Abstract
Objectives: This study aimed to investigate factors associated with sleep quality in healthcare students and to determine whether depressive and anxiety symptoms may explain some of the associations between sleep quality and self-rated health. Study design: This is a cross-sectional study at wave one. Methods: A total of 637 healthcare students were recruited via a stratified random sampling method in Hangzhou, China. The Sleep Quality Questionnaire (SQQ) and the four-item Patient Health Questionnaire (PHQ-4) were used to assess sleep quality, depressive, and anxiety symptoms, respectively. Self-rated health was assessed via a self-developed questionnaire of both physical and psychological health. Structural equation modeling was used to examine the direct and indirect effects of sleep quality on self-rated health through depressive and anxiety symptoms. Results: Students engaged in part-time employment (p = 0.022), who had poor perceived employment prospects (p = 0.009), and who did not participate in recreational sports (p = 0.008) had worse sleep quality. Structural equation modeling revealed a significant total effect of sleep quality on self-rated health (b = 0.592, p < 0.001), a significant direct effect of both sleep quality and depressive and anxiety symptoms on self-rated health (b = 0.277, 95% CI: 0.032–0.522), and a significant indirect effect of sleep quality on self-rated health through depressive and anxiety symptoms (b = 0.315, 95% CI: 0.174–0.457). Conclusions: Depressive and anxiety symptoms partially explain the association between sleep quality and self-rated health. Intervening upon sleep quality, depressive, and anxiety symptoms may bolster the self-rated health of healthcare students.
Keywords: sleep quality, self-rated health, anxiety, depression, mediation, healthcare students
1. Introduction
Sleep disorders have a global burden. Prior research has reported the prevalence of any sleep disorders to be 36.730% in the general population, 41.160% in college students, and even higher in healthcare students [1,2]. A meta-analysis of 50 studies that used the Pittsburgh Sleep Quality Index (PSQI) to quantify sleep quality revealed that the overall prevalence of poor sleep quality among healthcare student cohorts was 52.700% [2].
Previous studies have demonstrated a significant association between stress and low sleep quality—for healthcare students, and the main source of stress is academic demands [3]. Compared with college students in other specialties/majors, healthcare students are exposed to unique stressors and demands, including tough courses, demanding course content, long tenure in school, lack of leisure time, and excessive self-pressure for performance, all of which can lead to high levels of stress and low levels of sleep quality [4,5]. Moreover, due to the outbreak of the Coronavirus disease 2019 (COVID-19), several outbreak prevention and control measures (e.g., work stoppages, school closures, and closure management) ensued, all of which may have a negative impact on sleep among university students [6,7]. Not only that, due to lockdowns, going out for recreation or exercising became difficult [8]. Therefore, people are more likely to relax by playing games, watching videos, and using social media software, with sedentary behavior increasing substantially [9]. The extended use of electronic products also increases the risk of addiction. It has been shown that individuals addicted to the Internet have significantly less sleep time and lower sleep quality [10]. At the same time, the levels of stress, anxiety, and depression may also have enhanced which may have a significant impact on health [11,12].
Sleep, a biological necessity, has clear relevance for self-rated health [13]. The World Health Organization defines “health” as an optimal state of physical, mental, emotional, intellectual, and social being [14]. Common disease states which interfere with achieving optimal health, such as diabetes and obesity, are very prevalent worldwide in both adults and children [15]. Excessive or short sleep duration, difficulty falling asleep, and low levels of slow-wave sleep all are associated with an increased risk of type 2 diabetes [16,17]. A meta-analysis showed an increased risk of atherosclerosis, coronary heart disease, hypertension, and stroke in individuals with both short and excessively long sleep duration [18,19]. These are only some of the many examples of disrupted sleep being associated with reduced health status.
Disturbed sleep has been implicated in numerous psychiatric conditions (e.g., schizophrenia, affective disorders, depression, and Alzheimer’s disease) [20,21,22]. In fact, sleep disturbances have been reported in 30–80% of patients with schizophrenia, and improving sleep is one of the top reported priorities among people with schizophrenia [23]. Up to 90% of patients experiencing an acute depressive episode also report persistent sleep difficulties. Interestingly, clinical research suggests that changes in sleep may precede the occurrence of anxiety and depression, and not the reverse [24,25]. General college students have high rates of anxiety and depression, with even higher rates reported among healthcare students [26].
There is a strong rationale for greater attention to the sleep quality of healthcare students, as they will become essential healthcare workers in the near future. Due to socio-economic and cultural differences, the extant literature on sleep quality, depressive and anxiety symptoms, and self-rated health may not be applicable to individuals in China. The lack of applicable data makes it difficult to propose possible interventions to improve sleep quality among Chinese healthcare students [27]. Additionally, there is a dearth of research investigating how depressive and anxiety symptoms may explain the association between sleep quality and self-rated health among healthcare students. Hence, we aimed to investigate the following problems among Chinese healthcare students: (a) if sleep quality was associated with self-rated health, and (b) if depressive and anxiety symptoms explained any observed associations between sleep quality and self-rated health. We hypothesized that: (i) sleep quality would be positively associated with self-rated health, and (ii) depressive and anxiety symptoms would mediate the association between sleep quality and self-rated health. In other words, we investigated whether good sleep quality may reduce depressive and anxiety symptoms in healthcare students, which in turn may increase self-rated health.
2. Materials and Methods
2.1. Study Design and Procedure
The present study employed an observational, cross-sectional design. Surveys were applied using a paper-and-pencil self-administered method, and all design elements adhered to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines [28]. Healthcare students were recruited using a stratified random sampling method according to matriculation year and major from Hangzhou, China, during the fall semester of 2020. Data were collected during a low-risk COVID-19 infection period in the region of the school.
Data collection was conducted during breaks between classes, and all students who reported to class on data collection days were included. The exclusion criteria were as follows: (1) international students who could not fully understand and write Chinese; (2) students who were on suspension or long-term medical leave. Well-trained investigators notified potential participants of the research purpose before the survey, and verbal informed consent was obtained from all individual participants included in the study. All surveys were scanned for missing data upon completion, and any identified missing data were completed before the participant was compensated for time. Each participant received CNY 2 (around USD 0.300) upon completion of the survey as compensation for their time. Participants could withdraw from the study at any point.
2.2. Measures
2.2.1. Sleep Quality Questionnaire (Chinese Version)
The Sleep Quality Questionnaire (SQQ) was developed to assess sleep quality in non-clinical populations over the previous month. It is composed of 10 items and two subscales: Daytime Sleepiness Subscale (DSS) (e.g., “I sometimes felt sleepy during the day”) and Sleep Difficulty Subscale (SDS) (e.g., “I felt like I did not get a deep sleep”) [29]. Responses are reported on a five-point Likert scale (from “0 = strongly agree” to “4 = strongly disagree”), with total scores ranging from 0 to 40, with higher scores indicating poorer sleep quality. The SQQ has shown good measurement properties (i.e., reliability, internal consistency, construct validity, criterion validity, and content validity) and stable two-factor structure (i.e., measurement invariance) in large multicenter studies [29,30,31,32,33].
2.2.2. Patient Health Questionnaire (Chinese Version)
The four-item Patient Health Questionnaire (PHQ-4), composed of the two-item Patient Health Questionnaire and the two-item Generalized Anxiety Disorder scale (GAD), is used to assess depressive and anxiety symptoms during the past two weeks [34]. Participants rated how often they experienced each of the four items on a four-point Likert scale ranging from 0 (“not at all”) to 3 (“nearly every day”), with higher scores indicating more depressive and anxiety symptoms [35]. The Chinese version of the PHQ-4 (retrieved from: https://www.phqscreeners.com; accessed on 29 August 2019) has shown acceptable internal consistency [Cronbach’s α = 0.870 (95% CI: 0.852–0.886)] [30].
2.2.3. Self-Rated Health Questionnaire
Self-rated health was assessed with a simple, two-item questionnaire that included an item focused on self-rated physical health and an item focused on self-rated mental health. Each item response was recorded on a five-point Likert scale (“1 = excellent, 2 = good, 3 = average, 4 = poor, and 5 = extremely poor”). Total scores represent the numerical sum of both items and range from 2 to 10, with higher scores representing poorer overall self-rated health. The Cronbach’s α of the Self-Rated Health Questionnaire (SRHQ) was 0.706 in this wave.
2.2.4. Sample Description
The following sample variables were collected: gender (male, female), age (<20, ≥20), home location (urban, rural, or suburban), only child (yes, no), academic year (first year, second year, or third year), family income (<CNY 10,000, ≥CNY 10,000; unit: CNY 1 ≈ USD 0.150), part-time employment (yes, no), leisure time sports involvement (yes, no), perceived employment prospects (excellent, good, average, poor, or extremely poor), engagement in hobbies (yes, no), preferred coping strategies (actively cope, push through, or ignore problems), and academic major (clinical medicine, preventive medicine, nursing, pharmacy, health policy and management, health services and management, or master of medicine).
2.3. Statistical Analysis
The database was built in EpiData (version 3.1) software. Statistical analysis was conducted with R (version 4.1.2) and JASP (version 0.16.1). For missing values (0.229%), continuous variables were replaced by mean (i.e., age) and categorical variables were replaced by median (e.g., gender, home location, and academic year) [36]. A one-sample t-test and one-way analysis of variance (ANOVA) were used to compare differences in the SQQ scores between subgroups (e.g., academic year and part-time employment). Spearman’s correlation was used to evaluate the association among the SQQ, PHQ-4, and SRHQ.
A structural equation model (SEM) was used to model the direct, indirect, and total effects of sleep quality on self-rated health, and whether depressive and anxiety symptoms explained any observed associations. First, the direct effects of sleep quality on self-rated health were estimated. If the direct effects were significant, the mediating variables (i.e., depressive and anxiety symptoms) were added to the model, allowing for analyses of indirect effects and total effects. A bias-corrected (percentile method) bootstrap procedure (1000 bootstrap procedures) was used to estimate the model parameters. To assess the goodness-of-fit of the models, we used the following threshold values of fit indices: Chi-square/degree of freedom (χ2/df): 2.000–3.000, Root Mean Square Error of Approximation (RMSEA) < 0.080, Standardized Root Mean Residual (SRMR) < 0.080, Goodness of Fit Index (GFI) > 0.900, Tucker–Lewis Index (TLI) > 0.900, Comparative Fit Index (CFI) > 0.900, Adjusted Goodness-of-Fit Index (AGFI) > 0.500, and Parsimony Normed Fit Index (PNFI) > 0.500 [37,38,39].
3. Results
3.1. Sample Characteristics
After removing invalid questionnaires (e.g., selecting one option for the entire page of the questionnaire), the final sample was 637. Three-quarters of the respondents were female, and 40% of the students were an only child. The number of those who had no part-time employment (82.732%) was significantly higher than the number who did have outside employment (17.268%). A total of 84.144% of the respondents had a “good” and “average” attitude toward employment prospects. Worse sleep quality was found in students who were: less than 20 years of age (p = 0.007); sophomores (p = 0.034); participated in part-time jobs (p = 0.022); did not engage in leisurely sports (p = 0.008); had relatively low perceived employment prospects (p = 0.009); had no hobbies (p = 0.014); and preferred ignoring problems as a coping strategy (p < 0.001) (Table 1).
Table 1.
Characteristics of participants (n = 637).
| Variable | n (%) | SQQ Total | Statistics | |||
|---|---|---|---|---|---|---|
| Mean | SD | df | t/F | p | ||
| Gender | 1 | 2.382 | 0.123 | |||
| Male | 156 (24.490) | 17.462 | 6.539 | |||
| Female | 481 (75.510) | 18.345 | 6.104 | |||
| Age | 1 | 7.326 | 0.007 | |||
| <20 | 458 (71.900) | 18.544 | 6.187 | |||
| ≥20 | 179 (28.100) | 17.067 | 6.194 | |||
| Home location | 2 | 2.528 | 0.081 | |||
| Urban | 246 (38.619) | 17.622 | 6.064 | |||
| Rural | 236 (37.049) | 18.055 | 6.300 | |||
| Suburban | 155 (24.333) | 19.045 | 6.280 | |||
| Only child | 1 | 2.396 | 0.122 | |||
| Yes | 257 (40.345) | 17.665 | 6.273 | |||
| No | 380 (59.655) | 18.442 | 6.172 | |||
| Academic year | 2 | 3.386 | 0.034 | |||
| First year | 274 (43.014) | 17.810 | 6.464 | |||
| Second year | 161 (25.275) | 19.224 | 5.967 | |||
| Third year | 202 (31.711) | 17.688 | 6.002 | |||
| Family income | 1 | 0.040 | 0.842 | |||
| <CNY 10,000 | 261 (40.973) | 18.188 | 6.205 | |||
| ≥CNY 10,000 | 376 (59.027) | 18.088 | 6.238 | |||
| Part-time employment | 1 | 5.276 | 0.022 | |||
| Yes | 110 (17.268) | 19.364 | 5.967 | |||
| No | 527 (82.732) | 17.871 | 6.246 | |||
| Leisure time sports involvement | 1 | 7.068 | 0.008 | |||
| Yes | 316 (49.608) | 17.472 | 6.314 | |||
| No | 321 (50.392) | 18.776 | 6.067 | |||
| Perceived employment prospects | 4 | 3.431 | 0.009 | |||
| Excellent | 56 (8.791) | 17.982 | 7.129 | |||
| Good | 347 (54.474) | 17.715 | 5.996 | |||
| Average | 189 (29.670) | 18.228 | 6.340 | |||
| Poor | 39 (6.122) | 21.564 | 5.389 | |||
| Extremely poor | 6 (0.942) | 18.000 | 6.099 | |||
| Engagement in hobbies | 1 | 6.133 | 0.014 | |||
| Yes | 451 (70.801) | 17.738 | 6.338 | |||
| No | 186 (29.199) | 19.075 | 5.831 | |||
| Preferred coping strategies | 2 | 22.558 | <0.001 | |||
| Active copy | 375 (58.870) | 18.664 | 5.793 | |||
| Push through | 211 (33.124) | 16.237 | 6.240 | |||
| Ignore problems | 51 (8.006) | 22.020 | 6.701 | |||
| Academic major | 6 | 1.483 | 0.181 | |||
| Clinical medicine | 127 (18.937) | 18.378 | 6.279 | |||
| Preventive medicine | 98 (15.385) | 18.612 | 5.452 | |||
| Nursing | 93 (14.600) | 18.774 | 6.216 | |||
| Pharmacy | 95 (14.914) | 18.789 | 5.909 | |||
| Health policy and management | 87 (13.658) | 17.471 | 6.077 | |||
| Health services and management | 76 (11.931) | 17.566 | 6.616 | |||
| Master of Medicine | 61 (9.576) | 16.459 | 7.208 | |||
SD, Standard Deviation; df, degrees of freedom; SQQ Total, Total score of the Sleep Quality Questionnaire; Family income unit: CNY 1 ≈ USD 0.150.
3.2. Associations among Sleep Quality, Mental Health Symptoms, and Self-Rated Health
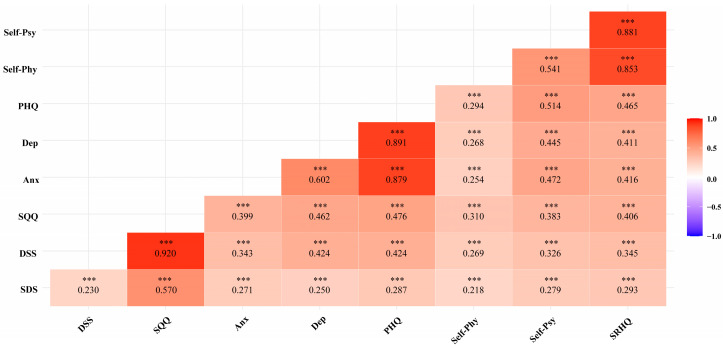
The Spearman’s correlation coefficients for scores among the SQQ, PHQ-4, and SRHQ were all clustered around 0.400 and 0.500. The coefficients between the scores of the SQQ and PHQ-4 (r = 0.476), between the PHQ-4 and SRHQ (r = 0.465), and between the SQQ and SRHQ (r = 0.406) were all of the moderate/large magnitudes. Please see Figure 1 for a full list of the correlation coefficients.
Figure 1.
Spearman’s correlation matrix of the SQQ, PHQ, and SRHQ. Note: SDS, Sleep Difficulty Subscale; DSS, Daytime Sleepiness Subscale; SQQ, Sleep Quality Questionnaire; Anx, Anxiety; Dep, Depression; PHQ, Patient Health Questionnaire; Self-Phy, Self-Rated Physical Condition; Self-Psy, Self-Rated Psychological Condition; SRHQ, Self-Rated Health Questionnaire; *** p < 0.001.
3.3. Structural Equation Model: Direct, Indirect, and Total Effects of Sleep Quality on Self-Rated Health through Mental Health Symptom
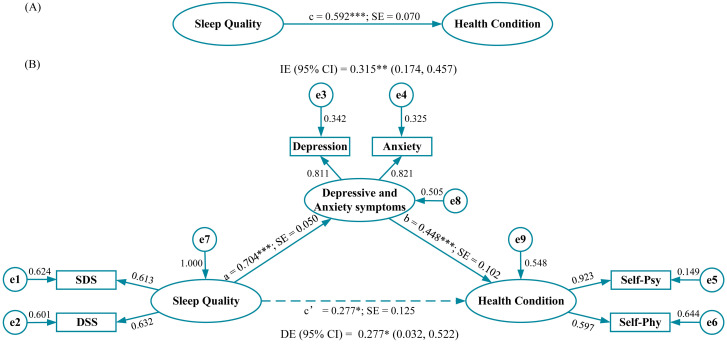
The total effect of sleep quality on self-rated health was 0.592 (p < 0.001) (Figure 2A). Standardized regression coefficients between sleep quality, depressive and anxiety symptoms, and self-rated health are displayed in Figure 2B. Statistical significant paths were observed between sleep quality and depressive and anxiety symptoms (a = 0.704), and between depressive and anxiety symptoms and self-rated health (b = 0.448). The direct effect between sleep quality and self-rated health, accounting for depressive and anxiety symptoms, was 0.227 (95% CI: 0.032–0.522, p < 0.050). The indirect effect of sleep quality on self-rated health through depressive and anxiety symptoms was 0.315 (95% CI: 0.174–0.457, p < 0.010). The fit of the model was excellent (RMSEA = 0.069, SRMR = 0.027, GFI = 0.987, χ2/df = 4.075, TLI = 0.959, CFI = 0.984, AGFI = 0.955, and PNFI = 0.391), except for the PNFI of 0.391 which was slightly below the threshold (Table 2).
Figure 2.
Path coefficients for simple mediation analysis on sleep quality (n = 637). (A) The total effect of sleep quality on health condition and (B) the effect of sleep quality on self-rated health when anxiety and depression are included as a mediator. Note: Dotted line represents the effect of sleep quality on health condition when anxiety and depression are included as a mediator. Factor loadings are standardized. a, b, c, and c’, standardized regression coefficients; e, measurement errors; SDS, Sleep Difficulty Subscale; DSS, Daytime Sleepiness Subscale; Self-Psy, Self-Rated Psychological Condition; Self-Phy, Self-Rated Physical Condition; SE, Standard Error; IE, Indirect Effect; DE, Direct Effect; *** p < 0.001; ** p < 0.010; * p < 0.050.
Table 2.
Evaluation of the goodness-of-fit of the models (n = 637).
| GOF Index | Mediation Model | Threshold |
|---|---|---|
| Absolute measures | ||
| RMSEA (90% CI) | 0.069 (0.042, 0.099) | <0.080 |
| SRMR | 0.027 | <0.080 |
| GFI | 0.987 | >0.900 |
| χ2/df | 4.075 | 2.000–3.000 |
| Incremental fit measures | ||
| TLI | 0.959 | >0.900 |
| CFI | 0.984 | >0.900 |
| Parsimony measures | ||
| AGFI | 0.955 | >0.900 |
| PNFI | 0.391 | >0.500 |
GOF, goodness-of-fit; RMSEA, Root Mean Square Error of Approximation; SRMR, Standardized Root Mean Residual; GFI, Goodness-of-Fit Index; χ2, Chi-square; df, degree of freedom; TLI, Tucker–Lewis Index; CFI, Comparative Fit Index; AGFI, Adjusted Goodness-of-Fit Index; PNFI, Parsimony Normed Fit Index; CI, Confidence Interval.
4. Discussion
Our study had three main findings: (i) depressive and anxiety symptoms, and a host of descriptive characteristics (such as perceived employment prospects, academic year, family income, and leisure time sports involvement) were associated with sleep quality; (ii) associations among sleep quality, depressive and anxiety symptoms, and self-rated health all were statistically significant (and of moderate/strong strength); and (iii) sleep quality was positively associated with self-rated health; depressive and anxiety symptoms mediated the relationship between sleep quality and self-rated health.
Lower sleep quality among healthcare students has been well-documented and the present study replicated these previous findings [40,41]. The results showed that sleep quality was lower for an individual with poor perceived employment prospects. Unstable working conditions and unemployment may disrupt sleep by promoting anxiety about the future (i.e., insecurity) [42,43]. Raising the employment expectations of those located at the margins of the labor market may be beneficial in preventing the widening of employment-related health inequalities [44]. Although participation in part-time employment and sleep outcomes have been understudied, a German study found that men with part-time employment were more likely to have sleep difficulties than individuals with full-time employment [45]. Whether part-time employment itself or other factors are responsible for the decrease in sleep quality is unknown, and further research is needed. We have also found that engagement in leisure time physical activity was associated with sleep quality. Improvement in sleep quality resulting from exercise is well documented. Moderate aerobic exercise training is recommended as a non-pharmacological treatment option for people with poor sleep [46].
Consistent with previous research, poorer sleep quality was associated with depressive and anxiety symptoms. Previous research has shown that sleep disturbance is a strong predictor of subsequent affective disorders, anxiety, and suicide in longitudinal studies [47]. Importantly, the reduction in sleep problems has been shown to be effective in reducing the incidence of depression at one-year follow-ups [48]. As such, a body of evidence now suggests that sleep disorders often occur prior to depressive and anxiety symptoms and may be a prodromal symptom of subsequent mental disorders. Timely intervention for sleep disorders may prevent the subsequent onset or exacerbation of depressive and anxiety symptoms. Consistent with our findings, prevention and intervention of sleep disorders may be the most appropriate and cost-effective way to reduce the rate of depression and anxiety [49].
The effect of sleep quality on self-rated health was shown to be partially mediated through depressive and anxiety symptoms. Importantly, self-rated health is a good measure of objective and subjective health and has documented high reliability [50]. Self-rated health has also been shown to be significantly associated with many important medical endpoints (e.g., health risk behaviors, disease states, disability, and mortality) [50]. Healthcare students, a group with increased levels of medical knowledge and relatively high sensitivity to physical conditions, may be more likely to perceive their own physical and mental health conditions—they may be more self-aware [51]. Previous research has shown that people with psychological complaints tend to have lower ratings of their health status [52,53]. Numerous previous studies have shown that common psychological problems (e.g., depression and anxiety) are associated with self-rated health [54,55,56,57,58]. Novel to our current study, we found that depressive and anxiety symptoms partially explain the link between sleep and self-rated health. Although causal inferences cannot be drawn from this study directly, the role of depressive and anxiety symptoms in the link between sleep quality and self-rated health is noteworthy. Future work should examine methods to improve sleep in healthcare students as a means to also target associated mental health and physical health conditions [59].
4.1. Strengths and Limitations
The present study has several strengths. The survey was conducted in person, allowing for visual confirmation that study participants were drawn from the desired subject pool. Additionally, we were able to quickly scan paper documents to identify and address sources of potential missing data. The sample size of the study was large and included a diverse set of healthcare students. Lastly, this study examines a potential process, namely, depressive and anxiety symptoms, through which poor sleep quality may be exerting its effects on self-rated health. This is an important step in moving the literature forward.
There are also several disadvantages of the present investigation. First, given the study design, it is not possible to draw causal conclusions. Second, all data were obtained through subjective assessments, as opposed to objective measures, which has the potential to result in a self-reporting bias. Third, the SRHQ, as a self-developed questionnaire, needs further validation for its measurement properties. Fourth, the survey was conducted during COVID-19, but no COVID-19-related information was collected to understand the current impact of COVID-19 policy on healthcare students. Finally, as this study only enrolled healthcare students, the sample is relatively homogeneous and the study findings may not generalize to non-healthcare student samples.
4.2. Future Directions
Subsequent studies would be well suited to collect longitudinal measurements in order to further elucidate causality. Longitudinal data are necessary to model the complex interplay of dynamic changes in sleep quality, depressive and anxiety symptoms, and health. Secondly, our results suggest partial mediation of the effects of sleep quality on self-rated health through depressive and anxiety symptoms, suggesting the presence of other mediators that should be further explored [60]. Lastly, future research should continue to recruit increasingly diverse samples to ensure that our studies apply to traditionally under-represented individuals.
5. Conclusions
Sleep quality is associated with self-rated health and this association partially works through increased levels of depressive and anxiety symptoms. Healthcare students face numerous demands and experience poor sleep, heightened levels of depressive and anxiety symptoms, and low self-rated health. Sleep health education programs and routine screening with the SQQ may be possible mitigation strategies. Future research should examine longitudinal changes in sleep quality, depressive and anxiety symptoms, and self-rated health, as well as begin the process of development and initial testing of potential sleep health interventions. Compromises in the health of future healthcare providers could have dire consequences for large swaths of the population.
Acknowledgments
The authors would like to thank the study participants and the research assistants for their contributions. In addition, the authors are grateful to editors and two reviewers for their precious opinions and suggestions.
Author Contributions
Conceptualization, R.M.; methodology, R.M.; software, C.J. and R.M.; validation, C.J., J.M.D., K.S., Y.Z. and R.M.; formal analysis, C.J., Y.Z., J.M.D. and R.M.; investigation, R.M.; resources, H.M. and R.M.; data curation, R.M., Y.Z., C.J., Y.Y., M.H., H.G., Y.R., T.L. and H.M.; writing—original draft preparation, Y.Z. and C.J.; writing—review and editing, J.M.D., K.S., C.J., Y.Z., B.Z., B.A.O. and R.M.; visualization, C.J.; supervision, R.M.; project administration, R.M.; funding acquisition, R.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study has been reviewed and approved by the Institutional Review Board of Hangzhou Normal University Division of Health Sciences, China (reference no. 20190076), thus ensuring that it adhered to the standards set by the Declaration of Helsinki.
Informed Consent Statement
Admittedly, this study was eligible for exempt review and use of a formal informed consent form containing all the elements of consent is not required for research under exempt review. All healthcare students freely consented to answer the questionnaires and provided their verbal informed consent before data collection. The authors confirmed full respect and protection of individual privacy rights before, during, and after the data collection and processing.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This study was funded by the Medical Research Fund of Zhejiang Province, grant number 2023RC073, and the Research Initiation Fund of Hangzhou Normal University, grant number RWSK20201003.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Jahrami H.A., Alhaj O.A., Humood A.M., Alenezi A.F., Fekih-Romdhane F., AlRasheed M.M., Saif Z.Q., Bragazzi N.L., Pandi-Perumal S.R., BaHammam A.S., et al. Sleep disturbances during the COVID-19 pandemic: A systematic review, meta-analysis, and meta-regression. Sleep Med. Rev. 2022;62:101591. doi: 10.1016/j.smrv.2022.101591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rao W.-W., Li W., Qi H., Hong L., Chen C., Li C.-Y., Ng C.H., Ungvari G.S., Xiang Y.-T. Sleep quality in medical students: A comprehensive meta-analysis of observational studies. Sleep Breath. 2020;24:1151–1165. doi: 10.1007/s11325-020-02020-5. [DOI] [PubMed] [Google Scholar]
- 3.Almojali A.I., Almalki S.A., Alothman A.S., Masuadi E.M., Alaqeel M.K. The prevalence and association of stress with sleep quality among medical students. J. Epidemiol. Glob. Health. 2017;7:169–174. doi: 10.1016/j.jegh.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Damiano R.F., de Oliveira I.N., da Ezequiel O.S., Lucchetti A.L., Lucchetti G. The root of the problem: Identifying major sources of stress in Brazilian medical students and developing the Medical Student Stress Factor Scale. Braz. J. Psychiatry. 2021;43:35–42. doi: 10.1590/1516-4446-2019-0824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiang C., Mastrotheodoros S., Zhu Y., Yang Y., Hallit S., Zhao B., Fan Y., Huang M., Chen C., Ma H., et al. The Chinese Version of the Perceived Stress Questionnaire-13: Psychometric Properties and Measurement Invariance for Medical Students. Psychol. Res. Behav. Ma. 2023;16:71–83. doi: 10.2147/PRBM.S385510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yin F., Chen C., Song S., Chen Z., Jiao Z., Yan Z., Yin G., Feng Z. Factors Affecting University Students’ Sleep Quality during the Normalisation of COVID-19 Epidemic Prevention and Control in China: A Cross-Sectional Study. Sustainability. 2022;14:10646. doi: 10.3390/su141710646. [DOI] [Google Scholar]
- 7.Viselli L., Salfi F., D’Atri A., Amicucci G., Ferrara M. Sleep Quality, Insomnia Symptoms, and Depressive Symptomatology among Italian University Students before and during the COVID-19 Lockdown. Int. J. Env. Res. Public Health. 2021;18:13346. doi: 10.3390/ijerph182413346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kowalsky R.J., Farney T.M., Kline C.E., Hinojosa J.N., Creasy S.A. The impact of the covid-19 pandemic on lifestyle behaviors in U.S. college students. J. Am. Coll. Health. 2021:1–6. doi: 10.1080/07448481.2021.1923505. [DOI] [PubMed] [Google Scholar]
- 9.Meyer J., McDowell C., Lansing J., Brower C., Smith L., Tully M., Herring M. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 US Adults. Int. J. Env. Res. Public Health. 2020;17:6469. doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alimoradi Z., Lin C.-Y., Broström A., Bülow P.H., Bajalan Z., Griffiths M.D., Ohayon M.M., Pakpour A.H. Internet addiction and sleep problems: A systematic review and meta-analysis. Sleep Med. Rev. 2019;47:51–61. doi: 10.1016/j.smrv.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Zhong Y., Ma H., Liang Y.F., Liao C.J., Zhang C.C., Jiang W.J. Prevalence of smartphone addiction among Asian medical students: A meta-analysis of multinational observational studies. Int. J. Soc. Psychiatry. 2022;68:1171–1183. doi: 10.1177/00207640221089535. [DOI] [PubMed] [Google Scholar]
- 12.Elmer T., Mepham K., Stadtfeld C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE. 2020;15:e0236337. doi: 10.1371/journal.pone.0236337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steptoe A., Peacey V., Wardle J. Sleep Duration and Health in Young Adults. Arch. Int. Med. 2006;166:1689–1692. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 14.Park S., Lee Y., Yoo M., Jung S. Wellness and sleep quality in Korean nursing students: A cross-sectional study. Appl. Nurs. Res. 2019;48:13–18. doi: 10.1016/j.apnr.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 15.Cappuccio F.P., Taggart F.M., Kandala N.-B., Currie A., Peile E., Stranges S., Miller M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cappuccio F.P., D’Elia L., Strazzullo P., Miller M.A. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2010;33:414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tasali E., Leproult R., Ehrmann D.A., Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc. Natl. Acad. Sci. USA. 2008;105:1044–1049. doi: 10.1073/pnas.0706446105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cappuccio F.P., Cooper D., D’Elia L., Strazzullo P., Miller M.A. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur. Heart J. 2011;32:1484–1492. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 19.Gottlieb D.J., Redline S., Nieto F.J., Baldwin C.M., Newman A.B., Resnick H.E., Punjabi N.M. Association of Usual Sleep Duration With Hypertension: The Sleep Heart Health Study. Sleep. 2006;29:1009–1014. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 20.Wulff K., Gatti S., Wettstein J.G., Foster R.G. Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat. Rev. Neurosci. 2010;11:589–599. doi: 10.1038/nrn2868. [DOI] [PubMed] [Google Scholar]
- 21.Baglioni C., Nanovska S., Regen W., Spiegelhalder K., Feige B., Nissen C., Reynolds Iii C.F., Riemann D. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol. Bull. 2016;142:969–990. doi: 10.1037/bul0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kahn-Greene E.T., Killgore D.B., Kamimori G.H., Balkin T.J., Killgore W.D.S. The effects of sleep deprivation on symptoms of psychopathology in healthy adults. Sleep Med. 2007;8:215–221. doi: 10.1016/j.sleep.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 23.Cohrs S. Sleep Disturbances in Patients with Schizophrenia. CNS Drugs. 2008;22:939–962. doi: 10.2165/00023210-200822110-00004. [DOI] [PubMed] [Google Scholar]
- 24.Posmontier B. Sleep quality in women with and without postpartum depression. J. Obst. Gyn. Neo. 2008;37:722–737. doi: 10.1111/j.1552-6909.2008.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Monti J.M., Monti D. Sleep disturbance in generalized anxiety disorder and its treatment. Sleep Med. Rev. 2000;4:263–276. doi: 10.1053/smrv.1999.0096. [DOI] [PubMed] [Google Scholar]
- 26.Dahlin M., Joneborg N., Runeson B. Stress and depression among medical students: A cross-sectional study. Med. Educ. 2005;39:594–604. doi: 10.1111/j.1365-2929.2005.02176.x. [DOI] [PubMed] [Google Scholar]
- 27.Sun Y., Wang H., Jin T., Qiu F., Wang X. Prevalence of Sleep Problems Among Chinese Medical Students: A Systematic Review and Meta-Analysis. Front. Psychiatry. 2022;13:753419. doi: 10.3389/fpsyt.2022.753419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P., Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull. World. Health. Organ. 2007;85:867–872. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kato T. Development of the Sleep Quality Questionnaire in healthy adults. J. Health Psychol. 2014;19:977–986. doi: 10.1177/1359105313482168. [DOI] [PubMed] [Google Scholar]
- 30.Luo Y., Fei S., Gong B., Sun T., Meng R. Understanding the Mediating Role of Anxiety and Depression on the Relationship Between Perceived Stress and Sleep Quality Among Health Care Workers in the COVID-19 Response. Nat. Sci. Sleep. 2021;13:1747–1758. doi: 10.2147/NSS.S313258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meng R., Kato T., Mastrotheodoros S., Dong L., Fong D.Y.T., Wang F., Cao M., Liu X., Yao C., Cao J., et al. Adaptation and validation of the Chinese version of the Sleep Quality Questionnaire. Qual. Life Res. 2022 doi: 10.1007/s11136-022-03241-9. [DOI] [PubMed] [Google Scholar]
- 32.Meng R. Ph.D. Dissertation. Wuhan University; Wuhan, China: 2020. Development and Evaluation of the Chinese Version of the Sleep Quality Questionnaire. (In Chinese) [Google Scholar]
- 33.Meng R., Lau E.Y.Y., Spruyt K., Miller C.B., Dong L. Assessing Measurement Properties of a Simplified Chinese Version of Sleep Condition Indicator (SCI-SC) in Community Residents. Behav. Sci. 2022;12:433. doi: 10.3390/bs12110433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spitzer R.L., Kroenke K., Williams J.B.W. Validation and Utility of a Self-report Version of PRIME-MDThe PHQ Primary Care Study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K., Spitzer R.L., Williams J.B.W., Löwe B. An Ultra-Brief Screening Scale for Anxiety and Depression: The PHQ–4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 36.Buhi E.R., Goodson P., Neilands T.B. Out of sight, not out of mind: Strategies for handling missing data. Am. J. Health Behav. 2008;32:83–92. doi: 10.5993/AJHB.32.1.8. [DOI] [PubMed] [Google Scholar]
- 37.Joseph F., Hair W.C.B., Babin B.J., Anderson R.E. Multivariate Data Analysis: Pearson New International Edition. 7th ed. Pearson; London, UK: 2009. [Google Scholar]
- 38.Kline R.B. Principles and Practice of Structural Equation Modeling. 4th ed. Guilford Publications; New York, NY, USA: 2015. [Google Scholar]
- 39.Mulaik S.A., James L.R., Van Alstine J., Bennett N., Lind S., Stilwell C.D. Evaluation of goodness-of-fit indices for structural equation models. Psychol. Bull. 1989;105:430–445. doi: 10.1037/0033-2909.105.3.430. [DOI] [Google Scholar]
- 40.Lukowski A.F., Karayianis K.A., Kamliot D.Z., Tsukerman D. Undergraduate Student Stress, Sleep, and Health before and during the COVID-19 Pandemic. Behav. Med. 2022. ahead of print . [DOI] [PubMed]
- 41.Liu B., Gao F., Zhang J., Zhou H., Sun N., Li L., Liang L., Ning N., Wu Q., Zhao M. Sleep Quality of Students from Elementary School to University: A Cross-Sectional Study. Nat. Sci. Sleep. 2020;12:855–864. doi: 10.2147/NSS.S266493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mai Q.D., Jacobs A.W., Schieman S. Precarious sleep? Nonstandard work, gender, and sleep disturbance in 31 European countries. Soc. Sci. Med. 2019;237:112424. doi: 10.1016/j.socscimed.2019.112424. [DOI] [PubMed] [Google Scholar]
- 43.Grandner M.A., Patel N.P., Gehrman P.R., Xie D., Sha D., Weaver T., Gooneratne N. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11:470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Virtanen P., Vahtera J., Broms U., Sillanmäki L., Kivimäki M., Koskenvuo M. Employment trajectory as determinant of change in health-related lifestyle: The prospective HeSSup study. Eur. J. Public Health. 2008;18:504–508. doi: 10.1093/eurpub/ckn037. [DOI] [PubMed] [Google Scholar]
- 45.Kretschmer V., Riedel N. Effects of atypical employment on difficulties in falling asleep and maintaining sleep—Gender differences in the lidA study. Gesundheitswesen. 2015;77:e77–e84. doi: 10.1055/s-0034-1398600. [DOI] [PubMed] [Google Scholar]
- 46.Chennaoui M., Arnal P.J., Sauvet F., Léger D. Sleep and exercise: A reciprocal issue? Sleep Med. Rev. 2015;20:59–72. doi: 10.1016/j.smrv.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 47.Johnson E.O., Roth T., Breslau N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. J. Psychiatr. Res. 2006;40:700–708. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 48.Eaton W.W., Badawi M., Melton B. Prodromes and precursors: Epidemiologic data for primary prevention of disorders with slow onset. Am. J. Psychiatry. 1995;152:967–972. doi: 10.1176/ajp.152.7.967. [DOI] [PubMed] [Google Scholar]
- 49.Alvaro P.K., Roberts R.M., Harris J.K. A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression. Sleep. 2013;36:1059–1068. doi: 10.5665/sleep.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hull T.H. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications [Book Review] J. Popul. Res. 2007;24:133. doi: 10.1007/BF03031882. [DOI] [Google Scholar]
- 51.Latas M., Stojković T., Ralić T., Jovanović S., Spirić Z., Milovanović S. Medical students’ health-related quality of life—A comparative study. Vojnosanit. Pregl. 2014;71:751–756. doi: 10.2298/VSP1408751L. [DOI] [PubMed] [Google Scholar]
- 52.Maharlouei N., Akbari M., Khabbaz Shirazy M., Yazdanpanah D., Lankarani K.B. Factors associated with self-rated health status in Southwestern Iran: A population-based study. Public Health. 2016;140:179–185. doi: 10.1016/j.puhe.2016.06.027. [DOI] [PubMed] [Google Scholar]
- 53.Maguire P.A., Reay R.E., Raphael B. Correlates of a single-item Self-Rated Mental Health Question in people with schizophrenia. Australas Psychiatry. 2016;24:473–477. doi: 10.1177/1039856216638789. [DOI] [PubMed] [Google Scholar]
- 54.Sun W., Watanabe M., Tanimoto Y., Shibutani T., Kono R., Saito M., Usuda K., Kono K. Factors associated with good self-rated health of non-disabled elderly living alone in Japan: A cross-sectional study. BMC Public Health. 2007;7:297. doi: 10.1186/1471-2458-7-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Demirchyan A., Thompson M.E. Determinants of self-rated health in women: A population-based study in Armavir Marz, Armenia, 2001 & 2004. Int. J. Equity Health. 2008;7:25. doi: 10.1186/1475-9276-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu Z., Su H., Zou Y., Chen J., Wu J., Chang W. Self-rated health of Chinese adolescents: Distribution and its associated factors. Scand J. Caring. Sci. 2011;25:780–786. doi: 10.1111/j.1471-6712.2011.00893.x. [DOI] [PubMed] [Google Scholar]
- 57.Haddock C.K., Poston W.S.C., Pyle S.A., Klesges R.C., Vander Weg M.W., Peterson A., Debon M. The validity of self-rated health as a measure of health status among young military personnel: Evidence from a cross-sectional survey. Health Qual. Life Out. 2006;4:57. doi: 10.1186/1477-7525-4-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Haseli-Mashhadi N., Pan A., Ye X., Wang J., Qi Q., Liu Y., Li H., Yu Z., Lin X., Franco O.H. Self-Rated Health in middle-aged and elderly Chinese: Distribution, determinants and associations with cardio-metabolic risk factors. BMC Public Health. 2009;9:368. doi: 10.1186/1471-2458-9-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yeo S.C., Jos A.M., Erwin C., Lee S.M., Lee X.K., Lo J.C., Chee M.W.L., Gooley J.J. Associations of sleep duration on school nights with self-rated health, overweight, and depression symptoms in adolescents: Problems and possible solutions. Sleep Med. 2019;60:96–108. doi: 10.1016/j.sleep.2018.10.041. [DOI] [PubMed] [Google Scholar]
- 60.Zhao X., Lynch J.G., Jr., Chen Q. Reconsidering Baron and Kenny: Myths and Truths about Mediation Analysis. J. Consum. Res. 2010;37:197–206. doi: 10.1086/651257. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.