Abstract
Background. Overweight and obesity are associated with atrial fibrillation (AF), and bariatric surgery (BS), able to induce sustained and prolonged weight loss, might represent the ideal treatment in the prevention of AF. Previous studies could not definitely establish a role for weight loss and BS in preventing incident AF so far. During the last few years, several studies on the effect of bariatric surgery on cardiovascular diseases have been published, and we performed a systematic review and meta-analysis to evaluate the role of weight loss through BS in the prevention of incident AF in obesity. Methods. This meta-analysis followed the PRISMA guideline. Eligible studies were controlled trials evaluating the appearance of atrial fibrillation in patients undergoing weight loss through BS as compared with patients receiving medical treatment. Quality of studies was assessed according to the Newcastle-Ottawa Quality Assessment Scale, and risk-of-bias was evaluated employing the Egger’s test. All analyses were run by a random-effects model according to Hartung and Knapp and sensitivity analyses were performed. Heterogeneity was assessed through Q and I2 statistics for each comparison, and potential publication bias was formally investigated. Results. Ten studies were included in the meta-analysis, and the overall result was statistically significant [OR = 0.665 (0.475–0.929), p = 0.017], with significant heterogeneity (Q = 48.98, p < 0.001; I2 = 81.6%), but with no publication bias. In sensitivity analyses, the amount of weight loss, percentage of patients with diabetes and value of the Newcastle-Ottawa Quality Assessment Scale, were all associated with significance of effect. Since age was different in one study, a sensitivity analysis was performed by excluding this study; OR was similar [OR = 0.608 (0.454–0.814), p < 0.001]; heterogeneity was reduced but still significant (Q = 35.74, p < 0.001, I2 = 77.6%) and again no publication bias was detected. Conclusions. Bariatric surgery as compared to medical treatment is associated with reduced appearance of incident AF.
Keywords: surgery, bariatric surgery, atrial fibrillation, weight loss, obesity, meta-analysis, body weight, body mass index
1. Introduction
Overweight and obesity are associated with higher prevalence of co-morbidities, including cardiovascular diseases (heart failure, ischemic heart disease, stroke), renal failure and cancer, and with reduced life expectancy and reduced quality of life [1]. Recent studies have highlighted the association between obesity and atrial fibrillation (AF), showing that two different kinds of AF (incident AF and persistent/recurrent AF) can occur in obesity. Various studies have shown that obesity is associated with an increased prevalence of incident AF and persistent/recurrent AF [2,3]; in addition, weight gain is associated with increased prevalence of incident AF [4], while no data are available for persistent/recurrent AF. In addition to being a risk factor for the development of well-known comorbidities, such as dyslipidemia, type 2 diabetes mellitus, arterial hypertension and obstructive sleep apnea, obesity may increase the risk of AF through several mechanisms, including structural and electrical remodeling, which contribute to the development of an arrhythmogenic environment. This view is supported by clinical epidemiology [2,3,4], as well as by experimental studies, showing the effect of short-term weight gain in remodeling of heart atria, in increasing fibrous tissue deposition, in increasing expression of endothelin receptors and abnormalities in atrial conduction, in increasing AF inducibility [5], and in increasing pericardial fat volumes; histological samples of the atrial myocardium from regions adjacent to pericardial fat deposits showed infiltration of epicardial fat into the myocardium, resulting in potential voltage abnormalities, conduction block, and increased AF vulnerability [6].
Weight loss, obtained especially through bariatric surgery, can significantly counteract several consequences of obesity [7,8]. Bariatric surgery, as compared with diet, exercise, and drugs, is able to induce sustained and prolonged weight loss, and to prevent dyslipidemia, type 2 diabetes mellitus, arterial hypertension and obstructive sleep apnea, cardiovascular disease, cancer, and kidney disease [9], effects that occur regardless of the patients metabolic status [10]; the effect on the reduction of mortality is debated, as it has been seen that in young patients (age < 43 years), especially in the presence of diabetes it could increase mortality [11]. Bariatric surgery is associated, beyond weight loss, with other important changes, namely improved endothelial function [12] and reduced sub-inflammation [13], reduced prevalence of arterial hypertension [14] left ventricular hypertrophy, improved glucose tolerance and reduced insulin resistance [14], improved quality of life [15], thus possibly representing the ideal treatment in the prevention of AF. It remains to be established if these factors could contribute independently from weight loss in preventing AF.
Pilot studies showed the beneficial effect of bariatric surgery on slowing heart rate [16,17], and heart rate recovery after exercise, which reflects the balance of cardiac autonomic input from the sympathetic and parasympathetic systems. In addition, weight loss, especially sustained weight loss through bariatric surgery, has been shown to be beneficial in reducing progression of incident AF to recurrent AF [18,19]. However, a role for bariatric surgery in prevention of incident AF is still controversial; meta-analyses performed on studies available at the time of publication [20,21], have been contradictory in establishing a role of weight loss in preventing incident AF. The scenario has changed during the last two years since more studies on the effect of bariatric surgery on cardiovascular diseases have been published [22,23].
The aim of this study was to understand the role of weight loss in preventing incident AF. Therefore, we performed an updated systematic review and meta-analysis to evaluate the role of prolonged and substantial weight loss through bariatric surgery in the prevention of incident AF in obesity.
2. Methods
2.1. Search Strategy and Inclusion Criteria
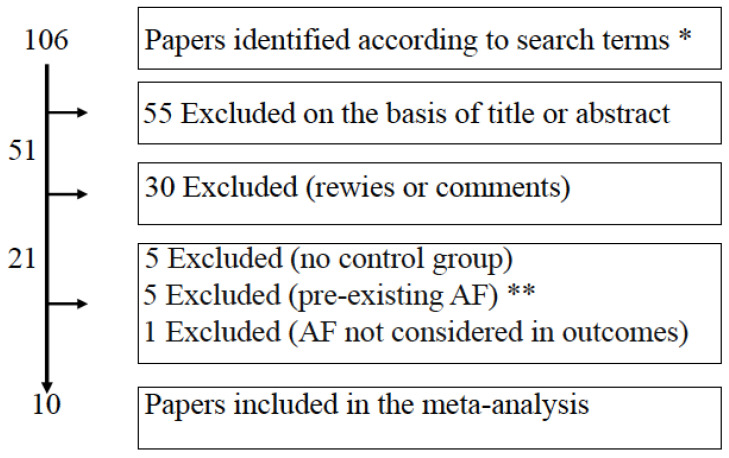
This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline [24]. Eligible studies were controlled trials evaluating the appearance of atrial fibrillation in patients undergoing weight loss through bariatric surgery as compared with patients receiving medical treatment. Full reports, published in any language, were included. Two independent authors (AEP, LC) searched relevant literature in databases including PubMed, Embase, and Cochrane Library from inception until 30 October 2022. The following keyword was used for disease: atrial fibrillation. To define exposure, the following keywords were used: obesity, overweight, weight loss, weight reduction, loss of weight, decrease in weight, weight decrease, weight changes, changes in weight, bariatric surgery (laparoscopic adjustable gastric banding, gastric bypass, sleeve gastrectomy, biliopancreatic diversion, biliointestinal bypass). The title and abstracts written in English language were reviewed to recognize eligible studies on the impact of weight loss on the appearance of atrial fibrillation. Additional studies were also manually searched through the references cited in reviews. Cohort as well as case-control studies were included. If the results of one study were reported in more publications, only the most recent and complete data were included in analysis. When required, authors of the studies were also contacted by mail to yield more details. The following studies were excluded: descriptive studies, editorials, review articles, systematic reviews and meta-analyses, and studies that did not provide risk ratios or effect sizes. Decisions on trials to include were taken by the authors (AEP, LC, CLR, SM, ET, FF), and disagreements were resolved by discussion. The reason for exclusion of other trials was specified (lack of details, no controls, pre-existing AF, Figure 1). Ten studies [22,25,26,27,28,29,30,31,32,33] fulfilled the inclusion criteria (Table 1 shows details of the 10 studies included in this meta-analysis). The protocol of the meta-analysis has been registered (Prospero, CRD42022374548).
Figure 1.
Flow-chart of the analysis performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA). After screening of literature according to search terms, most paper were excluded for reasons indicated in the squares. * Search terms: “atrial fibrillation” AND (“bariatric surgery” OR “biliopancreatic diversion” OR “gastric bypass” OR “roux-en-Y” OR “sleeve gastrectomy” OR “biliointestinal bypass” OR “adjustable gastric banding”) ** AF atrial fibrillation.
Table 1.
Details of the studies analyzed.
| Authors and Year | Ref. | Study | Bariatric (BS) Surgical Procedure | BS Patients (% Women) |
Follow-Up (y) | Age (y) | BMI (kg/m2) | Control Patients (% Women) |
Follow-Up (y) | Age (y) |
BMI (kg/m2) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jamaly 2016 | [25] | cohort prospective | VGB (68%) AGB (19%), RYGB (13%) | 2000 (70.7) | 19 | 47.2 | 42.4 | 2021 (71.2) | 19 | 48.6 | 40.1 | ||||||
| Lynch 2019 | [26] | cohort retrospective | RYGB or LSG | 2522 (83.1) | 6.2 | 42 | 47.1 | 2522 (83.4) | 8 | 42 | 47.7 | ||||||
| Aminian 2019 | [27] | cohort retrospective | RYGB or LSG or AGB or BPD | 2135 (70.2) | 3.3 | 52.5 | 45.1 | 10734 (68.4) | 4 | 54.8 | 42.6 | ||||||
| Singh 2020 | [28] | cohort retrospective | RYGB or LSG or AGB-or BPD | 5087 (80.4) | 3.9 | 45.3 | -- | 9858 (81.1) | 3.9 | 45.3 | -- | ||||||
| Srivatsa 2020 | [29] | cohort retrospective | RYGB or LSG | 1581 (78.7) | 5.5 | 49 | -- | 3162 (78.7) | 5.5 | 49 | -- | ||||||
| Moussa 2021 | [30] | cohort retrospective | Various BS procedures | 3077 (77.3) | 12.3 | 50 | 43.5 | 3077 (77.3) | 12.3 | 50 | 43.1 | ||||||
| Höskuldsdóttir 2021 | [31] | cohort retrospective | RYGB | 5321 (66.6) | 4.5 | 49 | 42 | 5321 (68.1) | 4.5 | 47 | 41 | ||||||
| Rassen 2021 | [32] | cohort retrospective | 44% GA, 8% GR, 50% GIB | 291 (69.2) | 2.5 | 57.9 | 42.6 | 461 (61.6) | 2.5 | 59 | 42.1 | ||||||
| Näslund 2021 | [33] | cohort prospective | RYGB or LSG | 509 (42.8) | 4.6 | 53 | 40.6 | 509 (42.8) | 4.6 | 53.2 | 39.7 | ||||||
| Yuan 2021 | [22] | cohort retrospective | RYGB | 308 (82.5) | 15 | 44.2 | 46.4 | 701 (76.6) | 15 | 43.6 | 44.8 | ||||||
| Authors and year | Ref. | Total patients | Main BS type | Mean age (y) | Mean Follow-up (y) | Mean BMI (kg/m2) | WL (%) BS patients | WL (%) control patients | % DM BS patients | % DM control patients |
%
HTN BS |
%
HTN con |
%
CAD BS |
% CAD
con |
%
HF BS |
%
HF con |
NOS score |
| Jamaly 2016 | [25] | 4021 | 1 | 47.9 | 19 | 41.2 | −20 | 0 | 17 | 13 | 78.3 | 63.6 | 3.0 | 2.9 | 3.0 | 2.9 | 8 |
| Lynch 2019 | [26] | 5044 | 2 | 42 | 7.1 | 47.4 | −58 | −3.8 | 29 | 10 | 42.5 | 43.5 | -- | -- | 4.9 | 4.6 | 7 |
| Aminian 2019 | [27] | 12869 | 2 | 53.6 | 3.65 | 43.8 | −18 | -- | 100 | 100 | 91.5 | 79.8 | 9.6 | 5.5 | 11.1 | 12.5 | 6 |
| Singh 2020 | [28] | 14945 | 3 | 45.3 | 3.9 | -- | −20 | −0.8 | 22 | 20 | 31.5 | 29.9 | .04 | 3.3 | .8 | .8 | 7 |
| Srivatsa 2020 | [29] | 4743 | 2 | -- | 5.5 | -- | −60 | -- | 23 | 16 | 37.4 | 33.7 | 2.7 | 2.9 | 6 | ||
| Moussa 2021 | [30] | 6154 | 3 | 50 | 12.3 | 43.3 | −9 | +4.1 | 22 | 23 | 41.4 | 30.3 | 11.9 | 16.9 | 15.7 | 14.5 | 6 |
| Höskuldsdóttir 2021 | [31] | 10642 | 2 | 48 | 4.5 | 41.5 | −22 | −4.8 | 100 | 100 | 47.1 | 59.8 | 7.4 | 5.9 | 2.7 | 3.7 | 6 |
| Rassen 2021 | [32] | 752 | 3 | 58.4 | 2.5 | 42.3 | −20 | -- | 100 | 100 | 65.2 | 71.7 | 24.6 | 24.9 | 15.9 | 26.6 | 4 |
| Näslund 2021 | [33] | 1018 | 2 | 53.1 | 4.6 | 40.1 | −28 | -- | 41 | 45 | 88.9 | 88.4 | 12.5 | 12.9 | 9.8 | 10 | 5 |
| Yuan 2021 | [22] | 1009 | 2 | 43.9 | 15 | 45.6 | −26.5 | −8.25 | 21 | 39 | 44.15 | 56.0 | 4.9 | 5.2 | .3 | 3.7 | 8 |
BS = bariatric surgery; VGB = vertical banded gastrotomy; RYGB = gastric bypass; LSG = sleeve gastrectomy; AGB = adjustable gastric banding; GA = gastrectomy; GR = gastric resection; GIB = gastric intestinal bypass. Main BS type: 1 = restrictive surgeries (VGB, AGB); 2 = metabolic surgeries (LSG, RYGB); 3 = various surgeries (LSG, RYGB, AGB, GA, GR, GIB) WL = weight loss; DM = diabetes mellitus; HTN = hypertension; CAD = coronary artery disease; HF = heart failure; NOS = Newcastle Ottawa Scale.
2.2. Data Extraction
The following data were extracted: name of the first author, year of publication, type of study, type of bariatric surgery, number of patients who have undergone surgery and number of control patients. For both groups additional items were extracted: percentage of male and female patients, duration of follow-up, mean age, mean BMI (for the first group before surgery and for control at the start of follow-up), percentage of weight lost during follow-up, percentage of patients diagnosed with type 2 diabetes, with hypertension, with coronary artery disease and with heart failure. The details for each study are shown in Table 1. For the analysis, event rate was extracted per outcome parameter for each group and unadjusted and adjusted HRs with their 95% confidence intervals (CIs) for the association with outcome of interest.
2.3. Quality Assessment
Quality of reports was assessed independently by reviewers according to Newcastle-Ottawa Quality Assessment Scale (NOS) for Cohort Studies [34]. The NOS scale is based on a “star system” in which a study is judged from three broad perspectives: study group selection, group comparability, and ascertaining the outcome of interest. The variables considered are: risk of bias linked to the selection of participants, confounding variables, performance, detection and measurement of exposure, attrition and reporting biases. The length of follow-up was set at a minimum of 5 years to be evaluated as adequate. Disagreement for the quality assessment was resolved by discussion. A score was eventually built, classifying poor, intermediate, or good quality, based on the number of the above criteria available for each paper. The NOS score is reported in Table 2.
Table 2.
Newcastle Ottawa Scale of the studies considered in this meta-analysis [34]. The explication of this scale is reported in the Supplementary File.
| Studies Author/Pub Year |
Selection | Comparability | Outcome | Total Score | Conclusion | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 1 | 2 | 1 | 2 | 3 | |||
| Jamaly 2016 [25] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 8 | Good |
| Lynch 2019 [26] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 7 | Good |
| Aminian 2019 [27] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 6 | Intermediate |
| Singh 2020 [28] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 7 | Good |
| Srivatsa 2020 [29] | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 6 | Intermediate |
| Moussa 2021 [30] | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 6 | Intermediate |
| Höskuldsdóttir 2021 [31] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 6 | Intermediate |
| Rassen 2021 [32] | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 4 | Poor |
| Näslund 2021 [33] | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 5 | Poor |
| Yuan 2021 [22] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 8 | Good |
2.4. Statistical Analysis
Intervention effect (weight loss vs. controls) was expressed as odds ratio (OR), with 95% confidence intervals (CIs); all analyses were performed by a random-effects model according to Hartung and Knapp [35]. Heterogeneity was assessed through Q and I2 statistics for each comparison, and potential sources of heterogeneity were discussed where appropriate [36]. Heterogeneity was considered statistically significant for a p value < 0.05. Through meta-regression, we also evaluated, the possible role of several patients’ and study characteristics on the incidence of new cases of atrial fibrillation (AF). This was done independently of statistically significant heterogeneity. The dependent variable was the incidence of cases of AF. The role of each covariate in heterogeneity was expressed by Wald test estimated by the meta-regression. The following covariates were included in the meta-regression analysis: number of patients enrolled, age, kind of study (prospective or retrospective), percentage of persons with diabetes mellitus, NOS score, duration of follow-up, body mass index (BMI) of each study (weighted means of intervention and control patients), amount of weight loss and efficacy of treatment (vs. controls) in each study. Meta-regression was performed considering all studies together. In a secondary analysis, we also evaluated the existence of a potential publication bias, that means the tendency of authors and editors to publish studies in which the experimental results achieved statistical significance, more favorably than in studies in which the results were not significant, which would ultimately introduce bias into the overall published literature [37]. Funnel-plot asymmetry was evaluated by using the Egger’s test for small study effects through the meta-bias routine [38]. Sensitivity analyses were also performed by considering the prevalent kind of BS employed in the studies [i.e., restrictive surgery (VGB = vertical banded gastrotomy; AGB = adjustable gastric banding), metabolic surgery (LSG = laparoscopic sleeve gastrectomy; RYGB = roux-en-y gastric bypass), or a mixture of procedures (GA = gastrectomy; GR = gastric resection; GIB = gastric intestinal bypass) plus AGB, LSG and RYGB], percentage of patients with diabetes mellitus, percent weight loss, and exclusion of studies showing substantial variation in basal conditions from other studies. To this end, the Baujat method was used to identify outliers in this model [39]. The Baujat method detects outliers by analyzing the change of the general effect by systematically leaving out one study at a time, i.e., the contribution of this study to the between-study heterogeneity statistic Q, and contribution to I2 [40]. A leave-one-out sensitivity analysis was also conducted to assess each study’s influence on the pooled estimate by omitting one study at a time and recalculating the combined estimates for the remaining studies. All statistical analyses were performed by Stata 17 (Stata Corporation, College Station, TX, USA) for MacIntosh.
3. Results
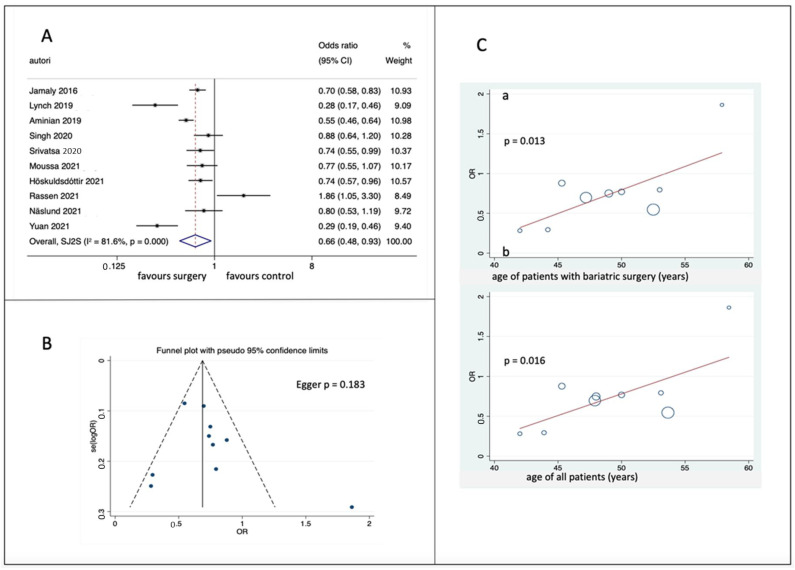
Ten studies were included in the meta-analysis (Figure 2A); in 6 out of 10 studies, the effect of bariatric surgery was statistically significant per se, and the overall result was statistically significant [OR = 0.665 (0.475–0.929), p = 0.017]. Heterogeneity was significant (Q = 48.98, p < 0.001; I2 = 81.6%). In contrast, the meta-funnel showed no publication bias (Figure 2B), and at meta-regression, only age correlated with the effect (p = 0.013 when considering the age of patients undergoing BS, p = 0.016 when considering the age of the whole cohort (Figure 2C). No other item correlated with the OR. Number of patients enrolled, nature of the study (prospective or retrospective), NOS score, duration of follow-up, body mass index (BMI) of each study (weighted means of intervention and control patients), amount of weight lost, percentage of patients with diabetes, did not yield significant correlations at meta-regression. Supplementary File (Supplementary Table S1) reports sensitivity analyses which were performed.
Figure 2.
(A) Forest plot of pooled hazard ratios of atrial fibrillation [22,25,26,27,28,29,30,31,32,33]; (B) funnel plots with 95% CI; (C) meta-regression analysis of effect as a function of age of BS patients (a) and of the whole cohorts (b). OR = Odds Ratio; 95% CI = confidence interval; SE, standard error.
In a second sensitivity analysis, the effect of the percentage of weight loss was considered; the effect was significant for a weight loss ≥ 22%, [OR = 0.525 (0.316–0.872), 0.013], with lower but still significant heterogeneity (Q = 25.52, p < 0.001, I2 = 84.2%); the effect was non-significant for a weight loss < 22%, [OR = 0.827 (0.539–1.271), p = 0.387] with lower but still significant heterogeneity (Q = 22.30, p < 0.001, I2 = 82.1%). Then, the role of the percentage of patients with diabetes was considered; for a percentage < 100% (7 studies), the effect was significant [OR = 0.596 (0.406–0.875), p = 0.008], with significant heterogeneity (Q = 30.19, p < 0.001, I2 = 80.1%); for a percentage = 100% (3 studies), the effect was non-significant [OR = 0.880 (0.394–1.969), p = 0.756, NS)], but still with significant heterogeneity (Q = 18.43, p < 0.001, I2 89.1%). Finally, the effect was evaluated according to the Newcastle-Ottawa Quality Assessment Scale (NOS); the effect was statistically significant [OR = 0.570 (0.365–0.890), p = 0.013] for higher NOS score (above mean NOS), and heterogeneity was significant (Q = 29.64 p < 0.001, I2 = 83.1%); the effect was non-significant for NOS score below mean NOS [OR = 0.840 (0.477–1.478), p = 0.545], and heterogeneity was still significant (Q = 19.27 p < 0.001, I2 = 84.43%). Since one study [32] showed a different age from other studies and contributed to I2 heterogeneity for more than 13% [39,40], a sensitivity analysis was performed by excluding this study (Supplementary Figure S1); OR was similar [OR = 0.62 (95% CI 0.51–0.76, p < 0.001)]; heterogeneity was reduced but was still significant (Q = 35.70, p < 0.001; I2 = 77.6%), and again the meta-funnel showed no publication bias. At meta-regression BMI correlated with the effect (p = 0.052 when considering BMI of patients undergoing BS, p = 0.054 when considering BMI of the whole cohort); more, the OR for weight loss < 22% became significant [OR = 0.696 (0.547–0.885), p = 0.003)], with small heterogeneity (Q = 9.71, p = 0.021, I2 = 69.1%); similarly, the OR for percentage of patients with diabetes was significant [OR = 0.629 (0.443–0.893), p = 0.010)], and the heterogeneity was small (Q = 3.92, p = 0.048, I2 = 74.5%). According to the Newcastle-Ottawa Quality Assessment Scale (NOS), the effect was statistically significant [OR = 0.661 (0.498–0.878), p = 0.004] with very small heterogeneity (Q = 5.34, p = 0.096, I2 = 62.6%). The kind of BS procedure employed was the basis for an additional sensitivity analysis: when restrictive surgeries were employed (VGB and AGB, one study), the OR was 0.697 (0.584–0.832), p = 0.001; when metabolic surgeries were employed (LSG and RYGB, 6 studies, the OR was 0.531(0.354–0.797), p = 0.002, with small but significant heterogeneity (Q = 26.34, p = 0.001, I2 = 81.0%); finally, when mixed surgeries were considered (see Table 1 for details, the OR was not-significant [1.033 (0.610–1.750), p = 0.904]. with small heterogeneity (Q = 7.10, p = 0.029, I2 = 71.8%); the effect was not different when one study [32] was excluded [OR = 0.824 (0.642–1.057), p = 0.128], and heterogeneity was almost nil (Q = 0.33, p = 0.564, I2 = 0.0%).
No publication bias was detected. In summary, a fair part of the heterogeneity was due to one study [28]. Finally, also when other methods of analysis were employed, namely fixed model (RR) instead of random model (OR) or direct analysis of RR as reported by the authors of the studies (ES), the effect was always similarly significant (Supplementary Table S2). Supplementary Table S3 reports the Newcastle-Ottawa Quality Assessment Scale (NOS).
Supplementary Table S4 shows a comparison of baseline clinical conditions of patients undergoing bariatric surgery (BS) and controls in the ten studies included in this meta-analysis. A total of 61,197 patients (22,831 patients undergoing BS and 38,366 control patients receiving medical treatment) was considered; from the Table it appears that the former and the latter patients were well matched as to age, BMI, duration of follow-up, percentage of patients with diabetes, with hypertension, with coronary heart disease, with heart failure; as expected, weight loss was different in BS and in control patients.
4. Discussion
Both incident AF and persistent/recurrent AF can occur in obesity. There are similarities and differences; for instance, obesity is associated with increased prevalence of both incident AF and persistent/recurrent AF [2,3], and weight gain is associated with incident AF [4] while no data are available for persistent/recurrent AF. The reasons why obesity is associated with AF are still largely unknown; obesity is a risk factor for the development of several comorbidities, namely diabetes, arterial hypertension and obstructive sleep apnea, dyslipidemia, that can lead to cardiovascular disease such as coronary heart disease and heart failure [41]; obesity may increase the risk of AF through several mechanisms, including structural and electrical remodeling, which contribute to the development of the arrhythmogenic milieux. This has been shown in experimental studies in sheep [5], in which increased pericardial fat volumes are associated with infiltration of epicardial fat into the myocardium, resulting in potential voltage abnormalities, conduction block, and increased AF vulnerability [6].
It is well established that bariatric surgery induces sustained and prolonged weight loss and thus might represent the ideal treatment to prevent AF through weight loss. Weight loss, especially sustained weight loss through bariatric surgery, can be beneficial in reducing the progress of incident AF to recurrent AF [18,19], but large studies and even meta-analyses failed to establish a role of weight loss in preventing incident AF [20,21].
The present meta-analysis shows that bariatric surgery, compared to medical treatment, is associated with reduced appearance of incident AF, similar to what has been seen for persistent/recurrent AF. The effect was statistically significant in six out of ten studies analyzed, and the overall effect was statistically significant. In addition, the effect was related to the percentage of weight lost and was more evident for cohorts not entirely consisting of patients with diabetes. Lastly, sensitivity analysis showed that after exclusion of one single study [32], the results were even more statistically significant. At meta-regression, only age negatively correlated with effect, and at higher age the effect was lower. After exclusion of one study [32], in which age of the patients was higher than the rest of the studies, and contribution to heterogeneity was significant [39,40], only BMI correlated with effect, indicating a greater effect for higher BMI. All sensitivity analyses reported in the Supplementary File show that the effect was statistically significant under most conditions, and that most of the negative results were due to one single study that was different from others, mainly for the age of the patients. In addition, the effect was similar when calculated as a random model, fixed model, or when evaluated through risk ratios (RR)s as published by the authors of the papers considered in this meta-analysis.
This meta-analysis has several limitations. The first limitation is that, from the studies included, we do not have data on the duration of obesity, even though age of BS and control patients was not different. Secondly, we could only analyze obesity as expressed by body mass index, not through measures of fat distribution [42]. Although BMI is strongly correlated with percent body fat across populations, there are limitations in its predictive ability to estimate body fat for any given individual, in particular in regard of visceral adiposity. In fact, visceral adiposity as measured by WC, WHR, or detailed imaging methods has been shown to be a risk factor independently of BMI [43]. Thirdly, BS is associated with loss of fat-free mass together with fat mass, and muscle loss is an important component of fat free mass [44]. Under conditions of accelerated loss of fat and muscle mass, such as thyrotoxicosis, an increased frequency of accelerated heart rhythm and AF are observed [45]. With BS, no significant changes of thyroid hormones are observed [46], and the only involvement of heart muscle seems to be a remodeling of heart chambers, a situation that does not increase the risk of AF [47]. Finally, different meta-analyses led to different results regarding the effect of BS on incident AF. The main reason is probably the number of studies considered; the strength of our study is that 10 studies were included, while in two previous meta-analyses [20,21] only seven studies were considered. Differently from previous meta-analyses [2,4,18,19,20,21], all analyses were performed by a random-effects model according to Hartung and Knapp [35], that is straightforward and outperforms the standard DerSimonian-Laird method [48], especially when less than ten studies are considered [49]; also, when other methods of analysis were employed, such as fixed model (RR) analysis, or direct analysis of RR as reported by the authors of the studies (ES), the effect was similarly significant; finally, one study [32] was excluded in this meta-analysis because of a clear difference of age of patients compared to other studies. All these differences deserve a comment; first, the role of age might be of importance in AF, as it is in other cardiovascular diseases. In keeping with this possibility, we have shown for the first time that bariatric surgery is associated with reduced all-cause mortality and reduced cardiovascular mortality [7]; however, in a second meta-analysis, we were able to show that age can be of importance in affecting prevention of all-cause mortality and of mortality due to cancer and diabetes [8]. A different possibility is that the amount of weight loss is important, as indicated in this meta-analysis and as reported by Jones et al. [50], who showed that a weight loss of less than 5% is not able to prevent incident AF. The quality of studies assessed through the NOS score might also be of importance, as indicated by our sensitivity analysis; in fact, the effect was statistically significant for higher NOS score (i.e., above mean NOS), but was non-significant for NOS score below mean NOS score.
One should also remember that bariatric surgery does not only mean prolonged and substantial weight loss; bariatric surgery is associated with reduced incidence of diabetes, cardiovascular disease, cancer, and liver and kidney disease [9], effects that occur regardless of the patients’ metabolic status [10].
In summary, bariatric surgery is associated with reduced incident AF in patients affected by obesity. This might be instrumental in reducing cardiovascular morbidity and mortality in people with obesity [41], but more studies are needed to determine the amount of weight loss needed to prevent AF. Moreover, a causal relationship still needs to be confirmed between weight loss and prevention of AF; bariatric surgery is associated, beyond weight loss, with other important changes, namely improved endothelial function [12] and reduced sub-inflammation [13], reduced prevalence of arterial hypertension [14] and of left ventricular hypertrophy, improved glucose tolerance and reduced insulin resistance [14,16], improved quality of life [15]. It remains to be established if these factors, not clearly defined in the studies considered, could also contribute independently from weight loss in preventing AF.
5. Conclusions
Bariatric surgery as compared to medical treatment is significantly associated with reduced incident AF, possibly mainly through prolonged and sustained weight loss. The present report is of great value, and consistent with previous data demonstrating that prolonged and sustained weight loss prevent progression of incident AF to recurrent AF.
Acknowledgments
This study was supported by a grant (Ricerca Corrente) of the Italian Ministry of Health (Ministero della Salute) to IRCCS MultiMedica.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15040940/s1, Supplementary Table S1: sensitivity analyses; Supplementary Table S2: comparison of results obtained with random model (OR), fixed model, and risk ratios published by authors; Supplementary Figure S1: Meta-analysis after exclusion of study [32]; Supplementary Table S3: The Newcastle Ottawa Scale [34]; Supplementary Table S4: Comparison of baseline conditions of patients undergoing bariatric surgery (BS) and controls in the ten studies included in this meta-analysis.
Author Contributions
The study was a project of A.E.P., C.W.L.R. and F.F., A.E.P. and L.C. searched literature, E.T. performed meta-analyses. C.W.L.R. and S.M. improved and supervised the project. All authors contributed to writing the MS. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was exempt from ethics approval as only data from previously published studies were retrieved and synthesized.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available from the corresponding author on the basis of reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Calle E.E., Thun M.J., Petrelli J.M., Rodriguez C., Heath C.W. Body-mass index and mortality in a prospective cohort of U.S. adults. N. Engl. J. Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 2.Wanahita N., Messerli F.H., Bangalore S., Gami A.S., Somers V.K., Steinberg J.S. Atrial fibrillation and obesity—Results of a meta-analysis. Am. Heart J. 2008;155:310–315. doi: 10.1016/j.ahj.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Zhuang J., Lu Y., Tang K., Peng W., Xu Y. Influence of body mass index on recurrence and quality of life in atrial fibrillation patients after catheter ablation: A meta-analysis and systematic review. Clin. Cardiol. 2013;36:269–275. doi: 10.1002/clc.22108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aune D., Sen A., Schlesinger S., Norat T., Janszky I., Romundstad P., Tonstad S., Riboli E., Vatten L.J. Body mass index, abdominal fatness, fat mass and the risk of atrial fibril-lation: A systematic review and dose-response meta-analysis of prospective studies. Eur. J. Epidemiol. 2017;32:181–192. doi: 10.1007/s10654-017-0232-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abed H.S., Samuel C.S., Lau D.H., Kelly D.J., Royce S.G., Alasady M., Mahajan R., Kuklik P., Zhang Y., Brooks A.G., et al. Obesity results in progressive atrial structural and electrical remodeling: Implications for atrial fibrillation. Heart Rhythm. 2013;10:90–100. doi: 10.1016/j.hrthm.2012.08.043. [DOI] [PubMed] [Google Scholar]
- 6.Mahajan R., Lau D.H., Brooks A.G., Shipp N.J., Manavis J., Wood J.P., Finnie J.W., Samuel C.S., Royce S.G., Twomey D.J., et al. Electrophysiological, electroanatomical, and structural remodeling of the atria as consequences of sustained obesity. J. Am. Coll. Cardiol. 2015;66:1–11. doi: 10.1016/j.jacc.2015.04.058. [DOI] [PubMed] [Google Scholar]
- 7.Pontiroli A.E., Morabito A. Long-term prevention of mortality in morbid obesity through bariatric surgery. A systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann. Surg. 2011;253:484–487. doi: 10.1097/SLA.0b013e31820d98cb. [DOI] [PubMed] [Google Scholar]
- 8.Pontiroli A.E., Ceriani V., Tagliabue E. Compared with Controls, Bariatric Surgery Prevents Long-Term Mortality in Persons with Obesity Only Above Median Age of Cohorts: A Systematic Review and Meta-Analysis. Obes. Surg. 2020;30:2487–2496. doi: 10.1007/s11695-020-04530-3. [DOI] [PubMed] [Google Scholar]
- 9.Pontiroli A.E., Zakaria A.S., Fanchini M., Osio C., Tagliabue E., Micheletto G., Saibene A., Folli F. A 23-year study of mortality and development of co-morbidities in patients with obesity undergoing bariatric surgery (laparoscopic gastric banding) in comparison with medical treatment of obesity. Cardiovasc. Diabetol. 2018;17:161. doi: 10.1186/s12933-018-0801-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sesti G., Folli F., Perego L., Hribal M.L., Pontiroli A.E. Effects of weight loss in metabolically healthy obese subjects after laparoscopic adjustable gastric banding and hypocaloric diet. PLoS ONE. 2011;6:e17737. doi: 10.1371/journal.pone.0017737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pontiroli A.E., Ceriani V., Tagliabue E., Zakaria A.S., Veronelli A., Folli F., Zanoni I. Bariatric surgery, compared to medical treatment, reduces morbidity at all ages but does not reduce mortality in patients aged <43 years, especially if diabetes mellitus is present: A post hoc analysis of two retrospective cohort studies. Acta Diabetol. 2020;57:323–333. doi: 10.1007/s00592-019-01433-3. [DOI] [PubMed] [Google Scholar]
- 12.García de la Torre N., Rubio M.A., Bordiú E., Cabrerizo L., Aparicio E., Hernández C., Sánchez-Pernaute A., Díez-Valladares L., Torres A.J., Puente M., et al. Effects of weight loss after bariatric surgery for morbid obesity on vascular endothelial growth factor-A, adipocytokines, and insulin. J. Clin. Endocrinol. Metab. 2008;93:4276–4281. doi: 10.1210/jc.2007-1370. [DOI] [PubMed] [Google Scholar]
- 13.Veronelli A., Laneri M., Ranieri R., Koprivec D., Vardaro D., Paganelli M., Folli F., Pontiroli A.E. White blood cells in obesity and diabetes: Effects of weight loss and normalization of glucose metabolism. Diabetes Care. 2004;27:2501–2502. doi: 10.2337/diacare.27.10.2501. [DOI] [PubMed] [Google Scholar]
- 14.Boido A., Ceriani V., Cetta F., Lombardi F., Pontiroli A.E. Bariatric surgery and prevention of cardiovascular events and mortality in morbid obesity: Mechanisms of action and choice of surgery. Nutr. Metab. Cardiovasc. Dis. 2015;25:437–443. doi: 10.1016/j.numecd.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Raaijmakers L.C., Pouwels S., Thomassen S.E., Nienhuijs S.W. Quality of life and bariatric surgery: A systematic review of short- and long-term results and comparison with community norms. Eur. J. Clin. Nutr. 2017;71:441–449. doi: 10.1038/ejcn.2016.198. [DOI] [PubMed] [Google Scholar]
- 16.Wasmund S.L., Owan T., Yanowitz F.G., Adams T.D., Hunt S.C., Hamdan M.H., Litwin S.E. Improved heart rate recovery after marked weight loss induced by gastric bypass surgery: Two-year follow up in the Utah Obesity Study. Heart Rhythm. 2011;8:84–90. doi: 10.1016/j.hrthm.2010.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pontiroli A.E. Heart rate and sympathetic activity after obesity surgery. Heart Rhythm. 2011;8:e1. doi: 10.1016/j.hrthm.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 18.Aldaas O.M., Lupercio F., Han F.T., Hoffmayer K.S., Krummen D., Ho G., Raissi F., Birgersdotter-Green U., Feld G.K., Hsu J.C. Meta-analysis of Effect of Modest (≥10%) Weight Loss in Management of Overweight and Obese Patients with Atrial Fibrillation. Am. J. Cardiol. 2019;124:1568–1574. doi: 10.1016/j.amjcard.2019.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park D.Y., An S., Murthi M., Kattoor A.J., Kaur A., Ravi V., Huang H.D., Vij A. Effect of weight loss on recurrence of atrial fibrillation after ablative therapy: A systematic review and meta-analysis. J. Interv. Card. Electrophysiol. 2022;64:763–771. doi: 10.1007/s10840-022-01168-2. [DOI] [PubMed] [Google Scholar]
- 20.Chokesuwattanaskul R., Thongprayoon C., Bathini T., Sharma K., Watthanasuntorn K., Lertjitbanjong P., Pachariyanon P., Prechawat S., Mao M.A., Torres-Ortiz A., et al. Incident atrial fibrillation in patients undergoing bariatric surgery: A systematic review and meta-analysis. Intern. Med. J. 2020;50:810–817. doi: 10.1111/imj.14436. [DOI] [PubMed] [Google Scholar]
- 21.Van Veldhuisen S.L., Gorter T.M., van Woerden G., de Boer R.A., Rienstra M., Hazebroek E.J., van Veldhuisen D.J. Bariatric surgery and cardiovascular disease: A systematic review and meta-analysis. Eur. Heart J. 2022;43:1955–1969. doi: 10.1093/eurheartj/ehac071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yuan H., Medina-Inojosa J.R., Lopez-Jimenez F., Miranda W.R., Collazo-Clavell M.L., Sarr M.G., Chamberlain A.M., Hodge D.O., Bailey K.R., Wang Y., et al. The Long-Term Impact of Bariatric Surgery on Development of Atrial Fibrillation and Cardiovascular Events in Obese Patients: An Historical Cohort Study. Front. Cardiovasc. Med. 2021;8:647118. doi: 10.3389/fcvm.2021.647118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doumouras A.G., Wong J.A., Paterson J.M., Lee Y., Sivapathasundaram B., Tarride J.E., Thabane L., Hong D., Yusuf S., Anvari M. Bariatric Surgery and Cardiovascular Outcomes in Patients with Obesity and Cardiovascular Disease: A Population-Based Retrospective Cohort Study. Circulation. 2021;143:1468–1480. doi: 10.1161/CIRCULATIONAHA.120.052386. [DOI] [PubMed] [Google Scholar]
- 24.Moher D.A., Tetzlaff J., Altman D.G. PRISMA group preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jamaly S., Carlsson L., Peltonen M., Jacobson P., Sjöström L., Karason K. Bariatric Surgery and the Risk of New-Onset Atrial Fibrillation in Swedish Obese Subjects. J. Am. Coll. Cardiol. 2016;68:2497–2504. doi: 10.1016/j.jacc.2016.09.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lynch K.T., Mehaffey J.H., Hawkins R.B., Hassinger T.E., Hallowell P.T., Kirby J.L. Bariatric surgery reduces incidence of atrial fibrillation: A propensity score-matched analysis. Surg. Obes. Relat. Dis. 2019;15:279–285. doi: 10.1016/j.soard.2018.11.021. [DOI] [PubMed] [Google Scholar]
- 27.Aminian A., Zajichek A., Arterburn D.E., Wolski K.E., Brethauer S.A., Schauer P.R., Kattan M.W., Nissen S.E. Association of metabolic surgery with major adverse cardiovascular outcomes in patients with type 2 diabetes and obesity. JAMA. 2019;322:1271–1282. doi: 10.1001/jama.2019.14231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh P., Subramanian A., Adderley N., Gokhale K., Singhal R., Bellary S., Nirantharakumar K., Tahrani A.A. Impact of bariatric surgery on cardiovascular outcomes and mortality: A population-based cohort study. Br. J. Surg. 2020;107:432–442. doi: 10.1002/bjs.11433. [DOI] [PubMed] [Google Scholar]
- 29.Srivatsa U.N., Malhotra P., Zhang X.J., Beri N., Xing G., Brunson A., Ali M., Fan D., Pezeshkian N., Chiamvimonvat N., et al. Bariatric surgery to aLleviate OCcurrence of Atrial Fibrillation Hospitalization-BLOC-AF. Heart Rhythm O2. 2020;1:96–102. doi: 10.1016/j.hroo.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moussa O., Ardissino M., Eichhorn C., Reddy R.K., Khan O., Ziprin P., Darzi A., Collins P., Purkayastha S. Atrial fibrillation and obesity: Long-term incidence and outcomes after bariatric surgery. Eur. J. Prev. Cardiol. 2021;28:e22–e24. doi: 10.1177/2047487320904515. [DOI] [PubMed] [Google Scholar]
- 31.Höskuldsdóttir G., Sattar N., Miftaraj M., Näslund I., Ottosson J., Franzén S., Svensson A.M., Eliasson B. Potential Effects of Bariatric Surgery on the Incidence of Heart Failure and Atrial Fibrillation in Patients With Type 2 Diabetes Mellitus and Obesity and on Mortality in Patients With Preexisting Heart Failure: A Nationwide, Matched, Observational Cohort Study. J. Am. Heart Assoc. 2021;10:e019323. doi: 10.1161/JAHA.120.019323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rassen J.A., Murk W., Schneeweiss S. Real-world evidence of bariatric surgery and cardiovascular benefits using electronic health records data: A lesson in bias. Diabetes Obes. Metab. 2021;23:1453–1462. doi: 10.1111/dom.14338. [DOI] [PubMed] [Google Scholar]
- 33.Näslund E., Stenberg E., Hofmann R., Ottosson J., Sundbom M., Marsk R., Svensson P., Szummer K., Jernberg T. Association of Metabolic Surgery With Major Adverse Cardiovascular Outcomes in Patients With Previous Myocardial Infarction and Severe Obesity: A Nationwide Cohort Study. Circulation. 2021;143:1458–1467. doi: 10.1161/CIRCULATIONAHA.120.048585. [DOI] [PubMed] [Google Scholar]
- 34.Wells G.A., Shea B., Higgins J.P., Sterne J., Tugwell P., Reeves B.C. Checklists of methodological issues for review authors to consider when including non-randomized studies in systematic reviews. Res. Synth. Methods. 2013;4:63–77. doi: 10.1002/jrsm.1077. [DOI] [PubMed] [Google Scholar]
- 35.Hartung J., Knapp G. A refined method for the meta-analysis of controlled clinical trials with binary outcome. Stat. Med. 2001;20:3875–3889. doi: 10.1002/sim.1009. [DOI] [PubMed] [Google Scholar]
- 36.Higgins J.P., Thompson S.G., Spiegelhalter D.J. A re-evaluation of random-effects meta-analysis. J. R. Stat. Soc. Ser. A Stat. Soc. 2009;172:137–159. doi: 10.1111/j.1467-985X.2008.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim S.Y., Park J.E., Lee Y.J., Seo H.-J., Sheen S.-S., Hahn S., Jang B.-H., Son H.-J. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J. Clin. Epidemiol. 2013;66:408–414. doi: 10.1016/j.jclinepi.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 38.Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baujat B., Mahé C., Pignon J.P., Hill C. A graphical method for exploring heterogeneity in meta-analyses: Application to a meta-analysis of 65 trials. Stat. Med. 2002;21:2641–2652. doi: 10.1002/sim.1221. [DOI] [PubMed] [Google Scholar]
- 40.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ambrosio G., Camm A.J., Bassand J.P., Corbalan R., Kayani G., Carluccio E., Mantovani L.G., Virdone S., Kakkar A.K., GARFIELD-AF Investigators Characteristics, treatment, and outcomes of newly diagnosed atrial fibrillation patients with heart failure: GARFIELD-AF. ESC Heart Fail. 2021;8:1139–1149. doi: 10.1002/ehf2.13156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Neefs J., Boekholdt S.M., Khaw K.T., Luben R., Pfister R., Wareham N.J., Meulendijks E.R., Sanders P., de Groot J.R. Body mass index and body fat distribution and new-onset atrial fibrillation: Substudy of the European Prospective Investigation into Cancer and Nutrition in Norfolk (EPIC-Norfolk) study. Nutr. Metab. Cardiovasc. Dis. 2019;29:692–700. doi: 10.1016/j.numecd.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Powell-Wiley T.M., Poirier P., Burke L.E., Després J.P., Gordon-Larsen P., Lavie C.J., Lear S.A., Ndumele C.E., Neeland I.J., Sanders P., et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation. 2021;143:e984–e1010. doi: 10.1161/CIR.0000000000000973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nuijten M.A.H., Eijsvogels T.M.H., Monpellier V.M., Janssen I.M.C., Hazebroek E.J., Hopman M.T.E. The magnitude and progress of lean body mass, fat-free mass, and skeletal muscle mass loss following bariatric surgery: A systematic review and meta-analysis. Obes. Rev. 2022;23:e13370. doi: 10.1111/obr.13370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Opacic D., van Bragt K.A., Nasrallah H.M., Schotten U., Verheule S. Atrial metabolism and tissue perfusion as determinants of electrical and structural remodelling in atrial fibrillation. Cardiovasc. Res. 2016;109:527–541. doi: 10.1093/cvr/cvw007. [DOI] [PubMed] [Google Scholar]
- 46.Dall’Asta C., Paganelli M., Morabito A., Vedani P., Barbieri M., Paolisso G., Folli F., Pontiroli A.E. Weight loss through gastric banding: Effects on TSH and thyroid hormones in obese subjects with normal thyroid function. Obesity. 2010;18:854–857. doi: 10.1038/oby.2009.320. [DOI] [PubMed] [Google Scholar]
- 47.Abed H.S., Nelson A.J., Richardson J.D., Worthley S.G., Vincent A., Wittert G.A., Leong D.P. Impact of weight reduction on pericardial adipose tissue and cardiac structure in patients with atrial fibrillation. Am. Heart J. 2015;169:655–662.e2. doi: 10.1016/j.ahj.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 48.IntHout J., Ioannidis J.P., Borm G.F. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med. Res. Methodol. 2014;14:25. doi: 10.1186/1471-2288-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Felsch M., Beckmann L., Bender R., Kuss O., Skipka G., Mathes T. Performance of several types of beta-binomial models in comparison to standard approaches for meta-analyses with very few studies. BMC Med. Res. Methodol. 2022;22:319. doi: 10.1186/s12874-022-01779-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jones N.R., Taylor K.S., Taylor C.J., Aveyard P. Weight change and the risk of incident atrial fibrillation: A systematic review and meta-analysis. Heart. 2019;105:1799–1805. doi: 10.1136/heartjnl-2019-314931. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available from the corresponding author on the basis of reasonable request.