Abstract
Objectives:
While many prior studies have shown that high average levels of nurse staffing in nursing homes are associated with fewer hospitalizations, some studies have not, suggesting that the average nursing level may mask a more complex relationship. This study examines this issue by investigating the associations of daily staffing patterns and daily hospitalizations and Emergency Department (ED) visits.
Design:
Retrospective analyses of national Payroll Based Journal (PBJ) staffing data merged with the Minimum Data Set.
Setting and Participants:
15,718 nursing homes nationally reporting PBJ data during 2017-2019, their staff, and residents.
Methods:
We estimated facility-day-level models as conditional facility fixed-effect Poisson regressions with robust standard errors. The dependent variables were daily numbers of hospitalization and ED visits and the independent variables of interest were the number of RN, LPN, and CNA hours on the same and prior days.
Results:
The daily number of hospital transfers averaged 0.28 (SD 0.21). Daily total direct-care staffing hours averaged 288.7 (SD 188.2) with RNs accounting for 35.0, LPNs for 68.7 and CNAs for 185.0. Higher staffing was associated with more hospitalizations on the concurrent day. Higher staffing on the day prior was associated with fewer hospitalizations. The effect size was larger for RNs and LPNs [same day=~2%; prior day=~ (−0.7%) - (−0.9%)] than for CNAs [same day<1%; prior day< −0.5%]. ED visits not leading to hospitalizations, and analyses for sub-samples exhibited similar findings.
Conclusions and Implications:
Our findings suggest that staff can address developing problems and prevent admissions the next day and identify emergent problems and hospitalize the same day. They also underscore the complex array of nursing home factors involved in hospitalization and ED visits, including the influence of daily staffing variation, suggesting the need for further research to better understand the associations between staffing and appropriate resident transfers to the hospital or the ED, and the potential implications for quality metrics in these domains.
Keywords: Nursing homes, staffing, hospitalizations, ed visits, quality
Brief Summary:
It’s time to think about more than average quarterly nursing home staffing. Important paper considers relationship between daily staffing variation and daily hospitalization.
INTRODUCTION
Nursing homes are expected to provide most of the medical care their residents require in-house and minimize hospitalizations. While some conditions, like acute myocardial infarction, almost always require hospitalization, many not only can be treated in the nursing home, but hospitalizing the resident may actually increase the risk of iatrogenic events and discontinuity of care contributing to further deterioration in the resident’s condition, functional decline, and delirium.1-3 Therefore, a low hospitalization rate has long been considered a marker of high-quality nursing home care. Measures of appropriate hospitalizations were included in the Centers for Medicare & Medicaid Services (CMS) nursing home value-based payment demonstration4 and measures of hospitalizations are included as quality indicators in the Nursing Home Care Compare (NHCC) report card published by CMS.5,6
Factors influencing hospitalizations have been studied extensively, with many studies examining staffing levels as explanatory variables because staffing, whether registered nurses (RNs), licensed practical nurses (LPNs), or certified nurse assistants (CNAs), provide direct day-to-day patient care and are likely to be intimately involved in the care processes and decisions leading to hospitalizations. These studies, summarized by several recent reviews,7-12 revealed mixed evidence about the relationship between staffing and hospitalization, with some failing to identify the expected association of higher staffing levels with lower hospitalization rates. The authors of these reviews identified a set of common limitations as likely reasons for the failure to find the expected associations between staffing and hospitalizations. These limitations include reliance on staffing data from the CMS Online Survey Certification and Reporting (OSCAR) System or the system that replaced it, the Certification and Survey Provider Enhanced Reporting (CASPER), both of which collect staffing data once a year and may be inaccurate,13,14 the cross-sectional nature of most studies, and the lack of statistical control for other variables that might be important, such as presence of other providers paid by the facility (e.g. nursing administrators, nurse practitioners, medical directors), and inability to distinguish between employed and contract staff.
We present analyses that address some of these prior limitations utilizing a new dataset, the Payroll Based Journal (PBJ), which provides daily staffing data based on each nursing home’s payroll information, and is more accurate and more detailed than prior data. We take the novel approach of analyzing day-to-day patterns of hospitalizations as they relate to RNs’, LPNs’, and CNAs’ daily staffing levels for all nursing homes in the US, as well as facilities at the top and bottom of the staffing distribution, offering a complementary perspective to prior studies. We test the hypothesis that the observed associations between average higher staffing and fewer hospitalizations will also be observed between same day and prior day staffing and hospitalizations.
METHODS
Sample
The sample included all 15,718 Medicare and Medicaid certified nursing homes in the country during the period January 2017 through August 2019. The analysis for emergency department (ED) visits not followed by a hospitalization was based on Outpatient Claims files, which are limited to Medicare Fee-for-Service residents and included 15,608 nursing homes (99.3%).
Data Sources
The PBJ includes the number of hours paid daily for each staff type, including RNs, LPNs, CNAs, therapy staff, physicians, administrators and others, by nursing home. It also provides daily patient census.
We merged the PBJ data with resident level data, calculated from the Minimum Data Set (MDS) 3.0, at the facility-day level. The MDS includes assessments for all nursing home residents with information about age, gender, case mix (Resource Utilization Group – RUGs IV), cognitive impairment, Alzheimer’s or related dementias (ADRD) diagnoses, and dates of hospitalization and death. For some analyses we also utilized the Medicare Outpatient Claims for ED visits not followed by a hospital admission. We also merged in the Master Beneficiary Summary File, to identify residents enrolled in Medicare Advantage during their nursing home stays, the Nursing Home Five-Star Quality Rating data, and facility characteristics reported in Long-Term-Care Focus.15
Analyses
The study was approved by the lead author’s University’s IRB.
Analyses were conducted at the facility-day level. Time-dependent variables were calculated for each nursing home, as counts or averages for each day.
Dependent Variables
The dependent variable were the count of daily discharges from the nursing home to an acute care or psychiatric hospital as reported on the MDS discharge or transfer to the ED not followed by a hospital admission as reported on the Outpatient claim.
Daily-Varying Independent Variables
There were six independent variables of interest: RNs, LPNs, and CNAs hours on the transfer-day to the hospital (or the ED) and RNs, LPNs, and CNAs hours on the day prior to transfer. For example, when examining the number of transfers on July 1, we measure staffing on that same day (July 1) and on the preceding day (June 30).
Daily control variables included: Percent male residents in the facility on the day of transfer, percent residents who are less than 65, 65-74, 75-84, with 85+ as reference, and percent of residents enrolled in Medicare Advantage on the transfer day. Case-mix on the day of transfer was controlled by 66 variables. Each variable corresponds to one of the 66 RUGs categories and indicates the number of residents classified into that RUG on that date based on their most recent MDS assessment. Also included were a set of monthly indicator variables controlling for time trends.
Stratification variables for sub-analyses
We performed stratified analyses to examine hypotheses about different patterns of associations between staffing and hospitalizations in facilities with specific characteristics, as follows: 1) facility quality measured by the 5-Star Quality Measures (QMs) ratings and the 5-Star Survey ratings published in Nursing Home Care Compare and averaged over the study period; 2) average total direct-care nursing (sum of RNs, LPNs and CNAs) hours over the study period; 3) average hospitalizations over the study period; 4) for-profit and non-profit ownership; 5) percent of residents covered by Medicare; and 6) percent of residents with ADRD and cognitive impairment.
Estimated Models
We estimated a facility-day-level model, with hospitalization on each day as the dependent variable and nursing hours by type (RN, LPN and CNA) on the same day and on the day prior as the six independent variables of interest, controlling for all other variables described above: age, sex, case-mix count, all of them calculated for the transfer day, and the month. The model was estimated as a conditional facility fixed-effect, Poisson regression, with robust standard errors. The facility fixed-effects approach controls for all time-invariant differences between nursing homes (e.g. ownership).
We estimated a base case model on the full sample. We then stratified the sample by facility characteristics as described above, and estimated models for subsamples defined by the bottom and top 30th percentiles of the distribution for each characteristic. We also estimated a full sample model that separated employed and contract nursing staff and a full sample model that added other personnel types (if salaried by the facility) including hours of Director of Nursing-RN, RN Administrators, LPN Administrators, Medical Directors, Other MDs, Nurse Practitioners, Nurse Aides in Training, and Medication Aides.
We present the regression results for the staffing variables as a change in the percent of daily hospitalizations associated with a 1 full time equivalent (i.e., 8 hours) increase in the staffing variable, holding all other variables constant.a The p-values reported are for the actual coefficients.
Sensitivity Analyses
To test the robustness of our findings to different assumptions we performed several sensitivity analyses:
To account for possible mismatches in dates between the hospital and ED data and the nursing home data, we estimated models where transfer was matched more liberally, within 1 day of the discharge from the nursing home.
To investigate sensitivity to the number of prior days’ staffing included, we estimated models with 1) no variables for staffing on prior days, and 2) two variables for staffing one- and two-days prior.
To test the sensitivity of our stratified analyses to the definition of the strata threshold, all analyses were repeated with thresholds set to 85% and 15%.
To test whether our results are driven by the known phenomenon of lower staffing on weekends16 or on Mondays and Fridays (as observed in our data, see below) we performed an analysis limited to hospitalizations during mid-week only (Tuesdays, Wednesdays, and Thursdays).
RESULTS
Table 1 presents descriptive statistics for the analytic sample. The average daily number of hospital transfers was 0.28 (SD 0.21) and transfers to the ED not followed by a hospitalization was 0.11 (SD 0.07). Average daily total direct care staffing hours (including employed and contract staff) was 288.7 (SD 188.2). Of those, RNs accounted for 35.0, LPNs for 68.7 and CNAs for 185.0 hours, mostly accounted for by employed staff.
Table 1:
Descriptive Statistics
| Number of Nursing Homes |
Mean | Standard Deviation |
|
|---|---|---|---|
| Dependent Variables: Measured Daily | |||
| Discharges from nursing home to acute care or psychiatric hospital | 15,718 | 0.28 | 0.21 |
| Emergency department visits not followed by a hospitalization | 15,608 | 0.11 | 0.07 |
| Independent Variables: | |||
| Nursing Homes and Resident Variables Measured Daily | |||
| RN hours per day | 15,718 | 35.0 | 33.3 |
| Salaried | 15,718 | 34.0 | 32.2 |
| Contract | 15,718 | 1.0 | 5.6 |
| LPN hours per day | 15,718 | 68.7 | 48.8 |
| Salaried | 15,718 | 66.4 | 47.0 |
| Contract | 15,718 | 2.3 | 7.6 |
| CNA hours per day | 15,718 | 185.0 | 124.8 |
| Salaried | 15,718 | 180.0 | 121.0 |
| Contract | 15,718 | 5.0 | 17.9 |
| Total direct care nurse staffing - per day | 15,718 | 288.7 | 188.2 |
| Director of Nursing (RN) per day | 15,718 | 5.0 | 1.7 |
| RN Administrator per day | 15,718 | 11.7 | 12.5 |
| LPN Administrator hours per day | 15,718 | 6.0 | 8.7 |
| Nurse Aide in training hours per day | 15,718 | 2.6 | 7.3 |
| Medication Aide hours per day | 15,718 | 6.6 | 14.8 |
| Medical Director hours per day | 15,718 | 0.4 | 0.7 |
| Other MD hours per day | 15,718 | 0.2 | 2.0 |
| Nurse Practitioner hours per day | 15,718 | 0.3 | 1.2 |
| Daily resident census | 15,718 | 85.2 | 52.8 |
| % of residents in Medicare Advantage | 15,718 | 26.1 | 19.0 |
| % of residents who are male | 15,718 | 35.7 | 11.8 |
| % of residents under 65 | 15,718 | 15.8 | 14.7 |
| % of residents aged 65-74 | 15,718 | 18.5 | 8.0 |
| % of residents aged 75-84 | 15,718 | 27.0 | 6.8 |
| % of residents aged 85 and over | 15,718 | 38.7 | 18.0 |
| Facility Characteristics Measured Quarterly or Annua | |||
| Average Quality Measures (QMs) 5-Star Rating (1-5) | 13,422 | 3.8 | 1.0 |
| Average Survey 5-Star Rating (1-5) | 13,455 | 2.8 | 1.1 |
| % of residents with Medicare payer | 14,960 | 13.3 | 13.4 |
| % of residents with Medicaid payer | 14,960 | 60.1 | 23.5 |
| % of residents with ADRD and cognitive impairment diagnoses | 15,718 | 47.7 | 16.2 |
| Number of Nursing Homes |
Percent | ||
| For profit ownership | 10,479 | 70.1 | |
| Non-profit ownership | 4,481 | 30.0 | |
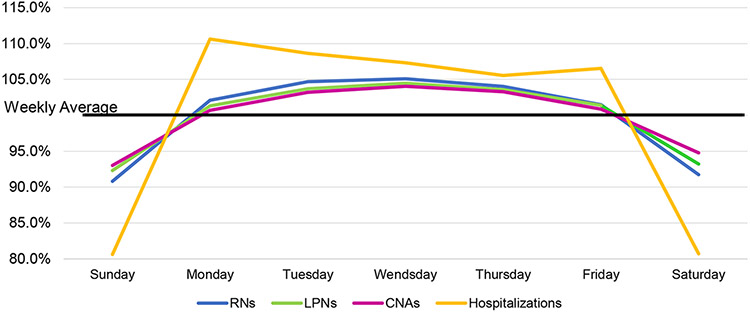
Figure 1 depicts daily staffing variations. It shows, separately for RNs, LPNs and CNAs, the average number of hours per resident-day for each day of the week as a percent of the number of hours per resident-day averaged over the week, thus identifying days with staffing above and below average. All three staff types exhibit the same pattern, with the highest in midweek – Tuesday through Thursday – with about 2-5 percentage points decline on Friday and Monday, and the largest decline on the weekend – of over 10 percentage points from the mid-week high. The biggest decline is for RNs and the smallest for CNAs. The figure also shows the daily variation in hospitalizations as percent of its weekly average. Hospitalizations follow a similar pattern to that of staffing, with a lower percent during the weekend compared with weekdays. The range of the differences between weekdays and weekend is larger for hospitalizations than for staffing, at about 25-30 percentage points.
Figure 1: Staffing per Resident-Day and Hospitalizations by Day of the Week as Percent of the Weekly Average*.
Note: The weekly average is calculated separately for each of the 4 variables depicted in the chart.
The Y scale shows how the value of the variable on any given day deviates from the weekly average for that variable.
Example: On Sunday, hospitalizations are 81% of the hospitalization weekly average, RNs are at 91% of the RN weekly average, LPNs are at 95.5% of the LPN weekly average, and CNAs are at 96% of the CNA weekly average.
Table 2 presents the results of the regression models, examining the relationships between staffing and hospitalizations for the base case, which includes the full sample, all nursing homes and all residents, followed by results of two models with different staffing specifications and then the stratified models. The table presents, for each model, the daily percent change in number of hospitalizations for a 1 full time staff (FTE) increase. The full base case model is provided in Appendix Table 1.
Table 2 –
Summary of Findings: Base Case and Stratified Analyses – Percent Change in Daily Hospitalizations Due to an Increase of a One Full Time Equivalent Staff Position*
| Same Day | Previous Day | |||||
|---|---|---|---|---|---|---|
| RNs | LPNs | CNAs | RNs | LPNs | CNAs | |
| Base Case, full sample | ||||||
|
2.3%
[2.1, 2.4] (<.001) |
2.1%
[2.0, 2.2] (<.001) |
0.6%
[0.5, 0.7] (<.001) |
−0.8%
[−0.9, −0.7] (<.001) |
−0.8%
[−0.9, −0.7] (<.001) |
−0.4%
[−0.4, −0.3] (<.001) |
|
| Models with different specifications, full sample: | ||||||
| 1) Separate staffing variables for employed and contract staff by type in same model, full sample | ||||||
| Employed Staff |
2.3%
[2.2, 2.4] (<.001) |
2.1%
[2.0, 2.3] (<.001) |
0.6%
[0.6, 0.7] (<.001) |
−0.8%
[−0.9, −0.7] (<.001) |
−0.8%
[−0.9, −0.8] (<.001) |
−0.4%
[−0.4, −0.3] (<.001) |
| Contract Staff |
1.7%
[1.3, 2.1] (<.001) |
1.4%
[1.2, 1.6] (<.001) |
0.3%
[0.2, 0.5] (<.001) |
−0.4% [−0.7, −0.1] (0.017) |
−0.0% [−0.2, 0.1] (0.698) |
−0.1% [−0.2, 0.1] (0.383) |
| 2) Adding variables for non-nursing FTE providers to the model**, full sample | ||||||
|
1.5%
[1.3, 1.6] (<.001) |
1.5%
[1.4, 1.6] (<.001) |
0.0% [−0.0, 0.1] (0.149) |
−0.3%
[−0.4, −0.2] (<.001) |
−0.2%
[−0.3, −0.1] (<.001) |
−0.1%
[−0.2, −0.1] (<.001) |
|
| 3) NH Quality measured by 5 Star QMs stratification | ||||||
| High Average Quality 5-Star Rating (>=4.75) |
2.4%
[2.1, 2.7] (<.001) |
2.1%
[1.8, 2.5] (<.001) |
0.5%
[0.3, 0.7] (<.001) |
−0.9%
[−1.2, −0.6] (<.001) |
−0.8%
[−1.0, −0.6] (<.001) |
−0.3%
[−0.4, −0.1] (0.001) |
| Low Average Quality 5-Star Rating (<2.5) |
2.0%
[1.6, 2.4] (<.001) |
2.0%
[1.7, 2.4] (<.001) |
0.8%
[0.7, 1.0] (<.001) |
−0.6%
[−0.9, −0.3] (<.001) |
−0.8%
[−1.0, −0.6] (<.001) |
−0.3%
[−0.5, −0.1] (0.001) |
| 4) NH Quality measured by 5 Star Survey stratification | ||||||
| High Average Survey 5-Star Rating (>=4) |
2.4%
[2.0, 2.7] (<.001) |
2.0%
[1.6, 2.3] (<.001) |
0.5%
[0.2, 0.7] (0.003) |
−0.7%
[−0.9, −0.4] (<.001) |
−0.7%
[−1.0, −0.5] (<.001) |
−0.3%
[−0.5, −0.1] (0.001) |
| Low Average Survey 5-Star Rating (<2) |
2.3%
[2.1, 2.5] (<.001) |
2.2%
[2.0, 2.4] (<.001) |
0.7%
[0.6, 0.8] (<.001) |
−0.9%
[−1.1, −0.8] (<.001) |
−0.9%
[−1.0, −0.8] (<.001) |
−0.4%
[−0.5, −0.3] (<.001) |
| 5) Total nursing level stratification | ||||||
| High Average Nursing Level (above 70th percentile) |
2.3%
[2.1, 2.5] (<.001) |
2.0%
[1.8, 2.2] (<.001) |
0.4%
[0.2, 0.5] (<.001) |
−0.9%
[−1.1, −0.7] (<.001) |
−0.8%
[−1.0, −0.7] (<.001) |
−0.2%
[−0.3, −0.1] (<.001) |
| Low Average Nursing Level (30th percentile & below) |
2.1%
[1.9, 2.4] (<.001) |
2.2%
[2.0, 2.5] (<.001) |
0.9%
[0.8, 1.1] (<.001) |
−0.7%
[−0.9, −0.5] (<.001) |
−0.9%
[−1.0, −0.7] (<.001) |
−0.5%
[−0.6, −0.4] (<.001) |
| 6) Hospitalization level stratification | ||||||
| High Hospitalization Rate (above 70th percentile) |
2.4%
[2.2, 2.6] (<.001) |
2.3%
[2.1, 2.5] (<.001) |
0.7%
[0.5, 0.8] (<.001) |
−0.9%
[−1.1, −0.8] (<.001) |
−0.9%
[−1.1, −0.8] (<.001) |
−0.5%
[−0.6, −0.3] (<.001) |
| Low Hospitalization Rate (30th percentile & below) |
2.0%
[1.7, 2.4] (<.001) |
1.6%
[1.3, 1.9] (<.001) |
0.4%
[0.3, 0.5] (<.001) |
−0.6%
[−0.7, −0.4] (<.001) |
−0.5%
[−0.7, −0.3] (<.001) |
−0.2%
[−0.3, −0.1] (<.001) |
| 7) Non-profit versus for-profit nursing homes | ||||||
| Non-profit nursing homes |
1.9%
[1.7, 2.1] (<.001) |
1.4%
[1.2, 1.6] (<.001) |
0.5%
[0.4, 0.6] (<.001) |
−0.7%
[−0.9, −0.5] (<.001) |
−0.6%
[−0.8, −0.5] (<.001) |
−0.2%
[−0.3, −0.1] (<.001) |
| For-profit nursing homes |
2.5%
[2.3, 2.6] (<.001) |
2.4%
[2.3, 2.5] (<.001) |
0.7%
[0.6, 0.8] (<.001) |
−0.8%
[−1.0, −0.7] (<.001) |
−0.8%
[−0.9, −0.8] (<.001) |
−0.5%
[−0.5, −0.4] (<.001) |
| 8) High versus low Medicare census nursing homes | ||||||
| High Medicare nursing homes (above 70th percentile) |
2.4%
[2.2, 2.6] (<.001) |
2.2%
[2.0, 2.4] (<.001) |
0.7%
[0.5, 0.8] (<.001) |
−0.8%
[−1.0, −0.7] (<.001) |
−0.9%
[−1.1, −0.8] (<.001) |
−0.4%
[−0.6, −0.3] (<.001) |
| Low Medicare nursing homes (30th percentile & below) |
2.0%
[1.8, 2.3] (<.001) |
1.8%
[1.6, 2.0] (<.001) |
0.6%
[0.5, 0.7] (<.001) |
−0.6%
[−0.8, −0.4] (<.001) |
−0.6%
[−0.8, −0.5] (<.001) |
−0.4%
[−0.5, −0.3] (<.001) |
| 9) Nursing homes with high and low percent of residents with Alzheimer Disease and Associated Dementias (ADRD) and Cognitive Impairment | ||||||
| High ADRD (above 70th percentile) |
2.1%
[1.9, 2.3] (<.001) |
1.9%
[1.7, 2.2] (<.001) |
0.5%
[0.4, 0.6] (<.001) |
−0.7%
[−0.8, −0.6] (<.001) |
−0.7%
[−0.9, −0.6] (<.001) |
−0.3%
[−0.4, −0.2] (<.001) |
| Low ADRD (30th percentile & below) |
2.7%
[2.5, 2.8] (<.001) |
2.4%
[2.3, 2.6] (<.001) |
0.8%
[0.7, 0.9] (<.001) |
−1.0%
[−1.1, −0.8] (<.001) |
−1.0%
[−1.1, −0.9] (<.001) |
−0.6%
[−0.7, −0.5] (<.001) |
| 10) Residents transferred to the Emergency Department but not followed by a hospitalization | ||||||
| Based on Outpatient claims files that include FFS residents only |
1.4%
[1.3, 1.6] (<.001) |
1.5%
[1.3, 1.6] (<.001) |
0.1%
[0.1, 0.2] (<.001) |
−0.4%
[−0.5, −0.3] (<.001) |
−0.4%
[−0.5, −0.3] (<.001) |
−0.1%
[−0.1, −0.0] (0.023) |
Each line reports findings from a separate regression model which also controls for age, gender, case mix, seasonality and facility fixed effects. Models differ by either staffing variables (e.g. salaried vs. contract), or facility characteristics (e.g. low quality vs. high quality)
Additional providers included DON-RN, RN Administrator, LPN Administrator, Medical Director, Other MD, Nurse Practitioner, Nurses Aid in Training, Medication Aid.
All models exhibit the same general findings. On the same day as the hospitalization, more staff is associated with more hospitalizations, typically with a stronger effect for RNs and LPNs, often around 2%, compared with CNAs, typically with less than 1% and often less than 0.5%. More staff on the day prior is associated with fewer hospitalizations, again mostly with stronger effects for RNs and LPNs, mostly between −0.7% to −0.9% and smaller effects for CNAs, bellow −0.5%.
All effects are significant at the 0.001 level, except for 2 models. The model with separate covariates for employed and contract staff has very low previous day effects with p values of 0.02, 0.7, and 0.4 for contract RNs, LPNs and CNAs respectively. The model with additional types of non-nursing staff has a very low same day and non-significant (p=0.15) effect for CNAs.
The sensitivity analyses described above have similar findings. A model without any lags shows a positive association between staffing and hospitalization on the same day. Adding two-days lags show a positive same day effect and negative effects 1 and 2 days prior to the transfer. Appendix Table 2 shows summary results for dyads defined with different thresholds and for the midweek days sample.
DISCUSSION
In this study we evaluated the association between daily staffing and hospitalization and found that it depends on the day of transfer to the hospital. High staffing was protective against hospitalization on the following day, but high staffing measured on the concurrent day with the hospitalization was associated with more hospitalizations. These findings were very robust, observed not only in the full sample and base-case, but also in all other model specifications, when estimated separately for employed and contract staff, when non-nursing staff were added to the model, and when the model was estimated on stratified samples.
While the protective effect of high staffing on hospitalization has been observed in many previous studies,7-12 evidence for high staffing increasing the risk of hospitalization for nursing home residents is novel, to our knowledge. We believe that these unexpected findings are due to the fact that for the first time we are able to analyze daily staffing data. All prior studies of the associations between staffing and hospitalizations relied on staffing data averaged over large periods of time, which likely masked this phenomenon.
What might be the explanation for these two different associations between staffing and hospitalizations? The same-day increased hospitalization with higher staffing is likely due to staff’s increased ability to monitor residents and identify those residents that may require immediate transfer. We note that the same-day effect is over 3 times larger for RNs and LPNs than for CNAs. As the former are the ones likely to perform assessments and make transfer recommendations, this offers further support for the explanation. The protective effect of the prior-day high staffing on hospitalization may also be explained by staff having increased ability to monitor and identify residents with clinical issues requiring interventions. In these cases the interventions available in-house might avert further decline and prevent the need for hospitalization when given time. Hence, increased staffing coupled with more time (i.e. the additional day or two) mean that some hospitalizations can be prevented, such that on net, the effect of increased staffing is to lower hospitalizations.
Comparing the magnitude of the associations across strata dyads in many cases offers further support for these explanations. For example, we find higher effect sizes for employed staff who know the residents better and are, therefore, more likely to ascertain their needs than contract staff. We find higher effect sizes for RNs in nursing homes with higher 5-Star ratings for both the Quality Measures and the Survey, as well as facilities that have higher total nursing levels. The high Medicare facilities, which have more post-acute patients who are more likely to have higher patient acuity and skilled needs that might require rehospitalizations also exhibit larger effects than nursing homes with fewer Medicare patients. Nursing homes with higher census of patients with ADRD diagnoses have lower effect size compared with nursing homes with fewer patients with these diagnoses, possibly reflecting a more judicious approach towards hospital transfer for patients with ADRD, as high quality care practices would suggest. Although another less benign possibility is that residents with ADRD are less likely to express themselves and staff may not recognize the need to hospitalize as often.
We note that the short-term patterns we observe are not likely to be due to long-term staff shortages. Our sensitivity analysis comparing nursing homes with high and low average staffing found the same staffing to hospitalization associations among both, suggesting that long term staffing differences do not explain away these patterns. We also note that we did not to control for turnover because it is likely one of the mechanisms for daily staffing variations, and including it would mask the effect of interest. Future studies examining factors leading to daily staffing patterns should include turnover.
Several limitations of this study should be mentioned. Due to data limitation our estimates of ED transfers were limited to FFS residents only. Second, the associations we found are not necessarily causal; however, we used a strong facility fixed-effects design to control for confounding by all time-invariant facility-level characteristics. Third, our staffing measures are at the facility level and we cannot identify the staff hours received by individual residents or groups of residents, such as those with ADRD, or whether or not residents had private duty nurses or family involvement. Finally, these quantitative data cannot establish the mechanisms driving the associations we find. For example, we did not have data about nurses’ training to start IVs in the nursing home, mange TPN or tube feeding. Furthermore, we focused on staffing only and had no information about availability of other resources such as lab and x-ray results within 4-8 hours; specialists; hospice services; and seven days-per-week therapy services, all of which are considered important for preventing hospitalizations.3
CONCLUSIONS AND IMPLICATIONS
This is the first study, to our knowledge, to examine short-term patterns of staffing in nursing homes and their associations with hospitalizations and ED transfers not followed by a hospitalization. The richness of the PBJ data allowed us to examine daily staffing patterns vis-a-vis daily outcomes and revealed patterns that have not been observed before. Our findings reaffirm the importance of staffing to hospitalization and ED outcomes, even when inspected on a microlevel, and offer a new perspective for understanding the roles of different staffing types. Specifically, our findings suggest that staffing patterns, especially for RNs and LPNs, play a key role in assessing and triaging residents, both in identifying those residents who require immediate hospitalization, thus contributing to the higher number of hospitalization on the same day, and in identifying those where hospitalizations can be averted if appropriate action is taken early enough.
An indirect implication of our study is that a simple count or rate of hospitalizations may not be a good marker for quality, and a more nuanced approach should be considered. The use of hospitalization and rehospitalization rates has become ubiquitous as a quality metric. At the same time, it has long been recognized that some hospitalizations are necessary, and that failing to transfer may be a sign of poor quality. Our study reinforces the need to remember this caveat and continue to refine quality metrics to try to disentangle appropriate and inappropriate transfers.
This study offers new observations about the associations between staffing and hospitalizations. Its strength is its reliance on national data. This, however, is also its weakness. It cannot get into the details of the underlying processes of care, which lead to the outcomes and associations we observe, and some of the questions we raised above. Future studies, relying on other data sources and different methods, should address these questions, as well as the mechanisms leading to daily staffing variations.
Acknowledgments:
Debra Saliba is an employee of the Veterans Administration. The views presented here do not represent those of the Department of Veteran’s Affairs. The sponsor had no role except for funding.
Funding Source:
This work was supported by National Institutes of Health (Grant R01 AG066742). Disclaimer: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG066742. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix
Appendix Table 1:
Full Regression Model of Base Case: Full Sample
Dependent Variable: Number of Hospitalizations from the Nursing Home
Conditional fixed-effects Poisson regression
Number of observations = 14,620,886
Number of groups = 15,718
observations per group:
min = 27
avg = 930.2
max = 1,002
Wald chi2(110) = 11866.77
Log pseudolikelihood = −8927513.8
Prob > chi2 = 0.0000
(Std. err. Adjusted for clustering on id)
| Coefficient | Robust std. err. |
z | P>z | 95% conf. | interval | ||
|---|---|---|---|---|---|---|---|
| RN hours | 0.002795 | 7.79E-05 | 35.87 | <0.001 | 0.002642 | 0.002947 | |
| LPN hours | 0.002603 | 6.94E-05 | 37.48 | <0.001 | 0.002466 | 0.002739 | |
| CAN hours | 0.000774 | 4.62E-05 | 16.76 | <0.001 | 0.000683 | 0.000864 | |
| 1 day lag RN hours | −0.00102 | 6.05E-05 | −16.81 | <0.001 | −0.00114 | −0.0009 | |
| 1 day lag LPN hours | −0.00101 | 5.14E-05 | −19.69 | <0.001 | −0.00111 | −0.00091 | |
| 1 day lag CNA hours | −0.00046 | 3.82E-05 | −11.95 | <0.001 | −0.00053 | −0.00038 | |
| Percent male | 0.003463 | 0.000207 | 16.73 | <0.001 | 0.003058 | 0.003869 | |
| Percent age 65 or less | 0.005515 | 0.000368 | 14.98 | <0.001 | 0.004794 | 0.006236 | |
| pctage65_74 | 0.006117 | 0.000293 | 20.86 | <0.001 | 0.005543 | 0.006692 | |
| pctage75_84 | 0.004348 | 0.000237 | 18.38 | <0.001 | 0.003884 | 0.004811 | |
| Percent Medicare Advantage | −0.00173 | 0.000231 | −7.5 | <0.001 | −0.00218 | −0.00128 | |
| Jan-17 | −0.00582 | 0.017593 | −0.33 | 0.741 | −0.0403 | 0.028666 | |
| Feb-17 | 0.154582 | 0.005393 | 28.67 | <0.001 | 0.144012 | 0.165151 | |
| Mar-17 | 0.174678 | 0.007983 | 21.88 | <0.001 | 0.159032 | 0.190324 | |
| Apr-17 | 0.128258 | 0.00882 | 14.54 | <0.001 | 0.110971 | 0.145545 | |
| May-17 | 0.115096 | 0.008917 | 12.91 | <0.001 | 0.097618 | 0.132573 | |
| Jun-17 | 0.099164 | 0.008807 | 11.26 | <0.001 | 0.081904 | 0.116424 | |
| Jul-17 | 0.065309 | 0.008853 | 7.38 | <0.001 | 0.047958 | 0.082661 | |
| Aug-17 | 0.087147 | 0.008749 | 9.96 | <0.001 | 0.069999 | 0.104295 | |
| Sep-17 | 0.090546 | 0.008594 | 10.54 | <0.001 | 0.073701 | 0.107391 | |
| Oct-17 | 0.096721 | 0.008598 | 11.25 | <0.001 | 0.079868 | 0.113573 | |
| Nov-17 | 0.099547 | 0.008659 | 11.5 | <0.001 | 0.082575 | 0.116518 | |
| Dec-17 | 0.152027 | 0.008327 | 18.26 | <0.001 | 0.135707 | 0.168347 | |
| Jan-18 | 0.231686 | 0.007924 | 29.24 | <0.001 | 0.216155 | 0.247217 | |
| Feb-18 | 0.174271 | 0.007959 | 21.9 | <0.001 | 0.158672 | 0.18987 | |
| Mar-18 | 0.142361 | 0.008027 | 17.74 | <0.001 | 0.126629 | 0.158093 | |
| Apr-18 | 0.122641 | 0.008195 | 14.97 | <0.001 | 0.106579 | 0.138703 | |
| May-18 | 0.093686 | 0.008257 | 11.35 | <0.001 | 0.077503 | 0.109869 | |
| Jun-18 | 0.078696 | 0.008139 | 9.67 | <0.001 | 0.062744 | 0.094648 | |
| Jul-18 | 0.070025 | 0.008036 | 8.71 | <0.001 | 0.054275 | 0.085775 | |
| Aug-18 | 0.083819 | 0.007951 | 10.54 | <0.001 | 0.068236 | 0.099403 | |
| Sep-18 | 0.078109 | 0.007946 | 9.83 | <0.001 | 0.062536 | 0.093683 | |
| Oct-18 | 0.091745 | 0.007728 | 11.87 | <0.001 | 0.076599 | 0.10689 | |
| Nov-18 | 0.07834 | 0.007808 | 10.03 | <0.001 | 0.063037 | 0.093644 | |
| Dec-18 | 0.094132 | 0.007611 | 12.37 | <0.001 | 0.079215 | 0.109049 | |
| Jan-19 | 0.141538 | 0.007398 | 19.13 | <0.001 | 0.127038 | 0.156038 | |
| Feb-19 | 0.142629 | 0.007009 | 20.35 | <0.001 | 0.128893 | 0.156366 | |
| Mar-19 | 0.138552 | 0.006835 | 20.27 | <0.001 | 0.125157 | 0.151948 | |
| Apr-19 | 0.113781 | 0.006824 | 16.67 | <0.001 | 0.100407 | 0.127155 | |
| May-19 | 0.085539 | 0.006785 | 12.61 | <0.001 | 0.072242 | 0.098836 | |
| Jun-19 | 0.061354 | 0.006765 | 9.07 | <0.001 | 0.048094 | 0.074614 | |
| Jul-19 | 0.058282 | 0.006559 | 8.89 | <0.001 | 0.045427 | 0.071138 | |
| Aug-19 | 0.038236 | 0.005584 | 6.85 | <0.001 | 0.027291 | 0.04918 | |
| Major RUG Group |
RUG Code |
Coefficient | Robust std. err. |
z | P>z | 95% conf. | interval |
| Behavioral Symptoms and Cognitive Performance | ba1 | 0.006547 | 0.000531 | 12.33 | <0.001 | 0.005506 | 0.007588 |
| ba2 | 0.004166 | 0.001641 | 2.54 | 0.011 | 0.00095 | 0.007381 | |
| bb1 | 0.008505 | 0.000531 | 16 | <0.001 | 0.007464 | 0.009547 | |
| bb2 | 0.003671 | 0.001543 | 2.38 | 0.017 | 0.000646 | 0.006695 | |
| Clinically Complex | ca1 | 0.010229 | 0.00088 | 11.62 | <0.001 | 0.008504 | 0.011954 |
| ca2 | 0.011779 | 0.001703 | 6.92 | <0.001 | 0.008441 | 0.015117 | |
| cb1 | 0.011881 | 0.000864 | 13.75 | <0.001 | 0.010187 | 0.013575 | |
| cb2 | 0.016374 | 0.003438 | 4.76 | <0.001 | 0.009635 | 0.023113 | |
| cc1 | 0.010164 | 0.000562 | 18.08 | <0.001 | 0.009062 | 0.011266 | |
| cc2 | 0.010332 | 0.002008 | 5.15 | <0.001 | 0.006396 | 0.014267 | |
| cd1 | 0.010293 | 0.000593 | 17.37 | <0.001 | 0.009131 | 0.011455 | |
| cd2 | 0.010185 | 0.001986 | 5.13 | <0.001 | 0.006293 | 0.014077 | |
| ce1 | 0.008007 | 0.000937 | 8.55 | <0.001 | 0.006171 | 0.009844 | |
| ce2 | 0.008822 | 0.003826 | 2.31 | 0.021 | 0.001324 | 0.01632 | |
| Extensive Services | es1 | 0.011822 | 0.001398 | 8.45 | <0.001 | 0.009081 | 0.014562 |
| es2 | 0.010938 | 0.001597 | 6.85 | <0.001 | 0.007807 | 0.014068 | |
| es3 | 0.008712 | 0.001996 | 4.37 | <0.001 | 0.004801 | 0.012624 | |
| Special Care High | hb1 | 0.010922 | 0.000974 | 11.22 | <0.001 | 0.009014 | 0.01283 |
| hb2 | 0.008333 | 0.001727 | 4.82 | <0.001 | 0.004948 | 0.011718 | |
| hc1 | 0.009431 | 0.000878 | 10.74 | <0.001 | 0.00771 | 0.011152 | |
| hc2 | 0.006885 | 0.001626 | 4.23 | <0.001 | 0.003698 | 0.010072 | |
| hd1 | 0.009922 | 0.000776 | 12.79 | <0.001 | 0.008401 | 0.011443 | |
| hd2 | 0.006278 | 0.001619 | 3.88 | <0.001 | 0.003105 | 0.00945 | |
| he1 | 0.010329 | 0.001079 | 9.58 | <0.001 | 0.008214 | 0.012443 | |
| he2 | 0.006903 | 0.002076 | 3.33 | 0.001 | 0.002835 | 0.010971 | |
| Special Care Low | lb1 | 0.015033 | 0.001058 | 14.21 | <0.001 | 0.01296 | 0.017106 |
| lb2 | 0.014114 | 0.003702 | 3.81 | <0.001 | 0.006859 | 0.021369 | |
| lc1 | 0.011452 | 0.000577 | 19.87 | <0.001 | 0.010322 | 0.012582 | |
| lc2 | 0.011764 | 0.002169 | 5.42 | <0.001 | 0.007513 | 0.016014 | |
| ld1 | 0.010339 | 0.000576 | 17.94 | <0.001 | 0.00921 | 0.011468 | |
| ld2 | 0.011236 | 0.001692 | 6.64 | <0.001 | 0.007919 | 0.014553 | |
| le1 | 0.009884 | 0.000764 | 12.93 | <0.001 | 0.008386 | 0.011382 | |
| le2 | 0.007856 | 0.002206 | 3.56 | <0.001 | 0.003532 | 0.01218 | |
| Reduced Physical Functioning | pa1 | 0.00777 | 0.00052 | 14.95 | <0.001 | 0.006751 | 0.008788 |
| pa2 | 0.008026 | 0.001431 | 5.61 | <0.001 | 0.005222 | 0.010831 | |
| pb1 | 0.007634 | 0.000539 | 14.15 | <0.001 | 0.006577 | 0.008691 | |
| pb2 | 0.008797 | 0.001105 | 7.96 | <0.001 | 0.006631 | 0.010963 | |
| pc1 | 0.008381 | 0.00045 | 18.64 | <0.001 | 0.0075 | 0.009263 | |
| pc2 | 0.00676 | 0.000747 | 9.05 | <0.001 | 0.005297 | 0.008224 | |
| pd1 | 0.0084 | 0.000413 | 20.32 | <0.001 | 0.007589 | 0.00921 | |
| pd2 | 0.00553 | 0.000874 | 6.33 | <0.001 | 0.003817 | 0.007243 | |
| pe1 | 0.006693 | 0.000671 | 9.98 | <0.001 | 0.005378 | 0.008008 | |
| pe2 | 0.004636 | 0.001325 | 3.5 | <0.001 | 0.002039 | 0.007233 | |
| Rehab and Rehab Plus Extensive | rha | 0.008448 | 0.000604 | 13.98 | <0.001 | 0.007264 | 0.009633 |
| rhb | 0.011513 | 0.000632 | 18.22 | <0.001 | 0.010274 | 0.012751 | |
| rhc | 0.011504 | 0.000568 | 20.26 | <0.001 | 0.010391 | 0.012617 | |
| rhl | 0.016735 | 0.003125 | 5.35 | <0.001 | 0.010609 | 0.022861 | |
| rhx | 0.017419 | 0.002393 | 7.28 | <0.001 | 0.012729 | 0.022108 | |
| rla | 0.007349 | 0.000721 | 10.19 | <0.001 | 0.005935 | 0.008762 | |
| rlb | 0.008029 | 0.000986 | 8.14 | <0.001 | 0.006097 | 0.009961 | |
| rlx | 0.015218 | 0.004622 | 3.29 | 0.001 | 0.006159 | 0.024276 | |
| rma | 0.007689 | 0.000466 | 16.49 | <0.001 | 0.006775 | 0.008603 | |
| rmb | 0.009195 | 0.00043 | 21.38 | <0.001 | 0.008352 | 0.010038 | |
| rmc | 0.009279 | 0.000433 | 21.43 | <0.001 | 0.008431 | 0.010128 | |
| rml | 0.013684 | 0.00393 | 3.48 | <0.001 | 0.005982 | 0.021386 | |
| rmx | 0.007214 | 0.003217 | 2.24 | 0.025 | 0.000909 | 0.013519 | |
| rua | 0.010369 | 0.000443 | 23.42 | <0.001 | 0.009501 | 0.011236 | |
| rub | 0.009272 | 0.000424 | 21.86 | <0.001 | 0.008441 | 0.010103 | |
| ruc | 0.011112 | 0.000476 | 23.35 | <0.001 | 0.01018 | 0.012045 | |
| rul | 0.015571 | 0.002003 | 7.78 | <0.001 | 0.011646 | 0.019496 | |
| rux | 0.012584 | 0.002795 | 4.5 | <0.001 | 0.007106 | 0.018063 | |
| rva | 0.01164 | 0.00059 | 19.73 | <0.001 | 0.010484 | 0.012796 | |
| rvb | 0.012082 | 0.000608 | 19.86 | <0.001 | 0.01089 | 0.013274 | |
| rvc | 0.013594 | 0.000609 | 22.32 | <0.001 | 0.012401 | 0.014788 | |
| rvl | 0.025555 | 0.002493 | 10.25 | <0.001 | 0.020668 | 0.030441 | |
| rvx | 0.021725 | 0.001883 | 11.54 | <0.001 | 0.018034 | 0.025416 | |
| Unknown | 0.032939 | 0.002768 | 11.9 | 0 | <0.001 | 0.038364 | |
Appendix Table 2:
Sensitivity Analysis Summary of Findings: – Percent Change in Daily Hospitalizations Due to an Increase of a One Full Time Equivalent Staff Position*
| Same Day | Previous Day | |||||
|---|---|---|---|---|---|---|
| RNs | LPNs | CNAs | RNs | LPNs | CNAs | |
| Models Estimated on Stratified Samples | ||||||
| Midweek days only | ||||||
|
1.0%
[0.9, 1.1] (<.001) |
1.0%
[0.9, 1.1] (<.001) |
0.0%
[−0.0, 0.1] (0.698) |
−0.5%
[−0.6, −0.4] (<.001) |
−0.4%
[−0.5, −0.3] (<.001) |
−0.0% [−0.1, 0.0] (0.148) |
|
| NH Quality measured by 5 Star QMs | ||||||
| High Average Quality 5-Star Rating (70th percentile) |
2.5%
[2.2, 2.7] (<.001) |
2.2%
[1.9, 2.5] (<.001) |
0.5%
[0.3, 0.7] (<.001) |
−0.9%
[−1.1, −0.7] (<.001) |
−0.8%
[−1.0, −0.6] (<.001) |
−0.3%
[−0.4, −0.1] (<.001) |
| Low Average Quality 5-Star Rating (30th percentile) |
2.1%
[1.9, 2.3] (<.001) |
2.1%
[1.9, 2.3] (<.001) |
0.9%
[0.8, 1.0] (<.001) |
−0.8%
[−1.0, −0.6] (<.001) |
−0.9%
[−1.1, −0.8] (<.001) |
−0.4%
[−0.5, −0.3] (<.001) |
| NH Quality measured by 5 Star Survey | ||||||
| High Average Survey 5-Star Rating (70th percentile) |
2.4%
[2.1, 2.8] (<.001) |
2.2%
[1.9, 2.5] (<.001) |
0.5%
[0.3, 0.8] (<.001) |
−0.8%
[−1.0, −0.6] (<.001) |
−0.8%
[−1.1, −0.6] (<.001) |
−0.3%
[−0.5, −0.2] (<.001) |
| Low Average Survey 5-Star Rating (30th percentile) |
2.3%
[2.1, 2.6] (<.001) |
2.2%
[2.0, 2.4] (<.001) |
0.7%
[0.6, 0.8] (<.001) |
−0.9%
[−1.1, −0.8] (<.001) |
−0.9%
[−1.0, −0.8] (<.001) |
−0.4%
[−0.5, −0.3] (<.001) |
| Total nursing level variations | ||||||
| High Average Nursing Level (85th percentile) |
2.2%
[1.9, 2.5] (<.001) |
1.8%
[1.6, 2.1] (<.001) |
0.3%
[0.1, 0.5] (<.001) |
−0.8%
[−0.9, −0.6] (<.001) |
−0.7%
[−0.9, −0.5] (<.001) |
−0.2%
[−0.3, −0.1] (0.004) |
| Low Average Nursing Level (15th percentile) |
2.1%
[1.7, 2.4] (<.001) |
2.3%
[1.9, 2.7] (<.001) |
1.0%
[0.7, 1.2] (<.001) |
−0.9%
[−1.3, −0.6] (<.001) |
−0.9%
[−1.2, −0.6] (<.001) |
−0.7%
[−0.9, −0.5] (<.001) |
| Hospitalization level variations | ||||||
| High Hospitalization Rate (85th percentile) |
2.5%
[2.2, 2.7] (<.001) |
2.4%
[2.2, 2.6] (<.001) |
0.7%
[0.5, 0.8] (<.001) |
−1.0%
[−1.2, −0.8] (<.001) |
−1.0%
[−1.2, −0.9] (<.001) |
−0.5%
[−0.6, −0.4] (<.001) |
| Low Hospitalization Rate (15th percentile) |
1.9%
[1.3, 2.5] (<.001) |
1.6%
[1.2, 2.0] (<.001) |
0.5%
[0.3, 0.6] (<.001) |
−0.3%
[−0.6, −0.1] (0.013) |
−0.2%
[−0.4, 0.1] (0.226) |
−0.3%
[−0.5, −0.1] (0.001) |
| High versus low Medicare census nursing homes | ||||||
| High Medicare facilities (85th percentile) only |
2.5%
[2.2, 2.8] (<.001) |
2.3%
[2.0, 2.6] (<.001) |
0.5%
[0.1, 0.8] (0.004) |
−0.9%
[−1.1, −0.7] (<.001) |
−0.9%
[−1.1, −0.7] (<.001) |
−0.4%
[−0.7, −0.2] (<.001) |
| Low Medicare facilities (15th percentile) only |
1.9%
[1.5, 2.3] (<.001) |
1.7%
[1.4, 2.1] (<.001) |
0.6%
[0.5, 0.8] (<.001) |
−0.5%
[−0.8, −0.4] (<.001) |
−0.6%
[−0.8, −0.4] (<.001) |
−0.3%
[−0.5, −0.2] (<.001) |
| High versus low Medicaid census nursing homes | ||||||
| High Medicaid facilities (70th percentile) only |
2.1%
[1.9, 2.4] (<.001) |
2.2%
[1.9, 2.4] (<.001) |
0.8%
[0.7, 0.9] (<.001) |
−0.7%
[−0.9, −0.5] (<.001) |
−0.8%
[−0.9, −0.6] (<.001) |
−0.4%
[−0.5, −0.3] (<.001) |
| Low Medicaid facilities (30th percentile) only |
2.3%
[2.1, 2.5] (<.001) |
2.1%
[1.9, 2.3] (<.001) |
0.4%
[0.3, 0.6] (<.001) |
−0.8%
[−1.0, −0.6] (<.001) |
−0.7%
[−0.9, −0.6] (<.001) |
−0.3%
[−0.4, −0.2] (<.001) |
| High Medicaid facilities (85th percentile) only |
1.9%
[1.6, 2.3] (<.001) |
2.0%
[1.7, 2.3] (<.001) |
0.8%
[0.6, 0.9] (<.001) |
−0.8%
[−1.0, −0.5] (<.001) |
−0.8%
[−1.0, −0.6] (<.001) |
−0.3%
[−0.4, −0.1] (<.001) |
| Low Medicaid facilities (15th percentile) only |
2.2%
[1.8, 2.6] (<.001) |
2.00%
[1.7, 2.3] (<.001) |
0.3%
[0.1, 0.6] (0.013) |
−0.9%
[−1.2, −0.6] (<.001) |
−0.9%
[−1.1, −0.7] (<.001) |
−0.2%
[−0.4, −0.0] (0.014) |
| Nursing homes with high and low percent of patients with Alzheimer Disease and Associated Dementias (ADRD) and Cognitive Impairment | ||||||
| High ADRD (85th percentile) |
2.1%
[1.9, 2.4] (<.001) |
2.3%
[2.0, 2.6] (<.001) |
0.6%
[0.4, 0.7] (<.001) |
−0.6%
[−0.8, −0.4] (<.001) |
−0.7%
[−0.9, −0.5] (<.001) |
−0.4%
[−0.5, −0.2] (<.001) |
| Low ADRD (15th percentile) |
2.8%
[2.6, 3.1] (<.001) |
2.5%
[2.2, 2.8] (<.001) |
0.9%
[0.7, 1.0] (<.001) |
−1.1%
[−1.3, −0.9] (<.001) |
−1.0%
[−1.2, −0.9] (<.001) |
−0.6%
[−0.8, −0.5] (<.001) |
Each line reports findings from a separate regression model which also controls for age, gender, case mix, seasonality and facility fixed effects. Models differ by either staffing variables (e.g. salaried vs. contract), or facility characteristics (e.g. low quality vs. high quality) and sample (full and stratified). Bolded entries are those significant at the p<0.001.
Footnotes
To calculate this percent we used the formula %ΔE(y∣x) = 100*(exp(β*Δx) where %ΔE(y∣x)= expected % change in daily hospitalizations.
Conflicts of Interest: None of the authors have any conflict of interest.
Contributor Information
Dana B. Mukamel, Department of Medicine, Division of General Internal Medicine; University of California, Irvine 100 Theory, Suite 120, Irvine, CA 92617-3056.
Debra Saliba, University of California Los Angeles Borun Center at David Geffen School of Medicine, 10945 Le Conte Ave., Suite 2339, Los Angeles, CA 90095-1687; Veterans Administration GRECC, Los Angeles, CA; RAND Health, Santa Monica, CA.
Heather Ladd, Department of Medicine, Division of General Internal Medicine; iTEQC Research Program; University of California, Irvine; 100 Theory, Suite 120, Irvine, CA 92617-3056.
R. Tamara Konetzka, Department of Public Health Sciences, The University of Chicago, 5841 South Maryland Ave MC2000, Chicago, IL 60637–1447.
References
- 1.Creditor MC. Hazards of hospitalization of the elderly. Annals of internal medicine. 1993;118(3):219–223. [DOI] [PubMed] [Google Scholar]
- 2.Dwyer R, Gabbe B, Stoelwinder JU, Lowthian J. A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age and ageing. 2014;43(6):759–766. [DOI] [PubMed] [Google Scholar]
- 3.Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs: [see editorial comments by Drs. Jean F. Wyman and William R. Hazzard, pp 760-761]. Journal of the American Geriatrics Society. 2010;58(4):627–635. [DOI] [PubMed] [Google Scholar]
- 4.CMS.gov. Nursing Home Value-Based Purchasing Demonstration. 2009; https://innovation.cms.gov/innovation-models/nursing-home-value-based-purchasing. Accessed November 24, 2021.
- 5.CMS.gov. Nursing Homes - Quality of Resident Care. https://data.cms.gov/provider-data/topics/nursing-homes/quality-of-resident-care/#quality-of-resident-care-data-collection-periods. Accessed November 24, 2021.
- 6.Saliba D, Weimer DL, Shi Y, Mukamel DB. Examination of the New Short-Stay Nursing Home Quality Measures: Rehospitalizations, Emergency Department Visits, and Successful Returns to the Community. Inquiry. 2018;Jan-Dec(55):46958018786816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laging B, Ford R, Bauer M, Nay R. A meta-synthesis of factors influencing nursing home staff decisions to transfer residents to hospital. Journal of advanced nursing. 2015;71(10):2224–2236. [DOI] [PubMed] [Google Scholar]
- 8.Backhaus R, Verbeek H, van Rossum E, Capezuti E, Hamers JP. Nurse staffing impact on quality of care in nursing homes: a systematic review of longitudinal studies. Journal of the American Medical Directors Association. 2014;15(6):383–393. [DOI] [PubMed] [Google Scholar]
- 9.Spilsbury K, Hewitt C, Stirk L, Bowman C. The Relationship Between Nurse Staffing And Quality Of Care In Nursing Homes: A Systematic Review. International journal of nursing studies. 2011;48(6):732–750. [DOI] [PubMed] [Google Scholar]
- 10.Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors Of Nursing Home Hospitalization: A Review Of The Literature. Medical care research and review : MCRR. 2008;65(1):3–39. [DOI] [PubMed] [Google Scholar]
- 11.Castle NG. Nursing Home Caregiver Staffing Levels and Quality of Care: A Literature Review. Journal of Applied Gerontology. 2008;27(4):375–405. [Google Scholar]
- 12.Bostick JE, Rantz MJ, Flesner MK, Riggs CJ. Systematic review of studies of staffing and quality in nursing homes. Journal of the American Medical Directors Association. 2006;7(6):366–376. [DOI] [PubMed] [Google Scholar]
- 13.Kash BA, Hawes C, Phillips CD. Comparing Staffing Levels in the Online Survey Certification and Reporting (OSCAR) System with the Medicaid Cost Report Data: Are Differences Systematic? The Gerontologist. 2007;47(4):480–489. [DOI] [PubMed] [Google Scholar]
- 14.Feng Z, Katz PR, Intrator O, Karuza J, Mor V. Physician and nurse staffing in nursing homes: the role and limitations of the Online Survey Certification and Reporting (OSCAR) system. Journal of the American Medical Directors Association. 2005;6(1):27–33. [DOI] [PubMed] [Google Scholar]
- 15.LTC Focus Brown University. Facts on Care in the US - Create Custom Reports on Long-Term Care. https://ltcfocus.org/. Accessed May 11, 2022. [Google Scholar]
- 16.Centers for Medicare & Medicaid Services. Design for Care Compare Nursing Home Five-Star Quality Rating System: Technical Users’ Guide- January 2022; January https://www.cms.gov/medicare/provider-enrollment-and-certification/certificationandcomplianc/downloads/usersguide.pdf. Accessed March 31, 2022. [Google Scholar]