Abstract
The rationale and importance of folic acid supplementation during pregnancy for fetal congenital defect prevention are accepted worldwide. Moreover, a sufficient plasma concentration of folates can reduce the incidence of spontaneous abortions, and support the normal expansion of placental blood vessels, ensuring physiological placental blood flow, thus promoting appropriate fetal growth and development. Furthermore, there is emerging evidence that long-term supplementation with folic acid can effectively prevent preeclampsia. Preeclampsia is unique to the human species in complications during pregnancy, which contributes to maternal and perinatal mortality worldwide. In the pathogenesis of preeclampsia abnormal placental invasion, the excess of antiangiogenic factors and maternal–placental syndrome play a key role. Increased blood levels of homocysteine during pregnancy are associated with the risk of preeclampsia. Moreover, hyperhomocysteinemia has been proposed to be an independent risk factor for preeclampsia. Folate supplementation helps to decrease elevated levels of homocysteine; thus, the role of folic acid supplementation in pregnancy is even more important. Multiple reports suggest that folate administration decreases the level of serum homocysteine and, therefore, reduce the risk and severity of preeclampsia. However, the association between folic acid supplementation and the decreased risk of preeclampsia has been investigated with controversial conclusions. Currently, the optimal dose of folic acid that is effective for preeclampsia prevention remains uncertain. In this review, we aim to summarize the accumulated knowledge on the role of folic acid in the pathogenesis of preeclampsia, and the possible impact of folate supplementation on the decreased risk of preeclampsia.
Keywords: folic acid, folate, MTHFR, homocysteine, pregnancy, preeclampsia
1. Introduction
Preeclampsia is one of the most serious complications during pregnancy leading to multiple maternal and perinatal complications [1], and it is becoming progressively more common in developed countries [2]. Preeclampsia remains a common cause of maternal and fetal morbidity and mortality [1,2,3,4]. A worldwide trend in delaying childbearing, especially in high-income countries, contributes to the risk factors associated with preeclampsia, which include advanced maternal age, obesity, insulin resistance, and other somatic conditions [2]. Inadequate or the lack of prenatal care in part explains the high and increasing prevalence of preeclampsia in developing countries [1,2,3].
The exact etiological factors of preeclampsia remain unclear. However, it is believed that two crucial steps play an important role in the pathogenesis of preeclampsia: abnormal placentation followed by maternal–placental syndrome related to an excess of antiangiogenic factors [1,2,5,6]. These currently proven hypotheses on preeclampsia as a placental disease help in the management of the related manifestations.
Preeclampsia is considered a uniquely challenging condition due to existing questions about its etiology, pathogenesis, and therapeutic management that simultaneously affect the mother and fetus [6]. Multiple research studies have been conducted to investigate the possible preventative and treatment options for preeclampsia [1,3,7,8,9]. Accumulating evidence has suggested that folic acid metabolism abnormalities and elevated levels of blood homocysteine contribute to the development of hypertensive disorders in pregnancy, including preeclampsia [8,10,11]. Many studies confirm that folate administration can help to reduce elevated blood homocysteine levels [8,12,13,14,15,16,17,18]. However, the association between folic acid supplementation and decreased risk of preeclampsia has been investigated with inconsistent conclusions and different suggested doses [7,8,19,20,21,22,23,24]. Whether folate administration in pregnancy can contribute to the prevention of preeclampsia remains uncertain [7].
Thus, in this review, we aim to summarize and update the accumulated knowledge on the role of folic acid in the pathogenesis of preeclampsia, and the possible impact of folate supplementation on the decreased risk of preeclampsia. A better understanding of folic acid metabolism in preeclampsia might open new opportunities for the prevention of preeclampsia and related adverse pregnancy outcomes.
2. Materials and Methods
A non-systematic literature review was performed by the authors, searching the available data on folic acid supplementation in pregnancy and the possible effects for preeclampsia prevention. The literature search was conducted in Scopus, Web of Science, PubMed, EBSCO, and Google Scholar databases up to the current time (2022), using the following keywords, combinations of keywords, and MeSH IDs (if available): “folate”, “folic acid” (MeSH Unique ID: D005492), “pteroylpolyglutamic acids” (MeSH Unique ID: D011624), “tetrahydrofolates” (MeSH Unique ID: D013763), “folic acid deficiency” (MeSH Unique ID: D005494), “folate metabolism”, “methylenetetrahydrofolate reductase”, “MTHFR” (MeSH Unique ID: D042965), “MTHFR deficiency”(MeSH Unique ID: C565512), “methylenetetrahydrofolate reductase deficiency” (MeSH Unique ID: C537357), “homocysteine” (MeSH Unique ID: D006710), “hyperhomocysteinemia” (MeSH Unique ID: D020138), “hypertension, pregnancy-induced” (MeSH Unique ID: D046110), “preeclampsia” (MeSH Unique ID: D011225), “preeclampsia prevention”, “obstetrical complication” (MeSH Unique ID: D007744), “prognosis” (MeSH Unique ID: D011379). The most relevant to the subject of the discussion, peer-reviewed publications have been read and employed for the review based on the authors’ evaluations. The results of the research have been divided into different sections and subsections in a logical sequence to illustrate what has been reported on the topic of discussion.
3. Results and Discussion
3.1. Folic Acid
Folic acid (pteroylglutamic acid) is one of the B-group vitamins important for cell development [4,25,26,27,28,29]. The term ‘folate’ covers a number of various forms, all of which contain a pteroyl group [30]. Natural folate (Vitamin B9) is a water-soluble substance that exists as tetrahydrofolate and methyltetrahydrofolate [4,30]. Folic acid is a synthetic, artificial substance widely used for food fortification and as a dietary supplement [4,27,30]. Folates can be found in high concentrations in the liver and in vegetables [29].
Folic acid and its role in health were first recognized in 1930 by Lucy Wills [25,28,31]. Later, in 1945, folic acid was successfully synthesized in the form of pteroylmonoglutamate with a therapeutic activity equal to the natural form [25,32]. Folate deficiency is closely linked to elevated plasma homocysteine, which is a serious risk factor for cardiovascular complications and stroke [14,27,29,33]. Additionally, a low folic acid status is associated with the “altered methylation of DNA that may affect gene expression and uracil-induced genomic instability” [27]. These metabolic changes may increase the risk of cancer, Alzheimer’s disease, and cognitive dysfunction [25,27,29,33].
In modern medicine folic acid is recognized as a major component of the periconceptional care for women [8,25,27,29]. A deficiency in folic acid can lead to fetal congenital defects and megaloblastic anemia in the mother [25,28,29]. Currently, the World Health Organization (WHO) recommends 400 µg daily folic acid supplementation [34,35]. Thus, many countries have created national programs for mandatory folic acid food fortification to fight inadequate dietary folate consumption, and to reduce the prevalence of folate-related diseases [27,29].
3.1.1. Folic Acid Metabolism
In the human body, folate is absorbed in the mucosal epithelial cells [27,29,36]. A folylpoly-glutamate carboxypeptidase enzyme plays a primary role in this physiologic process, which results in monoglutamate forms [27,29,36]. After ingestion, most folic acid is absorbed in the upper part of the small intestine by a specific pH- and energy-dependent transport mechanism [27,36,37]. Once folic acid and derivatives appear in the enterocytes and are metabolized to 5-methyltetrahydrofolate (5-MTHF), it is exported into the portal vein [29]. The liver has a high affinity for folic acid but a lower affinity for the removal of 5-methyltetrahydrofolate (5-MTHF) [27]. This fact allows a fraction of the 5-MTHF to proceed without obstacles into the systemic circulation [27,29,36,37].
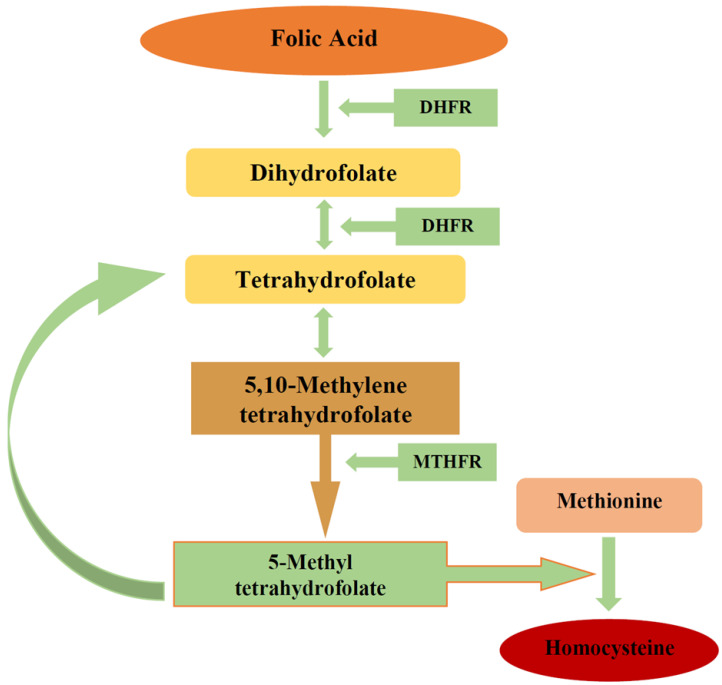
Further, some of the folate in hepatocytes is secreted in bile and then reabsorbed in the intestine [29]. The overall process of folic acid metabolism includes many steps and enzymes (Figure 1). Folic acid’s biological activity relies on the action of the dihydrofolate reductase (DHFR) enzyme produced in the liver [29,30]. In order to carry out its biological function, folic acid needs to be reduced by DHFR to dihydrofolate, and then to tetrahydrofolate [36]. Then, it is converted to its biologically active form 5-MTHF (Figure 1) [36].
Figure 1.
Folic acid metabolism. Figure legend: DHFR—dihydrofolate reductase; MTHFR—methylenetetrahydrofolate reductase.
The intestinal metabolism of folic acid to 5-MTHF is pH-dependent and according to studies appears to be extensive at pH 6.0 and minor at pH 7.5 [25,27,28]. Notably, high oral doses of folate (260–280 μg) have been reported to lead to the direct appearance of untransformed/unmetabolized folic acid in systemic circulation [27,29]. This indicates that intestinal conversion is not a mandatory premise for folate absorption and transport [27]. Thus, physiological and high doses of oral folic acid could pass through different metabolic pathways.
3.1.2. Folic Acid Function
Folates are crucial to human cell development and function as a component and accelerator for essential biochemical reactions [4,30] and for cell multiplication and differentiation processes [38]. Folic acid plays an essential role in nucleotide metabolism important for DNA synthesis and methylation [25,27,30]. Folic acid and its derivatives function as acceptors or receptors for one-carbon units and function as co-enzymes involved in various methylation reactions [29,37].
Folates are also proposed to have important roles in other physiological processes required for a successful pregnancy, including antioxidant protection, angiogenesis, endothelial-dependent vascular relaxation, and homocysteine methylation [17,29,33,37,38,39]. These steps are important for chorion and placental development and the establishment of placental circulation, enabling fetal growth and development and favorable pregnancy outcomes [38].
Folate has different functions, including the metabolism of methionine to homocysteine (Figure 1), purine and pyrimidine synthesis, and DNA methylation [17,29,37,40]. Therefore, a low folate status might lead to chronic diseases caused by inadequate DNA synthesis and gene expression. Folate deficiency is associated with an increased risk of cardiovascular diseases, cancers, and cognitive dysfunction, including Alzheimer’s disease [17,27,29,33,39]. In addition, genetic polymorphisms of the methylenetetrahydrofolate reductase (MTHFR) enzyme result in elevated homocysteine levels and serves as an independent risk factor for folate-associated diseases [17,29,33,39].
Folate deficiency in the vast majority of cases occurs due to an inadequate dietary intake, which leads to decreased plasma folate levels followed by increased concentrations of homocysteine [17]. Moreover, low levels of folic acid and high concentrations of homocysteine in the blood are potential causes of neural tube defects [17].
3.1.3. MTHFR Gene Physiology and Polymorphism
Another enzyme that plays an important role in folate metabolism is 5,10-methylenetetrahydrofolate reductase. The MTHFR enzyme is mapped to chromosome 1 (1p36.3) [15,41]. The enzyme functions in the reduction from 5,10-methylenetetrahydrofolate to 5-MTHF (Figure 1) [15,27,29,37]. The 5,10-MTHF conversion to 5-MTHF under MTHFR enables the production of methyl donors for the conversion of homocysteine to methionine [15]. Thus, MTHFR takes an essential role in homocysteine metabolism to methionine from 5-MTHF, which acts as a substrate for vitamin B12-dependent methioninesynthase (Figure 1) [15,17,29].
The MTHFR gene has been reported to possess one common mutation, C677T, linked to serious enzymatic deficiency and fourteen rare mutations, which are associated with severe enzymatic deficiency [15,16,41]. The C677T polymorphism is a point mutation at position 677 on the MTHFR gene characterized by the substitution of cysteine with thymine [15,42]. Following this mutation in the gene, alanine is substituted for valine, which leads to a deleterious effect on plasma homocysteine metabolism—high plasma homocysteine levels (hyperhomocysteinemia) and low folate levels [15,29,42,43]. Homocysteine is a homolog of cysteine (amino acid) with one additional methylene group and containing a sulfhydryl group [42,44]. The normal homocysteine levels range between 5 and 15 μmol/L [42,45]. Levels of 15 to 30 μmol/L are accepted as a mild increase, levels of 30 to 100 μmol/L reflect a moderate increase, while a value > 100 μmol/L is classified as severe hyperhomocysteinemia [42,45].
The prevalence of the MTHFR 677C > T varies depending on ethnic background and place of residence [15,43,46]. The allele frequency has been found to be higher in the Southern European population (Italian and Hispanics) and lower in Germans, and African Americans [15,46]. Among Caucasians living in Canada, the United States (US), Brazil, and Australia, the homozygous mutation is reported in up to 15% of the population [15,46]. Limited data are available about the Asian population. The Japanese population has been reported to have a homozygous mutation in 11–15% of the population [15,17]. Some limited reports are available from Central Asia. In Kazakhstan, low folate status and mild homocysteinemia were reported among the Kazakh population [16,18]. The cited study showed that MTHFR C677T mutation levels were high [16,18]. Similar findings were reported among the Kazakh ethnic minority in China, where low serum folic acid levels and high methylation of MTHFR gene were found [47,48,49,50]. A low frequency of the MTHFR 677C > T mutation was found in the sub-Saharan African population [15,51]. Due to the above-discussed metabolic pathways, when folic acid or vitamin B12 levels are inadequate, the metabolism of homocysteine is also affected, leading to hyperhomocysteinemia [15,29,30]. Polymorphism of the MTHFR gene at position 677C > T may affect the enzyme’s role in the homocysteine pathway [15,16,17,18].
High plasma homocysteine levels have been proven to serve as a risk factor for multiple conditions such as atherosclerosis, coronary artery disease, essential hypertension, retinal vein occlusion, venous thromboembolism, cancers, infertility, and pregnancy complications (preeclampsia, recurrent pregnancy loss, etc.) [14,27,29,33,52,53,54]. Hyperhomocysteinemia has been reported in 40% of patients with coronary artery disease, and cerebral or peripheral artery disease [15,53]. The exact mechanism of how increased levels of homocysteine leads to the development of vascular endothelial pathology is still unknown. Some of the hypothesized mechanisms include hyperproliferation of vascular smooth muscle cells accompanied by endothelial dysfunction, oxidative damage, and a further increase in collagen synthesis, and damage to the arterial wall elastic layer [53].
The MTHFR C677T polymorphisms are associated with various diseases and pregnancy complications, including preeclampsia [15]. Thus, the role of folic acid supplementation in pregnancy is essential and attempts to find new applications of folates to prevent pregnancy-related conditions/complications are under investigation.
3.2. The Role of Folic Acid Supplementation in Pregnancy
Most women of childbearing age have no adequate dietary supply of folic acid [36,55,56,57]. Thus, the importance of folate administration during pregnancy for fetal congenital defect prevention is accepted worldwide [4,34,58]. An intake of 400 μg/day folic acid during the preconception period [34,55,58] and the first trimester of pregnancy ensures adequate folate blood levels during the organogenesis and decreases the risk of neural tube defects by 50–70% [4,34,36,56,57]. International guidelines recommend the administration of folic acid at doses between 400 and 800 μg/day [56,57] High-dosage folate supplementation (4–5 mg/day) should only be used for women at high risk, suffering from infertility, pregnancy loss, and previous newborns with neural tube defect [57].
Moreover, genetic polymorphisms of the MTHFR gene leading to hyperhomocysteinemia potentially could elevate the risk of congenital anomalies [4,36,55,56]. The effect of elevated homocysteine in combination with low levels of folic acid increases the risk of birth defects. To allow a sufficient supply of folate for persons with reduced MTHFR enzymatic activity, supplementation with a combination of folic acid and 5-MTHF can be performed [55,57]. Folic acid supplementation allows for the reduction of high blood levels of homocysteine [4,59], thus decreasing the risk of venous thromboembolic complications in pregnancy.
Inadequate folate supplementation has been associated with miscarriage, placental abruption, and intrauterine growth restriction (IUGR) [38,60,61]. Therefore, some studies have investigated the possibility of IUGR [60,62,63,64] and pre-term birth [63,65,66,67] prevention by the administration of folic acid [4]. However, the results are controversial: according to the limited reports, higher maternal folate levels could significantly lower the risk of pre-term birth [66,67], while other findings contrast this [65]. Some other researchers have reported an association between higher maternal levels of folate in early pregnancy with gestational diabetes mellitus risk [68]. Thus, since there are conflicting data on the positive effects of folic acid supplementation, neural tube defect prevention by daily folic acid supplementation remains the most important and proven intervention [4,65].
Folic Acid in the Fetus and Placenta
As the folic acid concentration in fetal blood flow is much higher than that in maternal, some researchers hypothesized that “folic acid intake during pregnancy could lead to the accumulation of inactive metabolites in fetal serum” [4]. In addition, a significantly higher concentration of 5-MTHF was reported in umbilical cord blood than in the corresponding mothers’ blood [4,69].
Results of an in vitro study demonstrated that the placental physiology and function may be compromised in conditions of folate deficiency, and “not necessarily” in conditions of folic acid excess [70]. However, other researchers report contrasting data after experimental investigation. In a recent experimental study Luan et al., (2021) proposed that “moderate increases” in folic acid intake during pregnancy may result in placental metabolic variations, leading to gene expression changes, specifically responsible for angiogenesis [4,71]. This may contribute to abnormal behavior in offspring [71]. The authors suggest determining a safe upper limit for folic acid supplementation during pregnancy [71]. Thus, further studies should aim to clarify the therapeutic window of folic acid intake during pregnancy.
3.3. Preeclampsia
3.3.1. Epidemiology of Preeclampsia
Preeclampsia is a hypertensive disorder of pregnancy, which complicates up to 5–8% of pregnancies globally and is one of the major causes of maternal and perinatal mortality worldwide [1,3,6,8,9]. The prevalence of preeclampsia varies among different racial and ethnic groups by 7–11% [72]. This may be explained by racial and ethnic genetic structure variations. As was highlighted in a recent report, in the US, racial and ethnic minority groups, such as non-Hispanic Black women and American Indian women, are more affected by preeclampsia [72]. Studies report that human leukocyte antigen G (HLA-G) mutations may contribute to the development of preeclampsia [72,73,74,75]. This partially explains the increased risk of preeclampsia among women of African ancestry, as studies have demonstrated that the maternal HLA-G genotype is significantly associated with the risk of preeclampsia in African American women [72,76,77,78]. Furthermore, genetic variations in HLA-G may play a role in miscarriage and pre-term birth, which are known to be linked with HLA-G polymorphism [73,74,75].
In addition to maternal genetic variants that may predispose to preeclampsia, the fetal genome has also been found to be associated with the increased risk of preeclampsia [79,80,81]. Studies investigating the role of the fetal genome in the development of preeclampsia reported that dysregulation of the FMS-like tyrosine kinase 1 (FLT1) locus in the fetal genome is a fundamental molecular defect in preeclampsia [80], consequently, variants in the fetal genome near FLT1 are associated with an increased risk of preeclampsia [79,80,81]. Thus, more studies on factors leading to the lower or higher prevalence of preeclampsia among various ethnic groups could provide a better understanding of the pathogenesis of preeclampsia and ways to prevent it.
The prevalence of preeclampsia is of specific importance in controlling maternal mortality. Globally, more than 50% of maternal deaths in the period of 2003–2009 were due to hypertensive disorders, hemorrhage, and sepsis [82,83]. Causes of maternal mortality vary depending on the world region and a particular country’s income. The most frequent causes are postpartum hemorrhage and hypertensive disorders in pregnancy, with rates of mortality due to these complications varying from 36.9% in northern African countries to 16.3% in high-income countries [83]. Maternal deaths due to hypertension in pregnancy are most common in Latin America and the Caribbean, accounting for up to 26% of deaths [3,82,83]. Even in high-resource settings, in high-income countries, around 16% of maternal mortality cases are attributed to hypertensive disorders, while in low- and middle-income countries (LMICs) hypertensive disorders are responsible for up to 25% of maternal mortality cases [3,84]. Cases of hypertensive disorders in pregnancy, including preeclampsia, are increasing worldwide [2]. In the US, in the period of 17 years (1987–2004), the rate of preeclampsia increased by 25% [3,85].
Women with pregnancy complicated by preeclampsia may have infants with neurocognitive dysfunctions and suboptimal development in the offspring [1,2,8]. Hypertension and preeclampsia during pregnancy may also serve as risk factors for diabetes and cardiovascular disease in later life [8,9].
3.3.2. Pathogenesis of Preeclampsia
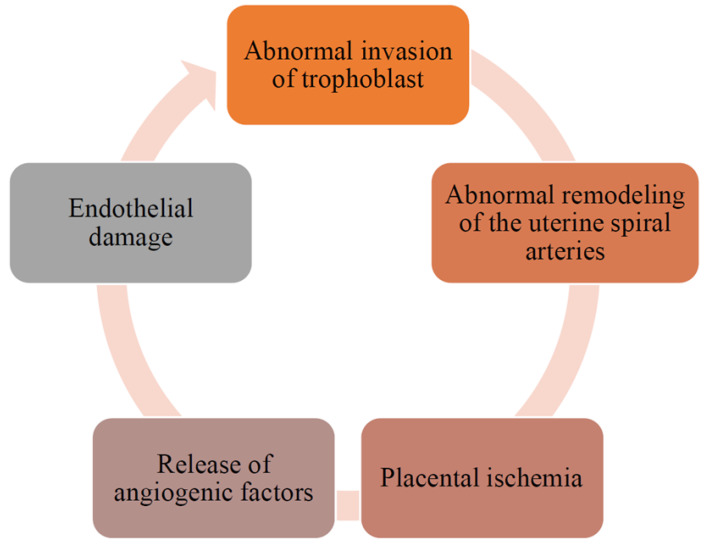
Although the pathogenesis of preeclampsia is not yet fully understood, the main pathological mechanisms have been clarified [1,2,5,6]. The main hypothesis explaining preeclampsia development is a defective trophoblastic invasion with associated utero-placental hypoperfusion [1,2,5,6,86]. Based on the available evidence, a two-stage model of preeclampsia pathogenesis was developed: (1) abnormal remodeling of the uterine spiral arteries leading to placental ischemia; (2) the release of antiangiogenic factors by the ischemic placenta into the maternal circulation with the subsequent development of endothelial damage (Figure 2) [1,2,4,6]. Multiple factors are involved in the pathogenesis of preeclampsia: vascular endothelial growth factor (VEGF), transforming growth factor beta (TGF-β), placental growth factor (PlGF), soluble FMS-like tyrosine kinase 1(sFlt-1) and soluble endoglin (sEng) nitric oxide (NO), angiotensin receptor 1 antibodies (AT1-AAs), etc. [1,2,5,6]. These factors equally contribute to the development of gestational hypertension, preeclampsia, and IUGR [2]. However, this two-step theory does not explain the specific manifestations of preeclampsia (symptoms and signs), which are different from gestational hypertension and/or IUGR [2,6]. Thus, preeclampsia is always caused by compromised placental perfusion; however, other risk factors contributing to preeclampsia remain unclear [2,6,8]. Authors should discuss the results and how they can be interpreted from the perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
Figure 2.
Pathogenesis of preeclampsia.
3.3.3. The Role of MTHFR Polymorphism and Hyperhomocysteinemia in Preeclampsia
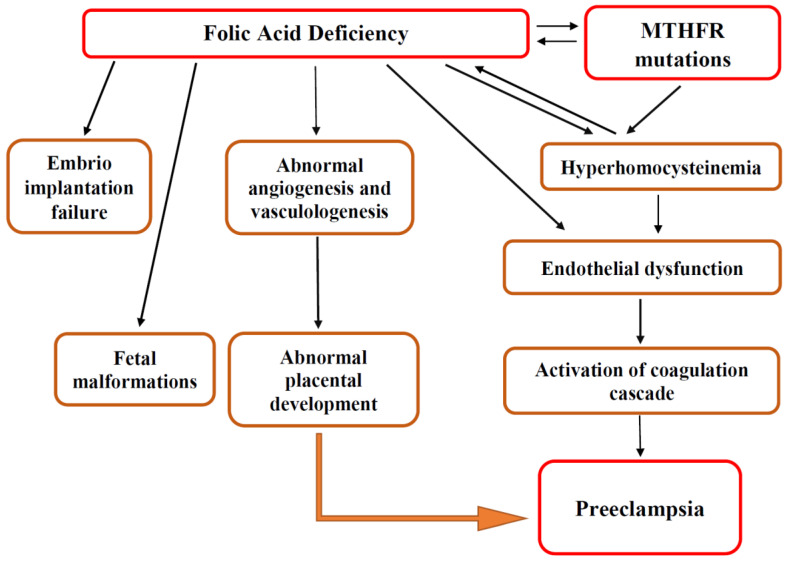
Pregnancy is associated with major physiological and immunological changes in a woman’s organs and organ systems, which are controlled by “methylation patterns of certain candidate genes” [87]. The MTHFR gene is one of the genes taking a pivotal role during pregnancy by virtue of thrombotic events or methylation [87]. The MTHFR C677T polymorphism results in low enzymatic activity and an accumulation of homocysteine [87]. Hyperhomocysteinemia leads to thrombotic events in a vascular bed of various localizations, including the placenta, causing severe conditions (Figure 3) [14,27,29,33,52,53,54].
Figure 3.
Role of folic acid and MTHFR polymorphisms in preeclampsia. Figure legend: MTHFR—methylenetetrahydrofolate reductase.
Increased blood levels of homocysteine during pregnancy are associated with multiple pregnancy complications, including preeclampsia, spontaneous abortions, IUGR, and placental abruption [54,88,89,90]. Moreover, elevated plasma homocysteine has been proposed to be an independent risk factor for preeclampsia [88,89,90]. Hyperhomocysteinemia results in the induction of inflammatory determinants including the expression of adhesion molecules, leukocyte adhesion, and endothelial cells damage [42,54]. In turn, endothelial injury promotes oxidative stress, reduces NO bioavailability, and increases the production of vascular procoagulants [42,54,86]. Further, endothelial damage leads to decreased protein C activation, which further contributes to local pro-coagulation.
Several case–control studies and systematic reviews have reported that hyperhomocysteinemia is associated with preeclampsia [13,54,91,92,93,94,95]. These studies found the average homocysteine levels to be significantly higher in women with preeclampsia compared to healthy controls (p < 0.001). Furthermore, Acilmis et al., (2011) reported that the maternal and fetal homocysteine blood levels were significantly higher in patients with severe preeclampsia compared to preeclampsia and healthy controls [94]. These data support the hypothesis that hyperhomocysteinemia might be associated with the severity of preeclampsia [94].
Moreover, recent studies reported that the MTHFR C677T gene polymorphism seems to play a significant role in preeclampsia [87], thus contributing to the hyperhomocysteinemia state. These findings suggest that folic acid supplementation in women could decrease the level of serum homocysteine and, therefore, reduce the risk/severity of preeclampsia (Figure 3) [8,13].
3.4. Folic Acid Supplementation for Preeclampsia Prevention
As placental development is a cornerstone in preeclampsia pathogenesis, the placental growth processes take special attention. Placental development and circulation require angiogenesis, which is critical for the development of a physiological placental blood flow and normal development of the fetus (Figure 3) [2,5,6,38]. Folic acid plays an essential role in this process via induced angiogenesis, through a NO-dependent mechanism [38]. Thus, folic acid supplementation for preeclampsia prevention remains a hot topic for researchers’ discussions and investigations.
Studies report that adequate folic acid supplementation from the onset of pregnancy supports physiological trophoblastic proliferation and angiogenesis and helps avoid increased levels of homocysteine that can be seen in the third trimester [4,40,88]. Several investigations’ results suggest that folate supplementation is beneficial for the reduction of preeclampsia and gestational hypertension incidences (Table 1) [8,12,22,38,96,97,98,99,100,101,102,103].
Table 1.
Folic acid supplementation for preeclampsia prevention.
| Authors | Population | Recommendations | Reference | |
|---|---|---|---|---|
| Dose | Time and Duration | |||
| Manizheh et al., 2009 | Iranian | Folic acid, 500 μg/day–5 mg/day | From early pregnancy until delivery | [12] |
| Kim et al., 2014 | South Korean | Folic acid, 400 μg/day–1.0 mg/day daily for at least | Two-three months before conception and throughout pregnancy | [101] |
| Martinussen et al., 2015 | USA | Folic acid, <200 μg/day, 200 < 600 μg/day, ≥600 μg/day | One month before pregnancy, first-trimester pregnancy | [102] |
| Wang et al., 2015 | Chinese | Dietary folic acid intake (from 151.6 μg/day to ≥274 μg/day) | Throughout the whole pregnancy | [98] |
| Vanderlelie et al., 2016 | Australian | Folic acid, 800 μg/day | The first trimester of pregnancy | [99] |
| Wen et al., 2016 | Canadian | Folic acid, ≥1.0 mg/day |
First and early second trimester of pregnancy | [97] |
| Han et al., 2020 | Chinese | Folic acid, <400, 400, and >400 μg/day | Before and during pregnancy | [100] |
| Zheng et al., 2020 | Chinese | Folic acid, 4 mg/day | Three months before pregnancy for the entire pregnancy | [103] |
First-trimester folate-only supplementation (not multivitamins) has been associated with a reduction in the risk of preeclampsia (AOR 0.42, 95% CI: 0.13, 0.98) [99]. A study by Wang et al., (2015) on the Chinese population who followed the dietary intake of folate during pregnancy was associated with a reduced risk of severe preeclampsia (OR: 0.52, 95% CI: 0.31, 0.87) with a significant dose-related response, but not in mild preeclampsia [98]. A Canadian prospective study reported an association of ≥1.0 mg folic acid supplementation with a lower rate of preeclampsia, “and the results were statistically significant in women with an increased risk of developing preeclampsia” [97]. These studies support the hypothesis that folate supplementation and dietary folic acid intake during pregnancy are associated with a reduced risk of preeclampsia.
High doses (>1.0 mg/day) of folic acid intake and prolonging the period of folate supplementation beyond the first trimester of pregnancy was proposed to aid in preeclampsia prevention through the support of physiologic angiogenesis [4,38,95]. Some authors investigated the possible role of folic acid in the regulation of trophoblastic invasion and the development of the placenta [38,40]. The beneficial effect of extended folate administration through a pregnancy course for a reduced incidence of preeclampsia was suggested [38,95,96]. Moreover, longer-term folic acid supplementation in pregnancy was proposed to reduce the secondary systemic symptoms of preeclampsia due to its favorable effects on endothelial function [38].
However, others demonstrated no association between folic acid supplementation and preeclampsia [4,8,20,23,24,104,105]. A study on the Danish population fail to show that folate was related to preeclampsia risk [23]. The same conclusion was made by researchers from Columbia who found that prenatal consumption of folic acid did not decrease the risk of preeclampsia in the Columbian population [105]. A recent systematic review, which aimed “to investigate the effect of maternal folic acid supplementation during pregnancy on the risk of preeclampsia and gestational hypertension” reported little evidence for the association between maternal folic acid administration and decreased risk of preeclampsia [4,20]. In addition, the FACT trial, a double-blind, phase III, randomized controlled, multicenter study did not show benefits from prolonged supplementation with 4.0 mg/day of folic acid for preeclampsia prevention [21]. The most recent study on the effect of high-dose (4 mg/day throughout pregnancy) folic acid supplementation for preeclampsia prevention in twin pregnancies did not show any benefits [106].
However, since increased levels of homocysteine lead to endothelial dysfunction (thus associated with preeclampsia pathogenesis), and taking into consideration the fact that 5-MTHF is the active form of folate directly involved in the metabolism of homocysteine into methionine, folate administration during pregnancy could prevent hyperhomocysteinemia and play an important role in preeclampsia prevention [4,38,94]. Moreover, 5-MTHF was reported to have the ability to stimulate the endothelial production of NO, which has anticoagulant activity through vasodilatatory and antiplatelet functions [4,107,108,109]. Therefore, in spite of the controversies reported about the role of folic acid supplementation for preeclampsia prevention, there is a pathophysiological background behind the continuous investigations in this field.
The genetic background of racial and ethnic diversity is under continuous investigation in modern genetics, and studies of the human populations’ genetic structure have found variations between racial and ethnic groups [72,73,74]. The fact that there is a disparity in preeclampsia prevalence among different racial and ethnic groups [72,73] could suggest specific pathogenetic pathways of the condition. Thus, investigations to evaluate folic acid supplementation for the prevention of preeclampsia should take into consideration the genetic and ethnic background of study participants, doses, and periods of folic acid administration. Therefore, further studies are required to outline the protocol for effective folic acid supplementation in women to prevent preeclampsia.
4. Conclusions
The essential role of folate supplementation in pregnancy for neural tube defect prevention is doubtless. However, the association between the dosage of folic acid supplementation and the potency of its effect in other pregnancy-related conditions should be clarified. Further investigations to evaluate the opportunity of folic acid supplementation for preeclampsia risk reduction should take into consideration the dose-dependent effects, duration of administration, and ethnic background of patients. Therefore, more case–control studies need to be conducted to clarify the role of folic acid supplementation in preeclampsia prevention.
Acknowledgments
The review was prepared as a part of Ph.D. candidate (Lyazzat Kaldygulova) commitment.
Author Contributions
Conceptualization, L.K. and A.T.; data curation, L.K., G.A., A.G. and T.U.; formal analysis, G.A., A.G. and L.K.; methodology, L.K. and G.A.; project administration, L.K.; software, L.K.; supervision, A.T. and A.G.; visualization, G.A. and T.U.; writing—original draft, L.K. writing—review and editing, G.A. and T.U. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data related to this article could be retrieved from authors (gulzhanat.aimagambetova@nu.edu.kz) per reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Ives C.W., Sinkey R., Rajapreyar I., Tita A.T.N., Oparil S. Preeclampsia—Pathophysiology and Clinical Presentations. J. Am. Coll. Cardiol. 2020;76:1690–1702. doi: 10.1016/j.jacc.2020.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Phipps E., Prasanna D., Brima W., Jim B. Preeclampsia: Updates in Pathogenesis, Definitions, and Guidelines. Clin. J. Am. Soc. Nephrol. 2016;11:1102–1113. doi: 10.2215/CJN.12081115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ACOG Gestational Hypertension and Preeclampsia. Obstet. Gynecol. 2020;135:1492–1495. doi: 10.1097/AOG.0000000000003892. [DOI] [PubMed] [Google Scholar]
- 4.Ferrazzi E., Tiso G., Di Martino D. Folic acid versus 5- methyl tetrahydrofolate supplementation in pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;253:312–319. doi: 10.1016/j.ejogrb.2020.06.012. [DOI] [PubMed] [Google Scholar]
- 5.El-Sayed A.A.F. Preeclampsia: A Review of the Pathogenesis and Possible Management Strategies Based on Its Pathophysiological Derangements. Taiwan J. Obstet. Gynecol. 2017;56:593–598. doi: 10.1016/j.tjog.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Rana S., Lemoine E., Granger J.P., Karumanchi S.A. Preeclampsia: Pathophysiology, challenges, and perspectives. Circ. Res. 2019;124:1094–1112. doi: 10.1161/CIRCRESAHA.118.313276. [DOI] [PubMed] [Google Scholar]
- 7.Hua X., Zhang J., Guo Y., Shen M., Gaudet L., Janoudi G., Walker M., Wen S.W. Effect of folic acid supplementation during pregnancy on gestational hypertension/preeclampsia: A systematic review and meta-analysis. Hypertens. Pregnancy. 2016;35:447–460. doi: 10.1080/10641955.2016.1183673. [DOI] [PubMed] [Google Scholar]
- 8.Liu C., Liu C., Wang Q., Zhang Z. Supplementation of folic acid in pregnancy and the risk of preeclampsia and gestational hypertension: A meta-analysis. Arch. Gynecol. Obstet. 2018;298:697–704. doi: 10.1007/s00404-018-4823-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hauspurg A., Countouris M.E., Catov J.M. Hypertensive Disorders of Pregnancy and Future Maternal Health: How Can the Evidence Guide Postpartum Management? Curr. Hypertens. Rep. 2019;21:96. doi: 10.1007/s11906-019-0999-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanchez S.E., Zhang C., Malinow M.R., Ware-Jauregui S., Larrabure G., Williams M.A. Plasma Folate, Vitamin B12, and Homocyst(e)ine Concentrations in Preeclamptic and Normotensive Peruvian Women. Am. J. Epidemiol. 2001;153:474–480. doi: 10.1093/aje/153.5.474. [DOI] [PubMed] [Google Scholar]
- 11.Vollset S.E., Refsum H., Irgens L.M., Emblem B.M., Tverdal A., Gjessing H.K., Monsen A.L.B., Ueland P.M. Plasma total homocysteine, pregnancy complications, and adverse pregnancy outcomes: The Hordaland Homocysteine Study. Am. J. Clin. Nutr. 2000;71:962–968. doi: 10.1093/ajcn/71.4.962. [DOI] [PubMed] [Google Scholar]
- 12.Manizheh S.M., Mandana S., Hassan A., Amir G.H., Mahlisha K.S., Morteza G. Comparison study on the effect of prenatal administration of high dose and low dose folic acid. Saudi Med. J. 2009;30:88–97. [PubMed] [Google Scholar]
- 13.Shahbazian N., Jafari R.M., Haghnia S. The evaluation of serum homocysteine, folic acid, and vitamin B12 in patients complicated with preeclampsia. Electron. Physician. 2016;8:3057–3061. doi: 10.19082/3057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dai C., Fei Y., Li J., Shi Y., Yang X. A Novel Review of Homocysteine and Pregnancy Complications. BioMed Res. Int. 2021;2021:6652231. doi: 10.1155/2021/6652231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liew S.-C., Gupta E.D. Methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism: Epidemiology, metabolism and the associated diseases. Eur. J. Med. Genet. 2015;58:1–10. doi: 10.1016/j.ejmg.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Akilzhanova A., Takamura N., Kusano Y., Karazhanova L., Yamashita S., Saito H., Aoyagi K. Association between C677T/MTHFR genotype and homocysteine concentration in a Kazakh population. Asia Pac. J. Clin. Nutr. 2008;17:325–329. [PubMed] [Google Scholar]
- 17.Hiraoka M., Kagawa Y. Genetic polymorphisms and folate status. Congenit. Anom. 2017;57:142–149. doi: 10.1111/cga.12232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Razbekova M., Issanov A., Chan M.-Y., Chan R., Yerezhepov D., Kozhamkulov U., Akilzhanova A., Chan C.-K. Genetic factors associated with obesity risks in a Kazakhstani population. BMJ Nutr. Prev. Health. 2021;4:90–101. doi: 10.1136/bmjnph-2020-000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kindler H.L. Systemic Treatments for Mesothelioma: Standard and Novel. Curr. Treat. Options Oncol. 2008;9:171–179. doi: 10.1007/s11864-008-0071-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bulloch R.E., Lovell A.L., Jordan V.M.B., McCowan L.M.E., Thompson J.M.D., Wall C.R. Maternal folic acid supplementation for the prevention of preeclampsia: A systematic review and meta-analysis. Paediatr. Périnat. Epidemiol. 2018;32:346–357. doi: 10.1111/ppe.12476. [DOI] [PubMed] [Google Scholar]
- 21.Wen S.W., White R.R., Rybak N., Gaudet L.M., Robson S., Hague W., Simms-Stewart D., Carroli G., Smith G., Fraser W.D., et al. Effect of high dose folic acid supplementation in pregnancy on pre-eclampsia (FACT): Double blind, phase III, randomised controlled, international, multicentre trial. BMJ. 2018;362:k3478. doi: 10.1136/bmj.k3478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Ocampo M.P.G., Araneta M.R.G., Macera C.A., Alcaraz J.E., Moore T.R., Chambers C.D. Folic acid supplement use and the risk of gestational hypertension and preeclampsia. Women Birth. 2018;31:e77–e83. doi: 10.1016/j.wombi.2017.08.128. [DOI] [PubMed] [Google Scholar]
- 23.Catov J.M., Bodnar L.M., Olsen J., Olsen S., A Nohr E. Periconceptional multivitamin use and risk of preterm or small-for-gestational-age births in the Danish National Birth Cohort. Am. J. Clin. Nutr. 2011;94:906–912. doi: 10.3945/ajcn.111.012393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hassan A.G.M., Shehata N.A. Comparison between the roles of low-dose aspirin and folic acid in preventing preeclampsia among high-risk women screened by uterine artery Doppler at 22–24 weeks of gestation. Evid. Based Women’s Health J. 2015;5:111–117. doi: 10.1097/01.EBX.0000466601.40481.95. [DOI] [Google Scholar]
- 25.Davis R.E. Clinical Chemistry of Folic Acid. Adv. Clin. Chem. 1986;25:233–294. doi: 10.1016/s0065-2423(08)60127-4. [DOI] [PubMed] [Google Scholar]
- 26.Talaulikar V.S., Arulkumaran S. Folic Acid in Obstetric Practice: A Review. Obstet. Gynecol. Surv. 2011;66:240–247. doi: 10.1097/OGX.0b013e318223614c. [DOI] [PubMed] [Google Scholar]
- 27.Wright A.J.A., Dainty J.R., Finglas P. Folic acid metabolism in human subjects revisited: Potential implications for proposed mandatory folic acid fortification in the UK. Br. J. Nutr. 2007;98:667–675. doi: 10.1017/S0007114507777140. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberg I.H. Absorption and malabsorption of folates. Clin. Haematol. 1976;5:589–618. doi: 10.1016/S0308-2261(21)00112-0. [DOI] [PubMed] [Google Scholar]
- 29.Ebara S. Nutritional role of folate. Congenit. Anom. 2017;57:138–141. doi: 10.1111/cga.12233. [DOI] [PubMed] [Google Scholar]
- 30.Menezo Y., Elder K., Clement A., Clement P. Folic Acid, Folinic Acid, 5 Methyl TetraHydroFolate Supplementation for Mutations that Affect Epigenesis through the Folate and One-Carbon Cycles. Biomolecules. 2022;12:197. doi: 10.3390/biom12020197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bastian H. Lucy Wills (1888–1964): The life and research of an adventurous independent woman. J. R. Coll. Physicians Edinb. 2008;38:89–91. [PubMed] [Google Scholar]
- 32.Angier R.B., Boothe J.H., Hutchings B.L., Mowat J.H., Semb J., Stokstad E.L., Subbarow Y., Waller C.W., Cosulich D.B., Fahrenbach M.J., et al. Synthesis of a compound identical with the L. casei factor isolated from liver. Science. 1945;102:227–228. doi: 10.1126/science.102.2644.227. [DOI] [PubMed] [Google Scholar]
- 33.Hasan T., Arora R., Bansal A.K., Bhattacharya R., Sharma G.S., Singh L.R. Disturbed homocysteine metabolism is associated with cancer. Exp. Mol. Med. 2019;51:1–13. doi: 10.1038/s12276-019-0216-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization Recommendations on Antenatal Care for a Positive Pregnancy Experience. [(accessed on 18 November 2022)]. Available online: https://apps.who.int/iris/bitstream/handle/10665/250796/97892415?sequence.
- 35.Oh C., Keats E.C., Bhutta Z.A. Vitamin and Mineral Supplementation During Pregnancy on Maternal, Birth, Child Health and Development Outcomes in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. Nutrients. 2020;12:491. doi: 10.3390/nu12020491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Gool J.D., Hirche H., Lax H., De Schaepdrijver L. Folic acid and primary prevention of neural tube defects: A review. Reprod. Toxicol. 2018;80:73–84. doi: 10.1016/j.reprotox.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Lan X., Field M.S., Stover P.J. Cell cycle regulation of folate-mediated one-carbon metabolism. Wiley Interdiscip. Rev. Syst. Biol. Med. 2018;10:e1426. doi: 10.1002/wsbm.1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Williams P.J., Bulmer J.N., Innes B.A., Broughton Pipkin F. Possible Roles for Folic Acid in the Regulation of Trophoblast Invasion and Placental Development in Normal Early Human Pregnancy. Biol. Reprod. 2011;84:1148–1153. doi: 10.1095/biolreprod.110.088351. [DOI] [PubMed] [Google Scholar]
- 39.Molloy A.M. Genetic aspects of folate metabolism. In: Stanger O., editor. Water Soluble Vitamins. Clinical Research and Future Application. Springer; Dordrecht, The Netherlands: 2011. pp. 105–130. [Google Scholar]
- 40.Rahat B., Hamid A., Bagga R., Kaur J. Folic Acid Levels During Pregnancy Regulate Trophoblast Invasive Behavior and the Possible Development of Preeclampsia. Front. Nutr. 2022;9:847136. doi: 10.3389/fnut.2022.847136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goyette P., Sumner J.S., Milos R., Duncan A.M.V., Rosenblatt D.S., Matthews R.G., Rozen R. Human methylenetetrahydrofolate reductase: Isolation of cDNA, mapping, and mutation identification. Nat. Genet. 1994;7:195–200. doi: 10.1038/ng0694-195. [DOI] [PubMed] [Google Scholar]
- 42.Al Mutairi F. Hyperhomocysteinemia: Clinical Insights. J. Central Nerv. Syst. Dis. 2020;12:1179573520962230. doi: 10.1177/1179573520962230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kang S., Zhou J., Wong P., Kowalisyn J., Strokosch G. Intermediate homocysteinaemia: A thermolabile variant of meth-ylenetrahydrofolate reductase. Am. J. Hum. Genet. 1988;43:414–421. [PMC free article] [PubMed] [Google Scholar]
- 44.Kumar A., Palfrey H.A., Pathak R., Kadowitz P.J., Gettys T.W., Murthy S.N. The metabolism and significance of homocysteine in nutrition and health. Nutr. Metab. 2017;14:78. doi: 10.1186/s12986-017-0233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xie R., Jia D., Gao C., Zhou J., Sui H., Wei X., Zhang T., Han Y., Shi J., Bai Y. Homocysteine induces procoagulant activity of red blood cells via phosphatidylserine exposure and microparticles generation. Amino Acids. 2014;46:1997–2004. doi: 10.1007/s00726-014-1755-6. [DOI] [PubMed] [Google Scholar]
- 46.Dean L. Methylenetetrahydrofolate reductase deficiency. In: Pratt V.M., Scott S.A., Pirmohamed M., Esquivel B., Kattman B.L., Malheiro A.J., editors. Medical Genetics Summaries. National Center for Biotechnology Information (US); Bethesda, MD, USA: 2012. [PubMed] [Google Scholar]
- 47.Qin J.-M., Wang X.-M., Chen B., Yang L., Li F., He L., Liao P.-H. Study on the ingestion of folate and polymorphism of MTHFR C677T with esophageal cancer in Xinjiang Kazakh. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi. 2008;29:30–33. [PubMed] [Google Scholar]
- 48.Yang Y.-B., Shang Y.-H., Tan Y.-L., Kang X.-J., Meng M., Zhao Z.-X. Methylenetetrahydrofolate Reductase Polymorphisms and Susceptibility to Esophageal Cancer in Chinese Populations: A Meta-Analysis. Asian Pac. J. Cancer Prev. 2014;15:1345–1349. doi: 10.7314/APJCP.2014.15.3.1345. [DOI] [PubMed] [Google Scholar]
- 49.Dong Y., Yi X., Yujie Z., Huixia Z., Yan C. Relationship between the Methylation of Folic Acid Metabolism-Related Genes and the Incidence and Prognosis of Esophageal Cancer among Ethnic Kazakhs. J. Cancer. 2018;9:2865–2875. doi: 10.7150/jca.25270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guo S., Pang H., Guo H., Zhang M., He J., Yan Y., Niu Q., Muratbek, Rui D., Li S., et al. Ethnic Differences in the Prevalence of High Homocysteine Levels Among Low-Income Rural Kazakh and Uyghur Adults in Far Western China and Its Implications for Preventive Public Health. Int. J. Environ. Res. Public Health. 2015;12:5373–5385. doi: 10.3390/ijerph120505373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adjalla C.E., Amouzou E.K., Sanni A., Abdelmouttaleb I., Chabi N.W., Namour F., Soussou B., Guéant J.-L. Low Frequency of Mutated Methylenetetrahydrofolate Reductase 677 C→T and 1298 A→C Genetics Single Nucleotide Polymorphisms (SNPs) in Sub-Saharan Populations. Clin. Chem. Lab. Med. (CCLM) 2003;41:1028–1032. doi: 10.1515/CCLM.2003.158. [DOI] [PubMed] [Google Scholar]
- 52.Osunkalu V., Taiwo I., Makwe C., Quao R. Methylene tetrahydrofolate reductase and methionine synthase gene polymorphisms as genetic determinants of pre-eclampsia. Pregnancy Hypertens. 2020;20:7–13. doi: 10.1016/j.preghy.2020.02.001. [DOI] [PubMed] [Google Scholar]
- 53.Ganguly P., Alam S.F. Role of homocysteine in the development of cardiovascular disease. Nutr. J. 2015;14:6. doi: 10.1186/1475-2891-14-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gaiday A.N., Tussupkaliyev A.B.T., Bermagambetova S.K., Zhumagulova S.S., Sarsembayeva L.K., Dossimbetova M.B., Daribay Z.Z. Effect of homocysteine on pregnancy: A systematic review. Chem. Biol. Interact. 2018;293:70–76. doi: 10.1016/j.cbi.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 55.Saussele T. Supplementation with folic acid before and during pregnancy. Med. Mon. Fur Pharm. 2008;31:469–472. [PubMed] [Google Scholar]
- 56.Berger M.M., Shenkin A., Schweinlin A., Amrein K., Augsburger M., Biesalski H.-K., Bischoff S.C., Casaer M.P., Gundogan K., Lepp H.-L., et al. ESPEN micronutrient guideline. Clin. Nutr. 2022;41:1357–1424. doi: 10.1016/j.clnu.2022.02.015. [DOI] [PubMed] [Google Scholar]
- 57.Wilson R.D., O’Connor D.L. Guideline No. 427: Folic Acid and Multivitamin Supplementation for Prevention of Folic Acid–Sensitive Congenital Anomalies. J. Obstet. Gynaecol. Can. 2022;44:707–719.e1. doi: 10.1016/j.jogc.2022.04.004. [DOI] [PubMed] [Google Scholar]
- 58.Jankovic-Karasoulos T., Furness D.L., Leemaqz S.Y., Dekker G.A., Grzeskowiak L.E., Grieger J.A., Andraweera P.H., McCullough D., McAninch D., McCowan L.M., et al. Maternal folate, one-carbon metabolism and pregnancy outcomes. Matern. Child Nutr. 2020;17:e13064. doi: 10.1111/mcn.13064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tian T., Yang K.-Q., Cui J.-G., Zhou L.-L., Zhou X.-L. Folic Acid Supplementation for Stroke Prevention in Patients with Cardiovascular Disease. Am. J. Med. Sci. 2017;354:379–387. doi: 10.1016/j.amjms.2017.05.020. [DOI] [PubMed] [Google Scholar]
- 60.George L., Mills J.L., Johansson A.L., Nordmark A., Olander B., Granath F., Cnattingius S. Plasma folate levels and risk of spontaneous abortion. JAMA. 2002;288:1867–1873. doi: 10.1001/jama.288.15.1867. [DOI] [PubMed] [Google Scholar]
- 61.Wen S.W., Zhou J., Yang Q., Fraser W., Olatunbosun O., Walker M. Maternal exposure to folic acid antagonists and placenta-mediated adverse pregnancy outcomes. CMAJ. 2008;179:1263–1268. doi: 10.1503/cmaj.080859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ding Y.-X., Cui H. Effects of Folic Acid on DNMT1, GAP43, and VEGFR1 in Intrauterine Growth Restriction Filial Rats. Reprod. Sci. 2017;25:366–371. doi: 10.1177/1933719117715128. [DOI] [PubMed] [Google Scholar]
- 63.Alvestad S., Husebye E.S.N., Christensen J., Dreier J.W., Sun Y., Igland J., Leinonen M.K., Gissler M., Gilhus N.E., Tomson T., et al. Folic Acid and Risk of Preterm Birth, Preeclampsia, and Fetal Growth Restriction Among Women with Epilepsy. Neurology. 2022;99:e605–e615. doi: 10.1212/WNL.0000000000200669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hovdenak N., Haram K. Influence of mineral and vitamin supplements on pregnancy outcome. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012;164:127–132. doi: 10.1016/j.ejogrb.2012.06.020. [DOI] [PubMed] [Google Scholar]
- 65.Saccone G., Berghella V. Folic acid supplementation in pregnancy to prevent preterm birth: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016;199:76–81. doi: 10.1016/j.ejogrb.2016.01.042. [DOI] [PubMed] [Google Scholar]
- 66.Sharif M.E., Mohamedain A., Ahmed A.A., Nasr A.M., Adam I. Folic acid level and preterm birth among Sudanese women. Matern. Health Neonatol. Perinatol. 2017;3:25. doi: 10.1186/s40748-017-0065-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li B., Zhang X., Peng X., Zhang S., Wang X., Zhu C. Folic Acid and Risk of Preterm Birth: A Meta-Analysis. Front. Neurosci. 2019;13:1284. doi: 10.3389/fnins.2019.01284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen X., Zhang Y., Chen H., Jiang Y., Wang Y., Wang D., Li M., Dou Y., Sun X., Huang G., et al. Association of Maternal Folate and Vitamin B12 in Early Pregnancy with Gestational Diabetes Mellitus: A Prospective Cohort Study. Diabetes Care. 2020;44:217–223. doi: 10.2337/dc20-1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Obeid R., Kasoha M., Kirsch S.H., Munz W., Herrmann W. Concentrations of unmetabolized folic acid and primary folate forms in pregnant women at delivery and in umbilical cord blood. Am. J. Clin. Nutr. 2010;92:1416–1422. doi: 10.3945/ajcn.2010.29361. [DOI] [PubMed] [Google Scholar]
- 70.Ahmed T., Fellus I., Gaudet J., MacFarlane A.J., Fontaine-Bisson B., Bainbridge S.A. Effect of folic acid on human trophoblast health and function in vitro. Placenta. 2016;37:7–15. doi: 10.1016/j.placenta.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 71.Luan Y., Leclerc D., Cosín-Tomás M., Malysheva O.V., Wasek B., Bottiglieri T., Caudill M.A., Rozen R. Moderate Folic Acid Supplementation in Pregnant Mice Results in Altered Methyl Metabolism and in Sex-Specific Placental Transcription Changes. Mol. Nutr. Food Res. 2021;65:e2100197. doi: 10.1002/mnfr.202100197. [DOI] [PubMed] [Google Scholar]
- 72.Johnson J.D., Louis J.M. Does race or ethnicity play a role in the origin, pathophysiology, and outcomes of preeclampsia? An expert review of the literature. Am. J. Obstet. Gynecol. 2020;226:S876–S885. doi: 10.1016/j.ajog.2020.07.038. [DOI] [PubMed] [Google Scholar]
- 73.Yong H.E.J., Murthi P., Brennecke S.P., Moses E.K. Genetic approaches in preeclampsia. In Preeclampsia. Methods and Protocols. In: Murthi P., Vaillancourt C., editors. Springer; New York, NY, USA: 2017. pp. 53–72. [Google Scholar]
- 74.Lokki A.I., Heikkinen-Eloranta J.K., Laivuori H. The Immunogenetic Conundrum of Preeclampsia. Front. Immunol. 2018;9:2630. doi: 10.3389/fimmu.2018.02630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dunk C.E., Bucher M., Zhang J., Hayder H., Geraghty D.E., Lye S.J., Myatt L., Hackmon R. Human Leukocyte Antigen HLA-C, HLA-G, HLA-F and HLA-E placental profiles are altered in Early Severe Preeclampsia and Preterm Birth with Chorioamnionitis. Am. J. Obstet. Gynecol. 2022;227:641.e1–641.e13. doi: 10.1016/j.ajog.2022.07.021. [DOI] [PubMed] [Google Scholar]
- 76.Loisel D.A., Billstrand C., Murray K., Patterson K., Chaiworapongsa T., Romero R., Ober C. The maternal HLA-G 1597 C null mutation is associated with increased risk of pre-eclampsia and reduced HLA-G expression during pregnancy in African-American women. Mol. Hum. Reprod. 2012;19:144–152. doi: 10.1093/molehr/gas041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Eche S., Mackraj I., Moodley J. Circulating fetal and total cell-free DNA, and sHLA-G in black South African women with gestational hypertension and pre-eclampsia. Hypertens. Pregnancy. 2017;36:295–301. doi: 10.1080/10641955.2017.1385794. [DOI] [PubMed] [Google Scholar]
- 78.Phoswa W.N., Ramsuran V., Naicker T., Singh R., Moodley J. HLA-G Polymorphisms Associated with HIV Infection and Preeclampsia in South Africans of African Ancestry. BioMed Res. Int. 2020;2020:1697657. doi: 10.1155/2020/1697657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McGinnis R., The FINNPEC Consortium. Steinthorsdottir V., O Williams N., Thorleifsson G., Shooter S., Hjartardottir S., Bumpstead S., Stefansdottir L., Hildyard L., et al. Variants in the fetal genome near FLT1 are associated with risk of preeclampsia. Nat. Genet. 2017;49:1255–1260. doi: 10.1038/ng.3895. [DOI] [PubMed] [Google Scholar]
- 80.Gray K., Saxena R., Karumanchi S.A. Genetic predisposition to preeclampsia is conferred by fetal DNA variants near FLT1, a gene involved in the regulation of angiogenesis. Am. J. Obstet. Gynecol. 2017;218:211–218. doi: 10.1016/j.ajog.2017.11.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kikas T., Inno R., Ratnik K., Rull K., Laan M. C-allele of rs4769613 Near FLT1 Represents a High-Confidence Placental Risk Factor for Preeclampsia. Hypertension. 2020;76:884–891. doi: 10.1161/HYPERTENSIONAHA.120.15346. [DOI] [PubMed] [Google Scholar]
- 82.Say L., Chou D., Gemmill A., Tunçalp Ö., Moller A.-B., Daniels J., Gülmezoglu A.M., Temmerman M., Alkema L. Global causes of maternal death: A WHO systematic analysis. Lancet Glob. Health. 2014;2:E323–E333. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 83.Geller S.E., Koch A.R., Garland C.E., MacDonald E.J., Storey F., Lawton B. A global view of severe maternal morbidity: Moving beyond maternal mortality. Reprod. Health. 2018;15:31–43. doi: 10.1186/s12978-018-0527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.McLaren Z.M., Sharp A., Hessburg J.P., Sarvestani A.S., Parker E., Akazili J., Johnson T.R., Sienko K.H. Cost effectiveness of medical devices to diagnose pre-eclampsia in low-resource settings. Dev. Eng. 2017;2:99–106. doi: 10.1016/j.deveng.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wallis A.B., Saftlas A.F., Hsia J., Atrash H.K. Secular Trends in the Rates of Preeclampsia, Eclampsia, and Gestational Hypertension, United States, 1987–2004. Am. J. Hypertens. 2008;21:521–526. doi: 10.1038/ajh.2008.20. [DOI] [PubMed] [Google Scholar]
- 86.Roberts J., Cooper D. Pathogenesis and genetics of pre-eclampsia. Lancet. 2001;357:53–56. doi: 10.1016/S0140-6736(00)03577-7. [DOI] [PubMed] [Google Scholar]
- 87.Mishra J., Talwar S., Kaur L., Chandiok K., Yadav S., Puri M., Sachdeva M., Lakshmy R., Saraswathy K. Differential global and MTHFR gene specific methylation patterns in preeclampsia and recurrent miscarriages: A case-control study from North India. Gene. 2019;704:68–73. doi: 10.1016/j.gene.2019.04.036. [DOI] [PubMed] [Google Scholar]
- 88.Moussa H.N., Nasab S.H., A Haidar Z., Blackwell S.C., Sibai B.M. Folic acid supplementation: What is new? Fetal, obstetric, long-term benefits and risks. Future Sci. OA. 2016;2:FSO116. doi: 10.4155/fsoa-2015-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cotter A.M., Molloy A., Scott J.M., Daly S.F. Elevated plasma homocysteine in early pregnancy: A risk factor for the development of severe preeclampsia. Am. J. Obstet. Gynecol. 2001;185:781–785. doi: 10.1067/mob.2001.117304. [DOI] [PubMed] [Google Scholar]
- 90.Mujawar S.A., Patil V.W., Daver R.G. Study of Serum Homocysteine, Folic Acid and Vitamin B12 in Patients with Preeclampsia. Indian J. Clin. Biochem. 2011;26:257–260. doi: 10.1007/s12291-011-0109-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kharb S., Aggarwal D., Bala J., Nanda S. Evaluation of Homocysteine, Vitamin B12 and Folic Acid Levels During all the Trimesters in Pregnant and Preeclamptic Womens. Curr. Hypertens. Rev. 2017;12:234–238. doi: 10.2174/1573402112666161010151632. [DOI] [PubMed] [Google Scholar]
- 92.Guven M.A., Coskun A., Ertas I.E., Aral M., Zencırcı B., Oksuz H. Association of Maternal Serum CRP, IL-6, TNF-α, Homocysteine, Folic Acid and Vitamin B12 Levels with the Severity of Preeclampsia and Fetal Birth Weight. Hypertens. Pregnancy. 2009;28:190–200. doi: 10.1080/10641950802601179. [DOI] [PubMed] [Google Scholar]
- 93.Kharb S., Nanda S. Patterns of Biomarkers in Cord Blood During Pregnancy and Preeclampsia. Curr. Hypertens. Rev. 2017;13:57–64. doi: 10.2174/1573402113666170126101914. [DOI] [PubMed] [Google Scholar]
- 94.Acilmis Y.G., Dikensoy E., Kutlar A.I., Balat O., Cebesoy F.B., Ozturk E., Cicek H., Pence S. Homocysteine, folic acid and vitamin B12 levels in maternal and umbilical cord plasma and homocysteine levels in placenta in pregnant women with pre-eclampsia. J. Obstet. Gynaecol. Res. 2010;37:45–50. doi: 10.1111/j.1447-0756.2010.01317.x. [DOI] [PubMed] [Google Scholar]
- 95.McNulty B., McNulty H., Marshall B., Ward M., Molloy A.M., Scott J.M., Dornan J., Pentieva K. Impact of continuing folic acid after the first trimester of pregnancy: Findings of a randomized trial of Folic Acid Supplementation in the Second and Third Trimesters. Am. J. Clin. Nutr. 2013;98:92–98. doi: 10.3945/ajcn.112.057489. [DOI] [PubMed] [Google Scholar]
- 96.Wen S.W., Chen X.-K., Rodger M., White R.R., Yang Q., Smith G., Sigal R.J., Perkins S.L., Walker M.C. Folic acid supplementation in early second trimester and the risk of preeclampsia. Am. J. Obstet. Gynecol. 2008;198:45.e1–45.e7. doi: 10.1016/j.ajog.2007.06.067. [DOI] [PubMed] [Google Scholar]
- 97.Wen S.W., Guo Y., Rodger M., White R.R., Yang Q., Smith G.N., Perkins S.L., Walker M.C. Folic Acid Supplementation in Pregnancy and the Risk of Pre-Eclampsia—A Cohort Study. PLoS ONE. 2016;11:e0149818. doi: 10.1371/journal.pone.0149818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang Y., Zhao N., Qiu J., He X., Zhou M., Cui H., Lv L., Lin X., Zhang C., Zhang H., et al. Folic acid supplementation and dietary folate intake, and risk of preeclampsia. Eur. J. Clin. Nutr. 2015;69:1145–1150. doi: 10.1038/ejcn.2014.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vanderlelie J., Scott R., Shibl R., Lewkowicz J., Perkins A., Scuffham P. First trimester multivitamin/mineral use is associated with reduced risk of pre-eclampsia among overweight and obese women. Matern. Child Nutr. 2014;12:339–348. doi: 10.1111/mcn.12133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Han T.B., Guo L.L., Yang F.F., Zhao F., Du W.Q., Wang Y., Shen J.X., Feng Y.L., Yang H.L., Zhang Y.W., et al. Folic acid supplementation before and during pregnancy and the risk of preeclampsia. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:1894–1899. doi: 10.3760/cma.j.cn112338-20191218-00895. [DOI] [PubMed] [Google Scholar]
- 101.Kim M.W., Ahn K.H., Ryu K.-J., Hong S.-C., Lee J.S., Nava-Ocampo A.A., Oh M.-J., Kim H.-J. Preventive Effects of Folic Acid Supplementation on Adverse Maternal and Fetal Outcomes. PLoS ONE. 2014;9:e97273. doi: 10.1371/journal.pone.0097273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Martinussen M.P., Bracken M.B., Triche E.W., Jacobsen G.W., Risnes K.R. Folic acid supplementation in early pregnancy and the risk of preeclampsia, small for gestational age offspring and preterm delivery. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015;195:94–99. doi: 10.1016/j.ejogrb.2015.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zheng L., Huang J., Kong H., Wang F., Su Y., Xin H. The effect of folic acid throughout pregnancy among pregnant women at high risk of pre-eclampsia: A randomized clinical trial. Pregnancy Hypertens. 2020;19:253–258. doi: 10.1016/j.preghy.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 104.Li Z., Ye R., Zhang L., Li H., Liu J., Ren A. Folic Acid Supplementation During Early Pregnancy and the Risk of Gestational Hypertension and Preeclampsia. Hypertension. 2013;61:873–879. doi: 10.1161/HYPERTENSIONAHA.111.00230. [DOI] [PubMed] [Google Scholar]
- 105.Ayala-Ramírez P., Serrano N., Barrera V., Bejarano J.P., Silva J.L., Martínez R., Gil F., Olaya-C M., García-Robles R. Risk factors and fetal outcomes for preeclampsia in a Colombian cohort. Heliyon. 2020;6:e05079. doi: 10.1016/j.heliyon.2020.e05079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Corsi D.J., Gaudet L.M., El-Chaar D., White R.R., Rybak N., Harvey A., Muldoon K., Wen S.W., Walker M. Effect of high-dose folic acid supplementation on the prevention of preeclampsia in twin pregnancy. J. Matern. Neonatal Med. 2020;35:503–508. doi: 10.1080/14767058.2020.1725882. [DOI] [PubMed] [Google Scholar]
- 107.Antoniades C., Shirodaria C., Warrick N., Cai S., De Bono J., Lee J., Leeson P., Neubauer S., Ratnatunga C., Pillai R., et al. 5-Methyltetrahydrofolate Rapidly Improves Endothelial Function and Decreases Superoxide Production in Human Vessels. Circulation. 2006;114:1193–1201. doi: 10.1161/CIRCULATIONAHA.106.612325. [DOI] [PubMed] [Google Scholar]
- 108.Antoniades C., Shirodaria C., Leeson P., Baarholm O.A., Van-Assche T., Cunnington C., Pillai R., Ratnatunga C., Tousoulis D., Stefanadis C., et al. MTHFR 677 C>T Polymorphism Reveals Functional Importance for 5-Methyltetrahydrofolate, Not Homocysteine, in Regulation of Vascular Redox State and Endothelial Function in Human Atherosclerosis. Circulation. 2009;119:2507–2515. doi: 10.1161/CIRCULATIONAHA.108.808675. [DOI] [PubMed] [Google Scholar]
- 109.Yuyun M.F., Ng L., Ng G.A. Endothelial dysfunction, endothelial nitric oxide bioavailability, tetrahydrobiopterin, and 5-methyltetrahydrofolate in cardiovascular disease. Where are we with therapy? Microvasc. Res. 2018;119:7–12. doi: 10.1016/j.mvr.2018.03.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data related to this article could be retrieved from authors (gulzhanat.aimagambetova@nu.edu.kz) per reasonable request.