Abstract
Primary gastric malignant lymphoma is a rare tumor. The complications associated with lymphoma are perforation, bleeding, or upper gastrointestinal stricture. While it is well known that perforations in gastric lymphoma often occurs during chemotherapy, spontaneous perforation is extremely rare in patients who did not receive chemotherapy. This complication requires a surgical treatment.
Keywords: B‐cell lymphoma, emergency, gastric perforation, malignant lymphoma
Primary gastric malignant lymphoma is a rare tumor. The complications associated with this lymphoma are perforation, bleeding, or upper gastrointestinal stricture. While the perforation in gastric lymphoma during chemotherapy is well known, spontaneous perforation is extremely rare in chemotherapy‐naive patients.
1. INTRODUCTION
Gastrointestinal non‐Hodgkin lymphoma is the most common form of extra nodal lymphoma. 1 The complications associated with this lymphoma are perforation, bleeding, or upper gastrointestinal stricture. 2 Diffuse large B‐cell malignant lymphoma is the most frequent type of non‐Hodgkin gastric localization. Gastric perforation in diffuse large B‐cell lymphoma (DLBCL) during chemotherapy is a well‐known event. However, spontaneous gastric perforation in the absence of chemotherapy administration is extremely rare. 1 It is a potential life‐threatening complication. 3 Its management requires an emergent medical treatment and a surgical intervention. Even though this complication occurs in chemotherapy‐naïve patients, postoperative morbidity and mortality are increased due to a marked delay in initiating of chemotherapy. 3 In this article, we report a case of spontaneous gastric perforation of DLBCL in a chemotherapy‐naïve patient.
2. CASE PRESENTATION
A 39‐year‐old patient in the investigational phase, 2 months after the diagnosis of gastric malignant lymphoma, was presented to our emergency department with an acute abdominal pain. He had a severe epigastric pain for 12 h. His physical examination showed a fever (38.2°C), a tachycardia (100 bpm), a blood pressure of 90/60 mm Hg, and a distended painful abdomen.
Blood tests showed high white blood cell counts (10,700/mm3) and high CRP levels (59 mg/L).
Abdomen plain film showed small bowel's air‐fluid levels. Abdominal computed tomography revealed intraperitoneal free gas, a 12‐cm retro‐gastric fluid collection (Figure 1A), and a defect in the posterior gastric wall. The latter appeared to be very thickened (Figure 1B) and obviously tumoral.
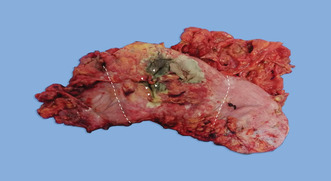
FIGURE 1.
Axial (A) and coronal (B) views of an abdominal CT‐scan (with contrast medium injection) showing free intraperitoneal gas (pink arrow heads), a stomach wall thickening related to a gastric tumor (yellow arrow heads) that is perforated (white arrow) causing a large (12 cm) fluid collection (white star) in the lesser omental sac.
The diagnosis of perforated gastric cancer complicated with peritonitis was made, and an urgent intervention was performed.
The patient underwent an emergent laparotomy. There was a large gastric tumor (15 cm) and a collection in the level of the lesser omental sac. The evacuation of this collection revealed a large perforation (6 cm) in the posterior wall of the stomach body within a widely necrotic gastric tumor (Figure 2).
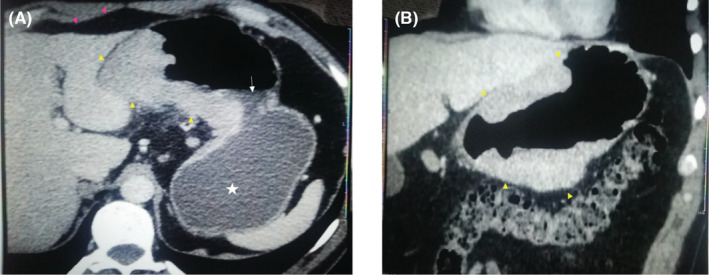
FIGURE 2.
Intraoperative views showing the perforation (white and black arrows) within a widely necrotic (yellow arrow heads) tumor in the posterior wall of the stomach.
A total gastrectomy with D2 lymphadenectomy without splenopancreatectomy was performed in addition to a Roux‐en‐Y eso‐jejunostomy. The resection was R0.
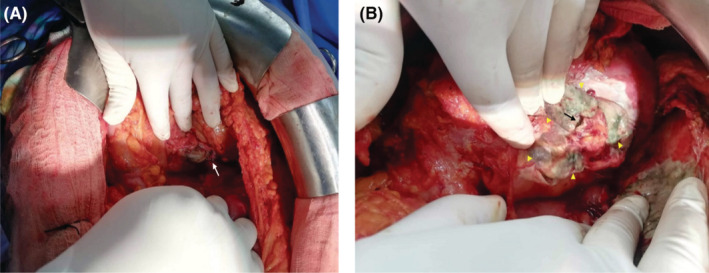
The specimen revealed an extensive gangrene in the gastric wall (Figure 3).
FIGURE 3.
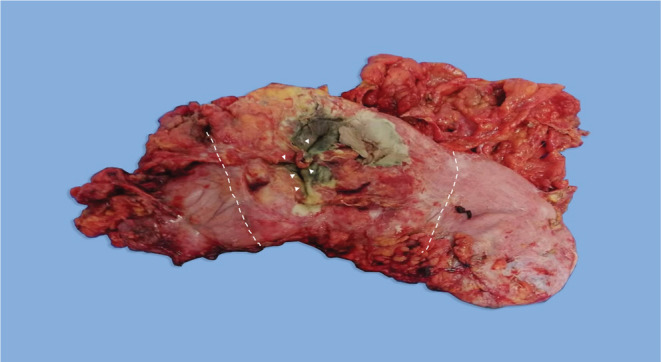
Surgical specimen (total gastrectomy) showing a large (15 cm) tumor (between the two dashed lines) in the body of the stomach. There is a perforation (white head arrows) within a large area of tumor necrosis (black tissues).
Pathological examination found DLBCL of the stomach and lymph nodes (Figure 4). It showed that the perforation was related to tumor necrosis.
FIGURE 4.
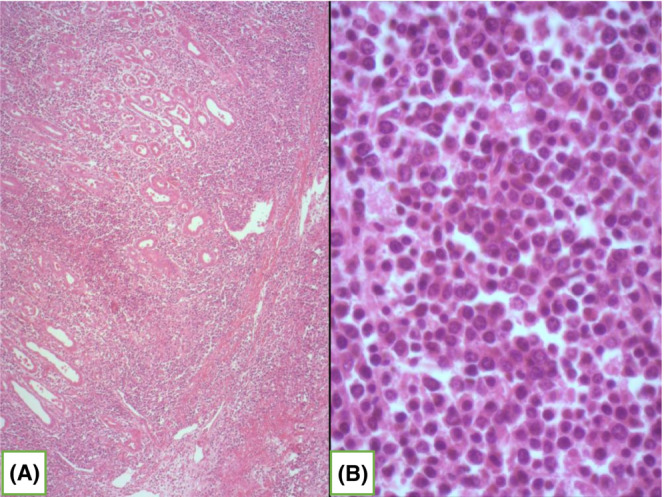
(A) Pathological examinations showing an infiltration of the gastric wall by diffuse blue proliferation HE×50; (B) Proliferation of large neoplastic lymphoid cells (usually 5 × normal lymphocytes) with amphophilic or basophilic cytoplasm, eccentric nuclei with one or more nucleoli (HE×400).
Immunohistochemical staining showed that the tumor to be positive to CD20, CD10, BCL‐6, and Ki67 (50%) but negative to BCL‐2 (Figure 5).
FIGURE 5.
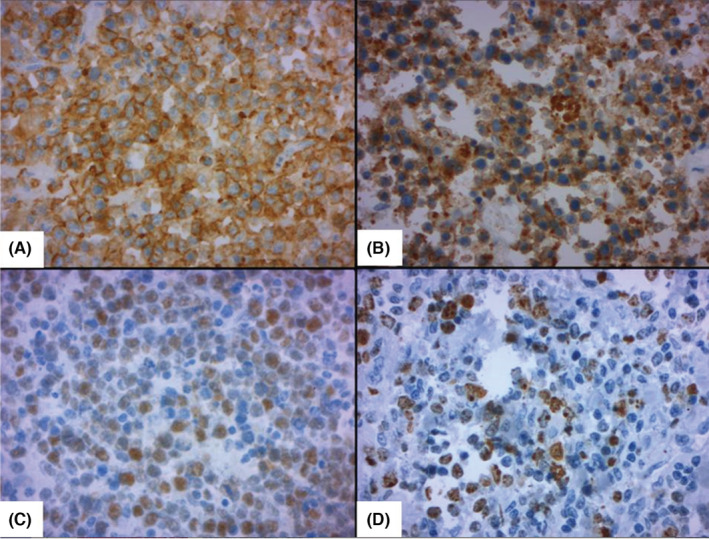
(A) Positive staining with CD20; (B) Positive staining with CD10; (C) Positive staining with Bcl6; (D) 50% of cells express Ki67.
On the fourth postoperative day, the patient presented high fever, dyspnea, and elevated white blood cells. The patient had a low flow fistula of the eso‐jejunostomy that was successfully treated with antibiotherapy and parenteral nutrition.
Then, he received a chemotherapy based on rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R‐CHOP).
3. DISCUSSION
Malignant lymphoma of the gastrointestinal tract is classified as extranodal and nodal. 1 It constitutes merely 1%–5% of this system's malignancies. 4 , 5 The stomach is the most commonly affected organ. 1 Extranodal lymphomas, which are more common, originate in the gastrointestinal tract. 6 In 40% of the cases, it presents as low‐grade mucosa‐associated lymphoid tissue (MALT), and in 60% as high‐grade DLBCL 7 , 8 , 9 (our present case). Primary gastric lymphoma is rare (1%–5% of all gastric tumors). 10 A study by Dawson et al. 4 described the following five major features as the criteria for primary malignant lymphoma of the intestinal tract: (1) no evidence of enlarged mediastinal lymph nodes in chest radiographs; (2) no palpable superficial lymphadenopathy; (3) prominent bowel lesions at laparotomy; (4) no tumors in the liver or spleen; and (5) normal total and differential white blood cell counts. The patient had a large ulcer in the stomach without infiltration of other organs. The present case fulfilled all the cited criteria, so it was considered to be a primary gastric lymphoma. It has a natural history of slow progression; most cases occur in male individuals of 50 years old or older, with primary gastric lymphoma being the most common in the sixth decade. 2
Primary gastric lymphoma is often asymptomatic or presents with non‐specific symptoms. The diagnosis is frequently delayed. Abdominal pain (50%) and dyspepsia (30%) are the most common presentations. 1 , 11
It is known that the perforation occasionally occurs in patients receiving chemotherapy (about 0.9%–1.1% of cases). 8 , 9 But spontaneous perforation of malignant gastric lymphoma without chemotherapy is rare. 1 , 8 The largest series of cases published in Japan between 1985 and 2013 showed 15 cases of spontaneous primary gastric lymphoma before chemotherapy that required gastrectomy in the greatest literature review in 2015. 1 , 6
Spontaneous perforation of a chemotherapy‐naïve gastrointestinal lymphoma occurs due to tumor necrosis reaching the subserosa, with or without a concurrent ulcer. Ceniceros‐Cabrales et al. 12 reported that there are two different causes of spontaneous perforation. First, the perforation may result from an ulcer that has a thin connective tissue in the absence of tumor. Second, spontaneous perforation may result from an ulcer and tumor necrosis that has reached the subserosa.
The management of the perforation of the gastric lymphoma is dual: the management of the perforation and the management of the lymphoma. The most important step is the intraoperative decision‐making.
The best treatment should be chosen according to tumor location, clinical stage, and pathologic pattern. Overall 5‐year survival reported for multimodal therapy is between 50 and 70%. 13
Four surgical options are possible:
Total gastrectomy is generally indicated in case of a large tumor. It can also be performed in the following situations: early acute peritonitis or large perforation within an extensive tumor necrosis, especially around the perforation. All these conditions were met in our patient who required a total gastrectomy. 13
Distal gastrectomy can be performed in case of a tumor in the distal or middle part of the stomach, which is usually left with a cardiac stump showing better results for the anastomosis compared to oesophagojejunostomy. 13
Atypical or wedge gastrectomy can be performed for small tumors.
A suture of the perforation (with or without excision of its edges) can be done in case of a small perforation without extensive tumor necrosis. It should also be performed as a “damage control surgery” when the patient is in shock or has an advanced peritonitis or with severe comorbidties. After that, the patient should undergo a chemotherapy (R‐CHOP) or radical surgery. 13 In addition, in case of a perforation of an associated gastric ulcer, the simple suture seems the most adequate option. On the other hand, suturing tumor tissue is not always guaranteed.
Spontaneous perforation without chemotherapy raises the problem of the histological type of the gastric tumor because the surgical strategy toward an adenocarcinoma is different from that of lymphoma which, in addition, usually has a better prognosis.
Distal and total gastrectomies performed in an emergency setting are generally associated with high rates of morbidity and mortality. So, they should be avoided whenever possible and a simple suture of the perforation may be attempted.
The surgeon should therefore choose the optimal surgical technique taking all the following factors into account: the general condition of the patient, the severity of the acute peritonitis, the characteristics of the gastric DLBCL (size, location, and extent of necrosis), and the perforation type (width, location, edges quality).
4. CONCLUSION
Malignant gastric lymphoma, accounting only for 1% of primary gastric carcinoma, is usually a DLBCL. Less than 1% of malignant gastric lymphomas perforate. While it is relatively well known that perforations often occur during chemotherapy, they are rare in patients not receiving chemotherapy and require a oncological surgical approach before medical chemotherapy.
AUTHORS' CONTRIBUTION
R. Daoud conceived the idea for the document and contributed to the writing and editing of the manuscript. H. Harbi contributed to the writing and editing of the manuscript. R. Kallel reviewed and edited the manuscript. T. S. Boudawara reviewed and edited the manuscript. A. Kchaou contributed to the literature review, manuscript writing, editing, and review of the manuscript. All authors read and approved the final manuscript.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
None declared.
ETHICAL APPROVAL
Personal data have been respected.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENTS
None declared.
Daoud R, Harbi H, Kallel R, Sallemi‐Boudawara T, Kchaou A, Boujelbene S. Spontaneous perforation of primary gastric diffuse large B‐cell lymphoma. Clin Case Rep. 2023;11:e6994. doi: 10.1002/ccr3.6994
DATA AVAILABILITY STATEMENT
Personal data of the patient were respected. No data is available for this submission.
REFERENCES
- 1. Ohkura Y, Lee S, Kaji D, et al. Spontaneous perforation of primary gastric malignant lymphoma: a case report and review of the literature. World J Surg Oncol. 2015;13:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chang Y‐T, Huang M‐Y, Shih H‐H, Wu C‐C, Lu T‐Y, Lin P‐C. Gastric MALT lymphoma presented with primary perforation in an adolescent: a case report. BMC Pediatr. 2019;19:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim JS, Rou WS, Ahn BM, et al. Gastric perforation caused by primary gastric diffuse large B cell lymphoma. Korean J Gastroenterol. 2015;65(1):43‐47. [DOI] [PubMed] [Google Scholar]
- 4. Dawson IMP, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961;49:80‐89. [DOI] [PubMed] [Google Scholar]
- 5. Ghai S, Pattison J, Ghai S, O'Malley ME, Khalili K, Stephens M. Primary gastrointestinal lymphoma: spectrum of imaging findings with pathologic correlation 1. Radiographics. 2007;27:1371‐1388. [DOI] [PubMed] [Google Scholar]
- 6. Yabuki K, Tamasaki Y, Satoh K, Maekawa T, Matsumoto M. Primary gastric lymphoma with spontaneous perforation: report of a case. Surg Today. 2000;30:1030‐1033. [DOI] [PubMed] [Google Scholar]
- 7. Sano R. Classification of Malignant Gastric Lymphoma. Igakushoin; 1987:257‐275. [Google Scholar]
- 8. Koch P, Probst A, Berdel WE, et al. Treatment results in localized primary gastric lymphoma: data of patients registered within the German multicenter study (GIT NHL 02/96). J Clin Oncol. 2005;23:7050‐7059. [DOI] [PubMed] [Google Scholar]
- 9. El Asmar A, Khattar F, Alam M, El Rassi Z. Spontaneous perforation of primary gastric B‐cell lymphoma of MALT: a case report and literature review. Clin Case Rep. 2016;4(11):1049‐1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ghai S, Pattison J, Ghai S, O'Malley ME, Khalili K, Stephens M. Primary gastrointestinal lymphoma: spectrum of imaging findings with pathologic correlation. Radiographics. 2007;27:1371‐1388. [DOI] [PubMed] [Google Scholar]
- 11. Brooks JJ, Enterline HT. Primary gastric lymphomas: a clinicopathologic study of 58 cases with long‐term follow‐up and literature review. Cancer. 1983;51:701‐711. [DOI] [PubMed] [Google Scholar]
- 12. Ceniceros‐Cabrales AP, Sánchez‐Fernández P. Linfoma difuso de células grandes B gástrico perforado: reporte de un caso y revisión de la literatura. Rev Gastroenterol Mex. 2019;84:412‐414. [DOI] [PubMed] [Google Scholar]
- 13. Chen G, Zhang MM, Zhu JM, et al. Damage control surgery saves patient with gastric lymphoma from radical gastrectomy. J Coll Physicians Surg Pak. 2021;31(8):978‐998. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Personal data of the patient were respected. No data is available for this submission.


