Abstract
Purpose
Overcrowding is a problem that affects emergency departments (ED) all over the world; it occurs due to a disproportion between user demand and the physical, human and structural resources available. Essential prerequisites to assessing and managing the phenomenon are its accurate measurement and an understanding of its impact. The objective of this systematic review is to identify the characteristics of the problem, analyzing the proposed strategies aimed at improving patient flow, delay in services provided and overcrowding of emergency departments.
Methods
To achieve our objectives, a manual computerized search was performed in the bibliographic databases using as keywords “Emergency Department”, “Overcrowding”, “Emergency Room”, “Emergency Service”, “Emergency Unit”“,Emergency Ward”, “Emergency Outpatient Unit”, “Emergency Hospital”, “Crowding”, “Mass Gathering”, “Management” and “Comprehensive Health Care”. Two independent reviewers analyzed abstracts, titles and full text articles for admissibility, according to the selected inclusion and exclusion criteria.
Results
The process lead to include 19 articles. It was possible to group the solutions proposed in five categories: work organization, investment in primary care, creation of new dedicated professional figures, work and structural modifications and implementation of predictive simulation models using mathematical algorithms.
Conclusion
The most effective measures to guarantee an improvement in the flow of patients are represented by both improving the efficiency of human resources and by developing predictive mathematical models, regardless of the type of hospital and its location. Considering the complexity of EDs and the multiple characteristics of overcrowding and that the causes of crowding are different and site-specific, a careful examination of the specifics of each ED is necessary to identify improving fields.
Keywords: patients flow management, human resource efficiency, predictive mathematical models, patients overload, overflowing
Introduction
Overcrowding in emergency departments is a globally widespread problem. Technically, ED overcrowding occurs due to a disproportion between health demand, consisting of the number of patients waiting care, and the available physical and/or human and/or structural resources necessary to satisfy it.1 It can also be defined as the situation in which the function of the ED is hampered mainly due to the excessive number of patients waiting to be examined, undergoing evaluation and treatment or waiting to leave, compared to the physical capacity or to the available personnel of the emergency room.2 Among the main causes that affect patients’ flow into an emergency room, the scientific literature reports the imbalances between the capacity of the ED and admission to triage for patients, the growing number of unscheduled emergency room visits,3–5 large numbers of patients who persist in the expectation of receiving ongoing care in the ED for minor illnesses and excessive demand of diagnostic test.5,6
Both an accurate ED crowding measurement and an evidence-based understanding of the impact of ED overcrowding are prerequisites before attempting to find solutions. The best-known models of the emergency system are based on 3 macro phases:7 the volume of patients arriving (input), the time to process and/or treat patients (throughput), and the volume of patients leaving the ED (output). Any combination involving a rise in input, a delayed throughput, or a decreased output can lead to crowding.8 The input phase refers to an excessive and significant ED-access of users, determined in recent years by the onset of new care needs, which can take place urgently by ambulance, by nursing homes, by family or by specialized doctors, by police or by autonomous choice. The throughput phase refers to a slowing down of the ED internal pathways, and in particular of the triage phase, medical examination, and all the diagnostic activities that require the collaboration of specialized consultants. Finally, the output phase includes both the difficulty in hospitalizing due to unavailability of a bed in the destination ward, and the difficulty in discharging the patient, inevitably causing the length of hospitalization to be prolonged.1
The input, throughput and output factors can determine a prolonged stay of already-evaluated-patients inside the ED, waiting for the bed into a specialize ward. This phenomenon is already known as “boarding”, and it determines a considerable absorption of operational resources within the emergency services; this has consequences for patients, health care operators and for the system as a whole. Table 1 reassumes the main variable influencing each of the three phases of the emergency system (Table 1).
Table 1.
Main Causes of Ed Overcrowding Broken Down by Factor
| Phase | Influencing Variables |
|---|---|
| Input | Population aging with increased demand for hospitalization |
| Difficulties in accessing urgent healthcare services | |
| Distorted information provided by mass media | |
| Bad health education | |
| Mismanagement of treatable diseases at home | |
| Lack of seasonal disease prophylaxis | |
| Inappropriate hospitalization request | |
| Increase of the poor population with consequent difficulty to face health costs | |
| Failed intervention on ED Frequent Users | |
| Throughput | Failure to optimize triage activities |
| Architectural limits of ED department | |
| Excessive practice of defensive medicine | |
| Efficiency of diagnostic services | |
| Health care understaffing | |
| Collaboration lack between health personnel | |
| Output | Hospital bed shortage |
| Failure to identify available beds | |
| Shortage of hospital discharge rooms | |
| Delayed and prolonged discharge | |
| Lack of social services to facilitate difficult patients’ discharge |
Despite the efforts employed and the knowledge acquired so far, the problem of ED overcrowding persists globally, demonstrating how few evidence-based-solutions have been achieved to improve the flow of patients in ED, with a growing attention to the use of simulation models, predictive algorithms and artificial intelligence aimed at optimizing the resources already present.9,10 The objectives of this systematic review is to I) identify overcrowding features, II) analyze the proposed strategies aimed at improving the flow of patients, the delay in services provided and the ED overcrowding.
Materials and Methods
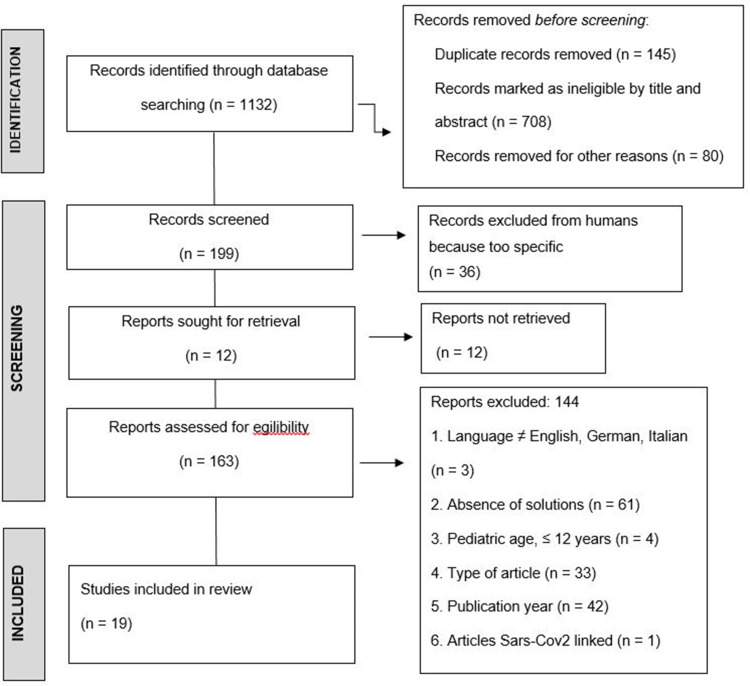
In this review article, we performed a computerized database search to identify relevant articles. We searched for published articles in bibliographic databases, including PubMed, Scopus, Web of Science (last search on 29/01/2022). A manual search of bibliographies of the identified papers and relevant information to meet the objectives of this study was performed. Two independent reviewers screened abstracts and titles for eligibility. When the reviewers felt that the abstract or the title were potentially useful, full copies of the article were retrieved and considered for eligibility by both reviewers. When discrepancies occurred between reviewers, the reasons were identified, and a final decision was made based on a third senior reviewer agreement. Keywords used in the search were “Emergency Department (ED)”, “Overcrowding”, “Emergency Room”, “Emergency Service”, “Emergency Unit”, “Emergency Ward”, “Emergency Outpatient Unit”, “Emergency Hospital”, “Crowding”, “Mass Gathering”, “Management” and “Comprehensive Health Care”. The selection of these terms was made by MeSH service in PubMed website databases. Thus, we obtained 436 articles from PubMed, 623 articles from Scopus and 73 articles from Web Of Science, for a total of 1132 articles. By loading each bibliographic database’s search extract files (.bib and.nbib) into the Zotero tool, 145 duplicates were eliminated.
An additional 708 records were excluded after applying the title and abstract eligibility criteria, while 80 articles were excluded for other reasons (for example: paid access). The full texts of 199 articles were reviewed. Of these, 163 articles met the inclusion criteria and were evaluated for eligibility, and 36 articles were excluded because they were too specific, as they examined the problem of overcrowding exclusively in relation to particular clinical conditions (for example: opiate intoxication, cardiac arrest, following traumatic episodes or in conjunction with large mass events).
After reading the full text and in light of the eligibility criteria (Table 2), 19 studies were included in this systematic review. Figure 1 shows the search and selection process according to the PRISMA 2020 statement11 (Figure 1 and checklist reported in the Supplementary File).
Table 2.
Elegibility Criteria
| Inclusion | Exclusion |
|---|---|
| Timeline 2012–2022 | 2011 ≤ Time > 2022 |
| Age ≥ 13 anni | Age ≤ 12 |
| Articles with proposed solutions | Systematic Reviews, Descriptive articles without solutions |
| English, German, Italian languages | Languages other than English, German, Italian |
| Relationship between Sars-Cov2 virus and ED overcrowding | |
| Correlation with acute or chronic diseases/disorders |
Figure 1.
Flowchart of the search and selection process of articles according to the PRISMA statement. No automation tools were used to screen articles.
The independent reviewers manually extracted the data, that was inputted into a standardized excel database, in which, for each included article, were inserted article title, authors, year of publication, time period analyzed, duration of the observation period, country, scientific journal, type of article, causes, consequences, overcrowding measurement scales, solutions, presence or absence of simulation models, predictive algorithms, artificial intelligence, outcomes of the improvement actions undertaken, study limits and macro phases involved (input, throughput, output).
The literature search was limited to journal articles and governmental documents in English, German and Italian, with a time horizon between 2012 and 2022. The main reasons for exclusion were: (1) correlation between ED overcrowding and the prevalence of acute or chronic diseases/disorders, (2) impact of Sars-Cov2 virus on ED overcrowding, (3) systematic reviews, (4) descriptive articles without solutions on the overcrowding problem and (5) pediatric hospital/pediatric age.
Results
With regard to timeline set (2012–2022), 11% of the articles were published in 2012, 16% in 2014, 5% in 2015, 11% in 2016, 21% in 2018, 16% in 2019, 5% in 2020 and 16% in 2021. From full text reading of the 19 articles, we extracted the observation period of the overcrowding phenomenon for each study, resulting in an average of 903.47 days with a minimum interval of 14 days and a maximum of 4382. The selected articles come from 11 different countries, among which the USA (39%) and Taiwan (11%), and the most represented type of article was observational study (53%) (Figure 2).
Figure 2.
Source and type of articles selected for the review study.
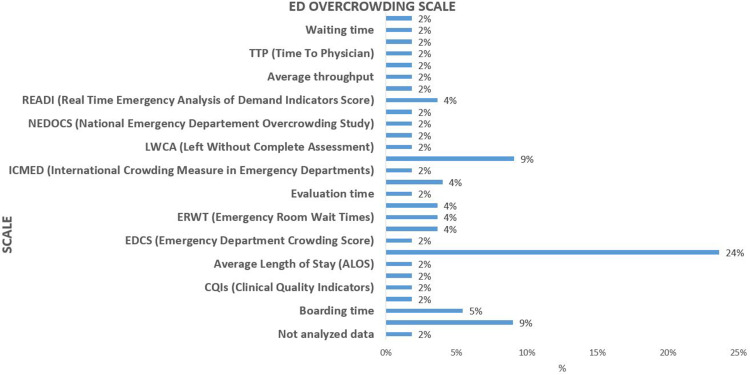
Overcrowding indicators are classified as outcome indicators or process indicators within the emergency room, and also divided in static, dynamic or temporal dynamic.1 We identified these indicators in each article as reference to manage and monitor the phenomenon. In particular, on a total of 27 measurement scales found (Figure 3), the most represented are ED LOS (Length of Stay, 24%), LWBS (Leaving Without Being Seen, 9%) and the Door to Evaluation Time (9%); moreover, causes and consequences of ED overcrowding have been classified (Table 3).
Figure 3.
Measurement scales used as indicators to monitor the phenomenon of overcrowding.
Table 3.
Causes and Consequences of Ed Overcrowding
| Causes | Item |
|---|---|
| Structural causes | Shortage of ED physical space3,4,10 |
| Technological causes | – |
| Human causes | Increase in unscheduled access3,5,9,11–13 |
| Inadequate ED access5,6,10,13–17 | |
| Increase of elderly people15,16,18,19 | |
| Increased demand from patients for specialized care11,17,18 | |
| Rising burden of chronic disease19 | |
| Excessive diagnostic test demand5 | |
| Defensive medicine6 | |
| Managerial causes | Rising Emergency Department closures3 |
| Increased patients waiting to be hospitalized5,15,17 | |
| Insufficient numbers of health workers4,10,13–15,20 | |
| Lack of availability of beds3,4,6 | |
| Flow patients’ Bad management12,17,21 | |
| Ambulance diversion22 | |
| Mismanagement resources allocation10,16,20 | |
| Limited access to primary care15 | |
| Reduced health funding13 | |
| Inability to discharge patients6,13,23 | |
| Delayed services and consultations4,16,21,24 | |
| Outcomes | |
| On patients | Increased in-hospital death4,12,14,15,19,20,23,24 |
| Increased patients who left without complete assessment24 | |
| Increased patients leaving the emergency room without being seen10,12–14,16–18,20,22 | |
| Increased patients’ pain and suffering22 | |
| Patient dissatisfaction13–15,17,19,21–23 | |
| Delay treatments16,17,23 | |
| Inbed delay patients16 | |
| Delay in identification and treatment6,12 | |
| On healthcare workers | Increased of the preventable medical mistakes22 |
| Health workers burnout14,17,19,20 | |
| Decreased quality of care6,11,16,17,21 | |
| Work related stress20 | |
| On the system | Maximum waiting time for medical examination > 4 h13 |
| Prolonged ED Lengths Of Stay3,4,10,14–16,18,19,23,24 | |
| Rising health care cost12,13,16,17,21 | |
| Increased waiting time6,12,22 | |
| Ambulance diversion12,21 | |
| Waste of medical resources6 | |
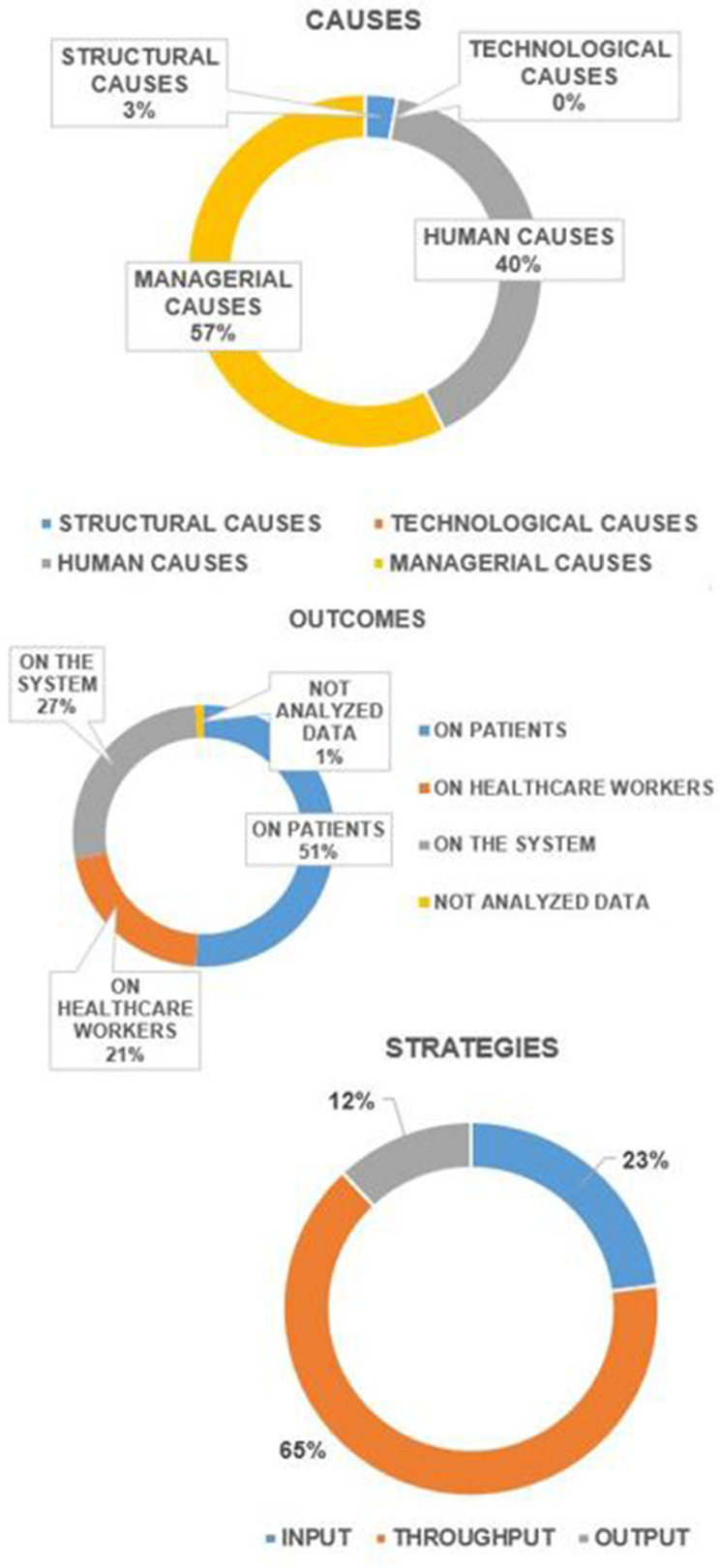
During data extraction, to investigate ED overcrowding causes and consequences, it was necessary to make data homogeneous by grouping each result into macro categories; therefore, as reported in Figure 3, we divided them into: managerial causes (57%), human causes (40%), structural causes (3%) and technological causes (0%). Data relating to the consequences show those on patients (51%), on the system (27%) and on healthcare workers (21%) and not analyzed data (1%). Regarding the analysis of the strategies identified to overcome the problem of ED overcrowding, each proposed solution was classified on its area of influence on the input, throughput and output processes (Table 4). The strategies implemented to overcome the ED overcrowding focused on new solutions to improve the ED internal pathways (throughput), which represent 65% of the total, compared to the input (12%) and output (23%) (Figure 4).
Table 4.
Proposed Solutions to Overcome Ed Overcrowding
| Actions involving input | Ensuring priority of hospitalization for ED patients4 |
| Transfers between institutions permetted only if there are no patients awaiting admission in the ED4 | |
| Ambulances diversion to other hospitals presumed less crowded18 | |
| Incentivizing patients with less serious conditions to see their family doctor first, before going to the ED16 | |
| Addition of clinical assistant to each ED shift22 | |
| Investing in primary care16,17 | |
| To build home care and post acute care resources such as long-term care or rehabilitation services6 | |
| Forecasting emergency department flow3,10,17 | |
| Transference of admitted patients out of the ED rooms and into inpatient hallways15,19 | |
| Discourage boarding of admitted patients in ED exam rooms14 | |
| Actions involving throughput | Time-series analysis used to develop statistical models in order to forecast the patients flow in the ED10 |
| Increase bed of internal medicine19 | |
| Increase outflow of internal medicine patients from the ED to the internal medicine departments19 | |
| The access block viewed as a whole hospital problem and not only an ED problem23 | |
| The creation of a Patient Partner role21 | |
| Adding a dedicated triage space for patients who arrive by emergency medical services (EMS triage)13,14 | |
| Establishment of a rapid assessment unit (RAU) in ED21 | |
| Decrease requests for unnecessary advance diagnostic tests5 | |
| Development of a dashboard which provides real-time information regarding ED crowding20 | |
| Early identification of events that may worsen patient’s health24 | |
| Create a real time tool to inform patients about waiting times17,22 | |
| Improve the ED information system5,6,20 | |
| Improve patients post acute care6 | |
| Having a comprehensive view of patient flow in ED3 | |
| Optimize staff and resources3,10,15,18,23 | |
| Implementing additional resources and alternate care pathways3 | |
| Hospital beds priority at ED4 | |
| Patients registration process simply and fast15,21 | |
| Early identification of patients needing hospitalization or discharge24 | |
| Earlier administration of important therapies such as analgesia and antibiotics24 | |
| Close monitoring of specialties with the highest percentage of emergency room visits (cardiology, gastroenterology and pulmonology)11 | |
| Supplemented Triage and Rapid Treatment (START)24 | |
| Improve triage effectiveness12 | |
| Speed up the request for necessary diagnostic tests5,24 | |
| Actions involving output | Increased partnerships with social care service providers to facilitate discharge13 |
| To follow in the clinic patients already evaluated for the first time in the ED11 | |
| Discharge of ED patients before 12:00 and discharge of internal medicine patients by the morning shift19 | |
| Review of all patients in hospital for 14 days or more13 | |
| Decanting non-emergency lower acuity patients from the ED to a primary care clinic16 |
Figure 4.
ED overcrowding: identified causes, consequences and implemented strategies.
Discussion
From the selected articles, it was possible to group the proposed strategies into macro categories: work organization, investing in primary care, creation of new dedicated professional figures, structural works and modifications and implementation of simulation predictive models using mathematical algorithms. A deeper discussion by macro-categories follows.
Work Organization
Many scientific articles aim to compare how the number of ED patients involved in throughput and output can affect patients waiting time on input.5 Although in the literature there are studies that demonstrate how to improve the throughput processes, it is necessary to keep in mind that there are differences in the triage organization, when considering different countries.12–14 Therefore, it is important to use a continuous, rigorous, standardized monitoring of the activities implemented, employing analytical strategies to evaluate the results.5 At this stage, work organization is comparable with optimization of staff and resources already present, especially when financial tension and limited resources challenge hospitals to provide timely and effective care.3–15 Beyond optimizing available resources, the most effective strategies to reduce overcrowding are early and targeted interventions, such as: earlier identification of subtle presentations of life threats, earlier starting of diagnostic testing, earlier administration of important therapies,12 real-time information on ED overcrowding,16 creating a tool that predicts waiting times to inform patients,17 reducing the number of potentially avoidable diagnostic tests and treatments performed,5 discharging patients before noon,18 re-evaluating all patients staying in hospital for 14 days or more to facilitate their discharge.19 The proposed solutions, although effective, are not exempt from evident limitations: arbitrary choice of ED LOS threshold values,16 changes implemented only in an urban and medium-sized ED,20 implementation of improvement actions in an ED already functioning,18 ignoring ED patients’ satisfaction or the impact of physician bias on waiting time.21 However, the limitation regarding the choice of ED LOS cutoff values could easily be overcome by focusing on the interactions between the different factors constituting the rating scale, as these allow a deeper analysis for planning, thus improving decision-making.22
Investing in Primary Care
As both the population age and the burden of chronic disease grows, people need complex care, that should be organized according to an accessible care pathway model.23 A difficult and delayed access by patients to diagnostic tests prescribed by their family doctor can lead to improper ED use and its consequent overcrowding. Ansah et al24 and Ferreira Amorim et al17 concluded that there is an inappropriate ED use and that an enhanced primary care system is needed to reduce ED crowding. Indeed, Wang et al6 found that families continue to use ED to obtain care for elderly or disabled patients, whose needs should be met in a long-term care facility.
A strengthened primary care system has the potential to improve population health outcomes and, consequently, to reduce the demand for non-emergency care in the ED. In view of these results, the involvement of political leaders is essential to design a cost-effective way to improve primary care and to co-locate general practice clinics across all EDs, to which all non-emergency patients may be sent.
Creation of New Dedicated Professional Figures
Several authors agree that it is very important to involve and train staff19,20 before successfully designing and implementing new improvement actions; therefore, new dedicated professional figures have been proposed to contribute to both the physical and structural changes in ED, and the reorganization of patients’ flow. For instance, the figure of the patient partner emerges; this new figure is focused on the initial presentation of the patient, positioning of the bed, quick registration of the patient on the computerized medical record.20 It is also recommended a rapid evaluation unit (RAU), medical evaluation, complete registration at the patient’s bed after medical visits and nursing services, patient stabilization and start of treatment.20 Therefore, it is important to invest in training the personnel already hired and in relocating doctors and nurses already assigned to triage in the RAU.
In order to significantly improve the flow of patients, decrease the workload of healthcare personnel and increase the patient experience, a patient-centered care model has been also proposed, requiring limited healthcare costs. A similar solution is proposed by Huang et al21 with the identification of a clinical assistance, a professional figure in charge of managing the flow of incoming patients, entrusting them in an orderly and efficient way to doctors, informing them of expected waiting times and managing the anxious states that patients and their relatives may present. At the same time, this so-called clinical assistance was involved in all administrative matters, as it helped the patients in the compilation of required forms and in answering all non-medical questions. The study shows how, in a crowded ED, the introduction of the professional figure of the clinical assistance effectively reduces both ED LOS and the number of patients who leave ED without being seen by healthcare workers. Finally, the need to involve social assistance services in multidisciplinary meetings about long-term hospitalizations, to facilitate difficult discharges, is transversal in the literature.
Structural Works and Modifications
ED transformation is considered a manageable, strategic, economic, and sustainable solution, and has a positive impact on both patient care experience and input factors. In addition to the ED structural changes, the number of beds in the internal medicine wards should be increased, with the clear intention of improving discharge from the emergency room in the morning,25 and avoiding boarding. Valipoor et al,26 limiting their analysis to the structural environment, identified strategies for assessing the impact of ED crowding and long waiting times, such as a reorganization of internal spaces to ensure first patients’ evaluation, using hallway beds/chairs and enlarging the triage area dedicated to emergency. Similarly, in Stanford ED,18 an ED vertical flow model was created, removing fold-down horizontal stretchers and replacing them with multiple chairs that allowed for the assessment and medical management in an upright sitting position. Each structural change undertaken has shown to be statistically effective in reducing ED overcrowding, but has also resulted in conflicting effects, such as increased dissatisfaction among the medical and nursing staff due to an increased number of admissions in a limited number of hours.25 Moreover, the expansion of the triage area may not be as effective in other EDs,26 where the problem regard human resources, rather than the physical expansion of ED spaces.20
Implementation of Simulation Predictive Models Using Mathematical Algorithms
In the last two years, digital information around the world has more than doubled, and this trend is likely going to increase exponentially. Medicine is the protagonist of this growth. This is demonstrated by the explosion of the IoMT (Internet of Medical Things) and by the use of new analysis models, such as machine learning techniques, to learn from data, with the final aim to generate predictive models27 that allow to understand that certain combinations of values can provide the solution of the problem in real time. According to these premises, also in the analyzed literature, there is a wide use of simulation models. Ansah et al24 employed the dynamic system (SD), creating virtual simulation models in order to develop and test the solution strategies before their implementation. Simul817 is a model also capable of generating solutions to help healthcare managers to improve ED overcrowding in different scenarios. This forecasting and simulation model is able to predict the patient’s requests for admission and ED waiting time, to assist in human resources planning, process design, to guide educational strategies for staff and to improve decision making of health care managers.17 The simulation of discrete events (DES)26 is another model used to explore the impact of the implementation of different strategies on ED flow patients. Another system that acts primarily on productivity is the Dynamic Grouping and Priority Algorithm (DGP),28 which identifies the most appropriate patient groups for hospitalization, assigning them a priority level based on patient information and organization of the ED in real time.28 Considering the diversion of ambulances29 to nearby hospitals as a last resort to temporarily alleviate ED overcrowding, Lin et al30 developed a simulation series system to evaluate starting criteria and deviation intervals, analyzing the access block causes, crowding index, patients LOS (Lenght of Stay), probability of adverse events and the effect of the choices made to solve the problem.
The Experience in a Hospital Reality
This systematic review gave to the authors an opportunity to proceed with a careful analysis of the organization of the ED of our hospital, which is also afflicted by the problem of overcrowding. In this historical period, in which there is a chronic shortage of medical staff, it is essential to guarantee the best effectiveness of the resources already available. In agreement with the results obtained, and considering the computerization process already underway, we focused on input\throughput factors. In collaboration with the service of clinical engineering, we have expanded the ED premises, renovating them in order to obtain a waiting room with an info-point distinct from the triage area. In this way, we were able to ensure greater efficiency in the management of low priority tags, improving the triage working condition, and providing timely information on the status of patients’ health to family members, thus also limiting episodes of violence against healthcare workers. Training courses were carried out for both nursing and medical staff, implementing a random monitoring system of the ambulance block in the emergency room.
At the same time, based on historical data on the ED access, we are trying to evaluate the best mathematical model to timely predict the highest risk of overcrowding and implement the stated preparedness plan. Time will tell us what has been implemented.
Conclusion
The problem of ED overcrowding is extremely widespread, and the effort that health authorities and governments are making to counteract this problem is undeniable. Although the number of selected articles is limited, it is enough to conclude that the most effective weapon to ensure a significant process of improving patients’ flow in ED is represented by improving efficiency in human resources and in the technological development of predictive mathematical models, regardless of the type of hospital and its location. Healthcare professionals should be directly involved, informed of the strategies undertaken to combat ED overcrowding and properly trained to expand their skills and responsibilities. Considering that causes of ED crowding are variable and require site-specific solutions,3 but also considering the complex nature of emergency departments and the multiple characteristics of overcrowding, a careful examination of the specific functioning of each ED is necessary to identify the negative impacts, improve treatment time and patience experience, and to plan strategies to combat the phenomenon by acting on input, throughput or output.
Disclosure
The main limitation of this review is the limited number of article selected, followed by the variability in study design and methodological quality of included articles. The observational studies included varied in the quality of methodology descriptions, outcome evaluation, and reporting: this made the comparison between studies’ results difficult. Moreover, this study included only articles written in English, Italian and German; therefore, some pertinent studies may have been excluded. This research received no funding. The authors report no conflicts of interest in this work.
References
- 1.Ministero della Salute. Linee di indirizzo nazionali per lo sviluppo del piano di gestione del sovraffollamento in pronto soccorso; 2019. Available from: www.salute.gov.it/portale/documentazione/p6_2_2_1.jsp?lingua=italiano&id=3143. Accessed February 17, 2023.
- 2.Yarmohammadian MH, Rezaei F, Haghshenas A, Tavakoli N. Overcrowding in emergency departments: a review of strategies to decrease future challenges. J Res Med Sci. 2017;22. doi: 10.4103/1735-1995.200277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hurwitz JE, Lee JA, Lopiano KK, Scott A, Keesling J, Tyndall JA. A flexible simulation platform to quantify and manage emergency department crowding. BMC Med Inform Decis Mak. 2014;14:14–50. doi: 10.1186/1472-6947-14-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oray NC, Yanturali S, Atilla R, Ersoy G, Topacoglu H. A new model in reducing emergency department crowding: the electronic blockage system. Turk J Emerg Med. 2016;14:64–70. doi: 10.5505/1304.7361.2014.13285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doupe MB, Chateau D, Chochinov A, et al. Comparing the effect of throughput and output factors on emergency department crowding: a retrospective observational cohort study. Ann Emerg Med. 2018;72(4):410–419. doi: 10.1016/j.annemergmed.2018.04.001 [DOI] [PubMed] [Google Scholar]
- 6.Wang Z, Xiong X, Wang S, Yan J, Springer M, Dellinger RP. Causes of emergency department overcrowding and blockage of access to critical services in Beijing: a 2-year study. J Emerg Med. 2018;5(54):665–673. doi: 10.1016/j.jemermed.2018.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brent R, Magid DJ, Karin V, Solberg LI, Lurie N, Camargo CA. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42(2):173–180. doi: 10.1067/mem.2003.302 [DOI] [PubMed] [Google Scholar]
- 8.Badr S, Nyce A, Awan T, Cortes D, Mowdawalla C, Rachoin J-S. Measures of emergency department crowding, a systematic review. how to make sense of a long list. OAEM. 2022;4(14):5–14. doi: 10.2147/OAEM.S338079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ataman MG, Sarıyer G. Predicting waiting and treatment times in emergency departments using ordinal logistic regression models. Am J Emerg Med. 2021;46:45–50. doi: 10.1016/j.ajem.2021.02.061 [DOI] [PubMed] [Google Scholar]
- 10.Sariyer G, Ataman MG. How machine learning facilitates decision making in emergency departments: modelling diagnostic test orders. Int J Clin Pract. 2021;75(12). doi: 10.1111/ijcp.14980 [DOI] [PubMed] [Google Scholar]
- 11.PRISMA transparent reporting of systematic reviews and meta-analyses, “PRISMA flow diagram”. Available from: https://www.prisma-statement.org//PRISMAStatement/FlowDiagram. Accessed February 17, 2023.
- 12.White BA, Brown DFM, Sinclair J, et al. Supplemented Triage and Rapid Treatment (START) improves performance measures in the emergency department. J Emerg Med. 2012;42(3):322–328. doi: 10.1016/j.jemermed.2010.04.022 [DOI] [PubMed] [Google Scholar]
- 13.Holroyd BR, Bullard MJ, Latoszek K, et al. Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial. Acad Emerg Med. 2007;14:702–708. doi: 10.1197/j.aem.2007.04.018 [DOI] [PubMed] [Google Scholar]
- 14.Weintraub B, Hashemi T, Kucewicz R, et al. Creating an enhanced triage area improves emergency department throughput. Int Emerg Nurs. 2006;32(6):502–505. doi: 10.1016/j.jen.2006.09.006 [DOI] [PubMed] [Google Scholar]
- 15.Afilal M, Yalaoui F, Dugardin F, Amodeo L, Laplanche D, Blua P. Forecasting the emergency department patients flow. J Med Syst. 2016;40(7). doi: 10.1007/s10916-016-0527-0 [DOI] [PubMed] [Google Scholar]
- 16.Martin N, Bergs J, Eerdekens D, Depaire B, Verelst S. Developing an emergency department crowding dashboard: a design science approach. Int Emerg Nurs. 2018;39:68–76. doi: 10.1016/j.ienj.2017.08.001 [DOI] [PubMed] [Google Scholar]
- 17.Amorim FF, de Almeida KJQ, Sanderson Cesar Macedo B, et al. Reducing overcrowding in an emergency department: a pilot study. Rev Assoc Med Bras. 2019;65(12):1476–1481. doi: 10.1590/1806-9282.65.12.1476 [DOI] [PubMed] [Google Scholar]
- 18.Wallingford G, Joshi N, Callagy P, Stone J, Brown I, Shen S. Introduction of a horizontal and vertical split flow model of emergency department patients as a response to overcrowding. J Emerg Nurs. 2018;44(4):345–352. doi: 10.1016/j.jen.2017.10.017 [DOI] [PubMed] [Google Scholar]
- 19.Sethi S, Boulind C, Reeve J, Carney A, Bruijns S. Effect of hospital interventions to improve patient flow on emergency department clinical quality indicators. Emerg Med J. 2020;37:787–792. doi: 10.1136/emermed-2019-208579 [DOI] [PubMed] [Google Scholar]
- 20.Sayah A, Lai-Becker M, Kingsley-Rocker L, Scott-Long T, Kelly O’ C, Lobon LF. Emergency department expansion versus patient flow improvement: impact on patient experience of care. J Emerg Med. 2016;50(2):339–348. doi: 10.1016/j.jemermed.2015.06.068 [DOI] [PubMed] [Google Scholar]
- 21.Edward Pei-Chuan H, Sot Shih-Hung L, Fang C-C, et al. The impact of adding clinical assistants on patient waiting time in a crowded emergency department. Emerg Med J. 2013;30(12):1017–1019. doi: 10.1136/emermed-2012-201611 [DOI] [PubMed] [Google Scholar]
- 22.Sarıyer G, Ataman MG, Kızıloğlu İ. Analyzing main and interaction effects of length of stay determinants in emergency departments. Int J Health Policy Manag. 2020;9(5):198–205. doi: 10.15171/ijhpm.2019.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.OECD.org. Organization for economic co-operation and development; 2019. Available from: https://www.oecd.org/health/primary-care.htm. Accessed February 17, 2023.
- 24.Ansah JP, Ahmad S, Lee LH, et al. Modeling emergency department crowding: restoring the balance between demand for and supply of emergency medicine. PLoS One. 2021;16:e0244097. doi: 10.1371/journal.pone.0244097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mendlovic J, Zalut T, Munter G, Ofer Merin AM, Katz DE, Katz DE. Mixed effect of increasing outflow of medical patients from an emergency department. Isr J Health Policy Res. 2021;10. doi: 10.1186/s13584-021-00491-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Valipoor S, Hatami M, Hakimjavadi H, Swan WA, De Portu G, De Portu G. Data-driven design strategies to address crowding and boarding in an emergency department: a discrete-event simulation study. HERD. 2021;14(2):161–177. doi: 10.1177/1937586720969933 [DOI] [PubMed] [Google Scholar]
- 27.Musacchio N, Guaita G, Ozzello A, et al. Intelligenza artificiale e Big Data in ambito medico: prospettive, opportunità, criticità. JAMD. 2018;21(3):1. [Google Scholar]
- 28.Omar M, Okudan Kremer GE. Dynamic patient grouping and prioritization: a new approach to emergency department flow improvement. Health Care Manag Sci. 2014;19:192–205. doi: 10.1007/s10729-014-9311-1 [DOI] [PubMed] [Google Scholar]
- 29.Tuller D; Ambulance Diversion. Efforts to mitigate ambulance diversion have been effective, but questions remain for future progress. Available from: https://www.healthaffairs.org/do/10.1377/hpb20160602.353150/full/healthpolicybrief_158.pdf. Accessed February 17, 2023.
- 30.Lin C-H, Kao C-Y, Huang C-Y. Managing emergency department overcrowding via ambulance diversion: a discrete event simulation model. J Formos Med Assoc. 2015;114(1):64–71. doi: 10.1016/j.jfma.2012.09.007 [DOI] [PubMed] [Google Scholar]