Abstract
Background and Objective: Various periorbital rejuvenation techniques have been introduced over the last 3 decades. This study highlights important milestones in the evolution of periorbital rejuvenation surgery by identifying the 100 most-cited articles in this field. Material and Methods: The Web of Science citation index was used to identify the 100 most-cited articles concerning periorbital rejuvenation. Articles published in English from January 1989–April 2020 describing periorbital rejuvenation-related surgical techniques, facial aging, and anatomy were included. The terms “lower blepharoplasty”, “upper blepharoplasty”, “browlift”, “browplasty”, “endobrow lift”, “endoscopic brow”, “Foreheadplasty”, “lower eyelid anatomy”, “upper eyelid anatomy”, “forehead lift”, “eyelid rejuvenation”, “canthopexy”, “canthoplasty”, “eyelid fat pad”, “orbital fat pad”, “tear trough”, and “eyelid bags” were entered into the citation search. Web of Science Core Collection was the database used for the search. A manual review of the initial 159 studies was performed. Articles describing reconstructive or non-invasive techniques, injectable fillers, lasers, and neurotoxins were excluded. Of the 100 most-cited articles, the publication year, specialty journal, the corresponding author’s primary specialty, the focus of the article, the corresponding author’s country of residence, the type of study, and the level of evidence were analyzed. Results: The mean number of citations per article was 75 ± 42. There were more articles published from 1989–1999 (n = 53) than later decades. Most articles originated from the USA (n = 82) and were published in plastic surgery journals (n = 81). Plastic surgery was the primary specialty of the corresponding authors (n = 71), followed by oculoplastic surgery (n = 22). Most articles (n = 69) reported on surgical techniques. Of the clinical studies (n = 69), 45 (79%) provided level IV evidence. Conclusions: Of the 100 most-cited studies on periorbital rejuvenation, studies focusing on periorbital anatomy, aging, and surgical techniques comprised the most-cited publications. An anatomically based approach accounting for age-related changes in the periorbital structures is paramount in the field of contemporary periorbital rejuvenation.
Keywords: blepharoplasty, browlift, eyelid anatomy, facelift, facial aging, fat compartment, fat graft, periorbital rejuvenation
1. Introduction
The human face is composed of layers that play a role in facial appearance and aging. These layers are arranged in five lamellar components that are clearly defined in the scalp and range from superficial to deep, as follows: skin, subcutaneous tissue, the musculo-aponeurotic layer (superficial musculoaponeurotic system—SMAS), loose areolar tissue, and the deep fascia or periosteum. Facial rejuvenation is based on the manipulation and re-draping of these tissue layers as well as specific anatomic attachments including ligaments, adhesions, and septa.
Rejuvenation, a word originating from the Latin words “re” and “juvenis”, meaning “young again”, has always been a historic interest in various cultures and civilizations. The first historically reported procedures for periorbital rejuvenation date back to the first century and stem from Aulus Cornelius Celsus’s seventh book of his encyclopedia De Medicina Ovto Libri [1]. Later accounts of the cauterization of excess eyelid skin by Arabian surgeons were reported in the 10th century [2]. In the 17th century, Ambroise Pare [3] performed corrections of excess eyelid skin. In 1896, Fuchs [4] introduced the word “blepharochalasis” to describe the thin, wrinkled eyelids of a teenager. In 1924, Bourguet [5] described transconjunctival lower eyelid blepharoplasty. In 1931, Claoué [6] and Passot [7] described the removal of the bulging fat pad in the lower eyelid, which was previously described by Bourguet through a transconjunctival approach. In 1947, Pierce et al. [8] described a technique of excising the corrugator supercilii muscle to treat frowning in a teacher. This was followed by Bames [9] in 1957, who described a technique for skin ellipse excision directly above the brow and the complete resection of the corrugator supercilii muscle to correct brow ptosis and frowning, respectively. In the same decade, Castañares [10] published a landmark article in which he described the orbital fat pad compartments in detail. He based his new blepharoplasty technique on this anatomical description, which became the basis for modern blepharoplasty. Subsequent reports in the late 1960s and 1970s by Rhees [11], Loeb [12], and Furnas [13] described the excision of redundant orbicularis oculi muscle tissue and bulging fat pads, emphasizing the importance of conservative resection.
An in-depth understanding of the periorbital anatomy and corresponding sub-units is paramount when planning rejuvenation in this area [14,15,16]. As various rejuvenation techniques have been introduced over the last 3 decades and our understanding of periorbital anatomy and aging has evolved, we aim to highlight the important milestones in our understanding of periorbital aging and the anatomy and evolution of periorbital rejuvenation surgical techniques. The 100 most-cited articles on aesthetic periorbital surgery were identified and presented in chronological order to serve as a resource for surgeons and trainees. Current approaches to eyelid and eyebrow rejuvenation are also presented.
2. Methods
The Web of Science TM citation index was used to identify the 100 most-cited articles related to the topic of periorbital rejuvenation. Articles that were published in the English language from January 1989 to April 2020 were included in the study. The last 3 decades were selected as the timeframe of our study to ensure that the articles included were fundamental yet relevant to current periorbital surgical techniques. The terms “lower blepharoplasty”, “upper blepharoplasty”, “browlift”, “browplasty”, “endobrow lift”, “endoscopic brow”, “Foreheadplasty”, “lower eyelid anatomy”, “upper eyelid anatomy”, “forehead lift”, “eyelid rejuvenation”, “canthopexy”, “canthoplasty”, “eyelid fat pad”, “orbital fat pad”, “tear trough”, and “eyelid bags” were used in the citation search. The Web of Science Core Collection database was used in the search. A manual review of the initial 159 studies identified was performed. Articles that described non-invasive techniques, injectable fillers, lasers, neurotoxins, or periorbital reconstructive surgery were excluded. Articles describing periorbital rejuvenation-related surgical techniques, facial aging, and anatomy were included. After identifying the articles meeting the inclusion criteria, the top 100 were chosen to be highlighted in this article (Figure 1). In addition to citation count, the articles were further categorized by publication year, publishing journal, corresponding author’s primary specialty, focus of article, corresponding author’s country of residence, type of study, and level of evidence. The level of evidence was determined based on the methods described by Sullivan et al. [17].
Figure 1.
Methods flow chart. Abbreviations: WoS = Web of Science.
3. Results
The initial search was limited to 159 articles. Then, the abstracts of the most-cited 159 articles were individually reviewed. The 100 most-cited articles on periorbital rejuvenation are listed in this study (Table 1). The 100 most-cited articles were published between 1989 and 2020, spanning a 30-year period. The mean number of citations per article was 75 (standard deviation—SD: 42). There was a higher prevalence of articles published between 1989 and 1999 (n = 53) than later decades (Figure 2). Most articles (81%) were published in plastic surgery journals, of which 78% were published in the Plastic and Reconstructive Surgery Journal (n = 63) and originated from the United States (n = 82, 82%) (Figure 3 and Figure 4). Plastic and reconstructive surgery was the primary specialty of the corresponding authors in 71% of articles (n = 71), followed by oculoplastic surgery (n = 22) (Figure 5).
Table 1.
Details of the 100 Most-Cited Articles.
| Rank | Corresponding Author | Title | Year | Journal | Citations | Author’s Specialty | Country | Focus of Article | Study Type | Level of Evidence |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Pessa, J.E. [21] | The fat compartments of the face: anatomy and clinical implications for cosmetic surgery | 2007 | Plast. Reconst. Surg. | 333 | PRS | USA | Anatomy | Basic science | |
| 2 | Hamra, S.T. [22] | Arcus marginalis release and orbital fat preservation in midface rejuvenation | 1995 | Plast. Reconst. Surg. | 224 | PRS | USA | Technique | Clinical | IV |
| 3 | Lambros, V. [23] | Observations on periorbital and midface aging | 2007 | Plast. Reconst. Surg. | 204 | PRS | USA | Aging | Clinical | IV |
| 4 | Knize, D.M. [24] | An anatomically based study of the mechanism of eyebrow ptosis | 1996 | Plast. Reconst. Surg. | 175 | PRS | USA | Anatomy | Basic science | |
| 5 | Isse, N.G. [25] | Endoscopic facial rejuvenation—endoforehead, the functional lift—case-reports | 1994 | Aesthetic Plast. Surg. | 166 | PRS | USA | Technique | Clinical | V |
| 6 | Hester, T.R. [26] | Evolution of technique of the direct transblepharoplasty approach for the correction of lower lid and midfacial aging: maximizing results and minimizing complications in a 5-year experience | 2000 | Plast. Reconst. Surg. | 128 | PRS | USA | Technique | Clinical | IV |
| 7 | Hamra, S.T. [27] | The zygorbicular dissection in composite rhytidectomy: an ideal midface plane | 1998 | Plast. Reconst. Surg. | 128 | PRS | USA | Technique | Clinical | V |
| 8 | Mendelson, B.C. [16] | Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus | 2002 | Plast. Reconst. Surg. | 127 | PRS | Australia | Anatomy | Basic science | |
| 9 | Hykin, P.G. [18] | Age-related morphological changes in lid margin and meibomian gland anatomy | 1992 | Cornea | 121 | OPHT | UK | Aging | Clinical | II |
| 10 | Ramirez, O.M. [28] | Endoscopic techniques in facial rejuvenation—an overview .1. | 1994 | Aesthetic Plast. Surg. | 120 | PRS | USA | Technique | Review | |
| 11 | Baylis, H.I. [29] | Transconjunctival lower eyelid blepharoplasty—technique and complications | 1989 | Ophthalmology | 114 | OPHT | USA | Technique | Clinical | IV |
| 12 | Hamra, S.T. [30] | The role of orbital fat preservation in facial aesthetic surgery—a new concept | 1996 | Clinic in Plast. Surg. | 113 | PRS | USA | Technique | Clinical | V |
| 13 | Goldberg, R.A. [31] | Transconjunctival orbital fat repositioning: transposition of orbital fat pedicles into a subperiosteal pocket | 2000 | Plast. Reconst. Surg. | 111 | OPHT | USA | Technique | Clinical | IV |
| 14 | Jeong, S. [32] | The Asian upper eyelid—an anatomical study with comparison to the Caucasian eyelid | 1999 | Arch. Opthalmol. | 102 | OPHT | South Korea | Anatomy | Basic science | |
| 15 | Codner, M.A. [33] | Primary transcutaneous lower blepharoplasty with routine lateral canthal support: a comprehensive 10-year review | 2008 | Plast. Reconst. Surg. | 99 | PRS | USA | Technique | Clinical | IV |
| 16 | Pessa, J.E. [34] | Changes in ocular globe-to-orbital rim position with age: implications for aesthetic blepharoplasty of the lower eyelids | 1999 | Aesthetic Plast. Surg. | 99 | PRS | USA | Aging | Clinical | IV |
| 17 | Vasconez, L.O. [35] | Endoscopic techniques in coronal brow lifting | 1994 | Plast. Reconst. Surg. | 97 | PRS | USA | Technique | Clinical | IV |
| 18 | Fagien, S. [36] | Algorithm for canthoplasty: the lateral retinacular suspension: a simplified suture canthopexy | 1999 | Plast. Reconst. Surg. | 95 | OPHT | USA | Technique | Review | |
| 19 | Van Den Bosch, W.A. [37] | Topographic anatomy of the eyelids, and the effects of sex and age | 1999 | Br . J . Ophthalmol. | 94 | OPHT | Netherlands | Anatomy | Clinical | IV |
| 20 | Patipa, M. [38] | The evaluation and management of lower eyelid retraction following cosmetic surgery | 2000 | Plast. Reconst. Surg | 89 | OPHT | USA | Technique | Review | |
| 21 | Kikkawa, D.O. [39] | Relations of the superficial musculoaponeurotic system to the orbit and characterization of the orbitomalar ligament | 1996 | Ophthalmic Plast. Reconst. Surg. | 89 | OPHT | USA | Aging | Basic Science | |
| 22 | Jelks, G.W. [40] | The inferior retinacular lateral canthoplasty: a new technique | 1997 | Plast. Reconst. Surg. | 88 | PRS | USA | Technique | Clinical | V |
| 23 | Rohrich, R.J. [41] | The anatomy of suborbicularis fat: implications for periorbital rejuvenation | 2009 | Plast. Reconst. Surg. | 86 | PRS | USA | Anatomy | Basic Science | |
| 24 | Little, J.W. [42] | Three-dimensional rejuvenation of the midface: volumetric resculpture by malar imbrication | 2000 | Plast. Reconst. Surg. | 86 | PRS | USA | Technique | Clinical | IV |
| 25 | Hamra, S.T. [43] | Repositioning the orbicularis oculi muscle in the composite rhytidectomy | 1992 | Plast Reconst Surg | 86 | PRS | USA | Technique | Review | |
| 26 | Gunter, J.P. [44] | Aesthetic analysis of the eyebrows | 1997 | Plast Reconst Surg | 85 | PRS | USA | Anatomy | Clinical | IV |
| 27 | Flowers, R.S. [45] | Canthopexy as a routine blepharoplasty component | 1993 | Clin. Plast. Surg. | 84 | PRS | USA | Technique | Review | |
| 28 | Mullins, J.B. [46] | Complications of the transconjunctival approach—a review of 400 cases | 1997 | Arch. Otoloaryngol.-H N Surg. | 82 | ENT | USA | Technique | Clinical | IV |
| 29 | Aiache, A.E. [47] | The suborbicularis oculi fat pads—an anatomic and clinical-study | 1995 | Plast. Reconst. Surg. | 82 | PRS | USA | Technique | Clinical | V |
| 30 | McKinney, P. [48] | Criteria for the forehead lift | 1991 | Aesthetic Plast. Surg. | 82 | PRS | USA | Technique | Clinical | IV |
| 31 | Rohrich, R.J. [49] | Current concepts in aesthetic upper blepharoplasty | 2004 | Plast. Reconst. Surg. | 78 | PRS | USA | Technique | Review | |
| 32 | Thorne, C.H. [50] | The tear trough and lid/cheek junction: anatomy and implications for surgical correction | 2009 | Plast. Reconst. Surg. | 77 | PRS | USA | Anatomy | Basic Science | |
| 33 | Richard, M.J. [51] | Analysis of the anatomic changes of the aging facial skeleton using computer-assisted tomography | 2009 | Ophthalmic Plast. Reconst. Surg. | 75 | OPHT | USA | Aging | Clinical | IV |
| 34 | Knize, D.M. [52] | Transpalpebral approach to the corrugator supercilii and procerus muscles | 1995 | Plast. Reconst. Surg. | 74 | PRS | USA | Technique | Clinical | IV |
| 35 | Barton, F.E. [53] | Fat extrusion and septal reset in patients with the tear trough triad: a critical appraisal | 2004 | Plast. Reconst. Surg. | 73 | PRS | USA | Technique | Clinical | IV |
| 36 | McCord, C.D. [54] | Redraping the inferior orbicularis arc | 1998 | Plast. Reconst. Surg. | 73 | OPHT | USA | Technique | Review | |
| 37 | Wong, C.-H. [55] | The tear trough ligament: anatomical basis for the tear trough deformity | 2012 | Plast. Reconst. Surg. | 71 | PRS | Singapore | Anatomy | Basic Science | |
| 38 | Zarem, H.A. [56] | Expanded applications for transconjunctival lower lid blepharoplasty | 1991 | Plast. Reconst. Surg. | 70 | PRS | USA | Technique | Review | |
| 39 | Meyer, D.R. [57] | Anatomy of the orbital septum and associated eyelid connective tissues—implications for ptosis surgery | 1991 | Ophthalmic Plast. Reconst. Surg. | 70 | OPHT | USA | Anatomy | Basic Science | |
| 40 | McCord, C.D. [58] | Browplasty and browpexy—an adjunct to blepharoplasty | 1990 | Plast. Reconst. Surg. | 70 | OPHT | USA | Technique | Clinical | V |
| 41 | Goldberg, R.A. [59] | What causes eyelid bags? analysis of 114 consecutive patients | 2005 | Plast Reconst Surg. | 69 | OPHT | USA | Anatomy | Clinical | IV |
| 42 | Hass, A.N. [60] | Incidence of post-blepharoplasty orbital hemorrhage and associated visual loss | 2004 | Ophthalmic Plast. Reconst. Surg. | 68 | OPHT | USA | Technique | Clinical | IV |
| 43 | Hamra, S.T. [61] | The role of the septal reset in creating a youthful eyelid-cheek complex in facial rejuvenation | 2004 | Plast . Reconst . Surg .. | 68 | PRS | USA | Technique | Review | |
| 44 | Fagien, S. [62] | Advanced rejuvenative upper blepharoplasty: enhancing aesthetics of the upper periorbita | 2002 | Plast. Reconst. Surg. | 67 | OPHT | USA | Technique | Review | |
| 45 | Knize, D.M. [63] | Limited-incision forehead lift for eyebrow elevation to enhance upper blepharoplasty | 1996 | Plast. Reconst. Surg. | 67 | PRS | USA | Technique | Clinical | IV |
| 46 | Ramirez, O.M. [64] | Three-dimensional endoscopic midface enhancement: A personal quest for the ideal cheek rejuvenation | 2002 | Plast. Reconst. Surg. | 66 | PRS | USA | Technique | Clinical | IV |
| 47 | Mendelson, B.C. [65] | Surgical anatomy of the midcheek: Facial layers, spaces, and the midcheek segments | 2008 | Clin. in Plast. Surg. | 64 | PRS | Australia | Anatomy | Review | |
| 48 | Park, D.H. [66] | Anthropometry of Asian eyelids by age | 2008 | Plast. Reconst. Surg. | 63 | PRS | South Korea | Aging | Clinical | IV |
| 49 | Freund, R.M. [67] | Correlation between brow lift outcomes and aesthetic ideals for eyebrow height and shape in females | 1996 | Plast. Reconst. Surg. | 63 | PRS | USA | Technique | Clinical | IV |
| 50 | Baker, D.C. [19] | Endoscopic brow lift: a retrospective review of 628 consecutive cases over 5 years | 2003 | Plast. Reconst. Surg. | 62 | PRS | USA | Technique | Clinical | III |
| 51 | Byrd, H.S. [68] | The deep temporal lift: a multiplanar, lateral brow, temporal, and upper face lift | 1996 | Plast. Reconst. Surg. | 61 | PRS | USA | Technique | Basic science | |
| 52 | McGraw, B.L. [69] | Post-blepharoplasty ectropion—prevention and management | 1991 | Arch Otoloaryngol. H N Surg. | 61 | ENT | Canada | Technique | Clinical | IV |
| 53 | Janis, J.E. [70] | Anatomy of the corrugator supercilii muscle: part i. corrugator topography | 2007 | Plast. Reconst. Surg. | 60 | PRS | USA | Anatomy | Basic Science | |
| 54 | Trepsat, F. [71] | Periorbital rejuvenation combining fat grafting and blepharoplasties | 2003 | Aesthetic Plast. Surg. | 60 | PRS | Switzerland | Technique | Review | |
| 55 | Daniel, R.K. [72] | Endoscopic forehead lift: an operative technique | 1996 | Plast. Reconst. Surg. | 60 | PRS | USA | Technique | Clinical | IV |
| 56 | Carraway, J.H. [73] | The prevention and treatment of lower lid ectropion following blepharoplasty | 1990 | Plast. Reconst. Surg. | 60 | PRS | USA | Technique | Review | |
| 57 | McCord, C.D. [74] | Lateral canthal anchoring | 2003 | Plast. Reconst. Surg. | 59 | OPHT | USA | Technique | Review | |
| 58 | Rohrich, R.J. [75] | Evolving fixation methods in endoscopically assisted forehead rejuvenation: controversies and rationale | 1997 | Plast. Reconst. Surg. | 59 | PRS | USA | Technique | Review | |
| 59 | Jones, B.M. [76] | Endoscopic brow lift: a personal review of 538 patients and comparison of fixation techniques | 2004 | Plast. Reconst. Surg. | 58 | PRS | UK | Technique | Clinical | IV |
| 60 | May, J.W. [77] | Retro-orbicularis oculus fat (roof) resection in aesthetic blepharoplasty—a 6-year study in 63 patients | 1990 | Plast. Reconst. Surg. | 58 | PRS | USA | Technique | Clinical | IV |
| 61 | Lisman, R.D. [78] | Blepharoplasty complications | 2010 | Plast. Reconst. Surg. | 57 | OPHT | USA | Technique | Review | |
| 62 | Elkwood, A. [79] | National plastic surgery survey: brow lifting techniques and complications | 2001 | Plast. Reconst. Surg. | 57 | PRS | USA | Technique | Review | |
| 63 | Paul, M.D. [80] | The evolution of the brow lift in aesthetic plastic surgery | 2001 | Plast. Reconst. Surg. | 57 | PRS | USA | Technique | Review | |
| 64 | Hamra, S.T. [81] | Frequent face lift sequelae: hollow eyes and the lateral sweep: cause and repair | 1998 | Plast. Reconst. Surg. | 56 | PRS | USA | Technique | Review | |
| 65 | Loeb, R. [82] | Naso-jugal groove leveling with fat tissue | 1993 | Clin. Plast. Surg. | 56 | PRS | Brazil | Technique | Review | |
| 66 | Connell, B.F. [83] | The forehead lift—techniques to avoid complications and produce optimal results | 1989 | Aesthetic Plast. Surg. | 56 | PRS | USA | Technique | Review | |
| 67 | Rohrich, R.J. [84] | The five-step lower blepharoplasty: blending the eyelid-cheek junction | 2011 | Plast. Reconst. Surg. | 55 | PRS | USA | Technique | Clinical | IV |
| 68 | Flowers, R.S. [85] | Upper blepharoplasty by eyelid invagination—anchor blepharoplasty | 1993 | Clin. Plast. Surg. | 55 | PRS | USA | Technique | Clinical | V |
| 69 | Wong, C.H. [86] | Facial soft-tissue spaces and retaining ligaments of the midcheek: defining the premaxillary space | 2013 | Plast. Reconst. Surg. | 53 | PRS | Singapore | Anatomy | Basic Science | |
| 70 | Jelks, G.W. [87] | Evolution of the lateral canthoplasty: techniques and indications | 1997 | Plast. Reconst. Surg. | 53 | PRS | USA | Technique | Clinical | IV |
| 71 | Goldberg, R.A. [88] | Eyelid anatomy revisited—dynamic high-resolution magnetic-resonance images of whitnall ligament and upper eyelid structures with the use of a surface coil | 1992 | Arch . Opthalmo l. | 53 | PRS | USA | Anatomy | Clinical | IV |
| 72 | Yaremchuk, M.J. [89] | Changes in eyebrow position and shape with aging | 2009 | Plast. Reconst. Surg. | 52 | PRS | USA | Aging | Clinical | IV |
| 73 | Lambros, V. [90] | Models of facial aging and implications for treatment | 2008 | Clin. Plast. Surg. | 52 | PRS | USA | Aging | Review | |
| 74 | Nahai, F. [91] | Transconjunctival blepharoplasty for upper and lower eyelids | 2010 | Plast. Reconst. Surg. | 51 | PRS | USA | Technique | Clinical | IV |
| 75 | Tyers, A.G. [92] | The direct brow lift: efficacy, complications, and patient satisfaction | 2004 | Br. J. Ophthalmol. | 51 | OPHT | UK | Technique | Clinical | IV |
| 76 | Patel, B.C.K. [93] | Management of post-blepharoplasty lower eyelid retraction with hard palate grafts and lateral tarsal strip | 1997 | Plast. Reconst. Surg. | 51 | OPHT | USA | Technique | Clinical | IV |
| 77 | Pessa, J.E. [94] | The orbicularis retaining ligament of the medial orbit: closing the circle | 2008 | Plast. Reconst. Surg. | 50 | PRS | USA | Anatomy | Basic Science | |
| 78 | Kawamoto, H.K. [95] | The tear “trouf” procedure: transconjunctival repositioning of orbital unipedicled fat | 2003 | Plast. Reconst. Surg. | 50 | PRS | USA | Technique | Clinical | IV |
| 79 | Ramirez, O.M. [96] | Endoscopically assisted biplanar forehead lift | 1995 | Plast. Reconst. Surg. | 50 | PRS | USA | Technique | Clinical | IV |
| 80 | Troilius, C. [97] | Subperiosteal brow lifts without fixation | 2004 | Plast. Reconst. Surg. | 49 | PRS | Sweden | Technique | Clinical | II |
| 81 | Furnas, D.W. [98] | Festoons, mounds, and bags of the eyelids and cheek | 1993 | Clin. Plast. Surg. | 49 | PRS | USA | Anatomy | Review | |
| 82 | Shore, J.W. [99] | Operative complications of the transconjunctival inferior fornix approach | 1991 | Ophthalmology | 49 | OPHT | USA | Technique | Clinical | V |
| 83 | De la Plaza, R. [100] | Supraperiosteal lifting of the upper 2/3 of the face | 1991 | Br. J. Plast. Surg. | 49 | PRS | Spain | Technique | Clinical | IV |
| 84 | De la Torre, J. [101] | Endoscopic forehead lift: review of technique, cases, and complications | 2002 | Plast. Reconst. Surg. | 48 | PRS | USA | Technique | Clinical | IV |
| 85 | Chung, K.Y. [102] | Infraorbital dark circles: definition, causes, and treatment options | 2009 | Derm. Surg. | 47 | Dermatology | South Korea | Technique | Review | |
| 86 | Moy, R.L. [103] | Objective changes in brow position, superior palpebral crease, peak angle of the eyebrow, and jowl surface area after volumetric radiofrequency treatments to half of the face | 2004 | Derm. Surg. | 47 | Dermatology | USA | Technique | Clinical | IV |
| 87 | Isse, N.G. [104] | Endoscopic forehead lift—evolution and update | 1995 | Clin. Plast. Surg. | 47 | PRS | USA | Technique | Clinical | IV |
| 88 | Hamra, S.T. [105] | A study of the long-term effect of malar fat repositioning in face lift surgery: short-term success but long-term failure | 2002 | Plast. Reconst. Surg. | 45 | PRS | USA | Technique | Clinical | IV |
| 89 | Starck, W.J. [106] | Objective evaluation of the eyelids and eyebrows after blepharoplasty | 1996 | J. Oral Maxillofac. Surg. | 45 | OMS | USA | Technique | Clinical | IV |
| 90 | Cook, T.A. [107] | The versatile midforehead lift | 1989 | Arch. Otoloaryngol. H N Surg. | 45 | ENT | USA | Technique | Clinical | IV |
| 91 | Knize, D.M. [108] | Anatomic concepts for brow lift procedures | 2009 | Plast. Reconst. Surg. | 44 | PRS | USA | Anatomy | Review | |
| 92 | Core, G.B. [109] | Endoscopic browlift | 1995 | Clin. Plast. Surg. | 44 | PRS | USA | Technique | Review | |
| 93 | Rudkin, G.H. [110] | Magnetic resonance imaging characterization of orbital changes with age and associated contributions to lower eyelid prominence | 2008 | Plast. Reconst. Surg. | 43 | PRS | USA | Aging | Clinical | IV |
| 94 | Carter, S.R. [20] | The Asian lower eyelid: A comparative anatomic study using high-resolution magnetic resonance imaging | 1998 | Ophthalmic Plast. Reconst. Surg. | 43 | OPHT | USA | Anatomy | Clinical | III |
| 95 | Kakizaki, H. [111] | Lower eyelid anatomy An update | 2009 | Ann. Plast. Surg. | 42 | OPHT | Japan | Anatomy | Review | |
| 96 | Paul, M.D. [112] | The evolution of the midface lift in aesthetic plastic surgery | 2006 | Plast. Reconst. Surg. | 42 | PRS | USA | Technique | Review | |
| 97 | Pessa, J.E. [113] | The malar septum: The anatomic basis of malar mounds and malar edema. | 1997 | Aesthetic Surg. J. | 42 | PRS | USA | Anatomy | Basic Science | |
| 98 | Ramirez, O.M. [114] | The anchor subperiosteal forehead lift | 1995 | Plast. Reconst. Surg. | 42 | PRS | USA | Technique | Clinical | IV |
| 99 | Guyuron, B. [115] | Corrugator supercilii muscle resection through blepharolplasty Incision | 1995 | Plast. Reconst. Surg. | 42 | PRS | USA | Technique | Clinical | IV |
| 100 | Kakizaki, H. [116] | Upper eyelid anatomy An update | 2009 | Ann. Plast. Surg. | 41 | OPHT | Japan | Anatomy | Review |
Abbreviations: PRS = plastic and reconstructive surgery; OPHT = ophthalmology; OMS = oral and maxillofacial surgery; ENT = ear, nose, and throat.
Figure 2.
Categorization of the 100 most-cited articles by their publication decade.
Figure 3.
Categorization of the 100 most-cited articles by journal of publication. Abbreviations: Plast = plastic; Reconst = reconstructive; Surg = surgery, Derm = dermatologic; Br = British; J = journal.
Figure 4.
Categorization of the 100 most-cited articles by country of residence of the corresponding author.
Figure 5.
Categorization of the 100 most-cited articles by surgical specialty of the corresponding author.
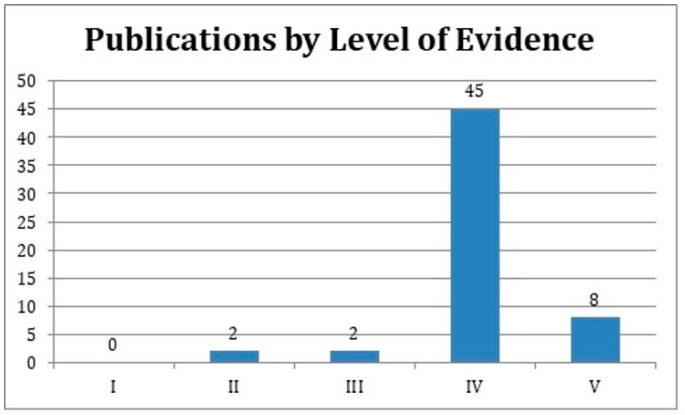
Of the 100 articles, 69 described surgical techniques, followed by anatomy (n = 22) and aging (n = 9). Clinical studies encompassed 57% of the top 100 most-cited articles, followed by review articles (n = 29) and basic science studies (n = 14). Clinical articles were classified according to their Level of Evidence. None of the studies provided level I evidence. Two studies [18] qualified as providing level II evidence, and two articles [19,20] provided level III evidence. Of the remaining 57 most-cited clinical studies, 45 studies (79%) provided level IV and 8 provided level V evidence (14%) (Figure 6).
Figure 6.
The levels of evidence of publications classified as clinical studies.
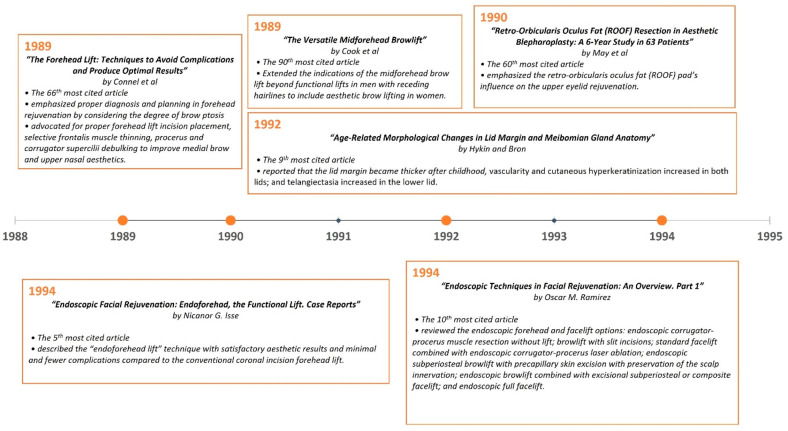
A timeline of the articles was created to better visualize the evolution of periorbital rejuvenation surgery techniques (Figure 7, Figure 8, Figure 9, Figure 10, Figure 11 and Figure 12). The most clinically relevant articles within each 5-year period are featured in the timeline.
Figure 7.
Most impactful articles from 1989 to 1994.
Figure 8.
Most impactful articles from 1995 to 1999.
Figure 9.
Most impactful articles from 2000 to 2004.
Figure 10.
Most impactful articles from 2005 to 2009.
Figure 11.
Most impactful articles from 2010 to 2020.
Figure 12.
Summative timeline of the most impactful articles on the topic of periorbital rejuvenation from 1989 through 2020.
4. Discussion
Facial aging is a result of changes in the five lamellar structures of the face and the underlying facial bony skeleton. Throughout life, there is apparent descent, atrophy, or hypertrophy of certain compartments within the face that make it appear more aged [23,34,117]. Aging is manifested in the lateral translation of the orbits, glabellar protrusion, the expansion of the supraorbital ridges, the deepening and lateral expansion of the cheeks, the three-dimensional enlargement of the nose, and an increase in chin prominence, as described by Enlow [118] and Mendelson and Wong [119]. The interplay between the bony skeleton, supporting ligaments, fat compartments, and facial mimetic muscles is influenced by physiological, genetic, and environmental factors [120]. These factors involve bone remodeling and functional effects of the surrounding muscles’ action (i.e., the effects of chronic orbicularis oculi contraction on lateral brow position). The youthful eye is characterized by an almond-shaped palpebral fissure with a slight upward slope from the medial to lateral canthus. Concerning periorbital aging, Lambros [23,121] noted “the eyes seem to get smaller as one ages, the entire lid aperture gets smaller because the lower lid rises, the upper lid falls, the lid gets shorter from the side, and the fat pads enlarge” [26,122]. Therefore, surgeons treating periorbital aging should consider all of these structures and the accompanying changes to achieve optimal rejuvenation. The improvement in the anatomical understanding of periorbital structures over the last 3 decades has contributed to a better understanding of the aging process and has enhanced the surgical strategies used to achieve more youthful and attractive eyes [10,21,47,55,117,123,124,125,126].
4.1. Evolution of Periorbital Rejuvenation over the Last 3 Decades
Periorbital rejuvenation has evolved to include a multitude of approaches to addressing aging-related changes of the orbit such as skin excision, SMAS re-draping, orbicularis oculi muscle repositioning, fat pad reduction or transposition, the release of the orbicularis-retaining ligament (ORL), and micro/nano fat grafting [26,31,43,47,127]. A comprehensive approach to upper eyelid rejuvenation includes the brow and forehead. Similarly, for lower lid rejuvenation, the midface is involved [128].
In 1989, Cook et al. [107] reported their experience in extending the indications of the midforehead brow lift beyond functional lifts in men with receding hairlines to include aesthetic brow lifting in women. The authors described their surgical technique, which included staggering midforehead elliptical excisions, the undermining of the inferior forehead skin, and the placement of suspension sutures in the mid and lateral brow. Good results among 52 female patients were reported. This study was ranked 90th among the top 100 most-cited articles. In the same year, Connell et al. [83] reported their approach to forehead lifting and emphasized proper diagnosis and planning with respect to forehead rejuvenation by considering the degree of brow ptosis associated with the upper eyelid skin’s laxity. They advocated for the proper placement of forehead lift incisions, selective frontalis muscle thinning, and procerus and corrugator supercilii debulking to improve medial brow and upper nasal aesthetics. In 1994, Isse [25] described his endoscopic “endoforehead lift” technique in a total of 61 cases, and his article became the 5th most-cited article. The author reported that he was able to achieve satisfactory cosmetic results with minimal and fewer complications when compared to the conventional coronal incision forehead lift. That same year, Ramirez [28] reviewed different endoscopic forehead and facelift options (the 10th most-cited article). These included endoscopic corrugator-procerus muscle resection without a lift, a browlift with slit incisions, a standard facelift combined with endoscopic corrugator-procerus laser ablation, an endoscopic subperiosteal browlift with precapillary skin excision and the preservation of the scalp’s innervation, an endoscopic browlift combined with an excisional subperiosteal or composite facelift, and an endoscopic full facelift. In 1996, Knize [63] described his limited-incision forehead lift technique to achieve eyebrow elevation for an enhanced upper blepharoplasty. In this technique, the author used temporal scalp incisions of only 4.5 to 5 cm in length while also performing a transpalpebral resection of the corrugator supercilii muscles and a transection of the procerus muscle. This created a more acceptable aesthetic result compared to the coronal scalp incision, thus minimizing the risk of injuring the supraorbital nerve branches and being comparable to the endoscopic techniques in this regard. This article has become the 45th most-cited article related to periorbital rejuvenation. By the early 2000s, the endoscopic brow/forehead lift had gained significant popularity [19,35,75,76]. In 2004, Jones and Grover [76] reported their experience with 538 endoscopic brow lift cases and compared the outcomes of two different fixation techniques: fibrin glue versus polydioxanone sutures tied through bone tunnels. The authors found that the endoscopic brow lift provided a significant increase in the pupil to brow height while fixation with polydioxanone sutures tied through bone tunnels produced a significantly more stable result than fibrin glue.
In 1995, Hamra [22] described arcus marginalis release and the advancement of lower eyelid fat as an alternative to its excision to avoid the resulting hollow contour deformity, which is now synonymous with “the operated appearance”. In his study of 152 cases, which is the second most-cited article, Hamra reported satisfactory results with a minimal rate of complication. In 2000, Goldberg [31] described the transposition of orbital fat pedicles into a subperiosteal pocket through a transconjunctival approach. That same year, Hester et al. [26] published a retrospective review of 757 patients who underwent direct trans-lower eyelid blepharoplasty to correct midfacial aging. In this sixth most-cited paper (n = 128), the authors described a sub-periosteal approach to the lower eyelid and midface as opposed to traditional lateral vector techniques. Two years later, Muzaffar et al. [16] described the ORL, which became an important structure to release while performing orbicularis oculi suspension (re-draping) and canthopexy. In 2012, Mendelson et al. [55] described the tear trough ligament, a true osteocutaneous ligament, and its contribution to tear trough (nasojugal groove) deformity due to the ligament’s tethering effect. The authors proposed a complete release of this ligament, especially in patients with moderate to severe deformity.
As a topic of continued debate, it is also worth discussing the popularity and preference for the transcutaneous and transconjunctival approaches to lower blepharoplasty. Both techniques have been represented in the top 100 cited article list but there was a greater number of articles advocating the transconjunctival approach (n = 5 versus n = 1). In their study in 2008, Codner et al. [33] reviewed their experience with primary lower transcutaneous blepharoplasty via a subciliary skin incision in 264 patients over 10 years, which was the 15th most-cited article included in our study. The authors reported that nine (3.5%) patients had eyelid malposition that required operative correction while one (0.4%) patient had an orbital hematoma. They concluded that lateral canthal support should be considered a routine component of lower transcutaneous blepharoplasty. In 2010, Pacella et al. [91] reviewed the anatomy, indications, and outcomes of lower transconjunctival blepharoplasty in their article (the 74th most-cited article). In their senior author’s personal experience (Dr. Foad Nahai) with 300 lower lid blepharoplasties between 1992 and 1995, the complication rate for the transconjunctival group was 5% (6 out of 120 patients) versus 13% (24 out of 180 patients) for the transcutaneous group. In the transconjunctival group, there was no lid retraction, which was a complication experienced by 3.3% (n = 6) in the transcutaneous group. The authors concluded that the transconjunctival lower blepharoplasty was a safe and effective procedure for periorbital rejuvenation. They also noted that in cases of excessive skin laxity, a transcutaneous approach compared to the transconjunctival blepharoplasty may achieve better results with the addition of lateral canthoplasty and/or lateral canthal anchoring procedure to minimize the risk of lower-lid malposition. The importance of the proper assessment and diagnosis of factors that may contribute to lower-lid malposition was highlighted by Jelks et al. [40,87,129]. As such, lateral canthoplasty for managing potential lower-lid malposition after blepharoplasty has become routine practice in contemporary lower blepharoplasty.
As emphasized in this article, the studies on facial aging and anatomy have impacted periorbital rejuvenation strategies significantly. In 1992, Hykin and Bron [18] studied the age-related changes in the eyelid margin in 80 subjects, and this article has become the ninth most-cited article (n = 121). In the study, it was reported that with aging, the lid margin became thicker after childhood, lid margin vascularity and cutaneous hyperkeratinization increased in both lids, and telangiectasia increased in the lower lid. The description of suborbicularis orbital fat (SOOF) by Aiache and Ramirez [47] in 1995 also influenced the correction strategies for deformities in the lower eyelids, just as retroorbicularis oculus fat (ROOF) influenced the upper eyelid rejuvenation technique pioneered by Owsley [130] and May [77]. In the following year, Knize’s [24] anatomical study on 20 (40 half-head) fresh cadavers was published and has since become the 4th most-cited article (n = 175). The author reported that eyebrow ptosis occurs more profoundly on the brow’s lateral segment, and this was promoted by the changes in the galeal fat pad, the preseptal fat pad, and the subgaleal fat pad glide plane space. In addition, he described the impact of the dynamic interactions between the frontalis muscle’s resting tone and gravity, and the corrugator supercilii and the lateral orbicularis oculi muscles’ hyperactivity on lateral eyebrow position. In 2007, the cadaveric study by Rohrich and Pessa [21] described the subcutaneous fat pad compartments, constituting another important contribution to a more in-depth understanding of facial anatomy. This is the most-cited article of the articles related to periorbital rejuvenation within the last 3 decades. Another important publication that impacted rejuvenation strategies was Lambros’ [23] observational study published in the same year, which has become the third most-cited article (n = 204). He compared the 10- to 50-year-old photographs of 130 subjects with their recently taken follow-up photographs to assess the effects of aging on the face. The interesting findings from this study included the lateral movement of the arc peak, the apparent decrease in eye size, and the relative stability of the position of the lid–cheek junction over time.
Although not the subject of this article, injectables play an important role in modern periorbital rejuvenation. In 1981, bovine collagen became the first agent that was approved for cosmetic injection by the FDA [131]. The introduction of hyaluronic acid in 2003 initiated a new era for non-surgical peri-orbital and facial rejuvenation. According to statistics released by the American Society of Plastic Surgeons (ASPS), 79.5% of 2,676,970 soft tissue filler procedures performed in 2018 used hyaluronic acid fillers [132]. These fillers are currently used widely by a multitude of practitioners across multiple specialties with satisfactory aesthetic results; however, their relatively short-lived effect is the main drawback compared to these surgical techniques. Another important factor, which is not accounted for in the cited articles but impacts eyelid and brow rejuvenation trends nonetheless, is society’s evolving perception of beauty in each era and the influence of pop culture and social media on such trends. What Westmore postulated as the ideal female brow position in the 1980s has now been replaced by the more lateral position of the brow’s peak closer to the lateral canthus [133].
As we have summarized, the current surgical techniques of periorbital rejuvenation have evolved as our understanding of facial has anatomy progressed. More conservative fat and muscle excisions with which to prevent the “operated” appearance and post-operative complications dominate our current approaches to peri-orbital rejuvenation [49]. Twenty-one percent of the one hundred most-cited articles within the last 31 years focused on periorbital anatomy and its clinical relevance to periorbital aesthetic surgery. This list of articles offers a comprehensive compilation of studies to readers interested in advancing their knowledge of periorbital rejuvenation.
This study is not without limitations. There is potential for citation bias contributing to the citation rankings in this study. Authors may tend to select references that support their conclusions [134]. Self-citation can also play a role in citation bias [135]. Furthermore, the number of citations in the last decade remained the lowest among the 3 decades reported (Figure 2). This does not mean that these articles were of lesser importance or had a lower impact on practice changes; rather, it reflects the time factor required for these articles to be cited. Lastly, as more articles on the same topic are published, the authors have a larger pool of references from which to cite, thus generating a dilution effect concerning the articles published in later years compared to the older citations.
4.2. Current Approaches to Brow and Eyelid Rejuvenation
There are three surgical approaches to browlift: trans-blepharoplasty brow lift, direct brow lift, and trans-forehead brow/forehead lift. The latter two have the longest-lasting effect [136]. Direct browlifts are most often used in patients with brow ptosis due to a nerve injury, such as those with Bell’s Palsy, but they are also good options for men with a receded hairline and women who desire only a lateral brow lift [137]. It is the most predictable method for browlift, as the incision is placed just above the superior end of the brow or along a rhytid near the brow. In addition, the degree of lift one can expect post-operatively is proportional to the amount of tissue removed [138]. However, scars are a major concern with respect to direct brow lift and there is currently a move towards more minimally invasive approaches [136,139,140].
The endoscopic approach is another technique that was popular in the last 3 decades and may still be practiced by some surgeons. However, other techniques, such as the gliding brow lift, are gaining more popularity. The gliding brow lift can elevate the brow without raising the forehead’s height [141]. One advantage of this technique is that it requires only two 3 mm scalp incisions in the frontotemporal area. The surgeon undermines directly above the frontalis and galea down to 1 cm below the eyebrows. A plane of subcutaneous tissue is elevated and then sutured to the frontalis and galea via a hemostatic net to maintain brow elevation. As with any new technique, there are early, middle, and late adopters, resulting in a variable lag time between the introduction of a surgical technique and publications supporting its safety or efficacy. Figure 13 demonstrates a summary of the types of incisions used in the different types of browlift.
Figure 13.
Illustration demonstrating the different types of incisions used for browlift surgery.
Upper blepharoplasty is often combined with browlift surgery. Current methods of upper eyelid blepharoplasty are more conservative and refrain from the removal of the orbicularis oculi and excessive orbital fat resection to prevent a hollowed-out appearance. Modern lower blepharoplasty has shifted from fat resection to volume redistribution or augmentation through fat transposition or micro and nano fat grafting [142,143]. While these techniques may be more popular in current practice, citations supporting their use may underreport their popularity.
There are two main surgical approaches to lower blepharoplasty: a transcutaneous and transconjunctival approach. Based on questionnaires sent out to members of the American Society of Ophthalmic Plastic and Reconstructive Surgery who perform blepharoplasty, more surgeons use the transconjunctival approach [144]. Some advantages of the transconjunctival approach include the absence of scarring following surgery, decreased recurrence of lower-lid bulging, and the avoidance of complications such as vertical lid shortening [145]. Fat repositioning and canthal suspension were frequently performed along with lower blepharoplasty [144]. Regarding fat repositioning, the planes of dissection are subperiosteal, supraperiosteal, and intra-SOOF. The complication rates in these three planes are low when performed by experienced surgeons, but there is a high learning curve. Dissecting the supraperiosteal plane runs the risk of injuring the blood vessels, while using the subperiosteal plane does not allow for the release of the ORL, tear trough, and lid–cheek junction. To address this, a new approach using the midcheek spaces for orbital fat repositioning has been proposed, offering improvements in terms of lower-lid fat and herniated orbital fat and a decreased prominence of the lid–cheek junction [146]. Additionally, combining lower eyelid surgery with midface rejuvenation surgery can result in greater cosmetic outcomes, depending on the degree of lower eyelid skin laxity, midface descent, and midface volume [147].
While women accounted for 85% of blepharoplasty procedures in the United States, a transconjunctival approach is preferred in men undergoing lower blepharoplasty, as their primary concern was found to be the formation of the deep palpebromalar groove and tear-trough deformity [148,149]. A transconjunctival approach permits easy access to the periorbital fat compartments for fat excision.
5. Conclusions
Over the last 3 decades, periorbital rejuvenation techniques have evolved in tandem with our knowledge of periorbital anatomy and aging. Studies focusing on periorbital anatomy, aging, and surgical techniques were the most-cited publications. An anatomically based approach that is customized for each patient and accounts for age-related changes in the periorbital structures is paramount in contemporary periorbital rejuvenation.
Author Contributions
Conceptualization, B.A.S.; methodology, D.K., D.S.K. and B.A.S.; validation, D.K., C.-H.W. and B.A.S.; formal analysis, D.K., D.S.K. and B.A.S.; investigation, D.K., D.S.K. and B.A.S.; resources, D.K. and C.A.S.; data curation, D.K., D.S.K. and B.A.S.; writing—original draft preparation, D.K., C.-H.W. and B.A.S.; writing—review and editing, D.K. and C.A.S.; visualization, D.K. and C.A.S.; supervision, B.A.S.; project administration, B.A.S.; All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Financial Disclosure
None of the authors have financial interests in any of the products, devices, or drugs mentioned in this manuscript.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Lazzeri D., Agostini T., Figus M., Nardi M., Spinelli G., Pantaloni M., Lazzeri S. The Contribution of Aulus Cornelius Celsus (25 B.C.–50 A.D.) to Eyelid Surgery. Orbit. 2012;31:162–167. doi: 10.3109/01676830.2011.648816. [DOI] [PubMed] [Google Scholar]
- 2.Dupuis C., Rees T.D. Historical notes on blepharoplasty. Plast. Reconstr. Surg. 1971;47:246–251. doi: 10.1097/00006534-197103000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Pare A. The Workes of that Famous Chirurgion Ambrose Parey. Richard Cotes and Willi; London, UK: 1649. [Google Scholar]
- 4.Fuchs E. Veber Blepharochalasis (Erschlaffung der Lidhaut) Vien Klin Wchnschr; Berlin, Germany: 1896. pp. 109–110. [Google Scholar]
- 5.Bourguet J. Les hernies graisseuses de l’orbite. Notre traiternent chi· rurgical. Bull. Acad. Med. 1924;92:3. [Google Scholar]
- 6.Claoué C. Documents de Chirurgie Plastique Esthétique Compte Rendu. Des séances la Société Sci Esthétique; Paris, France: 1931. pp. 344–353. [Google Scholar]
- 7.Passot R. Chirurgie Esthetique Pure (Technique et Fesultate) Gast Doin &Cie; Baden, Germany: 1931. [Google Scholar]
- 8.Pierce G.W., Klabunde E.H., Bergeron V.L. Useful procedures in plastic surgery. Plast. Reconstr. Surg. 1947;2:358–361. doi: 10.1097/00006534-194707000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Bames H.O. Frown disfigurement and ptosis of eyebrows. Plast. Reconstr. Surg. 1957;19:337–340. doi: 10.1097/00006534-195704000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Castanares S. Blepharoplasty for herniated intraorbital fat; anatomical basis for a new approach. Plast. Reconstr. Surg. (1946) 1951;8:46–58. doi: 10.1097/00006534-195107000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Rees T.D. Technical aid in blepharoplasty. Plast. Reconstr. Surg. 1968;41:497–498. doi: 10.1097/00006534-196805000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Loeb R. Necessity for partial resection of the orbicularis oculi muscle in blepharoplasties in some young patients. Plast. Reconstr. Surg. 1977;60:176–178. doi: 10.1097/00006534-197708000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Furnas D.W. Festoons of orbicularis muscle as a cause of baggy eyelids. Plast. Reconstr. Surg. 1978;61:540–546. doi: 10.1097/00006534-197804000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Mendelson B.C. Surgery of the superficial musculoaponeurotic system: Principles of release, vectors, and fixation. Plast. Reconstr. Surg. 2002;109:824–825. doi: 10.1097/00006534-200202000-00077. [DOI] [PubMed] [Google Scholar]
- 15.Moss C.J., Mendelson B.C., Taylor G.I. Surgical anatomy of the ligamentous attachments in the temple and periorbital regions. Plast. Reconstr. Surg. 2000;105:1475–1490. doi: 10.1097/00006534-200004000-00035. [DOI] [PubMed] [Google Scholar]
- 16.Muzaffar A.R., Mendelson B.C., Adams W.P. Surgical Anatomy of the Ligamentous Attachments of the Lower Lid and Lateral Canthus. Plast. Reconstr. Surg. 2002;110:873–884. doi: 10.1097/00006534-200209010-00025. [DOI] [PubMed] [Google Scholar]
- 17.Sullivan D.M., Chung K.C.M., Eaves F.F.I.M., Rohrich R.J.M. The Level of Evidence Pyramid: Indicating Levels of Evidence in Plastic and Reconstructive Surgery Articles. Plast. Reconstr. Surg. 2021;148:68S–71S. doi: 10.1097/01.prs.0000794868.07051.b4. [DOI] [PubMed] [Google Scholar]
- 18.Hykin P.G., Bron A.J. Age-Related Morphological Changes in Lid Margin and Meibomian Gland Anatomy. Cornea. 1992;11:334–342. doi: 10.1097/00003226-199207000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Chiu E.S., Baker D.C. Endoscopic Brow Lift: A Retrospective Review of 628 Consecutive Cases over 5 Years. Plast. Reconstr. Surg. 2003;112:628–633. doi: 10.1097/01.PRS.0000071042.11435.2E. [DOI] [PubMed] [Google Scholar]
- 20.Carter S.R., Seiff S.R., Grant P.E., Vigneron D.B. The Asian lower eyelid: A comparative anatomic study using high-resolution magnetic resonance imaging. Ophthalmic Plast. Reconstr. Surg. 1998;14:227–234. doi: 10.1097/00002341-199807000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Rohrich R.J., Pessa J.E. The Fat Compartments of the Face: Anatomy and Clinical Implications for Cosmetic Surgery. Plast. Reconstr. Surg. 2007;119:2219–2227. doi: 10.1097/01.prs.0000265403.66886.54. [DOI] [PubMed] [Google Scholar]
- 22.Hamra S.T. Arcus Marginalis Release and Orbital Fat Preservation in Midface Rejuvenation. Plast. Reconstr. Surg. 1995;96:354–362. doi: 10.1097/00006534-199508000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Lambros V. Observations on Periorbital and Midface Aging. Plast. Reconstr. Surg. 2007;120:1367–1376. doi: 10.1097/01.prs.0000279348.09156.c3. [DOI] [PubMed] [Google Scholar]
- 24.Knize D.M. An Anatomically Based Study of the Mechanism of Eyebrow Ptosis. Plast. Reconstr. Surg. 1996;97:1321–1333. doi: 10.1097/00006534-199606000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Isse N.G. Endoscopic facial rejuvenation: Endoforehead, the functional lift. Case reports. Aesthetic Plast. Surg. 1994;18:21–29. doi: 10.1007/BF00444243. [DOI] [PubMed] [Google Scholar]
- 26.Hester T.R., Jr., Codner M.A., McCord C.D., Nahai F., Giannopoulos A. Evolution of technique of the direct transblepharoplasty approach for the correction of lower lid and midfacial aging: Maximizing results and minimizing complications in a 5-year experience. Plast. Reconstr. Surg. 2000;105:393–406. doi: 10.1097/00006534-200001000-00065. [DOI] [PubMed] [Google Scholar]
- 27.Hamra S.T. The Zygorbicular Dissection in Composite Rhytidectomy: An Ideal Midface Plane. Plast. Reconstr. Surg. 1998;102:1646–1657. doi: 10.1097/00006534-199810000-00051. [DOI] [PubMed] [Google Scholar]
- 28.Ramirez O.M. Endoscopic techniques in facial rejuvenation: An overview. Part I. Aesthetic Plast. Surg. 1994;18:141–147. doi: 10.1007/BF00454473. [DOI] [PubMed] [Google Scholar]
- 29.Baylis H.I., Long J.A., Groth M.J. Transconjunctival Lower Eyelid Blepharoplasty. Ophthalmology. 1989;96:1027–1032. doi: 10.1016/S0161-6420(89)32787-4. [DOI] [PubMed] [Google Scholar]
- 30.Hamra S.T. The role of orbital fat preservation in facial aesthetic surgery. A new concept. Clin. Plast. Surg. 1996;23:17–28. [PubMed] [Google Scholar]
- 31.Goldberg R.A. Transconjunctival Orbital Fat Repositioning: Transposition of Orbital Fat Pedicles into a Subperiosteal Pocket. Plast. Reconstr. Surg. 2000;105:743–748. doi: 10.1097/00006534-200002000-00044. [DOI] [PubMed] [Google Scholar]
- 32.Jeong S., Lemke B.N., Dortzbach R.K., Park Y.G., Kang H.K. The Asian upper eyelid: An anatomical study with comparison to the Caucasian eyelid. Arch. Ophthalmol. 1999;117:907–912. doi: 10.1001/archopht.117.7.907. [DOI] [PubMed] [Google Scholar]
- 33.Codner M.A., Wolfli J.N., Anzarut A. Primary Transcutaneous Lower Blepharoplasty with Routine Lateral Canthal Support: A Comprehensive 10-Year Review. Plast. Reconstr. Surg. 2008;121:241–250. doi: 10.1097/01.prs.0000295377.03279.8d. [DOI] [PubMed] [Google Scholar]
- 34.Pessa J.E., Desvigne L.D., Lambros V.S., Nimerick J., Sugunan B., Zadoo V.P. Changes in ocular globe-to-orbital rim position with age: Implications for aesthetic blepharoplasty of the lower eyelids. Aesthetic Plast. Surg. 1999;23:337–342. doi: 10.1007/s002669900295. [DOI] [PubMed] [Google Scholar]
- 35.Vasconez L.O., Core G.B., Gamboa-Bobadilla M., Guzman G., Askren C., Yamamoto Y. Endoscopic Techniques in Coronal Brow Lifting. Plast. Reconstr. Surg. 1994;94:788–793. doi: 10.1097/00006534-199411000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Fagien S. Algorithm for canthoplasty: The lateral retinacular suspension: A simplified suture canthopexy. Plast. Reconstr. Surg. 1999;103:2042–2053. doi: 10.1097/00006534-199906000-00039. [DOI] [PubMed] [Google Scholar]
- 37.Bosch W.A.V.D., Leenders I., Mulder P. Topographic anatomy of the eyelids, and the effects of sex and age. Br. J. Ophthalmol. 1999;83:347–352. doi: 10.1136/bjo.83.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patipa M. The Evaluation and Management of Lower Eyelid Retraction following Cosmetic Surgery. Plast. Reconstr. Surg. 2000;106:438–453. doi: 10.1097/00006534-200008000-00033. [DOI] [PubMed] [Google Scholar]
- 39.Kikkawa D.O., Lemke B.N., Dortzbach R.K. Relations of the Superficial Musculoaponeurotic System to the Orbit and Characterization of the Orbitomalar Ligament. Ophthalmic Plast. Reconstr. Surg. 1996;12:77–88. doi: 10.1097/00002341-199606000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Jelks G.W., Glat P.M., Jelks E.B., Longaker M.T. The Inferior Retinacular Lateral Canthoplasty: A New Technique. Plast. Reconstr. Surg. 1997;100:1262–1270. doi: 10.1097/00006534-199710000-00030. [DOI] [PubMed] [Google Scholar]
- 41.Rohrich R.J., Arbique G.M., Wong C., Brown S., Pessa J.E. The Anatomy of Suborbicularis Fat: Implications for Periorbital Rejuvenation. Plast. Reconstr. Surg. 2009;124:946–951. doi: 10.1097/PRS.0b013e3181b17b76. [DOI] [PubMed] [Google Scholar]
- 42.Little J.W. Three-Dimensional Rejuvenation of the Midface: Volumetric Resculpture by Malar Imbrication. Plast. Reconstr. Surg. 2000;105:267–285. doi: 10.1097/00006534-200001000-00046. [DOI] [PubMed] [Google Scholar]
- 43.Hamra S.T. Repositioning the Orbicularis Oculi Muscle in the Composite Rhytidectomy. Plast. Reconstr. Surg. 1992;90:14–22. doi: 10.1097/00006534-199207000-00002. [DOI] [PubMed] [Google Scholar]
- 44.Gunter J.P., Antrobus S.D. Aesthetic Analysis of the Eyebrows. Plast. Reconstr. Surg. 1997;99:1808–1816. doi: 10.1097/00006534-199706000-00002. [DOI] [PubMed] [Google Scholar]
- 45.Flowers R.S. Canthopexy as a routine blepharoplasty component. Clin. Plast. Surg. 1993;20:351–365. doi: 10.1016/S0094-1298(20)31227-X. [DOI] [PubMed] [Google Scholar]
- 46.Mullins J.B., Holds J.B., Branham G.H., Thomas J.R. Complications of the Transconjunctival Approach. Arch. Otolaryngol. Neck Surg. 1997;123:385–388. doi: 10.1001/archoto.123.4.385. [DOI] [PubMed] [Google Scholar]
- 47.Aiache A.E., Ramirez O.H. The suborbicularis oculi fat pads: An anatomic and clinical study. Plast. Reconstr. Surg. 1995;95:37–42. doi: 10.1097/00006534-199501000-00005. [DOI] [PubMed] [Google Scholar]
- 48.McKinney P., Mossie R.D., Zukowski M.L. Criteria for the forehead lift. Aesthetic Plast. Surg. 1991;15:141–147. doi: 10.1007/BF02273847. [DOI] [PubMed] [Google Scholar]
- 49.Rohrich R.J., Coberly D.M., Fagien S., Stuzin J.M. Current Concepts in Aesthetic Upper Blepharoplasty. Plast. Reconstr. Surg. 2004;113:32e–42e. doi: 10.1097/01.PRS.0000105684.06281.32. [DOI] [PubMed] [Google Scholar]
- 50.Haddock N.T., Saadeh P.B., Boutros S., Thorne C.H. The Tear Trough and Lid/Cheek Junction: Anatomy and Implications for Surgical Correction. Plast. Reconstr. Surg. 2009;123:1332–1340. doi: 10.1097/PRS.0b013e31819f2b36. [DOI] [PubMed] [Google Scholar]
- 51.Richard M.J., Morris C., Deen B.F., Gray L., Woodward J.A. Analysis of the Anatomic Changes of the Aging Facial Skeleton Using Computer-Assisted Tomography. Ophthalmic Plast. Reconstr. Surg. 2009;25:382–386. doi: 10.1097/IOP.0b013e3181b2f766. [DOI] [PubMed] [Google Scholar]
- 52.Knize D.M. Transpalpebral approach to the corrugator supercilii and procerus muscles. Plast. Reconstr. Surg. 1995;95:52–60. doi: 10.1097/00006534-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 53.Barton F.E., Ha R., Awada M. Fat Extrusion and Septal Reset in Patients with the Tear Trough Triad: A Critical Appraisal. Plast. Reconstr. Surg. 2004;113:2115–2121. doi: 10.1097/01.PRS.0000122409.00716.34. [DOI] [PubMed] [Google Scholar]
- 54.Mccord C.D., Codner M.A., Hester R.T. Redraping the Inferior Orbicularis Arc. Plast. Reconstr. Surg. 1998;102:2471–2479. doi: 10.1097/00006534-199812000-00034. [DOI] [PubMed] [Google Scholar]
- 55.Wong C.H., Hsieh M.K.H., Mendelson B. The tear trough ligament: Anatomical basis for the tear trough deformity. Plast. Reconstr. Surg. 2012;129:1392–1402. doi: 10.1097/PRS.0b013e31824ecd77. [DOI] [PubMed] [Google Scholar]
- 56.Zarem H.A., Resnick J.I. Expanded applications for transconjunctival lower lid blepharoplasty. Plast. Reconstr. Surg. 1991;88:215. doi: 10.1097/00006534-199108000-00006. [DOI] [PubMed] [Google Scholar]
- 57.Meyer D.R., Linberg J.V., Wobig J.L., McCormick S.A. Anatomy of the Orbital Septum and Associated Eyelid Connective Tissues. Ophthalmic Plast. Reconstr. Surg. 1991;7:104–113. doi: 10.1097/00002341-199106000-00004. [DOI] [PubMed] [Google Scholar]
- 58.McCord C.D., Doxanas M.T. Browplasty and browpexy: An adjunct to blepharoplasty. Plast. Reconstr. Surg. 1990;86:248–254. doi: 10.1097/00006534-199008000-00007. [DOI] [PubMed] [Google Scholar]
- 59.Goldberg R.A., McCann J.D., Fiaschetti D., Ben Simon G.J. What Causes Eyelid Bags? Analysis of 114 Consecutive Patients. Plast. Reconstr. Surg. 2005;115:1395–1402. doi: 10.1097/01.PRS.0000157016.49072.61. [DOI] [PubMed] [Google Scholar]
- 60.Hass A.N., Penne R.B., Stefanyszyn M.A., Flanagan J.C. Incidence of Postblepharoplasty Orbital Hemorrhage and Associated Visual Loss. Ophthalmic Plast. Reconstr. Surg. 2004;20:426–432. doi: 10.1097/01.IOP.0000143711.48389.C5. [DOI] [PubMed] [Google Scholar]
- 61.Hamra S.T. The Role of the Septal Reset in Creating a Youthful Eyelid-Cheek Complex in Facial Rejuvenation. Plast. Reconstr. Surg. 2004;113:2124–2141. doi: 10.1097/01.PRS.0000122410.19952.E7. [DOI] [PubMed] [Google Scholar]
- 62.Fagien S. Advanced Rejuvenative Upper Blepharoplasty: Enhancing Aesthetics of the Upper Periorbita. Plast. Reconstr. Surg. 2002;110:278–291. doi: 10.1097/00006534-200207000-00047. [DOI] [PubMed] [Google Scholar]
- 63.Knize D.M. Limited-Incision Forehead Lift for Eyebrow Elevation to Enhance Upper Blepharoplasty. Plast. Reconstr. Surg. 1996;97:1334–1342. doi: 10.1097/00006534-199606000-00002. [DOI] [PubMed] [Google Scholar]
- 64.Ramirez O.M. Three-dimensional endoscopic midface enhancement: A personal quest for the ideal cheek rejuvenation. Plast. Reconstr. Surg. 2002;109:329–340. doi: 10.1097/00006534-200201000-00052. [DOI] [PubMed] [Google Scholar]
- 65.Mendelson B.C., Jacobson S.R. Surgical Anatomy of the Midcheek: Facial Layers, Spaces, and the Midcheek Segments. Clin. Plast. Surg. 2008;35:395–404. doi: 10.1016/j.cps.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 66.Park D.H., Choi W.S., Yoon S.H., Song C.H. Anthropometry of Asian Eyelids by Age. Plast. Reconstr. Surg. 2008;121:1405–1413. doi: 10.1097/01.prs.0000304608.33432.67. [DOI] [PubMed] [Google Scholar]
- 67.Freund R.M., Nolan W.B. Correlation Between Brow Lift Outcomes and Aesthetic Ideals for Eyebrow Height and Shape in Females. Plast. Reconstr. Surg. 1996;97:1343–1348. doi: 10.1097/00006534-199606000-00003. [DOI] [PubMed] [Google Scholar]
- 68.Byrd H.S., Andochick S.E. The Deep Temporal Lift: A Multiplanar, Lateral Brow, Temporal, and Upper Face Lift. Plast. Reconstr. Surg. 1996;97:928–937. doi: 10.1097/00006534-199604001-00007. [DOI] [PubMed] [Google Scholar]
- 69.McGraw B.L., Adamson P.A. Postblepharoplasty ectropion. Prevention and management. Arch. Otolaryngol. Head Neck Surg. 1991;117:852–856. doi: 10.1001/archotol.1991.01870200046006. [DOI] [PubMed] [Google Scholar]
- 70.Janis J.E., Ghavami A., Lemmon J.A., Leedy J.E., Guyuron B. Anatomy of the Corrugator Supercilii Muscle: Part I. Corrugator Topography. Plast. Reconstr. Surg. 2007;120:1647–1653. doi: 10.1097/01.prs.0000282725.61640.e1. [DOI] [PubMed] [Google Scholar]
- 71.Trepsat F. Periorbital Rejuvenation Combining Fat Grafting and Blepharoplasties. Aesthetic Plast. Surg. 2003;27:243–253. doi: 10.1007/s00266-003-2126-y. [DOI] [PubMed] [Google Scholar]
- 72.Daniel R.K., Tirkanits B. Endoscopic Forehead Lift: An Operative Technique. Plast. Reconstr. Surg. 1996;98:1148–1157. doi: 10.1097/00006534-199612000-00003. [DOI] [PubMed] [Google Scholar]
- 73.Carraway J.H., Mellow C.G. The Prevention and Treatment of Lower Lid Ectropion Following Blepharoplasty. Plast. Reconstr. Surg. 1990;85:971–981. doi: 10.1097/00006534-199006000-00025. [DOI] [PubMed] [Google Scholar]
- 74.McCord C.D., Boswell C.B., Hester T.R. Lateral Canthal Anchoring. Plast. Reconstr. Surg. 2003;112:222–237. doi: 10.1097/01.PRS.0000066340.85485.DF. [DOI] [PubMed] [Google Scholar]
- 75.Rohrich R.J., Beran S.J. Evolving fixation methods in endoscopically assisted forehead rejuvenation: Controversies and rationale. Plast. Reconstr. Surg. 1997;100:1575–1582. doi: 10.1097/00006534-199711000-00032. [DOI] [PubMed] [Google Scholar]
- 76.Jones B.M., Grover R. Endoscopic brow lift: A personal review of 538 patients and comparison of fixation techniques. Plast. Reconstr. Surg. 2004;113:1242–1250. doi: 10.1097/01.PRS.0000110206.25586.78. [DOI] [PubMed] [Google Scholar]
- 77.May J.W., Jr., Fearon J., Zingarelli P. Retro-orbicularis oculus fat (ROOF) resection in aesthetic blepharoplasty: A 6-year study in 63 patients. Plast. Reconstr. Surg. 1990;86:682–689. doi: 10.1097/00006534-199010000-00011. [DOI] [PubMed] [Google Scholar]
- 78.Lelli G.J., Jr., Lisman R.D. Blepharoplasty complications. Plast. Reconstr. Surg. 2010;125:1007–1017. doi: 10.1097/PRS.0b013e3181ce17e8. [DOI] [PubMed] [Google Scholar]
- 79.Elkwood A., Matarasso A., Rankin M., Elkowitz M., Godek C.P. National plastic surgery survey: Brow lifting techniques and complications. Plast. Reconstr. Surg. 2001;108:2143–2150. doi: 10.1097/00006534-200112000-00057. [DOI] [PubMed] [Google Scholar]
- 80.Paul M.D. The Evolution of the Brow Lift in Aesthetic Plastic Surgery. Plast. Reconstr. Surg. 2001;108:1409–1422. doi: 10.1097/00006534-200110000-00049. [DOI] [PubMed] [Google Scholar]
- 81.Hamra S.T. Frequent Face Lift Sequelae: Hollow Eyes and the Lateral Sweep: Cause and Repair. Plast. Reconstr. Surg. 1998;102:1658–1666. doi: 10.1097/00006534-199810000-00052. [DOI] [PubMed] [Google Scholar]
- 82.Loeb R. Naso-jugal groove leveling with fat tissue. Clin. Plast. Surg. 1993;20:393–400. doi: 10.1016/S0094-1298(20)31230-X. [DOI] [PubMed] [Google Scholar]
- 83.Connell B.F., Lambros V.S., Neurohr G.H. The forehead lift: Techniques to avoid complications and produce optimal results. Aesthetic Plast. Surg. 1989;13:217–237. doi: 10.1007/BF01570355. [DOI] [PubMed] [Google Scholar]
- 84.Rohrich R.J., Ghavami A., Mojallal A. The five-step lower blepharoplasty: Blending the eyelid-cheek junction. Plast. Reconstr. Surg. 2011;128:775–783. doi: 10.1097/PRS.0b013e3182121618. [DOI] [PubMed] [Google Scholar]
- 85.Flowers R.S. Upper Blepharoplasty By Eyelid Invagination. Clin. Plast. Surg. 1993;20:193–207. doi: 10.1016/S0094-1298(20)31211-6. [DOI] [PubMed] [Google Scholar]
- 86.Wong C.H., Mendelson B. Facial soft-tissue spaces and retaining ligaments of the midcheek: Defining the premaxillary space. Plast. Reconstr. Surg. 2013;132:49–56. doi: 10.1097/PRS.0b013e3182910a57. [DOI] [PubMed] [Google Scholar]
- 87.Glat P.M., Jelks G.W., Jelks E.B., Wood M., Gadangi P., Longaker M.T. Evolution of the Lateral Canthoplasty: Techniques and Indications. Plast. Reconstr. Surg. 1997;100:1396–1405. doi: 10.1097/00006534-199711000-00003. [DOI] [PubMed] [Google Scholar]
- 88.Goldberg R.A., Wu J.C., Jesmanowicz A., Hyde J.S. Eyelid anatomy revisited. Dynamic high-resolution magnetic resonance images of Whitnall’s ligament and upper eyelid structures with the use of a surface coil. Arch. Ophthalmol. 1992;110:1598–1600. doi: 10.1001/archopht.1992.01080230098030. [DOI] [PubMed] [Google Scholar]
- 89.Matros E., Garcia J.A., Yaremchuk M.J. Changes in Eyebrow Position and Shape with Aging. Plast. Reconstr. Surg. 2009;124:1296–1301. doi: 10.1097/PRS.0b013e3181b455e8. [DOI] [PubMed] [Google Scholar]
- 90.Lambros V. Models of Facial Aging and Implications for Treatment. Clin. Plast. Surg. 2008;35:319–327. doi: 10.1016/j.cps.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 91.Pacella S.J., Nahai F.R., Nahai F. Transconjunctival blepharoplasty for upper and lower eyelids. Plast. Reconstr. Surg. 2010;125:384–392. doi: 10.1097/PRS.0b013e3181c2a534. [DOI] [PubMed] [Google Scholar]
- 92.Booth A.J., Murray A., Tyers A.G. The direct brow lift: Efficacy, complications, and patient satisfaction. Br. J. Ophthalmol. 2004;88:688–691. doi: 10.1136/bjo.2003.019232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Patel B.C., Patipa M., Anderson R.L., McLeish W. Management of postblepharoplasty lower eyelid retraction with hard palate grafts and lateral tarsal strip. Plast. Reconstr. Surg. 1997;99:1251–1260. doi: 10.1097/00006534-199705000-00007. [DOI] [PubMed] [Google Scholar]
- 94.Ghavami A., Pessa J.E., Janis J., Khosla R., Reece E.M., Rohrich R.J. The Orbicularis Retaining Ligament of the Medial Orbit: Closing the Circle. Plast. Reconstr. Surg. 2008;121:994–1001. doi: 10.1097/01.prs.0000299941.62645.4e. [DOI] [PubMed] [Google Scholar]
- 95.Kawamoto H.K., Bradley J.P. The tear “TROUF” procedure: Transconjunctival repositioning of orbital unipedicled fat. Plast. Reconstr. Surg. 2003;112:1903–1907. doi: 10.1097/01.PRS.0000091238.72843.7E. [DOI] [PubMed] [Google Scholar]
- 96.Ramirez O.M. Endoscopically Assisted Biplanar Forehead Lift. Plast. Reconstr. Surg. 1995;96:323–333. doi: 10.1097/00006534-199508000-00010. [DOI] [PubMed] [Google Scholar]
- 97.Troilius C. Subperiosteal Brow Lifts without Fixation. Plast. Reconstr. Surg. 2004;114:1595–1603. doi: 10.1097/01.PRS.0000138758.48043.44. [DOI] [PubMed] [Google Scholar]
- 98.Furnas D.W. Festoons, mounds, and bags of the eyelids and cheek. Clin. Plast. Surg. 1993;20:367–385. doi: 10.1016/S0094-1298(20)31228-1. [DOI] [PubMed] [Google Scholar]
- 99.Westfall C.T., Shore J.W., Nunery W.R., Hawes M.J., Yaremchuk M.J. Operative Complications of the Transconjunctival Inferior Fornix Approach. Ophthalmology. 1991;98:1525–1528. doi: 10.1016/S0161-6420(91)32094-3. [DOI] [PubMed] [Google Scholar]
- 100.De la Plaza R., Valiente E., Arroyo J.M. Supraperiosteal lifting of the upper two-thirds of the face. Br. J. Plast. Surg. 1991;44:325–332. doi: 10.1016/0007-1226(91)90143-8. [DOI] [PubMed] [Google Scholar]
- 101.De Cordier B.C., Jorge I., AI-Hakeem M.S., Rosenberg L.Z., Gardner P.M., Costa-Ferreira A., Vasconez L.O. Endoscopic forehead lift: Review of technique, cases, and complications. Plast. Reconstr. Surg. 2002;110:1558–1568. doi: 10.1097/01.PRS.0000029815.87106.CB. [DOI] [PubMed] [Google Scholar]
- 102.Roh M.R., Chung K.Y. Infraorbital Dark Circles: Definition, Causes, and Treatment Options. Dermatol. Surg. 2009;35:1163–1171. doi: 10.1111/j.1524-4725.2009.01213.x. [DOI] [PubMed] [Google Scholar]
- 103.Nahm W.K., Su T.T., Rotunda A.M., Moy R.L. Objective changes in brow position, superior palpebral crease, peak angle of the eyebrow, and jowl surface area after volumetric radiofrequency treatments to half of the face. Dermatol. Surg. 2004;30:922–928. doi: 10.1111/j.1524-4725.2004.30263.x. [DOI] [PubMed] [Google Scholar]
- 104.Isse N.G. Endoscopic forehead lift. Evolution and update. Clin. Plast. Surg. 1995;22:661–673. doi: 10.1016/S0094-1298(20)31167-6. [DOI] [PubMed] [Google Scholar]
- 105.Hamra S.T. A study of the long-term effect of malar fat repositioning in face lift surgery: Short-term success but long-term failure. Plast. Reconstr. Surg. 2002;110:940–951. doi: 10.1097/00006534-200209010-00035. [DOI] [PubMed] [Google Scholar]
- 106.Starck W.J., Griffin J.E., Jr., Epker B.N. Objective evaluation of the eyelids and eyebrows after blepharoplasty. J. Oral Maxillofac. Surg. 1996;54:297–302. doi: 10.1016/S0278-2391(96)90746-6. [DOI] [PubMed] [Google Scholar]
- 107.Cook T.A., Brownrigg P.J., Wang T.D., Quatela V.C. The Versatile Midforehead Browlift. Arch. Otolaryngol. Neck Surg. 1989;115:163–168. doi: 10.1001/archotol.1989.01860260037011. [DOI] [PubMed] [Google Scholar]
- 108.Knize D.M. Anatomic Concepts for Brow Lift Procedures. Plast. Reconstr. Surg. 2009;124:2118–2126. doi: 10.1097/PRS.0b013e3181bd0726. [DOI] [PubMed] [Google Scholar]
- 109.Core G.B., Vasconez L.O., Graham H.D., 3rd Endoscopic browlift. Clin. Plast. Surg. 1995;22:619–631. doi: 10.1016/S0094-1298(20)31164-0. [DOI] [PubMed] [Google Scholar]
- 110.Darcy S.J., Miller T.A., Goldberg R.A., Villablanca J.P., Demer J.L., Rudkin G.H. Magnetic Resonance Imaging Characterization of Orbital Changes with Age and Associated Contributions to Lower Eyelid Prominence. Plast. Reconstr. Surg. 2008;122:921–929. doi: 10.1097/PRS.0b013e3181811ce8. [DOI] [PubMed] [Google Scholar]
- 111.Kakizaki H., Malhotra R., Madge S.N., Selva D. Lower eyelid anatomy: An update. Ann. Plast. Surg. 2009;63:344–351. doi: 10.1097/SAP.0b013e31818c4b22. [DOI] [PubMed] [Google Scholar]
- 112.Paul M.D., Calvert J.W., Evans G.R.D. The Evolution of the Midface Lift in Aesthetic Plastic Surgery. Plast. Reconstr. Surg. 2006;117:1809–1827. doi: 10.1097/01.prs.0000218839.55122.c0. [DOI] [PubMed] [Google Scholar]
- 113.Pessa J.E., Garza J.R. The Malar Septum: The Anatomic Basis of Malar Mounds and Malar Edema. Aesthetic Surg. J. 1997;17:11–17. doi: 10.1016/S1090-820X(97)70001-3. [DOI] [PubMed] [Google Scholar]
- 114.Ramirez O.M. The anchor subperiosteal forehead lift. Plast. Reconstr. Surg. 1995;95:993–1003. doi: 10.1097/00006534-199505000-00006. [DOI] [PubMed] [Google Scholar]
- 115.Guyuron B., Michelow B.J., Thomas T. Corrugator Supercilii Muscle Resection Through Blepharoplasty Incision. Plast. Reconstr. Surg. 1995;95:691–696. doi: 10.1097/00006534-199504000-00010. [DOI] [PubMed] [Google Scholar]
- 116.Kakizaki H., Malhotra R., Selva D. Upper eyelid anatomy: An update. Ann. Plast. Surg. 2009;63:336–343. doi: 10.1097/SAP.0b013e31818b42f7. [DOI] [PubMed] [Google Scholar]
- 117.Fratila A.A.M., Schenck T.L., Redka-Swoboda W., Zilinsky I., Pavicic T., Cotofana S. The Anatomy of the Aging Face: A Review. Facial Plast. Surg. 2016;32:253–260. doi: 10.1055/s-0036-1582234. [DOI] [PubMed] [Google Scholar]
- 118.Enlow D.H. A morphogenetic analysis of facial growth. Am. J. Orthod. 1966;52:283–299. doi: 10.1016/0002-9416(66)90169-2. [DOI] [PubMed] [Google Scholar]
- 119.Mendelson B., Wong C.-H. Changes in the Facial Skeleton With Aging: Implications and Clinical Applications in Facial Rejuvenation. Aesthetic Plast. Surg. 2012;36:753–760. doi: 10.1007/s00266-012-9904-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Okada H.C., Alleyne B., Varghai K., Kinder K., Guyuron B. Facial changes caused by smoking: A comparison between smoking and nonsmoking identical twins. Plast. Reconstr. Surg. 2013;132:1085–1092. doi: 10.1097/PRS.0b013e3182a4c20a. [DOI] [PubMed] [Google Scholar]
- 121.Lambros V. 3D Facial Averaging: A Breakthrough. [(accessed on 23 November 2020)]. Available online: http://www.vallambros.com/facial-aging-3d.html.
- 122.Asaad M., Kelarji A.B., Jawhar C.S., Banuelos J., Taslakian E., Wahood W., Sharaf B. Eyebrow Height Changes with Aging: A Systematic Review and Meta-analysis. Plast. Reconstr. Surg. Glob. Open. 2019;7:e2433. doi: 10.1097/GOX.0000000000002433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Stuzin J.M., Baker T.J., Gordon H.L. The relationship of the superficial and deep facial fascias: Relevance to rhytidectomy and aging. Plast. Reconstr. Surg. 1992;89:441. doi: 10.1097/00006534-199203000-00007. [DOI] [PubMed] [Google Scholar]
- 124.Furnas D.W. The Retaining Ligaments of the Cheek. Plast. Reconstr. Surg. 1989;83:11–16. doi: 10.1097/00006534-198901000-00003. [DOI] [PubMed] [Google Scholar]
- 125.Mendelson B.C., Muzaffar A.R., Adams W.P., Jr. Surgical anatomy of the midcheek and malar mounds. Plast. Reconstr. Surg. 2002;110:885–896. doi: 10.1097/00006534-200209010-00026. [DOI] [PubMed] [Google Scholar]
- 126.Ozturk C.N., Larson J.D., Ozturk C., Zins J.E. The SMAS and fat compartments of the nose: An anatomical study. Aesthetic Plast. Surg. 2013;37:11–15. doi: 10.1007/s00266-012-0012-1. [DOI] [PubMed] [Google Scholar]
- 127.Espinoza G.M., Holds J.B. Evolution of eyelid surgery. Facial Plast. Surg. Clin. 2005;13:505–510. doi: 10.1016/j.fsc.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 128.Lam V.B., Czyz C.N., Wulc A.E. The Brow-Eyelid Continuum: An Anatomic Perspective. Clin. Plast. Surg. 2013;40:1–19. doi: 10.1016/j.cps.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 129.Tepper O.M., Steinbrech D., Howell M.H., Jelks E.B., Jelks G.W. A Retrospective Review of Patients Undergoing Lateral Canthoplasty Techniques to Manage Existing or Potential Lower Eyelid Malposition: Identification of Seven Key Preoperative Findings. Plast. Reconstr. Surg. 2015;136:40–49. doi: 10.1097/PRS.0000000000001363. [DOI] [PubMed] [Google Scholar]
- 130.Owsley J.Q. Resection of the Prominent Lateral Fat Pad During Upper Lid Blepharoplasty. Plast. Reconstr. Surg. 1980;65:4–9. doi: 10.1097/00006534-198001000-00002. [DOI] [PubMed] [Google Scholar]
- 131.Fagien S., Klein A.W. A Brief Overview and History of Temporary Fillers: Evolution, Advantages, and Limitations. Plast. Reconstr. Surg. 2007;120:8S–16S. doi: 10.1097/01.prs.0000248788.97350.18. [DOI] [PubMed] [Google Scholar]
- 132.American Society of Plastic Surgeons 2018 Plastic Surgery Statistics Report. 2018. [(accessed on 5 August 2020)]. Available online: www.PlasticSurgery.org.
- 133.Hamamoto A., Liu T., Wong B. Identifying Ideal Brow Vector Position: Empirical Analysis of Three Brow Archetypes. Facial Plast. Surg. 2013;29:076–082. doi: 10.1055/s-0033-1333841. [DOI] [PubMed] [Google Scholar]
- 134.Gøtzsche P.C. Citation bias: Questionable research practice or scientific misconduct? J. R. Soc. Med. 2022;115:31–35. doi: 10.1177/01410768221075881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mavrogenis A.F., Ruggieri P., Papagelopoulos P.J. Editorial: Self-citation in Publishing. Clin. Orthop. Relat. Res. 2010;468:2803–2807. doi: 10.1007/s11999-010-1480-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Karimi N., Kashkouli M.B., Sianati H., Khademi B. Techniques of Eyebrow Lifting: A Narrative Review. J. Ophthalmic Vis. Res. 2020;15:218–235. doi: 10.18502/jovr.v15i2.6740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Levine M.R., Allen R.C. Manual of Oculoplastic Surgery. 5th ed. Springer; New York, NY, USA: 2018. [Google Scholar]
- 138.Perry J.D., Hwang C.J. Direct Browlift. Clin. Plast. Surg. 2022;49:409–414. doi: 10.1016/j.cps.2022.03.002. [DOI] [PubMed] [Google Scholar]
- 139.Terella A.M., Wang T.D. Technical Considerations in Endoscopic Brow Lift. Clin. Plast. Surg. 2013;40:105–115. doi: 10.1016/j.cps.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 140.Raggio B.S., Winters R. Endoscopic Brow Lift, in StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2022. [PubMed] [Google Scholar]
- 141.Viterbo F., Auersvald A., O’Daniel T.G. Gliding Brow Lift (GBL): A New Concept. Aesthetic Plast. Surg. 2019;43:1536–1546. doi: 10.1007/s00266-019-01486-3. [DOI] [PubMed] [Google Scholar]
- 142.Rohrich R.J., Villanueva N.L., Afrooz P.N. Refinements in Upper Blepharoplasty: The Five-Step Technique. Plast. Reconstr. Surg. 2018;141:1144–1146. doi: 10.1097/PRS.0000000000004439. [DOI] [PubMed] [Google Scholar]
- 143.Patel B.C., Malhotra R. Upper Eyelid Blepharoplasty. StatPearls Publishing; Treasure Island, FL, USA: 2022. [PubMed] [Google Scholar]
- 144.Kossler A.L., Peng G.L., Yoo D.B., Azizzadeh B., Massry G.G. Current Trends in Upper and Lower Eyelid Blepharoplasty Among American Society of Ophthalmic Plastic and Reconstructive Surgery Members. Ophthalmic Plast. Reconstr. Surg. 2018;34:37–42. doi: 10.1097/IOP.0000000000000849. [DOI] [PubMed] [Google Scholar]
- 145.Bhattacharjee K., Ghosh S., Ugradar S., Azhdam A.M. Lower eyelid blepharoplasty: An overview. Indian J. Ophthalmol. 2020;68:2075–2083. doi: 10.4103/ijo.IJO_2265_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Jin Y., Gao W., Teo H.M.T., Lin X. Transconjunctival Lower Blepharoplasty Using Midcheek Spaces for Orbital Fat Transposition (S.O.F.T.) Ann. Plast. Surg. 2021;86:620–626. doi: 10.1097/SAP.0000000000002864. [DOI] [PubMed] [Google Scholar]
- 147.Liao H.T. Lower Eyelid and Midface Rejuvenation: Suborbicularis Oculi Fat Lift. Facial Plast. Surg. Clin. 2021;29:497–509. doi: 10.1016/j.fsc.2021.06.003. [DOI] [PubMed] [Google Scholar]
- 148.Rostami S., de la Torre J.I., Czyz C.N. Lower Eyelid Blepharoplasty. StatPearls Publishing; Treasure Island, FL, USA: 2022. [PubMed] [Google Scholar]
- 149.Rao V., Sullivan P.K. Lower Lid Blepharoplasty in Men. Clin. Plast. Surg. 2022;49:213–220. doi: 10.1016/j.cps.2021.12.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.