Abstract
The COVID-19 pandemic has influenced people’s lives in diverse ways. The authors utilized latent class analysis, a person-centered approach, to examine distinct patterns of COVID-related stressors and their associations with alcohol-related, mental health, and quality of life outcomes. Participants were 463 adults who completed the baseline assessment of the NIAAA COVID-19 Pandemic Impact on Alcohol Study from June 2020 to January 2022. Using cross-sectional data, three analytic methods (continuous sum score, categorical grouping, and latent class analysis) were applied to model 17 COVID-related stressors. Regression analyses indicated higher COVID-related stress and endorsement of 4 or more COVID-related stressors were generally associated with worse health-related outcomes. Latent class analysis revealed four classes: Class 1: Minimal COVID-Related Impact (51.6%); Class 2: Work Interruptions (24.8%); Class 3: Family/Friends Affected by COVID (14.5%); and Class 4: Serious Financial Stress (9.1%). Racial/ethnic minorities were more likely to be in Class 3, whereas individuals with more years of education and higher income were less likely to be in Class 4. Individuals with a history of alcohol use disorder were more likely to be in Classes 2 and 4. Compared with Class 1, Class 4 reported highest levels of perceived stress, problematic alcohol use, anxiety symptoms, depressive symptoms, alcohol craving, loneliness, drinking to cope, and lowest levels of physical, psychological, social, and environment quality of life. COVID-related stressors disproportionately affected minority and vulnerable groups. Individuals who experienced multiple financial stressors had the greatest risk for negative health-related outcomes and may benefit from holistic interventions and community outreach.
Keywords: alcohol misuse, mental health, quality of life, stress and coping, health disparities
The COVID-19 pandemic has impacted people’s lives in diverse ways. During the early phase of the pandemic, 10.1% of the US population were being laid-off or furloughed and 35.2% of workers switched from commuting to remote work (Brynjolfsson et al., 2020). Essential workers who had to work in proximity to other coworkers were at elevated risk for exposure to coronavirus (Béland et al., 2020). Among parents, disruption to daily routines and the lack of childcare might pose increased stress to the family (Brown et al., 2020; Kusin & Choo, 2021). According to the Survey of Household Economics and Decision-making in April 2020, one-fourth of the respondents reported a reduction in income and over 13% reported inability to pay monthly bills and struggled financially to make ends meet (Dhongde, 2020). The wide-ranging negative impact of the pandemic on people’s employment, income, childcare, and related financial problems can be conceptualized as COVID-related stressors which may contribute to mental health problems during the pandemic (Ettman et al., 2020b).
Consistent with the biopsychosocial model (Engel, 1977), understanding how pre-existing racial/ethnic and socioeconomic disparities may contribute to COVID-related stressors would inform approaches to mitigate the psychosocial burden and health inequity experienced by disadvantaged populations (Halkitis, 2020). Indeed, disparities in social determinants of health have been exacerbated during the COVID-19 pandemic (Dubowitz et al., 2021; Fang et al., 2021; Green et al., 2021). Job losses were disproportionately high among racial/ethnic minorities, workers without college degrees, and essential workers from low-income household (Angelucci et al., 2020; Gemelas et al., 2021). Racial/ethnic minority disparities in COVID-related infections, hospitalization, and death are well-documented (Asch et al., 2021; Kathe & Wani, 2021; Kimani et al., 2021). Individuals with Alcohol Use Disorder (AUD) represent a vulnerable group at risk for COVID-related complications (Bailey et al., 2021; Clay & Parker, 2020; Murthy & Narasimha, 2021). Social isolation and disruption to in-person support group may further increase anxiety, depression and risk of relapse among individuals with AUD (Sarangi & Eskander, 2021; Yazdi et al., 2020). Moreover, financial stress during the COVID-19 pandemic may be particularly associated with more mental health problems (Bareket-Bojmel et al., 2020; Jiang et al., 2021). Taken together, individuals who belong to a racial/ethnic minority group may be at greater risk for exposure to COVID-specific stressors, and those with less education, lower income, or a history of AUD may have fewer coping resources to manage one or more types of stress that were attributable to the COVID-19 pandemic.
Although the above studies shed light on health disparities in a specific area affected by COVID-19, none captured the diverse ways in which COVID-19 impacted minority and vulnerable groups in an integrated analysis. A limitation of prior studies concerned the aggregation of different types of COVID-related stressors together as either a continuous variable (Alon-Tirosh et al., 2021) or a categorical variable (Ettman et al., 2020b). The use of latent class analysis (LCA) can overcome this limitation and effectively capture heterogeneity in the exposure to COVID-related stressors. Notably, this approach can identify hidden groups of individuals who share a similar set of COVID-related stressors. The identification of these latent classes can lead to a better understanding of what proportion of the sample was affected by specific types of COVID-related stress, who might be at risk, and which type of COVID-related stress might be most consistently associated with adverse health-related outcomes.
The goal of the present study was to examine the associations between COVID-related stressors and a wide range of mental health, alcohol-related, and quality of life outcomes. To facilitate comparisons of findings across studies, we first tested these associations using two common variable-centered approaches (continuous sum score and categorical grouping). The LCA approach was then utilized as a novel analytic method and was compared to the two variable-centered approaches. We hypothesized that higher COVID-related stress would be associated with worse mental health, alcohol-related, and quality of life outcomes. To understand health disparities, the associations of demographic characteristics, history of AUD, and enrollment phase with latent class membership were also examined. We hypothesized that individuals from minority and disadvantaged groups would more likely be members of the latent classes characterized by higher probabilities of COVID-related stress exposure.
Method
Participants
From June 3, 2020 to January 6, 2022, 491 adults were enrolled in the NIAAA COVID-19 Pandemic Impact on Alcohol Study (C19-PIA Study), an ongoing longitudinal study that follows participants over a 2-year period. Following verbal informed consent obtained by phone, participants began the baseline assessment. To reduce participants’ burden, the baseline assessment was divided into two parts. The first part (Baseline 1) focused on COVID-related experiences and outcomes of primary interest and was administered by phone. The second part (Baseline 2) focused on variables of secondary interest, including mental health and alcohol-related risk factors (e.g., loneliness and drinking to cope) and quality of life domains, and was administered as an online survey for most participants. Of the 378 participants who responded to the Baseline 2 survey, 21 participants (5.6%) requested to complete the survey by phone. Such an accommodation was provided to ensure that participants who were less familiar with the use of the internet (including older participants and those with less education or lower income) could have an equal opportunity to access and complete the survey. Participants who completed Baseline 1 only were compensated with $25, and those who completed both Baseline 1 and Baseline 2 were compensated with $50. The number of days lapsed in between Baseline 1 and Baseline 2 ranged from 0 to 113 days, with an average of 15.3 days and a mode of 9 days.
The analytic sample (N = 463) was restricted to participants who had complete data on history of AUD and all primary outcomes. Of these participants, 49.5% (n = 229) were tested for COVID-19 and 2.4% (n = 11) reported testing positive for COVID-19. In terms of geographical location, 84.7% of participants in the C19-PIA Study resided in Maryland (55.5%), Virginia (12.3%), and Washington D. C. (16.9%). A detailed breakdown of the other states can be found in Supplemental Table 1. All participants were previously screened under the NIAAA natural history protocol (Kwako et al., 2019), where demographic characteristics and history of AUD were obtained. The parent study included individuals who were 18 years of age or older and both participants with AUD and participants without AUD. To maximize generalizability, exclusion criteria were minimal and only excluded those who were pregnant or under legal confinement. The C19-PIA Study protocol was approved by the NIH Intramural Institutional Review Board and is registered in clinicaltrials.gov (NCT04391816). Data and study materials are not publicly available and can be provided upon request in a deidentified form.
Measures
COVID-Related Stressors.
The COVID-19 Community Survey Question Bank was developed by the US Centers for Disease Control and Prevention (CDC) as a resource to facilitate use of common measures across research studies (Centers for Disease Control and Prevention, 2020). Two questions from this resource assessed changes in work, childcare, and financial situations that were attributable to the COVID-19 pandemic (13 items). We further enriched this set of items by adding 1 item on being an essential worker and 3 items on having a family member or close friend/partner being infected with, hospitalized for, or died of COVID-19, yielding a total of 17 COVID-related impact items. As part of Baseline 1, participants were asked “How has the COVID-19 outbreak affected you?” The wording, frequency, and percent of endorsement of these 17 items are presented in Table 1. Distinguished from other items, more remote work than usual can be considered a positive measure or “privilege” that increases flexibility and reduces exposure to diseases (Angelucci et al., 2020; Béland et al., 2020; Yancy, 2020). Thus, item 1 was reversed coded for the computation of the continuous sum score and categorical grouping of COVID-related stress. In the LCA, the item probability of more remote work can be directly estimated such that reverse coding was not necessary and item 1 was preserved in its original form for ease of interpretation.
Table 1.
Endorsement of COVID-Related Stressors (N = 463)
| COVID-Related Impact Items | Frequency | Percent |
|---|---|---|
|
| ||
| 1. Worked remotely or from home more than you usually do | 217 | 46.9% |
| 2. Worked more hours than usual | 130 | 28.1% |
| 3. Worked reduced hours | 135 | 29.2% |
| 4. Was not able to work | 95 | 20.5% |
| 5. Worked outside the home as an essential worker | 138 | 29.8% |
| 6. Had difficulty arranging for childcare | 20 | 4.3% |
| 7. Incurred increased costs for childcare expenses | 18 | 3.9% |
| 8. Income or pay has been reduced | 124 | 26.8% |
| 9. Not paid at all | 70 | 15.1% |
| 10. Did not have enough money to pay rent | 57 | 12.3% |
| 11. Did not have enough money to pay for food | 42 | 9.1% |
| 12. Did not have enough money to pay for gas | 38 | 8.2% |
| 13. Had serious financial problems | 78 | 16.8% |
| 14. Did not have a regular place to sleep or stay | 13 | 2.8% |
| 15. Had a family member or close friend/partner that contracted COVID-19 infection | 152 | 32.8% |
| 16. Had a family member or close friend/partner that was hospitalized due to COVID-19 infection | 79 | 17.1% |
| 17. Had the death of a family member or close friend/partner due to COVID-19 infection | 46 | 9.9% |
Note. Item 1 was reverse coded for the computation of COVID-related stress continuous sum score and categorical grouping of COVID-related stress. The original item 1 without reverse coding was utilized as an indicator in the LCA.
Primary Outcomes.
Five primary outcomes were assessed as part of Baseline 1. Perceived stress was measured using the Perceived Stress Scale (Cohen et al., 1983), with a Cronbach’s alpha of 0.92 (all Cronbach’s alphas presented were obtained in the current sample from the C19-PIA Study). Problematic alcohol use was assessed using the 10-item Alcohol Use Disorders Identification Test (Saunders et al., 1993), with a Cronbach’s α of 0.94. Anxiety symptoms were measured using the Generalized Anxiety Disorder-7 (Spitzer et al., 2006), with a Cronbach’s alpha of 0.92. Depressive symptoms were measured using the Patient Health Questionnaire-9 (Kroenke et al., 2001), with a Cronbach’s alpha of 0.89. Among drinkers only, alcohol craving was assessed using the 5-item Penn Alcohol Craving Scale (Flannery et al., 1999), with a Cronbach’s alpha of 0.95.
Secondary Outcomes.
Six secondary outcomes (three broad constructs) were assessed as part of Baseline 2. Social isolation was measured using the UCLA Loneliness Scale (Russell et al., 1978), with a Cronbach’s alpha of 0.97. Among drinkers only, drinking to cope was assessed using the coping subscale of the Drinking Motives Questionnaire-Revised (Cooper, 1994), with a Cronbach’s alpha of 0.92. Quality of life was measured using the World Health Organization Quality Of Life BREF, which has four domains mapping on physical health, psychological health, social relationships, and environment quality of life (WHOQOL Group, 1998). The Cronbach’s alphas for these four domains were 0.82, 0.88, 0.78, and 0.84, respectively.
Demographic Characteristics and History of AUD.
Participants’ age was assessed at Baseline 1 of the C19-PIA Study. Information on gender, race, ethnicity, years of education, annual household income, and AUD were drawn from the NIAAA natural history protocol database. History of AUD was assessed using the Structural Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV or DSM-5 (First, 2015).
Enrollment Phase.
The recruitment of participants into the C19-PIA Study occurred in between June 3, 2020 to January 6, 2022. The time of enrollment covered different stages of the pandemic and could be a confounding factor in the associations of COVID-related stressors with alcohol-related, mental health, and quality of life outcomes. To control for the potential confounding effect, we coded enrollment timing into four phases based on frequency distributions while referencing COVID-infection level and related state government policies in the Washington D.C. Metro area: 22.7% Phase 1 (June 3 to July 31, 2020); 30.2% Phase 2 (August 1 to November 22, 2020); 27.4% Phase 3 (November 23, 2020 to February 28, 2021); and 19.7% Phase 4 (March 1, 2021 to January 6, 2022).
Statistical Analyses
Three analytic approaches were utilized and compared in this study. In the first approach, the sum of COVID-related stressors was computed and treated as a continuous variable. In the second approach, categorical grouping of COVID-related stressors was computed and treated as a three-level categorical variable with low, medium, and high stress levels (Ettman et al., 2020b). The cutoffs for this categorical grouping variable were based on the distribution of COVID-related stressors endorsement in the current sample. In the third approach, latent classes of COVID-related stressors were obtained using LCA and was treated as an empirically derived categorical variable.
We presented the data analyses in the following sequence. First, LCA was conducted by comparing a series of 5 latent class models using all 17 COVID-related impact items. The optimal number of latent classes was determined based on information criteria, likelihood-based tests, and interpretability of latent classes (Nylund et al., 2007). Prior to comparing the three analytic approaches, the proportions of latent class membership by demographic characteristics, history of AUD, and enrollment phase were examined with statistical tests drawn from multinomial logistic regressions. Latent class differences in health-related outcomes were then evaluated using univariate linear regression models and compared with the two alternative analytic methods (continuous sum score and categorical grouping). In the final step, the robustness of latent class differences in health-related outcomes was tested using multivariate regression models controlling for age, gender, race, ethnicity, years of education, household income, history of AUD, and enrollment phase as covariates. LCA was conducted in Mplus 8.4 and all other analyses were conducted in Stata 16.1.
As for missing data, 71.3% of the analytic sample had complete data on all study variables and all participants had complete data on all primary outcomes. Missing data patterns in years of education, household income, and secondary outcomes are detailed in Supplemental Table 2. Participants with missing data on any secondary outcomes did not differ from participants without missing data in terms of age, gender, race, ethnicity, and latent class membership. Missing data in all regression analyses were handled using multiple imputation with chained equations (Royston & White, 2011). Sensitivity analyses showed that all significant main findings were replicated in complete case analyses without multiple imputation.
Results
The study sample had a mean age of 44.8 years (SD = 14.2; Range from 21.2 to 96.4 years) and was 48.6% female and 51.4% male. Racial composition was 50.5% White, 33.9% Black/African American, and 15.6% Other. Ethnic composition was 89.0% Not Hispanic, 7.8% Hispanic, and 3.2% Not Reported/Unknown. Years of education (valid percent) were 22.8% <13 years (n = 102), 54.5% 13–16 years (n = 244), and 22.8% ≥17 years (n = 102). As for annual household income (valid percent), 25.3% reported earning less than $20,000 (n = 114), 43.2% reported earning $20,000–74,999 (n = 195), and 31.5% reported earning $75,000 or more (n = 142). A history of AUD was found in 41.9% of the sample (n = 194).
Three Analytic Methods
As shown in Table 1, endorsement of COVID-related impact items ranged from 2.8% for “did not have a regular place to sleep or stay” to 46.9% for “worked remotely or from home more than you usually do.” Work-related interruptions such as increased or reduced work hours and not being able to work were frequently endorsed (20.5%–29.8% for items 2–5), whereas 16.9% of participants reported that they “had serious financial problems” (item 13). About one-third (32.8%) of participants reported that they “had a family member or close friend/partner that contracted COVID-19 infection” (item 15).
Figure 1 shows a comparison of the three analytic methods that were applied to model COVID-related stressors. In Figure 1A, the continuous sum score ranged from 0 to 12 and had a mean of 3.2 COVID-related stressors with positive skewness. In Figure 1B, the three-group categorization classified 30.7% of participants as low COVID-related stress (endorsed 0–1 items), 32.2% as medium COVID-related stress (endorsed 2–3 items), and 37.2% as high COVID-related stress (endorsed 4+ items). Figure 1C illustrates the optimal four-class solution identified in the LCA, which was supported by the lowest Bayesian information criterion and significant likelihood ratio tests for up to four classes (see Supplemental Table 3, for model fit statistics). The item probabilities of all 17 COVID-related impact items are presented for the four latent classes.
Figure 1.
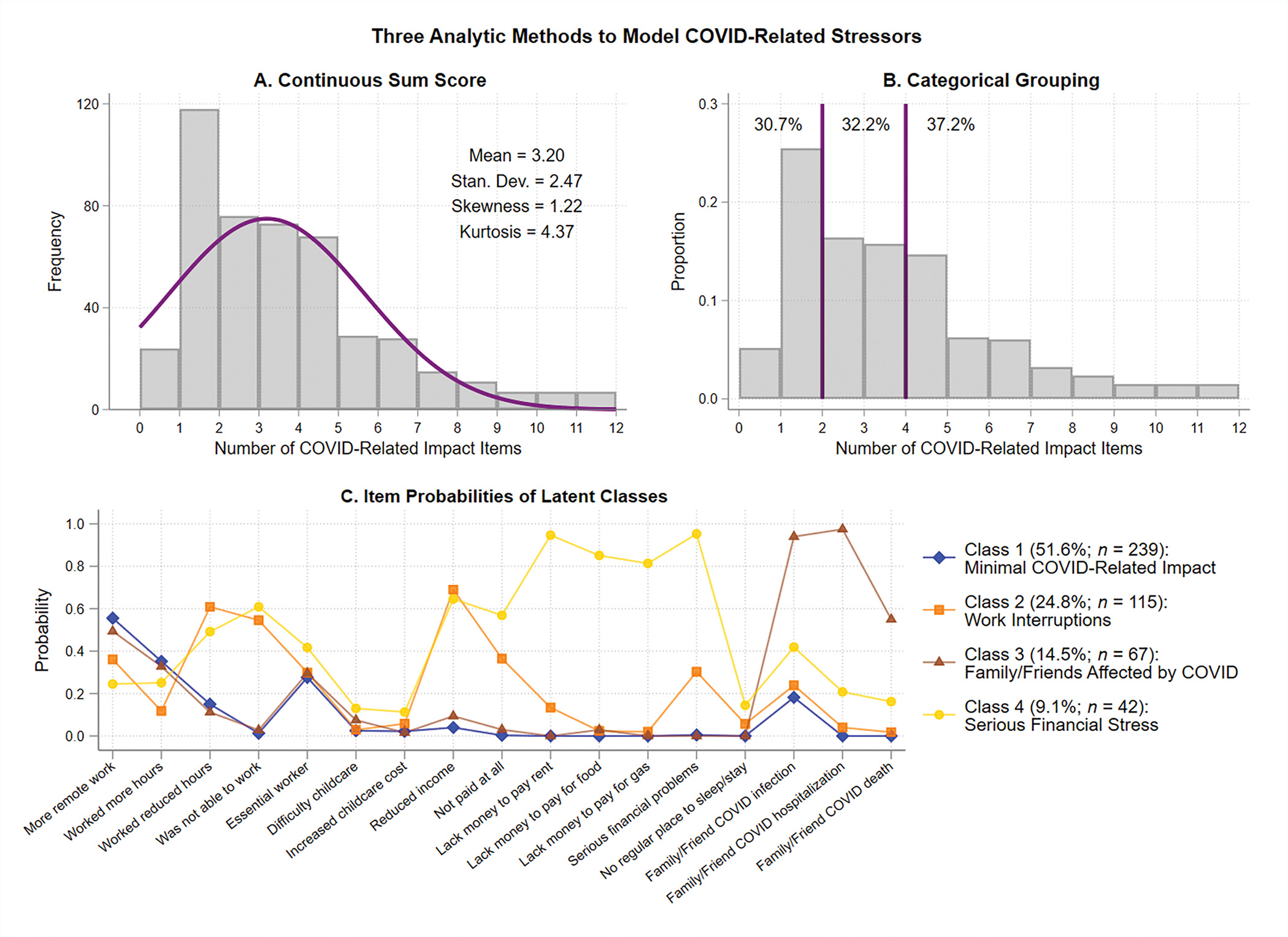
Continuous Sum Score, Categorical Grouping, and Latent Class Analysis of COVID-Related Stressors
Note. Panel A shows the frequency distribution of COVID-related stressors and the mean, standard deviation, skewness, and kurtosis of the computed continuous sum score. Panel B shows a three-level categorical grouping of COVID-related stressors into low (30.7%), medium (32.2%), and high (37.2%) levels. Panel C shows the optimal four-class solution empirically derived from latent class analysis. See the online article for the color version of this figure.
The four latent classes empirically derived from the LCA were well-differentiated and highly interpretable. Class 1 had low probabilities of stressors related to work or finances and low probabilities of family/friends affected by COVID and was labeled as “Minimal COVID-Related Impact” (51.6%). Of note, Class 1 also reported moderate probabilities of having more remote work and working more hours. Class 2 had moderate probabilities of working reduced hours, unable to work, or experiencing reduced pay; however, the probabilities of having serious financial problems and lacking money to pay for rent, food, or gas remained low. This class was labelled as “Work Interruptions” (24.8%). Class 3 had high probabilities of having a family/friend who contracted COVID-19 and hospitalized, and moderate probability that a family/friend died of COVID-19, but otherwise had item probabilities that were very similar to those in Class 1. This class was labelled as “Family/Friends Affected by COVID” (14.5%). Class 4 had high probabilities of work interruptions; in addition, they also reported serious financial problems including reduced pay or not paid at all, and lacking money to pay for rent, food, and gas. This class was labelled as “Serious Financial Stress” (9.1%).
Health Disparities in Latent Class Membership
Figure 2 shows the latent class proportions by demographic characteristics, history of AUD, and enrollment phase. Compared with individuals 18–34 years old, individuals 35–54 years old (32.1% vs. 16.5%; p = 0.002) and 55+ years old (25.9% vs. 16.5%; p = 0.028) were more likely to be in Class 2 (Work Interruptions). Compared with Whites, Black/African Americans were more likely to be in Class 3 (Family/Friends Affected by COVID; 21.0% vs. 9.8%; p = 0.003) and Class 4 (Serious Financial Stress; 14.0% vs. 7.3%; p = 0.022). Compared with individuals who were not Hispanic/Latino, Hispanics/Latinos were more likely to be in Class 3 (Family/Friends Affected by COVID; 30.6% vs. 13.1%; p = 0.024). Compared with individuals with <13 years of education, individuals with 13–16 years of education were less likely to be in Classes 2 (Work Interruptions; 23.4% vs. 30.4%; p = 0.026) and 3 (Family/Friends Affected by COVID; 12.7% vs. 18.6%; p = 0.028); moreover, individuals with 17+ years of education were less likely to be in Classes 2 (Work Interruptions; 20.6% vs. 30.4%; p = 0.008) and 4 (Serious Financial Stress; 2.9% vs. 13.7%; p = 0.002). Compared with individuals who made <$20,000 in their household, those who earned $20,000-$74,999 (23.6% vs. 30.7%; p = 0.042) and $75,000 or more (20.4% vs. 30.7%; p = 0.006) were less likely to be in Class 2 (Work Interruptions). Notably, none of the individuals who made $75,000 or more in their household were classified into Class 4 (Serious Financial Stress). Individuals with a history of AUD were more likely than individuals without a history of AUD to be in Class 2 (Work Interruptions; 36.1% vs. 16.7%; p < 0.001) and Class 4 (Serious Financial Stress; 11.9% vs. 7.1%; p = 0.008). Compared with individuals enrolled in phase 1, individuals enrolled in phase 2 were less likely to be in Class 2 (Work Interruptions; 18.6% vs. 32.4%; p = 0.011).
Figure 2.
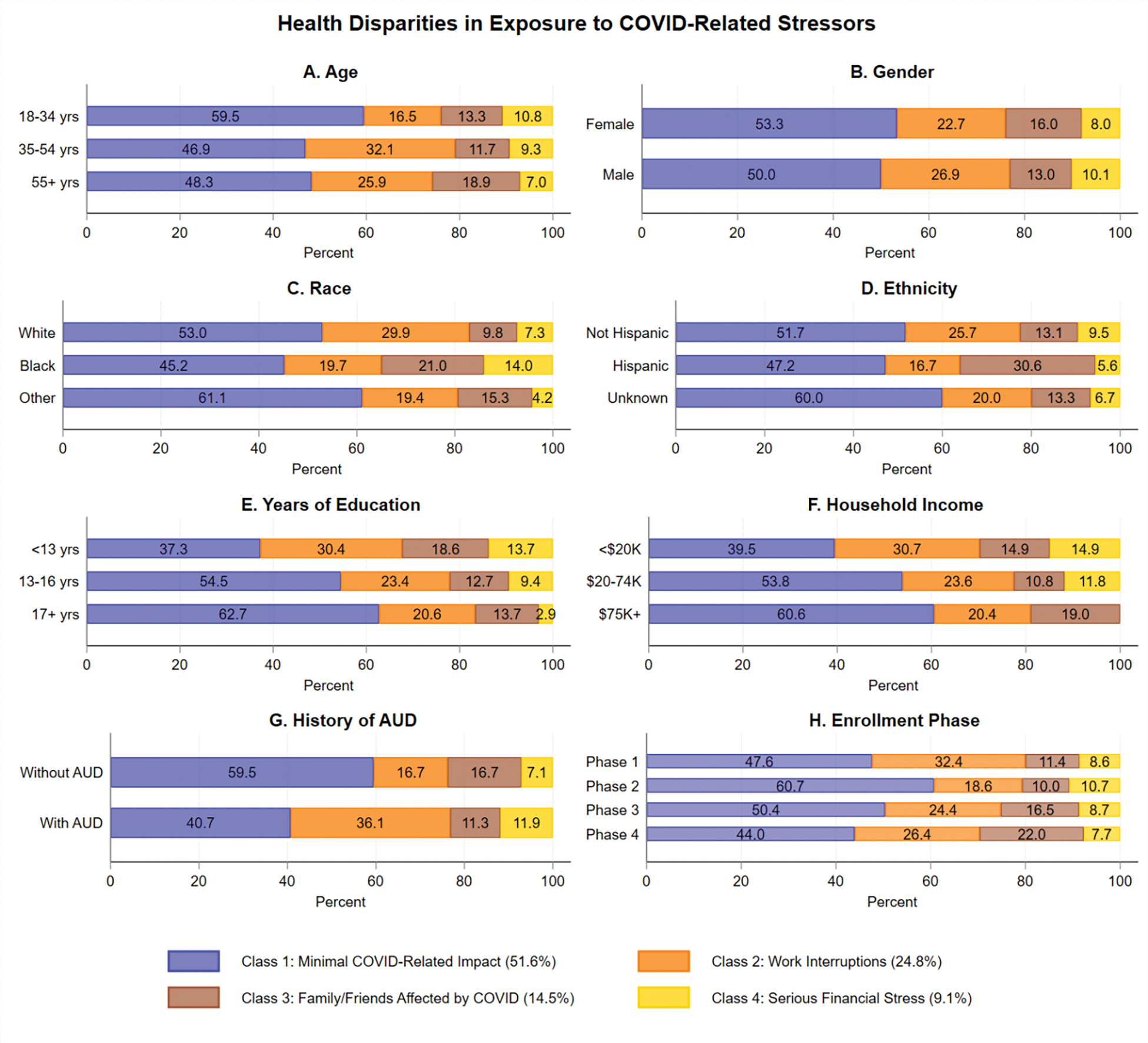
Proportions of Latent Class Membership by Demographic Characteristics, History of AUD, and Enrollment Phase
Note. This figure shows the proportions of the four latent classes by age (Panel A), gender (Panel B), race (Panel C), ethnicity (Panel D), years of education (Panel E), household income (Panel F), history of AUD (Panel G), and enrollment phase (Panel H). AUD = alcohol use disorder. See the online article for the color version of this figure.
Latent Classes and Health-Related Outcomes
Figure 3 presents a comparison of the LCA approach to the continuous sum score and categorical grouping methods. In Panels A1 and B1, the continuous COVID impact sum score was positively associated with perceived stress (b = .86, p < .001) and problematic alcohol use (b = .84, p < .001), but it was unclear if there were dose-response relationships. Panels A2 and B2 demonstrate that, compared with individuals who had 0–1 COVID-related stressors, those who had 4 or more COVID-related stressors reported higher levels of perceived stress (b = 3.78, p < 0.001) and problematic alcohol use (b = 3.99, p = 0.001), yet it was unclear what type of stressors drove the associations. Panel A3 shows that the LCA approach can isolate four distinct groups, such that Class 2 (Work Interruptions; b = 2.52, p = 0.007) and Class 4 (Serious Financial Stress; b = 7.61, p < 0.001) scored higher on perceived stress than Class 1 (Minimal COVID-Related Impact Class). Similarly, Panel B3 shows that Class 2 (b = 6.13, p < 0.001) and Class 4 (b = 6.55, p < 0.001) scored higher on problematic alcohol use than Class 1. Panels C to E illustrate a similar pattern of findings extended to anxiety symptoms, depressive symptoms, and alcohol craving, in which Class 2 and Class 4 had elevated scores relative to Class 1. The regression coefficients and the 95% confidence intervals of all these regression models comparing the three analytic methods are presented in Supplemental Table 4.
Figure 3.
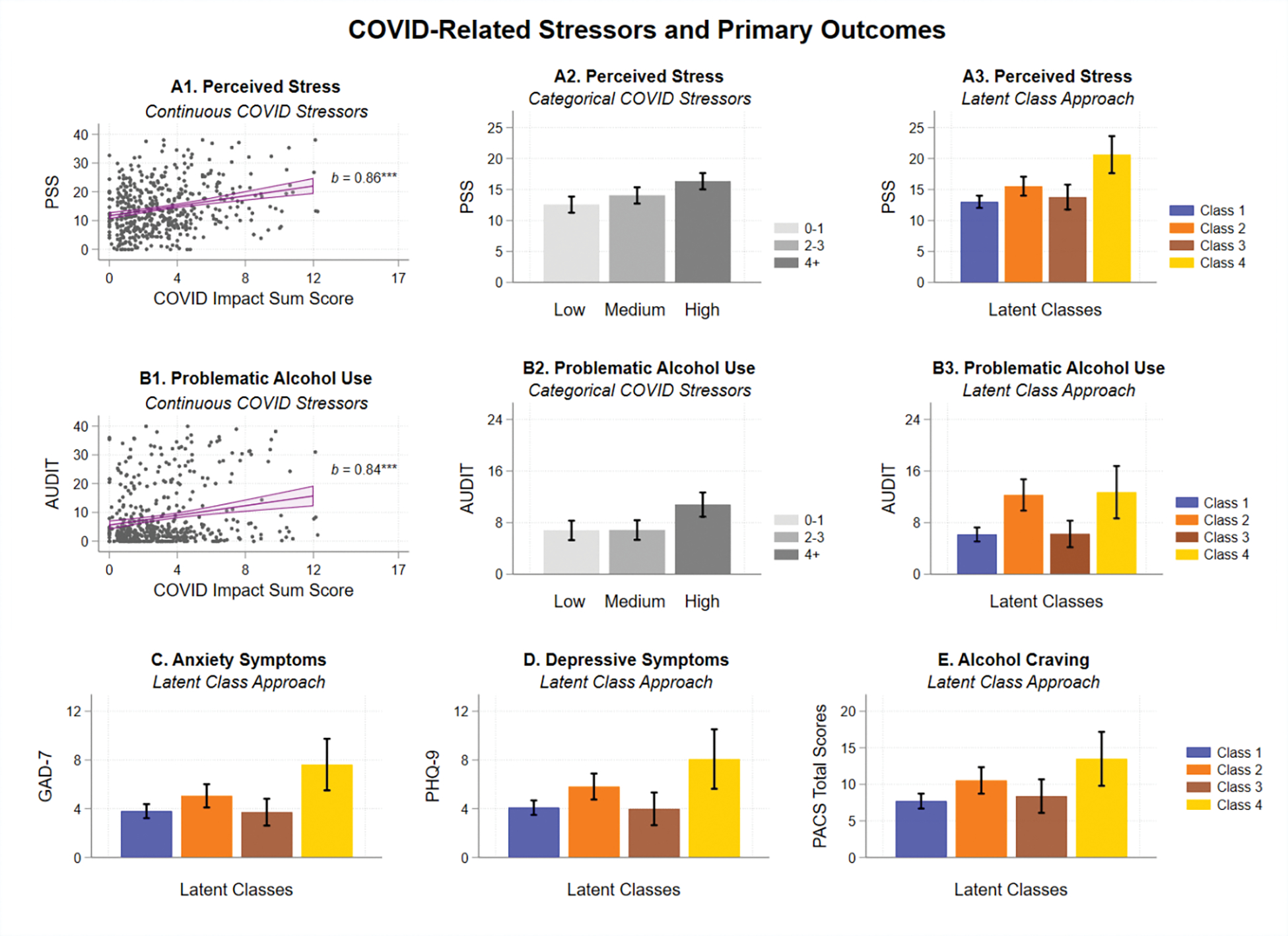
Associations Between COVID-Related Stressors and Primary Outcomes From Baseline 1 Survey
Note. Two common variable-centered approaches are illustrated for perceived stress (Panels A1 and A2) and problematic alcohol use (Panels B1 and B2). These two variable-centered approaches are contrasted with the latent class analysis approach illustrated in Panels A3 and B3, which showed the highest levels of perceived stress and problematic alcohol use in Class 4 (Serious Financial Stress). Panels C, D, and E illustrate that a similar pattern was found for anxiety symptoms, depressive symptoms, and alcohol cravings, respectively. Error bars indicate 95% confidence intervals. PSS = Perceived Stress Scale; AUDIT = Alcohol Use Disorders Identification Test; GAD-7 = Generalized Anxiety Disorder-7; PHQ-9 = Patient Health Questionnaire-9; PACS = Penn Alcohol Craving Scale. See the online article for the color version of this figure.
Figure 4 illustrates the same pattern of latent class differences extended to the secondary outcomes of loneliness (Panel A), drinking to cope (Panel B), and four quality of life domains (Panels C to F), with slight elevations in outcomes observed in Class 2 (Work Interruptions) relative to Class 1 (Minimal COVID-Related Impact Class), and more substantial elevations in outcomes observed in Class 4 (Serious Financial Stress) relative to Class 1. Together, these findings demonstrate the LCA approach was best at isolating the type of stress that drove the associations with outcomes. In the final step, multivariate regression models were used to control for age, gender, race, ethnicity, years of education, household income, history of AUD, and enrollment phase as covariates. The results from these models are presented in Supplemental Table 5. In adjusted analyses, the associations between Class 2 and health-related outcomes were mostly attenuated except for loneliness, physical quality of life, and environment quality of life. In contrast, the associations between Class 4 and all health-related outcomes remained significant after controlling for covariates, suggesting robust associations between experiences of serious financial stress (as reflected in Class 4 membership) and adverse health-related outcomes that were independent of individuals’ demographic characteristics, years of education, household income, history of AUD, and enrollment phase.
Figure 4.
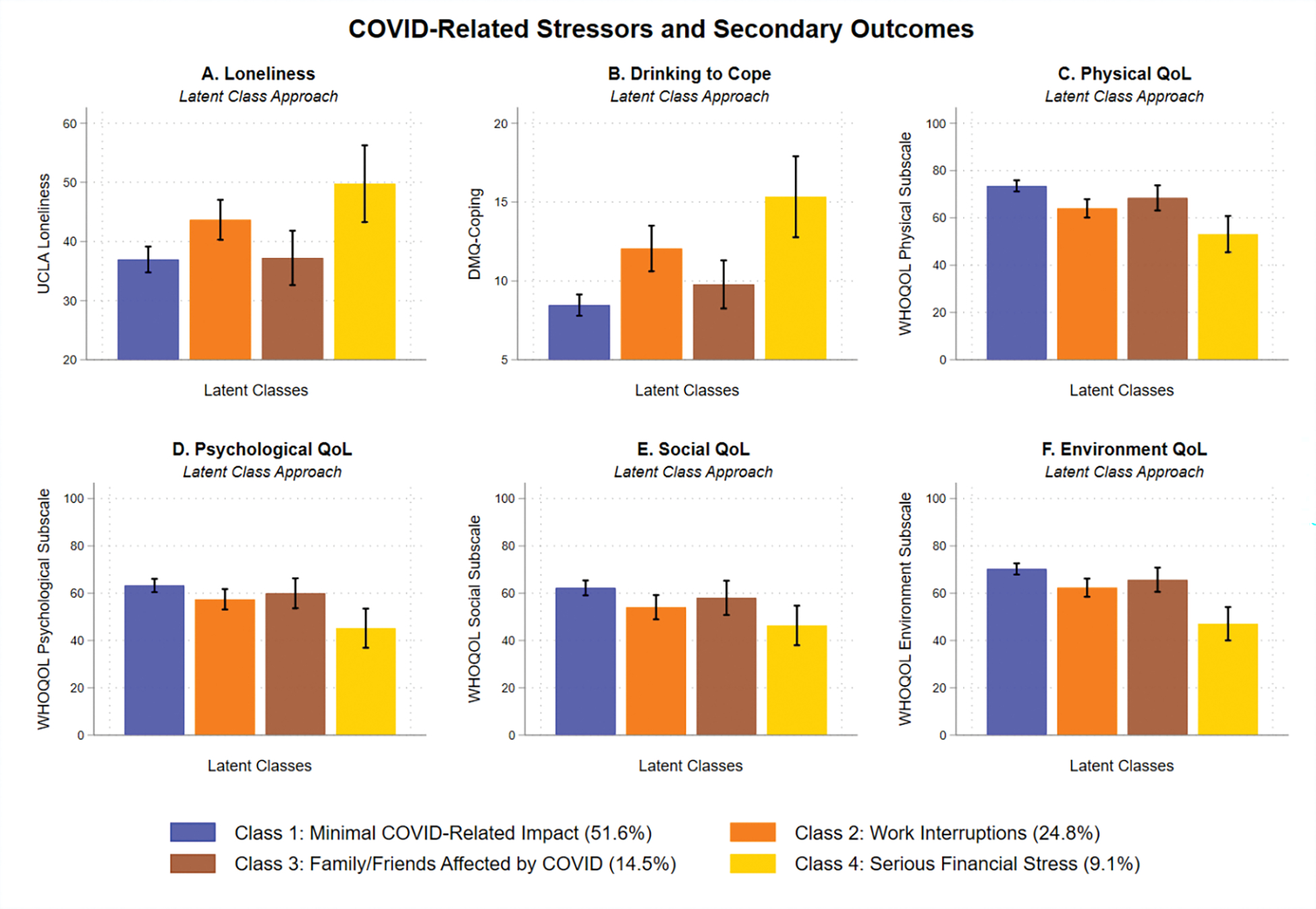
Associations Between COVID-Related Stressors and Secondary Outcomes From Baseline 2 Survey
Note. Utilizing the latent class analysis approach, a consistent pattern emerged in which Class 4 (Serious Financial Stress) scored the highest on secondary outcomes of interest, including loneliness (Panel A), drinking to cope (Panel B), and the four domains of QoL (Panels C, D, E, and F). Error bars indicate 95% confidence intervals. UCLA Loneliness = University of California, Los Angeles Loneliness Scale; DMQ-Coping = Drinking Motives Questionnaire-Revised - Coping Subscale; WHOQOL = World Health Organization Quality of Life-BREF; QoL = quality of life. See the online article for the color version of this figure.
Discussion
The COVID-19 pandemic has posed various types of stressors that may adversely impact health-related outcomes (Gruber et al., 2021), but there is no consensus on how to best construct a multidimensional COVID-related stress variable using the commonly administered items developed by the CDC. Recent measurement studies of COVID-related stress were either constructed based on a disaster-specific framework (Park et al., 2020; Tambling et al., 2021) or modeled after anxiety-related measures (Ahorsu et al., 2020; Taylor et al., 2020). These measures have strong theoretical grounding and can be used to capture individuals’ cognitive appraisals of their situation. Different from these instruments, the 17 COVID-related impact items utilized in the present study were derived from the CDC COVID-19 Community Survey Question Bank (CDC, 2020) and focused more on objective challenges encountered (e.g., “worked reduced hours”) rather than individuals’ cognitive appraisals, e.g., “Pressure to ‘make the most of’ COVID-19 or ‘find a silver lining’ while quarantining” (Park et al., 2020) or “I am most afraid of coronavirus-19” (Ahorsu et al., 2020). These items are suited to understand the contextual challenges individuals encountered during the COVID-19 pandemic, and its utilization can be complementary to the other instruments that were theoretically grounded in the disaster-specific framework or the anxiety literature. The present study contributes to the COVID-19 literature by illustrating how LCA can be effectively applied to identify subgroups of individuals who encountered work-related interruptions (24.8%), COVID-19-specific impact among family/friends (14.5%), and serious financial challenges (9.1%), with a highly consistent pattern emerged showing latent class differences in a wide range of alcohol-related, mental health, and quality of life outcomes.
The use of latent classes to examine disparities showed unique patterns across demographic characteristics and enrollment phase, including greater work interruptions among older individuals and less work interruptions from August 1 to November 22, 2020 (enrollment phase 2). Individuals who were Black/African American and Hispanic/Latino were more likely to have family/friends being affected by COVID-19 (Class 3) than individuals who were White, reinforcing findings from population studies showing higher rates of COVID-related hospitalization and death among racial/ethnic minorities (Acosta et al., 2021; Alsan et al., 2020). Black/African Americans were also more likely to report having serious financial stress (Class 4), but the examination of years of education and household income further revealed striking socioeconomic disparities in exposure to COVID-related stressors. These findings provide the essential socioeconomic context for understanding racial/ethnic minority health disparities (Chowkwanyun & Reed, 2020). Additionally, individuals with AUD were identified as a vulnerable group at risk for encountering work-related interruptions and financial stressors (Bailey et al., 2021; Clay & Parker, 2020; Murthy & Narasimha, 2021). Collectively, these findings indicate the need for holistic interventions and community outreach to minority and vulnerable groups to mitigate the negative effects of COVID-related stressors (Kim et al., 2020; Mein, 2020; Webb Hooper et al., 2020). Interventions aimed to improve health equity may take a multidisciplinary approach to address both individual needs and social determinants of health.
Work-related changes and disruptions were common during the COVID-19 pandemic (Kniffin et al., 2021). However, the latent class that had the worst health-related outcomes was Class 4 which was characterized by substantial disruption to work combined with serious financial difficulties, including moderate probability of not getting paid at all and high probabilities of not having money to pay rent, food, or gas, which is consistent with research studies highlighting the critical role of financial stress in the context of the COVID-19 pandemic (Ettman et al., 2020a; Jiang et al., 2021). Food insecurity was estimated to affect 44–64% of low-income U.S. adults and was associated increased stress, anxiety, and depression (Wolfson & Leung, 2020; Wolfson et al., 2021). The lack of financial security could trigger economic anxiety, which was rated as high as health anxiety in a cross-national study (Bareket-Bojmel et al., 2020). While income disparities in COVID-19 infections, food and housing insecurity, and health care access have been documented (Hall et al., 2021; Jay et al., 2020; Nie et al., 2021; Tan et al., 2021), the current study uniquely showed that the latent class with serious financial stressors had worse alcohol-related, mental health, and quality of life outcomes. These findings highlight the need to provide tangible assistance, social support, and coping skills to these individuals to prevent problematic alcohol use, mental health problems, and reduced quality of life across multiple domains.
The identification of four distinct latent profiles underscores variability in the type(s) of COVID-related stress encountered by individuals during the pandemic and suggests a need for tailored interventions that meet individuals where they are at. For individuals in Class 1 who experienced minimal COVID-related impact, general education on coping with psychological stress, such as normalizing expectable emotional responses, disseminating evidence-based coping strategies, and identifying behavioral health resources, may be informative to the public as a prevention strategy (Horesh & Brown, 2020; Kaslow et al., 2020). For individuals in Classes 2 and 3 who encountered work-related interruptions or had family/friends affected by COVID-19, brief and low-intensity interventions that focus on these specific stressful events may be appropriate and can increase reach to the target individuals (Gruber et al., 2021; Schleider et al., 2022). For individuals in Class 4 who experienced significant financial stressors, more intensive and holistic interventions may be necessary to address the multiple stressors and health disparities associated with mental health problems during COVID-19 (Loeb et al., 2021). At a broader societal level, public health psychology approaches targeting structural factors that lead to health inequity hold promise in mitigating the disproportionate psychosocial burden (including fear, stigma, and medical mistrust) among marginalized populations (Halkitis, 2020).
This study has several limitations. First, the study sample was relatively small and was not representative of the general population. Although generalizability of findings was limited, the diversity of the sample was a strength. Second, data on history of AUD, years of education, and household income were drawn from the natural history protocol and could reflect participants’ past rather than current situation. Similarly, variability in time lapsed from Baseline 1 to Baseline 2 could reflect delayed measurement of secondary outcomes, although this concern may be partially mitigated by the consistency of findings across multiple outcomes. Third, social desirability bias may be greater in surveys administered via the phone than over the Internet. Moreover, participants who did not complete the online survey had missing data on secondary outcomes which could have introduced biases in the regression estimates. Fourth, the availability of stimulus checks and the role of inflation were not assessed but could have influenced participants’ financial situation. Similarly, vaccine access and vaccination status were not measured but could have impacted the severity of COVID-19 stressors across enrollment phases. More research is needed to examine financial resources and protection from vaccination as potential buffers against the adverse impact of COVID-related stressors on health-related outcomes. Finally, cross-sectional data gathered during the pandemic were analyzed and causal inferences cannot be drawn. For instance, although financial stressors attributable to COVID-19 can lead to problematic alcohol use, problematic alcohol use can also negatively impact financial well-being, highlighting the need for longitudinal follow-up of study participants to disentangle these complex and potentially bi-directional associations over time.
Using a person-centered approach, about half of the participants were classified into latent classes that were characterized by exposure to different types of COVID-related stressors, capturing substantial heterogeneity in COVID-related experiences during the pandemic. In a diverse sample, racial and ethnic minorities were more likely to have family/friends affected by COVID-19, whereas individuals with AUD were more likely to encounter work interruptions and financial stressors. Close to 1 in 10 participants (9.1%) reported serious financial stress, which was consistently associated with adverse alcohol-related, mental health, and quality of life outcomes. These findings underscore the need for holistic interventions and community outreach to help alleviate the adverse and potentially long-term impact of COVID-related stressors and improve health equity among minority and vulnerable populations.
Supplementary Material
Public Significance Statement.
This study examined different types of stressors that people encountered during the COVID-19 pandemic such as work interruptions, financial stress, and knowing someone infected with COVID-19. Individuals who experienced multiple financial stressors made up a small minority but had higher mental health and alcohol-related problems, as well as lower quality of life. This group of individuals may benefit from holistic interventions and community outreach.
Acknowledgements:
The authors would like to thank Sumedha Chawla, Beth Lee, Megan Carraco, Sheila Walsh, Betsy Davis, Cheryl Jones, Samantha Fede, Alyssa Brooks, Tonette Vinson, Yvonne Horneffer, LaToya Sewell, the ClinDB IT team (Thuy Van, Etienne Lamoreaux, Denise Gates-Nee, Nancy Agarwal, Patty Bates, Jonathan Folkers), and the intrepid postbaccalaureate Intramural Research Training Award fellows (Jared Axelowitz, Hannah Kim, Noa Leiter, Emma McCabe, Carlos Melendez, James Morris, Kurren Parida, Rhianna Vergeer, Ugne Ziausyte) for supporting the execution of the C19-PIA Study.
Funding Support:
This study was supported by NIAAA Division of Intramural Clinical and Biological Research (Z1A AA000130, Z1A AA000466) and a NIAID Intramural Targeted Anti-COVID (ITAC) Award.
Footnotes
Conflicts of Interest: The authors do not have any conflicts of interest to disclose.
Data Access and Preregistration: The study protocol was approved by the NIH Intramural Institutional Review Board and is registered in clinicaltrials.gov (NCT04391816). The analysis plan for this manuscript was not preregistered. Data and study materials are not publicly available and can be provided upon request in a deidentified form.
References
- Acosta AM, Garg S, Pham H, Whitaker M, Anglin O, O’Halloran A, Milucky J, Patel K, Taylor C, Wortham J, Chai SJ, Kirley PD, Alden NB, Kawasaki B, Meek J, Yousey-Hindes K, Anderson EJ, Openo KP, Weigel A, Monroe ML, Ryan P, Reeg L, Kohrman A, Lynfield R, Bye E, Torres S, Salazar-Sanchez Y, Muse A, Barney G, Bennett NM, Bushey S, Billing L, Shiltz E, Sutton M, Abdullah N, Talbot HK, Schaffner W, Ortega J, Price A, Fry AM, Hall A, Kim L, & Havers FP (2021, Oct 1). Racial and Ethnic Disparities in Rates of COVID-19-Associated Hospitalization, Intensive Care Unit Admission, and In-Hospital Death in the United States From March 2020 to February 2021. JAMA Netw Open, 4(10), e2130479. 10.1001/jamanetworkopen.2021.30479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, & Pakpour AH (2020, Mar 27). The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict, 1–9. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alon-Tirosh M, Hadar-Shoval D, Asraf K, Tannous-Haddad L, & Tzischinsky O (2021, Sep 15). The Association between Lifestyle Changes and Psychological Distress during COVID-19 Lockdown: The Moderating Role of COVID-Related Stressors. Int J Environ Res Public Health, 18(18). 10.3390/ijerph18189695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsan M, Stantcheva S, Yang D, & Cutler D (2020, Jun 1). Disparities in Coronavirus 2019 Reported Incidence, Knowledge, and Behavior Among US Adults. JAMA Netw Open, 3(6), e2012403. 10.1001/jamanetworkopen.2020.12403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelucci M, Angrisani M, Bennett DM, Kapteyn A, & Schaner SG (2020). Remote work and the heterogeneous impact of covid-19 on employment and health. National Bureau of Economic Research. 10.3386/w27749 [DOI] [Google Scholar]
- Asch DA, Islam MN, Sheils NE, Chen Y, Doshi JA, Buresh J, & Werner RM (2021, Jun 1). Patient and Hospital Factors Associated With Differences in Mortality Rates Among Black and White US Medicare Beneficiaries Hospitalized With COVID-19 Infection. JAMA Netw Open, 4(6), e2112842. 10.1001/jamanetworkopen.2021.12842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey KL, Samuelson DR, & Wyatt TA (2021, Feb). Alcohol use disorder: A pre-existing condition for COVID-19? Alcohol, 90, 11–17. 10.1016/j.alcohol.2020.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bareket-Bojmel L, Shahar G, & Margalit M (2020, May 29). COVID-19-Related Economic Anxiety Is As High as Health Anxiety: Findings from the USA, the UK, and Israel. Int J Cogn Ther, 1–9. 10.1007/s41811-020-00078-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Béland L-P, Brodeur A, & Wright T (2020). The short-term economic consequences of Covid-19: exposure to disease, remote work and government response. IZA Discussion Paper No. 13159. 10.2139/ssrn.3584922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SM, Doom JR, Lechuga-Peña S, Watamura SE, & Koppels T (2020, Dec). Stress and parenting during the global COVID-19 pandemic. Child Abuse Negl, 110(Pt 2), 104699. 10.1016/j.chiabu.2020.104699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brynjolfsson E, Horton JJ, Ozimek A, Rock D, Sharma G, & TuYe H-Y (2020). COVID-19 and remote work: an early look at US data. National Bureau of Economic Research. 10.3386/w27344 [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). CDC COVID-19 Community Survey Question Bank (DRAFT) https://cde.nlm.nih.gov/formView?tinyId=Kcceysolt [PubMed]
- Chowkwanyun M, & Reed AL Jr. (2020, Jul 16). Racial Health Disparities and Covid-19 - Caution and Context. N Engl J Med, 383(3), 201–203. 10.1056/NEJMp2012910 [DOI] [PubMed] [Google Scholar]
- Clay JM, & Parker MO (2020). Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? The Lancet Public Health, 5(5), e259. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7195126/pdf/main.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. J Health Soc Behav, 24(4), 385–396. [PubMed] [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological assessment, 6(2), 117–128. [Google Scholar]
- Dhongde S (2020). Multidimensional economic deprivation during the coronavirus pandemic: Early evidence from the United States. PLoS One, 15(12), e0244130. 10.1371/journal.pone.0244130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz T, Dastidar MG, Troxel WM, Beckman R, Nugroho A, Siddiqi S, Cantor J, Baird M, Richardson AS, Hunter GP, Mendoza-Graf A, & Collins RL (2021, Mar). Food Insecurity in a Low-Income, Predominantly African American Cohort Following the COVID-19 Pandemic. Am J Public Health, 111(3), 494–497. 10.2105/ajph.2020.306041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel GL (1977, Apr 8). The need for a new medical model: a challenge for biomedicine. Science, 196(4286), 129–136. 10.1126/science.847460 [DOI] [PubMed] [Google Scholar]
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, & Galea S (2020a). Low assets and financial stressors associated with higher depression during COVID-19 in a nationally representative sample of US adults. Journal of Epidemiology and Community Health, 75(6), 501–508. 10.1136/jech-2020-215213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, & Galea S (2020b, Sep 1). Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open, 3(9), e2019686. 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang D, Thomsen MR, Nayga RM Jr., & Yang W (2021, Jul 7). Food insecurity during the COVID-19 pandemic: evidence from a survey of low-income Americans. Food Secur, 1–19. 10.1007/s12571-021-01189-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB (2015). Structured clinical interview for the DSM (SCID). In Cautin RL & Lilienfeld SO (Eds.), The encyclopedia of clinical psychology (pp. 1–6). Wiley. 10.1002/9781118625392.wbecp351 [DOI] [Google Scholar]
- Flannery B, Volpicelli J, & Pettinati H (1999). Psychometric properties of the Penn alcohol craving scale. Alcoholism: Clinical and Experimental Research, 23(8), 1289–1295. [PubMed] [Google Scholar]
- Gemelas J, Davison J, Keltner C, & Ing S (2021, Jan 15). Inequities in Employment by Race, Ethnicity, and Sector During COVID-19. J Racial Ethn Health Disparities, 1–6. 10.1007/s40615-021-00963-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green H, Fernandez R, & MacPhail C (2021, Nov). The social determinants of health and health outcomes among adults during the COVID-19 pandemic: A systematic review. Public Health Nurs, 38(6), 942–952. 10.1111/phn.12959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J, Prinstein MJ, Clark LA, Rottenberg J, Abramowitz JS, Albano AM, Aldao A, Borelli JL, Chung T, Davila J, Forbes EE, Gee DG, Hall GCN, Hallion LS, Hinshaw SP, Hofmann SG, Hollon SD, Joormann J, Kazdin AE, Klein DN, La Greca AM, Levenson RW, MacDonald AW, McKay D, McLaughlin KA, Mendle J, Miller AB, Neblett EW, Nock M, Olatunji BO, Persons JB, Rozek DC, Schleider JL, Slavich GM, Teachman BA, Vine V, & Weinstock LM (2021, Apr). Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am Psychol, 76(3), 409–426. 10.1037/amp0000707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN (2020, Dec). A new public health psychology to mend the chasm between public health and clinical care. Am Psychol, 75(9), 1289–1296. 10.1037/amp0000743 [DOI] [PubMed] [Google Scholar]
- Hall LR, Sanchez K, da Graca B, Bennett MM, Powers M, & Warren AM (2021, Oct 14). Income Differences and COVID-19: Impact on Daily Life and Mental Health. Popul Health Manag. 10.1089/pop.2021.0214 [DOI] [PubMed] [Google Scholar]
- Horesh D, & Brown AD (2020, May). Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychol Trauma, 12(4), 331–335. 10.1037/tra0000592 [DOI] [PubMed] [Google Scholar]
- Jay J, Bor J, Nsoesie EO, Lipson SK, Jones DK, Galea S, & Raifman J (2020, Dec). Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat Hum Behav, 4(12), 1294–1302. 10.1038/s41562-020-00998-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Y, Zilioli S, Balzarini RN, Zoppolat G, & Slatcher RB (2021). Education, Financial Stress, and Trajectory of Mental Health During the COVID-19 Pandemic. Clinical Psychological Science. 10.1177/21677026211049374 [DOI] [Google Scholar]
- Kaslow NJ, Friis-Healy EA, Cattie JE, Cook SC, Crowell AL, Cullum KA, Del Rio C, Marshall-Lee ED, LoPilato AM, VanderBroek-Stice L, Ward MC, White DT, & Farber EW (2020, Oct). Flattening the emotional distress curve: A behavioral health pandemic response strategy for COVID-19. Am Psychol, 75(7), 875–886. 10.1037/amp0000694 [DOI] [PubMed] [Google Scholar]
- Kathe NJ, & Wani RJ (2021, May 11). Determinants of COVID-19 Case Fatality Rate in the United States: Spatial Analysis Over One Year of the Pandemic. J Health Econ Outcomes Res, 8(1), 51–62. 10.36469/jheor.2021.22978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim EJ, Marrast L, & Conigliaro J (2020, Aug). COVID-19: Magnifying the Effect of Health Disparities. J Gen Intern Med, 35(8), 2441–2442. 10.1007/s11606-020-05881-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimani ME, Sarr M, Cuffee Y, Liu C, & Webster NS (2021, Jun 1). Associations of Race/Ethnicity and Food Insecurity With COVID-19 Infection Rates Across US Counties. JAMA Netw Open, 4(6), e2112852. 10.1001/jamanetworkopen.2021.12852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kniffin KM, Narayanan J, Anseel F, Antonakis J, Ashford SP, Bakker AB, Bamberger P, Bapuji H, Bhave DP, Choi VK, Creary SJ, Demerouti E, Flynn FJ, Gelfand MJ, Greer LL, Johns G, Kesebir S, Klein PG, Lee SY, Ozcelik H, Petriglieri JL, Rothbard NP, Rudolph CW, Shaw JD, Sirola N, Wanberg CR, Whillans A, Wilmot MP, & Vugt MV (2021, Jan). COVID-19 and the workplace: Implications, issues, and insights for future research and action. Am Psychol, 76(1), 63–77. 10.1037/amp0000716 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine, 16(9), 606–613. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1495268/pdf/jgi_01114.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusin S, & Choo E (2021, Jan 9). Parenting in the time of COVID-19. Lancet, 397(10269), 86. 10.1016/s0140-6736(20)32755-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwako LE, Schwandt ML, Ramchandani VA, Diazgranados N, Koob GF, Volkow ND, Blanco C, & Goldman D (2019, Sep 1). Neurofunctional Domains Derived From Deep Behavioral Phenotyping in Alcohol Use Disorder. Am J Psychiatry, 176(9), 744–753. 10.1176/appi.ajp.2018.18030357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb TB, Ebor MT, Smith-Clapham AM, Chin D, Novacek DM, Hampton-Anderson JN, Norwood-Scott E, Hamilton AB, Brown AF, & Wyatt GE (2021, Mar). How Mental Health Professionals Can Address Disparities in the Context of the COVID-19 Pandemic. Traumatology (Tallahass Fla), 27(1), 60–69. 10.1037/trm0000292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mein SA (2020, Aug). COVID-19 and Health Disparities: the Reality of “the Great Equalizer”. J Gen Intern Med, 35(8), 2439–2440. 10.1007/s11606-020-05880-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy P, & Narasimha VL (2021). Effects of the COVID-19 pandemic and lockdown on alcohol use disorders and complications. Current Opinion in Psychiatry, 34(4), 376–385. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8183243/pdf/coip-34-376.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie P, Ding L, Chen Z, Liu S, Zhang Q, Shi Z, Wang L, Xue H, Liu GG, & Wang Y (2021, Apr 26). Income-related health inequality among Chinese adults during the COVID-19 pandemic: evidence based on an online survey. Int J Equity Health, 20(1), 106. 10.1186/s12939-021-01448-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural equation modeling: A multidisciplinary Journal, 14(4), 535–569. [Google Scholar]
- Park CL, Russell BS, Fendrich M, Finkelstein-Fox L, Hutchison M, & Becker J (2020, Aug). Americans’ COVID-19 Stress, Coping, and Adherence to CDC Guidelines. J Gen Intern Med, 35(8), 2296–2303. 10.1007/s11606-020-05898-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royston P, & White IR (2011). Multiple imputation by chained equations (MICE): implementation in Stata. J Stat Softw, 45(4), 1–20. [Google Scholar]
- Russell D, Peplau LA, & Ferguson ML (1978, Jun). Developing a measure of loneliness. J Pers Assess, 42(3), 290–294. 10.1207/s15327752jpa4203_11 [DOI] [PubMed] [Google Scholar]
- Sarangi A, & Eskander N (2021). The Worsening Outcomes of the COVID-19 Lockdowns on Patients with a History of Alcoholism. Alcoholism Treatment Quarterly, 1–6. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993, Jun). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction, 88(6), 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Schleider JL, Mullarkey MC, Fox KR, Dobias ML, Shroff A, Hart EA, & Roulston CA (2022, Feb). A randomized trial of online single-session interventions for adolescent depression during COVID-19. Nat Hum Behav, 6(2), 258–268. 10.1038/s41562-021-01235-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Löwe B (2006, May 22). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Tambling RR, Russell BS, Park CL, Fendrich M, Hutchinson M, Horton AL, & Tomkunas AJ (2021, Feb). Measuring Cumulative Stressfulness: Psychometric Properties of the COVID-19 Stressors Scale. Health Educ Behav, 48(1), 20–28. 10.1177/1090198120979912 [DOI] [PubMed] [Google Scholar]
- Tan AX, Hinman JA, Abdel Magid HS, Nelson LM, & Odden MC (2021, May 3). Association Between Income Inequality and County-Level COVID-19 Cases and Deaths in the US. JAMA Netw Open, 4(5), e218799. 10.1001/jamanetworkopen.2021.8799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, & Asmundson GJG (2020, May). Development and initial validation of the COVID Stress Scales. J Anxiety Disord, 72, 102232. 10.1016/j.janxdis.2020.102232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb Hooper M, Nápoles AM, & Pérez-Stable EJ (2020, Jun 23). COVID-19 and Racial/Ethnic Disparities. Jama, 323(24), 2466–2467. 10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group WHOQOL. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological medicine, 28(3), 551–558. [DOI] [PubMed] [Google Scholar]
- Wolfson JA, Garcia T, & Leung CW (2021). Food Insecurity Is Associated with Depression, Anxiety, and Stress: Evidence from the Early Days of the COVID-19 Pandemic in the United States. Health Equity, 5(1), 64–71. 10.1089/heq.2020.0059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson JA, & Leung CW (2020, Jun 2). Food Insecurity and COVID-19: Disparities in Early Effects for US Adults. Nutrients, 12(6). 10.3390/nu12061648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancy CW (2020, May 19). COVID-19 and African Americans. Jama, 323(19), 1891–1892. 10.1001/jama.2020.6548 [DOI] [PubMed] [Google Scholar]
- Yazdi K, Fuchs-Leitner I, Rosenleitner J, & Gerstgrasser NW (2020). Impact of the COVID-19 Pandemic on Patients With Alcohol Use Disorder and Associated Risk Factors for Relapse. Front Psychiatry, 11, 620612. 10.3389/fpsyt.2020.620612 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


