Abstract
Background and Objectives
With the onset of the COVID-19 pandemic, there has been a significant decrease in colorectal cancer (CRC) screening leading to delayed diagnoses and increased cancer deaths. To mitigate these burgeoning gaps in care, we developed a medical student-led service learning project aimed at improving rates of colorectal cancer screening at the Farrell Health Center (FHC), a primary care practice within the Ambulatory Care Network (ACN) at New York-Presbyterian Hospital.
Methods
A cohort of 973 FHC patients aged 50–75 years were identified as possibly overdue for screening. Student volunteers reviewed patient charts to confirm screening eligibility and then contacted patients to offer colonoscopy or stool DNA test. Following the patient outreach intervention, medical student volunteers completed a questionnaire to assess the educational value for the service-learning experience.
Results
Fifty-three percent of identified patients were due for CRC screening; 67.8% of eligible patients were reached by volunteers. Among the patients reached, 47.0% were referred for CRC screening. No statistical significance was observed between likelihood of CRC screening acceptance and patient age or sex; 87% of medical student volunteers felt that the service-learning project was a valuable educational experience.
Conclusion
The student-led patient telehealth outreach program is an effective model for identifying and referring patients overdue for CRC screening and an enriching educational experience for preclinical medical students. The structure provides a valuable framework to address gaps in health care maintenance.
Introduction
In March 2020, New York City became the epicenter of the COVID-19 crisis. Disruptions in higher education alongside widespread desire to support the front lines led to the formation of Columbia University’s COVID-19 Student Service Corps (CSSC).1
The recommendation to delay elective procedures, including colonoscopies, as well as interruptions to routine health care maintenance visits decreased colorectal cancer (CRC) screening.2–4 Prepandemic colonoscopy screening rates showed underutilization—only 67% of 50–75-year-old adults and 44% of underinsured/uninsured individuals were up to date on CRC screening.5–7 By April 2021, colonoscopies had plummeted to 50% of the prior year.5,8 In a pandemic that has deepened health inequities, underresourced communities are particularly vulnerable to delays in CRC screening.9,10 Inspiration from prior CRC screening community projects mitigating health care gaps driven by insurance access, race, educational attainment, and income levels provided the foundation for the formation of this novel medical student service-learning project.11–15
Our team sought to address both the disruption in medical education and gaps in CRC screening by developing a telehealth-based outreach program. Our aim was twofold: (1) increase referrals for colorectal cancer screening, and (2) provide a service-learning opportunity with direct patient interaction for preclinical medical students.
Methods
Settings and Participants
This program was implemented at the Farrell Health Center (FHC), a family medicine practice at New York-Presbyterian Hospital providing care to medically underserved communities in Washington Heights, Inwood, and the Bronx. The FHC Institutional Review Board approved the program as quality improvement (AAAT3817). Nine hundred seventy-three patients were identified as overdue for screening (Figure 1). Eligibility included patients aged 50–75 years with no electronic medical record (EMR) documentation of a colonoscopy in the previous 10 years or fecal immunochemical test in the last 3 years. Fecal DNA testing was not in use at the clinic prior to this project.
Figure 1.
Enrollment in CRC Screening Project Consort Diagram
Abbreviations: CRC, colorectal cancer; ACN, accountable care network.
*Note: ineligibility is defined as any patient found to have had CRC screening within the screening appropriate time period and clear prior results within or outside the ACN network. Volunteers conducted thorough chart reviews and contacted outside clinics for documentation of prior procedures.
Project Structure
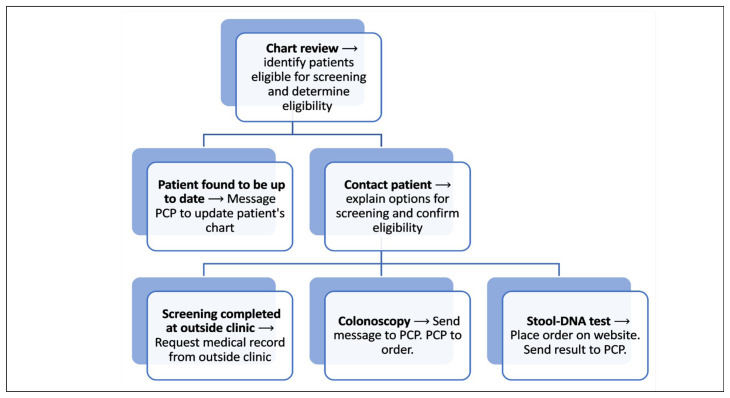
A team of three student leads and a supervising physician oversaw 49 student volunteers (37 medical students, 12 other medical-related students). Approximately 80% of volunteers were first-year medical students randomly selected to participate in this project as part of their preclinical curriculum. Service-learning objectives emphasized patient-centered care and communication (Figure 2). After the 6-week course, medical students were asked to complete a survey about their experience.16
Figure 2.
CRC Telemedicine Project Workflow for Student Volunteers
Student leads wrote English and Spanish call scripts for telephone encounters, providing uniform language and standardized screening questions to determine patient eligibility.17 Scripts were designed to heighten patients’ medical literacy by providing detailed information on available CRC options while guiding them through the decision-making process. Volunteers used Doximity, a HIPAA-compliant application, to call patients from the clinic’s phone number. Pacific Interpreter services were used when communicating with non-English-speaking patients.
Description of the Clinic Outreach Intervention
Volunteers used scripts to confirm patient eligibility and discuss the advantages and disadvantages of each test to allow for patient autonomy in the decision-making process. Following a screening decision, volunteers documented the telephone encounter in the EMR, messaged the primary care physician (PCP) summarizing the screening decision, and documented the patient encounter within an encrypted spreadsheet for internal review (Figure 2).
Data Analysis
We performed retrospective analysis with univariate descriptive statistics for eligible patients who were referred for CRC screening, patients who declined screenings, and patients unable to be reached. Bivariate χ2 test of independence compared screening decision against patients’ age, sex, and primary language. We also ran univariate statistics for postproject student survey results.
Results
Our chart review confirmed 53.5% (n=521) of all patients within the eligible age range as due for CRC screening. 373 (71.6%) of these patients were female (Table 1). 53.6% of patients reported Spanish and 33.2% reported English as their primary language. Volunteers successfully reached 338 (64.8%) of eligible patients. Fifty percent (n=170) of contacted patients were referred for CRC screening (55 for stool DNA test and 115 for colonoscopy); 15.1% (n=51) of contacted patients disclosed having a CRC screening in the last 10 years and 22.5% declined screening (n=117, Figure 1). A statistically significant relationship was found between patients’ primary language and CRC screening decision (P value <.01, Table 2).
Table 1.
Demographics of Eligible Patients
| Patient Demographics | n | % |
|---|---|---|
| Sex | ||
| Male | 148 | 28.4 |
| Female | 373 | 71.6 |
| Language | ||
| English | 173 | 33.2 |
| Spanish | 279 | 53.6 |
| Other1 | 43 | 8.2 |
| Unknown | 26 | 5.0 |
| Age (years) | ||
| Min | 50 | |
| Mean | 62 | |
| Max | 76 |
Note: Patient demographic information was derived from electronic medical record and not directly from the patient.
Other is a language category from the electronic medical record system reflecting patient self-selected categorization from intake forms, doctor visits, or patient preference.
Table 2.
Colorectal Cancer Screening Decisions Against Patient Demographics
| Prior Screening N (% Overall) (% Contacted‡) | Colonoscopy N (% Overall) (% Contacted‡) | Cologuard N (% Overall) (% Contacted‡) | Not Interested / Refused N (% Overall) (% Contacted‡) | Could Not Be Reached N (% Overall) | X2 | P Value | |
|---|---|---|---|---|---|---|---|
| All | |||||||
| 51 (9.8) (15.1) | 115 (22.1) (34.0) | 55 (10.6) (16.3) | 117 (22.4) (34.6) | 183 (35.1) | |||
| Sex | |||||||
| Male | 11 (2.1) (11.8) | 35 (6.7) (37.6) | 13 (2.5) (14.0) | 34 (6.5) (36.6) | 55 (10.6) | 2.29 | .68 |
| Female | 40 (7.7) (16.3) | 80 (15.4) (32.7) | 42 (8.1) (17.1) | 83 (15.9) (33.9) | 128 (24.6) | ||
| Language | |||||||
| English | 13 (2.5) (10.7) | 43 (8.3) (35.2) | 25 (4.8) (20.5) | 41 (7.9) (33.6) | 51 (9.8) | 20.0 | <.01* |
| Spanish | 33 (6.3) (18.1) | 65 (12.5) (35.7) | 21 (4.1) (11.6) | 63 (12.1) (34.6) | 97 (18.6) | ||
| Other | 5 (1.0) (14.7) | 7 (1.3) (20.6) | 9 (1.7) (26.5) | 13 (2.5) (38.2) | 35 (6.7) | ||
| Age (Years) | |||||||
| 50–54 | 6 (1.2) (9.2) | 28 (5.4) (43.1) | 10 (1.9) (15.4) | 21 (4.0) (32.3) | 37 (7.1) | 8.09 | .94 |
| 55–59 | 10 (1.9) (14.9) | 26 (5.0) (38.9) | 11 (2.1) (16.4) | 20 (3.8) (29.8) | 37 (7.1) | ||
| 60–64 | 12 (2.3) (18.8) | 16 (3.1) (25.0) | 11 (2.1) (17.2) | 25 (4.8) (39.0) | 37 (7.1) | ||
| 65–69 | 12 (2.3) (17.9) | 21 (4.0) (31.3) | 12 (2.3) (17.9) | 22 (4.2) (32.9) | 34 (6.5) | ||
| 70–76 | 11 (2.1) (14.7) | 24 (4.6) (32.0) | 11 (2.1) (14.7) | 29 (5.6) (38.6) | 38 (7.3) | ||
Denotes statistical significance
Denotes a percentage of the observed value over the total number of persons contacted. This percentage excludes those who could not be reached from the total population.
Statistically significant differences between colorectal cancer screening decisions were only found for the language of participant: English, Spanish, or Other (<0.01). Other category is comprised of all language outside of English or Spanish predetermined from the electronic medical record system used to extract patient demographic information.
The postclerkship survey was completed by 62.2% (n=23) of all medical student volunteers (n=37). Of all survey respondents, 86.9% (n=20) reported that this service-learning experience was valuable to their preclinical education; 86.9% (n=20) felt the project made them more comfortable speaking to patients; and 78.3% (n=18) reported improved understanding of health care delivery (Figure 3).
Figure 3.
CRC Student Volunteers Postproject Survey Responses
Discussion
The student-led patient telehealth outreach program is an effective model for identifying patients overdue for CRC screening and addressing gaps in healthcare maintenance, particularly during the COVID-19 pandemic, and is also a valuable service-learning experience for preclinical medical students.
At project onset, roughly less than 50% of patients were up to date on screening.7,9 Pandemic-related health care disruptions, health care hesitancy, and psychosocial stressors likely contributed to lower screening rates.18–20 Of patients contacted, half were referred for CRC screening demonstrating interest in being screened by the target population. Colonoscopy was selected more frequency than stool DNA test, likely impacted by the more stringent eligibility criteria for stool DNA tests and hesitancy to try new technology. Historically, Spanish-speaking patients’ CRC screening outcomes have lagged behind those of native English speakers.21 In this project, patients selected CRC screening at comparable frequencies regardless of language. Use of professional interpreter services in addition to extensive patient communication training for student volunteers increased CRC screening referrals at similar rates for both English and Spanish speakers. Future iterations of this project should track patient screening outcomes to confirm this finding.
In addition, the project provided medical students with an early opportunity to communicate clinical information with patients. During weekly discussion sessions, students reflected on patient barriers to accessing care in underresourced communities identified during patient calls.
Limitations include difficulty with record reconciliation from external sites, selection bias from uncontactable patients, and insufficient infrastructure to assess screening outcomes (eg, cancer detection). In the future, assessment of the project’s true educational impact would be improved by surveying medical student volunteers pre- and postproject, not by self-reported qualitative metrics but with robust objective structured clinical evaluations evaluating student-patient communication. Additionally, screening eligibility criteria based on the United States Preventative Services Task Force 2020 Guidelines have since expanded to adults aged 45–49 years and future iterations of this program should adjust eligibility criteria.
In conclusion, this CRC screening project demonstrated the utility and educational value of student volunteer-led outreach interventions, with potential to add value outside the context of a pandemic. Future directions include incorporating screening for breast and cervical cancer as well as implementing a systemic review process to determine outcomes of screening referrals.
Acknowledgments
The authors thank Urmi Desai, MD, the CSSC Faculty Co-Chair, and all CSSC Colorectal Cancer Screening student volunteers.
Presentations: This study was presented at the 2021 STFM Conference on Practice and Quality Improvement, September 2021 (virtual).
References
- 1. Grilo SA, Catallozzi M, Desai U, et al. Columbia COVID-19 Student Service Corps: harnessing student skills and galvanizing the power of service learning. [published online ahead of print, 2020 Nov 18] FASEB Bioadv. 2020;3(3):166–174. doi: 10.1096/fba.2020-00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CMS adult elective surgery and procedures recommendations. Centers for Medicare & Medicaid Services; [Accessed March 23, 2020]. Published 2020. https://www.cms.gov/files/document/31820-cms-adult-elective-surgery-and-procedures-recommendations.pdf . [Google Scholar]
- 3. Issaka RB, Taylor P, Baxi A, Inadomi JM, Ramsey SD, Roth J. Model-Based Estimation of Colorectal Cancer Screening and Outcomes During the COVID-19 Pandemic. JAMA Netw Open. 2021;4(4):e216454. doi: 10.1001/jamanetworkopen.2021.6454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.A Playbook for Reigniting Colorectal Cancer Screening as Communities Respond to the COVID-19 Pandemic. National Colorectal Cancer Roundtable; Retrieved December 10, 2020 from https://nccrt.org/resource/a-playbook-for-reigniting-colorectal-cancer-screening-as-communities-respond-to-the-covid-19-pandemic/ [Google Scholar]
- 5.Martin K, Kurowski D, Given P, Kennedy K, Clayton E. The impact of COVID-19 on the use of preventive health care. Health Care Cost Institute; [Accessed June 21, 2020]. Published 2020. Updated September 9, 2020. https://healthcostinstitute.org/hcci-research/the-impact-of-covid-19-on-the-use-of-preventive-health-care . [Google Scholar]
- 6.Cancer Stat Facts SEER: Colorectal Cancer. National Cancer Institute; https://seer.cancer.gov/statfacts/html/colorect.html . [Google Scholar]
- 7.Colorectal Cancer Facts & Figures 2020–2022. American Cancer Society; 2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-and-figures-2020-2022.pdf . [Google Scholar]
- 8.Colorectal cancer screening rates reach 44.1% in FQHCs in 2018. National Colorectal Cancer Roundtable; [Accessed August 20, 2020]. Published 2020. https://nccrt.org/colorectal-cancer-screening-rates-reach-44-1-in-fqhcs-in-2018/ [Google Scholar]
- 9. Balzora S, Issaka RB, Anyane-Yeboa A, Gray DM, II, May FP. Impact of COVID-19 on colorectal cancer disparities and the way forward. Gastrointest Endosc. 2020;92(4):946–950. doi: 10.1016/j.gie.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Delayed Cancer Screenings—A Second Look. Epic Health Research Network; [Accessed December 13, 2020]. from https://ehrn.org/articles/delayed-cancer-screenings-a-second-look/ [Google Scholar]
- 11. Baldwin LM, Schneider JL, Schwartz M, et al. First-year implementation of mailed FIT colorectal cancer screening programs in two Medicaid/Medicare health insurance plans: qualitative learnings from health plan quality improvement staff and leaders. BMC Health Serv Res. 2020;20(1):132. doi: 10.1186/s12913-019-4868-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mehta SJ, Jensen CD, Quinn VP, et al. Race/Ethnicity and Adoption of a Population Health Management Approach to Colorectal Cancer Screening in a Community-Based Healthcare System. J Gen Intern Med. 2016;31(11):1323–1330. doi: 10.1007/s11606-016-3792-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cruz-Correa M, Cordero F, Betancourt JP, et al. Implementation and Outcomes of a Community-Based Educational Program for Colorectal Cancer Prevention in Hispanics. J Fam Med Dis Prev. 2016;2(3):42. doi: 10.23937/2469-5793/1510042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Decker KM, Demers AA, Nugent Z, Biswanger N, Singh H. Reducing income-related inequities in colorectal cancer screening: lessons learned from a retrospective analysis of organised programme and non-programme screening delivery in Winnipeg, Manitoba. BMJ Open. 2016;6(2):e009470. doi: 10.1136/bmjopen-2015-009470. Published 2016 Feb 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Davis MM, Freeman M, Shannon J, et al. A systematic review of clinic and community intervention to increase fecal testing for colorectal cancer in rural and low-income populations in the United States - How, what and when? BMC Cancer. 2018;18(1):40. doi: 10.1186/s12885-017-3813-4. Published 2018 Jan 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drastal M.Student led covid-19 colorectal cancer screening telemedicine initiative post-volunteer survey. Student Led Covid-19 Colorectal Cancer Screening Telemedicine Initiative Post-Volunteer Survey STFM Resource Library. [Accessed July 25, 2022]. Published July 8, 2022. https://resourcelibrary.stfm.org/viewdocument/student-led-covid-19-colorectal-can?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments .
- 17.Drastal M. Call script for a patient needing colorectal cancer (CRC) screening in the student-led CRC telemedicine initiative. Student Led Covid-19 Colorectal Cancer Screening Telemedicine Initiative Post-Volunteer Survey. STFM Resource Library; [Accessed July 25, 2022]. Published July 8, 2022. https://resourcelibrary.stfm.org/viewdocument/student-led-colorectal-cancer-scree?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments . [Google Scholar]
- 18. Jones RM, Devers KJ, Kuzel AJ, Woolf SH. Patient-reported barriers to colorectal cancer screening: a mixed-methods analysis. Am J Prev Med. 2010;38(5):508–516. doi: 10.1016/j.amepre.2010.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lasser KE, Ayanian JZ, Fletcher RH, Good MJ. Barriers to colorectal cancer screening in community health centers: a qualitative study. BMC Fam Pract. 2008;9(1):15. doi: 10.1186/1471-2296-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kullgren JT, McLaughlin CG, Mitra N, Armstrong K. Nonfinancial barriers and access to care for U.S. adults. Health Serv Res. 2012;47(1 Pt 2):462–485. doi: 10.1111/j.1475-6773.2011.01308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Diaz JA, Roberts MB, Goldman RE, Weitzen S, Eaton CB. Effect of language on colorectal cancer screening among Latinos and non-Latinos. Cancer Epidemiol Biomarkers Prev. 2008;17(8):2169–2173. doi: 10.1158/1055-9965.EPI-07-2692. [DOI] [PMC free article] [PubMed] [Google Scholar]