Abstract
Rickettsia amblyommatis is a potentially pathogenic species of Rickettsia within the spotted fever group vectored by ticks. While many studies have been published on this species, there is debate over its pathogenicity and the inhibitory role it plays in diagnosing illnesses caused by other spotted fever group Rickettsia species. Many publications have recorded the high infection prevalence of R. amblyommatis in tick populations at a global scale. While this species is rather ubiquitous, questions remain over the epidemiological importance of this possible human pathogen. With tick-borne diseases on the rise, understanding the exact role that R. amblyommatis plays as a pathogen and inhibitor of infection relative to other tick-borne pathogens will help public health efforts. The goal of this review was to compile the known literature on R. amblyommatis, review what we know about its geographic distribution, tick vectors, and pathogenicity, assess relatedness between various international strains from ticks by phylogenetic analysis and draw conclusions regarding future research needed.
Keywords: Rickettsia amblyommatis, Amblyomma spp., Amblyomma americanum, lone star tick, tick-borne pathogens
1. Medical and Veterinary Importance of Ticks
Ticks and the pathogens they vector represent a significant threat to humans, livestock, companion animals, and wildlife. Ticks are responsible for transmitting a greater variety of pathogens than any other arthropod group [1,2]. Cases of tick-borne disease have been increasing within the United States, having doubled from >22,000 cases in 2004 to >48,000 cases in 2016, with Lyme disease accounting for 82% of these reports [3]. According to the CDC, reported tick-borne disease cases increased to 50,865 in the USA in 2019 [4]. Some of the tick-borne diseases that impact people include Lyme disease (Borrelia burgdorferi), Rocky Mountain spotted fever (Rickettsia rickettsii), tick-borne encephalitis (Flavivirus), babesiosis (Babesia microti), anaplasmosis (Anaplasma phagocytophilum), ehrlichiosis (Ehrlichia ewingii and Ehrlichia chaffeensis), and others [5,6]. Some of the most important species of ticks that are responsible for the spread of important human pathogens include Amblyomma americanum, Amblyomma maculatum, Dermacentor variabilis, Ixodes pacificus, Ixodes ricinus, Ixodes scapularis, Rhipicephalus sanguineus, and others [5,6,7]. These tick-borne diseases can be life-threatening, and while some vaccines have ongoing clinical trials, vaccine availability is currently lacking [8,9,10]. Tick-borne diseases are responsible for significant economic losses within the livestock industry and present a threat to public health worldwide [2]. The incidence of cases of tick-borne diseases is projected to increase as climate change continues to alter environmental conditions that may change the distribution of tick species [1,11,12,13]. This may be especially true for rickettsial spotted fever illnesses with ticks as their primary vector. Due to the enhancement of cell culture systems and molecular techniques, the number of identified species of Rickettsia has increased significantly over the past 40 years [14,15,16,17,18].
2. Materials and Methods
To write this review, five electronic databases (Web of Science, Google Scholar, PubMed, ScienceDirect, and SciELO) were searched during the time frame of 1 May to 5 December 2022 for relevant publications spanning multiple decades. To the best of our knowledge, we have written a review that is representative of all of the databases investigated. For this search, the following keywords were used: “Rickettsia amblyommatis”, “Rickettsia amblyommii”, and “Candidatus Rickettsia amblyommii”. The molecular phylogenetic analyses were completed using MEGA11 software (MEGA11: Molecular Evolutionary Genetics Analysis version 11) [19] using a maximum likelihood method on the Kimura 2-model (ML; bootstrap replicates: 1000). These blast searches were conducted on 3 February 2023.
3. Background on Rickettsia
The genus Rickettsia includes a diverse group of intracellular Gram-negative bacteria that are often the causative agents of disease for a variety of pathogens vectored by arthropods. Species within the genus of Rickettsia are split into four groups, including the spotted fever group (SFG), typhus group, Rickettsia bellii group, and the Rickettsia canadensis group [20,21,22]. It has also been recently shown that Candidatus Rickettsia mendelii is a separate basal group [23]. Rickettsia species are transmitted by a variety of arthropod vectors such as ticks, chiggers, fleas, and lice [24,25,26,27]. The maintenance of Rickettsia is dependent on animal hosts, mainly vertebrates; however, the role of these hosts in the life cycle of these bacteria is poorly understood [28]. Some hosts provide the necessary bloodmeal to ticks, and others provide essential supplemental components for the transmission of pathogens [28]. The spotted fever group (SFG) comprises the majority of tick-borne Rickettsia, consisting of 29 validly published species [29]. The primary reservoirs and vectors of SFG rickettsia are ticks. SFG rickettsia can move transstadially and transovarially, with some species of Rickettsia living within the entire life cycle of the tick [27,30]. Some species of Rickettsia are pathogenic and lethal causing serious morbidity in humans, while others are endosymbionts or symbionts not known to play an active role in human disease [30,31,32]. Some tick-borne Rickettsia species and the diseases they cause include R. rickettsii, R. parkeri, R. akari (spotted fever rickettsioses), R. africae (African tick bite fever), and R. australis (Australian tick typhus). In the United States, Rocky Mountain spotted fever (RMSF) caused by R. rickettsii is currently considered the most lethal identified rickettsial disease to humans [6,33,34]. Until 2010, most patients with tick-associated rickettsiosis were considered to have RMSF caused by Rickettsia rickettsii [35,36]. However, SFG rickettsial species elicit cross-reactive antibodies, and the immunofluorescence tests used by US public health labs cannot distinguish between the Rickettsia species that cause these different diseases [37]. Therefore, the CDC, as of 2010, now classifies cases formerly reported as RMSF as cases of SFG rickettsioses.
While rickettsioses are some of the oldest known vector-borne diseases, there is still much that is unknown and even debated, especially regarding each species’ potential pathogenicity and status as being infectious or symbiotic [14,27]. With the arrival of molecular techniques, the understanding of Rickettsia has expanded. Still, there remain gaps in our knowledge, and with endemic rickettsioses cases on the rise, it is essential to understand these diseases fully. Over the last two decades, there has been great debate over the pathogenicity and significance of a specific ubiquitous species of Rickettsia, Rickettsia amblyommatis, which will be the focus of this review.
Background on Rickettsia amblyommatis
Rickettsia amblyommatis (formerly Candidatus Rickettsia amblyommii) was first discovered in Tennessee, USA in 1973 from the tick, Amblyomma americanum [38,39]. After this initial finding, R. amblyommatis was discovered infecting A. americanum populations at high percentages in South Carolina, USA, and Arkansas, USA [38]. Since then, R. amblyommatis was discovered infecting tick populations at high prevalence worldwide, reaching greater than 90% in the USA and Panama [40,41,42]. While R. amblyommatis has primarily been isolated from ticks, it was recently discovered in chiggers (Leptotrombidium peromysci and Eutrombicula spp.) in North Carolina, USA [43]; however, this review will focus solely on ticks. Rickettsia amblyommatis was previously and informally described as Rickettsia amblyommii in the Stothard 1995 dissertation [44]. This species’ name as well as Candidatus R. amblyommii was used throughout publications until 2016 when Karpathy et al. [38] formally assigned the name, R. amblyommatis, to conform to the rules of the International Code of Nomenclature.
Since its initial discovery, R. amblyommatis has proven to be an increasingly prevalent tick-borne rickettsial species, having been detected in 34 species of ticks in 17 countries (Figure 1; Table 1). Most significantly, R. amblyommatis has continually been detected at high prevalence in the USA in A. americanum populations, a geographically widespread human-biting tick [9,40,45,46,47,48]. In addition to being ubiquitous, R. amblyommatis is reported to have interesting other properties such as preventing ticks from acquiring other coinfected species of Rickettsia [31,49], altering tick host-seeking behavior [50,51], and affecting the progression of disease symptoms when infecting humans [52,53]. This is the first review of R. amblyommatis. In this review, we compiled all known information on R. amblyommatis in published studies, specifically discuss its distribution, discovery in different tick species, and pathogenicity, examined phylogenetic relatedness of the various strains of R. amblyommatis detected in ticks by PCR and from isolates of R. amblyommatis globally, and consider possible future directions of research needed.
Figure 1.
World map displaying the distribution of Rickettsia amblyommatis-infected ticks. Map created using www.mapchart.net (accessed on 27 January 2023).
Table 1.
Summary of quantitative data obtained from peer-reviewed publications for R. amblyommatis-infected wild ticks collected globally. This table includes the location in which they were collected, the species of tick, the infection prevalence, and the collection type. Studies were included if R. amblyommatis was confirmed through conventional PCR and sequencing analysis.
| Location | Species of Tick | Infection Prevalence % a | Collection Type | Reference |
|---|---|---|---|---|
| AR, USA | A. maculatum | 28% (58/207) | Off-host (white-tailed deer, dogs) | [54] |
| AR, USA | A. americanum | 41.9% (463) b | Vegetation | [55] |
| AR, USA | A. americanum, A. maculatum, I. scapularis, Amblyomma spp. | NA c | Off-host (white-tailed deer, dogs) | [56] |
| AR, USA | A. americanum | 98% (42/43 pools) | Flagging, CO2 Trapping | [57] |
| FL, USA | A. americanum | 29% (391/1312) | Flagging | [58] |
| FL, USA | A. americanum | 29.5% (52/176) | Dragging | [50] |
| FL, USA | A. americanum | 38.0% (223/588) | Dragging | [51] |
| FL, USA | A. americanum | 57.1% (845/1479) | Flagging | [59] |
| FL, USA | A. americanum | 37.1% (56/151) | Flagging | [47] |
| FL, USA | A. americanum, D. variabilis | 57.3% (63/110), 35% (6/17) | Off-host (wild pig) | [60] |
| FL, USA | A. americanum, A. maculatum | 27.8% (5/18), 16.7% (1/6) | Black bears | [61] |
| GA, USA | A. americanum | 0.52% (1/194) | Dogs | [62] |
| GA, USA | A. americanum, D. variabilis, A. maculatum | 27.5% (117/426), 1.4% (2/142), 9.1% (4/22) | Off-host (humans) | [53] |
| GA, USA | A. americanum | 87% of pools (519/598) | Flagging | [63] |
| GA, USA | A. americanum | 44.7% (315/704) | Flagging | [47] |
| Guam, Marianna Islands, USA | A. breviscutatum, R. microplus | 2.67% (3/112) | Off-host (wild pig, Philippine deer) | [64] |
| IA, USA | A. americanum | 57.9% (11/19) | Flagging | [47] |
| KS, USA | A. americanum, D. variabilis | 93% nymphal pools, 94% adult pools, and 4.7% (169) | Dragging | [65] |
| KY, USA | A. americanum, D. variabilis | 27.8% (30/108), 1.1% (2/179) | Off-host (canine, hog, horse, raccoon, white-tailed deer, human) | [66] |
| KY, USA | D. variabilis | 0.8% (1/124) | Unknown e | [67] |
| LA, USA | A. americanum | 60% (3/5) | Off-host (black bears) | [41] |
| MD, USA | A. americanum | 87.9% (29/33 pools), 90% (27/30 individuals) | Flagging | [68] |
| MD, USA | A. americanum | 64.50% d | Dragging | [69] |
| MO, USA | A. americanum | 3.2% (40/1269) | Field surveillance | [70] |
| MO, USA | A. americanum, D. variabilis, I. scapularis | 89% (24/27 pools), 100% (7/7 pools), 50% (1/2) | Flagging | [71] |
| MO, USA | A. americanum | 74% (213/288) | Dragging, CO2 bait traps, Off-host (human) | [72] |
| MS, USA | A. americanum | 92.4% (73/79) | Dragging | [73] |
| NC, USA | A. americanum, A. maculatum, D. variabilis, I. scapularis | 90.9% (412/453), 28.6% (2/7), 20% (1/5), 8.3% (1/12) | Off-host (humans) | [40] |
| NC, USA | D. variabilis | 29.3% (156/532) | Flagging | [74] |
| NC, USA | A. americanum, D. variabilis | 56.4% (871/1590), 11.1% (4/36) | Flagging | [75] |
| NC, USA | A. americanum | 55.2% (216/391) | Flagging | [47] |
| Northeast, USA | D. variabilis | 1.7% (3/181) | Off-host (dogs) | [76] |
| NJ, USA | A. americanum | 6.6% (8/121) | Flagging | [47] |
| NJ, USA | A. americanum | 25% (465/1858) | Dragging | [77] |
| NJ, USA | A. americanum | 20% (49/245) | Sweeping vegetation | [78] |
| NJ, USA | A. americanum | 12.8% (36/281) | Dragging and standard walking | [79] |
| NY, USA | A. americanum | 58.35% (394/676) | Flagging | [80] |
| NY, USA | D. variabilis | 8.3% (1/12) | Unknown e | [67] |
| NY, USA | A. americanum | 41.7% (198/475) | Flagging | [47] |
| OH, USA | A. americanum | 30.2% (93/308) | Off-host (humans), Flagging | [81] |
| OH, USA | A. americanum | 38% (8/21) | Humans | [82] |
| OK, USA | A. americanum | 10% (6/60) | Flagging | [47] |
| OK, USA | A. americanum | 33.6% (146/434) | Unknown e | [83] |
| OK, USA | A. americanum | 17.6% (123/700) | Dry Ice Traps | [84] |
| RI, USA | A. americanum | 47.4% (18/38) | Flagging | [47] |
| SC, USA | A. americanum | 11.7% (545) b | Off-Vegetation | [55] |
| SC, USA | A. americanum | 45.6% (36/79) | Flagging | [47] |
| SC, USA | A. americanum, D. variabilis | 80% (84/105), 66.7% (10/15) | Off-host (Wild Pig) | [60] |
| TN, USA | A. americanum | 16.6% (96) b | Vegetation | [55] |
| TN, USA | A. americanum, D. variabilis | 40% (255/655), 2.5% (14/555) | Off-host (humans, wild animals, dogs) | [85] |
| TN, USA | A. americanum | 4.9% (45/926) | Dragging, CO2 baited trap | [86] |
| TX, USA | A. auricularium, A. geayi, A. longirostre | 28.6% (2/7), 33.3% (1/3), 11.9% (5/42) | Off-host (wild birds) | [87] |
| TX, USA | A. americanum, I. scapularis | 50% (41/82), 1.47% (2/136) | Dragging | [88] |
| TX, USA | A. americanum | 100% (68/68 pools) | Dry ice trapping, Dragging, and Flagging | [89] |
| TX, USA | A. inornatum | 100% (3/3) | Off-host (deer) | [90] |
| TX, USA | A. inornatum | Unknown g | CO2 Traps | [91] |
| TX, USA | A. americanum, A. cajennense | 30.3% (179), 32.3% (10) f | Off-host (humans) | [92] |
| VA, USA | A. americanum | 72.8% (pools) | Dragging | [93] |
| VA, USA | A. americanum | 80.3% of pools d | Flagging | [94] |
| VA, USA | D. variabilis | 4.2% (9/214) | Unknown e | [67] |
| VA, USA | A. americanum | 19% (65/340) | Dragging | [95] |
| USA | D. variabilis | 0.1% (7/5286) | Off-host (humans) | [96] |
| USA | A. americanum | 80.5% (58/72 pools), 66.5% (244/367) | Off-host (humans) | [48] |
| Córdoba, Argentina | A. neumanni | 23.6 (13/55) | Walking Survey, CO2 traps | [97] |
| Northern Argentina | A. neumanni | 21% (3/14) | Off-host and Flagging | [98] |
| Salta, Argentina | A. hadanii, A. neumannii | 21.3% (27/127), 44.4% (8/18) | Dragging | [99] |
| Salta, Argentina | A. tonelliae | 1.47% (1/68) | Dragging | [100] |
| Argentina | A. hadanii | 1.6% (1/60) | Vegetation and Off-host (cattle) | [101] |
| Australia | I. tasmani | 28.2% (22/78) | Off-host (koalas) | [102] |
| Belize | A. pacae | 100% (1/1) | Off-host (spotted paca) | [103] |
| Belize | A. cajennense, A. maculatum | 55.1% (81/147), 66.7% (2/3) | Off-host (dog) | [104] |
| Acre, Brazil | A. humerale | 33.3% (1/3) of A. humerale | Off-host (capybara) | [105] |
| Acre, Brazil | A. longirostre, A. geayi | 62.5% (5/8), 50% (1/2) | Off-host (wild birds) | [106] |
| Acre, Brazil | A. rotundatum | 14.3% (1/7) | Off-host (Amazon tree boa) | [107] |
| Amazonas, Brazil | A. humerale | 2.17% (1/46) | Off-host (tegu) | [108] |
| Bahia, Brazil | A. longirostre | 15.4% (2/13) | Off-host (wild birds) | [109] |
| Bahia, Brazil | A. longirostre, A. varium | 24.4% (11/45), 20% (1/5) | Off-host (wild birds) | [110] |
| Bahia, Brazil | A. longirostre | 23.7% (9/38) | Off-host (thin-spined porcupine and hairy dwarf porcupine) | [111] |
| Bahia, Brazil | A. auricularium, Ambylomma spp. larvae | 57.5% (46/80) | Off-host (gray short-tailed opossum, rodent, Brazilian three-banded armadillo) | [112] |
| Espírito Santo, Brazil | A. humerale | 50% (5/10) | Off-host (tortoise) | [113] |
| Maranhão, Brazil | A. cajennense | 1% (1/100) | Off-host (dogs) | [114] |
| Maranhão, Brazil | A. cajennense | 16.7% (3/18) | Off-host (horses) | [115] |
| Mato Grosso, Brazil | A. cajennense | 0.45% (3/665) | Off-host (horse, donkey) | [116] |
| Mato Grosso, Brazil | A. cajennense | 31% (5/16 pools) | Off-host (human) and flagging | [117] |
| Mato Grosso, Brazil | A. auricularium, A. cajennense | 100% (1/1), 69.4% (136/196) | Off-host (wild animals) | [118] |
| Mato Grosso, Brazil | A. cajennense, A. ovale | 3.3% (5/152), 15.4% (2/13) | Off-host (dogs) | [119] |
| Mato Grosso, Brazil | A. cajennense, A. coelebs | 38.4% (10/26), 70% (7/10) | Off-host | [120] |
| Mato Grosso, Brazil | A. sculptum | 1.2% (1/85 pools) | Off-host (Azara’s agouti) | [121] |
| Mato Grosso, Brazil | A. longirostre | 45.5% (5/9) | Off-host (wild birds) | [122] |
| Mato Grosso, Brazil | A. dubitatum | 5% (1/20) | Off-host (dog) | [123] |
| Mato Grosso, Brazil | A. cajennense, A. coelebs, A. humerale, Amblyomma spp. | NA g | Off-host (rodents, marsupials) | [124] |
| Minas Gerais, Brazil | A. longirostre | (13/49; 26%) | Off-host (wild birds) | [125] |
| Pará, Brazil | A. longirostre, A. humerale. | 70% (7/10), 22.2 % (2/9) | Off-host (wild animals) | [118] |
| Pará, Brazil | A. longirostre, A. geayi | 56.7% (38/67), 57.1% (4/7) | Off-host (birds) | [126] |
| Paraíba, Brazil | A. auricularium, A. longirostre | 23.1% (3/13), 45.5% (10/22) | Off-host (wild birds) | [127] |
| Paraná, Brazil | A. longirostre | 32.3% (11/34) | Off-host (wild Birds) | [128] |
| Paraná, Brazil | A. coelebs | 1.9% (8/420) | Off-host (ring-tailed coatis) | [129] |
| Pernambuco, Brazil | A. auricularium | 20% (1/5) | Off-host (rodent) | [130] |
| Pernambuco, Brazil | A. auricularium | 53.3% (8/15) | Off-host (skunk, rabbit) | [131] |
| Pernambuco, Brazil | A. pseudoconcolor | 90.9% (10/11) | Off-host (dog, six-banded armadillo) | [132] |
| Rio Grande do Norte, Brazil | A. auricularium | 11.1% (14/126 individuals and pools) | Off-host (white-eared opossum and xix-banded armadillo) | [133] |
| Rio Grande do Sul, Brazil | A. longirostre | 66.7% (2/3) | Off-vegetation, Dragging | [134] |
| Rondônia, Brazil | A. coelebs, A. cajennense | 14.3% (1/7), 26.8% (11/41) | Off-vegetation | [135] |
| Rondônia, Brazil | A. cajennense, A. oblongoguttatum | 6.3% (2/32) + 2 pools, 16.7% (1/6) | CO2 traps; drag flagging; off-vegetation | [136] |
| Santa Catarina, Brazil | A. longirostre | 100% (1/1) | Unknown e | [137] |
| São Paulo, Brazil | A. coelebs | Unknown g | Off-vegetation | [138] |
| Brazil | A. calcaratum, A. longirostre | 50% (1/2), 12.3% (9/73) | Off-host (wild Birds) | [139] |
| Brazil | A. sculptum | 0.5% (1/200) | Dragging | [140] |
| Chile | Ornithodoros sp. | 100% (4/4) | Off-host (rodent) | [141] |
| Caldas, Colombia | A. longirostre, A. varium, Ixodes sp. | 6.67% (3/45), 66.6% (2/3), 11.1% (1/9) | Off-host (wild Birds) | [142] |
| Villeta, Colombia | A. cajennense | 9.1% (1/11) | Off-host (humans) | [143] |
| Costa Rica | A. cajennense | 66.7% (10/15) | Off-host (horse) | [144] |
| Costa Rica | A. mixtum, A. ovale, D. nitens, R. sanguineus | NA g | Off-host (horses, cows, humans, dogs) and off-vegetation | [145] |
| Costa Rica | R. sanguineus | 16.7% (1/6 pools) | Off-host (dogs) | [146] |
| Costa Rica | A. longirostre, A. geayi | 7.4% (4/54 pools), 3.7% (2/54 pools) | Off-host (wild birds) | [147] |
| Cuba | A. mixtum | 35.7% (5/14) | Off-host (horses) | [148] |
| Cuba | A. mixtum, Amblyomma spp. | 73% pools (422) f | Off-host (horses and dogs) | [149] |
| El Salvador | A. mixtum, A. parvum, D. nitens, Amblyomma spp. | 77% (10/13), 50% (8/16), 8% (1/13), 11% (1/9) | Off-host (wild and domestic animals) | [150] |
| Regina, French Guiana | A. coelebs | 15.4% (2/13) | Off-host (white-lipped peccaries) | [151] |
| French Guiana | A. cajennense, many more | 25% f, NA g,f | Dragging, Flagging, Off-host | [152] |
| Honduras | A. longirostre, A. mixtum | 14% (1/7), 80% (4/5) | Off-host (wild birds, humans) | [153] |
| Reynosa, Mexico | R. sanguineus | 1% (3/292) | Off-host (domestic dogs) | [154] |
| Mexico | A. mixtum, A. oblongoguttatum, A. parvum | 33.5% (59/176), 3.17% (2/63), 5.7% (3/53) | Off-vegetation, Off-host (possum, ocelot, white-nosed coati) | [155] |
| Mexico | A. maculatum, A. mixtum | 9.8% (5/51), 13.2% (17/129) | Off-host (wild pigs) | [156] |
| Mexico | A. mixtum | 50% (1/2) | Off-host (iguana) | [157] |
| Mexico | A. mixtum | 40% (2/5) | Human | [158] |
| Nicaragua | A. ovale | 100% (1/1 pools) | Off-host (dogs) | [146] |
| Pakistan | R. microplus, H. anatolicum, and H. dromedarii | 4%(21/514) f | Off-host (buffalo, cattle, sheep, goat, donkey, camel) | [159] |
| Panama | A. mixtum, H. juxtakochi, Amblyomma spp. | 27.8% (5/18), 4.3% (1/23), 8.2% (12/146 pools) | Dragging | [160] |
| Panama | A. mixtum | 94.1% (48/51) | Off-host (tapir, horses) | [42] |
| Panama | A. cajennense, A. oblongoguttatum, A. ovale, R. sanguineus | 86.4% (38/44), 50% (2/4), 27.9% (12/43), 3.1% (2/64) | Off-host (dogs, horses, pig) | [161] |
| Panama | A. cajennense, D. nitens, R. sanguineus | 36.7% (11/30), 27.4% (17/62), 12.3% (7/57) | Off-host (horses, dogs) | [162] |
| Panama | A. mixtum, H. Juxtakochi, Immature Amblyomma spp. | 27.8% (5/18), 4.6% (3/65), 11.5% (12/104) | Dragging | [160] |
| Paraguay | A. longirostre | 11.8% (2/17) | Off-host (wild birds) | [163] |
a An infection prevalence % is calculated by dividing the number of ticks (in each species) reported to test positive for R. amblyommatis by the total number of ticks collected of that species and multiplying by 100. Values are listed in the respective order of the species listed in the species column. b Unable to locate the number of ticks infected in publication. c Unable to report infection prevalence % as not all positive tick samples were sequenced in this study. d This value is an average infection prevalence over a two-year period. e The publication did not specify the collection type. f The total number of ticks collected for each species not reported in the study. g Unable to calculate infection prevalence % with the information given in the study.
4. Distribution and Spread of Rickettsia amblyommatis
4.1. Tick Vectors
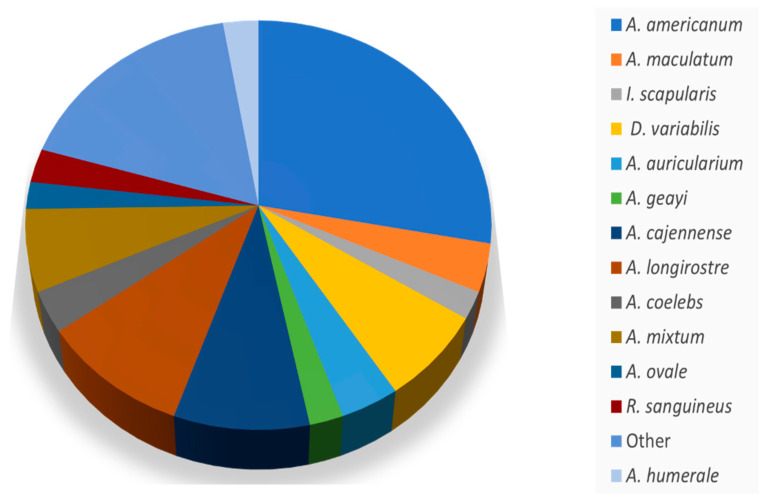
Rickettsia amblyommatis was reported in 34 species of ticks globally, with the majority within the genus Amblyomma. Figure 2 illustrates the proportion of each species of tick infected with R. amblyommatis reported in the literature. Amblyomma spp. made up about 83% of the ticks reported to be infected with R. amblyommatis (Figure 2). Through this literature search, A. americanum was found to be the most common species of tick infected with R. amblyommatis, making up about 27.8% of the reported tick species; A. americanum populations infection rates ranged from 1 to 90% (Table 1) [40,47,48,50,51,58,59,60,63,65,66,69,70,71,75,81,82,83,85,92,93,164]. Studies of the microbiome of ticks have found R. amblyommatis to be present in A. americanum and A. maculatum, specifically finding R. amblyommatis to be the most common member of Rickettsiales present within the lone star tick [164,165].
Figure 2.
A pie graph of the species of tick reported infected with Rickettsia amblyommatis. The legend labeled as “other” included species that were only seen reported in 1–3 instances. These species were as follows: A. breviscutatum, A. calcaratum, A. dubitatum, A. hadanii, A. humerale, A. inornatum, A. neumanni, A. oblongoguttatum, A. pacae, A. parvum, A. pseudoconcolor, A. rotundatum, A. tonelliae, A. varium, D. nitens, H. anatolicum, H. juxtakochi, Hyalomma dromedarii, Ornithodoros sp., I. tasmani, and R. microplus.
Amblyomma americanum is a human-biting tick and competent vector of the causative agents of RMSF, Human Monocytic Ehrlichiosis, tularemia, and heartland virus, and it is more recently known to cause a meat allergy in humans [45,166,167]. While A. americanum is native to the Southeastern United States, this tick is found to be significantly expanding in geographic range, perhaps due to a combination of its generalist tendencies and changing climatic conditions, which will likely further escalate the rise in tick-borne diseases [13,46,168,169,170,171]. This northward expansion has been so successful that A. americanum is now the most abundant species of tick in Long Island, New York [46,172,173,174]. This expansion and growth in populations could lead to shifts in disease prevalence by the possible displacement of other species of tick [80]. Due to A. americanum’s aggressive nature, successful expansion, and high rate of R. amblyommatis infection, it has been predicted that the number of infections of R. amblyommatis in people would increase with time [1,9,45,46,47,168]. However, in clinical settings, there is a lack of Rickettsia species-specific serological testing making it unclear if this prediction is occurring [34]. Amblyomma longirostre was the 2nd most common species of tick found to be infected with R. amblyommatis, making up about 10% of the infected species of tick reported. This species of tick has a geographic range from southern Mexico to Argentina with a wide distribution throughout Brazil [175].
Past studies have shown that ticks that are infected with a pathogen can experience changes in behavior, physiology, and survivability [176,177,178,179]. When a tick is infected with R. amblyommatis, the bacteria can be found in the ovaries, midgut, and salivary glands [9,180,181,182,183]. Ticks infected with R. amblyommatis displayed changes in their host-seeking behavior, such as spending less time questing compared to uninfected ticks [50,51]. It is unclear how this will affect the transmission dynamics and spread of R. amblyommatis. It is possible that infection with R. amblyommatis could cause a disruption in water balance dynamics in A. americanum, making ticks more susceptible to desiccation and preventing them from spending as much time host-seeking [51,177,184,185].
4.2. Geographic Range
In the USA, R. amblyommatis has a wide geographic range, being identified in ticks as far south as Florida, as far west as Kansas, and as far north as New York [47,65] (Figure 1; Table 1). Outside of the United States, R. amblyommatis was detected in Brazil, Argentina, Australia, Belize, Chile, Panama, Colombia, Costa Rica, Cuba, Mexico, Nicaragua, Honduras, Paraguay, Pakistan, French Guiana, and El Salvador [97,102,103,110,111,118,126,141,142,147,149,150,153,156,159,160,163,186] (Figure 1; Table 1). In Table 1, the geographic range of R. amblyommatis for different tick species and the percentage infected in the population sampled are summarized. Additionally, Bermudez and Troyo (2018) concluded that this species was the most common rickettsial species in Central America [187].
In North Carolina, USA, it was concluded that R. amblyommatis is the most common rickettsial exposure that humans experience after being bitten by a lone star tick [40]. These data give validity to the suggestion that “R. amblyommatis likely represents the most prevalent and widely distributed SFG rickettsial species in the Americas” [38]. There are several plausible explanations for the widespread distribution of R. amblyommatis; however, one possible factor explaining the geographic expansion of R. amblyommatis is likely the resurgence and expansion of white-tailed deer populations; this mammal is the preferred host of A. americanum [45,48,188,189]. Since A. americanum is the most frequent carrier of R. amblyommatis, movement by deer may have led to the geographic expansion of R. amblyommatis. Ticks are considered both the reservoir and the vector for R. amblyommatis which causes quicker and further spread of this spotted fever species as it does not have to depend on hosts to proliferate [27,55,131,189,190] and, indeed, the geography of tick-borne rickettsioses such as R. amblyommatis, may be mainly based on the distribution of the vector tick species [131,190]. Another aspect that could be helping fuel this spread could be Amblyomma spp.’s generalist tendencies when finding a host, increasing their likelihood of survival by finding a host quickly and moving to the next life stage [191].
4.3. Hosts of Rickettsia amblyommatis-Infected Ticks
Workers in the majority of field studies that have detected R. amblyommatis in tick populations have collected unfed host-seeking ticks while dragging or flagging. However, in some cases, ticks were collected from wild or domestic animals. These data provide some information about possible vertebrate reservoir hosts of R. amblyommatis and could help determine the geographic distribution of this Rickettsia species. While some tick-borne bacterial pathogens have known reservoirs, R. amblyommatis does not; as stated earlier, some have hypothesized that there is no vertebrate reservoir [55,189]. For example, Apperson et al. (2008) reported white-tailed deer to be negative for antibodies to R. amplyommii, suggesting deer are not becoming infected with this rickettsial species by lone star ticks [189]. We have compiled a list of all of the animals found with feeding ticks infected with R. amblyommatis (Table 1). This list includes a wide variety of animals, with the most common including humans, wild birds, dogs, horses, deer, and others (Table 1). Birds in particular play an important role in tick-borne diseases by spreading pathogenic bacteria over long distances to new areas [122,147,192,193]. Studies on infected ticks feeding on birds have the potential to explain some of the distribution patterns of R. amblyommatis. In a study carried out by Dolz et al. [147], most R. amblyommatis-infected ticks were found on resident passerine birds that did not migrate. However, one R. amblyommatis-infected tick was found on Catharus ustulatus, a thrush that migrates far distances such as from the USA to Argentina. This finding reveals that migrating birds could potentially play a role in the dispersion of R. amblyommatis over long distances. Additionally, Budachetri et al. [194] investigated the microbiome of birds and the ticks infesting them and did not find similarities between the microbiomes, leading them to conclude that migratory birds do not act as a reservoir host for R. amblyommatis but rather could possibly play a role as a means of dispersal for ticks and tick-borne pathogens. Mukherjee et al. [193], who conducted a study on exotic ticks infesting migrating songbirds, found these ticks to harbor high levels of Rickettsia spp. including R. amblyommatis and concluded that it is likely that birds can transport these ticks and tick-borne pathogens long distances.
5. Pathogenicity
There has long been conflicting information on whether R. amblyommatis is pathogenic to mammals. In 1981, Burgdorfer was unable to create rickettsial disease in guinea pigs when experimentally infected with R. amblyommatis; however, he found that this infection caused mild symptoms in meadow voles (Microtus pennsylvanicus) [55]. Despite that, the author concluded that R. amblyommatis was not pathogenic to humans due to the lack of symptoms such as a rash, headache, or fever reported by people in areas where R. amblyommatis tick infection prevalence was high. Since then, more studies have been conducted that have indicated that R. amblyommatis could induce illness in mammals. For example, mice that were intravenously infected with R. amblyommatis were found to have manifested mild disease, showing clinical symptoms such as weight loss [9]. However, it was seen that R. amblyommatis displayed an attachment deficiency to microvascular endothelial cells resulting in a slow growth rate, suggesting that mice would require high titers of R. amblyommatis to become infected and manifest symptoms of disease [9]. Similarly, Snellgrove et al. [195] found that when guinea pigs were inoculated with R. amblyommatis, some of the guinea pigs developed fever, orchitis, and dermatitis. Rivas et al. [196] found that when guinea pigs were inoculated with R. amblyommatis, the guinea pigs experienced an immune response in the form of antibody development, and two out of six of the animals displayed testicular alterations; however, no fever, weight loss, or other signs of infection were exhibited. Levin et al. [180] reported that guinea pigs developed a disseminated infection when fed upon by ticks infected with R. amblyommatis. Rickettsia rickettsii has also been shown to have highly varied levels of virulence in animal models; therefore, it is not surprising that this is the case with R. amblyommatis [9,197,198]. It is also possible that these differences in observed pathogenicity in guinea pigs could be due to varied strains of R. amblyommatis being used in the experiments [9].
While most researchers did not conduct serological testing on animals with attached ticks, there were some exceptions as well as studies on animals artificially infected with R. amblyommatis to evaluate transmission potential. Some studies did not report any clinical symptoms but were able to demonstrate the transmission of R. amblyommatis from infected ticks to the animals by detecting seroactivity, such as antibody titers to R. amblyommatis in rural dogs (Canis familiaris), rabbits (Oryctolagus cuniculus), white-eared possums (Didelphis albiventris), the black rat (Rattus rattus), and R. amblyommatis DNA was found in a single case in the blood of a dog [84,114,131,133,134,146,186,199]. The majority of the results from these mammal studies show a consistent pattern that supports the premise that R. amblyommatis may cause a self-limiting mild febrile illness in mammals and humans, with immune-compromised individuals being particularly vulnerable to infection with this pathogen [9,196].
5.1. Rickettsia amblyommatis in Humans
Little information is available on cases of R. amblyommatis infection in humans. While there are increasing numbers of cases of RMSF-like illnesses, there is a lack of detection of R. rickettsii in tick surveillance studies, suggesting that these illnesses are associated with the expanding range of A. americanum and possibly the transmission of R. amblyommatis [46,80]. Rickettsia amblyommatis being a prevalent bacterium does not necessarily prove that this species is causing disease in humans; however, studies mentioned previously have implicated that infection with R. amblyommatis is correlated with symptoms of disease. For example, one human patient was found to have a rash at a tick bite site, and PCR testing on the tick found it to be infected with R. amblyommatis, making this the first known association of R. amblyommatis with a rash [52]. The sequencing data obtained had an identical match to R. amblyommatis, accession number EF063690 [52]. Billeter et al. [52] discussed a situation where soldiers became ill with febrile symptoms after working in A. americanum-infested sites and stated that serological evidence indicated that infection with R. amblyommatis was the possible cause. In Georgia, USA, twelve residents experiencing tick bites met the criteria for a possible tick-borne illness by having ticks attached for 6 h or more and manifested clinical symptoms of a tick-borne illness after a 4-d incubation [53]. These residents obtained PCR testing of their attached ticks and eight were found to be infected with R. amblyommatis. Two of these individuals who had an R. amblyommatis-infected tick bite reported a bulls-eye rash (erythema migrans) [53]. However, these individuals had multiple ticks attached to them, and it could not be determined which tick was originally at the site of the rash. In North Carolina, USA, outdoor workers are experiencing an increased risk of tick-borne infections; in one serologic study, seroconversions to R. amblyommatis were demonstrated, indicating infection, but no symptoms were recorded in the workers [200]. While there have not been any cases where R. amblyommatis was isolated from human patients, serological evidence indicates that this species of Rickettsia could be the cause of human illnesses displayed as RMSF-like symptoms [9].
Apperson et al. [189] collected ticks in North Carolina, USA, where human cases of RMSF were high. The collected ticks were molecularly tested for bacterial pathogens and 11 out of 25 A. americanum pools were found to be positive for R. amblyommatis [189]. Human patients from the same county that were presumptively diagnosed with a tick-borne illness were serologically tested, and three out of six patients were diagnosed as probable RMSF cases showing a greater increase in IgG-class antibody titers between paired acute and convalescent sera to R. amblyommatis antigens but not to R. rickettsii antigens [189]. These results suggest that human cases of spotted fever rickettsiosis diagnosed as RMSF may actually be experiencing an infection with R. amblyommatis. The authors felt that further investigations were needed into the pathogenicity of R. amblyommatis in humans. Other studies have also suggested that R. amblyommatis is a human pathogen causing misdiagnoses with other rickettsial spotted fever illnesses such as RMSF [47,201,202].
The studies that have been discussed show that it is possible that R. amblyommatis is pathogenic and can result in clinical symptoms in humans and animals. However, an infection with this pathogen may result in a minor, self-limiting illness in most individuals, especially those who are immune compromised [9,196]. It is also worth noting that when attempting to diagnose rickettsial infections, there may be confounding effects as all SFG rickettsia induce cross-reading antibodies [35]. With that in mind, previous infection with R. amblyommatis could be mistakenly diagnosed as RMSF during serological testing. Another hypothesis is that simultaneous infection with R. amblyommatis and other spotted fever group rickettsiae species would result in a lack of clinical symptoms due to this coinfection providing cross-immunity [145,147]. Other species of Rickettsia have overlapping geographic ranges with R. amblyommatis, such as R. parkeri, which is considered pathogenic to humans [203]. This could result in issues during diagnosis. While there is serological confirmation of ticks infected with R. amblyommatis that have bitten humans, there is still no direct evidence that R. amblyommatis may cause human infection.
5.2. Coinfection Effects and Inhibition
Over 25 years ago, Telford et al. [204] warned of the unique impact coinfections could have on public health with a growing number of highly widespread diverse tick-borne pathogens. With A. americanum experiencing a markedly expanding geographic range, this could affect the likelihood of coinfections. Recent studies have shown that when R. rickettsii (RMSF) is coinfected with R. amblyommatis, the latter may act as a sort of protection, lowering the severity of RMSF through an elicited immune response. Blanton et al. [31] found that guinea pigs who were initially inoculated with R. amblyommatis did not become ill when exposed to R. rickettsii but guinea pigs without previous exposure to R. amblyommatis did become ill from R. rickettsii. This study provided evidence for the potential protective role that R. ambyommatis plays in the epidemiology of RMSF. A similar finding was reported by Wright et al. [49], where A. americanum was infected with R. amblyommii and was less likely to develop an R. parkeri infection when feeding alongside an R. parkeri-infected A. maculatum. Additionally, it was seen that R. amblyommatis-infected A. americanum were less likely to become infected nor maintain an infection of R. parkeri [49]. These studies show that it is likely that R. amblyommatis is displaying a form of rickettsial exclusion, making coinfection with another rickettsial species less likely [55,139]. These findings suggest that an increase in infection prevalence of R. amblyommatis in ticks might decrease cases of RMSF. Interestingly, after two decades of increasing cases of RMSF, in 2018 and 2019 there was a slight decrease in reported cases of RMSF [34]. Similar protective effects when R. amblyommatis is coinfected with other Rickettsia species might also occur; A. americanum, the main transmitter of R. amblyommatis, also transmits other pathogens [205]. Investigations into the effects of R. amblyommatis coinfection with other tick-borne pathogens affecting virulence, transmissibility, and clinical symptoms in hosts are clearly warranted.
6. Phylogenetic Analysis
The cultivation of Rickettsia species can vary depending on the cell line and culture system used. Sayler et al. [59] found that when culturing tick-borne organisms, it was best to use the cell lines acquired from the tick vector itself. Rickettsia amblyommatis has been propagated in the past in tick cell lines, mosquito cell lines, Vero cells, tissue cells, chicken fibroblast, primary embryonated chicken eggs, and the HUVEC line [38,59,69,135,206]. Karpathy et al. [38] established a pure culture of strain WB-8-2T (=CRIRC RAM004T=CSURP2882T) and assigned it as the type strain for R. amblyommatis. Prior to this, the species was isolated from A. americanum by Stothard et al. [44]. It was seen that this isolate was similar to other species of Rickettsia but proved to be unique through the analysis of the 17 kDa antigen gene [38]. The genome of R. amblyommatis of the strain GAT-3OV has been sequenced and submitted under the accession number NC_017028. The phylogenetic analysis completed by Karpathy et al. [38] was concatenated using five gene regions (rrs, gltA, sca0, sca5, and sca4) and showed that the most closely related Rickettsia species to R. amblyommatis were R. japonica and R. raoultii.
Past studies have hypothesized that various strains of R. amblyommatis could be genetically independent, with differences evolving based on the tick species and geographic location [99,190]. Dolz et al. [147] found that Costa Rican strains of R. amblyommatis showed intraspecific variation and found high associations with strains from some South American countries. With that in mind, we sought to create a phylogenetic tree of the R. amblyommatis sequences that were present in the NCBI database to compare strains and investigate the relationship between strains, location, and tick species. We created two trees, one that focused on the gene targeting the outer membrane protein A (ompA) and a second targeting outer membrane protein B (ompB). Sequences focusing on these two gene regions were selected as they have been noted to be polymorphic, with ompB being suitable for analyzing intraspecific differences in R. amblyommatis [190]. The methods involved in the creation of the phylogenetic trees can be seen in the Materials and Methods section.
In total, there were 104 sequences identified for ompA; however, 25 (24.04%) were not included due to their small size; only sequences greater than 406 base pairs were included in the analysis. The pairwise comparison of ompA sequences revealed similarity values between 97.27% and 100% among strains. For the analysis of ompB, 19 sequences were incorporated, and only sequences greater than 600 base pairs were included for a total of 618 base pairs in the final tree. The pairwise comparison of ompB sequences revealed similarity values between 98.2% and 100% among strains.
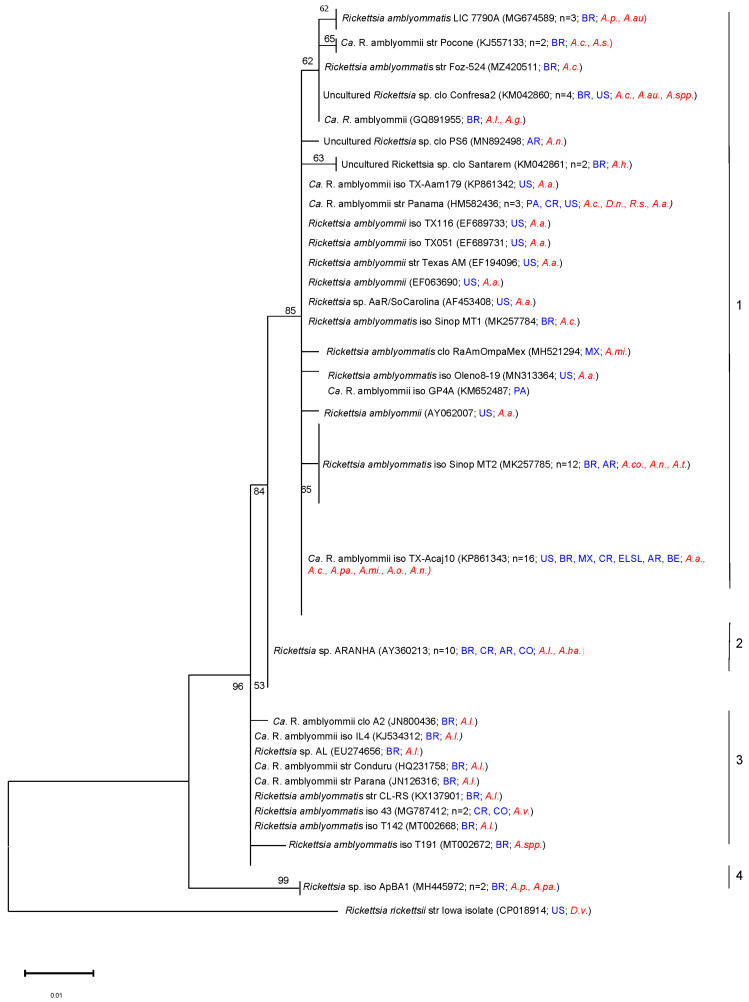
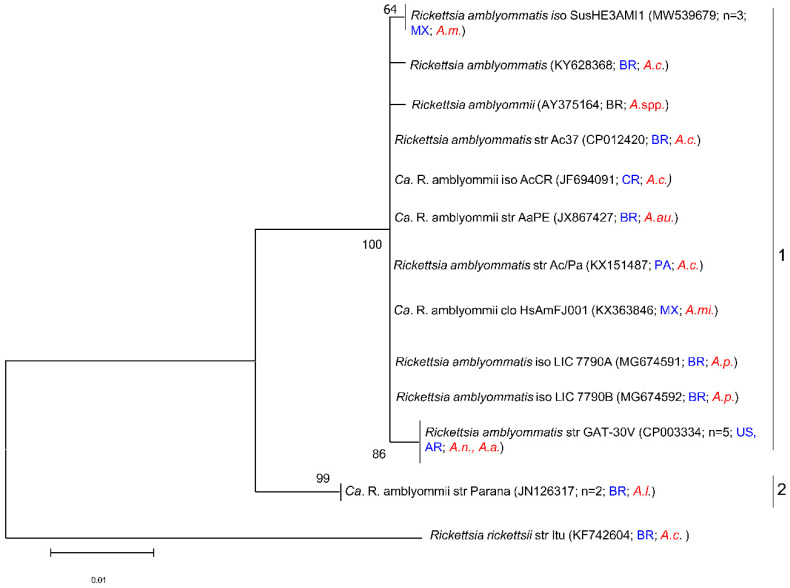
Phylogenetic analysis based on ompA gene sequences with maximum likelihood revealed four major branches (groups) among the R. amblyommatis strains (Figure 3). Group 1 consisted of 56 sequences, group 2 comprised ten strains of R. amblyommatis, group 3 contained ten sequences of R. amblyommatis, and group 4 had two sequences. The ompA phylogenetic analysis showed that R. amblyommatis did not display cluster organization for clusters 1,2, and 4 but did for cluster 3. Cluster 3 appears to be organized by tick species and geographic origin of the sequences where most of the sequences came from Brazil, with two being from Costa Rica and Colombia, and the majority of the sequences were obtained from A. longirostre. The lack of cluster organization in the other clusters could be due to the sequence length in this analysis (Figure 3). For example, in group 1 (N = 56), R. amblyommatis (Aa) sequences were identified to include as many as 14 different tick species from over eight different countries. Phylogenetic analysis of the ompB gene formed two groups (Figure 4). Group 1 contains 17 sequences and group 2 contains two sequences. These clusters do not appear to be organized by location or species of tick.
Figure 3.
Phylogenetic tree of published sequences and reports of Rickettsia amblyommatis in ticks. The analyses were based on the sequences of the ompA gene region of Rickettsia amblyommatis within 406 bp obtained from NCBI BLAST. This tree shows a collapsed version incorporating a total of 79 nucleotide sequences (n shows the total number of sequences included in that group). The phylogenetic analysis was completed using a maximum likelihood method on the Kimura 2-parameter model (ML; bootstrap replicates: 1000). This tree is collapsed with nodes organized by sequence differences of 0.001. Instances in which publications reported the species as “Rickettsia spp.” but indicated in the publication that the species was R. amblyommatis were included in this analysis. The GenBank accession numbers are given in parentheses. Scale bars indicate the number of substitutions per nucleotide position. The Rickettsia rickettsii Iowa isolate (CP018914) was included as an outgroup. Tick species included in this tree are as follows: A auricularium (A.au.), A. cajennense (A.c.), A. coelebs (A.co.), A. geayi (A.g.), A. hadanii (A.ha.), A. humerale (A.h.), A. longirostre (A.l.), A. americanum (A.a.), A. mixtum (A.mi.), A. neumanni (A.n.), A. oblongoguttatum (A.o.), A. pacae (A.pa.), A. parvum (A.par.), A. pseudoconcolor (A.p.), A. sculptum (A.s.), Amblyomma spp. (A.spp.), A. varium (A.v.), D. nitens (D.n.), D. variabilis (D.v.), and R. sanguineus (R.s.). The countries included in this tree are as follows: Brazil (BR), United States of America (US), Mexico (MX), Panama (PA), Argentina (AR), Costa Rica (CR), Belize (BE), El Salvador (ELSL), and Colombia (CO).
Figure 4.
Phylogenetic tree of published sequences and reports of Rickettsia amblyommatis in ticks. The analyses were based on 20 partial sequences of the ompB gene region of Rickettsia amblyommatis within 618 bp obtained from NCBI BLAST. The phylogenetic analysis was completed using a maximum likelihood method on the Kimura 2-parameter model (ML; bootstrap replicates: 1000). This tree is collapsed with nodes organized by sequence differences of 0.001 (n shows the total number of sequences included in that group). Instances in which papers reported the species as “Rickettsia spp.” but indicated in the publication that the species was R. amblyommatis were included in this analysis. The GenBank accession numbers are given in parentheses. Scale bars indicate the number of substitutions per nucleotide position. This phylogenetic tree was created using MEGA11. Tick species included in this tree are as follows: A. americanum (A.a.), A auricularium (A.au.), A. cajennense (A.c.), A. longirostre (A.l.), A. maculatum (A.m.), A. mixtum (A.mi.), A. neumanni (A.n.), A. pseudoconcolor (A.p.), and Amblyomma spp. (A.spp.). The countries included in this tree are as follows: Brazil (BR), the United States of America (US), Panama (PA), Argentina (AR), Mexico (MX), and Costa Rica (CR).
7. Conclusions and Future Directions
While there is still much that is unknown about R. amblyommatis, through the compilation of published work on this topic, we can see that some peer-reviewed studies have found R. amblyommatis to be mildly pathogenic to mammals and humans, that it influences the virulence of other pathogens when coinfected, and that there is intraspecific variation between strains of this pathogen. However, overall, there are inconsistencies, with some studies not finding proof of pathogenicity and others finding symptoms of disease associated with R. amblyommatis. Disease symptoms from infection have been seen in humans and laboratory animals; however, some laboratory challenge studies could not produce similar findings. Rickettsia amblyommatis’s status as a pathogen needs to be verified through further testing.
There remain many questions about R. amblyommatis, which could lead to productive research. One of the most important gaps in the knowledge is how coinfections with R. amblyommatis affect the virulence and the symptoms caused by coinfection with pathogens other than R. rickettsii. This could reveal if R. amblyommatis consistently diminishes the effects of other pathogens in coinfection or if this is only the case with R. rickettsii. It is also possible that a previous infection with R. amblyommatis could elicit antibodies that diminish the pathogenic effects of other SFG rickettsiae. Current common serological testing available in clinical settings lacks the resolution to detect the different SFG rickettsias, which prevents further understanding of the effects and distribution of R. amblyommatis in humans [34,201]. Studying the various strains of R. amblyommatis could elucidate if the genetic variability between the different strains leads to differences in the virulence or symptoms caused by each strain. Future studies are required that culture R. amblyommatis from different geographic regions and hosts as well as, elucidate the whole genome to characterize different isolates. This may lead to a better understanding of the diversity of R. amblyommatis strains, and perhaps their virulence. This research will facilitate the development of more specific pathogen-specific diagnostics.
Acknowledgments
The authors would also like to acknowledge the Department of Entomology and Plant Pathology at NCSU for the support of Elise A. Richardson through a graduate research assistantship.
Author Contributions
Conceptualization, E.A.R., R.M.R., C.S.A. and L.P.; methodology, E.A.R. and L.P.; validation, E.A.R., R.M.R. and L.P.; formal analysis, E.A.R., R.M.R. and L.P.; investigation, E.A.R. and L.P.; data curation, E.A.R.; writing—original draft preparation, E.A.R.; writing—review and editing, E.A.R., R.M.R., C.S.A. and L.P.; supervision, R.M.R. and L.P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
E.A.R. was supported by a grant from the Department of the Army, US Army Contracting Command, Aberdeen Proving Ground, Natick Contracting Division, Ft Detrick MD under a Deployed Warfighter Protection (DWFP) Program Grant W911QY1910003 and W911SR221005 awarded to R.M.R. R.M.R. was also supported by the NC Ag. Res. Station.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Sonenshine D.E. Range expansion of tick disease vectors in North America: Implications for spread of tick-borne disease. Int. J. Environ. Res. Public Health. 2018;15:478. doi: 10.3390/ijerph15030478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jongejan F., Uilenberg G. The global importance of ticks. Parasitology. 2004;129:S3–S14. doi: 10.1017/S0031182004005967. [DOI] [PubMed] [Google Scholar]
- 3.Rosenberg R., Lindsey N.P., Fischer M., Gregory C.J., Hinckley A.F., Mead P.S., Paz-Bailey G., Waterman S.H., Drexler N.A., Kersh G.J., et al. Vital signs: Trends in reported vectorborne disease cases—United States and territories, 2004–2016. Morb. Mortal. Wkly. Rep. 2018;67:496. doi: 10.15585/mmwr.mm6717e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), D. of V.-B.D. DVBD Tickborne Disease Surveillance Data Summary. [(accessed on 30 December 2022)]; Available online: https://www.cdc.gov/ticks/data-summary/index.html.
- 5.Madison-antenucci S., Kramer L.D., Gebhardt L.L. Emerging tick-borne diseases. Clin. Microbiol. Rev. 2020;33:e00083-18. doi: 10.1128/CMR.00083-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dantas-Torres F. Rocky Mountain spotted fever. Lancet Infect. Dis. 2007;7:724–732. doi: 10.1016/S1473-3099(07)70261-X. [DOI] [PubMed] [Google Scholar]
- 7.Piesman J., Eisen L. Prevention of tick-borne diseases. Annu. Rev. Entomol. 2007;53:323–343. doi: 10.1146/annurev.ento.53.103106.093429. [DOI] [PubMed] [Google Scholar]
- 8.Eisen R.J., Kugeler K.J., Eisen L., Beard C.B., Paddock C.D. Tick-borne zoonoses in the United States: Persistent and emerging threats to human health. ILAR J. 2017;58:319–335. doi: 10.1093/ilar/ilx005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yen W.Y., Stern K., Mishra S., Helminiak L., Sanchez-Vicente S., Kim H.K. Virulence potential of Rickettsia amblyommatis for spotted fever pathogenesis in mice. Pathog. Dis. 2021;79:24. doi: 10.1093/femspd/ftab024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lyme Disease|CDC. [(accessed on 20 May 2022)]; Available online: https://www.cdc.gov/lyme/index.html.
- 11.Eisen L. Climate change and tick-borne diseases: A research field in need of long-term empirical field studies. Int. J. Med. Microbiol. 2008;298:12–18. doi: 10.1016/j.ijmm.2007.10.004. [DOI] [Google Scholar]
- 12.Rocklöv J., Dubrow R. Climate change: An enduring challenge for vector-borne disease prevention and control. Nat. Immunol. 2020;21:479–483. doi: 10.1038/s41590-020-0648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bouchard C., Dibernardo A., Koffi J., Wood H., Leighton P.A., Lindsay L.R. Increased risk of tick-borne diseases with climate and environmental changes. Can. Commun. Dis. Rep. 2019;45:83–89. doi: 10.14745/ccdr.v45i04a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parola P., Paddock C.D., Raoult D. Tick-borne rickettsioses around the world: Emerging diseases challenging old concepts. Clin. Microbiol. Rev. 2005;18:719–756. doi: 10.1128/CMR.18.4.719-756.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raoult D. A new Rickettsial disease in the United States. Clin. Infect. Dis. 2004;38:812–813. doi: 10.1086/381896. [DOI] [PubMed] [Google Scholar]
- 16.Fournier P.E., Raoult D. Current knowledge on phylogeny and taxonomy of rickettsia spp. Ann. N. Y. Acad. Sci. 2009;1166:1–11. doi: 10.1111/j.1749-6632.2009.04528.x. [DOI] [PubMed] [Google Scholar]
- 17.Tahir D., Socolovschi C., Lou Marié J., Ganay G., Berenger J.M., Bompar J.M., Blanchet D., Cheuret M., Mediannikov O., Raoult D., et al. New Rickettsia species in soft ticks Ornithodoros hasei collected from bats in French Guiana. Ticks Tick. Borne. Dis. 2016;7:1089–1096. doi: 10.1016/j.ttbdis.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 18.Roucher C., Mediannikov O., Diatta G., Trape J.F., Raoult D. A new Rickettsia species found in fleas collected from human dwellings and from domestic cats and dogs in senegal. Vector-Borne Zoonotic Dis. 2012;12:360–365. doi: 10.1089/vbz.2011.0734. [DOI] [PubMed] [Google Scholar]
- 19.Tamura K., Stecher G., Kumar S. MEGA11: Molecular evolutionary genetics analysis version 11. Mol. Biol. Evol. 2021;38:3022–3027. doi: 10.1093/molbev/msab120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parola P., Paddock C.D., Socolovschi C., Labruna M.B., Mediannikov O., Kernif T., Abdad M.Y., Stenos J., Bitam I., Fournier P.E., et al. Update on tick-borne rickettsioses around the world: A geographic approach. Clin. Microbiol. Rev. 2013;26:657–702. doi: 10.1128/CMR.00032-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gunasekaran K., Bal D., Varghese G.M. Scrub Typhus and Other Rickettsial Infections. Indian J. Crit. Care Med. 2021;25:S138. doi: 10.5005/jp-journals-10071-23841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merhej V., Raoult D. Rickettsial evolution in the light of comparative genomics. Biol. Rev. 2011;86:379–405. doi: 10.1111/j.1469-185X.2010.00151.x. [DOI] [PubMed] [Google Scholar]
- 23.Igolkina Y., Nikitin A., Verzhutskaya Y., Gordeyko N., Tikunov A., Epikhina T., Tikunova N., Rar V. Multilocus genetic analysis indicates taxonomic status of “Candidatus Rickettsia mendelii” as a separate basal group. Ticks Tick. Borne. Dis. 2023;14:102104. doi: 10.1016/j.ttbdis.2022.102104. [DOI] [PubMed] [Google Scholar]
- 24.Abdad M.Y., Stenos J., Graves S. Rickettsia felis, an emerging flea-transmitted human pathogen. Emerg. Health Threat. 2017;4:7168. doi: 10.3402/ehtj.v4i0.7168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fournier P.-E., Ndihokubwayo J.-B., Guidran J., Kelly P.J., Raoult D. Human pathogens in body and head lice. Emerg. Infect. Dis. 2002;8:1515–1518. doi: 10.3201/eid0812.020111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Santibáñez P., Palomar A.M., Portillo A., Sonia S., Oteo J.A. The role of chiggers as human pathogens. An Overv. Trop. Dis. 2015;1:173–202. doi: 10.5772/61978. [DOI] [Google Scholar]
- 27.Socolovschi C., Mediannikov O., Raoult D., Parola P. The relationship between spotted fever group Rickettsiae and Ixodid ticks. Vet. Res. 2009;40:34. doi: 10.1051/vetres/2009017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eremeeva M.E., Dasch G.A. Challenges posed by tick-borne rickettsiae: Eco-epidemiology and public health implications. Front. Public Health. 2015;3:55. doi: 10.3389/fpubh.2015.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.List of Prokaryotic Names with Standing in Nomenclature- Genus Rickettsia. [(accessed on 30 December 2022)]. Available online: https://lpsn.dsmz.de/genus/rickettsia.
- 30.Parola P., Raoult D. Ticks and tickborne bacterial diseases in humans: An emerging infectious threat. Clin. Infect. Dis. 2001;32:897–928. doi: 10.1086/319347. [DOI] [PubMed] [Google Scholar]
- 31.Blanton L.S., Mendell N.L., Walker D.H., Bouyer D.H. “Rickettsia amblyommii” induces cross protection against lethal rocky mountain spotted fever in a guinea pig model. Vector-Borne Zoonotic Dis. 2014;14:557–562. doi: 10.1089/vbz.2014.1575. [DOI] [PubMed] [Google Scholar]
- 32.Niebylski M.L., Schrumpf M.E., Burgdorfer W., Fischer E.R., Gage K.L., Schwan T.G. Rickettsia peacockii sp. nov., a new species infecting wood ticks, Dermacentor andersoni, in western Montana. Int. J. Syst. Bacteriol. 1997;47:446–452. doi: 10.1099/00207713-47-2-446. [DOI] [PubMed] [Google Scholar]
- 33.Snowden J., Simonsen K.A. Rickettsia Rickettsiae. In StatPearls [Internet]. Treasure Island (FL) [(accessed on 30 December 2022)];2022 Available online: https://www.ncbi.nlm.nih.gov/books/NBK430881/
- 34.Epidemiology and Statistics|Rocky Mountain Spotted Fever (RMSF)|CDC. [(accessed on 20 July 2022)]; Available online: https://www.cdc.gov/rmsf/stats/index.html.
- 35.Goddard J. Historical and recent evidence for close relationships among Rickettsia parkeri, R. conorii, R. africae, and R. sibirica: Implications for rickettsial taxonomy. J. Vector Ecol. 2009;34:238–242. doi: 10.1111/j.1948-7134.2009.00032.x. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention Other Spotted Fever Group Rickettsioses. [(accessed on 30 December 2022)]; Available online: https://www.cdc.gov/otherspottedfever/#read.
- 37.Cragun W.C., Bartlett B.L., Ellis M.W., Hoover A.Z., Tyring S.K., Mendoza N., Vento T.J., Nicholson W.L., Eremeeva M.E., Olano J.P., et al. The expanding spectrum of eschar-associated rickettsioses in the United States. Arch. Dermatol. 2010;146:641–648. doi: 10.1001/archdermatol.2010.48. [DOI] [PubMed] [Google Scholar]
- 38.Karpathy S.E., Slater K.S., Goldsmith C.S., Nicholson W.L., Paddock C.D. Rickettsia amblyommatis sp. Nov., a spotted fever group Rickettsia associated with multiple species of Amblyomma ticks in North, Central and South America. Int. J. Syst. Evol. Microbiol. 2016;66:5236–5243. doi: 10.1099/ijsem.0.001502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Burgdorfer W., Cooney J.C., Thomas L.A. Zoonotic potential (Rocky Mountain spotted fever and tularemia) in the Tennessee Valley region. II. Prevalence of Rickettsia rickettsi and Francisella tularensis in mammals and ticks from Land between the Lakes. Am. J. Trop. Med. Hyg. 1974;23:109–117. doi: 10.4269/ajtmh.1974.23.109. [DOI] [PubMed] [Google Scholar]
- 40.Lee S., Kakumanu M.L., Ponnusamy L., Vaughn M., Funkhouser S., Thornton H., Meshnick S.R., Apperson C.S. Prevalence of Rickettsiales in ticks removed from the skin of outdoor workers in North Carolina. Parasites Vectors. 2014;7:607. doi: 10.1186/s13071-014-0607-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leydet B.F., Liang F.T. Detection of human bacterial pathogens in ticks collected from Louisiana black bears (Ursus americanus luteolus) Ticks Tick. Borne. Dis. 2013;4:191–196. doi: 10.1016/j.ttbdis.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bermúdez C.S., Zaldívar Y., Domínguez A.L., Hernández M., de Antinori M.E.B., Krawczak F.S. Rickettsia amblyommatis isolated from Amblyomma mixtum (Acari: Ixodida) from two sites in Panama. Ticks Tick. Borne. Dis. 2021;12:101597. doi: 10.1016/j.ttbdis.2020.101597. [DOI] [PubMed] [Google Scholar]
- 43.Ponnusamy L., Garshong R., McLean B.S., Wasserberg G., Durden L.A., Crossley D., Apperson C.S., Roe R.M. Rickettsia felis and other Rickettsia species in chigger mites collected from wild rodents in North Carolina, USA. Microorganisms. 2022;10:1342. doi: 10.3390/microorganisms10071342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stothard D. The Evolutionary History of the Genus Rickettsia as Inferred from 16S and 23S Ribosomal RNA Genes and the 17 Kilodalton Cell Surface Antigen Gene. Ohio State University; Columbus, OH, USA: 1995. [Google Scholar]
- 45.Childs J.E., Paddock C.D. The ascendancy of Amblyomma americanum as a vector of pathogen affecting humans in the United States. Annu. Rev. Entomol. 2003;48:307–344. doi: 10.1146/annurev.ento.48.091801.112728. [DOI] [PubMed] [Google Scholar]
- 46.Dahlgren F.S., Paddock C.D., Springer Y.P., Eisen R.J., Behravesh C.B. Expanding range of Amblyomma americanum and simultaneous changes in the epidemiology of spotted fever group Rickettsiosis in the United States. Am. J. Trop. Med. Hyg. 2016;94:35–42. doi: 10.4269/ajtmh.15-0580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mixson T.R., Campbell S.R., Gill J.S., Ginsberg H.S., Reichard M.V., Schulze T.L., Dasch G.A. Prevalence of Ehrlichia, Borrelia, and Rickettsial agents in Amblyomma americanum (Acari: Ixodidae) collected from nine states. J. Med. Entomol. 2006;43:1261–1268. doi: 10.1603/0022-2585(2006)43[1261:POEBAR]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 48.Jiang J., Yarina T., Miller M.K., Stromdahl E.Y., Richards A.L. Molecular detection of Rickettsia amblyommii in Amblyomma americanum parasitizing humans. Vector-Borne Zoonotic Dis. 2010;10:329–340. doi: 10.1089/vbz.2009.0061. [DOI] [PubMed] [Google Scholar]
- 49.Wright C.L., Sonenshine D.E., Gaff H.D., Hynes W.L. Rickettsia parkeri transmission to Amblyomma americanum by cofeeding with Amblyomma maculatum (Acari: Ixodidae) and potential for spillover. J. Med. Entomol. 2015;52:1090–1095. doi: 10.1093/jme/tjv086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richardson E.A., Taylor C.E., Jabot B., Martin E., Keiser C.N. The effects of habitat type and pathogen infection on tick host seeking behavior. Parasitology. 2021;149:59–64. doi: 10.1017/S0031182021001554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Richardson E.A., Buttrick D.J., Shablin S.A., Jabot B., Taylor C.E., Martin E.M., Keiser C.N. Exploring the effects of pathogen infection on tick behaviour from individuals to populations. Anim. Behav. 2022;186:85–92. doi: 10.1016/j.anbehav.2022.02.004. [DOI] [Google Scholar]
- 52.Billeter S.A., Blanton H.L., Little S.E., Levy M.G., Breitschwerdt E.B. Detection of “Rickettsia amblyommii” in association with a tick bite rash. Vector-Borne Zoonotic Dis. 2007;7:607–610. doi: 10.1089/vbz.2007.0121. [DOI] [PubMed] [Google Scholar]
- 53.Gleim E.R., Garrison L.E., Vello M.S., Savage M.Y., Lopez G., Berghaus R.D., Yabsley M.J. Factors associated with tick bites and pathogen prevalence in ticks parasitizing humans in Georgia, USA. Parasites Vectors. 2016;9:1–13. doi: 10.1186/s13071-016-1408-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Trout R., Dayton Steelman C., Szalanski A.L., Williamson P.C. Rickettsiae in Gulf Coast ticks, Arkansas, USA. Emerg. Infect. Dis. 2010;16:830. doi: 10.3201/eid1605.091314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Burgdorfer W., Hayes S., Thomas L. In: Rickettsiae and Rickettsial Diseases. Burgdorfer W., Anacker R., editors. Academic Press; New York, NY, USA: 1981. [Google Scholar]
- 56.Fryxell R.T.T., Steelman C.D., Szalanski A.L., Billingsley P.M., Williamson P.C. Molecular detection of Rickettsia species within ticks (Acari: Ixodidae) collected from Arkansas United States. J. Med. Entomol. 2015;52:500–508. doi: 10.1093/jme/tjv027. [DOI] [PubMed] [Google Scholar]
- 57.Blanton L.S., Walker D.H., Bouyer D.H. Rickettsiae and Ehrlichiae Within a City Park: Is the Urban Dweller at Risk? Vector Borne Zoonotic Dis. 2014;14:168–170. doi: 10.1089/vbz.2013.1473. [DOI] [PubMed] [Google Scholar]
- 58.De Jesus C.E., Ganser C., Kessler W.H., White Z.S., Bhosale C.R., Glass G.E., Wisely S.M. A survey of tick-borne bacterial pathogens in Florida. Insects. 2019;10:297. doi: 10.3390/insects10090297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sayler K.A., Wamsley H.L., Pate M., Barbet A.F., Alleman A.R. Cultivation of Rickettsia amblyommii in tick cells, prevalence in Florida lone star ticks (Amblyomma americanum) Parasites Vectors. 2014;7:270. doi: 10.1186/1756-3305-7-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ayres B.N., James A.M., Wehtje M.E., Nicholson W.L. Rickettsial agents detected in Ixodid Ticks (Acari: Ixodidae) collected from Sus scrofa (Artiodactyla: Suidae) in Florida and South Carolina. J. Entomol. Sci. 2022;57:351–362. doi: 10.18474/JES21-63. [DOI] [Google Scholar]
- 61.Yabsley M.J., Nims T.N., Savage M.Y., Durden L.A. Ticks and tick-borne pathogens and putative symbionts of black bears (Ursus americanus floridanus) from Georgia and Florida. J. Parasitol. 2009;95:1125–1128. doi: 10.1645/GE-2111.1. [DOI] [PubMed] [Google Scholar]
- 62.Stanley H., Rhodes D.V.L., Wikel S.K., Humberto A., Minervino H. Presence of Rickettsia species in ticks collected from companion animals in northeastern Georgia, United States. Vet.-Sci. 2021;8:37. doi: 10.3390/vetsci8030037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Killmaster L.F., Loftis A.D., Zemtsova G.E., Levin M.L. Detection of bacterial agents in Amblyomma americanum (Acari: Ixodidae) from Georgia, USA, and the use of a multiplex assay to differentiate Ehrlichia chaffeensis and Ehrlichia ewingii. J. Med. Entomol. 2014;51:868–872. doi: 10.1603/ME13225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cleveland C.A., Swanepoel L., Box E.K., De Nicola A., Yabsley M.J. Rickettsia species in ticks collected from wild pigs (Sus scrofa) and Philippine deer (Rusa marianna) on Guam, Marianna Islands, USA. Acta Trop. 2019;194:89–92. doi: 10.1016/j.actatropica.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 65.Berrada Z.L., Goethert H.K., Cunningham J., Telford S.R. Rickettsia rickettsii (Rickettsiales: Rickettsiaceae) in Amblyomma americanum (Acari: Ixodidae) from Kansas. J. Med. Entomol. 2011;48:461–467. doi: 10.1603/ME10130. [DOI] [PubMed] [Google Scholar]
- 66.Fritzen C.M., Huang J., Westby K., Freye J.D., Dunlap B., Yabsley M.J., Schardein M., Dunn J.R., Jones T.F., Moncayo A.C. Infection prevalences of common tick-borne pathogens in adult lone star ticks (Amblyomma americanum) and American dog ticks (Dermacentor variabilis) in Kentucky. Am. J. Trop. Med. Hyg. 2011;85:718. doi: 10.4269/ajtmh.2011.10-0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hecht J.A., Allerdice M.E.J., Dykstra E.A., Mastel L., Eisen R.J., Johnson T.L., Gaff H.D., Varela-Stokes A.S., Goddard J., Pagac B.B., et al. Multistate survey of American dog ticks (Dermacentor variabilis) for Rickettsia species. Vector Borne Zoonotic Dis. 2019;19:652–657. doi: 10.1089/vbz.2018.2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Stromdahl E.Y., Vince M.A., Billingsley P.M., Dobbs N.A., Williamson P.C. Rickettsia amblyommii infecting Amblyomma americanum larvae. Vector-Borne Zoonotic Dis. 2008;8:15–24. doi: 10.1089/vbz.2007.0138. [DOI] [PubMed] [Google Scholar]
- 69.Zhang X., Ren X., Norris D.E., Rasgon J.L. Distribution and infection frequency of ‘Candidatus Rickettsia amblyommii’ in Maryland populations of the lone star tick (Amblyomma americanum) and culture in an Anopheles gambiae mosquito cell line. Ticks Tick. Borne. Dis. 2012;3:38–42. doi: 10.1016/j.ttbdis.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hermance M., Marques Dos Santos R.I., Heinze D., Hausser N., Bouyer D.H., Thangamani S. Detection of Rickettsia amblyommii in ticks collected from Missouri, USA. Emerg. Microbes Infect. 2014;3:e34. doi: 10.1038/emi.2014.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Santanello C., Barwari R., Troyo A. Spotted fever group Rickettsiae in ticks from Missouri. Ticks Tick. Borne. Dis. 2018;9:1395–1399. doi: 10.1016/j.ttbdis.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 72.Hudman D.A., Sargentini N.J. Detection of Borrelia, Ehrlichia, and Rickettsia spp. in ticks in northeast Missouri. Ticks Tick. Borne. Dis. 2016;7:915–921. doi: 10.1016/j.ttbdis.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 73.Castellaw A.H., Showers J., Goddard J., Chenney E.F., Varela-Stokes A.S. Detection of vector-borne agents in lone star ticks, Amblyomma americanum (Acari: Ixodidae), from Mississippi. J. Med. Entomol. 2010;47:473–476. doi: 10.1093/jmedent/47.3.473. [DOI] [PubMed] [Google Scholar]
- 74.Kakumanu M.L., Ponnusamy L., Sutton H., Meshnick S.R., Nicholson W.L., Apperson C.S. Prevalence of Rickettsia species (Rickettsiales: Rickettsiaceae) in Dermacentor variabilis ticks (Acari: Ixodidae) in North Carolina. J. Med. Entomol. 2018;55:1284–1291. doi: 10.1093/jme/tjy074. [DOI] [PubMed] [Google Scholar]
- 75.Smith M.P., Ponnusamy L., Jiang J., Ayyash L.A., Richards A.L., Apperson C.S. Bacterial pathogens in Ixodid ticks from a Piedmont county in North Carolina: Prevalence of Rickettsial organisms. Vector-Borne Zoonotic Dis. 2010;10:939–952. doi: 10.1089/vbz.2009.0178. [DOI] [PubMed] [Google Scholar]
- 76.Duncan K.T., Grant A., Johnson B., Sundstrom K.D., Saleh M.N., Little S.E. Identification of Rickettsia spp. and Babesia conradae in Dermacentor spp. Collected from Dogs and Cats Across the United States. Vector Borne Zoonotic Dis. 2021;12:911–920. doi: 10.1089/vbz.2021.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Egizi A., Gable S., Jordan R.A. Rickettsia spp. Infecting lone star ticks (Amblyomma americanum) (Acari: Ixodidae) in Monmouth County, New Jersey. J. Med. Entomol. 2020;57:974–978. doi: 10.1093/jme/tjz251. [DOI] [PubMed] [Google Scholar]
- 78.Occi J., Egizi A.M., Goncalves A., Fonseca D.M. New Jersey-wide survey of spotted fever group Rickettsia (Proteobacteria: Rickettsiaceae) in Dermacentor variabilis and Amblyomma americanum (Acari: Ixodida: Ixodidae) Am. J. Trop. Med. Hyg. 2020;103:1009–1016. doi: 10.4269/ajtmh.20-0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schulze T.L., Jordan R.A., White J.C., Roegner V.E., Healy S.P. Geographical distribution and prevalence of selected Borrelia, Ehrlichia, and Rickettsia infections in Amblyomma americanum (Acari: Ixodidae) in New Jersey. Source J. Am. Mosq. Control. Assoc. 2011;27:236–244. doi: 10.2987/11-6111.1. [DOI] [PubMed] [Google Scholar]
- 80.Sanchez-Vicente S., Tagliafierro T., Coleman J.L., Benach J.L., Tokarz R. Polymicrobial nature of tick-borne diseases. MBio. 2019;10:e02055-19. doi: 10.1128/mBio.02055-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fitak R.R., Kelly D.J., Daniels M.K., Jiang J., Richards A.L., Fuerst P.A. The prevalence of rickettsial and ehrlichial organisms in Amblyomma americanum ticks collected from Ohio and surrounding areas between 2000 and 2010. Ticks Tick. Borne. Dis. 2014;5:797–800. doi: 10.1016/j.ttbdis.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 82.Kelly D.J., Carmichael J.R., Booton G.C., Poetter K.F., Fuerst P.A. Novel spotted fever group Rickettsiae (SFGR) infecting Amblyomma americanum ticks in Ohio, USA. Ann. N. Y. Acad. Sci. 2005;1063:352–355. doi: 10.1196/annals.1355.058. [DOI] [PubMed] [Google Scholar]
- 83.Small M., Brennan R.E. Detection of Rickettsia amblyommatis and Ehrlichia chaffeensis in Amblyomma americanum inhabiting two urban parks in Oklahoma. Vector-Borne Zoonotic Dis. 2021;21:385–387. doi: 10.1089/vbz.2020.2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Barrett A., Little S.E., Shaw E. “Rickettsia amblyommii” and R. montanensis infection in dogs following natural exposure to ticks. Vector-Borne Zoonotic Dis. 2014;14:20–25. doi: 10.1089/vbz.2013.1325. [DOI] [PubMed] [Google Scholar]
- 85.Moncayo A.C., Cohen S.B., Fritzen C.M., Huang E., Yabsley M.J., Freye J.D., Dunlap B.G., Huang J., Mead D.G., Jones T.F., et al. Absence of Rickettsia rickettsii and occurrence of other spotted fever group Rickettsiae in ticks from Tennessee. Am. J. Trop. Med. Hyg. 2010;83:653. doi: 10.4269/ajtmh.2010.09-0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Trout Fryxell R.T., Hendricks B.M., Pompo K., Mays S.E., Paulsen D.J., Operario D.J., Houston A.E. Investigating the adult Ixodid tick populations and their associated Anaplasma, Ehrlichia, and Rickettsia bacteria at a Rocky Mountain spotted fever hotspot in Western Tennessee. Vector Borne Zoonotic Dis. 2017;17:527–538. doi: 10.1089/vbz.2016.2091. [DOI] [PubMed] [Google Scholar]
- 87.Cohen E.B., Auckland L.D., Marra P.P., Hamer S.A. Avian migrants facilitate invasions of neotropical ticks and tick- borne pathogens into the United States. Appl. Environ. Microbiol. 2015;81:8366–8378. doi: 10.1128/AEM.02656-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hodo C.L., Forgacs D., Auckland L.D., Bass K., Lindsay C., Bingaman M., Sani T., Colwell K., Hamer G.L., Hamer S.A. Presence of diverse Rickettsia spp. and absence of Borrelia burgdorferi sensu lato in ticks in an East Texas forest with reduced tick density associated with controlled burns. Ticks Tick. Borne. Dis. 2020;11:101310. doi: 10.1016/j.ttbdis.2019.101310. [DOI] [PubMed] [Google Scholar]
- 89.Mendell N.L., Reynolds E.S., Blanton L.S., Hermance M.E., Londoño A.F., Hart C.E., Quade B.R., Esterly A.T., Hendrix B.B., Teel P.D., et al. Detection of Rickettsiae, Borreliae, and Ehrlichiae in ticks collected from Walker County, Texas, 2017-2018. Insects. 2019;10:315. doi: 10.3390/insects10100315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Olafson P.U., Buckmeier B.G., May M.A., Thomas D.B. Molecular screening for rickettsial bacteria and piroplasms in ixodid ticks surveyed from white-tailed deer (Odocoileus virginianus) and nilgai antelope (Boselaphus tragocamelus) in southern Texas. Int. J. Parasitol. Parasites Wildl. 2020;13:252–260. doi: 10.1016/j.ijppaw.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Medlin J.S., Cohen J.I., Beck D.L. Vector potential and population dynamics for Amblyomma inornatum. Ticks Tick. Borne. Dis. 2015;6:463–472. doi: 10.1016/j.ttbdis.2015.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mitchell E.A., Williamson P.C., Billingsley P.M., Seals J.P., Ferguson E.E., Allen M.S. Frequency and distribution of Rickettsiae, Borreliae, and Ehrlichiae detected in human-parasitizing ticks, Texas, USA. Emerg. Infect. Dis. 2016;22:312. doi: 10.3201/eid2202.150469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gaines D.N., Operario D.J., Stroup S., Stromdahl E., Wright C., Gaff H., Broyhill J., Smith J., Norris D.E., Henning T., et al. Ehrlichia and spotted fever group rickettsiae surveillance in Amblyomma americanum in Virginia through use of a novel six-plex real-time PCR assay. Vector-Borne Zoonotic Dis. 2014;14:307–316. doi: 10.1089/vbz.2013.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nadolny R.M., Wright C.L., Sonenshine D.E., Hynes W.L., Gaff H.D. Ticks and spotted fever group rickettsiae of southeastern Virginia. Ticks Tick. Borne. Dis. 2014;5:53–57. doi: 10.1016/j.ttbdis.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Miller M.K., Jiang J., Truong M., Yarina T., Evans H., Christensen T.P., Richards A.L. Emerging tick-borne Rickettsia and Ehrlichia at joint base Langley-Eustis, fort Eustis, Virginia. US. Army Med. Dep. J. 2016;3–16:22–28. [PubMed] [Google Scholar]
- 96.Stromdahl E.Y., Jiang J., Vince M., Richards A.L. Infrequency of Rickettsia rickettsii in Dermacentor variabilis removed from humans, with comments on the role of other human-biting ticks associated with spotted fever group Rickettsiae in the United States. Vector Borne Zoonotic Dis. 2011;11:969–977. doi: 10.1089/vbz.2010.0099. [DOI] [PubMed] [Google Scholar]
- 97.Labruna M.B., Pacheco R.C., Nava S., Brandão P.E., Richtzenhain L.J., Guglielmone A.A. Infection by Rickettsia bellii and Candidatus “Rickettsia amblyommii” in Amblyomma neumanni ticks from Argentina. Microb. Ecol. 2007;54:126–133. doi: 10.1007/s00248-006-9180-3. [DOI] [PubMed] [Google Scholar]
- 98.Saracho Bottero M.N., Tarragona E.L., Nava S. Spotted fever group rickettsiae in Amblyomma ticks likely to infest humans in rural areas from northwestern Argentina. Med. Buenos Aires. 2015;6:391–395. [PubMed] [Google Scholar]
- 99.Mastropaolo M., Tarragona E.L., Silaghi C., Pfister K., Thiel C., Nava S. High prevalence of “Candidatus Rickettsia amblyommii” in Amblyomma ticks from a spotted fever endemic region in north Argentina. Comp. Immunol. Microbiol. Infect. Dis. 2016;46:73–76. doi: 10.1016/j.cimid.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 100.Tarragona E.L., Cicuttin G.L., Mangold A.J., Mastropaolo M., Nazarena De Salvo M., Nava S. Rickettsia infection in Amblyomma tonelliae, a tick species from the Amblyomma cajennense complex. Ticks Tick. Borne. Dis. 2015;6:173–177. doi: 10.1016/j.ttbdis.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 101.Saracho-Bottero M.N., Tarragona E.L., Sebastian P.S., Venzal J.M., Mangold A.J., Guglielmone A.A., Nava S. Ticks infesting cattle and humans in the Yungas Biogeographic Province of Argentina, with notes on the presence of tick-borne bacteria. Exp. Appl. Acarol. 2018;74:107–116. doi: 10.1007/s10493-018-0208-4. [DOI] [PubMed] [Google Scholar]
- 102.Vilcins I.M.E., Old J.M., Deane E.M. Detection of a spotted fever group Rickettsia in the tick Ixodes tasmani collected from koalas in Port Macquarie, Australia. J. Med. Entomol. 2008;45:745–750. doi: 10.1093/jmedent/45.4.745. [DOI] [PubMed] [Google Scholar]
- 103.Lopes M.G., Junior J.M., Foster R.J., Harmsen B.J., Sanchez E., Martins T.F., Quigley H., Marcili A., Labruna M.B. Ticks and rickettsiae from wildlife in Belize, Central America. Parasit. Vectors. 2016;9:62. doi: 10.1186/s13071-016-1348-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Polsomboon S., Hoel D.F., Murphy J.R., Linton Y.-M., Motoki M., Robbins R.G., Bautista K., Briceno I., Achee N.L., Grieco J.P., et al. Molecular detection and identification of Rickettsia species in ticks (Acari: Ixodidae) collected from Belize, Central America. J. Med. Entomol. 2017;54:1718–1726. doi: 10.1093/jme/tjx141. [DOI] [PubMed] [Google Scholar]
- 105.Gruhn K.D., Ogrzewalska M., Rozental T., Farikoski I.O., Blanco C., de Souza Freitas L., de Lemos E.R.S., Ribeiro V.M.F. Evaluation of rickettsial infection in free-range capybaras (Hydrochoerus hydrochaeris Linnaeus, 1766) (Rodentia: Caviidae) and ticks (Acari: Ixodidae) in the Western Amazon, Brazil. Ticks Tick. Borne. Dis. 2019;10:981–986. doi: 10.1016/j.ttbdis.2019.04.007. [DOI] [PubMed] [Google Scholar]
- 106.Lima M.A., Universidade Federal do Acre. Martins T.F., Muñoz-Leal S., Guilherme E., Ogrzewalska M., Labruna M.B., Universidade de São Paulo. Cruz/ioc I.O. Ticks and tick-associated spotted fever group Rickettsia from birds in the Southwestern Brazilian Amazon. Rev. Colomb. Ciencias Pecu. 2018;31:26–35. doi: 10.17533/udea.rccp.v31n1a04. [DOI] [Google Scholar]
- 107.Mendoza-Roldan J.A., Ribeiro S.R., Castilho-Onofrio V., Marcili A., Simonato B.B., Latrofa M.S., Benelli G., Otranto D., Barros-Battesti D.M. Molecular detection of vector-borne agents in ectoparasites and reptiles from Brazil. Ticks Tick. Borne. Dis. 2021;12:101585. doi: 10.1016/j.ttbdis.2020.101585. [DOI] [PubMed] [Google Scholar]
- 108.Dantas-Torres F., Picelli A.M., da Sales K.G.S., de Sousa-Paula L.C., Mejia P., Kaefer I.L., Viana L.A., Pessoa F.A.C. Ticks on reptiles and amphibians in Central Amazonia, with notes on rickettsial infections. Exp. Appl. Acarol. 2022;86:129–144. doi: 10.1007/s10493-021-00682-8. [DOI] [PubMed] [Google Scholar]
- 109.Ogrzewalska M., Uezu A., Labruna M.B. Ticks (Acari: Ixodidae) infesting wild birds in the Atlantic Forest in northeastern Brazil, with notes on rickettsial infection in ticks. Parasitol. Res. 2011;108:665–670. doi: 10.1007/s00436-010-2111-8. [DOI] [PubMed] [Google Scholar]
- 110.Rocha J.M., de Oliveira P.B., Martins T.F., Faccini J.L.H., Sevá A.P., Luz H.R., Albuquerque G.R. Diversity of ticks and detection of Rickettsia amblyommatis infecting ticks on wild birds in anthropogenic landscapes in Bahia state, northeast Brazil. Exp. Appl. Acarol. 2021;84:227–239. doi: 10.1007/s10493-021-00616-4. [DOI] [PubMed] [Google Scholar]
- 111.McIntosh D., Bezerra R.A., Luz H.R., Faccini J.L.H., Gaiotto F.A., Giné G.A.F., Albuquerque G.R. Detection of Rickettsia bellii and Rickettsia amblyommii in Amblyomma longirostre (Acari: Ixodidae) from Bahia state, Northeast Brazil. Braz. J. Microbiol. 2015;46:879–883. doi: 10.1590/S1517-838246320140623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Maia M.O., Koppe V.C., Muñoz-Leal S., Martins T.F., Marcili A., Labruna M.B., Pacheco R.C. Detection of Rickettsia spp. in ticks associated to wild mammals in Northeastern Brazil, with notes on an undetermined Ornithodoros sp. collected from marsupials. Exp. Appl. Acarol. 2018;76:523–535. doi: 10.1007/s10493-018-0323-2. [DOI] [PubMed] [Google Scholar]
- 113.Acosta I.C.L., Martins T.F., Marcili A., Soares H.S., Krawczak F.S., Vieira F.T., Labruna M.B. Ticks (Acari: Ixodidae, Argasidae) from humans, domestic and wild animals in the state of Espírito Santo, Brazil, with notes on rickettsial infection. Vet. Parasitol. Reg. Stud. Reports. 2016;3–4:66–69. doi: 10.1016/j.vprsr.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 114.Costa F.B., Da Costa A.P., Moraes-Filho J., Martins T.F., Soares H.S., Ramirez D.G., Dias R.A., Labruna M.B. Rickettsia amblyommatis infecting ticks and exposure of domestic dogs to Rickettsia spp. in an Amazon-Cerrado transition region of northeastern Brazil. PLoS ONE. 2017;12:e0179163. doi: 10.1371/journal.pone.0179163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Filho E.F.A., Costa F.B., Moraes-Filho J., Dos Santos A.C.G., Do Vale T.L., da Costa A.P., Silva A.B., Labruna M.B., de Nogueira R.M.S. Exposure of Baixadeiro horses to Rickettsia spp. And to ticks infected by Rickettsia amblyommatis in the Baixada Maranhense micro-region, Maranhão, Brazil. Cienc. Rural. 2018;48:1–7. doi: 10.1590/0103-8478cr20180002. [DOI] [Google Scholar]
- 116.Alves A.D.S., Melo A.L.T., Amorim M.V., Borges A.M.C.M., Silva L.G.E., Martins T.F., Labruna M.B., Aguiar D.M., Pacheco R.C. Seroprevalence of Rickettsia spp. in equids and molecular detection of ‘Candidatus Rickettsia amblyommii’ in Amblyomma cajennense sensu lato ticks from the Pantanal region of Mato Grosso, Brazil. J. Med. Entomol. 2014;51:1242–1247. doi: 10.1603/ME14042. [DOI] [PubMed] [Google Scholar]
- 117.De Barros Lopes L., Guterres A., Rozental T., Carvalho De Oliveira R., Mares-Guia M.A., Fernandes J., Figueredo J.F., Anschau I., De Jesus S., Almeida A.B.M.V., et al. Rickettsia bellii, Rickettsia amblyommii, and Laguna Negra hantavirus in an Indian reserve in the Brazilian Amazon. Parasites Vectors. 2014;7:191. doi: 10.1186/1756-3305-7-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Soares H.S., Barbieri A.R.M., Martins T.F., Minervino A.H.H., de Lima J.T.R., Marcili A., Gennari S.M., Labruna M.B. Ticks and rickettsial infection in the wildlife of two regions of the Brazilian Amazon. Exp. Appl. Acarol. 2015;65:125–140. doi: 10.1007/s10493-014-9851-6. [DOI] [PubMed] [Google Scholar]
- 119.Melo A.L.T., Witter R., Martins T.F., Pacheco T.A., Alves A.S., Chitarra C.S., Dutra V., Nakazato L., Pacheco R.C., Labruna M.B., et al. A survey of tick-borne pathogens in dogs and their ticks in the Pantanal biome, Brazil. Med. Vet. Entomol. 2016;30:112–116. doi: 10.1111/mve.12139. [DOI] [PubMed] [Google Scholar]
- 120.Witter R., Martins T.F., Campos A.K., Melo A.L.T., Corrêa S.H.R., Morgado T.O., Wolf R.W., May-Júnior J.A., Sinkoc A.L., Strüssmann C., et al. Rickettsial infection in ticks (Acari: Ixodidae) of wild animals in midwestern Brazil. Ticks Tick. Borne. Dis. 2016;7:415–423. doi: 10.1016/j.ttbdis.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 121.de Serpa M.C.A., Luz H.R., Costa F.B., Weck B.C., Benatti H.R., Martins T.F., Correa L.S., Ramirez D.G., Rocha V., Dias T.C., et al. Small mammals, ticks and rickettsiae in natural and human-modified landscapes: Diversity and occurrence of Brazilian spotted fever in Brazil. Ticks Tick. Borne. Dis. 2021;12:101805. doi: 10.1016/j.ttbdis.2021.101805. [DOI] [PubMed] [Google Scholar]
- 122.Ramos D.G.d.S., Melo A.L.T., Martins T.F., da Alves A.S., dos Pacheco T.A., Pinto L.B., Pinho J.B., Labruna M.B., Dutra V., Aguiar D.M., et al. Rickettsial infection in ticks from wild birds from Cerrado and the Pantanal region of Mato Grosso, midwestern Brazil. Ticks Tick. Borne. Dis. 2015;6:836–842. doi: 10.1016/j.ttbdis.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 123.Machado-Ferreira E., Piesman J., Zeidner N.S., Soares C.A.G. A Prevalent Alpha-Proteobacterium Paracoccus sp. in a population of the cayenne ticks (Amblyomma Cajennense) from Rio de Janeiro, Brazil. Genet. Mol. Biol. 2012;35:862–867. doi: 10.1590/S1415-47572012005000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Colle A.C., Braga Mendonça R.F., Maia M.O., Freitas L.C., Martins T.F., Muñozleal S., Aguiar D.M., Labruna M.B., Rossi R.V., Pacheco R.C. Rickettsial survey and ticks infesting small mammals from the Amazon forest in midwestern Brazil. Syst. Appl. Acarol. 2020;25:78–91. doi: 10.11158/saa.25.1.6. [DOI] [Google Scholar]
- 125.Zeringóta V., Maturano R., Luz H.R., Senra T.O.S., Daemon E., Faccini J.L.H., McIntosh D. Molecular detection of Rickettsia rhipicephali and other spotted fever group Rickettsia species in Amblyomma ticks infesting wild birds in the state of Minas Gerais, Brazil. Ticks Tick. Borne. Dis. 2017;8:81–89. doi: 10.1016/j.ttbdis.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 126.Ogrzewalska M., Uezu A., Labruna M.B. Ticks (Acari: Ixodidae) infesting wild birds in the eastern Amazon, northern Brazil, with notes on rickettsial infection in ticks. Parasitol. Res. 2010;106:809–816. doi: 10.1007/s00436-010-1733-1. [DOI] [PubMed] [Google Scholar]
- 127.Lugarini C., Martins T.F., Ogrzewalska M., de Vasconcelos N.C.T., Ellis V.A., de Oliveira J.B., Pinter A., Labruna M.B., Silva J.C.R. Rickettsial agents in avian ixodid ticks in northeast Brazil. Ticks Tick. Borne. Dis. 2015;6:364–375. doi: 10.1016/j.ttbdis.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 128.Pacheco R.C., Arzua M., Nieri-Bastos F.A., Moraes-Filho J., Marcili A., Richtzenhain L.J., Barros-Battesti D.M., Labruna M.B. Rickettsial infection in ticks (Acari: Ixodidae) collected on birds in southern Brazil. J. Med. Entomol. 2012;49:710–716. doi: 10.1603/ME11217. [DOI] [PubMed] [Google Scholar]
- 129.Magalhães-Matos P.C., de Araújo I.M., de Valim J.R.A., Ogrzewalska M., Guterres A., Cordeiro M.D., Cepeda M.B., da Fonseca A.H. Detection of Rickettsia spp. in ring-tailed coatis (Nasua nasua) and ticks of the Iguaçu National Park, Brazilian Atlantic Rainforest. Ticks Tick. Borne. Dis. 2022;13:101891. doi: 10.1016/j.ttbdis.2021.101891. [DOI] [PubMed] [Google Scholar]
- 130.de Oliveira G.M.B., da Silva I.W.G., da Cruz Ferreira Evaristo A.M., de Azevedo Serpa M.C., Silva Campos A.N., Dutra V., Nakazato L., de Aguiar D.M., Bahia Labruna M., Horta M.C. Tick-borne pathogens in dogs, wild small mammals and their ectoparasites in the semi-arid Caatinga biome, northeastern Brazil. Ticks Tick. Borne. Dis. 2020;11:101409. doi: 10.1016/j.ttbdis.2020.101409. [DOI] [PubMed] [Google Scholar]
- 131.Saraiva D.G., Nieri-Bastos F.A., Horta M.C., Soares H.S., Nicola P.A., Pereira L.C.M., Labruna M.B. Rickettsia amblyommii infecting Amblyomma auricularium ticks in Pernambuco, northeastern Brazil: Isolation, transovarial transmission, and transstadial perpetuation. Vector-Borne Zoonotic Dis. 2013;13:615–618. doi: 10.1089/vbz.2012.1223. [DOI] [PubMed] [Google Scholar]
- 132.Silva A.B., Cardoso K.M., de Oliveira S.V., Costa R.M.F., Oliveira G., Amorim M., Alves L.C., Monteiro M.F.M., Gazeta G.S. Rickettsia amblyommatis infecting Amblyomma pseudoconcolor in area of new focus of spotted fever in northeast Brazil. Acta Trop. 2018;182:305–308. doi: 10.1016/j.actatropica.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 133.Lopes M.G., Krawczak F.D.S., De Lima J.T.R., Fournier G.F.D.S.R., Acosta I.D.C.L., Ramirez D.G., Marcili A., Labruna M.B., Gennari S.M. Occurrence of Ehrlichia canis and Hepatozoon canis and probable exposure to Rickettsia amblyommatis in dogs and cats in Natal, RN. Rev. Bras. Parasitol. Veterinária. 2018;28:151–156. doi: 10.1590/s1984-296120180065. [DOI] [PubMed] [Google Scholar]
- 134.Krawczak F.S., Binder L.C., Oliveira C.S., Costa F.B., Moraes-Filho J., Martins T.F., Sponchiado J., Melo G.L., Gregori F., Polo G., et al. Ecology of a tick-borne spotted fever in southern Brazil. Exp. Appl. Acarol. 2016;70:219–229. doi: 10.1007/s10493-016-0070-1. [DOI] [PubMed] [Google Scholar]
- 135.Labruna M.B., Whitworth T., Bouyer D.H., McBride J., Camargo L.M.A., Camargo E.P., Popov V., Walker D.H. Rickettsia bellii and Rickettsia amblyommii in Amblyomma ticks from the state of Rondônia, Western Amazon, Brazil. J. Med. Entomol. 2004;41:1073–1081. doi: 10.1603/0022-2585-41.6.1073. [DOI] [PubMed] [Google Scholar]
- 136.Aguirre A.A.R., Garcia M.V., da Costa I.N., Csordas B.G., da Rodrigues V.S., Medeiros J.F., Andreotti R. New records of tick-associated spotted fever group Rickettsia in an Amazon-Savannah ecotone, Brazil. Ticks Tick. Borne. Dis. 2018;9:1038–1044. doi: 10.1016/j.ttbdis.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 137.Pereira Medeiros A., Pereira de Souza A., Barbosa de Moura A., Sangaletti Lavina M., Bellato V., Aparecida Sartor A., Aparecida Nieri-Bastos F., José Richtzenhain L., Bahia Labruna M. Spotted Fever Group Rickettsia Infecting Ticks (Acari: Ixodidae) in the State of Santa Catarina, Brazil. Mem. Inst. Oswaldo Cruz. 2011;106:926–930. doi: 10.1590/S0074-02762011000800005. [DOI] [PubMed] [Google Scholar]
- 138.Silveira I., Martins T.F., Oleg Ario M.M., Peterka C., Guedes E., Ferreira F., Labruna M.B., Labruna M.B. Rickettsial Infection in Animals, Humans and Ticks in Paulic eia, Brazil. Zoonoses Public Health. 2015;62:525–533. doi: 10.1111/zph.12180. [DOI] [PubMed] [Google Scholar]
- 139.de Abreu D.P.B., Peixoto M.P., Luz H.R., Zeringóta V., Santolin Í.D.A.C., Famadas K.M., Faccini J.L.H., McIntosh D. Two for the price of one: Co-infection with Rickettsia bellii and spotted fever group Rickettsia in Amblyomma (Acari: Ixodidae) ticks recovered from wild birds in Brazil. Ticks Tick. Borne. Dis. 2019;10:101266. doi: 10.1016/j.ttbdis.2019.101266. [DOI] [PubMed] [Google Scholar]
- 140.Barbieri A.R.M., Szabó M.P.J., Costa F.B., Martins T.F., Soares H.S., Pascoli G., Torga K., Saraiva D.G., Ramos V.N., Osava C., et al. Species richness and seasonal dynamics of ticks with notes on rickettsial infection in a Natural Park of the Cerrado biome in Brazil. Ticks Tick. Borne. Dis. 2019;10:442–453. doi: 10.1016/j.ttbdis.2018.12.010. [DOI] [PubMed] [Google Scholar]
- 141.Muñoz-Leal S., Marcili A., Fuentes-Castillo D., Ayala M., Labruna M.B. A relapsing fever Borrelia and spotted fever Rickettsia in ticks from an Andean valley, central Chile. Exp. Appl. Acarol. 2019;78:403–420. doi: 10.1007/s10493-019-00389-x. [DOI] [PubMed] [Google Scholar]
- 142.Martínez-Sánchez E.T., Cardona-Romero M., Ortiz-Giraldo M., Tobón-Escobar W.D., Moreno-López D., Ossa-López P.A., Pérez-Cárdenas J.E., Labruna M.B., Martins T.F., Castaño-Villa G.J., et al. Rickettsia spp. in ticks (Acari: Ixodidae) from wild birds in Caldas, Colombia. Acta Trop. 2021;213:105733. doi: 10.1016/j.actatropica.2020.105733. [DOI] [PubMed] [Google Scholar]
- 143.Faccini-Martínez A., Ramírez-Hernández A., Forero-Becerra E., Cortés-Vecino J.A., Escandón P., Rodas J.D., Palomar A.M., Portillo A., Oteo J.A., Hidalgo M. Molecular evidence of different Rickettsia species in Villeta, Colombia. Vector Borne Zoonotic Dis. 2016;16:85–87. doi: 10.1089/vbz.2015.1841. [DOI] [PubMed] [Google Scholar]
- 144.Hun L., Troyo A., Taylor L., Barbieri A.M., Labruna M.B. First report of the isolation and molecular characterization of Rickettsia amblyommii and Rickettsia felis in Central America. Vector-Borne Zoonotic Dis. 2011;11:1395–1397. doi: 10.1089/vbz.2011.0641. [DOI] [PubMed] [Google Scholar]
- 145.Troyo A., Moreira-Soto R.D., Calderon-Arguedas Ó., Mata-Somarribas C., Ortiz-Tello J., Barbieri A.R.M., Avendaño A., Vargas-Castro L.E., Labruna M.B., Hun L., et al. Detection of Rickettsiae in fleas and ticks from areas of Costa Rica with history of spotted fever group rickettsioses. Ticks Tick. Borne. Dis. 2016;7:1128–1134. doi: 10.1016/j.ttbdis.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 146.Springer A., Montenegro V.M., Schicht S., Wölfel S., Schaper S.R., Chitimia-Dobler L., Siebert S., Strube C. Detection of Rickettsia monacensis and Rickettsia amblyommatis in ticks collected from dogs in Costa Rica and Nicaragua. Ticks Tick. Borne. Dis. 2018;9:1565–1572. doi: 10.1016/j.ttbdis.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 147.Dolz G., Castro R., Jiménez-Rocha A.E., Retamosa M., Alberti A. Strain diversity of Rickettsia amblyommatis in ticks infesting birds in the North Huetar conservation area of Costa Rica. Ticks Tick. Borne. Dis. 2019;10:1109–1112. doi: 10.1016/j.ttbdis.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 148.Díaz-Sánchez A.A., Chilton N.B., Roblejo-Arias L., Fonseca-Rodríguez O., Marrero-Perera R., Diyes C.P., Yunik M.E.M., Lobo-Rivero E., Corona-González B. Molecular detection and identification of spotted fever group rickettsiae in ticks collected from horses in Cuba. Med. Vet. Entomol. 2021;35:207–212. doi: 10.1111/mve.12480. [DOI] [PubMed] [Google Scholar]
- 149.Noda A.A., Rodríguez I., Miranda J., Mattar S., Cabezas-Cruz A. First report of spotted fever group Rickettsia in Cuba. Ticks Tick. Borne. Dis. 2016;7:1057–1058. doi: 10.1016/j.ttbdis.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 150.Romero L., Costa F.B., Labruna M.B. Ticks and tick-borne Rickettsia in El Salvador. Exp. Appl. Acarol. 2021;83:545–554. doi: 10.1007/s10493-021-00610-w. [DOI] [PubMed] [Google Scholar]
- 151.Parola P., Matsumoto K., Socolovschi C., Parzy D., Raoult D. A tick-borne Rickettsia of the spotted-fever group, similar to Rickettsia amblyommii, in French Guyana. Ann. Trop. Med. Parasitol. 2007;101:185–188. doi: 10.1179/136485907154557. [DOI] [PubMed] [Google Scholar]
- 152.Binetruy F., Buysse M., Barosi R., Duron O. Novel Rickettsia genotypes in ticks in French Guiana, South America. Sci. Rep. 2020;10:2537. doi: 10.1038/s41598-020-59488-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Novakova M., Literak I., Chevez L., Martins T.F., Ogrzewalska M., Labruna M.B. Rickettsial infections in ticks from reptiles, birds and humans in Honduras. Ticks Tick. Borne. Dis. 2015;6:737–742. doi: 10.1016/j.ttbdis.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 154.Salomon J., Angelica N., Santos F., Zecca I.B., Estrada-Franco J.G., Davila E., Hamer G.L., Rodriguez Perez M.A., Hamer S.A. Brown Dog Tick (Rhipicephalus sanguineus Sensu Lato) Infection with endosymbiont and human pathogenic Rickettsia spp., in Northeastern México. Res. Public Health. 2022;19:6249. doi: 10.3390/ijerph19106249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Guzmán-Cornejo C., Rebollo-Hernández A., Herrera-Mares A., Muñoz-Leal S., Del Castillo-Martínez L., López-Pérez A.M., Cabrera-Garrido M., Oceguera-Figueroa A. Rickettsia spp. in ticks from a tropical dry forest reserve on Mexico’s Pacific Coast. Ticks Tick. Borne. Dis. 2022;13:101911. doi: 10.1016/j.ttbdis.2022.101911. [DOI] [PubMed] [Google Scholar]
- 156.López-Pérez A.M., Sánchez-Montes S., Maya-Badillo B.A., Orta-Pineda G., Reveles-Félix S., Becker I., Bárcenas-Barreto K., Torres-Monroy A., Ojeda-Flores R., Sánchez-Betancourt J.I. Molecular detection of Rickettsia amblyommatis and Rickettsia parkeri in ticks collected from wild pigs in Campeche, Mexico. Ticks Tick. Borne. Dis. 2022;13:101844. doi: 10.1016/j.ttbdis.2021.101844. [DOI] [PubMed] [Google Scholar]
- 157.Sánchez-Montes S., Isaak-Delgado A.B., Guzmán-Cornejo C., Rendón-Franco E., Muñoz-García C.I., Bermúdez S., Morales-Diaz J., Cruz-Romero A., Romero-Salas D., Dzul-Rosado K., et al. Rickettsia species in ticks that parasitize amphibians and reptiles: Novel report from Mexico and review of the worldwide record. Ticks Tick. Borne. Dis. 2019;10:987–994. doi: 10.1016/j.ttbdis.2019.04.013. [DOI] [PubMed] [Google Scholar]
- 158.Sánchez-Montes S., Ríos-Muñoz C.A., Espinosa-Martínez D.V., Guzmán-Cornejo C., Berzunza-Cruz M., Becker I. First report of “Candidatus Rickettsia amblyommii” in west coast of Mexico. Ticks Tick. Borne. Dis. 2016;7:1139–1145. doi: 10.1016/j.ttbdis.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 159.Karim S., Budachetri K., Mukherjee N., Williams J., Kausar A., Jawadul Hassan M., Adamson S., Dowd S.E., Apanskevich D., Arijo A., et al. A study of ticks and tick-borne livestock pathogens in Pakistan. PLoS Negl. Trop. Dis. 2017;11:e0005681. doi: 10.1371/journal.pntd.0005681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Castro D.A.M., García S.G.G., Dzul-Rosado K., Aguilar A., Castillo J., Gabster A., Trejos D., Zavala-Castro J., Bermúdez C.S.E. Questing Amblyomma mixtum and Haemaphysalis juxtakochi (Acari: Ixodidae) infected with Candidatus “Rickettsia amblyommii” from natural environment in Panama Canal Basin, Panama. Trop. Med. Health. 2015;43:217–222. doi: 10.2149/TMH.2015-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bermúdez S.E., Eremeeva M.E., Karpathy S.E., Samudio F., Zambrano M.L., Zaldivar Y., Motta J.A., Dasch G.A. Detection and identification of Rickettsial agents in ticks from domestic mammals in eastern Panama. J. Med. Entomol. 2009;46:856–861. doi: 10.1603/033.046.0417. [DOI] [PubMed] [Google Scholar]
- 162.Bermúdez C.S.E., Zaldívar A.Y., Spolidorio M.G., Moraes-Filho J., Miranda R.J., Caballero C.M., Mendoza Y., Labruna M.B. Rickettsial infection in domestic mammals and their ectoparasites in El Valle de Antón, Coclé, Panamá. Vet. Parasitol. 2011;177:134–138. doi: 10.1016/j.vetpar.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 163.Ogrzewalska M., Literak I., Martins T.F., Labruna M.B. Rickettsial infections in ticks from wild birds in Paraguay. Ticks Tick. Borne. Dis. 2014;5:83–89. doi: 10.1016/j.ttbdis.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 164.Ponnusamy L., Gonzalez A., Van Treuren W., Weiss S., Parobek C.M., Juliano J.J., Knight R., Roe R.M., Apperson C.S., Meshnick S.R. Diversity of Rickettsiales in the microbiome of the lone star tick, Amblyomma americanum. Appl. Environ. Microbiol. 2014;80:354–359. doi: 10.1128/AEM.02987-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Budachetri K., Browning R.E., Adamson S.W., Dowd S.E., Chao C.-C., Ching W.-M., Karim S. An Insight Into the Microbiome of the Amblyomma maculatum (Acari: Ixodidae) J. Med. Entomol. 2014;51:119–129. doi: 10.1603/ME12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Commins S.P., James H.R., Kelly L.A., Pochan S.L., Workman L.J., Perzanowski M.S., Kocan K.M., Fahy J.V., Nganga L.W., Ronmark E., et al. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-α-1,3-galactose. J. Allergy Clin. Immunol. 2011;127:1286–1293.e6. doi: 10.1016/j.jaci.2011.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Goddard J., Varela-Stokes A.S. Role of the lone star tick, Amblyomma americanum (L.), in human and animal diseases. Vet. Parasitol. 2009;160:1–12. doi: 10.1016/j.vetpar.2008.10.089. [DOI] [PubMed] [Google Scholar]
- 168.Sagurova I., Ludwig A., Ogden N.H., Pelcat Y., Dueymes G., Gachon P. Predicted northward expansion of the geographic range of the tick vector Amblyomma americanum in North America under future climate conditions. Environ. Health Perspect. 2019;127:107014. doi: 10.1289/EHP5668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Raghavan R.K., Peterson A.T., Cobos M.E., Ganta R., Foley D. Current and future distribution of the lone star tick, Amblyomma americanum (L.) (Acari: Ixodidae) in North America. PLoS ONE. 2019;14:e0209082. doi: 10.1371/journal.pone.0209082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Raghavan R.K., Goodin D.G., Hanzlicek G.A., Zolnerowich G., Dryden M.W., Anderson G.A., Ganta R.R. Maximum entropy-based ecological niche model and bio-climatic determinants of lone star tick (Amblyomma americanum) niche. Vector-Borne Zoonotic Dis. 2016;16:205–211. doi: 10.1089/vbz.2015.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Molaei G., Little E.A.H., Williams S.C., Stafford K.C. Bracing for the worst—range expansion of the lone star tick in the northeastern United States. N. Engl. J. Med. 2019;381:2189–2192. doi: 10.1056/NEJMp1911661. [DOI] [PubMed] [Google Scholar]
- 172.Mixson T.R., Ginsberg H.S., Campbell S.R., Sumner J.W., Paddock C.D. Detection of Ehrlichia chaffeensis in adult and nymphal Amblyomma americanum (Acari: Ixodidae) ticks from Long Island, New York. J. Med. Entomol. 2004;41:1104–1110. doi: 10.1603/0022-2585-41.6.1104. [DOI] [PubMed] [Google Scholar]
- 173.Means R.G., White D.J. New distribution records of Amblyomma americanum (L.) (Acari: Ixodidae) in New York State. J. Vector Ecol. 1997;22:133–145. [PubMed] [Google Scholar]
- 174.Springer Y.P., Eisen L., Beati L., James A.M., Eisen R.J. Spatial istribution of counties in the continental United States with records of occurrence of Amblyomma americanum (Ixodida: Ixodidae) J. Med. Entomol. 2014;51:342–351. doi: 10.1603/ME13115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Luz H.R., Martins T.F., Teixeira R.H.F., Terassini F.A., Soares H.S., Soares J.F., Faccini J.L.H., Labruna M.B. Some biological and behavioral aspects of Amblyomma longirostre (Acari: Ixodidae) under laboratory and natural conditions. Syst. Appl. Acarol. 2018;23:1965–1971. doi: 10.11158/saa.23.10.8. [DOI] [Google Scholar]
- 176.Neelakanta G., Anderson J.F., Fikrig E., Sultana H., Fish D. Anaplasma phagocytophilum induces Ixodes scapularis ticks to express an antifreeze glycoprotein gene that enhances their survival in the cold. J. Clin. Investig. 2010;120:3179. doi: 10.1172/JCI42868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Herrmann C., Gern L. Survival of Ixodes ricinus (Acari: Ixodidae) under challenging conditions of temperature and humidity is influenced by Borrelia burgdorferi sensu lato infection. J. Med. Entomol. 2010;47:1196–1204. doi: 10.1603/ME10111. [DOI] [PubMed] [Google Scholar]
- 178.Romashchenko A.V., Ratushnyak A.S., Zapara T.A., Tkachev S.E., Moshkin M.P. The correlation between tick (Ixodes persulcatus Sch.) questing behaviour and synganglion neuronal responses to odours. J. Insect Physiol. 2012;58:903–910. doi: 10.1016/j.jinsphys.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 179.Belova O.A., Burenkova L.A., Karganova G.G. Different tick-borne encephalitis virus (TBEV) prevalences in unfed versus partially engorged ixodid ticks—Evidence of virus replication and changes in tick behavior. Ticks Tick. Borne. Dis. 2012;3:240–246. doi: 10.1016/j.ttbdis.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 180.Levin M.L., Schumacher L.B.M., Snellgrove A. Effects of Rickettsia amblyommatis infection on the vector competence of Amblyomma americanum ticks for Rickettsia rickettsii. Vector-Borne Zoonotic Dis. 2018;18:579–587. doi: 10.1089/vbz.2018.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Macaluso K.R., Sonenshine D.E., Ceraul S.M., Azad A.F. Infection and transovarial transmission of Rickettsiae in Dermacentor variabilis ticks acquired by artificial feeding. Vector-Borne Zoonotic Dis. 2004;1:45–53. doi: 10.1089/153036601750137660. [DOI] [PubMed] [Google Scholar]
- 182.Suwanbongkot C., Langohr I.M., Harris E.K., Dittmar W., Christofferson R.C., Macaluso K.R. Spotted fever group Rickettsia infection and transmission dynamics in Amblyomma maculatum. Infect. Immun. 2019;87:e00804-18. doi: 10.1128/IAI.00804-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Zanetti A.S., Pornwiroon W., Kearney M.T., Macaluso K.R. Characterization of Rickettsial infection in Amblyomma americanum (Acari: Ixodidae) by quantitative real-time polymerase chain reaction. J. Med. Entomol. 2008;45:267–288. doi: 10.1093/jmedent/45.2.267. [DOI] [PubMed] [Google Scholar]
- 184.Needham G.R., Teel P.D. Off-host physiological ecology of ixodid ticks. Annu. Rev. Entomol. 1991;36:659–681. doi: 10.1146/annurev.en.36.010191.003303. [DOI] [PubMed] [Google Scholar]
- 185.Busby A.T., Ayllon N., Kocan K.M., Blouin E.F., De La Fuente G., Galindo R.C., Villar M., De La Fuente J. Expression of heat shock proteins and subolesin affects stress responses, Anaplasma phagocytophilum infection and questing behaviour in the tick, Ixodes scapularis. Med. Vet. Entomol. 2012;26:92–102. doi: 10.1111/j.1365-2915.2011.00973.x. [DOI] [PubMed] [Google Scholar]
- 186.Lopes M.G., Muñoz-Leal S., de Lima J.T.R., da Fournier G.F.S.R., da Acosta I.C.L., Martins T.F., Ramirez D.G., Gennari S.M., Labruna M.B. Ticks, rickettsial and erlichial infection in small mammals from Atlantic forest remnants in northeastern Brazil. Int. J. Parasitol. Parasites Wildl. 2018;7:380–385. doi: 10.1016/j.ijppaw.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Bermúdez C.S.E., Troyo A. A review of the genus Rickettsia in Central America. Res. Rep. Trop. Med. 2018;9:103. doi: 10.2147/RRTM.S160951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Stafford K.C., Molaei G., Little E.A.H., Paddock C.D., Karpathy S.E., Labonte A.M. Distribution and establishment of the lone star tick in connecticut and implications for range expansion and public health. J. Med. Entomol. 2018;55:1561–1568. doi: 10.1093/jme/tjy115. [DOI] [PubMed] [Google Scholar]
- 189.Apperson C.S., Engber B., Nicholson W.L., Mead D.G., Engel J., Yabsley M.J., Dail K., Johnson J., Watson D.W. Tick-borne diseases in North Carolina: Is “Rickettsia amblyommii” a possible cause of Rickettsiosis reported as Rocky Mountain spotted fever? Vector-Borne Zoonotic Dis. 2008;8:597–606. doi: 10.1089/vbz.2007.0271. [DOI] [PubMed] [Google Scholar]
- 190.Sebastian P.S., Tarragona E.L., Saracho Bottero M.N., Nava S. Phylogenetic divergence between Rickettsia amblyommatis strains from Argentina. Comp. Immunol. Microbiol. Infect. Dis. 2020;69:101418. doi: 10.1016/j.cimid.2020.101418. [DOI] [PubMed] [Google Scholar]
- 191.Guzmán-Cornejo C., Montiel G., Pérez T.M. The Amblyomma (Acari: Ixodida: Ixodidae) of Mexico: Identification Keys, Distribution and Hosts. Zootaxa. 2011;2998:16–38. doi: 10.11646/zootaxa.2998.1.2. [DOI] [Google Scholar]
- 192.Cardona-Romero M., Martínez-Sánchez E.T., Alvarez-Londoño J., Pérez-Cárdenas J.E., Ossa-López P.A., Castaño-Villa G.J., Binder L.C., Faccini-Martínez Á.A., Rivera-Páez F.A. Seroprevalence and detection of Rickettsia spp. in wild birds of Arauca, Orinoquia region, Colombia. Vet. Parasitol. Reg. Stud. Rep. 2022;30:100720. doi: 10.1016/j.vprsr.2022.100720. [DOI] [PubMed] [Google Scholar]
- 193.Mukherjee N., Beati L., Sellers M., Burton L., Adamson S., Robbins R.G., Moore F., Karim S. Importation of exotic ticks and tick-borne spotted fever group rickettsiae into the United States by migrating songbirds. Ticks Tick. Borne. Dis. 2014;5:127–134. doi: 10.1016/j.ttbdis.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Budachetri K., Williams J., Mukherjee N., Sellers M., Moore F., Karim S. The microbiome of neotropical ticks parasitizing on passerine migratory birds. Ticks Tick. Borne. Dis. 2017;8:170–173. doi: 10.1016/j.ttbdis.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Snellgrove A.N., Krapiunaya I., Scott P., Levin M.L. Assessment of the pathogenicity of Rickettsia amblyommatis, Rickettsia bellii, and Rickettsia montanensis in a guinea pig model. Vector-Borne Zoonotic Dis. 2021;21:232–241. doi: 10.1089/vbz.2020.2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Rivas J.J., Moreira-Soto A., Alvarado G., Taylor L., Calderón-Arguedas O., Hun L., Corrales-Aguilar E., Morales J.A., Troyo A. Pathogenic potential of a Costa Rican strain of ‘Candidatus Rickettsia amblyommii’ in guinea pigs (Cavia porcellus) and protective immunity against Rickettsia rickettsii. Ticks Tick. Borne. Dis. 2015;6:805–811. doi: 10.1016/j.ttbdis.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 197.Clark T.R., Noriea N.F., Bublitz D.A.C., Ellison D.W., Martens C., Lutter E.I., Hackstadt T. Comparative genome sequencing of Rickettsia rickettsii strains that differ in virulence. Infect. Immun. 2015;83:1568–1576. doi: 10.1128/IAI.03140-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Galletti M.F.B.M., Paddock C.D., Hecht J.A., Biggerstaff B.J., Ritter J.M., Karpathy S.E. Isolate-dependent differences in clinical, pathological, and transcriptional profiles following in vitro and in vivo infections with Rickettsia rickettsii. Infect. Immun. 2021;89:e00626-20. doi: 10.1128/IAI.00626-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Kmetiuk L.B., Krawczak F.S., Machado F.P., Paploski I.A.D., Martins T.F., Teider-Junior P.I., Serpa M.C.A., Barbieri A.R.M., Bach R.V.W., Barros-Filho I.R., et al. Ticks and serosurvey of anti-Rickettsia spp. antibodies in wild boars (Sus scrofa), hunting dogs and hunters of Brazil. PLoS Negl. Trop. Dis. 2019;13:e0007405. doi: 10.1371/journal.pntd.0007405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Wallace J.W., Nicholson W.L., Perniciaro J.L., Vaughn M.F., Funkhouser S., Juliano J.J., Lee S., Kakumanu M.L., Ponnusamy L., Apperson C.S., et al. Incident tick-borne infections in a cohort of North Carolina outdoor workers. Vector Borne Zoonotic Dis. 2016;16:302–308. doi: 10.1089/vbz.2015.1887. [DOI] [PubMed] [Google Scholar]
- 201.Delisle J., Mendell N.L., Stull-Lane A., Bloch K.C., Bouyer D.H., Moncayo A.C. Human infections by multiple spotted fever group Rickettsiae in Tennessee. Am. J. Trop. Med. Hyg. 2016;94:1212–1217. doi: 10.4269/ajtmh.15-0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Vaughn M.F., Delisle J., Johnson J., Daves G., Williams C., Reber J., Mendell N.L., Bouyer D.H., Nicholson W.L., Moncayo A.C., et al. Seroepidemiologic study of human infections with spotted fever group rickettsiae in North Carolina. J. Clin. Microbiol. 2014;52:3960–3966. doi: 10.1128/JCM.01733-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Pornwiroon W., Bourchookarn A., Paddock C.D., Macaluso K.R. Immunoproteomic profiling of Rickettsia parkeri and Rickettsia amblyommii. Ticks Tick. Borne. Dis. 2015;6:829–835. doi: 10.1016/j.ttbdis.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Telford S.R., Dawson J.E., Katavolos P., Warner C.K., Kolbert C.P., Persing D.H. Perpetuation of the agent of human hranulocytic Ehrlichiosis in a deer tick-rodent cycle. Proc. Natl. Acad. Sci. USA. 1996;93:6209–6214. doi: 10.1073/pnas.93.12.6209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Agudelo Higuita N.I., Franco-Paredes C., Henao-Martínez A.F. The expanding spectrum of disease caused by the lone star tick, Amblyomma americanum. Infez. Med. 2021;29:378–385. doi: 10.53854/liim-2903-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Santibáñez S., Portillo A., Palomar A.M., Oteo J.A. Isolation of Rickettsia amblyommatis in HUVEC line. New Microbes New Infect. 2018;21:117–121. doi: 10.1016/j.nmni.2017.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.