Abstract
Translocase of outer mitochondrial membrane 40 (TOMM40) is located in the outer membrane of mitochondria. TOMM40 is essential for protein import into mitochondria. TOMM40 genetic variants are believed to increase the risk of Alzheimer’s disease (AD) in different populations. In this study, three exonic variants (rs772262361, rs157581, and rs11556505) and three intronic variants (rs157582, rs184017, and rs2075650) of the TOMM40 gene were identified from Taiwanese AD patients using next-generation sequencing. Associations between the three TOMM40 exonic variants and AD susceptibility were further evaluated in another AD cohort. Our results showed that rs157581 (c.339T > C, p.Phe113Leu, F113L) and rs11556505 (c.393C > T, p.Phe131Leu, F131L) were associated with an increased risk of AD. We further utilized cell models to examine the role of TOMM40 variation in mitochondrial dysfunction that causes microglial activation and neuroinflammation. When expressed in BV2 microglial cells, the AD-associated mutant (F113L) or (F131L) TOMM40 induced mitochondrial dysfunction and oxidative stress-induced activation of microglia and NLRP3 inflammasome. Pro-inflammatory TNF-α, IL-1β, and IL-6 released by mutant (F113L) or (F131L) TOMM40-activated BV2 microglial cells caused cell death of hippocampal neurons. Taiwanese AD patients carrying TOMM40 missense (F113L) or (F131L) variants displayed an increased plasma level of inflammatory cytokines IL-6, IL-18, IL-33, and COX-2. Our results provide evidence that TOMM40 exonic variants, including rs157581 (F113L) and rs11556505 (F131L), increase the AD risk of the Taiwanese population. Further studies suggest that AD-associated mutant (F113L) or (F131L) TOMM40 cause the neurotoxicity of hippocampal neurons by inducing the activation of microglia and NLRP3 inflammasome and the release of pro-inflammatory cytokines.
Keywords: Alzheimer’s disease, TOMM40, SNP, microglia, neuroinflammation, NLRP3, NF-κB, hippocampal neurons
1. Introduction
Alzheimer’s disease (AD), characterized by selective neurodegeneration in brain regions involved in emotional and cognitive function, is the most prevalent cause of dementia among older people [1]. Genetic variants increase the risk of developing AD [2,3,4]. The Apolipoprotein E (APOE) gene located at chromosome 19q13.32 is the strongest risk factor for AD and accounts for approximately 50% of the total risk contribution [5,6,7,8,9,10]. However, patients carrying APOE variants do not necessarily develop AD. Genome-wide association studies revealed that genetic variants neighboring APOE loci also increase AD risk [11,12]. Surrounding genes of the APOE loci, such as TOMM40 (Translocase of outer mitochondrial membrane 40), PVRL2, and APOC1, display a strong linkage disequilibrium in the APOE region and could also be involved in the pathogenesis of AD [13,14,15].
The TOMM40 gene is located adjacent to the 5′-upstream of the APOE gene and is one of the APOE-surrounding genes. TOMM40 is a channel-forming subunit of the mitochondrial TOMM complex that is required for protein import into mitochondria [16]. Many studies suggest that the TOMM40 gene may contribute to AD risk [17,18]. Single-nucleotide polymorphisms (SNPs) within the TOMM40 gene are associated with amyloid deposition and influence the metabolism of amyloid beta peptide (Aβ) [19,20,21]. Poly-T repeats’ polymorphism within intron 6 (rs10524523) of the TOMM40 gene has been shown to affect AD onset age and contribute to AD susceptibility by regulating the expression of APOE and TOMM40 genes [22,23,24]. Differential transcription of TOMM40 RNA in the brain has been shown to be an indicator of mitochondrial dysfunction in AD [17]. The majority of TOMM40 genetic variants that were associated with AD susceptibility often reside in noncoding regions with unclear functions [25]. In AD, the related quantitative traits of functional genetic variants of TOMM40 are still unclear. The pathogenic mechanism by which TOMM40 genetic variants increase the risk of AD remains unknown.
Microglial-mediated neuroinflammation, the inflammatory response of CNS, is involved in the etiopathogenesis of AD [26,27]. Under physiological status, microglia, which act as resident macrophages of CNS, mediate the development of CNS and regulate immune responses in CNS [28]. In the presence of pathological or inflammatory stimuli, microglia change from a resting state to an activated state and secrete pro-inflammatory cytokines, including interleukin-1β (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α), which subsequently cause the degeneration of CNS neurons [26,27,29]. Under pathological or inflammatory conditions, a crucial step for damage-associated molecular pattern (DAMP)- or pathogen-associated molecular pattern (PAMP)-induced microglial activation is the oligomerization and activation of the microglial NLRP3 inflammasome complex, which is composed of nucleotide-binding oligomerization domain and leucine-rich-repeat-and pyrin-domain-containing 3 (NLRP3), the apoptosis-associated speck-like protein containing a CARD (ASC), and pro-caspase-1 [30,31,32,33]. The dysregulated overactivity of the microglial NLRP3 inflammasome resulting from microglial activation is involved in the pathogenesis of AD [34,35,36].
Mitochondria are a major source of intracellular ROS and are sensitive to oxidative stress [37]. Mitochondrial malfunction is involved in the pathogenesis of AD [38]. TOMM40 is vital for maintaining mitochondrial function and is involved in the influx of proteins and Aβ into mitochondria [16,39,40]. In the brains of AD patients, Aβ is accumulated in the mitochondrial import channel and causes mitochondrial dysfunction [41]. Impaired TOMM40-mediated protein transport of mitochondria could lead to the accumulation of Aβ in mitochondrial cristae, which results in mitochondrial malfunction and the overproduction of ROS [42]. Increased formation of mitochondrial ROS activates the mitogen-activated protein kinase (MAPK) cascade, resulting in microglial activation [43]. Moreover, the overproduction of ROS activates the nuclear factor-κB (NF-κB) pathway, which causes activation of the NLRP3 inflammasome and neuroinflammation [44]. Therefore, it is possible that mutations of TOMM40 could cause mitochondrial malfunction and oxidative stress, resulting in microglial activation and increased risk of AD.
In this study, we identified genetic variants of the TOMM40-APOE region and determined the significance of TOMM40 variants in Taiwanese AD patients. Missense variants within the TOMM40 gene, rs157581 (c.339T > C, p.Phe113Leu) and rs11556505 (c.393C > T, p.Phe131Leu), were associated with increased risk of AD. Our results also demonstrated that mutant (F113L) or (F131L) TOMM40 caused activation of the NLRP3 inflammasome and microglia, leading to the release of pro-inflammatory cytokines and resulting in the cell death of hippocampal neurons.
2. Results
2.1. AD Patients Exhibit Genetic Variants within TOMM40 Gene
A high-density whole-genome association study showed strong associations between SNPs neighboring the APOE loci and AD risk [11]. Although APOE is a strong risk factor for AD, it is believed that additional factors with the APOE locus contribute to the pathogenesis of AD [18,45,46]. The TOMM40 gene is within APOE-surrounding regions and is located in proximity to the APOE gene [18,46]. DNA samples from 80 Taiwanese AD patients were examined using a targeted panel of whole-genome sequencing. When compared with the 1000 Genome Databases, genetic hotspots within the TOMM40-APOE region were identified as AD susceptibility (Table 1). Exonic variants included rs772262361 (a synonymous variant within TOMM40, c.198A > G, p.Ser66=), rs157581 (a missense variant in TOMM40, c.339T > C, p.Phe113Leu), rs11556505 (a missense variant within TOMM40, c.393C > T, p.Phe131Leu), and rs440446 (a missense variant in APOE, p.Asn14Lys) (Table 1). SNP rs772262361, located in the CpG-rich loci, was a novel mutation (Supplementary Figure S1). Intronic variants, including rs184017, rs2075650, and rs157582, were found in Taiwanese AD patients (Table 1). We further replicated the association of the three TOMM40 functional hotspots, including rs772262361, rs157581, and rs11556505, with AD susceptibility using another set of AD patients and controls.
Table 1.
Genetic variants within TOMM40-APOE region associated with risk of AD.
| Gene | SNP | Position | MAF (Cases/NC) | MAF * dbSNP | OR (95% CI) | p Value |
|---|---|---|---|---|---|---|
| PVRL2: Intron variant | rs394221 | 45368424 | 0.51/0.38 | 0.45 | 1.7 (1.2~2.4) | 0.001 |
| TOMM40:Synonymous, p.Ser66= | rs772262361 | 45394870 | 0.013/0.0 | 0.00004 | - | - |
| TOMM40: Intron | rs184017 | 45394969 | 0.34/0.16 | 0.20 | 2.8 (2.0~4.0) | 4.2 × 10−8 |
| TOMM40: Intron | rs2075650 | 45395619 | 0.25/0.07 | 0.13 | 4.2 (2.8~6.1) | 1.1 × 10−10 |
| TOMM40: Missense, p.Phe113Leu | rs157581 * | 45395714 | 0.38/0.23 | 0.23 | 2.1 (1.5~2.9) | 4.4 × 10−5 |
| TOMM40: Missense, p.Phe131Leu | rs11556505 * | 45396144 | 0.26/0.10 | 0.11 | 3.3 (2.2~4.8) | 2.5 × 10−8 |
| TOMM40: Intron | rs157582 | 45396219 | 0.34/0.18 | 0.22 | 2.4 (1.7~3.3) | 3.3 × 10−6 |
| APOE: Missense, p.Asn14Lys | rs440446 * | 45409167 | 0.56/0.33 | 0.38 | 2.6 (1.9~3.6) | 1.4 × 10−8 |
| APOE: Intron | rs769449 | 45412079 | 0.25/0.08 | 0.11 | 3.6 (2.4~5.3) | 2.7 × 10−9 |
* SNPs are missense variants.
2.2. Exonic SNP of TOMM40 Are Linked to Increased AD Susceptibility
The frequency of rs772262361 in Taiwan was further examined in normal controls (NC) of Taiwan Biobank (controls). All three functional variants (rs772262361, rs157581, and rs11556505) were evaluated in 213 normal controls (NC) that were ascertained in this study, 393 AD patients, and 1025 controls from Taiwan Biobank. The genotype and allele frequency of TOMM40 among NC, AD patients, and controls were displayed in Table 2. SNPs were considered in Hardy–Weinberg equilibrium at a significance level of 0.05. Two TOMM40 SNPs, rs157581 and rs11556505, were significantly associated with AD.
Table 2.
Demographics of normal controls (NC), AD patients, and controls from Taiwan Biobank.
| NC | AD Patients | Controls * | p Value 1 | p Value 2 | |
|---|---|---|---|---|---|
| Number | 213 | 393 | 1025 | ||
| Age (years) | 67.4 ± 10.3 | 74.0 ± 8.7 | 58.7 ± 5.4 | <0.0001 | <0.0001 |
| Men, N (%) | 111 (52.1) | 142 (36.1) | 524 (51.1) | 0.0001 | <0.0001 |
| Education (years) | 8.1 ± 4.5 | 6.2 ± 4.7 | 5.3 ± 1.1 | <0.0001 | <0.0001 |
| Hypertension, N (%) | 99 (46.5) | 191 (48.6) | 207 (20.2) | 0.62 | <0.0001 |
| Diabetes, N (%) | 153 (71.8) | 271 (69.0) | 81 (7.9) | 0.46 | <0.0001 |
| Global cognition, MMSE | 24.3 ± 5.4 | 16.5 ± 6.5 | 27.1 ± 2.6 | <0.0001 | <0.0001 |
| APOE ε4 carrier, N (%) | 12 (5.63) | 201 (51.2) | 166 (16.2) | <0.0001 | <0.0001 |
| TOMM40 | |||||
| rs772262361, p.Ser66 = AA/AG (%) | 100/0 | 99.5/0.5 | - | 0.24 ** | - |
| rs157581, p.Phe113Leu TT/TC/CC (%) | 67.3/30.3/2.4 | 40/49.9/10.1 | 59.9/35/5.1 | <0.0001 | <0.0001 |
| rs11556505, p.Phe131Leu CC/CT/TT (%) | 92.6/7.4/0 | 54.4/40/5.6 | 81.9/17.3/0.9 | <0.0001 | <0.0001 |
Data are expressed as percentages or mean ± S.D. * Controls from Taiwan Biobank were from the whole-genome sequencing (WGS) database from Taiwan Biobank. Comparisons were analyzed using χ2-tests (** Fisher’s exact test) or t-tests where appropriate. p-value 1: NC versus AD; p-value 2: Control from Taiwan Biobank versus AD.
2.3. AD-Associated TOMM40 Genetic Variants, but Not Wild-Type TOMM40, Causes Mitochondrial Dysfunction and Oxidative Stress of Microglial Cells
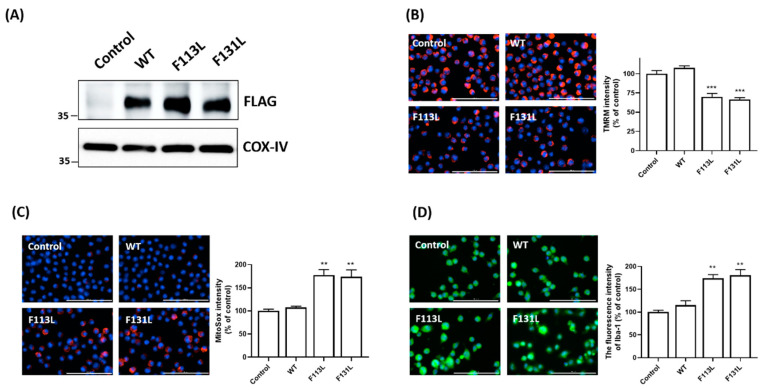
In this study, we hypothesized that the AD-associated genetic mutation of TOMM40 causes mitochondrial malfunction and oxidative stress in microglia. To test this hypothesis, WT TOMM40 and AD-associated TOMM40 genetic variants, (F113L) and (F131L) TOMM40, were transiently expressed in BV2 microglial cells (Figure 1A). Compared to control cells or cells expressing WT TOMM40, a reduction in the fluorescence intensity of TMRM, which is a dye of mitochondrial membrane potential (ΔΨm), and ΔΨm depolarization was found in BV2 microglial cells transfected with cDNA of (F113L) or (F131L) TOMM40 (Figure 1B). Imaging analysis of MitoSox showed that the fluorescence level of MitoSox and the mitochondrial level of superoxide, which is a major ROS, were significantly upregulated in BV2 microglial cells expressing (F113L) or (F131L) TOMM40 (Figure 1C).
Figure 1.
Mutant (F113L) or (F131L) TOMM40 causes dysfunction and oxidative stress of mitochondria, leading to microglial activation. (A) BV2 microglial cells were transfected with empty pcDNA3 vector (control), cDNA of FLAG-tagged wild-type (WT), (F113L), or (F131L) TOMM40. Immunoblotting assay showed that WT or mutant TOMM40 was expressed in the mitochondrial fraction of BV2 microglial cells. Cytochrome c oxidase subunit IV (COX-IV) was used as an internal control for mitochondrial fraction. (B) Compared to control cells or cells expressing WT TOMM40, decreased TMRM fluorescence intensity and depolarization of mitochondrial membrane potential were BV2 microglial cells expressing mutant (F113L) or (F131L) TOMM40. (C) Expression of mutant (F113L) or (F131L) TOMM40 significantly increased fluorescence intensity of MitoSox and mitochondrial superoxide level in BV2 microglial cells. (D) Immunofluorescence staining of microglial marker Iba-1demonstrated that expression of (F113L) or (F131L) TOMM40 led to activation of BV2 microglial cells by upregulating protein expression of Iba-1. Scale bar is 100 μm. Each bar represents mean ± S.D. value of four experiments. Each experiment was performed in triplicate. ** p < 0.01, *** p < 0.001 compared to control BV2 microglial cells.
2.4. AD-Associated TOMM40 Genetic Variants Cause Microglial Activation
Mutant (F113L) or (F131L) TOMM40-induced mitochondrial malfunction and oxidative stress (Figure 1B,C) could lead to the activation of microglial cells. In accordance with this hypothesis, immunofluorescence imaging staining demonstrated that compared with control cells or cells expressing WT TOMM40, upregulated protein expression of microglial protein marker ionized calcium-binding adaptor molecule 1 (Iba-1) was observed in BV2 microglia cells transfected with cDNA of (F113L) or (F131L) TOMM40 (Figure 1D).
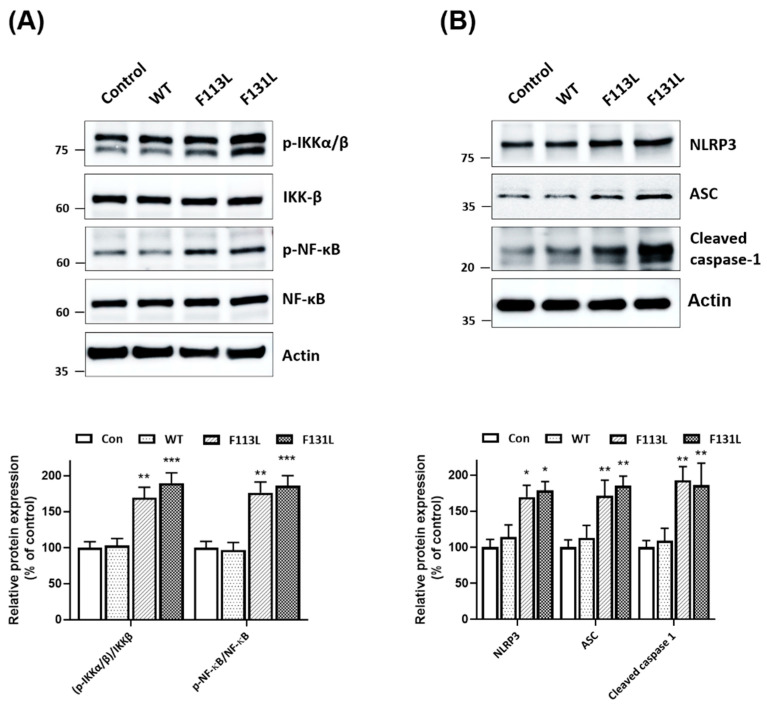
2.5. Mutant (F113L) or (F131L) TOMM40 Activates NF-κB Cascade and NLRP3 Inflammasome in Microglial Cells
In this study, it was hypothesized that (F113L) or (F131L) TOMM40-induced malfunction and oxidative stress of mitochondria leads to the activation of the NF-κB signaling cascade and the NLPR3 inflammasome in microglial cells. Consistent with this hypothesis, immunoblotting assays showed that the expression of (F113L) or (F131L) TOMM40 in microglial cells increased the protein expression of phospho-IKKα/βSer176/180 and active phospho-NF-κB p65 in BV2 microglial cells (Figure 2A). Immunoblotting assays demonstrated that mutant (F113L) or (F131L) TOMM40 caused the activation of the NLRP3 inflammasome by upregulating protein levels of NLRP3 and ASC and cleaved active caspase-1 in BV2 microglial cells (Figure 2B).
Figure 2.
TOMM40 genetic variants induce activation of NF-κB signaling and NLRP3 inflammasome in microglial cells. (A) Western blot analysis showed that expression of (F113L) or (F131L) TOMM40 induced activation of NF-κB cascade by increasing protein expression of phospho-IKKα/βSer176/180 and phospho-NF-κB p65Ser536 in BV2 microglial cells. (B) Compared with control or cDNA of WT TOMM40-transfected cells, transfection of cDNA encoding (F113L) or (F131L) TOMM40 caused activation of NLRP3 inflammasome by upregulating protein level of NLRP3 and ASC or cleaved caspase-1 in BV2 microglial cells. Each bar shows mean ± S.D. of four experiments. * p < 0.05, ** p < 0.01, *** p < 0.001 compared to control BV2 microglial cells.
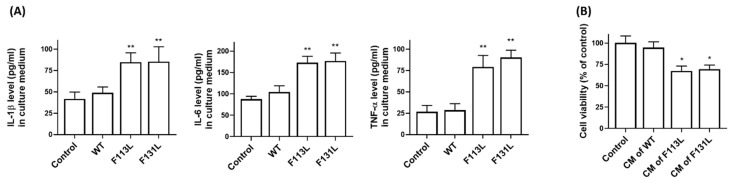
2.6. AD-Associated TOMM40 Genetic Variants Cause the Release of Pro-Inflammatory Cytokines from Microglia Cells, Leading to Cell Death of Hippocampal Neurons
NLPR3 inflammasome activation in microglial cells results in the overproduction and release of pro-inflammatory cytokines, leading to neuronal loss [40]. ELISA analysis indicated that the levels of pro-inflammatory cytokines, including IL-1β, IL-6, and TNF-α, were significantly increased in the culture medium (CM) from BV2 microglial cells expressing (F113L) or (F131L) TOMM40 (Figure 3A). To provide evidence that pro-inflammatory cytokines released from BV2 cells expressing (F113L) or (F131L) TOMM40 cause neuronal death, the CM of HT22 hippocampal neuronal cells was replaced with the CM of BV microglia transfected with cDNA of WT, (F113L), or (F131L) TOMM40. As shown in Figure 3B, the CM of BV2 microglial cells expressing (F113L) or (F131L) TOMM40 significantly decreased the cell viability of HT22 hippocampal neuronal cells.
Figure 3.
TOMM40 genetic variants induce the secretion of pro-inflammatory cytokines in microglial cells, leading to cell death of hippocampal neurons. (A) Compared to control cells or cells expressing WT TOMM40, BV2 microglial cells’ expression of (F113L) or (F131L) TOMM40 significantly increased secretion of pro-inflammatory IL-1β, IL-6, or TNF-α in culture medium of BV2 microglial cells. (B) Culture medium (CM) of HT22 hippocampal neurons was replaced with CM from BV2 microglial cells transfected with cDNA of WT, (F113L) or (F131L) TOMM40. One day after replacement, CM of BV2 microglia cells expressing mutant (F113L) or (F131L) TOMM40 significantly reduced cell viability of HT22 hippocampal neurons. Each bar represents mean ± S.D. of four experiments. Each experiment was performed in triplicate. * p < 0.05 or ** p < 0.01 compared to control BV2 microglial cells or HT22 hippocampal neurons.
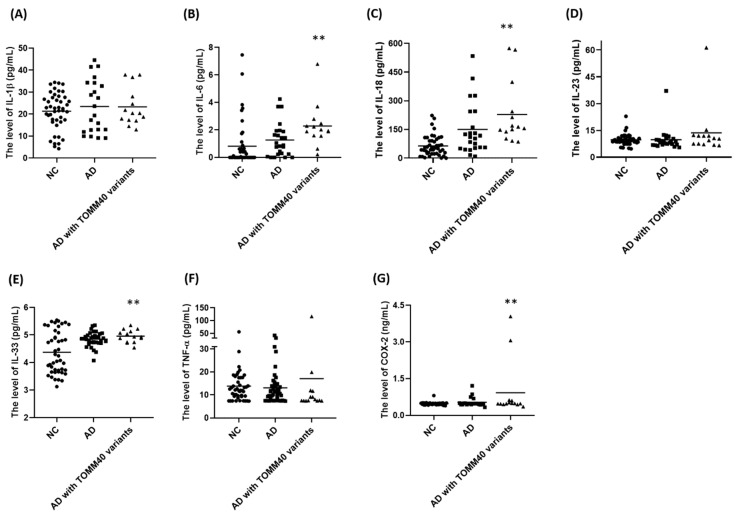
2.7. Plasma Levels of IL-6, IL-18, IL-33, and COX-2 Are Upregulated in AD Patients Carrying TOMM40 Genetic Variants
According to our hypothesis that AD-associated TOMM40 genetic variants cause microglial activation, plasma levels of cytokines and COX-2 are expected to be upregulated in AD patients carrying TOMM40 genetic variants. ELISA assays demonstrated that plasma levels of IL-6, IL-18, IL-33, and COX-2 were significantly increased in AD patients carrying TOMM40 genetic variants, including rs772262361, rs157581, and rs11556505 (Figure 4 and Table 3).
Figure 4.
Plasma levels of IL-6, IL-18, IL-33, and COX-2 are significantly increased in AD patients carrying TOMM40 genetic variants. (A–G) ELISA assay showed that, compared to NC or AD patients, plasma levels of IL-6, IL-18, IL-33, and COX-2 were significantly upregulated in AD patients carrying TOMM40 genetic variants, including rs772262361, rs157581, and rs11556505. ** p < 0.01 compared with NC.
Table 3.
The plasma level of cytokines or COX-2 between NC and AD.
| NC (n = 45) | AD (n = 37) | AD with TOMM40 Genetic Variants (n = 14) | p Value | |
|---|---|---|---|---|
| Age (years) | 72.1 ± 9.0 | 72.9 ± 6.0 | 71.29 ± 6.3 | 0.6740 |
| Men/Female | 21/24 | 14/23 | 4/10 | 0.4275 |
| APOE ε4 carrier (%) | 0 | 32.4 | 85.7 | <0.0001 |
| IL-1β (pg/mL) | 21.4 ± 8.4 | 23.1 ± 10.8 | 23.3 ± 8.6 | 0.3884 |
| IL-6 (pg/mL) | 0.8 ± 1.6 | 1.6 ± 1.5 | 2.3 ± 1.6 | 0.0237 |
| IL-18 (pg/mL) | 64.4 ± 53.0 | 193.5 ± 200.6 | 228.66 ± 164.7 | <0.0001 |
| IL-23 (pg/mL) | 9.7 ± 3.2 | 10.5 ± 8.9 | 13.7 ± 13.9 | 0.5867 |
| IL-33 (pg/mL) | 4.4 ± 0.8 | 4.9 ± 0.3 | 5.0 ± 0.2 | 0.0005 |
| TNF-α (pg/mL) | 13.8 ± 8.1 | 14.5 ± 18.9 | 17.1 ± 28.8 | 0.9342 |
| COX-2 (ng/mL) | 0.5 ± 0.06 | 0.7 ± 0.7 | 0.9 ± 1.1 | 0.0453 |
Data are expressed as percentages or mean ± S.D.
3. Discussion
The APOE gene located at chromosome 19q13.32 is a strong risk gene for AD and accounts for approximately 50% of AD cases [5,6]. APOE is involved in the clearance and aggregation of the amyloid-β peptide and tau neurofibrillary degeneration [8]. For AD pathology, APOE has been shown to be co-localized with cholesterol and fibrillary Aβ in neuritic plaques and neurofibrillary tangles [47]. APOE genotypes are linked to lipid homeostasis and neuroinflammation [48]. APOE ε2/ε3/ε4 alleles are haplotypes constructed by two missense variants, rs7412 and rs429358 [49]. The APOE ε4 allele is the strongest risk factor for AD in African American and Caucasian populations [50]. Compared with AD patients in western countries, the frequency of the APOE ε4 allele is lower in the Asian population [51]. The incidence of AD is similar between Caucasian and Chinese populations [52]. Other genetic modifiers are likely to contribute to the pathogenesis of AD in Asian patients [46,53]. Genetic variants in the TOMM40-APOE locus could increase the susceptibility of AD [18,46,54,55,56]. The TOMM40 gene adjacent to the APOE gene is in strong linkage disequilibrium with APOE [57]. Mutations within the TOMM40 gene are implicated in the increased risk and pathogenesis of AD [58,59,60,61]. Several functional SNPs within the TOMM40 gene are identified in late-onset AD (LOAD) [22]. In the Asian AD population, APOE and TOMM40 variants synergistically increase the risk of AD [46]. Therefore, TOMM40 could be an important risk factor for AD in the Taiwanese AD population.
In this study, we hypothesized that mutations of the TOMM40 gene contribute to increased AD susceptibility in the Taiwanese population. To test this hypothesis, NGS analysis was performed to identify the genetic variants with the TOMM40 locus of Taiwanese AD patients. In this study, exonic variants, including rs772262361, rs157581 (c.339T > C, p.Phe113Leu), rs11556505 (c.393C > T, p.Phe131Leu), and intronic variants, including rs184017, rs2075650, and rs157582, were identified in Taiwanese AD patients. Further genetic association studies suggest that two exonic SNPs of TOMM40, rs157581 and rs11556505, are linked to increased AD risk in the Taiwanese population. Previous studies reported that TOMM40 poly-T repeats polymorphism within intron 6 (rs10524523) decreases the onset age of AD and contributes to increased AD susceptibility in Caucasian populations by regulating the expression of TOMM40 and APOE transcription [23,62]. TOMM40 SNPs, including rs157580, rs2075650, and rs157581, increase the AD risk in Canadian and Italian populations [59,61]. TOMM40 rs10524523 is associated with decreased volume of gray matter and impaired cognition in AD patients [63]. TOMM40 SNPs, rs10524523 and rs2075650, are statistically related to cognitive function, brain integrity, and the alternation of the inflammatory pathway [64,65].
Microglia, which are innate immune cells of CNS, play a vital role in clearing pathogenic molecules and mediating the neuroinflammatory reaction [26,66]. Under pathological conditions, PAMP or DAMP induces the activation of microglia and NLRP3 inflammasome and resulting in neuroinflammation [34,67]. Activated microglia release pro-inflammatory cytokines, including TNF-α, IL-1β, and IL-6, and cause neuronal death [68,69]. Microglial activation-induced neuroinflammation is one of the important mechanisms underlying the pathogenesis of AD [26,70,71]. Several lines of evidence suggest that mitochondrial malfunction of microglia induces microglial activation and is involved in AD pathogenesis [66]. The accumulation of Aβ within mitochondria causes mitochondrial dysfunction and oxidative stress [70,72]. TOMM40 is essential for normal mitochondrial function by mediating the import of proteins, including Aβ, into mitochondria [40,73]. In this study, it was hypothesized that impaired function of AD-associated mutant TOMM40 including (F113L) and (F131L) TOMM40 could cause the accumulation of mitochondrial Aβ and result in mitochondrial malfunction and oxidative stress of microglia, leading to the activation of microglia and the NLRP3 inflammasome, the release of neurotoxic pro-inflammatory cytokines, and the subsequent cell death of hippocampal neurons. In accordance with our hypothesis, the expression of AD-associated TOMM40 genetic variants, (F113L) and (F131L) TOMM40, caused mitochondrial dysfunction by reducing mitochondrial membrane potential and oxidative stress by increasing the mitochondrial level of superoxide in BV2 microglial cells. AD-associated (F113L) or (F131L) TOMM40-induced mitochondrial malfunction and oxidative stress lead to the activation of the NLRP3 inflammasome and inflammatory NF-κB pathway in BV2 microglial cells. Furthermore, pro-inflammatory TNF-α, IL-1β, and IL-6 released by mutant (F113L) or (F131L) TOMM40-activated BV2 microglial cells cause the cell death of hippocampal neurons. Consistent with our hypothesis that AD-associated mutant (F113L) or (F131L) TOMM40 cause neurotoxicity and increase AD risk by inducing microglial activation, Taiwanese AD patients carrying TOMM40 missense (F113L) or (F131L) variants exhibit an increased plasma level of IL-6, IL-18, IL-33, and COX-2.
In summary, the results of this study provide evidence that TOMM40 exonic variants, including rs157581 (F113L) and rs11556505 (F131L), increase the AD risk in the Taiwanese population. Further studies suggest that AD-associated mutant (F113L) or (F131L) TOMM40 cause the neurotoxicity of hippocampal neurons by inducing the activation of microglia and NLRP3 inflammasome and the release of pro-inflammatory cytokines.
4. Materials and Methods
4.1. Patients and Control Subjects
The Institutional Review Board of Chang Gung Memorial Hospital governed this study (IRB No.201700444B0C602, 201802324B0, and 202002551B0). Ethical approval for this study was granted by the IRB of Taiwan Biobank (approval number: 201506095RINC and TWBR10801-01). All participants submitted informed consent. Probable AD patients and age-matched control participants were recruited from the Department of Neurology, Chang Gung Memorial Hospital, Linkou Medical Center. AD was diagnosed according to the criteria of the recommendations from the National Institute on Aging- Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease [74]. Patients who had a Modified Hachinski ischemic score of >4 or met the NINDS-AIREN criteria for vascular dementia were excluded [75]. This study included two control groups. One of the control groups was enrolled subjects who visited CGMH for a health exam or treatment for diseases other than neurodegenerative diseases or cerebrovascular diseases. The other control group was from whole-genome sequencing (WGS) from Taiwan Biobank. Taiwan Biobank has officially developed data from community volunteers (URL: https://tai-wanview.twbiobank.org.tw/browse3, accessed on 14 February 2023).
4.2. DNA Extraction, WGS and Data Processing
Genomic DNA was obtained from blood samples with Gentra Puregene Blood Kit (Qiagen). After library amplification, DNA was analyzed for deep-targeted sequencing on the Ion Torrent PGM system. The panel covering PVRL2 (GRCh38: 19:44,846,135-44,889,227), TOMM40 (GRCh38: 19:44,891,219-44,903,688, and APOE (GRCh38: 19:44,905,748-44,909,394) was used to examine the genetic variants in 80 AD patients. In total, 98.5% of target bases were read more than 20 times for the depth of coverage. Sequencing data were aligned to the hg38 human reference genome and analyzed using Torrent Suite Software. Variants were filtered by Bam-Utils v1.0.2. Filtered variants were annotated using SnpEff v4.2. The in-house genetic database was used to exclude variants in 250 healthy subjects. Integrative Genome Viewer (IGV) software (http://software.broadinstitute.org/igv/, accessed on 14 February 2023) was used for mutation analysis. Allele frequency <1% in 1000 Genomes were defined as rare genetic variants. The joint variant calling file (VCF) was annotated with refGene gene regions, single-nucleotide polymorphism (SNP) effects, functional effect prediction tools, and the Exome Variant Server (EVS) and 1000 Genomes minor allele frequencies (MAFs) using Annovar (http://www.openbioinformatics.org/annovar/, accessed on 14 February 2023). Annotated VCF was analyzed as follows: Variants in exons and splice sites of PVRL2, TOMM40, and APOE genes were extracted with MAF of <1% in genetic databases, including the dbSNP database and the 1000 Genomes project. The variants were further interpreted and then manually annotated using the Human Gene Mutation Database (HGMD, www.hgmd.cf.ac.uk, accessed on 14 February 2023), AD&FTD (www.molgen.ua.ac.be/admutations/, accessed on 14 February 2023), AlzForum (www.alzforum.org/mutations, accessed on 14 February 2023) databases, and literature searches. Genetic variants in target genes were confirmed using Sanger sequencing.
4.3. Sequencing and Genotyping of TOMM40 Genetic Variants
Genetic variants and SNPs of TOMM40 identified from the cohort were further confirmed by performing TaqMan analysis or Sanger DNA sequencing (Applied Biosystems, Framingham, MA, USA). SNP rs157581, rs11556505, and rs440446 were examined using TaqMan genotyping probes (C_3084827_10/rs157581, C_2769404_10/rs11556505, C_905012_20/rs440446, Thermo Fisher Scientific, Waltham, MA, USA).
4.4. Cell Culture
BV2 mouse microglial cells and HT22 mouse hippocampal neuronal cells were purchased from Elabscience (Cat. EP-ML-0697 and EP-CL-0493) and maintained in a DMEM medium containing 10% FBS. Cells were grown at 37 °C in humidified air with 5% CO2 and then sub-cultured into different culture plates.
4.5. Transfection of TOMM40 Genetic Variants
The cDNA of WT, (F113L), or (F131L) TOMM40 was subcloned into the pcDNA3 expression vector (Invitrogen, Carlsbad, CA, USA) containing the FLAG (DYKDDDDK)-tag sequence. WT or mutant TOMM40 plasmids were transfected into BV2 microglial cells using the Lipofectamine 2000 transfection reagent (Thermo Fisher Scientific). After transfection for 2 or 3 days, transfected cells were used for the experiments described below.
4.6. Determination of Mitochondrial Membrane Potential (ΔΨm) and Mitochondrial Superoxide
To analyze ΔΨm, control or transfected BV2 microglial cells interacted with 100 nM of ΔΨm-sensitive dye tetramethylrhodamine methyl ester (TMRM; Thermo Fisher Scientific) for 30 min at 37 °C. The mitochondrial level of superoxide was measured by incubating BV2 microglial cells for 30 min at 37 °C with 5 μM MitoSox Red dye (Thermo Fisher Scientific), which is oxidized by superoxide and produces red fluorescence. TMRM or MitoSox Red images of 36 fields per well were obtained with the aid of the LionHeart FX automatic microscope (BioTek, Winooski, VT, USA). Fluorescent signals of TMRM or MitoSox Red were quantified and analyzed using Gen5 software (BioTek).
4.7. Immunofluorescence Staining of Iba-1
BV2 microglial cells were fixed with 4% paraformaldehyde and permeabilized with 0.5% Triton X-100. Fixed cells interacted with the anti-Iba-1 primary antibody (iReal, Hsinchu, Taiwan). Cells then interacted with the Alexa Fluor 488-conjugated secondary antibody (Invitrogen). For each imaging experiment, thirty-six images of control or transfected BV2 microglial cells were taken using the LionHeart FX automatic microscope (BioTek), and fluorescence intensity was then analyzed using Gen5 software (BioTek).
4.8. Immunoblotting Assays
Proteins were extracted from control or transfected BV2 microglial cells using the RIPA lysis buffer. Proteins were separated using SDS-polyacrylamide gel electrophoresis and transferred to PVDF membranes. Membranes interacted overnight at 4 °C with diluted primary antibodies (Supplemental Table S1). After washing, membranes interacted with HRP-conjugated anti-rabbit or anti-mouse secondary antibodies. Subsequently, immunoreactive proteins were detected using the ECL kit. The relative protein level was quantified by using Image J software and normalized to β-actin.
4.9. Measurement of Pro-Inflammatory Cytokines in Culture Medium
The level of IL-1β, IL-6, or TNF-α was measured using an ELISA kit (Abcam, Waltham, MA, USA). Briefly, 100 μL of the culture medium of control or transfected BV2 microglial cells and cytokine standards were added to 96-well pales coated with the primary antiserum. Then, the biotinylated antibody was loaded into the wells. Following 1 h incubation, the HRP-streptavidin reagent was added to the 96 wells, and OD450 was measured using a microplate reader.
4.10. Determination of Cell Viability of HT22 Hippocampal Neurons
The culture medium (CM) of HT22 hippocampal neuronal cells was replaced with CM of control or transfected BV2 microglial cells. Following 24-h incubation, the cell viability of HT22 hippocampal neurons was assessed using the CCK-8 assay kit (Sigma-Aldrich). Briefly, WST-8 was applied to culture wells for 1 h, and then OD at 450 nm was measured with a spectrophotometer.
4.11. Measurement of Plasma Levels of Cytokines or COX-2
Plasma levels of IL-1β, IL-6, IL18, IL-23, IL-33, TNF-α, and COX-2 were determined using an ELISA kit (Abcam). Briefly, 10 μL of the plasma sample was loaded into 96-well pales coated with the primary antibody at 25 °C for 150 min. Subsequently, the biotinylated secondary antiserum was added to the wells. After 1 h incubation, the HRP-streptavidin reagent was loaded into the 96 wells, and then OD450 was detected on a microplate reader.
4.12. Statistics
All results were expressed as the mean ± S.D. value. Demographic data for clinical subjects and the frequencies of genotypes between AD patients and control subjects were compared using an χ2-test (Fisher’s exact test) or t-test, where appropriate. All results were analyzed by using the GraphPad Prism Program and SAS software version 9.1.3. For cells’ experimental results, statistical significance was evaluated by a one-way ANOVA with Tukey’s post-hoc test (multiple groups) or unpaired two-tailed Student’s t-test (two groups). Statistical differences were considered significant at a p-value of <0.05.
Acknowledgments
We thank the Whole-Genome Research Core Laboratory of Human Diseases, Chang Gung Memorial Hospital, Keelung, Taiwan, and the Taiwan Biobank for supporting the WGS database for the general Chinese population controls used in this study.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms24044085/s1.
Author Contributions
Y.-C.C. (Yi-Chun Chen), Y.-S.L., H.-L.W. and C.-C.C. conceptualized the study and designed the experiments. L.-S.W. and K.-H.W. performed the experiments and analyzed the data. S.-C.C., W.-M.H., Y.-H.H., Y.-Y.W. and Y.-C.C. (Yi-Chuan Chu) conceived and designed the experiments. Y.-C.C. (Yi-Chun Chen), H.-L.W. and C.-C.C. supervised the project and wrote the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The Institutional Review Board of Chang Gung Memorial Hospital governed this investigation (IRB No.201700444B0C602, 201802324B0 and 202002551B0). Ethical approval for the study was granted by the IRB of Taiwan Biobank before the study was conducted (approval number: 201506095RINC and TWBR10801-01).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was supported by the Chang Gung Medical Foundation, Taiwan (CMRPG3G0962, CMRPG3L1341 to YC Chen; CMRPG3K0952 and CMRPD1M0291 CMRPD1H0283 and CMRPD1M0141 to HL Wang; CMRPG3K0952, CMRPG3J0763 and CMRPD1M0291 to CC Chiu) and the Ministry of Science and Technology, Taiwan (MOST108-2314-B-182A-047, MOST110-2314-B-182A-070, 111-2314-B-182A-134-MY2 to YC Chen; MOST111-2326-B-182-001-MY3 MOST110-2320-B-182-003-MY3 to HL Wang; MOST109-2314-B-182-081-MY3 and MOST111-2326-B-182-001-MY3 to CC Chiu).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Scheltens P., De Strooper B., Kivipelto M., Holstege H., Chetelat G., Teunissen C.E., Cummings J., van der Flier W.M. Alzheimer’s disease. Lancet. 2021;397:1577–1590. doi: 10.1016/S0140-6736(20)32205-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jia L., Li F., Wei C., Zhu M., Qu Q., Qin W., Tang Y., Shen L., Wang Y., Shen L., et al. Prediction of Alzheimer’s disease using multi-variants from a Chinese genome-wide association study. Brain. 2021;144:924–937. doi: 10.1093/brain/awaa364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sierksma A., Escott-Price V., De Strooper B. Translating genetic risk of Alzheimer’s disease into mechanistic insight and drug targets. Science. 2020;370:61–66. doi: 10.1126/science.abb8575. [DOI] [PubMed] [Google Scholar]
- 4.Gatz M., Reynolds C.A., Fratiglioni L., Johansson B., Mortimer J.A., Berg S., Fiske A., Pedersen N.L. Role of genes and environments for explaining Alzheimer disease. Arch. Gen. Psychiatry. 2006;63:168–174. doi: 10.1001/archpsyc.63.2.168. [DOI] [PubMed] [Google Scholar]
- 5.Beecham G.W., Hamilton K., Naj A.C., Martin E.R., Huentelman M., Myers A.J., Corneveaux J.J., Hardy J., Vonsattel J.P., Younkin S.G., et al. Genome-Wide Association Meta-analysis of Neuropathologic Features of Alzheimer’s Disease and Related Dementias. PLoS Genet. 2014;10:e1004606. doi: 10.1371/journal.pgen.1004606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chuang W.L., Hsieh Y.C., Wang C.Y., Kuo H.C., Huang C.C. Association of apolipoproteins e4 and c1 with onset age and memory: A study of sporadic Alzheimer disease in Taiwan. J. Geriatr. Psychiatry Neurol. 2010;23:42–48. doi: 10.1177/0891988709351804. [DOI] [PubMed] [Google Scholar]
- 7.Genin E., Hannequin D., Wallon D., Sleegers K., Hiltunen M., Combarros O., Bullido M.J., Engelborghs S., De Deyn P., Berr C., et al. APOE and Alzheimer disease: A major gene with semi-dominant inheritance. Mol. Psychiatry. 2011;16:903–907. doi: 10.1038/mp.2011.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Serrano-Pozo A., Das S., Hyman B.T. APOE and Alzheimer’s disease: Advances in genetics, pathophysiology, and therapeutic approaches. Lancet Neurol. 2021;20:68–80. doi: 10.1016/S1474-4422(20)30412-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martens Y.A., Zhao N., Liu C.C., Kanekiyo T., Yang A.J., Goate A.M., Holtzman D.M., Bu G. ApoE Cascade Hypothesis in the pathogenesis of Alzheimer’s disease and related dementias. Neuron. 2022;110:1304–1317. doi: 10.1016/j.neuron.2022.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raulin A.C., Doss S.V., Trottier Z.A., Ikezu T.C., Bu G., Liu C.C. ApoE in Alzheimer’s disease: Pathophysiology and therapeutic strategies. Mol. Neurodegener. 2022;17:72. doi: 10.1186/s13024-022-00574-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coon K.D., Myers A.J., Craig D.W., Webster J.A., Pearson J.V., Lince D.H., Zismann V.L., Beach T.G., Leung D., Bryden L., et al. A high-density whole-genome association study reveals that APOE is the major susceptibility gene for sporadic late-onset Alzheimer’s disease. J. Clin. Psychiatry. 2007;68:613–618. doi: 10.4088/JCP.v68n0419. [DOI] [PubMed] [Google Scholar]
- 12.Andrews S.J., Fulton-Howard B., Goate A. Interpretation of risk loci from genome-wide association studies of Alzheimer’s disease. Lancet Neurol. 2020;19:326–335. doi: 10.1016/S1474-4422(19)30435-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guerreiro R.J., Hardy J. TOMM40 association with Alzheimer disease: Tales of APOE and linkage disequilibrium. Arch. Neurol. 2012;69:1243–1244. doi: 10.1001/archneurol.2012.1935. [DOI] [PubMed] [Google Scholar]
- 14.Yashin A.I., Fang F., Kovtun M., Wu D., Duan M., Arbeev K., Akushevich I., Kulminski A., Culminskaya I., Zhbannikov I., et al. Hidden heterogeneity in Alzheimer’s disease: Insights from genetic association studies and other analyses. Exp. Gerontol. 2018;107:148–160. doi: 10.1016/j.exger.2017.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lambert J.C., Ibrahim-Verbaas C.A., Harold D., Naj A.C., Sims R., Bellenguez C., DeStafano A.L., Bis J.C., Beecham G.W., Grenier-Boley B., et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat. Genet. 2013;45:1452–1458. doi: 10.1038/ng.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Humphries A.D., Streimann I.C., Stojanovski D., Johnston A.J., Yano M., Hoogenraad N.J., Ryan M.T. Dissection of the mitochondrial import and assembly pathway for human Tom40. J. Biol. Chem. 2005;280:11535–11543. doi: 10.1074/jbc.M413816200. [DOI] [PubMed] [Google Scholar]
- 17.Lee E.G., Chen S., Leong L., Tulloch J., Yu C.E. TOMM40 RNA Transcription in Alzheimer’s Disease Brain and Its Implication in Mitochondrial Dysfunction. Genes. 2021;12:871. doi: 10.3390/genes12060871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bezuch N., Bradburn S., Robinson A.C., Pendleton N., Payton A., Murgatroyd C. Superior Frontal Gyrus TOMM40-APOE Locus DNA Methylation in Alzheimer’s Disease. J. Alzheimers Dis. Rep. 2021;5:275–282. doi: 10.3233/ADR-201000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Valant V., Keenan B.T., Anderson C.D., Shulman J.M., Devan W.J., Ayres A.M., Schwab K., Goldstein J.N., Viswanathan A., Alzheimer’s Disease Neuroimaging Initiative et al. TOMM40 in Cerebral Amyloid Angiopathy Related Intracerebral Hemorrhage: Comparative Genetic Analysis with Alzheimer’s Disease. Transl. Stroke Res. 2012;3((Suppl. 1)):102–112. doi: 10.1007/s12975-012-0161-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siddarth P., Burggren A.C., Merrill D.A., Ercoli L.M., Mahmood Z., Barrio J.R., Small G.W. Longer TOMM40 poly-T variants associated with higher FDDNP-PET medial temporal tau and amyloid binding. PLoS ONE. 2018;13:e0208358. doi: 10.1371/journal.pone.0208358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferencz B., Karlsson S., Kalpouzos G. Promising Genetic Biomarkers of Preclinical Alzheimer’s Disease: The Influence of APOE and TOMM40 on Brain Integrity. Int. J. Alzheimers Dis. 2012;2012:421452. doi: 10.1155/2012/421452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roses A.D., Lutz M.W., Amrine-Madsen H., Saunders A.M., Crenshaw D.G., Sundseth S.S., Huentelman M.J., Welsh-Bohmer K.A., Reiman E.M. A TOMM40 variable-length polymorphism predicts the age of late-onset Alzheimer’s disease. Pharm. J. 2010;10:375–384. doi: 10.1038/tpj.2009.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Linnertz C., Anderson L., Gottschalk W., Crenshaw D., Lutz M.W., Allen J., Saith S., Mihovilovic M., Burke J.R., Welsh-Bohmer K.A., et al. The cis-regulatory effect of an Alzheimer’s disease-associated poly-T locus on expression of TOMM40 and apolipoprotein E genes. Alzheimers Dement. 2014;10:541–551. doi: 10.1016/j.jalz.2013.08.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Takei N., Miyashita A., Tsukie T., Arai H., Asada T., Imagawa M., Shoji M., Higuchi S., Urakami K., Kimura H., et al. Genetic association study on in and around the APOE in late-onset Alzheimer disease in Japanese. Genomics. 2009;93:441–448. doi: 10.1016/j.ygeno.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 25.Bekris L.M., Lutz F., Yu C.E. Functional analysis of APOE locus genetic variation implicates regional enhancers in the regulation of both TOMM40 and APOE. J. Hum. Genet. 2012;57:18–25. doi: 10.1038/jhg.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leng F., Edison P. Neuroinflammation and microglial activation in Alzheimer disease: Where do we go from here? Nat. Rev. Neurol. 2021;17:157–172. doi: 10.1038/s41582-020-00435-y. [DOI] [PubMed] [Google Scholar]
- 27.Mangalmurti A., Lukens J.R. How neurons die in Alzheimer’s disease: Implications for neuroinflammation. Curr. Opin. Neurobiol. 2022;75:102575. doi: 10.1016/j.conb.2022.102575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Colonna M., Butovsky O. Microglia Function in the Central Nervous System During Health and Neurodegeneration. Annu. Rev. Immunol. 2017;35:441–468. doi: 10.1146/annurev-immunol-051116-052358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muzio L., Viotti A., Martino G. Microglia in Neuroinflammation and Neurodegeneration: From Understanding to Therapy. Front. Neurosci. 2021;15:742065. doi: 10.3389/fnins.2021.742065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haque M.E., Akther M., Jakaria M., Kim I.S., Azam S., Choi D.K. Targeting the microglial NLRP3 inflammasome and its role in Parkinson’s disease. Mov. Disord. 2020;35:20–33. doi: 10.1002/mds.27874. [DOI] [PubMed] [Google Scholar]
- 31.Lunemann J.D., Malhotra S., Shinohara M.L., Montalban X., Comabella M. Targeting Inflammasomes to Treat Neurological Diseases. Ann. Neurol. 2021;90:177–188. doi: 10.1002/ana.26158. [DOI] [PubMed] [Google Scholar]
- 32.de Araujo F.M., Cuenca-Bermejo L., Fernandez-Villalba E., Costa S.L., Silva V.D.A., Herrero M.T. Role of Microgliosis and NLRP3 Inflammasome in Parkinson’s Disease Pathogenesis and Therapy. Cell. Mol. Neurobiol. 2022;42:1283–1300. doi: 10.1007/s10571-020-01027-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brahadeeswaran S., Sivagurunathan N., Calivarathan L. Inflammasome Signaling in the Aging Brain and Age-Related Neurodegenerative Diseases. Mol. Neurobiol. 2022;59:2288–2304. doi: 10.1007/s12035-021-02683-5. [DOI] [PubMed] [Google Scholar]
- 34.Milner M.T., Maddugoda M., Gotz J., Burgener S.S., Schroder K. The NLRP3 inflammasome triggers sterile neuroinflammation and Alzheimer’s disease. Curr. Opin. Immunol. 2021;68:116–124. doi: 10.1016/j.coi.2020.10.011. [DOI] [PubMed] [Google Scholar]
- 35.Hanslik K.L., Ulland T.K. The Role of Microglia and the Nlrp3 Inflammasome in Alzheimer’s Disease. Front. Neurol. 2020;11:570711. doi: 10.3389/fneur.2020.570711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heneka M.T., Kummer M.P., Stutz A., Delekate A., Schwartz S., Vieira-Saecker A., Griep A., Axt D., Remus A., Tzeng T.C., et al. NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice. Nature. 2013;493:674–678. doi: 10.1038/nature11729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moreira P.I., Santos M.S., Oliveira C.R. Alzheimer’s disease: A lesson from mitochondrial dysfunction. Antioxid. Redox Signal. 2007;9:1621–1630. doi: 10.1089/ars.2007.1703. [DOI] [PubMed] [Google Scholar]
- 38.Perez Ortiz J.M., Swerdlow R.H. Mitochondrial dysfunction in Alzheimer’s disease: Role in pathogenesis and novel therapeutic opportunities. Br. J. Pharmacol. 2019;176:3489–3507. doi: 10.1111/bph.14585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rehling P., Pfanner N., Meisinger C. Insertion of hydrophobic membrane proteins into the inner mitochondrial membrane--a guided tour. J. Mol. Biol. 2003;326:639–657. doi: 10.1016/S0022-2836(02)01440-7. [DOI] [PubMed] [Google Scholar]
- 40.Hansson Petersen C.A., Alikhani N., Behbahani H., Wiehager B., Pavlov P.F., Alafuzoff I., Leinonen V., Ito A., Winblad B., Glaser E., et al. The amyloid beta-peptide is imported into mitochondria via the TOM import machinery and localized to mitochondrial cristae. Proc. Natl. Acad. Sci. USA. 2008;105:13145–13150. doi: 10.1073/pnas.0806192105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Devi L., Prabhu B.M., Galati D.F., Avadhani N.G., Anandatheerthavarada H.K. Accumulation of amyloid precursor protein in the mitochondrial import channels of human Alzheimer’s disease brain is associated with mitochondrial dysfunction. J. Neurosci. 2006;26:9057–9068. doi: 10.1523/JNEUROSCI.1469-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abyadeh M., Gupta V., Chitranshi N., Gupta V., Wu Y., Saks D., Wander Wall R., Fitzhenry M.J., Basavarajappa D., You Y., et al. Mitochondrial dysfunction in Alzheimer’s disease—A proteomics perspective. Expert Rev. Proteom. 2021;18:295–304. doi: 10.1080/14789450.2021.1918550. [DOI] [PubMed] [Google Scholar]
- 43.Simpson D.S.A., Oliver P.L. ROS Generation in Microglia: Understanding Oxidative Stress and Inflammation in Neurodegenerative Disease. Antioxidants. 2020;9:743. doi: 10.3390/antiox9080743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.von Bernhardi R., Eugenin-von Bernhardi L., Eugenin J. Microglial cell dysregulation in brain aging and neurodegeneration. Front. Aging Neurosci. 2015;7:124. doi: 10.3389/fnagi.2015.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhou X., Chen Y., Mok K.Y., Kwok T.C.Y., Mok V.C.T., Guo Q., Ip F.C., Chen Y., Mullapudi N., Alzheimer’s Disease Neuroimaging I., et al. Non-coding variability at the APOE locus contributes to the Alzheimer’s risk. Nat. Commun. 2019;10:3310. doi: 10.1038/s41467-019-10945-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhu Z., Yang Y., Xiao Z., Zhao Q., Wu W., Liang X., Luo J., Cao Y., Shao M., Guo Q., et al. TOMM40 and APOE variants synergistically increase the risk of Alzheimer’s disease in a Chinese population. Aging Clin. Exp. Res. 2021;33:1667–1675. doi: 10.1007/s40520-020-01661-6. [DOI] [PubMed] [Google Scholar]
- 47.Michaelson D.M. APOE epsilon4: The most prevalent yet understudied risk factor for Alzheimer’s disease. Alzheimers Dement. 2014;10:861–868. doi: 10.1016/j.jalz.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 48.Rebeck G.W. The role of APOE on lipid homeostasis and inflammation in normal brains. J. Lipid Res. 2017;58:1493–1499. doi: 10.1194/jlr.R075408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Babenko V.N., Afonnikov D.A., Ignatieva E.V., Klimov A.V., Gusev F.E., Rogaev E.I. Haplotype analysis of APOE intragenic SNPs. BMC Neurosci. 2018;19((Suppl. 1)):16. doi: 10.1186/s12868-018-0413-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jun G., Naj A.C., Beecham G.W., Wang L.S., Buros J., Gallins P.J., Buxbaum J.D., Ertekin-Taner N., Fallin M.D., Friedland R., et al. Meta-analysis confirms CR1, CLU, and PICALM as alzheimer disease risk loci and reveals interactions with APOE genotypes. Arch. Neurol. 2010;67:1473–1484. doi: 10.1001/archneurol.2010.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hu P., Qin Y.H., Jing C.X., Lu L., Hu B., Du P.F. Does the geographical gradient of ApoE4 allele exist in China? A systemic comparison among multiple Chinese populations. Mol. Biol. Rep. 2011;38:489–494. doi: 10.1007/s11033-010-0132-0. [DOI] [PubMed] [Google Scholar]
- 52.Lobo A., Launer L.J., Fratiglioni L., Andersen K., Di Carlo A., Breteler M.M., Copeland J.R., Dartigues J.F., Jagger C., Martinez-Lage J., et al. Prevalence of dementia and major subtypes in Europe: A collaborative study of population-based cohorts. Neurologic Diseases in the Elderly Research Group. Neurology. 2000;54((Suppl. 5)):S4–S9. [PubMed] [Google Scholar]
- 53.Chiba-Falek O., Gottschalk W.K., Lutz M.W. The effects of the TOMM40 poly-T alleles on Alzheimer’s disease phenotypes. Alzheimers Dement. 2018;14:692–698. doi: 10.1016/j.jalz.2018.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lyall D.M., Harris S.E., Bastin M.E., Munoz Maniega S., Murray C., Lutz M.W., Saunders A.M., Roses A.D., Valdes Hernandez Mdel C., Royle N.A., et al. Alzheimer’s disease susceptibility genes APOE and TOMM40, and brain white matter integrity in the Lothian Birth Cohort 1936. Neurobiol. Aging. 2014;35:1513.e25–1513.e33. doi: 10.1016/j.neurobiolaging.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ridge P.G., Hoyt K.B., Boehme K., Mukherjee S., Crane P.K., Haines J.L., Mayeux R., Farrer L.A., Pericak-Vance M.A., Alzheimer’s Disease Genetics Consortium et al. Assessment of the genetic variance of late-onset Alzheimer’s disease. Neurobiol. Aging. 2016;41:200.e13–200.e20. doi: 10.1016/j.neurobiolaging.2016.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cervantes S., Samaranch L., Vidal-Taboada J.M., Lamet I., Bullido M.J., Frank-Garcia A., Coria F., Lleo A., Clarimon J., Lorenzo E., et al. Genetic variation in APOE cluster region and Alzheimer’s disease risk. Neurobiol. Aging. 2011;32:2107.e7–2107.e17. doi: 10.1016/j.neurobiolaging.2011.05.023. [DOI] [PubMed] [Google Scholar]
- 57.Yu L., Lutz M.W., Wilson R.S., Burns D.K., Roses A.D., Saunders A.M., Gaiteri C., De Jager P.L., Barnes L.L., Bennett D.A. TOMM40’523 variant and cognitive decline in older persons with APOE epsilon3/3 genotype. Neurology. 2017;88:661–668. doi: 10.1212/WNL.0000000000003614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ortega-Rojas J., Arboleda-Bustos C.E., Guerrero E., Neira J., Arboleda H. Genetic Variants and Haplotypes of TOMM40, APOE, and APOC1 are Related to the Age of Onset of Late-onset Alzheimer Disease in a Colombian Population. Alzheimer Dis. Assoc. Disord. 2022;36:29–35. doi: 10.1097/WAD.0000000000000477. [DOI] [PubMed] [Google Scholar]
- 59.Bagnoli S., Piaceri I., Tedde A., Bessi V., Bracco L., Sorbi S., Nacmias B. TOMM40 polymorphisms in Italian Alzheimer’s disease and frontotemporal dementia patients. Neurol. Sci. 2013;34:995–998. doi: 10.1007/s10072-013-1425-6. [DOI] [PubMed] [Google Scholar]
- 60.Lin R., Zhang Y., Yan D., Liao X., Gong G., Hu J., Fu Y., Cai W. Association of common variants in TOMM40/APOE/APOC1 region with human longevity in a Chinese population. J. Hum. Genet. 2016;61:323–328. doi: 10.1038/jhg.2015.150. [DOI] [PubMed] [Google Scholar]
- 61.Omoumi A., Fok A., Greenwood T., Sadovnick A.D., Feldman H.H., Hsiung G.Y. Evaluation of late-onset Alzheimer disease genetic susceptibility risks in a Canadian population. Neurobiol. Aging. 2014;35:936.e5–936.e12. doi: 10.1016/j.neurobiolaging.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 62.Zeitlow K., Charlambous L., Ng I., Gagrani S., Mihovilovic M., Luo S., Rock D.L., Saunders A., Roses A.D., Gottschalk W.K. The biological foundation of the genetic association of TOMM40 with late-onset Alzheimer’s disease. Biochim. Biophys. Acta Mol. Basis Dis. 2017;1863:2973–2986. doi: 10.1016/j.bbadis.2017.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Johnson S.C., La Rue A., Hermann B.P., Xu G., Koscik R.L., Jonaitis E.M., Bendlin B.B., Hogan K.J., Roses A.D., Saunders A.M., et al. The effect of TOMM40 poly-T length on gray matter volume and cognition in middle-aged persons with APOE epsilon3/epsilon3 genotype. Alzheimers Dement. 2011;7:456–465. doi: 10.1016/j.jalz.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen S., Sarasua S.M., Davis N.J., DeLuca J.M., Boccuto L., Thielke S.M., Yu C.E. TOMM40 genetic variants associated with healthy aging and longevity: A systematic review. BMC Geriatr. 2022;22:667. doi: 10.1186/s12877-022-03337-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li T., Pappas C., Le S.T., Wang Q., Klinedinst B.S., Larsen B.A., Pollpeter A., Lee L.Y., Lutz M.W., Gottschalk W.K., et al. APOE, TOMM40, and sex interactions on neural network connectivity. Neurobiol. Aging. 2022;109:158–165. doi: 10.1016/j.neurobiolaging.2021.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li Y., Xia X., Wang Y., Zheng J.C. Mitochondrial dysfunction in microglia: A novel perspective for pathogenesis of Alzheimer’s disease. J. Neuroinflamm. 2022;19:248. doi: 10.1186/s12974-022-02613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lin M.M., Liu N., Qin Z.H., Wang Y. Mitochondrial-derived damage-associated molecular patterns amplify neuroinflammation in neurodegenerative diseases. Acta Pharmacol. Sin. 2022;43:2439–2447. doi: 10.1038/s41401-022-00879-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lee S., Cho H.J., Ryu J.H. Innate Immunity and Cell Death in Alzheimer’s Disease. ASN Neuro. 2021;13:17590914211051908. doi: 10.1177/17590914211051908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang W.Y., Tan M.S., Yu J.T., Tan L. Role of pro-inflammatory cytokines released from microglia in Alzheimer’s disease. Ann. Transl. Med. 2015;3:136. doi: 10.3978/j.issn.2305-5839.2015.03.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Agrawal I., Jha S. Mitochondrial Dysfunction and Alzheimer’s Disease: Role of Microglia. Front. Aging Neurosci. 2020;12:252. doi: 10.3389/fnagi.2020.00252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kaur D., Sharma V., Deshmukh R. Activation of microglia and astrocytes: A roadway to neuroinflammation and Alzheimer’s disease. Inflammopharmacology. 2019;27:663–677. doi: 10.1007/s10787-019-00580-x. [DOI] [PubMed] [Google Scholar]
- 72.Cheignon C., Tomas M., Bonnefont-Rousselot D., Faller P., Hureau C., Collin F. Oxidative stress and the amyloid beta peptide in Alzheimer’s disease. Redox Biol. 2018;14:450–464. doi: 10.1016/j.redox.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pinho C.M., Teixeira P.F., Glaser E. Mitochondrial import and degradation of amyloid-beta peptide. Biochim. Biophys. Acta. 2014;1837:1069–1074. doi: 10.1016/j.bbabio.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 74.McKhann G.M., Knopman D.S., Chertkow H., Hyman B.T., Jack C.R., Jr., Kawas C.H., Klunk W.E., Koroshetz W.J., Manly J.J., Mayeux R., et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Roman G.C., Tatemichi T.K., Erkinjuntti T., Cummings J.L., Masdeu J.C., Garcia J.H., Amaducci L., Orgogozo J.M., Brun A., Hofman A., et al. Vascular dementia: Diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43:250–260. doi: 10.1212/WNL.43.2.250. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article.