Abstract
Aim
The aim of this review was to determine whether the caregivers of breast cancer patients who undergo psychosocial interventions report improvements in quality of life (QOL), depression, and anxiety.
Methods
This systematic review was conducted in accordance with the PRISMA guidelines. A systematic search was conducted in the CINAHL, Embase, PsycINFO, PubMed, Web of Science, CNKI and Wanfang databases from inception until March 1, 2022. Randomized controlled trials (RCTs) and quasiexperimental studies involving psychosocial interventions for caregivers of breast cancer patients were included. Cochrane's risk of bias tool and the Joanna Briggs Institute checklist were used to assess the risk of bias.
Results
This systematic review included eight original studies involving 528 caregivers of breast cancer patients. According to the meta-analyses, psychosocial interventions contributed significantly to improvements in QOL (SMD = 1.00, 95% CI [0.47, 1.54], p < 0.01), depression (SMD = −0.72, 95% CI [-1.02, −0.42], p < 0.01) and anxiety (SMD = −0.56, 95% CI [-0.86, −0.27], p < 0.01). Significant differences of psychosocial interventions on the QOL of caregivers were found in face-to-face and mixed-method psychosocial interventions (SMD = 0.97, 95% CI [0.19,1.75], p = 0.02; SMD = 1.45, 95% CI [0.86,2.05], p < 0.01) in the ≥3 months subgroup (SMD = 1.22, 95% CI [0.58,1.86], p < 0.01) but not in the spouses or partners subgroup (SMD = 0.83, 95% CI [-0.10,1.75], p = 0.08).
Conclusions
This systematic review revealed that breast cancer patients' caregivers who undergo psychosocial interventions report improvements in QOL and reduced levels of depression and anxiety. It is worthwhile to use face-to-face methods when psychosocial interventions are conducted for caregivers. Future studies should examine long-term psychosocial interventions for spouses or partners of breast cancer patients. However, because of the limited number of original studies and the low quality of some included studies, the results should be treated cautiously. To increase solid evidence in this field, higher quality, more original studies are needed.
Keywords: Caregivers, Breast cancer, Psychosocial interventions, Quality of life, Depression, Anxiety, Meta-analysis
1. Introduction
Among females with malignant tumours, the incidence rate of breast cancer is the highest. There have been 7.8 million breast cancer diagnoses in women over the past five years, and 2.3 million were diagnosed in 2020 alone. In 2020, breast cancer killed 685,000 individuals worldwide [1].
Physical health, mental health, and social well-being are profoundly affected by breast cancer. Such effects may include dealing with the shock of a diagnosis as well as side effects associated with treatment, such as nausea, vomiting, and fatigue. Furthermore, body image issues can result in psychological distress due to hair loss and changes in the breast and weight. In addition, breast cancer patients' lives may be further affected by changes in their role and family functions, occupation or employment, and financial situation. Many women will also have to face worsening diseases and impending deaths [2].
As a consequence of disease symptoms and invasive treatments, patients with breast cancer suffer from physical and psychological problems. The disease also places great demands on primary caregivers, including spouses, partners, children, parents, and other relatives, who face numerous psychosocial challenges. First, caregivers suffer anxiety and fear for a long time because they are afraid of the death of their loved ones [3]. Second, after the diagnosis, the caregiver must take a large amount of responsibility for care without any prior preparation [4]. In addition, the high cost of treatment places a heavy financial burden on caregivers [5]. Caregiving has also been found to affect caregivers' social interaction and work. The fear of recurrence often still exists for caregivers. If breast cancer recurs, the mental health of caregivers may be worse than that of the normal population, and their emotional well-being scores may be slightly lower than even those of breast cancer patients [6]. Furthermore, caregivers lack knowledge about managing patients' symptoms, incontinence, diet, and complex cancer drug regimens [7,8]. Consequently, quality of life (QOL), depression, and anxiety are adversely affected.
Several studies have indicated that breast cancer reduces caregivers' QOL and increases psychological distress [[9], [10], [11]]. Researchers have found that male spouse caregivers for breast cancer patients had worse QOL than the general population [12]. Psychological distress and anxiety were found to be the same or higher than in cancer patients [[13], [14], [15]]. A total of 8.9%–60% of breast cancer caregivers reported symptoms of significant depression [12,[16], [17], [18], [19]]. Approximately 8.9%–41% of breast caregivers reported anxiety [16,19,20]. The psychological stress of caregivers has a negative impact on the QOL of cancer survivors. Caregivers who are distressed may be unable to offer essential support as a result of their own mental distress [21]. Therefore, there is a need for interventions to improve the QOL and psychological status of breast cancer caregivers.
The term psychosocial intervention refers to nonpharmacologic interventions that address psychological and social factors rather than biological ones. It includes different types of interventions that have been shown to improve symptoms, QOL, and social functioning. In accordance with the European Society for Medical Oncology (ESMO) guidelines. A variety of psychosocial interventions are available, including psychosocial counselling, psychotherapy, psychoeducation, and other supportive interventions [22].
Psychosocial interventions that improve caregivers' psychological health have been demonstrated to be effective. Social and/or psychological interventions provide caregivers with information, affective support, psychological support, or practical support that enhance their capacity to cope [23]. Recently, an increasing number of original studies have examined psychosocial interventions' impact on QOL, depression and anxiety in primary caregivers caring for breast cancer patients [9,[24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34]]. However, the measurements and outcomes vary between these studies. Therefore, psychosocial interventions for caregivers should be systematically reviewed.
Systematic reviews have been conducted to assess the impact of psychosocial interventions on cancer caregivers and have reported improvements in caregivers' QOL or a reduction in depression and anxiety symptoms [[35], [36], [37], [38], [39]]. These reviews covered a variety of cancer types and provided useful insights into psychosocial interventions for caregivers caring for cancer patients. There is no systematic review to provide comprehensive evidence for the effects of psychosocial interventions on the breast cancer survivors' caregivers. The aim of this systematic review was to summarize and synthesize research findings regarding the psychosocial interventions' effectiveness on quality of life, depression, and anxiety in the caregivers of breast cancer patients.
2. Methods
2.1. Design
The PRISMA guidelines were followed for the conduct of this systematic review. We registered the research protocol in PROSPERO with registration number CRD42021268412.
2.2. Eligibility criteria
2.2.1. Population
This review considered studies on primary caregivers of patients with breast cancer, such as spouses or partners, parents, siblings, children and friends. Participants provided physical, psychological, or emotional care and support to patients with breast cancer.
2.2.2. Intervention
This review considered studies that evaluated the effectiveness of psychosocial interventions in primary caregivers of patients with breast cancer. Psychosocial interventions were performed in many forms, such as educational counselling, supportive health education through any format, follow-up programs, psychological support, social support (social skills training) and the FOCUS (Family involvement, Optimistic attitude, Coping effectiveness Uncertainty reduction, and Symptom management) Program. The interventions included either single-component interventions or multicomponent interventions. Interventions that were patient-focused without specific intervention components for caregivers were excluded.
2.2.3. Comparison
This review included studies that compared psychosocial interventions with any form of usual care or standard care. Usual care or standard care involved routine psychosocial care, education, counselling or support.
2.2.4. Outcomes
This review included the outcomes measured at postintervention and follow-up as follows: the total scores of QOL, depression and anxiety.
2.2.5. Study design
The review included randomized controlled trials (RCTs) and quasiexperimental studies in English or Chinese. Studies without full-text articles were not included.
2.3. Search methods
The search strategy was developed based on the PICOS (P: primary caregivers of breast cancer patients; I: psychosocial interventions; C: usual care or support control; O: QOL, depression and anxiety; S: RCTs and quasiexperimental studies). By using PICOS components and a preliminary search in Web of Science, Embase, PsycINFO, CINAHL, PubMed, Cochrane Library, Wanfang and CNKI, the search strategy was developed. A number of databases, such as Web of Science, Embase, PsycINFO, CINAHL, PubMed, Wanfang and CNKI, were searched. The following search terms were used: (Breast Neoplasms/Breast Neoplasm*/Breast tumour*/Breast Cancer/Breast Carcinomas/Human Mammary Neoplasm*) AND (Caregiver*/Care Giver*/Family Caregiver*/Spouse/Caregiver*) AND (Supportive intervention*/supportive therapy/Supportive Health Education/Follow-Up Program/Psychosocial intervention/education/counselling/therapy/treatment/behavioral therapy/Psychological support/psychotherapy/psychoeducation/mindfulness/Social support/social-skill training). These keywords and similar terms were used to comprehensively search for applicable studies. In different databases, search terms differed slightly. The reference lists of included studies were also manually searched. Each database was searched from inception until March 1, 2022.
2.4. Selection process
To eliminate duplicate studies, EndNote X9 was used to import all searched records. The two researchers independently reviewed all studies. Study screening was conducted in two stages. The first step was to exclude ineligible studies by scrutinizing titles and abstracts. Additionally, the researchers read the full text of each study to identify those that were eligible. A third reviewer was consulted if there was any disagreement between the two independent reviewers.
2.5. Quality appraisal
We assessed the risk of bias for the included RCTs according to the Cochrane manual for systematic review of interventions. There are six recommended bias domains: selection bias, detection bias, performance bias, reporting bias, attrition bias, and seven other items for each item. The bias risk was classified as ‘low risk’, ‘unclear’ or ‘high risk’. For quasiexperimental studies, the Joanna Briggs Institute appraisal instrument was used. It evaluates the comparability of participants and treatments, as well as the clarity of the “cause” and “effect”, the presence of a control group, several measures of the outcome, complete follow-up, measurements of the outcomes in comparisons that are dependable, and appropriate statistical analysis. The two independent reviewers independently assessed each of the included studies. If there were disagreements, the two reviewers discussed them or invited a third reviewer to resolve them.
2.6. Data extraction
Two independent reviewers used standardized data extraction tools to extract the following data from the included studies: author, publication year, country, study design, sample size, demographics of participants, interventions, comparator, duration of the intervention, follow-up, outcomes and ratings scales. If there were disagreements, the two reviewers discussed them or invited a third reviewer to resolve them.
2.7. Synthesis
Meta-analysis was performed using RevMan 5.4. Due to the use of continuous variables, when using the same measuring tool, mean differences (MD) were selected for the combination of effect quantities; otherwise, standard mean differences (SMD) were selected. The results were summarized with 95% confidence intervals (CIs). Statistical significance was considered for p values < 0.05. The standard chi-square test and I-squared statistic were used to estimate statistical heterogeneity. To evaluate the between-study heterogeneity, the I2 statistic was used. In cases of nonsignificant heterogeneity, the pooled analysis was performed using a fixed model. In cases of significant heterogeneity, the pooled analysis was performed using a random-effects model. To ensure that the meta-analysis results were reliable and stable, sensitivity analyses were conducted in this review. Subgroup analyses were conducted on the effectiveness of psychosocial interventions on QOL based on intervention methods (face-to-face versus non-face-to-face versus mixed-method), relationship to breast cancer patients (spouses or partners versus other relatives), and follow-up durations (<3 months versus ≥3 months).
3. Results
3.1. Search outcomes
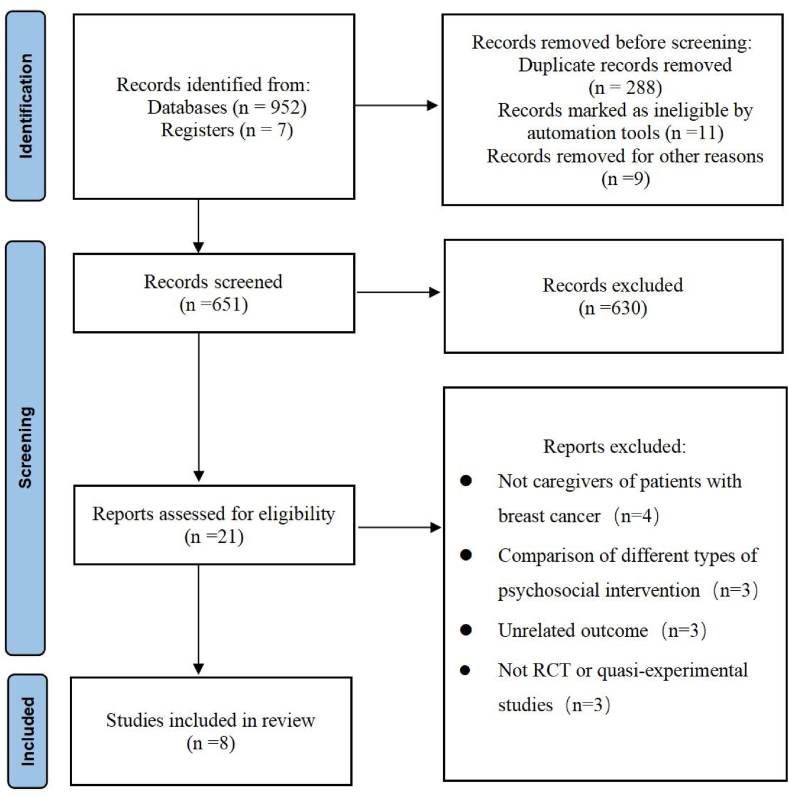
There were 959 records found by searching the databases and other sources. Following the removal of 308 duplicate records, 630 records were removed after screening the titles and abstracts. Next, after screening the full texts, 13 records were excluded for the following reasons: not caregivers of patients with breast cancer (n = 4), comparison of different types of psychosocial intervention (n = 3), unrelated outcomes (n = 3), and not RCTs or quasiexperimental studies (n = 3). Ultimately, 8 studies (6 RCTs and 2 quasiexperimental studies) were included [[26], [27], [28], [29], [30], [31], [32],34]. The PRISMA flow diagram is shown in Fig. 1.
Fig. 1.
The PRISMA flow diagram.
3.2. Description of the included studies
The included studies were from six countries: China (n = 3), the USA (n = 1), Iran (n = 1), Canada (n = 1), Nigeria (n = 1), and Italy (n = 1). The studies were published between 2009 and 2019. Six studies were RCTs, and two studies were quasiexperimental studies. A total of 528 caregivers were involved in this systematic review. The sample sizes ranged from 21 to 108. The caregivers of breast cancer patients were spouses, parents, children, siblings, or friends.
Forms of psychosocial interventions varied among the studies and included telephone plus internet health education [32,34], partners in coping programs [30], psychosocial interventions programs [26,29], mindfulness-based stress reduction training [31], web-based psychosocial supportive intervention [28] and psychoeducational support groups [27]. The intervention durations ranged from 9 days to 5 months. The detailed characteristics of the studies included in this review are listed in Table 1 [[26], [27], [28], [29], [30], [31], [32], [34]].
Table 1.
Characteristics of the included studies.
| Included study | Country | Study- design | Sample size (INT/CONT) | Relationship with patients | Intervention | Control | Intervention duration | Follow-up durations | Outcomes | Ratings scales |
|---|---|---|---|---|---|---|---|---|---|---|
| [32] | China | RCT | 80 (40/40) | Spouse (80) | Psychological support | Usual care | First day in the hospital until 15 days after surgery | 15 days after surgery | Depression, Anxiety | SDS, SAS |
| [30] | USA | RCT | 47 (24/23) | Partner (47) | PICP | Standard social work services | 9 × 1 h sessions, 5 months | 6, 12 months | QOL | QL-SP |
| [26] | Iran | RCT | 64 (32/32) | Parent (2) Sister (13) Brother (1) Child (31) Spouse (17) |
Supportive educational program based on COPE model | Conventional care | 9 days | 1 month | QOL | CQOL-C |
| [34] | China | RCT | 60 (30/30) | Spouse (60) | Supportive health education | Usual care | First day in the hospital until 3 months after surgery | 3 months after surgery | QOL | GQOLI-74 |
| [31] | China | RCT | 91 (45/46) | Spouse (91) | Mindfulness-based stress reduction training | Usual care | 8 × 2 h sessions, 8 weeks | 8 weeks | Anxiety, Depression | BDI, HAMA |
| [28] | Canada | RCT | 57 (29/28) | Spouse (57) | MaTT | Usual care | 4 weeks | 14, 28 and 56 days | QOL | CQOL-C |
| [29] | Nigeria | Quasi-experimental study | 108 (54/54) | Parent (17) Spouse (33) Sibling (19) Child (23) Friend (16) |
Psychosocial intervention programme | Routine care | 6 × 1.5 h sessions, 6 weeks | 6,12 weeks | QOL | CQOL-C |
| [27] | Italy | Quasi-experimental study | 21 (5/16) | Partner (7) Parent (1) Sibling (1) Child (12) |
Psychoeducational support groups | Standard care | 6 × 1.5 h sessions, 6 weeks | 3 months | Anxiety, Depression | CBAOE |
Notes: CONT, Control; COPE, Creativity, Optimism, Planning, and Expert information; INT, Intervention; MaTT, A web-based psychosocial supportive intervention entitled the Male Transition Toolkit; PICP, Partners in Coping Program; QOL, Quality of Life; SDS, Self-rating Depression Scale; SAS, Self-Rating Anxiety Scale; QL-SP, the Quality of Life Questionnaire for Spouses; CQOL-C, Caregiver Quality of Life Index-Cancer; GQOLI1-74, the Life Quality Comprehensive Evaluation Questionnaire scale; BDI, Beck Depression Inventory; HAMA, Hamilton anxiety scale; CBAOE, Cognitive Behavioral Assessment for Outcome Evaluation.
3.3. Quality appraisal of the included studies
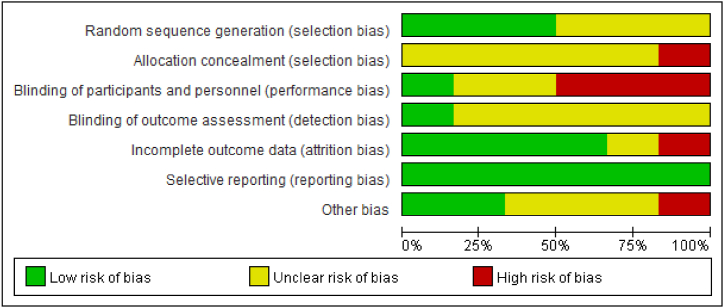
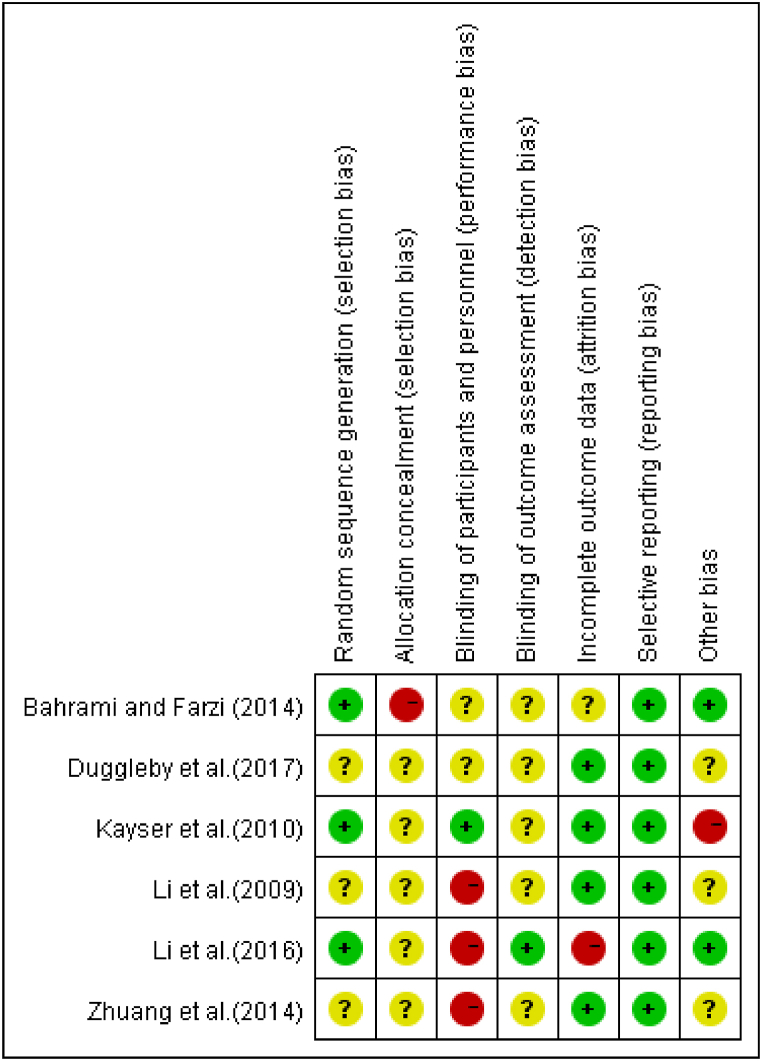
Six RCTs and two quasiexperimental studies were assessed for bias. The risk of selection bias was high in one study [26]; the risk of performance bias was high in three studies [31,32,34]; the risk of attrition bias was high in one study [31]; and a high risk of other bias was present in one study [30]. Fig. 2, Fig. 3 and Table 2 [27,29], present detailed results.
Fig. 2.
Risk of bias graph of the included RCTs.
Fig. 3.
Risk of bias summary of the included RCTs.
Table 2.
Risk of bias of the included quasiexperimental studies.
| Included study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| [29] | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| [27] | YES | unclear | unclear | YES | unclear | unclear | YES | YES | YES |
Notes.
1. Was the causal relationship in the study clearly stated?.
2. Whether the baselines were comparable between groups?.
3. Other than the intervention to be validated, were the other interventions received equally in each group?.
4. Did a control group exist?.
5. Were a variety of measures of outcomes performed before and after intervention?.
6. Was follow-up complete, and if not, was loss to follow-up reported and action taken to deal with loss to follow-up?.
7. Would the outcomes of each group be evaluated in the same way?.
8. Was the outcome measure reliable?.
9. Were the data analysis methods appropriate?.
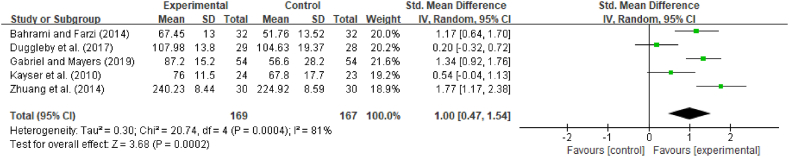
3.4. Effects of interventions on QOL
QOL was assessed in five studies (4 RCTs and 1 quasiexperimental study) using the QL-SP [30], CQOL-C [26,28,29] and GQOLI-74 [34]. As a result of the differences in the rating scales and follow-up durations, SMD was used. Due to a high level of heterogeneity, we used a random effects model (I2 = 81%, p < 0.01). As illustrated in Fig. 4, psychosocial interventions had a significant effect on the QOL of caregivers (SMD = 1.00, 95% CI [0.47, 1.54], p < 0.01). We performed sensitivity analysis and found that the overall effect size (SMD from 0.83 to 1.21) did not significantly change when any one of the five studies selected was removed, which means that the results were robust.
Fig. 4.
Effect of interventions on caregivers' QOL.
Subgroup analysis was performed based on the intervention methods, relationship to patients and follow-up durations. We categorized the psychosocial intervention forms into face-to-face, face-to-face and mixed-methods (face-to-face and telephone forms). As shown in Table 3 [26,[28], [29], [30],34], two studies used face-to-face methods, one study used non-face-to-face methods, and the other two studies used mixed methods. Significant differences were found in face-to-face and mixed-method psychosocial interventions (SMD = 0.97, 95% CI [0.19,1.75], p = 0.02; SMD = 1.45, 95% CI [0.86,2.05], p < 0.01) but not in the non-face-to-face subgroup (SMD = 0.20, 95% CI [−0.32,0.72], p = 0.46). To determine the influence of the relationship between caregivers and breast cancer patients, we categorized the relationship into “spouse or partner” and “other relatives” (parent, sibling, brother, etc.). Three studies involved spouses or partners of breast cancer patients, and two studies involved other relatives of breast cancer patients. A significant difference was found in the other relatives subgroup (SMD = 1,28, 95% CI [0.95,1.60], p < 0.01) but not in the spouses or partners subgroup (SMD = 0.83, 95% CI [−0.10,1.75], p = 0.08). The follow-up durations were categorized into two levels: <3 months and ≥3 months. Two studies included follow-up durations <3 months, and three studies included follow-up durations of ≥3 months. The effectiveness of psychosocial interventions on the QOL of caregivers was statistically significant in the ≥3 months subgroup (SMD = 1.22, 95% CI [0.58,1.86], p < 0.01), while there was no significant difference in the <3 months subgroup (SMD = 0.68, 95% CI [−0.27,1.63], p = 0.16).
Table 3.
Subgroup analysis of the effect of interventions on caregivers' QOL.
| Studies included | N | SMD | 95%CI | p | I2 | |
|---|---|---|---|---|---|---|
| Intervention methods | ||||||
| Face-to-face | [29,30] | 155 | 0.97 | [0.19,1.75] | 0.02 | 79% |
| Non-face-to-face | [28] | 57 | 0.20 | [-0.32,0.72] | 0.46 | |
| Mixd-methods | [26,34] | 124 | 1.45 | [0.86,2.05] | <0.01 | 54% |
| Relationship to patients | ||||||
| Spouses or partners | [28,30,34] | 164 | 0.83 | [-0.10,1.75] | 0.08 | 87% |
| Other relatives | [26,29] | 172 | 1.28 | [0.95,1.60] | <0.01 | 0% |
| Follow-up durations | ||||||
| <3 months | [26,28] | 121 | 0.68 | [-0.27,1.63] | 0.16 | 85% |
| ≥3months | [29,30,34] | 215 | 1.22 | [0.58,1.86] | <0.01 | 77% |
Note. SMD = standardized mean difference; Cl = confidence interval.
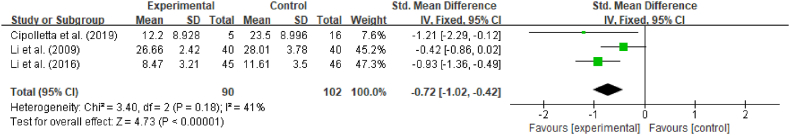
3.5. Effects of interventions on depression
The researchers examined the effectiveness of psychosocial interventions for reducing depression in three studies (2 RCTs and a quasiexperimental study) using the CBAOE [27], SDS [32] and BDI [31]. Since the rating scales differed, the SMD was used. Due to the low level of heterogeneity (p = 0.18, I2 = 41%), a fixed effects model was used. As shown in Fig. 5, psychosocial interventions had a significant effect on the level of depression among caregivers (SMD = −0.72, 95% CI [−1.02,-0.42], p < 0.01). We performed sensitivity analysis by removing the included studies one at a time. The overall effect size (SMD from −0.97 to −0.53) did not significantly change, which means that the results were robust.
Fig. 5.
Effect of interventions on caregivers' depression.
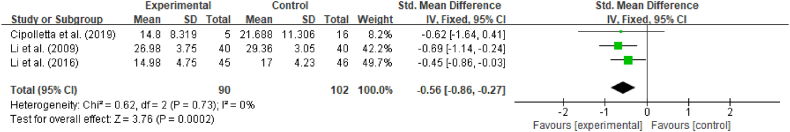
3.6. Effects of interventions on anxiety
Three studies, including two RCTs and one quasiexperimental study, examined the effect of psychosocial interventions on anxiety levels based on the CBAOE [27], SAS [32] and HAMA [31]. Since the rating scales differed, SMD was used. The fixed effects model was adopted due to the low level of heterogeneity (p = 0.73, I2 = 0%). As shown in Fig. 6, psychosocial interventions led to significantly lower anxiety scores among caregivers (SMD = −0.56, 95% CI [−0.86, −0.27], p < 0.01). We performed sensitivity analysis and found that the overall effect size (SMD from −0.68 to −0.47) did not significantly change when the included studies were removed one by one, which means that each individual study had little impact on the overall outcome.
Fig. 6.
Effect of interventions on caregivers' anxiety.
4. Discussion
This systematic review and meta-analysis revealed that psychosocial interventions are effective in improving caregivers' QOL and reducing depression and anxiety. Positive effects on QOL were found when the face-to-face method was used and when long-term psychosocial interventions were conducted. However, psychosocial interventions did not significantly improve the QOL of spouses or partners of breast cancer patients.
This systematic review examined five studies (including 336 caregivers with breast cancer) that assessed the effects of psychosocial interventions on caregivers’ QOL. Three of the five studies [26,29,34] reported that psychosocial interventions significantly improved QOL, while the other two studies [28,30] identified no significant effect. According to the current meta-analysis, psychosocial interventions significantly improved QOL.
Psychosocial interventions provide the caregivers of breast cancer patients with patient care-related information, answers to their concerns, and psychological support to help caregivers respond effectively to nursing challenges, thereby improving their QOL. The findings of this meta-analysis are consistent with those of previous systematic reviews [35,37,38,[40], [41], [42], [43], [44]]. According to some previous systematic reviews [36,45,46], it is difficult to determine whether psychosocial interventions are effective for caregivers caring for cancer patients due to the heterogeneity and weak quality of studies. According to another previous systematic review, interventions should be tailored based on the demographic characteristics and cultural context of informal caregivers to improve their QOL [44].
Subgroup analysis based on the intervention methods showed that the face-to-face and mixed intervention methods had a statistically significant effect on caregivers' QOL, while this effect was not found in the non-face-to-face intervention subgroup. Face-to-face interventions appear to enhance the development of therapeutic relationships and improve the compliance and effect of treatment, thereby leading to an increase in QOL among patients and their caregivers. This finding was supported by previous studies [47,48]. Therefore, it is worthwhile to use face-to-face methods when psychosocial interventions are conducted for caregivers in clinical settings. Subgroup analysis based on relationship to patients and follow-up durations showed that the interventions had no statistically significant effect on the QOL of spouses or partners or when the follow-up duration was <3 months. These findings may be due to spouses or partners suffered psychological distress and financial burden of breast cancer and a lack of information about the disease, which lead to low QOL [49]. Future research should focus on spouses or partners, and the intervention time should be longer (≥3 months) to improve the QOL of caregivers in practice.
Three studies (192 caregivers) explored the impact of psychosocial interventions on caregivers’ depression and anxiety. Two studies [31,32] found that psychosocial interventions significantly reduced depression and anxiety. One study [27] identified that the experimental and control groups had significant differences in depression but no significant difference in anxiety of the caregivers. The current meta-analysis found that psychosocial interventions significantly reduced depression and anxiety. Psychosocial interventions support the caregivers of breast cancer patients by helping them to strengthen interpersonal communication, seek additional social and economic support and emphasise self-care to reduce their depression and anxiety. The results of this meta-analysis were consistent with those of other systematic reviews [35,37,42,43]. However, a previous study indicated that it is difficult to confirm the effectiveness of psychosocial interventions among informal caregivers of patients suffering from cancer due to the heterogeneity across studies [46]. The heterogeneity of the included studies was low, but the risk of performance bias was high and there was a small sample size in some of the original studies. However, it is worthwhile to use psychosocial interventions to reduce depression and anxiety in clinical settings. Higher-quality studies and original studies with larger sample sizes should be conducted to validate the current findings.
5. Study limitations
Several limitations were identified in this systematic review. At the study level, the included studies had risks of bias, including selection, performance, and attrition bias, which might undermine the quality of the evidence. In addition, we did not conduct a subgroup analysis based on the intervention forms, relationship to patients and follow-up durations when analysing the effectiveness of psychosocial interventions on depression and anxiety due to the limited number of original studies. Furthermore, the included original studies were only published in English and Chinese, which limits their generalizability. Healthcare providers need to be cautious when they recommend psychosocial interventions for breast cancer patients' caregivers.
6. Conclusions
This systematic review indicated that breast cancer patients' caregivers who undergo psychosocial interventions report improvements in QOL and reduced levels of depression and anxiety. It is worthwhile to use face-to-face methods when psychosocial interventions are conducted for improving caregivers' QOL in clinical settings. Future studies should examine long-term psychosocial interventions for spouses or partners of breast cancer patients. However, because of the limited number of original studies and the low quality of some included studies, the results should be treated cautiously. To increase solid evidence in this field, higher-quality, more original studies are needed.
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This work was supported by the Education Department of Sichuan Province Foundation [SCJG20A084].
Data availability statement
Data included in article/supp. Material/referenced in article.
Declaration of interest's statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We gratefully acknowledge the librarians of Sichuan Vocational College of Health and Rehabilitation for retrieving potential articles and the experts and members of our group for their guidance and introduction to the meta-analysis. We appreciate the Education Department of Sichuan Province Foundation for its financial support. We also thank the editor and the reviewers for their useful feedback that improved this paper.
Contributor Information
Fang Ye, Email: yfx0239@svchr.edu.cn.
Jinmei Zou, Email: zjm20505@svchr.edu.cn.
References
- 1.World Health Organization . 2021. Breast Cancer.https://www.who.int/news-room/fact-sheets/detail/breast-cancer accessed. [Google Scholar]
- 2.Campbell-Enns H., Woodgate R. The psychosocial experiences of women with breast cancer across the lifespan: a systematic review protocol. JBI database of systematic reviews and implementation reports. 2015;13(1):112–121. doi: 10.11124/jbisrir-2015-1795. [DOI] [PubMed] [Google Scholar]
- 3.Wagner C.D., Tanmoy Das L., Bigatti S.M., Storniolo A.M. Characterizing burden, caregiving benefits, and psychological distress of husbands of breast cancer patients during treatment and beyond. Cancer Nurs. 2011;34(4):E21–E30. doi: 10.1097/NCC.0b013e31820251f5. [DOI] [PubMed] [Google Scholar]
- 4.Yabroff K.R., Kim Y. Time costs associated with informal caregiving for cancer survivors. Cancer. 2009;115(18 Suppl):4362–4373. doi: 10.1002/cncr.24588. [DOI] [PubMed] [Google Scholar]
- 5.Fekih-Romdhane F., Henchiri H., Ridha R., Labbane R., Cheour M. Psychological distress and caregiving burden among spouses of women with breast cancer. L'Encephale. 2019;45(2):190–192. doi: 10.1016/j.encep.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Northouse L.L., Mood D., Kershaw T., Schafenacker A., Mellon S., Walker J., Galvin E., Decker V. Quality of life of women with recurrent breast cancer and their family members. J. Clin. Oncol. : official journal of the American Society of Clinical Oncology. 2002;20(19):4050–4064. doi: 10.1200/JCO.2002.02.054. [DOI] [PubMed] [Google Scholar]
- 7.Bee P.E., Barnes P., Luker K.A. A systematic review of informal caregivers' needs in providing home-based end-of-life care to people with cancer. J. Clin. Nurs. 2009;18:1379–1393. doi: 10.1111/j.1365-2702.2008.02405.x. [DOI] [PubMed] [Google Scholar]
- 8.Kim Y., Carver C.S., Shaffer K.M., Gansler T., Cannady R.S. Cancer caregiving predicts physical impairments: roles of earlier caregiving stress and being a spousal caregiver. Cancer. 2015;121:302–310. doi: 10.1002/cncr.29040. [DOI] [PubMed] [Google Scholar]
- 9.Badger T., Segrin C., Pasvogel A., Lopez A.M. The effect of psychosocial interventions delivered by telephone and videophone on quality of life in early-stage breast cancer survivors and their supportive partners. J. Telemed. Telecare. 2013;19:260–265. doi: 10.1177/1357633x13492289. [DOI] [PubMed] [Google Scholar]
- 10.Geng H.M., Chuang D.M., Yang F., Yang Y., Liu W.M., Liu L.H., Tian H.M. Prevalence and determinants of depression in caregivers of cancer patients: a systematic review and meta-analysis. Medicine (Baltim.) 2018;97 doi: 10.1097/md.0000000000011863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Segrin C., Badger T.A. Interdependent psychological distress between Latinas with breast cancer and their supportive partners. J. Lat. Psychol. 2013;1:21. [Google Scholar]
- 12.Heidari Gorji M.A., Bouzar Z., Haghshenas M., Kasaeeyan A.A., Sadeghi M.R., Ardebil M.D. Quality of life and depression in caregivers of patients with breast cancer. BMC Res. Notes. 2012;5:310. doi: 10.1186/1756-0500-5-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kent E.E., Rowland J.H., Northouse L., Litzelman K., Chou W.Y., Shelburne N., Timura C., O'Mara A., Huss K. Caring for caregivers and patients: research and clinical priorities for informal cancer caregiving. Cancer. 2016;122:1987–1995. doi: 10.1002/cncr.29939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Northouse L.L., Katapodi M.C., Schafenacker A.M., Weiss D. The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Semin. Oncol. Nurs. 2012;28:236–245. doi: 10.1016/j.soncn.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Sklenarova H., Krümpelmann A., Haun M.W., Friederich H.C., Huber J., Thomas M., Winkler E.C., Herzog W., Hartmann M. When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer. 2015;121:1513–1519. doi: 10.1002/cncr.29223. [DOI] [PubMed] [Google Scholar]
- 16.Borstelmann N.A., Rosenberg S., Gelber S., Zheng Y., Meyer M., Ruddy K.J., Schapira L., Come S., Borges V., Cadet T., Maramaldi P., Partridge A.H. Partners of young breast cancer survivors: a cross-sectional evaluation of psychosocial concerns, coping, and mental health. J. Psychosoc. Oncol. 2020;38:670–686. doi: 10.1080/07347332.2020.1823546. [DOI] [PubMed] [Google Scholar]
- 17.Nik Jaafar N.R., Selamat Din S.H., Mohamed Saini S., Ahmad S.N., Midin M., Sidi H., Silim U.A., Baharudin A. Clinical depression while caring for loved ones with breast cancer. Compr. Psychiatr. 2014;55(Suppl 1):S52–S59. doi: 10.1016/j.comppsych.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Sahadevan S., Namboodiri V. Depression in caregivers of patients with breast cancer: a cross-sectional study from a cancer research center in South India. Indian J. Psychiatr. 2019;61:277–282. doi: 10.4103/psychiatry.IndianJPsychiatry_46_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang M., Ma F., Lan B., Cai J., Sun X., Xu B. Validity of distress thermometer for screening of anxiety and depression in family caregivers of Chinese breast cancer patients receiving postoperative chemotherapy. Chin. J. Cancer Res. 2020;32:476–484. doi: 10.21147/j.issn.1000-9604.2020.04.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Selamat Din S.H., Nik Jaafar N.R., Zakaria H., Mohamed Saini S., Ahmad S.N., Midin M. Anxiety disorders in family caregivers of breast cancer patients receiving oncologic treatment in Malaysia. Asian Pac. J. Cancer Prev. APJCP. 2017;18:465–471. doi: 10.22034/apjcp.2017.18.2.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Segrin C., Badger T.A., Sikorskii A., Crane T.E., Pace T.W.W. A dyadic analysis of stress processes in Latinas with breast cancer and their family caregivers. Psycho Oncol. 2018;27:838–846. doi: 10.1002/pon.4580. [DOI] [PubMed] [Google Scholar]
- 22.Turner J., Zapart S., Pedersen K., Rankin N., Luxford K., Fletcher J., National Breast Cancer Centre, Sydney, Australia, & National Cancer Control Initiative, Melbourne, Australia Clinical practice guidelines for the psychosocial care of adults with cancer. Psycho Oncol. 2005;14(3):159–173. doi: 10.1002/pon.897. [DOI] [PubMed] [Google Scholar]
- 23.Badr H., Smith C.B., Goldstein N.E., Gomez J.E., Redd W.H. Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: results of a randomized pilot trial. Cancer. 2015;121:150–158. doi: 10.1002/cncr.29009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Badger T.A., Segrin C., Hepworth J.T., Pasvogel A., Weihs K., Lopez A.M. Telephone-delivered health education and interpersonal counseling improve quality of life for Latinas with breast cancer and their supportive partners. Psycho Oncol. 2013;22:1035–1042. doi: 10.1002/pon.3101. [DOI] [PubMed] [Google Scholar]
- 25.Badger T.A., Segrin C., Sikorskii A., Pasvogel A., Weihs K., Lopez A.M., Chalasani P. Randomized controlled trial of supportive care interventions to manage psychological distress and symptoms in Latinas with breast cancer and their informal caregivers. Psychol. Health. 2020;35:87–106. doi: 10.1080/08870446.2019.1626395. [DOI] [PubMed] [Google Scholar]
- 26.Bahrami M., Farzi S. The effect of a supportive educational program based on COPE model on caring burden and quality of life in family caregivers of women with breast cancer. Iran. J. Nurs. Midwifery Res. 2014;19:119–126. [PMC free article] [PubMed] [Google Scholar]
- 27.Cipolletta S., Simonato C., Faccio E. The effectiveness of psychoeducational support groups for women with breast cancer and their caregivers: a mixed methods study. Front. Psychol. 2019;10:288. doi: 10.3389/fpsyg.2019.00288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duggleby W., Ghosh S., Struthers-Montford K., Nekolaichuk C., Cumming C., Thomas R., Tonkin K., Swindle J. Feasibility Study of an online intervention to support male spouses of women with breast cancer. Oncol. Nurs. Forum. 2017;44:765–775. doi: 10.1188/17.onf.765-775. [DOI] [PubMed] [Google Scholar]
- 29.Gabriel I.O., Mayers P.M. Effects of a psychosocial intervention on the quality of life of primary caregivers of women with breast cancer. Eur. J. Oncol. Nurs. 2019;38:85–91. doi: 10.1016/j.ejon.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Kayser K., Feldman B.N., Borstelmann N.A., Daniels A.A. Effects of a randomized couple-based intervention on quality of life of breast cancer patients and their partners. Soc. Work. Res. 2010;34:20–32. doi: 10.1093/swr/34.1.20. [DOI] [Google Scholar]
- 31.Li J., Gu L., Liu Y., Yang D. Effects of mindfulness-based stress reduction on anxiety and depression in spouses of patients with breast cancer. Chin. J. Behav. Med. Brain Sci. 2016:1104–1108. https://kns.cnki.net/kcms/detail/detail.aspx?FileName=ZGXX201612016&DbName=ZHYX2016 [Google Scholar]
- 32.Li Y., Fu S., Dai Y., Yu J. Psychological interventions for patients undergoing modified radical mastectomy and for their spouses. J. Nurs. Sci. 2009;24:67–68. https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFD2009&filename=HLXZ200918046&uniplatform=NZKPT&v=e329mwMbC-MgnCG0Rnjwk2fF_Dl0EzqJbm_e8RjMJ_K6f1tytFVjrQfl5D9PMnCr [Google Scholar]
- 33.Northouse L., Kershaw T., Mood D., Schafenacker A. Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psycho Oncol. 2005;14:478–491. doi: 10.1002/pon.871. [DOI] [PubMed] [Google Scholar]
- 34.Zhuang X., Zhao W., Feng D. Effect of psychological intervention on the postoperative quality of life of patients with breast cancer and their spouses. Hainan Med. J. 2014;25:776–778. [Google Scholar]
- 35.Fu F., Zhao H., Tong F., Chi I. A systematic review of psychosocial interventions to cancer caregivers. Front. Psychol. 2017;8:834. doi: 10.3389/fpsyg.2017.00834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gabriel I., Creedy D., Coyne E. A systematic review of psychosocial interventions to improve quality of life of people with cancer and their family caregivers. Nurs. Open. 2020;7:1299–1312. doi: 10.1002/nop2.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee J.Z.J., Chen H.C., Lee J.X., Klainin-Yobas P. Effects of psychosocial interventions on psychological outcomes among caregivers of advanced cancer patients: a systematic review and meta-analysis. Support. Care Cancer. 2021;29:7237–7248. doi: 10.1007/s00520-021-06102-2. [DOI] [PubMed] [Google Scholar]
- 38.Waldron E.A., Janke E.A., Bechtel C.F., Ramirez M., Cohen A. A systematic review of psychosocial interventions to improve cancer caregiver quality of life. Psycho Oncol. 2013;22:1200–1207. doi: 10.1002/pon.3118. [DOI] [PubMed] [Google Scholar]
- 39.Zhang Z., Wang S., Liu Z., Li Z. Psychosocial interventions to improve psychological distress of informal caregivers of cancer patients: a meta-analysis of randomized controlled trial. Am. J. Nurs. Sci. 2020;9:459–465. doi: 10.11648/j.ajns.20200906.24. [DOI] [Google Scholar]
- 40.Ahn S., Romo R.D., Campbell C.L. A systematic review of interventions for family caregivers who care for patients with advanced cancer at home. Patient Educ. Counsel. 2020;103:1518–1530. doi: 10.1016/j.pec.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chambers S.K., Pinnock C., Lepore S.J., Hughes S., O'Connell D.L. A systematic review of psychosocial interventions for men with prostate cancer and their partners. Patient Educ. Counsel. 2011;85:e75–e88. doi: 10.1016/j.pec.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 42.Cheng Q., Xu B., Ng M.S.N., Duan Y., So W.K.W. Effectiveness of psychoeducational interventions among caregivers of patients with cancer: a systematic review and meta-analysis. Int. J. Nurs. Stud. 2022;127 doi: 10.1016/j.ijnurstu.2021.104162. [DOI] [PubMed] [Google Scholar]
- 43.Kedia S.K., Collins A., Dillon P.J., Akkus C., Ward K.D., Jackson B.M. Psychosocial interventions for informal caregivers of lung cancer patients: a systematic review. Psycho Oncol. 2020;29:251–262. doi: 10.1002/pon.5271. [DOI] [PubMed] [Google Scholar]
- 44.Li Y., Li J., Zhang Y., Ding Y., Hu X. The effectiveness of e-Health interventions on caregiver burden, depression, and quality of life in informal caregivers of patients with cancer: a systematic review and meta-analysis of randomized controlled trials. Int. J. Nurs. Stud. 2022;127 doi: 10.1016/j.ijnurstu.2022.104179. [DOI] [PubMed] [Google Scholar]
- 45.Song L., Qan'ir Y., Guan T., Guo P., Xu S., Jung A., Idiagbonya E., Song F., Kent E.E. The challenges of enrollment and retention: a systematic review of psychosocial behavioral interventions for patients with cancer and their family caregivers. J. Pain Symptom Manag. 2021;62:e279–e304. doi: 10.1016/j.jpainsymman.2021.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Treanor C.J., Santin O., Prue G., Coleman H., Cardwell C.R., O'Halloran P., Donnelly M. Psychosocial interventions for informal caregivers of people living with cancer. Cochrane Database Syst. Rev. 2019;6:CD009912. doi: 10.1002/14651858.CD009912.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Son H., Son Y.J., Kim H., Lee Y. Effect of psychosocial interventions on the quality of life of patients with colorectal cancer: a systematic review and meta-analysis. Health Qual. Life Outcome. 2018;16(1):119. doi: 10.1186/s12955-018-0943-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wagner B., Horn A.B., Maercker A. Internet-based versus face-to-face cognitive-behavioral intervention for depression: a randomized controllednon-inferiority trial. J. Affect. Disord. 2014;152:113–121. doi: 10.1016/j.jad.2013.06.032. [DOI] [PubMed] [Google Scholar]
- 49.Lopes V.B., Lobo A.P.A., Da Silva Junior G.B., Melo A.K., Lamboglia C.G., Silva C.A.B.D. The experience of male spouses in the context of breast cancer: a systematic review of the literature. Psychol. Health Med. 2018;23(1):89–98. doi: 10.1080/13548506.2017.1332374. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supp. Material/referenced in article.