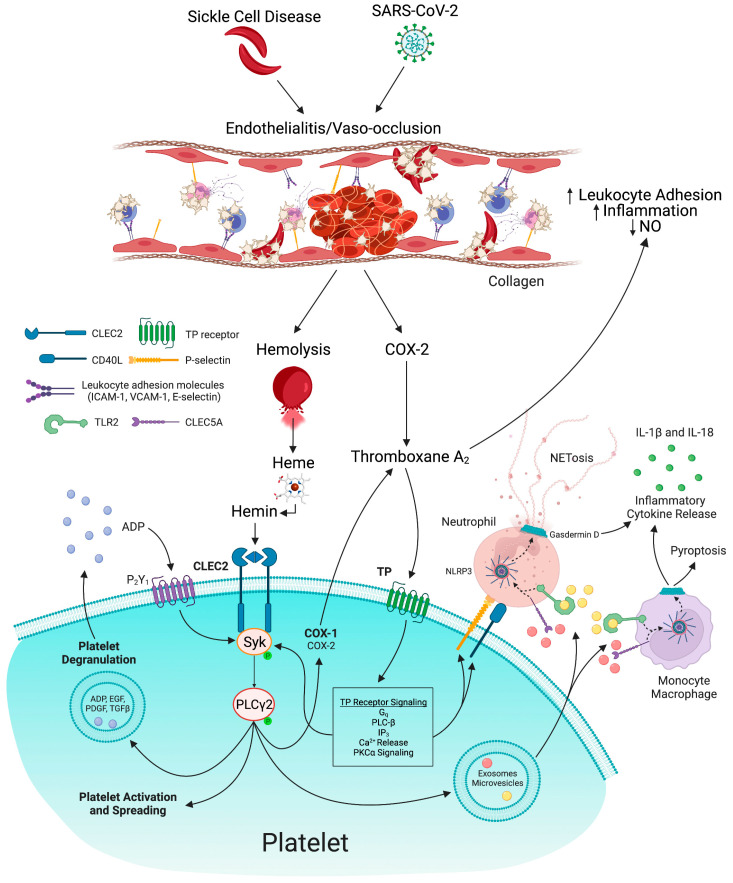
Figure 2.
Mechanisms of heme and thromboxane A2-mediated thrombo-inflammation in COVID-19 and sickle cell disease (SCD): Vaso-occlusion due to sickling or direct entry by SARS-CoV-2 virus leads to endothelial cell activation and damage, and hemolysis. COX-2 expression in endothelial cells promotes thromboxane A2 synthesis. Thromboxane A2 inhibits nitric oxide (NO) synthesis and promotes leukocyte adhesion and thrombo-inflammation. Free heme released from red blood cells is spontaneously oxidized to its ferric form, hemin. Hemin stimulates platelet CLEC2 signaling and thromboxane A2/TP receptor-dependent Syk phosphorylation leading to platelet activation, spreading, and degranulation. Platelets release exosomes and microvesicles, which stimulate the CLEC5A and TLR2 receptors on neutrophils. Subsequently, NLRP3 activation in neutrophils and monocytes promotes activation and assembly of gasdermin D, leading to the release of neutrophil extracellular traps and monocyte pyroptosis. NLRP3 inflammasome activation induces the release of proinflammatory cytokines, including IL-18 and IL-1β, thereby fueling thrombo-inflammation in COVID-19 and SCD. NO, nitric oxide; COX, cyclooxygenase; IL, interleukin; NETs, neutrophil extracellular traps; TP, thromboxane prostanoid receptor; CLEC, C-type lectin-like receptor; Syk, spleen tyrosine kinase; PLC, phospholipase C; PKC, protein kinase C; TLR, toll-like receptor; ADP, adenosine diphosphate; EGF, epidermal growth factor; PDGF, platelet-derived growth factor; TGF, transforming growth factor; NLRP3, NLR family pyrin domain containing 3.