Abstract
While hypothyroidism increases serum creatinine (Cr) levels, it is uncertain whether the elevation is mediated via a decline in the glomerular filtration rate (GFR) or the reflection of enhanced Cr production from the muscles or both. In the present study, we explored an association between urinary Cr excretion rate (CER) and hypothyroidism. A total of 553 patients with chronic kidney disease were enrolled in a cross-sectional study. Multiple linear regression analysis was performed to explore the association between hypothyroidism and urinary CER. The mean urinary CER was 1.01 ± 0.38 g/day and 121 patients (22%) had hypothyroidism. The multiple linear regression analysis revealed explanatory variables with urinary CER, including age, sex, body mass index, 24 h Cr clearance (24hrCcr), and albumin while hypothyroidism was not considered an independent explanatory variable. In addition, scatter plot analysis with regression fit line representing the association between estimated GFR calculated using s-Cr (eGFRcre) and 24hrCcr revealed that eGFRcre and 24hrCcr had strong correlations with each other in hypothyroid patients as well as euthyroid patients. Collectively, hypothyroidism was not considered an independent explanatory variable for urinary CER in the present study and eGFRcre is a useful marker to evaluate kidney function regardless of the presence of hypothyroidism.
Keywords: hypothyroidism, kidney function, urinary creatinine excretion
1. Introduction
It is well known that there is a strong interaction between thyroid function and kidney function [1]. An elevation in serum creatinine (s-Cr) levels is reported to be seen in hypothyroidism [2], and the replacement of thyroid hormone reversed the elevation of s-Cr levels. Similarly, a decline in s-Cr levels is observed in hyperthyroidism, and reversal of s-Cr can be seen after the normalization of thyroid function [3], suggesting that thyroid function affects s-Cr levels. While details of the mechanisms are still uncertain, it is suggested that hypothyroidism may cause renal dysfunction by the following mechanisms: reduced renal perfusion pressure through the decrease in cardiac output and the increase in vascular resistance [4,5], reduced sensitivity to the body’s sympathetic drive and renin–angiotensin–aldosterone system activity [6], and possible rhabdomyolysis [7].
However, it is still controversial whether thyroid function really regulates the glomerular filtration rate (GFR). While previous reports indicated decreased creatinine clearance in hypothyroidism [8], other reports suggested that increased s-Cr levels under hypothyroidism might be just the reflection of increased creatinine (Cr) production from the muscles independent of the GFR [9,10]. These mechanisms may include the following increased processes such as (1) synthesis of creatine, (2) storage of creatine in the muscle, (3) creatine–phosphocreatine cycle, (4) conversion of creatine or phosphocreatine into Cr, and (5) release of Cr from muscle tissue due to myopathy and/or rhabdomyolysis [9,10]. Indeed, serum levels of muscle enzymes including creatine phosphokinase have been reported to be increased in hypothyroidism [11]. What happens if hypothyroidism increases Cr production? Since the Cr production should equal urinary Cr excretion when the s-Cr levels are in a steady state [12], the increase in Cr production results in the increase in s-Cr levels independent of the GFR. In this situation, the estimated GFR calculated using s-Cr (eGFRcre) may not be a reliable measurement for kidney function. In contrast, 24 h Cr clearance (24hrCcr) levels are not affected by Cr production levels. Cystatin C (CysC), another marker of kidney function, has advantages for patients with muscle weakness since the evaluation is independent of muscle mass [13]. Since hypothyroidism reduces CysC production through a metabolic-rate-mediated mechanism [14] and treatment for hypothyroidism affects serum CysC levels [15], CysC is proposed as a possible biomarker for monitoring hypothyroidisms [16].
Since most of the previous reports analyzed the association between hypothyroidism and kidney function by eGFRcre [17,18,19], it is currently uncertain how hypothyroidism increases s-Cr levels, via an increase in urinary Cr excretion rate (CER) or a decrease in GFR, or both. In the present study, we conducted a cross-sectional study to evaluate the association between hypothyroidism and urinary CER.
2. Materials and Methods
2.1. Study Design and Participants
We retrospectively reviewed patients with a measurement of 24 h urine collection while hospitalized in the division of kidney, diabetes, and endocrine diseases at Okayama University Hospital. Data from 2006 to 2019 were collected from electronic-based records. Data collection was completed in 2020–2021. Our database of medical records provided 18,068 patients. Among these patients, we collected 629 patients with all the following data of the measurements of s-Cr, 24hrCcr, thyroid-stimulating hormone (TSH), free thyroxine (FT4), free triiodothyronine (FT3), 24 h urinary protein and Cr, total cholesterol, serum albumin, CysC, and glycated hemoglobin (HbA1c). We extracted 566 hypothyroid and euthyroid patients after excluding hyperthyroid and central hypothyroid patients. Other exclusion criteria were as follows: (1) age <18 years, (2) on dialysis, and (3) post-kidney transplantation. Consequently, 553 patients with chronic kidney disease were enrolled for a cross-sectional analysis (shown in Figure 1). The study was approved by the ethics committees of Okayama University Hospital Institutional Review Board (accredited ISO9001/2000), approved number (OKU-206-022). This study also followed the Declaration of Helsinki on medical protocol and ethics. As for informed consent, the contents of the research were posted on our department homepage and the hospital, and public informed consent was provided. As this is a cross-sectional study, the committee approved public informed consent.
Figure 1.
Flow diagram of the screening and enrollment of study patients.
2.2. Data Collection
The following clinicopathologic characteristics were collected at the time of the hospitalization: age, sex, body mass index (BMI), and the use of glucocorticoid, levothyroxine, angiotensin-converting-enzyme inhibitor (ACE-i), and angiotensin II receptor blocker (ARB). HbA1c data are presented as National Glycohemoglobin Standardization Program values according to the recommendations of the Japanese Diabetes Society and International Federation of Clinical Chemistry [20]. eGFRcre was evaluated by the equation developed by the Japanese Society of Nephrology (eGFRcre (mL/min/1.73 m2) = 194 × s-Cr (mg/dL)−1.094 × Age−0.287 (× 0.739 for females)) [21]. While the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [22] or the Modification of Diet in Renal Disease (MDRD) study equation is applied for eGFR calculation worldwide [23], it is reported that these equations tend to overestimate Japanese kidney function [24,25]. Since all the patients enrolled were Japanese, we applied the modified equation for Japanese in the study, which is widely used in Japan [21]. Nephrotic syndrome (NS) was defined by both substantial proteinuria (>3.5 g/24 h) and hypoalbuminemia (<3.0 g/dL). The 24hrCcr was calculated by: 24hrCcr (mL/min) = 24 h urinary Cr (mg/dL) × 24 h collected urine (mL/day)/24 (hour)/60 (min)/s-Cr (mg/dL) × 1.73/BSA. BSA was calculated by: BSA (m2) = body weight0.425 × height0.725 × 0.007184 [26]. Participants collected 24 h urine accurately, supervised by nurses in the hospital. Urine volume was recorded (mL), and Cr was measured by the enzyme method. Urinary CER was calculated by: urinary CER (g/day) = urine volume (mL/day) x urinary Cr (mg/dL)/105. Thyroid function was measured by using an electrochemiluminescence assay (Roche Diagnostics K.K., Cobas® 8000). The normal reference range in our institute for TSH was 0.27–4.2 µIU/mL, FT4 was 0.93–1.7 ng/dL, and FT3 was 2.3–4.0 pg/mL. In this study, hypothyroidism was defined as combined overt hypothyroidism (FT4 < 0.93 ng/dL and TSH > 4.2 µIU/L) and subclinical hypothyroidism (0.93 ≤ FT4 ≤ 1.7 ng/dL and TSH > 4.2 µIU/mL) like the previous reports [27,28]. Euthyroidism was defined as the status with normal TSH and FT4 regardless of their current or history of thyroidal diseases.
2.3. Statistical Analysis
The statistical analyses were performed by JMP version 14.0.0 (SAS Institute, Inc, Cary, NC, USA) and Stata/SE version 16.1 (Stata Corp LLC, College Station, TX, USA). Significance was defined as p-values less than 0.05. Data were expressed as n (%) for categorical variables and mean ± standard deviation (SD) for continuous variables. Categorical variables were analyzed with the chi-square test, while continuous variables were compared by using the student’s t-test or Mann–Whitney U test as appropriate. Correlations among urinary CER and continuous variables (age, eGFRcre, BMI, 24hrCcr, FT4, TSH, and FT3) were evaluated by Spearman’s correlation analysis. Multiple linear regression analysis was performed to explore the association of variates with urinary CER. For the analysis, candidate variables contained hypothyroidism, sex, age, BMI, and 24hrCcr. Correlations among 24hrCcr and eGFRcre under euthyroidism and hypothyroidism were evaluated by Spearman’s correlation analysis. p for trend was calculated by the Cochran–Armitage trend test or the Jonckheere–Terpstra test.
3. Results
3.1. Study Population and Clinical Characteristics
Among 629 patients in all the data sets, 553 patients met the selection criteria and were enrolled for the analysis (Figure 1). There were no patients with acute kidney injury or rhabdomyolysis. The characteristics of the participants stratified by tertiles of urinary CER are shown in Table 1. The average age was 60 ± 15 years and 52% of the patients were men. The average level of eGFRcre and 24hrCcr was 55.7 ± 30.5 mL/min/1.73 m2 and 64.6 ± 38.4 mL/min, respectively. The average urinary CER was 1.01 ± 0.38 g/day. Trend analyses revealed that patients showed higher 24hCCr, eGFRcre, albumin, hemoglobin, and FT3 levels (all the p-value for trends <0.001), younger age (p-value for trends <0.001), higher proportion of male gender (p-value for trends <0.001), higher BMI (p-value for trends <0.001), and lower proportion of hypothyroidism (p-value for trends 0.016) with higher urinary CER. To analyze the association between hypothyroidism and urinary CER, we stratified the patients by the presence or absence of hypothyroidism (Table 2). The number of participants with hypothyroidism and euthyroidism were 121 and 432, respectively. Patients with hypothyroidism had higher levels of s-Cr and urinary protein, had NS more frequently, and received more ACE-i/ARB agents. Patients with hypothyroidism also had lower eGFRcre, 24hrCcr, urinary CER, serum albumin, and HbA1c levels.
Table 1.
Characteristics of study participants stratified by tertiles of urinary creatinine excretion.
| Clinical Parameters | All Participants (n = 553) |
Low CER (n = 184) |
Middle CER (n = 184) |
High CER (n = 185) |
p for Trend |
|---|---|---|---|---|---|
| Sex (Male), n (%) | 285 (52) | 61 (33) | 83 (45) | 141 (76) | <0.001 ** |
| Age (yr) | 60 ± 15 | 65 ± 15 | 61 ± 14 | 55 ± 14 | <0.001 ** |
| BMI (kg/m2) | 24.3 ± 4.8 | 22.3 ± 3.9 | 24.6 ± 4.3 | 26.1 ± 5.4 | <0.001 ** |
| TSH (µU/mL) | 4.88 ± 15.97 | 5.54 ± 13.99 | 4.29 ± 11.33 | 4.81 ± 21.03 | 0.004 ** |
| FT4 (ng/dL) | 1.19 ± 0.21 | 1.17 ± 0.22 | 1.17 ± 0.19 | 1.22 ± 0.20 | 0.052 |
| FT3 (pg/mL) | 2.49 ± 0.60 | 2.27 ± 0.67 | 2.50 ± 0.49 | 2.72 ± 0.53 | <0.001 ** |
| Hypothyroidism n (%) | 121 (22) | 48 (26) | 44 (24) | 29 (16) | 0.016 * |
| s-Cr (mg/dL) | 1.44 ± 1.27 | 1.62 ± 1.41 | 1.44 ± 1.37 | 1.26 ± 0.97 | 0.826 |
| eGFRcre (mL/min/1.73 m2) | 55.7 ± 30.5 | 51.5 ± 35.8 | 55.2 ± 27.7 | 60.4 ± 26.9 | <0.001 ** |
| 24hrCcr (mL/min) | 64.6 ± 38.4 | 45.3 ± 31.1 | 64.9 ± 32.8 | 83.7 ± 40.7 | <0.001 ** |
| Urinary output (mL/day) | 1665 ± 710 | 1447 ± 617 | 1674 ± 674 | 1873 ± 769 | <0.001 ** |
| Urinary CER (g/day) | 1.01 ± 0.38 | 0.64 ± 0.14 | 0.97 ± 0.07 | 1.42 ± 0.31 | <0.001 ** |
| Urinary protein (g/day) | 2.1 ± 6.7 | 1.7 ± 3.9 | 2.5 ± 9.0 | 2.3 ± 6.3 | 0.562 |
| Albumin (g/dL) | 3.6 ± 0.8 | 3.4 ± 0.8 | 3.6 ± 0.8 | 3.8 ± 0.8 | <0.001 ** |
| Hemoglobin (g/dL) | 12.3 ± 2.3 | 11.6 ± 2.3 | 12.2 ± 2.1 | 13.2 ± 2.4 | <0.001 ** |
| Total cholesterol (mg/dL) | 196 ± 62 | 192 ± 63 | 196 ± 62 | 200 ± 60 | 0.134 |
| HbA1c (%) | 7.1 ± 2.0 | 6.9 ± 2.0 | 7.2 ± 2.1 | 7.1 ± 2.1 | 0.370 |
| Nephrotic syndrome n (%) | 52 (9) | 19 (10) | 20 (11) | 13 (7) | 0.277 |
| ACE-i/ARB intake n (%) | 128 (23) | 40 (22) | 42 (23) | 46 (25) | 0.477 |
| Levothyroxine intake n (%) | 55 (10) | 23 (13) | 18 (10) | 14 (8) | 0.114 |
| Glucocorticoid intake n (%) | 26 (5) | 13 (7) | 5 (3) | 8 (4) | 0.215 |
BMI, body mass index; TSH, thyroid-stimulating hormone; FT4, free thyroxine; FT3, free triiodothyronine; s-Cr, serum creatinine; eGFRcre, estimated glomerular filtration rate calculated by serum creatinine; 24hrCcr, 24 h creatinine clearance; urinary CER, urinary creatinine excretion rate; HbA1c, glycated hemoglobin; ACE-i, angiotensin-converting-enzyme inhibitor; ARB, angiotensin II receptor blocker. p for trend was calculated by the Cochran–Armitage trend test or the Jonckheere–Terpstra test. * p < 0.05, ** p < 0.01.
Table 2.
Characteristics of study participants stratified by thyroidal status.
| Clinical Parameters | All Participants (n = 553) |
Hypothyroidism (n = 121) |
Euthyroidism (n = 432) |
p-Value |
|---|---|---|---|---|
| Sex (Male), n (%) | 285 (52) | 66 (55) | 219 (51) | 0.454 |
| Age (yr) | 60 ± 15 | 63 ± 16 | 59 ± 15 | 0.224 |
| BMI (kg/m2) | 24.3 ± 4.8 | 24.8 ± 6.0 | 24.2 ± 4.8 | 0.208 |
| TSH (µIU/mL) | 4.88 ± 15.97 | 15.74 ± 31.91 | 1.84 ± 15.97 | <0.001 ** |
| FT4 (ng/dL) | 1.19 ± 0.21 | 1.03 ± 0.26 | 1.23 ± 0.16 | <0.001 ** |
| FT3 (pg/mL) | 2.49 ± 0.60 | 2.25 ± 0.73 | 2.56 ± 0.53 | <0.001 ** |
| s-Cr (mg/dL) | 1.44 ± 1.27 | 2.14 ± 1.67 | 1.24 ± 1.06 | <0.001 ** |
| Cystatin C (mg/L) | 1.66 ± 1.06 | 2.21 ± 1.17 | 1.51 ± 0.98 | <0.001 ** |
| eGFRcre (mL/min/1.73 m2) | 55.7 ± 30.5 | 38.9 ± 26.0 | 60.5 ± 30.1 | <0.001 ** |
| 24hrCcr (mL/min) | 64.6 ± 38.4 | 41.4 ± 29.9 | 71.2 ± 38.0 | <0.001 ** |
| Urinary output (mL/day) | 1665 ± 710 | 1579 ± 745 | 1689 ± 699 | 0.134 |
| Urinary CER (g/day) | 1.01 ± 0.38 | 0.91 ± 0.35 | 1.04 ± 0.38 | 0.001 ** |
| Urinary protein (g/day) | 2.1 ± 6.7 | 3.5 ± 5.7 | 1.8 ± 7.0 | <0.001 ** |
| Albumin (g/dL) | 3.6 ± 0.8 | 3.2 ± 1.0 | 3.7 ± 0.7 | <0.001 ** |
| Hemoglobin (g/dL) | 12.3 ± 2.3 | 12.0 ± 2.4 | 12.5 ± 2.3 | 0.042 * |
| Total cholesterol (mg/dL) | 196 ± 62 | 204 ± 72 | 194 ± 59 | 0.110 |
| HbA1c (%) | 7.1 ± 2.0 | 6.5 ± 1.6 | 7.2 ± 2.1 | <0.001 ** |
| Nephrotic syndrome n (%) | 52 (9) | 25 (21) | 27 (6) | <0.001 ** |
| ACE-i/ARB intake n (%) | 128 (23) | 40 (33) | 88 (20) | 0.003 ** |
| Levothyroxine intake n (%) | 55 (10) | 34 (28) | 21 (5) | <0.001 ** |
| Glucocorticoid intake n (%) | 26 (5) | 7 (6) | 19 (4) | 0.524 |
BMI, body mass index; TSH, thyroid-stimulating hormone; FT4, free thyroxine; FT3, free triiodothyronine; s-Cr, serum creatinine; eGFRcre, estimated glomerular filtration rate calculated by serum creatinine; 24hrCcr, 24 h creatinine clearance; urinary CER, urinary creatinine excretion rate; HbA1c, glycated hemoglobin; ACE-i, angiotensin-converting-enzyme inhibitor; ARB, angiotensin II receptor blocker. p-values were obtained by Student’s t-test or Mann–Whitney U test or Pearson’s chi-square test. * p < 0.05, ** p < 0.01.
3.2. Hypothyroidism Is Not an Independent Explanatory Variable for Urinary CER
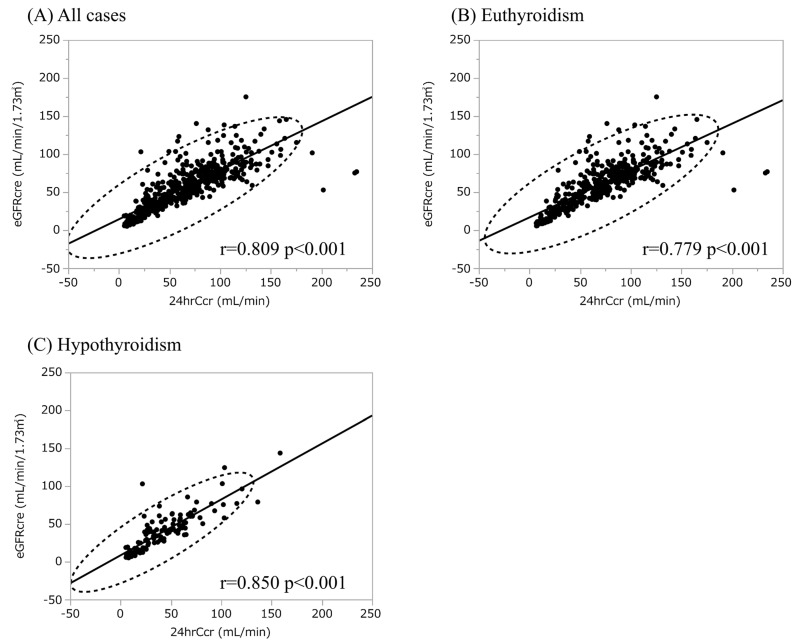
To explore whether thyroid function affects Cr production, we compared the urinary CER between euthyroidism and hypothyroidism (Table 2). The urinary CER was rather lower in hypothyroid patients compared with the levels in euthyroid patients. The enrolled patients with hypothyroidism showed lower kidney function and protein-energy wasting syndrome, i.e., lower skeletal muscle mass, which may contribute to reduced urinary CER [29,30,31]. We next conducted scatter plot analysis to explore the association between urinary CER with variables, which revealed a weak positive correlation with 24hrCcr while there was no apparent correlation with age, BMI, FT3, FT4, and TSH (Figure 2). Male patients had higher urinary CER compared with female patients, compatible with the previous report (Figure 2). To further analyze the explanatory variables for urinary CER, univariate and multiple linear regression analyses were applied (Table 3 and Table 4), in which age, sex, BMI 24hrCcr, and albumin were detected as an independent explanatory variable for urinary CER while neither hypothyroidism nor FT3 was detected. Because both thyroid function and renal function are affected by NS [32], we also conducted the analyses using the data excluding patients with NS. The characteristics of the participants without NS stratified by thyroid function and the results of multiple linear regression analyses are shown in the Supplementary Materials, Tables S1 and S2, respectively, in which neither hypothyroidism nor FT3 was detected as an independent explanatory variable for urinary CER. Collectively, it is unlikely that an increase in s-Cr is also mediated by increased Cr production due to hypothyroidism, suggesting that eGFRcre is a reliable marker to evaluate kidney function even under hypothyroidism. To further evaluate the reliability of eGFRcre under hypothyroidism, we conducted scatter plot analysis with a regression fit line representing the association between eGFRcre and 24hrCcr under the categories of thyroid function (Figure 3), which revealed that eGFR and 24hrCcr had strong correlations with each other in hypothyroid patients as well as euthyroid patients (r = 0.850; p < 0.001 and r = 0.779; p < 0.001, respectively).
Figure 2.
The association between urinary creatinine excretion rate and variables. Urinary CER, urinary creatinine excretion rate; eGFRcre, estimated glomerular filtration rate calculated by serum creatinine; BMI, body mass index; 24hrCcr, 24 h creatinine clearance; FT4, free thyroxine; TSH, thyroid-stimulating hormone; FT3, free triiodothyronine.
Table 3.
Univariate regression analysis of urinary creatinine excretion rate and variables.
| Variable | B | 95% CI | β | t | p-Value |
|---|---|---|---|---|---|
| Sex (Male) | 0.138 | 0.108 to 0.167 | 0.366 | 9.22 | <0.001 ** |
| Age | −0.007 | −0.009 to −0.005 | −0.267 | −6.52 | <0.001 ** |
| BMI | 0.028 | 0.022 to 0.034 | 0.362 | 9.12 | <0.001 ** |
| TSH | −0.001 | −0.003 to 0.001 | −0.041 | −0.97 | 0.333 |
| FT4 | 0.217 | 0.064 to 0.369 | 0.118 | 2.79 | 0.006 ** |
| FT3 | 0.192 | 0.142 to 0.243 | 0.304 | 7.48 | <0.001 ** |
| Hypothyroidism | 0.064 | 0.027 to 0.103 | 0.143 | 3.39 | <0.001 ** |
| s-Cr | −0.034 | −0.058 to −0.009 | −0.113 | −2.67 | 0.008 ** |
| eGFRcre | 0.002 | 0.001 to 0.003 | 0.135 | 3.21 | 0.001 ** |
| 24hrCcr | 0.005 | 0.004 to 0.006 | 0.503 | 13.65 | <0.001 ** |
| Urinary output | 0.000 | 0.000 to 0.000 | 0.271 | 6.60 | <0.001 ** |
| Urinary protein | 0.001 | −0.003 to 0.006 | 0.026 | 0.62 | 0.536 |
| Albumin | 0.099 | 0.061 to 0.137 | 0.212 | 5.09 | <0.001 ** |
| Hemoglobin | 0.045 | 0.032 to 0.058 | 0.277 | 6.76 | <0.001 ** |
| Total cholesterol | 0.000 | −0.000 to 0.001 | 0.015 | 0.36 | 0.719 |
| HbA1c | 0.018 | 0.002 to 0.033 | 0.096 | 2.27 | 0.024 * |
| Nephrotic syndrome | −0.031 | −0.085 to 0.023 | −0.048 | −1.14 | 0.255 |
| ACE-i/ARB intake | 0.005 | 0.032 to 0.043 | 0.012 | 0.28 | 0.779 |
| Levothyroxine intake | −0.052 | −0.105 to −0.000 | −0.083 | −1.97 | 0.050 * |
| Glucocorticoid intake | 0.064 | −0.010 to 0.138 | 0.072 | 1.69 | 0.091 |
BMI, body mass index; TSH, thyroid-stimulating hormone; FT4, free thyroxine; FT3, free triiodothyronine; s-Cr, serum creatinine; eGFRcre, estimated glomerular filtration rate calculated by serum creatinine; 24hrCcr, 24 h creatinine clearance; urinary CER, urinary creatinine excretion rate; HbA1c, glycated hemoglobin; ACE-i, angiotensin-converting-enzyme inhibitor; ARB, angiotensin II receptor blocker; B, unstandardized regression coefficient; β, standardized coefficient; CI, confidence interval for B. * p <0.05, ** p < 0.01.
Table 4.
Multiple regression analysis of urinary creatinine excretion rate and variables. (A) Adjusted for presence of hypothyroidism, sex, age, BMI, 24hCcr, albumin, and hemoglobin. (B) Adjusted for FT3, sex, age, BMI, 24hCcr, albumin, and hemoglobin.
| Variable | B | 95% CI | β | t | p-Value |
|---|---|---|---|---|---|
| (A) | |||||
| Hypothyroidism | 0.025 | −0.035 to 0.085 | 0.031 | 0.83 | 0.407 |
| Sex (male) | 0.173 | 0.152 to 0.194 | 0.459 | 16.23 | <0.001 ** |
| Age | −0.003 | −0.004 to −0.001 | −0.107 | −3.60 | <0.001 ** |
| BMI | 0.027 | 0.023 to 0.031 | 0.344 | 12.49 | <0.001 ** |
| 24hrCcr | 0.005 | 0.005 to 0.006 | 0.526 | 15.95 | <0.001 ** |
| Albumin | 0.050 | 0.023 to 0.078 | 0.108 | 3.61 | <0.001 ** |
| Hemoglobin | −0.004 | −0.014 to 0.005 | −0.027 | −0.89 | 0.372 |
| Constant | 0.067 | <0.001 ** | |||
| (B) | |||||
| FT3 | 0.017 | −0.024 to 0.058 | 0.027 | 0.82 | 0.410 |
| Sex (male) | 0.172 | 0.151 to 0.192 | 0.455 | 16.05 | <0.001 ** |
| Age | −0.003 | −0.004 to −0.001 | −0.105 | −3.54 | <0.001 ** |
| BMI | 0.027 | 0.022 to 0.031 | 0.342 | 12.36 | <0.001 ** |
| 24hrCcr | 0.005 | 0.004 to 0.006 | 0.512 | 16.02 | <0.001 ** |
| Albumin | 0.043 | 0.013 to 0.072 | 0.091 | 2.87 | 0.004 ** |
| Hemoglobin | −0.004 | −0.014 to 0.005 | −0.028 | −0.90 | 0.368 |
| Constant | 0.049 | <0.001 ** | |||
BMI, body mass index; 24hrCcr, 24 h creatinine clearance; B, unstandardized regression coefficient; ꞵ, standardized coefficient; CI, confidence interval for B. Model R2 = 0.596, adjusted R2 = 0.590. **p < 0.01. FT3, free triiodothyronine; BMI, body mass index; 24hrCcr, 24 h creatinine clearance; B, unstandardized regression coefficient; ꞵ, standardized coefficient; CI, confidence interval for B. Model R2 = 0.595, adjusted R2 = 0.590. ** p < 0.01.
Figure 3.
The association between eGFRcre and 24hCcr. (A) The association between eGFRcre and 24hCcr in all cases. (B) The association between eGFRcre and 24hCcr in euthyroid cases. (C) The association between eGFRcre and 24hCcr in total hypothyroid cases. eGFRcre, estimated glomerular filtration rate calculated by serum creatinine; 24hrCcr, 24 h creatinine clearance.
4. Discussion
While it is well known that hypothyroidism increases s-Cr levels [3], details of the mechanisms are still uncertain. It is suggested that hypothyroidism reduces kidney function via decreased cardiac output, increased vascular resistance, and an altered renin–angiotensin–aldosterone system [4,5,6] (Figure 4). In addition, it has also been suggested that increased s-Cr levels under hypothyroidism are via altered Cr metabolism by increased Cr production [9] (Figure 4). In the present study, hypothyroidism was not detected as an explanatory variable for urinary CER. Thus, it is unlikely that hypothyroidism increases Cr production (Figure 4), suggesting that increased s-Cr levels under hypothyroidism are predominantly via reduced kidney function. It is estimated that more than 98% of Cr is from muscle [33], where it is produced and secreted into serum at a continuous rate [34]. S-Cr is almost exclusively excreted in the urine [35]. Thus, the urinary CER, reported to be around 1 g/day [36], has been recognized as a marker of muscle mass [37], and Cr generation must approximately equal Cr excretion under stable kidney function. Indeed, it is reported that the large variance in urinary CER was accounted for by muscle mass determined by dual energy x-ray absorptiometry, and mid-arm muscle area by computed tomography [12,38,39]. In general, muscle mass does not change rapidly within individuals, and elevations in s-Cr typically reflect decrements in GFR. Under hypothyroidisms, several muscle manifestations may be observed including muscle weakness, myalgia, muscle cramps, and Hoffman syndrome as well as rhabdomyolysis [7]. Though the pathogenesis of myopathy caused by hypothyroidisms is not entirely understood, several mechanisms, such as altered glycogenolytic and oxidative metabolism, contractile proteins, and neuro-mediated damages, were proposed [7]. While muscle damages may affect the Cr generation and/or secretion from the muscles, which may result in the increase in urinary CER, we did not find a significance regarding urinary CER between hypothyroidisms and euthyroidisms. Nevertheless, hypothyroidisms-induced rhabdomyolysis need to be carefully monitored since rhabdomyolysis may cause acute kidney injury [40]. Similar to muscle mass, urinary CER is reported to have a positive correlation with male gender, and a negative correlation with age and eGFRcre [12,41,42]. Lower urinary CER is reported to be associated with death and end-stage renal disease among chronic kidney disease (CKD) patients, indicating the clinical significance of urinary CER [42].
Figure 4.
The mechanisms influencing serum creatinine levels under hypothyroidism. Cr, creatinine; s-Cr, serum creatinine; RAAS, renin–angiotensin–aldosterone system.
While the presence of hypothyroidisms was not an independent explanatory variable for urinary CER, age, sex, BMI, and 24hrCcr were associated with urinary CER as previously reported [12,41,42]. In addition, albumin was also detected as an independent explanatory variable for urinary CER. Patients of younger age, higher BMI, and higher 24hrCcr as well as male gender showed higher urinary CER probably because these patients are more likely to have more muscle mass. We also indicated that eGFRcre and 24hrCcr had strong correlations with each other under hypothyroidism as well as under euthyroidism, implying the parallel fluctuation between 24hrCcr and eGFRcre. Collectively, eGFRcre is a reliable marker to evaluate kidney function regardless of the presence or absence of hypothyroidism. Since it has been reported that thyroid hormone replacement therapy significantly improved kidney function and attenuated the rate of decline in kidney function in CKD patients with hypothyroidism [43], the appropriate treatment with the appropriate diagnosis of hypothyroidism may delay CKD progression.
There are several limitations in this study. First, the sample size is relatively small in a single university hospital and the participants are mainly hospitalized for education or examination in the division of kidney, diabetes, and endocrine diseases, thus most of the participants had CKD and diabetes mellitus; therefore, selection bias cannot be excluded. In addition, kidney and thyroid function might be affected due to the medical condition for hospitalization. Therefore, it is difficult to generalize our results to patients without CKD and diabetes mellitus. Second, 52 patients with NS were included in the study. Since hypothyroidism is a well-known complication of NS [32] due to the increased urinary excretion of thyroid hormone and thyroxine-binding globulin [44], the degree of proteinuria may affect the results. Nevertheless, the univariate regression analysis revealed that the level of urinary protein excretion was not an explanatory variable for urinary CER. In addition, we also conducted the multivariate analysis using the data excluding patients with NS, in which hypothyroidism was not detected as an independent explanatory variable for urinary CER, suggesting that the inclusion of patients with NS is less likely to affect the conclusion. Third, thyroid autoantibodies or other autoimmune antibodies were not evaluated in this study. Therefore, the possibility of a common underlying autoimmune process related to hypothyroidism cannot be excluded. Forth, we were unable to exclude the possible effect on Cr secretion into renal tubules under thyroid dysfunction. To exclude this possibility, further analysis, such as a comparison with inulin clearance or 51Cr-EDTA clearance [45] as an accurate method to measure GFR is required. Lastly, a cross-sectional study is insufficient to draw definitive conclusions about the association between hypothyroidism and urinary CER; therefore, future prospective analyses with measurements of urinary CER, renal function, and thyroid function as well as muscle mass before and after thyroid hormone replacement therapy are required for further clarification.
5. Conclusions
Our study indicated that hypothyroidism was not considered an independent explanatory variable for urinary CER in the present study and eGFRcre is reliable to evaluate kidney function regardless of the presence of hypothyroidism. Future prospective studies are required for further clarification.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diagnostics13040669/s1, Table S1: Characteristics of study participants without nephrotic syndrome stratified by thyroidal status; Table S2: Multiple regression analysis of urinary creatinine excretion rate and variables in patients without nephrotic syndrome.
Author Contributions
Conceptualization, N.M.-U. and K.T. (Kenji Tsuji); methodology, N.M.-U. and K.T. (Kenji Tsuji); formal analysis, N.M.-U., K.T. (Kenji Tsuji), K.T. (Kensaku Takahashi), K.F. and S.K.; investigation, N.M.-U., K.T. (Kenji Tsuji), K.T. (Kensaku Takahashi), K.F., H.T., S.K., K.I. and H.A.U.; writing—original draft preparation, N.M.-U. and K.T. (Kenji Tsuji); writing—review and editing, K.T. (Kensaku Takahashi), K.F., H.T., S.K., K.I., H.A.U. and J.W.; supervision, J.W.; funding acquisition, K.T. (Kenji Tsuji). All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was approved by the ethics committees of Okayama University Hospital Institutional Review Board (accredited ISO9001/2000), approved number (OKU-206-022). This study also followed the Declaration of Helsinki on medical protocol and ethics.
Informed Consent Statement
The contents of the research are posted on our department homepage and are available at the hospital, and public informed consent was provided. As this is a cross-sectional study, the committee approved public informed consent.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available as these have not been anonymized but are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Japanese Society for the Promotion of Science (JSPS)/Grant-in-Aid for Young Scientists (20K17283, to K.T. (Kenji Tsuji)).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.den Hollander J.G., Wulkan R.W., Mantel M.J., Berghout A. Correlation between severity of thyroid dysfunction and renal function. Clin. Endocrinol. 2005;62:423–427. doi: 10.1111/j.1365-2265.2005.02236.x. [DOI] [PubMed] [Google Scholar]
- 2.Verhelst J., Berwaerts J., Marescau B., Abs R., Neels H., Mahler C., De Deyn P.P. Serum creatine, creatinine, and other guanidino compounds in patients with thyroid dysfunction. Metabolism. 1997;46:1063–1067. doi: 10.1016/S0026-0495(97)90279-1. [DOI] [PubMed] [Google Scholar]
- 3.Simeoni M., Cerantonio A., Pastore I., Liguori R., Greco M., Foti D., Gulletta E., Brunetti A., Fuiano G. The correct renal function evaluation in patients with thyroid dysfunction. J. Endocrinol. Investig. 2016;39:495–507. doi: 10.1007/s40618-015-0402-8. [DOI] [PubMed] [Google Scholar]
- 4.Hammond H.K., White F.C., Buxton I.L., Saltzstein P., Brunton L.L., Longhurst J.C. Increased myocardial beta-receptors and adrenergic responses in hyperthyroid pigs. (Pt 2)Am. J. Physiol. 1987;252:H283–H290. doi: 10.1152/ajpheart.1987.252.2.H283. [DOI] [PubMed] [Google Scholar]
- 5.Walker J.D., Crawford F.A., Kato S., Spinale F.G. The novel effects of 3,5,3’-triiodo-L-thyronine on myocyte contractile function and beta-adrenergic responsiveness in dilated cardiomyopathy. J. Thorac. Cardiovasc. Surg. 1994;108:672–679. doi: 10.1016/S0022-5223(94)70292-6. [DOI] [PubMed] [Google Scholar]
- 6.Asmah B.J., Wan Nazaimoon W.M., Norazmi K., Tan T.T., Khalid B.A. Plasma renin and aldosterone in thyroid diseases. Horm. Metab. Res. 1997;29:580–583. doi: 10.1055/s-2007-979105. [DOI] [PubMed] [Google Scholar]
- 7.Sindoni A., Rodolico C., Pappalardo M.A., Portaro S., Benvenga S. Hypothyroid myopathy: A peculiar clinical presentation of thyroid failure. Review of the literature. Rev. Endocr. Metab. Disord. 2016;17:499–519. doi: 10.1007/s11154-016-9357-0. [DOI] [PubMed] [Google Scholar]
- 8.Montenegro J., Gonzalez O., Saracho R., Aguirre R., Gonzalez O., Martinez I. Changes in renal function in primary hypothyroidism. Am. J. Kidney Dis. 1996;27:195–198. doi: 10.1016/S0272-6386(96)90539-9. [DOI] [PubMed] [Google Scholar]
- 9.Wilkins L., Fleischmann W. Effects of Thyroid on Creatine Metabolism with a Discussion of the Mechanism of Storage and Excretion of Creatine Bodies. J. Clin. Investig. 1946;25:360–377. doi: 10.1172/JCI101717. [DOI] [PubMed] [Google Scholar]
- 10.Nørrelund H., Hove K.Y., Brems-Dalgaard E., Jurik A.G., Nielsen L.P., Nielsen S., Jørgensen J.O., Weeke J., Møller N. Muscle mass and function in thyrotoxic patients before and during medical treatment. Clin. Endocrinol. 1999;51:693–699. doi: 10.1046/j.1365-2265.1999.00861.x. [DOI] [PubMed] [Google Scholar]
- 11.Klein I., Mantell P., Parker M., Levey G.S. Resolution of abnormal muscle enzyme studies in hypothyroidism. Am. J. Med. Sci. 1980;279:159–162. doi: 10.1097/00000441-198005000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Ix J.H., de Boer I.H., Wassel C.L., Criqui M.H., Shlipak M.G., Whooley M.A. Urinary creatinine excretion rate and mortality in persons with coronary artery disease: The Heart and Soul Study. Circulation. 2010;121:1295–1303. doi: 10.1161/CIRCULATIONAHA.109.924266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jayagopal V., Keevil B.G., Atkin S.L., Jennings P.E., Kilpatrick E.S. Paradoxical changes in cystatin C and serum creatinine in patients with hypo- and hyperthyroidism. Clin. Chem. 2003;49:680–681. doi: 10.1373/49.4.680. [DOI] [PubMed] [Google Scholar]
- 14.Schmid C., Ghirlanda-Keller C., Zwimpfer C., Zoidis E. Triiodothyronine stimulates cystatin C production in bone cells. Biochem. Biophys. Res. Commun. 2012;419:425–430. doi: 10.1016/j.bbrc.2012.02.040. [DOI] [PubMed] [Google Scholar]
- 15.Xin C., Xie J., Fan H., Sun X., Shi B. Association Between Serum Cystatin C and Thyroid Diseases: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2021;12:766516. doi: 10.3389/fendo.2021.766516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greco M., Foti D.P., Aversa A., Fuiano G., Brunetti A., Simeoni M. Cystatin C, a Controversial Biomarker in Hypothyroid Patients under Levothyroxine Therapy: THYRenal, a Pilot Cohort Observational Study. J. Clin. Med. 2020;9:2958. doi: 10.3390/jcm9092958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deng X., Tang C., Wu J., Han R., Fang F. Changes of nutritional status and the variations of serum indicators of patients with chronic kidney disease accompanied by hypothyroidism taking thyroid hormone replacement therapy as the therapeutic models. Saudi J. Biol. Sci. 2019;26:2091–2095. doi: 10.1016/j.sjbs.2019.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang Y., Wang Y., Tao X.J., Li Q., Li F.F., Lee K.O., Li D.M., Ma J.H. Relationship between Thyroid Function and Kidney Function in Patients with Type 2 Diabetes. Int. J. Endocrinol. 2018;2018:1871530. doi: 10.1155/2018/1871530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patil V.P., Shilpasree A.S., Patil V.S., Pravinchandra K.R., Ingleshwar D.G., Vani A.C. Evaluation of renal function in subclinical hypothyroidism. J. Lab. Physicians. 2018;10:50–55. doi: 10.4103/JLP.JLP_67_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kashiwagi A., Kasuga M., Araki E., Oka Y., Hanafusa T., Ito H., Tominaga M., Oikawa S., Noda M., Kawamura T., et al. International clinical harmonization of glycated hemoglobin in Japan: From Japan Diabetes Society to National Glycohemoglobin Standardization Program values. J. Diabetes Investig. 2012;3:39–40. doi: 10.1111/j.2040-1124.2012.00207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsuo S., Imai E., Horio M., Yasuda Y., Tomita K., Nitta K., Yamagata K., Tomino Y., Yokoyama H., Hishida A., et al. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 2009;53:982–992. doi: 10.1053/j.ajkd.2008.12.034. [DOI] [PubMed] [Google Scholar]
- 22.Levey A.S., Stevens L.A., Schmid C.H., Zhang Y.L., Castro A.F., 3rd, Feldman H.I., Kusek J.W., Eggers P., Van Lente F., Greene T., et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levey A.S., Coresh J., Greene T., Stevens L.A., Zhang Y.L., Hendriksen S., Kusek J.W., Van Lente F., Chronic Kidney Disease Epidemiology C. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 24.Horio M., Imai E., Yasuda Y., Watanabe T., Matsuo S. Modification of the CKD epidemiology collaboration (CKD-EPI) equation for Japanese: Accuracy and use for population estimates. Am. J. Kidney Dis. 2010;56:32–38. doi: 10.1053/j.ajkd.2010.02.344. [DOI] [PubMed] [Google Scholar]
- 25.Imai E., Horio M., Nitta K., Yamagata K., Iseki K., Hara S., Ura N., Kiyohara Y., Hirakata H., Watanabe T., et al. Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease. Clin. Exp. Nephrol. 2007;11:41–50. doi: 10.1007/s10157-006-0453-4. [DOI] [PubMed] [Google Scholar]
- 26.Du Bois D., Du Bois E.F. A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition. 1989;5:303–311. discussion 312–313. [PubMed] [Google Scholar]
- 27.Pan B., Du X., Zhang H., Hua X., Wan X., Cao C. Relationships of Chronic Kidney Disease and Thyroid Dysfunction in Non-Dialysis Patients: A Pilot Study. Kidney Blood Press Res. 2019;44:170–178. doi: 10.1159/000499201. [DOI] [PubMed] [Google Scholar]
- 28.Lo J.C., Chertow G.M., Go A.S., Hsu C.Y. Increased prevalence of subclinical and clinical hypothyroidism in persons with chronic kidney disease. Kidney Int. 2005;67:1047–1052. doi: 10.1111/j.1523-1755.2005.00169.x. [DOI] [PubMed] [Google Scholar]
- 29.Carrero J.J., Johansen K.L., Lindholm B., Stenvinkel P., Cuppari L., Avesani C.M. Screening for muscle wasting and dysfunction in patients with chronic kidney disease. Kidney Int. 2016;90:53–66. doi: 10.1016/j.kint.2016.02.025. [DOI] [PubMed] [Google Scholar]
- 30.Carrero J.J., Stenvinkel P., Cuppari L., Ikizler T.A., Kalantar-Zadeh K., Kaysen G., Mitch W.E., Price S.R., Wanner C., Wang A.Y., et al. Etiology of the protein-energy wasting syndrome in chronic kidney disease: A consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM) J. Ren. Nutr. 2013;23:77–90. doi: 10.1053/j.jrn.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 31.Wang X.H., Mitch W.E. Mechanisms of muscle wasting in chronic kidney disease. Nat. Rev. Nephrol. 2014;10:504–516. doi: 10.1038/nrneph.2014.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feinstein E.I., Kaptein E.M., Nicoloff J.T., Massry S.G. Thyroid function in patients with nephrotic syndrome and normal renal function. Am. J. Nephrol. 1982;2:70–76. doi: 10.1159/000166587. [DOI] [PubMed] [Google Scholar]
- 33.Hunter A. Creatine and Creatinine. Volume 24 Longmans, Green and Company Limited; London, UK: 1928. [Google Scholar]
- 34.Heymsfield S.B., Arteaga C., McManus C., Smith J., Moffitt S. Measurement of muscle mass in humans: Validity of the 24-hour urinary creatinine method. Am. J. Clin. Nutr. 1983;37:478–494. doi: 10.1093/ajcn/37.3.478. [DOI] [PubMed] [Google Scholar]
- 35.Goldman R. Creatinine excretion in renal failure. Proc. Soc. Exp. Biol. Med. 1954;85:446–448. doi: 10.3181/00379727-85-20912. [DOI] [PubMed] [Google Scholar]
- 36.Diago C.A.A., Senaris J.A.A. Should we pay more attention to low creatinine levels? Endocrinol. Diabetes Nutr. (Engl. Ed.) 2020;67:486–492. doi: 10.1016/j.endinu.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 37.Burger M. Die Bedeutung des Kreatininkoefizienten fur die quantitative bewertund der muskulatur als korpergewichtskomponente. Z. Ges. Exp. Med. 1919;9:361–399. [Google Scholar]
- 38.Rule A.D., Bailey K.R., Schwartz G.L., Khosla S., Lieske J.C., Melton L.J., 3rd For estimating creatinine clearance measuring muscle mass gives better results than those based on demographics. Kidney Int. 2009;75:1071–1078. doi: 10.1038/ki.2008.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heymsfield S.B., McManus C., Smith J., Stevens V., Nixon D.W. Anthropometric measurement of muscle mass: Revised equations for calculating bone-free arm muscle area. Am. J. Clin. Nutr. 1982;36:680–690. doi: 10.1093/ajcn/36.4.680. [DOI] [PubMed] [Google Scholar]
- 40.Baghi M.A., Sirajudeen J., Naushad V.A., Alarbi K.S., Benshaban N. Severe hypothyroidism-induced rhabdomyolysis: A case report. Clin. Case Rep. 2021;9:e05107. doi: 10.1002/ccr3.5107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tynkevich E., Flamant M., Haymann J.P., Metzger M., Thervet E., Boffa J.J., Vrtovsnik F., Houillier P., Froissart M., Stengel B., et al. Decrease in urinary creatinine excretion in early stage chronic kidney disease. PLoS ONE. 2014;9:e111949. doi: 10.1371/journal.pone.0111949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wilson F.P., Xie D., Anderson A.H., Leonard M.B., Reese P.P., Delafontaine P., Horwitz E., Kallem R., Navaneethan S., Ojo A., et al. Urinary creatinine excretion, bioelectrical impedance analysis, and clinical outcomes in patients with CKD: The CRIC study. Clin. J. Am. Soc. Nephrol. 2014;9:2095–2103. doi: 10.2215/CJN.03790414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shin D.H., Lee M.J., Lee H.S., Oh H.J., Ko K.I., Kim C.H., Doh F.M., Koo H.M., Kim H.R., Han J.H., et al. Thyroid hormone replacement therapy attenuates the decline of renal function in chronic kidney disease patients with subclinical hypothyroidism. Thyroid. 2013;23:654–661. doi: 10.1089/thy.2012.0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mario F.D., Pofi R., Gigante A., Rivoli L., Rosato E., Isidori A.M., Cianci R., Barbano B. Hypothyroidism and Nephrotic Syndrome: Why, When and How to Treat. Curr. Vasc. Pharmacol. 2017;15:398–403. doi: 10.2174/1570161115999170207114706. [DOI] [PubMed] [Google Scholar]
- 45.Soveri I., Berg U.B., Bjork J., Elinder C.G., Grubb A., Mejare I., Sterner G., Back S.E., Group S.G.R. Measuring GFR: A systematic review. Am. J. Kidney Dis. 2014;64:411–424. doi: 10.1053/j.ajkd.2014.04.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available as these have not been anonymized but are available from the corresponding author on reasonable request.