Significance
While it is well established that social attributes predict mortality, mortality prediction models used in clinical, population health, and research settings rely almost exclusively on demographics and medical comorbidities. In this study of 8,250 older adults from the Health and Retirement Study, we develop and validate a parsimonious index of Social Frailty, which uses age, gender, and eight social characteristics to predict 4-y mortality risk. We demonstrate that this prognostic index accurately risk-stratifies older adults and improves the prediction of commonly used comorbidity- and function-based risk models.
Keywords: mortality, risk prediction, social determinants, frailty, aging
Abstract
While social characteristics are well-known predictors of mortality, prediction models rely almost exclusively on demographics, medical comorbidities, and function. Lacking an efficient way to summarize the prognostic impact of social factor, many studies exclude social factors altogether. Our objective was to develop and validate a summary measure of social risk and determine its ability to risk-stratify beyond traditional risk models. We examined participants in the Health and Retirement Study, a longitudinal, survey of US older adults. We developed the model from a comprehensive inventory of 183 social characteristics using least absolute shrinkage and selection operator, a penalized regression approach. Then, we assessed the predictive capacity of the model and its ability to improve on traditional prediction models. We studied 8,250 adults aged ≥65 y. Within 4 y of the baseline interview, 22% had died. Drawn from 183 possible predictors, the Social Frailty Index included age, gender, and eight social predictors: neighborhood cleanliness, perceived control over financial situation, meeting with children less than yearly, not working for pay, active with children, volunteering, feeling isolated, and being treated with less courtesy or respect. In the validation cohort, predicted and observed mortality were strongly correlated. Additionally, the Social Frailty Index meaningfully risk-stratified participants beyond the Charlson score (medical comorbidity index) and the Lee Index (comorbidity and function model). The Social Frailty Index includes age, gender, and eight social characteristics and accurately risk-stratifies older adults. The model improves upon commonly used risk prediction tools and has application in clinical, population health, and research settings.
Risk prediction and prognostication are core to clinical medicine, medical research, and healthcare policy. For example, life expectancy informs benefits and harms of cancer screening, baseline risk measurement is central to observational research, and risk adjustment is crucial in quality measures (1–3). Traditional approaches to risk prediction rely heavily on measuring the prognostic impact of medical comorbidities (3–5). These efforts have yielded widely used summary measures of medical risk.
However, a rich literature also demonstrates that a wide range of social factors meaningfully predicts health outcomes (6–8). For example, social support predicts reduced rates of nursing home stays (9), loneliness portends higher rates of functional decline and death (10), and social network strength is associated with lower rates of cognitive decline (11).
Although social attributes are predictive of key aging outcomes, we lack an efficient way to summarize the prognostic impact of social factors. Practicality is a key impediment—for use in a clinical, research, or policy setting, a social risk model is more likely to be implemented if it is easy to use. The few existing social risk models that have been developed are expansive inventories (12–15). These models are comprehensive and predictive, albeit unwieldy to implement. Some have sought to address usability by relying exclusively on area-level data. Such efforts produced the Center for Disease Control’s Social Vulnerability Index (16), the Area Deprivation Index (17), and the English Indicies of Deprivation (18), which are useful for area-level interventions and planning. However, such measures cannot assess an individual’s risk because inferences from group-level analyses cannot be reliably applied to individuals within those groups, a principle known as ecological fallacy (19). Codifying which social elements to include is challenging; as a result, many studies exclude social risk factors altogether and, in doing so, run the risk of biased measurement (20, 21).
The primary aim of this study was to create the Social Frailty Index, a parsimonious person-level social risk prediction model derived from a comprehensive inventory of social characteristics that predicts mortality in older adults. Our goal was to identify a small subset of risk factors that reflects social risk, not to identify causal factors or all possible social risk factors. Our second aim was to determine if the Social Frailty Index improves risk stratification beyond existing risk models.
Methods
Study Participants.
We developed a longitudinal cohort of older adults from the Health and Retirement Study (HRS) to develop the Social Frailty Index. The HRS is a longitudinal, nationally representative survey of more than 43,000 Americans aged 50 y and older (22–24). The goal of the HRS is to measure changes in health, wealth, social structure, and function as participants age. Participants are interviewed every 2 y by phone, in person or via Internet surveys. We included participants who were 65 y and older who completed the Psychosocial and Lifestyle Questionnaire in 2010 or 2012. The 2010 cohort was used to develop the model, and the 2012 cohort was used to validate the model. Because the questionnaire is administered to a random half of the total HRS cohort every 2 y, there is no overlap between 2010 and 2012 respondents.
Social Predictors.
We identified predictors using the Social Frailty in Older Adults framework, a framework articulated by sociologists and gerontologists based on Social Production Function theory—it conceptualizes Social Frailty as “a lack of resources to fulfill one’s basic social needs.” (25) The framework identifies four social domains relevant to aging—General Resources, Social Resources, Social Activities, and Fulfillment of Basic Social Needs. Using the HRS core interview and the Psychosocial and Lifestyle Questionnaire, we identified 472 potential social predictors. Two investigators (SJS, SO) independently reviewed each predictor to determine if it fits within the Social Frailty in Older Adults framework. Any differences were reconciled through consensus discussion. This process yielded 183 candidate predictors (SI Appendix, Appendix 1).
Outcome.
Our primary outcome was all-cause mortality 4 y after the interview, mirroring the time horizon used in prior mortality prediction studies (4). Mortality was determined using a combination of the National Death Index and HRS surviving family member exit interviews; none were lost to follow up, and no observations were censored. We identified three secondary outcomes, all assessed over 4 y—loss of activity of daily living (ADL) independence, prolonged nursing home stay, and hospitalization. Loss of ADL independence was defined as being fully ADL independent at baseline interview and requiring help with one or more ADLs at 4 y. Nursing home use was defined as spending 90 nights or more in a nursing home within 4 y of the interview. Hospitalization was defined as self-reported hospital admission lasting two nights or more.
Development and Validation of the Primary Model.
We used the 2010 cohort to derive the prediction model. We determined the functional form of continuous predictors by assessing linear, log transformation, and exponential transformation against the primary outcome, mortality at 4 y, using a logistic regression model. We selected the functional form with the lowest Bayesian information criterion (BIC). We determined the functional form of ordinal predictors by assessing linear, categorical, and manual categorization against the primary outcome selecting the functional form with the lowest BIC. Missing predictors were imputed using single imputation. Categorical variables were imputed with the mode value, and continuous variables were imputed with the median value. Median missingness was 2.6% interquartile range (IQR 2.0, 3.5), and maximum missingness was 12% for a question asking participants to rank their perceived position on a societal ladder (SI Appendix, Appendix 2).
We used a two-step procedure to derive the prediction model (26). First, from the set of 183 predictors, we used least absolute shrinkage and selection operator (LASSO) regression to identify a small subset of predictors. We identified a lambda parameter that produced the lowest mean-squared error using tenfold cross-validation. We then chose the largest value of lambda with a mean square error within one SE of the minimum (“one SE” rule) to prioritize parsimony (27). Then, we used the selected predictors to fit a logistic regression model that estimated the 4-y risk of death. In this step, we removed several additional predictors to improve parsimony and face validity and reduce collinearity. Removing these predictors improved the model BIC and only marginally affected the area under the receiver operating characteristic curve (AUC) (0.74 to 0.73). This final model was then validated in the 2012 cohort. In the validation cohort, we determined discrimination and calibration. We also determine the model’s discriminatory capacity for secondary outcomes. In the 2012 cohort, we determined if the Social Frailty Index could further stratify participants' mortality risk beyond the Lee Index and beyond the Charlson score in the subset with Medicare claims linkage (3, 4).
We report all results with 95% CIs or two-sided P value. The a priori significance threshold was P < 0.05. We performed analyses using SAS 9.4 (Cary, NC) and R 4.0.3 (Vienna, Austria). The transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD) checklist can be found in SI Appendix, Appendix 3 (28).
Results
Baseline Characteristics.
4,302 participants were included in the 2010 development cohort (SI Appendix, Appendix 4). The development cohort’s median age was 75 y, and 57% were women (Table 1). Regarding health and function, 27% reported fair or poor health, 56% reported ever using tobacco, and 26% had a screening test consistent with cognitive impairment or dementia. Within 4 y of the baseline interview, 22% of study participants in both the development cohort (960/4,302) and validation cohort (882/3,948) had died.
Table 1.
Cohort characteristics, demographics, health status, and function
| 2010 Development cohort (n = 4,302) | 2012 Validation cohort (n = 3,948) | |
|---|---|---|
| Demographics | ||
| Age, years, (median [IQR]) | 75 [70, 80] | 75 [71, 80] |
| Women (%) | 2,444 (57) | 2,308 (58) |
| Health Status | ||
| Fair or poor self-reported health (%) | 1,169 (27) | 1,116 (28) |
| Significant pain (%) | 240 (6) | 211 (5) |
| Diabetes (%) | 1,033 (24) | 1,020 (26) |
| Cancer (excluding minor skin cancer) (%) | 907 (21) | 850 (22) |
| Heart disease (%) | 1,350 (31) | 1,323 (34) |
| Stroke (%) | 465 (11) | 478 (12) |
| Arthritis (%) | 2,973 (69) | 2,797 (71) |
| Depression (%) | 489 (12) | 474 (12) |
| Ever tobacco use (%) | 2,398 (56) | 2,219 (57) |
| Function | ||
| Help with any ADL (%) | 377 (9) | 375 (10) |
| Cognition (%) | ||
| Dementia | 266 (6) | 270 (7) |
| Impairment, not dementia | 870 (20) | 813 (21) |
| Intact | 3,166 (74) | 2,865 (73) |
| Visual impairment (%) | 952 (22) | 917 (23) |
| Hearing impairment (%) | 1,113 (26) | 1,039 (26) |
ADL—activities of daily living; IQR—interquartile range.
In the domain of General Resources and Life History, 19% had less than a high school education, and 27% were military veterans (Table 2). Regarding Social Resources, 62% were married or partnered, 92% had living children, and 64% reported they “often have someone they can talk to.” In Social Activities, 6% reported meeting with their children less than yearly, and 65% reported writing or emailing friends monthly or more frequently. Concerning Fulfillment of Basic Social Needs, 5% reported often feeling isolated from others, 76% reported rarely being treated with less courtesy or respect than other people (never or less than once a year), and 12% reported not having a major activity such as a job, looking after the home, or volunteer work.
Table 2.
Cohort social characteristics
| 2010 Development cohort (n = 4,302) | 2012 Validation cohort (n = 3,948) | |
|---|---|---|
| General Resources and Life History | ||
| Race (%) | ||
| Black | 500 (12) | 485 (12) |
| White | 3,665 (85) | 3,315 (84) |
| Hispanic ethnicity (%) | 278 (6) | 321 (8) |
| Local area is full of rubbish and litter* | 733 (18) | 755 (20) |
| Low self-reported control over financial situation† (%) | 441 (10) | 402 (11) |
| Military veteran (%) | 1,152 (27) | 968 (25) |
| Satisfaction with daily life and leisure activities (1 to 5 scale) (median [IQR])‡ | 2 [1, 3] | 2 [1, 3] |
| Not at all satisfied with retirement (%) | 192 (5) | 181 (5) |
| Education (%) | ||
| Less than high school | 834 (19) | 829 (21) |
| High school | 1,685 (39) | 1,459 (37) |
| Some college | 897 (21) | 860 (22) |
| College and above | 885 (21) | 800 (20) |
| Social Resources | ||
| Married or Partnered (%) | ||
| Married or partnered | 2,666 (62) | 2,353 (60) |
| Never married | 107 (2) | 103 (3) |
| Separated or divorced | 374 (9) | 398 (10) |
| Widowed | 1,155 (27) | 1,094 (28) |
| Living children (%) | 3,799 (92) | 3,367 (92) |
| Has friends (%) | 3,877 (93) | 3,481 (91) |
| Number of living siblings (median [IQR]) | 2 [1, 3] | 2 [1, 4] |
| Often has someone they can talk to (%) | 2,690 (64) | 2,453 (63) |
| Social Activities | ||
| Presently working for pay (%) | 738 (18) | 630 (16) |
| Activities with grandchildren, niece/nephews, or neighborhood children (median [IQR])§ | 5 [4, 7] | 5 [4, 7] |
| Does no volunteering or charity work (%) | 2,205 (53) | 2,163 (56) |
| Goes to a sport, social, or other club (median [IQR])¶ | 6 [5, 7] | 6 [5, 7] |
| Meets with children less than once a year (%) | 246 (6) | 276 (7) |
| Writes or emails friends monthly or more frequently (%) | 2,581 (65) | 2,348 (64) |
| Fulfillment of Basic Social Needs | ||
| Feel isolated from others (%) | ||
| Often | 211 (5) | 194 (5) |
| Some of the time | 1,013 (24) | 1,018 (26) |
| Hardly ever or never | 2,948 (69) | 2,600 (66) |
| Often feel in tune with the people around you (%) | 1,990 (48) | 1,814 (47) |
| Feel part of a group of friends | ||
| Often | 2,023 (48) | 1,817 (47) |
| Some of the time | 1,593 (38) | 1,430 (37) |
| Hardly ever or never | 572 (14) | 602 (16) |
| You are treated with less courtesy or respect than other people (never or less than once a year) (%) | 3,209 (76) | 2,923 (76) |
| People act as if they think you are not smart (never or less than once a year) (%) | 3,336 (79) | 3,068 (80) |
*Defined as (≥4 on 1 to 7 scale where 1 = area is kept very clean, 7 = area is always full of rubbish and litter).
†Defined as (≤3 on 0 to 10 scale where 1 = no control at all, 10 = very much control).
‡On a 1 to 5 scale (1 = completely satisfied, 5 = not at all).
§On a 1 to 7 scale (1 = daily, 7 = never/not relevant).
¶Sport, social, or other clubs on a 1 to 7 scale (1 = daily, 7 = never/not relevant).
Categorization in the table is reflective of the functional form most predictive of the primary outcome in the development cohort.
Model Development Results.
The model development procedure yielded a model of ten predictors from all four domains in the Social Frailty in Older Adults Framework (Table 3). The ten predictors include age and gender, two measures of General Resources and Life Events (neighborhood cleanliness; perceived control over their financial situation), one measure of Social Resource and Social Activities (has children and meets with them less than yearly), three measures of Social Activities (working for pay; less active with grandchildren, neighborhood children, nieces/nephews; no volunteering or charity work), and two measures reflecting Fulfillment of Basic Social Needs (feeling isolated from others; being treated with less courtesy or respect).
Table 3.
Individual predictors in the Social Frailty Index
| Domain | Predictor | Odds Ratio (95% CI) |
|---|---|---|
| Demographics | Age, per 1-y increase | 1.12 (1.11 to 1.13) |
| Demographics | Gender, male | 1.74 (1.58 to 1.90) |
| General Resources and Life History | Local area is full of rubbish and litter* | 1.42 (1.22 to 1.62) |
| General Resources and Life History | Low self-reported control over financial situation† | 1.55 (1.31 to 1.79) |
| Social Resource/Social Activities | Has children and meets with children less than once a year | 1.64 (1.34 to 1.95) |
| Social Activities | Activities with grandchildren, niece/nephews or neighborhood children‡ | 1.11 (1.06 to 1.16) |
| Social Activities | Not working for pay at the present time | 1.74 (1.46 to 2.01) |
| Social Activities | Does no volunteering or charity work | 1.62 (1.45 to 1.79) |
| Fulfillment of Basic Social Needs | Feeling isolated from others | |
| Some of the time vs. hardly ever or never | 1.29 (1.15 to 1.43) | |
| Often vs. hardly ever or never | 1.67 (1.53 to 1.80) | |
| Fulfillment of Basic Social Needs | You are treated with less courtesy or respect than other people (a few times a year or more often) | 1.34 (1.15 to 1.53) |
*Defined as (≥4 on 1 to 7 scale where 1 = area is kept very clean, 7 = area is always full of rubbish and litter).
†Defined as (≤3 on 0 to 10 scale where 1 = no control at all, 10 = very much control).
‡Grandchildren, neighborhood children, nieces/nephews, on a 1 to 7 scale (1 = daily, 7 = never/not relevant), continuous model intercept −9.2 on the logit scale.
Beyond age and gender, which are commonly used in prediction models, in the final model, the most prominent predictors of death include not working for pay (OR 1.74, 95% CI 1.46 to 2.01), meeting with children less than once a year (OR 1.64, 95% CI 1.34 to 1.95), and often feeling isolated from others (OR 1.67, 95% CI 1.53 to 1.80).
Race, a candidate predictor, was not selected by the modeling procedure for the final model. Structural determinants like race demand special attention, given the profound and pervasive impact of racism on health. We conducted a sensitivity analysis and found that adding race and interactions between risk factors and race did not improve the model (SI Appendix, Appendix 5).
Validation Measures.
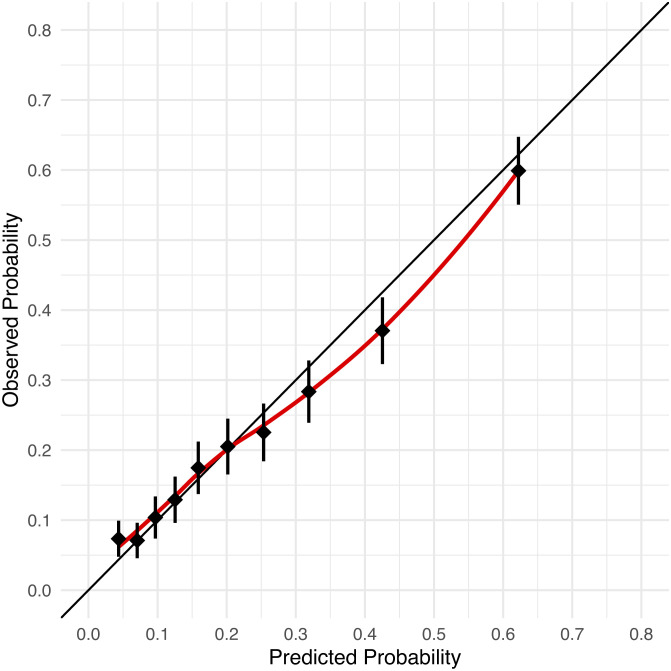
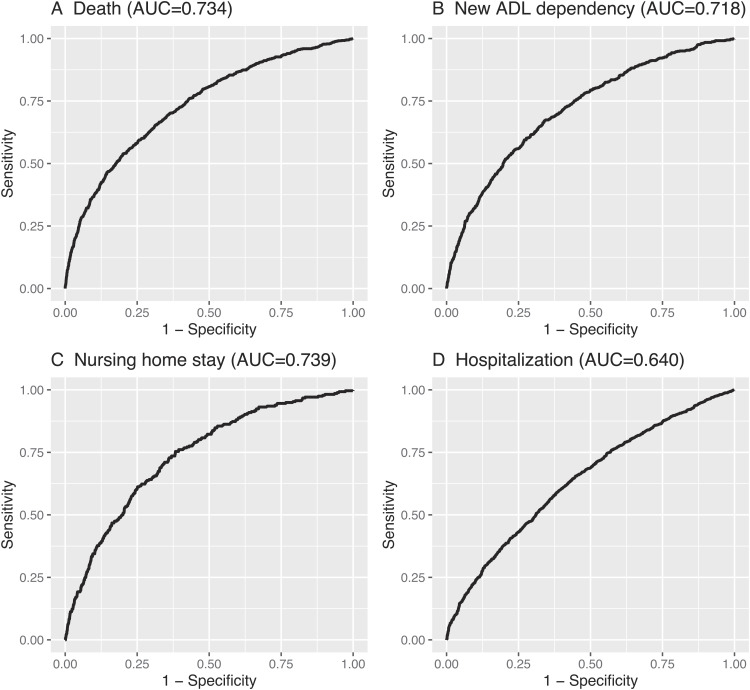
The Social Frailty Index performed well in the 2012 validation cohort. The model was well calibrated (Fig. 1), observed and expected mortality rates in the validation data were highly correlated. In the lowest decile, the observed 4-y mortality was 7.3% (predicted 4.4%), and in the highest decile, was 59.9% (predicted 62.2%). The model discriminated well with an AUC of 0.76 (95% CI 0.75 to 0.78) to predict death in the development cohort and 0.73 (95% CI 0.72 to 0.75) in the validation cohort (Fig. 2). In the validation cohort, 28% developed a new ADL dependency (1,016/3,652), 9.6% had a long-term nursing home stay (341/3,543), and 51% had a hospitalization (1,746/3,406). The Social Frailty model also performed well when used to predict new ADL dependence (AUC 0.72, 95% CI 0.70 to 0.74) and nursing home stays (AUC 0.74, 95% CI 0.71 to 0.77). The model performed modestly when used to predict hospitalization (AUC 0.64, 95% CI 0.62 to 0.66).
Fig. 1.
Calibration of Social Frailty Index in validation cohort. Plot of observed by predicted probability of 4-y mortality in the validation cohort, by decile of predicted risk.
Fig. 2.
Receiver operator curve for the Social Frailty Index to predict (A) Death, (B) New ADL dependence (C) Nursing home stay, and (D) Hospitalization in the 2012 validation cohort. Plots demonstrate the discriminatory capacity of the Social Frailty Index when it is used to predict four different aging-orientated outcomes in the validation cohort. Discrimination is measured by the c-statistic also known as the area under the receiver operator characteristic curve (AUC). An AUC of 0.5 is model no better than chance, and 1.0 indicates a model with perfect discrimination.
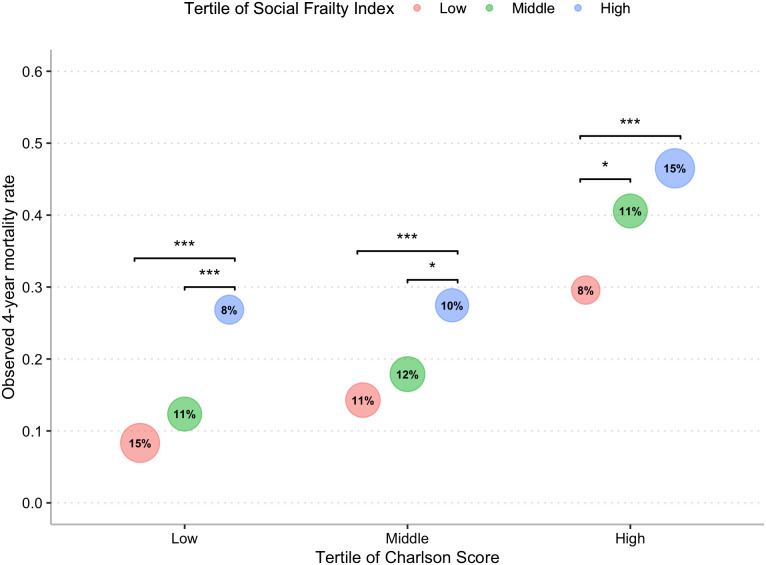
Risk Stratification beyond Charlson Score.
The Social Frailty Index meaningfully risk-stratified participants beyond the Charlson score, a commonly used medical comorbidity index. The Social Frailty Index and the Charlson score were weakly correlated (Pearson’s correlation of 0.17, CI 0.12 to 0.21, P < 0.001) in a subset of the validation cohort who have 12 mo of Medicare claims data before their baseline interview (2,226 of 3,948). Fig. 3 illustrates that the Social Frailty Index risk-stratifies beyond the Charlson score in all three tertiles of the Charlson score. For example, in the validation cohort's highest tertile of Charlson score, the observed mortality rate with a high Social Frailty Index score was 47% vs. 30% in the low Social Frailty tertile (P < 0.001).
Fig. 3.
Observed mortality in 2012 validation cohort by Social Frailty and Charlson score. The bubble chart compares observed mortality in the validation cohort by tertile of Social Frailty within tertiles of Charlson score, a comorbidity risk model. The Charlson score cohort was calculated in a subset of the study cohort where 12 mo of Medicare data were available to calculate a Charlson score (2,226 of 3,948). Since the Charlson score does not include age, when comparing it with the Social Frailty Index, we remove age from the Social Frailty Index to provide a fair comparison. The area of each bubble is proportional to the total validation cohort that falls the specific group (e.g., 15% of the cohort has a low Charlson score and low Social Frailty Index score). Significantly different values are highlighted by a bracket. ***P < 0.001, **P < 0.01, *P < 0.05. Results presented in tabular form in SI Appendix, Appendix 7.
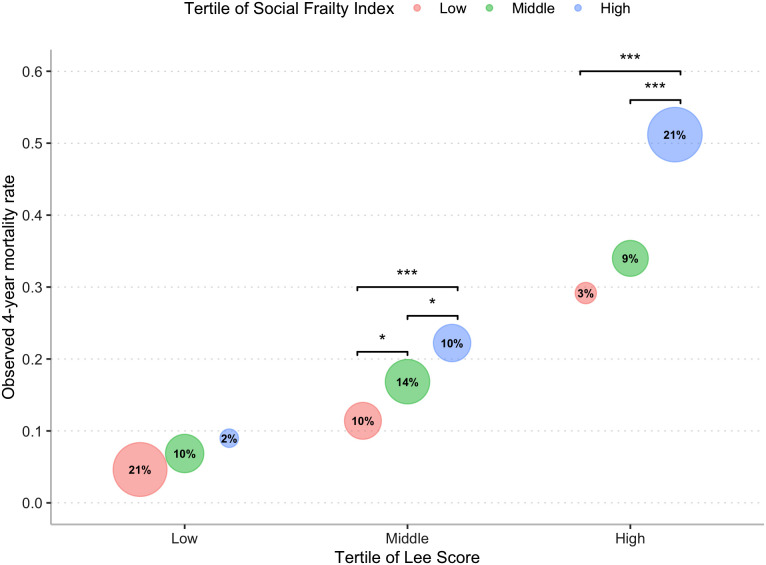
Risk Stratification beyond Lee Index.
The Social Frailty Index stratified participants’ risk beyond the Lee Index, a commonly used model that uses comorbidities and function to predict mortality. The Social Frailty Index and the Lee Index were modestly correlated (Pearson’s correlation of 0.63, CI 0.61 to 0.65, P < 0.001). Fig. 4 illustrates that the Social Frailty Index risk-stratifies beyond the Lee Index, specifically those with Middle or High Lee Index scores. For example, in the highest tertile of Lee score in the validation cohort, the observed mortality rate with a high Social Frailty Index score was 51% vs. 29% in the low Social Frailty tertile (P < 0.001).
Fig. 4.
Observed mortality in 2012 validation cohort by Social Frailty and Lee Index. The bubble chart compares observed mortality in the validation cohort by tertile of Social Frailty within tertiles of the Lee Index score, a comorbidity and function risk model. The area of each bubble is proportional to the total validation cohort that falls the specific group (e.g., 21% of the cohort has a low Lee Index score and low Social Frailty Index score). Significantly different values are highlighted by a bracket. ***P < 0.001, **P < 0.01, *P < 0.05. Results presented in tabular form in SI Appendix, Appendix 7.
The Social Frailty Index slightly improved the discrimination of both the Charlson score and the Lee Index (SI Appendix, Appendix 6).
Discussion
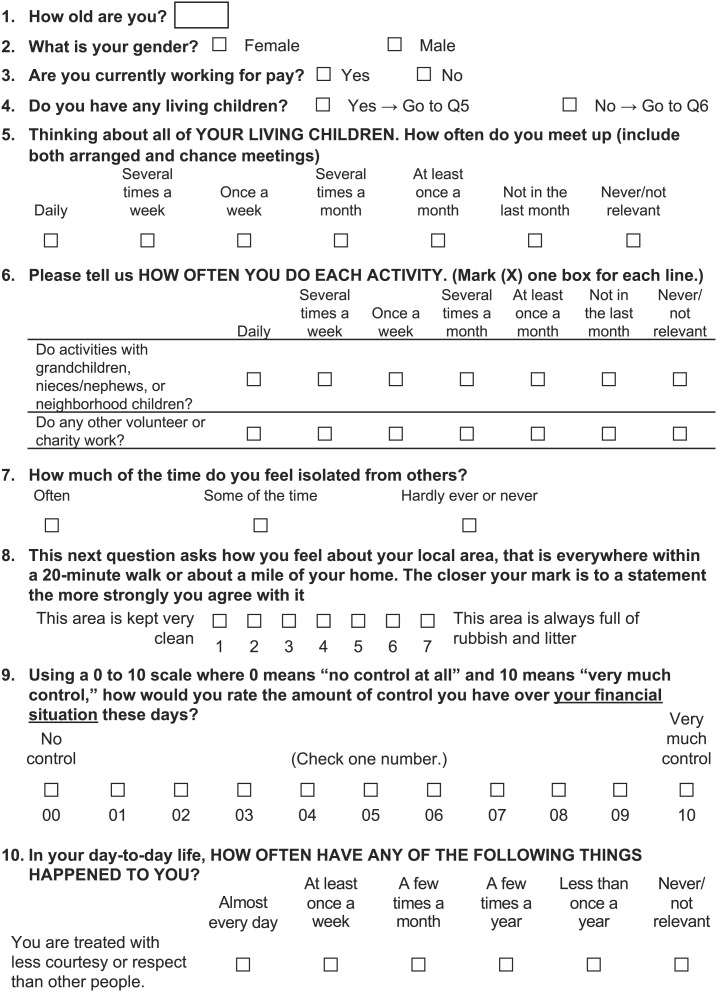
Using a comprehensive social well-being survey of older adults, we developed and validated the Social Frailty Index, which predicts the risk of death over 4 y (Fig. 5). We demonstrate that a small subset of social predictors can meaningfully stratify mortality risk in a nationally representative cohort of older adults. Further, the Social Frailty Index improves risk stratification beyond the Charlson score, a commonly used medical comorbidity model, and the Lee Index, a commonly used mortality prediction model. Where mortality prediction is important for older adults, this study demonstrates social risk factors represent an important and often unaccounted for risk domain.
Fig. 5.
Social Frailty Index instrument. This figure illustrates an instrument that can be used in clinical or research settings to calculate the Social Frailty Index. The instrument inputs can be used with the model detailed in Table 3 to calculate an individuals estimated 4-y mortality risk. An online version is available at https://sachinjshah.shinyapps.io/Social_Frailty_Index/.
This study builds on prior work incorporating social risk factors into prediction models in at least two noteworthy ways. First, we build on a wealth of studies establishing that social factors predict mortality by distilling the many hundreds of known social risk factors into an efficient summary index of social risk. The resulting Social Frailty Index is a parsimonious model drawn from a comprehensive survey that can reasonably be exported. Second, we show that a comorbidity score alone is insufficient for risk stratification. We found social risk and medical comorbidities risk are not well correlated. Thus, when added to the Charlson model or Lee Index, the Social Frailty Index meaningfully recasts the predicted risk for a substantial number of individuals. Where risk stratification is important, these results support supplementation of traditional prediction models with the Social Frailty Index. There are several applications of the Social Frailty Index in clinical care and medical research.
Clinicians can use the Social Frailty Index to inform clinical care of older adults, but the approach must be thoughtful to avoid worsening disparities. Clinicians can use the web version of this Index to supplement commonly used prediction tools to help older adults engage in advanced care planning and weigh medical interventions. Because of the time-lagged benefit of many medical interventions, mortality prediction models are used to identify those with shorter life expectancies who may experience more harm and less benefit from such interventions (1). Clinicians should be aware that our social lives predict longevity. However, they should avoid using the Social Frailty Index to limit the care of higher-than-average-risk older adults under the pretense that such individuals are at-risk for poor outcomes. For example, using the Socially Frailty Index to recommend against a surgical intervention because a patient is deemed to be “socially frail” would plainly worsen structural barriers. Instead, this tool should be used to identify at-risk individuals and intensively develop solutions to improve their access to high-quality care. For example, an at-risk individual could be referred to a social worker pre-operatively to identify barriers to successful recovery and find solutions ahead of the planned surgery (e.g., meal delivery, around-the-clock in-home caregiving for a period).
Collection in prospective observational studies is also a natural use case for the index, since prognostics prognostic adjustment is central to observational research. The study of any risk factor hinges on accounting for the baseline risk differential in those with and without the prognostic factor in question. Current approaches rely heavily on medical comorbidities for prognostic adjustment. Adding the Social Frailty Index would help account for an acknowledged, but challenging to measure risk domain. In interventional studies, investigators may seek to understand if the effect of intervention differs by Social Frailty. In both instances, the index would have to be administered to participants during their baseline interview.
Additionally, the Social Frailty Index can address policymakers, actuaries, and healthcare delivery organizations’ need for accurate risk adjustment. For policymakers, quality measurement in health care turns on accurate baseline risk measurement. In a 2017 report, the National Academy of Medicine detailed the importance of including social risk factors in comorbidities-based risk models (29). However, social factors have yet to be included in quality measures, partly because it is not clear which measures to use. Failing to account for social dimensions in risk adjustment can further structural inequities. For example, Medicare’s Hospital Readmission Reduction Program penalizes hospitals for excess readmissions as determined by a medical comorbidity risk adjustment model. A long-standing critique of this program has been that because the risk adjustment model does not account for social factors, it effectively penalizes hospitals that serve socially marginalized communities (30, 31). Additional work is needed to use the index developed here at the scale needed for national risk adjustment measurement. One path forward is to map the index to existing International Classification of Disease (ICD) social determinants of health codes (“Z codes”) to validate a claims-based version of the Social Frailty Index. Separately, actuaries may find such an index useful in augmenting population-level mortality and long-term nursing home projections by collecting the Social Frailty Index from their clients. However, allowing social risk factors to affect individual premium pricing would magnify disparities. Finally, Accountable Care Organizations (ACOs) commonly use claims and electronic health record data to identify patients for interventions like intensive care management. However, these methods do not adequately capture patients’ social dimensions, resulting in socially advantaged persons being preferentially selected into such programs (32, 33). Many ACOs already collect social determinants data and could add the Social Frailty Index to allocate care management programs more accurately.
The study design and data have limitations that are important to consider when interpreting the results. First, the risk factors in the Social Frailty Index are not necessarily causal; that is, it should not be taken to mean that addressing the risk factors identified in the model will reduce mortality risk. To inform causality, one could use this index to enroll persons at high-social risk in randomized trials that test interventions designed to ameliorate social risk. Additionally, the goal of this endeavor was to identify a small subset of social factors that best capture social risk. Thus, the absence of a putative factor in the index does not imply it was not predictive, rather that it was possible to capture the prognostic value of that risk factor across the study population through the risk factors already included in the model. Finally, in this study, the development and validation cohorts were separated by 2 y, a structure that lends credibility to the generalizability of the Social Frailty Index (34). Future validation outside of the HRS will prove helpful in characterizing the robustness of the Social Frailty Index. Avenues for validation include adding the Social Frailty Index to existing, longitudinal prospective cohorts (e.g., National Social Life, Health and Aging Project) and recruiting community participants for a stand-alone prospective validation study. Claims-based validation using ICD “Z codes” may be possible in the future; however, at present, social determinants of health Z codes are rarely documented because there is no national financial incentive to document such codes in the USA. Importantly, validation studies should focus on populations typically underrepresented in survey studies, like seniors living in poverty and racial and ethnic minorities.
In summary, the Social Frailty Index is a short survey that uses social risk factors to estimate the 4-y mortality risk in adults 65 y and older. The ten-item index obtained by patient report can be used to assess mortality risk and the risk of disability and prolonged nursing home stays. The model improves upon existing risk prediction tools and has applications in clinical, population health, and research settings.
Ethical Review.
The University of California, San Francisco, Committee on Human Research, approved analysis for this study and waived the requirement for patient consent (Institutional Review Board No. 16‐19185).
Supplementary Material
Appendix 01 (PDF)
Acknowledgments
We would like to thank Dr. Leah Karliner and Dr. Michael Steinman for their participation in the advisory panel for this study. Funding: This study was funded by the National Institute on Aging (R03AG060090, P30AG044281) and the National Heart, Lung, and Blood Institute (K24HL141354). Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author contributions
Author contributions: S.J.S., M.C.F., and K.E.C. designed research; S.J.S., S.O., and S.Y.J. performed research; S.J.S., S.Y.J., and W.J.B. analyzed data; S.J.S., M.C.F., and K.E.C obtained funding for the work; and S.J.S., S.O., S.Y.J., W.J.B., M.C.F., and K.E.C. wrote the paper.
Competing interests
The authors have organizational affiliations to disclose: S.O. also reported personal fees from EpiExcellence LLC outside the submitted work. The authors have research support to disclose: S.J.S, S.O., S.Y.J., W.J.B., and K.E.C. reported funding from the National Institute on Aging/NIH. M.C.F. reported grants from the National Heart, Lung, and Blood Institute/NIH during the conduct of the study and grants from Patient-Centered Outcomes Research Institute outside the submitted work.
Footnotes
This article is a PNAS Direct Submission.
Data, Materials, and Software Availability
Researchers can apply to the Health and Retirement Study (https://hrs.isr.umich.edu/) to access the data used in this study (24). Final code will be made available at github.com/sachinjshah.
Supporting Information
References
- 1.Lee S. J., et al. , Time lag to benefit after screening for breast and colorectal cancer: Meta-analysis of survival data from the United States, Sweden, United Kingdom, and Denmark. BMJ 346, e8441 10.1136/bmj.e8441 (2013), 10.1136/bmj.e8441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernheim S. M., et al. , National patterns of risk-standardized mortality and readmission for acute myocardial infarction and heart failure. Circ. Cardiovasc. Qual. Outcomes 3, 459–467 (2010), 10.1161/CIRCOUTCOMES.110.957613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Charlson M. E., Pompei P., Ales K. L., MacKenzie C. R., A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 40, 373–383 10.1016/0021-9681(87)90171-8(1987), 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 4.Lee S. J., Lindquist K., Segal M. R., Covinsky K. E., Development and validation of a prognostic index for 4-year mortality in older adults. JAMA 295, 801–808 (2006), 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- 5.Schonberg M. A., Davis R. B., McCarthy E. P., Marcantonio E. R., Index to predict 5-year mortality of community-dwelling adults aged 65 and older using data from the national health interview survey. J. Gen. Intern. Med. 24, 1115–1122 (2009), 10.1007/s11606-009-1073-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGinnis J. M., Williams-Russo P., Knickman J. R., The case for more active policy attention to health promotion. Health Affairs 21, 78–93 10.1377/hlthaff.21.2.78(2002), 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- 7.Holt-Lunstad J., Smith T. B., Layton J. B., Social relationships and mortality risk: A meta-analytic review. PLoS Med. 7, e1000316 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Puterman E., et al. , Predicting mortality from 57 economic, behavioral, social, and psychological factors. Proc. Natl. Acad. Sci. U.S.A. 117, 16273–16282 (2020), 10.1073/pnas.1918455117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah S. J., Fang M. C., Wannier S. R., Steinman M. A., Covinsky K. E., Association of social support with functional outcomes in older adults who live alone. JAMA Intern. Med. Published online November 15 (2021), 10.1001/jamainternmed.2021.6588. [DOI] [PMC free article] [PubMed]
- 10.Perissinotto C. M., Cenzer I. S., Covinsky K. E., Loneliness in older persons: A predictor of functional decline and death. Arch Intern. Med. 172, 1078–1084 (2012), 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fratiglioni L., Wang H. X., Ericsson K., Maytan M., Winblad B., Influence of social network on occurrence of dementia: A community-based longitudinal study. Lancet 355, 1315–1319 10.1016/S0140-6736(00)02113-9(2000), 10.1016/S0140-6736(00)02113-9. [DOI] [PubMed] [Google Scholar]
- 12.Andrew M. K., Mitnitski A. B., Rockwood K., Social vulnerability, frailty and mortality in elderly people. PLOS One 3, e2232 (2008), 10.1371/journal.pone.0002232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andrew M. K., Rockwood K., Social vulnerability predicts cognitive decline in a prospective cohort of older Canadians. Alzheimer’s Dement. 6, 319–325.e1 (2010), 10.1016/j.jalz.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Andrew M. K., Mitnitski A., Kirkland S. A., Rockwood K., The impact of social vulnerability on the survival of the fittest older adults. Age Ageing 41, 161–165 10.1093/ageing/afr176(2012), 10.1093/ageing/afr176. [DOI] [PubMed] [Google Scholar]
- 15.Wallace L. M. K., Theou O., Pena F., Rockwood K., Andrew M. K., Social vulnerability as a predictor of mortality and disability: Cross-country differences in the survey of health, aging, and retirement in Europe (SHARE). Aging Clin. Exp. Res. 27, 365–372 (2015), 10.1007/s40520-014-0271-6. [DOI] [PubMed] [Google Scholar]
- 16.Flanagan B. E., Gregory E. W., Hallisey E. J., Heitgerd J. L., Lewis B., A social vulnerability index for disaster management. J. Homeland Secur. Emerg. Manag. 8 (2011), 10.2202/1547-7355.1792. [DOI] [Google Scholar]
- 17.Kind A. J. H., et al. , Neighborhood socioeconomic disadvantage and 30-day rehospitalization. Ann. Intern. Med. 161, 765–774 (2014), 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Noble S., et al. , The English Indices of Deprivation 2019. (Ministry of Housing, Communities and Local Government, 2019). [Google Scholar]
- 19.Piantadosi S., Byar D. P., Green S. B., The ecological fallacy. Am. J. Epidemiol. 127, 893–904 (1988). [DOI] [PubMed] [Google Scholar]
- 20.Lewis G. H., “Impactibility models”: Identifying the subgroup of high-risk patients most amenable to hospital-avoidance programs. Milbank Q. 88, 240–255 (2010), 10.1111/j.1468-0009.2010.00597.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Designing and Implementing Medicaid Disease and Care Management Programs. Section 3: Selecting and Targeting Populations for a Care Management Program. Agency for Healthcare Research & Quality; 2014. https://www.ahrq.gov/patient-safety/settings/long-term-care/resource/hcbs/medicaidmgmt/index.html. Accessed 19 October 2017.
- 22.Juster F. T., Suzman R., An overview of the health and retirement study. J. Hum. Res. 30, S7–S56 (1995), 10.2307/146277. [DOI] [Google Scholar]
- 23.Sonnega A., et al. , Cohort profile: The health and retirement study (HRS). Int. J. Epidemiol. 43, 576–585 (2014), 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weir D. R., Data from “Health and Retirement Study”. Public Survey Data. https://hrsdata.isr.umich.edu/data-products/public-survey-data. Accessed 01 December 2019.
- 25.Bunt S., Steverink N., Olthof J., Schans C. P., Hobbelen J. S. M., Social frailty in older adults: A scoping review. Eur. J. Ageing 14, 323–334 (2017), 10.1007/s10433-017-0414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhao S., Witten D., Shojaie A., In defense of the indefensible: A very naïve approach to high-dimensional inference. Stat. Sci. 36, 562–577 (2021), 10.1214/20-STS815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Friedman J., Hastie T., Tibshirani R., Regularization paths for generalized linear models via coordinate descent. J. Stat. Soft. 33, 10 (2010), 10.18637/jss.v033.i01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Collins G. S., Reitsma J. B., Altman D. G., Moons K. G. M., Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. Ann. Intern. Med. 162, 55–63 (2015), 10.7326/M14-0697. [DOI] [PubMed] [Google Scholar]
- 29.Committee on Accounting for Socioeconomic Status in Medicare Payment Programs, “Board on Population Health and Public Health Practice, Board on Health Care Services, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine” in Accounting for Social Risk Factors in Medicare Payment, Kwan L. Y., Stratton K., Steinwachs D. M., Eds. (National Academies Press, Washington, DC, 2017), 10.17226/23635. [DOI] [PubMed] [Google Scholar]
- 30.Rogstad T. L., Gupta S., Connolly J., Shrank W. H., Roberts E. T., Social risk adjustment in the hospital readmissions reduction program: A systematic review and implications for policy. Health Affairs 41, 1307–1315 (2022), 10.1377/hlthaff.2022.00614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wadhera R. K., Yeh R. W., Joynt Maddox K. E., The hospital readmissions reduction program — time for a reboot. N. Engl. J. Med. 380, 2289–2291 10.1056/NEJMp1901225(2019), 10.1056/NEJMp1901225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garcia M. E., Uratsu C. S., Sandoval-Perry J., Grant R. W., Which complex patients should be referred for intensive care management? A mixed-methods analysis. J. Gen. Intern. Med. 33, 1454–1460 10.1007/s11606-018-4488-5(2018), 10.1007/s11606-018-4488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Obermeyer Z., Powers B., Vogeli C., Mullainathan S., Dissecting racial bias in an algorithm used to manage the health of populations. Science 366, 447–453 (2019). [DOI] [PubMed] [Google Scholar]
- 34.Justice A. C., Covinsky K. E., Berlin J. A., Assessing the generalizability of prognostic information. Ann. Intern. Med. 130, 515–524 (1999), 10.7326/0003-4819-130-6-199903160-00016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 01 (PDF)
Data Availability Statement
Researchers can apply to the Health and Retirement Study (https://hrs.isr.umich.edu/) to access the data used in this study (24). Final code will be made available at github.com/sachinjshah.