Abstract
Background/Objectives
In 2013, the KSA made Central Board for Accreditation of Healthcare Institutions (CBAHI) accreditation mandatory for all healthcare facilities, including primary health care centres (PHCs) and set a target to have 502 PHCs accredited by 2020. However, there is a real gap in knowledge and research on the impact of CBAHI accreditation on PHCs. This absence of research has been linked to the lack of understanding of the accreditation programme. Therefore, it was recommended by scholars that the KSA could learn from the experience of other countries to improve policy implementation and avoid future complications.
Methods
This study aimed to explore lessons that KSA can draw from developed and developing countries that have implemented accreditation programmes for PHCs. We performed a literature review using a systematic approach to identify articles related to the accreditation of PHCs. The identified articles were examined by applying evaluation criteria in respect of prospective policy transfer.
Results
The research results yielded 22 publications from different countries. There were variations among the countries in the specific information acquired. However, Denmark had the highest number of articles providing detailed information. Regarding their aims, most studies shared the same goal of improving quality and patient safety. Generally, there was limited discussion of policy failure compared with policy success. In addition, most of the countries were in the process of implementing local accreditation. Almost all of the countries that had implemented external programmes were developing countries. In terms of application criteria, most cases made recommendations for the programme or for PHCs.
Conclusion
Analysis indicated that because of the differences in information between countries and settings, there is no ideal country-based experience from which the KSA can transfer lessons. Lessons from outside the KSA would need careful consideration when adopting them in the local context of the Kingdom.
Keywords: Accreditation, Developed and developing countries, Policy transfer, Primary health centres, KSA
Abbreviations: PHCs, primary health care centres; CBAHI, the Central Board for Accreditation of Healthcare Institutions; KSA, Kingdom of Saudi Arabia; PT, Policy Transfer
الملخص
أهداف البحث
في عام 2013، جعلت المملكة العربية السعودية اعتماد المجلس المركزي لاعتماد مؤسسات الرعاية الصحية (سباهي) إلزاميا لجميع مرافق الرعاية الصحية، بما في ذلك مراكز الرعاية الصحية الأولية، وحددت هدفا لاعتماد 502 من مراكز الرعاية الصحية الأولية بحلول عام 2020. ومع ذلك، هناك فجوة حقيقية في المعرفة والبحث حول تأثير اعتماد المركز السعودي لاعتماد المنشآت الصحية على مراكز الرعاية الصحية الأولية. تم ربط هذا النقص في البحث بعدم فهم برنامج الاعتماد. لذلك، أوصى الباحثين بأن المملكة العربية السعودية يمكن أن تتعلم من تجارب الدول الأخرى لتحسين تنفيذ السياسات وتجنب التعقيدات المستقبلية.
طرق البحث
تهدف هذه الدراسة إلى استكشاف الدروس التي يمكن للمملكة العربية السعودية استخلاصها من الدول المتقدمة والنامية التي نفذت برامج اعتماد للرعاية الصحية الأولية. تقوم الدراسة بمراجعة الأدبيات باستخدام منهج منظم للبحث عن مقالات تدرس اعتماد مراكز الرعاية الصحية الأولية. تم فحص المقالات من خلال تطبيق معايير التقييم فيما يتعلق بنقل السياسة المرتقب.
النتائج
أسفرت نتائج البحث عن 22 منشورا من دول مختلفة. كانت هناك اختلافات بين البلدان في تفاصيل المعلومات الموجودة. ومع ذلك، كان لدى الدنمارك أكبر عدد من المقالات التي تقدم معلومات مفصلة. فيما يتعلق بأهدافها، شاركت معظم الدراسات نفس الهدف المتمثل في تحسين الجودة وسلامة المرضى. بشكل عام، كانت هناك مناقشة محدودة لفشل السياسة مقارنة بنجاح السياسة. بالإضافة إلى ذلك، كانت معظم الدول في طور تنفيذ الاعتماد المحلي. وكانت جميع الدول التي نفذت برامج خارجية تقريبا من الدول النامية. من حيث معايير التطبيق، قدمت غالبية الحالات توصيات للبرنامج أو للرعاية الصحية الأولية.
الاستنتاجات
تشير هذه المراجعة إلى أنه بسبب الاختلاف في المعلومات بين الدول والأماكن، لا توجد تجربة بلد مثالية يمكن للمملكة العربية السعودية أن تنقل الدروس منها. سوف تحتاج الدروس من خارج المملكة العربية السعودية إلى دراسة متأنية عند تبنيها في السياق المحلي للمملكة.
الكلمات المفتاحية: مراكز الصحة الأولية؛ الاعتماد؛ نقل السياسات؛ المملكة العربية السعودية؛ الدول المتقدمة والنامية.
Introduction
Quality improvement (QI) has become an essential part of health service activities1 and the QI concept has inspired the development of accreditation programmes in the healthcare sector.2 Accreditation has become one of the common methods that many countries use for improving quality, patient safety, performance, efficiency, and the effectiveness of using health resources, which can result in a better health outcome.3,4 Accreditation has been promoted as the driving process for a full range of improvements and encompasses all the components of service delivery: structures, processes and outcomes.5,6
The accreditation idea developed from the United States (US), which was the origin of the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), the reference model of accreditation programmes that is used around the world.7 As the JCAHO programme has been transferred to many countries and adjusted to different settings,8 the number of accreditation programmes has rapidly increased and expanded from developed to developing countries.6
The KSA was an early adopter of health accreditation programmes in the Middle East region,9 in order to improve the levels of service quality and provide a safer work environment.10 The KSA government also launched a local accreditation programme, the Central Board for Accreditation of Healthcare Institutions (CBAHI) (see Section 2.6), which was mandated to grant the CBAHI accreditation to healthcare facilities, including primary health care centres (PHCs).6 Furthermore, the CBAHI is one of the initiatives that aims to improve the quality objective of the Health Sector Transformation Program (HSTP) under the 2030's vision of the Kingdom. However, the KSA is considered to be in the early stages of adopting accreditation.9 Therefore, there are significant challenges that hinder the successful implementation of these programmes.11
In order to increase accreditation, developing countries need to be able to assess studies that compare existing accreditation programmes and their outcomes, as well as those investigating factors that facilitate or constrain the development and processes of accreditation programmes.8 However, there is a major absence of research on CBAHI accreditation; this might be a reason for the lack of understanding of the programme.6 Furthermore, most studies on the CBAHI are hospital-focused; there is limited research on PHCs. This can be understood as accreditation in PHCs being relatively new in comparison with that in hospital settings.12
Thus, there is a need for further research to explore the mechanisms for improving the accreditation implementation processes in PHC settings as this might help to avoid future problems. Policy transfer (PT) theory is a useful tool for analysing policy processes and the transfer of policies from one country or context to another, such as the transfer of accreditation policy.13 Since the KSA is still in the early stages of implementing accreditation for PHCs, it would be useful to seek lessons from other countries around the world that have implemented this type of accreditation to improve its implementation in PHCs in the Kingdom.
The KSA is a unique context in research. According to the World Bank (WB) countries classification, KSA is a high-income country (HIC) based on the level of income per capita.14,15 However, the United Nations Development Program (UNDP) classifies countries based on per capita and the consideration of human assets and economic vulnerability; thus, not all HICs in the WB classification are ‘developed’, including countries such as Kuwait, Latvia, Oman, and KSA.16 Thus, since the KSA shares some characteristics with developed and developing countries, it would be valuable to learn from the experience of both of these groups with regards to accreditation policy for PHCs.
This research aimed to explore lessons that can be taken from both developed and developing countries by the KSA in the implementation of accreditation programmes for PHCs. The research uses the framework of Mossberger et al.17 to assess the transferability of policy, which is further discussed in Section 3. The research question that the study seeks to answer is ‘What are the lessons that the KSA can learn from the experiences of developed or developing countries with regards to implementing accreditation programmes for PHCs?’
Background
What is accreditation?
Accreditation is defined as “the systematic assessment of hospitals against accepted standards” (15, p. 156). Mansour, Boyd and Walshe13 suggested that accreditation programmes are described in the literature in terms of five components: accreditation body, standards, the survey process, surveyors, and incentives. Various definitions of accreditation are found in the literature, as shown in Table 1, including the CBAHI's definition of accreditation. However, the current research adopts the definition provided by Shaw19 as this seems to be more of a definition than a description of the accreditation process, unlike the other definitions; it also highlights the importance of organizational performance.
Table 1.
Definitions of accreditation.
| Citation | Definition |
|---|---|
| World Health Organization (7, p. 59). | “Accreditation is usually performed by a multidisciplinary team of health professionals and is assessed against published standards for the environment in which clinical care is delivered.” |
| Braithwaite et al. (17, p. 14). | “The certification of a programme, service, organisation, institution or agency by an authorised external body in accordance with predetermined criteria, usually expressed as standards, typically measuring structures and processes.” |
| Al-Awa et al. (18, p. 206). | “Accreditation is the process whereby a designated accreditation body assesses the competence of the verification body to carry out its functions according to relevant standards/guidelines and application legislation (if relevant); it is an ongoing cycle process.” |
| Hinchcliff et al. (19, p. 979). | “The purpose of accreditation programmes is to monitor and promote, via self and external assessment, healthcare organisation performance against predetermined optimal standards.” |
| Smits, Supachutikul and Mate (20, p. 8). | The International Society for Quality in Health Care definition is as follows: “A public recognition by a healthcare accreditation body of the achievement of accreditation standards by a healthcare organization, demonstrated through an independent external peer assessment of that organization's level of performance in relation to the standards”. |
| Shaw (16, p. 229). | “Accreditation is a dynamic system aimed at organizational development of all participating institutions by recognizing degrees of excellence in compliance with optimum standards of organizational performance.” |
| CBAHI (24, p. 13) | “Healthcare accreditation is a process of comprehensive and integrated assessment, carried out by an impartial and independent party, in order to measure the level of compliance by the healthcare facility with quality and safety standards that are previously established by that supervising party” |
An accreditation process is an ongoing cycle of monitoring and assessing a health organization against predetermined optimal standards using different means, such as self-appraisal, peer review interviews, or scrutiny of documentation.20, 21, 22 Assessment is usually performed by a team of health professionals from multiple disciplines.7,23 After the assessment phase, the health organization can be granted accreditation or given time to make the recommended corrections, or lose its accreditation status if the organization's performance is below the stipulated standards.20 Therefore, accreditation has a reputation as a key driver for the improvement of quality and patient safety and as a means of enabling the public to recognize that a healthcare organization has met the national quality standards or benchmarks.24, 25, 26
History of accreditation
Accreditation started more than 100 years ago and was first introduced by the American College of Surgeons who set quality standards for surgical training called the “Minimum Standard for Hospitals”.18,27,28 These standards were developed into a multidisciplinary programme of standardization that led to the formation of the JCAHO, which represented the formal beginning of accreditations in the US.7,28 Since that time, JCAHO standards have been transferred to many countries and have been adopted in various settings; other standards have been directly or indirectly derived from the JCAHO.8,27
Accreditation began to spread in the 1990s. Although the beginning of this spread was slow, it accelerated in the 1980s and 1990s, mainly in developed countries, and in recent years has been adopted in developing countries.24 It has been argued that the rapid growth of accreditation programmes was partly because of media pressure to report inadequacies in the quality and patient safety of healthcare services.3 Consequently, healthcare accreditation has become an integral part of the healthcare system in more than 70 countries across the world.29 However, there is still concern about the lack of firm evidence for the effect of accreditation on healthcare organizations.1 The next section will further discuss the available evidence on accreditation in health.
An overview of research on accreditation in healthcare
Since it emerged, accreditation has become a common area of research in developed countries and, more recently, in developing countries.24 Despite its widespread use, accreditation has been criticized in many respects: for being too rigid, insufficient, and because its impact on the quality of care is difficult to measure.24 In general, findings from empirical studies show that healthcare accreditation is a tool used to promote the improvement of healthcare organization performance.30 Some researchers report that accreditation is related to high quality when comparing accredited and non-accredited hospitals, but it is uncertain whether this is due to the effects of accreditation or other factors.28
On the other hand, others have reported that accreditation promotes organizational performance, stimulates clinical processes and outcomes, and improves the quality of clinical care and patient safety.30 These variations might be due to the different contexts of the studies or could be related to the method of implementation.25 Some countries have more knowledge and experience in accreditation or have more resources than others. For example, the lack of resources in low- and middle-income countries (LMICs) is a major challenge to the development and sustainability of accreditation.13
Literature reviews of the impact of accreditation are not able to provide strong claims to support its effectiveness in terms of quality of care due to the limitations of the available studies.1,3,21,22,28 However, a lack of convincing evidence is not a reason to abandon accreditation.28 If accreditation reinforces the effectiveness and communication of interdisciplinary teams, and enhances the use of evidence-based decision-making indicators, it could lead to improvements in health outcomes.3 Moreover, some researchers have shown that accreditation is positively associated with organizational culture and leadership.1,20 There is no doubt that accreditation will continue in the future, and there are no alternatives to this model as yet.20
Most accreditation literature is hospital-based19; however, with the shifting priority from treatment to prevention, there has been increased attention paid to implementing accreditation for PHCs.7 Therefore, this research aimed to focus on accreditation for PHCs.
Accreditation in primary health care
PHC accreditation programme standards were initiated from hospital accreditations31 and involves the assessment of the organization against a set of standards.32 The first PHC accreditation standards were established in the early 1990s in Australia.32 Later, the Australian PHC standards were developed in New Zealand, Indonesia, the US, and Europe.32 It seems that accreditation models developed in Australia, the United Kingdom (UK), New Zealand, and Canada had the greatest effect on the development of PHC accreditation models worldwide.12,32
PHC quality assessment and improvement have become a priority for many developing countries. Many countries initiated PHC accreditation programmes in collaboration with PHC accreditation models from the US, Canada and The International Society for Quality in Health Care (ISQua).33 For example, the KSA in 2011, and Lebanon and Jordan in 2009, developed their own PHC accreditation programmes.32 Only the Jordanian and KSA accreditation programmes were accredited by ISQua.32
Nevertheless, with the lack of strong evidence of accreditation in general, little research has measured the effect of accreditation on healthcare outcomes or quality improvement in PHCs.12 There is also a limitation on the number of high-quality PHC accreditation studies due to the short history of accreditation for PHCs.32 Furthermore, there is a need for more research to be undertaken before validating the usefulness of accreditation in improving care within the primary care domain12. However, although there is an absence of evidence relating to the effectiveness of accreditation for PHCs, many countries have adopted this process and made it compulsory. For example, the KSA is one of the countries that have made accreditation mandatory for all healthcare facilities, including PHCs. The following section discusses the health system in KSA.
The healthcare system in KSA: an overview
The Saudi health system is facing many challenges with the PHCs such as increased costs and demand, the capacity of the workforce, inequitable access to the services, and the quality and safety of services.34 There is a poor distribution of secondary and tertiary hospitals across the Kingdom with inadequate and inconsistent primary care.35 An in-depth review by the MOH of the PHCs revealed that it lacks a qualified workforce in chronic disease management; in addition, they have limited communication and interpersonal skills.36 Furthermore, due to the lack of consistent protocols and pathways for treatment, and the incomplete measurement of patient processes and outcomes, there are significant gaps in the quality of services delivered to patients.35
However, KSA is going under major reform in line with KSA's Vision 2030s which was announced in 2016 and is promising huge improvements and developments. In response to this vision, the Saudi Ministry of Health (MOH) has created the HSTP that has four main goals: to facilitate access to healthcare services, improve the quality and efficiency of health services, promote the prevention of health risks, and enhance traffic safety.
Many efforts were made to achieve the HSTP objectives. The MOH has been gradually establishing health clusters in the country's different regions; each cluster is an independent, comprehensive, and integrated network of healthcare providers, and they are reflective of the regional demographics, available facilities, and capacities.37 Additionally, to establish a PHC system that meets the Saudi population's expectations, the MOH is imposing quality standards set by the CBAHI for all levels of care, including the PHCs.36
Accreditation in the KSA's health system
The interest in accreditation started in the KSA prior to the 2030's vision. In 2000, the KSA established the Makkah Regional Quality Programme (MRQP) to improve the quality of health services in this region.6 The MRQP standards were borrowed from the JCAHO and quality systems implemented in Canadian hospitals.11 Later, the MOH incorporated the MRQP into the national CBAHI accreditation programme, aiming to expand quality improvement standards to the whole country.38 Generally, CBAHI's include three major types of standards: structure/input standards, activity and procedure standards, and outcome standards which were developed by peer experts to set the best measurable, realizable and assessable performance.39
In 2013, the ministry mandated CBAHI accreditation as a prerequisite for the renewal of operating licences for private and public health organizations (e.g., hospitals, PHCs, blood banks and medical laboratories).6,38 In line with this vision, the MOH started by using the CBAHI to evaluate 2386 PHCs and selected 502 PHCs from 20 different regions as a target to be accredited between the period of October 2016 and May 2020.40 Furthermore, the CBAHI is providing frequent updates throughout the year on the status of accreditation in PHC facilities on its official website. For instance, in the 2022 update, CBAHI had accredited 600 PHCs out of 1024 visited PHCs.41 This can be considered major progress towards the HSTP objectives and achievements.
Although the KSA depends on CBAHI accreditation as a way of promoting quality in healthcare organizations, evidence is still limited.42 Furthermore, most published studies on the CBAHI have not identified positive outcomes.6 It has been claimed that CBAHI standards cannot reduce medical errors or health service complications and it seems that they focus more on measuring the process than the outcomes.11,43 However, although CBAHI literature is highly focused on the hospital context, there is one study that compared CBAHI-accredited and non-CBAHI-accredited PHCs and claims that CBAHI-accredited PHCs demonstrated higher scores according to the criteria of the study.44
There is clearly a real gap in knowledge of the impact of the CBAHI on PHCs. Almutairi and Al Shamsi45 note that there has been little information available about the quality of primary health care since the last review of the quality of PHCs in the KSA of Al-Ahmadi and Roland.46
The absence of research could be a result of a lack of understanding with regards to the accreditation programme.6 Therefore, scholars suggest that research on the effectiveness of the CBAHI is needed to identify its outcomes and would help to improve the programme,6 as it has been suggested that CBAHI standards need to be more strongly linked to the KSA health system context.42
However, despite the call for further research on CBAHI accreditation effects, the KSA is still in the early stages of implementing accreditation and does not have enough knowledge. Therefore, there is a need to learn from the international experience of implementing accreditation in healthcare sectors, particularly for PHCs, as implementation is facing many challenges in improving quality.45 To avoid unintended consequences, find a better solution for the problem, and improve its accreditation policy, the KSA is advised to consider further research into the experiences of other countries.45
It has been recommended that future research be undertaken to explore the nature and uptake of accreditation in primary care.12 It is also suggested that research focuses more on comprehensive theoretical frameworks for studying accreditation effects and the purpose that accreditation serves.28,30 Therefore, this research explores the experience of countries implementing accreditation for PHCs using the lens of a PT theoretical framework, which is discussed in the following section.
Policy transfer: a lessons drawing tool for accreditation
What is policy transfer?
Policy transfer and lesson drawing have become common concepts within public policy analysis and political studies.47 This strategy has been used to explain processes within and between various political contexts47 and has gradually emerged as part of the comparative politics literature.48 PT has been deployed by policy analysts as a general concept that embraces the different reasons for public organizations to be engaged in policy learning.49
Dolowitz and Marsh (45, p.344) define PT as “a process in which knowledge about policies, administrative arrangements and institutions, in one time and/or place, is used in the development of policies, administrative arrangements, and institutions in another time and/or place”. This is a policy development theory that aims to make sense of a process in which knowledge about policies or systems in one sector or level of governance is used to develop another sector, policy or system.49 This is not an explanatory theory but is viewed more as an analogical model that implies similarities between two entities.50
One of the frequently cited reasons for PT is innovation and experimentation through applying an existing solution in a different way.17 There are three types of transfer process: voluntary (lesson-drawing), direct coercive transfer, and a mixture of the two (negotiated).48,49 The type of transfer will vary between cases as PT depends on many factors, such as the location of the transfer and the policymakers involved in the process.51
PT gives policymakers the possibility to draw lessons from other nations that have faced the same problems. A policy can transfer with some adaptations if the lesson is positive but, if lessons are negative, the response will be based on observing what not to do based on watching the mistakes of others.52 Policymakers who are interested in improving quality or making more rational decisions might engage in a search process of policies and practices in other countries.53 Furthermore, the absence of a scientific consensus, lack of knowledge, a crisis or a political conflict can induce policymakers to look elsewhere to experiments that have been developed in response to similar conditions.53
However, there is a concern about the ability of policymakers to assess the effect of a proposed policy or programme before it takes place.17 Sometimes, policymakers are persuaded by ideas from abroad and plan a policy application without a rational evaluation of the idea,17 following the assumption that when a policy was successful in one country, it will be successful in another.51 These cases may lead to policy failure. According to Dolowitz and Marsh,51 uninformed, inappropriate, or incomplete transfer can cause policy failure. Therefore, the following section introduces the criteria for assessing policy transfer proposed by Mossberger et al.17 for policymakers to make prospective policy evaluations.
Prospective policy evaluation framework
This framework helps to assess PT as a form of prospective policy evaluation. It offers policymakers information and guidance on an appropriate way to engage with PT, and gives them the ability to predict the effect of a policy before its adoption.17 PT requires awareness of information about the policy or programme applied elsewhere and a prospective evaluation to assess the policy and its application in a new and different setting.17 Therefore, this framework provides a set of criteria that is required to engage in a rational examination of a policy that is under consideration for transfer and the possibility of its application in a new setting.17
The first criterion is Awareness, which focuses on the scope of information and the adequacy and accuracy of information as two important criteria for information quality. The quality of the information obtained by prospective adopters has an important impact on their capacity to evaluate its usefulness.17 The second criterion is Assessment, the process of which should consider the similarity of problems and goals, policy performance, and differences in settings. The final criterion is Application and depends on adequate information and a thorough assessment of the nature of the problem, policy aims, performance, and environment.17
Methodology
Rationale for selecting the research method: systematic literature review
There are different approaches to conducting a literature review (LR): a full systematic review; a rapid review; a traditional literature review; a narrative review; a structured review; and a scoping review.54 A systematic review is a detailed review of high-quality literature that is conducted by a team of researchers to identify the available literature on a specific topic, undertaken by quality appraisal of the relevant evidence and includes a re-analysis of results, which is referred to as meta-analysis.55 However, it is not always possible to conduct a full systematic review if there is a lack of time and resources. Thus, this research conducted an LR using a systematic approach, which is referred to as a systematic literature review (SLR).56 This is one of the review types that can be conducted with a stand-alone reviewer.57
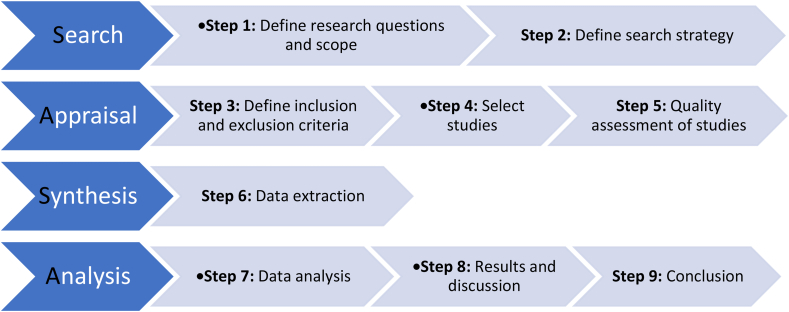
To undertake an SLR, several steps should be followed. However, there is different guidance in the literature according to the type of LR being conducted. A review will commonly start by identifying a research question, then conducting a search, followed by appraising and analysing the relevant literature, using a systematic approach.55 However, this review is carried out by one researcher hence it is recommended to generate an explicit research protocol or strategy that helps to reduce the possibility of researcher bias in data selection and analysis.58 Grant and Booth59 presented a simple analytical framework for identifying the research protocols for an SLR: Search, Appraisal, Synthesis and Analysis (SALSA). This review was conducted according to the SALSA steps shown in Figure 1. Data analysis was performed against the PT framework17 which can seek more than one answer to the research question. According to Kraus et al.,60 for SLRs, having more than one answer for research questions or hypotheses will help to overcome biases and resulting in a high level of confidence in the review article (see Fig. 2).
Figure 1.
SALSA steps for an SLR.59
Figure 2.
PRISMA flowchart.83
Search
Research question
-
-
What are the lessons that the KSA can learn from developed and developing countries' experience of implementing accreditation programmes for PHCs?
Search strategy
The search used a systematic approach to identify relevant studies. A rapid search using the Google Scholar search engine was conducted prior to the main search by using broad terms such as “accreditation in primary health care” to identify the available literature, determine the search strategy, and set the search terms. The search was conducted in August 2021 using the Web of Science database as one of the main databases for all subjects, especially in social sciences. The search used the following keywords and Boolean operators: “accreditation” AND “primary health care” OR “general practice” OR “primary care” OR “primary healthcare”. Although there are many research efforts that investigated accreditation within health care, the number of studies on PHCs was considerably limited; hence, this research screened all published papers within the scope of the research without a time-bounded period.
Appraisal
Study selection, screening, and quality assessment
The selection of the studies was based on the inclusion and exclusion criteria outlined below. Generally, there was no limitation to the period of time or a specific study design; however, non-English-language studies were excluded due to the lack of time for translation. Only studies with primary data were included because researchers of primary studies in the subject area tend to refer to the same base studies.57
Inclusion criteria
-
1.
Studies using primary data collection.
-
2.
Published in English.
-
3.
Focus on accreditation programmes implemented for PHCs in any country except the KSA.
-
4.
Studies that discuss accreditation for PHCs in general after its implementation.
Exclusion criteria
-
1.
Non-empirical studies or studies not based on primary data collection.
-
2.
Non-English-language studies.
-
3.
Studies conducted in the KSA.
-
4.
A focus on other health settings, such as hospitals.
-
5.
Studies are not available for free.
Quality assessment
SLRs usually require a quality assessment to check the quality and relevance of the studies included in the review. According to Gough,61 a study might meet the initial inclusion criteria but may not meet the quality and relevance criteria for the review. It is important to assess the extent to which each piece of the evidence contributes to answering the review question.61 This review used the Weight of Evidence (WoE) framework offered by Gough61 to appraise the quality and relevance of the studies selected for this review. The framework has three criteria to assess the study WoE (A, B, and C) that include different dimensions: Transparency, Accuracy, Accessibility, Specificity, Purposivity, Utility and Propriety (TAPUPAS) as shown in Table 2. Articles that met five dimensions or more were classified as high and moderate quality studies that checked less than five dimensions, and studies that only checked three or less considered as low. The weight of each study is presented in the table of included studies in Appendix 1.
Table 2.
TAPUPAS dimensions and WoE framework for appraising the quality and relevance of reviews.61
| Weight of Evidence (A) | Weight of Evidence (B) | Weight of Evidence (C) |
|---|---|---|
| Generic quality of execution of study | Review specific on appropriateness of method | Review specific in focus/approach of study to the review question |
|
Transparency: clarity of purpose Accuracy: accurate Accessibility: understandable Specificity: method-specific quality |
Purposivity: fit for purpose method |
Utility: provides relevant answers Propriety: legal and ethical research |
Synthesis
Data extraction
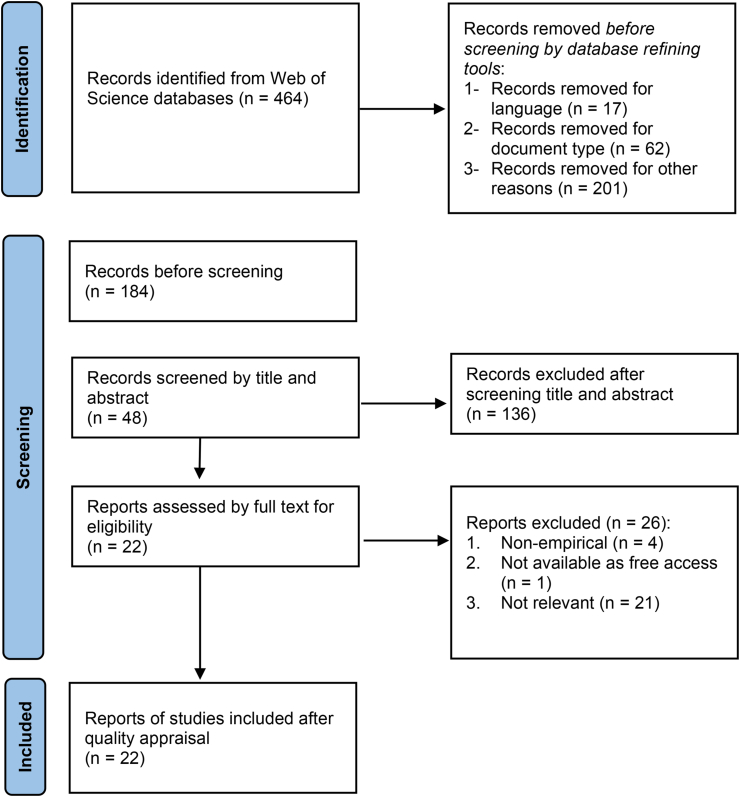
The research database search yielded 464 references. After using the database refining tools, 184 articles were screened by their titles and abstracts: 136 articles were excluded and 48 were assessed by reviewing the full text to check eligibility. Finally, 22 studies were included in the review based on the inclusion criteria and quality appraisal outlined above .33,62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82 The screening and selection steps are presented in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart in Figure 1. The data extracted from each study were charted using a table with the following headings: reference, study objective, study design, study sample, study location, key findings, and quality/relevance, as shown in Appendix 1.
Findings
Descriptive results
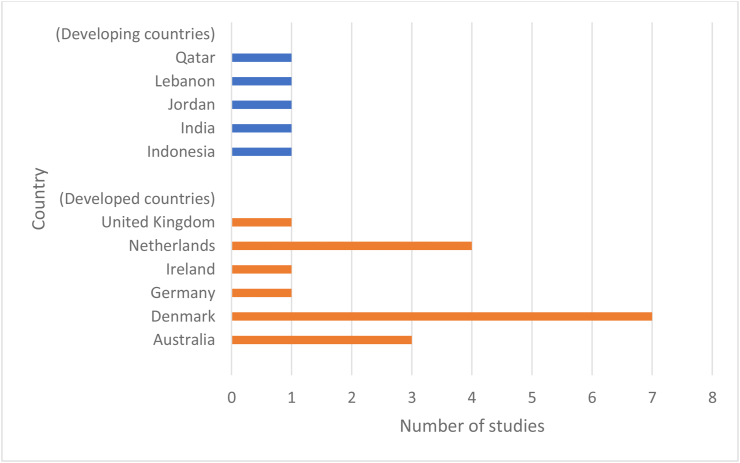
The research results yielded 22 publications on accreditation in the primary healthcare context. The characteristics of the studies included (objectives, study design, settings, quality, and key findings) are presented in Appendix 1. The studies included in the review were conducted in 11 different countries, as shown in Figure 3. The majority of the 22 studies (n = 17) were situated in developed countries and only five were conducted in developing countries. Denmark had the highest number of studies (n = 7). It was noted that all Denmark studies were conducted in the period between 2017 and 2021 which is after the accreditation scheme become mandatory in 2016.81,82 It is important to note that in relation to terminology, some countries use the term general practice (GP) when referring to PHCs; this is noted in the reported findings.
Figure 3.
Number of studies included in the review.
Prospective policy evaluation
This section is discussed in accordance with the Mossberger et al.17 framework for prospective policy evaluation discussed earlier in section three and presented in Appendix 2. The table template was inspired by Powell et al.84
Awareness
Scope of information
Policymakers who are interested in PT should have information about the different locations that have used the policy.17 This information should cover variations between policies and whether the transferred policies have proven successful, been implemented in countries with similar problems, or have similarities in other areas.17
In Australia, Abou Elnour et al.73 examined the impact of Australian General Practice Accreditation Limited (AGPAL) accreditation on GP patient safety and indicated some room for improvement. Debono et al.76 analysed the strengths and limitations of the GP accreditation programme and Tirimacco et al.62 concluded some lessons from their evaluation of accreditation programmes.
Moving to Europe, in Germany, Szecsenyi et al.77 explored the effectiveness of European Practice Assessment (EPA) of PHCs focusing on quality and safety. In the UK, Campbell et al.78 presented an evaluation of the Primary Medical Care Provider Accreditation (PMCPA) pilot version content and development. Riain et al.79 focused on the role of leadership in developing an accreditation system for practitioners in GP in Ireland.
In Denmark, Andersen et al.80 evaluated the impact of mandatory accreditation for GP. Later, Andersen et al.65 analysed whether there was a correlation between general practitioners' retirement, job satisfaction and attitudes and mandatory accreditation. Due et al.81 explored the experience and attitudes of staff towards understanding accreditation standards, and later examined surveyors’ reflections on accreditation standards based on survey visits.82 During mandatory accreditation, different implementation support was provided to PHCs and Overgaard Jensen et al.66 analysed the usefulness of the support provided and its variations. Kousgaard et al.63 explored how general practitioners and staff experienced the impact of the mandatory accreditation programme in Denmark; Riisgaard et al.64 investigated whether the accreditation of GP in Denmark promoted patient-reported quality of care and patient satisfaction.
In studies located in the Netherlands, van Doorn-Klomberg et al.67 explored the impact of an accreditation programme on the quality of care related to diabetes, chronic obstructive pulmonary disease and cardiovascular disease. Nouwens et al.68 assessed the impact of the programme based on the experience of professionals. Nouwens et al.69,70 identified the effectiveness and efficiency of an accreditation programme focusing on cardiovascular risk management (CVRM). Nouwens et al.69 mainly focused on a practice accreditation programme, whereas Nouwens et al.70 focused on improvement plans for the programme.
In developing countries, studies from India75 and Lebanon33 examined the impact of accreditation on PHCs. In Indonesia, Limato et al.72 analysed the factors that influenced the process of QI in PHCs. Ghareeb et al.74 presented the changes after adopting an accreditation programme for PHCs in Qatar, and in Jordan, Alyahya et al.71 explored the perception of accreditation among PHC staff.
Adequacy and accuracy of information
Policy adopters or countries that borrow policies need accurate information about the programmes concerned, including their evaluation results and criticisms.17 This information can be obtained from sources such as conferences, site visits, or published materials.17 However, these sources of information are not usually available.84 Therefore, this section examines the amount of detail contained in studies.
Information varied from one country to another in the studies reviewed and within the same country. For example, in Australian cases, Debono et al.76 provided more details related to program strengths, enablers, and limitations than Tirimacco et al.62 and Abou Elnour et al.73 In the studies from Germany,77 the UK78 and Ireland,79 Szecsenyi et al.77 provided less detailed information than Campbell et al.78 and Riain et al.79 regarding practice and process of the program.
Most of the cases from Denmark had highly detailed information.63,64,80, 81, 82 However, there were fewer details in the two other studies.65,66 There was no significant variation in the level of detail in studies conducted in the Netherlands.67, 68, 69, 70 In the cases reported in Jordan,71 Lebanon33 and Indonesia,72 there was more information than the cases examined in Qatar74 and India.75
Assessment
Similarity of problems and goals
To avoid policy failure, adopting countries should identify the policy goals and the problems the policy has addressed and recognize the differences and similarities in problems and goals.17
In Australia, both Tirimacco et al.62 and Abou Elnour et al.73 refer to the goal of accreditation as mainly being to improve the quality of care. Debono et al.76 highlighted the problem associated with the low engagement of stakeholders with accreditation. Cases from Germany77 and the UK78 had the goal of continuous quality improvement. A study from Ireland79 discussed the goal of defining the accreditation standards as governing the care of service delivery.
All the studies conducted in Denmark reviewed in this study were derived from the mandatory accreditation scheme in GP to achieve a national goal.63, 64, 65, 66,80, 81, 82 However, in the Netherlands, all the cases shared the same goals of the improvement of quality, clinical procedures and outcomes.67, 68, 69, 70
All the cases from developing countries mainly highlighted their goals. In Jordan,71 the goal was to reduce harm to patients and improve health outcomes. Cases in Lebanon and Indonesia33,72 referred to the goal of improving quality of care. However, El-Jardali et al.33 pointed to another goal of accreditation, which is moving the focus of the healthcare system from treatment to preventive services. In Qatar's study,74 accreditation was developed to set standards and to enhance the quality of care, and in India,75 the goal of accreditation was to have public recognition of healthcare reliability and authenticity.
Policy performance
The adopted policy should be assessed by policymakers to measure the extent of its success or the aspects in which it was successful.17 Nonetheless, problems do not mean a total rejection of a policy.17
In Australia, Abou Elnour et al.73 noted that accreditation had a positive impact on improving some quality and safety aspects in GP. Debono et al.76 discussed the strengths and weaknesses of the accreditation programme and factors that influenced programme success, such as stakeholder engagement or disengagement. However, Tirimacco et al.62 had no clear discussion of success or failure but instead outlined recommendations for improving accreditation implementation.
With regards to Germany,77 there was a significant improvement in all domains of the EPA after implementation in GP. In the UK,78 the PMCPA was acceptable to most of the clinics but employees (especially managers) were complaining about the workload. However, in the case of Ireland,79 there was no clear success or failure.
In cases located in Denmark, Andersen et al.80 noted that changes were ambiguous in terms of the chosen clinical outcomes. Andersen et al.65 suggested that practice retirement was connected with job dissatisfaction but not with mandatory accreditation schemes. Due et al.81 emphasized the importance of support for staff to understand accreditation standards. Due et al.82 also noted that the success of the survey visit was highly dependent on the ability of staff to convey realistic information about the practice. Kousgaard et al.63 pointed out that accreditation can affect GP clinics in many different ways but that staff sometimes believed that accreditation effects were low compared with the resources used. Overgaard Jensen et al.66 discussed types of support for GP during the accreditation process. Riisgaard et al.64 concluded that accreditation did not promote patient satisfaction.
In the Netherlands, van Doorn-Klomberg et al.67 noted that only a few improvements in the quality of PHC found were attributed to the accreditation programme. Nouwens et al.69 found that it was important for practices to have more information about the effectiveness and efficiency of an accreditation programme. Both Nouwens et al.70 and Nouwens et al.68 concluded that accreditation in GP did not have a positive effect on all outcome elements.
In Jordan, Alyahya et al.71 demonstrated that coercive pressure may have compelled PHCs to implement accreditation although this may have led to dysfunctional consequences. Limato et al.72 noted that the success of QI intervention in Indonesian PHCs depended on many factors, such as leadership. Accreditation was an important step to improving the quality of PHCs in Lebanon's case.33 In the Qatar study, the accreditation was related with QI and organizational learning.74 Joseph75 reported that in order to have successful accreditation in India, it must be used as a tool for the comprehensive and continuous transformation of healthcare services, including infrastructural and interpersonal aspects.
Differences in settings
Borrowing countries that seek a policy that is appropriate to its local context85 should assess the extent to which the features of their policy environment differ from the policy's original setting and whether these differences matter in terms of implementation or outcomes.17 Such assessment includes the existence of other policies that affect efficacy and contextual variables, such as political, social, and economic institutions, political culture, public opinion, and the available resources.17
All of the Australian cases examined discussed AGPAL. However, neither Tirimacco et al.62 nor Abou Elnour et al.73 discussed any other variation in the Australian setting. However, Debono et al.76 discussed the Practice Incentives Program (PIP); this is the source of funding that supports GP activities.
In Germany, Szecsenyi et al.77 studied the EPA as coordinated by the AQUA-Institute and noted that the programme involved both quality assessment and quality improvement. The studies conducted in the UK78 and Ireland79 analysed the local accreditation programme. However, in the Ireland study, Riain et al.79 also discussed the complex nature of the healthcare system and the lack of significant resource allocation.
All the cases in Denmark were derived from the mandatory accreditation policy and examined local accreditation.63, 64, 65, 66,80, 81, 82 However, only two studies discussed the regional support received by PHCs during the implementation of accreditation.66,81
Similarly, all of the cases in the Netherlands studied the same local accreditation programme. Some cases noted that the Dutch accreditation programme for PHCs focused strongly on chronic illness care.68, 69, 70 However, there was only one study that discussed the role of bundled payment in the Dutch accreditation process.67
Moving to the developing countries considered in this review, Alyahya et al.71 discussed the effect of coercive pressure and limited resources in Jordan. Limato et al.72 noted the importance of financial and human resources in Indonesia. Similarly, El-Jardali et al.33 discussed the effect of a lack of financial resources in Lebanon. Joseph75 discussed the weak structural health system in India and suggested that it was important to integrate accreditation policy at all health system levels. Most of the cases in developing countries analysed local accreditation with the support or collaboration of external accreditation bodies. However, it seems that Qatar had only implemented an external accreditation programme: the Accreditation Canada International (ACI).74
Application
The final criterion is whether the policy information in another country is to be utilized in the decision-making process.17 It is important at this point in the PT to ensure that the application is based on accurate and adequate information and an assessment of the nature of the problem, the goals of the policy, policy performance, and the policy environment.17 However, the studies analysed are official materials from government bodies and, therefore, this criterion will highlight the recommendations of studies based on the country's experience of accreditation for PHCs.
All Australian studies offered recommendations to improve the accreditation implementation in PHCs.62,73,76 The studies set in the UK78 and Germany77 offered clearer recommendations than the case examined in Ireland.79 In Denmark, all cases had clear recommendations but these varied between studies in terms if either being related to the accreditation programme or to GP.63, 64, 65, 66,80, 81, 82 Similarly, all of the studies reviewed by the Netherlands offered recommendations. However, some emphasized the importance of having further evidence about the effectiveness and efficiency of the programme,67,70 whereas others focused more on the programme itself.68,69
Most of the studies located in developing countries, such as Jordan,71 Lebanon,33 and India,75 provided a direct discussion of their recommendations in each of their conclusions. In comparison, Qatar's study74 did not have clear recommendations and Limato et al.72 only discussed the important factors relating to the accreditation process in Indonesia.
Discussion
The main purpose of this review was to explore lessons that the KSA could draw from the experience of developed and developing countries with regards to implementing accreditation for PHCs. The review assessed the transferability of the lessons provided by these countries to the KSA accreditation policy using the policy evaluation criteria: awareness, assessment, and application of the Mossberger et al. framework.17 Appendix 2 shows the analysis of each article according to prospective policy transfer criteria.
In the criteria for awareness, the scope of information covered different locations. Each article focused on one specific country with repetition for some countries. However, among the countries that had more than one article, we found that information varied between different articles. This can be beneficial for the KSA to gain sight of the locations that adopted the same policy. In addition, the adequacy and accuracy of information were different between countries and within studies in the same country. For example, Australia, Denmark, and the Netherlands were the only countries of those examined in the review (both developed and developing) that had multiple studies. Although Australia had implemented accreditation for PHCs before Denmark, it was surprising to see that Denmark (seven studies) had produced more studies than Australia (three studies); this could be due to the mandatory accreditation scheme. This could indicate that, as a developed country, Denmark has information that is more helpful for the KSA and had applied the same mandatory accreditation; this is a key similarity between the two countries. However, other countries might have more information but this might not be documented or remains hidden from outsiders.24
This review also investigated the similarity of goals and problems as part of the assessment criterion. Most of the cases considered sharing the theme of accreditation as improving patient safety and quality of care as a goal. This appears to be similar to the KSA in terms of focussing on the goal of implementing accreditation for PHCs (see Section 2). However, there was a lack of detail relating to the problems encountered in most cases. This shortage of information can cause difficulties in recognizing the differences in problems that can unexpectedly lead to policy failure.17 In terms of policy performance, the majority of studies indicated policy success and some discussed policy failure. Although most cases in developed and developing countries highlighted some policy success, it seems that the studies conducted in Denmark focused on policy failure. This could be related to the mandatory accreditation scheme, as Denmark was the only country among those included that had applied this scheme for PHCs. However, this variation in experience among countries would provide a clearer vision of accreditation success or failure in different settings, as it has been argued that a balanced assessment for PT should include evidence of policy effects, advantages and limitations of the policy, or variations on a policy idea.17
Regarding the difference in settings, most accreditation programmes in developed countries, such as Australia and Denmark, were governed by local independent institutions; this is unlike the situation in developing countries, where programmes are more likely to be launched in collaboration with external accreditation bodies from other countries and are usually managed by the government. This concurs with the findings of Braithwaite et al.14 and Mansour et al.13 in respect of accreditation programmes in LMICs being less independent, typically inspired by international models, and more legally associated with the government. In addition, most of the developing country cases in the review noted the issue of a lack of resources and the weak infrastructure of the health system. This was in line with the conclusion of the review by Mansour, Boyd and Walshe13 in that a lack of financial resources was a significant problem for many developing LMICs.
Turning to the final criterion, application, most of the studies offer recommendations. There was agreement on recommendations among developed and developing countries. The recommendations were related to different aspects of the implementation process: provide education and training; provide support for staff and organizations during implementation; offer financial incentives; improve programme standards; change the organizational culture; assess the readiness of PHCs before the actual implementation and staff involvement and collaboration in the process; and promote awareness and the attitude of staff towards accreditation. This finding is consistent with Braithwaite et al.,14 who argued that regardless of country characteristics, accreditation programmes were influenced by factors such as continuing support from government, incentives to encourage participation in accreditation, and ongoing refinement and improvement of accreditation programmes. However, to learn from these suggestions, the KSA might have to consider other factors, such as culture. According to Andersen et al.,80 other countries that aim to learn from Denmark's experience have to make further considerations for differences in healthcare systems and cultural factors.
This review indicates that as the KSA has a unique context, there is no specific nation that is more suitable than the others from which to draw lessons. For example, according to some criteria, Denmark seems a more appropriate model, as it offers the most detailed information and shares the existence of a mandatory accreditation scheme. On the other hand, Denmark does not share other aspects, such as the administrative structure of the country or its culture. Qatar was expected to offer more lessons as a country from the same region and one that shares some of the KSA's cultural attributes. However, information from Qatar was very limited and there was a difference in the setting; for example, Qatar applied for external accreditation from the ACI.
The similarities among the recommendations from the various countries considered in this review might indicate that there are factors that need to be considered regardless of the country concerned, such as providing ongoing education, training, and support for organizations and staff. However, the way in which this support should be provided is based on what is appropriate for the local culture. The different settings of each country play a major role in the differences between the transferred lessons. This suggests that it is important for policymakers to consider what is suitable for the KSA context when looking for lessons from other nations.
Recommendations
Although financial resources are one of the important factors in implementing accreditation in healthcare organizations, human resources are the backbone of any healthcare system and the shortage of health workforce has been an international concern.34 The KSA has 27,38 physicians and 58,9 nurses and midwives per 10,000 population86; this is lower than the average number of the same personnel in Organisation for Economic Co-operation and Development (OECD) countries.87 Thus, it would seem to be important to pay personnel more attention, especially during the process of implementing an accreditation programme as this tends to increase the workload, which may affect job satisfaction.65 In addition, with regards to information, it might be appropriate for policymakers to look for sources other than the published literature, such as conferences or formal evaluation.17 This is because publications can be limited and are not always provided by the government.
Limitations
This review has several limitations. First, although this study has broad inclusion criteria to maximize the number of studies considered, one of the key limitations of this review is the small sample of studies. Second, although each study was quality appraised using the WoE framework, most of the relevant studies were included due to the limited number of studies that focused on PHCs. Third, due to a lack of time, this review only included English-language publications, which may have affected the results.
Despite the limitations of the findings within this review, our research remains important for the KSA to learn from other countries’ experience of accreditation programmes for PHCs, to maximize the effectiveness of their implementation. Future research could draw lessons from one specific nation, such as Denmark, or focus on lessons learned about a specific dimension of PHCs.
Conclusion
The KSA has made the CBAHI accreditation programme mandatory for all healthcare facilities in the country, including PHCs. In light of the country's 2030's vision, this is expected to help the health sector to achieve the objective of improving quality in the HSTP. However, insufficient levels of knowledge and understanding have been acquired and the KSA is still considered to be in the early stages of adopting this accreditation policy. Therefore, this study aimed to review the available literature and explore lessons that could be drawn by the KSA from developed and developing countries that had implemented accreditation programmes for PHCs. This review included 22 studies from different countries. The review addressed the lessons learned by using the PT evaluation framework17 as this is a useful framework for policymakers to assess and analyse the accreditation policy lessons of different countries.
The review indicated that, due to variations in the amount of information between countries, differences in settings, and the unique situation of the KSA, there is no ideal country-based experience from which the KSA can transfer lessons. Denmark was the country that offered the greatest amount of information; however, this setting might not be close enough to the culture of the KSA. Moreover, although Qatar was expected to be more suitable for the KSA, the information available was very limited. However, it would be beneficial for the KSA to learn from Qatar's recommendations, since their accreditation programmes are influenced by similar factors. One of the important recommendations provided from this review is to provide staff with more attention and support, especially during the implementation process, as they are closer to the accreditation activities.
Regardless of this study's limitations, its contribution can be helpful for policy and decision-makers in the KSA, as it gives an overview of other countries that have adopted a similar policy, together with information about their experience.
Acknowledgment
This study was completed as part of the master's degree requirements. The author would like to acknowledge the scholarship provider King Abdul-Aziz University and would like to thank Prof. Martin Powell for all his support and guidance.
Footnotes
Peer review under responsibility of Taibah University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtumed.2022.12.012.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Greenfield D., Braithwaite J. Health sector accreditation research: a systematic review. Int J Qual Health Care. 2008;20:172–183. doi: 10.1093/intqhc/mzn005. [DOI] [PubMed] [Google Scholar]
- 2.Alshamsi A.I., Thomson L., Santos A. What impact does accreditation have on workplaces? A qualitative study to explore the perceptions of healthcare professionals about the process of accreditation. Front Psychol. 2020;11:1–13. doi: 10.3389/fpsyg.2020.01614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicklin W. 2013. The value and impact of health care accreditation : a literature review, Accreditation Canada. 1; pp. 1–16.http://www.accreditation.ca/uploadedFiles/Value of Accreditation_EN.pdf [Google Scholar]
- 4.Pomey M.P., Lemieux-Charles L., Champagne F., Angus D., Shabah A., Contandriopoulos A.P. Does accreditation stimulate change? A study of the impact of the accreditation process on Canadian healthcare organizations. Implement Sci. 2010;5 doi: 10.1186/1748-5908-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braithwaite J., Westbrook J., Pawsey M., Greenfield D., Naylor J., Iedema R., et al. A prospective, multi-method, multi-disciplinary, multi-level, collaborative, social-organisational design for researching health sector accreditation [LP0560737] BMC Health Serv Res. 2006;6:1–10. doi: 10.1186/1472-6963-6-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Almasabi M., Thomas S. The impact of Saudi hospital accreditation on quality of care: a mixed methods study. Int J Health Plann Manag. 2017;32:e261–e278. doi: 10.1002/hpm.2373. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization . World Health; 2003. Quality and accreditation in health care services: a global review. [Google Scholar]
- 8.Mansour W. 2018. Policy transfer of hospital accreditation to low-middle income countries: drawing lessons from eastern mediterranean countries. [Google Scholar]
- 9.Khan S., Yousefinezhadi T., Hinchcliff R. The impact of hospital accreditation in selected Middle East countries: a scoping review. J Health Organisat Manag. 2021 doi: 10.1108/JHOM-04-2021-0159. [DOI] [PubMed] [Google Scholar]
- 10.Alasmari S., Williams S., Rich N., Rea D. Sustainability of quality improvement initiatives within the Saudi ministry of health hospitals: an institutional overview. Saudi J Health Syst Res. 2021;1:3–10. doi: 10.1159/000514179. [DOI] [Google Scholar]
- 11.Alasmari A. 2018. Measurement of healthcare quality: a mixed-methods comparative study of accredited and non-accredited hospitals in KSA.http://usir.salford.ac.uk/id/eprint/50286/ [Google Scholar]
- 12.O'Beirne M., Zwicker K., Sterling P.D., Lait J., Robertson H.L., Oelke N.D. The status of accreditation in primary care. Qual Prim Care. 2013;21:23–31. [PubMed] [Google Scholar]
- 13.Mansour W., Boyd A., Walshe K. The development of hospital accreditation in low- and middle-income countries: a literature review. Health Pol Plann. 2020;35:684–700. doi: 10.1093/heapol/czaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Braithwaite J., Shaw C.D., Moldovan M., Greenfield D., Hinchcliff R., Mumford V., et al. Comparison of health service accreditation programs in low- and middle-income countries with those in higher income countries: a cross-sectional study. Int J Qual Health Care. 2012;24:568–577. doi: 10.1093/intqhc/mzs064. [DOI] [PubMed] [Google Scholar]
- 15.World Bank, World Bank Country and Lending Groups, (n.d.). https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 16.United Nations . 2020. World economic situation and prospects.https://www.un.org/development/desa/dpad/publication/world-economic-situation-and-prospects-2020/ [Google Scholar]
- 17.Mossberger K., Wolman H. Policy transfer as a form of prospective policy evaluation: challenges and recommendations. Publ Adm Rev. 2003;63:428–440. doi: 10.1111/1540-6210.00306. [DOI] [Google Scholar]
- 18.Jovanović B. Hospital accreditation as method for assessing quality in healthcare. Arch Oncol. 2005;13:156–157. [Google Scholar]
- 19.Shaw C. Accreditation is not a stand-alone solution. East Mediterr Health J. 2015;21:226–231. doi: 10.26719/2015.21.3.226. [DOI] [PubMed] [Google Scholar]
- 20.Braithwaite J., Greenfield D., Westbrook J., Pawsey M., Westbrook M., Gibberd R., et al. Health service accreditation as a predictor of clinical and organisational performance: a blinded, random, stratified study. Qual Saf Health Care. 2010;19:14–21. doi: 10.1136/qshc.2009.033928. [DOI] [PubMed] [Google Scholar]
- 21.Al-Awa B., De Wever A., Melot C., Devreux I. An overview of patient safety and accreditation: a literature review study. Res J Med Sci. 2011;5:200–223. doi: 10.3923/rjmsci.2011.200.223. [DOI] [Google Scholar]
- 22.Hinchcliff R., Greenfield D., Moldovan M., Westbrook J.I., Pawsey M., Mumford V., et al. Narrative synthesis of health service accreditation literature. BMJ Qual Saf. 2012;21:979–991. doi: 10.1136/bmjqs-2012-000852. [DOI] [PubMed] [Google Scholar]
- 23.Ng G.K.B., Leung G.K.K., Johnston J.M., Cowling B.J. Factors affecting implementation of accreditation programmes and the impact of the accreditation process on quality improvement in hospitals: a SWOT analysis. Hong Kong Med J. 2013;19:434–446. doi: 10.12809/hkmj134063. [DOI] [PubMed] [Google Scholar]
- 24.Smits H., Supachutikul A., Mate K.S. Hospital accreditation: lessons from low- and middle-income countries. Glob Health. 2014;10:1–8. doi: 10.1186/s12992-014-0065-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Melo S. The impact of accreditation on healthcare quality improvement: a qualitative case study. J Health Organisat Manag. 2016;30:1242–1258. doi: 10.1108/JHOM-01-2016-0021. [DOI] [PubMed] [Google Scholar]
- 26.Pomey M.P., François P., Contandriopoulos A.P., Tosh A., Bertrand D. Paradoxes of French accreditation. Qual Saf Health Care. 2005;14:51–55. doi: 10.1136/qshc.2004.011510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alkhenizan A., Shaw C. Impact of accreditation on the quality of healthcare services: a systematic review of the literature. Ann Saudi Med. 2011;31:407–416. doi: 10.4103/0256-4947.83204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brubakk K., Vist G.E., Bukholm G., Barach P., Tjomsland O. A systematic review of hospital accreditation: the challenges of measuring complex intervention effects. BMC Health Serv Res. 2015;15 doi: 10.1186/s12913-015-0933-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greenfield D., Braithwaite J. Developing the evidence base for accreditation of healthcare organisations: a call for transparency and innovation. Qual Saf Health Care. 2009;18:162–163. doi: 10.1136/qshc.2009.032359. [DOI] [PubMed] [Google Scholar]
- 30.Swathi K.S., Gopalkrishna B., Somu G. Impact of accreditation on performance of healthcare organizations. Int J Qual Serv Sci. 2020;12:85–108. doi: 10.1108/IJQSS-10-2018-0085. [DOI] [Google Scholar]
- 31.Scrivens E. Putting continuous quality improvement into accreditation: improving approaches to quality assessment. Qual Saf Health Care. 1997;6:212–218. doi: 10.1136/qshc.6.4.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tabrizi J.S., Gharibi F. Primary healthcare accreditation standards: a systematic review. Int J Health Care Qual Assur. 2019;32:310–320. doi: 10.1108/IJHCQA-02-2018-0052. [DOI] [PubMed] [Google Scholar]
- 33.El-Jardali F., Hemadeh R., Jaafar M., Sagherian L., El-Skaff R., Mdeihly R., et al. The impact of accreditation of primary healthcare centers: successes, challenges and policy implications as perceived by healthcare providers and directors in Lebanon. BMC Health Serv Res. 2014;14 doi: 10.1186/1472-6963-14-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al Asmri M., Almalki M.J., Fitzgerald G., Clark M. The public health care system and primary care services in KSA: a system in transition. East Mediterr Health J. 2020;26:468–476. doi: 10.26719/emhj.19.049. [DOI] [PubMed] [Google Scholar]
- 35.Ministry of Health . 2007. Health sector transformation strategy. [DOI] [Google Scholar]
- 36.Al Khashan H., Abogazalah F., Alomary S., Nahhas M., Alwadey A., Al-Khudhair B., et al. Primary health care reform in KSA: progress, challenges and prospects. East Mediterr Health J. 2021;27:1016–1026. doi: 10.26719/emhj.21.042. [DOI] [PubMed] [Google Scholar]
- 37.AlMubarak S.H., Alfayez A.S., Alanazi A.T., Alwuhaimed L.A., Bo Hamed S.S. Autonomy, accountability, and competition: the privatisation of the Saudi health care system. J Taibah Univ Med Sci. 2021;16:144–151. doi: 10.1016/j.jtumed.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Central Board for Accreditation of, Institutions Healthcare . CBAHI; 2015. CBAHI at a glance.https://portal.cbahi.gov.sa/english/about-us/cbahi-at-a-glance [Google Scholar]
- 39.CBAHI, CBAHI Standards, (n.d.). https://portal.cbahi.gov.sa/english/cbahi-standards (accessed 3 November 2022).
- 40.Alsakkak M.A., Alwahabi S.A., Alsalhi H.M., Shugdar M.A. Outcome of the first Saudi central board for accreditation of healthcare institutions (CBAHI) primary health care accreditation cycle in KSA. Saudi Med J. 2017;38:1132–1136. doi: 10.15537/smj.2017.11.20760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.CBAHI . 2022. Status of accreditation for healthcare facilities.https://portal.cbahi.gov.sa/english/statusaccreditation/s [Google Scholar]
- 42.Alkhenizan A., Shaw C. Assessment of the accreditation standards of the central board for accreditation of healthcare institutions in KSA against the principles of the international society for quality in health care (ISQua) Ann Saudi Med. 2010;30:386–389. doi: 10.4103/0256-4947.67082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Al Otaibi A., Kattan W., Nabil A. The impact of Saudi (CBAHI) accreditation on enhancing patient safety and improving the quality of care indicators. La Prensa Med Argentina. 2020;106:1–5. doi: 10.47275/0032-745X-198. [DOI] [Google Scholar]
- 44.Almuraikhi A., Alzahrani F. Assessment of primary health-care centers in Dammam and Khobar, KSA. A comparison between. Int J Sci Res. 2019;8:1–5. [Google Scholar]
- 45.Almutairi A.G., Al Shamsi H.S. Challenges to quality primary health care in KSA and potential improvements implemented by other systems: systematic review. Global J Health Sci. 2020;12:1. doi: 10.5539/gjhs.v12n9p1. [DOI] [Google Scholar]
- 46.AL-Ahmadi H., Roland M. Quality of primary health care in KSA: a comprehensive review. Int J Qual Health Care. 2005;17:331–346. doi: 10.1093/intqhc/mzi046. [DOI] [PubMed] [Google Scholar]
- 47.Benson D., Jordan A. What have we learned from policy transfer research? Dolowitz Marsh Revisit. 2012;9:366–378. doi: 10.1111/j.1478-9302.2011.00240.x. [DOI] [Google Scholar]
- 48.Dolowitz D., Marsh D. Who learns what from whom: a review of the policy transfer literature. Polit Stud Assoc. 1996;21:343–351. [Google Scholar]
- 49.Evans M. 2009. Policy transfer in critical perspective; pp. 243–268. Policy transfer in critical perspective, 30. [DOI] [Google Scholar]
- 50.Evans M., Davies J. Understanding policy transfer: a Multi-level; multi-disciplinary perspective. Publ Adm. 1999;77:361–385. [Google Scholar]
- 51.Dolowitz D.P., Marsh D. Learning from abroad: the role of policy transfer in contemporary policy-making. Governance. 2000;13:5–23. doi: 10.1111/0952-1895.00121. [DOI] [Google Scholar]
- 52.Rose R. What is lesson-drawing. J Publ Pol. 1991;11:3–30. https://www.jstor.org/stable/4007336 [Google Scholar]
- 53.Stone D. Learning lessons and transferring policy across time, space and disciplines. Polit Stud Assoc. 1999;19:51–59. [Google Scholar]
- 54.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 55.Aveyard H. McGraw-Hill Education; Maidenhead, United Kingdom: 2018. Doing a literature review in health and social care: a practical guide.http://ebookcentral.proquest.com/lib/bham/detail.action?docID=6212137 [Google Scholar]
- 56.Booth A., Sutton A., Papaioannou D. 2nd ed. SAGE Publications Inc.; London: 2016. Systematic approaches to a successful literature review. [Google Scholar]
- 57.Okoli C. A guide to conducting a standalone systematic literature review. Commun Assoc Inf Syst. 2015;37:879–910. doi: 10.17705/1CAIS.03743. [DOI] [Google Scholar]
- 58.Kitchenham B., Charters S. 2007. Guidelines for performing systematic literature reviews in software engineering. [Google Scholar]
- 59.Grant M.J., Booth A. 2009. A typology of reviews: an analysis of 14 review types and; pp. 91–108. [DOI] [PubMed] [Google Scholar]
- 60.Kraus S., Dasí-rodríguez S. 2020. The art of crafting a systematic literature review in entrepreneurship research; pp. 1023–1042. [Google Scholar]
- 61.Gough D. Weight of evidence: a framework for the appraisal of the quality and relevance of evidence. Res Pap Educ. 2007;22:213–228. doi: 10.1080/02671520701296189. [DOI] [Google Scholar]
- 62.Tirimacco R., Glastonbury B., Laurence C.O., Bubner T.K., Shephard M.D., Beilby J.J. Development of an accreditation program for point of care testing (PoCT) in general practice. Aust Health Rev. 2011;35:230–234. doi: 10.1071/AH09792. [DOI] [PubMed] [Google Scholar]
- 63.Kousgaard M.B., Thorsen T., Due T.D. Experiences of accreditation impact in general practice - a qualitative study among general practitioners and their staff. BMC Fam Pract. 2019;20:1–13. doi: 10.1186/s12875-019-1034-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Riisgaard H., Waldorff F.B., Kirstine Andersen M., Pedersen L.B. Does accreditation of general practice promote patient-reported quality of care? A natural cluster randomised experiment. BMJ Open. 2020;10:1–10. doi: 10.1136/bmjopen-2019-034465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Andersen M.K., Pedersen L.B., Waldorff F.B. Retirement, job satisfaction and attitudes towards mandatory accreditation: a Danish survey study in general practice. BMJ Open. 2018;8:1–6. doi: 10.1136/bmjopen-2017-020419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Overgaard Jensena M.L., Bro F., Mygind A. Implementation of healthcare accreditation in Danish general practice: a questionnaire study exploring general practitioners' perspectives on external support. Scand J Prim Health Care. 2021;39:85–91. doi: 10.1080/02813432.2021.1882084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Van Doorn-Klomberg A.L., Braspenning J.C.C., Wolters R.J., Bouma M., Wensing M. Effect of accreditation on the quality of chronic disease management: a comparative observational study. BMC Fam Pract. 2014;15:1–8. doi: 10.1186/s12875-014-0179-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nouwens E., Van Lieshout J., Wensing M. Determinants of impact of a practice accreditation program in primary care: a qualitative study. BMC Fam Pract. 2015;16:1–8. doi: 10.1186/s12875-015-0294-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nouwens E., Van Lieshout J., Adang E., Bouma M., Braspenning J., Wensing M. Effectiveness and efficiency of a practice accreditation program on cardiovascular risk management in primary care: study protocol of a clustered randomized trial. Implement Sci. 2012;7 doi: 10.1186/1748-5908-7-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nouwens E., van Lieshout J., Bouma M., Braspenning J., Wensing M. Effectiveness of improvement plans in primary care practice accreditation: a clustered randomized trial. PLoS One. 2014;9 doi: 10.1371/journal.pone.0114045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Alyahya M., Hijazi H., Harvey H. Explaining the accreditation process from the institutional isomorphism perspective: a case study of Jordanian primary healthcare centers. Int J Health Plann Manag. 2018;33:102–120. doi: 10.1002/hpm.2397. [DOI] [PubMed] [Google Scholar]
- 72.Limato R., Tumbelaka P., Ahmed R., Nasir S., Syafruddin D., Ormel H., et al. What factors do make quality improvement work in primary health care? Experiences of maternal health quality improvement teams in three Puskesmas in Indonesia. PLoS One. 2019;14 doi: 10.1371/journal.pone.0226804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Abou Elnour A., Hernan A.L., Ford D., Clark S., Fuller J., Johnson J.K., et al. Surveyors' perceptions of the impact of accreditation on patient safety in general practice. Med J Aust. 2014;201:S56–S59. doi: 10.5694/mja14.00198. [DOI] [PubMed] [Google Scholar]
- 74.Ghareeb A., Said H., El Zoghbi M. Examining the impact of accreditation on a primary healthcare organization in Qatar. BMC Med Educ. 2018;18 doi: 10.1186/s12909-018-1321-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Joseph S. Impact assessment of accreditation in primary and secondary public health-care institutions in Kerala, India. Indian J Publ Health. 2021;65:110. doi: 10.4103/ijph.ijph_827_20. [DOI] [PubMed] [Google Scholar]
- 76.Debono D., Greenfield D., Testa L., Mumford V., Hogden A., Pawsey M., et al. Understanding stakeholders' perspectives and experiences of general practice accreditation. Health Pol. 2017;121:816–822. doi: 10.1016/j.healthpol.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 77.Szecsenyi J., Campbell S., Broge B., Laux G., Willms S., Wensing M., et al. Effectiveness of a quality-improvement program in improving management of primary care practices. Can Med Assoc J. 2011;183:E1326–E1333. doi: 10.1503/cmaj.110412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Campbell S.M., Chauhan U., Lester H. 2010. Primary medical care provider accreditation (PMCPA): pilot evaluation; pp. 295–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Riain A.N., Collins C., O'Sullivan T. Developing accreditation for community based surgery: the Irish experience. Leader Health Serv. 2018;31:33–46. doi: 10.1108/LHS-01-2017-0001. [DOI] [PubMed] [Google Scholar]
- 80.Andersen M.K., Pedersen L.B., Siersma V., Bro F., Reventlow S., Søndergaard J., et al. Accreditation in general practice in Denmark: study protocol for a cluster-randomized controlled trial. Trials. 2017;18:1–9. doi: 10.1186/s13063-017-1818-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Due T.D., Thorsen T., Kousgaard M.B. Understanding accreditation standards in general practice - a qualitative study. BMC Fam Pract. 2019;20:1–12. doi: 10.1186/s12875-019-0910-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Due T.D., Thorsen T., Kousgaard M.B. The survey visit as a key evaluative event in accreditation-a qualitative study of survey visit experiences among surveyors and general practice professionals. BMC Fam Pract. 2021;22 doi: 10.1186/s12875-021-01497-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Powell M., King–Hill S. Intra-crisis learning and prospective policy transfer in the COVID-19 pandemic. Int J Sociol Soc Pol. 2020;40:877–892. doi: 10.1108/IJSSP-07-2020-0339. [DOI] [Google Scholar]
- 85.Portnoi L.M. Policy borrowing and reform education, globalization processing and local ccontext. Palgrave Macmillan US; New York: 2016. Mapping educational policy borrowing and lending; pp. 147–173. [DOI] [Google Scholar]
- 86.World Health Organization . Glob. Heal. Obs.; 2022. Medical doctors (per 10 000 population)https://www.who.int/data/gho/data/indicators/indicator-details/GHO/medical-doctors-(per-10-000-population [Google Scholar]
- 87.OECD, Health resources - doctors - OECD data, (n.d.). https://data.oecd.org/healthres/doctors.htm (accessed 7 November 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.