Abstract
African Animal Trypanosomiasis (AAT), caused predominantly by Trypanosoma brucei brucei, T. vivax and T. congolense, is a fatal livestock disease throughout Sub-Saharan Africa. Treatment options are very limited and threatened by resistance. Tubercidin (7-deazaadenosine) analogs have shown activity against individual parasites but viable chemotherapy must be active against all three species. Divergence in sensitivity to nucleoside antimetabolites could be caused by differences in nucleoside transporters. Having previously characterized the T. brucei nucleoside carriers, we here report the functional expression and characterization of the main adenosine transporters of T. vivax (TvxNT3) and T. congolense (TcoAT1/NT10), in a Leishmania mexicana cell line (‘SUPKO’) lacking adenosine uptake. Both carriers were similar to the T. brucei P1-type transporters and bind adenosine mostly through interactions with N3, N7 and 3′-OH. Expression of TvxNT3 and TcoAT1 sensitized SUPKO cells to various 7-substituted tubercidins and other nucleoside analogs although tubercidin itself is a poor substrate for P1-type transporters. Individual nucleoside EC50s were similar for T. b. brucei, T. congolense, T. evansi and T. equiperdum but correlated less well with T. vivax. However, multiple nucleosides including 7-halogentubercidines displayed pEC50>7 for all species and, based on transporter and anti-parasite SAR analyses, we conclude that nucleoside chemotherapy for AAT is viable.
Keywords: Trypanosoma vivax, Trypanosoma congolense, nucleoside antimetabolite, adenosine transporter, nucleoside transporter, animal trypanosomiasis, nagana, tubercidin analog
1. Introduction
African Animal Trypanosomiasis (AAT) is caused by multiple Trypanosoma species including T. brucei brucei, T. b. rhodesiense, T. congolense, T. evansi, T. equiperdum and T. vivax, and has remained one of the most important livestock diseases in sub-Saharan Africa, where it causes direct and indirect losses amounting to USD 4.75 billion annually [1]. Although the related human disease HAT has been targeted for elimination by the WHO by 2030 [2], it appears that AAT will continue to be around at least for decades. Despite some promising progress for T. vivax, implementation of a vaccine is at best years away, even for any single Trypanosoma species [3,4,5]. Control by chemotherapy is hampered by the paucity of drugs, and the widespread resistance to them [6,7]. This would leave control of the tsetse fly vector as the main option for AAT control, but this is difficult in the vast rural areas where it would be required and is further challenged by the spread of mechanically transmitted T. vivax and T. evansi, and the sexually transmitted T. equiperdum, inside and outside Africa [8,9,10]. Thus, tsetse control, while important, will not be enough. This, coupled with the problem of drug resistance [11,12], emphasizes the need for more effort in the study of veterinary trypanosomes [13].
In the last 60 years, only one new veterinary trypanocide has been introduced to the field, melarsomine (Cymelarsan, MelCy), which was developed in the late 1980s [14]; the other veterinary trypanocides in use are all 60 years old or more [15]. Therefore, the need for safer and more effective trypanocides cannot be overemphasized, especially considering the slim chances of vaccine development [5]. Furthermore, different isolates of veterinary trypanosomes have shown great variability in their drug sensitivity profile, which often leads to treatment failure and devastating impact on agricultural and rural economy of developing countries [11,16]. However, with the genetic differences between the three species causing AAT becoming clearer, it appears that differences in drug sensitivity can result from differences in their capacity to internalize the drugs [17,18] and loss of the unique transporters involved often contributes to drug resistance [19,20,21,22]. It is thus clear that in AAT drug design, one should consider exploiting the specific transporters for guiding drugs to their intracellular targets. This is important given that drug transport directly through the phospholipid membrane, i.e., by simple diffusion, is now believed to be negligible [23].
Purine salvage is an essential feature in protozoan parasites, which lack the capacity for the de novo synthesis of this essential nutrient [24,25]. Therefore, these parasites have developed highly specialized transporters in their membrane for the internalization of the hydrophilic nucleosides from the host environment [26]. To date, all protozoan purine and pyrimidine transporter genes identified have been of the Equilibrative Nucleoside Transporter (ENT) family [25,26,27,28,29,30], although there is a quite strong likelihood that some protozoan purine and/or pyrimidine carriers are expressed by other gene families [31,32]. Where this has been investigated, it was found that the trypanosomatid nucleoside transporters are concentrative proton symporters that exclude uric acid; acidification of the cytosol is prevented by H+-ATPases in the plasma membrane [33,34,35]. This feature distinguishes protozoan from mammalian ENT transporters, which allow only facilitated diffusion [36,37]. The coupling to the protonmotive force provides the energy for active transport, concentrating the substrate in the cell and making it possible to selectively target the transporters for the highly effective accumulation of toxic nucleoside drugs in trypanosomatids [26,38].
Brucei-group trypanosomes express two types of nucleoside transporters: multiple adenosine/inosine/guanosine carriers (P1-type) and the adenosine/adenine transporter (P2), encoded by a single gene [39,40,41,42]. The P2 transporter interacts with its substrates through the unprotonated N1, C6-NH2 and N9 of the purine ring [43,44,45], making it highly effective for the uptake of the toxic nucleosides tubercidin, cordycepin [46,47] and the 3′-deoxy-7-deazaadenosine analogs that combine the features of both nucleoside antibiotics [38,48]. Moreover, the transport of currently used drugs including diamidines, pentamidine and melaminophenyl arsenicals in brucei group trypanosomes depends on the P2 transporter [20,49,50,51]. However, the P1 transporter can also be critical for the uptake of other toxic nucleosides through interaction with the N3, N7, 3′-OH and 5′-OH functional groups [26,39,40,44]. Therefore, while T. congolense and T. vivax lack orthologues of the P2 transporter [52], the presence of a P1-type transporter in all three species causing AAT would present a unique chemotherapeutic potential.
Phylogenetic analysis has revealed the presence of a single nucleoside transporter gene in T. congolense (named TcoAT1 or TcoNT10) and identified four putative nucleoside transporter genes in T. vivax genome [52,53]. TcoAT1 was earlier hypothesized to be a P2-type transporter and a determinant of drug resistance in T. congolense, based on the identification of mutations in the gene encoding the transporter, in diminazene-resistant field isolates [54]. Already diagnostic tests for the detection of a single point mutation in TcoAT1 have been developed and improved [54,55], and applied either alone or in combination with other methods [56,57,58]. However, the expression of the TcoAT1 gene in B48, a multidrug-resistant T. brucei strain lacking TbAT1 [59], did not result in any significant increase in uptake or sensitivity to diminazene, pentamidine or melarsomine [52]. More recently, laboratory-generated diminazene resistant strains of T. congolense did not show a reduced uptake of diminazene compared to the diminazene-sensitive control and were devoid of mutations in the TcoAT1 gene [60]. The functional characterization thus shows that TcoAT1 is a P1-type rather than a P2-type nucleoside transporter. Despite the interest in TcoAT1, the transporter’s substrate affinity and chemotherapeutic potential are yet to be fully characterized.
Four putative T. vivax ENT genes are suggested to encode for P1-type transporters due to their phylogenetic proximity to T. congolense, T. cruzi and T. brucei P1 transporters [52,53]. However, these T. vivax putative ENT’s have not been studied to date. Other pathogenic trypanosomatids such as T. cruzi and Leishmania spp. also express several P1-type nucleoside transporters [27,61]. Leishmania spp. nucleoside transporters (NT1 and NT2) are evolutionary conserved in L. donovani, L. major and L. mexicana; Leishmania NT1 is an adenosine and pyrimidine nucleoside transporter that is encoded by two closely related genes (NT1.1 and NT1.2), while NT2 transports inosine and guanosine [61,62,63]. Thus, broad-spectrum nucleoside transporters are common among kinetoplastid parasites while the P2 adenosine/adenine transporter is restricted to brucei-group trypanosomes.
We recently reported a sequential knock-out of the LmexNT1.1, NT1.2 and NT2 genes using CRISPR/Cas9 technology [64] in promastigotes, resulting in a mutant model with null background purine and pyrimidine nucleoside uptake named SUPKO, which was validated as a surrogate system that allows the functional transgenic expression and characterization of protozoan nucleoside transporters [29]. Here, we use this system to express TcoAT1 and the putative T. vivax ENTs in order to establish their substrate preferences. In parallel, we studied the transport of adenosine in bloodstream forms of T. congolense to establish whether this activity can be ascribed to TcoAT1. The ultimate aim of this effort is to investigate whether there are nucleoside transporters in all of the main Trypanosoma spp. that cause AAT (T. brucei, T. congolense, T. vivax) that display sufficiently similar substrate preferences so that the same (class of) nucleoside analogs will be efficiently taken up by all three species, with the hope of finding nucleoside antimetabolites that can effectively treat AAT caused by all three species. That could lead to a treatment of AAT regardless of the infecting species. Nucleoside analogs have recently emerged as potent agents against protozoan parasites including T. brucei, T. cruzi, T. congolense and Trichomonas vaginalis [39,48,65,66,67,68], but the first efforts to identify analogs that are active against all three AAT pathogens had only limited success [69].
2. Results
2.1. Nucleoside Transport Activity in T. congolense
The genome of T. congolense contains 17 ENT-family transporter genes but only one aligns phylogenetically with the well-characterized nucleoside transporters of other kinetoplastid species, the others with the T. brucei NT8/NBT1 nucleobase transporters [70,71] and the T. cruzi NB1 hypoxanthine/guanine transporter [27,53]. The 16 putative nucleobase transporter genes divide into two distinct clades of 8 genes each (Supplemental Figure S1). Clade 1 consists of 8 closely related genes, 7 of which encode a protein of 339 amino acids, the last of 352 amino acids. Importantly, each are predicted to have just six transmembrane domains (TMDs), which makes it very unlikely that they are able to function as ENT transporters, which typically have 10 or 11 TMDs [37]. The second clade contains 7 genes encoding full-length transporters of 441–447 amino acids and 10 or 11 TMDs, as well as 1 apparently truncated gene encoding a protein of 320 amino acids and just 7 TMDs (Supplemental Table S1). A multiple alignment of the T. congolense nucleobase transporters shows that the Clade 1 genes lack the canonical C-terminal sequence of ~100 amino acids (Supplemental Figure S2). This analysis shows that the T. congolense reference genome contains 7 putative nucleobase transporters, 1 nucleoside transporter and 9 apparently truncated copies that are unlikely to contribute to pyrimidine or purine uptake.
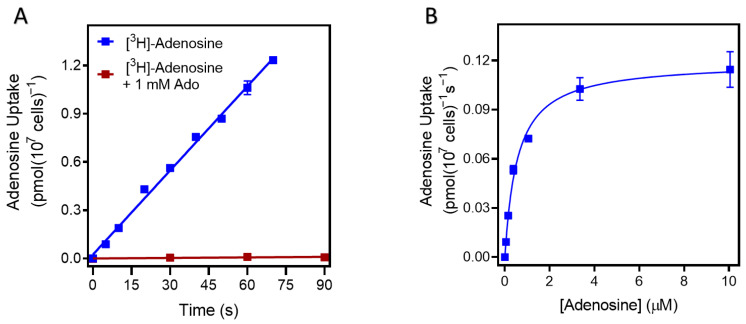
The sole T. congolense nucleoside transporter, TcoAT1/TcoNT10 (TcIL3000_9_2500 or TcIL3000.A.H_000665800; TriTrypDB), was shown to increase the transport of adenosine and inosine when expressed in a T. brucei surrogate [52]. However, nucleoside transport in cultured or ex vivo T. congolense cells has not yet been reported. We determined the rate of adenosine uptake in cultured T. congolense IL3000 as 0.014 ± 0.0037 pmol(107 cells)−1s−1 (n = 2). Uptake of 50 nM [3H]-adenosine was linear (r2 = 0.996) over 70 s and was saturable, as transport in the presence of 1 mM unlabeled adenosine was not significantly different from zero (p = 0.18, F-test) (Figure 1A). Thus, a 30 s incubation time was selected for further inhibition studies in T. congolense, as being well inside the linear phase of uptake. This allowed for the transporter’s Km for adenosine to be determined as 0.48 ± 0.03 µM and the Vmax as 0.11 ± 0.02 pmol(107 cells)−1s−1 (n = 3) (Figure 1B). In each experiment, the Hill slope was very close to −1 consistent with a single transporter being responsible for the adenosine uptake observed; 1 mM adenosine saturated the transporter completely (Figure 1A,B). In addition, inosine and guanosine inhibited adenosine uptake with Ki values of 0.27 ± 0.02 µM and 1.06 ± 0.07 µM, respectively. However, the pyrimidines cytidine, thymidine and uridine showed poor inhibition of adenosine uptake with Ki values >90-fold higher than those for the purines (Table 1).
Figure 1.
The uptake of 0.05 µM [3H]-adenosine in T. congolense IL3000. (A) Uptake over time, and (B) uptake at a fixed time point of 30 s, in the presence of unlabeled adenosine for the Km determination, using 0–1 mM adenosine in bloodstream forms of T. congolense. Graphs show one representative experiment out of two (panel A) or three (panel B) independent repeats, each carried out in triplicate. Error bars represent standard error of the mean (SEM).
Table 1.
Km and Ki values for nucleosides on the transport of [3H]-adenosine by T. congolense IL3000 and of T. b. brucei P1.
| Compound | Tc Km or Ki (µM) |
ΔG0 (kJ/mol) |
n | Tbb P1 1 (µM) |
ΔG0 (kJ/mol) |
|---|---|---|---|---|---|
| Adenosine | 0.48 ± 0.03 | −36.0 | 3 | 0.36 ± 0.05 | −36.8 |
| Tubercidin | 403 ± 120 | −19.3 | 3 | 78 ± 6.4 | −23.4 |
| Cordycepin | 12.0 ± 2 | −28.0 | 3 | 210 ± 48 | −21.0 |
| Inosine | 0.27 ± 0.02 | −37.5 | 3 | 0.44 ± 0.10 | −36.3 |
| Guanosine | 1.06 ± 0.07 | −34.1 | 3 | 1.8 ± 0.3 | −32.7 |
| Uridine | 390 ± 9.1 | −19.4 | 3 | 830 ± 86 | −18.7 |
| Thymidine | 94.6 ± 11.5 | −23.0 | 3 | 44 ± 10 | −11.4 |
| Cytidine | 1176 ± 148 | −16.7 | 3 | >250 |
IC50 values obtained were converted to Ki based on the Km of adenosine and determined using a [3H]-adenosine concentration of 0.05 µM. All experiments were performed in triplicate. IC50 values were based on a minimum of 5 points on the curve, which was extrapolated to zero when necessary but only when inhibition at the highest concentration already exceeded 50%. ΔG0, Gibbs free energy of interaction. 1 values taken from De Koning and Jarvis [44] for easy side-by-side comparison.
The previously reported Ki values for P1-mediated uptake in T. b. brucei bloodstream forms [44] were also included in this table. It can be seen that the affinity for both purine and pyrimidine nucleosides was very similar for both transport systems. Indeed, as in T. b. brucei P1, N7 of the purine ring and the 3′-hydroxy group are shown to be important for adenosine binding by the T. congolense adenosine transporter as shown by the reduced affinity for tubercidin (7-deazaadenosine) and cordycepin (3′-deoxyadenosine), respectively. This profile is in sharp contrast to the substrate preferences of the T. b. brucei P2 transporter, which has high affinity for adenosine, cordycepin, tubercidin and adenine but not for inosine and guanosine [44,47], and we conclude that nucleoside salvage in T. congolense is through a P1-type transporter.
2.2. Expression of T. congolense and T. vivax Nucleoside Transporters in a L. mexicana NT-Null Cell Line
2.2.1. Nucleoside Transporters of T. vivax
In T. congolense, only TcoAT1 is identified as a nucleoside transporter. On the other hand, four of the putative ENT-family genes in T. vivax showed closest proximity to T. brucei and T. congolense P1-type nucleoside transporter clade while three other ENT-family genes and two shorter fragments aligned best with the nucleobase transporter gene cluster (Table 2) [52,53]. The ENT-family genes of T. vivax were given numerical names TvxNT1—TvNT7, with the first four aligning with nucleoside transporters and the other three as nucleobase transporters. TvxNT4 lacked the C-terminal sequence of ~100 amino acids, much like some of the T. congolense nucleobase transporters discussed above, and it remains to be seen whether any one of them is functional. TvxNT5 has an intact C-terminal sequence but misses the first 51 amino acids including TMD1. It seems possible that some of these truncations may be due to inaccuracies in genome assembly.
Table 2.
ENT family genes of T. vivax.
| Gene ID | Given Name | Number of Amino Acids | Number of TMDs |
Closest Related T. brucei Transporter |
Remarks |
|---|---|---|---|---|---|
| Nucleoside transporters | |||||
| TcIL3000_9_2500 | TcoAT1/TcoNT10 | 472 | 10 | TbNT10 | P1-type |
| TvY486_0202110 | TvxNT1 | 472 | 11 | TbNT4 | P1-type |
| TvY486_1112030 | TvxNT2 | 470 | 11 | TbNT12 | P1-type |
| TvY486_0043680 | TvxNT3 | 464 | 10 | TbNT6 | P1-type |
| TvY486_0014570 | TvxNT4 | 373 | 7 | TbNT10 | P1-type |
| Nucleobase transporters | |||||
| TvY486_0011610 | (fragment) | 284 | 6 | NT8 | ----- |
| TvY486_1103750 | (fragment) | 150 | 4 | NT8 | ----- |
| TvY486_1103760 | TvxNT5 | 385 | 9 | NT8 | NBT |
| TvY486_0041960 | TvxNT6 | 437 | 10 | NT8 | NBT |
| TvY486_1103740 | TvxNT7 | 436 | 10 | NT8 | NBT |
Gene IDs from TriTrypDB. NBT, nucleobase transporter. TMDs called by TMHMM—2.0.
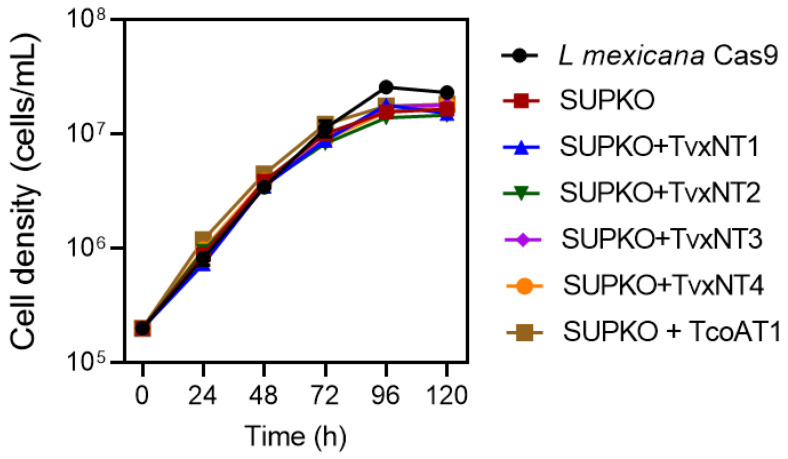
We have earlier reported the successful characterization of trypanosomatid nucleoside transporters by cloning and expression in T. brucei TbAT1-KO and TbNBT1-KO surrogates [31,52]. However, both surrogates exhibited background nucleoside and nucleotide uptake, thus limiting the extent to which the exogenous transporter can be characterized. Here we used a L. mexicana promastigote line with null nucleoside (NT1.1, NT1.2 and NT2-KO; ‘SUPKO’) or null nucleobase uptake (NT3-KO) as surrogates [29]. TcoAT1 and each of the four T. vivax ENT family putative nucleoside transporters (TvxNT1–4) and TcoAT1 were PCR-amplified from genomic DNA, cloned into the pNUS-HcN vector, and transfected into SUPKO as described [72]. We observed that SUPKO and all of the transgenic lines generated displayed identical growth relative to the parental LmexCas9 cell line, but that LmexCas9 reached a statistically significant higher cell density (two-tailed t-test, p < 0.05) (Figure 2). There were differences in growth rate or cell density between SUPKO and the cells expressing the T. congolense or T. vivax ENT transporters. This can be explained by the possibility that none of these transporters carried sufficient nucleosides to make up for the loss of the L. mexicana nucleoside transporters NT1.1, NT1.2 and NT2.
Figure 2.
Growth curve of L. mexicana Cas9, SUPKO, and SUPKO clones expressing T. congolense and T. vivax nucleoside transporters. Cells were seeded at density of 2 × 105 cells/mL in HOMEM medium and counted manually in a Neubauer chamber viewed under microscope every 24 h. Graph was plotted using the average count of three independent determinations (Mean ± SEM; n = 3). When error bars are not shown they fall within the symbol.
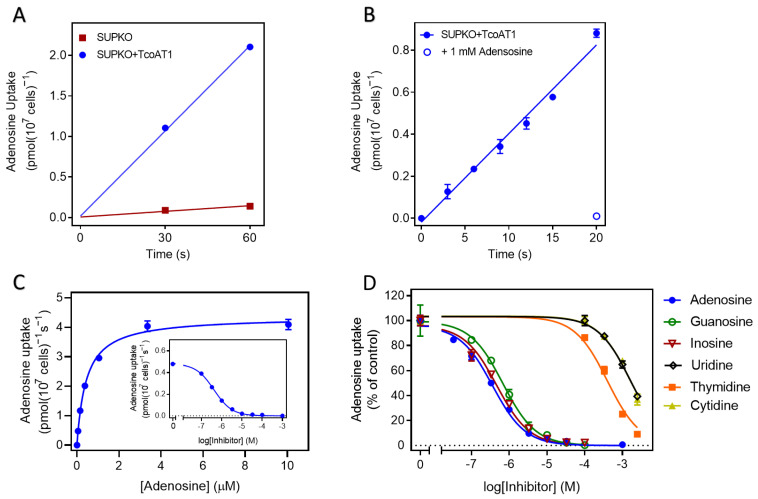
2.2.2. TcoAT1 Basic Characterization and Adenosine Binding Model
The expression of TcoAT1 in SUPKO restored the uptake of [3H]-adenosine. SUPKO+TcoAT1 strongly increased the rate of uptake of [3H]-adenosine over 60 s relative to SUPKO (0.035 ± 0.001 vs. 2.3 × 10−3 ± 3.5 × 10−4 pmol(107 cells)−1s−1 (p = 0.0017, F-test) (Figure 3A). The uptake of [3H]-adenosine in SUPKO was not significantly different from zero (p = 0.10, F-test), whereas uptake in SUPKO+TcoAT1 was significant (p = 0.018) and linear (not significantly non-linear, p > 0.99, runs test). In a separate experiment, linearity of adenosine uptake in SUPKO+TcoAT1 was tested with more points over 20 s. Again, there was no significant deviation from linearity (p = 0.20) and the rate was highly similar to the first experiment (0.012 ± 0.002 pmol(107 cells)−1s−1); the addition of 1 mM of unlabeled adenosine completely inhibited [3H]-adenosine uptake, indicating a complete saturation of the transporter (Figure 3B).
Figure 3.
Uptake of 0.05 µM [3H]-adenosine in L. mexicana SUPKO expressing TcoAT1. (A) Uptake in L. mexicana SUPKO and SUPKO+TcoAT1 over 60 s. The expression of TcoAT1 restored adenosine uptake in SUPKO. Data represent averages ± SEM of triplicate determinations. (B) Uptake of [3H]-adenosine in L. mexicana SUPKO+TcoAT1 within linear phase of 20 s. (C) Adenosine uptake by SUPKO+TcoAT1 in the presence of 0–1 mM unlabeled adenosine. Graph shows one representative out of three independent experiments carried out in triplicate all showing a similar result. (D). Substrate specificity of TcoAT1 determined by uptake assays. TcoAT1 has high affinity for both amino- and oxopurines. Inhibition constants (Ki) for purines were lower than those of pyrimidines. Adenosine uptake is presented as percentage of no-inhibitor control. Figure shows one representative out of three independent experiments carried out in triplicate (% adenosine uptake average ± SEM).
Using 10 s incubation, being well inside the linear phase of uptake, the affinity of various purines and pyrimidines to the transporter was determined. These kinetic studies revealed TcoAT1 to be a high affinity purine transporter with specificity for adenosine, inosine and guanosine (Figure 3C,D) with a Km for adenosine of 0.42 ± 0.03 µM (Figure 3C, Table 3), statistically identical to the value obtained for adenosine uptake in T. congolense bloodstream forms (p = 0.30). Also consistent with the transport results in T. congolense, this transporter discriminates against pyrimidine nucleosides. Furthermore, TcoAT1, like T. b. brucei P1 [44], displayed low affinity for purine nucleobases. This suggests that both the ribose sugar and the purine ring are important for the interaction of this transporter with its substrates.
Table 3.
Ki for purines on the transport of 0.05 µM [3H]-adenosine by TcoAT1 expressed in SUPKO.
| Purine | Km or Ki (μM) | ΔG0 | δ(ΔG0) | n |
|---|---|---|---|---|
| Adenosine | 0.42 ± 0.03 | −36.4 | 3 | |
| Inosine | 0.55 ± 0.09 | −35.7 | 0.68 | 3 |
| Guanosine | 0.80 ± 0.09 | −34.8 | 1.62 | 3 |
| 2′-deoxyadenosine | 0.50 ± 0.07 | −36.0 | 0.44 | 3 |
| 5′-deoxyadenosine | 0.45 ± 0.08 | −36.2 | 0.18 | 3 |
| Cordycepin | 4.59 ± 0.63 | −30.5 | 5.94 | 3 |
| 2′,3′-dideoxyinosine | 85.4 ± 7.1 | −23.2 | 12.51 | 3 |
| 2′,3′-dideoxyadenosine | 51.9 ± 2.6 | −24.4 | 11.95 | 3 |
| 1-deazaadenosine | 1.03 ± 0.34 | −34.2 | 2.24 | 4 |
| 3-deazaadenosine | 138 ± 37 | −22.0 | 14.37 | 3 |
| Tubercidin | 754 ± 54.3 | −17.8 | 18.58 | 3 |
| Uridine | 1467 ± 172 | −16.2 | 20.23 | 3 |
| Thymidine | 434 ± 46.4 | −19.2 | 17.21 | 4 |
| Cytidine | 1577 ± 69.2 | −16.0 | 20.41 | 3 |
| Adenine | 761± 103 | −17.8 | 18.60 | 5 |
| Hypoxanthine | 61.2 ± 3.26 | −24.0 | 11.68 | 3 |
EC50 values obtained were converted to Ki based on the Km of adenosine. All experiments were performed in triplicate. IC50 values were based on a minimum of 5 points on the curve, which was extrapolated to zero when necessary but only when inhibition at the highest concentration already exceeded 50%.
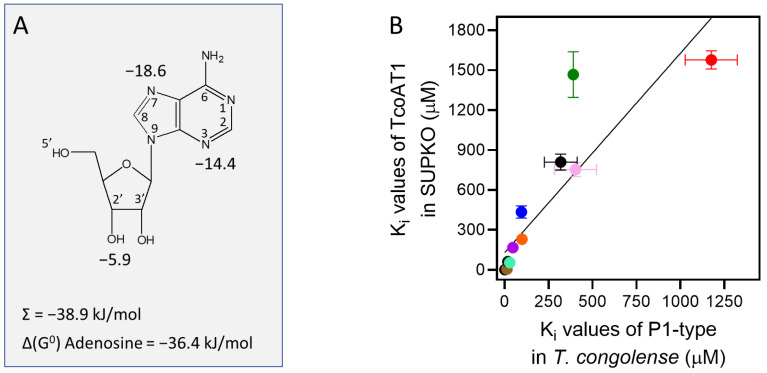
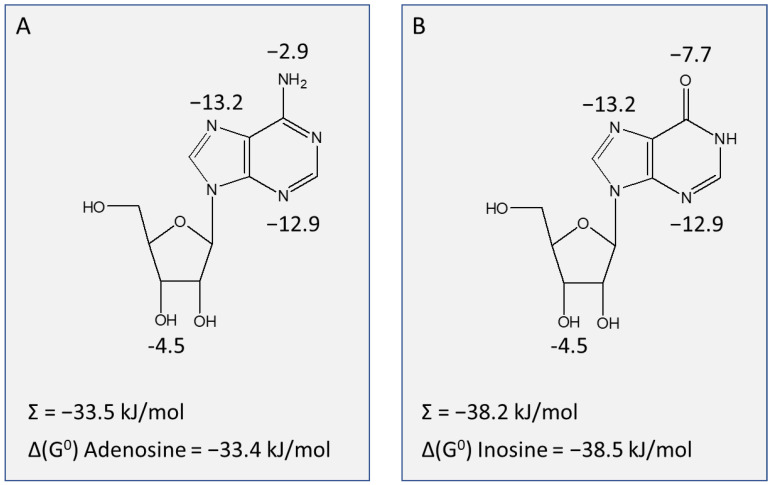
To determine the functional groups of the ribose moiety that contribute positively to interactions with the TcoAT1 binding site, the 2′-, 3′- and 5′-hydroxy groups were investigated. While both 2′-deoxyadenosine and 5′-deoxyadenosine did not show a significant difference in affinity compared to adenosine (p > 0.4), 3′-deoxyadenosine (cordycepin) presented a 10-fold difference in activity compared to adenosine (Ki 4.59 ± 0.63 μM, p = 0.006), corresponding to a loss of 5.94 kJ/mol in the Gibbs free energy of binding (ΔG0) (Table 3). However, 2′,3′-dideoxyadenosine and adenine presented even lower affinity, with Ki values of 51.9 ± 2.6 µM and 761± 103 µM, respectively. These observations, taken together, reveal that the 3′-oxygen is the most important functional group of ribose for recognition by the transporter. In its absence, it appears that some of the binding is taken over by the 2′-hydroxy, indicating a degree of flexibility. In addition, hypoxanthine and 2′,3′-dideoxyinosine showed a lower affinity compared to inosine. These observations are all consistent with a hydrogen bond of ~12 kJ/mol between the TcoAT1 substrate binding site and the ribose moiety, mostly through 3′-hydroxy, with a possible assist from the 2′ position. The main interactions with the purine ring occur at N3 and N7, given the large loss of interaction energy for 3-deazaadenosine (14.4 kJ/mol) and tubercidin (18.6 kJ/mol), respectively. The 6-position and N1 do not seem to contribute significantly to binding, as shown by the pairwise comparisons of adenosine vs. inosine (p = 0.31) and adenosine vs. 1-deazaadenosine (p = 0.25). These observations result in the binding model for adenosine by TcoAT1 depicted in Figure 4A.
Figure 4.
Model of adenosine uptake by TcoAT1. (A) Model for the interactions between adenosine and the TcoAT1 binding pocket, showing interactions at N3, N7 and 3′-OH, with Gibbs free energy of interaction indicated in kJ/mol. The sum of these energies and the experimental value for the adenosine ΔG0 is also indicated. (B) Correlation of Ki values for nucleosides and nucleobases in T. congolense TcoAT1-type and TcoAT1 expressed in SUPKO. The Ki values obtained for each substrate revealed a similar affinity trend for TcoAT1 in the parasite and when expressed in the SUPKO surrogate (r2 = 0.78). Slope was significantly different from zero (p < 0.0001 by F-test).
Although uptake assays in T. congolense IL3000 and in SUPKO+TcoAT1 did not produce exactly identical Ki values for most of the substrates, the pattern of affinity across the inhibitors was comparable in both cell lines. On average, the Ki value is consistently ~2-fold higher in TcoAT1 expressed in SUPKO than measured in T. congolense IL3000; in a correlation plot the slope was 1.98 (r2 = 0.78; Figure 4B). This small difference is likely owing to a difference in the lipid composition of the plasma membrane of L. mexicana and of T. congolense bloodstream forms. When combined with the Hill scope for these assays being close to −1, as well as the phylogenetic evidence, this greatly strengthens the hypothesis that TcoAT1 is the principal purine nucleoside transporter in T. congolense—at a minimum for adenosine. Pyrimidine uptake in T. brucei is mostly in the form of uracil [73,74] rather than nucleosides but this is yet to be investigated in T. congolense.
2.2.3. TvxNT3 Basic Characterization and Adenosine Binding Model
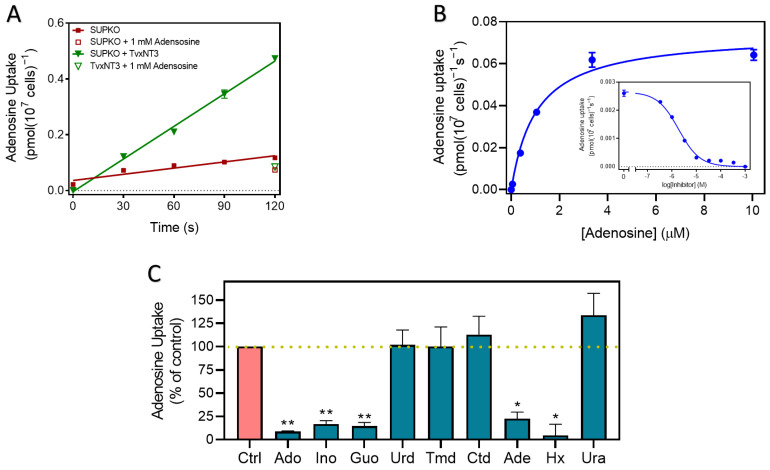
Following the incubation of SUPKO clones expressing each of the four T. vivax putative nucleoside transporters with [3H]-adenosine, only clones carrying T. vivax NT3 (SUPKO+TvxNT3) showed a level of uptake of 50 nM adenosine that was significantly higher than the untransfected SUPKO control (3.9 × 10−3 vs. 7.4 × 10−4 pmol(107 cells)−1s−1; p < 0.0001, F-test; Figure 5A); uptake was linear for 120 s. Further screening with other nucleosides (100 nM [3H]-guanosine, 25 nM [3H]-cytidine, 100 nM [3H]-thymidine and 100 nM [3H]-uridine) did not reveal any differences in uptake between untransfected SUPKO and SUPKO transfected with the other three T. vivax NTs either (p > 0.05) and we thus proceeded with the detailed characterization of TvxNT3, using [3H]-adenosine as the probe.
Figure 5.
[3H]-adenosine (0.05 µM) uptake by TvxNT3 expressed in SUPKO. (A) Uptake over 120 s compared to control, and (B) Uptake in the presence of 0–1 mM unlabeled adenosine. (C) Adenosine uptake in SUPKO+TvxNT3 in the presence of unlabeled nucleosides and nucleobases. Purine and pyrimidine nucleobases and nucleosides at 100 µM competed with 0.05 µM of [3H]-adenosine for transport through TvxNT3. Figure shows the average of three independent experiments, each carried out in triplicate (% adenosine uptake average ± SEM, n = 3). Statistically significant difference from the control was determined by an unpaired, two-tailed t-test; *, p < 0.05; **, p < 0.01.
Figure 5B shows a dose-dependent inhibition of 50 nM [3H]-adenosine uptake by unlabeled adenosine, showing complete saturation at high concentrations; conversion to a Michaelis-Menten plot yielded a Km of 1.41 ± 0.35 µM (n = 3).
SUPKO + TvxNT3 cells were incubated with 50 nM [3H]-adenosine in the presence of 100 µM of pyrimidine and purine nucleosides and nucleobases to determine the transporter’s substrate specificity. Out of these compounds, adenosine, inosine, guanosine, adenine and hypoxanthine inhibited the uptake of [3H]-adenosine significantly (n = 3; p < 0.05 or p < 0.01), and to less than 25% of the uninhibited control (Figure 5C). This indicates that TvxNT3 exhibits broad specificity for purine nucleosides and nucleobases but not for pyrimidines. The dose-dependent inhibitor assays of adenosine uptake were then carried out using 90 s incubation, which is within the linear phase of adenosine uptake for this transporter (Figure 5A). This allowed for the determination of the inhibition constant (Ki) of various purine and pyrimidines for this transporter.
The purine ring was the main site of interaction with the transporter binding pocket, as purine bases and nucleosides both displayed high affinity with Ki values for inosine, guanosine, adenine and hypoxanthine all below 3 µM, whereas pyrimidine nucleosides uridine and thymidine had orders of magnitude lower affinity (Table 4). Among purine nucleosides, inosine exhibited an approximately 7.7-fold lower Ki value for the transporter, than adenosine and guanosine.
Table 4.
Ki for purines on the transport of [3H]-adenosine by TvxNT3.
| Ki | |||||
|---|---|---|---|---|---|
| AVG | SEM | n | ΔG0 | δ(ΔG0) | |
| Adenosine | 1.41 | 0.35 | 3 | −33.38 | |
| Guanosine | 1.37 | 0.13 | 3 | −33.45 | 0.07 |
| Inosine | 0.18 | 0.05 | 3 | −38.46 | 5.08 |
| 2′-deoxyadenosine | 1.06 | 0.29 | 3 | −34.1 | 0.70 |
| 5′-deoxyadenosine | 1.10 | 0.12 | 3 | −34.0 | 0.63 |
| Cordycepin | 8.6 | 1.4 | 3 | −28.91 | −4.47 |
| Tubercidin | 287 | 55 | 3 | −20.21 | −13.17 |
| Nebularine | 4.6 | 1.1 | 4 | −30.4 | −2.94 |
| 6-thioinosine | 4.03 | 0.78 | 4 | −30.8 | −7.7 |
| 3-deazainosine | 33.0 | 17.4 | 4 | −25.6 | −12.9 |
| Adenine | 2.43 | 0.14 | 2 | −32.04 | −1.34 |
| Hypoxanthine | 1.75 | 0.17 | 3 | −32.85 | −7.45 |
| Uridine | 720 | 110 | 3 | −17.93 | −15.45 |
| Thymidine | 603 | 51 | 3 | −18.37 | −15.01 |
The high affinity to TvxNT3 shown by hypoxanthine and adenine appears to suggests that high affinity for this transporter is not dependent on the ribose sugar, unlike the T. brucei and T. congolense P1 transporters, but similar to P2 [44]. Yet, while the removal of 2’-OH and 5’-OH from adenosine did not affect its affinity, the removal of 3’-OH caused a 6-fold decrease in affinity, corresponding to a loss of 4.47 kJ/mol in the Gibbs free energy of interaction. This clearly shows that 3′-OH does in fact positively contribute to the binding of purine nucleosides, as it does for the T. b. brucei P1 transporter [44] and TcoAT1. Moreover, the energy difference δ(ΔG0) between inosine and hypoxanthine was determined to be 5.61 kJ/mol and the Ki values were highly significantly different (p = 0.0021)—similarly indicating a contribution of ribose in the binding of inosine. In contrast, the δ(ΔG0) between adenosine and adenine was only 1.34 kJ/mol and the Ki values were not significantly different (p = 0.17). The conclusion of these seemingly contradictory results must be that nucleosides bind differently in the TvxNT3 binding pocket from nucleobases. Adenine in particular clearly makes either additional interactions or perhaps stronger interactions than the adenine moiety of adenosine. This situation is similar to that recently shown for the Toxoplasma gondii transporter Tg244440 [28].
We investigated the interactions of the purine nucleosides with TvxNT3, in order to delineate the limitations of modifications that can made while retaining uptake through this transporter. The importance of N7 for binding followed from the low affinity displayed for tubercidin (7-deazaadenosine; δ(ΔG0) = 13.2 kJ/mol relative to adenosine). A strong interaction was also evidenced for N3, by the δ(ΔG0) of 12.9 kJ/mol between inosine and 3-deazainosine (Table 4). It appears that the 6-amine group of adenosine makes at best a minor contribution (δ(ΔG0) = 2.9 kJ/mol, adenosine vs. nebularine) and that the significant difference (p = 0.045) in affinity between adenosine and inosine is the result of a positive contribution of the 6-oxo group (δ(ΔG0) = 7.7 kJ/mol, inosine vs. 6-thioinosine; p = 0.016). These data suggest that the nucleoside binding mode is not dissimilar to the known binding mode of T. brucei P1, especially N3, N7, 3′-OH being the main contact points (Al-Salabi et al., 2007), and the sum of the proposed interactions closely matches that of the observed ΔG0 for adenosine (Figure 6A). However, inosine is bound slightly different from T. b. brucei P1 in that there is a significant interaction with 6-oxo; for this nucleoside too, the sum of the interactions (N3, 6-oxo, N7 and 3′-hydroxy) closely matches the experimental value calculated from the Km (Figure 6B).
Figure 6.
Binding model for TvxNT3 showing points of interaction in adenosine (A) and inosine (B), with the Gibbs free energy of the interaction indicated in kJ/mol. The sum of the interactions and the experimental interaction energies are also indicated.
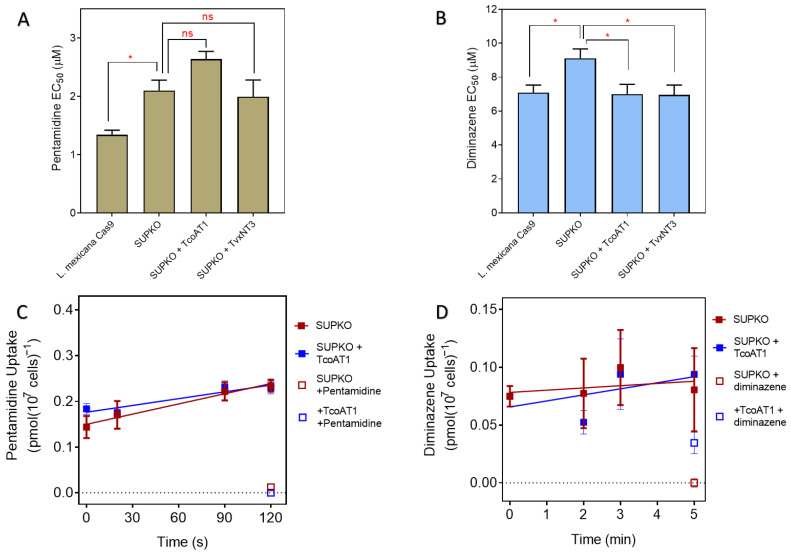
2.3. P1 Transporters Do Not Transport Any of the Trypanocides in Current Clinical Use
We previously reported that the expression of TcoAT1 in multidrug-resistant T. brucei B48 did not result in an increase in sensitivity to diminazene and pentamidine [52]. To confirm this important observation and to investigate whether T. vivax NT3 has any role in sensitivity or resistance to the trypanocides in use, we carried out drug sensitivity and uptake assays in L. mexicana Cas9, SUPKO, SUPKO+TcoAT1 and the SUPKO+TvxNT3 cell lines in parallel. While SUPKO is slightly less sensitive to pentamidine (1.57-fold) compared to the parental line L. mexicana Cas9, the expression of either TcoAT1 or TvxNT3 in SUPKO did not result in a significant increase in sensitivity to pentamidine (Figure 7A), although the expression of the T. b. brucei pentamidine transporter TbAQP2 in L. mexicana has been shown to sensitize these cells 40-fold to pentamidine [75]. In addition, SUPKO showed only a 1.27-fold decrease in sensitivity to diminazene compared to L. mexicana Cas9 (Figure 7B). Expression of TcoAT1 or TvxNT3 in SUPKO did not sensitize the cells to pentamidine and only marginally increased sensitivity diminazene, effectively reversing the minor difference between SUPKO and the parental Cas9 cells (Figure 7A,B). The EC50 values of two other trypanocides, melarsomine and suramin, to which Leishmania spp are not normally sensitive, remained >100 µM in all the cell lines investigated. Similar to pentamidine, melarsomine sensitivity increased greatly upon expression of TbAQP2 [75].
Figure 7.
Effect of expression of T. congolense and T. vivax nucleoside transporters on the activity and uptake of trypanocides in L. mexicana. (A) Pentamidine sensitivity and (B) Diminazene sensitivity. Sensitivity is represented as EC50 averages of 4 independent determinations (mean ± SEM). * p < 0.05; ns = not significant by unpaired Student’s t-test. Uptake of (C) 25 nM [3H]-Pentamidine or (D) 50 nM [3H]- in SUPKO+TcoAT1 and SUPKO control cells. At each predetermined time point, uptake was stopped in the corresponding sample by the addition of high concentration of unlabeled substrate followed by centrifugation. Graph was plotted using the average uptake (mean ± SEM) in pmol(107 cells)−1) of an experiment performed in triplicate. Lines were calculated by linear regression.
We next investigated the rate of uptake of [3H]-Pentamidine (Figure 7C) and [3H]-diminazene (Figure 7D) between SUPKO and SUPKO+TcoAT1. The slopes and intercepts of SUPKO and of SUPKO+TcoAT1 were not significantly different (p > 0.05), indicating that the expression of TcoAT1 had no effect on the uptake of either trypanocide. This supports the previous evidence that, unlike P2, P1-type nucleoside transporters are not carriers of currently used trypanocides of the diamidine and melaminophenyl arsenical classes [52,60] and can be targeted as conduits for new drugs without a risk of transport-related cross-resistance [38,65].
2.4. Trypanosomal P1 as Carrier of Novel Nucleoside Drugs
2.4.1. Affinity of Nucleoside Drugs to T. congolense Nucleoside Transporters
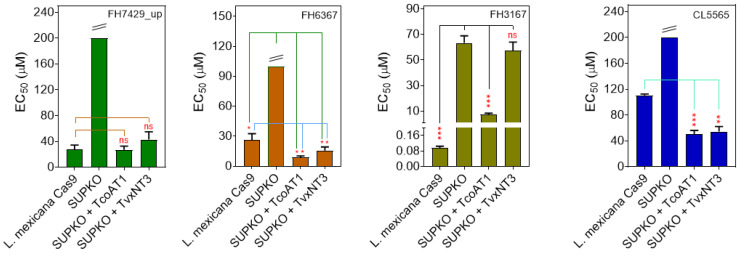
The potential of the T. brucei P1 nucleoside transporter as a conduit for toxic nucleoside drugs has been described [38]. Therefore, we tested some nucleoside analogs against L. mexicana Cas9, SUPKO, SUPKO+TcoAT1 and SUPKO+TvxNT3 in parallel. The CRISPR/Cas9 deletion of nucleoside transporters in L. mexicana resulted in significant reduction in the sensitivity of the resultant SUPKO line to tubercidin analogs (Figure 8; Table 5). Notably, SUPKO exhibited ~660-fold resistance to FH3167 (7-deaza-7-fluoroadenosine) compared to parental L. mexicana Cas9 cell line, presumably due to the deletion of the LmexNT1.1 and NT1.2 transporters. Similarly, SUPKO lost sensitivity to FH7429_u (7-bromo-7-deaza-3′-deoxyadenosine) to above the 250 µM cutoff, and also displayed significant resistance to FH6367 (7-trifluoromethyl-7-deazaadenosine) (Figure 8). The expression of either TcoAT1 or TvxNT3 in SUPKO restored the lost sensitivity to most of the 7-substituted tubercidin analogs, but not to tubercidin itself (Table 5), which we have above shown to be a poor substrate for both TcoAT1 and TvxN3. The degree to which the sensitivity was increased upon expression of the T. congolense and T. vivax adenosine transporters differed from partial restoration (e.g., FH3167) to a significantly higher level of sensitivity than Cas9 (e.g., FH6367), presumably reflecting the relative efficiency of transport by the L. mexicana and Trypanosoma transporters. On this basis it appears that TcoAT1 and TvxNT3 prefer trifluoromethyl and the larger halogens (I > Br > Cl > F) on position 7 of tubercidin. Aromatic substitutions at this position (2-pyridine; TH1008) do not seem to be tolerated.
Figure 8.
The sensitivity of T. congolense and T. vivax nucleoside transporters to nucleoside analogs. The expression of TcoAT1 and TvxNT3 in SUPKO restored sensitivity to tubercidin analogs. Sensitivity is represented as EC50 averages of three independent determinations (mean ± SEM). * p < 0.05; ** p < 0.01; *** p < 0.001; ns = not significant by unpaired Student’s t-test compared with SUPKO. The double line above some bars indicates that the true value could not be extrapolated beyond 250 µM.
Table 5.
Effect of the expression of nucleoside transporters on the sensitivity of tubercidin analogs.
| Compound | 3′ | 6-Subst | 7-Subst | LmexCas9 | SUPKO | SUPKO+TcoAT1 | SUPKO+TvxNT3 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| EC50 (µM) | EC50 (µM) | RF (Cas9) | EC50 (µM) | RF (SUPKO) | EC50 (µM) | RF (SUPKO) | ||||
| Tubercidin | OH | NH2 | 0.44 ± 0.06 | >100 | >230 | >100 | - | >100 | - | |
| Cordycepin | NH2 | 91.6 ± 12.9 | >100 | >1.09 | >100 | - | >100 | - | ||
| FH7429_u | NH2 | Br | 27.3 ± 7.0 | >200 | >3.6 | 27.0 ± 5.8 | >7.4 | 42.9 ± 12.0 | >2.33 | |
| FH7429_d | NH2 | 15.1 ± 1.7 | >100 | >6.63 | 65.3 ± 7.6 | >1.53 | >100 | - | ||
| FH6367 | OH | NH2 | CF3 | 26.1 ± 6.4 | >100 | >3.83 | 3.79 ± 0.34 | >26.4 | 7.4 ± 1.4 | >13.5 |
| FH3169 | OH | NH2 | Cl | 0.23 ± 0.005 | 15.4 ± 2.7 | 67.7 | 9.41 ± 0.56 | 1.64 | 15.9 ± 2.5 | 0.97 |
| TH1008 | OH | NH2 | Pyridin-2-yl | 11.7 ± 0.5 | >100 | >8.5 | >100 | - | >100 | - |
| TH1003 | OH | NH2 | Br | 2.43 ± 0.14 | >100 | >41.2 | 71.1 ± 5.0 | >1.4 | >100 | - |
| FH3167 | OH | NH2 | F | 0.096 ± 0.009 | 63.4 ± 5.5 | 660 | 7.5 ± 0.9 | 8.48 | 57.2 ± 6.8 | 1.1 |
| CL4510 | OH | OCH3 | 0.39 ± 0.05 | 2.28 ± 0.21 | 5.84 | 2.2 ± 0.03 | 1.03 | 2.05 ± 0.04 | 1.1 | |
| FH8517 | NH2 | F | 3.09 ± 0.04 | 9.96 ± 2.04 | 3.22 | 6.1 ± 0.7 | 1.64 | 9.42 ± 1.41 | 1.06 | |
| FH8505 | NH2 | ethynyl | 92.7 ± 4.3 | >100 | >1.08 | 89.9 ± 12.5 | >1.1 | 80.0 ± 7.7 | >1.25 | |
| FH8496 | NH2 | I | 51.8 ± 10.3 | 52.6 ± 0.0 | 1.01 | 23.9 ± 5.6 | >2.2 | 40.0 ± 9.2 | >1.2 | |
| FH9531 | OH | O-iPr | Cl | >100 | >100 | - | >100 | - | >100 | - |
| FH10659 | NH2 | -vinyl | >100 | >100 | - | >100 | - | >100 | - | |
| Pentamidine | 1.43 ± 0.05 | 1.83 ± 0.29 | 1.28 | 1.73 ± 0.20 | 1.1 | 2.31 ± 0.18 | 0.77 | |||
EC50 values were obtained using the resazurin-based assay in 96-well plates, with doubling dilutions over 1 or 2 rows (11 or 23 dilutions) as necessary to obtain a full EC50. Data listed are the average of 3 or more experiments and SEM. When inhibition was less than 50% at 100 µM the value is listed as >100. RF is the Resistance Factor relative to the cell line given in brackets, e.g., RF(cas9) = EC50(SUPKO)/EC50(Cas9).
For the 3′-deoxytubercidins, a similar pattern was observed with respect to the 7-position substitutions. The unsubstituted analog (FH7429_d) displayed only a marginal (TcoAT1) or no measurable sensitization (TvxNT3) upon expression of the transporters. In contrast, the Trypanosoma transporters sensitized 7-iodo analog (FH8496) beyond Cas9, the 7-bromo (FH7429_u) and 7-ethyn (FH8505) displayed the same EC50 as Cas9 but the 7-fluoro (FH8517) had higher EC50 values than Cas9. These results show how the side-by-side comparison of nucleoside analog activity against cell lines that are identical, except for the expression of specific nucleoside transporters, can quickly lead to insights into the SAR of what these carriers may take up.
In order to strengthen this conclusion, we next explored whether the same pattern holds for direct measurements of transporter inhibition constants Ki and interaction energy ΔG0. In T. congolense IL3000, the tubercidin analogs competed with adenosine for uptake through the transporter, hypothesized to be TcoAT1, in a dose-dependent manner. It was observed that, of the 3′-deoxytubercidins, the 7-F and unsubstituted analogs displayed a lower affinity for the T. congolense adenosine transporter than the 7-I, 7-Cl and 7-ethene analogs (Table 6). However, the values in terms of Gibbs free energy of interaction were within ~4 kJ/mol of each other and it must be remembered that the Ki value is an inhibition constant and does not necessarily inform on uptake rates: a compound may display high binding affinity as an inhibitor without being transported at all. However, compounds that showed the highest activity against the whole parasites, such as FH8470 (7-chloro-7-deaza-3′-deoxyadenosine), also typically exhibited higher affinity to the transporter compared to tubercidin (Table 6). The Ki values for TcoAT1 expressed in SUPKO were similar and followed the same ranking as the adenosine uptake in IL3000 bloodstream forms, further supporting the hypothesis that TcoAT1 is the main, and apparently only, adenosine transporter in T. congolense. A further set of analogs was then tested on TcoAT1 expressed in SUPKO to further build out the SAR. TH1012 (7-phenyltubercidin), a powerful lead compound against Trichomonas vaginalis [68], displayed low affinity to TcoAT1, with a Ki value of 146 ± 58 µM. Interestingly, 6-methoxy-7-deazapurine riboside (CL4510) displayed strong activity against L. mexicana Cas9 in that assay, which was largely retained (EC50 = 2.3 µM) in SUPKO and not changed by the expression of TcoAT1 or TvxNT3. This raises the intriguing possibility that this analog, and possibly others, may be taken up by kinetoplastid cells independent from the known nucleoside transporters.
Table 6.
Km or Ki, ΔG0 and δ(ΔG0) for toxic nucleosides on the transport of [3H]-adenosine by TcoAT1 expressed in L. mexicana SUPKO and by T. congolense IL3000 bloodstream forms.
| TcoAT1 in L. mexicana SUPKO | T. congolense IL300 | |||||
|---|---|---|---|---|---|---|
| Km or Ki (μM) | ΔG0 (kJ/mol) |
n | Km or Ki
(μM) |
ΔG0 (kJ/mol) |
n | |
| Adenosine | 0.42 ± 0.03 | −36.4 | 3 | 0.48 ± 0.03 | −36.0 | 3 |
| Tubercidin | 693 ± 25 | −17.8 | 3 | 403 ± 120 | −19.4 | 3 |
| Cordycepin | 4.6 ± 0.6 | −30.5 | 3 | 12.0 ± 2.0 | −28.1 | 3 |
| FH7429_u | 259 ± 11 | −20.5 | 3 | |||
| FH7429_d | 810 ± 60 | −18.0 | 3 | 319 ± 93 | −19.9 | 3 |
| FH8496 | 135 ± 11 | −20.6 | 3 | 46.2 ± 1.7 | −24.7 | 3 |
| FH8470 | 60.6 ± 10.7 | −24.1 | 3 | 17.5 ± 3.4 | −27.1 | 4 |
| FH8517 | 229 ± 15 | −20.8 | 3 | 98.1 ± 2.3 | −22.9 | 3 |
| FH10659 | 59.3 ± 4.3 | −17.7 | 4 | 28.5 ± 8.1 | −25.9 | 6 |
| TH1012 | 146 ± 58 | −21.9 | 3 | |||
| CL4510 | 226 ± 26 | −20.8 | 3 | |||
2.4.2. Affinity of Nucleoside Drugs to T. vivax Nucleoside Transporters
Similar to the P1-type transporters in T. brucei and T. congolense, TvxNT3 showed a preference for 7-bromo-3′-deoxy-tubercidin (FH 7429_u) over the 7-unsubstituted analog (FH 7429_d) although the affinity for both was quite low (Table 7). A difference with TcoAT1, however, was that the replacement of 6-amine with OMe (CL4510) lowered the Ki for tubercidin by an order of magnitude, consistent with our conclusion that position 6 contributes positively to the interaction with TvxNT3 (Figure 6) but not TcoAT1 (Figure 4).
Table 7.
Ki for toxic nucleosides on the transport of [3H]-adenosine by TvxNT3 expressed in SUPKO.
| Km or Ki (µM) | ΔG0 (kJ/mol) | n | |
|---|---|---|---|
| Adenosine | 1.41 ± 0.35 | −33.4 | 3 |
| Tubercidin | 287 ± 55 | −20.2 | 3 |
| Cordycepin | 8.57 ± 1.45 | −28.9 | 3 |
| FH 7429_u | 169 ± 4 | −21.5 | 3 |
| FH 7429_d | 388 ± 13 | −19.5 | 3 |
| CL4510 | 16.1 ± 2.8 | −27.4 | 3 |
| CL5565 | 32.0 ± 9.2 | −25.7 | 3 |
| FH15963 | 225 ± 42 | −20.8 | 3 |
| FH15967 | 109 ± 30 | −22.6 | 3 |
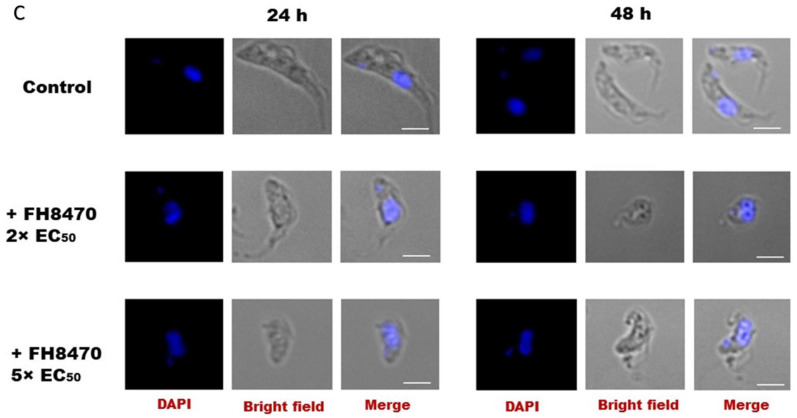
2.4.3. Antitrypanosomal Activity of Nucleoside Analogs In Vitro
A series of nucleoside analogs was screened for activity against BSF T. congolense IL3000 and the diminazene-resistant T. congolense strain 6C3 to determine the potential for cross-resistance with diminazene aceturate [60], T. b. brucei clone B48—all expressing only P1-type adenosine transporters [76]—in addition to T. evansi and T. equiperdum. EC50 values for these strains and species are displayed in Table 8, alongside EC50 values for T. vivax obtained from Mabille et al. [69]. Clearly, the 7-halogenated-3′-deoxytubercidins had highly potent activity against all the AAT trypanosomes: Br > I ~ Cl > F. It was also observed that 3′-deoxytubercidin was a more potent agent against T. b. brucei B48 and T. congolense than tubercidin (17.2-fold and 150-fold, respectively).
Table 8.
Effect of tubercidin analogs with substitutions on C7 on Trypanosoma species and strains in vitro.
| T. congolense IL3000 | T. congolense 6C3 | T. vivax ** | T.b.b. B48 | T. evansi | T. equiperdum | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Compound | C7 | 2′-OH | 3′-OH | 6-Position | EC50 (µM) | EC50 (µM) | RF † | EC50 (µM) | EC50 (µM) | EC50 (µM) | EC50 (µM) |
| Tubercidin | None | + | + | NH2 | 3.16 ± 0.50 | 1.83 ± 0.39 | 0.58 | 4.30 ± 1.30 | |||
| Cordycepin | None | + | − | NH2 | 2.46 ± 0.42 | 2.16 ± 0.44 | 0.88 | 0.12 ± 0.02 | |||
| FH7429_d * | None | + | − | NH2 | 0.021 ± 0.001 * | 0.019 ± 0.002 * | 0.91 | 3.48 ± 0.09 | 0.25 ± 0.02 | 0.017 ± 0.002 | 0.0026 ± 0.0006 |
| FH10677 | None | − | + | NH2 | 43.3 ± 14.5 | 10.9 ± 2.3 | 0.25 | >64.0 | 38.0 ± 2.3 | >100 | 17.4 ± 2.3 |
| FH7429_u | Br | + | − | NH2 | 0.00069 ± 0.00007 | 0.00049 ± 0.00009 | 0.71 | 0.018 ± 0.003 | 0.0048 ± 0.0005 | 0.00090 ± 0.00022 | 0.00051 ± 0.00007 |
| FH8496 | I | + | − | NH2 | 0.0054 ± 0.0010 | 0.0030 ± 0.0002 | 0.56 | 0.056 ± 0.001 | 0.024 ± 0.002 | 0.0037 ± 0.0012 | 0.0015 ± 0.0005 |
| FH8470 * | Cl | + | − | NH2 | 0.0012 ± 0.0002 | 0.00066 ± 0.00003 | 0.53 a | 0.096 ± 0.082 | 0.0068 ± 0.0009 | 0.0018 ± 0.0002 | 0.00057 ± 0.00008 |
| FH8517 | F | + | − | NH2 | 0.0052 ± 0.0003 | 0.0031 ± 0.0003 | 0.60 | 0.50 ± 0.01 | 0.013 ± 0.002 | 0.0040 ± 0.0006 | 0.00052 ± 0.00011 |
| FH10679 | Br | − | + | NH2 | 0.51 ± 0.09 | 0.31 ± 0.07 | 0.60 | 4.30 ± 0.90 | 1.04 ± 0.19 | 1.74 ± 0.53 | 0.067 ± 0.013 |
| TH1003 | Br | + | + | NH2 | 0.79 ± 0.14 | 0.52 ± 0.031 | 0.66 | 0.74 ± 0.04 | 1.40 ± 0.09 | 0.48 ± 0.06 | 0.085 ± 0.026 |
| FH3169 | Cl | + | + | NH2 | 0.86 ± 0.12 | 0.75 ± 0.14 | 0.87 | 0.053 ± 0.007 | 1.84 ± 0.33 | 0.62 ± 0.06 | 0.12 ± 0.018 |
| FH3167 | F | + | + | NH2 | 0.45 ± 0.62 | 0.48 ± 0.10 | 1.06 | 0.038 ± 0.006 | 0.16 ± 0.03 | 0.18 ± 0.023 | 0.032 ± 0.007 |
| FH6367 | CF3 | + | + | NH2 | 1.80 ± 0.44 | 0.89 ± 0.17 | 0.50 | 0.82 ± 0.09 | 0.90 ± 0.13 | 0.68 ± 0.11 | 0.19 ± 0.03 |
| FH9531 | Cl | + | + | O-iPr | 4.04 ± 0.36 * | 3.23 ± 0.36 * | 0.80 | 0.12 ± 0.01 | |||
| FH8505 | ethynyl | + | − | NH2 | 0.017 ± 0.002 | 0.0080 ± 0.002 | 0.46 a | 0.16 ± 0.01 | 0.031 ± 0.004 | 0.0078 ± 0.0020 | 0.0026 ± 0.0008 |
| FH10659 | vinyl | + | − | NH2 | 0.056 ± 0.004 | 0.040 ± 0.003 | 0.70 | 1.57 ± 0.43 | 0.038 ± 0.0015 | 0.011 ± 0.001 | |
| TH1008 * | Pyridin-2-yl | + | + | NH2 | 0.17 ± 0.05 | 0.056 ± 0.013 | 0.33 | 12.9 ± 4.4 | 0.39 ± 0.03 | 0.040 ± 0.005 | 0.061 ± 0.005 |
| Diminazene | 0.23 ± 0.04 | 1.32 ± 0.43 | 5.7 a | 0.34 ± 0.13 | |||||||
| Pentamidine | 0.55 ± 0.11 | 0.44 ± 0.15 | 0.79 | 0.34 ± 0.06 | |||||||
All EC50 values were obtained by Alamar Blue (resazurin) assays and are shown as averages in nM (±SEM) of at least 3 independent determinations. EC50 values were obtained using the resazurin-based assay in 96-well plates, with doubling dilutions over 1 or 2 rows (11 or 23 dilutions) as necessary to obtain a full EC50. When inhibition was less than 50% at 100 µM the value is listed as >100. 6C3 = diminazene resistant; B48 = multidrug-resistant T. brucei strain. † RF = resistance factor, in comparison to wild-type or parental strain, being EC50 (test strain)/EC50(control strain). a p ≤ 0.05 by unpaired Student’s t-test. * EC50 obtained from Hulpia et al. [38]. ** EC50 obtained from Mabille et al. [69], added for comparison only.
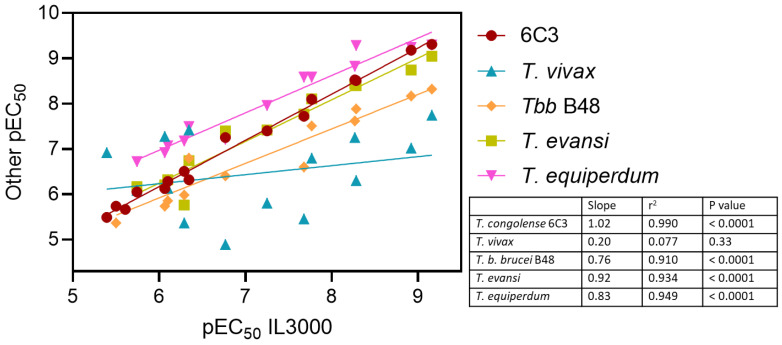
The comparison between T. congolense strains IL3000 and 6C3 shows that most compounds displayed high activity with no cross-resistance to diminazene (Table 8). Indeed, a correlation plot of pEC50 values for these strains yielded an r2 of 0.99 and a slope of 1.020 (significantly non-zero, p < 0.0001, F-test), i.e., a near perfect agreement between the datasets (Figure 9). Although we have previously shown that tubercidin is dependent on the P2 transporter for activity against T. b. brucei, and therefore cross-resistant with pentamidine [46,48], the 7-halotubercidins and 7-halo-3′-deoxytubercidins are not [38].
Figure 9.
Correlation between the −10log(EC50) (pEC50) of adenosine antimetabolites against T. congolense IL3000 with the pEC50 for other Trypanosoma cell lines or species. Lines were obtained by linear regression and slopes, correlation coefficients and p value for slope being non-zero were calculated by GraphPad Prism v8.
A similar SAR pattern was also observed for T. b. brucei B48, T. evansi and T. equiperdum, likewise yielding strong correlations with the IL3000 pEC50s (all r2 > 0.90; Figure 9). In contrast, using the dataset of Table 8, there was a poor correlation with the pEC50s of T. vivax (r2 = 0.077; slope 0.199 ± 0.198, not significantly different from zero, p = 0.34)—this despite the adenosine transporters of T. vivax and T. congolense being quite similar (Section 2.2). A closer look reveals that 3′-deoxytubercidin analogs with larger N7 substitutions (FH8505, FH10659, TH1008), or none (FH7429_d) performed particularly poorly against T. vivax (10–165-fold compared to T. congolense). The halogenated 3′-deoxytubercidins did display mid-nanomolar EC50s against T. vivax, but the values were still 10–96-fold higher than for T. congolense and similar trends were in evidence relative to T. b. brucei, T. evansi and T. equiperdum and it appears that 3′-deoxytubercidins are generally less active against T. vivax than against other African trypanosome species. Indeed, whereas the 7-fluoro and 7-chloro-3′-deoxytubercidin were much more active than the equivalent tubercidin with intact ribose against all AAT trypanosome species, the reverse was the case for T. vivax. However, the excellent activity of 7-halo-3′-deoxytubercidins against T. evansi and T. equiperdum (Table 8) makes them highly promising leads for the treatment of non-tsetse transmitted animal trypanosomiasis, specifically surra and dourine.
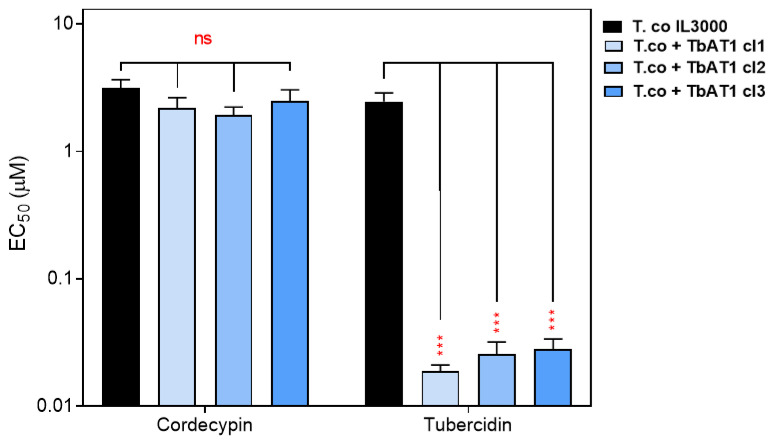
The P2/TbAT1 transporter mediates the uptake of multiple trypanocides, but this transporter is lost in many drug-resistant strains [20,43,50,51,77]. Thus, nucleoside analogs that do not utilize this transporter have higher potential for development as new drugs that replace the ones for which resistance has already developed. This prompted us to determine whether P2/AT1 is involved in the uptake of the 6-position-modified 7-deazapurineriboside analogs, using a T. congolense IL3000-based cell line expressing TbAT1 [18]. Standard resazurin-based drug sensitivity assays showed that as expected, TbAT1 expression caused a highly significant sensitization to tubercidin (p < 0.0001) in three independent clones (Figure 10), as tubercidin is a good substrate of TbAT1/P2 [46] but at best a poor substrate for the T. congolense adenosine transporter, TcoAT1 (Table 6) and as a result tubercidin is a relatively poor agent against T. congolense (Table 8).
Figure 10.
Effect of expression of TbAT1 on the sensitivity of T. congolense to tubercidin. Sensitivity is represented as average EC50 (mean ± standard error of mean) of three independent determinations. *** p < 0.001; ns = not significant by unpaired Student’s t-test.
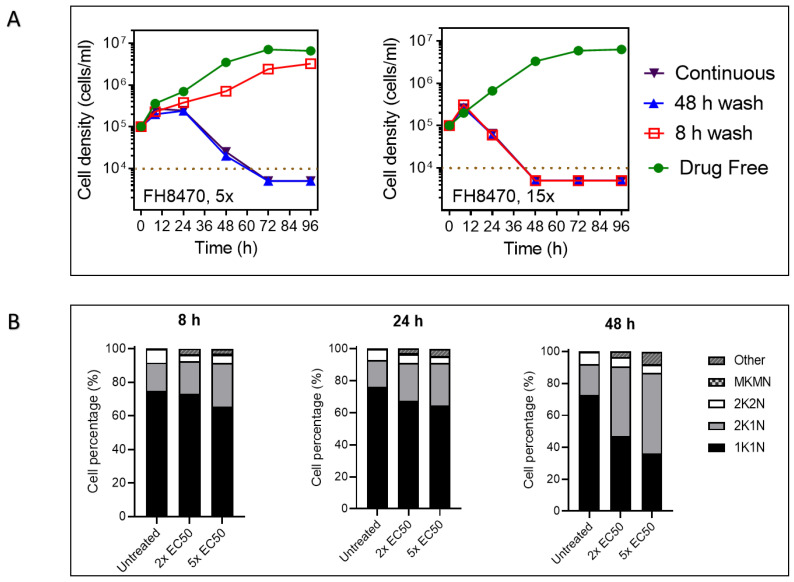
2.4.4. The Effect of Tubercidin Analogs on Growth, Cell Cycle and Morphology of T. congolense
The effects of short and long exposure to a representative tubercidin analog on the growth of BSF T. congolense were investigated as described previously [38]. A short exposure (8 h) of T. congolense to a concentration of 15 × EC50 FH8470 resulted in the death of the cells within 48 h, whether the drug was continuously present or washed out. On the other hand, exposure for 48 h or continuously to 5 × EC50 FH8470 killed the parasites within 72 h (Figure 11A, right panel). Clearly, the compound, at that concentration, induces irreversible damage to the cells which causes them to die later. No live trypanosomes were recovered at the 96 h point (i.e., 88 h after the removal of the compound) and it thus appears that these compounds are trypanocidal. Exposure to a lower concentration of 5 × EC50 showed a similar pattern but required a longer exposure time before the effect became irreversible (Figure 11A, left panel).
Figure 11.
The effect of tubercidin analog FH8470 on growth, cell cycle and morphology of T. congolense. (A) Manual cell count of cultures grown in the presence or absence of 5 × or 15 × EC50 of tubercidin analog FH8470. For short exposure, cultures were washed through centrifugation and resuspended in fresh medium. The dotted brown line indicates the detection limit, being 104 cells/mL. For the purpose of this graphical representation, where no cells were observed in the counting chamber, the value of 5 × 103 or 4 × 103 was entered. (B) Effect of nucleoside analog FH8470 on the cell cycle progression in T. congolense. Cells were seeded at 105 cells/mL in growth medium with or without test drug at the desired concentration. At each predetermined period, approximately 106 cells were harvested, transferred to a glass slide and fixed. The slide was then DAPI-treated and covered with a coverslip, and images were acquired using Olympus IX71 DeltaVision Core System fluorescent microscope (Applied Precision, GE, Rača, Slovakia). The configurations of nucleus and kinetoplast for at least 300 cells were observed in each group; 1K1N = one kinetoplast and one nucleus; 2K1N = two kinetoplasts and two nuclei; 2K2N = two kinetoplasts and two nuclei; MKMN = multiple kinetoplasts and/or nuclei; other = other aberrations such as no nucleus or no kinetoplast. Graphs show percentage mean ± SEM of three independent determinations. (C) Images of T. congolense cells exposed to nucleoside analog FH8470 for 24 h or 48 h. Test drug at desired concentration was added to BSF T. congolense culture followed by incubation for 24 h or 48 h. Cells were harvested at predetermined point, applied to a glass slide, fixed and treated with DAPI before the slide was covered with a coverslip. Images were acquired using a Delta Vision Core fluorescent microscope and analyzed using ImageJ software. Treated culture showed higher percentage of cells with conjoined nuclei and two kinetoplasts, often accompanied by mottled cell surface and loss of slender BSF shape. White bar represents 3 µM.
The nucleus and kinetoplast configuration of a trypanosomatid cell reflect the cell cycle phase at that point in time [78,79]. Therefore, the effect of a test drug on cell cycle progression can be investigated by comparing the DNA content/configuration of drug-exposed Trypanosoma cell population with that of an untreated control [80,81]. In an untreated T. congolense IL3000 BSF culture, we observed that 70–80% of the cells present with a single kinetoplast and nucleus throughout the initial lag and logarithmic growth phases, which indicates a preparatory or early G1 phase of cell cycle (Figure 11B). A further 15–20% of the cells bear two kinetoplasts and a single nucleus (2K1N) while 5–8% show a two kinetoplasts and two nuclei configuration (2K2N) representing the G1/G2 and M phase of the cell cycle, respectively; this is a normal distribution for log phase trypanosomes [82]. The addition of 2× or 5× EC50 of FH8470 to a T. congolense culture resulted in a progressive decrease in the percentage of cells at 1K1N, and an increase in the percentage of cells at 2K1N DNA configuration (Figure 11B). As early as at the 8 h mark, the number of cells with 2N2K configuration was reduced by 40–50% of untreated control and this remained depressed throughout. These data strongly suggest that FH8470 arrests cell cycle progression, most likely through the inhibition of nuclear DNA synthesis and/or mitosis.
Several cells at 24 h and 48 h post-treatment with either 2× or 5× EC50 of FH8470 presented with two kinetoplasts and conjoined nuclei, indicating failure to complete nuclear division. Such nuclei have typically lost the usual round shape and appeared larger than the nuclei in cells bearing a single kinetoplast. In addition, a large percentage of the cells exposed to FH8470 have lost the slender BSF shape and had a mottled cellular membrane arising from either direct damage, or perhaps from pressure exerted by the larger conjoined nucleus (Figure 11C).
2.5. Toxicity of Tubercidin Analogs on Mammalian Cells
The use of the resazurin assay to investigate the toxicity of test compounds on mammalian cells and to quantify their selectivity for parasite cells has been reported previously [83]. Most of the assayed tubercidin analogs exhibited low toxicity against human embryonic kidney (HEK) cells (Table 9), which translated into high selectivity to the parasites. We hypothesize that this is likely because their entry into the cell, through high affinity adenosine transporters with broad specificity, is lacking in mammalian cells, which feature carriers with much lower affinity [26,37]. Alternatively, the enzymes of purine metabolism in mammalian cells may not activate these nucleoside prodrugs, as known for allopurinol and formycin B, which derive selective toxicity at not being processed to the AMP analog in mammalian cells [84]. Notably, the 3′-deoxytubercidin analogs showed the highest selectivity for parasites, especially FH7429_u, FH7429_d, FH8470 and FH8496 (Table 9). In contrast, FH6367, featuring an intact ribose, showed higher toxicity to HEK cells than to T. evansi and T. congolense.
Table 9.
Toxicity of tubercidin analogs with substitutions on C7 against human embryonic kidney (HEK) cells.
| HEK EC50 (µM) | SI † T. evansi | SI † T. equiperdum | SI † T. congolense | |
|---|---|---|---|---|
| FH7429_u | 2.18 ± 0.41 | 2430 | 4271 | 3158 |
| FH7429_d | >200 | >11,800 | >76,000 | 9700 |
| FH6367 | 0.49 ± 0.01 | 0.7 | 2.6 | 0.3 |
| FH3169 | 4.55 ± 0.19 | 7.4 | 37 | 5.3 |
| TH1008 | 18.5 ± 1.5 | 466 | 303 | 110 |
| TH1003 | 2.37 ± 0.12 | 4.9 | 28 | 3.0 |
| FH8470 | 12.0 ± 0.32 | 6830 | 21,100 | 9800 |
| FH3167 | 0.49 ± 0.05 | 2.7 | 15 | 1.1 |
| FH8517 | 1.71 ± 0.11 | 431 | 3310 | 330 |
| FH8505 | 1.17 ± 0.06 | 151 | 446 | 68 |
| FH8496 | 4.91 ± 0.03 | 1340 | 3260 | 902 |
| FH10679 | >200 | >115 | >3000 | >390 |
| FH10677 | >200 | >12 | >4.6 |
† SI = selectivity index of parasite species in comparison to HEK cells, being EC50 (HEK cells)/EC50 (parasite species). The EC50s were determined using resazurin-based assays in 96 well plates, using doubling dilutions from 100 µM across one row (11-dilutions). Data shown are the average and SEM of at least 3 independent determinations.
3. Discussion
The lack of capacity for de novo synthesis of purines by protozoa [25] has resulted in the development of a class of highly specialized and highly efficient membrane transporters for the internalization of this essential nutrient [26]. However, the three main AAT-causing pathogens in Africa, T. b. brucei, T. congolense and T. vivax have not received the same level of attention from researchers over the past decades. The availability and ease with which T. b. brucei could be cultured and manipulated have resulted in an over-reliance on this one species in trypanosomatid research. In contrast, the study of T. congolense and T. vivax has been limited by the unavailability of cellular and genetic modification tools for a long time, and even more by the challenges of their in vitro culture which even now is limited to a few strains of T. congolense, while T. vivax can only be maintained briefly ex vivo, but still not cultured. However, the use of the brucei model in animal trypanosomiasis research is limited by genetic, pharmacological and metabolic differences between T. brucei and T. congolense (and presumably T. vivax), which are becoming ever more apparent [60,85]. For T. congolense, although in vitro axenic culture has been available for some time [86], reliable and functional genetic modification tools have only recently been developed [87]. Unfortunately, long-term axenic culture and culture techniques for T. vivax are not yet established and only a few strains reliably achieve infection in mice [88,89,90].
The T. brucei nucleoside transporters have been thoroughly studied for three decades. In this species, two types of nucleoside transporters, P1 and P2, have been identified, and their substrate specificity well characterized [34,39,41,46,91]. P1 is a broad-specificity high-affinity purine transporter that interacts with nucleoside substrates through the N3, N7, 3′-OH, and 5′-OH functional groups that are common to all the natural purine nucleosides [40,44]. On the other hand, the P2 transporter is exclusively an aminopurine carrier that interacts through N1, C6-NH2, N9 and π-π stacking of purine ring. The high affinity to the N(1)=C(6)-NH2 motif has allowed it to mediate the uptake of drugs such as diamidines, isometamidium and melaminophenyl arsenicals [92,93]). While P1-type transporters are also expressed in other trypanosomatids, the P2 transporter has so far only been found in the brucei group trypanosomes. Specifically, Leishmania spp. and T. cruzi express two P1-type transporters, each with their different kinetic characteristics [27,61].
While the P2 transporter has therefore been very successfully leveraged to deliver chemotherapy, the development of resistance to these old drugs has resulted in the circulation of populations without a functional P2 transporter [7]. The discovery that the P1 rather than P2 is expressed in other pathogenic trypanosomatids [27,52,61] has opened up the possibility for a more effective targeting of the multi-species disease AAT, particularly since no equivalent of P2 is expressed in T. congolense or T. vivax [53].
Purine metabolism in T. congolense and T. vivax is not yet fully understood. Earlier studies have pointed out that adenosine cleavage in T. congolense depends on purine nucleoside phosphorylase, whereas T. vivax and T. brucei utilize purine nucleoside hydrolase for that purpose [94]. The T. congolense BSF culture supernatants showed significant accumulation of guanine and xanthine, likely as the by-products of hydrolysis of guanosine and xanthosine by the parasite hydrolases/nucleosidases [85].
TcoAT1 is closest to T. brucei NT10 out of the eight gene variants that code for P1-type transporters in the T. brucei genome [52], suggesting it should be a broad specificity purine nucleoside transporter. Conforming to these expectations, we have found TcoAT1 to be a high affinity transporter for adenosine (Km = 0.42 µM), inosine (Ki = 0.55 µM) and guanosine (Ki = 0.8 µM). In addition, this transporter excludes purine nucleobases and pyrimidines. These findings are consistent with our earlier findings [52] but provide far more detail than was possible in the T. brucei B48 expression system and shows the utility of the L. mexicana SUPKO cell line as recently shown with the characterization of the T. vaginalis ENT3 nucleoside transporter [29]. Considering the essential need of adenosine, guanosine and inosine, it is not surprising that the single transporter expressed in this species mediates the uptake of all three. The earliest studies on nucleoside transport in T. congolense showed that excess unlabeled adenosine, inosine, and guanosine could reciprocally and completely inhibit each other’s uptake [95]. A more recent study involving the heterologous expression of TcoAT1 in the T. brucei TbAT1-null clone B48 has shown an increase in the uptake of adenosine and inosine [52]. The TcoAT1 characteristics observed in this study are highly similar to NT10 expressed by the short-stumpy BSF and procyclic forms of T. brucei, with Km values of 0.41 µM for adenosine and 0.53 µM for inosine (Table 10) [40] but also quite similar to the BSF P1-type transport [44].
Table 10.
Kinetic parameters of nucleoside transporters of T. brucei brucei, T. congolense and T. vivax.
| Transporter | Substrate | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| ADE | ADO | GUA | GUO | HYP | INO | CTD | TMD | URD | |
| TbP2/AT1 | 0.38 a; 0.30 c | 0.59 a; 0.92 c | NE 3,c | >500 c | NE 4,c | NE 3,c | NE 2,c | NE 2,c | |
| TbP1/NT2 | NE 3,c | 0.15 a; 0.26 b; 0.38 c | 1.8 c | NE 1,c | 0.44 c | NE 3,c | 44 c | 830 c | |
| TbNT5 d | 2 | 2.2 | 49.4 | ||||||
| TbNT6 d | 1.4 | 4.3 | |||||||
| TbNT7 d | 0.3 | 1.8 | |||||||
| TbNT9 e | 148 | 0.068 | 6.2 | 320 | 2.75 | 510 | 235 | ||
| TbNT10 e | 0.41 | 0.53 | |||||||
| TbNT11 f | 2.7; 8 | 266 | 651 | 141 | |||||
| TbNT8/H4 g | 2.6 | 860 | 2.6 | 4.7 | 0.55 | 20 | 95 | ||
| TcoAT1 | 786 | 0.42 | 0.80 | 61.2 | 0.55 | 1630 | 49.6 | 147 | |
| TvxNT3 | 2.43 | 1.41 | 1.37 | 1.75 | 0.086 | >100 | 603 | 720 | |
Values in bold represent Km values; all others are Ki values. ADE, adenine; ADO, adenosine; GUA, guanine; GUO, guanosine; HYP, hypoxanthine; INO, inosine; CTD, cytidine; TMD, thymidine; URD, uridine; NE, no effect at 1 1 mM, 2 500 μM, 3 250 μM, 4 100 μM. a Carter and Fairlamb [41]; b De Koning et al. [34]; c De Koning and Jarvis [44]; d Sanchez et al. [39]; e Al-Salabi et al. [40]); f Ortiz et al. [96]; g Burchmore et al. [70]. Data for T. congolense (Tco) and T. vivax (Tvx) transporters were from this study. NE, no effect at the stated concentration.
While TcoAT1 and TvxNT3 have large differences in their affinity to nucleobases, they both showed high affinity to adenosine, inosine and guanosine in similar fashion to P1 nucleoside transporters of T. brucei [40]. These three transporters similarly interact with nucleoside substrates, with the main contact points being N7, N3 and 2′-OH. T. brucei P1 additionally interacts with the 5′-OH, which does not seem to be involved in T. congolense and T. vivax adenosine transport.
A further difference is a contribution by the 6-keto group of inosine to binding by TvxNT3 only. The permissibility for nucleobases for TvxNT3 is the result of only a minor contribution from the 2′-OH (−4.5 kJ/mol) relative to the TcoAT1 (~12 kJ/mol) and TbbP1 interactions of 15 and 14 kJ/mol for 2′-OH and 5′-OH, respectively [44]. In addition, purine nucleobases may be able to assume an energetically favorable orientation in the TvxNT3 binding pocket that is different from the nucleoside binding. The high affinity of TvxNT3 for purines is maintained by the extra interaction at position 6 and the two strong hydrogen bonds at N3 and N7. The similarities in binding modes explain that all three carriers function as broad specificity purine-selective nucleoside transporters, while the differences explain some of the disparities regarding specific nucleoside analogs.
The presence of transporters with highly similar characteristics regarding nucleoside binding and permissibility in T. brucei, T. congolense and T. vivax presents an interesting avenue for drug development. The disparity in innate sensitivity to diamidine and arsenical between T. brucei and T. congolense has been shown to result from a lack of AT1 and AQP2 transporters in T. congolense [18]. We have confirmed that the expression of P1 transporters of T. congolense and T. vivax does not affect the sensitivity of the currently used drugs diminazene, pentamidine, melarsomine and suramin. This suggests that purine nucleoside analogs can be designed to target the P1 transporters of veterinary trypanosomes with minimal risk of cross-resistance to the current trypanocides. Therefore, we tested the chemotherapeutic potential of the TcoAT1 and TvxNT3 using toxic nucleoside analogs with reported affinity to T. brucei P1. It was found that the expression of either TcoAT1 or TvxNT3 in the resistant L. mexicana SUPKO sensitized these NT-null cells to most of the tubercidin analogs—clear proof of internalization through the expressed heterologous carriers.
The uptake of toxic nucleosides, particularly tubercidin and cordycepin, has to date been thought to be mediated largely by the P2 transporter in T. brucei: the TbAT1-KO strain showed 77-fold and 17-fold resistance to tubercidin and cordycepin, respectively [46,47]. In a recent study, a tubercidin resistance factor of 28.7 was reported in TbAT1-KO compared to the wild type (0.15 ± 0.03 vs. 4.3 ± 1.3 μM EC50) [38]. In this study, the EC50 of tubercidin in T. congolense, was determined as 3.16 ± 0.50 μM, similar to T. brucei lacking TbAT1. T. b. brucei B48 exhibits similar sensitivity to tubercidin as T. congolense, as both parasites express only a P1-type transporter. Several modifications were carried out on the purine ring and/or the ribose sugar in order to generate tubercidin analogs with improved targeting of the trypanosomal P1 transporter. We have recently reported the structure activity relationship (SAR) of the tubercidin analogs in T. brucei [66].
Given the similarity in activity of tubercidin against T. brucei B48 or TbAT1-KO and T. congolense, we expected that the modification of tubercidin will also yield improved activity against T. congolense and T. vivax. We investigated the hypothesis through a series of comparative drug sensitivity tests and uptake assays in whole parasites and isolated transporters expressed in surrogates. For this purpose, cell lines expressing adenosine transporters of T. congolense (TcoAT1) and T. vivax (TvxNT3) in L. mexicana NT1+NT2-KO (SUPKO) were utilized. In parallel, the analogs were also tested directly on the organisms, the combination of the two screens, plus the transporter affinity studies, allowing more insightful conclusions on separating issues of transporter permeability and transporter-independent sensitivity of the parasites for the nucleosides tested.
As expected, some tubercidin analogs presented sub-micromolar activity dependent on the expression of TcoAT1 or TvxNT3, with a similar pattern of SAR to T. brucei P1 [66]. Of particular note, the incorporation of the cordycepin motif (3′-deoxyadenosine) into tubercidin (7-deazaadenosine) resulted in higher in vitro activity against T. congolense, T. evansi, T. equiperdum and T. brucei B48, although it did not result in higher affinity to TbbP1 [38], TcoAT1 and TvxNT3 transporters. The addition of a functional group to the C-7 of tubercidin yielded still higher activity, and greatly improved affinity to the P1 transporters of all the three species. In general, tubercidin analogs bearing the larger halogen groups at C-7 were more active than those containing a fluor or a small unsaturated or an aromatic substituent. Only against T. vivax did the 3′-deoxytubercidin analogs display lower activity than the equivalent ribonucleoside, but this cannot be attributed to a difference in adenosine transporter, as TvxNT3 was in fact much less dependent on interactions with the ribose and specifically 3′-OH (δ(ΔG0 4.5 kJ/mol relative to adenosine) than TcoAT1 (δ(ΔG0) 5.9 kJ/mol) or TbbP1 (δ(ΔG0) 15 kJ/mol [44]), and the expression of TvxNT3 sensitized SUPKO to 7-bromo-3′-deoxytubercidin (FH7429_u). Thus, the relative insensitivity of T. vivax to 3′-deoxytubercidins can be confidently attributed to a specific difference with other animal trypanosomes at the level of intracellular target enzymes. Regardless, it should still be noted that the 7-Cl, 7-Br and 7-I-3′-deoxytubercidins were the most potent nucleosides against T. vivax identified here, with EC50 values between 18 and 96 nM. The low-nM or sub-nM activity of these compounds against T. evansi and T. equiperdum make them exciting candidates for the treatment of surra and dourine.
Given that the 3′-deoxy modification was unfavorable for T. vivax, leading to an unequal level of activity of 3′-deoxytubercidin analogs among the three AAT-causing species, a different modification was carried out. The C-6 amino group of tubercidin was substituted with different groups while ribose remained intact, to yield C-6 alkylated tubercidin analogs. Very recently, 6-methyltubercidin analogs were reported to exert comparable activity against T. b. rhodesiense, T. cruzi and L. infantum [97,98]. This broad-spectrum antikinetoplastid activity is uncommon and affirms the potential of targeting multiple trypanosomatid species through P1-type nucleoside transporters. Thus, future efforts into discovery of pan-AAT nucleoside drugs should focus on 6-substituted tubercidin analogs. While these analogs were not as active as the 3′-deoxytubercidin analogs in T. brucei, T. congolense, T. equiperdum and T. evansi, the multispecies activity they have exhibited at ˂ 0.2 µM EC50 makes them more promising candidates to target both AAT and the non-tsetse transmitted animal trypanosomiases (NTTAT). As the areas of endemicity of veterinary trypanosomes increasingly overlap on the global map [5], there is an urgent need to develop drugs that are active against all five Trypanosoma species.
An ideal chemotherapeutic agent should be selectively toxic to the target cell while sparing the host cell. Therefore, we tested the toxicity of tubercidin analogs against human embryonic kidney (HEK) cells using the standard Alamar Blue assay. Most of the tubercidin analogs exhibited low activity against HEK cells, which translates into high selectivity indexes (SI). Specifically, the 3′-deoxytubercidin analogs demonstrated very high selectivity to parasites especially FH7429_u, FH7429_d, FH8470 and FH8496. The only exception was FH6367, with an intact ribose, which showed higher toxicity to HEK cells than to T. evansi and T. congolense. As with almost every other veterinary trypanocide [1], a nucleoside drug against AAT would be injected intramuscular rather than administered orally, which would ensure rapid distribution in the bloodstream without the complications of intestinal absorption, stability in stomach acids or the complications of the ruminant digestive system. We have previously shown that 3′-deoxy-tubercidin is curative in a T. b. brucei mouse model, even for the difficult to treat stage, where the parasite has infected the central nervous system [38]. It should be noted that this compound cured the AAT model by both oral and intraperitoneal administration [38].
Widespread resistance to the currently used trypanocides has continued to undermine the vital role chemotherapy plays in the control of animal trypanosomiases [99]. It is therefore important that new drugs neither share similar targets with the currently used trypanocides nor exhibit a potential for cross-resistance. The fact that the modified tubercidin analogs reported here mostly utilize P1-type transporters, and not the multidrug P2 transporter is a welcome development. Nevertheless, we tested the tubercidin analogs against the diminazene-resistant T. congolense strain 6C3, which displays reduced mitochondrial membrane potential [60]. There was no significant difference in the sensitivity of 6C3 and the wild type to the tubercidin analogs. Since multiple trypanocides including diminazene, isometamidium, pentamidine and nifurtimox target mitochondria [60,79,100,101], the risk of cross-resistance between the tubercidin analogs and these drugs is low.
To start exploring the mechanism of action of the tubercidin analogs, T. congolense culture was exposed to one of the analogs, and the cell growth rate, cell cycle and morphology were examined. We observed that the killing of trypanosomes by low concentrations of these compounds can be reversed or delayed by the removal of drug pressure after short exposure, but the drug action becomes rapidly irreversible at higher concentrations. Furthermore, the addition of 2 × or 5 × EC50 of FH8470 to T. congolense culture resulted in a progressive decrease in the percentage of cells bearing 1K1N, with a corresponding increase in the percentage of cells at 2K1N DNA configuration and decrease in 2K2N cells. This suggests that FH8470 prevents the cells from completing M phase, thus inhibiting nuclear division. This is corroborated by the appearance of several cells with conjoined nuclei among the cells bearing double kinetoplasts, indicating a failure to divide. Such nuclei typically have lost the usual round shape and appear larger than the nuclei in cells bearing 1K. In a previous study [79], it was reported that >10% of T. brucei cells treated with melarsoprol bear conjoined nuclei and double kinetoplasts. Further investigations revealed that the melarsoprol-mediated inhibition of nuclear division is mediated by multiple kinases [79].
In a previous study, RNAi has indicated that tubercidin inhibits multiple enzymes in the glycolytic pathway in T. brucei including hexokinase and phosphoglycerate kinase [102]. However, recently, a genome-wide RNAi in T. b. brucei identified that six RNAi inserts including those targeting the TbAT1 transporter and adenosine kinase (ADKIN; Tb927.6.2300) are involved in the action of 3′-deoxytubercidin. Subsequently, the roles of TbAT1 transporter and ADKIN were confirmed, with the targeted knockdown of both genes resulting in significant resistance to 3′-deoxytubercidin [38]. Interestingly, the selected 3′-deoxytubercidin analogs showed metabolic stability in experiments simulating phase I and phase II metabolism, which affirms their potential as therapeutic agents [66].
4. Materials and Methods
4.1. Cell lines and Culture
The bloodstream form (BSF) of wild-type and mutant parasites belonging to the Trypanozoon subgroup including T. b. brucei s427, T. evansi AnTat 3/3 and T. equiperdum BoTat1 [20] were cultured in supplemented HMI-9 medium and maintained as described [18]. BSF T. congolense IL3000 and derived mutants were cultured in TCBSF3 [86] without blood cells, as previously described [81]. Promastigotes of L. mexicana Cas9 and derived cell lines were grown as described [29] with L. mexicana Cas9 maintained in 32 μg/mL hygromycin while the mutant SUPKO+NT strains were maintained with neomycin G418 at 50 μg/mL ([64]. Human embryonic kidney (HEK) cells were cultured and maintained as reported [83].
4.2. Genetic Manipulation of L. mexicana Promastigotes
The information for the T. congolense adenosine transporter (TcoAT1) and four putative T. vivax nucleoside transporters was obtained in the TritrypDB (tritrypdb.org/tritrypdb) genome database. Primers were designed to flank each gene upstream of the 5′ end (forward) and downstream of the 3′ end (reverse) as described (primer sequences in Supplementary Table S2). Following amplification from the genomic DNA of T. congolense or T. vivax, DNA for each extracted gene was ligated into the pNUS-HcN expression vector doubly digested with NdeI using the NEBuilder kit according to the manufacturer’s instructions (New England Biolabs). Construct was transformed into competent E. coli cells, and ligation was confirmed by restriction enzyme digestion of isolated plasmid DNA followed by Sanger sequencing (Source BioScience, Nottingham, UK). Confirmed plasmids were then transfected into L. mexicana cell line in which both NT1 and NT2 were doubly knocked out (SUPKO) and derived from L. mexicana Cas9 [64] as described [29]. Clones grown in medium containing 50 μg/mL neomycin (G418) were collected for further confirmation by PCR with genomic DNA using a forward primer of the transporter gene and a reverse primer of the plasmid.
4.3. Drug Toxicity Assays
The activity of clinical trypanocides and the nucleoside analogs against various cell lines was assessed using a resazurin-based (Alamar blue) drug sensitivity assay to determine the EC50 in different cell lines, which also allowed for the investigation of cross-resistance and for toxicity to mammalian cells, exactly as described, in 96-well plates using 11 doubling dilutions of a test compound starting at 100 µM, and a drug-free control [18,103]. EC50 values were determined by plotting to an equation for a sigmoid curve with variable slope (GraphPad Prism 8). All values were the average of at least three independent determinations on different days.
For the direct assessment of test compounds on parasite growth, a manual cell count of cultures grown in the presence or absence of test drugs was carried out to determine the effect of test drugs on the multiplication rate of the parasites as described [83]. The cells were adjusted to the required density in 2 mL of the appropriate medium with or without the drug/compound of interest, in a 24-well plate, followed by incubation under standard conditions. The cells were then manually counted at intervals with a Neubauer cell chamber using a phase-contrast light microscope (Axioscope, Zeiss, Jena, Germany).
To assess the effect of the drug on the cellular morphology and configuration of nuclei and kinetoplasts, treated cells were collected after incubation period, fixed, DAPI-treated and viewed under an Olympus IX71 DeltaVision Core System microscope (Applied Precision, GE) using the SoftWoRx suite 2.0 software (Applied Precision, GE). At least 300 cells were scored per slide for the number of kinetoplasts (K) and nuclei (N) as 1N1K, 1N2K, 2N2K, MKMN (M = many) and ‘others’ (aberrant N/K distribution) [81].
4.4. Radiolabel Drug and Nucleoside Uptake Assays
Uptake assays using radiolabeled trypanocides and/or nucleosides were carried out as described previously [27,104]. Briefly, parasite cultures were harvested, washed twice in assay buffer (33 mM HEPES, 98 mM NaCl, 4.6 mM KCl, 0.5 mM CaCl2, 0.07 mM MgSO4, 5.8 mM NaH3PO4, 0.03 mM MgCl2, 23 mM NaHCO3, 14 mM D-glucose, pH 7.3), then resuspended and adjusted to a density of 1 × 108 cells/mL in assay buffer. The radiolabeled permeant in the presence or absence of different concentrations of potential inhibitors reconstituted in 100 μL assay buffer was deposited on top of 250 μL oil mix in microcentrifuge tubes; 1 × 107 parasites in 100 μL assay buffer were added to the tube and incubated for a pre-determined interval. The reaction was stopped by the addition of 1 mL of a high concentration of ice-cold unlabeled substrate in assay buffer (‘stop solution’) and centrifugation, or by immediate centrifugation at 145,000 rpm as appropriate. The microcentrifuge tubes were flash-frozen, and the bottom of each tube containing the cell pellet was cut off and transferred to a scintillation vial. Cell pellets were lysed in 2% SDS, after which scintillation fluid (Scintlogic U, Lablogic) was added, followed by overnight incubation in the dark. Scintillation was measured in a 300SL (Hidex) scintillation counter (Hidex). All the assays were conducted in triplicate and analysis was carried out using Microsoft Excel and GraphPad Prism. All kinetic parameters were obtained on at least 3 separate occasions.
The dose-dependent uptake assay allowed for the affinity of nucleoside analogs to different nucleoside transporters to be determined by measuring the extent to which the analogs compete with and inhibit the uptake of radiolabel adenosine [27]. This allowed for the determination of biochemical parameters such as Km and Vmax through the application of the Michaelis–Menten equation V0 = Vmax([substrate]/([substrate] + Km)). The 50% Inhibitory Concentration (IC50) of the purines and pyrimidines and their analogs was determined from non-linear regression to sigmoid curves with variable slope (Prism 8), and the IC50 of the inhibitor and the Km of the labeled permeant were then used to calculate the inhibition constant (Ki) of the analogs through the Cheng–Prusoff equation: Ki = IC50/(1 + (L/Km)), where L denotes the radiolabel concentration [105]. The calculated Ki was in turn used to determine the Gibbs free energy (ΔG0) of the inhibitor–transporter interaction using the equation: ΔG0 = -RTln(Ki), where R represents the gas constant and T symbolizes the absolute temperature in Kelvin [104].
5. Conclusions
We have fully characterized the substrate specificity and chemotherapeutic potential of TcoAT1. The presented data adds to the evidence that this transporter is purely a P1-type nucleoside transporter with no role in the uptake and sensitivity of trypanocides in current clinical use. In addition, we have cloned and characterized the functions of a T. vivax purine transporter (TvxNT3) for the first time, which is also a P1-type transporter, although with higher permissibility for nucleobases. We concluded that the very similar substrate recognition by the TcoAT1, TvxNT3 and T. brucei P1 transporters can be utilized in designing nucleoside drugs for the treatment of nagana. A series of P1-type 7-deaza nucleoside substrates was designed and tested; promising activity was found against the five major pathogenic trypanosomes of veterinary importance. Most of these compounds presented low toxicity to mammalian cells, no cross resistance to existing trypanocides, and by-passed the multidrug carrier P2/AT1. Preliminary observations regarding the mechanism of action of these nucleoside drugs show major impacts on mitosis.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms24043144/s1.
Author Contributions
Conceptualization, H.P.D.K. and M.A.U.; methodology, M.A.U. and M.J.N.; formal analysis, H.P.D.K. and G.C.; investigation, M.A.U., M.M.A., H.Z., R.C., K.W., K.I., J.I.A. and M.M.; resources, S.V.C.; writing—original draft preparation, M.A.U. and H.P.D.K.; writing—review and editing, G.C. and S.V.C.; supervision, R.J.S.B., G.C., S.V.C. and H.P.D.K.; funding acquisition, H.P.D.K. All authors have read and agreed to the published version of the manuscript.
Informed Consent Statement
Not applicable.
Data Availability Statement
All relevant data are included in the manuscript and Supplemental Materials.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the Biotechnology and Biological Sciences Research Council (BBSRC) of the UK through an Impact Accelerator Award (grant number BB/S506734/1), the Fonds Wetenschappelijk Onderzoek (www.fwo.be; grant numbers G033618N, G013118N) and the University of Antwerp (www.uantwerpen.be; grant number IOF-PoC 42404). M.A.U. was funded through a studentship from the Petroleum Technology Development Fund (Abuja, Nigeria). M.M.A. received a PhD studentship from the Libyan government and M.J.N. a fellowship from the Saudi Ministry for Higher Education. J.I.A. was funded by a studentship from Shaqra University, Ministry of Education, Dawadmi 11961, Saudi Arabia. LMPH is a partner of the Excellence Centre ‘Infla-Med’ (www.uantwerpen.be/infla-med). H.P.D.K. and G.C. participate in COST Action OneHealthdrugs (CA21111).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Giordani F., Morrison L.J., Rowan T.G., De Koning H.P., Barrett M.P. The animal trypanosomiases and their chemotherapy: A review. Parasitology. 2016;143:1862–1889. doi: 10.1017/S0031182016001268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Franco J.R., Cecchi G., Priotto G., Paone M., Diarra A., Grout L., Simarro P.P., Zhao W., Argaw D. Monitoring the elimination of human African trypanosomiasis at continental and country level: Update to 2018. PLoS Negl. Trop. Dis. 2020;14:e0008261. doi: 10.1371/journal.pntd.0008261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Autheman D., Crosnier C., Clare S., Goulding D.A., Brandt C., Harcourt K., Tolley C., Galaway F., Khushu M., Ong H., et al. An invariant Trypanosoma vivax vaccine antigen induces protective immunity. Nature. 2021;595:96–100. doi: 10.1038/s41586-021-03597-x. [DOI] [PubMed] [Google Scholar]
- 4.La Greca F., Magez S. Vaccination against trypanosomiasis: Can it be done or is the trypanosome truly the ultimate immune destroyer and escape artist? Hum. Vaccin. 2011;7:1225–1233. doi: 10.4161/hv.7.11.18203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magez S., Li Z., Nguyen H.T.T., Pinto Torres J.E., Van Wielendaele P., Radwanska M., Began J., Zoll S., Sterckx Y.G. The history of anti-trypanosome vaccine development shows that highly immunogenic and exposed pathogen-derived antigens are not necessarily good target candidates: Enolase and ISG75 as examples. Pathogens. 2021;10:1050. doi: 10.3390/pathogens10081050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delespaux V., De Koning H.P. Drugs and drug resistance in African trypanosomiasis. Drug Resist. Updat. 2007;10:30–50. doi: 10.1016/j.drup.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 7.De Koning H.P. The drugs of sleeping sickness: Their mechanisms of action and resistance, and a brief history. Trop. Med. Infect. Dis. 2020;5:14. doi: 10.3390/tropicalmed5010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Desquesnes M., Dargantes A., Lai D.H., Lun Z.R., Holzmuller P., Jittapalapong S. Trypanosoma evansi and surra: A review and perspectives on transmission, epidemiology and control, impact, and zoonotic aspects. Biomed. Res. Int. 2013;2013:321237. doi: 10.1155/2013/321237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Osório A.L., Madruga C.R., Desquesnes M., Soares C.O., Ribeiro L.R., Costa S.C. Trypanosoma (Duttonella) vivax: Its biology, epidemiology, pathogenesis, and introduction in the New World–a review. Mem. Inst. Oswaldo Cruz. 2008;103:1–13. doi: 10.1590/S0074-02762008000100001. [DOI] [PubMed] [Google Scholar]
- 10.Gizaw Y., Megersa M., Fayera T. Dourine: A neglected disease of equids. Trop. Anim. Health Prod. 2017;49:887–897. doi: 10.1007/s11250-017-1280-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anene B.M., Onah D.N., Nawa Y. Drug resistance in pathogenic African trypanosomiasis: What hopes for the future? Vet. Parasitol. 2001;96:83–100. doi: 10.1016/S0304-4017(00)00427-1. [DOI] [PubMed] [Google Scholar]
- 12.Wilkinson S.R., Kelley J.M. Trypanocidal drugs: Mechanisms, resistance and new targets. Expert Rev. Mol. Med. 2009;11:e31. doi: 10.1017/S1462399409001252. [DOI] [PubMed] [Google Scholar]
- 13.Morrison L.J., Vezza L., Rowan T., Hope J.C. Animal African trypanosomiasis: Time to increase focus on clinically relevant parasite and host species. Trends Parasitol. 2016;32:599–607. doi: 10.1016/j.pt.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Zweygarth E., Kaminsky R. Evaluation of an arsenical compound (RM 110, mel Cy, Cymelarsan) against susceptible and drug-resistant Trypanosoma brucei brucei and T. b. evansi. Trop. Med. Parasitol. 1990;41:208–212. [PubMed] [Google Scholar]
- 15.Kinabo L.D.B. Pharmacology of existing drugs for animal trypanosomiasis. Acta Trop. 1993;54:169–183. doi: 10.1016/0001-706X(93)90091-O. [DOI] [PubMed] [Google Scholar]
- 16.Geerts S., Holmes P.H., Eisler M.C., Diall O. African bovine trypanosomiasis: The problem of drug resistance. Trends Parasitol. 2001;17:25–28. doi: 10.1016/S1471-4922(00)01827-4. [DOI] [PubMed] [Google Scholar]
- 17.Munday J.C., Settimo L., De Koning H.P. Transport proteins determine drug sensitivity and resistance in a protozoan parasite, Trypanosoma brucei. Front. Pharmacol. 2015;6:32. doi: 10.3389/fphar.2015.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ungogo M.A., Campagnaro G.D., Alghamdi A.H., Natto M.J., De Koning H.P. Differences in transporters rather than drug targets are the principal determinants of the different innate sensitivities of Trypanosoma congolense and Trypanozoon subgenus trypanosomes to diamidines and melaminophenyl arsenicals. Int. J. Mol. Sci. 2022;23:2844. doi: 10.3390/ijms23052844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vincent I.M., Creek D., Watson D.G., Kamleh M.A., Woods D.J., Wong P.E., Burchmore R.J., Barrett M.P. A molecular mechanism for eflornithine resistance in African trypanosomes. PLoS Pathog. 2010;6:e1001204. doi: 10.1371/journal.ppat.1001204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stewart M.L., Burchmore R.J.S., Clucas C., Hertz-Fowler C., Brook K., Tait A., McLeod A., Turner C.M.R., De Koning H.P., Wong P.E., et al. Multiple genetic mechanisms lead to the loss of functional TbAT1 expression in drug resistant trypanosomes. Eukaryot. Cell. 2010;9:336–343. doi: 10.1128/EC.00200-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baker N., De Koning H.P., Mäser P., Horn D. Drug resistance in African trypanosomiasis: The melarsoprol and pentamidine story. Trends Parasitol. 2013;29:110–118. doi: 10.1016/j.pt.2012.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alghamdi A.H., Munday J.C., Campagnaro G.D., Gurvic D., Svensson F., Okpara C.E., Kumar A., Quintana J., Martin Abril M.E., Milić P., et al. Positively selected modifications in the pore of TbAQP2 allow pentamidine to enter Trypanosoma brucei. eLife. 2020;9:e56416. doi: 10.7554/eLife.56416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kell D.B. The transporter-mediated cellular uptake and efflux of pharmaceutical drugs and biotechnology products: How and why phospholipid bilayer transport Is negligible in real biomembranes. Molecules. 2021;26:5629. doi: 10.3390/molecules26185629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hassan H.F., Coombs G.H. Purine and pyrimidine metabolism in parasitic protozoa. FEMS Microbiol. Rev. 1988;4:47–83. doi: 10.1111/j.1574-6968.1988.tb02708.x-i1. [DOI] [PubMed] [Google Scholar]
- 25.De Koning H.P., Bridges D.J., Burchmore R. Purine and pyrimidine transport in protozoa: From biology to therapy. FEMS Microbiol. Rev. 2005;29:987–1020. doi: 10.1016/j.femsre.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 26.Campagnaro G.D., De Koning H.P. Purine and pyrimidine transporters of pathogenic protozoa-conduits for therapeutic agents. Med. Res. Rev. 2020;40:1679–1714. doi: 10.1002/med.21667. [DOI] [PubMed] [Google Scholar]
- 27.Campagnaro G.D., de Freitas Nascimento J., Girard R.B.M., Silber A.M., De Koning H.P. Cloning and characterisation of the Equilibrative Nucleoside Transporter family of Trypanosoma cruzi: Ultra-high affinity and selectivity to survive in the intracellular niche. Biochim. Biophys. Acta Gen. Subj. 2018;1862:2750–2763. doi: 10.1016/j.bbagen.2018.08.015. [DOI] [PubMed] [Google Scholar]
- 28.Campagnaro G.D., Elati H.A.A., Balaska S., Martin Abril M.E., Natto M.J., Hulpia F., Lee K., Sheiner L., Van Calenbergh S., De Koning H.P. A Toxoplasma gondii oxopurine transporter binds nucleobases and nucleosides using different binding modes. Int. J. Mol. Sci. 2022;23:710. doi: 10.3390/ijms23020710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aldfer M.M., AlSiari T.A., Elati H.A.A., Natto M.J., Alfayez I.A., Campagnaro G.D., Sani B., Burchmore R.J.S., Diallinas G., De Koning H.P. Nucleoside transport and nucleobase uptake null mutants in Leishmania mexicana for the routine expression and characterisation of purine and pyrimidine transporters. Int. J. Mol. Sci. 2022;23:8139. doi: 10.3390/ijms23158139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aldfer M.M., Alfayez I.A., Campagnaro G.D., Gayen N., Elmahallawy E.K., Murillo A.M., Marsiccobetre S., Van Calenbergh S., Silber A.M., De Koning H.P. TcrNT2 is a conduit for the uptake of 5-F-2’deoxyuridine and tubercidin analogues in Trypanosoma cruzi. Molecules. 2022;27:8045. doi: 10.3390/molecules27228045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campagnaro G.D., Alzahrani K.J.H., Munday J.C., De Koning H.P. Trypanosoma brucei bloodstream forms express highly specific and separate transporters for adenine and hypoxanthine; evidence for a new protozoan purine transporter family? Mol. Biochem. Parasitol. 2018;220:46–56. doi: 10.1016/j.molbiopara.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 32.De Koning H.P. Pyrimidine transporters of protozoa–A class apart? Trends Parasitol. 2007;23:190. doi: 10.1016/j.pt.2007.03.004. [DOI] [Google Scholar]
- 33.De Koning H.P., Jarvis S.M. Hypoxanthine uptake through a purine-selective nucleobase transporter in Trypanosoma brucei brucei procyclics is driven by protonmotive force. Eur. J. Biochem. 1997;247:1102–1110. doi: 10.1111/j.1432-1033.1997.01102.x. [DOI] [PubMed] [Google Scholar]
- 34.De Koning H.P., Watson C.J., Jarvis S.M. Characterisation of a nucleoside/proton symporter in procyclic Trypanosoma brucei brucei. J. Biol. Chem. 1998;273:9486–9494. doi: 10.1074/jbc.273.16.9486. [DOI] [PubMed] [Google Scholar]
- 35.Stein A., Vaseduvan G., Carter N.S., Ullman B., Landfear S.M., Kavanaugh M.P. Equilibrative nucleoside transporter family members from Leishmania donovani are electrogenic proton symporters. J. Biol. Chem. 2003;278:35127–35134. doi: 10.1074/jbc.M306188200. [DOI] [PubMed] [Google Scholar]
- 36.Young J.D., Yao S.Y., Baldwin J.M., Cass C.E., Baldwin S.A. The human concentrative and equilibrative nucleoside transporter families, SLC28 and SLC29. Mol. Aspects Med. 2013;34:529–547. doi: 10.1016/j.mam.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 37.Boswell-Casteel R.C., Hays F.A. Equilibrative nucleoside transporters–a review. Nucleosides Nucleotides Nucleic Acids. 2017;36:7–30. doi: 10.1080/15257770.2016.1210805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hulpia F., Mabille D., Campagnaro G.D., Schumann G., Maes L., Roditi I., Hofer A., De Koning H.P., Galjon G., Van Calenbergh S. Combining tubercidin and cordycepin scaffolds results in highly active candidates to treat late-stage sleeping sickness. Nat. Commun. 2019;10:5564. doi: 10.1038/s41467-019-13522-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanchez M.A., Tryon R., Green J., Boor I., Landfear S.M. Six related nucleoside/nucleobase transporters from Trypanosoma brucei exhibit distinct biochemical functions. J. Biol. Chem. 2002;277:21499–21504. doi: 10.1074/jbc.M202319200. [DOI] [PubMed] [Google Scholar]
- 40.Al-Salabi M.I., Wallace L.J.M., Lüscher A., Mäser P., Candlish D., Rodenko B., Gould M.K., Jabeen I., Ajith S.N., De Koning H.P. Molecular interactions underlying the unusually high adenosine affinity of a novel Trypanosoma brucei nucleoside transporter. Mol. Pharmacol. 2007;71:921–929. doi: 10.1124/mol.106.031559. [DOI] [PubMed] [Google Scholar]
- 41.Carter N.S., Fairlamb A.H. Arsenical-resistant trypanosomes lack an unusual adenosine transporter. Nature. 1993;361:173–176. doi: 10.1038/361173a0. [DOI] [PubMed] [Google Scholar]
- 42.Mäser P., Sütterlin C., Kralli A., Kaminsky R. A nucleoside transporter from Trypanosoma brucei involved in drug resistance. Science. 1999;285:242–244. doi: 10.1126/science.285.5425.242. [DOI] [PubMed] [Google Scholar]
- 43.Carter N.S., Barrett M.P., De Koning H.P. A drug resistance determinant from Trypanosoma brucei. Trends Microbiol. 1999;7:469–471. doi: 10.1016/S0966-842X(99)01643-1. [DOI] [PubMed] [Google Scholar]
- 44.De Koning H.P., Jarvis S.M. Adenosine transporters in bloodstream forms of T. b. brucei: Substrate recognition motifs and affinity for trypanocidal drugs. Mol. Pharmacol. 1999;56:1162–1170. doi: 10.1124/mol.56.6.1162. [DOI] [PubMed] [Google Scholar]
- 45.Munday J.C., Tagoe D.N.A., Eze A.A., Krezdorn J.A., Rojas López K.E., Alkhaldi A.A.M., McDonald F., Still J., Alzahrani K.J., Settimo L., et al. Functional analysis of drug resistance-associated mutations in the Trypanosoma brucei adenosine transporter 1 (TbAT1) and the proposal of a structural model for the protein. Mol. Microbiol. 2015;96:887–900. doi: 10.1111/mmi.12979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Geiser F., Lüscher A., De Koning H.P., Seebeck T., Mäser P. Molecular pharmacology of adenosine transport in Trypanosoma brucei: P1/P2 revisited. Mol. Pharmacol. 2005;68:589–595. doi: 10.1124/mol.104.010298. [DOI] [PubMed] [Google Scholar]
- 47.Vodnala S.K., Lundbäck T., Yeheskieli E., Sjöberg B., Gustavsson A.L., Svensson R., Olivera G.C., Eze A.A., De Koning H.P., Hammarström L.G.J., et al. Structure-activity relationships of synthetic cordycepin analogues as experimental therapeutics for African trypanosomiasis. J. Med. Chem. 2013;56:9861–9873. doi: 10.1021/jm401530a. [DOI] [PubMed] [Google Scholar]
- 48.Hulpia F., Campagnaro G.D., Scortichini M., Van Hecke K., Maes L., De Koning H.P., Caljon G., Van Calenbergh S. Revisiting tubercidin against kinetoplastid parasites: Aromatic substitutions at position 7 improve activity and reduce toxicity. Eur. J. Med. Chem. 2019;164:689–705. doi: 10.1016/j.ejmech.2018.12.050. [DOI] [PubMed] [Google Scholar]
- 49.Carter N.S., Berger B.J., Fairlamb A.H. Uptake of diamidine drugs by the P2 nucleoside transporter in melarsen-sensitive and -resistant Trypanosoma brucei brucei. J. Biol. Chem. 1995;270:28153–28157. doi: 10.1074/jbc.270.47.28153. [DOI] [PubMed] [Google Scholar]
- 50.De Koning H.P., MacLeod A., Barrett M.P., Cover B., Jarvis S.M. Further evidence for a link between melarsoprol resistance and P2 transporter function in African trypanosomes. Mol. Biochem. Parasitol. 2000;106:181–185. doi: 10.1016/S0166-6851(99)00206-6. [DOI] [PubMed] [Google Scholar]
- 51.Witola W.H., Inoue N., Ohashi K., Onuma M. RNA-interference silencing of the adenosine transporter-1 gene in Trypanosoma evansi confers resistance to diminazene aceturate. Exp. Parasitol. 2004;107:47–57. doi: 10.1016/j.exppara.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 52.Munday J.C., Rojas López K.E., Eze A.A., Delespaux V., Van Den Abbeele J., Rowan T., Barrett M.P., Morrison L.J., De Koning H.P. Functional expression of TcoAT1 reveals it to be a P1-type nucleoside transporter with no capacity for diminazene uptake. Int J. Parasitol. Drugs Drug Resist. 2013;3:69–76. doi: 10.1016/j.ijpddr.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jackson A.P., Allison H.C., Barry J.D., Field M.C., Hertz-Fowler C., Berriman M. A cell-surface phylome for African trypanosomes. PLoS Negl. Trop. Dis. 2013;7:e2121. doi: 10.1371/journal.pntd.0002121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Delespaux V., Chitanga S., Geysen D., Goethals A., Van den Bossche P., Geerts S. SSCP analysis of the P2 purine transporter TcoAT1 gene of Trypanosoma congolense leads to a simple PCR-RFLP test allowing the rapid identification of diminazene resistant stocks. Acta Trop. 2006;100:96–102. doi: 10.1016/j.actatropica.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 55.Vitouley H.S., Mungube E.O., Allegye-Cudjoe E., Diall O., Bocoum Z., Diarra B., Randolph T.F., Bauer B., Clausen P.H., Geysen D., et al. Improved PCR-RFLP for the detection of diminazene resistance in Trypanosoma congolense under field conditions using filter papers for sample storage. PLoS Negl. Trop. Dis. 2011;5:e1223. doi: 10.1371/journal.pntd.0001223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mamoudou A., Delespaux V., Chepnda V., Hachimou Z., Andrikaye J.P., Zoli A., Geerts S. Assessment of the occurrence of trypanocidal drug resistance in trypanosomes of naturally infected cattle in the Adamaoua region of Cameroon using the standard mouse test and molecular tools. Acta Trop. 2008;106:115–118. doi: 10.1016/j.actatropica.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 57.Mewamba E.M., Farikou O., Kamga R.M.N., Magang M.E.K., Tume C., Tiofack A.A.Z., Ravel S., Simo G. Molecular identification of diminazene aceturate-resistant strains of Trypanosoma congolense in naturally infected domestic animals of Yoko in the centre region of Cameroon. Vet. Parasitol. Reg. Stud. Rep. 2020;20:100405. doi: 10.1016/j.vprsr.2020.100405. [DOI] [PubMed] [Google Scholar]
- 58.Simo G., Magang E.M.K., Mewamba E.M., Farikou O., Kamga R.M.N., Tume C., Solano P., Ravel S. Molecular identification of diminazene aceturate resistant trypanosomes in tsetse flies from Yoko in the Centre region of Cameroon and its epidemiological implications. Parasite Epidemiol. Control. 2020;9:e00135. doi: 10.1016/j.parepi.2020.e00135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bridges D., Gould M.K., Nerima B., Mäser P., Burchmore R.J.S., De Koning H.P. Loss of the High Affinity Pentamidine Transporter is responsible for high levels of cross-resistance between arsenical and diamidine drugs in African trypanosomes. Mol. Pharmacol. 2007;71:1098–1108. doi: 10.1124/mol.106.031351. [DOI] [PubMed] [Google Scholar]
- 60.Carruthers L.V., Munday J.C., Ebiloma G.U., Steketee P., Jayaraman S., Campagnaro G.D., Ungogo M.A., Donnachie A., Lemgruber L., Rowan T.G., et al. Diminazene resistance in Trypanosoma congolense is not caused by reduced transport capacity but associated with reduced mitochondrial membrane potential. Mol. Microbiol. 2021;116:564–588. doi: 10.1111/mmi.14733. [DOI] [PubMed] [Google Scholar]
- 61.Alzahrani K.J.H., Ali J.A.M., Eze A.A., Looi W.L., Tagoe D.N.A., Creek D.J., Barrett M.P., De Koning H.P. Functional and genetic evidence that nucleoside transport is highly conserved in Leishmania species: Implications for pyrimidine-based chemotherapy. Int. J. Parasitol. Drugs Drug Resist. 2017;7:206–226. doi: 10.1016/j.ijpddr.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vasudevan G., Carter N.S., Drew M.E., Beverley S.M., Sanchez M.A., Seyfang A., Ullman B., Landfear S.M. Cloning of Leishmania nucleoside transporter genes by rescue of a transport-deficient mutant. Proc. Natl. Acad. Sci. USA. 1998;95:9873–9878. doi: 10.1073/pnas.95.17.9873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Carter N.S., Drew M.E., Sanchez M., Vasudevan G., Landfear S.M., Ullman B. Cloning of a novel inosine-guanosine transporter gene from Leishmania donovani by functional rescue of a transport-deficient mutant. J. Biol. Chem. 2000;275:20935–20941. doi: 10.1074/jbc.M002418200. [DOI] [PubMed] [Google Scholar]
- 64.Beneke T., Madden R., Makin L., Valli J., Sunter J., Gluenz E. A CRISPR Cas9 high-throughput genome editing toolkit for kinetoplastids. R. Soc. Open Sci. 2017;4:170095. doi: 10.1098/rsos.170095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hulpia F., Campagnaro G.D., Alzahrani K.J., Alfayez I.A., Ungogo M.A., Mabille D., Maes L., De Koning H.P., Caljon G., Van Calenbergh S. Structure-activity relationship exploration of 3′-deoxy-7-deazapurine nucleoside analogues as anti-Trypanosoma brucei agents. ACS Infect. Dis. 2020;6:2045–2056. doi: 10.1021/acsinfecdis.0c00105. [DOI] [PubMed] [Google Scholar]
- 66.Hulpia F., Bouton J., Campagnaro G.D., Alfayez I.A., Mabille D., Maes L., De Koning H.P., Caljon G., Van Calenbergh S. C6-O-alkylated 7-deazainosine nucleoside analogues: Discovery of potent and selective anti-sleeping sickness agents. Eur. J. Med. Chem. 2020;188:112018. doi: 10.1016/j.ejmech.2019.112018. [DOI] [PubMed] [Google Scholar]
- 67.De Almeida Fiuza L.F., Batista D.G.J., Girão R.D., Hulpia F., Finamore P., Aldfer M.M., Elmahallawy E.K., De Koning H.P., Moreira O.C., Van Calenbergh S., et al. Phenotypic evaluation of nucleoside analogues against Trypanosoma cruzi infection: In vitro and in vivo approaches. Molecules. 2022;27:8087. doi: 10.3390/molecules27228087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Natto M.J., Hulpia F., Kalkman E.R., Baillie S., Alhejeli A., Miyamoto Y., Eckmann L., Van Calenbergh S., De Koning H.P. Deazapurine nucleoside analogues for the treatment of Trichomonas vaginalis. ACS Infect. Dis. 2021;7:1752–1764. doi: 10.1021/acsinfecdis.1c00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mabille D., Ilbeigi K., Hendrickx S., Ungogo M.A., Hulpia F., Lin C., Maes L., De Koning H.P., Van Calenbergh S., Caljon G. Nucleoside analogues for the treatment of animal African trypanosomiasis. Int. J. Parasitol. Drugs Drug Resist. 2022;19:21–30. doi: 10.1016/j.ijpddr.2022.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Burchmore R., Wallace L.J.M., Candlish D., Al-Salabi M.I., Beal P., Barrett M.P., Baldwin S.A., De Koning H.P. Cloning, heterologous expression, and in situ characterization of the first high affinity nucleobase transporter from a protozoan. J. Biol. Chem. 2003;278:23502–23507. doi: 10.1074/jbc.M301252200. [DOI] [PubMed] [Google Scholar]
- 71.Henriques C., Sanchez M.A., Tryon R., Landfear S.M. Molecular and functional characterization of the first nucleobase transporter gene from African trypanosomes. Mol. Biochem. Parasitol. 2003;130:101–110. doi: 10.1016/S0166-6851(03)00167-1. [DOI] [PubMed] [Google Scholar]
- 72.Tetaud E., Lecuix I., Sheldrake T., Baltz T., Fairlamb A.H. A new expression vector for Crithidia fasciculata and Leishmania. Mol. Biochem. Parasitol. 2002;120:195–204. doi: 10.1016/S0166-6851(02)00002-6. [DOI] [PubMed] [Google Scholar]
- 73.Gudin S., Quashie N.B., Candlish D., Al-Salabi M.I., Jarvis S.M., Ranford-Cartwright L.C., De Koning H.P. Trypanosoma brucei: A survey of pyrimidine transport activities. Exp. Parasitol. 2006;114:103–108. doi: 10.1016/j.exppara.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 74.Ali J.A.M., Creek D.J., Burgess K., Allison H.C., Field M.C., Mäser P., De Koning H.P. Pyrimidine salvage in Trypanosoma brucei bloodstream forms and the trypanocidal action of halogenated pyrimidines. Mol. Pharmacol. 2013;83:439–453. doi: 10.1124/mol.112.082321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Munday J.C., Eze A.A., Baker N., Glover L., Clucas C., Aguinaga Andrés D., Natto M.J., Teka I.A., McDonald J., Lee R.S., et al. Trypanosoma brucei Aquaglyceroporin 2 is a high affinity transporter for pentamidine and melaminophenyl arsenic drugs and is the main genetic determinant of resistance to these drugs. J. Antimicrob. Chemother. 2014;69:651–663. doi: 10.1093/jac/dkt442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Matovu E., Stewart M., Geiser F., Brun R., Mäser P., Wallace L.J.M., Burchmore R.J., Enyaru J.C.K., Barrett M.P., Kaminsky R., et al. Mechanisms of Arsenical and Diamidine Uptake and Resistance in Trypanosoma brucei. Eukaryot. Cell. 2003;2:1003–1008. doi: 10.1128/EC.2.5.1003-1008.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Graf F.E., Ludin P., Wenzler T., Kaiser M., Brun R., Pati Pyana P., Büscher P., De Koning H.P., Horn D., Mäser P. Aquaporin 2 mutations in Trypanosoma brucei gambiense field isolates correlate with decreased susceptibility to pentamidine and melarsoprol. PLoS Negl. Trop. Dis. 2013;7:e2475. doi: 10.1371/journal.pntd.0002475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hammarton T.C. Cell cycle regulation in Trypanosoma brucei. Mol. Biochem. Parasitol. 2007;153:1–8. doi: 10.1016/j.molbiopara.2007.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Thomas J.A., Baker N., Hutchinson S., Dominicus C., Trenaman A., Glover L., Alsford S., Horn D. Insights into antitrypanosomal drug mode-of-action from cytology-based profiling. PLoS Negl. Trop. Dis. 2018;12:e0006980. doi: 10.1371/journal.pntd.0006980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ibrahim H.M., Al-Salabi M.I., El Sabbagh N., Quashie N.B., Alkhaldi A.A., Escale R., Smith T.K., Vial H.J., De Koning H.P. Symmetrical choline-derived dications display strong anti-kinetoplastid activity. J. Antimicrob. Chemother. 2011;66:111–125. doi: 10.1093/jac/dkq401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Giordani F., Khalaf A.I., Gillingwater K., Munday J.C., De Koning H.P., Suckling C.J., Barrett M.P., Scott F.J. Novel Minor Groove Binders cure animal African trypanosomiasis in an in vivo mouse model. J. Med. Chem. 2019;62:3021–3035. doi: 10.1021/acs.jmedchem.8b01847. [DOI] [PubMed] [Google Scholar]
- 82.De Koning H.P., Gould M.K., Sterk G.J., Tenor H., Kunz S., Luginbuehl E., Seebeck T. Pharmacological validation of Trypanosoma brucei phosphodiesterases as novel drug targets. J. Infect. Dis. 2012;206:229–237. doi: 10.1093/infdis/jir857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nvau J.B., Alenezi S., Ungogo M.A., Alfayez I.A.M., Natto M.J., Igoli J.O., Gray A.I., Ferro V.A., Watson D.G., De Koning H.P. Antiparasitic and cytotoxic activity of Bokkosin, a novel diterpene substituted chromanyl benzoquinone from Calliandra portoricensis. Front. Chem. 2020;8:574103. doi: 10.3389/fchem.2020.574103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Spector T., Jones T.E., LaFon S.W., Nelson D.J., Berens R.L., Marr J.J. Monophosphates of formycin B and allopurinol riboside: Interactions with leishmanial and mammalian succino-AMP synthetase and GMP reductase. Biochem. Pharmacol. 1984;33:1611–1617. doi: 10.1016/0006-2952(84)90282-X. [DOI] [PubMed] [Google Scholar]
- 85.Steketee P.C., Dickie E.A., Iremonger J., Crouch K., Paxton E., Jayaraman S., Alfituri O.A., Awuah-Mensah G., Ritchie R., Schnaufer A., et al. Divergent metabolism between Trypanosoma congolense and Trypanosoma brucei results in differential sensitivity to metabolic inhibition. PloS Path. 2021;17:e1009734. doi: 10.1371/journal.ppat.1009734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Coustou V., Guegan F., Plazolles N., Baltz T. Complete in vitro life cycle of Trypanosoma congolense: Development of genetic tools. PLoS Negl. Trop. Dis. 2010;4:e618. doi: 10.1371/journal.pntd.0000618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Awuah-Mensah G., McDonald J., Steketee P.C., Autheman D., Whipple S., D’Archivio S., Brandt C., Clare S., Harcourt K., Wright G.J., et al. Reliable, scalable functional genetics in bloodstream-form Trypanosoma congolense in vitro and in vivo. PLoS Path. 2021;17:e1009224. doi: 10.1371/journal.ppat.1009224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chamond N., Cosson A., Blom-Potar M.C., Jouvion G., d’Archivio S., Medina M., Droin-Bergère S., Huerre M., Goyard S., Minoprio P. Trypanosoma vivax infections: Pushing ahead with mouse models for the study of Nagana. I. Parasitological, hematological and pathological parameters. PLoS Negl. Trop. Dis. 2010;4:e792. doi: 10.1371/journal.pntd.0000792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.d’Archivio S., Medina M., Cosson A., Chamond N., Rotureau B., Minoprio P., Goyard S. Genetic engineering of Trypanosoma (Dutonella) vivax and in vitro differentiation under axenic conditions. PLoS Negl. Trop. Dis. 2011;5:e1461. doi: 10.1371/journal.pntd.0001461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.D’Archivio S., Cosson A., Medina M., Lang T., Minoprio P., Goyard S. Non-invasive in vivo study of the Trypanosoma vivax infectious process consolidates the brain commitment in late infections. PLoS Negl. Trop. Dis. 2013;7:e1976. doi: 10.1371/journal.pntd.0001976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sanchez M.A., Ullman B., Landfear S.M., Carter N.S. Cloning and functional expression of a gene encoding a P1 type nucleoside transporter from Trypanosoma brucei. J. Biol. Chem. 1999;274:30244–30249. doi: 10.1074/jbc.274.42.30244. [DOI] [PubMed] [Google Scholar]
- 92.De Koning H.P. Transporters in African trypanosomes: Role in drug action and resistance. Int. J. Parasitol. 2001;31:512–522. doi: 10.1016/S0020-7519(01)00167-9. [DOI] [PubMed] [Google Scholar]
- 93.Lüscher A., De Koning H.P., Mäser P. Chemotherapeutic strategies against Trypanosoma brucei: Drug targets vs. drug targeting. Curr. Pharm. Des. 2007;13:555–567. doi: 10.2174/138161207780162809. [DOI] [PubMed] [Google Scholar]
- 94.Ogbunude P.O.J., Ikediobi C.O., Ukoha A.I. Adenosine cycle in African trypanosomes. Ann. Trop. Med. Parasitol. 1985;79:7–11. doi: 10.1080/00034983.1985.11811883. [DOI] [PubMed] [Google Scholar]
- 95.James D.M., Born G.V.R. Uptake of purine bases and nucleosides in African trypanosomes. Parasitology. 1980;81:383–393. doi: 10.1017/S0031182000056110. [DOI] [PubMed] [Google Scholar]
- 96.Ortiz D., Sanchez M.A., Quecke P., Landfear S.M. Two novel nucleobase/pentamidine transporters from Trypanosoma brucei. Mol. Biochem. Parasitol. 2009;163:67–76. doi: 10.1016/j.molbiopara.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lin C., Ferreira de Almeida Fiuza L., Cardoso Santos C., Ferreira Nunes D., Cruz Moreira O., Bouton J., Karalic I., Maes L., Caljon G., Hulpia F., et al. 6-Methyl-7-aryl-7-deazapurine nucleosides as anti-Trypanosoma cruzi agents: Structure-activity relationship and in vivo efficacy. ChemMedChem. 2021;16:2231–2253. doi: 10.1002/cmdc.202100144. [DOI] [PubMed] [Google Scholar]
- 98.Lin C., Hulpia F., Karalic I., De Schepper L., Maes L., Caljon G., Van Calenbergh S. 6-Methyl-7-deazapurine nucleoside analogues as broad-spectrum antikinetoplastid agents. Int. J. Parasitol. Drugs Drug Resist. 2021;17:57–66. doi: 10.1016/j.ijpddr.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Richards S., Morrison L.J., Torr S.J., Barrett M.P., Manangwa O., Mramba F., Auty H. Pharma to farmer: Field challenges of optimizing trypanocide use in African animal trypanosomiasis. Trends Parasitol. 2021;37:831–843. doi: 10.1016/j.pt.2021.04.007. [DOI] [PubMed] [Google Scholar]
- 100.Fidalgo L.M., Gille L. Mitochondria and trypanosomatids: Targets and drugs. Pharm. Res. 2011;28:2758–2770. doi: 10.1007/s11095-011-0586-3. [DOI] [PubMed] [Google Scholar]
- 101.Eze A.A., Gould M.K., Munday J.C., Tagoe D.N.A., Stelmanis V., Schnaufer A., De Koning H.P. Loss of mitochondrial membrane potential is a late adaptation of Trypanosoma brucei brucei to isometamidium preceded by mutations in the γ subunit of the F1F0-ATPase. PLoS Negl. Trop. Dis. 2016;10:e0004791. doi: 10.1371/journal.pntd.0004791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Drew M.E., Morris J.C., Wang Z., Wells L., Sanchez M., Landfear S.M., Englund P.T. The adenosine analog tubercidin inhibits glycolysis in Trypanosoma brucei as revealed by an RNA interference library. J. Biol. Chem. 2003;278:46596–46600. doi: 10.1074/jbc.M309320200. [DOI] [PubMed] [Google Scholar]
- 103.Anyam J.V., Daikwo P.E., Ungogo M.A., Nweze N.E., Igoli N.P., Gray A.I., De Koning H.P., Igoli J.O. Two New Antiprotozoal Diterpenes from the Roots of Acacia nilotica. Front. Chem. 2021;9:624741. doi: 10.3389/fchem.2021.624741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wallace L.J.M., Candlish D., De Koning H.P. Different substrate recognition motifs of human and trypanosome nucleobase transporters: Selective uptake of purine antimetabolites. J. Biol. Chem. 2002;277:26149–26156. doi: 10.1074/jbc.M202835200. [DOI] [PubMed] [Google Scholar]
- 105.Cheng Y., Prusoff W.H. Relationship between the inhibition constant (Ki) and the concentration of inhibitor which causes 50 per cent inhibition (I50) of an enzymatic reaction. Biochem. Pharmacol. 1973;22:3099–3108. doi: 10.1016/0006-2952(73)90196-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are included in the manuscript and Supplemental Materials.