Abstract
Background
The purpose of our study is to assess the methodology of overlapping systematic reviews related to cemented vs uncemented hip hemiarthroplasties for the treatment of femoral neck fractures to find the study with the best evidence. Also, we assess the gaps in methodology and information to help with direction of future studies.
Methods
A systematic search was conducted in September 2022 using Pubmed, Embase, and Cochrane Library. Clinical outcome data and characteristics of each study were extracted to see which treatment had better favorability. The outcomes and characteristics extracted from each study includes, first author, search date, publication journal and date, number of studies included, databases, level of evidence, software used, subgroup analyses that were conducted, and heterogeneity with the use of I2 statistics Methodological quality information was extracted from each study using four different methodologic scores (Oxford Levels of Evidence; Assessment of Multiple Systematic Reviews (AMSTAR); Quality of reporting of meta-analyses (QUROM); Oxman and Guyatt. After that, the Jadad decision algorithm was used to identify which studies in our sample contained the best available evidence. Finally, overlap of each systematic review was assessed using Corrected Covered Area (CCA) to look at redundancy and research waste among the systematic reviews published on the topic.
Results
After screening, 12 studies were included in our sample. For the Oxford Levels of Evidence, we found that all the studies were Level I evidence. For the QUORUM assessment, we had 1 study with the highest score of 18. Additionally, we did the Oxman and Guyatt assessment, where we found 4 studies with a maximum score of 6. Finally, we did an AMSTAR assessment and found 2 studies with a score of 9. After conducting the methodological scores; the authors determined that Li. L et al 2021 had the highest quality. In addition, it was found that the CCA found among the primary studies in each systematic review calculated to .22. Any CCA above .15 is considered “very high overlap”.
Conclusions
The best available evidence suggests that Cemented HAs are better at preventing Prosthesis-related complications. Conversely, the best evidence also suggests that Cemented HA also results in longer operative time and increased intraoperative blood loss. When conducting future systematic reviews related to the topic, we ask that authors restrict conducting another systematic review until new evidence emerges so as not to confuse the clinical decision-making of physicians.
Introduction
As of 2019, the global incidence of hip fractures exceeds 14 million–a 90% increase since 1990 [1]. People who experience hip fractures are prone to a wide range of complications that can result in death and decreased quality of life (QoL) [2–4]. Hip fractures are commonplace within elderly populations; in the United States, over 300,000 older individuals are hospitalized for hip fractures every year [5]. Femoral neck fractures commonly occur in this population, sustained through low-energy falls. For these elderly patients (65 years or older), both total hip arthroplasty and hemiarthroplasty are equally valid treatment options [6–9].
The hemiarthroplasty procedure varies on the nature of the fracture. Surgeons may approach fractures from different angles and planes, consider unipolar vs bipolar femoral head implants, and elect for cement vs non-cemented techniques. Germane to cement and non-cement technique, best practice remains uncertain due to the variation in results from primary studies and meta-analyses. In September 2014, Middleton et al. reported significantly higher re-operation rates for those undergoing an uncemented operation (p = 0.005) [10]. Four months later, Grammatopoulos et al. reported no significant difference in the re-operation rate between the cemented and uncemented groups (p = 0.36) [11]. A meta-analysis conducted by Li et al., as published in Plos One reported no significant difference in postoperative hip function between cemented and uncemented hemiarthroplasties at two months (p = .82) [12]. In contrast, Lin et al. published a meta-analysis in Medicine that stated that cemented hemiarthroplasties resulted in better postoperative hip function at 12 months (p = .01) [13]. Further, these meta-analyses cite variable outcome measurement and heterogeneity as key barriers to comprehensive pooled analyses, leaving a small sample of trials from which to draw important clinical conclusions.
We believe that the prevalence of small sample sizes, inconsistent outcome measures, and variable heterogeneity may be driving discrepant results in the hemiarthroplasty literature base. The purpose of our study is to conduct an overlapping analysis of systematic reviews/meta-analyses exploring cemented vs uncemented hemiarthroplasty outcomes. Secondly, we plan on conducting methodology assessments among the studies within our sample. Finally, we hope to precisely demonstrate gaps and provide practical solutions for improving the hemiarthroplasty evidence base for future research and improved patient care.
Materials and methods
This systematic review was done in adherence with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [14]. Ethical approval or patient consent is not required for this review due to its secondary nature. Our methodology follows a similar design as Zhao et al [15]. A systematic search was conducted in September 2022 using Pubmed, Embase, and Cochrane Library. Two reviewers reviewed each title and abstract followed by a full-text screen to identify articles that met the inclusion criteria. Senior authors settled disagreements. The search string used is as follows: (cement OR cemented) AND (uncement OR uncemented OR noncement OR noncemented OR cementless) AND (hemiarthroplasty OR arthroplasty OR replacement) AND (hip OR femur OR femoral) AND (fracture OR fractures) AND (systematic review OR meta analyses OR meta analysis OR review) (’cement’ OR ’cemented’) AND (’uncement’ OR ’uncemented’ OR ’noncement’ OR ’noncemented’ OR ’cementless’) AND (’hemiarthroplasty’ OR ’arthroplasty’ OR ’replacement’) AND (’hip’ OR ’femur’ OR ’femoral’) AND (’fracture’ OR ’fractures’) AND (’systematic review’ OR ’meta analyses’ OR ’meta analysis’ OR ’review’).
Inclusion and exclusion criteria
Inclusion criteria for the study were as listed: 1.) Systematic review and Meta-analysis that juxtapose Cemented vs Uncemented Hemiarthroplasties for the treatment of Femoral Neck Fractures; 2.) included sample must contain solely randomized controlled trials (RCTs); 3.) report at least one outcome in comparison of the two treatment modalities; 4.) English-written articles; 5.) Analyses must only include human studies. Exclusion criteria included any systematic review without a meta-analysis or data pooling; also, narrative reviews, meeting abstracts, and meta-analyses with non-RCT studies were excluded.
Data extraction
For each study included in the sample, we extracted: First author, search date, publication journal and date, number of studies included, databases, level of evidence, software used, subgroup analyses that were conducted, and heterogeneity with the use of I2 statistics. Also, clinical outcome data were extracted to see which treatment had better favorability.
Quality assessment
Methodological information was extracted using four different methodologic scores. The following methodologic scores were conducted for the 11 studies in our sample in a double and blind fashion: Oxford Levels of Evidence [16, 17]; Assessment of Multiple Systematic Reviews (AMSTAR) [18, 19]; Quality of reporting of meta-analyses (QUROM) [20]; Oxman and Guyatt Index [21]. Any disagreements were solved in consensus.
Heterogeneity assessment
When conducting a meta-analysis, heterogeneity is assessed using I2 statistics. When the assessment yields a result that is greater than 50%, then heterogeneity is deemed to exist. Therefore two authors assessed whether sensitivity or subgroup analyses were carried out to identify the source of the heterogeneity.
Application of Jadad decision algorithm
The Jadad decision algorithm was used to identify which studies in our sample contained the best available evidence. Jadad et al. [22] describe that discordance of meta-analyses is derived from 6 separate reasons: clinical question, study selection and inclusion, data extraction, assessment of study quality, assessment of the ability to combine studies, and statistics used for data synthesis. Two reviewers conducted the algorithm independently, then, through consensus, decided which meta-analysis represents the best evidence.
Assessment of overlap among primary studies
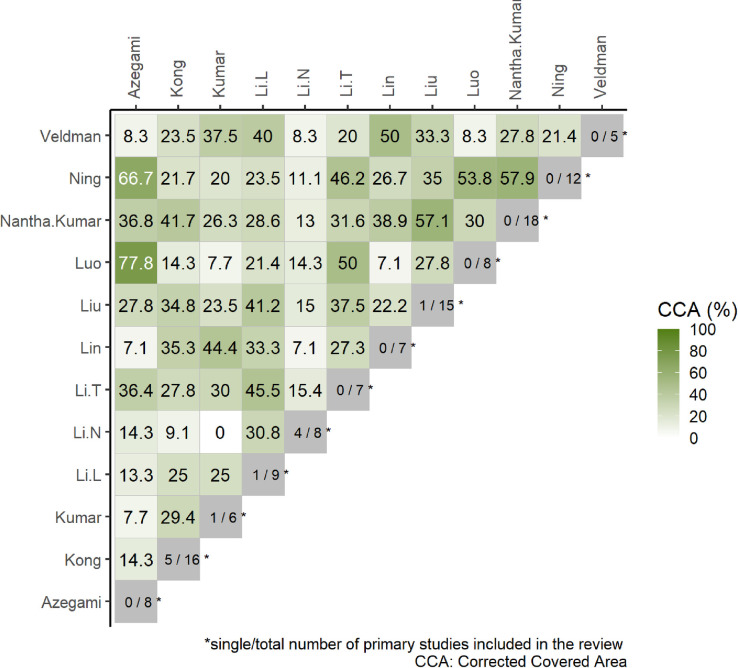
Two investigators extracted the primary studies from the systematic reviews (SRs) within our sample. Afterward, the overlap of primary studies between systematic reviews was calculated using the corrected covered area (CCA) tool developed by Pieper et al. [23]. Each of the studies will be compared against one another and yield a CCA value. After obtaining all the CCA values between the studies, they will be averaged to get an overall CCA value. The interpretation of CCA is as follows: 0-.05 = slight overlap, .06-.1 = moderate overlap, .11-.15 = high overlap, and >.15 = very high overlap.
Results
Literature search
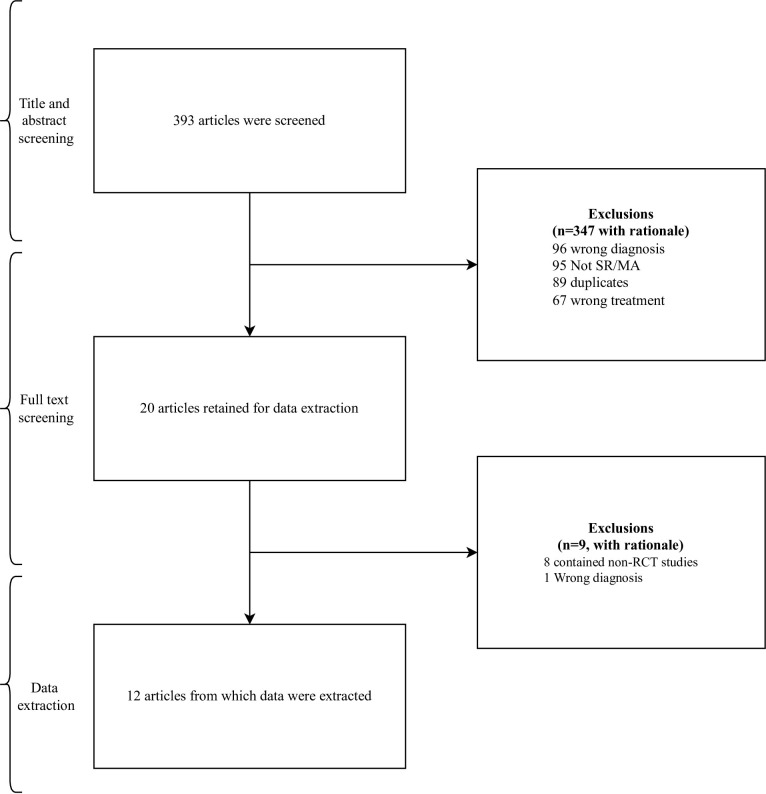
The initial search string found 393 studies. After screening, 12 studies were included in our sample (Fig 1) [12, 13, 24–33]. The overlapping meta-analyses were published between 2011 to 2021 in different journals, with the number of RCTs in the sample ranging from 5 to 18 (Table 1). The RCTs were published from 1977 to 2021 (Table 2).
Fig 1. Flow chart.
Table 1. Characteristics.
| Author (year) | Publication date | Journal | Search Date | # of RCTs |
|---|---|---|---|---|
| Liu B (2020) | August 2020 | Medicine | December 2018 | 15 |
| Kong (2020) | June 2020 | Experimental and Therapeutic Medicine | February 2019 | 16 |
| Li N (2020) | February 2020 | Medicine | December 2018 | 8 |
| Luo X (2012) | December 2011 | Archives of Orthopaedic and Trauma Surgery | December 2010 | 8 |
| Kumar P (2019) | January 2019 | European Journal of Orthopaedic Surgery & Traumatology | February 2018 | 4 |
| Azegami S (2011) | September 2011 | HIP International | September 2009 | 8 |
| Li T (2013) | July 2013 | PLOS One | December 2012 | 7 |
| Ning G (2014) | December 2012 | European Journal of Orthopaedic Surgery & Traumatology | March 2012 | 12 |
| Lin FF (2019) | February 2019 | Medicine | February 2016 | 7 |
| Veldman HD (2017) | April 2017 | The Bone & Joint Journal | April 2016 | 5 |
| Nantha Kumar N *(2020) | August 2020 | The Bone & Joint Journal | February 2020 | 18 |
| Li L (2021) | June 2021 | Archives of Orthopaedic and Trauma Surgery | January 2020 | 11 |
Table 2. Included RCTs in each systematic review.
| Liu | Kong | Li N | Luo | Kumar | Azegami | Li T | Ning | Lin | Veldman | Nantha Kumar | Li L | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sonne-Holm 1982 [57] | Y | Y | Y | Y | Y | Y | Y | |||||
| Dorr 1986 [58] | Y | Y | Y | Y | ||||||||
| Emery et al. 1991 [59] | Y | Y | Y | Y | Y | Y | Y | Y | Y | |||
| Figved 2009 [60] | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| Moroni 2009 [61] | Y | Y | Y | |||||||||
| DeAngelis 2012 [62] | Y | Y | Y | Y | Y | Y | Y | Y | Y | |||
| Taylor 2012 [63] | Y | Y | Y | Y | Y | Y | Y | Y | Y | |||
| Talsnes 2013 [64] | Y | Y | Y | Y | Y | Y | Y | |||||
| Langslet 2014 [65] | Y | Y | Y | Y | Y | Y | Y | |||||
| Inngul 2015 [66] | Y | Y | Y | |||||||||
| Harper and Gregg 1992 [67] | Y | Y | Y | Y | ||||||||
| Branfoot 2000 [68] | Y | Y | Y | |||||||||
| Santini 2005 [69] | Y | Y | Y | Y | Y | Y | ||||||
| Parker 2010 [70] | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| Cumming and Parker 2012 [71] | Y | Y | ||||||||||
| Sadr and Arden 1977 [72] | Y | Y | Y | Y | ||||||||
| Vidovic 2013 [73] | Y | Y | ||||||||||
| Barenius 2018 [74] | Y | Y | ||||||||||
| Moerman 2017 [75] | Y | Y | Y | Y | ||||||||
| Parker and Cawley 2020 [76] | Y | Y | ||||||||||
| Vidovic 2015 [77] | Y | |||||||||||
| Khorami 2016 [78] | Y | Y | ||||||||||
| Li 2017 [79] | Y | |||||||||||
| Ma 2016 [80] | Y | |||||||||||
| Prashanth and Niranjan 2017 [81] | Y | |||||||||||
| Mohabey 2017 [82] | Y | |||||||||||
| Movrin 2020 [83] | Y | |||||||||||
| Du 2014 [84] | Y | |||||||||||
| Pan 2013 [85] | Y |
Search methods for systematic reviews/meta-analyses
While all literature searches were conducted appropriately, we found variations in the databases that were searched. All 12 studies searched the Embase database, while 11 studies searched Cochrane Library, 9 studies searched Pubmed, and 6 studies searched Medline. In addition, databases such as SCOPUS, Web of Science, CNKI, WANFANG, CINAHL, VIP database, and Google Scholar were searched in the included studies. Other aspects of methodology were shown to vary, including language restrictions and publication status restrictions. We found that 5 studies had English-only language restrictions, while 7 studies did not have language restrictions. We also had only 1 study disclose a grey literature search for unpublished literature. Of the other studies, 7 specified that published literature was the only type that would be reviewed by the authors, while 4 studies did not specify. For further information on the search methodology of each study, refer to Table 3.
Table 3. Search methodology.
| Author (year) | Language Restriction | Publication status Restriction | Pubmed | Embase | SCOPUS | Medline | Cochrane Library | Web of Science | CNKI | WANFANG | CINAHL | VIP Database | Google Scholar |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Liu B (2020) | Yes | NA | * | * | * | * | |||||||
| Kong X (2020) | No | NA | * | * | * | * | * | ||||||
| Li N (2020) | No | Yes | * | * | * | ||||||||
| Luo X (2012) | Yes | Yes | * | * | * | ||||||||
| Kumar P (2019 | Yes | Yes | * | * | * | ||||||||
| Azegami S (2011) | No | No | * | * | * | * | |||||||
| Li T (2013) | Yes | Yes | * | * | * | * | * | ||||||
| Ning G (2014) | Yes | Yes | * | * | * | * | * | ||||||
| Lin FF (2019) | No | NA | * | * | * | * | |||||||
| Veldman HD (2017) | No | NA | * | * | * | * | |||||||
| Nantha Kumar N (2020) | No | Yes | * | * | * | * | * | * | |||||
| Li L (2021) | No | Yes | * | * | * | * |
Methodological quality
There was continued discordance with the different software used by the studies in our sample. The software used in our sample includes RevMan (which 9 studies used), STATA (which 2 studies used), and one study did not specify. All of the studies contained a Sensitivity/Subgroup Analysis. In addition, only 4 of the studies in the sample assessed publication bias. (Table 4).
Table 4. Methodologic information.
| Primary Study Design | Level of Evidence | Software use | Grade Use | Sensitivity/Subgroup Analysis | Publication Bias | |
|---|---|---|---|---|---|---|
| Liu B (2020) | RCT | I | RevMan | No | Yes | No |
| Kong X (2020) | RCT | I | RevMan | No | No | Yes |
| Li N (2020) | RCT | I | RevMan | No | Yes | No |
| Luo X (2012) | RCT | I | RevMan | No | Yes | No |
| Kumar P (2019) | RCT | I | RevMan | Yes | Yes | No |
| Azegami S (2011) | RCT | I | NA | No | No | No |
| Li T (2013) | RCT | I | RevMan | Yes | Yes | No |
| Ning G (2014) | RCT | I | STATA | No | Yes | Yes |
| Lin FF (2019) | RCT | I | RevMan | No | Yes | No |
| Veldman HD (2017) | RCT | I | RevMan | No | No | Yes |
| Nantha Kumar N (2020) | RCT | I | STATA | No | Yes | Yes |
| Li L (2021) | RCT | I | RevMan | Yes | Yes | Yes |
We also conducted 4 different methodological quality assessments of the sample to determine the highest quality study. We found that all the studies were Level I evidence based on the Oxford Levels of Evidence. For the QUORUM assessment, we had 1 study with the highest score of 18. Additionally, we did the Oxman and Guyatt assessment, where we found 4 studies with a maximum score of 6. Finally, we did an AMSTAR assessment and found 2 studies with a score of 9. (Table 5) After a consensus discussion, the authors determined that Li. L et al. [33] had the highest quality.
Table 5. Methodologic scores.
| QUORUM | Oxman-Guyatt | AMSTAR | ||
|---|---|---|---|---|
| Cemented versus uncemented hemiarthroplasty for elderly patients with displaced fracture of the femoral neck | Liu | 16 | 5 | 7 |
| Meta‐analysis of the effect of cemented and uncemented hemiarthroplasty on displaced femoral neck fracture in the elderly | Kong | 16 | 4 | 7 |
| Cemented versus uncemented hemi-arthroplasty for femoral neck fractures in elderly patients: A systematic review and meta-analysis of randomized controlled trials | Li | 17 | 5 | 8 |
| Systematic review of cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures in older patients | Luo | 12 | 3 | 4 |
| Hemiarthroplasty for neck of femur fractures: to cement or not? A systematic review of literature and meta‐analysis | Kumar | 16 | 6 | 7 |
| Cemented versus uncemented hemiarthroplasty for hip fractures: a systematic review of randomised controlled trials | Azegami | 12 | 4 | 6 |
| Cemented versus Uncemented Hemiarthroplasty for Femoral Neck Fractures in Elderly Patients: A Meta- Analysis | Li | 17 | 5 | 7 |
| Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: an updated meta-analysis | Ning | 17 | 4 | 8 |
| Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures A meta-analysis of randomized controlled trails | Lin | 17 | 6 | 7 |
| Cemented versus cementless hemiarthroplasty for a displaced fracture of the femoral neck A SYSTEMATIC REVIEW AND META-ANALYSIS OF CURRENT GENERATION HIP STEMS | Veldman | 17 | 6 | 8 |
| Effectiveness and safety of cemented and uncemented hemiarthroplasty in the treatment of intracapsular hip fractures A SYSTEMATIC REVIEW AND META-ANALYSIS OF RANDOMIZED CONTROLLED TRIALS | Nantha Kumar | 17 | 5 | 9 |
| Cemented versus uncemented hemiarthroplasty for the management of femoral neck fractures in the elderly: a meta-analysis and systematic review | Li L | 18 | 6 | 9 |
Heterogeneity evaluation
All of the studies in the sample contained I2 statistics. There were varying results in our sample. Certain variables with little to no heterogeneity were cardiovascular complications and reoperations/revisions. Other stats with a high rate of heterogeneity were prosthetic-related complications and operation time. To account for the heterogeneity, 9 studies conducted sensitivity/subgroup analyses. (Table 6).
Table 6. Pooled analysis of each meta-analysis and I2 statistics.
| Liu | Kong | Li N | Luo | Kumar | Azegami | Li T | Ning | Lin | Veldman | Nantha Kumar | Li L | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HHS/functional | N/51% | N/78% | C/0% | C/0% | N/51% / C/0% | N | N/85% | |||||
| Postoperative Pain | C/66% | C/0% | N/65% | N/0% | C/0% | N/80.2% | C/0% | |||||
| Reoperation and Revision | N/0% | N/0% | N/0% | N/0% | N/0% | N/0% | N/0% | N/74% / N/74% | C/0% | |||
| General Complications | N/0% | N/0% | C/90% | N/0% | N/0% | N/0% | N | N | ||||
| Local Complications | N/0% | C/73.3% | N/0% | N | ||||||||
| Prosthetic-related Complications | C/41% | C/55% | C/42% | C/41% | C/38% | |||||||
| Intraoperative Fractures | N/0% | N/0% | N/0% | C/0% | C/74% | |||||||
| Periprosthetic Fractures | C/16% | C/30% | C/0% | C/74% | ||||||||
| Prosthesis Dislocation | N/0% | N/0% | N/0% | N/74% | ||||||||
| Postoperative Deep Infection | N/74% | |||||||||||
| Wound Infections | N/7% | N | ||||||||||
| UTI/medical | N/0% | N/0% | ||||||||||
| Perioperative Mortality | N/0% | N/0% | ||||||||||
| 0–6 months- mortality | N/0% | N | N/0% | |||||||||
| 1 year- mortality | N/0% | N/0% | N/0% | N/0% | L/0% | N/0% | N/34% | N/50% | N/0% | N/13% | ||
| Length of Hospital Stay | N/0% | C/84% | N/0% | N/0% | N/0% | |||||||
| Operation Time | L/45% | L/77% | N/51% | L/64% | L/20% | L/10.9% | L/52% | L/46% | L | L/38% | ||
| Intraoperative Blood Loss | N/56% | N/85% | N/57% | N/52% | N/14% | N/36.2% | N/0% | L/41% | N | |||
| Incision Infection | N/0% | |||||||||||
| Pulmonary Embolism | N/0% | L/0% | ||||||||||
| Cardiovascular | N/0% | N/0% | N/0% | N/0% | N/0% | N/0% | ||||||
| DVT | N/0% | N/0% | ||||||||||
| Pneumonia | N/0% | N/62% | N/0% | |||||||||
| Cerebrovascular incident | N/0% | N/0% | N/0% | |||||||||
| "Local" and "general" complicationsnot reported in detail | "Local complications" | Cardiovascular and Cerebrovascular complications were merged to gether | - Mortality was not specific on time range -Complications not specified | Cardiovascular and Cerebrovascular complications were merged to gether |
* N = No Difference, C = Cemented HA favored, L = Cementless HA favored
Results of Jadad decision algorithm
When conducting the Jadad decision algorithm, the methodology helps identify the best current evidence in treatment. The first step is identifying if studies are asking the same question, which they are. While they are asking the same question, they do not have the same number of primary trials in their sample and their criteria for study selection was different. As a result, we conducted 4 different methodological analyses for each of the studies. We found that Li L et al. [33] was the highest methodological study and therefore was selected.
Overlap assessment using CCA
We found 34 RCT primary studies cited within the 12 SRs in our sample. After comparing the 12 SRs, our sample yielded 66 CCA data points for each comparison. When gauging each individual comparison, we found that 48 of the 66 comparisons had a CCA value greater than .15. There were 8 CCAs between .10 and .15., 9 CCAs between .06 and .10, and 1 CCA between 0 and .05. After conducting our analysis, our sample contained a CCA value of .22. (Fig 2).
Fig 2. CCA heat map.
Discussion
Our study found that the highest quality meta-analyses related to the treatment of femoral neck fractures using cemented vs uncemented hemiarthroplasties (HAs) were Li L et al. [33] Li L et al. found a statistical significance that Cemented had better results in terms of postoperative pain, reoperations and revisions, and Prosthetic related complications compared to Uncemented HAs. On the other hand, Uncemented Arthroplasties were associated with lower operation times compared to Cemented.
Many RCTs have been conducted comparing Cemented and Uncemented HAs as a treatment option for Femoral Neck fractures, showing discordant results. Therefore, multiple meta-analyses were also conducted to pool the data together and see the results. But, these meta-analyses also show discordant results. As a result, there is continued debate on the best treatment method. Overall consensus suggests that the decision should be based on surgeon preference, philosophy, and expertise [34]. Specific attributes of each treatment that physicians consider when deciding which option to use would include Mortality and/or short-term outcomes such as complications, and revisions [35].
Mortality
In terms of mortality, hip fractures have a high mortality rate that continues to increase [3, 36, 37]. Therefore, treatment must be done promptly. Huette et al. discuss how specific factors such as Age, Time of Surgery, and a Lee Score greater than 3 lead to higher 1-year mortality rates [38]. When considering the type of HA to treat a patient with a hip fracture, physicians are finding disagreement based on the available evidence [39, 40]. We found that of the 10 studies that analyzed the data on 1-year Mortality, 9 studies stated that there was no statistical difference between mortality of Cemented vs Uncemented HA. Kumar et al. was the only study statistically significant for mortality favoring Uncemented HAs [28]. Although there was a statistical difference between the included RCTs, the authors state that the data could have been subject to bias based on intraoperative plan changes based on bone quality and size of the medullary canal.
Reoperation and revision rates are essential to determining treatment since it has been shown that revisions are associated with higher mortality in individuals that undergo hip arthroplasties [41]. Our sample had 8 studies that looked at this, and all studies found that there was no difference in reoperation/revision rates between Cemented and Uncemented HAs. This is intriguing because our sample shows statistical significance for Cemented HAs having a lower prosthetic-related complications rate than Uncemented HAs.
Prosthetic-related complications
It is agreed upon that patients’ short-term experience after HA surgery is essential for positive outcomes [35]. Similarly to mortality, various studies show discordance regarding short-term outcomes after HA. For example, studies have reported that there is a high risk of thigh pain for the Uncemented implants, in contrast, Rolfson et al. have reported that 1st-year postoperative outcomes are better in patients that undergo Uncemented HA compared to Cemented HA [42–44]. A variety of outcomes were assessed in the meta-analyses within our sample. To start, 4 studies looked at overarching prosthetic-related complications, and all found that Cemented HAs were preferable, with two of the studies showing low heterogeneity associated with their results [12, 24, 28, 31]. We also looked at specific prosthetic-related complications. No statistical significance was found favoring either treatment for avoiding dislocations, but the same studies found statistical significance for Cemented HAs more favorable in avoiding periprosthetic fractures [13, 25, 26, 32].
Research wastage
Our study also analyzed the overlap in primary literature displayed among the SRs using CCA. It was found that the CCA found among the SRs was .22, which is considered among the highest degree of overlap according to Pieper et al. [23]. In addition to conducting our analysis, we interestingly found, of the 11 studies within our sample, 6 systematic reviews were published on the same topic between 2019–2020 [13, 24–26, 28, 32]. While it is ok for overlap of meta-analyses, there needs to be significant new empirical evidence; however, the publication of numerous meta-analyses over the same topic in a short time frame is concerning, as it could contribute to the confusion already associated with the treatment path of femoral neck fractures [45, 46]. Siontis et al. discuss how the overlap of systematic reviews can be warranted, but the publication of numerous similar meta-analyses over a short period contributes to wasted research efforts and confusion among readers [46]. Authors must be wiery of this and wait to publish more reviews on the topic until higher-quality RCTs are published. In addition, to avoid the redundancy of hemiarthroplasty meta-analyses and improve future studies, we discuss the steps below that can be conducted to improve upon the studies in our sample.
Firstly, we recommend that before authors conduct an SR, they conduct a literature search for existing studies to prevent redundancy in the literature. We also recommend that journals conduct the same literature search during the submission process to see if there is a gap in the literature the study fills. Secondly, only 1 of the studies in our sample looked at unpublished literature when conducting their search [29]. Searches for unpublished literature data are essential, due to the presence of publication bias in orthopaedic literature [47]. Due to publication bias, Cochrane Collaboration requires that systematic reviews published in their journal have at least one search for unpublished clinical trials. It was found that only 7% of Orthopaedic Systematic Reviews conducted a clinical trial registry search with almost 60% of Orthopaedic Systematic Reviews potentially adding unpublished clinical trial data to their sample, allowing for more accurate effect sizes by reducing publication bias [48–50]. In addition, it is necessary for future systematic reviews to conduct assessments on publication bias within their sample. Only 4 of the studies in the sample conducted funnel plots to look for publication bias within their study [25, 30–32]. This is problematic, considering PRISMA states that an assessment of the risk of publication bias should be conducted [51]. This is due to the overrepresentation of significant results in published literature. As a result, underpowered studies can have distorted conclusions due to publication bias [52]. Finally, when conducting meta-analyses, after conducting a sensitivity analysis to identify the heterogeneity within a meta-analysis, it should be common practice to conduct a random-effects model to remove the heterogeneity from the analysis [53, 54]. While sensitivity analyses were conducted, there were still outcomes in the meta-analyses with an I2>50% which shows that large heterogeneity is present. By decreasing the heterogeneity within the sample, the relevance of the results will increase, allowing for stronger inference of conclusions [55, 56].
Limitations
This study has a few limitations. First, we only included studies published in English. Any studies that were non-English that fit our inclusion criteria could have been overlooked. Additionally, there is some subjectivity to the Oxman & Guyatt score that was used for the methodology analysis. We conducted the score in a blinded fashion to limit the subjectivity bias and had trained Orthopaedic Surgeons to consult if we could not come to a consensus. Finally, while we used a comprehensive search strategy for the methodology, there could have been studies that were missed.
Conclusions
This is the first overlapping analysis of overlapping systematic reviews assessing the treatment of femoral neck fractures with Cemented vs. Uncemented HAs. The best available evidence suggests that Cemented HAs are better at preventing Prosthesis-related complications. Conversely, the best evidence also suggests that Cemented HA also results in longer operative time and increased intraoperative blood loss. Both options are viable, but the physician should consider these results to determine the best avenue of treatment for each patient. In addition, until new/better research is produced to change the literature regarding Cemented vs Uncemented HAs, journals should limit the publication of systematic reviews regarding the topic.
Supporting information
(PDF)
Data Availability
The data are available in the paper and on the Open Science Framework repository (https://osf.io/vh8es/).
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.GBD 2019 Fracture Collaborators. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021;2: e580–e592. doi: 10.1016/S2666-7568(21)00172-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhandari M, Devereaux PJ, Tornetta P 3rd, Swiontkowski MF, Berry DJ, Haidukewych G, et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005;87: 2122–2130. doi: 10.2106/JBJS.E.00535 [DOI] [PubMed] [Google Scholar]
- 3.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17: 1726–1733. doi: 10.1007/s00198-006-0172-4 [DOI] [PubMed] [Google Scholar]
- 4.Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ. 2010;340: c2332. doi: 10.1136/bmj.c2332 [DOI] [PubMed] [Google Scholar]
- 5.Hip fractures among older adults. 30 Sep 2020 [cited 6 Oct 2022]. Available: https://www.cdc.gov/falls/hip-fractures.html
- 6.Summary section. National Institute for Health and Care Excellence (NICE); 2017. Available: https://www.ncbi.nlm.nih.gov/books/NBK550549/
- 7.Protzman RR, Burkhalter WE. Femoral-neck fractures in young adults. J Bone Joint Surg Am. 1976;58: 689–695. Available: https://www.ncbi.nlm.nih.gov/pubmed/932067 [PubMed] [Google Scholar]
- 8.Bhandari M, Swiontkowski M. Management of Acute Hip Fracture. N Engl J Med. 2017;377: 2053–2062. doi: 10.1056/NEJMcp1611090 [DOI] [PubMed] [Google Scholar]
- 9.HEALTH Investigators, Bhandari M, Einhorn TA, Guyatt G, Schemitsch EH, Zura RD, et al. Total Hip Arthroplasty or Hemiarthroplasty for Hip Fracture. N Engl J Med. 2019;381: 2199–2208. doi: 10.1056/NEJMoa1906190 [DOI] [PubMed] [Google Scholar]
- 10.Middleton RG, Uzoigwe CE, Young PS, Smith R, Gosal HS, Holt G. Peri-operative mortality after hemiarthroplasty for fracture of the hip: does cement make a difference? Bone Joint J. 2014;96-B: 1185–1191. doi: 10.1302/0301-620X.96B9.33935 [DOI] [PubMed] [Google Scholar]
- 11.Grammatopoulos G, Wilson HA, Kendrick BJL, Pulford EC, Lippett J, Deakin M, et al. Hemiarthroplasty using cemented or uncemented stems of proven design: a comparative study. Bone Joint J. 2015;97-B: 94–99. doi: 10.1302/0301-620X.97B1.34138 [DOI] [PubMed] [Google Scholar]
- 12.Li T, Zhuang Q, Weng X, Zhou L, Bian Y. Cemented versus uncemented hemiarthroplasty for femoral neck fractures in elderly patients: a meta-analysis. PLoS One. 2013;8: e68903. doi: 10.1371/journal.pone.0068903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin FF, Chen YF, Chen B, Lin CH, Zheng K. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: A meta-analysis of randomized controlled trails. Medicine. 2019;98: e14634. doi: 10.1097/MD.0000000000014634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology. 2009. pp. e1–e34. doi: 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 15.Zhao Y, Yang S, Ding W. Unilateral versus bilateral pedicle screw fixation in lumbar fusion: A systematic review of overlapping meta-analyses. PLoS One. 2019;14: e0226848. doi: 10.1371/journal.pone.0226848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85: 1–3. Available: https://www.ncbi.nlm.nih.gov/pubmed/12533564 [PubMed] [Google Scholar]
- 17.Slobogean G, Bhandari M. Introducing levels of evidence to the Journal of Orthopaedic Trauma: implementation and future directions. J Orthop Trauma. 2012;26: 127–128. doi: 10.1097/BOT.0b013e318247c931 [DOI] [PubMed] [Google Scholar]
- 18.Shea BJ, Bouter LM, Peterson J, Boers M, Andersson N, Ortiz Z, et al. External validation of a measurement tool to assess systematic reviews (AMSTAR). PLoS One. 2007;2: e1350. doi: 10.1371/journal.pone.0001350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62: 1013–1020. doi: 10.1016/j.jclinepi.2008.10.009 [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354: 1896–1900. doi: 10.1016/s0140-6736(99)04149-5 [DOI] [PubMed] [Google Scholar]
- 21.Oxman AD, Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol. 1991;44: 1271–1278. doi: 10.1016/0895-4356(91)90160-b [DOI] [PubMed] [Google Scholar]
- 22.Jadad AR, Cook DJ, Browman GP. A guide to interpreting discordant systematic reviews. CMAJ. 1997;156: 1411–1416. Available: https://www.ncbi.nlm.nih.gov/pubmed/9164400 [PMC free article] [PubMed] [Google Scholar]
- 23.Pieper D, Antoine S-L, Mathes T, Neugebauer EAM, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67: 368–375. doi: 10.1016/j.jclinepi.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 24.Liu B, Li A, Wang J, Wang H, Zhai G, Ma H, et al. Cemented versus uncemented hemiarthroplasty for elderly patients with displaced fracture of the femoral neck: A PRISMA-compliant meta-analysis of randomized controlled trial. Medicine. 2020;99: e21731. doi: 10.1097/MD.0000000000021731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kong X. Meta-analysis of the effect of cemented and uncemented hemiarthroplasty on displaced femoral neck fracture in the elderly. Exp Ther Med. 2020;20: 2173–2183. doi: 10.3892/etm.2020.8921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li N, Zhong L, Wang C, Xu M, Li W. Cemented versus uncemented hemi-arthroplasty for femoral neck fractures in elderly patients: A systematic review and meta-analysis of randomized controlled trials. Medicine. 2020;99: e19039. doi: 10.1097/MD.0000000000019039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luo X, He S, Li Z, Huang D. Systematic review of cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures in older patients. Arch Orthop Trauma Surg. 2012;132: 455–463. doi: 10.1007/s00402-011-1436-9 [DOI] [PubMed] [Google Scholar]
- 28.Kumar P, Rajnish RK, Neradi D, Kumar V, Agarwal S, Aggarwal S. Hemiarthroplasty for neck of femur fractures: to cement or not? A systematic review of literature and meta-analysis. Eur J Orthop Surg Traumatol. 2019;29: 731–746. doi: 10.1007/s00590-019-02364-z [DOI] [PubMed] [Google Scholar]
- 29.Azegami S, Gurusamy KS, Parker MJ. Cemented versus uncemented hemiarthroplasty for hip fractures: a systematic review of randomised controlled trials. Hip Int. 2011;21: 509–517. doi: 10.5301/HIP.2011.8640 [DOI] [PubMed] [Google Scholar]
- 30.Ning G-Z, Li Y-L, Wu Q, Feng S-Q, Li Y, Wu Q-L. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: an updated meta-analysis. Eur J Orthop Surg Traumatol. 2014;24: 7–14. doi: 10.1007/s00590-012-1151-4 [DOI] [PubMed] [Google Scholar]
- 31.Veldman HD, Heyligers IC, Grimm B, Boymans TAEJ. Cemented versus cementless hemiarthroplasty for a displaced fracture of the femoral neck: a systematic review and meta-analysis of current generation hip stems. Bone Joint J. 2017;99-B: 421–431. doi: 10.1302/0301-620X.99B4.BJJ-2016-0758.R1 [DOI] [PubMed] [Google Scholar]
- 32.Kumar NN, Kunutsor SK, Fernandez MA, Dominguez E, Parsons N, Costa ML, et al. Effectiveness and safety of cemented and uncemented hemiarthroplasty in the treatment of intracapsular hip fractures. The Bone & Joint Journal. 2020. pp. 1113–1121. doi: 10.1302/0301-620x.102b9.bjj-2020-0282.r1 [DOI] [PubMed] [Google Scholar]
- 33.Li L, Zhao X, Yang X, Yang L, Xing F, Tang X. Cemented versus uncemented hemiarthroplasty for the management of femoral neck fractures in the elderly: a meta-analysis and systematic review. Arch Orthop Trauma Surg. 2021;141: 1043–1055. doi: 10.1007/s00402-020-03737-4 [DOI] [PubMed] [Google Scholar]
- 34.Konan S, Abdel MP, Haddad FS. Cemented versus uncemented hip implant fixation: Should there be age thresholds? Bone Joint Res. 2019;8: 604–607. doi: 10.1302/2046-3758.812.BJR-2019-0337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maggs J, Wilson M. The Relative Merits of Cemented and Uncemented Prostheses in Total Hip Arthroplasty. Indian J Orthop. 2017;51: 377–385. doi: 10.4103/ortho.IJOrtho_405_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR, et al. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA. 2011;305: 1560–1567. doi: 10.1001/jama.2011.478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brox WT, Roberts KC, Taksali S, Wright DG, Wixted JJ, Tubb CC, et al. The American Academy of Orthopaedic Surgeons Evidence-Based Guideline on Management of Hip Fractures in the Elderly. J Bone Joint Surg Am. 2015;97: 1196–1199. doi: 10.2106/JBJS.O.00229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huette P, Abou-Arab O, Djebara A-E, Terrasi B, Beyls C, Guinot P-G, et al. Risk factors and mortality of patients undergoing hip fracture surgery: a one-year follow-up study. Sci Rep. 2020;10: 9607. doi: 10.1038/s41598-020-66614-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garland A, Gordon M, Garellick G, Kärrholm J, Sköldenberg O, Hailer NP. Risk of early mortality after cemented compared with cementless total hip arthroplasty: a nationwide matched cohort study. Bone Joint J. 2017;99-B: 37–43. doi: 10.1302/0301-620X.99B1.BJJ-2016-0304.R1 [DOI] [PubMed] [Google Scholar]
- 40.Okike K, Chan PH, Prentice HA, Paxton EW, Burri RA. Association Between Uncemented vs Cemented Hemiarthroplasty and Revision Surgery Among Patients With Hip Fracture. JAMA. 2020;323: 1077–1084. doi: 10.1001/jama.2020.1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khan T, Middleton R, Alvand A, Manktelow ARJ, Scammell BE, Ollivere BJ. High mortality following revision hip arthroplasty for periprosthetic femoral fracture. Bone Joint J. 2020;102-B: 1670–1674. doi: 10.1302/0301-620X.102B12.BJJ-2020-0367.R1 [DOI] [PubMed] [Google Scholar]
- 42.Murray DW. Cemented femoral fixation: the North Atlantic divide. Bone Joint J. 2013;95-B: 51–52. doi: 10.1302/0301-620X.95B11.32976 [DOI] [PubMed] [Google Scholar]
- 43.Yamada H, Yoshihara Y, Henmi O, Morita M, Shiromoto Y, Kawano T, et al. Cementless total hip replacement: past, present, and future. J Orthop Sci. 2009;14: 228–241. doi: 10.1007/s00776-008-1317-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rolfson O, Donahue GS, Hallsten M, Garellick G, Kärrholm J, Nemes S. Patient-reported outcomes in cemented and uncemented total hip replacements. Hip Int. 2016;26: 451–457. doi: 10.5301/hipint.5000371 [DOI] [PubMed] [Google Scholar]
- 45.Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. 2010;7: e1000326. doi: 10.1371/journal.pmed.1000326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Siontis KC, Hernandez-Boussard T, Ioannidis JPA. Overlapping meta-analyses on the same topic: survey of published studies. BMJ. 2013;347: f4501. doi: 10.1136/bmj.f4501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scott J, Checketts JX, Cooper CM, Boose M, Wayant C, Vassar M. An Evaluation of Publication Bias in High-Impact Orthopaedic Literature. JB JS Open Access. 2019;4: e0055. doi: 10.2106/JBJS.OA.18.00055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reddy AK, Anderson JM, Gray HM, Fishbeck K, Vassar M. Clinical Trial Registry Use in Orthopaedic Surgery Systematic Reviews. J Bone Joint Surg Am. 2021;103: e41. doi: 10.2106/JBJS.20.01743 [DOI] [PubMed] [Google Scholar]
- 49.Conn VS, Valentine JC, Cooper HM, Rantz MJ. Grey literature in meta-analyses. Nurs Res. 2003;52: 256–261. doi: 10.1097/00006199-200307000-00008 [DOI] [PubMed] [Google Scholar]
- 50.McAuley L, Pham B, Tugwell P, Moher D. Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? Lancet. 2000;356: 1228–1231. doi: 10.1016/S0140-6736(00)02786-0 [DOI] [PubMed] [Google Scholar]
- 51.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6: e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Provencher MT, Brand JC, Rossi MJ, Lubowitz JH. Are Orthopaedic Systematic Reviews Overly Prevalent? Arthroscopy. 2016;32: 955–956. doi: 10.1016/j.arthro.2016.04.005 [DOI] [PubMed] [Google Scholar]
- 53.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007;28: 105–114. doi: 10.1016/j.cct.2006.04.004 [DOI] [PubMed] [Google Scholar]
- 54.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7: 177–188. doi: 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 55.Lau J, Ioannidis JP, Schmid CH. Summing up evidence: one answer is not always enough. Lancet. 1998;351: 123–127. doi: 10.1016/S0140-6736(97)08468-7 [DOI] [PubMed] [Google Scholar]
- 56.Petitti DB. Approaches to heterogeneity in meta-analysis. Stat Med. 2001;20: 3625–3633. doi: 10.1002/sim.1091 [DOI] [PubMed] [Google Scholar]
- 57.Sonne-Holm S, Walter S, Steen Jensen J. Moore Hemi-Arthroplasty with and Without Bone Cement in Femoral Neck Fractures:A Clinical Controlled Trial. Acta Orthopaedica Scandinavica. 1982. pp. 953–956. doi: 10.3109/17453678208992854 [DOI] [PubMed] [Google Scholar]
- 58.Dorr LD, Glousman R, Hoy AL, Vanis R, Chandler R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J Arthroplasty. 1986;1: 21–28. doi: 10.1016/s0883-5403(86)80006-7 [DOI] [PubMed] [Google Scholar]
- 59.Emery RJ, Broughton NS, Desai K, Bulstrode CJ, Thomas TL. Bipolar hemiarthroplasty for subcapital fracture of the femoral neck. A prospective randomised trial of cemented Thompson and uncemented Moore stems. J Bone Joint Surg Br. 1991;73: 322–324. doi: 10.1302/0301-620X.73B2.2005165 [DOI] [PubMed] [Google Scholar]
- 60.Figved W, Opland V, Frihagen F, Jervidalo T, Madsen JE, Nordsletten L. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clin Orthop Relat Res. 2009;467: 2426–2435. doi: 10.1007/s11999-008-0672-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moroni A, Pegreffi F, Romagnoli M, Hoang-Kim A, Tesei F, Giannini S. RESULTS IN OSTEOPOROTIC FEMORAL NECK FRACTURES TREATED WITH CEMENTED VS UNCEMENTED HIP ARTHROPLASTY. Orthopaedic Proceedings. 2009;91-B: 167–167. doi: 10.1302/0301-620X.91BSUPP_I.0910167b [DOI] [Google Scholar]
- 62.DeAngelis JP, Ademi A, Lewis CG. Cemented Versus Uncemented Hemiarthroplasty for Displaced Femoral Neck Fractures: A Prospective Randomized Trial With Early Follow-up. J Orthop Trauma. 2012;26: 135. doi: 10.1097/BOT.0b013e318238b7a5 [DOI] [PubMed] [Google Scholar]
- 63.Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am. 2012;94: 577–583. doi: 10.2106/JBJS.K.00006 [DOI] [PubMed] [Google Scholar]
- 64.Talsnes O, Hjelmstedt F, Pripp AH, Reikerås O, Dahl OE. No difference in mortality between cemented and uncemented hemiprosthesis for elderly patients with cervical hip fracture.A prospective randomized study on 334 patients over 75 years. Archives of Orthopaedic and Trauma Surgery. 2013. pp. 805–809. doi: 10.1007/s00402-013-1726-5 [DOI] [PubMed] [Google Scholar]
- 65.Langslet E, Frihagen F, Opland V, Madsen JE, Nordsletten L, Figved W. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin Orthop Relat Res. 2014;472: 1291–1299. doi: 10.1007/s11999-013-3308-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Inngul C, Blomfeldt R, Ponzer S, Enocson A. Cemented versus uncemented arthroplasty in patients with a displaced fracture of the femoral neck: a randomised controlled trial. Bone Joint J. 2015;97-B: 1475–1480. doi: 10.1302/0301-620X.97B11.36248 [DOI] [PubMed] [Google Scholar]
- 67.Harper WM, Gregg PJ. The treatment of intracapsular proximal femoral fractures: a randomized prospective trial. J Bone Joint Surg Br. [Google Scholar]
- 68.Branfoot T, Faraj AA, Porter P. Cemented versus uncemented Thompson’s prosthesis: a randomised prospective functional outcome study. Injury. [DOI] [PubMed] [Google Scholar]
- 69.Santini S, Rebeccato A, Bolgan I, Turi G. Hip fractures in elderly patients treated with bipolar hemiarthroplasty: comparison between cemented and cementless implants. J Orthop Traumatol. 2005;6: 80–87. doi: 10.1007/s10195-005-0086-5 [DOI] [Google Scholar]
- 70.Parker MI, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures: A randomised controlled trial in 400 patients. J Bone Joint Surg Br. 2010;92: 116–122. doi: 10.1302/0301-620X.92B1.22753 [DOI] [PubMed] [Google Scholar]
- 71.Cumming D, Parker MJ. Randomised trial of cemented versus uncemented hemiarthroplasty for displaced intracapsular fractures. Injury Extra. 2007. p. 25. doi: 10.1016/j.injury.2006.06.083 [DOI] [Google Scholar]
- 72.Sadr B, Arden GP. A comparison of the stability of proplast-coated and cemented Thompson prostheses in the treatment of subcapital femoral fractures. Injury. 1977;8: 234–237. doi: 10.1016/0020-1383(77)90137-1 [DOI] [PubMed] [Google Scholar]
- 73.Vidovic D, Matejcic A, Punda M, Ivica M, Tomljenovic M, Bekavac-Beslin M, et al. Periprosthetic bone loss following hemiarthroplasty: a comparison between cemented and cementless hip prosthesis. Injury. 2013;44 Suppl 3: S62–6. doi: 10.1016/S0020-1383(13)70201-8 [DOI] [PubMed] [Google Scholar]
- 74.Barenius B, Inngul C, Alagic Z, Enocson A. A randomized controlled trial of cemented versus cementless arthroplasty in patients with a displaced femoral neck fracture: a four-year follow-up. Bone Joint J. 2018;100-B: 1087–1093. doi: 10.1302/0301-620X.100B8.BJJ-2017-1593.R1 [DOI] [PubMed] [Google Scholar]
- 75.Moerman S, Mathijssen NMC, Niesten DD, Riedijk R, Rijnberg WJ, Koëter S, et al. More complications in uncemented compared to cemented hemiarthroplasty for displaced femoral neck fractures: a randomized controlled trial of 201 patients, with one year follow-up. BMC Musculoskeletal Disorders. 2017. doi: 10.1186/s12891-017-1526-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Parker MJ, Cawley S. Cemented or uncemented hemiarthroplasty for displaced intracapsular fractures of the hip: a randomized trial of 400 patients. Bone Joint J. 2020;102-B: 11–16. doi: 10.1302/0301-620X.102B1.BJJ-2019-1041.R1 [DOI] [PubMed] [Google Scholar]
- 77.Vidović D, Punda M, Daraboš N, Bekavac-Bešlin M, Bakota B, Matejčić A. Regional bone loss following femoral neck fracture: A comparison between cemented and cementless hemiarthroplasty. Injury. 2015;46 Suppl 6: S52–6. doi: 10.1016/j.injury.2015.10.069 [DOI] [PubMed] [Google Scholar]
- 78.Khorami M, Arti H, Aghdam AA. Cemented versus uncemented hemiarthroplasty in patients with displaced femoral neck fractures. Pak J Med Sci Q. 2016;32: 44–48. doi: 10.12669/pjms.321.8461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jianguo LI. Comparison of the effects and complications of biotype and cement-based artificial hip prosthesis in the treatment of femoral neck fracture in the elderly. Clinical Medicine of China. 2017; 1127–1130. doi: 10.3760/cma.j.issn.1008-6315.2017.12.017 [DOI] [Google Scholar]
- 80.Ma C, Jiang F, Huang C, Liu Z. Contrast of effect and prognosis of artificial hip joint maken by biomaterials and bone-cement for femoral neck fracture. Jianyan Yixue Yu Linchuang. [Google Scholar]
- 81.Prashanth YS, Niranjan M. Comparative Study of Surgical Management of Fracture Neck of Femur with Cemented Versus Uncemented Bipolar Hemiarthroplasty. J Clin Diagn Res. 2017;11: RC17–RC21. doi: 10.7860/JCDR/2017/22598.9454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mohabey AV, Warjukar PR, Ravikumar M. Functional outcome of cemented versus uncemented modular bipolar hemiarthroplasty in proximal femoral neck fractures. Int J Orthop Sci. 2017;3: 609–611. doi: 10.22271/ortho.2017.v3.i4i.83 [DOI] [Google Scholar]
- 83.Movrin I, Department of Traumatology, University Medical Centre Maribor, Maribor, Slovenia. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: A randomized controlled trial with two years follow-up. Acta Orthopaedica et Traumatologica Turcica. 2020. pp. 83–88. doi: 10.5152/j.aott.2020.01.432 [DOI] [PMC free article] [PubMed]
- 84.Du Z. Analysis of the effect of cemented and uncemented artificial double femoral head replacement. Chin Med Eng. 2014, pp. 29–30 [Google Scholar]
- 85.Pan S. Comparison of the effects of cemented and uncemented hemiarthroplasty in the treatment of displaced femoral neck fractures. Chin J Postgrad Med. 2013, 36: 41–43 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
The data are available in the paper and on the Open Science Framework repository (https://osf.io/vh8es/).