Abstract
Objectives
This study aims to report a delayed Gardner syndrome diagnosis mimicking temporomandibular ankylosis.
Methods
An 11-year-old patient was treated at the Hospital Josina Machel, Luanda, Angola for severe chronic trismus without TMJ involvement. Some difficulties in diagnosis and final results were discussed
Case report
A delayed diagnosis of Gardner syndrome was treated by the authors. The delay was due to a lack of timely CT scans and some COVID-19 pandemic restrictions. This delay worsened the patient´s clinical condition for several months. Classic surgical gap arthroplasty has been used and considered successful, particularly when material is scarce.
Conclusions
Classical surgical techniques are still very useful in some parts of the world that do not rely on modern technology. International collaboration through teledentistry, case review over the Internet, and humanitarian or educational missions are very helpful in low-income countries.
Keywords: Angola, Ankylosis, Case report, Delayed diagnosis, Gardner syndrome, Pathology, Oral
Introduction
Eldon J Gardner described and characterized the rare syndrome that bears his name in 1951. The myriad of changes consist of multiple intestinal polyposis, osteomas, and epidermoid cysts, alongside dental anormalities [1]. A genetic mutation in the gene for adenomatous polyposis coli on chromosome 5 is considered to be primarily responsible [2]. The high penetrance and high incidence of tumors associated with Gardner syndrome (GS) make early diagnosis and family counseling important.
Patients with suspected GS must undergo endoscopy to assess the presence of multiple intestinal polyps. Temporomandibular ankylosis is not directly related to GS but makes it impossible to perform an endoscopy. This work aims to report a case of suspected Gardner syndrome in a patient with chronic and severe trismus. This situation has resulted in a delayed diagnosis.
Material and Methods
This is a retrospective case report according to the recommendations of the CARE guideline [3]. The authors examined and operated on a child patient with severe chronic trismus. The patient was operated on at Hospital Josina Machel, Luanda, Angola, according to the guidelines of Good Clinical Practice and the principles of the Declaration of Helsinki. Delayed diagnosis of Gardner syndrome has been discussed in this article.
Case Report
An 11-year-old male patient was referred to the Hospital Josina Machel in Luanda. The main complaint was severe trismus for more than a year. The patient was disconnected from daily school activities and isolated at home. Exactly how often, the caregivers could not say. A lack of interest, apathy, anxiety, and feelings of insecurity have been identified for some depressive symptoms. The panoramic radiograph showed multiple mandibular and maxillary masses in addition to a few unerupted teeth. The authors suspected GS (Fig. 1). Due to severe trismus, the patient was unable to undergo endoscopy to evaluate for intestinal polyposis. A CT scan was performed which showed no evidence of ankylosis of the temporomandibular joint (TMJ) (Fig. 2). Surgical planning included removal of osteomas to assess development of TMJ ankylosis (Fig. 3).
Fig. 1.
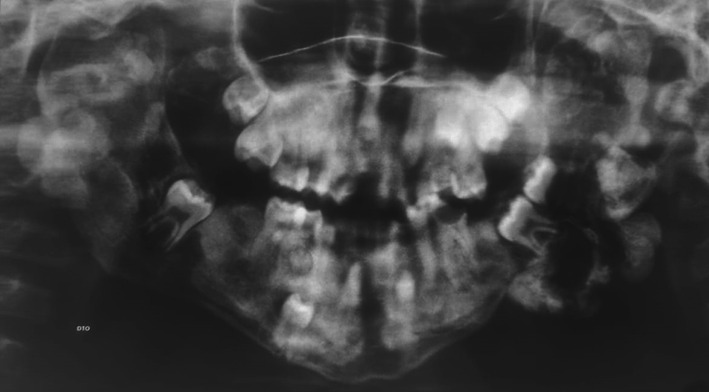
Panoramic radiography. Note the mandibular masses in the TMJ region and several unerupted teeth
Fig. 2.

CT scan showing no evidence of TMJ ankylosis
Fig. 3.
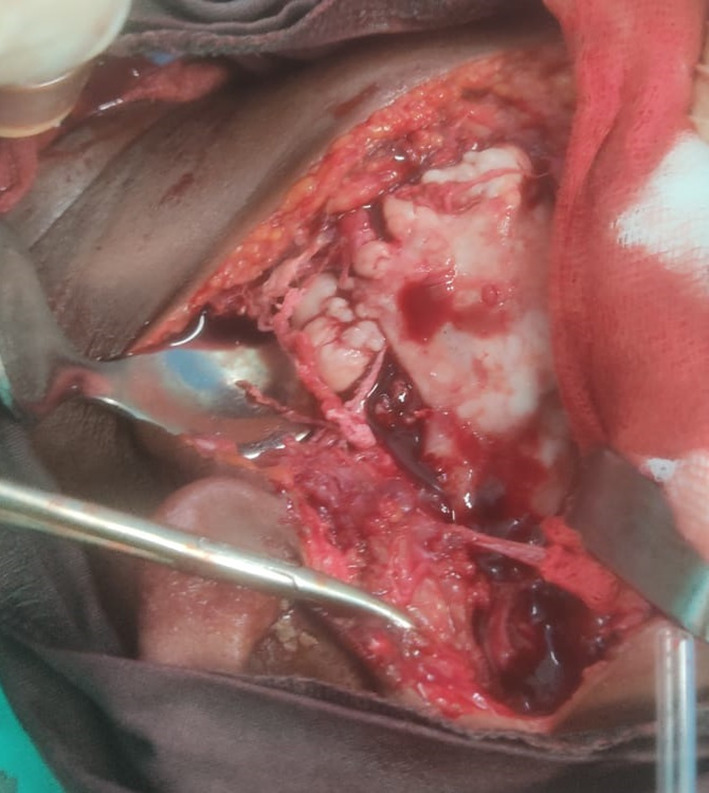
Intraoperative aspect of osteomas
The patient underwent mandibular osteoma removal under general anesthesia. At the same time, some teeth that had not erupted were removed (Fig. 4). Due to the extensive deformity of the temporomandibular region caused by osteomas, a mandibular osteotomy just below the TMJ was performed to simulate gap arthroplasty. A joint prosthesis was not used due to high costs and logistical problems. Transoperatively, the patient was able to open his mouth normally. The operation was considered successful according to the authors.
Fig. 4.

Removed osteomas and unerupted teeth
Two weeks after osteoma removal, the patient underwent regular endoscopy. Intestinal polyps were found and the delayed diagnosis of GS was achieved. The patient and his family were satisfied with the diagnosis and treatment. They all returned to their everyday lives without any kind consequences.
For logistical reasons, neither anatomo-pathologic examination nor genetic testing was performed. The hospital where the patient was operated has a large number of patients and does not have sufficient tomographic equipment to meet the needs. For this reason, many patients are evaluated preoperatively, but postoperative follow-up is through clinical evaluation. The use of CT scans for postoperative assessment, as in the present case, is uncommon.
Discussion
The late diagnosis of maxillofacial pathology has been a regular problem in Angola. For financial, logistical, and cost reasons, Angolan maxillofacial surgeons need to increase their clinical and radiological knowledge in order to be able to make an adequate definitive diagnosis. Although the importance of genetic testing is well known [4], genome sequencing is not available in most parts of the African continent. Although these tests are of great value not only for the patient but for the whole family to detect disease mutations and diagnose cancer early [2], this does not correspond to the Angolan reality.
Chronic trismus is defined as restricted mouth opening for at least one year [5]. With a multiple etiology, including anatomical, syndromic, oncological, infectious, and TMJ diseases, this is always a challenging situation. Diagnosis is an important question. Magnetic resonance imaging (MRI) is considered the gold standard for assessing TMJ [6]. Unfortunately, apart from some difficulties in clinical interpretation, no MRI was available in our provincial hospital.
MRI and genetic testing are not available to the authors. An anatomo-pathological study has been suspended due to the COVID-19 pandemic as it was being conducted in Brazil. Diagnosis of GS is based on clinical findings, gastrointestinal endoscopy, and genetic testing [7]. Although some items were missing from this diagnostic triad, a definitive diagnosis was possible. This case highlights the importance of constant updating and recycling of knowledge. This is particularly evident in pathological cases since some pathologies are rarely or usually not seen, even in specialized services.
Custom TMJ prostheses are a reality in middle-income and developed countries. Planning, cutting templates and the entire prosthesis can be digitally individualized and achieve a gold standard in TMJ replacement [8]. The high cost of this replacement system is prohibitive for several countries worldwide and much of the African continent. Some non-prosthesis surgical techniques are still performed worldwide to treat TMJ ankylosis [9]. Surgical intervention on TMJ, condyle, ramus, and/or coronoid process is still possible in some regions today, with predictable results being achieved in addition to the preservation of esthetics and function. This step can be performed alone or in conjunction with orthognathic surgery or bone grafts [10–12].
The internet has opened up a world of possibilities. Teledentistry, case reviews and knowledge sharing are available to a large number of maxillofacial surgeons working in hard-to-reach regions. An international collaboration between Angola and Brazil achieves some results [13, 14]. Humanitarian missions in low-income countries are extremely useful but come at a high cost [15]. While online collaboration cannot solve several problems, it is an inexpensive way to receive scientific updates and case discussions. Altruism is a helpful situation that expands knowledge and opportunities for both parties.
Conclusions
When Gardner syndrome is suspected, maxillofacial surgeons must increase their knowledge and skills to make a definitive diagnosis, counsel patients and loved ones, and prevent future complications. Temporomandibular osteoplasty is useful in regions where a prosthetic option is not possible. International online collaboration is a great form of sharing experiences and awareness.
Authors' Contribution
All authors contributed equally to this manuscript. All authors read and approved the final manuscript.
Funding
This article was not supported by any grant.
Declarations
Conflict of interest
There is no conflict of interest.
Ethical Approval
This article is exempt from ethical approval since it was performed in our district general hospital. This study was conducted following Good Clinical Practice guidelines and the principles of the Declaration of Helsinki.
Human or Animal Rights
The authors certify that they have obtained appropriate patient consent forms.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Koh K-J, Park H-N, Kim K-A. Gardner syndrome associated with multiple osteomas, intestinal polyposis, and epidermoid cysts. Imaging Sci Dent. 2016;46(4):267–272. doi: 10.5624/isd.2016.46.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gu X, Li X, Xu J, Yang J, Li H, Wu Q, et al. Accumulated genetic mutations leading to accelerated initiation and progression of colorectal cancer in a patient with Gardner syndrome: a case report. Medicine (Baltimore) 2021;100(13):e25247. doi: 10.1097/MD.0000000000025247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache. 2013;53(10):1541–1547. doi: 10.1111/head.12246. [DOI] [PubMed] [Google Scholar]
- 4.Lv Z, Wang C, Wu L, Guo B, Zhang D, Zhang Y, et al. Identification of a mutL-homolog 1 mutation via whole-exome sequencing in a Chinese family with Gardner syndrome. Mol Med Rep. 2018;18(1):987–992. doi: 10.3892/mmr.2018.9063. [DOI] [PubMed] [Google Scholar]
- 5.Smeets M, Van Dessel J, Croonenborghs T-M, Politis C, Jacobs R, Bila M. A retrospective study on the predictive factors in chronic trismus. Br J Oral Maxillofac Surg. 2021;S0266–4356(21):30–39. doi: 10.1016/j.bjoms.2021.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Eckstein FM, Wurm MC, Eckstein M, Wiesmüller M, Müller M, Jehn P, et al. Imaging, histopathological degree of degeneration and clinical findings - do these correlate in patients with temporomandibular joint disorders. J Stomatol oral Maxillofac Surg. 2021;S2468–7855(21):108–117. doi: 10.1016/j.jormas.2021.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Wexell CL, Bergenblock S, Kovács A. A case report on gardner syndrome with dental implant treatment and a long-term follow-up. J Oral Maxillofac Surg. 2019;77(8):1617–1627. doi: 10.1016/j.joms.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Franco JMPL, Bezerra TP, Pita-Neto ICP, da Silveira Santos DF, Rêgo RD. Treatment of the temporomandibular joint ankylosis with a customized prosthesis in a single stage: the use of 3D cutting guides and virtual surgical planning. J Maxillofac Oral Surg. 2021;20(4):702–705. doi: 10.1007/s12663-021-01562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Selvaraj DSS, Ommen AG, Ebenezer J. Coronoidoplasty in TMJ ankylosis treatment. BMJ Case Rep. 2020;13(8):e235698. doi: 10.1136/bcr-2020-235698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karakawa R, Yoshimatsu H, Yano T. Coronoidectomy, condylectomy, and free vascularized fibula osteomusculocutaneous flap transfer for severe trismus due to contracture of the oral mucosa and temporomandibular joint ankylosis after maxillectomy: a case report. Microsurgery. 2021;42(2):187–191. doi: 10.1002/micr.30838. [DOI] [PubMed] [Google Scholar]
- 11.Cascone P, Runci Anastasi M, Maffia F, Vellone V. Slice functional condylectomy and piezosurgery: a proposal in unilateral condylar hyperplasia treatment. J Craniofac Surg. 2021;32(5):1836–1837. doi: 10.1097/SCS.0000000000007224. [DOI] [PubMed] [Google Scholar]
- 12.Hoang TA, Lee KC, Chuang SK. Simultaneous condylar reconstruction by free ramus osteotomy graft after complete condylectomy for osteochondroma. J Craniofac Surg. 2021;32(5):e477–e479. doi: 10.1097/SCS.0000000000007464. [DOI] [PubMed] [Google Scholar]
- 13.Filipe L, Cassule YS, Grillo R, Pozzer L, Bueno BU, Teixeira RG. Relationship between mysticism and severe odontogenic infections in Africa: what to do?: Mysticism and severe infections in Africa. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022;S2212–4403(22):00007–14. doi: 10.1016/j.oooo.2022.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Lucamba AJ, Grillo R, Bueno BU, Teixeira RG. Foley´s cateter as a coadjuvant on middle face reconstruction. Brazilian J Oral Maxillofac Surg. 2022;22(1):26–29. [Google Scholar]
- 15.Bouaoud J, Ndiaye MM, Benassarou M, Toure S, Schouman T, Bertolus C. Humanitarian maxillofacial mission’s success requires experienced surgeons, careful planning, and meeting with the local’s care needs. J Oral Maxillofac Surg. 2021;79(10):1999.e1–1999.e9. doi: 10.1016/j.joms.2021.05.011. [DOI] [PubMed] [Google Scholar]


