Abstract
Lactobacillus plantarum (L. plantarum) is a probiotic that has emerged as novel therapeutic agents for managing various diseases, such as cancer, atopic dermatitis, inflammatory bowel disease, and infections. In this study, we investigated the potential mechanisms underlying the anticancer effect of the metabolites of L. plantarum. We cultured L. plantarum cells to obtain their metabolites, created several dilutions, and used these solutions to treat human colonic Caco-2 cells. Our results showed a 10% dilution of L. plantarum metabolites decreased cell viability and reduced the expression of autophagy-related proteins. Moreover, we found co-treatment with L. plantarum metabolites and chloroquine, a known autophagy inhibitor, had a synergistic effect on cytotoxicity and downregulation of autophagy-related protein expression. In conclusion, we showed the metabolites from the probiotic, L. plantarum, work synergistically with chloroquine in killing Caco-2 cells and downregulating the expression of autophagy-related proteins, suggesting the involvement of autophagy, rather than apoptosis, in their cytotoxic effect. Hence, this study provides new insights into new therapeutic methods via inhibiting autophagy.
Keywords: probiotics, metabolites, Lactobacillus, chloroquine, autophagy, tetramethylrhodamine ethyl ester (TMRE)
1. Introduction
Colorectal cancer (CRC) is one of the most common types of cancer worldwide in 2020, ranking third in incidence and second in mortality [1,2]. The rising prevalence of CRC is caused by increased meat intake, decreased physical activity, excessive alcohol consumption, and continuous smoking [3,4]. The main causes of death due to CRC are the recurrence and metastasis of cancer cells [5,6,7].
Autophagy is a catabolic recycling process where unnecessary and damaged cellular components are removed, and hence, it is essential for maintaining cellular homeostasis [8,9,10]. Autophagy can be divided into macroautophagy, microautophagy, chaperone-mediated autophagy, and crinophagy [11], with macroautophagy being the most well-characterized. Autophagosomes fuse with lysosomes to form autolysosomes after trapping cellular components for degradation and recycling as substrates in many other places. Therefore, impaired autophagy pathways can affect cellular functions and contribute to the pathogenesis of many diseases [12,13,14].
Lactobacillus plantarum (L. plantarum), a rod-shaped gram-positive bacterium, is a probiotic that has various beneficial effects on its hosts [15]. In recent decades, with increasing interest in probiotics, L. plantarum and its metabolites have emerged as novel therapeutic agents for managing various diseases, such as cancer, atopic dermatitis, inflammatory bowel disease, and infections [16,17,18,19,20,21]. In particular, owing to high mortality rates and globally rising incidences, elucidating the anticancer effects of L. plantarum and its metabolites is important for developing novel therapeutics for the treatment of various cancers.
The anticancer effects and its underlying mechanisms of L. plantarum and other Lactobacillus species have been previously reported [22,23,24,25]. L. salivarin REN suppressed the upregulation of COX-2 expression and therefore, decreased the rate of oral carcinogenesis [26,27]. L. hilgardii also showed an anticancer effect via inducing apoptosis pathways [22]. Moreover, Lactobacillus species are known to regulate autophagy. For instance, L. casei ATC 393, L. rhamnosus GG, and L. reuteri ZJ617 have been reported to regulate autophagy [26]. L. casei ATC 393 alleviated dysregulated autophagy induced by H2O2 via activating the Nrf2-signaling pathway and reducing MMP reduction and intestinal permeability [28]. L. rhamnosus GG increased phosphorylation of EGFR and Akt and decreased autophagy activity in Salmonella Infantis-infected conditions [29]. L. rhamnosus GG also increased T cell maturation and cell proliferation and thus, downregulated the production of IL-2, IL-4, and IL-10 [30]. L. reuteri ZJ617 increased the tight junction and decreased MAPK, NFκB, and autophagy-signaling pathways [31].
Many studies have reported L. plantarum effectively suppressed the growth of resistant CRC cells [25,32]. Most of the mechanisms that explain the anticancer effect of L. plantarum have been with a focus on apoptosis. However, other Lactobacillus species have shown to regulate autophagy [22,33,34]. Therefore, we hypothesized the anticancer effect of L. plantarum is related to autophagy regulation. The objective of this study is to investigate the autophagy-related anticancer effect of L. plantarum metabolites in colorectal adenocarcinoma cells. We aimed to test whether L. plantarum metabolites reduce the viability of colon cancer cells and to investigate the inhibitory effects of L. plantarum metabolites on the expression of autophagy-related proteins and mitochondrial dysfunction.
2. Results
2.1. L. plantarum Metabolites Reduced the Cell Viability of Caco-2 Human Colorectal Cancer Cells
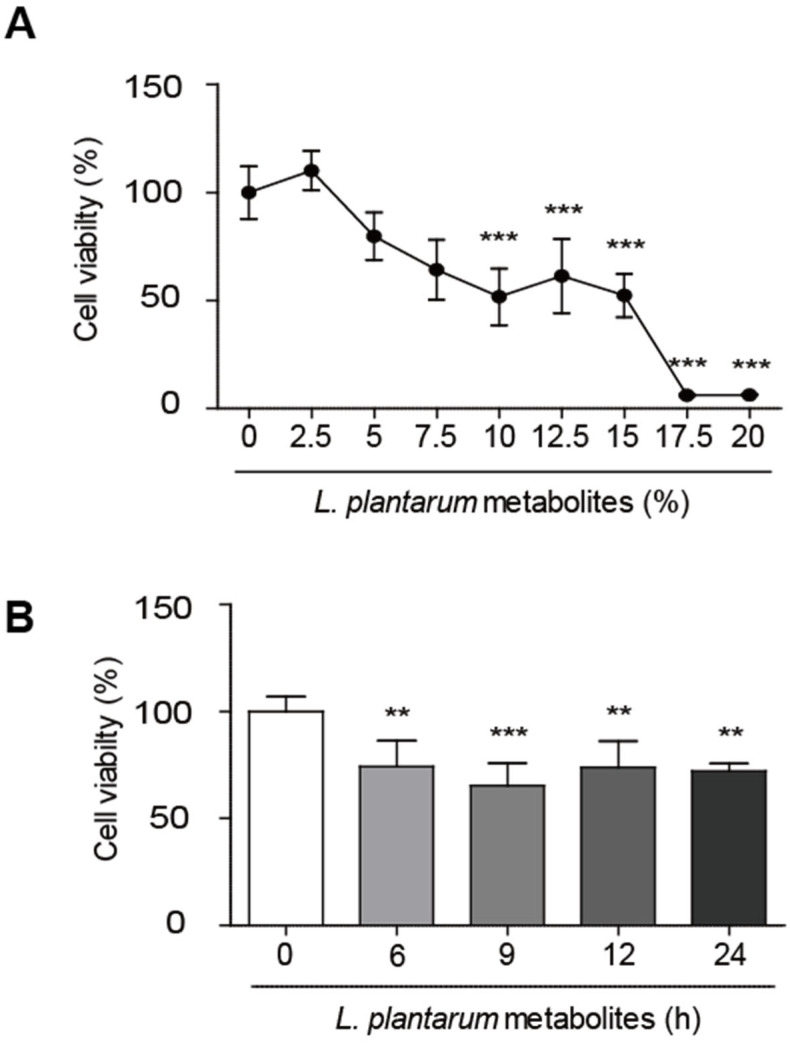
An MTT assay was used to investigate the effects of varying concentrations of L. plantarum metabolites on the viability of Caco-2 cells. L. plantarum metabolites were diluted with Caco-2 culture media without antibiotics at various ratios, and Caco-2 cells were treated with the diluted L. plantarum metabolites for 24 h. As shown in Figure 1A, L. plantarum metabolites exhibited no cytotoxicity at concentrations up to 5%. Cell viability was reduced significantly from 10% dilution of L. plantarum metabolites, and IC50 of L. plantarum metabolites was about 10.03%. Caco-2 cells were also treated with L. plantarum metabolites from 6 h to 24 h; as seen in Figure 1B; cell viability was significantly decreased in all L. plantarum metabolites-treated groups.
Figure 1.
Lactobacillus plantarum metabolites decreased the viability of human colon cancer cells. (A) Caco-2 cells were treated with L. plantarum metabolites at various concentrations from 2.5% to 20% for 24 h. Cell viability was detected using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) (0.5 mg/mL) assays. (B) Caco-2 cells were treated with a 10% dilution of L. plantarum metabolites from 6 h to 24 h. Cell viability was detected using an MTT assay. Data are presented as the mean ± SD. ** p < 0.01 and *** p < 0.001 compared to untreated control; one-way ANOVA was followed by Tukey’s post hoc test.
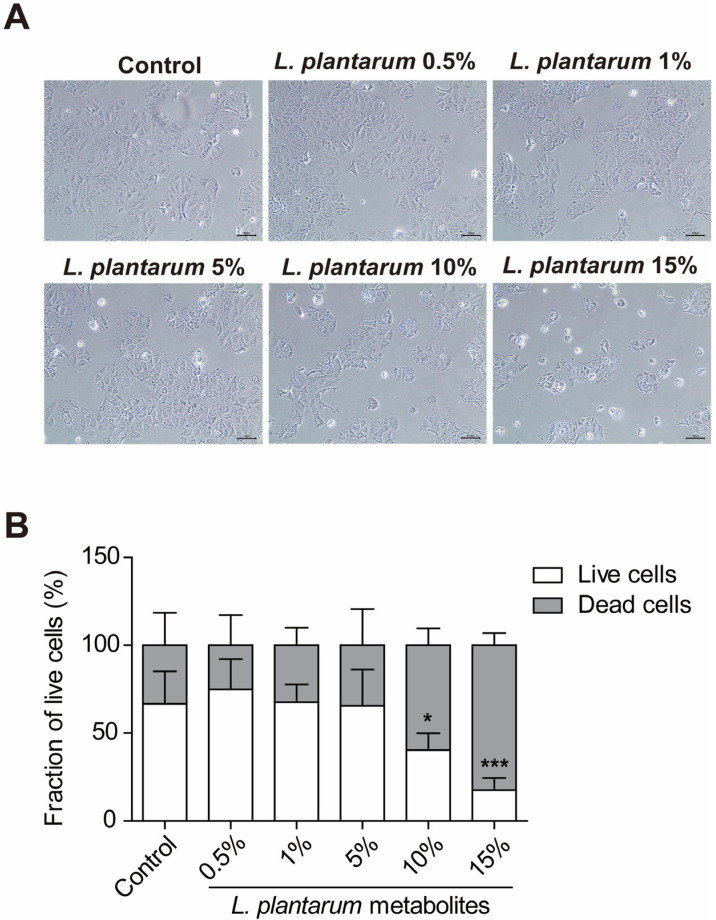
Cell viability was also analyzed using microscopic imaging, as shown in Figure 2A (100× magnification). Caco-2 cells were treated with various concentrations of L. plantarum metabolites for 24 h again. There were no noticeable differences in the 5% L. plantarum metabolite-treated group compared to the untreated control group. However, the fraction of live cells decreased in the 10% L. plantarum metabolite-treated group significantly, and almost all cells died after treatment with 15% L. plantarum metabolites, as seen in Figure 2B. Therefore, we set the L. plantarum metabolite concentration to 10% in the succeeding experiments.
Figure 2.
Lactobacillus plantarum metabolites decreased the survival of colon cancer cells in a concentration-dependent manner. Caco-2 cells were treated with L. plantarum metabolites at concentrations ranging from 0.5% to 15% for 24 h. (A) All images were obtained using an MIC-Eyecam-3Mpixel microscope digital camera at 100× magnification. Scale bar, 100 μm. (B) The graph indicated the fraction of live cells. Data shown are mean ± SD. * p < 0.05, *** p < 0.001 compared to live cells with control group with two-way ANOVA.
2.2. L. plantarum Metabolites Downregulated the Expression of Autophagy Markers in Caco-2 Cells
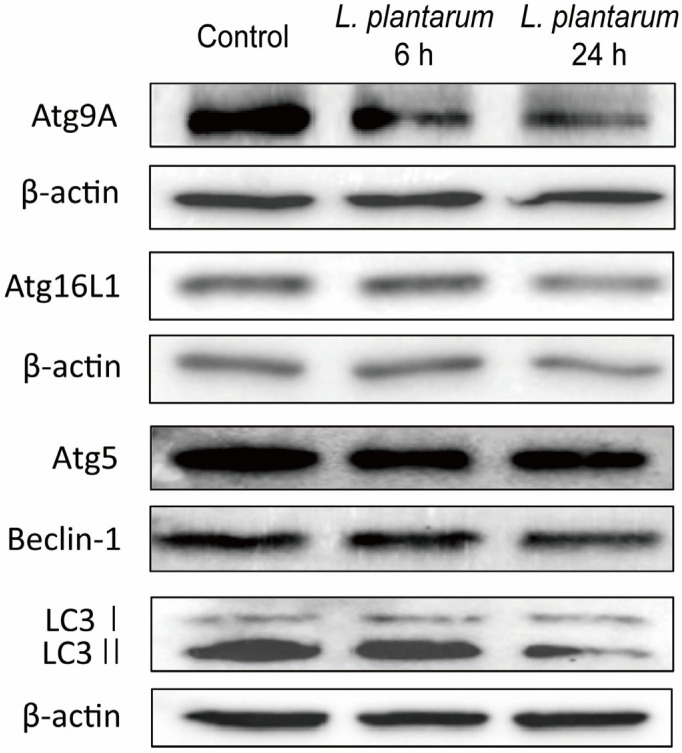
The expression of autophagy markers, such as Atg9A, Atg16L1, Atg5, Beclin-1, and LC3 I/II, was determined to investigate the effect of L. plantarum metabolites on autophagy. Western blot analyses showed the levels of Atg9A, Atg16L1, Atg5, and Beclin-1 decreased following treatment with 10% L. plantarum metabolites. The expression of autophagy markers was further reduced in the 24 h-treated group than in the 6 h-treated group. The accumulation of LC3 to LC3 II was decreased in the group treated with L. plantarum metabolites for 24 h (Figure 3).
Figure 3.
Lactobacillus plantarum metabolites suppressed the expression of autophagy-related proteins in colon cancer cells. Caco-2 cells were treated with a 10% dilution of L. plantarum metabolites for 6 or 24 h. Representative western blot band images of Atg9A, Atg16L1, Atg5, Beclin-1, LC3 I/II, and β-actin expression in Caco-2 cells are presented. β-actin is used as a loading control.
2.3. L. plantarum Metabolites Enhanced the Autophagy Inhibition Ability of CQ in Caco-2 Cells
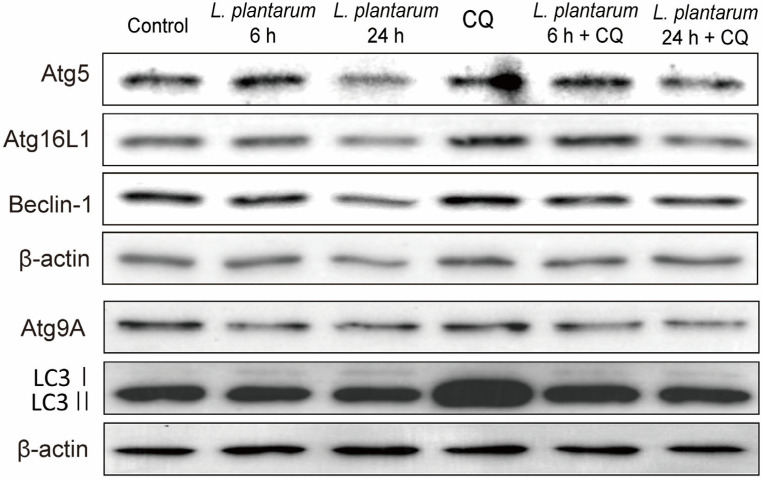
To verify the inhibitory effect of the L. plantarum metabolites on autophagy, we used chloroquine (CQ), a well-known autophagy inhibitor, and measured the expression levels of Atg9A, LC3 I/II, Atg5, Atg16L1, and Beclin-1. During autophagy, the autophagosome engulfs cytoplasmic components, and the cytoplasmic form of LC3 I is transformed into LC3 II, which is then recruited to the autophagosome membrane. When the autophagosome fuses with the lysosome and components within the autophagosome are degraded, LC3 II is also degraded [35]. Atg5 is involved in the expansion of the phagophoric membrane in autophagic vesicles and after activation, forms a complex with Atg16L1 to perform its function. Atg5 is also required for the formation of the LC3 I/II complex [36]. Atg9A contributes to membrane growth of the autophagosome [37]. Beclin-1 plays an important role in the regulation of autophagy and apoptosis by interacting with Bcl-2 or PI3K [38].
As before, Caco-2 cells were treated with L. plantarum metabolites for 6 or 24 h, and 100 μM CQ was added 45 min before harvesting the cells. CQ is known to block autolysosome formation, leading to an increase in LC3 II and other autophagy marker proteins, while L. plantarum metabolites decreased autophagy protein expression (Figure 3 and Figure 4). Co-treatment with L. plantarum metabolites and CQ may balance the protein expression levels compared to L. plantarum metabolites alone. The protein level of Atg9A decreased in the L. plantarum metabolites and CQ co-treatment groups compared to L. plantarum metabolites alone. The expression levels of Atg5, Atg16L1, and Beclin-1 slightly decreased in the L. plantarum metabolites alone treatment group and the L. plantarum metabolites and CQ co-treatment groups. CQ-mediated LC3 II accumulation decreased in the L. plantarum metabolites and CQ co-treatment groups (Figure 4).
Figure 4.
Co-treatment with Lactobacillus plantarum metabolites further suppressed the expression of autophagy-related proteins in colon cancer cells than treatment with chloroquine (CQ) alone. Caco-2 cells were pretreated with a 10% dilution of L. plantarum metabolites for 6 or 24 h and then treated with CQ (100 μM) for 45 min before harvesting the cell extracts. The protein levels of Atg9A, LC3 I/II, Atg5, Atg16L1, Beclin-1, and β-actin were then observed using western blot analysis. β-actin is used as a loading control.
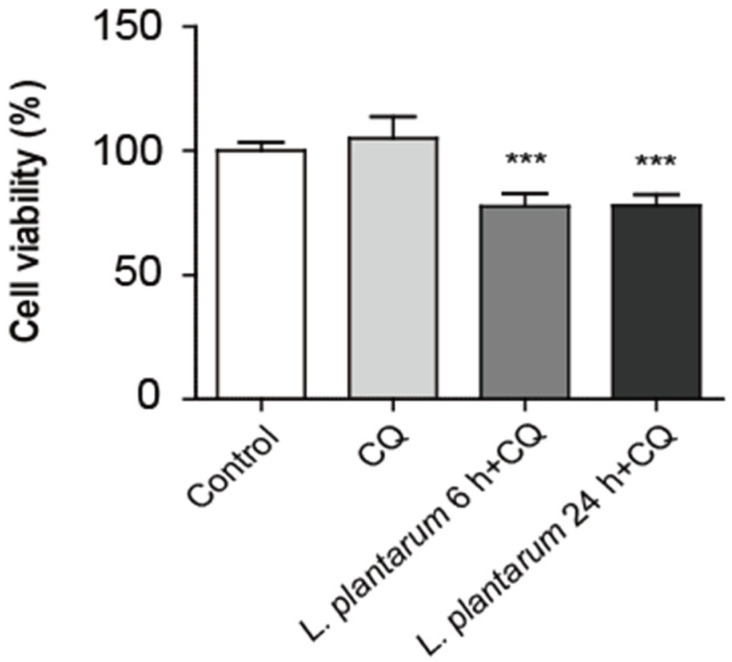
2.4. Co-Treatment with L. plantarum Metabolites and CQ Decreased Caco-2 Cell Viability More than CQ Treatment Alone
The MTT assay was used to determine the difference between the L. plantarum metabolites treatment time and the effects of CQ treatment on the viability of Caco-2 cells. Here, 10% L. plantarum metabolites and 100 μM CQ were used to treat Caco-2 cells for 45 min. There was no significant difference between the control and CQ treatment-only groups. Cell viability was decreased upon co-treatment with L. plantarum metabolites and CQ, regardless of treatment time (Figure 5).
Figure 5.
Co-treatment with Lactobacillus plantarum metabolites and CQ further decreased the viability of colon cancer cells than treatment with CQ alone. Caco-2 cells were treated with a 10% dilution of L. plantarum metabolites for 6 or 24 h and then treated with CQ (100 μM) for 45 min before harvesting the cells. Cell viability was detected using an MTT assay. Data are presented as the mean ± SD. *** p < 0.001; one-way ANOVA was followed by Tukey’s post hoc test.
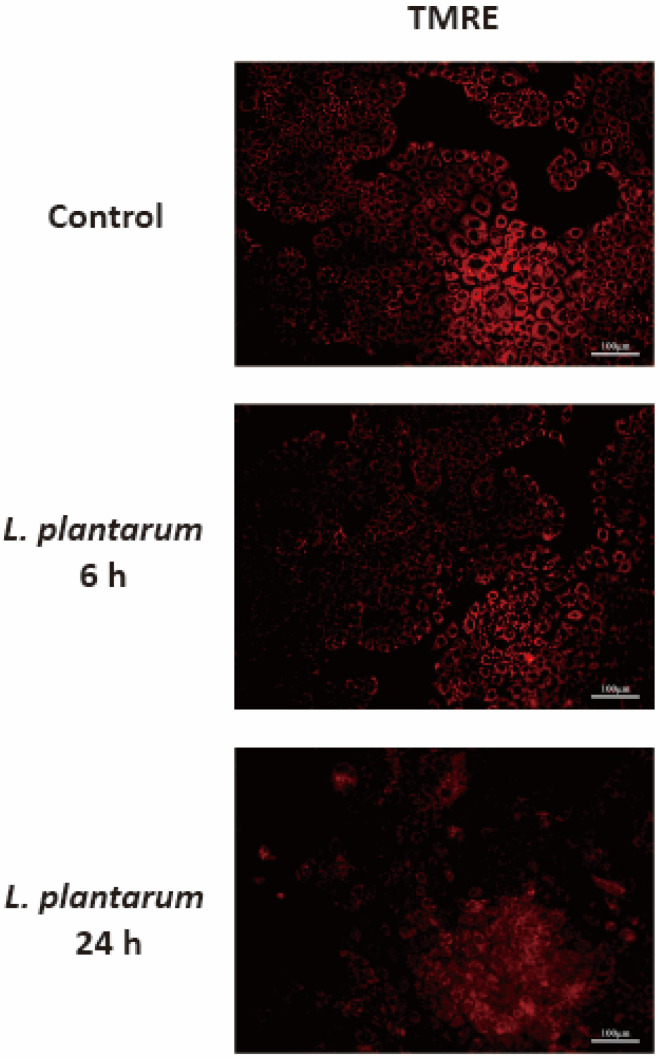
2.5. L. plantarum Metabolites Induced Mitochondrial Dysfunction in Caco-2 Cells
Impaired autophagic activity is related to mitochondrial dysfunction. tetramethylrhodamine ethyl ester (TMRE) staining was performed to investigate whether autophagy inhibition induced by L. plantarum metabolites was associated with mitochondrial dysfunction. The mitochondrial membrane potential of Caco-2 cells was determined using a fluorescence microscopy. The intensity of TMRE was reduced in cells treated with L. plantarum metabolites for 6 h and further reduced in the group treated for 24 h. This implies the mitochondrial membranes of Caco-2 cells were depolarized by the L. plantarum metabolites (Figure 6).
Figure 6.
Lactobacillus plantarum metabolites induced mitochondrial dysfunction in colon cancer cells. Caco-2 cells were treated with L. plantarum metabolites for 6 or 24 h and then stained with tetramethylrhodamine ethyl ester (TMRE, 0.05 μM) for 20 min. The presented images were obtained using a fluorescence microscopy with the same conditions and settings. Scale bar, 100 μm.
3. Discussion
Metabolic shift is a major hallmark of cancer [39]. Cancer cells require large amounts of ATP and change their metabolism from oxidative phosphorylation to aerobic glycolysis [40,41]. Metabolic reprogramming in cancer cells is characterized by increased glucose uptake and lactate production, called the “Warburg effect” [42,43]. Reportedly, metabolic reprogramming is also related to chemoresistance, with some reports showing that targeting altered metabolism is effective in overcoming chemoresistance [44,45,46,47]. The chemotherapeutic agent 5-fluorouracil (5-FU) is the most widely used first-line treatment for CRC and is used as a monotherapy or in combination with other anticancer drugs, such as oxaliplatin or irinotecan [48,49]. It has been shown 5-FU is an effective CRC treatment; however, it can induce drug resistance as a side effect [50]. CRC cells that are 5-FU-resistant show cancer stem-cell-like properties and can induce early tumor recurrence or metastasis [51,52]. Therefore, novel therapeutic strategies are needed to overcome chemoresistance and increase the efficacy of anticancer drugs [53,54,55].
The relieving effect of L. plantarum on intestinal inflammation has been reported in other studies [56,57]. The gene expression and production of anti-inflammatory factors (IL-10, TGF-β1, and TGF-β2) increased in Caco-2 cells and a DSS-induced mouse model [58,59]. L. plantarum reduced the gene expression and production of pro-inflammatory cytokines (IL-1β, IL-6, TNF-α, MPO, and IFN-γ) and suppressed inflammatory responses to normalize the immune barrier [60]. Additionally, in vivo, L. plantarum administration reduced the incidence of DSS-induced colitis. In clinical, L. plantarum uptake maintained the integrity and permeability of intestinal epithelial cells and increased mucin secretion from goblet cells [61]. Therefore, L. plantarum reduced chronic mucosal inflammation and ulcerative colitis symptoms. Chronic intestinal inflammation is important because chronic intestinal inflammation can lead to the development of CRC [62]. Short-chain fatty acids (SCFAs) are also suggested as the main cause for the effect of relieving intestinal inflammation of L. plantarum. SCFAs are metabolites of gut microbiota, and L. plantarum can also produce SCFAs. SCFAs have immunomodulatory effects and can reduce the expression of pro-inflammatory factors [63]. The reduction of inflammatory responses by SCFAs can effectively contribute to alleviating the symptoms of ulcerative colitis and CRC.
L. plantarum and its metabolites have an inhibitory effect on chemoresistant CRC cells, especially 5-FU-resistant CRC cells [32,51,53,54]. L. plantarum can exhibit anticancer effects by increasing the cytotoxicity and death of CRC cells or reducing NLRP3 and ERK phosphorylation. L. plantarum metabolites can reverse the altered metabolism in cancer, including the reversion of transformed glycolysis to normal glycolysis [6]. Cancer cells require more ATP than normal cells; therefore, their glycolytic rate increases, and they can also undergo aerobic glycolysis [64]. Altered glycolysis increases glucose uptake and lactate production [42] and can promote acidic conditions, one of the hallmarks of cancer as well as chemoresistance [45,65,66,67,68]. However, L. plantarum metabolites can reverse altered glycolysis mechanisms, thereby decreasing cancer cell proliferation, increasing apoptosis, and decreasing chemoresistance [53,54]. Thus, L. plantarum metabolites can induce therapeutic effects and prevent cancer recurrence.
There have been some reports on the anticancer effects of L. plantarum and other Lactobacillus strains. For instance, L. salivarin REN can decrease the rate of oral carcinogenesis. L. casei ATC 393, L. rhamnosus GG, and L. reuteri ZJ617 have also been reported to show anticancer effects, which are elicited via autophagy-related mechanisms rather than apoptosis [26,28,29,30,31,69]. Many studies reported L. plantarum effectively suppresses resistant CRC cells. Most of the mechanisms that explain CRC cell suppression have been described with a focus on apoptosis. Therefore, we conducted experiments focusing on autophagy.
In this study, L. plantarum metabolites exhibited cytotoxicity from 10% dilution against colon cancer cell lines, as evidenced by the MTT assay and imaging analysis results. Additionally, a 10% dilution of L. plantarum metabolites significantly decreased colon cancer cell viability after treatment from 6 h to 24 h. Treatment with L. plantarum metabolites for 6 or 24 h also reduced the expression of autophagy-related proteins, such as Atg9, Atg5, Atg16L1, and Beclin-1. Upon treatment with CQ, a well-known autophagy inhibitor, L. plantarum metabolites further reduced expression levels of all four proteins of interest as compared to treatment with CQ alone. Treatment with CQ alone did not decrease the viability of colon cancer cells; however, co-treatment with L. plantarum metabolites and CQ significantly decreased cell viability. Using TMRE staining, L. plantarum metabolites were shown to depolarize the mitochondrial membranes of colon cancer cells. Further experiments are warranted to investigate the precise role of L. plantarum metabolites in each step of the autophagy process and the alteration of autophagy marker expression over time. In addition, it is recommended that L. plantarum metabolites are tested and verified in chemoresistant CRC cells.
Whether autophagy promotes or suppresses the growth of cancer cells has not yet been elucidated [68]; however, reports that autophagy inhibition can suppress cancer are highly prevalent [67,70,71,72]. Autophagy can provide the necessary nutrients and energy to cancer cells and increase angiogenesis [73,74]. Cancer cells can easily overcome stress conditions and increase their rate of metastasis and invasion [75,76]. CQ is a well-known autophagy inhibitor, but it is difficult to be taken up by cells in an acidic tumor environment [77]. Therefore, L. plantarum is recommended as a novel agent to overcome chemoresistance by inhibiting autophagy. Moreover, L. plantarum metabolites can increase the suppressive activity of anticancer agents.
Autophagy is a complex process composed of several sequential steps [78]. Our western blot analysis data suggest L. plantarum metabolites and co-treatment with CQ regulate different stages of autophagy. CQ is known to impede the formation of autolysosome, causing an increase in LC3-II and other autophagy marker proteins. Our findings indicate an elevated expression of LC3-II and other autophagy makers after CQ treatment. On the other hand, L. plantarum metabolites appear to obstruct phagophore and autophagosome formation, including the steps of vesicle nucleation and vesicle elongation, resulting in decreased expression of autophagy proteins. Co-treatment of L. plantarum metabolites and CQ may balance the protein expression levels compared to treatment with L. plantarum metabolites alone.
CQ has previously been shown to enhance the sensitivity of the anticancer drug cisplatin in cholangiocarcinoma cells by increasing intracellular, particularly mitochondrial, reactive oxygen species mediated by glucose metabolism and reducing the antioxidant capacity of cells [79]. Therefore, it is possible that CQ may amplify the sensitivity of L. plantarum metabolites in cancer cells with high autophagy flow. While probiotics, such as L. plantarum, are utilized in anticancer therapies, their modes of action are not yet fully understood. Our study suggests a new mechanism by which L. plantarum metabolites suppress autophagy to produce an anticancer effect. In the future, we aim to further investigate the exact role of L. plantarum metabolites in each step of the autophagy process and to study the alteration of autophagy marker expression over time.
In conclusion, our results demonstrate L. plantarum metabolites are effective agents for inhibiting autophagy in colon cancer cells as they decrease cell viability and downregulate autophagy-related protein expression. When co-treated with CQ, L. plantarum metabolites were more effective at downregulating autophagy-related protein expressions than CQ alone. In addition, L. plantarum metabolites caused mitochondrial dysfunction by depolarizing the mitochondrial membranes. Thus, L. plantarum metabolites have the ability to decrease autophagy activity in colonic cancer cells. These results suggest the autophagy inhibition effect of L. plantarum could be useful as a new agent for treating cancer cells.
4. Materials and Methods
4.1. Preparation of L. plantarum Metabolites
Lactobacillus plantarum (KCTC 3108) was purchased from the Korean Collection for Type Cultures (KCTC). To activate L. plantarum, the bacterial suspension was spread on BactoTM Lactobacilli MRS Broth (MRS, BD sciences, San Jose, CA, USA) agar plates and incubated at 37 °C for 24 h. After colony formation, a single colony was transferred to 20 mL fresh MRS medium and incubated at 37 °C for 24 h to obtain a preculture suspension. To obtain L. plantarum metabolites, 1 mL of the precultured bacterial suspension was transferred to 40 mL of fresh MRS medium and incubated at 37 °C for 96 h. Thereafter, the suspension was centrifuged (3000× g, 10 min, 4 °C), and the supernatant was filtered using a syringe filter (0.2 μm pore size, Sartorius, Goettingen, Germany). The filtered L. plantarum metabolites (brown-colored clear solution) were stored at 4 °C until further use.
4.2. Cell Culture and Treatment
The human colonic epithelial cell line, Caco-2 (Cat. No: HTB-37TM), was obtained from the American Type Culture Collection (Manassas, VA, USA). Cells were cultured in high-glucose (4.5 g/L) Dulbecco’s Modified Eagle’s Medium containing 10% heat-inactivated fetal bovine serum (Hyclone Laboratories, Logan, UT, USA) without any antibiotics at 37 °C in a 5% CO2 atmosphere. The L. plantarum metabolites were diluted at various ratios: 0.5:99.5 (0.5%), 1:99 (1%), 2.5:97.5 (2.5%), 5:95 (5%), 7.5:92.5 (7.5%), 10:90 (10%), 12.5:87.5 (12.5%), 15:85 (15%), 17.5:82.5 (17.55), and 20:80 (20%). The diluted L. plantarum metabolites were also treated for 6 h, 9 h, 12 h, and 24 h at a fixed 10% dilution rate.
Caco-2 cells were plated in T-25 flasks at 2 × 106 cells. The L. plantarum metabolites were diluted in media without antibiotics. CQ (Sigma-Aldrich, St. Louis, MO, USA) was diluted to a final concentration of 100 μM before use.
4.3. Cell Viability Assay
Caco-2 cells were treated with various concentrations of L. plantarum metabolites for 24 h. After incubation, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) solution (0.5 mg/mL, Sigma-Aldrich) was added to the cells, followed by incubation for 2 h at 37 °C in the dark. After forming purple formazan crystals, the spent medium was removed, and the cells were incubated with 100 μL of dimethyl sulfoxide until the purple formazan crystals were completely dissolved. The absorbance of each well was then measured at 570 nm using a Multiskan GO microplate spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA).
Cell viability was also investigated using microscopic imaging. Caco-2 cells were treated with the same concentrations of L. plantarum metabolites for 24 h. After incubation, the spent medium was removed, and the plate was observed and photographed using an MIC-Eyecam-3Mpixel Microscope Digital Camera (Eyecam, Clarity Medical Systems, Pleasanton, CA, USA). Scale bar, 100 μm. The total magnification of the images is 100×. The fraction of live cells was measured using Image J 1.47.
4.4. Western Blot Analysis
After treatment with L. plantarum metabolites for 24 h, total protein extracts from whole-cell lysates of Caco-2 cells were prepared in a protein extraction solution (ELPIS Biotech, Daejeon, Republic of Korea) containing a protease inhibitor (Sigma-Aldrich). The cell lysates were vortexed and incubated on ice for 1 h. The cell lysates were then centrifuged at 15,000× g for 20 min at 4 °C. Protein concentrations were measured using a Pierce BCA Protein Assay Kit (Thermo Fisher Scientific). The protein solutions were then boiled at 95 °C for 5 min, and equal amounts of protein were loaded and separated using a 10% sodium dodecyl sulfate-polyacrylamide gel. Proteins were transferred to polyvinylidene difluoride membranes using a 500 mA transfer membrane for 1 h. Membranes blocked with 5% skim milk in 1× Tris-buffered saline with Tween-20 buffer (TBS-T) for 1 h at room temperature (RT). After blocking, the membranes were incubated overnight at 4 °C with primary antibodies against the following molecules: autophagy-related 9A (Atg9A) (Cat. No: NB110-56893, 1:1000, Novus Biologicals, Englewood, CO, USA), autophagy-related 5 (Atg5) (Cat. No:12994, 1:1000, Cell Signaling Technology, Danvers, MA, USA), autophagy-related 16-like 1 (Atg16L1) (Cat. No: NB110-82384, 1:1000; Novus Biologicals), Beclin-1 (Cat. No:3945, 1:1000, Cell Signaling Technology), lipidated form of microtubule-associated protein 1A/1B-light chain 3 I/II (LC3 I/II) (Cat. No:12741, 1:1000; Cell Signaling Technology), and β-actin (Cat. No: A5441, 1:10,000, Sigma-Aldrich). The membranes were washed seven times with TBS-T and incubated with horseradish peroxidase-conjugated goat anti-rabbit antibody (1:10,000; Enzo Life Sciences, Farmingdale, NY, USA) for 2 h at RT. Finally, the proteins were detected using an enhanced chemiluminescence detection system (WesternBrightTM ECL, Advansta, Menol Park, CA, USA). Original images for blots are published in Supplementary Materials.
4.5. TMRE Staining
Caco-2 cells were seeded at a density of 2 × 105 cells in 35 mm confocal dishes. The cells were then treated with L. plantarum metabolites for 6 or 24 h. After incubation, the cells were treated with 0.05 μM TMRE (Cayman Chemical Company, Ann Arbor, MI, USA) for 20 min at 37 °C. After incubation, the cells were washed with cold phosphate-buffered saline (PBS) (pH 7.5) (Hyclone Inc., Logan, UT, USA). Images were obtained using a Nikon ECLIPSE TE 2000-U microscope (Nikon, Tokyo, Japan).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/molecules28041890/s1, Figure S1: Western blot analysis of Atg5, Atg9A, Atg16L1, Beclin-1, and LC3I/II proteins in Caco-2 cells treated with L. plantarum; Figure S2: Western blot analysis of Atg5, Atg9A, Atg16L1, Beclin-1, and LC3I/II proteins in Caco-2 cells treated with L. plantarum and CQ.
Author Contributions
Conceptualization, E.I., J.-W.Y. and S.H.R.; methodology, J.L. and S.P.H.; software, S.P.; validation, S.J., Y.K. and D.L.; formal analysis, S.J., Y.K. and D.L.; investigation, S.J., Y.K., S.P., D.L., J.L. and S.P.H.; data curation, S.J. and E.I.; writing—original draft preparation, S.J. and E.I.; writing—review and editing, S.J., Y.K., S.P., D.L., J.L., S.P.H., J.-W.Y., S.H.R. and E.I.; supervision, E.I. and J.-W.Y.; funding acquisition, J.-W.Y. and E.I. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was supported by 2021 BK21 FOUR Program of Pusan National University and by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. NRF-2022R1A2C2004340 to J.-W.Y.) and (No. NRF-2022R1A2C1012377 to E.I.).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Miller K.D., Nogueira L., Mariotto A.B., Rowland J.H., Yabroff K.R., Alfano C.M., Jemal A., Kramer J.L., Siegel R.L. Cancer treatment and survivorship statistics, 2019. CA A Cancer J. Clin. 2019;69:7–34. doi: 10.3322/caac.21565. [DOI] [PubMed] [Google Scholar]
- 3.Arnold M., Abnet C.C., Neale R.E., Vignat J., Giovannucci E.L., McGlynn K.A., Bray F. Global Burden of 5 Major Types of Gastrointestinal Cancer. Gastroenterology. 2020;159:335–349. doi: 10.1053/j.gastro.2020.02.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arnold M., Sierra M.S., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683–691. doi: 10.1136/gutjnl-2015-310912. [DOI] [PubMed] [Google Scholar]
- 5.Hull M.A., Rees C.J., Sharp L., Koo S. A risk-stratified approach to colorectal cancer prevention and diagnosis. Nature reviews. Gastroenterol. Hepatol. 2020;17:773–780. doi: 10.1038/s41575-020-00368-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee K.C., Wu K.L., Yen C.K., Chang S.F., Chen C.N., Lu Y.C. Inhibition of NLRP3 by Fermented Quercetin Decreases Resistin-Induced Chemoresistance to 5-Fluorouracil in Human Colorectal Cancer Cells. Pharmaceuticals. 2022;15:798. doi: 10.3390/ph15070798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rawla P., Barsouk A., Hadjinicolaou A.V., Barsouk A. Immunotherapies and Targeted Therapies in the Treatment of Metastatic Colorectal Cancer. Med. Sci. 2019;7:83. doi: 10.3390/medsci7080083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Her J.Y., Lee Y., Kim S.J., Heo G., Choo J., Kim Y., Howe C., Rhee S.H., Yu H.S., Chung H.Y., et al. Blockage of protease-activated receptor 2 exacerbates inflammation in high-fat environment partly through autophagy inhibition. Am. J. Physiol. Gastrointest. Liver Physiol. 2021;320:G30–G42. doi: 10.1152/ajpgi.00203.2020. [DOI] [PubMed] [Google Scholar]
- 9.Kim Y., Lee Y., Heo G., Jeong S., Park S., Yoo J.W., Jung Y., Im E. Modulation of Intestinal Epithelial Permeability via Protease-Activated Receptor-2-Induced Autophagy. Cells. 2022;11:878. doi: 10.3390/cells11050878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saha S., Panigrahi D.P., Patil S., Bhutia S.K. Autophagy in health and disease: A comprehensive review. Biomed. Pharmacother. 2018;104:485–495. doi: 10.1016/j.biopha.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 11.Csizmadia T., Juhász G. Crinophagy mechanisms and its potential role in human health and disease. Prog. Mol. Biol. Transl. Sci. 2020;172:239–255. doi: 10.1016/bs.pmbts.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Chung K.W., Kim K.M., Choi Y.J., An H.J., Lee B., Kim D.H., Lee E.K., Im E., Lee J., Im D.S., et al. The critical role played by endotoxin-induced liver autophagy in the maintenance of lipid metabolism during sepsis. Autophagy. 2017;13:1113–1129. doi: 10.1080/15548627.2017.1319040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chung K.W., Chung H.Y. The Effects of Calorie Restriction on Autophagy: Role on Aging Intervention. Nutrients. 2019;11:2923. doi: 10.3390/nu11122923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glick D., Barth S., Macleod K.F. Autophagy: Cellular and molecular mechanisms. J. Pathol. 2010;221:3–12. doi: 10.1002/path.2697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim J., Hlaing S.P., Lee J., Saparbayeva A., Kim S., Hwang D.S., Lee E.H., Yoon I.-S., Yun H., Kim M.-S. Exfoliated bentonite/alginate nanocomposite hydrogel enhances intestinal delivery of probiotics by resistance to gastric pH and on-demand disintegration. Carbohydr. Polym. 2021;272:118462. doi: 10.1016/j.carbpol.2021.118462. [DOI] [PubMed] [Google Scholar]
- 16.Paolillo R., Carratelli C.R., Sorrentino S., Mazzola N., Rizzo A. Immunomodulatory effects of Lactobacillus plantarum on human colon cancer cells. Int. Immunopharmacol. 2009;9:1265–1271. doi: 10.1016/j.intimp.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 17.Chuah L.-O., Foo H.L., Loh T.C., Mohammed Alitheen N.B., Yeap S.K., Abdul Mutalib N.E., Abdul Rahim R., Yusoff K. Postbiotic metabolites produced by Lactobacillus plantarum strains exert selective cytotoxicity effects on cancer cells. BMC Complement. Altern. Med. 2019;19:114. doi: 10.1186/s12906-019-2528-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prakoeswa C.R.S., Bonita L., Karim A., Herwanto N., Umborowati M.A., Setyaningrum T., Hidayati A.N., Surono I.S. Beneficial effect of Lactobacillus plantarum IS-10506 supplementation in adults with atopic dermatitis: A randomized controlled trial. J. Dermatol. Treat. 2022;33:1491–1498. doi: 10.1080/09546634.2020.1836310. [DOI] [PubMed] [Google Scholar]
- 19.Le B., Yang S.H. Efficacy of Lactobacillus plantarum in prevention of inflammatory bowel disease. Toxicol. Rep. 2018;5:314–317. doi: 10.1016/j.toxrep.2018.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valdez J.C., Peral M.C., Rachid M., Santana M., Perdigon G. Interference of Lactobacillus plantarum with Pseudomonas aeruginosa in vitro and in infected burns: The potential use of probiotics in wound treatment. Clin. Microbiol. Infect. 2005;11:472–479. doi: 10.1111/j.1469-0691.2005.01142.x. [DOI] [PubMed] [Google Scholar]
- 21.Liu J., Gu Z., Song F., Zhang H., Zhao J., Chen W. Lactobacillus plantarum ZS2058 and Lactobacillus rhamnosus GG use different mechanisms to prevent Salmonella infection in vivo. Front. Microbiol. 2019;10:299. doi: 10.3389/fmicb.2019.00299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pourramezan Z., Oloomi M., Kasra-Kermanshahi R. Antioxidant and Anticancer Activities of Lactobacillus Hilgardii Strain AG12a. Int. J. Prev. Med. 2020;11:132. doi: 10.4103/ijpvm.IJPVM_307_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ryu J.Y., Kang H.R., Cho S.K. Changes Over the Fermentation Period in Phenolic Compounds and Antioxidant and Anticancer Activities of Blueberries Fermented by Lactobacillus plantarum. J. Food Sci. 2019;84:2347–2356. doi: 10.1111/1750-3841.14731. [DOI] [PubMed] [Google Scholar]
- 24.Riaz Rajoka M.S., Zhao H., Lu Y., Lian Z., Li N., Hussain N., Shao D., Jin M., Li Q., Shi J. Anticancer potential against cervix cancer (HeLa) cell line of probiotic Lactobacillus casei and Lactobacillus paracasei strains isolated from human breast milk. Food Funct. 2018;9:2705–2715. doi: 10.1039/C8FO00547H. [DOI] [PubMed] [Google Scholar]
- 25.Sheng S., Fu Y., Pan N., Zhang H., Xiu L., Liang Y., Liu Y., Liu B., Ma C., Du R., et al. Novel exopolysaccharide derived from probiotic Lactobacillus pantheris TCP102 strain with immune-enhancing and anticancer activities. Front. Microbiol. 2022;13:1015270. doi: 10.3389/fmicb.2022.1015270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kamaluddin W.N.F.W., Rismayuddin N.A.R., Ismail A.F., Aidid E.M., Othman N., Mohamad N.A.H., Arzmi M.H. Probiotic inhibits oral carcinogenesis: A systematic review and meta-analysis. Arch. Oral Biol. 2020;118:104855. doi: 10.1016/j.archoralbio.2020.104855. [DOI] [PubMed] [Google Scholar]
- 27.Zhang M., Wang F., Jiang L., Liu R., Zhang L., Lei X., Li J., Jiang J., Guo H., Fang B., et al. Lactobacillus salivarius REN inhibits rat oral cancer induced by 4-nitroquioline 1-oxide. Cancer Prev. Res. 2013;6:686–694. doi: 10.1158/1940-6207.CAPR-12-0427. [DOI] [PubMed] [Google Scholar]
- 28.Yan S., Qiao L., Dou X., Song X., Chen Y., Zhang B., Xu C. Biogenic selenium nanoparticles by Lactobacillus casei ATCC 393 alleviate the intestinal permeability, mitochondrial dysfunction and mitophagy induced by oxidative stress. Food Funct. 2021;12:7068–7080. doi: 10.1039/D0FO03141K. [DOI] [PubMed] [Google Scholar]
- 29.Zhang W., Zhu Y.H., Yang G.Y., Liu X., Xia B., Hu X., Su J.H., Wang J.F. Lactobacillus rhamnosus GG Affects Microbiota and Suppresses Autophagy in the Intestines of Pigs Challenged with Salmonella Infantis. Front. Microbiol. 2018;8:2705. doi: 10.3389/fmicb.2017.02705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Behzadi E., Hosseini H.M., Fooladi A.A.I. The inhibitory impacts of Lactobacillus rhamnosus GG-derived extracellular vesicles on the growth of hepatic cancer cells. Microb. Pathog. 2017;110:1–6. doi: 10.1016/j.micpath.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 31.Zhu T., Mao J., Zhong Y., Huang C., Deng Z., Cui Y., Liu J., Wang H.L. reuteri ZJ617 inhibits inflammatory and autophagy signaling pathways in gut-liver axis in piglet induced by lipopolysaccharide. J. Anim. Sci. Biotechnol. 2021;12:110. doi: 10.1186/s40104-021-00624-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.An J., Seok H., Ha E.M. GABA-producing Lactobacillus plantarum inhibits metastatic properties and induces apoptosis of 5-FU-resistant colorectal cancer cells via GABAB receptor signaling. J. Microbiol. 2021;59:202–216. doi: 10.1007/s12275-021-0562-5. [DOI] [PubMed] [Google Scholar]
- 33.Sun M., Liu W., Song Y., Tuo Y., Mu G., Ma F. The Effects of Lactobacillus plantarum-12 Crude Exopolysaccharides on the Cell Proliferation and Apoptosis of Human Colon Cancer (HT-29) Cells. Probiotics Antimicrob. Proteins. 2021;13:413–421. doi: 10.1007/s12602-020-09699-8. [DOI] [PubMed] [Google Scholar]
- 34.Hiraishi N., Kanmura S., Oda K., Arima S., Kumagai K., Mawatari S., Tanoue S., Sasaki F., Hashimoto S., Ido A. Extract of Lactobacillus plantarum strain 06CC2 induces JNK/p38 MAPK pathway-mediated apoptosis through endoplasmic reticulum stress in Caco2 colorectal cancer cells. Biochem. Biophys. Rep. 2019;20:100691. doi: 10.1016/j.bbrep.2019.100691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tanida I., Ueno T., Kominami E. LC3 and Autophagy. Methods Mol. Biol. 2008;445:77–88. doi: 10.1007/978-1-59745-157-4_4. [DOI] [PubMed] [Google Scholar]
- 36.Mehrpour M., Esclatine A., Beau I., Codogno P. Overview of macroautophagy regulation in mammalian cells. Cell Res. 2010;20:748–762. doi: 10.1038/cr.2010.82. [DOI] [PubMed] [Google Scholar]
- 37.Maeda S., Yamamoto H., Kinch L.N., Garza C.M., Takahashi S., Otomo C., Grishin N.V., Forli S., Mizushima N., Otomo T. Structure, lipid scrambling activity and role in autophagosome formation of ATG9A. Nat. Struct. Mol. Biol. 2020;27:1194–1201. doi: 10.1038/s41594-020-00520-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhong Y., Wang Q.J., Li X., Yan Y., Backer J.M., Chait B.T., Heintz N., Yue Z. Distinct regulation of autophagic activity by Atg14L and Rubicon associated with Beclin 1-phosphatidylinositol-3-kinase complex. Nat. Cell Biol. 2009;11:468–476. doi: 10.1038/ncb1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 40.Chen Z., Lu W., Garcia-Prieto C., Huang P. The Warburg effect and its cancer therapeutic implications. J. Bioenerg. Biomembr. 2007;39:267–274. doi: 10.1007/s10863-007-9086-x. [DOI] [PubMed] [Google Scholar]
- 41.Alfarouk K.O., Verduzco D., Rauch C., Muddathir A.K., Adil H.H., Elhassan G.O., Ibrahim M.E., Orozco J.D.P., Cardone R.A., Reshkin S.J., et al. Glycolysis, tumor metabolism, cancer growth and dissemination. A new pH-based etiopathogenic perspective and therapeutic approach to an old cancer question. Oncoscience. 2014;1:777–802. doi: 10.18632/oncoscience.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Warburg O. On the origin of cancer cells. Science. 1956;123:309–314. doi: 10.1126/science.123.3191.309. [DOI] [PubMed] [Google Scholar]
- 43.Vander Heiden M.G., Cantley L.C., Thompson C.B. Understanding the Warburg effect: The metabolic requirements of cell proliferation. Science. 2009;324:1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Martinez-Outschoorn U.E., Lin Z., Ko Y.H., Goldberg A.F., Flomenberg N., Wang C., Pavlides S., Pestell R.G., Howell A., Sotgia F., et al. Understanding the metabolic basis of drug resistance: Therapeutic induction of the Warburg effect kills cancer cells. Cell Cycle. 2011;10:2521–2528. doi: 10.4161/cc.10.15.16584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu R.H., Pelicano H., Zhou Y., Carew J.S., Feng L., Bhalla K.N., Keating M.J., Huang P. Inhibition of glycolysis in cancer cells: A novel strategy to overcome drug resistance associated with mitochondrial respiratory defect and hypoxia. Cancer Res. 2005;65:613–621. doi: 10.1158/0008-5472.613.65.2. [DOI] [PubMed] [Google Scholar]
- 46.Cairns R.A., Harris I.S., Mak T.W. Regulation of cancer cell metabolism. Nature reviews. Cancer. 2011;11:85–95. doi: 10.1038/nrc2981. [DOI] [PubMed] [Google Scholar]
- 47.Zhao Y., Butler E.B., Tan M. Targeting cellular metabolism to improve cancer therapeutics. Cell Death Dis. 2013;4:e532. doi: 10.1038/cddis.2013.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Longley D.B., Harkin D.P., Johnston P.G. 5-fluorouracil: Mechanisms of action and clinical strategies. Nat. Rev. Cancer. 2003;3:330–338. doi: 10.1038/nrc1074. [DOI] [PubMed] [Google Scholar]
- 49.Montagnani F., Chiriatti A., Turrisi G., Francini G., Fiorentini G. A systematic review of FOLFOXIRI chemotherapy for the first-line treatment of metastatic colorectal cancer: Improved efficacy at the cost of increased toxicity. Color. Dis. Off. J. Assoc. Coloproctol. G. B. Irel. 2011;13:846–852. doi: 10.1111/j.1463-1318.2010.02206.x. [DOI] [PubMed] [Google Scholar]
- 50.Papanastasopoulos P., Stebbing J. Molecular basis of 5-fluorouracil-related toxicity: Lessons from clinical practice. Anticancer. Res. 2014;34:1531–1535. [PubMed] [Google Scholar]
- 51.An J., Ha E.M. Combination Therapy of Lactobacillus plantarum Supernatant and 5-Fluouracil Increases Chemosensitivity in Colorectal Cancer Cells. J. Microbiol. Biotechnol. 2016;26:1490–1503. doi: 10.4014/jmb.1605.05024. [DOI] [PubMed] [Google Scholar]
- 52.Longley D.B., Johnston P.G. Molecular mechanisms of drug resistance. J. Pathol. 2005;205:275–292. doi: 10.1002/path.1706. [DOI] [PubMed] [Google Scholar]
- 53.Kim H.J., An J., Ha E.M. Lactobacillus plantarum-derived metabolites sensitize the tumor-suppressive effects of butyrate by regulating the functional expression of SMCT1 in 5-FU-resistant colorectal cancer cells. J. Microbiol. 2022;60:100–117. doi: 10.1007/s12275-022-1533-1. [DOI] [PubMed] [Google Scholar]
- 54.An J., Ha E.M. Extracellular vesicles derived from Lactobacillus plantarum restore chemosensitivity through the PDK2-mediated glucose metabolic pathway in 5-FU-resistant colorectal cancer cells. J. Microbiol. 2022;60:735–745. doi: 10.1007/s12275-022-2201-1. [DOI] [PubMed] [Google Scholar]
- 55.Hammond W.A., Swaika A., Mody K. Pharmacologic resistance in colorectal cancer: A review. Ther. Adv. Med. Oncol. 2016;8:57–84. doi: 10.1177/1758834015614530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaliyamoorthy V., Jacop J.P., Thirugnanasambantham K., Ibrahim H.I.M., Kandhasamy S. The synergic impact of lignin and Lactobacillus plantarum on DSS-induced colitis model via regulating CD44 and miR 199a alliance. World J. Microbiol. Biotechnol. 2022;38:233. doi: 10.1007/s11274-022-03424-z. [DOI] [PubMed] [Google Scholar]
- 57.Park M., Park E.J., Kim S.H., Lee H.J. Lactobacillus plantarum ATG-K2 and ATG-K6 Ameliorates High-Fat with High-Fructose Induced Intestinal Inflammation. Int. J. Mol. Sci. 2021;22:4444. doi: 10.3390/ijms22094444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu Y., Li A., Liu H., Zhang Z., Zhang C., Ma C., Zhang L., Zhang J. Lactobacillus plantarum HNU082 alleviates dextran sulfate sodium-induced ulcerative colitis in mice through regulating gut microbiome. Food Funct. 2022;13:10171–10185. doi: 10.1039/D2FO02303B. [DOI] [PubMed] [Google Scholar]
- 59.Hasannejad-Bibalan M., Mojtahedi A., Eshaghi M., Rohani M., Pourshafie M.R., Talebi M. The effect of selected Lactobacillus strains on dextran sulfate sodium-induced mouse colitis model. Acta Microbiol. Et Immunol. Hung. 2020;67:138–142. doi: 10.1556/030.2020.00834. [DOI] [PubMed] [Google Scholar]
- 60.Yu P., Ke C., Guo J., Zhang X., Li B. Lactobacillus plantarum L15 Alleviates Colitis by Inhibiting LPS-Mediated NF-κB Activation and Ameliorates DSS-Induced Gut Microbiota Dysbiosis. Front. Immunol. 2020;11:575173. doi: 10.3389/fimmu.2020.575173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Prantera C., Scribano M.L., Falasco G., Andreoli A., Luzi C. Ineffectiveness of probiotics in preventing recurrence after curative resection for Crohn’s disease: A randomised controlled trial with Lactobacillus GG. Gut. 2002;51:405–409. doi: 10.1136/gut.51.3.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rogler G. Chronic ulcerative colitis and colorectal cancer. Cancer Lett. 2014;345:235–241. doi: 10.1016/j.canlet.2013.07.032. [DOI] [PubMed] [Google Scholar]
- 63.Venegas D.P., De la Fuente M.K., Landskron G., González M.J., Quera R., Dijkstra G., Harmsen H.J.M., Faber K.N., Hermoso M.A. Corrigendum: Short Chain Fatty Acids (SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases. Front. Immunol. 2019;10:1486. doi: 10.3389/fimmu.2019.01486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gatenby R.A., Gillies R.J. Why do cancers have high aerobic glycolysis? Nat. Rev. Cancer. 2004;4:891–899. doi: 10.1038/nrc1478. [DOI] [PubMed] [Google Scholar]
- 65.Shi Y., Meng L., Zhang C., Zhang F., Fang Y. Corrigendum to “Extracellular vesicles of Lacticaseibacillus paracasei PC-H1 induce colorectal cancer cells apoptosis via PDK1/AKT/Bcl-2 signaling pathway”. Microbiol. Res. 2022;259:126955. doi: 10.1016/j.micres.2021.126955. [DOI] [PubMed] [Google Scholar]
- 66.Ganapathy-Kanniappan S., Geschwind J.F. Tumor glycolysis as a target for cancer therapy: Progress and prospects. Mol. Cancer. 2013;12:1–11. doi: 10.1186/1476-4598-12-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kawaguchi M., Aoki S., Hirao T., Morita M., Ito K. Autophagy is an important metabolic pathway to determine leukemia cell survival following suppression of the glycolytic pathway. Biochem. Biophys. Res. Commun. 2016;474:188–192. doi: 10.1016/j.bbrc.2016.04.098. [DOI] [PubMed] [Google Scholar]
- 68.Chu Y., Chang Y., Lu W., Sheng X., Wang S., Xu H., Ma J. Regulation of Autophagy by Glycolysis in Cancer. Cancer Manag. Res. 2020;12:13259. doi: 10.2147/CMAR.S279672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Xu C., Qiao L., Ma L., Guo Y., Dou X., Yan S., Zhang B., Roman A. Biogenic selenium nanoparticles synthesized by Lactobacillus casei ATCC 393 alleviate intestinal epithelial barrier dysfunction caused by oxidative stress via Nrf2 signaling-mediated mitochondrial pathway. Int. J. Nanomed. 2019;14:4491–4502. doi: 10.2147/IJN.S199193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Levy J.M.M., Towers C.G., Thorburn A. Targeting autophagy in cancer. Nature reviews. Cancer. 2017;17:528–542. doi: 10.1038/nrc.2017.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Levy J.M.M., Zahedi S., Griesinger A.M., Morin A., Davies K.D., Aisner D.L., Kleinschmidt-DeMasters B.K., Fitzwalter B.E., Goodall M.L., Thorburn J., et al. Autophagy inhibition overcomes multiple mechanisms of resistance to BRAF inhibition in brain tumors. eLife. 2017;6:e19671. doi: 10.7554/eLife.19671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Goussetis D.J., Gounaris E., Wu E.J., Vakana E., Sharma B., Bogyo M., Altman J.K., Platanias L.C. Autophagic degradation of the BCR-ABL oncoprotein and generation of antileukemic responses by arsenic trioxide. Blood. 2012;120:3555–3562. doi: 10.1182/blood-2012-01-402578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kocaturk N.M., Akkoc Y., Kig C., Bayraktar O., Gozuacik D., Kutlu O. Autophagy as a molecular target for cancer treatment. Eur. J. Pharm. Sci. Off. J. Eur. Fed. Pharm. Sci. 2019;134:116–137. doi: 10.1016/j.ejps.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 74.Liang L., Hui K., Hu C., Wen Y., Yang S., Zhu P., Wang L., Xia Y., Qiao Y., Sun W., et al. Autophagy inhibition potentiates the anti-angiogenic property of multikinase inhibitor anlotinib through JAK2/STAT3/VEGFA signaling in non-small cell lung cancer cells. J. Exp. Clin. Cancer Res. 2019;38:71. doi: 10.1186/s13046-019-1093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhou Y., Tozzi F., Chen J., Fan F., Xia L., Wang J., Gao G., Zhang A., Xia X., Brasher H., et al. Intracellular ATP levels are a pivotal determinant of chemoresistance in colon cancer cells. Cancer Res. 2012;72:304–314. doi: 10.1158/0008-5472.CAN-11-1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bhattacharya B., Low S.H., Soh C., Mustapa N.K., Beloueche-Babari M., Koh K.X., Loh J., Soong R. Increased drug resistance is associated with reduced glucose levels and an enhanced glycolysis phenotype. Br. J. Pharmacol. 2014;171:3255–3267. doi: 10.1111/bph.12668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pellegrini P., Strambi A., Zipoli C., Hägg-Olofsson M., Buoncervello M., Linder S., De Milito A. Acidic extracellular pH neutralizes the autophagy-inhibiting activity of chloroquine: Implications for cancer therapies. Autophagy. 2014;10:562–571. doi: 10.4161/auto.27901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Thévenod F., Lee W.K. Live and Let Die: Roles of Autophagy in Cadmium Nephrotoxicity. Toxics. 2015;3:130–151. doi: 10.3390/toxics3020130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Qu X., Sheng J., Shen L., Su J., Xu Y., Xie Q., Wu Y., Zhang X., Sun L. Autophagy inhibitor chloroquine increases sensitivity to cisplatin in QBC939 cholangiocarcinoma cells by mitochondrial ROS. PLoS ONE. 2017;12:e0173712. doi: 10.1371/journal.pone.0173712. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.