancers increased markedly between April and June 2020 compared to the same time period in 2019, likely to compensate for a lack of surgical capacity due to the pandemic [44]. The impact of the COVID-19 pandemic on radiotherapy was also compounded by the cyber-attack on the national health IT systems on May 14th 2021, which resulted in an immediate need to shut down all health IT systems, resulting in the instant loss of radiation services across many national specialist centres. This unexpected event had a profound impact on service provision; however, through rapid collaboration with private sector providers, the impact of treatment gaps and delays on affected patients was minimised [45].
1.8. Perspectives from palliative care
The pandemic had a seismic impact on the care of the dying and on the traditional family and community response to death in Ireland. Infection control measures in hospital settings led to reduced visiting and increased patient mental and physical isolation. For palliative care physicians and teams, normal practice was significantly altered. Advanced communication which underpins optimal patient assessments was impeded by infection control practices and the utilisation of personal protective equipment (PPE). In the hospital setting, palliative care teams played a vital role in training and supporting non-specialists in symptom management and end-of-life care through guideline and decision-tool development [46], [47], [48]. Notably, care shifted from inpatient palliative units to the hospital and community setting, as patients were afraid of hospital-acquired (nosocomial) COVID-19 infection and of restricted hospital visiting [46], [47]. Virtual technology use increased to 83.7 % of visits from a pre-pandemic level of 21.6 % [46]. Traditionally in Ireland deaths are a rallying cry to a community to provide support and sympathy, however public health restrictions dramatically reduced funeral observances, magnifying the grief experienced by family members [49]. The impact of these circumstances is being assessed in a national bereavement survey [50].
1.9. Perspectives from community cancer support services
In Ireland, a network of cancer counselling and support centres has been established nationally to provide community-based emotional, psychological, and practical support to people with cancer and their families, free of charge [51], [52]. The critical role that community cancer support centres offer in supporting cancer survivor needs has been well documented [52]. Due to the pandemic all centres ceased in-person visits for at least 16 months [53], [54], [55], [56], compounding the distress experienced. This also compounded stressors due to disruptions of services, reduced social support, and fear of contracting the virus [57], [58]. Community support services adapted with the provision of virtual access through webinars, support groups, exercise programmes, guided meditation, stress management and self-management programmes and one-to-one counselling using online platforms. The Irish Cancer Society facilitated the establishment of ‘Together 4 Cancer Concern’, a virtual support network for patients [59]. These community cancer support centres are usually supported by local fundraising efforts. Because these could not occur, there was rapid decline in income in some centres [54], [55], [56], leading to reliance on pandemic associated national financial governmental supports.
1.10. Perspectives from healthcare workers
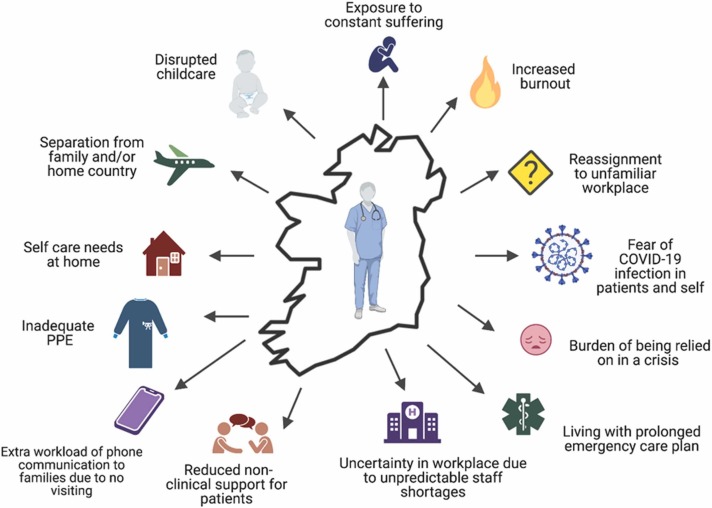
At a European level, the impact of the pandemic on cancer healthcare workers has been substantial, with a recent study indicating that 4 out of 10 cancer professionals experienced burnout, while 3 out of 10 had symptoms of clinical depression [60]. Fig. 2 summarises, from an Irish perspective, challenges discussed that were experienced by healthcare workers (HCW) that require further research.
Fig. 2.
Summary illustration of the working group discussions of the impact of the pandemic on healthcare workers.
A testimony on the pandemic impact from the perspective of a HCW was sought and is in Box 2. Limited studies have been conducted within the Irish setting. One study surveyed 472 HCWs from the Southeast of Ireland and found that 42.6 % of respondents had positive screens for depression and 45.1 % had positive screens for anxiety and stress [61]. To mitigate these impacts, the study recommended involvement of HCWs in decision making, timely communication, access to rest areas, improved staffing levels, staggered rosters, access to on-site mental health supports, more frequent multidisciplinary training sessions, and access to childcare facilities [61]. While this study of HCWs in Ireland assessed the experience of doctors and nurses, these issues extended to other frontline workers. Foley et al. reported similar findings from a survey of radiographers working in Ireland through the pandemic, with 40 % of responding radiographers reporting levels of burnout and 30 % contemplating a career change [62]. Additional studies on the long-term multifaceted impact of the pandemic on HCWs is needed including on the impact on international graduate HCW who constitute 21.6 % of registered doctors in Ireland [63], [64]. Further, during the first wave the majority of students affiliated with pre-registration healthcare programmes were removed from placements with the exception of intern student nurses and midwives. This led to logistical challenges in reorganising clinical placements. Whilst key stakeholders discussed the logistics of fast tracking the registration of nurses and doctors, this did not happen.
Box 2. Testimony from an oncology liaison nurse providing their insight into the impact of the COVID-19 pandemic.
Testimony from an oncology liaison nurse.
“Cancer patients isolated themselves from family and friends and were fearful of contracting the virus. The upset was evident and redeployment of oncology nurse specialists exacerbated this distress. Patients were anxious about attending the hospital for their chemotherapy or imaging appointments. Many patients on systemic anti-cancer therapy have stopped working unless their workplace facilitates working from home. I have seen a significant increase in financial worries among my patients. Cancer patients have missed out on so much in their social and personal lives over the past two years due to the anxiety of becoming infected.
As nurses, we have always been taught about the importance of nonverbal communication- a reassuring smile or gentle touch to make a patient feel at ease. During the pandemic, we had to physically distance ourselves from our patients, minimise the time we spent with them, and wear full PPE. As an oncology liaison nurse specialist, I have developed relationships with my patients and their families over several years, therefore it was incredibly difficult to deliver bad news to patients while maintaining a distance of 2 m and not being able to reach out and hold their hand. I hope that I never again have to wear full PPE with a dying patient, standing in place of a family member who could not be there due to visiting restrictions. It saddens me that patients have passed through the cancer services over the past two years and have never seen a staff member smile. Visiting restrictions meant patients attended appointments alone. The number of phone calls oncology nurses received each day increased hugely as family members who could not attend appointments or visit inpatients sought information. Educating patients regarding their systemic anti-cancer treatment was now done over the phone rather than in person. Personally, being a nurse in an acute hospital during the COVID-19 pandemic meant that when my uncle was diagnosed with relapsed acute myeloid leukaemia in April 2021, I could not be there for him as much as I felt I should have been due to the fear that I was a potential risk to him. During the highest recorded COVID cases per day in January 2022, my family and I were privileged that we could nurse him at home. His final wish was that he would not die in a hospital or hospice where visiting restrictions meant he could not have all his loved ones with him; not every cancer patient was as fortunate.
On a positive note, healthcare workers’ ability to come together and initiate change in a time of crisis was evident when changes, which previously may have taken months to years to initiate, happened overnight. We embraced telemedicine and many consults with patients took place through virtual clinics. Temporary walls were built, protecting the oncology unit from the rest of the hospital so that the chemotherapy day-ward could continue to operate safely.
In the hospital where I work, the first Acute Oncology Service (AOS) in Ireland was established in response to the COVID-19 pandemic. AOS has now been integrated as an essential part of our service and 26 Nurse Specialist posts have since been appointed throughout the country in all hospitals where cancer patients are cared for.
As the COVID-19 pandemic eases, oncology nurses are seeing an increase in newly diagnosed cancer patients and patients who have being diagnosed with more advanced stage cancers due to delays in attending their GP or cancellation of routine screening. The biggest challenge faced by cancer nurses now is shortages in nursing staff. As society continues to open, we must continue to act as advocates for our high risk, vulnerable patients so that they do not feel that they are being left behind.”
*A testimony was directly sought from an oncology liaison nurse to reflect on the individual pandemic impact.
1.11. Perspectives from cancer clinical trials and cancer research
Cancer Trials Ireland (www.cancertrials.ie) is Ireland’s national clinical trials cooperative group and coordinates activity in 17 cancer clinical trial units across the country. A detailed overview of the pandemic’s impact reported a 54 % decline in clinical trial accrual, including a 90 % reduction in accrual to radiotherapy trials which persisted for over 18 months [65]. The transition to telehealth was also adopted within the clinical trial setting for remote clinic visits and monitoring. In response to the pandemic, flexibility in trial conduct, staff recruitment and retention, the need for harmonisation of processes, and research staff support in the context of remote working, were identified as priorities at the first National Cancer Retreat held virtually in May 2021 [66] and in hybrid form in May 2022 [67]. Furthermore, observational research trials and biobanking studies for translational research were impacted, as elective operations and patient clinics were curtailed. A review by the Health Research Board of their grant holders found that 90 % of all active grants reviewed reported an impact due to COVID-19 restrictions or related reasons. Among the grant holders, 61 % reported reduced access to facilities, 29 % reported a reduction in data acquisition, 16 % highlighted staff reassignments and 12 % reported recruitment issues, as the most frequently reported pandemic impacts [68]. Though it will be more difficult to quantify, the impact on laboratory-based research through the closure of laboratories, and impact on innovation and knowledge-sharing must be considered due to the lack of in-person working environment and the absence of national and international in-person research meetings [69]. However, it has also been acknowledged that in the post-pandemic era, this represents a time to re-imagine research endeavours [70].
1.12. Perspectives from cancer registration
The National Cancer Registry Ireland (NCRI) collects cancer surveillance information to enable the planning and management of cancer services, the overview of cancer control activities and the promotion and facilitation of cancer research in Ireland. The impact of the pandemic was predominantly observed on the completion of cancer case registration, disrupted due to the pivot to remote working. Difficulty in accessing data remotely was encountered, as well as a reduction in personnel, which was mirrored in cancer registries across Europe [71]. Multiple international cancer registries have reported a reduction in the number of cancer notifications in 2020 [71], [72], [73], [74], [75]. At the end of 2022, the NCRI undertook an updated assessment of the impact of the pandemic on cancer registration in Ireland [76]. Comparing notifications for cancers diagnosed in 2020, received by October 2022, to those expected based on historic trends, it was estimated that there was a shortfall of 10 % of cases [76]. A further analysis was undertaken by the NCRI on microscopically-verified cancers diagnosed in 2020 and this suggested a reduction of 11 %. In Northern Ireland, data from the Northern Ireland Cancer Registry found that during the April-December period when COVID-19 was present, the number of cases of cancer diagnosed decreased by 18.2% (1,980 patients) from 10,861 per year in 2018 - 2019 to 8,881 in 2020. This despite a previous year on year increase in cases as the population aged [77]. Ongoing analyses will continue to monitor this impact.
2. Future directions
The working group perspectives outlined in this discussion paper offer a snapshot into the multi-layered impacts of the COVID-19 pandemic on different aspects of cancer care in Ireland. Learnings from the pandemic offer opportunities for knowledge generation and innovation in delivering the best possible care and research for our patients. To reduce the impact of future pandemics and disruptions to national and community cancer services, the stakeholder group discussed mitigation strategies, summarised in Fig. 3.
Fig. 3.
Strategies discussed by the working group for mitigating the impact of future disruption to national and community cancer services.
As reflected in Fig. 3, suggested strategies for strengthening services to help reduce the impact of COVID-19 disruption, include optimising opportunities for enhanced innovation, providing data and intelligence in near real-time, increasing investment in cancer services, strategies to protect public health (particularly relating to cancer prevention), and provision of adequate infrastructure. These are concordant with recommendations from professional societies and organisations [78] and reflect the threefold increased risk of pandemics in the future [79]. Additional support for digital infrastructure was recognised across many of the multi-disciplinary perspectives, including enhanced cybersecurity to mitigate further cyber-attacks, harmonised diagnostic services between and within public and private hospitals to improve inter-hospital connectivity and integration of multidisciplinary patient care. One such specific example is the COVID-19 national real-time databases which could be a model for a comprehensive national cancer database that should not only include new cancer diagnoses but could integrate data for primary care, diagnostics, pathology, medical oncology, surgery, radiology and cancer recurrence, cancer genetics and molecular tumour classification. To track cancer-related activity and improve cancer services, the availability of high-quality data covering all cancer types from all relevant sources including public, private, and voluntary health care systems in as close to real-time as possible, is imperative. This recommendation, made in the Faculty of Pathology, RCPI-led report would be facilitated by implementation of the ‘eHealth Strategy for Ireland’ [10]. Such an integrated database could monitor a patient’s journey across the cancer continuum from symptom onset to survivorship care, providing an integrated data ecosystem for cancer surveillance in near real-time and in the identification of the impacts of newer treatments for guiding clinical trial activity and survivorship needs.
This stakeholder discussion provided an insight into the impact of the pandemic on both patients and healthcare workers. As outlined by the NCRI, the number of cancer patients and survivors is projected to increase [11], [10] and measures should be adopted to recruit, support and retain oncology HCWs to address this increase. Suggested strategies for strengthening the cancer workforce include enhanced flexible support for retention of EU and non-EU HCWs (Fig. 3).
In the past two years, major advances have been made in our understanding of COVID-19 [80], [81]. While vaccination schemes have reduced the impact of the illness, patients with cancer remain vulnerable, with higher hospitalisation and mortality rates [82]. Services remain susceptible to continued disruption [83] and concerns persist about delayed cancer diagnosis [84]. The stakeholder group sought: to provide a platform for communicating across traditional healthcare divides, identify novel sources of insight and data that can help to further examine the impact, highlight challenges such as staff, resourcing and data acquisition, integrate learning from international experience, and identify new routes with which to give near real-time insight to inform potential mitigation strategies such as health policy and resourcing. Even in well-resourced and coordinated health systems, the existing impact of COVID-19 will be felt for many years. This gives an urgency to improve stakeholder communications globally and the development of dynamic real-time, data-informed mitigations into specific parts of the health system, to help ensure that the worst impacts, some of which may yet be modifiable, are less than they might otherwise be [85]. A snapshot into the impact on cancer services in Ireland is provided in this discussion paper, however acknowledgment must be given to the many other aspects of cancer services and care not discussed here that were also impacted by the pandemic, including cancer rehabilitation, nutrition, physiotherapy and psycho-oncology services, all of which contribute to the modern cancer continuum. While pandemics expose vulnerabilities, they also represent opportunities to accelerate innovation, and given the continued onset of the pandemic, additional efforts now need to evolve into a longer-term strategy of mitigation and implementation. Future studies examining the longer-term impact of continued waves will provide knowledge to help mitigate the impact on cancer patients and services and reduce the impact of future pandemics on cancer services, and most importantly on cancer patients.
Ethical approval
No ethical approval was required for conducting this work.
Funding statement
This work is supported by the Irish Cancer Society through the Research Grant CMP21BEMU. The opinions, findings and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the view of the funders. MM is supported by funding provided by the Health Research Board.
CRediT authorship contribution statement
All authors contributed to the writing of the manuscript. SOR and HKC prepared the manuscript figures. All authors reviewed the manuscript, Concept and design: SOR, HKC, KB, MM, Generation, collection, and assembly of manuscript: SOR, HKC, DM, LB, TMC, ROC, CK, SL, JF, MC, PF, KF, VM, MJOL, SG, LY, EMCA, JH, AG, ML, PK, SS, TMCW, MH, KR, PK, AM, MC, HPR, PR, PW, PT, MZ, KB, MM, Manuscript writing: SOR, HKC, DM, LB, TMC, ROC, CK, SL, JF, MC, PF, KF, VM, MJOL, SG, LY, EMCA, JH, AG, ML, PK, SS, TMCW, MH, KR, PK, AM, MC, HPR, PR, PW, PT, MZ, KB, MM, Final approval of manuscript: SOR, HKC, DM, LB, TMC, ROC, CK, SL, JF, MC, PF, KF, VM, MJOL, SG, LY, EMCA, JH, AG, ML, PK, SS, TMCW, MH, KR, PK, AM, MC, HPR, PR, PW, PT, MZ, KB, MM.
Disclosure/conflict of interest statement
All authors have declared that they have no conflicts of interest.
Acknowledgements
The authors would like to thank the COVID-19 and Cancer Working Group and project Advisory Group for providing valuable support for the manuscript.
References
- 1.Perumal V., Curran T., Hunter M. First case of COVID-19 in Ireland. Ulst. Med. J. 2020;89:128. [PMC free article] [PubMed] [Google Scholar]
- 2.Cazelles B., Nguyen-Van-Yen B., Champagne C., Comiskey C. Dynamics of the COVID-19 epidemic in Ireland under mitigation. BMC Infect. Dis. 2021;21:735. doi: 10.1186/s12879-021-06433-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burke S., Parker S., Fleming P., Barry S., Thomas S. Building health system resilience through policy development in response to COVID-19 in Ireland: From shock to reform. Lancet Reg. Health – Eur. 2021;9 doi: 10.1016/j.lanepe.2021.100223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kennelly B., O'Callaghan M., Coughlan D., Cullinan J., Doherty E., Glynn L., et al. The COVID-19 pandemic in Ireland: An overview of the health service and economic policy response. Health Pol. Technol. 2020;9:419–429. doi: 10.1016/j.hlpt.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Sullivan G., Jacob S., Barrett P.M., Gallagher J. Covid-19 presentation among symptomatic healthcare workers in Ireland. Occup. Med (Lond. ) 2021;71:95–98. doi: 10.1093/occmed/kqab012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Conti Cyber Attack on the HSE. Independent post incident review. Commissioned by the HSE Board in conjunction with the CEO and executive management team. Available at: 〈https://www.hse.ie/eng/services/publications/conti-attack-on-the-hse-full-report.pdf〉.
- 7.Faul C., Robinson J., Carey J., McArdle O., Ryan L., Woods R., et al. Effect of the cyberattack targeting the Irish Health System in May 2021 on Radiation Treatment at St. Luke's radiation oncology network. Adv. Radiat. Oncol. 2022;7 doi: 10.1016/j.adro.2022.100993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.COVID-19 Cumulative Infection Collaborators. Estimating global, regional, and national daily and cumulative infections with SARS-CoV-2through Nov 14 2021: a statistical analysis. Lancet 2022; 399:2351–2380. 10.1016/S0140-6736(22)00484-6. [DOI] [PMC free article] [PubMed]
- 9.www.covid19ireland-geohive.hub.arcgis.com accessed Oct 4th 2022.
- 10.https://www.gov.ie/en/publication/a89819-national-cancer-strategy-2017-2026.
- 11.CancerIncidenceProjections_NCRI_summaryreport_09042019_final.pdf.
- 12.Dhada S., Stewart D., Cheema E., Hadi M.A., Paudyal V. Cancer services during the COVID-19 pandemic: systematic review of patient's and caregiver's experiences. Cancer Manag. Res. 2021;13:5875–5887. doi: 10.2147/CMAR.S318115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haldane V., Zhang Z., Abbas R.F., Dodd W., Lau L.L., Kidd M.R., et al. National primary care responses to COVID-19: a rapid review of the literature. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-041622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murphy M., Scott L.J., Salisbury C., Turner A., Scott A., Denholm R., et al. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br. J. Gen. Pract. 2021;71:e166–e177. doi: 10.3399/BJGP.2020.0948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park S., Elliott J., Berlin A., Hamer-Hunt J., Haines A. Strengthening the UK primary care response to covid-19. Bmj. 2020;370:m3691. doi: 10.1136/bmj.m3691. [DOI] [PubMed] [Google Scholar]
- 16.Homeniuk R., Collins C. How COVID-19 has affected general practice consultations and income: general practitioner cross-sectional population survey evidence from Ireland. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-044685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bone A.E., Finucane A.M., Leniz J., Higginson I.J., Sleeman K.E. Changing patterns of mortality during the COVID-19 pandemic: Population-based modelling to understand palliative care implications. Pall Med. 2020;34:1193–1201. doi: 10.1177/0269216320944810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones D., Neal R.D., Duffy S.R.G., Scott S.E., Whitaker K.L., Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care. Lancet Oncol. 2020;21:748–750. doi: 10.1016/S1470-2045(20)30242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beran D., Aebischer Perone S., Castellsague Perolini M., Chappuis F., Chopard P., Haller D.M., et al. Beyond the virus: ensuring continuity of care for people with diabetes during COVID-19. Prim Care. Diabetes. 2021;15:16–17. doi: 10.1016/j.pcd.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nicholson E., Mc Donnell T., Conlon C., Barrett M., Cummins F., Kenny C., Mc Auliffe E. Parental hesitancy and concerns around accessing paediatric unscheduled healthcare during the COVID-19 a cross sectional survey. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17249264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Healthy Ireland Survey https://www.gov.ie/en/publication/9ef45-the-healthy-ireland-survey-2021/.
- 22.Reynolds C.M.E., Purdy J., Rodriguez L., McAvoy H. Factors associated with changes in consumption among smokers and alcohol drinkers during the COVID-19 'lockdown' period. Eur. J. Public Health. 2021;31:1084–1089. doi: 10.1093/eurpub/ckab050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Central Statistics Office Social Impact of COVID-19 Survey - CSO - Central Statistics Office
- 24.Royal College of Physicians of Ireland, Faculty of Pathology. Deploying Data Driven Intelligence to measure the impact of COVID-19 on cancer care and cancer patients. December 2020. Available from: https://rcpi-live-cdn.s3.amazonaws.com/wp-content/uploads/2021/01/Cancer-Care-and-COVID19-Report.pdf.
- 25.Royal College of Physicians of Ireland, Faculty of Pathology. Cancer care in Ireland in 2020: The impact of the COVID-19 pandemic. December 2021. Available from: https://rcpi.access.preservica.com/uncategorized/IO_ec89e5fa-3e55-471f-94eb-423b56720e8e/.; https://www.rcpi.ie/news/releases/rcpi-faculty-of-pathology-launches-new-report-on-cancer-care-during-covid-19-pandemic/.
- 26.National screening service. The road to recovery: the impact of the COVID-19 pandemic on cancer screening June 2021 update https://www.screeningservice.ie/news/news.php?idx=263.
- 27.COVIDSurg Collaborative. Delaying surgery for patients with a previous SARS-CoV-2 infection. Br J. Surg., 2020;107:e601-e602.https://doi.org/10.1002/bjs.12050. [DOI] [PMC free article] [PubMed]
- 28.Donlon N.E., Hayes C., Davern M., Bolger J.C., Irwin S.C., Butt W.T., et al. Impact of COVID-19 on the diagnosis and surgical treatment of colorectal cancer: a national perspective. Dis. Colon Rectum. 2021;64:1305–1309. doi: 10.1097/DCR.0000000000002230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maringe C., Spicer J., Morris M., Purushotham A., Nolte E., Sullivan R., et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glasbey J.C., Nepogodiev D., Simoes J.F.F., Omar O., Li E., Venn M.L., et al. Elective cancer surgery in COVID-19-free surgical pathways during the SARS-CoV-2 pandemic: an international, multicenter, comparative cohort study. J. Clin. Oncol. 2021;39:66–78. doi: 10.1200/JCO.20.01933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.STARSurg Collaborative and COVIDSurg Collaborative. Death following pulmonary complications of surgery before and during the SARS-CoV-2 pandemic. Br. J. Surg., 2021;108:1448–1464 https://doi.org/10.1093/bjs/znab336. [DOI] [PMC free article] [PubMed]
- 32.Kavanagh F.G., Callanan D., Connolly C., Brinkman D., Fitzgerald C., Elsafty N., et al. Pre-operative testing for SARS-CoV-2 and outcomes in otolaryngology surgery during the pandemic: a multi-center experience. Laryngoscope Invest. Otolaryngol. 2021;6:773–779. doi: 10.1002/lio2.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.COVIDSurg Collaborative. Head and neck cancer surgery during the COVID-19 pandemic: An international, multicenter, observational cohort study. Cancer, 2021;127:2476–2488. 〈 10.1002/cncr.33320〉. [DOI] [PubMed]
- 34.Curigliano G., Banerjee S., Cervantes A., Garassino M.C., Garrido P., Girard N., et al. Managing cancer patients during the COVID-19 pandemic: an ESMO multidisciplinary expert consensus. Ann. Oncol. 2020;31:1320–1335. doi: 10.1016/j.annonc.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.American Society of Clinical Oncology. ASCO Coronavirus Resources | ASCO.
- 36.Fitzpatrick O R.N.D., Linehan A., Coyne Z., Hennessy M., Clarke M., et al. Delivery of systemic anti-cancer therapy during the COVID-19 pandemic. Ir. J. Med Sci. 2022;191:559–562. doi: 10.1007/s11845-021-02631-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Reilly D., Carroll H., Lucas M., Sui J., Al Sendi M., McMahon D., et al. Virtual oncology clinics during the COVID-19 pandemic. Ir. J. Med Sci. 2021;190:1295–1301. doi: 10.1007/s11845-020-02489-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Cancer Control Programme https://www.hse.ie/eng/services/list/5/cancer/profinfo/covid-19.html
- 39.Linehan A., Fitzpatrick O., Cowzer D., Hennessy M.A., Coyne Z.L., Nolan A., et al. COVID-19-related mortality in cancer patients in an Irish setting. Ir. J. Med Sci. 2022;191:2013–2018. doi: 10.1007/s11845-01-02815-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kuderer N.M., Choueiri T.K., Shah D.P., Shyr Y., Rubinstein S.M., Rivera D.R., et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395:1907–1918. doi: 10.1016/S0140-6736(20)31187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murray Brunt A., Haviland J.S., Wheatley D.A., Sydenham M.A., Alhasso A., Bloomfield D.J., et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5-year efficacy and late normal tissue effects results from a multicentre, non-inferiority, randomised, phase 3 trial. Lancet. 2020;395:1613–1626. doi: 10.1016/S0140-6736(20)30932-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Cancer Control Programme cd19-096-nccp-advice-on-rt-capacity-escalation-plan.pdf (hse.ie).
- 43.American Society of Therapeutic Radiation Oncology. COVID-19 Recommendations and Information - American Society for Radiation Oncology (ASTRO) - American Society for Radiation Oncology (ASTRO).
- 44.Spencer K., Jones C.M., Girdler R., Roe C., Sharpe M., Lawton S., et al. The impact of the COVID-19 pandemic on radiotherapy services in England, UK: a population-based study. Lancet Oncol. 2021;22:309–320. doi: 10.1016/S1470-2045(20)30743-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Flavin A., O'Toole E., Murphy L., Ryan R., McClean B., Faul C., et al. A national cyberattack affecting radiation therapy: the Irish experience. Adv. Radiat. Oncol. 2022;7(5) doi: 10.1016/j.adro.022.100914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dunleavy L., Preston N., Bajwah S., Bradshaw A., Cripps R., Fraser L.K., et al. 'Necessity is the mother of invention': Specialist palliative care service innovation and practice change in response to COVID-19. Results from a multinational survey (CovPall) Pall Med. 2021;35:814–829. doi: 10.1177/02692163211000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oluyase A.O., Hocaoglu M., Cripps R.L., Maddocks M., Walshe C., Fraser L.K., et al. The challenges of caring for people dying From COVID-19: a multinational, Observational Study (CovPall) J. Pain. Sympt Manag. 2021;62:460–470. doi: 10.1016/j.jpainsymman.2021.01.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carroll H.K., Broderick A., McCarthy O., Kennedy M., Bambury R., Power D.G., et al. 1292P A review of in-hospital end-of-life care (EOLC) for oncology patients during the COVID-19 pandemic. Ann. Oncol. 2022;33:S1134. [Google Scholar]
- 49.O'Mahony S. Mourning our dead in the covid-19 pandemic. BMJ. 2020;369:m1649. doi: 10.1136/bmj.m1649. [DOI] [PubMed] [Google Scholar]
- 50.Irish Hospice Foundation National Bereavement Support Service Survey - Irish Hospice Foundation.
- 51.National Cancer Contol Programme living with and beyond cancer in ireland.pdf (hse.ie).
- 52.National Cancer Control Programme nccp-best-practice-guidance-2022.pdf (hse.ie).
- 53.Marie Keating Foundation 〈https://www.mariekeating.ie/cancer-information/cancer-support-services-ireland〉.
- 54.Cork ARC Cancer Support House Annual Statement 2020 Cork_ARC-Annual-Report.pdf (corkcancersupport.ie).
- 55.ARC Cancer Support Center Annual Report 2020 arc-2020-signed-financial-statements-website.pdf (arccancersupport.ie).
- 56.ARC Cancer Support Center Annual Report 20211 arc-2021-signed-financial-statements-website.pdf (arccancersupport.ie).
- 57.Massicotte V., Ivers H., Savard J. COVID-19 pandemic stressors and psychological symptoms in breast cancer patients. Curr. Oncol. 2021;28(1):294–300. doi: 10.3390/curroncol28010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Erdoğan A.P., Ekinci F., Acar Ö., Göksel G. Level of COVID-19 fear in cancer patients. East Curr. Psych. 2022;29:9. [Google Scholar]
- 59.Together 4 Cancer Concern Together 4 Cancer Concern – your support for cancer distress during coronavirus | Irish Cancer Society.
- 60.Lawler M., Crul M. Data must underpin our response to the covid-19 pandemic's disastrous impact on cancer. BMJ. 2022;376:o282. doi: 10.1136/bmj.o282. [DOI] [PubMed] [Google Scholar]
- 61.Ali S., Maguire S., Marks E., Doyle M., Sheehy C. Psychological impact of the COVID-19 pandemic on healthcare workers at acute hospital settings in the South-East of Ireland: an observational cohort multicentre study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Foley S.J., O'Loughlin A., Creedon J. Early experiences of radiographers in Ireland during the COVID-19 crisis. Insights Imaging. 2020;11:104. doi: 10.1186/s13244-020-00910-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McGinnity, F., H. Russell, I. Privalko, S. Enright. COVID-19 and non-Irish nationals in Ireland, Dublin: ESRI and Department of Children, Equality, Disability, Integration and Youth, 2020. 〈 10.26504/bkmnext404〉. [DOI]
- 64.Medical Council. medical-workforce-intelligence-report-20214.pdf (medicalcouncil.ie).
- 65.O'Reilly S., Murphy V., Mulroe E., Tucker L., Carragher F., Marron J., et al. The SARS-CoV-2 pandemic and cancer trials ireland: impact, resolution and legacy. Cancers. 2022;14:2247. doi: 10.3390/cancers14092247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cancer Trials Ireland Retreat-Report-FINAL-redacted.pdf (cancertrials.ie).
- 67.Cancer Trials Ireland 2022-Retreat-Report-FINAL.pdf (cancertrials.ie).
- 68.Personal communication Dr Teresa Maguire, Health Research Board Oct 24th 2022.
- 69.Sands T.R. Keeping your lab together in the COVID-19 era. Genome Biol. 2021;22:234. doi: 10.1186/s13059-021-02457-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kozlov M. Reinventing the NIH. Nature. 2022;605:22–24. doi: 10.1038/d41586-022-01101-7. [DOI] [PubMed] [Google Scholar]
- 71.Neamţiu L., Martos C., Giusti F., Negrão Carvalho R., Randi G., Dimitrova N., et al. Impact of the first wave of the COVID-19 pandemic on cancer registration and cancer care: a European survey. Eur. J. Public Health. 2022;32:311–315. doi: 10.1093/eurpub/ckab214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dinmohamed A.G., Visser O., Verhoeven R.H.A., Louwman M.W.J., van Nederveen F.H., Willems S.M., et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol. 2020;21:750–751. doi: 10.1016/S1470-2045(20)30265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zadnik V., Mihor A., Tomsic S., Zagar T., Bric N., Lokar K., et al. Impact of COVID-19 on cancer diagnosis and management in Slovenia - preliminary results. Radiol. Oncol. 2020;54:329–334. doi: 10.2478/raon-2020-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Skovlund C.W., Friis S., Dehlendorff C., Nilbert M.C., Mørch L.S. Hidden morbidities: drop in cancer diagnoses during the COVID-19 pandemic in Denmark. Acta Oncol. 2021;60:20–23. doi: 10.1080/0284186X.2020.1858235. [DOI] [PubMed] [Google Scholar]
- 75.Peacock H.M., Tambuyzer T., Verdoodt F., Calay F., Poirel H.A., De Schutter H., Francart J., Van Damme N., Van Eycken L. Decline and incomplete recovery in cancer diagnosis during the COVID-19 pandemic in Belgium, a year long population based analysis. ESMO Open. 2021;6(4) doi: 10.1016/j.esmoop.2021.100197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.National Cancer Registry, Cancer in Ireland 1994–2020: Annual report of the National Cancer Registry 2022, https://www.ncri.ie/publications/statistical-reports/cancer-ireland-1994-2020-annual-statistical-report-national-cancer, p. 2022.
- 77.Northern Ireland Cancer Registry Official Statistics. Available from: https://www.qub.ac.uk/research-centres/nicr/CancerInformation/official-statistics/.
- 78.Pacheco R.L., Martimbianco A.L.C., Roitberg F., Ilbawi A., Riera R. Impact of Strategies for Mitigating Delays and Disruptions in Cancer Care Due to COVID-19: Systematic Review. JCO Global Oncology. 2021:342–352. doi: 10.1200/GO.20.00632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gostin L.O. Living in an Age of Pandemics: From COVID-19 to MonkeypoxPolio Dis X. JAMA Health Forum. 2022;3(9) doi: 10.1001/jamahealthforum.2022.4062. [DOI] [PubMed] [Google Scholar]
- 80.Merad M., Blish C.A., Sallusto F., Iwasaki A. The immunology and immunopathology of COVID-19. Science. 2022;375:1122–1127. doi: 10.1126/science.abm8108. [DOI] [PubMed] [Google Scholar]
- 81.Elkrief A., Wu J.T., Jani C., Enriquez K.T., Glover M., Shah M.R., et al. Learning through a pandemic: the current state of knowledge on COVID-19 and cancer. Cancer Discov. 2022;12:303–330. doi: 10.1158/2159-8290.CD-21-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang W., Kaelber D.C., Xu R., Berger N.A. Breakthrough SARS-CoV-2 infections, hospitalizations, and mortality in vaccinated patients with cancer in the US between december 2020 and november 2021. JAMA Oncol. 2022;8:1027–1034. doi: 10.1001/jamaoncol.2022.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.World Health Organisation. Third round of the global pulse survey on continuity of essential health services during the COVID-19 pandemic: November–December 2021. 〈https://www.who.int/./WHO-2019-nCoV-EHS_continuity-survey-2022.1〉.
- 84.Kaufman H.W., Chen Z., Niles J.K., Fesko Y.A. New cancer diagnosis still lagging in the United States in the second full year of the COVID-19 pandemic. JCO Clin. Cancer Inf. 2022:6e2200102. doi: 10.1200/CCI.22.00102. [DOI] [PubMed] [Google Scholar]
- 85.Soerjomataram I., Bray F., Lansdorp-Vogelaar I., Ginsburg O., Rahal R., Sullivan R., et al. COVID-19 and Cancer Global Modelling Consortium (CCGMC): A global reference to inform national recovery strategies. J. Cancer Policy. 2022;32 doi: 10.1016/j.jcpo.2022.100328. [DOI] [PMC free article] [PubMed] [Google Scholar]