Abstract
Spontaneous external iliac artery dissection in highly trained athletes is becoming more recognized, but the reason as to why they are occurring remains a mystery. We present a patient with acute limb ischemia secondary to arterial dissection after strenuous exercise. Imaging showed complete occlusion of the distal common iliac artery, and the patient underwent successful revascularization of the right lower extremity using a hybrid approach.
Keywords: External iliac artery, Common femoral artery, Dissection, Interposition graft
Isolated external iliac artery (EIA) dissection without involvement of the aorta is quite rare.1 Most dissections occur in the renal and mesenteric arteries.2 Causes of dissection can range from blunt trauma, arterial catheterization, connective tissue disorders, atherosclerosis, and physical strain.3 Much of the isolated dissections in the literature involve patients with connective tissue disorders; very few of these deal with intense exercise. The most serious complications are rupture and acute limb ischemia (ALI). Treatments include conservative management, endovascular treatment, and open surgery.
We report a case of ALI secondary to EIA dissection that combines this rare phenomenon with use of exogenous testosterone. This patient agreed to publication of all case details and images.
Case report
A 54-year-old man with a past medical history of portal vein thrombosis (PVT) along with the use of exogenous testosterone presented to the emergency room with acute right lower extremity pain and increasing numbness after lifting weights in his home. There was no palpable femoral pulse, no Doppler flow for either the dorsalis pedis (DP) or posterior tibial (PT) was present on examination. Computed tomography angiography (CTA) three-dimensional reconstruction and coronal view of the CTA revealed a complete occlusion of the right distal common iliac artery (CIA) (Figs 1 and 2).
Fig 1.
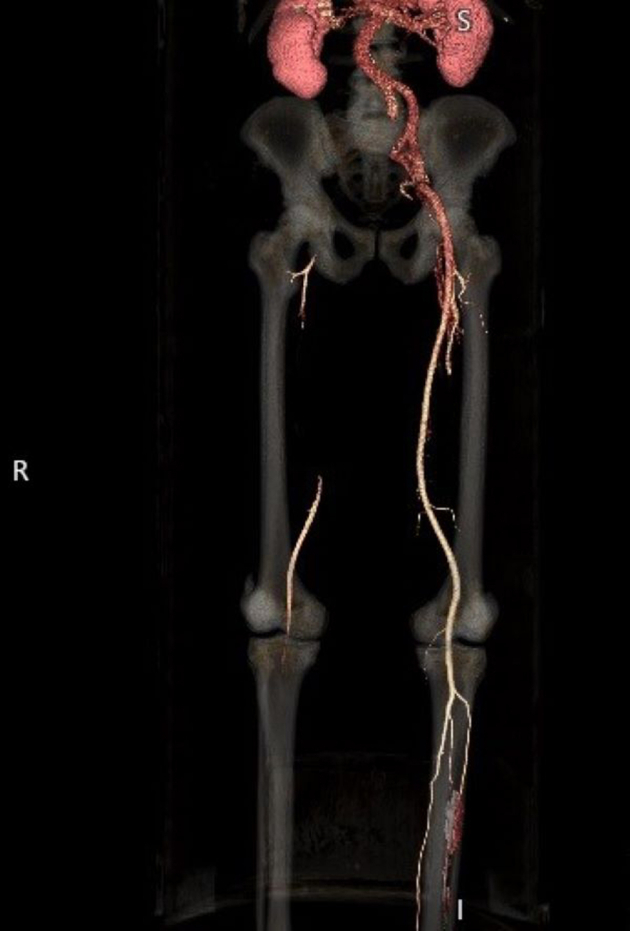
Three-dimensional reconstruction of computed tomography angiography (CTA) images showing occlusion of the right common iliac artery (CIA).
Fig 2.

Coronal view of computed tomography angiography (CTA) showing lack of contrast opacification in the mid right common iliac artery (CIA).
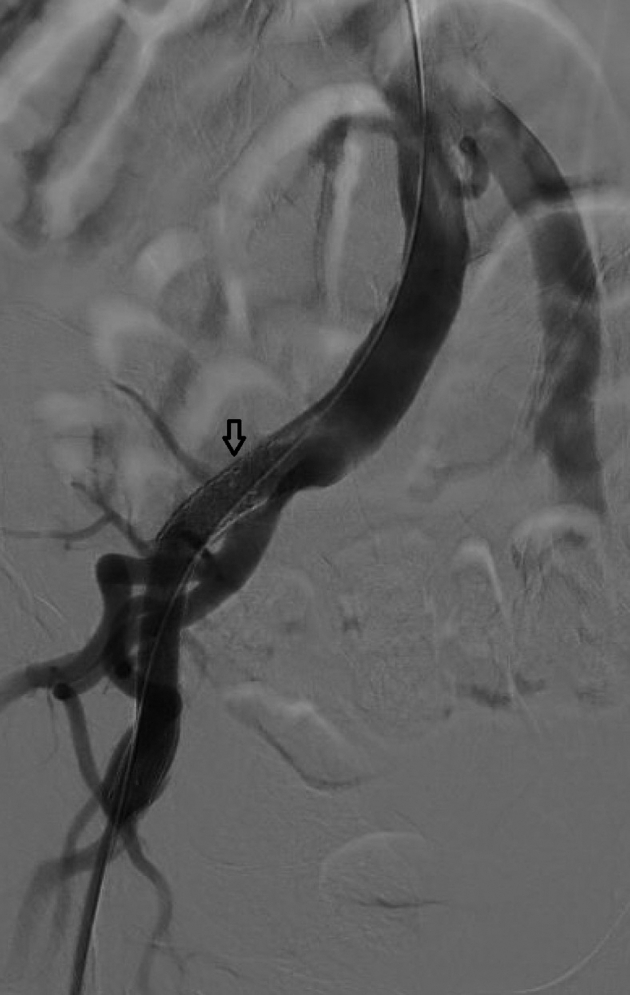
The decision was made to take the patient to the operating room for exploration of the right groin. A hockey stick incision was made. The tissue planes were noted to be blood tinged in appearance, similar to that of traumatic injury. Control was obtained with vessel loops and an arteriotomy was made into the common femoral artery (CFA), demonstrating both a true and false lumen with extensive thrombus (Fig 3). The dissection flap extended just proximal to the femoral bifurcation. There was no backbleeding from the superficial femoral artery. Wire access was obtained in the true lumen and an arteriogram was performed showing complete arterial occlusion extending up to the proximal aspect of the EIA within 2 cm of its origin as evidenced by normal flow into the right internal iliac artery (IIA) (Fig 4). This finding was in contrast with the finding of occlusion of the distal right CIA on the initial CTA. We hypothesized this was due to possible spiral dissection into the right IIA, which preserved some flow into the IIA. The timing of the contrast on the CTA likely was the reason for lack of flow seen in the IIA on the CTA images. An 8 mm × 10 cm long covered Viabahn stent (W.L. Gore & Associates, Newark, DE) was placed in the EIA just distal to the hypogastric artery. There was a lack of filling of the EIA, so a 10 × 29 mm balloon expandable Omnilink stent (Abbott, Chicago, IL) was placed cephalad to the covered stent with adequate overlap to tack the dissection flap. A subsequent arteriogram was performed showing excellent flow through the EIA stents (Fig 5).
Fig 3.

Femoral exposure with arteriotomy showing both the true and false lumen. Debakey forceps are holding the adventitia.
Fig 4.

Initial arteriogram showing lack of flow through the right external iliac artery (EIA).
Fig 5.
Completion arteriogram confirming flow through the right external iliac artery (EIA) stents. The arrow indicates the proximal extent of the Viabahn stent.
A #4 Fogarty balloon was then passed distally into the superficial femoral artery and popliteal artery, but no thromboembolic material was retrieved. Given that the dissection segment was quite long in the CFA and the adventitia of the artery was friable, we made the decision to replace the native CFA. The dissected CFA was then excised, and an 8-mm polytetrafluoroethylene interposition graft was used for reconstruction of the CFA. The proximal graft anastomosis was just distal to the stent at the junction of the EIA and CFA. The distal anastomosis was created in a bevel fashion to the femoral bifurcation. Even after reconstruction, there was still no palpable pulse or Doppler flow found in the right DP or PT; therefore, a medial incision just below the knee joint was made to expose and control the distal popliteal artery.
A #3 Fogarty was then passed distally into the infrapopliteal arteries which retrieved a 10- to 15-cm-long segment of embolic material composed of subacute thrombus; brisk back-bleeding was achieved. A four-compartment prophylactic fasciotomy was then completed with placement of negative pressure wound therapy. The patient did have marked muscular bulging at the end of the operation. The patient was found to have triphasic PT and a monophasic DP Doppler signal at the conclusion of the case. In the immediate postoperative setting, the patient had partial foot drop.
Further discussion with the patient postoperatively regarding the operative findings elicited no recent trauma, but he did endorse performing strenuous leg extensions leading to sudden pain that he stated resembled “pulling a muscle.” Concurrently, the patient had also recently been injecting testosterone to supplement his weight-lifting results. With his history of PVT, various blood tests were completed that revealed no genetic component to his presumed hypercoagulable state. Of note, the patient had not been taking any anticoagulation after the diagnosis of PVT years prior. He was prescribed apixaban 5 mg twice daily on discharge from the hospital. After discharge from the hospital, the patient has recovered well with his most recent ankle-brachial index measuring at 1.0 bilaterally and his foot drop had completely resolved in the ensuing 6 weeks. Plastic surgery performed skin grafting of his fasciotomy wounds. His postoperative surveillance regimen includes ankle-brachial index and iliac duplex imaging every 6 months for the first year and then yearly thereafter. Given the patient's body habitus, we may also consider CTA imaging.
Discussion
Two major questions remain after reviewing this patient's presentation: what factors specific to this patient could have led to an acute EIA dissection, and did exogenous testosterone play a role? It has been implied that increased flow as well as flow hemodynamics in bifurcating vessels lead to intimal injury and atherosclerosis.4 There is relatively high wall shear stress and multidirectional flow that contribute to intimal thickening and the development of atherosclerosis. Cardiac output increases dramatically during exercise. During this hyperdynamic state, there is increased turbulent blood flow, especially at the bifurcation of arteries, leading to increased shear stress on the arterial walls.1 It is this cycle of increased flow dynamics at these susceptible anatomic regions in conjunction with repetitive shear stress that causes intimal tears and subsequent dissection formation. Both of these factors are displayed in this patient as seen in the EIA as well as the high cardiac output seen during high-intensity exercise.5
Repetitive trauma to the artery from hypertrophy of the surrounding muscles, such as the psoas major, has been associated with the formation of endofibrosis, most significantly at the L5 cross-section, which further confirms the possibility of localized trauma to the artery on a regular basis.6 The etiology remains uncertain, but it is believed that chronic friction from hyperflexion of the hip joint may alter iliac artery anatomy. There is increased mechanical stress that results in traction and promotion of endofibrosis. This factor further leads to widespread calcification and intimal injury.6
An increased risk of venous thromboembolism has been linked to the use of exogenous testosterone. A common side effect of testosterone therapy is erythrocytosis, which leads to an increased risk of thrombosis. In the literature, thrombosis in the venous system is much more prevalent in those who use exogenous testosterone; in contrast, arterial thrombosis is quite rare and most often involves the renal or coronary arteries.7 Some studies do show the long-term effect of anabolic steroids and elevation in lipoproteins. This factor causes increased atherosclerotic burden and makes arterial walls more prone to dissection.8 In this case, it seems unlikely that testosterone use was the principal cause of arterial dissection. Although testosterone may increase the risk of thrombosis, there is no evidence to suggest an increased risk of intimal damage or arterial dissection.
Options for treating EIA dissection are quite varied and include a conservative approach, open surgery, and endovascular management. Open surgery is an excellent option for patients who present with ALI and strictly femoral disease. It is also a valid option in those who desire continued, competitive participation in athletic events.1 Repair options include aorto-/iliofemoral bypass with polytetrafluoroethylene or a Dacron interposition graft, resection with primary anastomosis, and femorofemoral bypass; all have varying results.2 An endovascular technique offers a minimally invasive method with reduction of wound complications. Both balloon angioplasty and stenting have been described; yet, stenting in addition to angioplasty is preferred to help adhere the intima to the media and eliminate flow within the dissection.5 In general, the endovascular technique is favored in disease involving only the iliac arteries. A hybrid approach, as seen in this case, is an excellent option for those presenting with ALI and have both iliac and femoral disease. In this instance, an iliofemoral bypass would have been a good option as well. Given that his body mass index was 34, we felt that a retroperitoneal exposure of the CIA in this patient would be challenging and that a covered stent would be an adequate treatment. Conservative management may be a viable option in patients who do not exhibit significant flow-limiting ischemia. Even in those instances, frequent follow-up is necessary and patients will be unlikely to resume their previous level of activity.
Conclusions
This case exemplifies a rare example of a physically active patient presenting with arterial dissection without a definitive cause. Although this patient was intermittently abusing exogenous testosterone, his presentation suggests the possibility of psoas muscle hypertrophy along with local hemodynamic factors and long-term repetitive vascular trauma resulting in arterial dissection.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Yamanaka Y., Yoshida T., Nagaoka E. Bilateral external iliac artery dissection in a middle-aged male athlete. Ann Vasc Dis. 2017;10:446–448. doi: 10.3400/avd.cr.17-00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hirai S., Hamanaka Y., Mitsui N., Isaka M., Kobayashi T. Spontaneous and isolated dissection of the external iliac artery: a case report. Ann Thorac Cardiovasc Surg. 2002;8:180–182. [PubMed] [Google Scholar]
- 3.Kondo S., Osanai H., Sakamoto Y., Uno H., Tagahara K., Hosono H., et al. Isolated bilateral external iliac artery dissections with emotional stress. Clin Case Rep. 2021;9:1312–1314. doi: 10.1002/ccr3.3762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zarins C.K., Giddens D.P., Bharadvaj B.K., Sottiurai V.S., Mabon R.F., Glagov S. Carotid bifurcation atherosclerosis. Quantitative correlation of plaque localization with flow velocity profiles and wall shear stress. Circ Res. 1983;53:502–514. doi: 10.1161/01.res.53.4.502. [DOI] [PubMed] [Google Scholar]
- 5.Cook P.S., Erdoes L.S., Selzer P.M., Rivera F.J., Palmaz J.C. Dissection of the external iliac artery in highly trained athletes. J Vasc Surg. 1995;22:173–177. doi: 10.1016/s0741-5214(95)70113-3. [DOI] [PubMed] [Google Scholar]
- 6.Fisher A.T., Tran K., Dossabhoy S.S., Sorondo S., Fereydooni A., Lee J.T. Anatomic factors contributing to external iliac artery endofibrosis in high-performance athletes. Ann Vasc Surg. 2022;79:399–400. doi: 10.1016/j.avsg.2022.05.011. [DOI] [PubMed] [Google Scholar]
- 7.Thompson K., Osorio L.G., Mughni S., Jordan J., Oyesanmi O. An interesting presentation of testosterone-induced arterial thrombosis. Cureus. 2021;13:e14972. doi: 10.7759/cureus.14972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heydari A., Asadmobini A., Sabzi F. Anabolic steroid use and aortic dissection in athletes: a case series. Oman Med J. 2020;35:e179. doi: 10.5001/omj.2020.120. [DOI] [PMC free article] [PubMed] [Google Scholar]


