Abstract
People with sickle cell disease (SCD) are at greater risk of severe illness and death from respiratory infections, including COVID-19, than people without SCD (Centers for Disease Control and Prevention, USA). Vaso-occlusive crises (VOC) in SCD and severe SARS-CoV-2 infection are both characterized by thrombo-inflammation mediated by endothelial injury, complement activation, inflammatory lipid storm, platelet activation, platelet-leukocyte adhesion, and activation of the coagulation cascade. Notably, lipid mediators, including thromboxane A2, significantly increase in severe COVID-19 and SCD. In addition, the release of thromboxane A2 from endothelial cells and macrophages stimulates platelets to release microvesicles, which are harbingers of multicellular adhesion and thrombo-inflammation. Currently, there are limited therapeutic strategies targeting platelet-neutrophil activation and thrombo-inflammation in either SCD or COVID-19 during acute crisis. However, due to many similarities between the pathobiology of thrombo-inflammation in SCD and COVID-19, therapies targeting one disease may likely be effective in the other. Therefore, the preclinical and clinical research spurred by the COVID-19 pandemic, including clinical trials of anti-thrombotic agents, are potentially applicable to VOC. Here, we first outline the parallels between SCD and COVID-19; second, review the role of lipid mediators in the pathogenesis of these diseases; and lastly, examine the therapeutic targets and potential treatments for the two diseases.
Keywords: sickle cell disease, COVID-19, SARS-CoV-2, vaso-occlusive crisis, pain, thromboxane, prostaglandin D2, thrombo-inflammation, acute chest syndrome, ramatroban
1. Introduction
During the current COVID-19 pandemic, over 550 million people have been infected with the SARS-CoV-2 virus, and more than 6 million people have died. Investigators have reported clinical outcomes of SCD patients who developed COVID-19 during the current pandemic [1,2,3,4,5,6]. Some studies have demonstrated a more effective antiviral response against SARS-CoV-2 in patients with SCD, leading to a lower incidence of COVID-19 complications [7,8,9]. However, most studies have reported worse outcomes with COVID-19 in SCD patients compared to the general population. Among 178 persons with SCD in the United States who were reported to an SCD-coronavirus case registry, 122 (69%) were hospitalized, and 13 (7%) died [2]. A study based on electronic health record data from a multisite research network compared outcomes of African Americans with COVID-19 with or without SCD or heterozygous states of sickle cell trait (SCT) [1]. After 1:1 propensity score matching (based on age, sex, and other preexisting comorbidities), patients with COVID-19 and SCD remained at a higher risk of hospitalization (relative risk [RR], 2.0; 95% CI, 1.5–2.7) and development of pneumonia (RR, 2.4; 95% CI, 1.6–3.4) and pain (RR, 3.4; 95% CI, 2.5–4.8), compared with African Americans without SCD or SCT.
In a prospective study of 3500 pediatric and adult patients with SCD treated at 5 academic centers in the U.S., 66 patients developed COVID-19 [3]. During a follow-up period of 3 months after diagnosis of SARS-CoV-2 infection, 75% of patients were hospitalized, and the mortality rate was 10.6%. Vaso-occlusive pain was the most common presenting symptom. Acute chest syndrome occurred in 60% of hospitalized patients and all patients with a fatal outcome. Older age and a history of pulmonary hypertension, congestive heart failure, chronic kidney disease, and stroke were risk factors for mortality. Laboratory parameters in those who died included higher creatinine, lactate dehydrogenase, and D-dimer levels. In hospitalized patients, anticoagulant use was twice more common in patients who survived. Furthermore, all mortality occurred in patients not on disease-modifying therapy for SCD.
In a genetic association study of 2729 persons with sickle cell trait (SCT) and 129,848 who were SCT-negative, individuals with SCT had a number of preexisting kidney conditions that were associated with unfavorable outcomes following COVID-19 [10]. The presence of SCT was associated with increased risk of mortality and acute kidney failure following COVID-19, suggesting that SCT is also a prognostic factor for COVID-19 [10].
Thus, SCD has, in fact, emerged as one of the most important comorbidities conferring a high risk of mortality from COVID 19 that far exceeds the risk associated with chronic kidney disease, leukemias and lymphomas, heart failure, diabetes, obesity, lung cancer, acute myocardial infarction, chronic obstructive pulmonary disease, tobacco use, ischemic heart disease, and hypertension in the most extensive comorbidity analysis of COVID-19 patients to date [11]. Other adverse outcomes may also include SCD-related chronic organ dysfunction, such as chronic persistent pain, lung, and kidney injury; fragmented care; poor access to quality care; and interruptions in care as a result of fear of exposure to COVID.
These case reports, case series, and registry-based cohorts provide evidence of a high risk of severe clinical course in SCD patients with COVID-19 and suggest an interaction between sickle cell and COVID-19 pathophysiology, while providing critical insights that may help generate mechanistic hypotheses and design prospective clinical trials.
It has been proposed that SCD is associated with impaired oxygen exchange, which may be further impeded during the inflammatory phase of COVID-19. However, complications, such as cerebrovascular events in SCD patients with COVID-19, have not been reported. Therefore, we postulate that endothelial injury, thrombo-inflammation, microvascular thrombosis, and resulting vaso-occlusive disease in SCD may be amplified by similar processes initiated by the SARS-CoV-2 virus and vice versa, adding to the risk of morbidity and mortality from any single disease. In this review, we examine the two diseases’ pathobiological processes and tease out the common pathways that may present a therapeutic target, potentially benefiting thousands of SCD patients worldwide during the COVID-19 pandemic.
2. Pathophysiology of Sickle Cell Disease and COVID-19
SCD affects millions of children and adults globally, including about 100,000 in the United States [12]. The average life expectancy of an SCD patient at birth is 42–47 years in the United States [13], compared to about 79 years for the general U.S. population. SCD has a profound adverse impact on the quality of life. The current therapeutic options for SCD include hydration, blood transfusions, hydroxyurea, L-glutamine, crizanlizumab, and voxelotor.
The clinical hallmark of SCD is vaso-occlusive crises (VOCs), also referred to as pain crises. Cerebral vasculopathy, in its most devastating form, results in arterial thrombosis, which leads to cerebral infarction and stroke in early childhood [14,15]. SCD remains one of the most common causes of stroke in children [16]. The risk of stroke is higher during the first decade and is more significant between ages 2 and 5, when it reaches about 1% per year [17]. About 10% of SCD patients have a clinically apparent stroke before the age of 20, and the risk increases to about 25% by the age of 45 years [17]. Thrombotic vasculopathy in SCD is accompanied by significant organ dysfunction, morbidity diminished quality of life, and premature mortality [18,19]. Despite recent therapeutic advances, SCD patients remain at a high risk of developing VOCs and vascular complications. Thus, it is imperative to address the scientific gaps in our understanding of the mechanisms underlying the thrombo-inflammatory state, which is generally characterized by sickle RBC-mediated endothelial inflammation/dysfunction and coagulation activation leading to vessel injury, leakage, and vascular thrombosis [15].
The SARS-CoV-2 infection causes COVID-19 disease, which in its severe form can present with thrombotic microangiopathy, pulmonary thrombosis, pedal acro-ischemia (“COVID-toes”), arterial clots, strokes, cardiomyopathy, coronary and systemic vasculitis, bleeding, deep venous thrombosis, pulmonary embolism, and microvascular thrombosis in renal, cardiac, and brain vasculature [20,21,22,23,24,25]. Furthermore, necropsies have revealed inflammatory microvascular thrombi containing neutrophils, platelets, and neutrophil extracellular traps (NETs) in the pulmonary, hepatic, renal, and cardiac microvasculature as the hallmark of severe COVID-19 disease and the underlying cause of multi-organ failure [24,26,27]. Similar thrombo-inflammatory processes mediated by cell-free hemoglobin have been observed and proposed in SCD, with emphasis on platelet activation [15,28], a key driver of thrombo-inflammation in COVID-19 [24]. Consistent with the above, COVID-19 has been associated with increased risk of thrombosis in patients with SCD [29]. Therefore, we propose that the emerging therapies targeting platelet-mediated thrombo-inflammation in COVID-19 may serve as potential therapies for VOC.
In SCD, VOC often causes acute chest syndrome (ACS), defined as the presence of fever and/or new respiratory symptoms, accompanied by a new pulmonary infiltrate on a chest X-ray [30]. This is very similar to acute pneumonia in COVID-19. However, there are significant differences in the clinical presentation and underlying pathological basis for thrombo-inflammation in COVID-19 versus SCD. The incidence rate of ACS is highest at 2 to 4 years of age among children with SCD, with a rate of 25.3 per 100 patient-years, and decreases to 8.87 per 100 patient-years in adults >20 years of age with HbSS [31]. On the other hand, acute pneumonia and respiratory failure are more common in adults with COVID-19 [32].
Pulmonary complications associated with COVID-19 or SCD reveal similar underlying pathobiology and therapeutic targets. Respiratory distress in COVID-19 occurs in part due to pulmonary platelet microvascular thrombosis [20]. However, the triggering events of ACS in SCD patients may vary. Although conventional wisdom suggests ACS occurs secondary to fat embolism in SCD, more recent evidence from CT studies has demonstrated in situ pulmonary thrombosis in 10–20% of ACS patients [33,34,35,36,37,38,39,40]. Interestingly, in 16% of 538 SCD patients with ACS, pulmonary infarction or thrombosis were the triggering events rather than infection or fat embolism [41]. Still, fat embolism due to bone marrow infarction occurs in about 40% of both children [42] and adults [43,44,45], and leads to disseminated pulmonary platelet thrombi with a sharp and significant decline in platelet count prior to death [46]. It has been proposed that platelet inhibition at steady state or in the hemodynamically stable acute crisis might be an important therapeutic addition to prevent the progression of ACS in SCD [46]. A comparative analysis of the pathobiology of SCD and COVID-19, particularly in the context of endothelial injury, platelet activation, and multicellular adhesion, may help to identify potential therapies for the thrombo-inflammation in both diseases.
3. Mechanisms of Multicellular Adhesion and Thrombo-Inflammation in Sickle Cell Disease and COVID-19
Complications associated with thrombo-inflammation in SCD have uncanny similarities to those in COVID-19. In SCD, injury to the red blood cell (RBC) membrane mediates endothelial damage and inflammation, leading to multi-organ vasculopathy [47]. Hemoglobin S polymerization impairs the deformability of the RBC and causes oxidative injury and destruction of the RBC [47]. RBC injury exposes phosphatidyl serine and releases Hb and other intracellular contents [47]. This, in turn, depletes NO, increases endothelial adherence, releases pro-inflammatory cytokines, and activates coagulation, causing ischemia, reperfusion injury, and vascular damage [47,48,49,50,51]. Similar inflammatory processes observed during SARS-CoV-2 infection are evidenced by the elevated expression of leukocyte adhesion molecules in the pulmonary vasculature [20] and the presence of a proinflammatory lipid/thromboxane storm [52].
3.1. Endothelial Cell Injury and Activation: Role in Thrombo-Inflammation in SCD and COVID-19
Endothelial cell injury and activation lie at the heart of the prothrombotic state in both SCD and COVID-19 (Figure 1). Vascular endothelium is activated in SCD, regardless of the patient’s clinical status, with markedly increased expression of adhesion molecules, including intercellular adhesion molecule 1 (ICAM-1), vascular-cell adhesion molecule 1 (VCAM-1), E-selectin, and P-selectin [53]. SARS-CoV-2 virus directly infects and damages the endothelial cells, which initiates a cascade of events, leading to intussusceptive angiogenesis and microvascular thrombosis [20]. SCD and COVID-19 are characterized by interactions among activated endothelial cells, platelets, and leukocytes, leading to thrombo-inflammation and vascular occlusion [54]. Most notably, endothelial inflammation induces surface expression of adhesion molecules, including P-selectin, and release of prothrombotic granule contents (von Willebrand factor and FVIII), both effects enhancing leukocyte/platelet adhesion [15]. Intravascular release of tissue factor (TF) also contributes to the polarization toward a prothrombotic state [23,55,56,57]. Release of cell-free heme activates converging inflammatory pathways, such as TLR4 signaling [58], formation of neutrophil extracellular traps (NETs) [24,59], and priming of the inflammasome (NLRP3) pathway, leading to the release of interleukin-1β (IL-1β) and IL-18 by leukocytes, platelets, and endothelial cells, which contributes to the development of a sterile thrombo-inflammatory state in SCD [28,51,60,61].
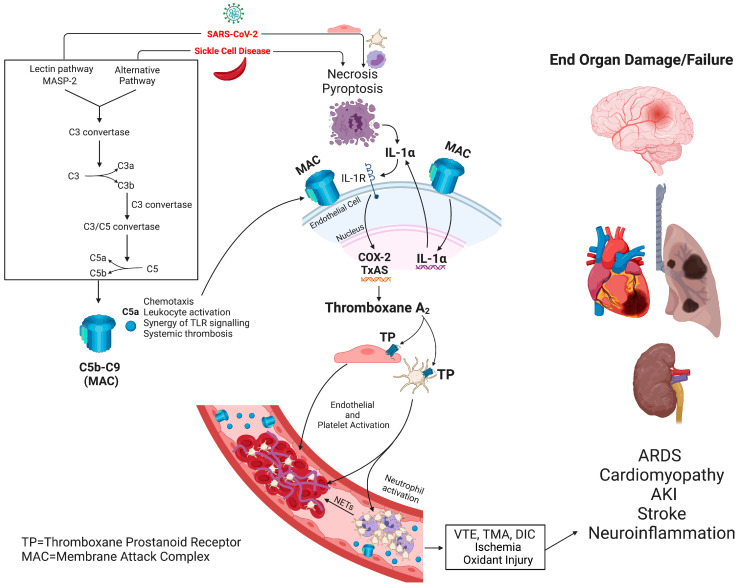
Figure 1.
Putative mechanism of complement-mediated microvascular thrombosis and vaso-occlusive disease in SCD and COVID-19: SARS-CoV-2 infection and sickle cell disease induce complement activation and formation of membrane attack complex leading to necrosis and pyroptosis of endothelial cells, platelets, and monocytes and accumulation of IL-1α. IL-1α stimulates the IL-1 receptor expressed on endothelial cells leading to thromboxane synthesis. Thromboxane A2 via the TP receptor activates platelets leading to platelet activation, platelet neutrophil partnership, neutrophil activation, and the release of neutrophil extracellular traps (NETs), thrombo-inflammation, oxidative stress, and subsequent end-organ damage and failure. The current review article is primarily focused on eicosanoid signaling in platelets; therefore, other receptors and pathways were excluded from Figure 1 for the reader’s convenience. COX, cyclooxygenase; IL, interleukin; NETs, neutrophil extracellular traps; TP, thromboxane prostanoid receptor; MAC, membrane attack complex; VTE, venous thromboembolism; TMA, thrombotic microangiopathy; DIC, disseminated intravascular thrombosis; ARDS, acute respiratory distress syndrome; AKI, acute kidney injury.
3.2. Platelet Activation: Role in Thrombo-Inflammation in SCD and COVID-19
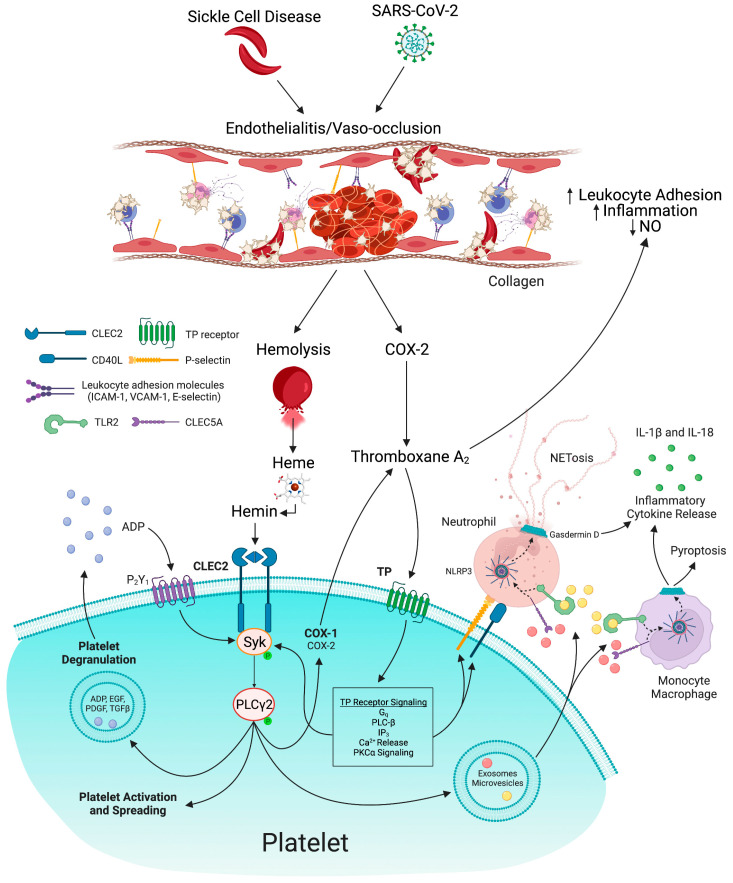
The pathogenesis of platelet activation in COVID-19 and SCD is multifactorial. COVID-19 and SCD activate platelets by association with the SARS-CoV-2 virus or direct activation with cell-free hemoglobin. Sickling and vaso-occlusion in SCD lead to hemolysis and subsequent release of cell-free hemoglobin [15]. Free plasma hemoglobin generates reactive oxygen species, a potent nitric oxide scavenger [62]. Nitric oxide scavenging promotes platelet activation and endothelial dysfunction [62]. Under physiological conditions, free heme is scavenged by the plasma protein hemopexin and is subsequently catabolized by heme oxygenase-1 into carbon monoxide, biliverdin, and ferrous iron (Fe2+) [63]. Acute or chronic hemolysis exhausts this scavenging system for heme, leading to an increase in free heme in the blood [63]. Upon release, reduced heme is rapidly and spontaneously oxidized in the blood into its ferric (Fe3+) form, hemin, with increased levels observed in hemolytic diseases [63]. Hemin has been implicated in the pathogenesis of ACS, one of the leading causes of death in SCD [64]. Hemin activates platelets as a ligand for C-type-lectin-like receptor 2 (CLEC2) [63]. Hemin-induced aggregation of human platelets is abolished by pre-incubation of hemin with a recombinant dimeric form of CLEC2 [63]. This indicates a role for platelet CLEC2 in sickle cell-mediated platelet activation (Figure 2). Cell-free heme also amplifies inflammation [65] by activating inflammatory pathways, including TLR signaling [66], gasdermin D-dependent NET formation [59,61], platelet-inflammasome activation, and generation of IL-1β-carrying platelet extracellular vesicles and priming of the inflammasome, leading to platelet-neutrophil aggregation and vaso-occlusion [28,51]. Consistent with the above, incubation of human peripheral neutrophils with VOC plasma produced significantly more NETs compared to non-sickle and steady state plasma [67]. NET generation in SCD is caused by sterile inflammation [61]. Additionally, during SCD-induced bone marrow infarction, the bone marrow undergoes stress reticulocytosis. As a result, it releases immature erythrocyte or reticulocytes [62] with surface expression of adhesion molecules, such as CD36 and α4β1 integrin [51,68], which contribute to platelet activation and thrombo-inflammation.
Figure 2.
Mechanisms of heme and thromboxane A2-mediated thrombo-inflammation in COVID-19 and sickle cell disease (SCD): Vaso-occlusion due to sickling or direct entry by SARS-CoV-2 virus leads to endothelial cell activation and damage, and hemolysis. COX-2 expression in endothelial cells promotes thromboxane A2 synthesis. Thromboxane A2 inhibits nitric oxide (NO) synthesis and promotes leukocyte adhesion and thrombo-inflammation. Free heme released from red blood cells is spontaneously oxidized to its ferric form, hemin. Hemin stimulates platelet CLEC2 signaling and thromboxane A2/TP receptor-dependent Syk phosphorylation leading to platelet activation, spreading, and degranulation. Platelets release exosomes and microvesicles, which stimulate the CLEC5A and TLR2 receptors on neutrophils. Subsequently, NLRP3 activation in neutrophils and monocytes promotes activation and assembly of gasdermin D, leading to the release of neutrophil extracellular traps and monocyte pyroptosis. NLRP3 inflammasome activation induces the release of proinflammatory cytokines, including IL-18 and IL-1β, thereby fueling thrombo-inflammation in COVID-19 and SCD. NO, nitric oxide; COX, cyclooxygenase; IL, interleukin; NETs, neutrophil extracellular traps; TP, thromboxane prostanoid receptor; CLEC, C-type lectin-like receptor; Syk, spleen tyrosine kinase; PLC, phospholipase C; PKC, protein kinase C; TLR, toll-like receptor; ADP, adenosine diphosphate; EGF, epidermal growth factor; PDGF, platelet-derived growth factor; TGF, transforming growth factor; NLRP3, NLR family pyrin domain containing 3.
SARS-CoV-2 viral hemagglutinins can bind to circulating red blood cells (RBCs) and induce agglutination and clumping of RBCs [69]. First, SARS-CoV-2 binds to RBCs in vitro [70] and clinically in COVID-19 patients [69,71]. Second, although fusion and replication of SARS-CoV-2 occur via ACE2, such hemagglutinating viruses initially attach to infective targets and clump with blood cells via much more abundantly distributed sialic acid glycoconjugate binding sites [69]. SARS-CoV-2, in particular, binds to these sialic acid sites [69]. Third, certain enveloped viruses express an enzyme, hemagglutinin esterase, that counteracts viral-RBC clumping, but is lacking in the SARS-CoV-2 virus [69]. These hemagglutinating properties of SARS-CoV-2 establish a framework for “catch and clump” induction of microvascular occlusion [69].
Subsequent hemolysis marked by elevated levels of LDH and thrombotic microangiopathy may play a role in platelet activation in COVID-19. Despite only minimal symptoms of COVID-19, 13 of the 34 children studied had thrombotic microangiopathy concurrent with complement activation marked by increased plasma sC5b-9 levels [72]. Furthermore, in 181 adults hospitalized for COVID-19, an increased percentage of schistocytes were correlated with decreased platelet count and increased markers of hemolysis, such as LDH [73]. The percentage of schistocytes was higher in those who died than those who survived [73]. Thus, thrombotic microangiopathy plays a significant role in platelet activation and morbidity in COVID-19, potentially through the release of free heme.
D-dimers are a prognostic marker of COVID-19 [74]. D-dimer levels are more likely to be abnormal in severely and critically ill patients, compared with mild and ordinary cases. At the same time, D-dimer levels of patients who died are significantly higher than those of surviving patients [74]. D-dimer levels are also raised in VOC and in most SCD patients with an abnormal chest X-ray (Table 1) [75] indicative of a prothrombotic state.
Table 1.
Comparative analysis of Plasma D-dimer levels in SCD during the steady state and sickle crisis and in COVID-19 patients.
| Subjects | Age/Reference | Plasma D-Dimer Levels | p-Value Compared to Controls | |
|---|---|---|---|---|
| Control | Disease State | |||
| Sickle Cell Disease | Adult [76] | HD (n = 35) 79 ± 25 ngh |
Steady State SCD n = 25 (Samples = 28) 566 ± 739 ng/mL |
p < 0.001 |
| SCD Painful Crisis n = 21 (Samples = 40) 1038 ± 1010 ng/mL |
p < 0.001 | |||
| 12–37 years [75] | SCD with pain crisis and normal chest X-ray (n episodes = 32) 584.2 µg/L (250–3119 µg/L) |
SCD with pain crisis and abnormal chest X-ray (n episodes = 13) 2117.0 µg/L (250–9143 µg/L) |
N/A | |
| Unventilated: 62.5 ± 8.4 Ventilated: 53.8 ± 9.3 [77] |
Hospitalized COVID-19 patients did not require artificial ventilation (n = 18) 650 ± 175 ng/mL |
Hospitalized COVID-19 patients requiring artificial ventilation (n = 11) 1250 ± 210 ng/mL |
p < 0.05 | |
| COVID-19 | 65.57 ± 13 years [78] | COVID-19 patients without pulmonary embolism (n = 118) 1310 ng/mL (800–2335) |
COVID-19 patients with pulmonary embolism (n = 44) 5364 ng/mL (2928–12,275) |
p = 0.001 |
Platelet activation plays a crucial role in both SCD and COVID-19. Platelet-derived microparticles are a biomarker of vaso-occlusive events in severe cases of SCD, while erythrocyte-derived microparticles are higher in non-severe disease [79]. Platelet extracellular vesicles and markers of platelet degranulation, including platelet factor 4 and serotonin in the blood, are also increased in COVID-19 [80].
In SCD, platelet activation and release of microparticles is likely mediated by heme-induced platelet CLEC2 receptor or NLRP3 inflammasome activation [28,63]. However, in COVID-19, heme-induced platelet CLEC2 activation has not been reported, to the best of our knowledge [81]. On the other hand, SARS-CoV-2 associates with platelets [80] possibly by binding of SARS-CoV-2 spike receptor binding domain (S-RBD) to dendritic cell-specific intercellular adhesion molecule-3-grabbing non-integrin (DC-SIGN) and liver/lymph node-specific intracellular adhesions molecule-3-grabbing integrin (L-SIGN) [82]. This is reminiscent of dengue virus-induced activation of platelets by binding to a DC-SIGN/CLEC2 hetero-multivalent receptor complex, resulting in CLEC2 activation and platelet degranulation with the release of extracellular vesicles, including exosomes and microvesicles [83].
Upon activation, the CLEC2 receptor undergoes tyrosine phosphorylation mediated by thromboxane A2 (TxA2) [84]. This leads to downstream phosphorylation of spleen tyrosine kinase and phospholipase γ2, potentiated by TxA2 [84]. This cooperation between CLEC2 and TxA2 signaling is critical for platelet activation (Figure 2) [84]. Platelet activation leads to the release of exosomes and microvesicles that further activate CLEC5A and TLR2 receptors on neutrophils and macrophages, thereby inducing NET formation and proinflammatory cytokine release [83]. Therefore, CLEC2 signaling is a potential therapeutic target in both SCD and COVID-19 (Figure 2).
3.3. P-Selectin: Role in Thrombo-Inflammation in SCD and COVID-19
Upregulation of P-selectin in endothelial cells and platelets contributes to the cell–cell interactions involved in vaso-occlusion and sickle cell-related pain crisis [85,86], and plasma levels of soluble P-selectin are markedly increased in vaso-occlusive SCD [87]. P-selectin is a well-recognized therapeutic target in SCD, and its inhibition by crizanlizumab, a humanized monoclonal antibody, significantly lowers rates of sickle cell-related pain crises [85]. Similarly, plasma levels of soluble P-selectin are markedly increased in COVID-19 [88]. Platelet P-selectin surface expression is upregulated in COVID-19 and positively correlates with platelet-monocyte aggregates in infected subjects [23]. In a randomized, placebo, controlled clinical trial amongst 54 hospitalized COVID-19 patients, crizanlizumab reduced P-selectin levels by 89% while promoting thrombolysis, as suggested by a 77% increase in D-dimers and decreased prothrombin fragments, but there was no difference in the clinical outcomes (the CRITICAL study) [89].
3.4. Tissue Factor: Role in Thrombo-Inflammation in SCD and COVID-19
TF is a transmembrane protein that functions as a high-affinity receptor for factors VII and VIIa and is the primary cellular initiator of blood coagulation during endothelial injury [90,91]. Formation of the TF-factor VIIa (FVIIa) complex leads to the activation of both FX and FIX, with subsequent thrombin generation, fibrin deposition, and activation of platelets [92]. Under normal conditions, endothelial cells and blood cells, such as monocytes, do not express TF [55]. On the other hand, total circulating microparticles expressing TF, mainly derived from monocytes and endothelial cells, are elevated in sickle cell crisis, compared to steady state and healthy controls [55]. Interestingly, TF inhibition in transgenic SCD mice significantly attenuates heme-induced microvascular stasis and prevents lung vaso-occlusion mediated by arteriolar neutrophil-platelet microemboli [93]. In severe COVID-19, platelet activation and TF expression by monocytes leading to platelet-monocyte interaction are associated with COVID-19 severity and mortality [23].
3.5. CD40L: Role in Thrombo-Inflammation in SCD and COVID-19
CD40L is a type II transmembrane protein expressed primarily by activated T cells, activated B cells, and platelets, and under inflammatory conditions, it is also induced on monocytic cells, natural killer cells, mast cells, and basophils [94,95]. CD40L binds to CD40 expressed on a variety of cells, including dendritic cells, monocytes, platelet, and macrophages [95]. CD40L/CD40 interactions are pivotal in different cellular immune processes [95]. Notably, platelets release CD40L, which contributes to chronic inflammation in SCD [96]. Elevated levels of circulating CD40L have been associated with acute chest syndrome (ACS) in SCD [96,97]. Platelets from SARS-CoV-2 patients are also more prone to release of soluble CD40L upon exposure to thrombin, compared to healthy controls [80].
Activated platelets are also a significant source of thrombospondin-1, another protein related to the incidence of ACS and vaso-occlusive episodes [98]. However, thrombospondin has not been examined in COVID-19, to the best of our knowledge.
3.6. NLRP3 Inflammasome: Role in Thromboinflammation in SCD and COVID-19
Platelets are known to play a role in the detection and regulation of infection [99]. Viruses, such as the dengue virus, lead to platelet activation [99]. Platelets sense pathogens and host damage through recognition of pathogen-associated molecular patterns or damage-associated molecular patterns (DAMPs) using receptors [99]. C-type lectin receptors DC-SIGN and CLEC2 are involved in the binding of different viruses, as well as the recognition of DAMPs, such as hemin and mitochondrial DNA [99]. Platelets are highly activated in COVID-19. They are likely involved in boosting the inflammasome capacity of innate immune cells, including human macrophages and neutrophils, and IL-1 production by monocytes [24,100,101,102]. An unknown platelet-derived soluble factor enhances NLRP3 transcription and inflammasome activation [102]. We postulate that CLEC2-induced platelet activation leads to the release of exosomes and microvesicles, which stimulate the CLEC5A and TLR2 receptors on innate immune cells, leading to NLRP3 inflammasome activation and pyroptosis [83].
SARS-CoV-2 virus also induces inflammasome activation and cell death by pyroptosis in human monocytes, hematopoietic stem/progenitor cells, and endothelial progenitor cells [103,104]. Pyroptosis was dependent on caspase-1 engagement, before IL-1ß production and inflammatory cell death [103]. Furthermore, examination of the whole blood transcriptome in COVID-19 patients has revealed that the dysregulated immune system in COVID-19 is characterized by highly specific neutrophil activation-associated signatures [105], with an increase in immature neutrophils with NLRP3 inflammasome activation [101].
NLRP3 inflammasome is also upregulated in SCD patients under steady state conditions, compared with healthy controls, and is further upregulated when patients experience an acute pain crisis [106]. Platelet-inflammasome activation led to the generation of IL-1β and caspase-1-carrying platelet extracellular vesicles that bind to neutrophils and promote platelet-neutrophil aggregation in lung arterioles of SCD mice in vivo and SCD human blood in microfluidics in vitro [28]. Inhibition of the inflammasome effector caspase-1 or IL-1β pathway attenuated platelet extracellular vesicle generation, prevented platelet-neutrophil aggregation, and restored microvascular blood flow [28]. More recent findings show that sterile inflammation in SCD promotes caspase-11/4-dependent activation (cleavage) of pyroptotic effector gasdermin-D (GSDMD) in neutrophils, which leads to generation of NETs in the liver [61]. These NETs embolize from the liver to the lung to promote P-selectin-independent lung vaso-occlusion in SCD [61]. Interestingly, GSDMD is highly expressed on the BALF and blood neutrophils of COVID-19 patients [107]. Image analysis of lung autopsies of patients who died from COVID-19 revealed the presence of NET structures associated with activated GSDMD-NT fraction [107]. In cell cultures of neutrophils from COVID-19 patients, disulfiram, a GSDMD inhibitor, inhibited release of NETs in a concentration-dependent manner [107]. Therefore, in both SCD and COVID-19, activation of inflammasome in platelets, monocytes, and neutrophils and GSDMD-dependent NETosis play a key role in initiating inflammation and tissue injury (Figure 2).
3.7. Nitric Oxide: Role in Thrombo-Inflammation in SCD and COVID-19
Both COVID-19 and SCD are associated with endothelial injury and activation. Following endothelial injury, nitric oxide (NO) has been shown to serve many vasoprotective roles, including inhibition of platelet aggregation and adherence to the site of injury, inhibition of leukocyte adherence, inhibition of vascular smooth muscle cell proliferation and migration, and stimulation of endothelial cell growth [51,62,108,109,110].
In SCD, cell-free plasma hemoglobin resulting from intravascular hemolysis consumes NO very rapidly [111], dramatically limiting NO bioavailability [112,113]. Inhaled NO has shown evidence of efficacy in mouse models of SCD, but in a phase II placebo-controlled trial of inhaled NO gas in SCD patients with VOC, NO did not improve the time to crisis resolution [114].
NO deficiency has also been observed among COVID-19 patients, and it may cause vascular smooth muscle contractions [115], reducing the ability to neutralize ROS and NO-mediated antiviral capability [116,117,118]. Nitric oxide has been widely proposed as a potential treatment for COVID-19 [119]. However, inhaled NO gas may be rapidly sequestered by superoxide, forming peroxynitrite, which is known to cause lung damage and cell death [120]. It is plausible that NO in SCD [114] and COVID-19 [121] could lack therapeutic benefit in an environment of oxidative stress or in the absence of sufficient L-arginine bioavailability [120].
3.8. TGFβ: Role in Thromboinflammation in SCD and COVID-19
The transforming growth factor (TGF-β) superfamily is composed of a large group of proteins that are fundamental in regulating various biological processes, such as extracellular deposition, cell differentiation and growth, tissue homeostasis and repair, and immune and inflammatory responses [122]. The TGF-β subfamily is a central mediator of fibrogenesis and a crucial regulator of fibroblast phenotype and function. There are three known isoforms of TGF-β expressed in mammalian tissue, including TGF-β1, 2, and 3. TGF-β1 is the most abundant and ubiquitously expressed isoform and is associated with the development of tissue fibrosis [122,123,124]. Various animal models support the role of TGF-β1 in mediating hepatic, renal, pulmonary, and cardiac fibrosis [125,126,127,128]. Interestingly, platelets contain 40 to 100 times more TGF-β1 than other cells and rapidly release TGF-β1 upon activation [129]. This is consistent with the positive correlation between plasma TGF-β1 and platelet and white blood cell counts in patients with steady state SCD [130,131]. Interestingly, early, untimely TGF-β responses in SARS-CoV-2 infection limit the antiviral function of natural killer (NK) cells [132]. Therefore, TGF-β has been proposed as a therapeutic target in both SCD and COVID-19 [130,132].
3.9. Lipoxygenase: Role in Thrombo-Inflammation in SCD and COVID-19
Activation of the lipoxygenase (LOX) pathway in SCD and COVID-19 promotes generation of arachidonic acid-derived eicosanoids. In isolated rat lungs, perfusion with HbSS peptide leads to more LOX metabolite LTC4, compared to HbAA-perfused lungs (10.40 ± 0.62 vs. 0.92 ± 0.22 ng/g dry lung weight (mean ± SEM; p = 0.0001)) [133]. Cysteinyl leukotrienes have been implicated in the pulmonary manifestations of SCD, including acute chest syndrome [133]. However, targeting of cysteinyl leukotriene receptor with montelukast did not improve pain, pulmonary function, or microvascular blood flow in a phase 2 randomized placebo-controlled trial in 42 adolescent/adult SCD patients [134].
LOX activity is increased in the plasma of COVID-19 patients, with higher activity in patients who survived [135]. LOX-derived leukotriene production is also significantly increased in the BALF of COVID-19 patients [136]. Montelukast has been shown to inhibit in vitro platelet activation induced by plasma from COVID-19 patients [137]. Montelukast prevented surface expression of tissue factor (TF) and P-selectin, and reduced circulating monocyte- and granulocyte-platelet aggregates and TF+-circulating microvesicles [137]. In a prospective randomized controlled study of montelukast in 180 hospitalized COVID-19 patients, patients receiving montelukast had significantly lower LDH, fibrinogen, D-dimer, CRP, and procalcitonin, compared to standard of care alone [138]. Additionally, treatment with montelukast significantly reduced the progression to macrophage activation syndrome and respiratory failure, while significantly reducing the length of hospital stay [138].
4. Thromboxane A2-A Key Mediator of Thrombo-inflammation by Regulation of Platelet Activation, NO Synthesis, and Expression of P-Selectin, CD40L, Tissue Factor, and TGF-β
Thromboxane A2 (TxA2), a key mediator of thrombosis, is released by platelets, endothelial cells, macrophages, and neutrophils [139]. TxA2 binds to the thromboxane-prostanoid (TP) receptor on platelets, thereby stimulating activation and aggregation of platelets [139]. Cooperation between TxA2/TP receptor and CLEC2 receptor signaling pathways is critical for CLEC2-induced platelet activation [84].
Thromboxane A2 generation is markedly stimulated in both SCD and COVID-19. In SCD, TxB2, and 2,3-dinor-TxB2, a terminal metabolite of TxB2, were significantly elevated in the urine and plasma of steady state SCD patients, compared to healthy HbAA controls (Table 2) [140,141]. Moreover, in isolated rat lungs co-perfused with sickle (HbSS) erythrocytes and platelet-rich plasma, TxA2 levels increased over 10-fold more than with normal (HbAA) erythrocytes [142]. In severe COVID-19 patients, bronchoalveolar lavage fluid presents a picture of an inflammatory lipid storm, with marked increases in fatty acid levels and a predominance of cyclooxygenase metabolites, notably, thromboxane B2 >> PGE2 > PGD2 [52]. Plasma levels of TxB2, a stable metabolite of TxA2, are also markedly increased in severe COVID-19 patients [23]. Interestingly, proinflammatory eicosanoids TxB2 and anti-inflammatory eicosanoids 15d-PDJ2 and 12HETE were elevated in the plasma of 66 COVID-19 survivors [135]. However, only the plasma levels of TxB2, and not 15d-PDJ2 or 12HETE, were elevated in 22 patients who died from COVID-19 [135]. Considering the marked increase of TxA2 in both SCD and COVID-19, we postulate the potential role of TxA2 in the pathogenesis of the proinflammatory state that contributes to the thrombo-inflammation observed in both diseases.
Table 2.
Comparative analysis of thromboxane levels in SCD, COVID-19, and asthmatics.
| Subjects | Source and Analyte | Thromboxane Levels | p-Value Compared to Controls | |
|---|---|---|---|---|
| Control | Disease State | |||
| Sickle Cell Disease | Plasma 2,3 dinor-TxB2 [140] (µg/L) (Mean ± SEM) |
HD (n = 12) 2.75 ± 0.83 |
Steady State SCD (n = 15) 21.53 ± 5.10 |
p < 0.001 |
| Plasma TxB2 [140] (µg/L) (Mean ± SEM) |
HD (n = 12) <0.005 |
Steady State SCD (n = 15) 0.543 ± 0.101 |
p < 0.05 | |
| Urinary TxB2 [140] (pg/mg creatinine) (Mean ± SEM) |
HD (n = 12) 0.41 ± 0.30 |
Steady State SCD (n = 15) 0.91 ± 0.13 |
p < 0.05 | |
| Urinary 2,3 dinor-TxB2 [140] (pg/mg creatinine) (mean ± SEM) |
HD (n = 12) 1.70 ± 0.032 |
Steady State SCD (n = 15) 2.81 ± 0.13 |
p < 0.01 | |
| Urinary 11-dehydro-TxB2 [141] (pg/mg creatinine) (Mean ± SEM) |
HD (n = 33) 299 ± 20 |
Steady State SCD (n = 49) 1227 ± 191 |
p = 0.0002 | |
| Vaso-Occlusive SCD (n = 15) 1836 ± 536 |
p = 0.0005 | |||
| COVID-19 | BALF TxB2 [52] (nmol/L) (Means) |
HD (n = 25) <0.250 |
Severe COVID-19 (n = 33) 12.0 |
p < 0.0001 |
| Plasma TxB2 [23] (ng/mL) (Median) |
HD (n = 11) 4.0 |
Severe COVID-19 (n = 35) 7.5 |
p < 0.05 | |
| Urinary 11-dehydro-TxB2 [143] (pg/mg creatinine) (Median (95% CI)) |
Without Events (n = 47) 4890 (5049–8290) |
With Events (n = 18) 7603 (7541–19,791) |
p = 0.002 | |
| <10 d of hospitalization (n = 35) 4801 (3817–9196) |
≥10 d of hospitalization (n = 30) 8614 (7990–14,316) |
p = 0.02 | ||
| No death (n = 48) 5360 (5907–10,038) |
Death (n = 6) 15,069 (1915–42,007) |
p = 0.004 | ||
| No Mechanical Ventilation (n = 56) 5137 (4498–7512) |
Mechanical Ventilation (n = 9) 20,121 (5364–41,015) |
p < 0.001 | ||
| Atopic Asthmatics | BALF TxB2 [144] (nmol/L) (Mean ± SEM) |
Before Allergen Challenge (n = 8) 0.130 ± 0.021 |
After Allergen Challenge (n = 8) 0.430 ± 0.108 |
p < 0.05 |
HD, healthy donor; BALF, bronchoalveolar lavage fluid.
There is growing evidence that cyclooxygenase enzymes, COX-1 and COX-2, mediate the thromboxane generation underlying thrombo-inflammation in SCD and COVID-19 [81]. COX-2 is an inducible enzyme, while COX-1 is constitutive. COX-2 expression is stimulated by inflammation, a cardinal feature of both VOC and COVID-19. Endothelial COX-2 expression was markedly increased in transgenic BERK SCD mice [145]. SARS-CoV-2 infection of iPSC-derived cardiomyocyte cells led to >50-fold increase in COX-2 gene expression (Dr. S. T. Reddy, UCLA, personal communication, based on analysis of the supplemental material in reference [146]. In addition to upregulating COX-2 in living human lung slices, the SARS-CoV-2 virus reduces the prostaglandin-degrading enzyme 15-hydroxyprostaglandin-dehydrogenase [147]. TxA2 generation is COX-2 mediated in states of high TxA2 generation, such as in inflammation, infection, and obesity [148]. Low-dose aspirin is unable to inhibit COX-2; hence, aspirin resistance is common in states with COX-2-dependent TxA2 generation [149]. TxA2 generation by platelets and endothelial cells stimulates expression of P-selectin, ICAM-1, and VCAM-1 on endothelial cells and release of tissue factor [150,151,152].
4.1. Thromboxane A2-Mediated P-Selectin Expression
TxA2 plays a role in the platelet expression of P-selectin. It was demonstrated that the percentage of P-selectin-positive platelets in TP receptor knockout mice on day 1 was significantly reduced, compared with that in wild-type mice [151]. Therefore, TxA2 blockade may be another effective method to target P-selectin without the need for IV administration of anti-P-selectin Ab [85].
4.2. Thromboxane A2-Mediated Tissue Factor Expression
TxA2 has been shown to mediate TF expression on endothelial cells and monocytes [152]. TP receptor agonism induced TF expression in endothelial cells. In contrast, a TP receptor antagonist reduced endothelial expression of TF after TNF-α induction [152,153]. Similarly, lipopolysaccharide-induced TF expression on human monocytes was abrogated by a TP receptor antagonist [154].
4.3. Thromboxane A2-Mediated CD40L Expression
Plasma CD40L has been correlated with urinary 11-dehydro-TxB2, a stable metabolite of TxA2 in diabetic patients [155]. Upon treatment with low dose aspirin (100 mg/day), plasma CD40L decreased, along with a reduction in urinary 11-dehydro-TxB2 and whole blood TxB2 production [155]. Patients with higher excretion of 11-dehydro-TxB2 had increased levels of CD40L [155]. Therefore, targeting TxA2 may reduce the release of CD40L, potentially preventing ACS and vaso-occlusion in SCD.
4.4. Thromboxane A2-Induced Suppression of NO Synthesis
NO inhibits platelet activation via phosphorylation of the thromboxane prostanoid (TP) receptor [156]. In both vascular smooth muscle cells and platelets, the vasodilatory and platelet inhibitory effects of NO are known to be mediated by cGMP, which inhibits phospholipase C activation, inositol 1,4,5-triphosphate generation, and [Ca2+]i mobilization [156]. NO stimulates cGMP production and activates cGMP-dependent protein kinase or G kinase [156]. TxA2 also directly inhibits nitric oxide synthase [157]. Nitrite accumulation was enhanced by TP receptor antagonists, seratrodast or ramatroban, in a model of IL-1β-stimulated rat aortic smooth muscle cells [157]. Therefore, TxA2 may play a role in NO deficiency in SCD, which would be alleviated by TP receptor blockade.
4.5. Thromboxane A2-Induced TGF-β Release
TxA2/TP receptor signaling stimulates activation of the TGF-β pathway [158,159]. Hypertensive PGI2 receptor knockout mice fed a high-salt diet exhibited elevated urinary TxA2 metabolites and left ventricular TP receptor overexpression, which accompanied cardiac collagen deposition and profibrotic TGF-β gene expression [160]. Inhibition of TxA2 biosynthesis with low-dose aspirin mitigated the increase in blood pressure, cardiac fibrosis, and left ventricular TGF-β gene expression [160]. Moreover, the number of myofibroblasts and extravasated platelets in the heart were also reduced [160]. This is consistent with TxA2-induced TGF-β gene expression in myofibroblasts [160].
5. Thromboxane A2 in Post-Capillary Venoconstriction in SCD and COVID-19
5.1. Post-Capillary Pulmonary Venous Constriction
Cardiopulmonary complications are the leading cause of death in patients with SCD, primarily resulting from diastolic heart failure (HF) and/or pulmonary hypertension (PH) [161]. From a hemodynamic standpoint, almost half of cases of SCD pulmonary hypertension reported in the literature have postcapillary or venous pulmonary hypertension [162]. Interestingly, U-46619, a TxA2 mimetic in a concentration of 1 nM, is sufficient to reduce the guinea pig pulmonary venous luminal area by 50% [163]. A 50% reduction in luminal area increases vascular resistance by 4-fold, indicating that sub-nanomolar concentrations of thromboxane A2 could produce meaningful increases in pulmonary venous resistance [163]. This is consistent with the measured effect of selective TP receptor antagonism in reducing pulmonary venous resistance and capillary pressure in patients with acute lung injury [164]. Moreover, TP receptor antagonism prevented right ventricular fibrosis and arrhythmias in a mouse model of pulmonary arterial hypertension [165]. Therefore, TxA2 released from platelets and pulmonary venous endothelial cells may cause: first, pulmonary venous hypertension and, second, left ventricular fibrosis secondary to elevated TGF-β levels and diastolic dysfunction.
TP receptor antagonism has also been shown to attenuate airway mucus hyperproduction induced by cigarette smoke [166] and reduce tissue edema in mouse models of acute lung injury [167]. In COVID-19, TP receptor blockade may rapidly reduce pulmonary capillary pressures, improve ventilation-perfusion matching, promote resolution of edema, reduce bronchoconstriction and airway mucus hyperproduction, improve lung compliance and gas exchange, and thereby mitigate respiratory distress and hypoxemia [168].
5.2. Post-Capillary Efferent Arteriole Constriction in Kidney Injury
Glomerular involvement is one of the most prominent renal manifestations observed in SCD. It is characterized by an early increase in glomerular filtration rate (GFR) associated with micro- or macroalbuminuria, followed by a gradual decline in GFR and chronic renal failure [169,170]. This is consistent with underlying vasculopathy in sickle cell nephropathy associated with cortical hyperperfusion, medullary hypoperfusion, and an increased stress-induced vasoconstrictive response [169]. Renal involvement is usually more severe in homozygous than heterozygous SCD. It contributes to diminished life expectancy and 16–18% of mortality in patients with SCD [169,171,172]. Acute kidney injury is emerging as a common and important sequelae of COVID-19, with rates as high as 33–43% in hospitalized patients [173,174,175,176]. In a prospective cohort study of 701 COVID-19 patients, proteinuria was reported in 43.9% of patients on admission to the hospital [177]. However, the involvement of hyperfiltration in COVID-19-associated kidney injury remains to be elicited.
Glomerular hyperfiltration is caused by either a net reduction of afferent (pre-capillary) arteriolar resistance or a net increase in efferent arteriolar (post-capillary) arteriolar resistance [178]. Thromboxane synthase inhibition or TP receptor antagonism in untreated streptozotocin-induced diabetic rats was shown to decrease renal blood flow, increase renal vascular resistance, and ameliorate renal hyperperfusion [179]. This is consistent with reduced microalbuminuria in diabetic patients treated with a TxA2 synthase inhibitor, likely due to a vasodilating effect predominantly exerted on the efferent arteriole [180,181]. However, this contrasts with in vitro findings that treatment of isolated perfused hydronephrotic rat kidney with TxA2 mimetic leads to preferential constriction of afferent arterioles [182]. Therefore, further studies are needed to clarify the role of TxA2 in post-capillary efferent arteriole constriction and glomerular involvement associated with vascular diseases, including SCD and COVID-19.
6. Complement Activation as an Inducer of Thrombo-Inflammation in SCD and COVID-19
The complement system is a critical innate immune defense against infections and an important driver of inflammation [183]. Activated complement can produce direct effector functions by target opsonization with cleaved complement component 3 (C3) and C4 fragments, promotion of inflammation with C3a and C5a, and direct cell lysis with the assembly of MAC C5b-9 complex [183]. Plasma concentrations of sC5b-9 are elevated in steady state SCD patients [184]. Complement deposition is also increased in cultured human endothelial cells incubated with SCD serum [184]. In SCD, levels of IL-1α were significantly higher in those with a history of acute splenic sequestration, a common feature of homozygous SCD, compared with matched normal controls [185]. The effect of complement activation on IL-1α and COX-2/TxA2 axes has been studied by treating porcine endothelial cells with human plasma containing xenoreactive antibodies and complement [186]. In this model, there is markedly increased expression of IL-1α, COX-2, and thromboxane synthase, leading to the generation of TxA2. The role of IL-1α in mediating the effect of complement activation was confirmed by the addition of an IL-1 receptor antagonist to the human serum, which prevented the release of PGE2 and TxA2 [186]. Therefore, complement activation can induce a prothrombotic state via the expression of IL-1α and COX-2, leading to generation of TxA2 (Figure 1).
Complement activation is also thought to play a critical role in immune-thrombosis and end-organ damage in COVID-19 [25]. Nucleocapsid protein of SARS-CoV-2 virus binds to the Mannan-binding, lectin-associated serine protease-2 (MASP-2), the lectin pathway’s effector enzyme, resulting in complement activation [187,188]. Lung tissue from deceased COVID-19 patients showed components of the lectin and terminal complement pathways, specifically MASP-2, complement factor 4d (C4d), and C5b-9 (i.e., the membrane attack complex) [187,188]. Activation of C4d (classical lectin pathway) and sC5b-9 (membrane attack complex) are also associated with respiratory failure in hospitalized adults with COVID-19 [189]. Furthermore, in children with COVID-19, there is evidence of complement activation with an increase in plasma sC5b-9 levels, even with only minimal symptoms of COVID-19, and 13 of the 34 children had thrombotic microangiopathy [72]. Most importantly, IL-1α is also released from necrotic and pyroptotic cells, including pneumocytes and endothelial cells, the primary site of an attack by SARS-CoV-2 [190].
7. Thromboxane A2 Is Enzymatically Converted into 11-Dehydro-Thromboxane A2, a Full Agonist of the Prostaglandin D2/DP2 Receptor Leading to Fibrosis and Inflammation
TxA2 is short-lived and rapidly transformed nonenzymatically in an aqueous solution to TxB2. TxB2 is further metabolized enzymatically to a series of compounds, of which 11-dehydro-TxB2 (11dhTxB2) is the major product found both in plasma and urine [191]. The dehydrogenase catalyzing the formation of 11dhTxB2 was tissue bound, with the highest activity in the lung [192]. Urinary excretion of 11dhTxB2 was markedly increased in recently hospitalized patients with COVID-19 and was predictive of plasma D-dimer levels, renal ischemia, the need for mechanical ventilation, and mortality [143]. Urinary 11dhTxB2 is also significantly elevated in SCD compared to healthy controls [141]. Interestingly, 11-dehydro-TxB2 is a full agonist of the D-prostanoid receptor 2 (DP2) for prostaglandin D2 (PGD2) [191].
PGD2/DP2 receptor signaling is known to mediate Th2 immune responses that are classically directed against extracellular non-phagocytosable pathogens, for instance, helminths [193,194,195]. The effectors for PGD2/DP2 receptor-mediated Th2 immune response are eosinophils, basophils, and mastocytes, as well as B cells (humoral immunity), and these are consistently elevated in COVID-19 [196]. IL-13, a type 2 cytokine released during PGD2/DP2 receptor signaling, increases hyaluronan accumulation in mouse lungs [197], and is universally correlated with ARDS, AKI, morality [198], and the need for mechanical ventilation in COVID-19 [197]. IL-13 is also known to upregulate monocyte-macrophage-derived suppressor cells (MDSC), which play a role in immune suppression and lymphopenia, a hallmark of severe COVID-19 disease [199,200,201,202].
PGD2/DP2 receptor signaling is thought to play a role in fibrosis. PGD2/DP2 receptor signaling exerts direct pro-apoptotic and pro-fibrotic actions on various cells, including islet cells, cardiomyocytes, and osteoclasts [203,204,205]. Moreover, PGD2/DP2 receptor-mediated IL-13 release is a significant inducer of fibrosis by stimulating the IL-13Rα2 receptor expressed on macrophages to release TGF-β1 [206]. Therefore, elevated levels of TxA2 in COVID-19 and SCD may be rapidly converted to 11dhTxB2 in the lungs, thereby leading to DP2 receptor signaling and fibrosis in the lungs and heart.
8. Therapeutic Options for Thrombo-inflammation in COVID-19 and SCD: Past, Present, and Future
Blood transfusion is the only treatment for SCD-associated vaso-occlusive crises or thrombotic events, such as acute painful episodes, cerebral infarction, and acute chest syndrome [207]. Widely varying anticoagulants, including heparin and its analogs, are used in both arterial and venous thrombosis associated with SCD, but they have proven ineffective in preventing acute pain episodes [208,209]. As a treatment of acute pain crisis in SCD, tinzaparin, low molecular weight heparin, was shown to reduce the severity and crisis duration in a double-blind, randomized, controlled trial [210].
Antiplatelet agents, such as aspirin, prasugrel, and ticagrelor, have also been tested in SCD (Table 3). In a double-blind crossover study of children with SCD, low-dose aspirin, an inhibitor of COX-1 action, did not affect the frequency and severity of vaso-occlusive crises, compared to placebo [211]. Prasugrel and ticagrelor are P2Y12 receptor antagonists that block platelet stimulation induced by ADP. In a double-blind, randomized, placebo-controlled trial of prasugrel in children and adolescents with SCD, prasugrel was found to be safe, but did not reduce the rate of vaso-occlusive crisis or diary-reported events over a 9–24-month period [212]. Ticagrelor demonstrated no effect on diary-reported pain in young adults with SCD [213]. However, as discussed above, heme-driven CLEC2-induced platelet activation is dependent on ADP stimulation of platelet P2Y1 receptor, but not the P2Y12 receptor [84], while prasugrel only blocks the latter [214]. The failure of prasugrel and ticagrelor may also indicate that other P2Y12 antagonists may not be effective in SCD [213,214]. Unfortunately, there are no approved P2Y1 antagonists to our knowledge. Moreover, other antiplatelet therapies have been tested in clinical trials, including eptifibatide, a platelet αIIbβ3 receptor blocker, which failed to improve time to crisis resolution or hospital discharge in SCD patients, though only 13 patients were enrolled in the study [215]. Meanwhile, targeting IL-1β downstream of inflammasome activation with canakinumab led to improved thrombo-inflammation and quality of life, including reduced days of hospitalization and pain [216]. P-selectin antibody (Crizanlizumab) is the only targeted therapy against thrombo-inflammation in SCD. However, prophylactic P-selectin inhibition by crizanlizumab led to only a ~50% reduction in hospitalization related to VOC, suggesting that P-selectin-independent pathways contribute to the remaining morbidity of VOC [85].
Table 3.
Efficacy trials of antiplatelet therapies in SCD.
| Study Design | Study Population | Intervention | Primary Outcome Measure and Result |
|---|---|---|---|
| Phase IIb Multicenter, double-blind, double-dummy, randomized, placebo-controlled, parallel-group [213] |
● Have SCD [homozygous sickle cell (HbSS) or sickle beta-zero thalassemia (HbSβ0)] ● Ages 18–30 years (mean 22.2 years old) ● Have ≥4 days of pain during the 4-week single-blind placebo baseline period prior to randomization ● If on hydroxycarbamide, a stable dose for 3 months prior to enrollment required ● If on erythropoietin, drug must have been prescribed 6 months before and at a stable dose for ≥3 months prior to randomization (n = 194) |
● Ticagrelor 10 mg plus matching placebo for ticagrelor 45 mg ● Ticagrelor 45 mg plus matching placebo for ticagrelor 10 mg ● Matching placebo for ticagrelor 10 and 45 mg Duration: 12 weeks |
Proportions of days with diary-reported SCD pain No significant difference between placebo and ticagrelor treatment groups |
| Phase III Multinational, double-blind, randomized, placebo-controlled, parallel-group [212] |
● Have SCD [homozygous sickle cell (HbSS) or sickle beta-zero thalassemia (HbSβ0)] ● Are participants with SCD who have had ≥2 episodes of vaso-occlusive crisis (VOC) in the past year ● Have a body weight ≥ 19 kilogram (kg) and are ≥ 2 and <18 years of age, inclusive at the time of screening ● If participants are ≥2 and ≤16 years of age, they must have had a transcranial Doppler within the last year (n = 341) |
● Prasugrel 0.08–0.12 mg/kg po once daily ● Placebo Duration: 9–24 months |
Number of Vaso-Occlusive Crisis (VOC) Events Per Participant Per Year (Rate of VOC) Terminated due to lack of efficacy |
| Phase III Double-blind crossover study [211] |
● Have sickle hemoglobinopathy observed regularly ● Ages 2–17 years old (mean 7.7 years old) ● The hematologic diagnosis was confirmed by cellulose acetate electrophoresis at pH 8.6 and citrate agar electrophoresis at pH 6.4 ● At least 50% compliant (n = 49) |
● Low dose aspirin ● Placebo |
Frequency and severity of VOC No significant difference between placebo and aspirin treatment groups |
Therapies targeting thrombo-inflammation in patients with COVID-19 are in clinical trials [217]. In a necropsy study of 68 COVID-19 patients, nearly 70% (48 out of 68) were treated with anticoagulants, and of those treated with anticoagulants, almost 50% had large thrombi, and nearly 90% had microvascular thrombi of arterioles and capillaries (42 out of 48). This demonstrates the lack of efficacy of anticoagulation in severe COVID-19 [218]. Furthermore, prohibitive signal for bleeding risk, in addition to futility, has recently led to the discontinuation of high-dose heparin arm in REMAP-CAP, ACTIV-4, and ATTACC studies in severe COVID-19 [218,219,220]. The momentum seems to be finally shifting to antiplatelet agents, both for prevention and treatment, even though the efficacy of these or other agents remains to be demonstrated in preclinical models of COVID-19.
Numerous clinical trials have been initiated to investigate the benefits of antiplatelet therapy in COVID-19. In the NIH ACTIV-4 trial, amongst 657 symptomatic outpatients with COVID-19, the major adverse cardiovascular or pulmonary outcomes were not significantly different for patients randomized to low-dose aspirin, apixaban (2.5 mg twice daily), apixaban (5.0 mg twice daily), or placebo [221]. However, the median time from diagnosis to randomization and from randomization to initiation of study treatment were 7 days and 3 days, respectively, suggesting that survival bias may account for a very low event rate in both placebo and treatment groups. Early administration of aspirin in ambulatory COVID-19 patients appears to provide significant benefit and correlates with a decrease in overall mortality [222], but was not effective in reducing progression to invasive mechanical ventilation or death in hospitalized patients, as reported in the Randomized Evaluation of COVID-19 thERapY (RECOVERY) trial, the world’s largest clinical trial of treatments for patients hospitalized with COVID-19 [223,224]. Aspirin irreversibly inhibits both COX enzymes (COX-1 >> COX-2), preventing prostaglandin production by cells until the new enzyme is produced [225]. Low doses of aspirin, typically 75 to 81 mg/day, are sufficient to irreversibly acetylate serine 530 of COX-1, but have little effect on COX-2 [225]. Therefore, the lack of efficacy of aspirin in hospitalized patients with COVID-19 may be due to inducible COX-2-mediated TxA2 generation and the failure of aspirin to inhibit the effects of TxA2 once synthesized. Moreover, the well-known phenomenon of aspirin resistance in the obese or the elderly has been attributed to increased expression of cytosolic phospholipase A2, and COX-2, which leads to increased generation of TxA2 [226]. Marked increase in TxA2 generation and COX-2 expression in severe COVID-19 raises the specter of aspirin resistance, especially in the elderly or obese patients, as in the general population [227,228]. Plasma from patients with COVID-19 triggered platelet and neutrophil activation and NET formation in vitro; the latter was blocked by therapeutic-dose low-molecular-weight heparin, but not by aspirin [229]. Moreover, the use of aspirin in children with COVID-19 is relatively contraindicated due to the risk of Reye’s syndrome [230].
Furthermore, COX-2 inhibitors are known to increase the risk of cardiovascular events and, therefore, are not advised in SCD or COVID-19 [231,232]. Blocking COX-1 or COX-2 may result in more challenges than cures because of their broad inhibition of several essential prostanoids other than TxA2 [233]. Although TxA2 synthase inhibitors suppress TxA2 formation, accumulation of the substrate prostaglandin (PG)H2 stimulates TP receptor on platelets and the endothelium, thereby inhibiting the antiplatelet action of TxA2 synthase inhibitors [234]. TP receptor antagonists block the activity of both TxA2 and PGH2 on platelets and the endothelium [234]. Thus, early administration of well-tolerated TP receptor antagonists may limit progression to severe COVID-19 [81] and may also be effective in SCD, considering the common pathobiology of thrombo-inflammation in the two disease states.
It has been proposed that blocking the deleterious effects of PGD2 and TxA2 with a dual DP2/TP receptor antagonist, ramatroban, might be beneficial in COVID-19 [136,235]. Ramatroban is a surmountable and potent antagonist of TP receptors. Ramatroban is orally bioavailable and has been used in Japan for the past 20 years as a treatment for allergic rhinitis. Ramatroban has been shown to provide rapid relief of symptoms and successfully treat four patients with severe COVID-19 [168]. This is consistent with the role of TP receptor antagonism in relieving postcapillary pressures, promoting resolution of edema, and improving lung compliance and gas exchange [164,168]. Notably, patients treated with ramatroban did not develop overt long-haul COVID symptoms after recovery from acute illness, supporting the anti-fibrotic effect of ramatroban, as demonstrated in a mouse model of silicosis [168,236].
Ramatroban is 100-150 times more potent than aspirin in inhibiting platelet aggregation, P-selectin expression, and sphingosine-1-phosphate (S1P) release from platelets [237,238,239]. S1P is chemotactic for monocytes and inhibition of S1P release reduces monocyte infiltration [239]. Ramatroban also decreases macrophage infiltration by inhibiting endothelial surface expression of ICAM-1 and VCAM-1, and inhibiting MCP-1 expression on endothelial cells in response to TNF-α or platelet-activating factor [237]. Additionally, the potentiation of CLEC2 signaling by TxA2 was abolished by 10 µM ramatroban, while 1 mM aspirin was only partially effective [84]. In addition to its anti-platelet action, ramatroban also improves vascular responsiveness [237]. With a plasma half-life of about 2 h, the antiplatelet action of ramatroban is reversible [237]. This is of advantage in the event of bleeding complications following anticoagulation in critically ill COVID-19 patients [240], and SCD patients with venous thromboembolism [241].
9. Conclusions
Thrombo-inflammation is a classic feature of both SCD-associated vaso-occlusive crisis and severe COVID-19. Thrombo-inflammation leads to microvascular thrombosis and thrombotic microangiopathy. Both diseases share the pathobiology of endothelial cell injury and activation, platelet activation, and platelet-leukocyte partnership, culminating in thrombo-inflammation. COX-2-mediated increase in TxA2 signaling may play an important role in platelet activation, leading to thrombo-inflammation in both SCD and COVID-19. The failure of the previous anticoagulant and antiplatelet strategies in both SCD and COVID-19 underlines the importance of identifying new therapeutic targets, such as TxA2 and/or PGD2, for the resolution of acute crisis in both diseases.
Acknowledgments
We are grateful to Kalpna Gupta, University of California Irvine, for helpful suggestions and discussion of concepts that form the basis of this manuscript. PS was supported by NIH-NHLBI, R01HL128297, and R01HL141080, American Heart Association 18TPA34170588, funds from the Hemophilia Center of Western Pennsylvania and Vitalant.
Abbreviations
SCD, sickle cell disease; SCT, sickle cell trait; VOC, vaso-occlusive crisis; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; coronavirus disease 2019; RBC, red blood cell; ACS, acute chest syndrome; ICAM-1, intracellular adhesion molecule 1; VCAM-1, vascular-cell adhesion molecule 1; MCP-1, monocyte chemoattractant protein 1; TLR, toll-like receptor; NETs, neutrophil extracellular traps; NO, nitric oxide; CLEC, C-type-lectin-like receptor; LDH, lactate dehydrogenase; TF, tissue factor; DC-SIGN, dendritic cell-specific intercellular adhesion molecule-3-grabbing non-integrin; L-SIGN, liver/lymph node-specific intracellular adhesions molecule-3-grabbing integrin; DAMPs, damage-associated molecular patterns; ROS, reactive oxygen species; Tx, thromboxane; COX, cyclooxygenase; IL, interleukin; TP receptor, thromboxane prostanoid receptor; DP receptor, D-prostanoid receptor; MASP, mannan-binding lectin-associated serine protease; MAC, membrane attack complex; PG, prostaglandin; TNF, tumor necrosis factor; GSDMD, gasdermin D; S1P, sphingosine-1-phosphate.
Author Contributions
A.G. and K.C.C. conceptualized and created the framework for the manuscript and wrote the original draft. P.S. and L.K. participated in drafting the final version. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
A.G. and K.C.C. have filed a patent application for using Ramatroban as an anti-thrombotic and immunomodulator in COVID-19 and hemolytic disease, including sickle cell disease. The patents have been licensed to KARE Biosciences. A.G. and K.C.C. are employees of KARE Biosciences. P.S. receives funding (not relevant to the current study) as a part of sponsored research agreements with CSL Behring Inc., IHP Therapeutics, and Novartis Pharmaceuticals Corporation. P.S. is also the recipient of the 2021 Bayer Hemophilia Award Program (not relevant to the current study). L.K. declared no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Singh A., Brandow A.M., Panepinto J.A. COVID-19 in individuals with sickle cell disease/trait compared with other Black individuals. Blood Adv. 2021;5:1915–1921. doi: 10.1182/bloodadvances.2020003741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Panepinto J.A., Brandow A., Mucalo L., Yusuf F., Singh A., Taylor B., Woods K., Payne A.B., Peacock G., Schieve L.A. Coronavirus Disease among Persons with Sickle Cell Disease, United States, March 20–May 21, 2020. Emerg. Infect. Dis. 2020;26:2473–2476. doi: 10.3201/eid2610.202792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Minniti C.P., Zaidi A.U., Nouraie M., Manwani D., Crouch G.D., Crouch A.S., Callaghan M.U., Carpenter S., Jacobs C., Han J., et al. Clinical predictors of poor outcomes in patients with sickle cell disease and COVID-19 infection. Blood Adv. 2021;5:207–215. doi: 10.1182/bloodadvances.2020003456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boga C., Asma S., Leblebisatan G., Sen N., Tombak A., Demiroglu Y.Z., Yeral M., Akin S., Yesilagac H., Habesoglu M.A., et al. Comparison of the clinical course of COVID-19 infection in sickle cell disease patients with healthcare professionals. Ann. Hematol. 2021;100:2195–2202. doi: 10.1007/s00277-021-04549-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arlet J.B., de Luna G., Khimoud D., Odievre M.H., de Montalembert M., Joseph L., Chantalat-Auger C., Flamarion E., Bartolucci P., Lionnet F., et al. Prognosis of patients with sickle cell disease and COVID-19: A French experience. Lancet Haematol. 2020;7:e632–e634. doi: 10.1016/S2352-3026(20)30204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alkindi S., Elsadek R.A., Al-Madhani A., Al-Musalhi M., AlKindi S.Y., Al-Khadouri G., Al Rawahi B., Al-Ruqeishi S., Al-Yazeedi J., Wali Y.A., et al. Impact of COVID-19 on vasooclusive crisis in patients with sickle cell anaemia. Int. J. Infect. Dis. 2021;106:128–133. doi: 10.1016/j.ijid.2021.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brousse V., Holvoet L., Pescarmona R., Viel S., Perret M., Visseaux B., Ferre V.M., Ithier G., Le Van Kim C., Benkerrou M., et al. Low incidence of COVID-19 severe complications in a large cohort of children with sickle cell disease: A protective role for basal interferon-1 activation? Haematologica. 2021;106:2746–2748. doi: 10.3324/haematol.2021.278573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patricia H., Slim A., Emilie-Fleur G., François G., Vincent B., Darragh D., Sebastien D., Pierre-Louis T., Patrick M., Caroline Le Van K., et al. The proteome of neutrophils in sickle cell disease reveals an unexpected activation of interferon alpha signaling pathway. Haematologica. 2020;105:2851–2854. doi: 10.3324/haematol.2019.238295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madany E., Okwan-Duodu D., Balbuena-Merle R., Hendrickson J.E., Gibb D.R. Potential Implications of a Type 1 Interferon Gene Signature on COVID-19 Severity and Chronic Inflammation in Sickle Cell Disease. Front. Med. 2021;8:679030. doi: 10.3389/fmed.2021.679030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verma A., Huffman J.E., Gao L., Minnier J., Wu W.-C., Cho K., Ho Y.-L., Gorman B.R., Pyarajan S., Rajeevan N., et al. Association of Kidney Comorbidities and Acute Kidney Failure with Unfavorable Outcomes after COVID-19 in Individuals with the Sickle Cell Trait. JAMA Intern. Med. 2022;182:796–804. doi: 10.1001/jamainternmed.2022.2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dun C., Walsh C.M., Bae S., Adalja A., Toner E., Lash T.A., Hashim F., Paturzo J., Segev D.L., Makary M.A. A Machine Learning Study of 534,023 Medicare Beneficiaries with COVID-19: Implications for Personalized Risk Prediction. medRxiv. 2020 doi: 10.1101/2020.10.27.20220970. [DOI] [Google Scholar]
- 12.CDC Data and Statistics on Sickle Cell Disease. [(accessed on 20 February 2022)]; Available online: https://www.cdc.gov/ncbddd/sicklecell/data.html.
- 13.American Society of Hematology Rare Patients with Sickle Cell Disease Live Nearly Twice as Long as Average. [(accessed on 20 February 2022)]. Available online: https://www.hematology.org/newsroom/press-releases/2016/rare-patients-with-sickle-cell-disease-live-nearly-twice-as-long-as-average#.
- 14.Adams R.J., McKie V.C., Hsu L., Files B., Vichinsky E., Pegelow C., Abboud M., Gallagher D., Kutlar A., Nichols F.T., et al. Prevention of a First Stroke by Transfusions in Children with Sickle Cell Anemia and Abnormal Results on Transcranial Doppler Ultrasonography. N. Engl. J. Med. 1998;339:5–11. doi: 10.1056/NEJM199807023390102. [DOI] [PubMed] [Google Scholar]
- 15.Arun S.S., Maria A.L.-I., Rakhi P.N. The molecular basis for the prothrombotic state in sickle cell disease. Haematologica. 2020;105:2368–2379. doi: 10.3324/haematol.2019.239350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Usmani A., Machado R.F. Vascular complications of sickle cell disease. Clin. Hemorheol. Microcirc. 2018;68:205–221. doi: 10.3233/CH-189008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cushman M., Cantrell R.A., McClure L.A., Howard G., Prineas R.J., Moy C.S., Temple E.M., Howard V.J. Estimated 10-year stroke risk by region and race in the United States: Geographic and racial differences in stroke risk. Ann. Neurol. 2008;64:507–513. doi: 10.1002/ana.21493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Naik R.P., Streiff M.B., Haywood C., Segal J.B., Lanzkron S. Venous thromboembolism incidence in the Cooperative Study of Sickle Cell Disease. J. Thromb. Haemost. 2014;12:2010–2016. doi: 10.1111/jth.12744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brunson A., Lei A., Rosenberg A.S., White R.H., Keegan T., Wun T. Increased incidence of VTE in sickle cell disease patients: Risk factors, recurrence and impact on mortality. Br. J. Haematol. 2017;178:319–326. doi: 10.1111/bjh.14655. [DOI] [PubMed] [Google Scholar]
- 20.Ackermann M., Verleden S.E., Kuehnel M., Haverich A., Welte T., Laenger F., Vanstapel A., Werlein C., Stark H., Tzankov A., et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19. N. Engl. J. Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goyal P., Choi J.J., Pinheiro L.C., Schenck E.J., Chen R., Jabri A., Satlin M.J., Campion T.R., Jr., Nahid M., Ringel J.B., et al. Clinical Characteristics of COVID-19 in New York City. N. Engl. J. Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guan W.-J., Ni Z.-Y., Hu Y., Liang W.-H., Ou C.-Q., He J.-X., Liu L., Shan H., Lei C.-L., Hui D.S.C., et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hottz E.D., Azevedo-Quintanilha I.G., Palhinha L., Teixeira L., Barreto E.A., Pao C.R.R., Righy C., Franco S., Souza T.M.L., Kurtz P., et al. Platelet activation and platelet-monocyte aggregates formation trigger tissue factor expression in severe COVID-19 patients. Blood. 2020;136:1330–1341. doi: 10.1182/blood.2020007252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nicolai L., Leunig A., Brambs S., Kaiser R., Weinberger T., Weigand M., Muenchhoff M., Hellmuth J.C., Ledderose S., Schulz H., et al. Immunothrombotic Dysregulation in COVID-19 Pneumonia is Associated with Respiratory Failure and Coagulopathy. Circulation. 2020;142:1176–1189. doi: 10.1161/CIRCULATIONAHA.120.048488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Song W.-C., Fitzgerald G.A. COVID-19, microangiopathy, hemostatic activation, and complement. J. Clin. Investig. 2020;130:3950–3953. doi: 10.1172/JCI140183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rapkiewicz A.V., Mai X., Carsons S.E., Pittaluga S., Kleiner D.E., Berger J.S., Thomas S., Adler N.M., Charytan D.M., Gasmi B., et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: A case series. EClinicalMedicine. 2020;24:100434. doi: 10.1016/j.eclinm.2020.100434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barnes B.J., Adrover J.M., Baxter-Stoltzfus A., Borczuk A., Cools-Lartigue J., Crawford J.M., Daßler-Plenker J., Guerci P., Huynh C., Knight J.S., et al. Targeting potential drivers of COVID-19: Neutrophil extracellular traps. J. Exp. Med. 2020;217:e20200652. doi: 10.1084/jem.20200652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vats R., Brzoska T., Bennewitz M.F., Jimenez M.A., Pradhan-Sundd T., Tutuncuoglu E., Jonassaint J., Gutierrez E., Watkins S.C., Shiva S., et al. Platelet Extracellular Vesicles Drive Inflammasome-IL-1β-Dependent Lung Injury in Sickle Cell Disease. Am. J. Respir. Crit. Care Med. 2020;201:33–46. doi: 10.1164/rccm.201807-1370OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.John N.A., John J., Kamblec P., Singhal A., Daulatabad V., Vamshidhar I.S. Patients with Sticky Platelet Syndrome, Sickle Cell Disease and Glanzmann Syndrome May Promulgate Severe Thrombosis if Infected with COVID-19. Maedica. 2021;16:268–273. doi: 10.26574/maedica.2020.16.2.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jain S., Bakshi N., Krishnamurti L. Acute Chest Syndrome in Children with Sickle Cell Disease. Pediatr. Allergy Immunol. Pulmonol. 2017;30:191–201. doi: 10.1089/ped.2017.0814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Castro O., Brambilla D.J., Thorington B., Reindorf C.A., Scott R.B., Gillette P., Vera J.C., Levy P.S. The acute chest syndrome in sickle cell disease: Incidence and risk factors. The Cooperative Study of Sickle Cell Disease. Blood. 1994;84:643–649. doi: 10.1182/blood.V84.2.643.643. [DOI] [PubMed] [Google Scholar]
- 32.Wilcox S.R. Management of respiratory failure due to COVID-19. BMJ. 2020;369:m1786. doi: 10.1136/bmj.m1786. [DOI] [PubMed] [Google Scholar]
- 33.Mekontso Dessap A., Deux J.F., Habibi A., Abidi N., Godeau B., Adnot S., Brun-Buisson C., Rahmouni A., Galacteros F., Maitre B. Lung imaging during acute chest syndrome in sickle cell disease: Computed tomography patterns and diagnostic accuracy of bedside chest radiograph. Thorax. 2014;69:144–151. doi: 10.1136/thoraxjnl-2013-203775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dako F., Hossain R., Jeudy J., White C. Dual-energy CT evidence of pulmonary microvascular occlusion in patients with sickle cell disease experiencing acute chest syndrome. Clin. Imaging. 2021;78:94–97. doi: 10.1016/j.clinimag.2021.03.018. [DOI] [PubMed] [Google Scholar]
- 35.Cao Y., Geng C., Li Y., Zhang Y. In situ Pulmonary Artery Thrombosis: A Previously Overlooked Disease. Front. Pharmacol. 2021;12:671589. doi: 10.3389/fphar.2021.671589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nouraie M., Zhang X., Srisuwananukorn A., Machado R.F., Gordeuk V.R., Gladwin M.T., Saraf S. Potential Contribution of Pulmonary Thromboembolic Disease in Pulmonary Hypertension in Sickle Cell Disease. Ann. Am. Thorac. Soc. 2020;17:899–901. doi: 10.1513/AnnalsATS.201911-840RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Winchenne A., Cecchini J., Deux J.F., De Prost N., Razazi K., Carteaux G., Galacteros F., Habibi A., Bartolucci P., Melica G., et al. A clinical risk score for pulmonary artery thrombosis during acute chest syndrome in adult patients with sickle cell disease. Br. J. Haematol. 2017;179:627–634. doi: 10.1111/bjh.14914. [DOI] [PubMed] [Google Scholar]
- 38.Adedeji M.O., Cespedes J., Allen K., Subramony C., Hughson M.D. Pulmonary thrombotic arteriopathy in patients with sickle cell disease. Arch. Pathol. Lab. Med. 2001;125:1436–1441. doi: 10.5858/2001-125-1436-PTAIPW. [DOI] [PubMed] [Google Scholar]
- 39.Thomas A.N., Pattison C., Serjeant G.R. Causes of death in sickle-cell disease in Jamaica. Br. Med. J. Clin. Res. Ed. 1982;285:633–635. doi: 10.1136/bmj.285.6342.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mekontso Dessap A., Deux J.F., Abidi N., Lavenu-Bombled C., Melica G., Renaud B., Godeau B., Adnot S., Brochard L., Brun-Buisson C., et al. Pulmonary artery thrombosis during acute chest syndrome in sickle cell disease. Am. J. Respir. Crit. Care Med. 2011;184:1022–1029. doi: 10.1164/rccm.201105-0783OC. [DOI] [PubMed] [Google Scholar]
- 41.Vichinsky E.P., Neumayr L.D., Earles A.N., Williams R., Lennette E.T., Dean D., Nickerson B., Orringer E., McKie V., Bellevue R., et al. Causes and Outcomes of the Acute Chest Syndrome in Sickle Cell Disease. N. Engl. J. Med. 2000;342:1855–1865. doi: 10.1056/NEJM200006223422502. [DOI] [PubMed] [Google Scholar]
- 42.Vichinsky E., Williams R., Das M., Earles A.N., Lewis N., Adler A., McQuitty J. Pulmonary fat embolism: A distinct cause of severe acute chest syndrome in sickle cell anemia. Blood. 1994;83:3107–3112. doi: 10.1182/blood.V83.11.3107.3107. [DOI] [PubMed] [Google Scholar]
- 43.Dang N.C., Johnson C., Eslami-Farsani M., Haywood L.J. Bone marrow embolism in sickle cell disease: A review. Am. J. Hematol. 2005;79:61–67. doi: 10.1002/ajh.20348. [DOI] [PubMed] [Google Scholar]
- 44.Godeau B., Schaeffer A., Bachir D., Fleury-Feith J., Galacteros F., Verra F., Escudier E., Vaillant J.N., Brun-Buisson C., Rahmouni A., et al. Bronchoalveolar lavage in adult sickle cell patients with acute chest syndrome: Value for diagnostic assessment of fat embolism. Am. J. Respir. Crit. Care Med. 1996;153:1691–1696. doi: 10.1164/ajrccm.153.5.8630622. [DOI] [PubMed] [Google Scholar]
- 45.Lechapt E., Habibi A., Bachir D., Galacteros F., Schaeffer A., Desvaux D., Brochard L., Housset B., Godeau B., Maitre B. Induced sputum versus bronchoalveolar lavage during acute chest syndrome in sickle cell disease. Am. J. Respir. Crit. Care Med. 2003;168:1373–1377. doi: 10.1164/rccm.200302-174OC. [DOI] [PubMed] [Google Scholar]
- 46.Anea C.B., Lyon M., Lee I.A., Gonzales J.N., Adeyemi A., Falls G., Kutlar A., Brittain J.E. Pulmonary platelet thrombi and vascular pathology in acute chest syndrome in patients with sickle cell disease. Am. J. Hematol. 2016;91:173–178. doi: 10.1002/ajh.24224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ballas S. The Evolving Pharmacotherapeutic Landscape for the Treatment of Sickle Cell Disease. Mediterr. J. Hematol. Infect. Dis. 2020;12:e2020010. doi: 10.4084/mjhid.2020.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vichinsky E. Emerging ‘A’ therapies in hemoglobinopathies: Agonists, antagonists, antioxidants, and arginine. Hematology. 2012;2012:271–275. doi: 10.1182/asheducation.V2012.1.271.3798318. [DOI] [PubMed] [Google Scholar]
- 49.Kotiah S.D., Ballas S.K. Investigational drugs in sickle cell anemia. Expert Opin. Investig. Drugs. 2009;18:1817–1828. doi: 10.1517/13543780903247463. [DOI] [PubMed] [Google Scholar]
- 50.Zennadi R., Moeller B.J., Whalen E.J., Batchvarova M., Xu K., Shan S., Delahunty M., Dewhirst M.W., Telen M.J. Epinephrine-induced activation of LW-mediated sickle cell adhesion and vaso-occlusion in vivo. Blood. 2007;110:2708–2717. doi: 10.1182/blood-2006-11-056101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sundd P., Gladwin M.T., Novelli E.M. Pathophysiology of Sickle Cell Disease. Annu. Rev. Pathol. Mech. Dis. 2019;14:263–292. doi: 10.1146/annurev-pathmechdis-012418-012838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Archambault A.-S., Zaid Y., Rakotoarivelo V., Doré É., Dubuc I., Martin C., Amar Y., Cheikh A., Fares H., El Hassani A., et al. Lipid storm within the lungs of severe COVID-19 patients: Extensive levels of cyclooxygenase and lipoxygenase-derived inflammatory metabolites. medRxiv. 2020 doi: 10.1101/2020.12.04.20242115. [DOI] [Google Scholar]
- 53.Solovey A., Lin Y., Browne P., Choong S., Wayner E., Hebbel R.P. Circulating activated endothelial cells in sickle cell anemia. N. Engl. J. Med. 1997;337:1584–1590. doi: 10.1056/NEJM199711273372203. [DOI] [PubMed] [Google Scholar]
- 54.Carden M.A., Little J. Emerging disease-modifying therapies for sickle cell disease. Haematologica. 2019;104:1710–1719. doi: 10.3324/haematol.2018.207357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shet A.S., Aras O., Gupta K., Hass M.J., Rausch D.J., Saba N., Koopmeiners L., Key N.S., Hebbel R.P. Sickle blood contains tissue factor–positive microparticles derived from endothelial cells and monocytes. Blood. 2003;102:2678–2683. doi: 10.1182/blood-2003-03-0693. [DOI] [PubMed] [Google Scholar]
- 56.Solovey A., Gui L., Key N.S., Hebbel R.P. Tissue factor expression by endothelial cells in sickle cell anemia. J. Clin. Investig. 1998;101:1899–1904. doi: 10.1172/JCI1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Skendros P., Mitsios A., Chrysanthopoulou A., Mastellos D.C., Metallidis S., Rafailidis P., Ntinopoulou M., Sertaridou E., Tsironidou V., Tsigalou C., et al. Complement and tissue factor-enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J. Clin. Investig. 2020;130:6151–6157. doi: 10.1172/JCI141374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Belcher J.D., Chen C., Nguyen J., Milbauer L., Abdulla F., Alayash A.I., Smith A., Nath K.A., Hebbel R.P., Vercellotti G.M. Heme triggers TLR4 signaling leading to endothelial cell activation and vaso-occlusion in murine sickle cell disease. Blood. 2014;123:377–390. doi: 10.1182/blood-2013-04-495887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang D., Xu C., Manwani D., Frenette P.S. Neutrophils, platelets, and inflammatory pathways at the nexus of sickle cell disease pathophysiology. Blood. 2016;127:801–809. doi: 10.1182/blood-2015-09-618538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rodrigues T.S., De Sá K.S.G., Ishimoto A.Y., Becerra A., Oliveira S., Almeida L., Gonçalves A.V., Perucello D.B., Andrade W.A., Castro R., et al. Inflammasomes are activated in response to SARS-CoV-2 infection and are associated with COVID-19 severity in patients. J. Exp. Med. 2021;218:e20201707. doi: 10.1084/jem.20201707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vats R., Kaminski T.W., Brzoska T., Leech J.A., Tutuncuoglu E., Katoch O., Jonassaint J.C., Tejero J., Novelli E.M., Pradhan-Sundd T., et al. Liver to lung microembolic NETs promote Gasdermin-D-dependent inflammatory lung injury in Sickle Cell Disease. Blood. 2022;140:1020–1037. doi: 10.1182/blood.2021014552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rees D.C., Williams T.N., Gladwin M.T. Sickle-cell disease. Lancet. 2010;376:2018–2031. doi: 10.1016/S0140-6736(10)61029-X. [DOI] [PubMed] [Google Scholar]
- 63.Joshua H.B., Martina C., Ying D., Eleyna M., Alexander S., Lubka T.R., Jordan D.D., Steve P.W., Julie R. Heme induces human and mouse platelet activation through C-type-lectin-like receptor-2. Haematologica. 2020;106:626–629. doi: 10.3324/haematol.2020.246488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Singla S., Sysol J.R., Dille B., Jones N., Chen J., Machado R.F. Hemin Causes Lung Microvascular Endothelial Barrier Dysfunction by Necroptotic Cell Death. Am. J. Respir. Cell Mol. Biol. 2017;57:307–314. doi: 10.1165/rcmb.2016-0287OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mendonça R., Silveira A.A.A., Conran N. Red cell DAMPs and inflammation. Inflamm. Res. 2016;65:665–678. doi: 10.1007/s00011-016-0955-9. [DOI] [PubMed] [Google Scholar]
- 66.Pitanga T.N., Oliveira R.R., Zanette D.L., Guarda C.C., Santiago R.P., Santana S.S., Nascimento V.M.L., Lima J.B., Carvalho G.Q., Maffili V.V., et al. Sickle red cells as danger signals on proinflammatory gene expression, leukotriene B4 and interleukin-1 beta production in peripheral blood mononuclear cell. Cytokine. 2016;83:75–84. doi: 10.1016/j.cyto.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 67.Chen G., Zhang D., Fuchs T.A., Manwani D., Wagner D.D., Frenette P.S. Heme-induced neutrophil extracellular traps contribute to the pathogenesis of sickle cell disease. Blood. 2014;123:3818–3827. doi: 10.1182/blood-2013-10-529982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kaul D.K., Finnegan E., Barabino G.A. Sickle Red Cell–Endothelium Interactions. Microcirculation. 2009;16:97–111. doi: 10.1080/10739680802279394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Scheim D. From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate, Then Clot Blood Cells in Pulmonary and Systemic Microvasculature. SSRN. 2020;28 doi: 10.2139/ssrn.3706347. [DOI] [Google Scholar]
- 70.Modrof J., Kerschbaum A., Farcet M.R., Niemeyer D., Corman V.M., Kreil T.R. SARS-CoV-2 and the safety margins of cell-based biological medicinal products. Biologicals. 2020;68:122–124. doi: 10.1016/j.biologicals.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lam L.M., Murphy S.J., Kuri-Cervantes L., Weisman A.R., Ittner C.A.G., Reilly J.P., Pampena M.B., Betts M.R., Wherry E.J., Song W.-C., et al. Erythrocytes Reveal Complement Activation in Patients with COVID-19. medRxiv. 2020 doi: 10.1101/2020.05.20.20104398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Diorio C., McNerney K.O., Lambert M., Paessler M., Anderson E.M., Henrickson S.E., Chase J., Liebling E.J., Burudpakdee C., Lee J.H., et al. Evidence of thrombotic microangiopathy in children with SARS-CoV-2 across the spectrum of clinical presentations. Blood Adv. 2020;4:6051–6063. doi: 10.1182/bloodadvances.2020003471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sweeney J.M., Barouqa M., Krause G.J., Gonzalez-Lugo J.D., Rahman S., Gil M.R. Evidence for secondary thrombotic microangiopathy in COVID-19. medRxiv. 2020 doi: 10.1101/2020.10.20.20215608. [DOI] [Google Scholar]
- 74.He X., Yao F., Chen J., Wang Y., Fang X., Lin X., Long H., Wang Q., Wu Q. The poor prognosis and influencing factors of high D-dimer levels for COVID-19 patients. Sci. Rep. 2021;11:1830. doi: 10.1038/s41598-021-81300-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dar J., Mughal I., Mekki T., Chapunduka Z., Hassan I. Raised D-dimer levels in acute sickle cell crisis and their correlation with chest X-ray abnormalities. Ger. Med. Sci. GMS E J. 2010;8:Doc25. doi: 10.3205/000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Francis R.B., Jr. Elevated fibrin D-dimer fragment in sickle cell anemia: Evidence for activation of coagulation during the steady state as well as in painful crisis. Haemostasis. 1989;19:105–111. doi: 10.1159/000215901. [DOI] [PubMed] [Google Scholar]
- 77.Bosevski M., Krstevski G., Bosevska G., Kapsarov K., Dodic E., Feehan J., Stojanoska L., Apostolopoulos V. The role of D-dimer in relation to the clinical course of patients with COVID-19. Acta Biochim. Biophys. Sin. 2020;53:119–120. doi: 10.1093/abbs/gmaa140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mouhat B., Besutti M., Bouiller K., Grillet F., Monnin C., Ecarnot F., Behr J., Capellier G., Soumagne T., Pili-Floury S., et al. Elevated D-dimers and lack of anticoagulation predict PE in severe COVID-19 patients. Eur. Respir. J. 2020;56:2001811. doi: 10.1183/13993003.01811-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nebor D., Bowers A., Connes P., Hardy-Dessources M.-D., Knight-Madden J., Cumming V., Reid M., Romana M. Plasma Concentration of Platelet-Derived Microparticles Is Related to Painful Vaso-Occlusive Phenotype Severity in Sickle Cell Anemia. PLoS ONE. 2014;9:e87243. doi: 10.1371/journal.pone.0087243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zaid Y., Puhm F., Allaeys I., Naya A., Oudghiri M., Khalki L., Limami Y., Zaid N., Sadki K., Haj R.B.E., et al. Platelets Can Associate with SARS-CoV-2 RNA and Are Hyperactivated in COVID-19. Circ. Res. 2020;127:1404–1418. doi: 10.1161/CIRCRESAHA.120.317703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Theken K.N., Fitzgerald G.A. Bioactive lipids in antiviral immunity. Science. 2021;371:237–238. doi: 10.1126/science.abf3192. [DOI] [PubMed] [Google Scholar]
- 82.Amraei R., Yin W., Napoleon M.A., Suder E.L., Berrigan J., Zhao Q., Olejnik J., Chandler K.B., Xia C., Feldman J., et al. CD209L/L-SIGN and CD209/DC-SIGN Act as Receptors for SARS-CoV-2. ACS Cent. Sci. 2021;7:1156–1165. doi: 10.1021/acscentsci.0c01537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sung P.-S., Huang T.-F., Hsieh S.-L. Extracellular vesicles from CLEC2-activated platelets enhance dengue virus-induced lethality via CLEC5A/TLR2. Nat. Commun. 2019;10:2402. doi: 10.1038/s41467-019-10360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Badolia R., Inamdar V., Manne B.K., Dangelmaier C., Eble J.A., Kunapuli S.P. G(q) pathway regulates proximal C-type lectin-like receptor-2 (CLEC-2) signaling in platelets. J. Biol. Chem. 2017;292:14516–14531. doi: 10.1074/jbc.M117.791012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ataga K.I., Kutlar A., Kanter J., Liles D., Cancado R., Friedrisch J., Guthrie T.H., Knight-Madden J., Alvarez O.A., Gordeuk V.R., et al. Crizanlizumab for the Prevention of Pain Crises in Sickle Cell Disease. N. Engl. J. Med. 2016;376:429–439. doi: 10.1056/NEJMoa1611770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bennewitz M.F., Jimenez M.A., Vats R., Tutuncuoglu E., Jonassaint J., Kato G.J., Gladwin M.T., Sundd P. Lung vaso-occlusion in sickle cell disease mediated by arteriolar neutrophil-platelet microemboli. JCI Insight. 2017;2:e89761. doi: 10.1172/jci.insight.89761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Voskaridou E., Aimilia M., Flevari P., Dimopoulou M., Komninaka V., Repa K., Papassotiriou I. Soluble P-Selectin Levels in Patients with Sickle Cell Disease Reflect Platelets’ Activation Rather Than Endothelial Dysfunction. Blood. 2019;134:4829. doi: 10.1182/blood-2019-122524. [DOI] [Google Scholar]
- 88.Goshua G., Pine A.B., Meizlish M.L., Chang C.H., Zhang H., Bahel P., Baluha A., Bar N., Bona R.D., Burns A.J., et al. Endotheliopathy in COVID-19-associated coagulopathy: Evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7:e575–e582. doi: 10.1016/S2352-3026(20)30216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Leucker T.M., Osburn W.O., Reventun P., Smith K., Claggett B., Kirwan B.-A., de Brouwer S., Williams M.S., Gerstenblith G., Hager D.N., et al. Effect of Crizanlizumab, a P-Selectin Inhibitor, in COVID-19: A Placebo-Controlled, Randomized Trial. JACC Basic Transl. Sci. 2021;6:935–945. doi: 10.1016/j.jacbts.2021.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Grover S.P., Mackman N. Tissue Factor. Arterioscler. Thromb. Vasc. Biol. 2018;38:709–725. doi: 10.1161/ATVBAHA.117.309846. [DOI] [PubMed] [Google Scholar]
- 91.Mackman N. Role of Tissue Factor in Hemostasis, Thrombosis, and Vascular Development. Arterioscler. Thromb. Vasc. Biol. 2004;24:1015–1022. doi: 10.1161/01.ATV.0000130465.23430.74. [DOI] [PubMed] [Google Scholar]
- 92.Pawlinski R., Pedersen B., Erlich J., Mackman N. Role of tissue factor in haemostasis, thrombosis, angiogenesis and inflammation: Lessons from low tissue factor mice. Thromb. Haemost. 2004;92:444–450. doi: 10.1160/TH04-05-0309. [DOI] [PubMed] [Google Scholar]
- 93.Sparkenbaugh E.M., Chen C., Brzoska T., Nguyen J., Wang S., Vercellotti G.M., Key N.S., Sundd P., Belcher J.D., Pawlinski R. Thrombin activation of PAR-1 contributes to microvascular stasis in mouse models of sickle cell disease. Blood. 2020;135:1783–1787. doi: 10.1182/blood.2019003543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Karpusas M., Hsu Y.M., Wang J.H., Thompson J., Lederman S., Chess L., Thomas D. 2 A crystal structure of an extracellular fragment of human CD40 ligand. Structure. 1995;3:1031–1039. doi: 10.1016/S0969-2126(01)00239-8. [DOI] [PubMed] [Google Scholar]
- 95.Elgueta R., Benson M.J., De Vries V.C., Wasiuk A., Guo Y., Noelle R.J. Molecular mechanism and function of CD40/CD40L engagement in the immune system. Immunol. Rev. 2009;229:152–172. doi: 10.1111/j.1600-065X.2009.00782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lee S.P., Ataga K.I., Orringer E.P., Phillips D.R., Parise L.V. Biologically active CD40 ligand is elevated in sickle cell anemia: Potential role for platelet-mediated inflammation. Arterioscler. Thromb. Vasc. Biol. 2006;26:1626–1631. doi: 10.1161/01.ATV.0000220374.00602.a2. [DOI] [PubMed] [Google Scholar]
- 97.Nicola C., Erich V.D.P. Thromboinflammatory mechanisms in sickle cell disease—Challenging the hemostatic balance. Haematologica. 2020;105:2380–2390. doi: 10.3324/haematol.2019.239343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Novelli E.M., Kato G.J., Ragni M.V., Zhang Y., Hildesheim M.E., Nouraie M., Barge S., Meyer M.P., Hassett A.C., Gordeuk V.R., et al. Plasma thrombospondin-1 is increased during acute sickle cell vaso-occlusive events and associated with acute chest syndrome, hydroxyurea therapy, and lower hemolytic rates. Am. J. Hematol. 2012;87:326–330. doi: 10.1002/ajh.22274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Portier I., Campbell R.A. Role of Platelets in Detection and Regulation of Infection. Arterioscler. Thromb. Vasc. Biol. 2020;41:70–78. doi: 10.1161/ATVBAHA.120.314645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Merad M., Martin J.C. Pathological inflammation in patients with COVID-19: A key role for monocytes and macrophages. Nat. Rev. Immunol. 2020;20:355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Courjon J., Dufies O., Robert A., Bailly L., Torre C., Chirio D., Contenti J., Vitale S., Loubatier C., Doye A., et al. Heterogeneous NLRP3 inflammasome signature in circulating myeloid cells as a biomarker of COVID-19 severity. Blood Adv. 2021;5:1523–1534. doi: 10.1182/bloodadvances.2020003918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Rolfes V., Ribeiro L.S., Hawwari I., Bottcher L., Rosero N., Maasewerd S., Santos M.L.S., Prochnicki T., Silva C.M.S., Wanderley C.W.S., et al. Platelets Fuel the Inflammasome Activation of Innate Immune Cells. Cell Rep. 2020;31:107615. doi: 10.1016/j.celrep.2020.107615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ferreira A.C., Soares V.C., de Azevedo-Quintanilha I.G., da Silva Gomes Dias S., Fintelman-Rodrigues N., Sacramento C.Q., Mattos M., de Freitas C.S., Temerozo J.R., Teixeira L., et al. SARS-CoV-2 induces inflammasome-dependent pyroptosis and downmodulation of HLA-DR in human monocytes. medRxiv. 2020 doi: 10.1101/2020.08.25.20182055. [DOI] [Google Scholar]
- 104.Kucia M., Ratajczak J., Bujko K., Adamiak M., Ciechanowicz A., Chumak V., Brzezniakiewicz-Janus K., Ratajczak M.Z. An evidence that SARS-CoV-2/COVID-19 spike protein (SP) damages hematopoietic stem/progenitor cells in the mechanism of pyroptosis in Nlrp3 inflammasome-dependent manner. Leukemia. 2021;35:3026–3029. doi: 10.1038/s41375-021-01332-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Aschenbrenner A.C., Mouktaroudi M., Krämer B., Oestreich M., Antonakos N., Nuesch-Germano M., Gkizeli K., Bonaguro L., Reusch N., Baßler K., et al. Disease severity-specific neutrophil signatures in blood transcriptomes stratify COVID-19 patients. Genome Med. 2021;13:7. doi: 10.1186/s13073-020-00823-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Vogel S., Arora T., Wang X., Mendelsohn L., Nichols J., Allen D., Shet A.S., Combs C.A., Quezado Z.M.N., Thein S.L. The platelet NLRP3 inflammasome is upregulated in sickle cell disease via HMGB1/TLR4 and Bruton tyrosine kinase. Blood Adv. 2018;2:2672–2680. doi: 10.1182/bloodadvances.2018021709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Silva C.M., Wanderley C.W.S., Veras F.P., Gonçalves A.V., Lima M.H.F., Toller Kawahisa J.E., Gomes G.F., Nascimento D.C., Silva Monteiro V.V., Paiva I.M., et al. Gasdermin-D activation by SARS-CoV-2 trigger NET and mediate COVID-19 immunopathology. medRxiv. 2022 doi: 10.1186/s13054-022-04062-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kibbe M., Billiar T., Tzeng E. Inducible nitric oxide synthase and vascular injury. Cardiovasc. Res. 1999;43:650–657. doi: 10.1016/S0008-6363(99)00130-3. [DOI] [PubMed] [Google Scholar]
- 109.Gladwin M.T., Sachdev V. Cardiovascular abnormalities in sickle cell disease. J. Am. Coll. Cardiol. 2012;59:1123–1133. doi: 10.1016/j.jacc.2011.10.900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Miller A.C., Gladwin M.T. Pulmonary complications of sickle cell disease. Am. J. Respir. Crit. Care Med. 2012;185:1154–1165. doi: 10.1164/rccm.201111-2082CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Liu X., Miller M.J.S., Joshi M.S., Sadowska-Krowicka H., Clark D.A., Lancaster J.R. Diffusion-limited Reaction of Free Nitric Oxide with Erythrocytes. J. Biol. Chem. 1998;273:18709–18713. doi: 10.1074/jbc.273.30.18709. [DOI] [PubMed] [Google Scholar]
- 112.Reiter C.D., Wang X., Tanus-Santos J.E., Hogg N., Cannon R.O., 3rd, Schechter A.N., Gladwin M.T. Cell-free hemoglobin limits nitric oxide bioavailability in sickle-cell disease. Nat. Med. 2002;8:1383–1389. doi: 10.1038/nm1202-799. [DOI] [PubMed] [Google Scholar]
- 113.Kyle Mack A., Kato G.J. Sickle cell disease and nitric oxide: A paradigm shift? Int. J. Biochem. Cell Biol. 2006;38:1237–1243. doi: 10.1016/j.biocel.2006.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gladwin M.T., Kato G.J., Weiner D., Onyekwere O.C., Dampier C., Hsu L., Hagar R.W., Howard T., Nuss R., Okam M.M., et al. Nitric Oxide for Inhalation in the Acute Treatment of Sickle Cell Pain Crisis: A Randomized Controlled Trial. JAMA. 2011;305:893–902. doi: 10.1001/jama.2011.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Green S.J. COVID-19 accelerates endothelial dysfunction and nitric oxide deficiency. Microbes Infect. 2020;22:149–150. doi: 10.1016/j.micinf.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Akerström S., Gunalan V., Keng C.T., Tan Y.J., Mirazimi A. Dual effect of nitric oxide on SARS-CoV replication: Viral RNA production and palmitoylation of the S protein are affected. Virology. 2009;395:1–9. doi: 10.1016/j.virol.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Akerström S., Mousavi-Jazi M., Klingström J., Leijon M., Lundkvist A., Mirazimi A. Nitric oxide inhibits the replication cycle of severe acute respiratory syndrome coronavirus. J. Virol. 2005;79:1966–1969. doi: 10.1128/JVI.79.3.1966-1969.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jin Y., Ji W., Yang H., Chen S., Zhang W., Duan G. Endothelial activation and dysfunction in COVID-19: From basic mechanisms to potential therapeutic approaches. Signal Transduct. Target. Ther. 2020;5:293. doi: 10.1038/s41392-020-00454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Alvarez R.A., Berra L., Gladwin M.T. Home Nitric Oxide Therapy for COVID-19. Am. J. Respir. Crit. Care Med. 2020;202:16–20. doi: 10.1164/rccm.202005-1906ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Claudia R.M., Frans A.K., Lisa L., Michael A., Nancy S., Melinee S., Ginny G., Lynne N., Elliott P.V. A randomized, placebo-controlled trial of arginine therapy for the treatment of children with sickle cell disease hospitalized with vaso-occlusive pain episodes. Haematologica. 2013;98:1375–1382. doi: 10.3324/haematol.2013.086637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Longobardo A., Montanari C., Shulman R., Benhalim S., Singer M., Arulkumaran N. Inhaled nitric oxide produces minimal improvement in oxygenation in COVID-19 related ARDS. Br. J. Anaesth. 2020;126:E44–E46. doi: 10.1016/j.bja.2020.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kubiczkova L., Sedlarikova L., Hajek R., Sevcikova S. TGF-β—An excellent servant but a bad master. J. Transl. Med. 2012;10:183. doi: 10.1186/1479-5876-10-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Derynck R., Jarrett J.A., Chen E.Y., Eaton D.H., Bell J.R., Assoian R.K., Roberts A.B., Sporn M.B., Goeddel D.V. Human transforming growth factor-beta complementary DNA sequence and expression in normal and transformed cells. Nature. 1985;316:701–705. doi: 10.1038/316701a0. [DOI] [PubMed] [Google Scholar]
- 124.Ask K., Bonniaud P., Maass K., Eickelberg O., Margetts P.J., Warburton D., Groffen J., Gauldie J., Kolb M. Progressive pulmonary fibrosis is mediated by TGF-beta isoform 1 but not TGF-beta3. Int. J. Biochem. Cell Biol. 2008;40:484–495. doi: 10.1016/j.biocel.2007.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bonniaud P., Margetts P.J., Kolb M., Schroeder J.A., Kapoun A.M., Damm D., Murphy A., Chakravarty S., Dugar S., Higgins L., et al. Progressive transforming growth factor beta1-induced lung fibrosis is blocked by an orally active ALK5 kinase inhibitor. Am. J. Respir. Crit. Care Med. 2005;171:889–898. doi: 10.1164/rccm.200405-612OC. [DOI] [PubMed] [Google Scholar]
- 126.Nakamura T., Sakata R., Ueno T., Sata M., Ueno H. Inhibition of transforming growth factor beta prevents progression of liver fibrosis and enhances hepatocyte regeneration in dimethylnitrosamine-treated rats. Hepatology. 2000;32:247–255. doi: 10.1053/jhep.2000.9109. [DOI] [PubMed] [Google Scholar]
- 127.Fukasawa H., Yamamoto T., Suzuki H., Togawa A., Ohashi N., Fujigaki Y., Uchida C., Aoki M., Hosono M., Kitagawa M., et al. Treatment with anti-TGF-beta antibody ameliorates chronic progressive nephritis by inhibiting Smad/TGF-beta signaling. Kidney Int. 2004;65:63–74. doi: 10.1111/j.1523-1755.2004.00393.x. [DOI] [PubMed] [Google Scholar]
- 128.Daniels C.E., Wilkes M.C., Edens M., Kottom T.J., Murphy S.J., Limper A.H., Leof E.B. Imatinib mesylate inhibits the profibrogenic activity of TGF-beta and prevents bleomycin-mediated lung fibrosis. J. Clin. Invest. 2004;114:1308–1316. doi: 10.1172/JCI200419603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Assoian R.K., Komoriya A., Meyers C.A., Miller D.M., Sporn M.B. Transforming growth factor-beta in human platelets. Identification of a major storage site, purification, and characterization. J. Biol. Chem. 1983;258:7155–7160. doi: 10.1016/S0021-9258(18)32345-7. [DOI] [PubMed] [Google Scholar]
- 130.Torres Lde S., Okumura J.V., da Silva D.G., Belini Júnior É., de Oliveira R.G., Mimura K.K., Lobo C.L., Oliani S.M., Bonini Domingos C.R. Plasma levels of TGF-β1 in homeostasis of the inflammation in sickle cell disease. Cytokine. 2016;80:18–25. doi: 10.1016/j.cyto.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 131.Santiago R.P., Carvalho M.O.S., Figueiredo C.V.B., Fiuza L.M., Oliveira R.M., Yahouédéhou S.C.M.A., Nascimento V.M.L., Lyra I.M., Araujo-Santos T., Luz N.F., et al. Associations between TGF-β1 Levels and Markers of Hemolysis, Inflammation, and Tissue Remodeling in Pediatric Sickle Cell Patients. Mediat. Inflamm. 2021;2021:4651891. doi: 10.1155/2021/4651891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Witkowski M., Tizian C., Ferreira-Gomes M., Niemeyer D., Jones T.C., Heinrich F., Frischbutter S., Angermair S., Hohnstein T., Mattiola I., et al. Untimely TGFβ responses in COVID-19 limit antiviral functions of NK cells. Nature. 2021;600:295–301. doi: 10.1038/s41586-021-04142-6. [DOI] [PubMed] [Google Scholar]
- 133.Opene M., Kurantsin-Mills J., Husain S., Ibe B.O. Sickle erythrocytes and platelets augment lung leukotriene synthesis with downregulation of anti-inflammatory proteins: Relevance in the pathology of the acute chest syndrome. Pulm. Circ. 2014;4:482–495. doi: 10.1086/677363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Field J.J., Kassim A., Brandow A., Embury S.H., Matsui N., Wilkerson K., Bryant V., Zhang L., Simpson P., DeBaun M.R. Phase 2 trial of montelukast for prevention of pain in sickle cell disease. Blood Adv. 2020;4:1159–1165. doi: 10.1182/bloodadvances.2019001165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Žarković N., Łuczaj W., Jarocka-Karpowicz I., Orehovec B., Baršić B., Tarle M., Kmet M., Lukšić I., Biernacki M., Skrzydlewska E. Diversified Effects of COVID-19 as a Consequence of the Differential Metabolism of Phospholipids and Lipid Peroxidation Evaluated in the Plasma of Survivors and Deceased Patients upon Admission to the Hospital. Int. J. Mol. Sci. 2022;23:11810. doi: 10.3390/ijms231911810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Archambault A.S., Zaid Y., Rakotoarivelo V., Turcotte C., Doré É., Dubuc I., Martin C., Flamand O., Amar Y., Cheikh A., et al. High levels of eicosanoids and docosanoids in the lungs of intubated COVID-19 patients. FASEB J. 2021;35:e21666. doi: 10.1096/fj.202100540R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Camera M., Canzano P., Brambilla M., Rovati G.E. Montelukast Inhibits Platelet Activation Induced by Plasma From COVID-19 Patients. Front. Pharmacol. 2022;13:784214. doi: 10.3389/fphar.2022.784214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kerget B., Kerget F., Aydın M., Karaşahin Ö. Effect of montelukast therapy on clinical course, pulmonary function, and mortality in patients with COVID-19. J. Med. Virol. 2022;94:1950–1958. doi: 10.1002/jmv.27552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Rucker D., Dhamoon A.S. Physiology, Thromboxane A2. StatPearls; Treasure Island, FL, USA: 2020. [PubMed] [Google Scholar]
- 140.Kurantsin-Mills J., Ibe B.O., Natta C.L., Raj J.U., Siegel R.S., Lessin L.S. Elevated urinary levels of thromboxane and prostacyclin metabolities in sickle cell disease reflects activated platelets in the circulation. Br. J. Haematol. 1994;87:580–585. doi: 10.1111/j.1365-2141.1994.tb08316.x. [DOI] [PubMed] [Google Scholar]
- 141.Foulon I., Bachir D., Galacteros F., Maclouf J. Increased in vivo production of thromboxane in patients with sickle cell disease is accompanied by an impairment of platelet functions to the thromboxane A2 agonist U46619. Arterioscler. Thromb. A J. Vasc. Biol. 1993;13:421–426. doi: 10.1161/01.ATV.13.3.421. [DOI] [PubMed] [Google Scholar]
- 142.Ibe B.O., Morris J., Kurantsin-Mills J., Raj J.U. Sickle erythrocytes induce prostacyclin and thromboxane synthesis by isolated perfused rat lungs. Am. J. Physiol. Lung Cell. Mol. Physiol. 1997;272:L597–L602. doi: 10.1152/ajplung.1997.272.4.L597. [DOI] [PubMed] [Google Scholar]
- 143.Tantry U.S., Bliden K.P., Cho A., Walia N., Dahlen J.R., Ens G., Traianova M., Jerjian C., Usman A., Gurbel P.A. First Experience Addressing the Prognostic Utility of Novel Urinary Biomarkers in Patients with COVID-19. Open Forum Infect. Dis. 2021;8:ofab274. doi: 10.1093/ofid/ofab274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wenzel S.E., Westcott J.Y., Smith H.R., Larsen G.L. Spectrum of prostanoid release after bronchoalveolar allergen challenge in atopic asthmatics and in control groups. An alteration in the ratio of bronchoconstrictive to bronchoprotective mediators. Am. Rev. Respir. Dis. 1989;139:450–457. doi: 10.1164/ajrccm/139.2.450. [DOI] [PubMed] [Google Scholar]
- 145.Kaul D.K., Liu X.-D., Chang H.-Y., Nagel R.L., Fabry M.E. Effect of fetal hemoglobin on microvascular regulation in sickle transgenic-knockout mice. J. Clin. Investig. 2004;114:1136–1145. doi: 10.1172/JCI200421633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sharma A., Garcia G., Jr., Wang Y., Plummer J.T., Morizono K., Arumugaswami V., Svendsen C.N. Human iPSC-Derived Cardiomyocytes Are Susceptible to SARS-CoV-2 Infection. Cell Rep. Med. 2020;1:100052. doi: 10.1016/j.xcrm.2020.100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Ricke-Hoch M., Stelling E., Lasswitz L., Gunesch A.P., Kasten M., Zapatero-Belinchón F.J., Brogden G., Gerold G., Pietschmann T., Montiel V., et al. Impaired immune response mediated by prostaglandin E2 promotes severe COVID-19 disease. PLoS ONE. 2021;16:e0255335. doi: 10.1371/journal.pone.0255335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Rouzer C.A., Marnett L.J. Cyclooxygenases: Structural and functional insights. J. Lipid Res. 2009;50:S29–S34. doi: 10.1194/jlr.R800042-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pillinger M.H., Capodici C., Rosenthal P., Kheterpal N., Hanft S., Philips M.R., Weissmann G. Modes of action of aspirin-like drugs: Salicylates inhibit erk activation and integrin-dependent neutrophil adhesion. Proc. Natl. Acad. Sci. USA. 1998;95:14540–14545. doi: 10.1073/pnas.95.24.14540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ishizuka T., Kawakami M., Hidaka T., Matsuki Y., Takamizawa M., Suzuki K., Kurita A., Nakamura H. Stimulation with thromboxane A2 (TXA2) receptor agonist enhances ICAM-1, VCAM-1 or ELAM-1 expression by human vascular endothelial cells. Clin. Exp. Immunol. 1998;112:464–470. doi: 10.1046/j.1365-2249.1998.00614.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Matsui Y., Amano H., Ito Y., Eshima K., Suzuki T., Ogawa F., Iyoda A., Satoh Y., Kato S., Nakamura M., et al. Thromboxane A2 receptor signaling facilitates tumor colonization through P-selectin-mediated interaction of tumor cells with platelets and endothelial cells. Cancer Sci. 2012;103:700–707. doi: 10.1111/j.1349-7006.2012.02200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bode M., Mackman N. Regulation of tissue factor gene expression in monocytes and endothelial cells: Thromboxane A2 as a new player. Vasc. Pharmacol. 2014;62:57–62. doi: 10.1016/j.vph.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Del Turco S., Basta G., Lazzerini G., Chancharme L., Lerond L., De Caterina R. Involvement of the TP receptor in TNF-alpha-induced endothelial tissue factor expression. Vascul. Pharmacol. 2014;62:49–56. doi: 10.1016/j.vph.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 154.Eligini S., Violi F., Banfi C., Barbieri S., Brambilla M., Saliola M., Tremoli E., Colli S. Indobufen inhibits tissue factor in human monocytes through a thromboxane-mediated mechanism. Cardiovasc. Res. 2006;69:218–226. doi: 10.1016/j.cardiores.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 155.Santilli F., Davì G., Consoli A., Cipollone F., Mezzetti A., Falco A., Taraborelli T., Devangelio E., Ciabattoni G., Basili S., et al. Thromboxane-Dependent CD40 Ligand Release in Type 2 Diabetes Mellitus. J. Am. Coll. Cardiol. 2006;47:391–397. doi: 10.1016/j.jacc.2005.03.079. [DOI] [PubMed] [Google Scholar]
- 156.Wang G.-R., Zhu Y., Halushka P.V., Lincoln T.M., Mendelsohn M.E. Mechanism of platelet inhibition by nitric oxide: In vivo phosphorylation of thromboxane receptor by cyclic GMP-dependent protein kinase. Proc. Natl. Acad. Sci. USA. 1998;95:4888–4893. doi: 10.1073/pnas.95.9.4888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Shiokoshi T., Ohsaki Y., Kawabe J., Fujino T., Kikuchi K. Downregulation of nitric oxide accumulation by cyclooxygenase-2 induction and thromboxane A2 production in interleukin-1β-stimulated rat aortic smooth muscle cells. J. Hypertens. 2002;20:455–461. doi: 10.1097/00004872-200203000-00021. [DOI] [PubMed] [Google Scholar]
- 158.Craven P.A., Studer R.K., DeRubertis F.R. Thromboxane/Prostaglandin Endoperoxide-Induced Hypertrophy of Rat Vascular Smooth Muscle Cells Is Signaled by Protein Kinase C-Dependent Increases in Transforming Growth Factor-β. Hypertension. 1996;28:169–176. doi: 10.1161/01.HYP.28.2.169. [DOI] [PubMed] [Google Scholar]
- 159.Negrete H., Studer R.K., Craven P.A., DeRubertis F.R. Role for transforming growth factor beta in thromboxane-induced increases in mesangial cell fibronectin synthesis. Diabetes. 1995;44:335–339. doi: 10.2337/diab.44.3.335. [DOI] [PubMed] [Google Scholar]
- 160.D’Agostino I., Tacconelli S., Bruno A., Contursi A., Mucci L., Hu X., Xie Y., Chakraborty R., Jain K., Sacco A., et al. Low-dose Aspirin prevents hypertension and cardiac fibrosis when thromboxane A2 is unrestrained. Pharmacol. Res. 2021;170:105744. doi: 10.1016/j.phrs.2021.105744. [DOI] [PubMed] [Google Scholar]
- 161.Wood K., Gladwin M., Straub A. Sickle cell disease: At the crossroads of pulmonary hypertension and diastolic heart failure. Heart. 2019;106:562–568. doi: 10.1136/heartjnl-2019-314810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Gordeuk V.R., Castro O.L., Machado R.F. Pathophysiology and treatment of pulmonary hypertension in sickle cell disease. Blood. 2016;127:820–828. doi: 10.1182/blood-2015-08-618561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Larsson A.K., Hagfjärd A., Dahlén S.E., Adner M. Prostaglandin D2 induces contractions through activation of TP receptors in peripheral lung tissue from the guinea pig. Eur. J. Pharmacol. 2011;669:136–142. doi: 10.1016/j.ejphar.2011.07.046. [DOI] [PubMed] [Google Scholar]
- 164.Schuster D.P., Kozlowski J., Brimiouelle S. Effect of thromboxane receptor blockade on pulmonary capillary hypertension in acute lung injury; Proceedings of the 2001 Meeting of the American Thoracic Society; San Francisco, CA, USA. 18–23 May 2001. [Google Scholar]
- 165.Carrier E.J., Kim K., Noll N.A., Macias-Perez I., Merryman W.D., Knollmann B.C., West J.D. Abstract 261: Activation of the Thromboxane/Prostanoid Receptor Contributes to Elevated End-Diastolic Calcium in Cardiomyocytes and Cardiac Fibrosis Following Right Ventricular Pressure Overload. Circ. Res. 2018;123:A261. doi: 10.1161/res.123.suppl_1.261. [DOI] [Google Scholar]
- 166.An J., Li J.Q., Wang T., Li X.O., Guo L.L., Wan C., Liao Z.L., Dong J.J., Xu D., Wen F.Q. Blocking of thromboxane A(2) receptor attenuates airway mucus hyperproduction induced by cigarette smoke. Eur. J. Pharmacol. 2013;703:11–17. doi: 10.1016/j.ejphar.2013.01.042. [DOI] [PubMed] [Google Scholar]
- 167.Kobayashi K., Horikami D., Omori K., Nakamura T., Yamazaki A., Maeda S., Murata T. Thromboxane A2 exacerbates acute lung injury via promoting edema formation. Sci. Rep. 2016;6:32109. doi: 10.1038/srep32109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ogletree M.L., Chiang K.C., Kulshreshta R., Agarwal A., Agarwal A., Gupta A. Treatment of COVID-19 pneumonia and acute respiratory distress with ramatroban, a thromboxane A2 and prostaglandin D2 receptor antagonist: A 4-Patient Case Series Report. Res. Sq. Platf. LLC. 2021 doi: 10.21203/rs.3.rs-474882/v7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Nath K.A., Hebbel R.P. Sickle cell disease: Renal manifestations and mechanisms. Nat. Rev. Nephrol. 2015;11:161–171. doi: 10.1038/nrneph.2015.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Audard V., Bartolucci P., Stehlé T. Sickle cell disease and albuminuria: Recent advances in our understanding of sickle cell nephropathy. Clin. Kidney J. 2017;10:475–478. doi: 10.1093/ckj/sfx027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Platt O.S., Brambilla D.J., Rosse W.F., Milner P.F., Castro O., Steinberg M.H., Klug P.P. Mortality In Sickle Cell Disease—Life Expectancy and Risk Factors for Early Death. N. Engl. J. Med. 1994;330:1639–1644. doi: 10.1056/NEJM199406093302303. [DOI] [PubMed] [Google Scholar]
- 172.Hamideh D., Alvarez O. Sickle cell disease related mortality in the United States (1999-2009) Pediatr. Blood Cancer. 2013;60:1482–1486. doi: 10.1002/pbc.24557. [DOI] [PubMed] [Google Scholar]
- 173.Hirsch J.S., Ng J.H., Ross D.W., Sharma P., Shah H.H., Barnett R.L., Hazzan A.D., Fishbane S., Jhaveri K.D., Abate M., et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98:209–218. doi: 10.1016/j.kint.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Chan L., Coca S.G. Acute Kidney Injury in the Time of COVID-19. Kidney360. 2020;1:588–590. doi: 10.34067/KID.0003722020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Gupta S., Coca S.G., Chan L., Melamed M.L., Brenner S.K., Hayek S.S., Sutherland A., Puri S., Srivastava A., Leonberg-Yoo A., et al. AKI Treated with Renal Replacement Therapy in Critically Ill Patients with COVID-19. J. Am. Soc. Nephrol. 2021;32:161–176. doi: 10.1681/ASN.2020060897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lau W.L., Zuckerman J.E., Gupta A., Kalantar-Zadeh K. The COVID-Kidney Controversy: Can SARS-CoV-2 Cause Direct Renal Infection? Nephron. 2021;145:275–279. doi: 10.1159/000513789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Cheng Y., Luo R., Wang K., Zhang M., Wang Z., Dong L., Li J., Yao Y., Ge S., Xu G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97:829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Tonneijck L., Muskiet M.H.A., Smits M.M., van Bommel E.J., Heerspink H.J.L., van Raalte D.H., Joles J.A. Glomerular Hyperfiltration in Diabetes: Mechanisms, Clinical Significance, and Treatment. J. Am. Soc. Nephrol. 2017;28:1023–1039. doi: 10.1681/ASN.2016060666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Uriu K., Kaizu K., Hashimoto O., Komine N., Etoh S. Acute and chronic effects of thromboxane A2 inhibition on the renal hemodynamics in streptozotocin-induced diabetic rats. Kidney Int. 1994;45:794–802. doi: 10.1038/ki.1994.105. [DOI] [PubMed] [Google Scholar]
- 180.Esmatjes E., Conget I., Gaya J., Fernandez M., Ferrer J., Rivera-Fillat F., Vilardell E. Effects of Thromboxane Synthesis Inhibitor Triflusal on Renal Hemodynamics in Microalbuminuric Diabetic Patients. Diabetes Care. 1990;13:1114–1117. doi: 10.2337/diacare.13.11.1114. [DOI] [PubMed] [Google Scholar]
- 181.Bresnahan B.A., Dufek S., Wu S., Lianos E.A. Changes in glomerular thromboxane A2 receptor expression and ligand binding following immune injury. Kidney Int. 1999;55:139–147. doi: 10.1046/j.1523-1755.1999.00227.x. [DOI] [PubMed] [Google Scholar]
- 182.Hayashi K., Loutzenhiser R., Epstein M. Direct evidence that thromboxane mimetic U44069 preferentially constricts the afferent arteriole. J. Am. Soc. Nephrol. 1997;8:25–31. doi: 10.1681/ASN.V8125. [DOI] [PubMed] [Google Scholar]
- 183.Morgan B.P., Harris C.L. Complement, a target for therapy in inflammatory and degenerative diseases. Nat. Rev. Drug Discov. 2015;14:857–877. doi: 10.1038/nrd4657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Roumenina L.T., Chadebech P., Bodivit G., Vieira-Martins P., Grunenwald A., Boudhabhay I., Poillerat V., Pakdaman S., Kiger L., Jouard A., et al. Complement activation in sickle cell disease: Dependence on cell density, hemolysis and modulation by hydroxyurea therapy. Am. J. Hematol. 2020;95:456–464. doi: 10.1002/ajh.25742. [DOI] [PubMed] [Google Scholar]
- 185.Driss A., Wilson N.O., Mason K., Hyacinth H.I., Hibbert J.M., Serjeant G.R., Stiles J.K. Elevated IL-1α and CXCL10 serum levels occur in patients with homozygous sickle cell disease and a history of acute splenic sequestration. Dis. Markers. 2012;32:295–300. doi: 10.1155/2012/479275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Bustos M., Coffman T.M., Saadi S., Platt J.L. Modulation of eicosanoid metabolism in endothelial cells in a xenograft model. Role of cyclooxygenase-2. J. Clin. Investig. 1997;100:1150–1158. doi: 10.1172/JCI119626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Gao T., Hu M., Zhang X., Li H., Zhu L., Liu H., Dong Q., Zhang Z., Wang Z., Hu Y., et al. Highly pathogenic coronavirus N protein aggravates lung injury by MASP-2-mediated complement over-activation. medRxiv. 2020 doi: 10.1101/2020.03.29.20041962. [DOI] [Google Scholar]
- 188.Magro C., Mulvey J.J., Berlin D., Nuovo G., Salvatore S., Harp J., Baxter-Stoltzfus A., Laurence J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl. Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Holter J.C., Pischke S.E., De Boer E., Lind A., Jenum S., Holten A.R., Tonby K., Barratt-Due A., Sokolova M., Schjalm C., et al. Systemic complement activation is associated with respiratory failure in COVID-19 hospitalized patients. Proc. Natl. Acad. Sci. USA. 2020;117:25018–25025. doi: 10.1073/pnas.2010540117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.England H., Summersgill H.R., Edye M.E., Rothwell N.J., Brough D. Release of Interleukin-1α or Interleukin-1β Depends on Mechanism of Cell Death. J. Biol. Chem. 2014;289:15942–15950. doi: 10.1074/jbc.M114.557561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Böhm E., Sturm G.J., Weiglhofer I., Sandig H., Shichijo M., McNamee A., Pease J.E., Kollroser M., Peskar B.A., Heinemann A. 11-Dehydro-thromboxane B2, a Stable Thromboxane Metabolite, Is a Full Agonist of Chemoattractant Receptor-homologous Molecule Expressed on TH2 Cells (CRTH2) in Human Eosinophils and Basophils. J. Biol. Chem. 2004;279:7663–7670. doi: 10.1074/jbc.M310270200. [DOI] [PubMed] [Google Scholar]
- 192.Westlund P., Kumlin M., Nordenström A., Granström E. Circulating and urinary thromboxane B2 metabolites in the rabbit: 11-dehydro-thromboxane B2 as parameter of thromboxane production. Prostaglandins. 1986;31:413–443. doi: 10.1016/0090-6980(86)90106-1. [DOI] [PubMed] [Google Scholar]
- 193.Spellberg B., Edwards J.E. Type 1/Type 2 Immunity in Infectious Diseases. Clin. Infect. Dis. 2001;32:76–102. doi: 10.1086/317537. [DOI] [PubMed] [Google Scholar]
- 194.Roncati L., Nasillo V., Lusenti B., Riva G. Signals of Th2 immune response from COVID-19 patients requiring intensive care. Ann. Hematol. 2020;99:1419–1420. doi: 10.1007/s00277-020-04066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Domingo C., Palomares O., Sandham D.A., Erpenbeck V.J., Altman P. The prostaglandin D2 receptor 2 pathway in asthma: A key player in airway inflammation. Respir. Res. 2018;19:189. doi: 10.1186/s12931-018-0893-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Lucas C., Wong P., Klein J., Castro T.B.R., Silva J., Sundaram M., Ellingson M.K., Mao T., Oh J.E., Israelow B., et al. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature. 2020;584:463–469. doi: 10.1038/s41586-020-2588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Donlan A.N., Sutherland T.E., Marie C., Preissner S., Bradley B.T., Carpenter R.M., Sturek J.M., Ma J.Z., Moreau G.B., Donowitz J.R., et al. IL-13 is a driver of COVID-19 severity. JCI Insight. 2021;6:e150107. doi: 10.1172/jci.insight.150107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Gómez-Escobar L.G., Hoffman K.L., Choi J.J., Borczuk A., Salvatore S., Alvarez-Mulett S.L., Galvan M.D., Zhao Z., Racine-Brzostek S.E., Yang H.S., et al. Cytokine signatures of end organ injury in COVID-19. Sci. Rep. 2021;11:12606. doi: 10.1038/s41598-021-91859-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Arima M., Fukuda T. Prostaglandin D2and TH2 Inflammation in the Pathogenesis of Bronchial Asthma. Korean J. Intern. Med. 2011;26:8. doi: 10.3904/kjim.2011.26.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Xue L., Gyles S.L., Wettey F.R., Gazi L., Townsend E., Hunter M.G., Pettipher R. Prostaglandin D2 Causes Preferential Induction of Proinflammatory Th2 Cytokine Production through an Action on Chemoattractant Receptor-Like Molecule Expressed on Th2 Cells. J. Immunol. 2005;175:6531–6536. doi: 10.4049/jimmunol.175.10.6531. [DOI] [PubMed] [Google Scholar]
- 201.Trabanelli S., Chevalier M.F., Martinez-Usatorre A., Gomez-Cadena A., Salome B., Lecciso M., Salvestrini V., Verdeil G., Racle J., Papayannidis C., et al. Tumour-derived PGD2 and NKp30-B7H6 engagement drives an immunosuppressive ILC2-MDSC axis. Nat. Commun. 2017;8:593. doi: 10.1038/s41467-017-00678-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Liu J., Li H., Luo M., Liu J., Wu L., Lin X., Li R., Wang Z., Zhong H., Zheng W., et al. Lymphopenia predicted illness severity and recovery in patients with COVID-19: A single-center, retrospective study. PLoS ONE. 2020;15:e0241659. doi: 10.1371/journal.pone.0241659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Abadpour S., Tyrberg B., Schive S.W., Huldt C.W., Gennemark P., Ryberg E., Rydén-Bergsten T., Smith D.M., Korsgren O., Skrtic S., et al. Inhibition of the prostaglandin D2–GPR44/DP2 axis improves human islet survival and function. Diabetologia. 2020;63:1355–1367. doi: 10.1007/s00125-020-05138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Zuo S., Kong D., Wang C., Liu J., Wang Y., Wan Q., Yan S., Zhang J., Tang J., Zhang Q., et al. CRTH2 promotes endoplasmic reticulum stress-induced cardiomyocyte apoptosis through m-calpain. EMBO Mol. Med. 2018;10:e8237. doi: 10.15252/emmm.201708237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Yue L., Durand M., Lebeau Jacob M.C., Hogan P., McManus S., Roux S., de Brum-Fernandes A.J. Prostaglandin D2 induces apoptosis of human osteoclasts by activating the CRTH2 receptor and the intrinsic apoptosis pathway. Bone. 2012;51:338–346. doi: 10.1016/j.bone.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 206.Fichtner-Feigl S., Strober W., Kawakami K., Puri R.K., Kitani A. IL-13 signaling through the IL-13α2 receptor is involved in induction of TGF-β1 production and fibrosis. Nat. Med. 2006;12:99–106. doi: 10.1038/nm1332. [DOI] [PubMed] [Google Scholar]
- 207.Debaun M.R., Jordan L.C., King A.A., Schatz J., Vichinsky E., Fox C.K., McKinstry R.C., Telfer P., Kraut M.A., Daraz L., et al. American Society of Hematology 2020 guidelines for sickle cell disease: Prevention, diagnosis, and treatment of cerebrovascular disease in children and adults. Blood Adv. 2020;4:1554–1588. doi: 10.1182/bloodadvances.2019001142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Naik R.P., Streiff M.B., Lanzkron S. Sickle cell disease and venous thromboembolism: What the anticoagulation expert needs to know. J. Thromb. Thrombolysis. 2013;35:352–358. doi: 10.1007/s11239-013-0895-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Biemond B.J., Tombak A., Kilinc Y., Al-Khabori M., Abboud M., Nafea M., Inati A., Wali Y., Kristensen J., Kowalski J., et al. Sevuparin for the treatment of acute pain crisis in patients with sickle cell disease: A multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Haematol. 2021;8:e334–e343. doi: 10.1016/S2352-3026(21)00053-3. [DOI] [PubMed] [Google Scholar]
- 210.Qari M.H., Aljaouni S.K., Alardawi M.S., Fatani H., Alsayes F.M., Zografos P., Alsaigh M., Alalfi A., Alamin M., Gadi A., et al. Reduction of painful vaso-occlusive crisis of sickle cell anaemia by tinzaparin in a double-blind randomized trial. Thromb. Haemost. 2007;98:392–396. doi: 10.1160/Th06-12-0718. [DOI] [PubMed] [Google Scholar]
- 211.Greenberg J., Ohene-Frempong K., Halus J., Way C., Schwartz E. Trial of low doses of aspirin as prophylaxis in sickle cell disease. J. Pediatr. 1983;102:781–784. doi: 10.1016/S0022-3476(83)80258-3. [DOI] [PubMed] [Google Scholar]
- 212.Heeney M.M., Hoppe C.C., Abboud M.R., Inusa B., Kanter J., Ogutu B., Brown P.B., Heath L.E., Jakubowski J.A., Zhou C., et al. A Multinational Trial of Prasugrel for Sickle Cell Vaso-Occlusive Events. N. Engl. J. Med. 2016;374:625–635. doi: 10.1056/NEJMoa1512021. [DOI] [PubMed] [Google Scholar]
- 213.Kanter J., Abboud M.R., Kaya B., Nduba V., Amilon C., Gottfridsson C., Rensfeldt M., Leonsson-Zachrisson M., HESTIA2 Study Investigators Ticagrelor does not impact patient-reported pain in young adults with sickle cell disease: A multicentre, randomised phase IIb study. Br. J. Haematol. 2019;184:269–278. doi: 10.1111/bjh.15646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Warlo E.M.K., Arnesen H., Seljeflot I. A brief review on resistance to P2Y12 receptor antagonism in coronary artery disease. Thromb. J. 2019;17:11. doi: 10.1186/s12959-019-0197-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Desai P.C., Brittain J.E., Jones S.K., McDonald A., Wilson D.R., Dominik R., Key N.S., Parise L.V., Ataga K.I. A pilot study of eptifibatide for treatment of acute pain episodes in sickle cell disease. Thromb. Res. 2013;132:341–345. doi: 10.1016/j.thromres.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Rees D.C., Kilinc Y., Unal S., Dampier C., Pace B.S., Kaya B., Trompeter S., Odame I., Mahlangu J., Unal S., et al. A randomized, placebo-controlled, double-blind trial of canakinumab in children and young adults with sickle cell anemia. Blood. 2022;139:2642–2652. doi: 10.1182/blood.2021013674. [DOI] [PubMed] [Google Scholar]
- 217.NIH Antithrombotic Therapy in Patients with COVID-19. [(accessed on 5 December 2022)]; Available online: https://www.covid19treatmentguidelines.nih.gov/adjunctive-therapy/antithrombotic-therapy/
- 218.Phend C. Trials Halt Full-Dose Clot Prophylaxis for Severe COVID-19. [(accessed on 1 January 2022)]. Available online: https://www.medpagetoday.com/infectiousdisease/covid19/90351.
- 219.Daviet F., Guervilly C., Baldesi O., Bernard-Guervilly F., Pilarczyk E., Genin A., Lefebvre L., Forel J.M., Papazian L., Camoin-Jau L. Heparin-Induced Thrombocytopenia in Severe COVID-19. Circulation. 2020;142:1875–1877. doi: 10.1161/CIRCULATIONAHA.120.049015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Hughes S. COVID-19 Anticoagulation Trials ‘Paused’ for Futility, Safety. [(accessed on 1 January 2022)]. Available online: https://www.medscape.com/viewarticle/943085.
- 221.Connors J.M., Brooks M.M., Sciurba F.C., Krishnan J.A., Bledsoe J.R., Kindzelski A., Baucom A.L., Kirwan B.-A., Eng H., Martin D., et al. Effect of Antithrombotic Therapy on Clinical Outcomes in Outpatients with Clinically Stable Symptomatic COVID-19: The ACTIV-4B Randomized Clinical Trial. JAMA. 2021;326:1703–1712. doi: 10.1001/jama.2021.17272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Osborne T.F., Veigulis Z.P., Arreola D.M., Mahajan S.M., Röösli E., Curtin C.M. Association of mortality and aspirin prescription for COVID-19 patients at the Veterans Health Administration. PLoS ONE. 2021;16:e0246825. doi: 10.1371/journal.pone.0246825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.RECOVERY Aspirin to be Investigated as a Possible Treatment for COVID-19 in the RECOVERY Trial. [(accessed on 8 December 2022)]. Available online: https://www.recoverytrial.net/news/aspirin-to-be-investigated-as-a-possible-treatment-for-covid-19-in-the-recovery-trial.
- 224.Horby P.W., Pessoa-Amorim G., Staplin N., Emberson J.R., Campbell M., Spata E., Peto L., Brunskill N.J., Tiberi S., Chew V., et al. Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. medRxiv. 2021 doi: 10.1101/2021.06.08.21258132. [DOI] [Google Scholar]
- 225.Giménez-Bastida J.A., Boeglin W.E., Boutaud O., Malkowski M.G., Schneider C. Residual cyclooxygenase activity of aspirin-acetylated COX-2 forms 15 R-prostaglandins that inhibit platelet aggregation. FASEB J. 2019;33:1033–1041. doi: 10.1096/fj.201801018R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Kim J.W., Zou Y., Yoon S., Lee J.H., Kim Y.K., Yu B.P., Chung H.Y. Vascular aging: Molecular modulation of the prostanoid cascade by calorie restriction. J. Gerontol. A Biol. Sci. Med. Sci. 2004;59:B876–B885. doi: 10.1093/gerona/59.9.B876. [DOI] [PubMed] [Google Scholar]
- 227.Petrucci G., Zaccardi F., Giaretta A., Cavalca V., Capristo E., Cardillo C., Pitocco D., Porro B., Schinzari F., Toffolo G., et al. Obesity is associated with impaired responsiveness to once-daily low-dose aspirin and in vivo platelet activation. J. Thromb. Haemost. 2019;17:885–895. doi: 10.1111/jth.14445. [DOI] [PubMed] [Google Scholar]
- 228.Eikelboom J.W., Hankey G.J., Thom J., Bhatt D.L., Steg P.G., Montalescot G., Johnston S.C., Steinhubl S.R., Mak K.-H., Easton J.D., et al. Incomplete Inhibition of Thromboxane Biosynthesis by Acetylsalicylic Acid. Circulation. 2008;118:1705–1712. doi: 10.1161/CIRCULATIONAHA.108.768283. [DOI] [PubMed] [Google Scholar]
- 229.Petito E., Falcinelli E., Paliani U., Cesari E., Vaudo G., Sebastiano M., Cerotto V., Guglielmini G., Gori F., Malvestiti M., et al. Association of Neutrophil Activation, more than Platelet Activation, with Thrombotic Complications in Coronavirus Disease 2019. J. Infect. Dis. 2021;223:933–944. doi: 10.1093/infdis/jiaa756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Macdonald S. Aspirin use to be banned in under 16 year olds. BMJ. 2002;325:988. doi: 10.1136/bmj.325.7371.988/c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Capuano A., Scavone C., Racagni G., Scaglione F. NSAIDs in patients with viral infections, including COVID-19: Victims or perpetrators? Pharmacol. Res. 2020;157:104849. doi: 10.1016/j.phrs.2020.104849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Das U.N. Can COX-2 inhibitor-induced increase in cardiovascular disease risk be modified by essential fatty acids? J. Assoc. Physicians India. 2005;53:623–627. [PubMed] [Google Scholar]
- 233.Antman E.M., DeMets D., Loscalzo J. Cyclooxygenase Inhibition and Cardiovascular Risk. Circulation. 2005;112:759–770. doi: 10.1161/CIRCULATIONAHA.105.568451. [DOI] [PubMed] [Google Scholar]
- 234.Patscheke H., Hornberger W., Zehender H. Pathophysiological role of thromboxane A2 and pharmacological approaches to its inhibition. Z Kardiol. 1990;79 Suppl 3:151–154. [PubMed] [Google Scholar]
- 235.Gupta A., Kalantar-Zadeh K., Srinivasa R.T. Ramatroban as a Novel Immunotherapy for COVID-19. Mol. Genet. Med. 2020;14:1–4. doi: 10.37421/jmgm.2020.14.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Pang J., Qi X., Luo Y., Li X., Shu T., Li B., Song M., Liu Y., Wei D., Chen J., et al. Multi-omics study of silicosis reveals the potential therapeutic targets PGD(2) and TXA(2) Theranostics. 2021;11:2381–2394. doi: 10.7150/thno.47627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Ishizuka T., Matsui T., Okamoto Y., Ohta A., Shichijo M. Ramatroban (BAY u 3405): A novel dual antagonist of TXA2 receptor and CRTh2, a newly identified prostaglandin D2 receptor. Cardiovasc. Drug Rev. 2004;22:71–90. doi: 10.1111/j.1527-3466.2004.tb00132.x. [DOI] [PubMed] [Google Scholar]
- 238.Kariyazono H., Nakamura K., Arima J., Ayukawa O., Onimaru S., Masuda H., Iguro Y., Majima H.J., Sakata R., Yamada K. Evaluation of anti-platelet aggregatory effects of aspirin, cilostazol and ramatroban on platelet-rich plasma and whole blood. Blood Coagul. Fibrinolysis. 2004;15:157–167. doi: 10.1097/00001721-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 239.Ulrych T., Böhm A., Polzin A., Daum G., Nüsing R.M., Geisslinger G., Hohlfeld T., Schrör K., Rauch B.H. Release of sphingosine-1-phosphate from human platelets is dependent on thromboxane formation. J. Thromb. Haemost. 2011;9:790–798. doi: 10.1111/j.1538-7836.2011.04194.x. [DOI] [PubMed] [Google Scholar]
- 240.Al-Samkari H., Karp Leaf R.S., Dzik W.H., Carlson J.C., Fogerty A.E., Waheed A., Goodarzi K., Bendapudi P., Bornikova L., Gupta S., et al. COVID and Coagulation: Bleeding and Thrombotic Manifestations of SARS-CoV-2 Infection. Blood. 2020;136:489–500. doi: 10.1182/blood.2020006520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Christen J.R., Bertolino J., Jean E., Camoin L., Ebbo M., Harlé J.R., Schleinitz N., Sarlon G., Bernit E. Use of Direct Oral Anticoagulants in Patients with Sickle Cell Disease and Venous Thromboembolism: A Prospective Cohort Study of 12 Patients. Hemoglobin. 2019;43:296–299. doi: 10.1080/03630269.2019.1689997. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.