Abstract
Synthesizing evidence to examine changes in suicide-related outcomes before and during the pandemic can inform suicide management during the COVID-19 crisis. We searched 13 databases as of December 2022 for studies reporting both the pre- and peri-pandemic prevalence of suicidal ideation, suicide attempts, or rate of death by suicide. A random-effects model was used to pool the ratio of peri- and pre-pandemic prevalence of suicidal ideation and attempt (Prevalence Ratio—PR) and rate of death by suicide (Rate Ratio; RR). We identified 51, 55, and 25 samples for suicidal ideation, attempt, and death by suicide. The prevalence of suicidal ideation increased significantly among non-clinical (PR = 1.142; 95% CI: 1.018–1.282; p = 0.024; k = 28) and clinical (PR = 1.134; 95% CI: 1.048–1.227; p = 0.002; k = 23) samples, and pooled estimates differed by population and study design. Suicide attempts were more prevalent during the pandemic among non-clinical (PR = 1.14; 95% CI: 1.053–1.233; p = 0.001; k = 30) and clinical (PR = 1.32; 95% CI: 1.17–1.489; p = 0.000; k = 25) participants. The pooled RR for death by suicide was 0.923 (95% CI: 0.84–1.01; p = 0.092; k = 25), indicating a nonsignificant downward trend. An upward trend of suicidal ideation and suicide attempts was observed during the COVID-19 pandemic, despite suicide rate remaining stable. Our findings suggest that timely prevention and intervention programs are highly needed for non-clinical adult population and clinical patients. Monitoring the real-time and long-run suicide risk as the pandemic evolves is warranted.
Keywords: suicidal ideation, suicide attempt, death by suicide, COVID-19 pandemic, meta-analysis
1. Introduction
Suicide constitutes a serious public health issue. Humans are usually vulnerable in the face of traumas such as wars and natural disasters, even choosing to end their own lives [1,2]. Several meta-analyses have examined suicide-related outcomes during infectious disease epidemics. The associations between epidemics and increased suicide risk are poorly supported [2,3,4], though a few review studies have reported higher suicide rates among older adults during SARS [4,5], more suicidal thoughts during an epidemic [2], and increased suicide attempts during SARS and Ebola [5]. It is unknown whether the COVID-19 pandemic and its consequences contribute to the rise of suicide risk. This study synthesized robust evidence to examine the potential changes in suicidal ideation, suicide attempt, and suicide before and during the COVID-19 pandemic.
The suicide risk was expected to be alarmingly severe over the short or long run following the outbreak of the COVID-19 pandemic, due to widespread and prolonged economic, social, health, and psychological vulnerability [6,7]. A few primary studies found an overall increase in the prevalence of suicidal ideation and attempts, and in the rate of death by suicide during the pandemic period compared with the pre-pandemic period [8,9,10], while other studies found a decreased trend [11,12,13], and some reported an overall stable trend [14,15,16]. Suicide studies during the pandemic tend to be methodologically poor [17], and high-quality evidence from an interrupted time-series study covering 33 countries showed no significant increases in suicide death in most countries/regions [18]. After synthesizing three studies, Prati et al. [19] found that the effect of the COVID-19 lockdown on suicide risk among the general population was not significant. Another meta-analysis [20] also indicated that the prevalence of suicidal behaviors and suicidal ideation did not increase significantly among youth from the general population and emergency department. In contrast, a living systematic review that included studies up to October 2020 found that the prevalence of suicidal ideation increased among COVID-19 patients, despite the fact that suicidal presentations in hospitals decreased [21]. Aligned with the upward trend found by a systematic review [22], the pooled prevalence of suicidal ideation and suicide attempt were estimated to be 10.81–12.1% and 4.86%, respectively [23,24], which were higher compared to the rates reported by pre-pandemic studies. Nevertheless, most of the existing reviews lack quantitative evaluation using intertemporal data [3,21,23], and the only meta-analysis comparing pre- and peri-pandemic prevalence included only young people [20]. As suicide outcomes may vary across populations while the pandemic progresses, it is necessary to keep track of suicidality and monitor the impact of the pandemic on suicide-related outcomes [17,25].
Suicide risk varies according to biological, clinical, psychological, social, cultural, and environmental factors [26,27]. For example, age and sex has shown mixed effects, so there is no consensus regarding whether young people or females are at a higher risk for suicide than others [28]. Financial loss and unemployment status drives suicide-related consequences [29]. The reporting styles (e.g., self-report or clinical interview) affects the accuracy of outcomes [28], and different timeframes for evaluation (a past period when occurrence of symptoms was measured, e.g., the past two weeks or lifetime) can also lead to different results [30]. Democracy of the government and COVID-19 pandemic-related variables were risk factors for developing suicidal ideation and suicidal behaviors during the COVID-19 pandemic in previous meta-analyses [23,31]. Therefore, investigating the factors that make one more vulnerable to suicide in the face of the pandemic is crucial for informing suicide management under the pandemic context.
This study aimed to (a) evaluate the impact of the COVID-19 pandemic on suicide by examining whether the prevalence of suicidal ideation and suicide attempt and the rate of suicide death change before and after the pandemic, and (b) to examine the potential moderators for effect sizes via subgroup analysis and meta-regression. Specifically, suicidal ideation is defined as thoughts about ending one’s own life with deliberate consideration (passive ideation) or the planning of possible techniques (active ideation); suicide attempt refers to an attempt to end one’s life that may lead to death; death by suicide is the act of intentionally causing one’s own death [32]. To investigate what factors could affect the trend of suicide-related outcomes, this meta-analysis examined the effect of study-level variables (i.e., study design, reporting style, timeframe for measurement, time for data collection, and risk of bias score), participant characteristics (i.e., population type and sex distribution), economic index (i.e., changes in gross domestic product and unemployment rate before and during the pandemic), and government-level COVID-19 index (i.e., resilience score, stringency index, containment and health index, and economic support index) on changes in the prevalence of suicidal ideation, suicide attempt, and death by suicide.
2. Methods
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist (Table S1) [33] and Meta-Analysis of observational studies in epidemiology guidelines [34]. The meta-analysis protocol was registered on PROSPERO (CRD42022326575; https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022326575; accessed on 8 December 2022).
2.1. Search Strategy
Two team members systematically searched for relevant literature in 13 electronic databases: PubMed, Web of Science, EMBASE, CINAHL, Academic Search Premier, PsycINFO, PsycARTICLES, Psychology and Behavioral Sciences Collection, WHO COVID database, China National Knowledge Infrastructure, Wanfang, and CQVIP. Preprint articles published on Medrxiv servers were also searched. The search covered literature published up to December 2022. The search terms were built following the CoCoPop mnemonic [35]. As we had no restrictions on population, there were no specific search terms for Pop: Condition (suicid* OR “suicidal ideation” OR “suicidal thoughts” OR “suicidal plan” OR “suicide attempt” OR “completed suicide” OR “death by suicide”) AND Context (“COVID*” OR coronavirus OR “2019-ncov” OR “SARS-CoV-2” OR “cov-19” OR “2019 pandemic”). Corresponding Chinese search terms were used in Chinese databases. In addition, the references of identified studies and relevant review articles were screened to expedite the identification of eligible research. An example of search can be found in File S1.
2.2. Inclusion and Exclusion Criteria
Inclusion criteria were that studies (a) reported the prevalence of at least one form of suicide-related outcome (i.e., suicidal ideation/thoughts, suicide attempt, and completed suicide), or sufficient information to compute these variables; (b) used a repeated cross-sectional (i.e., pseudo-longitudinal; multiple assessments on different samples), longitudinal (multiple assessments on the same sample), or retrospective design providing at least one set of data for pre- and peri-pandemic periods (as defined by the study); (c) included measurement of suicidal ideation/thoughts and attempts of participants and/or analyzed country-level or regional data for suicide death among the general population; (d) were peer-reviewed journal articles or preprints with full text available; and (e) were written in English or Chinese.
Exclusion criteria were that studies (a) were review articles, case reports, commentary, books, conference papers, or other documents that did not present empirical findings with detailed method illustrations; (b) had no sufficient data to calculate the effect sizes; and (c) were duplicate sources.
2.3. Selection Procedure and Data Extraction
All the searched articles retrieved from the databases were imported to EndNote 20 for reference management. After removing the duplicates, the remaining articles written in English were exported to ASReview version 0.18. (https://asreview.nl/; accessed on 8 December 2022), an open-source machine learning program, for efficient title and abstract screening [36], and Chinese articles were screened manually. We selected the default combination of naive Bayes, maximization, and TF–IDF (term frequency–inverse document frequency) as the active learning model, which can produce consistently good results across many datasets [36]. To train the active learning model, the authors pre-selected relevant and irrelevant articles from the imported literature set. The ASReview presented the article titles and abstracts in order of relevance, and the authors continued to judge the relevance of articles successively until 50 consecutive irrelevant articles were marked in a row [37]. Finally, two team members applied the inclusion and exclusion criteria to independently review the full texts of the remaining studies to identify the eligible ones. Any disagreements between the two reviewers were resolved by discussion with the PI.
The following information was extracted: (a) identification of the study (i.e., title, first author’s name, publication year, country/region); (b) methodological characteristics (i.e., study design, sample size, definitions of pre- and peri-pandemic period, assessment approach for suicidal ideation and attempt/sources of death data,); (c) sample characteristics (i.e., population type, age and female proportion); and (d) outcome (i.e., prevalence/number of participants reporting suicidal ideation and/or suicide attempt for each period, or prevalence ratio comparing pre- and peri-pandemic assessment, rate/number of suicide death for both periods, or rate ratio comparing pre- and peri-pandemic data). Coding information varied slightly for studies reporting suicidal ideation, attempt, and death by suicide. In case of insufficient information on the published article, we contacted the authors via email. To consider financial factors, we retrieved data of gross domestic product/gross state product and unemployment rates [38,39,40,41] for both the pre- and peri-pandemic periods as defined by each included study, and calculated the ratio (peri/pre) to see how changes in financial factors would link to the variation in suicide rates. In addition, to monitor the impact of government reaction on suicide rate, we derived a resilience score (defined as an average score of reopening progress, COVID status, and quality of life in a country during the pandemic) from Bloomberg’s Covid Resilience Ranking [42] for the latest data (29 June 2022), and COVID-19 government response indexes (i.e., stringency index, containment and health index, and economic support index) from the COVID-19 Government Response Tracker [43] for the latest data upon our analysis (9 December 2022). Two team members coded the included studies independently, and discrepancies were resolved through discussion with the PI.
2.4. Risk of Bias Assessment
The Joanna Briggs Institute (JBI) Critical Appraisal Instrument for prevalence studies was used to assess the risk of bias [35]. This instrument consists of nine items examining bias from a few factors (e.g., sample frame, sampling method, sample size, sample description, data analysis, measurement scale, and response rate). Each item can yield a score of 1 (the absence of bias) or 0 (the presence of bias). The total score ranged from 0 to 9, with a higher score indicating a lower risk of bias. Two members rated each study independently, and all disagreements between the two raters were resolved via discussion with the PI.
2.5. Statistical Analysis
Prevalence ratio (PR) or rate ratio (RR) represented the measure of effect size to examine the changes between the pre- and peri-pandemic periods in suicidal ideation, suicide attempt, and death by suicide. Specifically, prevalence ratios for suicidal ideation and attempt were calculated using event prevalence/count and sample size before and during the pandemic. For suicide death data, single estimate of the rate ratio with 95% CI for every included sample can be (a) directly extracted from publications or (b) calculated using rates of suicide death per 100,000 people in pre- and peri-pandemic periods [44]. To accommodate different types of input data, Comprehensive Meta-Analysis version 2.0 was used to conduct meta-analysis.
A random-effects model was used to pool PR or RR reported by each sample. We employed an index of Cochran’s Q, Tau2, and I2 statistics to test heterogeneity, with a p value of <0.05 for Q, Tau2, and I2 > 50% indicating significant between-study heterogeneity [45]. Publication bias was determined through visual inspection of the asymmetry of the funnel plot and Egger’s regression test [46]. Sensitivity analysis was conducted by omitting studies one by one (leave-one-out method) and excluding the studies with quality score ranked below 25% of the total before recalculating the pooled estimate, to determine the robustness of results [47].
Among our included samples, there were unneglectable heterogeneities regarding clinical and methodological characteristics. Some of the samples consisted of participants recruited from non-clinical settings (e.g., college or general population), and these were mainly prospective studies using self-report methods to measure suicidal outcomes, while the other samples were from clinical settings (e.g., emergency or psychiatric departments) whose suicide-related data were retrospectively extracted from medical diagnosis. Based on previous studies, the prevalence of suicidal ideation and suicide attempt can be different between individuals from non-clinical settings and clinical settings during both pre- and peri-pandemic periods [20,21,48,49]. Considering these differences in physical or mental health conditions, patterns of changes in suicide-related outcomes, and several methodological characteristics, the prevalence ratio for suicidal ideation and suicide attempts was analyzed by non-clinical and clinical samples. In general, the non-clinical sample refers to participants recruited from community and non-medical settings (e.g., college students and the general population), and the clinical sample refers to participants recruited from medical settings (e.g., patients from the emergency and psychiatric departments).
To determine the source of heterogeneity, we conducted subgroup analysis and meta-regression. Specifically, we used a mixed effect model in subgroup analysis, where a random-effects model was used to pool samples within each subgroup, and a fixed effect model was used to pool the subgroup to yield the overall estimates. Meta-regression was run under the random-effects model to examine the effects of continuous variables on ratio. For studies reporting the pre- and peri-pandemic prevalence of suicidal ideation and/or attempt, population group (adolescent, younger group, general population/adult, or special group), study design (repeated cross-sectional, longitudinal, or retrospective), method (self-report or diagnosis) and timeframe (≤2 weeks or >2 weeks) for measuring suicidal outcomes, data collection (March–August 2020, September 2020–January 2021, or February 2021+), female percentage and risk of bias score were considered as potential moderators for effect sizes. Specifically, time for data collection was divided into 6-month intervals beginning from the onset of the pandemic to capture the changes in the global pandemic situation according to data from the World Health Organization [50]. In addition, we examined the impact of changes in GDP (Peri/Pre), unemployment rate (Peri/Pre), and several government-level COVID-19 indexes (i.e., resilience score, stringency index, containment and health index, economic support index) on the ratio of death by suicide.
3. Results
3.1. Study Characteristics
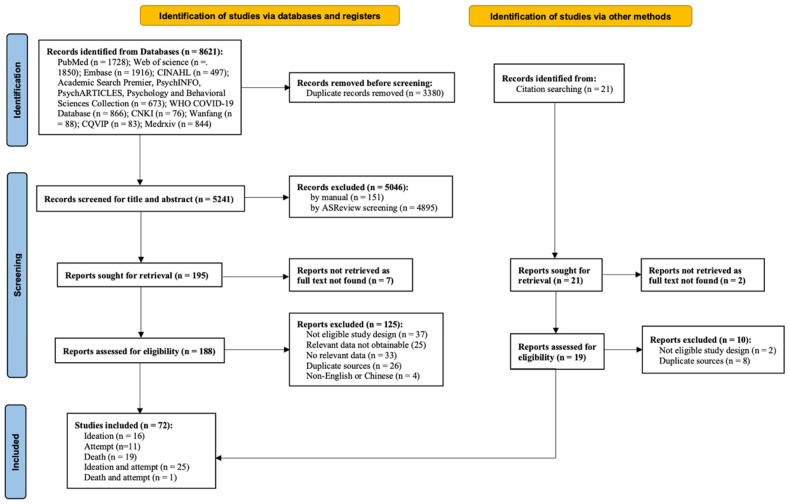
A total of 8642 studies were screened, with 72 studies (131 samples) meeting the inclusion criteria. Among them, 16 [10,11,51,52,53,54,55,56,57,58,59,60,61,62,63,64], 11 [65,66,67,68,69,70,71,72,73,74,75], and 19 [8,13,14,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91] only addressed changes in suicidal ideation, suicide attempt, and death by suicide, respectively; 25 [9,12,15,16,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112] reported both changes in suicidal ideation and attempt, and one study [113] reported both changes in death and attempt. The flow diagram of the study is depicted in Figure 1. The specific research information for ideation and attempt samples and death samples is shown in Table 1 and Table 2, respectively. Considering the unneglectable differences between non-clinical and clinical conditions, results for suicidal ideation and suicide attempt were reported separately based on the study settings. Specifically, the non-clinical sample was composed of adolescents, high school students, college students, the general population, hotline callers and military veterans, as stated by each included study; the clinical sample included pediatric and adult patients from emergency, psychiatric emergency, and inpatient departments, and those with certain medical conditions (i.e., obesity and eating disorder), as specified by each included study.
Figure 1.
PRISMA flow chart.
Table 1.
Characteristics for studies reporting suicidal ideation and suicide attempt.
| Study | Country | Study Design | Population Type | Sample Size | Participant Characteristic | Time Range | Outcome | Measurement | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean Age/Age Group | Female% | Pre-Pandemic Period | Peri-Pandemic Period | |||||||
| Acharya et al., 2022 [69] | India | Retrospective | Indoor Patients With Cut Throat Injury | Pre (10); Peri (14) | 25 (N = 17); 35 (N = 2); 45 (N = 4); 55 (N = 1) | 4.16% | Sept. 1st, 2019–Feb. 28th, 2020 | Mar. 1st–Aug. 31st for 2020 | Attempt | Diagnosis (Identified by tentative cut mark) |
| An et al., 2022 [58] | China | Retrospective | Hotline Callers | Pre (4940); Peri (5550) | Pre: <30 (76%), >30 (24%); Peri: <30 (74.4%), >30 (25.6%) | Pre (52.7%); Peri (60.6%) | Jan. 21st–Jun. 30th for 2019 | Jan. 21st–Jun. 30th for 2020 | Ideation | Self-report (Assessed by asking the caller Have you repeatedly thought about taking your life or hurting yourself in the last two weeks? Or have you felt too tired and without meaning to continue to live in the last two weeks? |
| Ayuso-Mateos et al., 2021 [51] | Spain | Longitudinal | General Population | 1103 | 54.82 | 64.8% | Jun. 17th 2019–Mar. 14th 2020 | May 21st 2020–Jun. 30th 2020 | Ideation | Self-report (An item of Composite International Diagnostic Interview: Whether the participant had had suicidal thoughts in the previous 12 months/30 days) |
| Berardelli et al., 2021 [92] | Italy | Retrospective | Psychiatric Patients | Pre (315); Peri (317) | 42.25 | 49.2% | May 2019–Mar. 9th 2020 | Mar. 10th–Dec. 2020 | Ideation Attempt |
Diagnosis (definition: thoughts about wishing to be dead or active thoughts of wanting to end one’s life) Diagnosis (Definition: a non-fatal, self-directed, potentially injurious behavior with an implicit or explicit intent to die; the behavior may or may not result in injury, and the intensity may vary, but the decision to act out the lethal intent must be present) |
| Berger et al., 2022 [59] | Switzerland | Retrospective | Emergency Psychiatric Adolescent Patients | Pre (109); Peri 1 (86); Peri 2 (164) | Pre (14.89); Peri 1 (14.81); Peri 2 (14.41) | Pre (56.6%); Peri 1 (57%); Peri 2 (64.2%) | Mar. 1st–Apr. 30th for 2019 | Mar. 1st–Apr. 30th for 2020; Mar. 1st–Apr. 30th for 2021 | Ideation | Diagnosis (Medical record) |
| Boldrini et al., 2021 [65] | Italy | Retrospective | Psychiatric Patients | Pre (3270); Peri 1 (589); Peri 2 (691) | 45.4 | 52.70% | March 1st–Jun. 30th for 2018–2019 | Mar. 1st–Apr. 30th for 2020; May 1st–Jun. 30th for 2020 | Attempt | Diagnosis (Medical record) |
| Bountress et al., 2022 [52] | United State | Longitudinal | College Students | 897 | 18.49 (Baseline) | 78.6% | Spring of 2019 | May 7th 2020–Jul. 17th 2020 | Ideation | Self-report (a Symptom Checklist-90 Revised: participants answered whether they had thought about killing themselves by yes or no). |
| Brailovskaia et al., 2021 [93] | Germany | Repeated Cross-sectional | College Students | Pre: 2016 (105); 2017 (117); 2018 (108); 2019 (154); Peri: 2020 (180) | Pre: 2016 (22.51); 2017 (22.53); 2018 (20.59); 2019 (21.98); Peri: 2020 (21.33) | Pre: 2016 (81.9%); 2017 (78.6%); 2018 (73.1%); 2019 (84.4%); Peri: 2020 (73.3%) | Oct.–Dec. for 2016–2019 | Oct.–Dec. for 2020 | Ideation Attempt |
Self-report (a Suicidal Behaviors Questionnaire-Revised: How often have you thought about killing yourself in the past year?) Self-report (A Suicidal Behaviors Questionnaire-Revised: Have you ever attempted suicide, and really hoped to die?) |
| Brausch et al., 2022 [102] | United State | Repeated Cross-sectional | High School Students | Pre (695); Peri (206) | Pre (15.5); Peri (15.6) | Pre (54.8%); Peri (57.8%) | 2018–2019 | 2020–2021 | Ideation Attempt |
Self-report (self-injurious thoughts and behaviors interview—short form; past year) |
| Caballero-Bermejo et al., 2022 [70] | Spain | Retrospective | Emergency Patients | Pre (528); Peri 1 (299); Peri 2 (355) | Pre (31.4); Peri 1(41.3); Peri 2 (38.3) | Pre (41.5%); Peri 2 (33.1%); Peri 2 (41.4%) | Jun.–Jul. for 2019 | Jun.–Jul. for 2020; Jun.–Jul. for 2021 | Attempt | Diagnosis (medical record) |
| Chadi et al., 2021 [60] | Canada | Retrospective | Emergency Adolescent Patients | Pre (24,824.5); Peri (18,988) | -- | -- | 2018–2019 | 2020 | Ideation | Diagnosis (International Classification of Diseases, 10th edition) |
| Danielsen et al., 2022 [11] | Denmark | Longitudinal | Young People | Pre (27,441); Peri (7597) | 20.7 (Wave 8) | Pre (56%); Peri (67%) | Jan. 1st 2018–Mar. 11th for 2020 | Mar. 12th 2020–Mar. 1st 2021 | Ideation | Self-report (Have you thought about taking your own life, even though you would not do it, within the last year?) |
| Díaz de Neira et al., 2021 [103] | Italy | Retrospective | Emergency Adolescent Patients; Psychiatric Adolescent Inpatients | Emergency sample: Pre (64); Peri (25); Psychiatric sample: Pre (31); Peri (18) | Emergency sample: Pre (14.2); Peri (15.36); Psychiatric Sample: Pre (15.55); Peri (15.17) | Emergency sample: Pre (62.5%); Peri (72%); Psychiatric Sample: Pre (64.5%); Peri (72.2%) | 2019 | 2020 | Ideation Attempt |
Diagnosis (medical record) |
| Ettman et al., 2020 [10] | United State | Repeated Cross-sectional | General Population | Pre (5085); Peri (1415) | Pre (46.57); Peri (45.62) | Pre (51.3%); Peri (50%) | 2017–2018 | Mar. 31st 2020–Apr. 13th 2020 | Ideation | Self-report (Item 9 of the Patient Heath Questionarie-9: Thoughts that you would be better off dead or of hurting yourself in some way over the past two weeks?) |
| Fidancı et al., 2021 [71] | Turkey | Retrospective | Pediatric Emergency Adolescents | Pre (55,678); Peri (19,061) | Pre (8.11); Peri (8.58) | Pre (47.6%); Peri (48.9%) | Apr.–Oct. for 2019 | Apr.–Oct. for 2020 | Attempt | Diagnosis (medical record) |
| Gatta et al., 2022 [94] | Italy | Repeated Cross-sectional | Psychiatric Adolescent Patients | Pre (102); Peri (96) | Pre (13.2); Peri (13.8) | Pre (63.7%); Peri (65.6%) | Feb. 2019–Feb. 2020 | Mar. 2020–Mar. 2021 | Ideation Attempt |
Diagnosis (medical record) |
| G’etaz et al., 2021 [66] | Switzerland | Retrospective | Prisoners | -- | -- | -- | 2016–2019 | 2020 | Attempt | Diagnosis (medical record) |
| Golubovic et al., 2022 [104] | Serbia | Retrospective | Psychiatric Adult patients | Pre (181); Peri (104) | 40.58 | 41.55% | May–Aug. for 2018–2019 | May–Aug. for 2020 | Ideation Attempt |
Diagnosis (definition: thoughts about wishing to be dead or active thoughts of wanting to end one’s life) Diagnosis (definition: nonfatal, self-directed, potentially injurious behavior with an implicit or explicit intent to die). |
| Gracia et al., 2021 [72] | Spain | Retrospective | Adolescent | Pre (835,030); Peri (835,430) | -- | -- | Mar. 2019–Mar. 2020) | Mar. 2020–Mar. 2021 | Attempt | Diagnosis (Six-item suicidality module of the Mini International Neuropsychiatric Interview) |
| Gratz et al., 2021 [53] | United State | Repeated Cross-Sectional | College Students | Pre1 (539); Pre2 (723); Peri (438) | Pre1 (19.39); Pre2 (19.26); Peri (19.53) | Pre1 (69.2%); Pre2 (64.9%); Peri (61.9%) | Fall 2014; Fall 2013 | Fall 2020 | Ideation | Self-report (pre: How often have you thought about killing yourself in the past year?; peri: Have you had thoughts of killing yourself in the past year?). |
| H. Kim et al., 2022 [55] | United State | Repeated Cross-Sectional Study | College Students | Pre (3643); Peri (4970) | Pre (18.85); Peri (19.5) | Pre (73.1%); Peri (69.7%) | Oct. 7th–Dec. 1st for 2019 | Mar. 2nd–May 9th for 2020 | Ideation | Self-report (Item 9 of the Patient Heath Questionarie-9: Thoughts that you would be better off dead or of hurting yourself in some way over the past two weeks?) |
| Habu et al., 2021 [73] | Japan | Retrospective | Emergency Call Patients | Pre (33,594); Peri (14,176) | Pre (60.1); Peri (62.8) | Pre (48.7%); Peri (49.2%) | Mar.–Aug. for 2018–2019 | Mar.–Aug. for 2020 | Attempt | Diagnosis (medical record) |
| Hill et al., 2020 [95] | United State | Retrospective | Pediatric Patients | Ideation: Pre (7520); Peri (5311) Attempt: Pre (7510); Peri (5302) | 14.52 | 59% | Jan.–Jul. for 2019 | Jan.–Jul. for 2020 | Ideation Attempt |
Self-report (Columbia-Suicide Severity Rating Scale) |
| Horita et al., 2022 [54] | Japan | Repeated Cross-Sectional | College Students | Pre (440); Peri 1 (766); Peri 2 (738) | -- | Pre (51.4%); Peri 1 (45.3%); Peri 2 (49.5%) | Apr. 15th–May 31st for 2019 | Apr. 20th–May 31st for 2020; Apr. 10th–May 31st for 2021 | Ideation | Self-report (an item of the Counseling Center Assessment of Psychological Symptoms: I have had thoughts of ending my life in the past 2 weeks). |
| Hörmann et al., 2021 [96] | Switzerland | Retrospective | Psychiatric Patients | Pre (1751); Peri (1591) | Pre: <30 (22.8%), 30–59 (61.55), 60+ (15.7%); Peri: <30 (24.4%), 30–59 (59.8%), 60+ (15.8%) | Pre (46.2%); Peri (46.7%) | Mar. 13th–May 11th for 2019 | Mar. 13th–May 11th for 2020 | Ideation Attempt |
Diagnosis (Arbeitsgemeinschaft für Methodik und Dokumentation in der Psychiatrie System) |
| Ibeziako et al., 2022 [105] | United State | Retrospective | Pediatric Psychiatric Patients | Pre (2020); Peri (1779) | Pre (8.11); Peri (8.58) | Pre (55.9%); Peri (65.8%) | Mar. 2019–Feb. 2020 | Mar. 2020–Feb. 2021 | Ideation Attempt |
Diagnosis (International Classification of Diseases, 10th edition) |
| Irigoyen-Otiñano et al., 2022 [106] | Spain | Retrospective | Psychiatric Emergency Patients | Pre (699); Peri 1 (903); Peri 2 (2190) | Pre (43.6); Peri 1 (39.6); Peri 2 (37.1) | Pre (60%); Peri 1 (59.2%); Peri 2 (60.5%) | Jan. 13th–Mar. 14th for 2020 | Mar. 15th–Jun. 20th for 2020; Oct. 25th 2020–May 9th 2021 | Ideation Attempt |
Diagnosis (medical record) Diagnosis (definition: a self-inflicted, potentially injurious behavior with a nonfatal outcome for which there is evidence, either explicit or implicit, of intent to die) |
| Kasal et al., 2022 [9] | Czechia | Repeated Cross-Sectional | General Population | Pre (3306); Peri 1(3021); Peri 2 (3000) | Pre (48.82); Peri 1 (46.84); Peri 2 (46.16) | Pre (53.7%); Peri 1 (52.3%); Peri 2 (51.1%) | Nov. 2017 | May 2020; Nov. 2020 | Ideation Attempt |
Self-report (Items of the Mini International Neuropsychiatric Interview: Think that you would be better off dead or wish you were dead? Want to harm yourself? Think about suicide? Have a suicide plan?) Self-report (Items of Mini International Neuropsychiatric Interview: Attempt suicide? Did you ever make a suicide attempt?) |
| Kim et al., 2021 [12] | South Korea | Repeated Cross-Sectional | Adolescents | Pre (48,443); Peri (44,216) | Pre (15); Peri (15.1) | Pre (48.7%); Peri (47.5%) | Jun. 3rd–Jul. 12th for 2019 | Aug. 3rd–Nov. 13th for 2020 | Ideation Attempt |
Self-report (single question: Participants were asked if they had considered suicide seriously within the past 12 months) Self-report (single question of if they had attempted suicide within the past 12 months) |
| King et al., 2022 [97] | Canada | Longitudinal (Matched Sample) | College Students | 1330 | Pre (18.5); Peri (18.8) | 67.2% | 2018–2019 | 2020–2021 | Ideation Attempt |
Self-report (Columbia-Suicide Severity Rating Scale) |
| Knudsen et al., 2021 [64] | Norway | Repeated Cross-Sectional | General Population | Pre (563); Peri 1 (691); Peri 2 (530); Peri 3 (370); | Pre (38.3); Peri 1(39.4); Peri 2 (39.2); Peri 3 (39.1) | Pre (56.6%); Peri 1(62.3%); Peri 2 (61.2%); Peri 3 (64.1%) | Jan. 28th–Mar. 11th for 2020 | Mar. 12th–May 31st for 2020; Jun. 1st–Jul. 31st 2020; Aug. 1st -Sept. 18th 2020 | Ideation | Diagnosis (Composite International Diagnostic Interview: Thoughts of killing oneself or wishing one was dead during the 30 days before the interview) |
| Koenig et al., 2021 [15] | Germany | Longitudinal (Matched Sample) | Adolescents | 324 | 14.93 | 69.3% | Nov. 26th 2018–Mar. 13th 2020 | Mar. 18th–Aug. 29th for 2020 | Ideation Attempt |
Self-report (Paykel Suicide Scale) |
| Kose et al., 2021 [107] | Turkey | Retrospective | Psychiatry Emergency Adolescents | Pre (128); Peri (66) | -- | -- | Mar.–Jun. for 2019 | Mar.–Jun. for 2020 | Ideation Attempt |
Diagnosis (medical record) |
| Lee and Hong, 2022 [108] | South Korea | Repeated Cross-Sectional | High School Students | Pre (57,303); Peri 1 (54,948); Peri2 (54,848) | Pre (15.08); Peri 1 (15.19); Peri2 (15.23) | Pre (48.2%); Peri 1 (48%); Peri2 (48.1%) | Jun.–Jul. for 2019 | Aug.–Nov. for 2020–2021 | Ideation Attempt |
Self-report (whether suicidal thoughts had occurred in the past 12 months) Self-report (whether suicide attempt had occurred in the past 12 months) |
| Liu et al., 2022 [61] | Canada | Repeated Cross-Sectional | General Population | Pre (57,034); Peri (5742) | Pre: 18–34 (28.4%), 35–64 (50.1%), 65+ (21.5%); Peri: 18–34 (24.8%), 35–64 (53%), 65+ (22.3%) | Pre (50.8%); Peri (50.7%) | Jan. 2nd–Dec. 24th for 2019 | Feb. 1–May 7 for 2021 | Ideation | Self-report (2021: have you seriously contemplated suicide since the COVID-19 pandemic began?; 2019: Have you ever seriously contemplated suicide and has this happened in the past 12 months?) |
| Mayne et al., 2021 [98] | United State | Repeated Cross-Sectional | Adolescents | Pre (43,504); Peri (47,684) | Pre (15.2); Peri (15.3) | Pre (49.3%); Peri (49.7%) | Jun.–Dec. for 2019 | Jun.–Dec. for 2020 | Ideation Attempt |
Self-report (Has there been a time in the past month when you have had serious thoughts about ending your life?) Self-report (Have you ever, in your whole life, tried to kill yourself or made a suicide attempt?) |
| McLoughlin et al., 2022 [62] | Ireland | Retrospective | Psychiatric Emergency Adolescent Patients | Pre (15); Peri 1 (23); Peri 2 (47) | 16.5 | Pre (46.7%); Peri 1 (60%); Peri 2 (72%) | Mar.–May for 2019 | Mar.–May for 2020–2021 | Ideation | Diagnosis (medical record) |
| Millner et al., 2022 [109] | United State | Retrospective | Pediatric Psychiatric Patients | Pre (1096); Peri (275) | Pre (15.82); Peri (15.13) | Pre (71.1%); Peri (88.7%) | April 2017 to March 12, 2020 | March 13, 2020 to April 2021 | Ideation Attempt |
Self-report (Self-Injurious Thoughts and Behaviors Interview Self-Report Version; past month). |
| Nichter et al., 2021 [56] | United State | Longitudinal | Military Veterans | 3078 | 63.2 | 8.4% | Nov. 18th 2019–Mar. 8th 2020 | Nov. 9th–Dec. 17th for 2020 | Ideation | Self-report (Item 2 of the Suicide Behaviors Questionnaire-Revised: How often have you thought about killing yourself in the past years?) |
| Nsamenang et al., 2022 [110] | Canada | Retrospective | Pediatric Patients with Obesity | Pre (145); Peri (189) | Pre (11.9); Peri (11.5) | Pre (45.5%); Peri (47.1%) | Dec.15th 2019–Mar. 15th 2020 | Dec.15th 2020– Mar. 15th 2021 | Ideation Attempt |
Diagnosis (medical record) |
| Reif-Leonhard et al., 2022 [113] | Germany | Retrospective | General Population | 765,000 | -- | -- | Mar.–Dec. 2019 | Mar.–Dec. 2020 | Attempt | Diagnosis (definition: deliberate self-harm with intend to die, irrespective of fatality probability) |
| Reuter et al., 2021 [99] | United State | Repeated Cross-Sectional | College Students | Ideation: Pre (619); Peri (491) Attempt: Pre (34); Peri (36) | Pre (20.3); Peri (20.6) | Pre (77.4%); Peri (83.8%) | Apr. 2018–Feb. 2020 | Nov. 2020–Apr. 2021 | Ideation Attempt |
Self-report (During the past 12 months, did you ever seriously consider attempting suicide?) Self-report (Did you actually attempt suicide?) |
| S. Y. Kim et al., 2022 [74] | South Korea | Repeated Cross-Sectional | General Population | Pre (6127); Peri (5746) | Pre (51.7); Peri (52) | Pre (50.3%); Peri (50%) | Jan.–Dec. for 2019 | Jan.–Dec. for 2020 | Attempt | Self-report (Have you ever attempted suicide within 1 year?) |
| Sacco et al., 2022 [63] | United State | Retrospective | Emergency Department Patients | Pre (122,148); Peri (27,874) | -- | -- | Mar. 15th–Jul. 31 for 2017–2019 | Mar. 15th–Jul. 31st for 2020 | Ideation | Diagnosis (International Classification of Diseases, 10th edition) |
| Salt et al., 2022 [111] | United State | Retrospective | Adult Patients; Pediatric Patients | Pre (845,992); Peri (714,578) | -- | -- | Mar. 18th–Sept. 18th for 2019 | Mar. 18th–Sept. 18th for 2020 | Ideation Attempt |
Diagnosis (International Classification of Diseases, 10th edition) |
| Seifert et al., 2020 [16] | Germany | Retrospective | Psychiatric Patients | Pre (476); Peri (374) | Pre (44.48); Peri (43.4) | Pre (47.9%); Peri (39.3%) | Mar. 16th–May 24th for 2019 | Mar. 16th–May 24th for 2019 | Ideation Attempt |
Diagnosis (Arbeitsgemeinschaft für Methodik und Dokumentation in der Psychiatrie System) |
| Sivertsen et al., 2022 [100] | Norway | Repeated Cross-Sectional | College Students | Pre 1 (8124); Pre 2 (13,663); Pre 3 (49,836); Peri (59,028) | Pre 1 (24.1); Pre 2 (23.55); Pre 3 (24.27); Peri (23.53) | Pre 1 (65.6%); Pre 2 (65.8%); Pre 3 (66.5%); Peri (69.1%) | Oct. 11th–Nov. 8th for 2010; Feb. 24th–Mar. 27th for 2014; Feb. 6th–Apr. 5th for 2018 | Mar. 1st–Apr. 6th for 2021 | Ideation Attempt |
Self-report (an item of the depression subscale of HSCL-25: In the past 2 weeks, including today, how much have you been bothered by thoughts of ending your life?) Self-report (an item of the Adult Psychiatric Morbidity Survey: Have you ever made an attempt to take your life, by taking an overdose of tablets or in some other way?) |
| Stańdo et al., 2022 [75] | Poland | Retrospective | General Population | -- | 13–24 (4556 million); 25–64 (20.714 million); 65+ (7.417 million) | -- | 2019 | 2020; 2021 | Attempt | Diagnosis (medical record) |
| Taquet et al., 2022 [101] | United State | Retrospective | Eating Disorder Adolescents Patients | Pre (19,843); Peri (8471) | Pre (16.34); Peri (16.25) | Pre (75.4%); Peri (78.1%) | Jan. 20th 2017–Jan. 19th 2020 | Jan. 20th 2020–Jan. 19th 2021 | Ideation Attempt |
Diagnosis (International Classification of Diseases, 10th edition; code R45.851) Diagnosis (International Classification of Diseases, 10th edition; code T14.91) |
| Thompson et al., 2021 [67] | United State | Retrospective | Psychiatric Patients | Pre (196); Peri (142) | Pre (14.53); Peri (15.06) | Pre (--); Peri (45.8%) | Apr. 13th–Sept. 14th for 2019 | Apr. 13th–Sept. 14th for 2020 | Attempt | Self-report (Have you made any suicide attempts in the 7 days before you came to the hospital?) |
| Valdez-Santiago et al., 2022 [68] | Mexico | Repeated Cross-Sectional | Adolescents | Pre (17,925); Peri (4913) | -- | -- | Jul. 2018–Jun. 2019 | Aug.–Nov. for 2020 | Attempt | Self-report (Have you ever attempted to harm yourself or deliberately cut, intoxicated or hurt yourself in any way for the purpose of dying? (2) Was this in the last 12 months? |
| Zhang et al., 2020 [112] | China | Longitudinal | Primary School Students | Pre (1271); Peri (1241) | 12.6 | 40.7% | Nov. 2019 | May 2020 | Ideation Attempt |
Self-report (Have you ever thought about killing yourself in the past 3 months?) Self-report (Have you ever tried to kill yourself in the past 3 months?) |
| Zhu et al., 2021 [57] | China | Longitudinal | High School Students | 1393 | 13.04 | 53.1% | Sept. 2019 | Jun. 2020 | Ideation | Self-report (Item 9 of the Patient Heath Questionarie-9: Thoughts that you would be better off dead or of hurting yourself in some way over the past two weeks?) |
--: Data not available.
Table 2.
Characteristics of studies reporting death by suicide.
| Study | Region | Data Sources | Time Range | GDP (Peri/Pre) | Unemployment Rate (Peri/Pre) | Main Findings | |
|---|---|---|---|---|---|---|---|
| Pre-Pandemic Period | Peri-Pandemic Period | ||||||
| Acharya et al., 2022 [8] | Nepal | Nepal Police Headquarter | Jul. 2017–Mar. 2020 (Jan.–Dec. 2019) * |
Apr. 2020–Jun. 2021 (Apr. 2020–Mar. 2021) * |
0.98 | 1.52 | An overall increase in the monthly suicide rate was found during the pandemic months (Increase in rate = 0.28, 95% CI: 0.12, 0.45). |
| Appleby et al., 2021 [14] | England (NHS sustainability and transformation partnerships region) | Real Time Surveillance (RTS) System | Apr.–Oct. for 2019 | Apr.–Oct. for 2020 | 0.98 | 1.14 | Comparison of the suicide rates after lockdown began in 2020 to those of the same months in 2019 showed no difference (IRR = 1.00, 95% CI: 0.92–1.09). |
| Arya et al., 2022 [76] | India | National Crime Records Bureau (NCRB) Data | 2010−2019 (2017) * | 2020 | 1 | 1.48 | Compared to 2017, an increase in annual suicide rate was found during the pandemic year (RR = 1.14, 95% CI: 1.13–1.14). |
| Chen et al., 2022 [77] | Taiwan | Taiwan’s Ministry of Health and Welfare | 2017–2019 | 2020 | 1.11 | 1.03 | Compared to previous years, a decrease in annual suicide rates after the outbreak was found (p = 0.05). |
| de la Torre-Luque et al., 2022 [78] | Spain | National Death Index | 2019 | 2020 | 0.92 | 1.1 | No significant differences in suicide mortality rates between 2019 and 2020 were found (p = 0.18). |
| Faust et al., 2021 [79] | Massachusetts, USA | Massachusetts Department of Health Registry of Vital Records and Statistics | 2015–2019 (2019) * | 2020 | 0.96 | 3.03 | During the pandemic period, the incident rate for suicide deaths in Massachusetts was 0.67 vs. 0.80 per 100,000 person months during the corresponding period in 2019 (IRR = 0.84; 95% CI, 0.64–1.00). |
| Gerstner et al., 2022 [80] | Ecuador | National Directorate of Crimes against Life, Violent Deaths, Disappearances, Extortion and Kidnapping (DINASED) | Jan. 2015–Feb. 2020 | Mar. 2020–Jun. 2021 | 0.99 | 1.62 | During the pandemic period, suicide rate was not significantly higher than expected (RR = 0.97; 95% CI, 0.92–1.02). |
| Larson et al., 2022 [81] | Michigan, USA | Michigan Department of Health and Human Services (MDHHS) | Jan. 1st, 2006–Mar. 12th, 2020 | Mar. 13th, 2020–Dec. 12th, 2021 | 0.95 | 2.43 | Compared with before, daily suicide incidence rate declined during the pandemic for both females (9.32%; p = 0.01) and males (20.64%; p = 0.04). |
| McIntyre et al., 2021 [13] | Canada | Canadian National Database | Mar. 2010–Feb. 2020 (Mar. 2019–Feb. 2020) * |
Mar. 2020–Feb. 2021 | 0.95 | 1.67 | Overall suicide mortality rate decreased from the March 2019–February 2020 period to the March 2020–February 2021 period (absolute difference of 1300 deaths). |
| Mitchel and Li, 2021 [82] | Connecticut, USA | Connecticut Office of the Chief Medical Examiner | Mar. 10th–May 20th for 2014–2019 | Mar. 10th–May 20th for 2020 | 0.96 | 1.64 | The age-adjusted suicide rate was 13% lower than the recent 5-year average during the same period. |
| Page et al., 2022 [83] | Australia | Australian Bureau of Statistics | 2019 | 2020; 2021 | 0.96; 1.11 | 1.25; 0.98 | The suicide rate in 2020 was lower than the 2019 rate, while the decrease was less noteworthy when considering the trend from the beginning of 20th century. |
| Palacio-Mejía et al., 2022 [84] | Mexico | National Epidemiological and Statistical Subsystem of Deaths | 2019 | 2020; 2021 | 0.89; 1.06 | 1.26; 1.26 | The suicide rate for 2019, 2020, and 2021 was 4.7, 5.3, and 5.4 per 100,000 people, respectively. |
| Radeloff et al., 2021 [114] | Leipzig, German | Leipzig Health Authority | 2010–2019 | 2020 | 1.05 | 0.8 | In 2020, suicides rates were lower in periods with severe COVID-19 restrictions (SR = 7.2, χ2 = 4.033, p = 0.045), compared with periods without restrictions (SR = 16.8) |
| Reif-Leonhard et al., 2022 [113] | Frankfurt/Main, German | Institute of Legal Medicine and Communal Health Authority | Mar.–Dec. for 2019 | Mar.–Dec. for 2020 | 0.99 | 1.23 | The number of completed suicides did not change between March–December 2019 and March–December 2020 (IRR = 0.94, p > 0.05). |
| Rogalska and Syrkiewicz-Switała, 2022 [86] | Poland | Ministry of Health | 2017–2019 | 2020 | 1.05 | 0.8 | The total number of annual suicide attacks shows an upward trend from 2017 to 2020. |
| Rück et al., 2020 [87] | Sweden | Statistics Sweden | Jan.–Jun. for 2019 | Jan.–Jun. for 2020 | 1.01 | 1.22 | Suicide rates in January-June 2020 revealed a slight decrease compared to the corresponding rates in January–June 2019 (relative decrease by −1.2% among men and −12.8% among women). |
| Ryu et al., 2022 [91] | South Korea | Statistics Korea’s Microdata Integrated Service | 2017–2019 (2019) * | 2020 | 0.99 | 1.03 | Compared to 2019 (26.9 per 100,000 people), the suicide rate declined in 2020 (25.7). |
| Stene-Larsen et al., 2022 [88] | Norway | Norwegian Cause of Death Registry | 2010– 2019 (2019) * | 2020 | 0.89 | 1.19 | During the pandemic period, the observed suicide rate (12.1 per 100,000 population) was not significantly higher than expected (12.3). |
| Tanaka and Okamoto, 2021 [89] | Japan | Ministry of Health, Labor and Welfare | Nov. 2016–Jan. 2020 | Feb.–Jun. for 2020; Jul.–Oct. for 2020 |
1; 0.98 | 1.11; 1.11 | During the first 5 months of the pandemic, monthly suicide rates declined by 14%. |
| Wei et al., 2021 [90] | Suzhou, China | Monitoring System of Death Causes of Suzhou Center for Disease Control and Prevention | Jan.–Apr. for 2015–2019 | Jan.–Apr. for 2020 | 1.19 | 0.96 | Suicide was among the top five causes of death, and suicide rate had normal fluctuation during the pandemic. |
CI = Confidence Interval; RR = Rate Ratio; IRR = Incidence Rate Ratio; SR = Suicide Rate. * These data were used for comparison.
3.2. Meta-Analysis of Suicidal Ideation for Non-Clinical and Clinical Samples
3.2.1. Overview
There were 41 studies with 51 samples (28 non-clinical and 23 clinical samples, respectively) included for the analysis of suicidal ideation. Specifically, several studies contributed more than one sample due to multiple peri-pandemic data collection [9,54,59,62,64,106,108] or subsets of participants [103,111]. With an average risk-of-bias score of 7.2 (range = 5–9), the majority of included studies had adequate size and information for the sample, addressed response rate properly, and employed appropriate statistical methods. The most common limitations were deficiencies in the sample representativeness and recruiting methods, and unclear measurements (Table S2). Both non-clinical and clinical settings showed an increased prevalence of suicidal ideation during the pandemic compared with pre-pandemic periods, and significant heterogeneity was found within each setting (Table 3).
Table 3.
Summary of meta-analysis results for studies reporting suicidal ideation in non-clinical and clinical settings.
| Study Setting | No. of Studies (Samples) | Pooled PR (95% CI; p-Value) | Heterogeneity | ||
|---|---|---|---|---|---|
| I 2 | tau 2 | Q (p-Value) | |||
| Non-clinical settings | 23 (28) | 1.142 (1.018–1.282; p = 0.024) | 97.734% | 0.081 | 1191.667 (0.00) |
| Clinical settings | 18 (23) | 1.134 (1.048–1.227; p = 0.002) | 71.029% | 0.018 | 75.939 (0.00) |
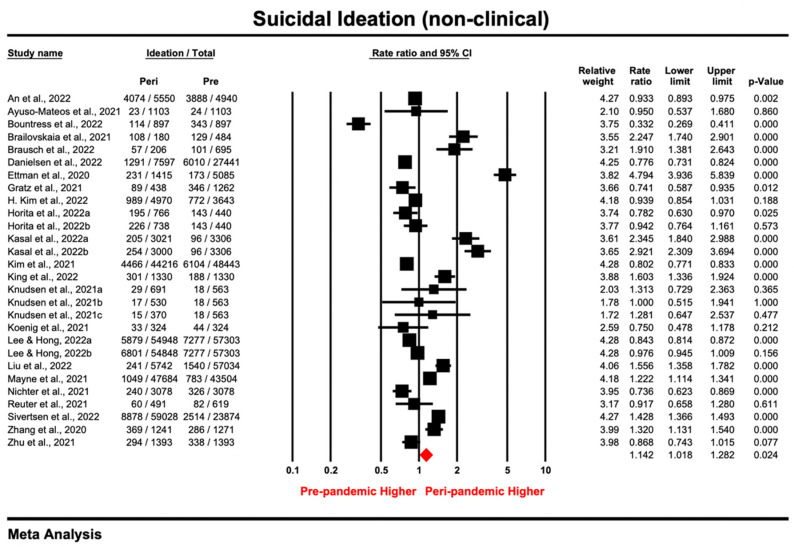
3.2.2. Non-Clinical Samples
The point estimates of suicidal ideation reported by 28 non-clinical samples ranged from 0.332 to 4.794, and the pooled prevalence ratio under the random effect model was 1.142 (95% CI: 1.018–1.282; p = 0.024), indicating a higher prevalence of suicidal ideation during the pandemic compared with the pre-pandemic period (Figure 2). The heterogeneity test results were significant (I2 = 97.734%, tau2 = 0.081, PQ < 0.05), indicating that there was a large difference in effect sizes between samples. Sensitivity analysis using leave-one-out method showed that most of the included samples did not affect the outcome substantially. However, when Ettman et al. [10] and Kasal et al. [9] were excluded separately, the respective pooled ratio (1.007–1.112) indicated a slight but non-significant increase in the peri-pandemic prevalence of suicidal ideation compared with pre-pandemic periods (Figure S1). No publication bias was observed among the non-clinical samples according to the funnel plot (Figure S2) and the non-significant results from Egger’s tests (intercept = 2.61, t = 1.48, p = 0.151).
Figure 2.
Forest plot for suicidal ideation of studies [9,10,11,12,15,51,52,53,54,55,56,57,58,61,64,93,97,98,99,100,102,108,112] conducting in the non-clinical setting (Prismatic colored as red refers to the pooled estimate).
The results of subgroup analysis are shown in Table 4; they suggest that the prevalence ratio varied by population type and study design. The highest PR was found among the general population (PR = 2.014, 95% CI: 1.604–2.529; p = 0.000), which indicated that suicidal ideation was twice as prevalent during the COVID-19 pandemic compared with before, while the prevalence of suicidal ideation in adolescents, younger (mostly college students) and special populations remained basically unchanged. After excluding the only one study [58] using retrospective design, the prevalence ratio was 1.318 (95% CI: 1.132–1.535; p = 0.000) for repeated cross-sectional studies, suggesting the significantly increased prevalence of suicidal ideation during the pandemic relative to pre-pandemic times; meanwhile, longitudinal studies showed a non-significant decrease (PR = 0.842; 95% CI: 0.666–1.063; p = 0.148). Meta-regression showed that neither female percentage nor quality score for non-clinical samples was associated with PR (Table S3).
Table 4.
Summary of subgroup analysis for non-clinical and clinical samples reporting suicidal ideation.
| Moderators | No. of Studies | Point Estimate (95% CI; p-Value) | Total Between | ||
|---|---|---|---|---|---|
| Q | df(Q) | p-Value | |||
| Non-clinical samples | |||||
| Population | 31.838 | 3 | 0.000 | ||
| Adolescents | 8 | 1.03 (0.849–1.248; p = 0.296) | |||
| Younger group 1 | 10 | 0.955 (0.803–1.136; p = 0.604) | |||
| General population | 8 | 2.014 (1.604–2.529; p = 0.000) | |||
| Special group 2 | 2 | 0.833 (0.574–1.208; p = 0.335) | |||
| Study design | 9.941 | 1 | 0.002 | ||
| Repeated cross-sectional | 19 | 1.318 (1.132–1.535; p = 0.000) | |||
| Longitudinal | 8 | 0.842 (0.666–1.063; p = 0.148) | |||
| Measurement tool | 0.033 | 1 | 0.857 | ||
| Self-report | 25 | 1.139 (1.012–1.283; p = 0.031) | |||
| Diagnosis | 3 | 1.194 (0.73–1.95; p = 0.48) | |||
| Timeframe for measurement | 0.156 | 1 | 0.693 | ||
| ≤2 weeks | 8 | 1.159 (0.95–1.414; p = 0.146) | |||
| >2 weeks | 19 | 1.217 (1.062–1.394; p = 0.005) | |||
| Data collection | 0.134 | 2 | 0.935 | ||
| Mar–Aug 2020 | 16 | 1.141 (0.964–1.35; p = 0.125) | |||
| Sept 2020–Jan 2021 | 8 | 1.118 (0.895–1.396; p = 0.325) | |||
| Feb. 2021+ | 4 | 1.199 (0.884–1.628; p = 0.243) | |||
| Clinical samples | |||||
| Population | 0.944 | 1 | 0.331 | ||
| Adolescent patients | 15 | 1.171 (1.057–1.297; p = 0.002) | |||
| Adult patients | 8 | 1.081 (0.953–1.225; p = 0.225) | |||
| Measurement tool | 0.259 | 1 | 0.611 | ||
| Self-report | 2 | 1.079 (0.872–1.336; p = 0.484) | |||
| Diagnosis | 21 | 1.146 (1.047–1.255; p = 0.003) | |||
| Timeframe for measurement | 0.067 | 1 | 0.796 | ||
| ≤2 weeks | 20 | 1.129 (1.129–1.027; p = 0.012) | |||
| >2 weeks | 3 | 1.158 (0.976–1.375; p = 0.093) | |||
| Data collection | 0.996 | 1 | 0.318 | ||
| Mar–Aug 2020 | 19 | 1.12 (1.031–1.217; p = 0.007) | |||
| Sept 2020–Feb 2021+ 3 | 4 | 1.292 (0.988–1.688; p = 0.061) | |||
1 An aggregate of young people (aged 19–24 years old) and college students. 2 An aggregate of hotline callers and military veterans. 3 We combined the only two samples (Irigoyen-Otiñano et al., 2022b [106]; Nsamenang et al., 2022 [110]) that collected data during Sept. 2020–Jan. 2021 and two samples after 2021 (Berger et al., 2022b [59]; McLoughlin et al., 2022b [62]).
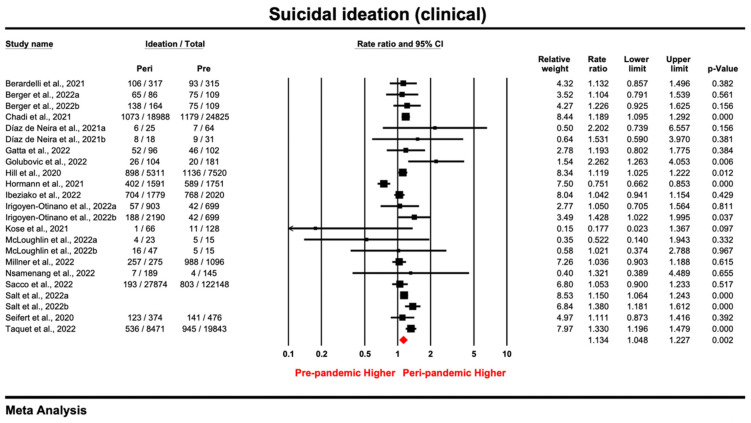
3.2.3. Clinical Samples
Of the 51 samples reporting suicidal ideation, 23 were conducted in a clinical setting. With a pooled estimate of 1.134 (95% CI: 1.048–1.227; p = 0.002), the prevalence ratio for each study ranged from 0.177 to 2.262 (Figure 3). As indicated by the results, there was significant heterogeneity among the samples (I2 = 71.029%, tau2 = 0.018, PQ < 0.05). By excluding samples one by one or samples with lower quality [62,96,107], sensitivity analysis showed that none of the samples affected the outcome substantially (Figures S3 and S4). Thus, despite variations across studies, the pooled estimate was robust enough to show an increasing trend of suicidal ideation among clinical patients during the pandemic. Through visual inspection of the funnel plot (Figure S5) and the non-significant results in the Egger’s tests (intercept = 0.096, t = 0.15, p = 0.882), the results showed that there was no publication bias among the clinical samples.
Figure 3.
Forest plot for suicidal ideation of studies [16,59,60,62,63,92,94,95,96,101,103,104,105,106,107,109,110,111] conducted in the clinical setting (Prismatic colored as red refers to the pooled estimate).
As all the clinical samples employed a retrospective design by extracting medical records, the subgroup analysis considered only population (adolescent vs. adult patients), method, and timeframe for measurement tool. According to Table 4, none of the above variables was a significant moderator for PR in the clinical samples. Nevertheless, meta-regression (Table S3) showed that study quality was positively associated with the ratio, suggesting that higher-quality studies tended to report a larger increase in suicidal ideation (B = 0.08, p < 0.05).
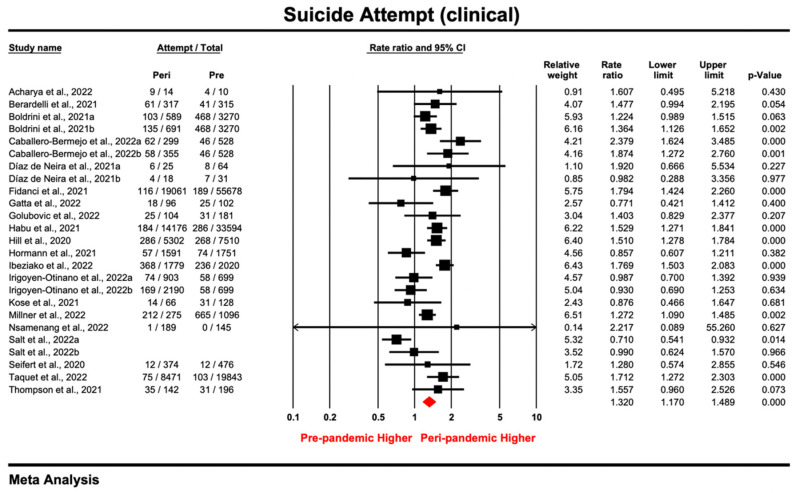
3.3. Meta-Analysis of Suicide Attempt for Non-Clinical and Clinical Samples
3.3.1. Overview
There were 37 studies with 55 samples (30 non-clinical and 25 clinical samples, respectively) included for the analysis of suicidal ideation. Specifically, several studies contributed more than one sample due to multiple peri-pandemic data collection [9,65,70,75,106,108] or subsets of participants [75,103,111]. With an average risk of bias score of 7.5 (range = 4–9), the majority of included studies had adequate size and information for their sample, and they employed appropriate sampling and statistical methods. The most common limitations were deficiencies in sample representativeness and unclear criteria for judging suicide attempt (Table S2). Both non-clinical and clinical settings showed increased suicide attempts during the pandemic, compared with pre-pandemic periods, and the increase was higher among clinical participants. Significant heterogeneity was found in each setting (Table 5).
Table 5.
Summary of meta-analysis results for studies reporting suicide attempt in non-clinical and clinical settings.
| Study Setting | No. of Studies (Samples) | Pooled PR (95% CI; p-Value) | Heterogeneity | ||
|---|---|---|---|---|---|
| I 2 | tau 2 | Q (p-Value) | |||
| Non-clinical settings | 17 (30) | 1.14 (1.053–1.233; p = 0.001) | 99.996% | 0.036 | 7601.38 (p = 0.000) |
| Clinical settings | 20 (25) | 1.32 (1.17–1.489; p = 0.000) | 70.021% | 0.052 | 80.056 (p = 0.000) |
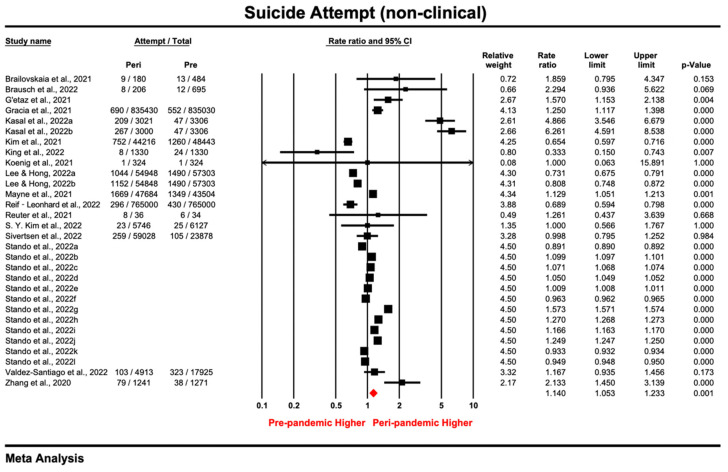
3.3.2. Non-Clinical Samples
The prevalence ratio of suicide attempt reported by 30 non-clinical samples ranged from 0.333 to 6.261, and the pooled prevalence ratio under the random effect model was 1.14 (95% CI: 1.053–1.233; p = 0.001), indicating that suicide attempts were more prevalent during the COVID-19 pandemic than during pre-pandemic periods (Figure 4). Though effect sizes were substantially heterogenous among the samples (I2 = 99.996%, tau2 = 0.036, PQ < 0.05), a sensitivity analysis using the leave-one-out method or by excluding lower quality studies [66] showed that the increased trend of suicide attempts was robust (Figures S6 and S7). Through visual inspection of the funnel plot (Figure S8) and the non-significant results of the Egger’s tests (intercept = 6.52, t = 0.17, p = 0.865), no publication bias among the non-clinical samples was observed.
Figure 4.
Forest plot for suicide attempt of studies [9,12,15,66,68,72,74,75,93,97,98,99,100,102,108,112,113] conducted in the non-clinical setting (Prismatic colored as red refers to the pooled estimate).
The results of the subgroup analysis are shown in Table 6. Excluding only one prisoner sample, the general population (PR = 1.218, 95% CI: 1.089–1.362; p = 0.001) showed the largest increase in suicide attempts compared with adolescent and younger samples, despite the fact that the differences were insignificant. Meta-regression showed that neither the female percentage nor the quality score for the non-clinical samples were associated with PR (Table S4).
Table 6.
Summary of subgroup analysis for non-clinical and clinical samples reporting suicide attempt.
| Moderators | No. of Studies | Point Estimate (95% CI; p-Value) | Total Between | ||
|---|---|---|---|---|---|
| Q | df(Q) | p-Value | |||
| Non-Clinical Samples | |||||
| Population | 4.005 | 2 | 0.135 | ||
| Adolescent | 13 | 1.062 (0.948–1.189; p = 0.3) | |||
| Younger group 1 | 4 | 0.942 (0.673–1.319; p = 0.73) | |||
| General population | 12 | 1.218 (1.089–1.362; p = 0.001) | |||
| Study design | 2.805 | 2 | 0.246 | ||
| Repeated cross-sectional | 12 | 1.245 (1.083–1.43; p = 0.002) | |||
| Longitudinal | 3 | 1.285 (0.817–2.02; p = 0.277) | |||
| Retrospective | 15 | 1.084 (0.983–1.195; p = 0.106) | |||
| Measurement tool | 2.788 | 1 | 0.095 | ||
| Self-report | 15 | 1.248 (1.093–1.425; p = 0.001) | |||
| Diagnosis | 15 | 1.084 (0.983–1.196; p = 0.106) | |||
| Timeframe for measurement | 2.809 | 1 | 0.094 | ||
| ≤2 weeks | 16 | 1.084 (0.983–1.196; p = 0.107) | |||
| >2 weeks | 14 | 1.249 (1.093–1.426; p = 0.001) | |||
| Data collection | 0.397 | 2 | 0.820 | ||
| Mar–Aug 2020 | 15 | 1.15 (1.025–1.289; p = 0.017) | |||
| Sept 2020–Jan 2021 | 7 | 1.174 (0.988–1.395; p = 0.069) | |||
| Feb. 2021+ | 8 | 1.101 (0.966–1.255; p = 0.149) | |||
| Clinical samples | |||||
| Population | 1.044 | 1 | 0.307 | ||
| Adolescent patients | 12 | 1.415 (1.185–1.68; p = 0.000) | |||
| Adult patients | 13 | 1.251 (1.068–1.464; p = 0.005) | |||
| Measurement tool | 0.256 | 1 | 0.613 | ||
| Self-report | 3 | 1.42 (1.036–1.948; p = 0.13) | |||
| Diagnosis | 22 | 1.299 (1.132–1.492; p = 0.000) | |||
| Timeframe for measurement | 0.628 | 1 | 0.428 | ||
| ≤2 weeks | 22 | 1.288 (1.121–1.479; p = 0.000) | |||
| >2 weeks | 3 | 1.158 (0.976–1.375; p = 0.012) | |||
| Data collection | |||||
| Mar–Aug 2020 | 22 | 1.323 (1.164–1.503; p = 0.000) | 0.016 | 1 | 0.901 |
| Sept 2020–Feb 2021+ 2 | 3 | 1.288 (0.685–1.918; p = 0.213) | |||
3.3.3. Clinical Samples
Of the 55 samples reporting suicide attempt, 25 were conducted in a clinical setting. With a pooled estimate of 1.32 (95% CI: 1.17–1.489; p = 0.000), the prevalence ratio for each study ranged from 0.71 to 2.379 (Figure 5), and the effect size was heterogenous (I2 = 70.021%, tau2 = 0.052, PQ < 0.05). The increased trend for suicide attempt during the pandemic was robust, as pooled estimates did not change substantially based on the results (Figures S9 and S10) of the leave-one-out sensitivity analysis and the analysis excluding lower quality studies [96,107]. Visual inspection of the funnel plot (Figure S11) and the non-significant results in the Egger’s tests (intercept = −0.63, t = 0.86, p = 0.397) indicated an absence of asymmetry in the funnel plot. These results showed no publication bias among the clinical studies reporting suicide attempt.
Figure 5.
Forest plot for suicide attempt of studies [16,65,67,69,70,71,73,92,94,95,96,101,103,104,105,106,107,109,110,111] conducted in the clinical setting (Prismatic colored as red refers to the pooled estimate).
All clinical samples (k = 25) employed a retrospective design by extracting medical records; subgroup analysis considered only population (adolescent or adult patients), method and timeframe for measurement tool, and time for data collection. According to subgroup analysis (Table 6) and meta-regression (Table S4), no significant moderators were found for PR of suicide attempts in the clinical samples.
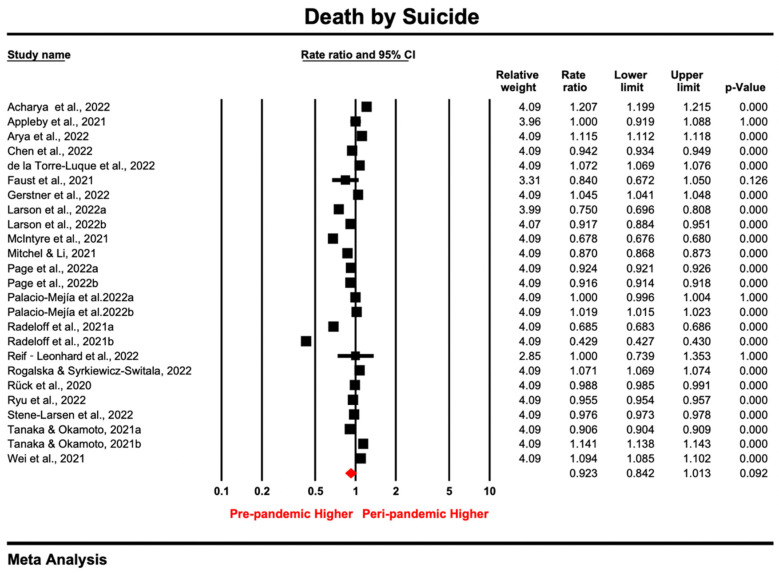
3.4. Meta-Analysis for Death by Suicide
A total of 25 samples were reported by 20 studies, as some studies included gender-specific [81] or multiple peri-pandemic [84,89,114] data. The risk-of-bias score for the included samples ranged from 5 to 9 (average = 7.8), and 75% of the samples scored above 7. All samples were nationally or regionally representative, while some of them did not provide detailed demographics, criteria for judging, or source of suicide death (Table S2).
As shown in Figure 6, the point estimate ranged from 0.429 to 1.207, and the pooled rate ratio for suicide death was 0.923 (95% CI: 0.84–1.01; p > 0.05) under the random-effect model. The heterogeneity test results were significant (I2 = 99.99%, tau2 = 0.055, PQ < 0.05), indicating a substantial difference in effect sizes across samples. By excluding samples one by one or samples with lower quality scores [14,77,78,83,86], sensitivity analysis showed robustness in the pooled ratio for death by suicide, as none of the samples affected the pooled estimate substantially (Figures S12 and S13). In addition, visual inspection of the funnel plot (Figure S14) and the non-significant results in the Egger’s tests (intercept = 11.99, t = 0.21, p = 0.837) indicated an absence of asymmetry in the funnel plot. These results showed that there was no publication bias when deriving the pooled estimate.
Figure 6.
Forest plot for studies [8,13,14,76,77,78,79,80,81,82,83,84,86,87,88,89,90,91,113,114] reporting death by suicide (Prismatic colored as red refers to the pooled estimate).
Meta-regression was conducted to test whether counties’ resilience and government-level economic and societal indexes during the pandemic would contribute to the between-study heterogeneity on death by suicide. However, the moderating effects for these indexes were not significant (Table S5). The subgroup analysis showed that the trends for suicide death were significantly different between national and regional samples (p = 0.01). Despite the country-level rate of death by suicide remaining stable (RR = 0.99, 95% CI: 0.91–1.1; p > 0.05), data from regional samples reported a decreased trend (RR = 0.82, 95% CI: 0.73–0.92; p = 0.001).
4. Discussion
To our knowledge, this work was the first meta-analysis that assessed the changes in the prevalence of suicidal ideation, suicide attempt, and rate of death by suicide before and during the COVID-19 pandemic across populations, using intertemporal data from repeated cross-sectional retrospective, longitudinal, and retrospective studies. We included 45 studies with 67 samples, and most of the included studies had a low risk of coverage bias, sample size estimation, and statistical analysis. Compared with the pre-pandemic period, the prevalence of suicidal ideation and suicide attempt increased significantly during the COVID-19 pandemic among both non-clinical and clinical samples, while the rate of death by suicide remained mostly unchanged in the synthesis of the existing evidence.
Our findings showed an upward trend of suicidal ideation and suicide attempt during the COVID-19 pandemic among both non-clinical and clinical samples. These results were consistent with a few studies during the pandemic, which warned about the increased risks of suicidal thoughts and behaviors relative to pre-pandemic periods among the general population and inpatients [22,23,24]. The outbreak of the COVID-19 pandemic had brought profound health, psychological, social, and economic consequences worldwide, which might have heightened various suicide risk factors [6,7]. As found by a meta-analysis looking at data spanning 50 years [115], hopelessness, mental health issues (e.g., depression and anxiety), socioeconomic status, and stressful life events were among the top predictors for suicide-related outcomes. These factors were also applied to the pandemic context [24]. During the pandemic, with lockdown measures implemented, individuals experienced overwhelming fears and worries about COVID-19 due to health issues, uncertainties about the future, stigmatization, and misinformation from media, which were associated with higher hopelessness under the pandemic context [116]. Additionally, the COVID-19 pandemic had been described as a tsunami, leading to mental disorders worldwide [117], and a wide range of studies had suggested the severe psychological impacts of increased distress, depression, anxiety, insomnia, and loneliness brought by the pandemic across populations [118,119,120,121]. These psychological symptoms might be long-lasting, increasing the risk for suicidality [7]. People also suffered from financial strain, unemployment, and economic uncertainty due to the global economic downturns, which constituted societal risk factors for developing suicidal ideation and attempts during the pandemic [122]. Recent studies have also reported the rise of other risk factors for suicide, such as weakened social support, poor health, increased interpersonal conflict, domestic violence, and alcohol consumption [6,123,124,125,126]. The wide-ranging adverse effects of the pandemic may have put individuals at a disadvantage and triggered the increased suicide-related outcomes.
Notably, the adult general population showed a larger increase in both suicidal ideation and suicide attempt, and the increase in suicidal ideation was particularly noticeable. The PR for suicidal ideation was 2.014 (95% CI: 1.604–2.529; p = 0.000), indicating a doubled prevalence of suicidal ideations during the pandemic, with a slight increase in suicide attempt (PR = 1.218; 95% CI: 1.089–1.362; p = 0.001). The adult general population in our study was aged above 25 and mostly in their 30s–50s. Middle-aged adults are usually the pillar of a family, with heavier financial and caregiving responsibilities. Thus, economic adversities and lockdown measures can threaten this population, making them more vulnerable to suicide [127]. In addition, the larger increase in ideation than attempt echoes the pyramid theory of suicidal trajectories [128]. According to the theory, suicide-related outcomes develop in an ascending flow from suicidal ideation at the bottom of the pyramid, moving up to plan and attempt, and ultimately reaching the peak of the pyramid, completed suicide. Individuals can stop at any stage once they have started the “suicidal career”, but most people only have suicidal thoughts, with few actually taking action [129]. The gap between these stages can be understood by the interpersonal theory of suicide, which suggests that despite a strong suicidal desire, the step toward attempt requires one’s ability (e.g., fearlessness and pain insensitivity) to act on the thoughts [130]. Thus, not everyone who develops suicidal ideation engages in suicidal behaviors, which can account for the differences in incremental movement from suicidal ideation to attempt during the pandemic among the non-clinical adult samples.
Interestingly, our clinical samples showed more increases in the prevalence of suicide attempt than suicidal ideation. These findings do not contradict the pyramid theory. Previous studies found that suicidal thoughts were often under-documented in clinical settings [131], and those who attempted suicide were more prone to present in emergency and psychiatric departments compared to those only with suicidal ideation. In addition, referral to health services was further hindered by the lockdown measures during the pandemic, resulting in a larger proportion of community individuals with only suicidal thoughts being underdiagnosed [132,133]. These reasons can also explain our results that suicidal ideation among non-clinical adults increased more than the clinical samples, which is congruent with a previous finding [20].
The results for suicidal ideation and attempt were mostly robust, based on the sensitivity analysis. The only exception was found by excluding several non-clinical samples one by one [9,10], the pooled estimates which changed substantially, and the fact that the increases in suicidal ideation became smaller and nonsignificant, indicating the peculiarly large increases in these studies. Both studies employed a repeated cross-sectional design; therefore, those who responded to the survey in two periods may have differed in characteristics. Though both studies collected data from nationwide adult samples during the pre- and peri-pandemic periods, participants recruited during the pandemic were experiencing more adverse conditions for suicidality, as mentioned above (e.g., mental disorders, economic disadvantage). This finding again suggests that suicide risk factors were magnified by the pandemic, and the adult population may have suffered more. In any case, our subgroup analysis among non-clinical samples showed that, compared with the longitudinal study, suicidal ideation reported by repeated cross-sectional studies increased more. Therefore, it is possible that stressors may have affected survey participation [10], as psychologically vulnerable individuals may pay more attention to mental health information during the pandemic due to attentional bias.
Suicide death did not change significantly in terms of the pooled RR during the pandemic, compared with the pre-pandemic period. This trend agrees with previous findings from 33 countries and individual groups [18,20]. However, the trend was different at the regional and country level, with a significant downward trend shown by using regional data (RR = 0.82, 95% CI: 0.73–0.92; p = 0.001). The difference was also found in the state of Connecticut, showing a lower suicide rate compared with the national level [82]. The possible explanation might be the small sample size or the larger coverage of a single race included by regional data, which is not representative of the national profile. This implies the need to consider regional differences and the representativeness of the samples when interpreting the suicide rate.
Our findings have significant implications for future suicide management. Although the overall rate of death by suicide did not increase, suicide concerns are still serious, as this study showed that suicidal ideation and suicide attempts have been more prevalent since the pandemic. Having suicidal desires and acting on the thoughts are the prior stages of final death by suicide; such suicidal processes can be unstable and vary in duration. For example, the average duration for females and males before displaying explicit suicidal acts was 52 and 31 months [129]. In other words, a “suicidal career” takes time to progress to the final stage, though this only applies to a small proportion of suicidal individuals [134]. Thus, the alarming increases in suicidal ideation and suicide attempts during the pandemic point to the need for prompt suicide screening and prevention—especially among the members of the general public who might be underdiagnosed—and specifically, timely interventions targeting suicidal individuals to halt their exacerbation.
This study has a few limitations. First, some included studies did not provide sufficient information (e.g., gender distributions and timeframe for measurement) to be coded for the moderation analysis, making our subgroup analysis and meta-regression results less convincing. Second, there may have been an overlap in the subgroup of the adult general population and younger group (mostly college students), as the studies targeting the general population usually included people above 18, despite the larger proportion being middle-aged. Third, considerable heterogeneity still exists in all outcomes, even after considering potential moderators, and none of the investigated factors can account for the variability among effect sizes for death by suicide, which was similar to the previous findings [18]. Future studies are recommended to examine other potential sources of heterogeneity. Finally, the included samples only covered data up to November 2021, most of which were conducted in 2020. Such a delay may have compromised the validity of our findings, as suicidality and its risk factors are fluid in nature and vary within short periods, according to the fluid vulnerability theory of suicide [135]. As the pandemic evolves, the present suicide situation might be changing, so it is necessary to have ongoing monitoring and real-time surveillance.
5. Conclusions
In conclusion, our study provides an overview of the changes in the prevalence of suicidal ideation and suicide attempts across populations and the national or regional rate of death by suicide since the outbreak of the COVID-19 pandemic. Although the overall rate of death by suicide remained basically unchanged during the pandemic, suicidal ideation and suicide attempt were more prevalent compared with the pre-pandemic period, especially among the adult general population and clinical patients. Considering the heightened suicide risk factors, such as mental health problems and economic vulnerability during the pandemic, large-scale suicide screening for the public and timely intervention programs for high-risk groups are highly needed. The continuously changing pandemic underscores the importance of ongoing monitoring and surveillance for suicidality.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20043346/s1, Figure S1. Sensitivity analysis for non-clinical samples reporting suicidal ideation (leave-one-out method); Figure S2. Funnel plot for non-clinical samples reporting suicidal ideation; Figure S3. Sensitivity analysis for clinical samples reporting suicidal ideation (leave-one-out method); Figure S4. Sensitivity analysis for clinical samples reporting suicidal ideation (exclude lower-quality samples); Figure S5. Funnel plot for clinical samples reporting suicidal ideation; Figure S6. Sensitivity analysis for non-clinical samples reporting suicide attempt (leave-one-out method); Figure S7. Sensitivity analysis for non-clinical samples reporting suicide attempt (exclude lower-quality samples); Figure S8. Funnel plot for non-clinical samples reporting suicide attempt; Figure S9. Sensitivity analysis for clinical samples reporting suicide attempt (leave-one-out method); Figure S10. Sensitivity analysis for clinical samples reporting suicide attempt (exclude lower-quality samples); Figure S11. Funnel plot for clinical samples reporting suicide attempt; Figure S12. Sensitivity analysis for samples reporting suicide death (leave-one-out method); Figure S13. Sensitivity analysis for samples reporting suicide death (exclude lower-quality samples); Figure S14. Funnel plot for samples reporting suicide death; Table S1. PRISMA checklist; Table S2. Risk of bias assessment; Table S3. Summary of meta-regression for non-clinical and clinical samples reporting suicidal ideation; Table S4. Summary of meta-regression for non-clinical and clinical samples reporting suicide attempt; Table S5. Summary of meta-regression for samples reporting death by suicide; File S1. Full search strategy.
Author Contributions
Conceptualization, N.X.Y. and J.H.; methodology, Y.Y. and J.H.; software, Y.Y.; validation, J.H.; formal analysis, Y.Y.; investigation, Y.Y.; resources, N.X.Y.; data curation, J.H.; writing—original draft preparation, Y.Y.; writing—review and editing, N.X.Y. and J.H.; visualization, Y.Y.; supervision, N.X.Y. and Q.L.; project administration, N.X.Y. and Q.L.; funding acquisition, N.X.Y. and Q.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, N.X.Y., upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This research was funded by the Research Grants Council of the Hong Kong Special Administrative Region, China (Collaborative Research Fund, Project No. C1031-18G).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Devitt P. Can we expect an increased suicide rate due to COVID-19? Ir. J. Psychol. Med. 2020;37:264–268. doi: 10.1017/ipm.2020.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rogers J., Chesney E., Oliver D., Begum N., Saini A., Wang S., McGuire P., Fusar-Poli P., Lewis G., David A.S. Suicide, self-harm and thoughts of suicide or self-harm in infectious disease epidemics: A systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 2021;30:e32. doi: 10.1017/S2045796021000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kahil K., Cheaito M.A., El Hayek R., Nofal M., El Halabi S., Kudva K.G., Pereira-Sanchez V., El Hayek S. Suicide during COVID-19 and other major international respiratory outbreaks: A systematic review. Asian J. Psychiatry. 2021;56:102509. doi: 10.1016/j.ajp.2020.102509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leaune E., Samuel M., Oh H., Poulet E., Brunelin J. Suicidal behaviors and ideation during emerging viral disease outbreaks before the COVID-19 pandemic: A systematic rapid review. Prev. Med. 2020;141:106264. doi: 10.1016/j.ypmed.2020.106264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zortea T.C., Brenna C.T., Joyce M., McClelland H., Tippett M., Tran M.M., Arensman E., Corcoran P., Hatcher S., Heisel M.J. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts: A systematic review. Crisis J. Crisis Interv. Suicide Prev. 2021;42:474. doi: 10.1027/0227-5910/a000753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O’Connor R.C., Pirkis J., Caine E.D. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM Int. J. Med. 2020;113:707–712. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Acharya B., Subedi K., Acharya P., Ghimire S. Association between COVID-19 pandemic and the suicide rates in Nepal. PLoS ONE. 2022;17:e0262958. doi: 10.1371/journal.pone.0262958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kasal A., Kuklová M., Kågström A., Winkler P., Formánek T. Suicide risk in individuals with and without mental disorders before and during the COVID-19 pandemic: An analysis of three nationwide cross-sectional surveys in Czechia. Arch. Suicide Res. 2022:1–15. doi: 10.1080/13811118.2022.2051653. [DOI] [PubMed] [Google Scholar]
- 10.Raifman J., Ettman C.K., Dean L., Barry C., Galea S. Economic precarity, social isolation, and suicidal ideation during the COVID-19 pandemic. medRxiv. 2020 doi: 10.1101/2020.10.05.20205955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danielsen S., Joensen A., Andersen P.K., Madsen T., Strandberg-Larsen K. Self-injury, suicidal ideation and -attempt and eating disorders in young people following the initial and second COVID-19 lockdown. medRxiv. 2022 doi: 10.1101/2022.03.08.22271980. [DOI] [Google Scholar]
- 12.Kim S.Y., Kim H.-R., Park B., Choi H.G. Comparison of stress and suicide-related behaviors among Korean youths before and during the COVID-19 pandemic. JAMA Netw. Open. 2021;4:e2136137. doi: 10.1001/jamanetworkopen.2021.36137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McIntyre R.S., Lui L.M., Rosenblat J.D., Ho R., Gill H., Mansur R.B., Teopiz K., Liao Y., Lu C., Subramaniapillai M. Suicide reduction in Canada during the COVID-19 pandemic: Lessons informing national prevention strategies for suicide reduction. J. R. Soc. Med. 2021;114:473–479. doi: 10.1177/01410768211043186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Appleby L., Richards N., Ibrahim S., Turnbull P., Rodway C., Kapur N. Suicide in England in the COVID-19 pandemic: Early observational data from real time surveillance. Lancet Reg. Health-Eur. 2021;4:100110. doi: 10.1016/j.lanepe.2021.100110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koenig J., Kohls E., Moessner M., Lustig S., Bauer S., Becker K., Thomasius R., Eschenbeck H., Diestelkamp S., Gillé V. The impact of COVID-19 related lockdown measures on self-reported psychopathology and health-related quality of life in German adolescents. Eur. Child Adolesc. Psychiatry. 2021;32:113–122. doi: 10.1007/s00787-021-01843-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seifert J., Meissner C., Birkenstock A., Bleich S., Toto S., Ihlefeld C., Zindler T. Peripandemic psychiatric emergencies: Impact of the COVID-19 pandemic on patients according to diagnostic subgroup. Eur. Arch. Psychiatry Clin. Neurosci. 2021;271:259–270. doi: 10.1007/s00406-020-01228-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knipe D., John A., Padmanathan P., Eyles E., Dekel D., Higgins J.P., Bantjes J., Dandona R., Macleod-Hall C., McGuinness L.A. Suicide and self-harm in low-and middle-income countries during the COVID-19 pandemic: A systematic review. PLOS Glob. Public Health. 2022;2:e0000282. doi: 10.1371/journal.pgph.0000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pirkis J., Gunnell D., Shin S., Del Pozo-Banos M., Arya V., Aguilar P.A., Appleby L., Arafat S.Y., Arensman E., Ayuso-Mateos J.L. Suicide numbers during the first 9–15 months of the COVID-19 pandemic compared with pre-existing trends: An interrupted time series analysis in 33 countries. EClinicalMedicine. 2022;51:101573. doi: 10.1016/j.eclinm.2022.101573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021;51:201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bersia M., Koumantakis E., Berchialla P., Charrier L., Ricotti A., Grimaldi P., Dalmasso P., Comoretto R.I. Suicide spectrum among young people during the COVID-19 pandemic: A systematic review and meta-analysis. EClinicalMedicine. 2022;54:101705. doi: 10.1016/j.eclinm.2022.101705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.John A., Eyles E., Webb R., Okolie C., Schmidt L., Arensman E., Hawton K., O’Connor R., Kapur N., Moran P., et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: Update of living systematic review. F1000Research. 2021;9:1097. doi: 10.12688/f1000research.25522.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pathirathna M.L., Nandasena H.M.R.K.G., Atapattu A.M.M.P., Weerasekara I. Impact of the COVID-19 pandemic on suicidal attempts and death rates: A systematic review. BMC Psychiatry. 2022;22:506. doi: 10.1186/s12888-022-04158-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dubé J.P., Smith M.M., Sherry S.B., Hewitt P.L., Stewart S.H. Suicide behaviors during the COVID-19 pandemic: A meta-analysis of 54 studies. Psychiatry Res. 2021;301:113998. doi: 10.1016/j.psychres.2021.113998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farooq S., Tunmore J., Ali M.W., Ayub M. Suicide, self-harm and suicidal ideation during COVID-19: A systematic review. Psychiatry Res. 2021;306:114228. doi: 10.1016/j.psychres.2021.114228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.John A., Pirkis J., Gunnell D., Appleby L., Morrissey J. Trends in suicide during the COVID-19 pandemic. BMJ. 2020;371:m4352. doi: 10.1136/bmj.m4352. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization Public Health Action for the Prevention of Suicide: A Framework. [(accessed on 1 December 2022)]. Available online: https://apps.who.int/iris/bitstream/handle/10665/75166/?sequence=1.
- 27.Wasserman I.M. The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide Life-Threat. Behav. 1992;22:240–254. [PubMed] [Google Scholar]
- 28.Turecki G., Brent D.A., Gunnell D., O’Connor R.C., Oquendo M.A., Pirkis J., Stanley B.H. Suicide and suicide risk. Nat. Rev. Dis. Prim. 2019;5:74. doi: 10.1038/s41572-019-0121-0. [DOI] [PubMed] [Google Scholar]
- 29.Stuckler D., Basu S., Suhrcke M., Coutts A., McKee M. The public health effect of economic crises and alternative policy responses in Europe: An empirical analysis. Lancet. 2009;374:315–323. doi: 10.1016/S0140-6736(09)61124-7. [DOI] [PubMed] [Google Scholar]
- 30.Coentre R., Góis C. Suicidal ideation in medical students: Recent insights. Adv. Med. Educ. Pract. 2018;9:873. doi: 10.2147/AMEP.S162626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mamun M.A. Suicide and suicidal behaviors in the context of COVID-19 pandemic in Bangladesh: A systematic review. Psychol. Res. Behav. Manag. 2021;14:695. doi: 10.2147/PRBM.S315760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; Washington, DC, USA: 2013. [Google Scholar]
- 33.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021;10:105906. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 35.Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid.-Based Healthc. 2015;13:147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 36.van de Schoot R., de Bruin J., Schram R., Zahedi P., de Boer J., Weijdema F., Kramer B., Huijts M., Hoogerwerf M., Ferdinands G. An open source machine learning framework for efficient and transparent systematic reviews. Nat. Mach. Intell. 2021;3:125–133. doi: 10.1038/s42256-020-00287-7. [DOI] [Google Scholar]
- 37.Ros R., Bjarnason E., Runeson P. A machine learning approach for semi-automated search and selection in literature studies; Proceedings of the 21st International Conference on Evaluation and Assessment in Software Engineering; Karlskrona, Sweden. 15–16 June 2017; pp. 118–127. [Google Scholar]
- 38.The World Bank GDP per Capita (Current US$) [(accessed on 1 December 2022)]. Available online: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD.
- 39.Statista Global Economic Indicators—Statistics & Facts. [(accessed on 1 December 2022)]. Available online: https://www.statista.com/topics/5442/global-economic-indicators/#topicHeader__wrapper.
- 40.Australian Bureau of Statistics Australian National Accounts: National Income, Expenditure and Product. [(accessed on 1 December 2022)]; Available online: https://www.abs.gov.au/statistics/economy/national-accounts/australian-national-accounts-national-income-expenditure-and-product/latest-release.
- 41.Jiangsu Provincial Bureau of Statistics GDP by City. [(accessed on 6 December 2022)]; Available online: http://tj.jiangsu.gov.cn/2022/nj02/nj0212.htm.
- 42.Bloomberg The COVID Resilience Ranking The Best and Worst Places to Be as World Enters Next COVID Phase. [(accessed on 10 December 2022)]. Available online: https://www.bloomberg.com/graphics/covid-resilience-ranking/
- 43.University of Oxford COVID-19 GOVERNMENT RESPONSE TRACKER. [(accessed on 9 December 2022)]. Available online: https://www.bsg.ox.ac.uk/research/research-projects/covid-19-government-response-tracker.
- 44.Large M.M., Nielssen O.B. Suicide in Australia: Meta-analysis of rates and methods of suicide between 1988 and 2007. Med. J. Aust. 2010;192:432–437. doi: 10.5694/j.1326-5377.2010.tb03580.x. [DOI] [PubMed] [Google Scholar]
- 45.Higgins J.P., Thomas J., Chandler J., Cumpston M., Li T., Page M.J., Welch V.A. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; Hoboken, NJ, USA: 2019. [Google Scholar]
- 46.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Copas J., Shi J.Q. Meta-analysis, funnel plots and sensitivity analysis. Biostatistics. 2000;1:247–262. doi: 10.1093/biostatistics/1.3.247. [DOI] [PubMed] [Google Scholar]
- 48.Goldston D.B. Assessment of Suicidal Behaviors and Risk among Children and Adolescents. National Institute of Mental Health; Bethesda, MD, USA: 2000. [Google Scholar]
- 49.Horvath L.O., Győri D., Komáromy D., Meszaros G., Szentiványi D., Balazs J. Nonsuicidal self-injury and suicide: The role of life events in clinical and non-clinical populations of adolescents. Front. Psychiatry. 2020;11:370. doi: 10.3389/fpsyt.2020.00370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Health Organization Global Situation. [(accessed on 6 December 2022)]. Available online: https://covid19.who.int/
- 51.Ayuso-Mateos J.L., Morillo D., Haro J., Olaya B., Lara E., Miret M. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: A longitudinal study in the general population. Epidemiol. Psychiatr. Sci. 2021;30:e49. doi: 10.1017/S2045796021000408. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 52.Bountress K.E., Cusack S.E., Conley A.H., Aggen S.H., Group S.f.S.W., Vassileva J., Dick D.M., Amstadter A.B. The COVID-19 pandemic impacts psychiatric outcomes and alcohol use among college students. Eur. J. Psychotraumatology. 2022;13:2022279. doi: 10.1080/20008198.2021.2022279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gratz K.L., Mann A.J., Tull M.T. Suicidal ideation among university students during the COVID-19 pandemic: Identifying at-risk subgroups. Psychiatry Res. 2021;302:114034. doi: 10.1016/j.psychres.2021.114034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Horita R., Nishio A., Yamamoto M. Lingering effects of COVID-19 on the mental health of first-year university students in Japan. PLoS ONE. 2022;17:e0262550. doi: 10.1371/journal.pone.0262550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim H., Rackoff G.N., Fitzsimmons-Craft E.E., Shin K.E., Zainal N.H., Schwob J.T., Eisenberg D., Wilfley D.E., Taylor C.B., Newman M.G. College mental health before and during the COVID-19 pandemic: Results from a nationwide survey. Cogn. Ther. Res. 2022;46:1–10. doi: 10.1007/s10608-021-10241-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nichter B., Hill M.L., Na P.J., Kline A.C., Norman S.B., Krystal J.H., Southwick S.M., Pietrzak R.H. Prevalence and trends in suicidal behavior among US military veterans during the COVID-19 pandemic. JAMA Psychiatry. 2021;78:1218–1227. doi: 10.1001/jamapsychiatry.2021.2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhu S., Zhuang Y., Paul L., Paul W. The changes of suicidal ideation status among young people in Hong Kong during COVID-19: A longitudinal survey. J. Affect. Disord. 2021;294:151–158. doi: 10.1016/j.jad.2021.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.An J., Yin Y., Zhao L., Tong Y., Liu N.H. Mental health problems among hotline callers during the early stage of COVID-19 pandemic. PeerJ. 2022;10:e13419. doi: 10.7717/peerj.13419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Berger G., Häberling I., Lustenberger A., Probst F., Franscini M., Pauli D., Walitza S. The mental distress of our youth in the context of the COVID-19 pandemic. Swiss Med. Wkly. 2022;152:w30142. doi: 10.4414/SMW.2022.w30142. [DOI] [PubMed] [Google Scholar]
- 60.Chadi N., Spinoso-Di Piano C., Osmanlliu E., Gravel J., Drouin O. Mental Health–related emergency department visits in adolescents before and during the COVID-19 pandemic: A multicentric retrospective study. J. Adolesc. Health. 2021;69:847–850. doi: 10.1016/j.jadohealth.2021.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu L., Pollock N.J., Contreras G., Tonmyr L., Thompson W. Prevalence of suicidal ideation among adults in Canada: Results of the second Survey on COVID-19 and mental health. Health Rep. 2022;33:13–21. doi: 10.25318/82-003-x202200500002-eng. [DOI] [PubMed] [Google Scholar]
- 62.McLoughlin A., Abdalla A., Gonzalez J., Freyne A., Asghar M., Ferguson Y. Locked in and locked out: Sequelae of a pandemic for distressed and vulnerable teenagers in Ireland: Post-COVID rise in psychiatry assessments of teenagers presenting to the emergency department out-of-hours at an adult Irish tertiary hospital. Ir. J. Med. Sci. 2022:1–8. doi: 10.1007/s11845-022-03080-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sacco D.L., Probst M.A., Schultebraucks K., Greene M.C., Chang B.P. Evaluation of emergency department visits for mental health complaints during the COVID-19 pandemic. J. Am. Coll. Emerg. Physicians Open. 2022;3:e12728. doi: 10.1002/emp2.12728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Knudsen A.K.S., Stene-Larsen K., Gustavson K., Hotopf M., Kessler R.C., Krokstad S., Skogen J.C., Øverland S., Reneflot A. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: A population-based repeated cross-sectional analysis. Lancet Reg. Health-Eur. 2021;4:100071. doi: 10.1016/j.lanepe.2021.100071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Boldrini T., Girardi P., Clerici M., Conca A., Creati C., Di Cicilia G., Ducci G., Durbano F., Maci C., Maone A. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: Reduced psychiatric hospitalizations and increased suicidality. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;110:110304. doi: 10.1016/j.pnpbp.2021.110304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gétaz L., Wolff H., Golay D., Heller P., Baggio S. Suicide attempts and Covid-19 in prison: Empirical findings from 2016 to 2020 in a Swiss prison. Psychiatry Res. 2021;303:114107. doi: 10.1016/j.psychres.2021.114107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Thompson E.C., Thomas S.A., Burke T.A., Nesi J., MacPherson H.A., Bettis A.H., Kudinova A.Y., Affleck K., Hunt J., Wolff J.C. Suicidal thoughts and behaviors in psychiatrically hospitalized adolescents pre-and post-COVID-19: A historical chart review and examination of contextual correlates. J. Affect. Disord. Rep. 2021;4:100100. doi: 10.1016/j.jadr.2021.100100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Valdez-Santiago R., Villalobos A., Arenas-Monreal L., González-Forteza C., Hermosillo-de-la-Torre A.E., Benjet C., Wagner F.A. Comparison of suicide attempts among nationally representative samples of Mexican adolescents 12 months before and after the outbreak of the Covid-19 pandemic. J. Affect. Disord. 2022;298:65–68. doi: 10.1016/j.jad.2021.10.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Acharya S., Dash R.K., Das A., Hota M., Mohapatra C., Dash S. An Epidemiological Study of Cut Throat Injury During COVID-19 Pandemic in a Tertiary Care Centre. Indian J. Otolaryngol. Head Neck Surg. 2022;74:2764–2769. doi: 10.1007/s12070-020-02239-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Caballero-Bermejo A.F., Ortega-Pérez J., Frontera-Juan G., Homar-Amengual C., Barceló-Martín B., Puiguriguer-Ferrando J. Acute poisoning among patients attended to in an emergency department: From the pre-pandemic period to the new normality. Rev. Clínica Española Engl. Ed. 2022;222:406–411. doi: 10.1016/j.rceng.2022.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fidancı İ., Taşar M.A., Akıntuğ B., Fidancı İ., Bulut İ. The impact of the COVID-19 pandemic on paediatric emergency service. Int. J. Clin. Pract. 2021;75:e14398. doi: 10.1111/ijcp.14398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gracia R., Pamias M., Mortier P., Alonso J., Pérez V., Palao D. Is the COVID-19 pandemic a risk factor for suicide attempts in adolescent girls? J. Affect. Disord. 2021;292:139–141. doi: 10.1016/j.jad.2021.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Habu H., Takao S., Fujimoto R., Naito H., Nakao A., Yorifuji T. Emergency dispatches for suicide attempts during the COVID-19 outbreak in Okayama, Japan: A descriptive epidemiological study. J. Epidemiol. 2021;31:511–517. doi: 10.2188/jea.JE20210066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim S.Y., Yoo D.M., Kwon M.J., Kim J.H., Kim J.-H., Wee J.H., Choi H.G. Depression, Stress, and Suicide in Korean Adults before and during the COVID-19 Pandemic Using Data from the Korea National Health and Nutritional Examination Survey. J. Pers. Med. 2022;12:1305. doi: 10.3390/jpm12081305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Stańdo J., Czabański A., Fechner Ż., Baum E., Andriessen K., Krysińska K. Suicide and Attempted Suicide in Poland before and during the COVID-19 Pandemic between 2019 and 2021. Int. J. Environ. Res. Public Health. 2022;19:8968. doi: 10.3390/ijerph19158968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Arya V., Page A., Spittal M.J., Dandona R., Vijayakumar L., Munasinghe S., John A., Gunnell D., Pirkis J., Armstrong G. Suicide in India during the first year of the COVID-19 pandemic. J. Affect. Disord. 2022;307:215–220. doi: 10.1016/j.jad.2022.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen Y.-Y., Yang C.-T., Pinkney E., Yip P.S.F. Suicide trends varied by age-subgroups during the COVID-19 pandemic in 2020 in Taiwan. J. Formos. Med. Assoc. 2022;121:1174–1177. doi: 10.1016/j.jfma.2021.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.de la Torre-Luque A., Pemau A., Perez-Sola V., Ayuso-Mateos J.L. Suicide mortality in Spain in 2020: The impact of the COVID-19 pandemic. Rev. De Psiquiatr. Y Salud Ment. 2022;587:1–4. doi: 10.1016/j.rpsm.2022.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Faust J.S., Shah S.B., Du C., Li S.-X., Lin Z., Krumholz H.M. Suicide deaths during the COVID-19 stay-at-home advisory in Massachusetts, March to May 2020. JAMA Netw. Open. 2021;4:e2034273. doi: 10.1001/jamanetworkopen.2020.34273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gerstner R.M., Narváez F., Leske S., Troya M.I., Analuisa-Aguilar P., Spittal M.J., Gunnell D. Police-reported suicides during the first 16 months of the COVID-19 pandemic in Ecuador: A time-series analysis of trends and risk factors until June 2021. Lancet Reg. Health-Am. 2022;14:100324. doi: 10.1016/j.lana.2022.100324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Larson P.S., Bergmans R.S. Impact of the COVID-19 pandemic on temporal patterns of mental health and substance abuse related mortality in Michigan: An interrupted time series analysis. Lancet Reg. Health-Am. 2022;10:100218. doi: 10.1016/j.lana.2022.100218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mitchell T.O., Li L. State-level data on suicide mortality during COVID-19 quarantine: Early evidence of a disproportionate impact on racial minorities. Psychiatry Res. 2021;295:113629. doi: 10.1016/j.psychres.2020.113629. [DOI] [PubMed] [Google Scholar]
- 83.Page A., Spittal M.J. A decline in Australian suicide during COVID-19? A reflection on the 2020 cause of death statistics in the context of long-term trends. J. Affect. Disord. Rep. 2022;9:100353. doi: 10.1016/j.jadr.2022.100353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Palacio-Mejía L.S., Hernández-Ávila J.E., Hernández-Ávila M., Dyer-Leal D., Barranco A., Quezada-Sánchez A.D., Alvarez-Aceves M., Cortés-Alcalá R., Fernández-Wheatley J.L., Ordoñez-Hernández I. Leading causes of excess mortality in Mexico during the COVID-19 pandemic 2020–2021: A death certificates study in a middle-income country. Lancet Reg. Health-Am. 2022;13:100303. doi: 10.1016/j.lana.2022.100303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Radeloff D., Genuneit J., Bachmann C.J. Suicides in Germany during the COVID-19 pandemic—An analysis based on data from 11 million inhabitants, 2017-2021. Dtsch. Arztebl. Int. 2022;119:502–503. doi: 10.3238/arztebl.m2022.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rogalska A., Syrkiewicz-Świtała M. COVID-19 and Mortality, Depression, and Suicide in the Polish Population. Front. Public Health. 2022;10:854028. doi: 10.3389/fpubh.2022.854028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rück C., Mataix-Cols D., Malki K., Adler M., Flygare O., Runeson B., Sidorchuk A. Will the COVID-19 pandemic lead to a tsunami of suicides? A Swedish nationwide analysis of historical and 2020 data. medRxiv. 2020 doi: 10.1101/2020.12.10.20244699. [DOI] [Google Scholar]
- 88.Stene-Larsen K., Raknes G., Engdahl B., Qin P., Mehlum L., Strom M.S., Reneflot A. Suicide trends in Norway during the first year of the COVID-19 pandemic: A register-based cohort study. Eur. Psychiatry. 2022;65:e26. doi: 10.1192/j.eurpsy.2022.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021;5:229–238. doi: 10.1038/s41562-020-01042-z. [DOI] [PubMed] [Google Scholar]
- 90.Wei X., Huang C., Wang L., Hua Y., Liu Z., Lu Y. Analysis of Injury Death of Suzhou During COVID-19 Epidemic. Health Educ. Health Promot. 2021;16:176–180. doi: 10.16117/j.cnki.31-1974/r.202102176. [DOI] [Google Scholar]
- 91.Ryu S., Nam H.J., Jhon M., Lee J.Y., Kim J.M., Kim S.W. Trends in suicide deaths before and after the COVID-19 outbreak in Korea. PLoS ONE. 2022;17:e0273637. doi: 10.1371/journal.pone.0273637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Berardelli I., Sarubbi S., Rogante E., Cifrodelli M., Erbuto D., Innamorati M., Lester D., Pompili M. The impact of the COVID-19 pandemic on suicide ideation and suicide attempts in a sample of psychiatric inpatients. Psychiatry Res. 2021;303:114072. doi: 10.1016/j.psychres.2021.114072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Brailovskaia J., Teismann T., Friedrich S., Schneider S., Margraf J. Suicide ideation during the COVID-19 outbreak in German university students: Comparison with pre-COVID 19 rates. J. Affect. Disord. Rep. 2021;6:100228. doi: 10.1016/j.jadr.2021.100228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gatta M., Raffagnato A., Mason F., Fasolato R., Traverso A., Zanato S., Miscioscia M. Sociodemographic and clinical characteristics of paediatric patients admitted to a neuropsychiatric care hospital in the COVID-19 era. Ital. J. Pediatr. 2022;48:23. doi: 10.1186/s13052-022-01213-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hill R.M., Rufino K., Kurian S., Saxena J., Saxena K., Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021;147:e2020029280. doi: 10.1542/peds.2020-029280. [DOI] [PubMed] [Google Scholar]
- 96.Hörmann C., Bandli A., Bankwitz A., De Bardeci M., Rüesch A., De Araujo T.V., Seifritz E., Kleim B., Olbrich S. Suicidal ideations and suicide attempts prior to admission to a psychiatric hospital in the first six months of the COVID-19 pandemic: Interrupted time-series analysis to estimate the impact of the lockdown and comparison of 2020 with 2019. BJPsych Open. 2022;8:e24. doi: 10.1192/bjo.2021.1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.King N., Pickett W., Rivera D., Byun J., Li M., Cunningham S., Duffy A. The impact of the COVID-19 pandemic on the mental health of first-year undergraduate students studying at a major Canadian university: A successive cohort study. Can. J. Psychiatry. 2022 doi: 10.1177/07067437221094549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mayne S.L., Hannan C., Davis M., Young J.F., Kelly M.K., Powell M., Dalembert G., McPeak K.E., Jenssen B.P., Fiks A.G. COVID-19 and adolescent depression and suicide risk screening outcomes. Pediatrics. 2021;148:e2021051507. doi: 10.1542/peds.2021-051507. [DOI] [PubMed] [Google Scholar]
- 99.Reuter P.R., Forster B.L., Kruger B.J. A longitudinal study of the impact of COVID-19 restrictions on students’ health behavior, mental health and emotional well-being. PeerJ. 2021;9:e12528. doi: 10.7717/peerj.12528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sivertsen B., Knapstad M., Petrie K., O’Connor R., Lønning K.J., Hysing M. Changes in mental health problems and suicidal behaviour in students and their associations with COVID-19-related restrictions in Norway: A national repeated cross-sectional analysis. BMJ Open. 2022;12:e057492. doi: 10.1136/bmjopen-2021-057492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Taquet M., Geddes J.R., Luciano S., Harrison P.J. Incidence and outcomes of eating disorders during the COVID-19 pandemic. Br. J. Psychiatry. 2022;220:262–264. doi: 10.1192/bjp.2021.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Brausch A.M., Whitfield M., Clapham R.B. Comparisons of mental health symptoms, treatment access, and self-harm behaviors in rural adolescents before and during the COVID-19 pandemic. Eur. Child Adolesc. Psychiatry. 2022 doi: 10.1007/s00787-022-02039-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Díaz de Neira M., Blasco-Fontecilla H., García Murillo L., Pérez-Balaguer A., Mallol L., Forti A., Del Sol P., Palanca I. Demand analysis of a psychiatric emergency room and an adolescent acute inpatient unit in the context of the COVID-19 pandemic in Madrid, Spain. Front. Psychiatry. 2021;11:557508. doi: 10.3389/fpsyt.2020.557508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Golubovic S.T., Zikic O., Nikolic G., Kostic J., Simonovic M., Binic I., Gugleta U. Possible impact of COVID-19 pandemic and lockdown on suicide behavior among patients in Southeast Serbia. Open Med Wars. 2022;17:1045–1056. doi: 10.1515/med-2022-0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ibeziako P., Kaufman K., Scheer K.N., Sideridis G. Pediatric Mental Health Presentations and Boarding: First Year of the COVID-19 Pandemic. Hosp. Pediatr. 2022;12:751–760. doi: 10.1542/hpeds.2022-006555. [DOI] [PubMed] [Google Scholar]
- 106.Irigoyen-Otiñano M., Nicolau-Subires E., González-Pinto A., Adrados-Pérez M., Buil-Reiné E., Ibarra-Pertusa L., Albert-Porcar C., Arenas-Pijoan L., Sánchez-Cazalilla M., Torterolo G., et al. Characteristics of patients treated for suicidal behavior during the pandemic in a psychiatric emergency department in a Spanish province. Rev. De Psiquiatr. Y Salud Ment. 2022 doi: 10.1016/j.rpsm.2022.03.004. [DOI] [PubMed] [Google Scholar]
- 107.Kose S., Inal-Kaleli I., Senturk-Pilan B., Cakcak E., Ucuncu B., Ozbaran B., Erermis S., Isik H., Saz E.U., Bildik T. Effects of a pandemic on child and adolescent psychiatry emergency admissions: Early experiences during the COVID-19 outbreak. Asian J. Psychiatry. 2021;61:102678. doi: 10.1016/j.ajp.2021.102678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lee B., Hong J.S. Short- and Long-Term Impacts of the COVID-19 Pandemic on Suicide-Related Mental Health in Korean Adolescents. Int. J. Environ. Res. Public Health. 2022;19:11491. doi: 10.3390/ijerph191811491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Millner A.J., Zuromski K.L., Joyce V.W., Kelly F., Richards C., Buonopane R.J., Nash C.C. Increased severity of mental health symptoms among adolescent inpatients during COVID-19. Gen. Hosp. Psychiatry. 2022;77:77–79. doi: 10.1016/j.genhosppsych.2022.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nsamenang S.A., Gutierrez C.A., Manayathu Jones J., Jenkins G., Tibelius S.A., Digravio A.M., Chamas B., Ewusie J.E., Geddie H., Punthakee Z., et al. Impact of SARS-CoV-2 pandemic on the mental and physical health of children enrolled in a paediatric weight management clinic. Paediatr. Child Health Can. 2022;27:S72–S77. doi: 10.1093/pch/pxac014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Salt E., Wiggins A.T., Cerel J., Hall C.M., Ellis M., Cooper G.L., Adkins B.W., Rayens M.K. Increased rates of suicide ideation and attempts in rural dwellers following the SARS-CoV-2 pandemic. J. Rural. Health. 2023;39:30–38. doi: 10.1111/jrh.12686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhang L., Zhang D., Fang J., Wan Y., Tao F., Sun Y. Assessment of mental health of Chinese primary school students before and after school closing and opening during the COVID-19 pandemic. JAMA Netw. Open. 2020;3:e2021482. doi: 10.1001/jamanetworkopen.2020.21482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Reif-Leonhard C., Lemke D., Holz F., Ahrens K.F., Fehr C., Steffens M., Grube M., Freitag C.M., Kolzer S.C., Schlitt S., et al. Changes in the pattern of suicides and suicide attempt admissions in relation to the COVID-19 pandemic. Eur. Arch. Psychiatry Clin. Neurosci. 2022 doi: 10.1007/s00406-022-01448-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Radeloff D., Papsdorf R., Uhlig K., Vasilache A., Putnam K., Von Klitzing K. Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. Epidemiol. Psychiatr. Sci. 2021;30:e16. doi: 10.1017/S2045796021000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Franklin J.C., Ribeiro J.D., Fox K.R., Bentley K.H., Kleiman E.M., Huang X., Musacchio K.M., Jaroszewski A.C., Chang B.P., Nock M.K. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol. Bull. 2017;143:187. doi: 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- 116.Saricali M., Satici S.A., Satici B., Gocet-Tekin E., Griffiths M.D. Fear of COVID-19, mindfulness, humor, and hopelessness: A multiple mediation analysis. Int. J. Ment. Health Addict. 2020;20:2154–2164. doi: 10.1007/s11469-020-00419-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Riedel-Heller S., Richter D. COVID-19 pandemic and mental health of the general public: Is there a tsunami of mental disorders? Psychiatr. Prax. 2020;47:452–456. doi: 10.1055/a-1290-3469. [DOI] [PubMed] [Google Scholar]
- 118.Barberis N., Cannavò M., Cuzzocrea F., Verrastro V. Suicidal behaviours during COVID-19 pandemic: A review. Clin. Neuropsychiatry. 2022;19:84. doi: 10.36131/cnfioritieditore20220202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry Res. 2020;291:113190. doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morb. Mortal. Wkly. Rep. 2020;69:1049. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ammerman B.A., Burke T.A., Jacobucci R., McClure K. Preliminary investigation of the association between COVID-19 and suicidal thoughts and behaviors in the US. J. Psychiatr. Res. 2021;134:32–38. doi: 10.1016/j.jpsychires.2020.12.037. [DOI] [PubMed] [Google Scholar]
- 124.Choudhury R. An Observational Analysis of Suicidal Deaths during COVID-19 Pandemic Lockdown at Lucknow, India. Indian J. Forensic Med. Toxicol. 2020;14:445–449. [Google Scholar]
- 125.Shrestha R., Siwakoti S., Singh S., Shrestha A.P. Impact of the COVID-19 pandemic on suicide and self-harm among patients presenting to the emergency department of a teaching hospital in Nepal. PLoS ONE. 2021;16:e0250706. doi: 10.1371/journal.pone.0250706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Li D.-J., Ko N.-Y., Chen Y.-L., Wang P.-W., Chang Y.-P., Yen C.-F., Lu W.-H. COVID-19-related factors associated with sleep disturbance and suicidal thoughts among the Taiwanese public: A Facebook survey. Int. J. Environ. Res. Public Health. 2020;17:4479. doi: 10.3390/ijerph17124479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gruber J., Prinstein M.J., Clark L.A., Rottenberg J., Abramowitz J.S., Albano A.M., Aldao A., Borelli J.L., Chung T., Davila J. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am. Psychol. 2021;76:409. doi: 10.1037/amp0000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hawton K., Van Heeringen K. The International Handbook of Suicide and Attempted Suicide. John Wiley & Sons; Hoboken, NJ, USA: 2000. [Google Scholar]
- 129.Joy S. Is It Possible to Accurately Forecast Suicide, or Is Suicide a Consequence of Forecasting Errors? Thesis, The University of Nottingham, Nottingham, UK. 2014. [(accessed on 15 December 2022)]. Available online: https://psychology.nottingham.ac.uk/staff/ddc/c8cxpa/further/Dissertation_examples/Joy_14.pdf.
- 130.Van Orden K.A., Witte T.K., Cukrowicz K.C., Braithwaite S.R., Selby E.A., Joiner T.E., Jr. The interpersonal theory of suicide. Psychol. Rev. 2010;117:575. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kemball R.S., Gasgarth R., Johnson B., Patil M., Houry D. Unrecognized suicidal ideation in ED patients: Are we missing an opportunity? Am. J. Emerg. Med. 2008;26:701–705. doi: 10.1016/j.ajem.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Carison A., Babl F.E., O’Donnell S.M. Increased paediatric emergency mental health and suicidality presentations during COVID-19 stay at home restrictions. Emerg. Med. Australas. 2022;34:85–91. doi: 10.1111/1742-6723.13901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Saunders N.R., Kurdyak P., Stukel T.A., Strauss R., Fu L., Guan J., Fiksenbaum L., Cohen E., Guttmann A., Vigod S. Utilization of physician-based mental health care services among Children and adolescents before and during the COVID-19 pandemic in Ontario, Canada. JAMA Pediatr. 2022;176:e216298. doi: 10.1001/jamapediatrics.2021.6298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hawton K., Bergen H., Waters K., Ness J., Cooper J., Steeg S., Kapur N. Epidemiology and nature of self-harm in children and adolescents: Findings from the multicentre study of self-harm in England. Eur. Child Adolesc. Psychiatry. 2012;21:369–377. doi: 10.1007/s00787-012-0269-6. [DOI] [PubMed] [Google Scholar]
- 135.Rudd M.D. Cognition and Suicide: Theory, Research, and Therapy. American Psychological Association; Washington, DC, USA: 2006. Fluid vulnerability theory: A cognitive approach to understanding the process of acute and chronic suicide risk; pp. 355–368. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, N.X.Y., upon reasonable request.