Abstract
Background—Non-communicable diseases (NCDs) affect a growing share of the population in Kosovo. The country faces challenges with NCDs management, specifically detecting, screening, and treating people with NCDs. Objective—To assess the management of NCDs, including the inputs that influence the provision of NCDs and outcomes of NCD management. Eligibility criteria—Studies had to report NCD management in Kosovo. Sources of evidence—We systematically searched Google Scholar, PubMed, Scopus, and Web of Science. Charting methods—The data were charted by two researchers. We extracted data on general study details and design and information on the management and outcomes of NCDs in Kosovo. Synthesis of results—For the mix of studies that were included in the review, thematic narrative synthesis was used. We developed a conceptual framework based on health production core components to analyze the data. Results—Kosovo’s health care system is available to provide basic care for patients with NCDs. However, there are serious limitations in the availability of key inputs providing care, i.e., funding, medicines, supplies, and medical staff. Additionally, in terms of the management of NCDs, there are areas for improvement, such as limited application of clinical pathways and guidelines and issues with referrals of patients among levels and sectors of care. Finally, it is worth noting that there is overall limited information on NCD management and outcomes. Conclusions—Kosovo provides only basic services and treatment of NCDs. The data reporting the existing situation on NCD management are limited. The inputs from this review are helpful for existing policy efforts by the government aimed to enhance NCD care in Kosovo. Funding—This study is part of the research done for a World Bank review of the state of NCDs in Kosovo and was funded through the Access Accelerated Trust Fund (P170638).
Keywords: NCD management, diabetes, hypertension, breast cancer, cervical cancer
1. Introduction
Kosovo is an upper-middle-income country with a population of 1.8 million, in South-Eastern Europe [1,2,3]. The average life expectancy in Kosovo is 71.9 [1] to 76.7 years [2,3]. The mortality rate of all causes has continued to fall in Kosovo, as with the rest of the European Region, though from 2006 to 2011, it has shown a slight trend of increase [3]. Non-communicable diseases (NCDs) affect a large share of the population in the country. About 21.6% of adults (18+ years) reported having a chronic disease in 2017 [1]. Women are more likely to report chronic diseases than men [1]. Cardiovascular diseases are the leading cause of morbidity and mortality, followed by malignant diseases and respiratory diseases [3,4,5,6]. Diabetes is also prevailing among the population [7]. Marginalized communities, such as Roma, Ashkali, and Egyptian people, are particularly vulnerable [8,9,10].
Due to convenient demographic trends, where most of Kosovo’s population is younger, there were few concerns about NCDs’ impact on the population’s health. However, demographic trends are changing with very swift changes in population lifestyle trends and exposure to environmental hazards, notably pollution. This all hints that Kosovo is, and will continue to be, facing an increasing number of people with NCDs and should adjust healthcare services provision to match these evolving needs.
NCD care in Kosovo is provided by all three levels of care, i.e., primary, secondary, and tertiary [10]. The primary healthcare system is the network of family medicine facilities. Secondary healthcare represents regional hospitals where specialized care is provided. Tertiary healthcare refers to research and teaching institutions that are supposed to provide high-end diagnosis and treatment. NCD care, as well as any type of care, is affected by numerous shortcomings of the health care system. For example, Kosovo has among the lowest ratios of physicians and nurses in Europe [11], with 1.44 physicians per 1000 inhabitants compared to the European Union (EU) average of 3.4 doctors per 1000 population. The relatively low and stagnant level of salaries in the public sector, the limited capacity of absorption of additional staff in the health care system, and the difficult working conditions, especially for the nurses, explain the concerning trend of migration of health professionals to European Union countries. Furthermore, the public health spending in Kosovo as a share of GDP is low relative to the regional and global per capita income comparators. In 2015, public health expenditure in Kosovo was 2.9 percent of the gross domestic product (GDP) and had been at such levels over the last two decades [4,12,13,14]. This is considerably lower than the EU average or averages for countries in South-Eastern Europe [4]. Private health expenditure, almost entirely in the form of out-of-pocket payments by households at the point of service, contributes an estimated 40 percent of total spending in the sector [10,11]. The application of standards of care is limited [15]. Medical practice is left to physician education, experience, and willingness to perform clinical procedures. This impacts how care is provided for any type of patient, including patients with NCDs.
Management of NCDs is complex and resource consuming undertaking, which includes detecting, and treating these diseases. The evidence on the management of NCDs in Kosovo is scattered in different reports and peer review publications. There is no common picture and understanding of the current situation regarding the management of NCDs in the country. Several serious efforts to improve the situation are under discussion, including developing a country NCDs strategy. To support the government and other interested stakeholders, we decided to perform a scoping review that will help generate a clearer picture of NCDs management in Kosovo with the hope that it will support decision making at times when there are ambitions to put forward strategies and policies that will address the current situation with NCDs in the country. Henceforth, the objective of this study is to assess the inputs that influence the delivery of NCDs care, the process of management of NCDs, and outcomes from such management of NCDs.
2. Methods
We performed a scoping review. A scoping review can provide an overview of the available research evidence [16,17,18,19]. Therefore, we performed a scoping review of the grey literature and peer review publications in line with the PRISMA extension for scoping reviews (PRISMA-ScR) statement [16].
2.1. Protocol and Registration
The protocol was developed for internal purposes, stating all eligibility criteria, search databases, search terms, data extraction sheet, and frameworks for analysis. However, the protocol was not published in advance.
2.2. Information Sources, Search Strategy, and Eligibility Criteria
We systematically searched four databases, i.e., Google Scholar, PubMed, Scopus, and Web of Science, from the beginning to January 2023, when the search was last updated. We performed two searches in Google Scholar. One was performed with Albanian, and another one with English search terms. The search strategy in the databases (i.e., PubMed) targeted relevant peer-review papers. The search strategy in Google Scholar targeted peer review papers and the grey literature, i.e., publications and reports by different agencies and institutions (national and international). The search strategy consisted of terms related to NCDs and terms referring to the country Kosovo (Supplementary Materials). Specifically, we used terms related to specific NCDs (i.e., hypertension, diabetes, breast cancer, cervical cancer) or general terms for NCDs (i.e., non communicable diseases, NCDs, etc.) and, with the exception of the Albanian language search in Google Scholar, search terms were related to the country, i.e., Kosovo. For the Albanian language search, we added the search term “chronic diseases”, as NCDs are often noted with such a term. We omit using country in Google Scholar search for the Albanian language to keep the search more comprehensive.
Studies were included in case they reported valid information on NCDs management in Kosovo. Key conditions (NCDs) of interest were diabetes, hypertension, breast cancer, and cervical cancer. Nevertheless, there was interest in NCDs in general. Therefore, if papers reported information on other NCDs or, in general, for NCDs, they were included. There were no restriction criteria on publication time or publishing language or type of study design. Studies were excluded only to remove duplicate data.
2.3. Selection of Sources of Evidence and Data Extraction
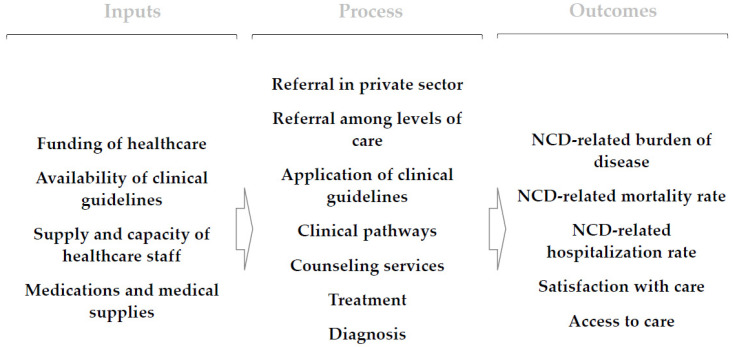
The acceptability of studies for inclusion was determined by screening titles and abstracts, followed by a full-text evaluation by an independent reviewer. Three researchers (IH, VA, and BK) examined the search results, analyzing titles and abstracts before conducting a full-text review. To categorize and extract the data, a data extraction sheet was created. The team gathered data independently and in duplicate for the study’s general details and information on NCDs management. We have not contacted authors or made any other effort to gather additional data related to included papers. We have used only information from included publications. When it comes to NCDs management, the extraction sheet had three main sections for collecting data, which largely follow the conceptual framework used for data analysis (Figure 1). The first section collected information management of NCDs (the process), i.e., diagnosis use in treatment (i.e., staging, risk assessment), counseling services, treatment of NCDs, clinical pathways, interaction with patients, referral of patients among levels of care, referral of patients to the private sector, application of protocols, and any other relevant info that did not fit in previous categories. The second section collected data on the factors (inputs) influencing the management of NCDs, i.e., funding of the healthcare system, supply with medication and medical supplies, supply and capacity of healthcare staff, availability of clinical guidelines, and other factors that would not fit in other categories. Finally, the last section collected information on outcomes of management of NCDs (outcomes), i.e., satisfaction with care, access to care, NCD-related mortality rate, NCD-related hospitalization rate, and NCD-related burden of disease. All section data were collected for specific NCDs, i.e., diabetes, hypertension, breast cancer, cervical cancer, or any NCD.
Figure 1.
The conceptual framework for analysis of NCDs management in Kosovo.
2.4. Critical Appraisal of Evidence
There was no standard quality assessment of studies. However, the team double-checked that the sources used to publish the findings were reliable. This is related to the fact that we wanted to gather all credible evidence to provide a thorough scoping review exercise that will benefit all parties interested in the situation with NCDs in Kosovo, be that the government or other national or international actors.
2.5. Synthesis of Results
The retrieved data were subjected to thematic synthesis [20]. The mix of studies considered in the review and the conceptual framework for data analysis lends to such a strategy. Thematic synthesis was carried out by three researchers (IH, VA, and PR). Each researcher independently performed the thematic analysis. Findings from all studies were collated under main themes and subthemes following a conceptual framework (Figure 1) for analysis designed using a health services production framework with three main elements, i.e., inputs, processes, and outcomes. Hence, our main themes were the management of NCDs (processes), inputs that determine the management of NCDs (inputs), and finally, outcomes of management of the NCDs (outcomes). Different subthemes were determined based on our interest and relevance of such information in understanding the NCDs management in the country, i.e., availability of protocols, referral of patients, etc.
3. Results
3.1. Selection of Sources of Evidence
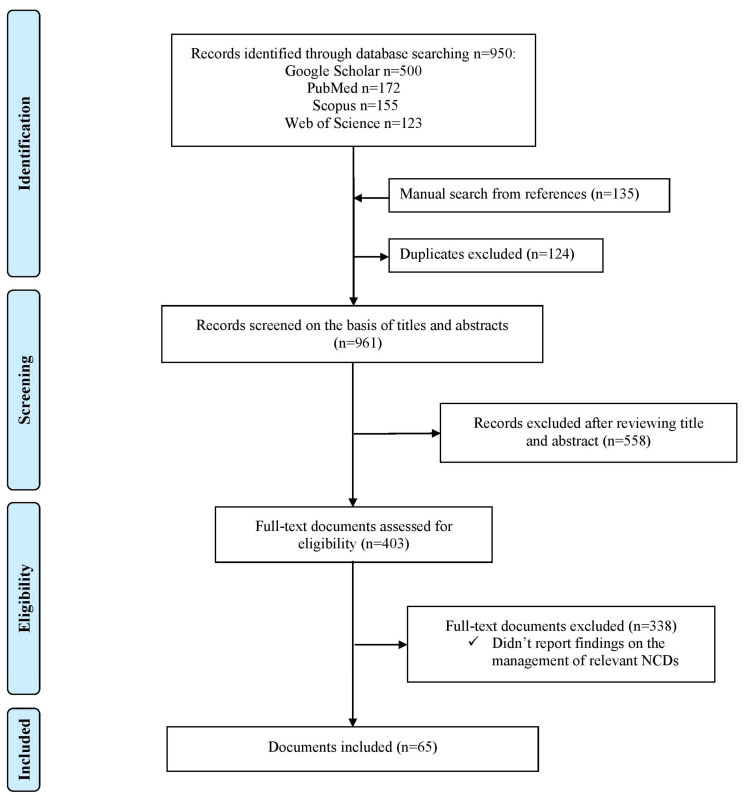
We identified 950 documents across four databases, i.e., 500 in Google Scholar, 172 in PubMed, 155 in Scopus, and 123 in Web of Science (Figure 2). One hundred and thirty-five documents were found with a manual search. One hundred and twenty-four duplicate documents were excluded from screening. Nine hundred and sixty-one documents were screened for eligibility by looking at the title and abstracts. Four hundred and three documents were reviewed in full text to assess eligibility. Finally, 65 documents were included in the evidence synthesis [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85].
Figure 2.
Selection of studies.
3.2. Characteristics of Sources of Evidence
We present the document characteristics in Table 1 and the Supplementary Materials. The documents were published between 2002 to 2022. Most of the documents, i.e., 57, were published from 2010 and on. Eighteen documents were published within the last five years. Most (i.e., 35) of the documents were peer reviewed papers published in academic journals, and 23 were different reports published by different agencies, and seven were policy briefs. Twenty-four documents reported information on inputs needed for NCDs management. Forty-one documents reported information on the processes related to NCDs management. Finally, 23 documents reported information on the outcomes of NCDs in Kosovo. Fourteen studies reported information on diabetes, 11 reported on hypertension, 13 documents reported information on breast cancer, five reported on cervical cancer, four reported on other NCDs, and 33 documents reported overall information on NCDs. Results of individual sources of evidence are presented in the Supplementary Materials. In the sections below, we provide a summary of these results.
Table 1.
Study characteristics.
| Author | Year | Type of Publication | Factors Influencing the Management of NCDs (Subthemes Reported) | Information on the Management of NCDs (Subthemes Reported) | Outcomes of Management of NCDs (Subthemes Reported) |
NCDs Reported |
|---|---|---|---|---|---|---|
| Barbullushi et al. [21] | 2002 | Journal article | Treatment, clinical pathways, application of clinical guidelines | Overall | ||
| Haxhikadrija et al. [22] | 2008 | Journal article | NCD-related mortality rate | Breast cancer | ||
| Knowles et al. [23] | 2008 | Report | Supply and capacity of healthcare staff | Diagnosis, treatment, clinical pathways, application of clinical guidelines | NCD-related burden of disease | Breast cancer, cervical cancer |
| Schneider et al. [24] | 2008 | Report | Funding of healthcare | Referral in private sector | Overall | |
| Ajvazi et al. [25] | 2009 | Journal article | Availability of clinical guidelines | Diabetes | ||
| Balkan Investigative Reporting Network [26] | 2009 | Report | Medications and medical supplies | Referral in private sector | Overall | |
| Devolli-Disha et al. [27] | 2009 | Journal article | Diagnosis | Breast cancer | ||
| FRIDOM [28] | 2009 | Report | Medications and medical supplies, availability of clinical guidelines | Referral in private sector | Overall | |
| Burkle [29] | 2010 | Journal article | NCD-related mortality rate | Overall | ||
| Percival et al. [30] | 2010 | Journal article | NCD-related mortality rate | Overall | ||
| Bakalli et al. [31] | 2011 | Journal article | NCD-related mortality rate | Hypertension | ||
| Begolli et al. [32] | 2011 | Report | Diagnosis, referral among levels of care, referral in private sector | Overall | ||
| Bielecka-Dabrowa et al. [33] | 2011 | Journal article | Diagnosis, treatment, application of clinical guidelines | Hypertension | ||
| Daullxhiu et al. [34] | 2011 | Journal article | NCD-related mortality rate | Hypertension | ||
| Health for All [35] | 2011 | Report | Access to care | Overall | ||
| O’Hanlon et al. [36] | 2011 | Journal article | Supply and capacity of healthcare staff | Overall | ||
| Balkan Investigative Reporting Network [37] | 2012 | Report | Medications and medical supplies | Referral among levels of care | Overall, diabetes | |
| Luta et al. [38] | 2012 | Journal article | Access to care | Overall | ||
| Ministry of Health [39] | 2012 | Report | Diagnosis, treatment | Overall | ||
| Arifi et al. [40] | 2013 | Journal article | NCD-related mortality rate | Diabetes | ||
| Hee Lee-Kwan et al. [41] | 2013 | Report | Funding of healthcare | Referral in private sector | Overall | |
| Hoxha [42] | 2013 | Report | Medications and medical supplies, supply and capacity of healthcare staff, funding of healthcare | Treatment, counseling services | Satisfaction with care | Overall, diabetes, breast cancer, cervical cancer |
| Balidemaj et al. [43] | 2014 | Journal article | Supply and capacity of healthcare staff | Treatment | Overall | |
| Bhabha et al. [44] | 2014 | Report | Access to care | Overall | ||
| Tahiri et al. [45] | 2014 | Journal article | Satisfaction with care | Overall | ||
| Uka [46] | 2014 | Report | Funding of healthcare | Overall | ||
| Vian [47] | 2014 | Report | Medications and medical supplies, funding of healthcare | Overall, breast cancer, cervical cancer | ||
| Davies et al. [48] | 2015 | Report | Supply and capacity of healthcare staff, availability of clinical guidelines | Diagnosis, treatment, clinical pathways, application of clinical guidelines | Breast cancer, cervical cancer | |
| Hoxha et al. [49] | 2015 | Policy brief | Medications and medical supplies, funding of healthcare | Treatment, counseling services, referral in private sector | Diabetes | |
| Hoxha et al. [50] | 2015 | Policy brief | Treatment | Access to care, satisfaction with care | Diabetes | |
| Hoxha et al. [51] | 2015 | Report | Medications and medical supplies, funding of healthcare | Referral in private sector | Overall | |
| Raunio et al. [52] | 2015 | Policy brief | Funding of healthcare | Access to care | Overall | |
| Raunio et al. [53] | 2015 | Policy brief | Access to care | Overall | ||
| Dixit et al. [54] | 2016 | Report | Counseling services | Access to care | Breast cancer | |
| Farnsworth et al. [55] | 2016 | Report | Diagnosis | Access to care | Hypertension, breast cancer | |
| Giordano et al. [56] | 2016 | Journal article | Diagnosis | Breast cancer | ||
| Kantar TNS [57] | 2016 | Report | Availability of clinical guidelines | Treatment, referral in private sector | Diabetes, hypertension | |
| Moore et al. [58] | 2016 | Journal article | Availability of clinical guidelines | Overall | ||
| Thompson et al. [59] | 2016 | Journal article | Availability of clinical guidelines | Counseling services | Hypertension | |
| Ramadani et al. [60] | 2016 | Journal article | NCD-related mortality rate | Other | ||
| Zahorka et al. [61] | 2016 | Report | Diagnosis, treatment | Hypertension | ||
| Zahorka et al. [62] | 2016 | Report | Referral among levels of care | Overall | ||
| Hoxha et al. [63] | 2017 | Policy brief | Referral among levels of care | Overall | ||
| Hoxha [64] | 2017 | Report | Referral in private sector | Overall | ||
| Hoxha et al. [65] | 2017 | Policy brief | Funding of healthcare | Overall, diabetes | ||
| Hoxha et al. [66] | 2017 | Policy brief | Satisfaction with care | Overall | ||
| Hughes et al. [67] | 2017 | Journal article | Treatment, clinical pathways | Diabetes | ||
| Bajraktari et al. [68] | 2018 | Journal article | Treatment | NCD-related mortality rate | Hypertension | |
| Jakupi et al. [69] | 2018 | Journal article | Medications and medical supplies, funding of healthcare | Other | ||
| Zejnullahu-Raci et al. [70] | 2018 | Journal article | Diagnosis, treatment | NCD-related mortality rate | Cervical cancer | |
| Bytyci et al. [71] | 2019 | Journal article | Counseling services, clinical pathways | Diabetes | ||
| Bytyqi-Damoni et al. [72] | 2019 | Journal article | Treatment | Diabetes | ||
| Cuperjani et al. [73] | 2019 | Journal article | Treatment | Breast cancer | ||
| World Health Organization [74] | 2019 | Report | Availability of clinical guidelines | Application of clinical guidelines | NCD-related hospitalization rate | Diabetes, hypertension |
| Ymerhalili et al. [75] | 2019 | Journal article | Clinical pathways | Diabetes, hypertension | ||
| Dimitrova et al. [76] | 2020 | Journal article | Availability of clinical guidelines | Overall | ||
| Eyvazzadeh et al. [77] | 2021 | Report | Referral among levels of care | Overall, breast cancer | ||
| Milosevic et al. [78] | 2021 | Journal article | Satisfaction with care | Overall | ||
| Podvorica et al. [79] | 2021 | Journal article | Counseling services | Other | ||
| Bytyci Katanolli et al. [80] | 2022 | Journal article | Counseling services | Overall | ||
| Bytyci Katanolli et al. [81] | 2022 | Journal article | Counseling services | Overall | ||
| Ejupi et al. [82] | 2022 | Journal article | Counseling services, treatment | Breast cancer | ||
| Hoxha et al. [83] | 2022 | Journal article | Treatment | Breast cancer | ||
| Hoxha et al. [84] | 2022 | Journal article | Application of clinical guidelines | Other | ||
| Obas et al. [85] | 2022 | Journal article | Diagnosis, treatment | Diabetes, hypertension, other |
NCD = Non Communicable Disease, UCCK = University Clinical Center of Kosovo
3.3. Inputs for NCDs Management
We found some evidence for medication and supplies, supply with healthcare staff, availability of clinical guidelines, and financing of NCD care. Kosovo’s healthcare system is underfunded, which is reflected in the lack of medical supplies and treatment within institutions [42]. The problems of supply with medication and medical supplies are a reoccurring issue for public health care providers at all levels of care [26,37,39,49,51]. This leaves the patients to pay for the drugs themselves [28]. In recent times, there have been significant improvements in the supply of drugs to health institutions [28].
Kosovo has one of the lowest supplies of healthcare staff in Europe. The immigration of health personnel from Kosovo has aggravated the supply of medical staff [43]. The capacities and clinical competence of medical staff are another domain where advancement is needed [36]. There have been several efforts by institutions to develop capacities for treating patients with NCDs. However, there is still a long way to go before improvements become dominant in the provision of care [42,48]. Supply issues hamper the provision of care related to NCDs [23,48]. The availability of clinical guidelines has been supported primarily by external assistance and has resulted in positive effects [31,59,84], but overall, it remains limited [59,76,84].
The current benefit package of care in Kosovo is financially unsustainable with public funding, resulting in frequent stock outs of basic materials and pharmaceuticals in health institutions. Although part of the benefit package, a large amount of pharmaceuticals are paid for out of pocket [24,41,49]. The establishment and functionalization of the Health Insurance Fund (HIF) has not been able to address funding gaps in the healthcare system regarding NCDs [65]. Another important problem are informal payments in the public sector [46].
3.4. Management of NCDs
We found some evidence on diagnostic, treatment, and counseling services. We also found some evidence for the application of clinical pathways and guidelines, as well as referral of patients with NCDs among levels of care and the private sector. Kosovo’s public health care system provides only basic diagnostics and treatment of NCDs. For hypertension diagnosis and assessment, healthcare providers use blood pressure measurement, blood tests, urine sample examination, and physical exams of patients [55]. Evidence reveals shortcomings in the assessment and examination of patients [61]. When it comes to breast or cervical cancer, unfortunately, a large proportion of cases are diagnosed in their late stages [48]. This is mainly due to ineffective breast and cervical cancer screening programs [48,55]. There is also a lack of information about disease staging [56]. Currently, several methods or tests are commonly used for breast cancer screening, including mammography, breast self-examination, clinical breast examination, and ultrasound [27,48,55].
Primary healthcare plays a vital role in the treatment of NCDs, i.e., diabetes and hypertension. However, there is a preference for specialist care [50]. Patients have access to general and specialized care in all three levels of care as well as the private sector. There is also evidence of the provision of comprehensive care [68,72]. However, as in the case of hypertension, it is often uncertain the extent of the management of patients via a holistic approach and therapeutic personalization [33]. In the case of breast cancer, there is widespread evidence of insufficient decision-making that is not based on best medical practice standards and inappropriate treatment and follow-up by providers and patients [23]. The surgical treatments for breast cancer have changed dramatically, from radical mastectomy to breast-conserving surgery [83]. About one-third of women with breast cancer in Kosovo still have a mastectomy [73]. Additionally, in the case of cervical cancer treatment, there are issues with the quality of the services, the coordination of care, and the establishment of a definitive diagnosis and treatment [48].
When it comes to counseling services, there is a lack of medical staff, especially nurses, who can counsel patients with NCDs [42]. If available, the consulting doctors are either family doctors or specialists in the public or private sectors [42]. Projects with external aid have supported primary healthcare institutions to establish motivational counseling services for type 2 diabetes and hypertension [71]. There is not much evidence on the availability of counseling services on breast cancer or other cancers. Earlier evidence points out that Kosovo has yet to develop a capacity to provide adequate counseling services in case of diagnosis and detection [54].
Work with clinical pathways and guidelines is primarily initiated and assisted through external aid [67,71,75]. Other than that, we found no evidence to support the implementation of clinical pathways in care delivery. The lack of a defined patient pathway for suspected cases of breast or cervical cancer exemplifies the problems related to NCDs management in the country [48]. From the initial presentation to definitive therapy, the patient’s care is challenging and ineffective. [23] Self-referral to secondary or tertiary clinics persists [23]. The application of protocols also seems to be limited according to existing evidence [33,48], but there are several important efforts to bring them to practice [48,74,84].
The existing referral mechanism for patients with NCDs is inefficient [61,77]. Regulations defining referral are not enforced [77]. Patients frequently forego primary care in favor of secondary or tertiary care, although primary care facilities can provide the required services [77]. The healthcare system needs guidelines that clearly define the duties and responsibilities of primary, secondary, and tertiary healthcare institutions, leaving little room for a formal referral system to be established [86]. The lack of a functional Health Information System (HIS) [37] and financial incentives via health financing arrangements [32] do not help with this situation. The establishment of Kosovo Hospital and University Clinical Services (KHUCS) did not improve referrals among institutions. [63]. Evidence suggests numerous issues with referrals in the private sector [26,28,32,51,57].
3.5. Outcomes from the Management of NCDs
We found little information on the outcomes of NCDs. We found some information on satisfaction with care, access to care, NCDs-related hospitalization rates, NCDs-related mortality rates, and little-to-no information on the NCDs-related burden of disease. Roughly half of the primary care users in Kosovo are satisfied with the overall medical experience [45]. Diabetic patients are most satisfied with visits to diabetes specialists and endocrinologists compared to primary care physicians [50]. Breast and cervical cancer patients appreciate care received at the secondary and tertiary care level [42].
Access to NCDs treatment can be limited for minority ethnic groups [44,55], except for the Serb population [54]. This is related to the difficulty of paying for medical treatment [53], availability of care [54], and discrimination [52]. Access is not limited only to ethnic groups. Access to care can be limited for those living in poverty, the elderly, people with disabilities, those living in remote areas, and women [44,54].
The number of diabetic and hypertensive hospitalizations in Kosovo has been increasing [74]. According to statistics, over half of the hospital deaths are caused by NCDs [29,30]. Arterial hypertension is one of the major risk factors for mortality and morbidity [68], often accompanied by atherosclerosis [31] or resulting in heart failure [34]. Cardiovascular, renal and lung illness, chronic back pain, and gastritis are the most common NCDs [40]. The epidemiological data suggest increasing breast and cervical cancer deaths. This is observed for other cancers, as well [60]. Women who live with cancer, without even essential medical or social assistance or support, bear the hidden weight of the disease [23].
4. Discussion
4.1. Summary of Findings
Kosovo’s health care system can provide basic care for patients with NCDs. At times, advanced care is available. However, there are serious limitations in the availability of key inputs for the provision of care, i.e., funding, medicines, supplies, as well as the medical staff. Additionally, in terms of the management of NCDs, there are shortcomings, such as limited application of clinical pathways and guidelines and issues with referrals of patients among levels and sectors of care. Finally, it is worth noting that there is overall limited information on NCDs management and, in particular, on NCDs outcomes.
4.2. Strengths and Weaknesses
A thorough and systematic search of the existing literature in some of the key databases, screening and extraction of data performed by at least two reviewers, as well as organized and conceptualized extraction and charting of data from studies, are some of the key strengths of this scoping review. Despite a thorough search, we may have missed relevant studies due to the general nature of our search, or documents may not have been registered in databases we have used. The depth of review in terms of understanding NCDs management may also be considered limited, which is largely conditional on the availability of data in the included papers. Some information may also be outdated. Nevertheless, it is worth noting that we found way more studies and information than we initially expected.
4.3. Context
To our knowledge, this is the first review of existing evidence on NCDs in Kosovo. It confirms many publicly known facts about the management of NCDs that are valid for most of the healthcare provided in the country. For example, studies have reported that the system is underfunded, [4,11,87] care availability is limited in quality and quantity, [4,83] issues exist relating to availability and impact of the application of clinical standards [4,15,84], and there are issues with supply with the workforce [11,88]. This review highlights the issues with a defragmented system of provision of NCD care, as well as efforts in the function of improvement of the existing situation. It does so by substantiating existing knowledge with the most recent available evidence. According to estimates, the worldwide economic burden of NCDs is anticipated to expand, and low- and middle-income countries will bear a greater portion of it as a result of population growth, aging, and globalization [89,90]. This will be a vital point to have in mind for policymakers in Kosovo, especially in light of changing demographic trends in Kosovo.
4.4. Implications for Policy, Practice, and Research
From this review, we can derive several learning points, i.e., issues to be addressed that can serve as the basis for the future work of relevant actors and, in particular, policymakers. Three main issues require the attention of policymakers and healthcare providers concerning the management of NCDs. Government and health care institutions (1) should put serious effort into improving the quality of care with regards to NCDs, (2) they should invest in human resources involved in the provision of care for NCDs, and (3) use health financing reform to protect the patients with NCDs financially with particular emphasis on vulnerable groups, such as minority communities, the elderly, and people from rural zones.
When it comes to quality improvement efforts, successful long-term treatment and management of NCDs in Kosovo will highly depend on the further transfer of knowledge, training of staff, and adoption, development, and implementation of clinical pathways and protocols. It will not be enough only to draw or adopt new protocols and standards. Also, external assistance can support but not replace internal efforts. Efforts will have to go deep into the roots of medical education, continuous medical education, and medical practice change. Radical efforts are needed in the adoption and implementation of clinical guidelines, as well as building the capacity and control mechanisms to ensure the clinical standards are enacted in NCDs care. Improvement efforts should touch all levels and sectors of care.
The Ministry of Health and healthcare institutions should engage in strategic planning that will mitigate the lack of clinical staff, especially medical doctors, and ensure long-term solutions for the proper supply of institutions with healthcare staff. The under-discussion NCDs strategy and medical staff payment level policies are perfect examples of that. In addition, incentives and measures are needed to be coupled with hospital development measures in the form of specialization of hospitals or the development of clinical excellence for the treatment of particular NCDs. This exercise is not just about proper supply numbers but also investment in the quality of their education and clinical excellence.
It is critical to construct health financial arrangements within existing health financing reform that ensure proper protection of people with NCDs, particularly from marginalized groups. Such mechanisms should ensure the availability of medications and services for people with NCDs. This is a long-term bet, but it is the only way to ensure sustainable protection of patients and their families from financial burdens associated with the healthcare they need. The under revision law on financing of healthcare and other policy measures that will follow are the moments for making such interventions.
This review notes the increasing amount of publication in relation to NCD care, as well as a trend in the use of advanced research designs to examine NCD care in Kosovo. Use of conjoint design in understanding clinical decision making with regard to NCDs care [84] or qualitative designs to understand the effects of NCDs-related counseling services on users of care are among notable examples. [81] These efforts should continue, be institutionally supported, and grow together with the data availability of NCDs care. Healthcare institutions are at a stage where they need specific information to understand existing problems and draw strategies that will address them.
5. Conclusions
Kosovo’s healthcare system is able to provide basic care for patients with NCDs. However, there are serious limitations in the availability of key inputs for the provision of care and proper management of NCDs that result in unfavorable NCDs outcomes. This review provides updated and reliable information that could be useful in the design of policy measures that aim to improve NCD management in Kosovo. Limited information on NCDs management, which is confirmed in this review, should be a call for a serious effort to document the management of NCDs in the country. Improvements will be easier to track, document, and understand with data.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20043299/s1, Table S1: Study characteristics and findings.
Author Contributions
The study was conceived by M.A. and H.T.H.N. and was designed by I.H., B.K., M.A., and H.T.H.N. The data were screened, extracted, and analyzed by I.H., V.A., B.K., and P.R. The manuscript was prepared by I.H., V.A., P.R., A.G.A., O.K. and it was critically reviewed by all authors. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable. This study used existing published data.
Informed Consent Statement
Not applicable.
Data Availability Statement
No data available.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This study is part of the research done for a World Bank review of the state of NCDs in Kosovo and APC was funded through the Access Accelerated Trust Fund (P170638).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.The World Bank . Policy Note on Kosovo Health Financing. World Bank; Prishtina, Kosovo: 2019. [Google Scholar]
- 2.Country Context. [(accessed on 6 April 2020)]. Available online: https://www.worldbank.org/en/country/kosovo/overview.
- 3.Ministria e Shndetësisë . Strategjia Sektoriale e Shëndetësisë 2017–2021. Ministria e Shndetësisë, Qeveria e Kosovës; Prishtina, Kosovo: 2016. [Google Scholar]
- 4.Sofia Stanculescu M., Neculau G., Atanasov P., Benkovic V., Bjelovic M., Goldstein J., Hoxha I., Ljaljevic A., Mitevska L., Mecineanu A. The Performance of Public Health-Care Systems in South-East Europe. Friedrich Ebert Stiftung Belgrade; Prishtina, Kosovo: 2014. [Google Scholar]
- 5.Oncology Clinic [(accessed on 13 May 2021)]. Available online: www.shskuk.rks-gov.net.
- 6.Islami D.A. Breast Cancer. Our Data and Challenges; In Proceedings of the 1st Pan-Albanian Conference on Breast Cancer; Prishtina, Kosovo. 25 October 2019. [Google Scholar]
- 7.Hoxha I., Fejza A., Malushaj I., Lumi D., Gashi M., Husaj I., Qarkaxhiu L., Gola L. Policy Brief 1—Diagnosis and The Gravity of Diabetes in Kosovo. Solidar Suisse; Prishtina, Kosovo: 2015. [Google Scholar]
- 8.Raunio E., Engel R., Fejza A., Telaku M., Hoxha I. Policy Brief 9—Nutrition and Life Choices in The Roma, Ashkali and Egyptian Communities. Solidar Suisse; Prishtina, Kosovo: 2015. [Google Scholar]
- 9.Telaku M., Engel R., Raunio E., Perry J., Rashiti A., Fejza A., Hoxha I. New National Health Insurance will Save Lives: Life Expectancy and Health in Kosovo’s Roma, Ashkali and Egyptian Communities. Solidar Suisse; Prishtina, Kosovo: Balkan Sunflowers Kosova; Prishtina, Kosovo: 2015. [Google Scholar]
- 10.Hoxha I., Muhaxheri E., Berisha V. A Proposal for a Health Insurance Plan: How Does It Affect Us? Solidar Suisse; Prishtina, Kosovo: 2012. [Google Scholar]
- 11.Marusic D., Ademi-Osmani A., Hoxha I., Ceglar J. Situation Analysis at Kosovo Hospital and University Clinical Services. Lux Development; Prishtina, Kosovo: 2017. [Google Scholar]
- 12.Hoxha I., Shaipi K. Analizë Krahasmitare E Skemave Të Sigurimit Shëndetësor Në EJL. Friedrich Ebert Stiftung; Prishtina, Kosovo: 2009. [Google Scholar]
- 13.Lee-Kwan S.H., Gittelsohn J., Hoxha I., Berisha V., Basha V. Kosovo Poverty Social Impact Analysis: Report of a Qualitative Study of Stakeholder Perceptions of Potential Health Insurance Reforms and Cost-Sharing Strategies. Johns Hopkins Bloomberg School of Public Health; Prishtina, Kosovo: 2013. [Google Scholar]
- 14.Schneider P., Langenbrunner J., Cho J., Kelmendi F., Tep S., Lebedeva V. Kosovo Health Financing Reform Study. World Bank; Prishtina, Kosovo: 2008. [Google Scholar]
- 15.Hoxha I., Duraj B., Xharra S., Avdaj A., Beqiri V., Grezda K., Selmani E., Avdiu B., Cegllar J., Marušič D., et al. Clinical Decision-Making for Appendectomy in Kosovo: A Conjoint Analysis. Int. J. Environ. Res. Public Health. 2022;19:4027. doi: 10.3390/ijerph192114027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 17.Peters M.D., Godfrey C.M., Khalil H., McInerney P., Parker D., Soares C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015;13:141–146. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 18.Arksey H., O’Malley L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 19.Sucharew H., Macaluso M. Progress Notes: Methods for Research Evidence Synthesis: The Scoping Review Approach. J. Hosp. Med. 2019;14:416–418. doi: 10.12788/jhm.3248. [DOI] [PubMed] [Google Scholar]
- 20.Lucas P.J., Baird J., Arai L., Law C., Roberts H.M. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med. Res. Methodol. 2007;7:4. doi: 10.1186/1471-2288-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barbullushi M., Elezi Y., Idrizi A. Kosovo 2002: The epidemiology of renal disease and the impact of 1999 Kosovo war on end-stage renal disease patients. Nephrol. Dial. Transplant. 2002;17:2275–2276. doi: 10.1093/ndt/17.12.2275. [DOI] [PubMed] [Google Scholar]
- 22.Haxhikadrija A., Voncina L., Hantchel D. Reproductive Health Services in Kosovo: An Investment with Long Term Benefits. UNFPA; Mitrovica, Kosovo: 2008. [Google Scholar]
- 23.Knowles S., Parker M. Female Genital Cancer in Kosovo: A Situational analysis of breast and cervical cancer. UNFPA; Mitrovica, Kosovo: 2008. [Google Scholar]
- 24.The World Bank . Kosovo Health Financing Reform Study. World Bank; Prishtina, Kosovo: 2008. [Google Scholar]
- 25.Ajvazi H., Goranci I., Goranci A., Govori V., Goranci D. Results of laser treatment-PRP to the diabetic retinopathy. Oftalmologia. 2009;53:74–78. [PubMed] [Google Scholar]
- 26.Balkan Investigative Reporting Network . Report on Kosovo’s Healthcare System. Balkan Investigative Reporting Network (BIRN); Prishtina, Kosovo: 2009. [Google Scholar]
- 27.Devolli-Disha E., Manxhuka-Kerliu S., Ymeri H., Kutllovci A. Comparative accuracy of mammography and ultrasound in women with breast symptoms according to age and breast density. Bosn. J. Basic Med. Sci. 2009;9:131–136. doi: 10.17305/bjbms.2009.2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.FRIDOM Project . Vertical Functional Review of the Kosovo Ministry of Health. FRIDOM Project; Prishtina, Kosovo: 2009. [Google Scholar]
- 29.Burkle F.M., Jr. Post-conflict health system recovery: The case of Kosovo. Prehospital Disaster Med. 2010;25:34–36. doi: 10.1017/S1049023X00007639. [DOI] [PubMed] [Google Scholar]
- 30.Percival V., Sondorp E. A case study of health sector reform in Kosovo. Confl. Health. 2010;4:7. doi: 10.1186/1752-1505-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bakalli A., Kocinaj D., Bakalli A., Krasniqi A. Relationship of hypertensive retinopathy to thoracic aortic atherosclerosis in patients with severe arterial hypertension. Clin. Exp. Hypertens. 2011;33:89–94. doi: 10.3109/10641963.2010.503307. [DOI] [PubMed] [Google Scholar]
- 32.Begolli I., Arënliu-Qosaj F. Public Health System Reform. Forum 2015; Prishtina, Kosovo: 2011. [Google Scholar]
- 33.Bielecka-Dabrowa A., Aronow W.S., Rysz J., Banach M. The Rise and Fall of Hypertension: Lessons Learned from Eastern Europe. Curr. Cardiovasc. Risk Rep. 2011;5:174–179. doi: 10.1007/s12170-010-0152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Daullxhiu I., Haliti E., Poniku A., Ahmeti A., Hyseni V., Olloni R., Vela Z., Elezi S., Bajraktari G., Daullxhiu T. Predictors of exercise capacity in patients with chronic heart failure. J. Cardiovasc. Med. 2011;12:223–225. doi: 10.2459/JCM.0b013e328343e950. [DOI] [PubMed] [Google Scholar]
- 35.Health for All . Improving Health of Roma, Ashkali and Egyptian Comunities in Fushë Kosovë. Health for All; Prishtina, Kosovo: 2011. [Google Scholar]
- 36.O’Hanlon K.P., Budosan B. Post-disaster recovery: A case study of human resource deployment in the health sector in post-conflict Kosovo. Prehospital Disaster Med. 2011;26:7–14. doi: 10.1017/S1049023X10000051. [DOI] [PubMed] [Google Scholar]
- 37.BIRN . Public Health Monitoring Report 2011. Balkan Investigative Reporting Network (BIRN); Prishtina, Kosovo: 2012. [Google Scholar]
- 38.Luta X., Draebel T. Kosovo-Serbs’ experiences of seeking healthcare in a post-conflict and ethnically segregated health system. Int. J. Public Health. 2013;58:377–383. doi: 10.1007/s00038-012-0403-8. [DOI] [PubMed] [Google Scholar]
- 39.Lux Dev . Capacity Building Within the MoH for Implementation of Healthcare Reforms. Lux Dev; Prishtina, Kosovo: 2011. [Google Scholar]
- 40.Arifi H.M., Duci S.B., Zatriqi V.K., Ahmeti H.R., Ismajli V.H., Gashi M.M., Zejnullahu Y.M., Mekaj A.Y. A retrospective study of 22 patients with necrotising fasciitis treated at the University Clinical Center of Kosovo (2005–2010) Int. Wound J. 2013;10:461–465. doi: 10.1111/j.1742-481X.2012.01005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee-Kwan S.H., Gittelsohn J. Kosovo Poverty Social Impact Analysis: Report of a Qualitative Study of Stakeholder Perceptions of Potential Health Insurance Reforms and Cost-Sharing Strategies. World Bank; Prishtina, Kosovo: 2013. [Google Scholar]
- 42.Hoxha I. The Performance of Public Health Care System in South-Eastern Europe. Friedrich Ebert Stiftung; Prishtina, Kosovo: 2013. [Google Scholar]
- 43.Balidemaj A., Balidemaj F. Globalization and Health in Kosovo. Eur. J. Soc. Sci. Educ. Res. 2014;1:193–198. doi: 10.26417/ejser.v2i1.p193-198. [DOI] [Google Scholar]
- 44.Harvard University . Post-war Kosovo and Its Policies Towards the Roma, Ashkali, and Egyptian Communities. François-Xavier Bagnoud Center for Health and Human Rights; Boston, MA, USA: Harvard School of Public Health; Boston, MA, USA: Harvard University; Boston, MA, USA: 2014. [Google Scholar]
- 45.Tahiri Z., Toci E., Rrumbullaku L., Hoti K., Roshi E., Burazeri G. Patients’ evaluation of primary health care services in Gjilan region, Kosovo. J. Public Health. 2014;36:161–169. doi: 10.1093/pubmed/fdt041. [DOI] [PubMed] [Google Scholar]
- 46.Uka A. Understanding Informal Patient Payments in Kosovo’s Health Care System. Health Policy Institute; Bratislava, Slovakia: 2014. [Google Scholar]
- 47.Vian T. Corruption Risk Assessment in the Health Sector in Kosovo. UNDP; Prishtina, Kosovo: Swiss Agency for Development and Cooperation; Berne, Switzerland: 2014. [Google Scholar]
- 48.Davies P., Ahmedi E., Berisha M. Assessment to Characterise the Current Situation & Capacities for the Prevention & Control of Breast, Cervical & Prostate Cancers in Kosovo. UNFPA; Prishtina, Kosovo: 2015. Technical Report. [Google Scholar]
- 49.Hoxha I., Fejza A., Malushaj I., Lumi D., Gashi M., Husaj I., Qarkaxhiu L., Gola L. Policy Brief 3—Health Costs and Affordability among Diabetic Patients. Solidar Suisse; Prishtina, Kosovo: 2015. [Google Scholar]
- 50.Hoxha I., Fejza A., Malushaj I., Lumi D., Gashi M., Husaj I., Qarkaxhiu L., Gola L. Policy Brief 2—Access to a Specialized Health Care Workforce for Diabetic Patients. Solidar Suisse; Prishtina, Kosovo: 2015. [Google Scholar]
- 51.Hoxha I., Zhubi M., Telaku M. Barriers in Access to Primary Health Care among Vulnerable Citizens in Kosovo. Save The Children Kosovo; Prishtina, Kosovo: 2015. [Google Scholar]
- 52.Raunio E., Engel R., Fejza A., Telaku M., Hoxha I. Policy Brief 10—Kosovo Roma, Ashkali and Egyptian Access to and Use of Health Care Services. Solidar Suisse; Prishtina, Kosovo: 2015. [Google Scholar]
- 53.Raunio E., Engel R., Fejza A., Telaku M., Hoxha I. Policy Brief 11—Cost of The Future Health Insurance Plan and Financial Implications for Roma, Ashkali, and Egyptians in Kosovo. Solidar Suisse; Prishtina, Kosovo: 2015. [Google Scholar]
- 54.Dixit A., Mishra M., Sandhu M., Delwiche K., Ajeti R., Goebbels K., Farnsworth N. Barriers to Accessing Healthcare for Women and Men in Kosovo. The Kosova Women’s Network; Prishtina, Kosovo: 2016. [Google Scholar]
- 55.Farnsworth N., Goebbels K., Ajeti R. Access to Healthcare in Kosovo. The Kosova Women’s Network; Prishtina, Kosovo: 2016. [Google Scholar]
- 56.Giordano L., Bisanti L., Salamina G., Ancelle Park R., Sancho-Garnier H., Espinas J., Berling C., Rennert G., Castagno R., Dotti M., et al. The EUROMED CANCER network: State-of-art of cancer screening programmes in non-EU Mediterranean countries. Eur. J. Public Health. 2016;26:83–89. doi: 10.1093/eurpub/ckv107. [DOI] [PubMed] [Google Scholar]
- 57.Kantar TNS . Knowledge, Attitudes, Practices and Behavior: Non-Communicable Diseases, Child Health and Citizens’ Right to Health in Kosovo. Kantar TNS; Prishtina, Kosovo: Swiss Tropical and Public Health Institute; Allschwil, Switzerland: 2016. [Google Scholar]
- 58.Moore J.E., Uka S., Vogel J.P., Timmings C., Rashid S., Gulmezoglu A.M., Straus S.E. Navigating barriers: Two-year follow up on recommendations to improve the use of maternal health guidelines in Kosovo. BMC Public Health. 2016;16:987. doi: 10.1186/s12889-016-3641-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thompson E., Harding A.L., Pond F., Hammond C., Taylor M. A Partnership to Improve Health Care in Kosovo: Dartmouth Medical School and Kosovar nurses worked together on a two-year project to rebuild primary health care in the postconflict city of Gjilan. Am. J. Nurs. 2006;106:72CC–72DD. doi: 10.1097/00000446-200611000-00027. [DOI] [Google Scholar]
- 60.Ramadani N., Dedushi K., Mucaj S., Kabashi S., Jerliu N., Hoxhaj A. The Frequency of Risk Factors on Trends of Pancreatic Cancer in Kosovo. Mater. Socio Med. 2016;28:108–111. doi: 10.5455/msm.2016.28.108-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Primary Health Care in Kosovo . Quality of Care Study 2016. Accessible Quality Healthcare; Prishtina, Kosovo: Swiss Tropical and Public Health Institute; Allschwil, Switzerland: Save the Children Schweiz; Prishtina, Kosovo: 2016. [Google Scholar]
- 62.Primary Health Care in Kosovo . Report on the Healthcare Management Survey in Kosovo. Accessible Quality Healthcare; Prishtina, Kosovo: Swiss Tropical and Public Health Institute; Allschwil, Switzerland: Save the Children; Prishtina, Kosovo: 2016. [Google Scholar]
- 63.Hoxha I., Braha M. Policy Brief 2: Problemi Me Shërbimin Spitalor Dhe Klinik Universitar Të Kosovës. Friedrich Ebert Stiftung; Prishtina, Kosovo: Center for Health Policy and Economics; Prishtina, Kosovo: 2017. [Google Scholar]
- 64.Hoxha I. Thematic Report—Health for “Luxembourg Initiative in Support of Civil Society in Kosovo”. Kosovo Civil Society Foundation; Prishtina, Kosovo: 2017. [Google Scholar]
- 65.Hoxha I., Braha M. Policy Brief 1: Propozimet Për Skemën E Sigurimeve Shëndetësore. Friedrich Ebert Stiftung; Prishtina, Kosovo: Center for Health Policy and Economics; Prishtina, Kosovo: 2017. [Google Scholar]
- 66.Hoxha I., Fejza A., Murataj N., Syla B., Delija B. Policy Brief 13—Family Physicians’ Perceptions and Preferences in Relation to Health Financing in Kosovo. Solidar Suisse; Prishtina, Kosovo: 2017. [Google Scholar]
- 67.Hughes J.D., Wibowo Y., Sunderland B., Hoti K. The role of the pharmacist in the management of type 2 diabetes: Current insights and future directions. Integr. Pharm. Res. Pract. 2017;6:15–27. doi: 10.2147/IPRP.S103783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bajraktari G., Henein M.Y. The uncertain/questionable prognostic value of exercise hypertension. J. Hypertens. Res. 2018:75–78. [Google Scholar]
- 69.Jakupi A., Godman B., Martin A., Haycox A., Baholli I. Utilization and Expenditure of Anti-cancer Medicines in Kosovo: Findings and Implications. Pharm. Open. 2018;2:423–432. doi: 10.1007/s41669-017-0066-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zejnullahu Raci P., Hosnjak L., Poljak M., Lepej S.Z., Vince A. Pre-vaccination prevalence of high-risk human papillomaviruses (HPV) in women from Kosovo and their related sociodemographic characteristics. Ginekol. Pol. 2018;89:485–494. doi: 10.5603/GP.a2018.0083. [DOI] [PubMed] [Google Scholar]
- 71.Bytyci A., Ymerhalili G., Dorner T.E., Stein K.V., Maxhera O. Pilot study of an integrated care model using the geriatric assessment tool. Wien. Klin. Wochenschr. 2019;131:273–277. doi: 10.1007/s00508-019-1512-7. [DOI] [PubMed] [Google Scholar]
- 72.Bytyqi-Damoni A., Kestane A., Taslimi P., Tuzun B., Zengin M., Bilgicli H.G., Gulcin İ. Novel carvacrol based new oxypropanolamine derivatives: Design, synthesis, characterization, biological evaluation, and molecular docking studies. J. Mol. Struct. 2020;1202 doi: 10.1016/j.molstruc.2019.127297. [DOI] [Google Scholar]
- 73.Cuperjani F., Gashi L., Kurshumliu F., Dreshaj S., Selimi F. Relationship between Ribosomal Protein S6-pS240 Expression and other Prognostic Factors in Non-Special Type Invasive Breast Cancer. Breast Care. 2019;14:171–175. doi: 10.1159/000491427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.World Health Organization . Primary health care in Kosovo: Rapid assessment. World Health Organization, Regional Office for Europe; Copenhagen, Denmark: 2019. [Google Scholar]
- 75.Ymerhalili G., Bytyci A., Maxhera O., Stein V., Dorner T. Integrated care for older people in Kosovo. Int. J. Integr. Care. 2019;19:226P. doi: 10.5334/ijic.s3226. [DOI] [Google Scholar]
- 76.Dimitrova M., Lakic D., Petrova G., Beslija S., Culig J. Comparative analysis of the access to health-care services and breast cancer therapy in 10 Eastern European countries. SAGE Open Med. 2020;8:922029. doi: 10.1177/2050312120922029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Eyvazzadeh A., Kumar P., Ramakrishna N. Breast Cancer Prevention in Kosovo: Understanding Capacity Constraints and Identifying Policy Options for Prevention. Nelson A. Rockefeller Center For Public Policy and the Social Sciences, Dartmouth College; Hanover, NH, USA: 2021. [Google Scholar]
- 78.Milosevic J., Milic M., Mirkovic M., Milosevic N., Novakovic T., Vitosevic Z., Djuric S., Stojanovic-Tasic M., Kulic L. Association between non-communicable diseases and satisfaction with healthcare and self-rated health: Experiences from post-conflict communities. Srp. Arh. Za Celok. Lek. 2021;149:16–23. doi: 10.2298/SARH191026086M. [DOI] [Google Scholar]
- 79.Podvorica E., Bekteshi T., Oruqi M., Kalo I. Education of the Patients Living with Heart Disease. Mater. Socio Med. 2021;33:10–15. doi: 10.5455/msm.2021.33.10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Katanolli A.B., Probst-Hensch N., Obas K.A., Gerold J., Zahorka M., Jerliu N., Ramadani Q., Fota N., Merten S. Perceived barriers to physical activity behaviour among patients with diabetes and hypertension in Kosovo: A qualitative study. Bmc Prim. Care. 2022;23:257. doi: 10.1186/s12875-022-01866-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bytyci-Katanolli A., Merten S., Kwiatkowski M., Obas K., Gerold J., Zahorka M., Jerliu N., Ramadani Q., Fota N., Probst-Hensch N. Non-communicable disease prevention in Kosovo: Quantitative and qualitative assessment of uptake and barriers of an intervention for healthier lifestyles in primary healthcare. BMC Health Serv. Res. 2022;22:647. doi: 10.1186/s12913-022-07969-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ejupi V., Demiri L., Qazimi B., Dragusha S. Study on current therapeutic management of breast cancer in hospital and university clinical service of Kosovo. Maced. Pharm. Bull. 2022;68:455–456. doi: 10.33320/maced.pharm.bull.2022.68.03.219. [DOI] [Google Scholar]
- 83.Hoxha I., Islami D.A., Uwizeye G., Forbes V., Chamberlin M.D. Forty-Five Years of Research and Progress in Breast Cancer: Progress for Some, Disparities for Most. JCO Glob. Oncol. 2022;8:e2100424. doi: 10.1200/GO.21.00424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hoxha I., Guda B., Hoti A., Zhubi E., Selmani E., Avdiu B., Cegllar J., Marušič D., Osmani A. Clinical Decision-Making for Heart Failure in Kosovo: A Conjoint Analysis. Int. J. Environ. Res. Public Health. 2022;19:4638. doi: 10.3390/ijerph192214638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Obas K.A., Bytyci-Katanolli A., Kwiatkowski M., Ramadani Q., Fota N., Jerliu N., Statovci S., Gerold J., Zahorka M., Probst-Hensch N. Strengthening Primary Healthcare in Kosovo Requires Tailoring Primary, Secondary and Tertiary Prevention Interventions and Consideration of Mental Health. Front. Public Health. 2022;10:794309. doi: 10.3389/fpubh.2022.794309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ministry of Health . Action Plan 2011–2014 for The Health Sector Strategy 2010–2014. Ministry of Health; Prishtina, Kosovo: 2010. [Google Scholar]
- 87.Hoxha I., Fejza A., Aliu M., Juni P., Goodman D.C. Health system factors and caesarean sections in Kosovo: A cross-sectional study. BMJ Open. 2019;9:e026702. doi: 10.1136/bmjopen-2018-026702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Collier J., Kienzler H. Barriers to cardiovascular disease secondary prevention care in the West Bank, Palestine—A health professional perspective. Confl. Health. 2018;12:27. doi: 10.1186/s13031-018-0165-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Murataj N., Syla B., Krasniqi Y., Bahtiri S., Bekaj D., Beqiri P., Hoxha I.S. Migration Intent of Health Care Workers during the COVID-19 Pandemic in Kosovo. Int. J. Environ. Res. Public Health. 2022;19:1122. doi: 10.3390/ijerph191711122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gheorghe A., Griffiths U., Murphy A., Legido-Quigley H., Lamptey P., Perel P. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: A systematic review. BMC Public Health. 2018;18:975. doi: 10.1186/s12889-018-5806-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data available.