Abstract
This study provides an overview of the literature on the cost-effectiveness of homecare services compared to in-hospital care for adults and older adults. A systematic review was performed using Medline, Embase, Scopus, Web of Science, CINAHL and CENTRAL databases from inception to April 2022. The inclusion criteria were as follows: (i) (older) adults; (ii) homecare as an intervention; (iii) hospital care as a comparison; (iv) a full economic evaluation examining both costs and consequences; and (v) economic evaluations arising from randomized controlled trials (RCTs). Two independent reviewers selected the studies, extracted data and assessed study quality. Of the 14 studies identified, homecare, when compared to hospital care, was cost-saving in seven studies, cost-effective in two and more effective in one. The evidence suggests that homecare interventions are likely to be cost-saving and as effective as hospital. However, the included studies differ regarding the methods used, the types of costs and the patient populations of interest. In addition, methodological limitations were identified in some studies. Definitive conclusions are limited and highlight the need for better standardization of economic evaluations in this area. Further economic evaluations arising from well-designed RCTs would allow healthcare decision-makers to feel more confident in considering homecare interventions.
Keywords: homecare, hospital care, adults, older adults, economic evaluation
1. Introduction
The global population is living longer. According to the World Health Organization (WHO), by 2050, people ≥ 60 years are expected to amount to 2.1 billion [1]. However, many of these additional years are not spent in good health or free from disability. Consequently, health systems face increased expenses owing to greater demand [2]. This has sparked interest in ongoing care in the home environment.
Although population aging is a relevant factor that drives the concerns of health systems regarding new models of care, it is not the only one [3]. The demand for care models in the home environment is followed by other equally relevant and eligible health needs, such as care provided to premature babies, children with chronic illnesses and adults with multiple, chronic and degenerative diseases. Thus, the relevance of homecare (HC) services stands out in the current and future health agendas of all healthcare systems, aiming to contribute to the transformation of practices and the configuration of substitutive health networks [4,5].
The increase in HC in several countries follows the interest of those who run health systems in the de-hospitalization process, rationalization of the use of hospital beds, cost reduction and the organization of patient-centered care. Furthermore, this demand poses another challenge for health systems, contributing to a change in the focus on care and the environment provided, aiming for healthcare based on humanization [6,7].
Most people who require long-term care prefer to receive it at home [8]. As healthcare costs rise worldwide, HC represents an opportunity to reduce avoidable adverse events and costs. Furthermore, HC may also offer one means of reducing admission in the hospital demand that result in facilitating the more efficient use of inpatient beds [9].
Systematic reviews have previously been undertaken; however, these have not focused on the comparison between HC services vs. hospital care. In addition, none included only economic evaluations arising from randomized controlled trials. One systematic review indicated that HC was cost-saving when compared to other healthcare modes. However, this review included mainly comparative design studies [10]. Tappenden et al. evaluated the clinical effectiveness of home-based, nurse-led health promotion programs in the United Kingdom. Although they showed that these interventions were clinically effective, only three of the 11 included studies performed cost analyses [11]. Flemming et al. compared the cost-effectiveness of new or improved HC services with usual care and found across the six areas of focus that positive or cost-effective results were reported in two groups (alternative nursing care and reablement/restorative care) [12].
Cost-effectiveness studies are considered the gold standard for developing accurate estimates of the value of health interventions to inform decision making [13]. Thus, a broader evaluation of HC services with a critical judgment of the results will help in decision-making regarding the applicability of such services in a unified health system. Therefore, this study aimed to provide an overview of the cost-effectiveness of HC services compared with in-hospital care for adults and older adults.
2. Materials and Methods
2.1. Registration and Protocol
A protocol for this systematic review was registered on PROSPERO: International prospective register of systematic reviews website (Registration number: CRD42022308742) and the findings were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14] (see Table S1 for the PRISMA checklist).
2.2. Review Question
The guiding question of this systematic review was: Are homecare services offered to adults and older adults more cost-effective than hospital services?
2.3. Elegibility Criteria
The following inclusion criteria, based on the acronym PICOS, where the acronym represents population (P), intervention (I), comparison (C), outcomes (O) and, (S) study design were used to select studies: (P) studies performed with adults and older adults; (I) studies that addressed HC services (any form of home health care for any disease prevention and treatment, rehabilitation and palliation); (C) the comparison should be hospital care; (O) full economic evaluation examining both the costs and consequences (cost-minimization, cost-effectiveness and cost-utility analyses). Secondary outcomes included: mortality, hospitalizations, readmissions, symptom control, quality of life (QoL), satisfaction with care and costs in a disaggregated way (use of resources with their respective costs); (S) economic evaluations arising from randomized controlled trials (RCTs).
We excluded studies if the interventions targeted caregivers, including aspects of HC provided outside the home, such as in an outpatient hospital or clinic. In addition, we excluded studies in which the comparison was hospital day care. Studies presented only as abstracts with no subsequent full report of the results were also excluded.
2.4. Search Methods for the Identification of Studies
We comprehensively searched electronic databases for records of economic evaluations arising from RCTs of HC interventions compared with hospital care. We performed searches using the MEDLINE (Ovid), Embase (Ovid), Scopus, Web of Science, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and Cochrane Central Register of Controlled Trials (CENTRAL or Cochrane Library) databases from inception to 13 April 2022. The search strategy used was based on the PICO(S) scheme and used in combination with Boolean operators. Table S2 presents all of the used search terms in their combinations. We also searched the reference lists of studies that met the inclusion criteria and reviews to identify additional relevant studies. No restrictions were applied in terms of languages or dates.
2.5. Study Selection
Duplicates were identified using the Endnote X9 Program. All duplicates were removed before the study selection process. Thereafter, the results were transferred to Rayyan QCRI, a systematic review web app. First, a pair of researchers (C.C., A.C.S., M.H. and T.B.) independently screened the titles and abstracts of the found records. The full texts of potentially eligible records were retrieved and independently screened (C.C., M.H. and A.C.S) to confirm inclusion. Disagreements were resolved through discussion by all researchers.
2.6. Data Extraction and Risk of Bias Assessment
Pairs of authors (C.C., A.C.F., M.H., T.B., J.D., D.C. and A.C.) independently extracted data and assessed study quality using standardized, piloted data extraction forms in Covidence (a web-based systematic review software program).
For each trial, the following data were extracted: trial information (author, year of publication, country); type of economic evaluation; funding and conflict(s) of interest; population baseline characteristics (age, sex, etc.); details regarding interventions and comparators; time horizon (the period over which the costs and effects are measured); the economic method used; perspective; year of costs; results/outcomes; and sensitivity analysis results. When information regarding any of the above was unclear or incomplete, we attempted to contact the authors of the original reports to request further details by email.
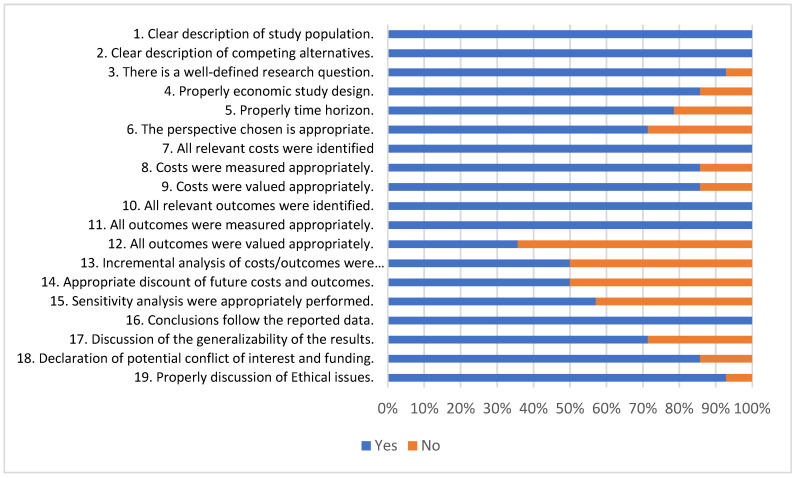
Regarding the economic evaluation, the quality appraisal of the studies was performed using the Consensus Health Economic Criteria (CHEC) list [15] that focuses only on the methodological quality of economic evaluations. The CHEC list was designed and is recommended for systematic reviews of trial-based economic evaluations. The tool consists of 19 yes-or-no questions for each category. For each question, “yes” was chosen if the study paid sufficient attention to a certain aspect and “no” if insufficient information was available in the article or in other published materials. Positive responses were scored as 1, whereas negative responses were scored as 0. The score for each item was summed and the total CHEC score was transformed to a percentage ranging from 0–100%. A critical appraisal plot (CHEC-list) was produced in Excel 2013.
Disagreements regarding data extraction and critical appraisal were resolved through discussion with all reviewers.
2.7. Data Synthesis
A PRISMA flowchart was used to synthesize the study selection process [14]. Since important differences regarding participants, interventions, diseases and follow-up period were found, a narrative synthesis was used to provide a descriptive summary of the participants’ characteristics and the findings from the included studies.
3. Results
3.1. Results of the Search
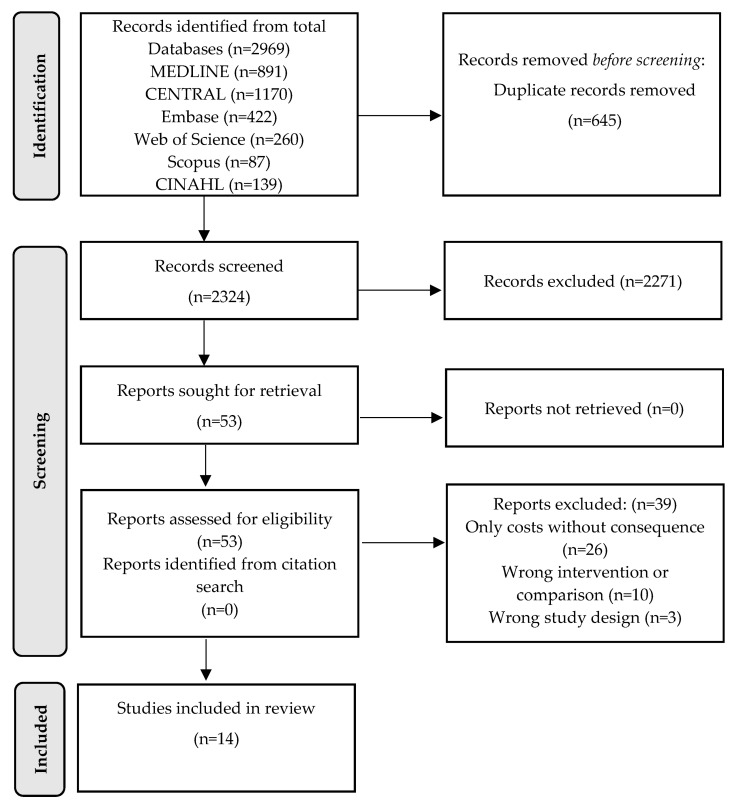
This literature search retrieved 2969 studies, of which 645 were removed as duplicates, leaving 2324 for title and abstract screening. Fifty-three potentially relevant references were obtained as the full text. At the full-text stage, 39 studies were excluded: 26 assessed only costs and not consequences, 10 did not fulfill the criteria for interventions or comparisons and three studies had the wrong study design. Finally, this review included 14 studies from which data were extracted. No studies were added from the reference lists of studies that met the inclusion criteria. A flow diagram of this process, according to PRISMA guidelines, is presented in Figure 1.
Figure 1.
PRISMA study flow diagram for search up to 13 April 2022.
3.2. Study Characteristics
Out the 14 studies, eight were conducted in the UK [16,17,18,19,20,21,22,23], three in the Netherlands [24,25,26], one from Sweden [27], one from Italy [28] and one from Iran [29]. The studies were mainly published before 2010. On grouping studies according to the International Classification of Diseases, we found that the most commonly studied illnesses corresponded to the circulatory system (n = 4) [16,17,27,28] and the respiratory system (n = 3) [19,24,25]. The number of participants in the trials varied from 31 to 1055. Six studies randomized older adult patients, two adults and the remainder included both young, middle-aged and older adults. The intervention and comparison covered different treatments related to the care required for the respective disease.
Five studies included home visits by specialist team [17,20,21,22,23,28,29], three studies included home visits by nurses (nursing care) [18,24,27] and three studies included visit by other specialists [16,19,26]. Additional intervention components included telemonitoring and nursing care [25].
Most of the included studies (n = 11) [16,17,18,19,20,21,22,23,24,25,26] received financial support from public healthcare or non-profit organizations. Two studies did not report funding sources [27,29] and one declared “no funding sources” [28].
The characteristics of the included studies are shown in Table 1.
Table 1.
Characteristics of the included studies.
| Study/Country | Disease | Intervention—Homecare | Comparison—Hospital | Sampling | Age Range | Funding |
|---|---|---|---|---|---|---|
| Certain infectious and parasitic diseases | ||||||
| Cohen et al. [16]/ UK | Recurrent or drug-resistant tuberculosis | Participants received home-based care from guardians trained to deliver intramuscular streptomycin. | Participants were admitted to the hospital for 60 days. | 205 | 30–44 | Public/Non-profit |
| Diseases of the circulatory system | ||||||
| Kalra et al. [17]/UK | Disabling stroke | Patients were managed in their own homes and care was provided by a specialist team (doctor, nurse and therapists), with support from district nursing and social services for nursing and personal care needs. Patients were under the joint care of the stroke physician and the GP. Each patient had an individualized, integrated care pathway outlining activities and the objectives of treatment, which were reviewed at weekly multidisciplinary meetings. This support was provided for a maximum of 3 months. | The stroke unit provided 24-h care delivered by a specialist multidisciplinary team based on clear guidelines for acute care, the prevention of complications, rehabilitation and secondary prevention. The stroke team involved management on general wards with specialist team support. The team undertook stroke assessments and advised ward-based nursing and therapy staff on acute care, secondary prevention and rehabilitation aspects. | 457 | 67–84 | Public/Non-profit |
| Patel et al. [27]/Sweden | Chronic heart failure | Patients are visited at home daily or on alternate days by the specialist nurse as determined by the patient’s health status. Home visits were terminated when a patient: (1) was symptomatically stable or improving; (2) had stable or falling weight; (3) had no signs of pulmonary rales; and (4) had no edema above the ankle. | The patients were treated in accordance with hospital treatment guidelines. | 31 | 67–87 | NA |
| Ricauda et al. [28]/Italy | First acute ischemic stroke | Patients received a HC program that emphasized a task- and context-oriented approach, which recommends that the patient perform guided, supervised and self-directed activities in a functional and familiar context. The standard daily intervention consisted of one visit by a physician, a nurse and a physical therapist. | The inpatient group received routine hospital rehabilitation services, which allocated physical therapists to patients assigned to both groups of the trial. | 120 | 74–89 | None |
| Taylor et al. [18]/ UK | Uncomplicated acute myocardial infarction | Patients were seen during hospital admission by a cardiac rehabilitation nurse and issued the Heart Manual to use over six consecutive weeks. | Patients attended outpatient classes once a week for 8–10 weeks. Classes lasted 2 h each and were conducted in groups of 8–10 people at the local hospital or, for a small number of patients, in one of the two community centers. | 104 | 51–76 | Public/Non-profit |
| Diseases of the respiratory system | ||||||
| Cox et al. [19]/UK | Chronic obstructive pulmonary disease | The intervention consisted of eight exercises (adapted to each participant’s capability). Four sessions over two weeks were delivered by a physiotherapist in the patient’s home. | A cycle ergometer was used to deliver exercises at hospital bedside. The prescription (cycle workload) was set by a physiotherapist. The patient completed 16 revolutions of the bike for both sets of limbs, three times a day for 5 consecutive days. | 58 | 55–79 | Public/Non-profit |
| Goossens et al. [24]/The Netherlands | Chronic obstructive pulmonary disease | For the first three days, all patients received usual hospital care. Starting on the fourth day, community nurses visited and provided care at least once or up to three times on the day of discharge and over the following three days. During the four days of home treatment, the emphasis was on recovering from exacerbation of symptoms. | Usual hospital care | 139 | 57–79 | Public/Non-profit |
| van den Biggelaar et al. [25]/The Netherlands | Neuromuscular disease or thoracic cage disorder | Patients received mechanical ventilation at home. | Patients started home mechanical ventilation in the hospital. | 96 | 42–70 | Public/Non-profit |
| Endocrine, nutritional and metabolic diseases | ||||||
| Jafary et al. [29]/Iran | Diabetic foot ulcers | Treatment was performed according to the clinical guidelines approved by Iran’s Ministry of Health. The home visit team consisted of a GP and 3 nurses. Following the initial home visit, additional home visits were conducted at least once a week. Patients could contact the HC providers when the need arose. | Conventional care at the hospital. | 120 | 48–73 | NA |
| Multiple health conditions | ||||||
| Coast et al. [20]/UK | Hospitalized but medically stable elderly patients | Patients able to receive early discharge from the hospital were allocated to home-based rehabilitative care provided by a multi-professional team (nurse, physiotherapist, occupational therapist and support workers). | Patients received routine hospital care with discharge at the usual time. | 241 | 72–84 | Public/Non-profit |
| Jones et al. [21]/UK | Mix of medical conditions | A GP maintained medical responsibility for 14 days. Multidisciplinary care (nurses, physiotherapists, occupational therapists, generic healthcare workers and cultural link worker) provided between four and 24 h of care per day. They provided access to equipment needed for home nursing such as hospital beds, mattresses, commodes, etc. | Acute hospital admission. | 199 | 77–89 | Public/Non-profit |
| Shepperd et al. [22]/UK | Mix of medical conditions | Care consisted of observation, the administration of (intravenous) drugs, nursing care (in addition to support from other professionals) 24 h a day in the patient’s home if necessary and the rehabilitation of patients at home. | Inpatient hospital care: patients recovering from a hip replacement, a knee replacement, or a hysterectomy; patients with chronic obstructive airway disease; and elderly patients with a mix of medical conditions. | 242 | 58–76 | Public/Non-profit |
| Singh et al. [23]/UK | Acute inpatient hospital care | The HC was based on an evaluation of CGA services received previously in the hospital and subsequently being provided at home. | An inpatient care group received CGA services. | 1055 | 76–90 | Public/Non-profit |
| Pregnancy, childbirth and the puerperium | ||||||
| Birnie et al. [26]/ The Netherlands |
High-risk pregnancies | A midwife performed a daily visit, conducted a cardiotocography and transmitted the tracings to the hospital. Women were seen weekly at the antenatal clinic. | Women were hospitalized and monitored daily. If necessary, they received additional diagnostics or treatment. | 150 | 24–37 | Public/Non-profit |
CGA: comprehensive geriatric assessment; COPD: chronic obstructive pulmonary disease; GP: general practitioner; HC: homecare; NA: not applicable.
3.3. Economic Evaluation
Eight studies performed a cost-effectiveness analysis [17,18,19,23,24,25,27,29] and six performed cost-minimization analyses [16,20,21,22,26,28]. The cost components were organized into three categories: direct medical, indirect and non-medical costs. Effectiveness was assessed in different ways and a range of outcome measures was used in the studies. The most commonly utilized was quality-adjusted life years (QALY), which was present in eight studies [17,18,19,23,24,25,27,29].
Eleven studies presented the cost perspective taken for the evaluation: only societal (n = 4) [16,17,25,29], only the public healthcare payer perspective (n = 2) [19,27] and five studies contained a combination of two perspectives [20,21,22,23,24]. Three studies did not report taking any perspective [18,26,28]. All studies had a time-horizon perspective and the period varied from days to 1.5 years. The most common time periods were three and six months, with four studies each.
Among the 14 studies included, HC, when compared with hospital care, was cost-saving in seven studies, cost-effective in two and more effective in one. For the management of exacerbations in COPD patients, there was no statistically significant difference between usual home and hospital care strategies [24]. However, exercise programs were cost-effective compared to usual care [19]. When comparing exercise programs, a hospital program was cost-saving (£796 per patient) despite the home-based program incremental effectiveness (0.04 QALY/patient) [19].
Four studies focused on diseases of the circulatory system, two assessed acute conditions (stroke and heart infarction) and two assessed chronic conditions (disabling stroke and heart failure) [17,18,27,28]. In three of them, HC strategies were cost-saving [17,27,28], even though Kalra’s results showed that stroke units (hospitals) were more effective (0.076 QALY/patient) [17].
For conditions that required acute care, including multiple events, the effectiveness of HC and hospital programs was similar [20,21,22,23]. However, hospital costs were higher, resulting in cost-saving HC strategies. The incremental costs of hospital programs were £205.58, £776 and £2840.00 per patient, respectively [20,21,23]. HC strategies for patients suffering from diabetic foot ulcers are cost-effective compared to hospital care. The incremental cost-effectiveness ratio (ICER) was US $117,300 per QALY [29].
Despite the effectiveness of HC and hospital treatment for patients requiring long-term injectable agents for the treatment of tuberculosis being similar, the hospital-at-home scheme was less costly than receiving care in the hospital—a cost difference of US $602.3 [16]. The same was observed in domiciliary antenatal fetal monitoring for high-risk pregnancies. Domiciliary monitoring is effective and reduces costs by one half [26].
Eight studies performed a sensitivity analysis [17,19,20,22,23,24,27,29]. In four of them, the results were not altered [19,20,23,29]. Goosens’s study [24] found that, from a societal perspective, the cost rose due to HC disappearing almost entirely. From a healthcare standpoint, the finding that HC led to cost savings was surrounded by almost no uncertainty. In Kalra’s study [17], if decision-makers were not willing to raise costs for QALY gains, there would be a 59% probability that HC would be the most cost-effective (i.e., optimal). This probability fell with increasing levels of willingness to pay for QALY gains, but remained higher than the other two strategies. In the work of Patel [22], sensitivity analysis altered the obtained values, but HC remained cost saving. Finally, reducing the length of hospital-at-home care changed the difference in total healthcare costs for patients with chronic obstructive airway disease.
All economic evaluations are described in Table 2.
Table 2.
Results of economic evaluation of included studies.
| Study | Economic Evaluation Type |
Effectiveness Outcomes |
Perspective/Time Horizon | Cost Description/Year of Costs | Costs | QALY | Cost-Effectiveness ICER/Cost/QALY |
Synthesis |
|---|---|---|---|---|---|---|---|---|
| Certain infectious and parasitic diseases | ||||||||
| Cohen et al. [16] | Cost-minimization analysis | Successful treatment (alive and upon receiving treatment) | Societal/ 7 weeks |
Direct medical; non-medical (food/diet, transportation, visits); indirect (income lost due to illness). Year: 2014 |
HC: US $498.0 Hosp: US $1100.3 Difference: US $ −602.3 |
Not reported | Not reported since effectiveness was similar | HC: cost-saving |
| Diseases of the circulatory system | ||||||||
| Kalra et al. [17] | Cost-effectiveness analysis | Mortality or institutionalization | Societal/12 months | Direct medical (hospital doctors, nursing care, physiotherapy, occupational therapy, psychologist, dentist, etc., consultations); non-medical (food/diet, visits, social work, companion). Year(s): 1997/1998 |
Mean costs HC: £6840 Hospital 1: £11,450 Hospital 2: £9527 Difference HC × Hospital 1: £4609.94 Difference HC × Hospital 2: £2686.78 Cost per day alive: HC: £36.07 Hospital 1: £37.98 Hospital 2: £50.90 Difference HC × Hospital 1: £ −1.91 Difference HC × Hospital 2: £ −14.83 |
HC: 0.221 Hospital: 0.297 Difference: 0.076 |
ICER for hospital £64,097 Homecare dominant Probability of avoiding death/institutionalization HC: 77.86 Hospital 1: 87.16 Hospital 2: 69.39 Cost per death/institutionalization avoided: HC: 0.46 Hospital 1: 0.44 Hospital 2: 0.73 |
Hospital: effective HC: cost-saving |
| Patel et al. [27] | Cost-utility analysis | QALY | Public health system/ 12 months |
Direct medical (nursing care, consultations); non-medical (transportation). Year: NA |
Home: €1122 Hospital: €5110 Difference: € −3988 |
Home: 0.71 Hospital: 0.64 |
Cost/QALY lower in home group, but values are not shown and the difference did not reach statistical significance. | HC: cost-saving |
| Ricauda et al. [28] | Cost-minimization analysis | Mortality;residual functional impairment;neurological deficits | NA/6 months | Direct medical (hospital doctors, nursing care, physiotherapy, occupational therapy, psychologist, dentist, etc., medication, labs/diagnosis). Year: NA |
Per day HC: US $163.0 Hospital: US $275.6 Difference: US $ −112.6 |
Not reported | Not reported since effectiveness was similar for all outcomes. | HC: cost-saving |
| Taylor et al. [18] | Cost-effectiveness analysis | QALY | NA/9 months | Direct medical (hospital doctors, nursing care, medication, labs/diagnosis); non-medical (transportation). Year(s): 2002/2003 |
HC: £3279 Hospital: £3201 Difference: £78 |
Home: 0.74 Hospital: 0.81 Difference: −0.06 |
Mean incremental cost per QALY: £ −644 | Difference not significant |
| Diseases of the respiratory system | ||||||||
| Cox et al. [19] | Cost-effectiveness analysis | QALY | Public health system/3 months | Direct medical (physiotherapy, occupational therapy, psychologist, dentist, etc., equipment); non-medical (transportation, visits, social work). Year(s): 2015/2016 |
HC: £4757 Hospital: £3961 Difference: £796 |
HC: 0.149 Hospital: 0.145 Difference: 0.04 |
ICER: HC and hospital dominant Probability more effective (QALYs) Home: −0.62 Hospital: −0.56 |
HC: more effective Hospital: cost-saving |
| Goossens et al. [24] | Cost-effectiveness and cost-utility | Incremental change in CCQ score; QALY |
Societal Public health system/3 months |
Direct medical (hospital doctors, nursing care, medication); non-medical (transportation); indirect (productivity losses); other (readmission). Year: 2009 |
Health care HC: €4129 Hospital: €4297 Difference: €168 Societal HC: €6304 Hospital: €5395 Difference: €880 |
HC: 0.170 Hospital: 0.175 Difference: −0.05 |
Health care perspective ICER: €31,111 Societal perspective ICER: Hospital dominant |
Difference not significant from either perspective |
| van den Biggelaar et al. [25] | Cost-effectiveness analysis | Change in arterial CO2; QoL | Societal/6 months | Direct medical (nursing care, physiotherapy, occupational therapy, psychologist, dentist, etc., equipment); non-medical. Year(s): 2017/2018 |
HC: €1500 Hospital: €4725 Difference: €3225 |
HC: 0.26 Hospital: 0.25 Difference: 0.01 |
Not reported | HC: cost-saving |
| Endocrine, nutritional and metabolic diseases | ||||||||
| Jafary et al. [29] | Cost-effectiveness analysis | QALY | Societal/6 months | Direct medical (hospital doctors, nursing care, medication); non-medical (transportation, visits); indirect (productivity losses). Year: 2017 |
HC: US $1545 Hospital: US $3891 Difference: US $ −2346 |
Home: 0.31 Hospital: 0.29 Difference: 0.02 |
ICER: −117.300 | HC: cost-effective |
| Multiple health conditions | ||||||||
| Coast et al. [20] | Cost-minimization analysis | QoL; satisfaction; physical functioning; length of stay; mortality | Individuals Public health system/3 months |
Direct medical (hospital doctors, nursing care, physiotherapy, occupational therapy, psychologist, dentist, etc., medication, labs/diagnosis, equipment); non-medical (food/diet, transportation, visits, social work, companion). Year: 1996 |
HC: £2516 Hospital: £3292 Difference: £ −776 |
Not reported | Not reported since effectiveness was similar | HC: cost-saving |
| Jones et al. [21] | Cost-minimization analysis | Mortality and change in health status (Barthel index, Sickness Impact Profile 68, EuroQol, Philadelphia Geriatric Morale Scale) | Individuals Public health system/8 months |
Direct medical (hospital doctors, nursing care, physiotherapy, occupational therapy, psychologist, dentist, etc.); non-medical (transportation, visits, social work). Year: NA |
HC: £3671.28 Hospital: £3876.86 Difference: £ −205.58 |
Not reported | Not reported since effectiveness was similar | HC: cost-saving |
| Shepperd et al. [22] | Cost-minimization analysis | QoL; mortality; Readmission |
Individuals Public health system/3 months |
NA Year(s): 1994/1995 |
Hip replacement HC: £911.39 Hospital: £815.70 Difference: £95.69 Knee replacement HC: £1461.62 Hospital: £1375.36 Difference: £86.26 Hysterectomy HC: £771.78 Hospital: £679.39 Difference: £92.39 Elderly medical HC: £1705.32 Hospital: £1388.76 Difference: £316.56 Chronic obstructive airways disease HC: £2379.67 Hospital: £1247.64 Difference: £1132.03 |
Not reported | Not reported since effectiveness was similar | Hospital: cost-saving for the studied conditions |
| Singh et al. [23] | Cost-effectiveness analysis | QALY; mortality; QoL |
Societal Public health system/6 months |
Direct medical (nursing care, physiotherapy, occupational therapy, psychologist, dentist, etc., medication, equipment); non-medical (transportation, visits); other (loss of income). Year(s): 1994/1995 |
HC: £19,067 Hospital: £21,907 Difference: £ −2840 |
Home: 0.245 Hospital: 0.247 Difference: −0.002 |
Probability of home intervention being cost-effective at threshold of £20,000 per QALY: 97% | HC: cost-effective |
| Pregnancy, childbirth and the puerperium | ||||||||
| Birnie et al. [26] | Cost-minimization analysis | Pretchtl neurologic optimality score: HC: 58.1 Hospital: 57.7 Mortality |
NA/Days until birth | Direct medical (nursing care, medication, labs/diagnosis); non-medical (food/diet, transportation, visits); other (monitoring sessions, professional home help, informal family care, premature pregnancy leave). Year: 1993 |
HC: US $1521 Hospital: US $3558 Difference: US $2037 |
Not reported | Not reported since effectiveness was similar for both outcomes | HC: cost-saving |
HC: homecare; QALY: quality-adjusted life years; QoL: quality of life.
3.4. Secondary Outcomes
All studies reported mortality as an outcome, but none detected differences between HC and the hospital. The same was observed for the seven studies that evaluated hospital readmissions [16,17,18,19,22,24,26]. Nine studies [17,18,19,20,21,22,23,24,25] applied a scale to evaluate quality of life (QoL). In one study, patients in the hospital-at-home group reported a significantly greater improvement in QoL compared to those in the hospital group [22].
Only two studies reported satisfaction as an outcome [17,20]. In one study, hospital-at-home patients perceived higher levels of involvement in decision-making [20]. In the other study, a significant difference favoring homecare was observed for being able to talk about problems with professionals, information on the nature and cause of stroke, the organization of care, support and the amount of contact with the specialist [17]. Adverse events were described in only four studies [16,19,28,29], three of them showing a higher number of adverse events in the hospital group [16,28,29]. Details about the secondary outcomes are listed in Table 3.
Table 3.
Results of secondary outcomes.
| Study | Mortality | Readmissions | QoL | Satisfaction | Adverse Events |
|---|---|---|---|---|---|
| Certain infectious and parasitic diseases | |||||
| Cohen et al. [16] | HC: 13/83 (15.7%) Hospital: 11/69 (13.9%) |
HC: 6/83 Hospital: 2/69 |
Not reported | Not reported | HC: 34/103 (33.0%) Hospital: 56/101 (55.4%) |
| Diseases of the circulatory system | |||||
| Kalra et al. [17] | HC: 21/144 (14.6%) SU: 13/152 (8.6%) ST: 34/149 (22.8%) |
HC: 13/144 (9.0%) SU: 8/152 (5.3%) ST: 11/149 (7.4%) |
HC: 75 SU: 80 ST: 80 |
Significant difference favoring HC for:
|
Not reported |
| Patel et al. [27] | HC: 2/13 (15%) Hospital: 2/18 (11%) |
Not reported | Not reported | Not reported | Not reported |
| Ricauda et al. [28] | Not reported | Not reported | Not reported | Not reported | HC: 28/60 (46.7%) Hospital: 34/60 (56.6%) |
| Taylor et al. [18] | HC: 4/60 (6.7%) Hospital: 1/44 (2.3%) |
HC: 9/60 (15%) Hospital: 6/44 (14%) |
HC: 4.66 Hospital: 4.87 |
Not reported | Not reported |
| Diseases of the respiratory system | |||||
| Cox et al. [19] | HC: 0/15 Hospital: 0/14 |
HC: 10/15 (66.7%) Hospital: 9/12 (75%) |
HC: 0.6 Hospital: 0.5 |
Not reported | HC: 15/15 (100%) Hospital: 13/14 (93.0%) |
| Goossens et al. [24] | HC: 1/70 Hospital: 1/69 |
HC: 17/70 (25%) Hospital: 17/69 (24%) |
HC: 0.677 Hospital: 0.672 |
Not reported | Not reported |
| van den Biggelaar et al. [25] | HC: 7/47 (15%) Hospital: 5/49 (10.2%) |
Not reported | HC: 50 Hospital: 51.7 |
Not reported | Not reported |
| Endocrine, nutritional and metabolic diseases | |||||
| Jafary et al. [29] | Within 6 months HC: 6/30 (20%) Hospital: 15/90 (16%) |
Not reported | Not reported | Not reported | HC: 0/30 (0.0%) Hospital: 16/90 (17.0%) |
| Multiple health conditions | |||||
| Coast et al. [20] | HC: 12/160 (7.5%) Hospital: 6/81 (7.4%) |
Not reported | Only reported the difference: −0.04 (−0.13 to 0.06) |
Excellent: HC: 50.7% (79/155) Hospital: 44.6% (31/70) |
Not reported |
| Jones et al. [21] | HC: 26/101 (25.7%) Hospital: 30/96 (31.3%) |
Not reported | HC: 0.64 Hospital: 0.63 |
Not reported | Not reported |
| Shepperd et al. [22] | Hip replacement: HC: 0/37 (0%) Hospital: 1/49 (2%) |
Hip replacement: HC: 2/37 (5%) Hospital: 1/49 (2%) |
Hip replacement: HC: 3.91 * Hospital: 3.2 * |
Not reported | Not reported |
| Knee replacement: HC: 0/47 (0%) Hospital: 0/39 (0%) |
Knee replacement: HC: 4/47 (9%) Hospital: 1/39 (3%) |
Knee replacement: HC: 3.35 Hospital: 3.25 |
|||
| Hysterectomy: HC: 0/114 (0%) Hospital: 0/124 (0%) |
Hysterectomy: HC: 7/114 (6%) Hospital: 13/124 (10%) |
Hysterectomy: HC: 3.18 Hospital: 3.34 |
|||
| Elderly medical: HC: 9/50 (18%) Hospital: 4/46 (9%) |
Elderly medical: HC: 13/50 (26%) Hospital: 5/46 (11%) |
Elderly medical: HC: 2.97 Hospital: 3.23 |
|||
| Chronic obstructive airway disease: HC: 3/15 (20%) Hospital: 3/17 (18%) |
Chronic obstructive airway disease: HC: 8/15 (53%) Hospital: 6/17 (35%) |
Chronic obstructive airway disease: HC: 3.54 Hospital: 2.82 |
|||
| Singh et al. [23] | HC: 114/673 (15%) Hospital: 58/326 (15%) |
Not reported | HC: 0.4334 Hospital: 0.4337 |
Not reported | Not reported |
| Pregnancy, childbirth and the puerperium | |||||
| Birnie et al. [26] | HC: 1/76 Hospital: 1/74 |
HC: 47/76 (61.8%) Hospital: 69/74 (93.2%) |
Not reported | Not reported | Not reported |
HC: homecare; QoL: quality of life.
3.5. Quality Appraisal of the Included Studies
Figure 2 summarizes the appraisal of reporting quality for each study using the CHEC list. Overall, there were some limitations to the quality of the identified studies, particularly concerning the poor consideration of the methods of outcome valuation (Q9), the discount on future costs and outcomes (Q14), the lack of incremental analysis and sensitivity analysis. As highlighted by Figure 2, all the studies fulfilled the items regarding the clear description of study population; the clear description of competing alternatives; the identification of all important and relevant outcomes; and the appropriated outcomes measures. Only two studies fulfilled all the assessed criteria [17,23]. Three studies fulfilled less than 70% of the assessed items [21,26,28]. See Table S3 for the details of quality appraisal of the included studies.
Figure 2.
Appraisal of economic evaluations using the quality CHEC list.
Q1. Is the study population clearly described?
Q2. Are competing alternatives clearly described?
Q3. Is a well-defined research question posed in an answerable format?
Q4. Is the economic study design appropriate to the stated objective?
Q5. Is the chosen time horizon appropriate for including the relevant costs and consequences?
Q6. Is the actual perspective chosen appropriate?
Q7. Are all important and relevant costs for each alternative identified?
Q8. Are all costs measured appropriately in physical units?
Q9. Are costs valued appropriately?
Q10. Are all important and relevant outcomes identified?
Q11. Are all outcomes measured appropriately?
Q12. Are outcomes valued appropriately?
Q13. Is an incremental analysis of costs and outcomes performed?
Q14. Are all future costs and outcomes discounted appropriately?
Q15. Are all important variables, whose values are uncertain, appropriately subjected to sensitivity analysis?
Q16. Do the conclusions follow from the data reported?
Q17. Does the study discuss the generalizability of the results to other settings and patient or client groups?
Q18. Does the article indicate that there is no potential conflict of interest with the study researcher(s) and/or funder(s)?
Q19. Are ethical and distributional issues discussed appropriately?
4. Discussion
Very few studies have considered the costs and outcomes of home healthcare interventions compared with hospital care for disease prevention, treatment, rehabilitation and palliation. The evidence suggests that home healthcare interventions are likely to be cost saving and as effective as hospital care interventions. However, the studies included in this review differ in terms of the methods used, types of costs and patient populations of interest. Thus, it was difficult to directly compare the individual results.
Although one might expect that, for acute emergency conditions or those related to surgical processes, the hospital would be the most cost-effective intervention, this review revealed that the studies showed similar effectiveness, except for Kalra’s study [17], where one of the options (hospitals) was more effective in treating stroke patients. In addition, in general, HC was cost-saving, except in the work of Shepperd [22]. This study was carried out in the 1990s in the UK, which was going through an important health system reform at the time, introducing the idea of care centered on individual needs [30]. This could be a possible explanation for the high cost of HC intervention. Furthermore, new technologies can lower the costs of HC.
Regarding effectiveness, results from other reviews found similar results and also report heterogeneity and scarcity of methodologically adequate studies. In a systematic review, Leong et al. showed that HC generally leads to similar or improved clinical outcomes compared to inpatient treatment [31]. For patients with decompensated heart failure, HC appears to increase the time to readmission and improve QoL compared with routine hospitalization. However, HC did not significantly reduce readmission or mortality [32]. In a systematic review of patients with chronic diseases who went to the emergency department, HC lowered the risk of hospital readmission and long-term care admission compared to in-hospital care. The mortality risk was similar between the two groups [33].
In terms of QoL, the findings were still similar. QoL is a broad and complex concept, defined as one’s perception of their position in life, culture and value systems in the context of life, as well as in relation to objectives, expectations, standards and concerns [34]. In this sense, obtaining a high QoL and a high level of HC services is challenging.
Despite the variety of diseases, perspectives, costs and outcomes, most studies have shown results favoring HC modalities. Nevertheless, it is necessary to understand and analyze each respective disease because it will impact demands that could be met at a better cost in the hospital environment. Important outcomes, such as adverse events and satisfaction, were assessed in a few studies. Care could emphasize practical wisdom in a close relationship with techno-scientific knowledge; that is, a set of instrumental actions considered adequate and correct by the actors involved. Hence, this implies considering human subjectivity, understanding the pursuit of happiness and ways of living throughout the course of illness [35].
A societal or health system perspective was adopted in most of the selected studies. Almost half of the study populations comprised older adults living in high-income countries. The societal impact differed between the retired and economically active populations. This should be considered in future research. With few exceptions, most diseases evaluated can have a significant impact on the productivity of the affected individuals or caregivers, both by impeding them from working and affecting mental well-being [36]. Decreased productivity can translate into lost income, which impacts people with illnesses and their families. Only two studies contained both the societal and health system perspectives [23,24]; however, if the inclusion of societal costs led to substantial changes in the outcomes, then this matter was poorly explored.
Notably, most of the included studies were conducted in the UK, which has a universal healthcare system called the National Health Service, as well as from the Netherlands, which has had a hybrid healthcare system (a multi-payer system based on managed competition between private insurers and providers) since 2006 [37,38]. Healthcare expenditure is rising worldwide and continues to be a concern for health systems [39]. There is an urgent need for cost-effectiveness assessments to support policies and actions. No studies have been performed in countries with only private health systems. There is apprehension about private equity firms that now own several of the largest HC chains in several countries [40]. The widespread use of predatory financial practices by these entities has raised concerns because they can prioritize profits over quality of care [41].
Finally, cost-effectiveness analysis was reduced when there was no integration between the levels of healthcare. An integrated healthcare system is essential to enable a connected, holistic view of the patient’s journey across different care settings such as hospitals, outpatient care and homes.
4.1. Strengths and Limitations
The strengths of this review include a registered protocol that addresses the items on the PRISMA checklist. Furthermore, we performed a comprehensive search strategy that was not limited by year or language. Two reviewers independently selected and extracted the studies and assessed their quality.
The studies were heterogeneous and there was considerable variation in their methods, outcomes and patient populations of interest, which made it difficult to compare them. In addition, important outcomes such as QoL, satisfaction and adverse events were not measured in most of the selected studies. Despite every effort being made to identify studies on this topic, the presence of publication bias cannot be excluded.
4.2. Future Research
Future studies should explore patient characteristics that impact the cost-effectiveness of home care, such as conditions of patients (acute or chronic conditions), age effect, household, financing model and coverage of national health systems. Further economic evaluations arising from well-designed RCTs with improved reporting would allow healthcare decision-makers to feel more confident in considering home healthcare interventions.
5. Conclusions
Current evidence for home healthcare interventions suggests that they are likely to be cost saving and as effective as hospital care interventions. Definitive conclusions are limited by quantity according to different conditions and quality, as this review identified some methodological constraints in the existing literature, highlighting the need for better standardization of economic evaluations in this area.
Acknowledgments
We would like to thanks to Livia Coelho for technical support.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20043373/s1, Table S1: PRISMA checklist; Table S2. Search strategy of the databases; Table S3. Quality appraisal of included studies. References [16,17,18,19,20,21,22,23,24,25,26,27,28,29] are cited in the supplementary materials.
Author Contributions
Conceptualization, C.C., A.C.S., J.D. and A.C.; methodology, C.C., A.C.S., J.D., A.C., M.H., T.B. and D.A.; validation, C.C., A.C.S., J.D., A.C., M.H., T.B. and D.A.; data curation, C.C., A.C.S., J.D., A.C., M.H., T.B. and D.A.; writing—original draft preparation, C.C., A.C.S., J.D. and A.C.; writing—review and editing, C.C. and R.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Brazilian National Council for Scientific and Technological Development (CNPq; grant #401904/2021-0). This funding source had no role in the design, execution, analysis, or interpretation of the data in this study.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.World Health Organization Fact sheet. 2022. [(accessed on 20 July 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
- 2.Collaborators G.B.D.A. Global, regional, and national burden of diseases and injuries for adults 70 years and older: Systematic analysis for the Global Burden of Disease 2019 Study. BMJ. 2022;376:e068208. doi: 10.1136/bmj-2021-068208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beard J.R., Bloom D.E. Towards a comprehensive public health response to population ageing. Lancet. 2015;385:658–661. doi: 10.1016/S0140-6736(14)61461-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rajao F.L., Martins M. Home Care in Brazil: An exploratory study on the construction process and service use in the Brazilian Health System. Cien Saude Colet. 2020;25:1863–1877. doi: 10.1590/1413-81232020255.34692019. [DOI] [PubMed] [Google Scholar]
- 5.Mendes E.V. As Redes de Atenção à Saúde [The Healthcare Networks] Organização Pan-Americana da Saúde; Brasília, Brazil: 2011. 549p [Google Scholar]
- 6.Veras R.P., Caldas C.P., Motta L.B., Lima K.C., Siqueira R.C., Rodrigues R.T., Santos L.M., Guerra A.C. Integration and continuity of Care in health care network models for frail older adults. Rev. Saude Publica. 2014;48:357–365. doi: 10.1590/S0034-8910.2014048004941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braga P.P., de Sena R.R., Seixas C.T., de Castro E.A., Andrade A.M., Silva Y.C. Supply and demand in home healthcare. Cien Saude Colet. 2016;21:903–912. doi: 10.1590/1413-81232015213.11382015. [DOI] [PubMed] [Google Scholar]
- 8.Foong H.Y., Siette J., Jorgensen M. Quality indicators for home- and community-based aged care: A critical literature review to inform policy directions. Australas J. Ageing. 2022;41:383–395. doi: 10.1111/ajag.13103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiao R., Miller J.A., Zafirau W.J., Gorodeski E.Z., Young J.B. Impact of Home Health Care on Health Care Resource Utilization Following Hospital Discharge: A Cohort Study. Am. J. Med. 2018;131:395–407 e35. doi: 10.1016/j.amjmed.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Fraser K.D. Are home care programs cost-effective? A systematic review of the literature. Care Manag. J. 2003;4:198–201. doi: 10.1891/cmaj.4.4.198.63696. [DOI] [PubMed] [Google Scholar]
- 11.Tappenden P., Campbell F., Rawdin A., Wong R., Kalita N. The clinical effectiveness and cost-effectiveness of home-based, nurse-led health promotion for older people: A systematic review. Health Technol. Assess. 2012;16:1–72. doi: 10.3310/hta16200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flemming J., Armijo-Olivo S., Dennett L., Lapointe P., Robertson D., Wang J., Ohinmaa A. Enhanced Home Care Interventions for Community Residing Adults Compared with Usual Care on Health and Cost-effectiveness Outcomes: A Systematic Review. Am. J. Phys. Med. Rehabil. 2021;100:906–917. doi: 10.1097/PHM.0000000000001734. [DOI] [PubMed] [Google Scholar]
- 13.Neumann P.J., Sanders G.D., Russell L.B., Siegel J.E., Ganiats T.G. Cost Effectiveness in Health and Medicine. 2nd ed. Oxford University Press; Oxford, UK: Oxford University Press; New York, NY, USA: 2017. 496p [Google Scholar]
- 14.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evers S., Goossens M., de Vet H., van Tulder M., Ament A. Criteria list for assessment of methodological quality of economic evaluations: Consensus on Health Economic Criteria. Int. J. Technol. Assess. Health Care. 2005;21:240–245. doi: 10.1017/S0266462305050324. [DOI] [PubMed] [Google Scholar]
- 16.Cohen D.B., Mbendera K., Maheswaran H., Mukaka M., Mangochi H., Phiri L., Madan J., Davies G., Corbett E., Squire B. Delivery of long-term-injectable agents for TB by lay carers: Pragmatic randomised trial. Thorax. 2020;75:64–71. doi: 10.1136/thoraxjnl-2018-212675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalra L., Evans A., Perez I., Knapp M., Swift C., Donaldson N. A randomised controlled comparison of alternative strategies in stroke care. Health Technol. Assess. 2005;9:1–79. doi: 10.3310/hta9180. [DOI] [PubMed] [Google Scholar]
- 18.Taylor R.S., Watt A., Dalal H.M., Evans P.H., Campbell J.L., Read K.L., Mourant A.J., Wingham J., Thompson D.R., Pereira Gray D.J. Home-based cardiac rehabilitation versus hospital-based rehabilitation: A cost effectiveness analysis. Int. J. Cardiol. 2007;119:196–201. doi: 10.1016/j.ijcard.2006.07.218. [DOI] [PubMed] [Google Scholar]
- 19.Cox M., O’Connor C., Biggs K., Hind D., Bortolami O., Franklin M., Collins B., Walters S., Wailoo A., Channell J., et al. The feasibility of early pulmonary rehabilitation and activity after COPD exacerbations: External pilot randomised controlled trial, qualitative case study and exploratory economic evaluation. Health Technol. Assess. 2018;22:1–204. doi: 10.3310/hta22110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coast J., Richards S.H., Peters T.J., Gunnell D.J., Darlow M.A., Pounsford J. Hospital at home or acute hospital care? A cost minimisation analysis. BMJ. 1998;316:1802–1806. doi: 10.1136/bmj.316.7147.1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones J., Wilson A., Parker H., Wynn A., Jagger C., Spiers N., Parker G. Economic evaluation of hospital at home versus hospital care: Cost minimisation analysis of data from randomised controlled trial. BMJ. 1999;319:1547–1550. doi: 10.1136/bmj.319.7224.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shepperd S., Harwood D., Gray A., Vessey M., Morgan P. Randomised controlled trial comparing hospital at home care with inpatient hospital care. II: Cost minimisation analysis. BMJ. 1998;316:1791–1796. doi: 10.1136/bmj.316.7147.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh S., Gray A., Shepperd S., Stott D.J., Ellis G., Hemsley A., Khanna P., Ramsay S., Schiff R., Tsiachristas A., et al. Is comprehensive geriatric assessment hospital at home a cost-effective alternative to hospital admission for older people? Age Ageing. 2022;51:afab220. doi: 10.1093/ageing/afab220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goossens L.M., Utens C.M., Smeenk F.W., van Schayck O.C., van Vliet M., van Litsenburg W., Braken M.W., Rutten-van Molken M.P. Cost-effectiveness of early assisted discharge for COPD exacerbations in The Netherlands. Value Health. 2013;16:517–528. doi: 10.1016/j.jval.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 25.van den Biggelaar R.J.M., Hazenberg A., Cobben N.A.M., Gaytant M.A., Vermeulen K.M., Wijkstra P.J. A Randomized Trial of Initiation of Chronic Noninvasive Mechanical Ventilation at Home vs In-Hospital in Patients with Neuromuscular Disease and Thoracic Cage Disorder: The Dutch Homerun Trial. Chest. 2020;158:2493–2501. doi: 10.1016/j.chest.2020.07.007. [DOI] [PubMed] [Google Scholar]
- 26.Birnie E., Monincx W.M., Zondervan H.A., Bossuyt P.M., Bonsel G.J. Cost-minimization analysis of domiciliary antenatal fetal monitoring in high-risk pregnancies. Obstet. Gynecol. 1997;89:925–929. doi: 10.1016/S0029-7844(97)00150-6. [DOI] [PubMed] [Google Scholar]
- 27.Patel H., Shafazand M., Ekman I., Hojgard S., Swedberg K., Schaufelberger M. Home care as an option in worsening chronic heart failure -- a pilot study to evaluate feasibility, quality adjusted life years and cost-effectiveness. Eur. J. Heart Fail. 2008;10:675–681. doi: 10.1016/j.ejheart.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 28.Ricauda N.A., Tibaldi V., Marinello R., Bo M., Isaia G., Scarafiotti C., Molaschi M. Acute ischemic stroke in elderly patients treated in Hospital at Home: A cost minimization analysis. J. Am. Geriatr. Soc. 2005;53:1442–1443. doi: 10.1111/j.1532-5415.2005.53433_5.x. [DOI] [PubMed] [Google Scholar]
- 29.Jafary M.R., Amini M.R., Sanjari M., Aalaa M., Goudarzi Z., Najafpour Z., Mohajeri Tehrani M.R. Comparison home care service versus hospital-based care in patients with diabetic foot ulcer: An economic evaluation study. J. Diabetes Metab. Disord. 2020;19:445–452. doi: 10.1007/s40200-020-00527-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanaka O.Y., Oliveira V.E. Reforms and organization of the British National Health System: Lessons to the Brazilian National Health System. Saude Soc. 2007;16:7–17. doi: 10.1590/S0104-12902007000100002. [DOI] [Google Scholar]
- 31.Leong M.Q., Lim C.W., Lai Y.F. Comparison of Hospital-at-Home models: A systematic review of reviews. BMJ Open. 2021;11:e043285. doi: 10.1136/bmjopen-2020-043285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qaddoura A., Yazdan-Ashoori P., Kabali C., Thabane L., Haynes R.B., Connolly S.J., Van Spall H.G. Efficacy of Hospital at Home in Patients with Heart Failure: A Systematic Review and Meta-Analysis. PLoS ONE. 2015;10:e0129282. doi: 10.1371/journal.pone.0129282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arsenault-Lapierre G., Henein M., Gaid D., Le Berre M., Gore G., Vedel I. Hospital-at-Home Interventions vs In-Hospital Stay for Patients with Chronic Disease Who Present to the Emergency Department: A Systematic Review and Meta-analysis. JAMA Netw. Open. 2021;4:e2111568. doi: 10.1001/jamanetworkopen.2021.11568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995;41:1403–1409. doi: 10.1016/0277-9536(95)00112-K. [DOI] [PubMed] [Google Scholar]
- 35.Ayres J.R.C.M. Cuidado e humanização das práticas de saúde [Care and humanization of health practices] In: Deslandes S.F., editor. Humanização dos Cuidados em Saúde: Conceitos, Dilemas e Práticas [Humanization of Health Care: Concepts, Dilemmas and Practices] Editora Fiocruz; Rio de Janeiro, Brazil: 2006. pp. 49–83. [Google Scholar]
- 36.Fouad A.M., Waheed A., Gamal A., Amer S.A., Abdellah R.F., Shebl F.M. Effect of Chronic Diseases on Work Productivity: A Propensity Score Analysis. J. Occup. Environ. Med. 2017;59:480–485. doi: 10.1097/JOM.0000000000000981. [DOI] [PubMed] [Google Scholar]
- 37.Hiam L., Orcutt M., Yates R. Universal health coverage in the UK. BMJ. 2019;367:l7054. doi: 10.1136/bmj.l7054. [DOI] [PubMed] [Google Scholar]
- 38.Kroneman M., Boerma W., van den Berg M., Groenewegen P., de Jong J., van Ginneken E. The Netherlands: Health system review. Health Syst. Transit. 2016;18:1–240. [PubMed] [Google Scholar]
- 39.World Health Organization . Global Spending on Health 2020: Weathering the Storm. World Health Organization; Geneva, Switzerland: 2020. 84p [Google Scholar]
- 40.Harrington C., Jacobsen F.F., Panos J., Pollock A., Sutaria S., Szebehely M. Marketization in long-term care: A cross-country comparison of large for-profit nursing home chains. Health Serv. Insights. 2017;10:1178632917710533. doi: 10.1177/1178632917710533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Corlet Walker C., Druckman A., Jackson T. A critique of the marketisation of long-term residential and nursing home care. Lancet Healthy Longev. 2022;3:e298–e306. doi: 10.1016/S2666-7568(22)00040-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.