Dear Editor,
Rabies is a preventable viral disease of mammals, caused by a neurotropic virus, Rabies virus. It is usually transmitted through the bite of an infected animal. Rabies virus is a bullet-shaped, single-stranded, negative-sense, non-segmented, enveloped RNA virus, that belongs to Lyssavirus, a member of the Rhabdoviridae family, Mononegavirales order (CDC, https://www.cdc.gov/rabies/about.html).
Rabies spreads to humans and among animals through bites and scratches of infected animals. Domestic dogs are the predominant source of rabies virus in developing countries, while wild animals are the primary carriers of rabies in developed countries. Nearly 99% of human rabies cases are caused by dog bites [1]. Reduced awareness, hyperactivity, hallucinations, hydrophobia, paralysis, coma, and sudden and uncontrollable death are some of the clinical signs of rabies.
Every year, rabies, one of the fatal viral diseases in the world, causes the deaths of about 60,000 people and over 3.7 million disability-adjusted life years (DALYs) lost. The incidence of rabies is most common in Asia and Africa; therefore, it can be said that it is a neglected tropical disease. A common but underreported issue in poor countries is dog bites. Nearly 80% of reported cases of rabies occur in rural areas of each country, and more than 40% of rabies fatalities involve children under the age of 15 years (WHO, https://www.who.int/publications/i/item/9789241513838). The most disadvantaged and marginalized groups bear this disease's most remarkable economic burden globally. People continue to die from rabies due to their low disease awareness, poverty, the disease's continuous transmission among dogs, and their lack of access to primary medical care like post-exposure prophylaxis (PEP) [2].
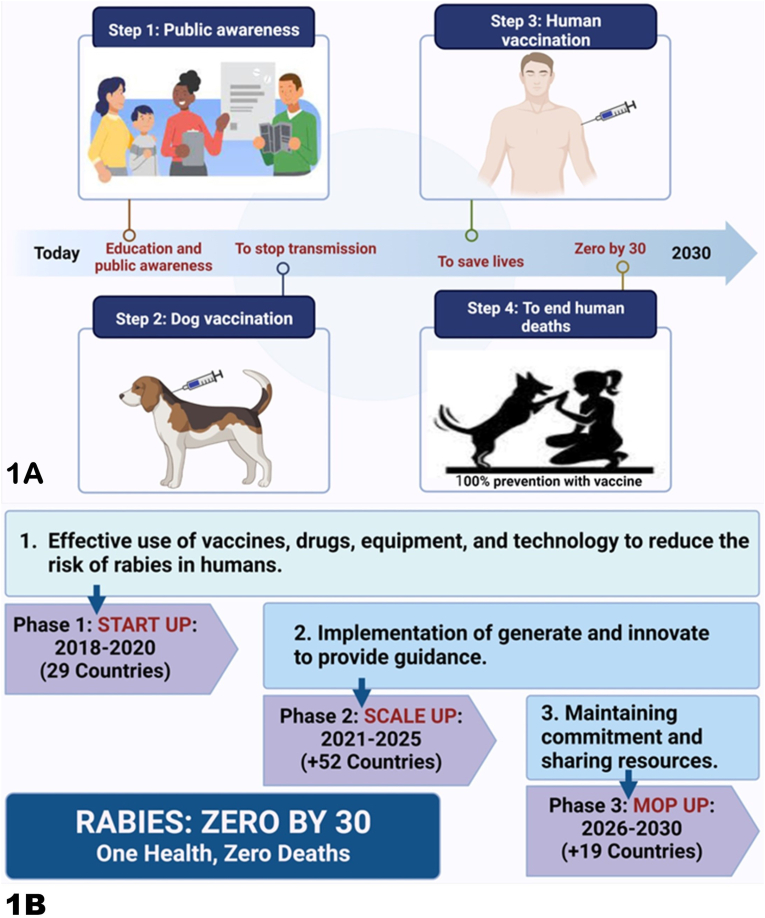
Three strategies have been demonstrated to be successful in controlling and preventing rabies; 1) raising awareness about rabies, 2) post-exposure prophylaxis (PEP), a series of rabies vaccines, and, in certain situations, rabies immunoglobulin (RIG), administered, and 3) By preventing rabies transmission at its source, mass vaccination of dogs has been proven to be a successful and cost effective way of saving lives. The prevention of disease transmission from dogs to humans and from dogs to other dogs depends on sustained vaccination coverage for 70% of the dog population. Therefore, eradicating rabies in dogs (e.g., dogs' vaccination) is essential for long-term prevention between dogs and humans [3] (Fig. 1A).
Fig. 1.
A. The global strategic plan against the elimination of rabies (Zero by 30 and One health).1B. Rabies One Health global program is implementing a three-phase eradication strategy as part of the global vision and mission to reach zero by 2030. Four global organizations-WHO, FAO, OIE, and GARC-came together to make this international and shared effort. By the end of 2030, no one should die from rabies because of this effort.
In many developing countries, insufficient animal control and intermittent vaccination campaigns have increased the chance of getting rabies from dogs. When money is invested in rabies eradication, the human and veterinary health systems improve, and lives are saved. The integrated rabies elimination strategy acts as a model of One Health cooperation. In the past, the global response has been fragmented and unorganized. The goal of eliminating all human-dog rabies deaths worldwide by 2030 has been set by the Global Alliance for Rabies Control (GARC), the World Organization for Animal Health (OIE), the Food and Agriculture Organization of the United Nations (FAO), and the World Health Organization (WHO) since 2015 (zero by 30). This main objective is precisely aligned with the Sustainable Development Goal (SDG) of the United Nations, which is to “improve the quality of healthcare and happiness for all at all ages”.
A widespread educational activity on rabies prevention and control in schools, community committees, instructional pamphlets, and network media is a requirement for the achievement of the goal. To achieve the goal of “Zero by 30”, the global strategy to tackle the rabies should also emphasize on the intersectoral collaboration including the medical doctors, veterinarians, ecologists, environmentalists, and law-enforcement agents [4].
Rabies is becoming a priority disease in many endemic countries. Since rabies is the most prevalent zoonotic disease in those regions, 17 of the 18 countries that prioritized it as of 2014 in One Health zoonotic disease priority workshops held in Africa, Asia, Eurasia, and the Americas. The international strategic plan to achieve zero by 2030 is focused on these countries. According to the theory of change announced by WHO, three global strategic objectives for the elimination of rabies have been prioritized: 1) Effective use of vaccines, drugs, tools, and technologies to reduce human rabies risk through dog vaccination and increased public awareness; 2) The development, innovation, and coordination of policies and guidelines coordinated with international and national strategies, encouraging technology and health innovations, and strengthening health and treatment systems; 3) The impact of international partnerships against rabies at national, regional, and global levels. A strong rabies program also needs to have access to qualified people in the fields of education, human health, and animal health [5]. The three three-phase strategies used by One Health to implement its global Zero by 30 goals include phase 1: Startup (countries where rabies is a priority, countries that are currently engaged in rabies control or countries with projects that might learn to implement projects more effectively in the future), phase 2: Scale up (maintaining support for Phase 1 participating countries while involving more countries), and phase 3: Mop up (engaging the remaining countries and completing the prospective program) (Fig. 1B).
Globalization, international traveling, and stray dogs are some of the challenges that face rabies eradication strategy. Through a One-Health approach, the Alliance Against Rabies aids countries in developing practical and feasible systems. Recently, there have been a few successful examples. The One Health India action plan is a model of leadership in India and can serve as an example for other rabies-endemic countries by 2030. As India carries about one-third of the global burden of rabies, it can play a key role in achieving this global aim. India has made it a priority to stop this preventable disease. Rabies cases have declined in Bangladesh, the Philippines, Sri Lanka, Tanzania, Vietnam, and South Africa. Mexico was the first country to get WHO permission to end dog-borne rabies as a public health issue (WHO, https://www.who.int/news-room/detail/21-12-2019-mexico-is-free-from-human-rabies-transmitted-by-dogs). To combat frequent killer diseases among humans and animals, including rabies, One-Health approaches are crucial to the sustainable prevention of neglected tropical diseases and eliminating health inequalities in underdeveloped communities.
CRediT authorship contribution statement
Maryam Shafaati: Conceptualization, Data Curation, Visualization, Writing - Original Draft, Writing - review & editing. Samaneh Akbarpour: Conceptualization, Data Curation, Visualization, Writing - Original Draft, Writing - review & editing. Priyanka: Conceptualization, Data Curation, Visualization, Writing - Original Draft, Writing - review & editing. AbdulRahman A Saied: Conceptualization, Data Curation, Visualization, Writing - Original Draft, Writing - review & editing. Om Prakash Choudhary: Conceptualization, Data Curation, Visualization, Supervision, Writing - Original Draft, Writing - review & editing.
Disclosure statement
All authors report no conflicts of interest relevant to this article.
Data availability statement
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Ethics statement
This manuscript does not contain any studies with animals performed by the author.
Funding
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgments
Fig. 1 has been created with BioRender (https://biorender.com/). The authors are thankful to their respective institutions/universities for the completion of this work.
References
- 1.Audu S.M., Mshelbwala P.P., Jahun B.M., Bouaddi K., Weese J.S. Two fatal cases of rabies in humans who did not receive rabies postexposure prophylaxis in Nigeria. Clinical Case Reports. 2019;7(4):749–752. doi: 10.1002/ccr3.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hampson K., Coudeville L., Lembo T., Sambo M., Kieffer A., Attlan M., et al. Estimating the global burden of endemic canine rabies. PLoS Neglected Tropical Diseases. 2015;9(4) doi: 10.1371/journal.pntd.0003709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hampson K., Ventura F., Steenson R., Mancy R., Trotter C., Cooper L., et al. The potential effect of improved provision of rabies post-exposure prophylaxis in Gavi-eligible countries: a modelling study. The Lancet Infectious Diseases. 2019;19(1):102–111. doi: 10.1016/S1473-3099(18)30512-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kardjadj M., Ben-Mahdi M.H. Epidemiology of dog-mediated zoonotic diseases in Algeria: a One Health control approach. New Microbes and New Infections. 2019;28:17–20. doi: 10.1016/j.nmni.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Minghui R., Stone M., Semedo M.H., Nel L. New global strategic plan to eliminate dog-mediated rabies by 2030. The Lancet Global Health. 2018;6(8):e828–e829. doi: 10.1016/S2214-109X(18)30302-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.