Abstract
Introduction: Despite several perioperative care advancements and innovations in surgical procedures and technologies, the incidence rate of anastomotic leaks (ALs) after colorectal surgery has not substantially decreased. Gut microbiota can play a critical role in the healing process of anastomotic tissue and alterations in its composition may be largely to blame for anastomotic insufficiency. The use of specific antibiotics for preoperative large bowel decontamination could significantly influence the rate of ALs. The aim of this study was to systematically assess the various antibiotic prophylactic regimen strategies for primary prevention of ALs during colorectal surgery, in view of the available evidence. Methods: A systematic review of the literature was conducted, and randomized clinical trials (RCTs) analyzing prophylactic antibiotic bowel preparation in colorectal surgery were included. PubMed, Embase, the Web of Science Core Collection, and the Cochrane Central Register of Controlled Trials were searched from inception through to 30 November 2022. The methodological quality of the included trials was evaluated. The primary outcome was AL rate; secondary outcomes were superficial/deep surgical site infections (SSIs). The PRISMA guidelines were used to carry out the present systematic review. Results: Thirteen RCTs published between 1977 and 2022, with a total of 4334 patients were included in the meta-analysis. Antibiotic prophylaxis was administered orally in 11/13 studies and intravenously in 2 studies. Patients randomly assigned to antibiotic prophylaxis, regardless of the regimen, had a reduced risk of ALs (p = 0.003) compared to mechanical bowel preparation (MBP) alone. The use of antibiotic prophylaxis was also more effective in significantly reducing SSIs (p < 0.001). Conclusions: The evidence points to an advantage of oral antibiotic prophylaxis in terms of AL rate, a significant contributor to perioperative morbidity, mortality, and rising healthcare expenditures. In light of such results, the use of antibiotic prophylaxis should be strongly encouraged prior to colorectal surgery.
Keywords: colorectal surgery, anastomotic leak, surgical site infection, antibiotics, prophylaxis
1. Introduction
Despite several perioperative care advancements and innovations in surgical procedures and technologies which have been developed over the past few decades, the incidence rate of anastomotic leaks (ALs) after colorectal surgery has not substantially decreased. ALs are currently reported to develop in 6–8% following colonic resections and between 7 and 20% after rectal surgery [1]. When ALs occur, the risk of postoperative mortality, length of hospital stay, cancer recurrence, permanent stomas, and total expenditures rise significantly [2,3]. The patient’s characteristics, cancer stage, and surgical technique are just a few of the many identified risk factors for anastomotic failure.
The hypothesis that gut microbiota can play a critical role in the healing process of anastomotic tissue and that alterations in its composition may be largely to blame for anastomotic insufficiency has been proposed by some authors [4,5,6]. In the endocrine, neurological, and metabolic systems, it is well established that microbiota and the host have a mutualistic interaction. The primary functions of gut microbiota are to maintain healthy bowel function, protect the intestinal barrier’s integrity, support mucosal immunity, protect the mucosa from infections, and produce bioactive substances [7]. Therefore, it is essential to protect the microbiota’s biodiversity in order to retain these functions.
In this regard, it has been previously shown that any surgical operation performed on the gut can significantly alter this biodiversity, which may affect how the anastomosis heals. In a mouse model, Shogan et al. found how colonic resection followed by the creation of an anastomosis caused significant alterations in the gut microbiota’s composition [6]. On the other hand, Cohn et al. successfully demonstrated in an animal model, how experimentally inducing peri-anastomotic colonic ischemia and administering intraluminal antibiotics directly at the level of the anastomosis could allow correct healing of the bowel tissue despite local ischemia, compared to the control group who did not receive any antibiotics, where complete disruption of the anastomosis occurred [8].
In consideration of the fundamental role played by the gut microbiota in anastomotic healing, the use of specific antibiotics for preoperative large bowel decontamination could significantly influence the rate of ALs. The aim of this study was to systematically assess the various antibiotic prophylactic regimen strategies and their role in preventing ALs during colorectal surgery, in view of the available evidence.
2. Results
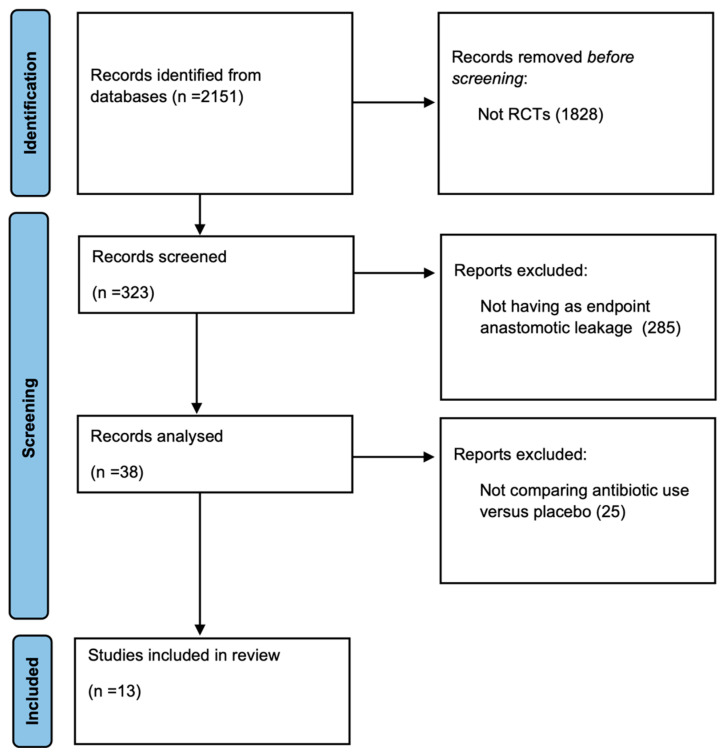
A total of 2151 studies were found in the electronic search. After reviewing titles and abstracts, 1828 studies were excluded, while 323 were screened. Out of these, 285 did not have anastomotic leakage as an endpoint. No eligible trials were found prior to 1973, and the first trial included in the meta-analysis was from 1977. The remaining 38 articles were analyzed and 25 were excluded because they did not compare antibiotic use with a placebo control group. Thus, 13 articles were included in the final analysis (Figure 1).
Figure 1.
Flowchart of article selection.
2.1. Methodological Quality Assessment
Regarding RCTs’ methodological quality, all studies reported using the random sequence generation methods and were double-blinded in eight studies, single-blinded in four studies, and open-label in one study. Methodological quality evaluated using Jadad’s validated scale revealed just one study with a score of 4 (7.7%); five studies obtained a score of 3 (38.5%); six studies (46.1%) obtained a score of 2; and one study received a score of 1 (7.7%) (Table 1). The overall risk of bias judgement according to the Cochrane risk-of-bias tool for randomized trials (RoB 2) was ‘high’ for 9 (69.2%) studies and with ‘some concerns’ for 4 (30.8%) trials (Table 2). The biggest risk of bias in this review derives from the selection of the reported result. The outcome domain anastomotic leak is not univocally measured and is mainly based on clinical judgement and/or radiologic exams, which may affect this outcome measure and increases the risk of bias.
Table 2.
Version 2 of the Cochrane risk-of-bias tool for randomized trials to assess the risk of bias in the findings of each study. The tool is structured into five domains. Trials are judged for each domain as either having a ‘Low’/’Some concerns’/’High’ risk of bias with an overall judgement of the risk.
| Author | 1. Risk of Bias Arising from the Randomization Process | 2.1 Risk of Bias Due to Deviations from the Intended Interventions (Effect of Assignment to Intervention) | 2.2 Risk of Bias Due to Deviations from the Intended Interventions (Effect of Adhering to Intervention) | 3. Risk of Bias Due to Missing Outcome Data | 4. Risk of Bias in the Measurement of the Outcome | 5. Risk of Bias in the Selection of the Reported Result | Overall Risk-of-Bias Judgement |
|---|---|---|---|---|---|---|---|
| Hojer et al. [9] | Low | Low | Low | Some concerns | Low | High | High |
| Matheson et al. [10] | Low | Low | Low | Some concerns | Low | High | High |
| Bartlett et al. [11] | Low | Low | Low | Some concerns | Low | Some concerns | Some concerns |
| Ishida et al. [12] | High | Low | High | Low | Low | High | High |
| Sato et al. [13] | Some concerns | Low | High | Low | Low | High | High |
| Sadahiro et al. [14] | Low | Low | Low | Some concerns | Low | High | High |
| Hjalmarsson et al. [15] | High | Low | High | Low | Low | High | High |
| Anjum et al. [16] | Low | Low | Low | Some concerns | Low | Low | Some concerns |
| Abis et al. [17] | High | Low | Some concerns | Low | Low | High | High |
| Koskenvuo et al. [18] | High | Low | High | Low | Low | High | High |
| Mulder et al. [19] | Low | Low | Low | Some concerns | Low | Some concerns | Some concerns |
| Papp et al. [20] | High | Some concerns | High | Low | Low | High | High |
| Futier et al. [21] | Low | Low | Low | Some concerns | Low | Some concerns | Some concerns |
Table 1.
Methodological quality assessment according to Jadad scores.
| Author | Jadad Scores for RCTs |
|---|---|
| Hojer et al. [9] | 2 |
| Matheson et al. [10] | 2 |
| Bartlett et al. [11] | 1 |
| Ishida et al. [12] | 2 |
| Sato et al. [13] | 2 |
| Sadahiro et al. [14] | 2 |
| Hjalmarsson et al. [15] | 3 |
| Anjum et al. [16] | 3 |
| Abis et al. [17] | 3 |
| Koskenvuo et al. [18] | 3 |
| Mulder et al. [19] | 2 |
| Papp et al. [20] | 3 |
| Futier et al. [21] | 4 |
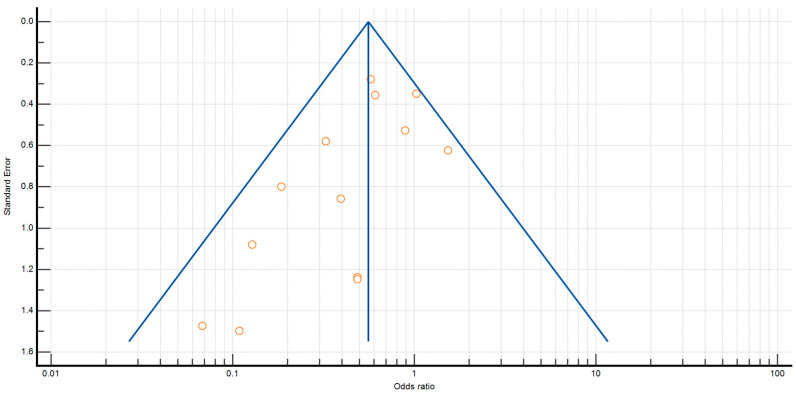
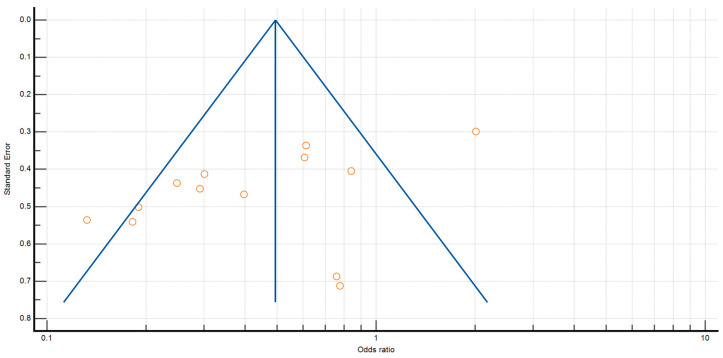
The p values for Egger’s and Begg’s tests for anastomotic leak were p = 0.0450 and p = 0.1127, respectively. Furthermore, the p value for Egger’s and Begg’s tests for surgical site infection was p = 0.0468 and p = 0.1795 (Figure 2 and Figure 3).
Figure 2.
Funnel plot for anastomotic leaks.
Figure 3.
Funnel plot for surgical site infections.
2.2. Primary Outcomes
A total of 4334 patients participated in the selected studies. All patients received mechanical bowel preparation (MBP). Two thousand forty-one patients received antibiotic prophylaxis, whereas 1943 received only MBP.
Table 3 shows the characterization of studies regarding the interventions investigated.
Table 3.
Characterization of included RCTs.
| Author | Year of Publication |
Study Design | Number of Patients |
Endpoints | Antibiotic Group | Control Group | Statistical Significance |
|---|---|---|---|---|---|---|---|
| Höjer et al. [9] | 1977 | Single-center, prospective, double-blinded, randomized trial | 118 | 58 | 60 | ||
| Anastomotic Leak | 2 | 5 | p < 0.001 | ||||
| SSI | 5 | 25 | p < 0.001 | ||||
| Matheson et al. [10] | 1978 | Single-center, double-blinded, randomized controlled trial | 110 | 51 | 59 | ||
| Anastomotic Leak | 0 | 7 | p < 0.02 | ||||
| SSI | 9 | 25 | p < 0.01 | ||||
| Bartlett et al. [11] | 1978 | Multicenter, double-blinded, randomized trial | 116 | 56 | 60 | ||
| Anastomotic Leak | 2 | 10 | p = 0.05 | ||||
| SSI | 5 | 21 | p = 0.002 | ||||
| Ishida et al. [12] | 2001 | Single-center, single-blinded, randomized controlled trial | 143 | 72 | 71 | ||
| Anastomotic Leak | 1 | 2 | p = 0.050 | ||||
| SSI | 8 | 17 | p = 0.035 | ||||
| Sato et al. [13] | 2009 | Multicenter, randomized trial | 100 | 49 | 51 | ||
| Anastomotic Leak | 7 | 5 | p = 0.8293 | ||||
| SSI | 20 | 23 | p = 0.8293 | ||||
| Sadahiro et al. [14] | 2014 | Single-center, double-blinded, randomized trial | 194 | 99 | 95 | ||
| Anastomotic Leak | 1 | 7 | p = 0.014 | ||||
| SSI | 18 | 17 | p = 0.004 | ||||
| Hjalmarsson et al. [15] | 2015 | Prospective, multicenter, single-blinded, randomized controlled trial | 985 | 486 | 499 | ||
| Anastomotic Leak | 17 | 17 | p = 0.95 | ||||
| SSI | 34 | 18 | p = 0.022 | ||||
| Anjum et al. [16] | 2017 | Single-center, double-blinded, prospective, randomized trial | 184 | 91 | 93 | ||
| Anastomotic Leak | 0 | 4 | p = 0.004 | ||||
| SSI | 8 | 26 | p = 0.001 | ||||
| Abis et al. [17] | 2018 | Superiority, open-label, multicenter, randomized trial | 455 | 228 | 227 | ||
| Anastomotic Leak | 14 | 22 | OR 0.61 (0.30–1.22) | ||||
| SSI | 5 | 24 | OR 0.19 (0.07–0.51) | ||||
| Koskenvuo et al. [18] | 2019 | Multicenter, parallel, single-blinded randomized trial | 396 | 196 | 200 | ||
| Anastomotic Leak | 7 | 8 | CI 1.13 (0.40–3.16) | ||||
| SSI | 13 | 21 | CI 1.65 (0.80–3.40) | ||||
| Mulder et al. [19] | 2020 | Multicenter, double-blind, placebo-controlled randomized trial | 78 | 39 | 39 | ||
| Anastomotic Leak | 1 | 2 | RR 0.50 (0.05–5.29) | ||||
| SSI | 4 | 5 | RR 0.80 (0.23–2.78) | ||||
| Papp et al. [20] | 2021 | Multicentre, prospective, randomized, assessor-blinded trial |
529 | 253 | 276 | ||
| Anastomotic Leak | 4 | 13 | p = 0.020 | ||||
| SSI | 8 | 27 | p = 0.001 | ||||
| Futier et al. [21] | 2022 | Multicenter, double-blinded, randomized, placebo-controlled trial | 926 | 463 | 463 | ||
| Anastomotic Leak | 22 | 37 | p = 0.046 | ||||
| SSI | 60 | 100 | p = 0.001 |
In 11 out of 13 studies, antibiotics were administered orally, while in the remaining two studies, patients received intravenous antibiotic prophylaxis (Table 4).
Table 4.
Routes of administration and regimens of antibiotic prophylaxis.
| Author | Antibiotic | Administration Regimen | Administration Route |
|---|---|---|---|
| Hojer et al. [9] | Doxycycline 200 mg | - Started 4–6 h preop., single dose - Continued o.d. for 5 days postop. |
Oral |
| Matheson et al. [10] | Neomycin 1 g and Metronidazole 200 mg | - Started 2 days preop. t.d.s. | Oral |
| Bartlett et al. [11] | Neomycin 1 g and Erythromycin 1 g | -Started 1 day preop. t.d.s. | Oral |
| Ishida et al. [12] | Metronidazole 400 mg and Kanamycin 500 mg | - Started 2 days preop. b.d. - Continued 3 days postop. b.d. |
Oral |
| Sato et al. [13] | Cefotiam | - Started during skin incision - Continued 3 days postop. t.d.s. |
Intravenous |
| Sadahiro et al. [14] | Kanamycin 0.5 g + Metronidazole 0.5 g | - Started 1 day preop. t.d.s. | Oral |
| Hjalmarsson et al. [15] | Sulfamethoxazole 800 mg/Trimethoprim 160 mg, and three tablets of Metronidazole 400 mg |
-Started 2 h preop. single dose | Oral |
| Anjum et al. [16] | Metronidazole 400 mg and Levofloxacin 200 mg | - Started 1 day preop. t.d.s. | Oral |
| Abis et al. [17] | 10 mL suspension containing 5 mL Amphotericin B 500 mg and 5 mL Colistin sulphate 100 mg and Tobramycin 80 mg | - Started 3 days preop. q.i.d. - Continued 3 days postop. |
Oral |
| Koskenvuo et al. [18] | Neomycin 2 g and Metronidazole 2 g | - Started 1 day preop. o.d. | Oral |
| Mulder et al. [19] | Tobramycin 16 mg/mL and Colistin sulphate 20 mg/mL |
- Started 3 days preop. q.i.d. | Oral |
| Papp et al. [20] | Ceftriaxone 2 g and Metronidazole 500 mg |
-Started 1 day preop t.d.s. | Intravenous |
| Futier et al. [21] | Ornidazole 1 g | -Started 12 h preop. o.d. | Oral |
(o.d: once daily; b.d: twice daily; t.d.s: three times daily; q.i.d: four times daily).
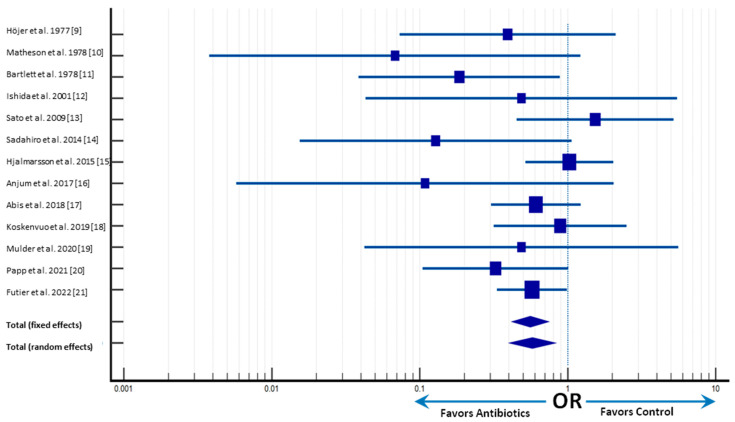
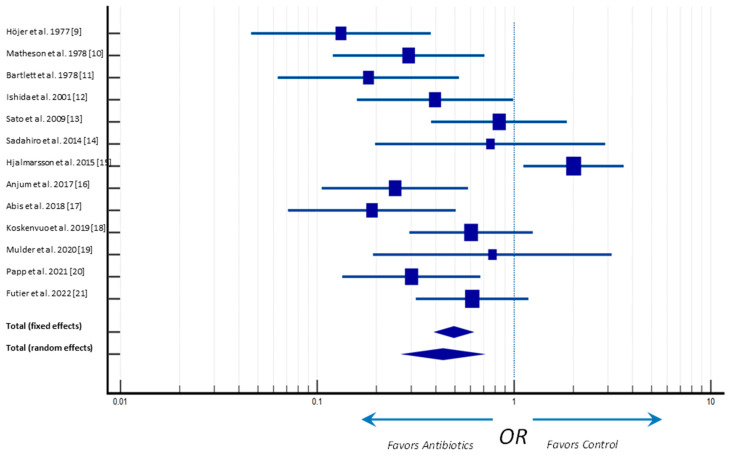
The individual and pooled odds ratio (OR) and risk differences of ALs are shown in Figure 4. The overall analyses indicated that patients randomly assigned to the antibiotic prophylaxis, regardless of the regimen or route of administration, had reduced risk of ALs (p = 0.003), compared with participants receiving MBP alone. Indeed, the meta-analysis average effect, represented by the center of the diamond, is located at the left of the vertical line center for both endpoints, favoring intervention (Figure 4).
Figure 4.
Forster plot of anastomotic leak rates. Odds ratio (OR) and 95% confidence intervals (CI) [9,10,11,12,13,14,15,16,17,18,19,20,21].
2.3. Secondary Outcomes
Throughout the studies, the definition of organ-space infection varied. Particularly, just one study made a distinction between organ-space infections, with most studies describing either radiological or clinical signs of SSIs.
Individual and pooled ORs and risk differences for the secondary analyses of SSIs are shown in Figure 5. The analysis of included RCTs showed that antibiotic prophylaxis was more effective, with respect to MBP alone, in significantly reducing SSIs (p < 0.001).
Figure 5.
Forster plot of surgical site infections. Odds ratio (OR) and 95% confidence intervals (CI) [9,10,11,12,13,14,15,16,17,18,19,20,21].
3. Discussion
Anastomotic leaks are a significant postoperative complication following surgery for colorectal disease and have a major impact on patient morbidity and mortality. The RCTs included in the present meta-analysis clearly highlight the beneficial effect of antibiotic prophylaxis, regardless of the type of regimen used, on the rate of both ALs and SSIs (p = 0.003 and p < 0.001, respectively) compared to MBP alone. In light of such results, the use of antibiotic prophylaxis prior to colorectal surgery should be strongly encouraged.
From the studies retrieved in the present systematic review, there was insufficient data from each different combination of an oral antibiotic agent, dose, time, and parenteral antibiotic details to conduct a meaningful analysis between subgroups. According to the patient’s preparation regimen, some contained only one preoperative dosage of an oral antibiotic or used different parenteral antibiotic regimens, which could be significantly biased.
The numerous variables, including differences in the type of antibiotic used, dosing methods, and route of administration, made it difficult to identify which of these three variables may have caused any discrepancy in outcomes.
Most studies used antibiotic combinations without comparing them to recognized prophylaxis approaches or offering a logical prophylaxis strategy based on what is known about colonic bacterial flora and the characteristics of postoperative ALs and SSIs in colorectal surgery.
Although gold-standard antibiotic regimens have been proposed by various scientific societies, with the goal of including the gold standard as the appropriate benchmark from which to judge the new antibiotic in all future investigations, only a few of the eligible studies actually implemented these recommended antibiotics.
Evidence from the review’s analysis suggests that the chosen antibiotic should cover both aerobic and anaerobic microorganisms. These results provide evidence that treating both types of bacteria, whether with a single agent or in a combination therapy, is more effective in reducing SSIs and ALs than treating only aerobic or only anaerobic bacteria.
Further investigation is necessary to determine the best timing and duration for dosing, as well as the incidence of longer-lasting negative effects, including Clostridium difficile pseudomembranous colitis.
The use of oral antibiotics with or without mechanical bowel preparation was initially investigated in the 1970s but later fell out of favor, reemerging only recently as a viable intervention given the high rate of superficial and organ/space SSIs, as well as ALs following colorectal surgery.
In response to specific conditions, such as large tumors, substantial blood loss, prolonged surgical procedures, and ischemia, the host produces local and systemic inflammatory signals during anastomotic construction. Bacteria respond to this altered environment by genic shifting and/or activation, resulting in increased virulence. If they are more prevalent, these pathogenic activated elements can bind to the anastomotic tissues, evade the immune system, and activate collagenase genes, intensifying the inflammatory response in the tissue. In addition to degrading collagen I, bacterial collagenases can also cause local tissue matrix metalloproteinases-9 (MMP-9) to degrade collagen IV. The anastomotic tissue can rupture as a result of this process [7].
Prior to surgery, identifying risk variables is a crucial step that enables the management of modifiable factors and surgical technique adaptation. The best course of action for this continues to be AL prevention, despite the lack of success of endorsed preventive programs to date.
Bowel regimes before elective colorectal surgery are rarely implemented across many institutions and are still primarily dependent on the surgeons’ preference. Oral antibiotic prophylaxis is typically not required, and even the type of mechanical bowel preparation varies from center to center.
In fact, the use of antibiotic prophylaxis is still not broadly regarded as a standard of care, despite research released in 1981 that already demonstrated its value in reducing infection rates and overall mortality, as well as establishing the need for no more placebo or control trials [22]. A Cochrane Review that showed a substantial decrease in surgical site infections in patients receiving parenteral antibiotic prophylaxis compared to those receiving no antibiotics or a placebo (RR 0.34, 95% CI 0.28–0.41, p = 0.0001) presented conclusive evidence in favor of this claim [23].
The 2019 clinical practice Guidelines of the American Society of Colon and Rectal Surgeons strongly advise mechanical bowel preparation paired with preoperative oral antibiotics [24]. This association appears to improve short-term oncological outcomes and lowers the frequency of surgical site infections, anastomotic leakage, and postoperative ileus [25].
Eight cohort studies and 23 RCTs published between 1980 and 2015 were included in a recent meta-analysis [26]. However, the authors also included various cohort studies emerging from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database, which most likely implies duplicate reporting of the same patient information. According to this study, surgical site infection rates were significantly lower in cohort study participants who received mechanical bowel preparation, oral antibiotics, and IV antibiotics compared to those who received only mechanical bowel preparation and IV antibiotics (RR 0.48, 95% CI 0.44–0.52, p = 0.00001). In another recent meta-analysis, Bellows et al. compared the effectiveness of IV antibiotics alone against IV antibiotics in combination with oral non-absorbable antibiotics before colorectal surgery while concentrating on surgical site infections [27]. This study comprised 16 RCTs that were published between 1980 and 2011, with a total of 2669 patients, and all the trials had mechanical bowel preparation as part of the protocol. According to this meta-analysis, there was no significant difference in anastomotic leak rates between oral and IV antibiotics compared with IV antibiotics alone (RR 0.63, 95% CI 0.28–1.41, p = 0.3), although there was a substantial decrease in superficial wound infection rates.
Over the past 50 years, there have been great controversies surrounding the use of antibiotic prophylaxis with or without mechanical bowel preparation. The composition of gut microbiota is altered by mechanical bowel preparation alone. In particular, mechanical bowel preparation raises intestinal pH, which promotes Proteobacteria and Enterobacteriaceae expansion and a decrease in Lactobacillaceae, changing the ratio of Gram+ to Gram- bacteria. When mechanical bowel preparation is administered in two or more doses as opposed to one, these side effects are not severe and last for a shorter amount of time [28,29].
Although some recent meta-analyses concluded that mechanical bowel preparation alone cannot lower the risk of ALs or intra-abdominal abscesses following colorectal surgery [30,31], the beneficial association between mechanical bowel preparation and oral antibiotics has been noted since the 1970s in lowering surgical complications, such as surgical site infections [30,31,32].
There are currently only a limited number of studies in the literature that assess how well a combination of mechanical bowel preparation, oral antibiotics, and probiotics prepare patients for colorectal resections. Nevertheless, some studies have indicated that using Bifidobacteria postoperatively may help maintain an optimal microbiota balance. The use of probiotics lessens and modulates the inflammatory response, enhances healing, and improves the composition of fecal microbiota in patients undergoing colorectal surgery [32,33]. Probiotic use before surgery is associated with a lower occurrence of postoperative complications, primarily ALs and infections, promoting a healthy recovery [34]. This raises the prospect that, in the event of anastomotic leakage, a favorable microbiota, already present at baseline or orally/locally administered may result in less severe sepsis and peritonitis.
Although antibiotic prophylaxis has been widely implemented in clinical practice, the underlying mechanisms for its effectiveness in reducing the rates of such dreaded complications are not fully understood. For this reason, it appears difficult to comment on the mechanistic benefit of a prophylactic regimen due to the numerous factors which need yet to be explored.
Study Limitations
Some limitations must be acknowledged in the present study. The most important factor contributing to clinical variability is the diversity of preoperative antibiotic prophylaxis regimens. Second, given the limited data and preliminary results, it is challenging to provide comprehensive guidance on the best prophylactic probiotic and antibiotic regimens for use in clinical practice. Third, the results were probably impaired by additional biases (mostly small trial bias), and only a few trials were sufficiently powered to address this problem. Finally, those studies not reporting anastomotic leaks either as a primary or secondary outcome were excluded from the present review as we considered this an incomplete outcome data bias.
4. Materials and Methods
4.1. Search Strategy and Selection of Trials
This study provides a systematic review and meta-analysis of previously published data emerging from randomized controlled trials, which was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA Statement) criteria [35] (PROSPERO Registration Number: CRD42023396144). The PICO strategy was used to formulate the guiding question: “What are the effects of antibiotics on anastomotic leakage and superficial skin infections during surgery for colorectal cancer?” [36]. The search was performed using the following electronic databases without any year restriction, from inception through to 30 September 2022: PubMed, Embase, the Web of Science Core Collection, and the Cochrane Central Register of Controlled Trials. All abstracts in the English language were screened for applicability. A manual search using the following keywords extracted from the Medical Subjects Heading (MeSH) was made: ‘colorectal surgery’ AND ‘antibiotics’ AND ‘antibiotic prophylaxis’ AND ‘leaks’ AND ‘dehiscence’ AND ‘surgical site infection’ AND ‘ssi’ AND ‘complications’ AND ‘randomized controlled trial’.
The eligibility criteria for the selection of articles, according to the PICO strategy were: RCTs with adults aged 18 years or over (population); use of preoperative antibiotics (intervention); comparison with no treatment (comparison); and incidence of anastomotic leakage and superficial skin infection (outcomes). The studies excluded were those not written in English, or that did not provide the full online abstract.
Two independent reviewers (LCG, MFR) screened and selected the trials to be included in the review. Conflicts were handled by consensus, and an adjudicator (JCM) was consulted when necessary. Only studies that were fully available and designed as randomized controlled trials evaluating the effects of different strategies of antibiotic prophylaxis before elective colorectal surgery and assessing postoperative complications (i.e., anastomotic leaks and surgical site infections) were included.
4.2. Critical Assessment of Trials and Collection of Data
Two independent reviewers evaluated the methodological quality of eligible trials using a validated scale [37]; in the event of a disagreement, the final score was decided by consensus. The quality scale included three components: (1) double-blinding, (2) randomization, and (3) dropouts. The scale ranged from 0 to 5, with a score of 0–2 for randomization, a score of 0–2 for blinding, and a score of 1 for dropouts. When the score is ≤2, a trial’s methodological quality is deemed poor/inappropriate according to Moher et al.
The two reviewers independently gathered data, which they then compared and cross-checked. Missing data was sought on the journal’s database and included if present. All studies with missing text or with insufficiently reported data were excluded.
Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) was used to assess the risk of bias.
The following data were retrieved for each RCT: sample size, type/modality of randomization, blinding, dropouts, type of antibiotic prophylaxis regimen, use of mechanical bowel preparation, anastomotic leaks, surgical site infections, other postoperative complications, and mortality.
4.3. Outcome Measures
Outcomes were evaluated on the basis of intention-to-treat. The primary outcome was the rate of anastomotic leaks, while secondary outcomes included superficial and deep organ/space surgical site infections (wound infection, wound dehiscence, pelvic abscess, peritonitis).
4.4. Risk of Bias Assessment
The Cochrane risk of bias tool was used to assess RCTs. We evaluated randomization sequence generation, allocation concealment, blinding, completeness of outcome data, and selective reporting for each RCT. Concealment of allocation was considered adequate if the randomized method described in the text did not allow the investigators and the participants to know or influence the intervention group before the randomized allocation. Publication bias was evaluated using Begg’s and Egger’s tests [38,39].
4.5. Statistical Analysis
Data analyses were carried out using MedCalc v20.211 statistical software [40]. Odds ratios were selected to describe the ratio of odds in the treatment group to the odds of the control group. The heterogeneity among the studies was checked using Cochrane’s Q [41] and the I2 statistical tests [42,43]. The model of random effects was adopted for the analysis.
5. Conclusions
The current systematic review, which is the broadest and most comprehensive one to date assessing the role of different regimens of antibiotic prophylaxis in preventing ALs after colorectal surgery, suggests that oral antibiotic bowel decontamination, whether used alone or in conjunction with mechanical bowel preparation, may have a considerable impact on the reduction in postoperative complications. When just RCT-based evidence is taken into account, it tends to attenuate the considerable positive impact of antibiotics suggested by large retrospective cohort and database studies. The evidence, however, points to an advantage of oral antibiotic bowel preparation both in terms of SSI and AL rates, significant contributors to perioperative morbidity, and rising healthcare expenditures. In light of our results, the use of antibiotic prophylaxis prior to colorectal surgery should be strongly encouraged. Nevertheless, before making more firm recommendations, further high-quality evidence is needed to distinguish between the advantages of the different antibiotic regimens and whether this is more beneficial alone or combined with mechanical bowel preparation in this setting.
Author Contributions
Conceptualization, L.C.-G.; methodology, L.C.-G. and M.F.R.; software, M.F.R.; validation, L.C.-G., M.F.R., G.C., M.C. and R.M.; formal analysis, M.F.R.; investigation, L.C.-G. and M.F.R.; resources, J.C.-M. and A.S.; data curation, L.C.-G. and M.F.R.; writing—original draft preparation, L.C.-G. and M.F.R.; writing—review and editing, G.C. and J.C.-M.; visualization, J.C.-M., A.S., V.D., M.C. and R.M.; supervision, L.C.-G.; project administration, M.F.R., J.C.-M., A.S.and V.D. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study did not require ethical approval.
Informed Consent Statement
Not applicable.
Data Availability Statement
The raw data is available upon reasonable request to the corresponding authors.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Chaouch M.A., Kellil T., Jeddi C., Saidani A., Chebbi F., Zouari K. How to Prevent Anastomotic Leak in Colorectal Surgery? A Systematic Review. Ann. Coloproctol. 2020;36:213–222. doi: 10.3393/ac.2020.05.14.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daniel V.T., Alavi K., Davids J.S., Sturrock P.R., Harnsberger C.R., Steele S.R., Maykel J.A. The utility of the delphi method in defining anastomotic leak following colorectal surgery. Am. J. Surg. 2020;219:75–79. doi: 10.1016/j.amjsurg.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Guyton K.L., Hyman N.H., Alverdy J.C. Prevention of Perioperative Anastomotic Healing Complications: Anastomotic Stricture and Anastomotic Leak. Adv. Surg. 2016;50:129–141. doi: 10.1016/j.yasu.2016.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Okada M., Bothin C., Kanazawa K., Midtvedt T. Experimental study of the influence of intestinal flora on the healing of intestinal anastomoses. Br. J. Surg. 1999;86:961–965. doi: 10.1046/j.1365-2168.1999.01161.x. [DOI] [PubMed] [Google Scholar]
- 5.Guyton K., Alverdy J.C. The gut microbiota and gastrointestinal surgery. Nat. Rev. Gastroenterol. Hepatol. 2017;14:43–54. doi: 10.1038/nrgastro.2016.139. [DOI] [PubMed] [Google Scholar]
- 6.Shogan B.D., Smith D.P., Christley S., Gilbert J.A., Zaborina O., Alverdy J.C. Intestinal anastomotic injury alters spatially defined microbiome composition and function. Microbiome. 2014;2:35. doi: 10.1186/2049-2618-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edomskis P., Goudberg M.R., Sparreboom C.L., Menon A.G., Wolthuis A.M., D’Hoore A., Lange J.F. Matrix metalloproteinase-9 in relation to patients with complications after colorectal surgery: A systematic review. Int. J. Color. Dis. 2020;36:1–10. doi: 10.1007/s00384-020-03724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohn I., Jr., Rives J.D. Antibiotic Protection of Colon Anastomoses. Ann. Surg. 1955;141:707–717. doi: 10.1097/00000658-195505000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Höjer H., Wetterfors J. Systemic Prophylaxis with Doxycycline in Surgery of the Colon and Rectum. Ann. Surg. 1978;187:362–368. doi: 10.1097/00000658-197804000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matheson D.M., Arabi Y., Baxter-Smith D., Alexander-Williams J., Keighley M.R.B. Randomized multicentre trial of oral bowel preparation and antimicrobials for elective colorectal operations. Br. J. Surg. 1978;65:597–600. doi: 10.1002/bjs.1800650902. [DOI] [PubMed] [Google Scholar]
- 11.Bartlett J.G., Condon R.E., Gorbach S.L., Clarke J.S., Nichols R.L., Ochi S. Veterans Administration Cooperative Study on Bowel Preparation for Elective Colorectal Operations: Impact of oral antibiotic regimen on colonic flora, wound irrigation cultures and bacteriology of septic complications. Ann. Surg. 1978;188:249–254. doi: 10.1097/00000658-197808000-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ishida H., Yokoyama M., Nakada H., Inokuma S., Hashimoto D. Impact of Oral Antimicrobial Prophylaxis on Surgical Site Infection and Methicillin-Resistant Staphylococcus aureus Infection After Elective Colorectal Surgery. Results of a Prospective Randomized Trial. Surg. Today. 2001;31:979–983. doi: 10.1007/s005950170006. [DOI] [PubMed] [Google Scholar]
- 13.Sato T., Takayama T., Fujii M., Song K., Matsuda M., Higaki T., Okada S. Systemic use of antibiotics does not prevent postoperative infection in elective colorectal surgery: A randomized controlled trial. J. Infect. Chemother. 2009;15:34–38. doi: 10.1007/s10156-008-0660-X. [DOI] [PubMed] [Google Scholar]
- 14.Sadahiro S., Suzuki T., Tanaka A., Okada K., Kamata H., Ozaki T., Koga Y. Comparison between oral antibiotics and probiotics as bowel preparation for elective colon cancer surgery to prevent infection: Prospective randomized trial. Surgery. 2014;155:493–503. doi: 10.1016/j.surg.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Hjalmarsson C., Karlberg J., Törnqvist P., Arbman G., Frisk B., Modin M., The TSM Study Group Orally Administered Trimethoprim-Sulfamethoxazole and Metronidazole as Infection Prophylaxis in Elective Colorectal Surgery. Surg. Infect. 2015;16:604–610. doi: 10.1089/sur.2014.059. [DOI] [PubMed] [Google Scholar]
- 16.Anjum N., Ren J., Wang G., Li G., Wu X., Dong H., Wu Q., Li J. A Randomized Control Trial of Preoperative Oral Antibiotics as Adjunct Therapy to Systemic Antibiotics for Preventing Surgical Site Infection in Clean Contaminated, Contaminated, and Dirty Type of Colorectal Surgeries. Dis. Colon Rectum. 2017;60:1291–1298. doi: 10.1097/DCR.0000000000000927. [DOI] [PubMed] [Google Scholar]
- 17.Abis G.S.A., Stockmann H.B.A.C., Bonjer H.J., van Veenendaal N., van Doorn-Schepens M.L.M., Budding A., Wilschut J., van Egmond M., Oosterling S.J., de Lange E.S.M., et al. Randomized clinical trial of selective decontamination of the digestive tract in elective colorectal cancer surgery (SELECT trial) Br. J. Surg. 2019;106:355–363. doi: 10.1002/bjs.11117. [DOI] [PubMed] [Google Scholar]
- 18.Koskenvuo L., Lehtonen T., Koskensalo S., Rasilainen S., Klintrup K., Ehrlich A., Pinta T., Scheinin T., Sallinen V. Mechanical and oral antibiotic bowel preparation versus no bowel preparation for elective colectomy (MOBILE): A multicentre, randomised, parallel, single-blinded trial. Lancet. 2019;394:840–848. doi: 10.1016/S0140-6736(19)31269-3. [DOI] [PubMed] [Google Scholar]
- 19.Mulder T., Bergh M.K.-V.D., Vlaminckx B., Roos D., De Smet A.M., Cappel R.D.V.T.N., Verheijen P., Brandt A., Smits A., Van Der Vorm E., et al. Prevention of severe infectious complications after colorectal surgery using oral non-absorbable antimicrobial prophylaxis: Results of a multicenter randomized placebo-controlled clinical trial. Antimicrob. Resist. Infect. Control. 2020;9:1–11. doi: 10.1186/s13756-020-00745-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papp G., Saftics G., Szabó B.E., Baracs J., Vereczkei A., Kollár D., Oláh A., Mészáros P., Dubóczki Z., Bursics A. Systemic versus Oral and Systemic Antibiotic Prophylaxis (SOAP) study in colorectal surgery: Prospective randomized multicentre trial. Br. J. Surg. 2021;108:271–276. doi: 10.1093/bjs/znaa131. [DOI] [PubMed] [Google Scholar]
- 21.Futier E., Jaber S., Garot M., Vignaud M., Panis Y., Slim K., Lucet J.-C., Lebuffe G., Ouattara A., El Amine Y., et al. Effect of oral antimicrobial prophylaxis on surgical site infection after elective colorectal surgery: Multicentre, randomised, double blind, placebo controlled trial. BMJ. 2022;379:e071476. doi: 10.1136/bmj-2022-071476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baum M.L., Anish D.S., Chalmers T.C., Sacks H.S., Smith H., Fagerstrom R.M. A Survey of Clinical Trials of Antibiotic Prophylaxis in Colon Surgery: Evidence against Further Use of No-Treatment Controls. N. Engl. J. Med. 1981;305:795–799. doi: 10.1056/NEJM198110013051404. [DOI] [PubMed] [Google Scholar]
- 23.Nelson R.L., Gladman E., Barbateskovic M. Antimicrobial prophylaxis for colorectal surgery. Cochrane Database Syst. Rev. 2014;2014:CD001181. doi: 10.1002/14651858.CD001181.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Migaly J., Bafford A.C., Francone T.D., Gaertner W.B., Eskicioglu C., Bordeianou L., Feingold D.L., Steele S.R. Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Use of Bowel Preparation in Elective Colon and Rectal Surgery. Dis. Colon Rectum. 2019;62:3–8. doi: 10.1097/DCR.0000000000001238. Erratum in Dis. Colon Rectum 2019, 62, e436. [DOI] [PubMed] [Google Scholar]
- 25.Zhang L.M., Schuitevoerder D., White M.G., Feldt S., Bs P.K., Hyman N., Shogan B.D. Combined mechanical and oral antibiotic bowel preparation is associated with prolonged recurrence-free survival following surgery for colorectal cancer. J. Surg. Oncol. 2021;124:1106–1114. doi: 10.1002/jso.26619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koullouros M., Khan N., Aly E.H. The role of oral antibiotics prophylaxis in prevention of surgical site infection in colorectal surgery. Int. J. Color. Dis. 2016;32:1–18. doi: 10.1007/s00384-016-2662-y. [DOI] [PubMed] [Google Scholar]
- 27.Bellows C.F., Mills K.T., Kelly T.N., Gagliardi G. Combination of oral non-absorbable and intravenous antibiotics versus intravenous antibiotics alone in the prevention of surgical site infections after colorectal surgery: A meta-analysis of randomized controlled trials. Tech. Coloproctol. 2011;15:385–395. doi: 10.1007/s10151-011-0714-4. [DOI] [PubMed] [Google Scholar]
- 28.Bachmann R., Leonard D., Delzenne N., Kartheuser A., Cani P.D. Novel insight into the role of microbiota in colorectal surgery. Gut. 2017;66:738–749. doi: 10.1136/gutjnl-2016-312569. [DOI] [PubMed] [Google Scholar]
- 29.Kiran R.P., Murray A.C.A., Chiuzan C., Estrada D., Forde K. Combined Preoperative Mechanical Bowel Preparation With Oral Antibiotics Significantly Reduces Surgical Site Infection, Anastomotic Leak, and Ileus After Colorectal Surgery. Ann. Surg. 2015;262:416–425. doi: 10.1097/SLA.0000000000001416. discussion 423–425. [DOI] [PubMed] [Google Scholar]
- 30.Slim K., Vicaut E., Panis Y., Chipponi J. Meta-analysis of randomized clinical trials of colorectal surgery with or without mechanical bowel preparation. Br. J. Surg. 2004;91:1125–1130. doi: 10.1002/bjs.4651. [DOI] [PubMed] [Google Scholar]
- 31.Slim K., Vicaut E., Launay-Savary M.-V., Contant C., Chipponi J. Updated Systematic Review and Meta-Analysis of Randomized Clinical Trials on the Role of Mechanical Bowel Preparation Before Colorectal Surgery. Ann. Surg. 2009;249:203–209. doi: 10.1097/SLA.0b013e318193425a. [DOI] [PubMed] [Google Scholar]
- 32.Nichols R.L., Broido P., Condon R.E., Gorbach S.L., Nyhus L.M. Effect of Preoperative Neornycin-Erythromycin Intestinal Preparation on the Incidence of Infectious Complications Following Colon Surgery. Ann. Surg. 1973;178:453–462. doi: 10.1097/00000658-197310000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mizuta M., Endo I., Yamamoto S., Inokawa H., Kubo M., Udaka T., Sogabe O., Maeda H., Shirakawa K., Okazaki E., et al. Perioperative supplementation with bifidobacteria improves postoperative nutritional recovery, inflammatory response, and fecal microbiota in patients undergoing colorectal surgery: A prospective, randomized clinical trial. Biosci. Microbiota Food Health. 2016;35:77–87. doi: 10.12938/bmfh.2015-017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carlini M., Grieco M., Spoletini D., Menditto R., Napoleone V., Brachini G., Mingoli A., Marcellinaro R. Implementation of the gut microbiota prevents anastomotic leaks in laparoscopic colorectal surgery for cancer:the results of the MIRACLe study. Updat. Surg. 2022;74:1253–1262. doi: 10.1007/s13304-022-01305-6. [DOI] [PubMed] [Google Scholar]
- 35.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgins J.P.T., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; Londes, France: 2011. [Google Scholar]
- 37.Jadad A.R., Moore R.A., Carroll D., Jenkinson C., Reynolds D.J.M., Gavaghan D.J., McQuay H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 38.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Begg C.B., Mazumdar M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 40.MedCalc® Statistical Software. MedCalc Software Ltd.; Ostend, Belgium: 2023. [(accessed on 27 December 2022)]. Version 20.211. Available online: https://www.medcalc.org . [Google Scholar]
- 41.Lau J., Ioannidis J.P., Schmid C. Quantitative Synthesis in Systematic Reviews. Ann. Intern. Med. 1997;127:820–826. doi: 10.7326/0003-4819-127-9-199711010-00008. [DOI] [PubMed] [Google Scholar]
- 42.Vos T., Barber R.M., Bell B., Bertozzi-Villa A., Biryukov S., Bolliger I., Charlson F., Davis A., Degenhardt L., Dicker D., et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Higgins J.P.T., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data is available upon reasonable request to the corresponding authors.