Abstract
The skin is the largest organ of the body and consists of an epidermis, dermis and subcutaneous adipose tissue. The skin surface area is often stated to be about 1.8 to 2 m2 and represents our interface with the environment; however, when one considers that microorganisms live in the hair follicles and can enter sweat ducts, the area that interacts with this aspect of the environment becomes about 25–30 m2. Although all layers of the skin, including the adipose tissue, participate in antimicrobial defense, this review will focus mainly on the role of the antimicrobial factors in the epidermis and at the skin surface. The outermost layer of the epidermis, the stratum corneum, is physically tough and chemically inert which protects against numerous environmental stresses. It provides a permeability barrier which is attributable to lipids in the intercellular spaces between the corneocytes. In addition to the permeability barrier, there is an innate antimicrobial barrier at the skin surface which involves antimicrobial lipids, peptides and proteins. The skin surface has a low surface pH and is poor in certain nutrients, which limits the range of microorganisms that can survive there. Melanin and trans-urocanic acid provide protection from UV radiation, and Langerhans cells in the epidermis are poised to monitor the local environment and to trigger an immune response as needed. Each of these protective barriers will be discussed.
Keywords: antimicrobial lipids, antimicrobial peptides, barrier function, epidermis, Langerhans cells, melanocytes
1. Permeability Barrier
The skin surface, including the linings and sweat gland ducts, provides anb extensive area for interactions between the skin and elements of its environment, including microorganisms [1]. The epidermis provides a number of protective mechanisms against physical and chemical assaults [2,3,4,5] and microbial colonization and invasion [6,7,8]. The permeability barroer provided by ceramides, cholesterol and free fatty acids in the intercellular spaces of the stratum corneum is the most fundamental of these protective mechanisms.
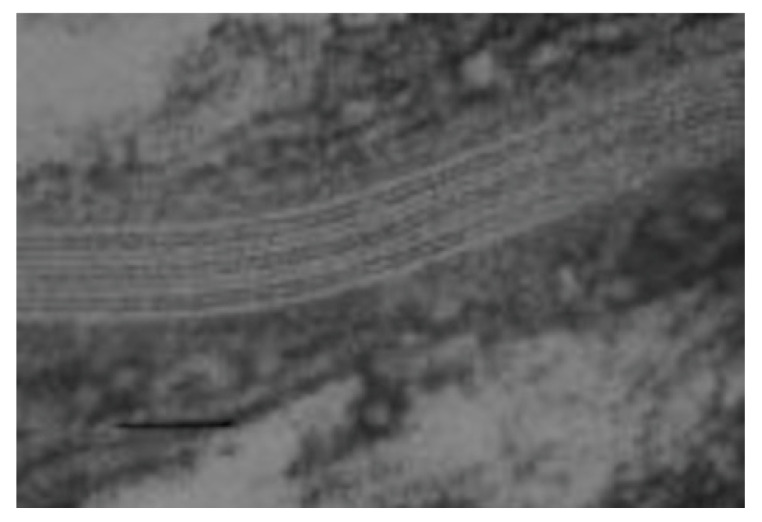
Ceramides were first identified as epidermal components by Nicolaides in 1965 [9]. This was based on an infrared spectrum of a lipid fraction recovered from a thin-layer chromatogram and was added as a footnote to the proof of the manuscript. In the mid- to late 1970s, the group headed by G.M. Gray at Birmingham, UK, made significant progress toward elucidating the structures of the epidermal glucosylceramides from the viable portion of the epidermis and the ceramides from the stratum corneum (reviewed in [5]). This group showed that the epidermal ceramides are structurally heterogenous, and contain normal fatty acids ranging from 14- through 30-carbons in length with the 24- and 26-carbon entities being the most abundant. They also identified 24- and 26-carbon long α-hydroxyacids among the amide-linked fatty acids. The bases included sphingosines and dihydrosphingosines in the chain length range of 16 through 22 carbons. An 18-carbon phytosphingosine was also identified. These studies demonstrated that keratinocytes accumulate increasing amounts of lipid as they differentiate, and that the composition of the lipid alters with differentiation. The stratum corneum lipids consist mainly of ceramides, cholesterol and free fatty acids. Much of the accumulating lipid is packaged into small organelles called lamellar granules [10]. In the uppermost granular cells, the bounding membrane of the lamellar granules fuses into the plasma membrane and the granule contents are extruded into the intercellular space, where they form multilamellar arrays shown in Figure 1 [5]. It was clear from this work that glucosylceramides and sphingomyelin accumulated in the viable portion of the epidermis and were converted to ceramides late at the end of the differentiation process. Porcine epidermis was identified as a good model for human epidermis.
Figure 1.
Transmission electron micrograph of an intercellular space in the stratum corneum [5]. The human skin specimen was fixed with ruthenium tetroxide. Bar = 50 nm.
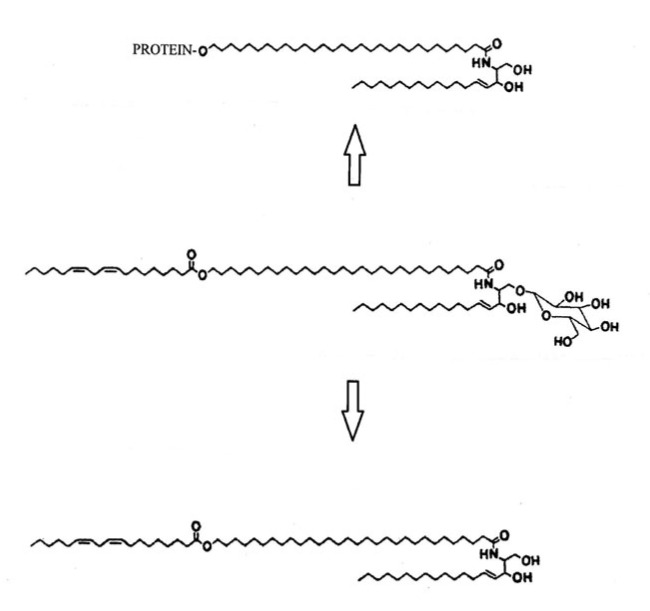
In 1983, the first complete set of epidermal ceramide structures was published, and these structures are shown in Figure 2 [5]. The least polar and most unusual of these ceramides consisted of mainly 30- through 34-carbon ω-hydroxyacids amide-linked to a series of sphingosine and dihydrosphingosine bases with linoleic acid ester-linked to the ω-hydroxyl group [5]. X-ray diffraction studies of stratum corneum have revealed that the intercellular lipids are organized in a predominant repeat distance of approximately 13 nm [11]. This 13 nm repeat has been referred to as the long periodicity phase. Subsequent studies have demonstrated that the linoleate-containing acylceramide, or CER EOS in the nomenclature system of Motta et al., is required for formation of the long periodicity phase [11,12,13]. Electron diffraction has revealed that the lateral lipid packing is predominately orthorhombic [14].
Figure 2.
Ceramide structures from porcine and human stratum corneum [5]. The numbers (1–6) on the right indicate ceramides from porcine stratum corneum, while human ceramides are indicated on the left in the nomenclature of Motta et al. [12]. The porcine ceramide designated as 4/5 separates into two separate bands. The more mobile fraction contains mostly 20- through 28-carbon α-hydroxyacids amide-linked to sphingosine and dihydrosphingosine bases. The less mobile fraction is mostly α-hydroxy palmitic acid amide-linked to the same bases. In the human CER AS, there is an α-hydroxyacid-containing component with a more uniform chain length distribution.
The first complete set of human epidermal ceramides was reported in 2003, and these structures are shown in Figure 2 [5]. In contrast with the ceramides from pig, those from the human have three acylceramides. One of these is essentially the same as the one from pig, but one contains phytosphingosine as the base component and another contains 6-hydroxysphingosine as the base. In addition, the human ceramides include CER NH and CER AH, which are not found among the porcine ceramides. More recently, more detailed analyses of the stratum corneum lipids have been done by HPLC coupled with mass spectrometry [15].
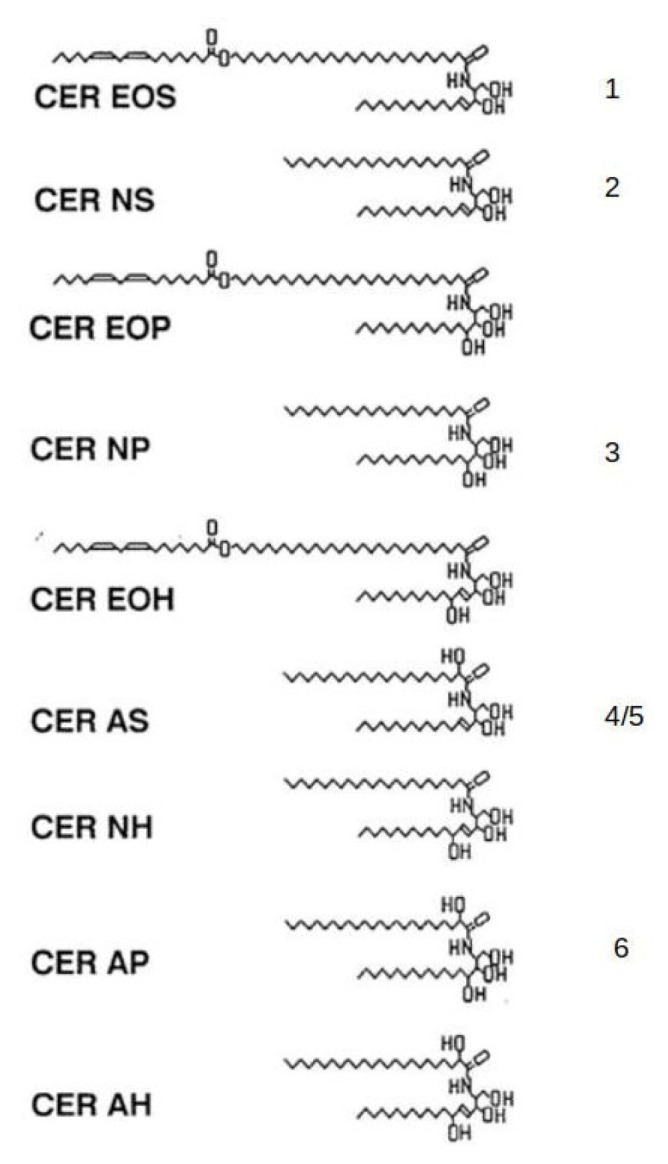
In the late 1980s, covalently bound ω-hydroxyceramides were reported in stratum corneum, and it was proposed that this lipid could be attached to the outer surface of the cornified envelope to form a lipid envelope [16]. Subsequent electron microscopic studies have supported this suggestion. This lipid is thought to be derived from the lamellar granule-associated linoleate-containing acylglucosylceramide shown in Figure 3 [5]. It has been suggested that the corneocyte lipid envelope may contribute to the chemical resistance of the stratum corneum and may also serve as a template upon which the lamellae formed by the free stratum corneum lipids orient themselves. It may have a role in cohesion of the stratum corneum, and it has been suggested that it may provide a semipermeable membrane around the corneocytes allowing passage of water but preventing the loss of other larger hygroscopic substances. It also may serve as a reservoir of the antimicrobial free long-chain bases under certain microbial stresses. The acylglucosylceramide is also the precursor of the acylceramide found in the intercellular spaces of the stratum corneum. The pathway by which the ω-hydroxyceramide becomes covalently attached to the cornified envelope has been reviewed [16].
Figure 3.
The linoleate-rich acylglucosylceramide (center) is the precursor of the acylceramide (bottom) and the covalently bound ω-hydroxyceramide [5]. This lipid is attached to the outer surface of the cornified envelope and has been referred to as the corneocyte lipid envelope, or CLE.
Recently, a 1-O-acylceramide has been reported as a minor component of stratum corneum lipids [17]. The total of this lipid class is about 5% of the total acylceramide, which is 1% or less of the total stratum corneum lipid. These mainly consist of C18:1 sphingosine with amide-linked fatty acids ranging from 14- through 34-carbons in length, and fatty acids ranging from 14- through 30-carbons in length ester-linked to the primary hydroxyl group of the long-chain base [18]. Minor species contained C16:1, C17:1, C18:2 and C19:1 sphingosines. The functional role of this lipid family is not presently known.
An alternative mechanism by which the intercellular lamellae of the stratum corneum are formed has been proposed on the basis of cryo-transmission electron microscopic images [19,20]. In this alternative, there are no lamellar granules. There is membrane continuity from the endoplasmic reticulum through the intercellular lamellae. Five steps or stages with different lipid composition and organization have been identified in this membrane unfolding process. The cryoelectron microscopic images show a granular pattern reflecting the secretory apparatus of the uppermost granular cell. This makes a transition to a lamellar pattern with a 50–55 angstrom periodicity. This undergoes another transition to a lamellar pattern with a 20–25 angstrom periodicity between the first and second corneocytes at the bottom of the stratum corneum. Above this level of the stratum corneum, the periodicity of the lamellae is 110–120 angstroms.
2. Roles of Filaggrin
Filaggrin contributes to the permeability barrier, the water holding capacity of the stratum corneum and protection against UVB.
Profilaggrin is the highly phosphorylated, histidine-rich protein that constitutes the bulk of the keratohyalin granules [21]. It is also rich in arginine. It has a high molecular weight (greater than 220,000) and is highly phosphorylated. In the late stages of differentiation, profilaggrin is dephosphorylated and proteolytically converted into filaggrin (filament-aggregating protein) with a molecular weight of 37,000 [22]. Ten to twelve filaggrin molecules are produced from one profilaggrin molecule [22]. As the cornified envelope is forming, the positively charged filaggrin molecules bind to and aggregate the keratin filaments, causing flattening of the cell to form the corneocyte. After aggregation of the keratin filaments, the arginines in filaggrin undergo conversion to citruline through the action of peptidylarginine deiminases 1 and 3 [23]. This reduces the charge of the filaggrin molecule and allows it to unwind from the aggregated keratin, and it is proteolytically degraded to its component amino acids by a combination of bleomycin hydrolase, caspase −14 and calpain 1 [24,25]. The free glutamine released from filaggrin spontaneously cyclizes to form pyrrolidine carboxylic acid (PCA), and the histidine is converted to trans-urocanic acid by histidine ammonia-lyase [26]. PCA, urocanic acid and the other amino acids released by degradation of filaggrin are the major components of what has been called the natural moisturizing factor. The high concentration of small molecules within the corneocyte results in a high osmotic strength, which allows the corneocytes to effectively retain water. The lipid envelope on the outside of the cornified envelope and the intercellular lipid lamellae probably assist in holding water inside the corneocytes.
Mutations of the fillaggrin gene result in ichthyosis vulgaris and atopic dermatitis [27,28]. Decreased barrier function associated with these conditions can lead to contact allergies [29,30]. Atopic dermatitis often leads to asthma, food allergies and allergic rhinitis [31].
3. Antimicrobial Lipids and Lysosome
The pH of the skin surface of healthy adults is below 5 [8]. Several factors contribute to this acidification. One of these is the liberation of fatty acids from sebaceous triglycerides by microbial lipases in the follicles and on the skin surface [32,33]. The production of short chain fatty acids by some of the commensal microorganisms on the skin is a second mechanism for acidification [34,35,36]. The sodium–hydrogen exchanger 1 is another mechanism for lowering the pH of the stratum corneum [37]. Finally, production of lactic acid through anaerobic glycolysis as cells move outward from the basal layer will contribute to lowering the pH [38]. The acidic pH of the skin surface limits the range of microorganisms that can survive there because most microorganisms grow best at a more neutral pH.
The surface of the skin is relatively dry and nutrient-poor, which also limits the microorganisms that can survive there [39]. Some of the commensals that are part of the microbiome produce antimicrobial metabolites that protect against potential pathogens [34,39,40,41]. The skin microbiome interacts with the epidermis to influence the physical, chemical and innate immune barriers. These interactions have recently been reviewed [42,43].
The dermis contains sebaceous glands and sweat glands embedded in the reticular dermis, and both types of glands secrete their products onto the skin surface. The sebaceous glands and sweat glands secrete lipids and aqueous sweat onto the skin surface. Both of these secretions provide some antimicrobial components. Human sweat contains lysozyme, and apocrine sweat contains the antifungal lipid, undecylenic acid [44,45,46].
It has long been recognized that lipids at the skin surface have antimicrobial properties [47,48]. Burtenshaw demonstrated that ethyl ether extracts of the skin surface contained material that could kill Staphylococcus aureus and some other bacteria. He speculated that this might be attributed to free fatty acids and demonstrated that some free fatty acids and mixtures of fatty acids were antimicrobial. Several years later, the human sebaceous fatty acid fraction was shown to have antifungal activity against Microsporum audouini, the fungus that causes ringworm of the scalp [49]. Upon fractionation, the odd-carbon short chain fatty acids (C7:0, C9:0 and C11:0) were identified as the active components. This explained Rothman’s observation that young children who got ringworm of the scalp, cradle cap, often had recurrence of this infection until they reached puberty, which is associated with a major increase in sebum secretion. As noted previously, triglycerides are synthesized in the sebaceous glands, and fatty acids are released from these sebaceous triglycerides through the action of microbial lipases in the follicle and on the skin surface [34]. Subsequently, lauric acid (C12:0) and monolaurin were found to be uniquely antimicrobial against a range of Gram-positive bacteria [48]. The previous work of Rothman and associates demonstrated that lauric acid is among the fatty acids that are liberated from sebaceous triglycerides, and this was subsequently confirmed by gas–liquid chromatographic analysis [49,50]. Both lauric acid and sapienic acid (C16:1Δ6), one of the more abundant sebaceous fatty acids, were shown to be capable of killing Gram-positive bacteria as well as the Gram-negative gingival pathogens Fusarium gingivalis and Porphyromonas gingivalis [48]. Sebacous lipids are present in human saliva [48]. Under conditions where lauric acid produced nearly complete killing, other saturated fatty acids known to be present in human sebum (C8:0, C10:0, C14:0, C16:0, C18:0 and C20:0) were inactive or had some degree of bacteriostatic activity. Lauric acid also has activity against fungi and enveloped viruses [51,52]. Sapienic acid has not yet been tested for antiviral activity.
Monolaurin is available from numerous sources as a dietary supplement. One study sought the benefits of monolaurin use [53]. Three peer-reviewed cases in which human infections were successfully treated with monolaurin were found; however, these were all cases of topical infections. It was suggested that taking monolaurin orally may have no benefit other than the nutritional value. However, another study suggested that monolaurin may provide protection against COVID-19 [54]. In this study, 51 healthcare workers who were about to start working with COVID-19 patients were recruited. Blood samples were collected after enrollment. Within three weeks of working with COVID-19 patients, 24 of these subjects had contracted COVID-19. Metabolomic analysis identified 322 low molecular weight metabolites. Of these, 21 were elevated in the subjects who did not become infected relative to those who were infected. One of these molecules was monolaurin. A second molecule in this protective set was N,N-dimethylglycine. It was noted that these two molecules are available as nutritional supplements, which could potentially provide resistance to infection by SARS-CoV-2.
Half of the lipid molecules in the intercellular spaces are ceramides containing sphingosine, dihydrosphingosine, phytosphingosine or 6-hydroxysphingosine as the long-chain base component, and the cornified envelope of the corneocytes has a covalently attached ω-hydroxyceramide containing the same long-chain bases [16]. Ceramidase activity capable of hydrolyzing the amide linkage of ceramides to release free fatty acid and long-chain base have been identified in epidermis [7]. Free long-chain bases have been detected in human stratum corneum [55]. Free long-chain bases have been shown to be potent antimicrobial agents against Gram-positive bacteria, some Gram-negative bacteria and Candida albicans [56,57]. Several observations suggest that the covalently bound ω-hydroxyceramides in the corneocyte lipid envelope may serve as a source of free long-chain base. For one thing, as essential fatty acid deficiency developed in young pigs, the transepidermal water loss (TEWL) increased, and this increase in TEWL was accompanied by a decrease in the amount of covalently bound ω-hydroxyceramide with an increasing amount of covalently bound ω-hydroxyacid, suggesting ceramidase action [57]. In addition, in both atopic dermatitis and psoriasis, where barrier function is compromised, the proportion of covalently bound ω-hydroxyceramides is reduced and the proportion of covalently bound ω-hydroxyacids is elevated compared to normal control stratum corneum [16,57]. This may be a defense mechanism to provide increased antimicrobial protection in the face of a compromised barrier [16].
4. Antimicrobial Peptides
There are also antimicrobial peptides at the skin surface. The cathelicidin LL-37 is synthesized by keratinocytes and is the only known cathelicidin in human epidermis. The name, LL-37, is based on the fact that the sequence of 37 amino acids begins with two leucines at the amino terminal end [58]. At physiological pH, LL-37 has a net positive charge of +6. It has been shown by means of nuclear magnetic resonance that residues 2–31 form two helical regions with a bend at residue 15 [59]. It was shown that the entire amphipathic helical region associated with the negatively charged surface of micelles. This is in support of the mechanistic possibility that the LL-37 binds to the negatively charged membrane of a potential pathogen while the less structured carboxyl end of the molecule disrupts the integrity of the membrane. In normal human epidermis, the level of LL-37 is relatively low, but production is increased in response to inflammatory conditions or infection [60]. It has been shown that LL-37 is present in lamellar granules [61]. Lamellar granules, which deliver their contents to the intercellular space as described above, have also been shown to contain lysozyme [62]. LL-37 has broad antimicrobial activity against a variety of Gram-positive and Gram-negative bacteria, fungi and enveloped viruses [63].
There are four major antimicrobial β-defensins expressed in human epidermis: hBD1, hBD2, hBD3 and hBD4. The beta defensins are all cationic and contain six cysteine residues which form three disulfide linkages locking the peptide into a β-sheet structure [64]. Like cathelicidins, the defensins have broad antimicrobial activity against a range of Gram-positive bacteria, Gram-negative bacteria, fungi and some enveloped viruses [64,65]. HBD1 contains 36 amino acids and has a net charge of +4 at physiological pH [62]. The hDB2 peptide contains 36 amino acids and has a net charge of +6 [65]. Gram-negative bacteria and fungi are killed by hDB2 at low concentrations, but Gram-positive bacteria are much more resistant [66]. It has been shown that hBD2 is packaged into lamellar bodies [66]. This is likely the mechanism by which the cathelicidins and the β-defensins are delivered to the stratum corneum. Fatty acids liberated from sebaceous triglycerides by microbial lipases upregulate hBD2 [67]. The hDB3 peptide contains 44 amino acid residues and has a net charge of +11 [64]. Gram-positive and Gram-negative bacteria and fungi are effectively killed by hDB3. The hDB4 molecule contains 47 amino acids and has a net charge of +7 [62]. Some Gram-negative bacteria and some Gram-positive bacteria were killed with low doses of hBD4, while others were much more resistant. The hBD2, hBD3 and hBD-4 have all been experimentally upregulated when primary keratinocytes in culture were exposed to calcium to induce differentiation [68]. They were also upregulated by exposure to bacteria, interleukin-1 and TNF-alpha, or the phorbol ester, 12-O-tetradecanoyl-phorbol-13-acetate (TPA) [69]. TPA induces an inflammatory response. hBD1 is constituently expressed in human epidermis, but its expression can be increased by the presence of microbial molecules such as lipopolysaccharide. hBD2, hBD3 and hBD4 are expressed at low levels under unchallenged conditions, but expression can be induced by exposure to inflammatory conditions or microbial components including viruses. In addition to their direct antimicrobial action, hBD-1 can act as a chemokine to attract immune cells to the epidermis, thereby linking innate and active immunity [70]. As with cathelicidin LL-37, the defensins are thought to interact with negatively charged microbial or viral membranes by virtue of their positive charge.
A third category of antimicrobial peptides is a family of dermcidin-derived peptides. The dermcidin precursor is constitutively produced in eccrine sweat glands [68]. More recently, it has been reported that the dermcidin precursor is also synthesized by human sebocytes [71]. The dermcidin precursor contains 110 amino acids and is negatively charged [72]. The precursor protein is acted upon by cathepsin D in sweat to liberate two antimicrobial peptides from the carboxy terminal end [73]. DCD-1 contains 47 amino acids and DCD-1L contains an additional leucine. Both DCD-1 and DCD-1L have a net charge of −2. The peptides were highly active against Escherischia coli, Escherischia faecalis, S.taphylococcus aureus and Candida albicans [72]. DCD-1L was also shown to be active against Acinetobacter baumannii, including some antibiotic-resistant strains [74,75]. When sweat was collected from the skin surface, 14 additional DCD-derived peptides were identified [76]. The number of amino acids in these peptides ranged from 24 through 46, and the charge ranged from −2 to +1. This truncation is most likely mediated by proteases on the stratum corneum surface. The proposed mechanism of action requires zinc [77]. The monomeric DCD-1L molecules in sweat are unstructured. The positively charged amino terminus binds electrostatically to the negatively charged phospholipids of the microbial membrane and this interaction induces a transition from unstructured random coil to an alpha-helical conformation. Additional DCD-1L molecules aggregate to an oligomeric state which is stabilized by zinc. This aggregate forms a pore which results in cell death. DCD-1L has been shown to form a hexameric complex before insertion into the microbial membrane [77]. The orientation of this channel within the membrane is influenced by the membrane lipid composition [78,79]. In recent years, dermcidins have been implicated in the etiology of some cancers [80]. Seriniquinones, a class of drug derived from a marine bacterium, were found to be active against a number of melanoma cell lines [81]. The mechanism of action was inactivation of dermcidins.
Yet another antimicrobial protein synthesized constitutively and secreted by keratinocytes is the 14.5 kDa RNase 7 [82]. RNase 7 is effective in killing a range of Gram-positive bacteria, Gram-negative bacteria and yeast. Although it is constitutively expressed at a high level, higher expression can be induced by inflammatory mediators. RNase 7 is secreted by keratinocytes and accumulates at the skin surface. The antibacterial activity of RNase 7 is independent of the enzymatic activity and is localized to the amino terminal end of the molecule [83]. Peptides derived from the amino terminal end of human RNase 7 are highly active against C. albicans. The mechanism of action involves first binding to the cell wall followed by membrane permeabilization [84]. RNase 7 can bind self-DNA, which could be released from damaged keratinocytes, and activate keratinocytes to produce and secrete the chemokine, IP-10. IP-10 attracts a range of immune cells to the epidermis, and this enhances the antiviral defense [83].
The S100 antimicrobial proteins are so named because they are soluble in 100% saturated aqueous ammonium sulfate at neutral pH [85]. There are currently 25 known S100 proteins expressed among vertebrates [86]. These proteins are generally small (10–12 KDa). They have two looped calcium binding sites, each of which is flanked by alpha-helical domains. There is a hinge domain between the central two alpha-helical domains, and there is a high degree of amino acid sequence homology from the amino terminal end through the alpha-helical domain closest to the carboxyl terminal end. The amino acid sequence near the amino terminus is variable. The active forms exist as antiparallel dimers, which are most often homodimers. Three of these S100 proteins (psoriasin, calmodulin and koebnerisin) are expressed in human keratinocytes. The S100 proteins play numerous roles in the immune system [87]. It has been suggested that certain S100 proteins collected by nasal swabbing could be useful as a prognostic marker of COVID-19 infection.
Psoriasin (S100A7) is expressed at low levels in normal human keratinocytes, but its expression is much upregulated in psoriatic epidermis and in atopic dermatitis [88,89]. Psoriasin is most effective in killing E. coli, but at higher concentrations it can kill other bacteria. At pH below 6, it killed E. coli and Bacillus megaterium by membrane permeabilizing and pore formation; however, at neutral pH it killed E. coli without permeabilization. In psoriatic subjects, the level of psoriasin in serum was significantly elevated relative to that in control serum; however, the degree of elevation did not correlate with disease severity [90]. In several superficial fungal infections, it has been shown that psoriasin is elevated [91,92,93]. Although direct activity against fungus was not demonstrated, it was found that psoriasin binds to β-glucan. This is a component of the C. albicans cell wall, and psoriasin thereby prevents C. albicans from adhering to the host surface. Subjects with anorexia nervosa do not suffer skin infections, which are common in generally malnourished individuals. This unusual disease resistance may be attributed, at least in part, to upregulation of both psoriasin and RNase 7 [94,95].
The active form of calprotectin is a heterodimer (S100A8/A9) [65]. Calprotectin, as well as the other S100 proteins, is a calcium-binding protein; however, it can also bind other divalent metal cations including Mn+2, Cu+2, Fe+2, Ni+2 and Zn+2 [96]. In skin wounding or infection, calprotectin provides what is called nutritional immunity by sequestering these essential nutrients [97]. Calprotectin has been shown to be effective in killing S. aureus, S. epidermidis, E. coli and C. albicans in vitro [97]. The C-terminal end of the one calprotectin chain has an amino acid sequence identical to the N-terminal end of neutrophil immobilizing factors. This may be significant for attracting granulocytes [96]. The severity of psoriasis is subjectively evaluated by the Psoriasis Area and Severity Index. The level of calprotectin at the psoriatic skin surface has been shown to correlate strongly with this index.
Koebnerisin (S100A15) has an amino acid sequence very similar to that of psoriasin [63]. It probably contributes to nutritional immunity in a manner similar to calprotectin. Koebnerisin is overexpressed in several inflammatory skin conditions including psoriasis, rosacea, hidradenitis suppurativa (acne inversa) and acne vulgaris [65,97,98].
SPINK9 is an inhibitor of kallikrein-like proteases and is involved in the regulation of desquamation. It is upregulated in type 1 diabetes [99]. Six N-terminal variants of SPIMK9 have been identified in human stratum corneum [100]. Three of these variants kill various strains of E. coli, but not yeast or other bacteria.
Increasing development of antibiotic-resistant microorganisms creates a need to identify new antimicrobials and, in this regard, antimicrobial peptides have gotten the attention of the pharmaceutical and agricultural industries [101,102,103,104,105]. More than 3000 naturally occurring antimicrobial peptides have been identified, and there is a database containing 24,243 natural and synthetic antimicrobial peptides [106]. More than 60 antimicrobial peptides have been approved by the FDA [107]. The natural antimicrobial peptides are susceptible to proteolytic degradation and are hemolytic [108,109]. The synthetic antimicrobial peptides are based on natural antimicrobial peptides in attempts to minimize toxicity, improve stability and retain or enhance activity [108,109,110,111].
5. Langerhans Cells
In human epidermis, the link between innate immunity and adaptive immunity is provided largely by the Langerhans cells [112,113]. Although they can be found throughout most of the viable epidermis, Langerhans cells are most abundant in the spinous layer [114]. Langerhans cells are dendritic, and the dendrites contact nearby keratinocytes. The extension and retraction of the dendrites is a dynamic process called dendrite surveillance extension and retraction cycling [115,116]. This process allows Langerhans cells to survey the environment throughout the viable epidermis and, by penetrating through the tight junctions between granular cells, to reach the stratum corneum [110,114,115,116]. Langerhans cells are equipped with various pattern recognition receptors including toll-like receptors (TLR2, TLR4 and TLR5) and the mannose-specific lectin langerin [110,111]. The toll-like receptors provide for bacterial recognition, while langerin recognizes certain viruses. Under normal conditions, Langerhans cells collect endogenous antigens and antigens of the microbiome and migrate to skin-draining lymph nodes [112]. Under these conditions, presentation of the antigens to naive T cells results in tolerance. The population of Langerhans cells in the epidermis under nonstressed conditions is maintained by in situ replication of Langerhans cells in the epidermis [112]. In cases of infection, the naive T cells in the lymph nodes are activated to produce antibodies against pathogens. During inflammation, some of the Langerhans cells that replace those migrating to lymph nodes arise from monocytes from the circulation [111]. Whether antigen presentation results in immune response or tolerance is dependent upon the state of maturity of the Langerhans cell [113]. In aged human skin, among other things, the number of Langerhans cells in the epidermis is decreased, and the incidence of skin infections increases [117,118].
6. Melanocytes
Melanocytes are dendritic cells found in the basal layer of the interfollicular epidermis [118]. They contain lysosome-related organelles called melanosomes which are the sites of pigment synthesis [119,120,121]. Melanin synthesis begins by the oxidation of tyrosine to DOPA and the oxidation of DOPA to DOPAquinone. These two oxidations are catalyzed by tyrosinase or either of two paralogues (Trp1 and Trp2) to produce the pigment eumelanin [120,121]. Tyrosinase is a copper-requiring enzyme [119]. Trp 1 is thought to also be a copper-requiring enzyme, while Trp 2 requires zinc. These tyrosinase paralogues determine the type and amount of melanin produced. A series of spontaneous reactions leads from DOPAquinone to the brown-black pigment eumelanin. Alternatively, DOPAquinone can react with cysteine to form cysteinylDOPA, which leads to formation of the yellow-red pigment pheomelanin. Numerous endogenous molecules can influence the activity of melanosomes [121]. Melatonin inhibits melanin formation by lowering tyrosinase activity levels [121]. The melanosomes travel through the dendrites and are transferred into the keratinocytes. Several mechanisms have been proposed for the actual transfer from the melanocyte dendrite into the cytoplasm of the keratinocyte [122,123]. Melanin/pheomelanin provides a degree of protection against ultraviolet-induced damage. Consistent with the role of protecting against UV-induced DNA damage, the melanosomes tend to cluster into a cap above the nucleus [123].
In addition to protective pigmentation, trans-urocanic acid produced during degradation of filaggrin is an ultraviolet chromophore [124]. When it absorbs UV, it isomerizes to cis-urocanic acid.
Acknowledgments
The authors would like to thank Nancy Wertz for helping in the preparation of this manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors have no conflict of interest.
Funding Statement
There was no funding for the preparation of this manuscript.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Gallo R.L. Human skin is the largest epithelial surface for interaction with microbes. J. Investig. Dermatol. 2017;137:1213–1214. doi: 10.1016/j.jid.2016.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwiecien K., Zegar A., Jung J., Brzoza P., Kwitniewski M., Godlewska U., Grygier B., Kwiecinska P., Morytko A., Cichy J. Architecture of antimicrobial skin defense. Cytokine Growth Factor Rev. 2019;49:70–84. doi: 10.1016/j.cytogfr.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Schurer N.Y., Plewig G., Elias P.M. Stratum corneum lipid function. Dermatologica. 1991;183:77–94. doi: 10.1159/000247644. [DOI] [PubMed] [Google Scholar]
- 4.van Smeden J., Bouwstra J.A. Stratum corneum lipids: Their role for the skin barrier function in healthy subjects and atopic dermatitis patients. Curr. Probl. Dermatol. 2016;49:8–26. doi: 10.1159/000441540. [DOI] [PubMed] [Google Scholar]
- 5.Wertz P.W. Roles of lipids in the permeability barriers of skin and oral mucosa. Int. J. Mol. Sci. 2021;22:5229. doi: 10.3390/ijms22105229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herman A., Herman A.P. Antimicrobial peptides activity in the skin. Skin Res. Tech. 2018;25:111–117. doi: 10.1111/srt.12626. [DOI] [PubMed] [Google Scholar]
- 7.Wertz P. Lipids and the permeability and antimicrobial barriers of the skin. J. Lipids. 2018;2018:5954034. doi: 10.1155/2018/5954034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Proksch E. pH in nature, humans and skin. J. Dermatol. 2018;45:1044–1052. doi: 10.1111/1346-8138.14489. [DOI] [PubMed] [Google Scholar]
- 9.Nicolaides N. Skin lipids II. Lipid class composition of samples from various species and anatomical locations. J. Am. Oil Chem. Soc. 1965;42:691–702. doi: 10.1007/BF02540042. [DOI] [PubMed] [Google Scholar]
- 10.Wertz P.W. Epidermal lamellar granules. Skin Pharmacol. Physiol. 2018;31:262–268. doi: 10.1159/000491757. [DOI] [PubMed] [Google Scholar]
- 11.Bouwstra J.A., Gooris G.S., van der Spek J.A., Bras W. Structural investigations of human stratum corneum by small-angle X-ray scattering. J. Investig. Dermatol. 1991;97:1005–1012. doi: 10.1111/1523-1747.ep12492217. [DOI] [PubMed] [Google Scholar]
- 12.Motta S., Monti M., Sesana S., Caputo R., Carelli S., Ghisoni R. Ceramide composition of the psoriatic scale. Biochim. Biophys. Acta. 1993;1182:147–151. doi: 10.1016/0925-4439(93)90135-N. [DOI] [PubMed] [Google Scholar]
- 13.Mojumdar E.H., Gooris G.S., Groen D., Barlow D.J., Lawrence M.J., Deme B., Bouwstra J.A. Stratum corneum lipid matrix: Location of acylceramide and cholesterol in the unit cell of the long periodicity phase. Biochim. Biophys. Acta. 2016;1858:1926–1934. doi: 10.1016/j.bbamem.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Pilgram G.S., Engelsma-van Pelt A.M., Koerten H.K., Bouwstra J.A. The effect of two azones on the lateral lipid organization of human stratum corneum and its permeability. Pharm. Res. 2000;17:796–802. doi: 10.1023/A:1007547906856. [DOI] [PubMed] [Google Scholar]
- 15.Kawana M., Mlyamoto M., Ohno Y., Kihara A. Comparative profiling and comprehensive quantification of stratum corneum ceramides in humans and mice by LC/MS/MS. J. Lipid Res. 2020;61:884–895. doi: 10.1194/jlr.RA120000671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wertz P.W. Lipid metabolic events underlying the formation of the corneocyte lipid envelope. Skin Pharmacol. Physiol. 2021;34:38–50. doi: 10.1159/000513261. [DOI] [PubMed] [Google Scholar]
- 17.Rabinonet M., Bayerie A., Marsching C., Jennemann R., Grone H.-J., Yidiz Y., Wachten D., Shaw W., Shayman J.A., Sandhoff R. 1-O-acylceramides are natural components of human and mouse epidermis. J. Lipid Res. 2013;54:3312–3321. doi: 10.1194/jlr.M040097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin M.-H., Miner J.H., Turk J., Hsu F.-F. Linear ion-trap MSn with high-resolution MS reveals structural diversity of 1-O-acylceramide family in mouse epidermis. J. Lipid Res. 2017;58:772–782. doi: 10.1194/jlr.D071647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Narangifard A., Wennberg C.L., den Hollander L., Iwai I., Han H., Lundborg M., Masich S., Lindahl E., Daneholt B., Norlen L. Molecular reorganization during the formation of the human skin barrier studied in situ. J. Investig. Dermatol. 2021;141:1243–1253. doi: 10.1016/j.jid.2020.07.040. [DOI] [PubMed] [Google Scholar]
- 20.Norlen L., Lundborg M., Wennberg C., Narangifard A., Daneholt B. The skin’s barrier: A cryo-EM based overview of its architecture and stepwise formation. J. Investig. Dermatol. 2022;147:285–292. doi: 10.1016/j.jid.2021.06.037. [DOI] [PubMed] [Google Scholar]
- 21.Fleckman P., Dale B.A., Holbrook K.A. Profilaggrin, a high-molecular-weight prercursor of filaggrin in human epidermis and cultured keratinocytes. J. Investig. Dermatol. 1985;85:507–512. doi: 10.1111/1523-1747.ep12277306. [DOI] [PubMed] [Google Scholar]
- 22.Drislane C., Irvine A.D. The role of filaggrin in atopic dermatitis and allergic disease. Ann. Allergy Asthma Immunol. 2020;124:36–43. doi: 10.1016/j.anai.2019.10.008. [DOI] [PubMed] [Google Scholar]
- 23.Cau L., Mechin M.-C., Simon M. Peptidylarginine deiminases and deiminated proteins at the epidermal barrier. Exp. Dermatol. 2018;27:852–858. doi: 10.1111/exd.13684. [DOI] [PubMed] [Google Scholar]
- 24.Kim Y., Lim K.-M. Skin barrier dysfunction and filaggrin. Arch. Pharm. Res. 2021;44:36–49. doi: 10.1007/s12272-021-01305-x. [DOI] [PubMed] [Google Scholar]
- 25.Barrett J.G., Scott I.R. Pyrrolidone carboxylic acid synthesis in guinea pig epidermis. J. Investig. Dermatol. 1983;81:122–124. doi: 10.1111/1523-1747.ep12542975. [DOI] [PubMed] [Google Scholar]
- 26.Scott I.R. Factors controlling the expressed activity of histidine ammonia-lyase in the epidermis and the resulting accumulation of urocanic acid. Biochem. J. 1981;194:829–938. doi: 10.1042/bj1940829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoober J.K., Eggink L. The discovery and function of filaggrin. Int. J. Mol. Sci. 2022;23:1455. doi: 10.3390/ijms23031455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Novak-Bilic G., Vucic M., Japundzic I., Mestrovic-Stefekov J., Stanic-Duktaj S., Lugovic-Mihic L. Irritant and allergic contact dermatitis-skin lesion characteristics. Acta Clin. Croat. 2018;57:713–720. doi: 10.20471/acc.2018.57.04.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elhaji Y., Sasseville D., Pratt M., Asai Y., Matheson K., McLean W.H.I., Hull P.R. Filaggrin gene loss-of-function mutations constitute a factor in patients with multiple contact allergies. Contact Dermat. 2019;80:354–358. doi: 10.1111/cod.13268. [DOI] [PubMed] [Google Scholar]
- 30.Leung D.Y.M., Berdyshev E., Goleva E. Cutaneous barrier dysfunction in allergic diseases. J. Allergy Clin. Immunol. 2020;145:1485–1497. doi: 10.1016/j.jaci.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weidinger S., Beck L.A., Bieber T., Kabashima K., Irvine A.D. Atopic dermatitis. Nat. Rev. Dis. Primers. 2018;4:1. doi: 10.1038/s41572-018-0001-z. [DOI] [PubMed] [Google Scholar]
- 32.Chen Z., Alonzo F. Bacterial lipolysis of immune-activating ligands promoites evasion of innate defenses. Proc. Natl. Acad. Sci. USA. 2019;116:3764–3773. doi: 10.1073/pnas.1817248116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li W., Zhang Z.-W., Luo Y., Liang N., Pi X.-X., Fan T.-M. Molecular epidemiology, in vitro susceptibility and exoenzyme screening of Malassezia clinical isolates. J. Med. Microbiol. 2020;69:436–442. doi: 10.1099/jmm.0.001161. [DOI] [PubMed] [Google Scholar]
- 34.Sweeney M.H., Kalan L.R. Living in your skin: Microbes, molecules, and mechanisms. Infect. Immunol. 2021;89:1–18. doi: 10.1128/IAI.00695-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schlatterer K., Peschei A., Kretschmer D. Short-chain fatty acid and FFAR2 activation-A new option for treating infections? Front. Cell. Infect. Microbiol. 2021;11:785833. doi: 10.3389/fcimb.2021.785833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang J.J., Chang T.-W., Jiang Y., Kao H.-J., Chiou B.-H., Kao M.-S., Huang C.-M. Commensal Staphylococcus aureus provokes immunity to protect against skin infections of methicillin-resistant Staphylococcus aureus. Int. J. Mol. Sci. 2018;19:1290. doi: 10.3390/ijms19051290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dang E., Man G., Lee D., Crummrine D.A., Mauro T.M., Elias P.M., Man M.-Q. Mutations in 3β-hydroxysteroid-δ8, δ7-isomerase paradoxically benefit epidermal permeability barrier homeostasis in mice. Exp. Dermatol. 2021;30:384–389. doi: 10.1111/exd.14236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rabinowitz J.D., Enerback S. Lactate: The ugly duckling of energy metabolism. Nat. Metab. 2020;2:566–571. doi: 10.1038/s42255-020-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rinnerthaler M., Richter K. The influence of calcium on the skin pH and epidermal barrier during aging. Curr. Probl. Dermatol. 2018;54:79–86. doi: 10.1159/000489521. [DOI] [PubMed] [Google Scholar]
- 40.Wertz P.W., de Szalay S. Innate antimicrobial defense of skin and oral mucosa. Antibiotics. 2020;9:159. doi: 10.3390/antibiotics9040159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Byrd A.L., Belkaid Y., Segre J.A. The human skin microbiome. Nat. Rev. Microbiol. 2018;16:143–155. doi: 10.1038/nrmicro.2017.157. [DOI] [PubMed] [Google Scholar]
- 42.Harris-Tryon T.A., Grice E.A. Microbiota and maintenance of skin barrier function. Science. 2022;376:940–945. doi: 10.1126/science.abo0693. [DOI] [PubMed] [Google Scholar]
- 43.Kim M., Lee H.-J. Skin barrier function and the microbiome. Int. J. Mol. Sci. 2022;23:13071. doi: 10.3390/ijms232113071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nakayashiki N. Sweat protein components tested by SDS-polyacrylamide gel electrophoresis followed by immunoblotting. Tohoku J. Exp. Med. 1990;161:25–31. doi: 10.1620/tjem.161.25. [DOI] [PubMed] [Google Scholar]
- 45.Wang J., He A., Zhu Y., Zhou G., Zhang T. Isolation, culture, and identification of ceruminous gland cells. J. Mol. Histol. 2022;53:227–237. doi: 10.1007/s10735-021-10040-y. [DOI] [PubMed] [Google Scholar]
- 46.Shapiro A.L., Rothman S. Undecylenic acid in the treatment of dermatomycoses. Arch. Dermatol. Syphilol. 1945;52:166–171. doi: 10.1001/archderm.1945.01510270024004. [DOI] [Google Scholar]
- 47.Burtenshaw J.M.L. The mechanism of self-disinfection of the human skin and its appendages. Epidemiol. Infect. 1942;42:189–210. doi: 10.1017/S0022172400035373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fischer C.L. Antimicrobial activity of host-derived lipids. Antibiotics. 2020;9:75. doi: 10.3390/antibiotics9020075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rothman S., Smiljanic A.M., Weitkamp A.W. Mechanism of spontaneous cure in puberty of ringworm of the scalp. Science. 1946;104:201–203. doi: 10.1126/science.104.2696.201. [DOI] [PubMed] [Google Scholar]
- 50.James A.T., Wheatley V.R. Studies of sebum 6. The determination of the component fatty acids of human forearm sebum by gas-liquid chromatography. Biochem. J. 1956;63:269–273. doi: 10.1042/bj0630269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.da Silva Lima R., Block J.M. Coconut oil: What do we really know about it so far? Food Qual. Saf. 2019;3:61–72. doi: 10.1093/fqsafe/fyz004. [DOI] [Google Scholar]
- 52.Joshi S., Kaushik V., Gode V., Mhaskar S. Coconut oil and immunity: What do we really know about it so far. J. Assoc. Physicians India. 2020;68:67–72. [PubMed] [Google Scholar]
- 53.Barker L.A., Bakkum B.W., Chapman C. The clinical use of monolauren as a dietary supplement: A review of the literature. J. Chiropr. Med. 2019;18:305–310. doi: 10.1016/j.jcm.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Barberis E., Amede E., Tavecchia M., Marengo E., Cittone M.G., Rizzi E., Pedrinwlli A.R., Tonello S., Minisini R., Pirisi M., et al. Understanding protection from SARS-CoV-2 using metabolomics. Sci. Rep. 2021;11:13796. doi: 10.1038/s41598-021-93260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Berdyshev E., Bronova I., Bronoff A.S., Goleva E., Leung D.Y.M. Human keratinocytes synthesize ultra long-chain sphingoid bases (Up to C28) that are abundant in skin stratum corneum. FASEB J. 2020;34:s1.03396. doi: 10.1096/fasebj.2020.34.s1.03396. [DOI] [Google Scholar]
- 56.Bibel D.J., Aly R., Shinefield H.R. Sphingosines: Antimicrobial barriers of the skin. Acta Derm. Venereol. 1993;73:407–411. doi: 10.2340/0001555573407411. [DOI] [PubMed] [Google Scholar]
- 57.Fischer C.L., Wertz P.W. Effects of endogenous lipids on the skin microbiome. In: Dayan N., editor. Skin Microbiome Handbook: From Basic Research to Product Development. 1st ed. Wyley; Hoboken, NJ, USA: 2020. pp. 219–236. [Google Scholar]
- 58.Zeth K., Sancho-Vaello E. Structural plasticity of LL-37 indicates elaborate functional adaptation mechanisms to bacterial target structures. Int. J. Mol. Sci. 2021;22:5200. doi: 10.3390/ijms22105200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang G. Structure of human host defense cathelicidin LL-37 and its smallest antimicrobial peptide KR-12 in lipid micelles. J. Biol. Chem. 2008;283:32637–32643. doi: 10.1074/jbc.M805533200. [DOI] [PubMed] [Google Scholar]
- 60.Kim J.E., Kim B.J., Jeong M.S., Seo S.J., Kim M.N., Hong C.K., Ro B.I. Expression and modulation of LL-37 in normal human keratinocytes, HaCaT cells, and inflammatory skin diseases. J. Korean Med. Sci. 2005;20:649–654. doi: 10.3346/jkms.2005.20.4.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Braff M.H., Di Nardo A., Gallo R.L. Keratinocytes store the antimicrobial peptide cathelicidin in lamellar bodies. J. Investig. Dermatol. 2005;124:394–400. doi: 10.1111/j.0022-202X.2004.23443.x. [DOI] [PubMed] [Google Scholar]
- 62.Raymond A.A., Gonzalez de Peredo G., Ishida-Yamamoto S.A., Stella A., Ishida-Yamamoto A., Bouyssie D., Serre G., Monsarrat B., Simon M. Lamellar bodies of human epidermis. Mol. Cell. Proteomics. 2008;7:2151–2175. doi: 10.1074/mcp.M700334-MCP200. [DOI] [PubMed] [Google Scholar]
- 63.Bandurska K., Berdowska B.-F.R., Krupa P. Unique features of human cathelicidin LL-37. BioFactors. 2015;41:289–300. doi: 10.1002/biof.1225. [DOI] [PubMed] [Google Scholar]
- 64.Shelley J.R., Davidson D.J., Dotin J.R. The dicotomous responses driven by β-defensins. Front. Immunol. 2020;11:1176. doi: 10.3389/fimmu.2020.01176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chessa C., Bodet C., Jousselin C., Wehbe M., Leveque N., Garcia K. Antiviral and immunomodulatory properties of antimicrobial peptides produced by human keratinocytes. Front. Microbiol. 2020;11:1155. doi: 10.3389/fmicb.2020.01155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Oren A., Ganz T., Liu L., Meerloo T. In human epidermis, beta-defensin 2 is packaged in lamellar bodies. Exp. Mol. Pathol. 2003;74:180–182. doi: 10.1016/S0014-4800(02)00023-0. [DOI] [PubMed] [Google Scholar]
- 67.Nakatsuji T., Kao M.C., Zhang L., Zouboulis C.C., Gallo R.L. Sebum free fatty acids enhance the innate immune defense of human sebocytes by upregulating beta-defensin-2 expression. J. Investig. Dermatol. 2010;130:985–994. doi: 10.1038/jid.2009.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Harder J., Meyer-Hoffert U., Schwichtenberg l., Schroeder J.-M. Differential gene induction of.; human beta-defensins (hBD-1, -2, -3, and -4) in keratinocytes is inhibited by retinoic acid. J. Investig. Dermatol. 2004;123:522–529. doi: 10.1111/j.0022-202X.2004.23234.x. [DOI] [PubMed] [Google Scholar]
- 69.Schroeder J.M., Harder J. Human beta-defensin-2. Int. J. Biochem. Cell Biol. 1999;31:645–651. doi: 10.1016/S1357-2725(99)00013-8. [DOI] [PubMed] [Google Scholar]
- 70.Rieg S., Garbe C., Sauer B., Kalbacher H., Schittek B. Dermcidin is constitutively produced by eccrine sweat glands and is not induced in epidermal cells under inflammatory skin conditions. Br. J. Dermatol. 2004;151:534–539. doi: 10.1111/j.1365-2133.2004.06081.x. [DOI] [PubMed] [Google Scholar]
- 71.Dahlhoff M., Zouboulis C.C., Schneider M.R. Expression of dermcidin in sebocytes supports a role for sebum in the constitutive innate defense of human skin. J. Dermatol. Sci. 2016;81:124–126. doi: 10.1016/j.jdermsci.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 72.Schittek B., Hipfel R., Saur B., Baur J., Kalbacher H., Stevanovic S., Schirle M., Schroeder K., Blin N., Meier F., et al. Dermcidin: A novel antibiotic peptide secreted by sweat glands. Nat. Immunol. 2001;2:1133–1137. doi: 10.1038/ni732. [DOI] [PubMed] [Google Scholar]
- 73.Baechle D., Flad T., Cansier A., Steffen H., Schittek B., Tolson J., Herrmann T., Dihazi H., Beck A., Mueller G.A., et al. Cathepsin D is present in human eccrine sweat and involved in the processing of the antimicrobial peptide DCD-1L. J. Biol. Chem. 2006;281:5406–5415. doi: 10.1074/jbc.M504670200. [DOI] [PubMed] [Google Scholar]
- 74.Nashani A., Sedighian H., Mirhosseini S.A., Ghazvini K., Zare H., Janangiri A. Antimicrobial peptides as a promising treatment option against Acinetobacter baumannii infections. Microb. Pathog. 2020;146:104238. doi: 10.1016/j.micpath.2020.104238. [DOI] [PubMed] [Google Scholar]
- 75.Farshadzadeh Z., Pourhajibagher M., Taheri B., Ekrami A., Modarressi M.H., Azimzadeh M., Bahador A. Antimicrobial and antibiofilm potencies of dermcidin-derived peptide CDC-1L against Acinetobacter baunannii: An in vivo wound healing model. BMC Microbiol. 2022;22:25. doi: 10.1186/s12866-022-02439-8. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 76.Burian M., Schittek B. The secrets of dermcidin action. Int. J. Med. Microbiol. 2015;305:283–286. doi: 10.1016/j.ijmm.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 77.Rieg S., Seeber S., Steffen H., Humeny A., Kalbacher H., Stevanovic S., Kimura A., Garbe C., Schittek B. Generation of multiple stable dermicidin-derived antimicrobial peptides in sweat of different body sites. J. Investig. Dermatol. 2006;126:354–365. doi: 10.1038/sj.jid.5700041. [DOI] [PubMed] [Google Scholar]
- 78.Becucci L., Valensin D., Innocenti M., Guidelli R. Dermcidin, an ionic antimicrobial peptide: Influence of lipid charge, pH and Zn2+ on its interaction with a biomimetic membrane. Soft Matter. 2014;10:616. doi: 10.1039/C3SM52400K. [DOI] [PubMed] [Google Scholar]
- 79.Zeth K., Sancho-Vaello E. The human antimicrobial peptides dermcidin and LL-37 show novel distinct pathways in membrane interactions. Front. Chem. 2017;5:86. doi: 10.3389/fchem.2017.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Song C., de Groot B.L., Sansom M.S.P. Lipid bilayer composition influences the activity of the antimicrobial peptide dermcidin channel. Biophys. J. 2019;116:1658–1666. doi: 10.1016/j.bpj.2019.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Puthumadthil N., Jayasree P., Kumar K.S., Nampoothiri K.M., Bajaj H., Mahendran K.R. Detecting the structural assembly pathway of human antimicrobial peptide pores at single-channel level. Biomater. Sci. 2019;7:3226–3237. doi: 10.1039/C9BM00181F. [DOI] [PubMed] [Google Scholar]
- 82.Qiu F., Long H., Zhang L., Liu J., Yang Z., Huang X. Dermcidin enhances the migration, invasion, and metastasis of hepatocellular carcinoma cells in vitro and in vivo. J. Clin. Transl. Hepatol. 2022;10:429–438. doi: 10.14218/JCTH.2021.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rademacher F., Dreyer S., Kopfnagel V., Glaser R., Werfel T., Harder J. The antimicrobial and immunomodulatory function of RNase 7 in skin. Front. Immunol. 2019;2019:2553. doi: 10.3389/fimmu.2019.02553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Salazar V.A., Arranz-Trulien J., Prats-Ejarque G., Torrent M., Andreu D., Pulido D., Boix E. Insight into the antifungal mechanism of action of human RNase N-terminal derived peptides. Int. J. Mol. Sci. 2019;20:4558. doi: 10.3390/ijms20184558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kopfnagel V., Dreyer S., Baumert K., Stark M., Harder J., Hofmann K., Kleine M., Buch A., Sodeik B., Werfel T. RNase 7 promotes sensing of self-DNA by human keratinocytes and activates an antiviral immune response. J. Investig. Dermatol. 2020;140:1589–1598. doi: 10.1016/j.jid.2019.09.029. [DOI] [PubMed] [Google Scholar]
- 86.Zimmer D.B., Cornwall E.H., Landar A., Song W. The S100 protein family: History, function, and expression. Brain Res. Bull. 1995;37:417–429. doi: 10.1016/0361-9230(95)00040-2. [DOI] [PubMed] [Google Scholar]
- 87.Gonzales L.L., Garrie K., Turner M.D. Role of S100 proteins in health and disease. Biochim. Biophys. Acta. 2020;2020:118677. doi: 10.1016/j.bbamcr.2020.118677. [DOI] [PubMed] [Google Scholar]
- 88.Singh P., Ali S.A. Multifunctional role of S100 protein family in the immune system: An update. Cells. 2022;11:2274. doi: 10.3390/cells11152274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Michalrk M., Gelhaus C., Hecht O., Podschun R., Schroder J.M., Leippe M., Grotzinger J. The human antimicrobial protein psoriasin acts by permeabilization of bacterial membranes. Develop. Comp. Biochem. 2009;33:470–476. doi: 10.1016/j.dci.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 90.Kurpet K., Chwatko G. S100 proteins as novel therapeutic targets in psoriasis and other autoimmune diseases. Molecules. 2022;27:6640. doi: 10.3390/molecules27196640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Borsky P., Fiala Z., Andrys C., Beeranek M., Hamakova K., Malkove A., Svadlakova T., Krejsek J., Palicka V., Borska L., et al. Alarmins HMGB1, IL-33, S100A7, and S100A12 in psoriasis vulgaris. Mediators Inflamm. 2020;2020:8465083. doi: 10.1155/2020/8465083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Brauner A., Alvendai C., Chromek M., Stopsack K.H., Ehrstrom S., Schroder J.M., Bohm-Starke N. Psoriasin, a novel anti-Candida albicans adhesin. J. Mol. Med. 2018;96:537–545. doi: 10.1007/s00109-018-1637-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Van Anh Pham C., Rademacher F., Hinrichs H., Beck-Jendroschek V., Harder M., Brasch J., Glaser R., Harder J. Expression of antimicrobial peptides is increased in tinea pedis. Mycoses. 2021;64:763–770. doi: 10.1111/myc.13279. [DOI] [PubMed] [Google Scholar]
- 94.Hermes B.M., Rademacher F., Chung C., Tiegs G., Bendix M.-C., de Zwaan M., Harder J., Baines J. Skin microbiota analysis in patients with anorexia nervosa and healthy-weight controls reveals microbial indicators of healthy weight and associations with the antimicrobial peptide psoriasin. Sci. Rep. 2022;123:15515. doi: 10.1038/s41598-022-19676-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kozlyuk N., Monteith A.J., Garcia V., Damo S.M., Skaar E.P., Chazin W.J. S100 proteins in the innate immune response to pathogens. Methods Mol. Biol. 2019:275–290. doi: 10.1007/978-1-4939-9030-6_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zygiel E.M., Nolan E.M. Transition metal sequestration by host-defense protein calprotectin. Annu. Rev. Biochem. 2018;87:621–643. doi: 10.1146/annurev-biochem-062917-012312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Brandtzaeg P., Gabrielsen T.O., Dale I., Muller F., Steinbakk M., Fagerhol M.K. The leucocyte protein L1 (calprotectin): A putative nonspecific defence factor at epithelial surfaces. Adv. Exp. Med. Biol. 1995;371A:201–206. doi: 10.1007/978-1-4615-1941-6_41. [DOI] [PubMed] [Google Scholar]
- 98.Batycka-Baran A., Hattinger E., Marchenkov A., Koziol M., Bieniek A., Szepietowski J., Ruzika T., Wolf R. Koebnerisin (S100A15): A novel player in the pathogenesis of rosacea. J. Amer. Acad. Dermatol. 2019;80:1753–1755. doi: 10.1016/j.jaad.2018.06.012. [DOI] [PubMed] [Google Scholar]
- 99.Zouboulis C.C., de Costa A.N., Makrantonaki E., Hou X.X., Almansouri D., Dudley J.T., Edwards H., Readhead B., Balthasar O., Jemec G.B.E., et al. Alterations in innate immunity and epithelial cell differentiation are the molecular pillars of hidradenitis suppurativa. J. Eur. Acad. Dermatol. Venereol. 2020;34:846–861. doi: 10.1111/jdv.16147. [DOI] [PubMed] [Google Scholar]
- 100.Mussa B.M., Venkatachalam T., Srivastava A., Al-Habshi A., Abdelgadir A., Al Awadi F., Hafidh K., Hamoudi R., Abusnana S. Identification of novel differentially expressed genes in type 1 diabetes mellitus complications using transcriptomic profiling of UAE patients: A multicenter study. Sci. Rep. 2022;12:16316. doi: 10.1038/s41598-022-18997-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wu Z., Wu Y., Fischer J., Bartels J., Schroder J.-M. Skin-derived SPINK9 kills Escherichia coli. J. Investig. Dermatol. 2018;139:1135–1142. doi: 10.1016/j.jid.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 102.Sultana A., Luo H., Ramakrishna S. Antimicrobial peptides and their applications in biomedical sector. Antibiotics. 2021;10:1094. doi: 10.3390/antibiotics10091094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Moretta A., Scieuzo C., Petrone A.M., Salvia R., Manniello M.D., Franco A., Lucchetti D., Vassallo A., Vogel H., Sqambato A., et al. Antimicrobial peptides: A new hope in biomedical and pharmaceutical fields. Front. Cell. Infect. Microbiol. 2021;11:668632. doi: 10.3389/fcimb.2021.668632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pulingam T., Parumasivam T., Gazzali A.M., Sulaiman A.M., Chee J.Y., Lakshmanan M., Chin C.F. Antimicrobial resistance: Prevalence, economic burden, mechanisms of resistance and strategies to overcome. Eur. J. Pharmaceut. Sci. 2022;170:106103. doi: 10.1016/j.ejps.2021.106103. [DOI] [PubMed] [Google Scholar]
- 105.Chen C.H., Lu T.K. Development and challenges of antimicrobial peptides for therapeutic applications. Antibiotics. 2020;9:24. doi: 10.3390/antibiotics9010024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Martenez-Culebras P., Gandia M., Garrigues S., Marcos J.F., Manzanares P. Antifungal peptides and proteins to control toxigenic fungi and mycotoxin biosynthesis. Int. J. Mol. Sci. 2021;22:13261. doi: 10.3390/ijms222413261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gawde U., Chakraborty S., Waghu F.H., Barai R.S., Khanderkar A., Indraguru R., Shirsat T., Idicula-Thomas S. CAMPR4: A database of natural and synthetic antimicrobial peptides. Nucleic Acid Res. 2022;2022:gkac933. doi: 10.1093/nar/gkac933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Booparai J.K., Sharma P.K. Mini review on antimicrobial peptides, sources, mechanism and recent applications. Protein Pept. Lett. 2020;27:4–16. doi: 10.2174/18755305MTAwENDE80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lei J., Sun L., Huang S., Zhu C., Li P., He J., Mackey V., Coy D.H., He Q. The antimicrobial peptides and their potential clinical applications. Am. J. Transl. Res. 2019;11:3919–3931. [PMC free article] [PubMed] [Google Scholar]
- 110.Mahlapuu M., Bjorn C., Ekblom J. Antimicrobial peptides as therapeutic agents: Opportunities and challenges. Crit. Rev. Biotechnol. 2020;40:978–992. doi: 10.1080/07388551.2020.1796576. [DOI] [PubMed] [Google Scholar]
- 111.Lima P.G., Oliveira J.T.A., Amaral J.L., Freitas C.D.T., Souza P.F.N. Synthetic antimicrobial peptides: Characteristics, design, and potential as alternative molecules to overcome microbial resistance. Life Sciences. 2021;278:119647. doi: 10.1016/j.lfs.2021.119647. [DOI] [PubMed] [Google Scholar]
- 112.West H.C., Bennett C.L. Redefining the role of Langerhans cells as immune regulators within the skin. Front. Immunol. 2018;8:1941. doi: 10.3389/fimmu.2017.01941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Deckers J., Hammand H., Hoste E. Langerhans cells: Sensing the environment in health and disease. Front. Immunol. 2018;9:93. doi: 10.3389/fimmu.2018.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hald B., Reider D., Nagele F., Spinoit A.-F., Pechriggi E., Romani N., Fritch H., Oswald J. Langerhans cells in hypospadias: An analysis of Langerin (CD207) and HLA-DR on epidermal sheets and full thickness skin sections. BMC Urol. 2019;19:114. doi: 10.1186/s12894-019-0551-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rajesh A., Wise L., Hibma M. The role of Langerhans cells in pathologies of the skin. Immunol. Cell Biol. 2019;97:700–713. doi: 10.1111/imcb.12253. [DOI] [PubMed] [Google Scholar]
- 116.Zhou L., Jiang A., Veenstra J., Ozog D.M., Mi Q.-S. The roles of skin Langerhans cells in immune tolerance and cancer immunity. Vaccines. 2022;10:1380. doi: 10.3390/vaccines10091380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Chambers E.S., Vukmanovic-Stejic M. Skin barreir immunity and aging. Immunology. 2019;160:116–125. doi: 10.1111/imm.13152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Vela-Romera A., Carriel V., Martin-Piedra M.A., Campos F., Chato-Astrain J., Prados-Olleta N., Campos A., Alaminos M., Garzon I. Characterization of the human ridges and non-ridged skin: A comparative histological, histochemical and immunochemical analysis. Histochem. Cell Biol. 2019;151:57–73. doi: 10.1007/s00418-018-1701-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Solano F. On the metal cofactor in the tyrosinase family. Int. J. Mol. Sci. 2018;19:633. doi: 10.3390/ijms19020633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ohbayashi N., Fukuda M. Recent advances in understanding the molecular basis of melanogenesis in melanocytes. F1000Research. 2020;9:F1000. doi: 10.12688/f1000research.24625.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sevilla A., Cheret J., Slominski R.M., Slominski A.T., Paus R. Revisiting the role of melatonin in human melanocyte physiology: A skin context perspective. J. Pineal Res. 2022;72:e12790. doi: 10.1111/jpi.12790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Moreiras H., Seabra M.C., Barral D.C. Melanin transfer in the epidermis: The pursuit of skin pigmentation control mechanisms. Int. J. Mol. Sci. 2021;22:4466. doi: 10.3390/ijms22094466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Benito-Martinez S., Salavessa L., Raposo G., Marks M.S. Melanin transfer and fate within keratinocytes in human skin pigmentation. Integrative Compar. Biol. 2021;61:1546–1555. doi: 10.1093/icb/icab094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hart P.H., Norval M. The multiple roles of urocanic acid in health and disease. J. Investig. Dermatol. 2021;141:496–502. doi: 10.1016/j.jid.2020.07.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.