With the 2010 passage of the Patient Protection and Affordable Care Act, CMS (Centers for Medicare and Medicaid Services) announced its intent to implement the HRRP (Hospital Readmissions Reduction Program). The HRRP is a Medicare value-based purchasing program designed to encourage hospitals to improve the quality of care by penalizing avoidable readmissions within 30 days of hospital discharge in patients with certain conditions. Hospitals with higher-than-expected all-cause readmissions in patients recently hospitalized with heart failure, pneumonia, or myocardial infarction received reduced Medicare reimbursements starting in October 2012. In October 2014, hospitalizations for chronic obstructive pulmonary disease (COPD) exacerbations were included in the CMS HRRP. Since then, health systems have been left with the task of adapting to this policy change.
When analyzing health policy and associated evidence, it is helpful to frame the stakeholders and relationships with an established conceptual framework, such as the Andersen model for healthcare usage (1), providing a schematic of intrinsic and external factors that may influence the outcomes (e.g., quality of care, readmissions, and costs of care) (Figure 1). Policies like HRRP do not exist in a vacuum; they influence health system behaviors and available resources to provide care, which in turn influence health outcomes beyond readmissions or expenditures, including mortality. Indirectly, policy decisions may influence patient perceptions of the health system and provider quality and change care-seeking behaviors, inducing a feedback loop on the availability of resources.
Figure 1.
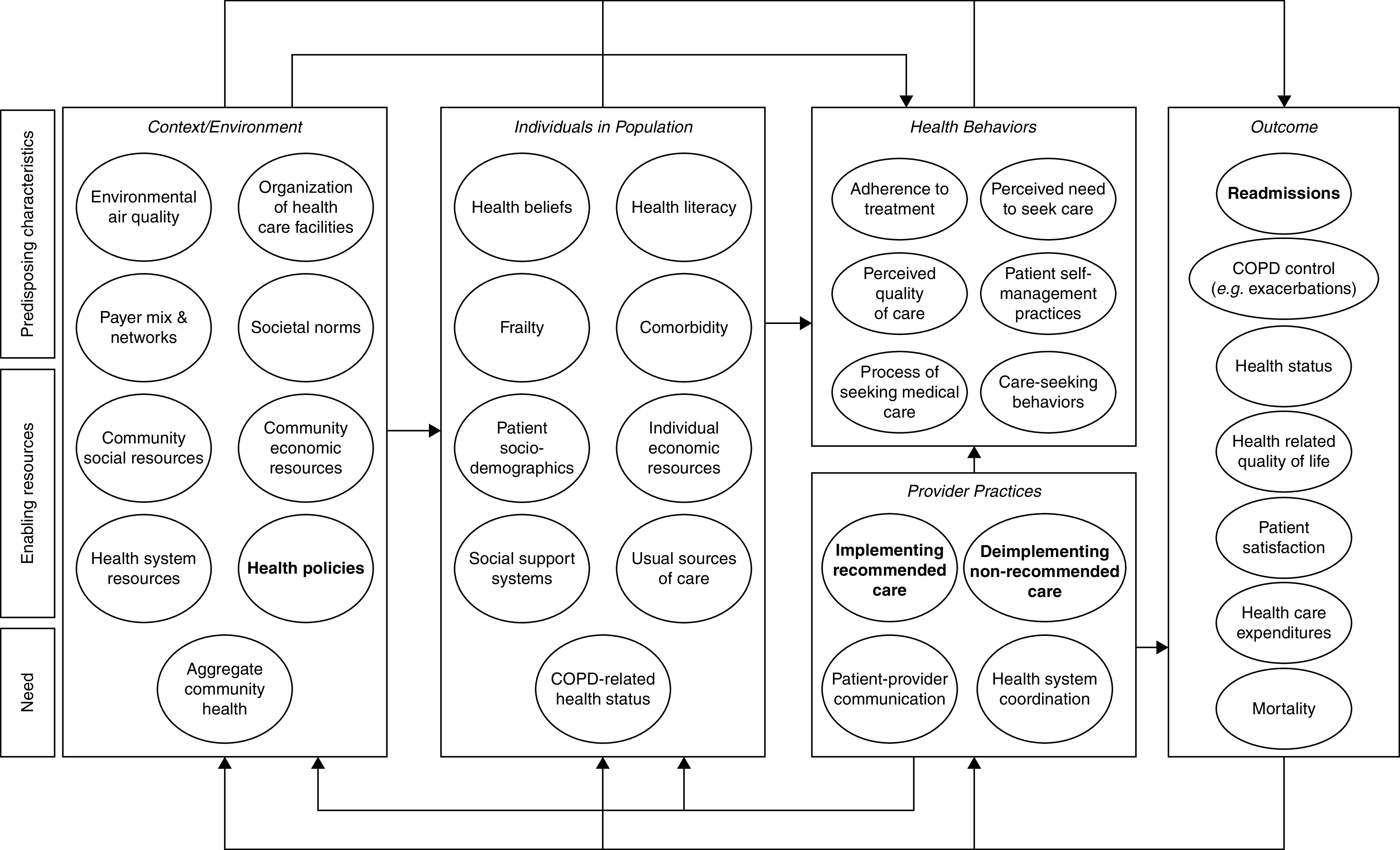
Adapted Andersen model (1) for healthcare usage. Rectangles represent domains with directional arrows representing potentially attributable relationships. Ovals represent nonexhaustive components within domains, which may also influence one another within the domain. Notably, feedback loops are also present. COPD = chronic obstructive pulmonary disease.
In this issue of the Journal, Rojas and colleagues (pp. 29–37) report the results of a large, retrospective cohort study about the quality of inpatient COPD care in the United States before (January 2010–September 2014) and after (October 2014–December 2018) the inclusion of COPD exacerbations in the CMS HRRP (2). They developed indicators for inpatient care using recommendations for or against specific evaluation and management strategies for patients hospitalized with COPD exacerbations included in the 2017 GOLD (Global Initiative for Chronic Obstructive Lung Disease) report and the ERS (European Respiratory Society)/ATS (American Thoracic Society) 2017 guidelines (3, 4).
Rojas and colleagues relied on the data available in the Premier Healthcare Database, which includes administrative claims data from approximately 25% of inpatient discharges in the United States. In their report, the authors analyzed data from nearly 950,000 hospital admissions for COPD exacerbations among patients aged 18 years or older that occurred between 2010 and 2018 among 995 U.S. hospitals. Although administrative claims are known to be lacking in clinical data, they use the type of sample needed for a robust analysis of healthcare usage and policy across multiple centers and contexts.
Results indicate that improvements in the quality of inpatient care across a broad set of indicators they examined have actually slowed (rather than accelerated) since the implementation of HRRP. The rate of change in the adoption of ideal care, defined as providing all elements of recommended care and none of the care that was not recommended, was only +0.11% per month after HRRP (compared with +0.24% per month before HRRP; P < 0.0001). As the authors acknowledge, there are several limitations in the interpretation of the study results because of the reliance on administrative claims data in the Premier Healthcare Database, including 1) errors in under- or overcounting patients as having COPD exacerbations; 2) lack of clinical data needed to confidently identify patients eligible for antibiotics, home oxygen, and mechanical ventilation; 3) undercounting of readmissions because of the inability to observe events occurring in hospitals that are not included in the Premier Healthcare Database; and 4) the inability to examine some key aspects of high-quality care, including patient–provider communication, care coordination, and other interventions to better engage patients during hospital-to-home transitions. Notwithstanding these limitations, the results of the study are, in our view, noteworthy. A policy change associated with a slowing of improvements in the quality of inpatient care for COPD exacerbation is more than disappointing, particularly when taken in the context of previous reports about 30-day readmissions and mortality among patients with COPD exacerbations after the implementation of the CMS HRRP (5).
Furthermore, COPD readmission rates have fallen by only small amounts—among Medicare beneficiaries, only 2.2% over the same time periods in the Rojas analyses, corresponding to about 0.4% more than the reduction observed in conditions not even subject to HRRP penalties (6). Other analyses have called into question whether readmission reductions are even attributable to the HRRP or if we are simply observing regression to the mean among poor-performing hospitals (7). Furthermore, an admission diagnosis related to COPD at the time of rehospitalization is less common than other conditions (8), highlighting that COPD care quality may not even be driving readmissions but rather the difficulties of providing care to patients with complex comorbidity. Improving COPD care quality is assuredly challenging, and in clinical trials, more than one program for COPD readmission reduction was associated with harm (9, 10).
Contextualizing this within the adapted Andersen model (Figure 1), it is important to also frame the change in outcome related to the feedback loops and other potential downstream effects, such as driving up adverse patient outcomes. Independent of care quality, there are existing concerns about increases in mortality as readmission rates have fallen for patients with COPD after the implementation of HRRP, described both in hospital-degree analyses of CMS Hospital Compare data (11, 12) and further corroborated in an analysis by Pueblo Neira and colleagues that showed a 0.7% increase in COPD mortality after HRRP implementation among Medicare fee-for-service beneficiaries (13).
Taken together, the question remains: does the HRRP accomplish what it set out to do? CMS indicates that the HRRP “[…] supports the national goal of improving health care for Americans by linking payment to the quality of hospital care” (14). It has been 8 years since the inclusion of COPD in the HRRP. Results of the study by Rojas and colleagues point to another crack in the façade. Sound health policy must follow evidence; it seems increasingly difficult to justify the HRRP through the lens of COPD, in which posthospital mortality increases are coupled with a slowing of improvements in the quality of inpatient care.
Footnotes
Supported by the National Institutes of Health/National Heart, Lung, and Blood Institute (L30HL134025 [R.G.B.]) and National Center for Advancing Translational Sciences (KL2TR001882). The findings and opinions in this manuscript do not necessarily represent those of the Department of Veterans Affairs or the U.S. Government.
Originally Published in Press as DOI: 10.1164/rccm.202208-1551ED on August 26, 2022
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc . 2005;51:95–124. [PubMed] [Google Scholar]
- 2.Rojas JC, Chokkara S, Zhu M, Lindenauer PK, Press VG.Care quality for patients with chronic obstructive pulmonary disease in the readmission penalty era Am J Respir Crit Care Med 2023;207:29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wedzicha JA, Miravitlles M, Hurst JR, Calverley PMA, Albert RK, Anzueto A, et al. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J . 2017;49:1600791. doi: 10.1183/13993003.00791-2016. [DOI] [PubMed] [Google Scholar]
- 4.Global Initiative for Chronic Obstructive Lung Disease Global strategy for the prevention, diagnosis, and management of COPD; 2017. [accessed 2022 Aug 10]. Available from: https://goldcopd.org/wp-content/uploads/2017/02/wms-GOLD-2017-FINAL.pdf.
- 5. LaBedz SL, Krishnan JA. Time to revisit the hospital readmissions reduction program for patients hospitalized for chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med . 2021;203:403–404. doi: 10.1164/rccm.202009-3392ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Buhr RG, Jackson NJ, Kominski GF, Dubinett SM, Mangione CM, Ong MK. Readmission rates for chronic obstructive pulmonary disease under the hospital readmissions reduction program: an interrupted time series analysis. J Gen Intern Med . 2020;35:3581–3590. doi: 10.1007/s11606-020-05958-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Joshi S, Nuckols T, Escarce J, Huckfeldt P, Popescu I, Sood N. Regression to the mean in the medicare hospital readmissions reduction program. JAMA Intern Med . 2019;179:1167–1173. doi: 10.1001/jamainternmed.2019.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Buhr RG, Jackson NJ, Dubinett SM, Kominski GF, Mangione CM, Ong MK. Factors associated with differential readmission diagnoses following acute exacerbations of chronic obstructive pulmonary disease. J Hosp Med . 2020;15:219–227. doi: 10.12788/jhm.3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fan VS, Gaziano JM, Lew R, Bourbeau J, Adams SG, Leatherman S, et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med . 2012;156:673–683. doi: 10.7326/0003-4819-156-10-201205150-00003. [DOI] [PubMed] [Google Scholar]
- 10. Rinne ST, Lindenauer PK, Au DH. Unexpected harm from an intensive COPD intervention. JAMA . 2019;322:1357–1359. doi: 10.1001/jama.2019.12976. [DOI] [PubMed] [Google Scholar]
- 11. LaBedz SL, Krishnan JA, Chung YC, Lindenauer PK, Spece LJ, Feemster LC, et al. Chronic obstructive pulmonary disease outcomes at veterans affairs versus non-veterans affairs hospitals. Chronic Obstr Pulm Dis . 2021;8:306–313. doi: 10.15326/jcopdf.2021.0201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Samarghandi A, Qayyum R. Effect of hospital readmission reduction program on hospital readmissions and mortality rates. J Hosp Med . 2019;14:E25–E30. doi: 10.12788/jhm.3302. [DOI] [PubMed] [Google Scholar]
- 13. Puebla Neira DA, Hsu ES, Kuo YF, Ottenbacher KJ, Sharma G. Readmissions reduction program: mortality and readmissions for chronic obstructive pulmonary disease. Am J Respir Crit Care Med . 2021;203:437–446. doi: 10.1164/rccm.202002-0310OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Medicare & Medicaid Services. Hospital readmissions reduction program (HRRP). [updated 2022. August 5; accessed 2022 Aug 10]. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.


