Abstract
Undoubtedly, diagnosing and managing infections is one of the most challenging issues for orofacial clinicians. As a result of the diversity of symptoms, complicated behavior, and sometimes confusing nature of these conditions, it has become increasingly difficult to diagnose and treat them. It also highlights the need to gain a deeper insight into the orofacial microbiome as we try to improve our understanding of it. In addition to changes in patients’ lifestyles, such as changes in diet, smoking habits, sexual practices, immunosuppressive conditions, and occupational exposures, there have been changes in patients’ lifestyles that complicate the issue. Recent years have seen the development of new infection treatments due to the increased knowledge about the biology and physiology of infections. This review aimed to provide a comprehensive overview of the types of infections in the mouth, including the types that viruses, fungi, or bacteria may cause. It is important to note that we searched the published literature in the Scopus, Medline, Google Scholar, and Cochran databases from 2010 to 2021 using the following keywords: “Orofacial/Oral Infections,” “Viral/Fungal/Bacterial Infections”, “Oral Microbiota” And “Oral Microflora” without limiting our search to languages and study designs. According to the evidence, the most common infections in the clinic include herpes simplex virus, human papillomavirus, Candida albicans, Aspergillus, Actinomycosis, and Streptococcus mutans. The purpose of this study is to review the new findings on characteristics, epidemiology, risk factors, clinical manifestations, diagnosis, and new treatment for these types of infectious diseases.
Keywords: oral fungal infections, oral bacterial infections, oral viral infections, orofacial infection, orofacial microbes
1. Introduction
The natural flora of the mouth is very diverse. After the large intestine, it has the second highest complexity in terms of microorganisms, including more than 700 microorganisms [1]. The tongue is the primary source of microbes in saliva and the major oral site for microbial growth [2]. Some bacterial, viral, and fungal agents can affect the skin and mucous membranes in the orofacial area. These factors can cross natural barriers and cause lesions of varying degrees. Some of them can even be life-threatening. The local and systemic factors determining the microbiota and genetics, as well as the individual factors such as diet, teeth brushing habits, dentures, dental procedures, mouthwashes, medications, etc., can be involved in the occurrence of orofacial infections [1,3,4,5,6,7]. Oral infections can occur under certain conditions, such as poor oral hygiene, antibiotic consumption, trauma, and dry mouth, and can damage the oral cavity. These infections also may spread into the nearby tissues and turn into systemic infections. For example, chronic oral infections are known to be a risk factor for cardiac disease [2].
Each tissue has specific microbes that are different from adjacent tissues’ microbes. Still, these microbes can be displaced under certain conditions, such as the effects of cytotoxic drugs, oral cancer, or epithelial atrophy [8,9]. The oral flora is divided into two categories, static and transient, which regularly balance with the host and protect against pathogenic microorganisms. The static flora on oral cavity surfaces is known as biofilm that can improve or protect oral health against pathogens, increase the virulence of potentially harmful microorganisms, and reduce the effectiveness of antimicrobial agents [10,11,12]. Infections caused by bacteria in the mouth include caries and periodontitis [8]. Microorganisms can attack different parts of the mouth via different mechanisms. For example, keratinized epithelial surfaces, such as the palate, become excessively keratinized, and their contained opportunistic microorganisms may lead to infection. The buccal and labial mucosa, as non-keratinized epithelial surfaces, may be occupied by dead or apoptotic cells that may be attacked by bacteria [10,13,14,15]. Despite the progression of several local or generalized treatment methods, orofacial infections may still cause severe discomfort and pain. Therefore, the popularity of the clinical presentation of those infections is dominant to their diagnosis, clinical management, and appropriate referral. The following review includes the most recognized orofacial infective agents and their clinical characteristics.
2. Herpes Simplex Virus
Herpes simplex virus [16] is one of 200 species of the Herpesviridae family and belongs to the subfamily Alphaherpesvirinae, the genus Simplexvirus. Despite differences in host and morphology, this family is thought to be originated from a common ancestor with tailed bacteriophages [17]. These viruses are about 120 to 200 nanometers in diameter. Structurally, they include a circled DNA containing a unique long (UL) segment and a unique short (US) segment (opposite repeats) [17,18]. In addition, they have an icosahedral symmetric capsid, protein coating, and a lipid bilayer cell-like envelope. Genome transcription and replication and the formation of new capsids occur in the host cell’s nucleus [18]. These viruses’ short reproductive cycle helps them rapidly destroy the host cells [17]. During the infection procedure, the envelope releases the capsid into the host cell’s cytoplasm after fusion with its plasma membrane. HSV can attack nerve tissue and multiply there (neuro-virulence). Eighty-three percent identical nucleotides and fifty percent homology in the sequence display a strong association between the two types of herpes virus: HSV-1 and 2 [17].
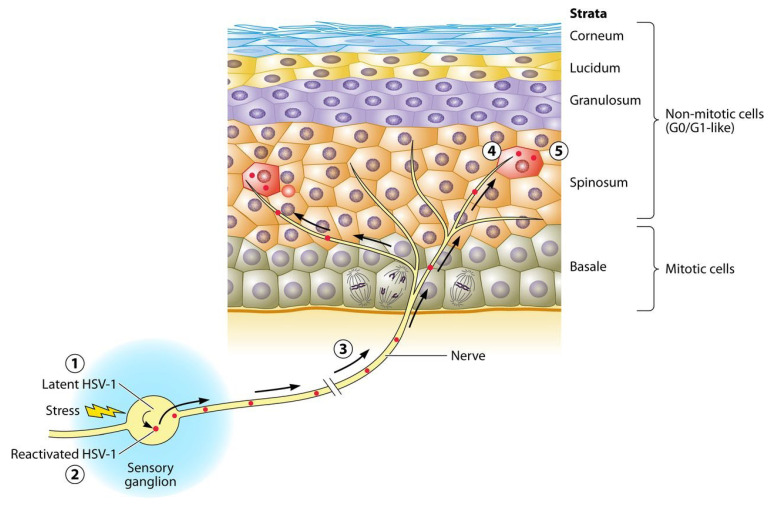
HSV is also recognized for its latency ability in trigeminal and sacral ganglion nuclei of the ganglia structures [17,19]. HSV fuses to the axon termini to establish latency and moves retrogradely along the sensory fibers (Figure 1) [17]. Then, it generates latency-associated transcripts (LATs) that enhance axon regeneration, reduce viral gene expression, and prevent nerve cell apoptosis [20].
Figure 1.
The latent infection of HSV-1 leads to permanent arrest in an G0/G1-like state in the sensory ganglia that will never reenter mitosis ①. During reactivation, virus genes are expressed in cells in the most permissive state ②. Then, reactivated virions travels in axons ③ to termini on the epidermis ④, and then transmitted to the spinosum and granulosum strata layers of the epidermis ⑤ [17].
2.1. Epidemiology
HSV is most commonly transmitted through asymptomatic shedding from an infected person’s mouth or genitals. It is mainly transmitted through proximity to an infected person in immunocompromised and immunocompetent individuals [21]. Recurrent HSV infections occur in one-third of the world’s population. HSV-1 and 2 usually infect the mucocutaneous of the mouth and genitals, respectively. The incidence of HSV is 40–95% worldwide, depending on the socio-economic status of the studied population, with higher rates in lower socio-economic populations. Sixty percent of adults with HSV-2 have orolabial herpes [21]. Generally, the seroprevalence of HSV increases with age and shows some correlations to the country’s income. Sixty percent higher seroprevalence in people over the age of 40 than in those under 20 suggests an increased risk of exposure that should be observed by health beneficiaries [22].
2.2. Clinical Presentation
The disease has no clinical signs at the initial acquisition or during periods of reactivation. However, symptoms occur in the active periods of the disease, following asymptomatic periods, on a rotating basis [23]. Clinical symptoms of the first episode of the disease include headache, fever, muscle aches, and inflammation of the lymph nodes [23]. Then, classic lesions are created that include fluid-filled vesicles that become purulent and dry. Genital herpes includes small blisters resulting in benign ulcers, whereas, in cold sores, several small blisters are aggregated [23]. Other vital clinical signs of common gingivitis include bleeding gums with edema and friable erythematosus. In addition, sores on the buccal mucosa and gums may be yellow based on a red halo. These oral lesions are often associated with anorexia. Symptoms in young children can include drooling, halitosis, and dehydration [23]. Herpetic vitiligo is another manifestation, which is painful, erythematous, and swollen lesions often occur in the distal phalanx of the hand, caused by HSV-1 or HSV-2. This lesion mainly affects the fingers (thumb) and rarely the palm [23]. HSV-1 eczema herpeticum of Kaposi varicelliform eruption is caused by poor immunity due to atopic dermatitis, burns, or topical immunosuppressants. The disease includes vesicular skin lesions [24]. HSV eye keratitis and HSV encephalitis are other complications caused by this virus. Eye involvement can lead to sensitive retinal necrosis, conjunctivitis, blepharitis, or chorioretinitis. Reaching this viral infection to the brain parenchyma leads to extensive hemorrhagic necrosis and vascular occlusion. Encephalitis is the worst outcome that can occur in a healthy person following this infection [24,25]. Patients with good immunity have milder symptoms in the recurrence period than in the early symptoms. In general, patients with HSV-1 usually have lesions around the lips and mouth. Several studies have reported a local burning prodrome with roughness or itching before the vesicles erupt. The lymph nodes in the affected area can become sensitive and enlarged without systemic symptoms and fever. Studies have shown that HSV-1 and Epstein–Barr virus (EBV) is associated with invasive periodontal disease caused by bacteria [26].
2.3. Diagnosis
Because most people with HSV-2 do not have the classic clinical symptoms, genital herpes is more challenging to diagnose than oral herpes and can be confused with related diseases such as fungal infections, lichen planus, atopic dermatitis, and urinary tract diseases. Diagnosis is confirmed by laboratory tests, including polymerase chain reaction (PCR), skin biopsy, immunofluorescence, and virus culture polymerase chain reaction (PCR). Blood and urine cultures determine previous and ongoing infections, respectively. PCR is more sensitive and accurate for diagnosing HSV in mucosal surfaces than vesicular fluid culture. In patients with a history of genital ulcers lacking active lesions, serological diagnostic tests are conducted [27].
2.4. Treatment
Although antiviral drugs, including acyclovir, valaciclovir, famciclovir, and penciclovir, reduce the disease’s incidence, duration, and severity, no way exists to remove the virus from the body. Painkillers and topical anesthetic treatments can relieve pain/fever and itching, respectively; however, their efficiency has been controversial [28]. In addition, intravenous infusion of acyclovir is recommended for eczema herpeticum to be limited and prevented from spreading to the eye [25]. Seizure control, fluids management, and intracranial pressure control will improve results in HSV-based eye keratitis [24,25]. Suppressive therapy, such as corticosteroids, is commonly used to improve pain and tenderness at the onset of symptoms. Oral acyclovir has a positive therapeutic effect on primary and recurrent HSV genital infections [25]. Some studies have discussed the antiviral activity of some essential oils on the HSV spp. (even acyclovir-resistant strains) through different mechanisms, such as inhibiting cell attachment. These studies also imply that the synergistic activity of the extracts and, thus, essential oils minimize the development of resistant virus strains [29,30]. A recent development in treating HSV is presented in Table 1.
Table 1.
Recent developments in treating orofacial viral infections.
| Species | Samples | Intervention | Outcomes | Ref. Year |
|---|---|---|---|---|
| HPV | Patients with progressed oropharyngeal cancer | Accelerated fractionation radiotherapy and standard-fractionation radiotherapy | Over 6o percent of patients were HPV-positive and showed better overall survival in 3 years compared to HPV-negative tumors. | [31] 2010 |
| HSV-2 | Patients with acute primary or recurrent HSV-2 | 1 g valacyclovir 3 times daily for 1 week, followed by 0.5 g valaciclovir twice daily for 1 year. |
The following-up prescription showed insufficiency in prohibiting recurrent meningitis. | [16] 2012 |
| HPV | Patients under cervical surgery | Three doses of quadrivalent HPV vaccine or placebo at days 1, 60, and 180 | Quadrivalent HPV vaccination after surgical treatment significantly reduced recurrent HPV-related diseases. | [32] 2012 |
| HSV-1 and 2 | Patients with HIV-1 and HSV-2 | Valacyclovir 1000 mg or acyclovir 400 mg twice a week for ~3 months | High-dose valacyclovir was more successful in reducing the plasma HIV-1 RNA levels compared to the standard dose. | [33] 2013 |
| HSV-2 | Patients with HIV and HSV-2 in co-infection | Patients randomly received valacyclovir or placebo (N = 35) | The CD4+ T-lymphocyte count or HIV viral load did not change, but asymptomatic HSV-2 shedding reduced slightly. | [34] 2014 |
| HSV-1 or HSV-2 | RCTs | Effectiveness of oral antiviral drugs (acyclovir, famciclovir, and valacyclovir) | Researchers found there was a significantly lower number of patients with at least one genital herpes recurrence when acyclovir, valacyclovir, or famciclovir was used to treat patients with at least four recurrences per year as compared with placebo in patients with at least four recurrences. | [35] 2014 |
| HPV | Patients examined for gingivitis | Three medicinal mushrooms: Laetiporus sulphureus, Ganoderma lucidum, and Trametes Versicolor | Laetiporus sulphureus exerted 5% oral HPV clearance, while Trametes Versicolor plus Ganoderma lucidum showed a clearance of 88%. | [36] 2014 |
| HPV-16 and HPV-18 | Patients from 36 gynecology practices in seven countries | 6 mg VGX-3100 or placebo | This vaccine is the first to show effectiveness against CIN2/3 associated with HPV-16 and HPV-18 and provides a new treatment outlook. | [37] 2015 |
| HSV-2 | Healthy adults with recurrent genital HSV-2 | 100 mg oral pritelivir with 500 mg valaciclovir once a day | People with frequently recurrent genital HSV-2 using pritelivir experienced a lower percentage of HSV+ swabs. | [38] 2016 |
| HPV | Patients with high-risk cervical HPV infection | An anti-HPV biological dressing (JB01-BD) | JB01-BD could effectively decrease the viral load. | [39] 2016 |
| HSV-1 and 2 | Patients with post-herpetic neuralgia | 200 mg or 400 mg valnivudine hydrochloride (FV-100) once daily, or 1000 mg valacyclovir three times daily | Treatment with FV-100 decreased the neuralgia in a dose-dependent manner better than valacyclovir. | [40] 2017 |
| HSV-2 | Adults with symptomatic HSV-2 | 30 or 60 µg antigen against glycoprotein D2 and viral transcription factor ICP4.2 | The GEN-003 vaccine combinations with higher amounts of antigen and adjuvant showed more efficacy. | [41] 2018 |
| HSV-2 | Patients with recurrent genital HSV-2 | A vaginal capsule of multistrain Lactobacillus brevis or oral acyclovir | Probiotic therapy with multi-strain L. brevis was a promising low-cost treatment for recurrent genital herpes simplex virus infection compared with acyclovir. | [42] 2018 |
| HPV | Patients with multiple common warts | Intramuscular and intralesional bivalent HPV vaccine | Both HPV vaccination roots showed potential for treating warts. | [43] 2019 |
| HSV-1 | Patients with herpetic stromal keratitis | Topical cyclosporine-A 2% eye drop with prednisolone acetate 1% eye drop | Both treatments could similarly improve the cornea’s optical density to a significant extent. | [44] 2019 |
| HPV | Patients with genital condylomatosis | Dry extracts of Echinacea purpurea and Elaeagnus angustifolia (HPVADL18®) | HPVADL18® was suggested as a potential adjuvant therapy for reducing recurrent lesions after treating genital condylomatosis. | [45] 2019 |
| HPV | Patients with high-risk HPV | A proprietary combination of antiviral biologics (REBACIN®) | The antiviral agent could significantly repress the expression of E7 and E6 oncogenes in HPV and clear persistent HPV infections. | [46] 2019 |
| HSV-1 and 2 | HIV-1-positive adults | 500 mg valaciclovir twice daily | Valaciclovir modestly lowered the HIV viral load but did not slow the CD4 count decline. | [47] 2019 |
| HPV | Patients with recurrent respiratory papillomatosis | 10 mg/kg avelumab every 2 weeks for three doses | Avelumab treatment led to fewer surgical interventions and reduced HPV viral load. | [48] 2019 |
| HSV-1 | Schizophrenic patients with or without HSV-1 | 1.5 g valacyclovir or placebo for 16 weeks | Valacyclovir showed no effect on the viral infection. HSV-1 infection co-occurred with a more severe form of schizophrenia. |
[49] 2019 |
| HSV-1 and 2 | Patients receiving mechanical ventilation for over 4 days | Intravenous acyclovir 5 mg/kg | Acyclovir did not decrease the duration of mechanical ventilation and did not increase the number of ventilator-free days in patients with HSV oropharyngeal reactivation. | [50] 2019 |
| HPV | Patients with anogenital warts | Podophyllotoxin cream 0.15% or imiquimod cream 5% with vaccination | Imiquimod and podophyllotoxin creams could similarly clear the wart, but the vaccine benefit was not observed. | [51] 2020 |
3. Human Papilloma Viruses
Papillomaviruses have a wide genetic diversity. Human papillomavirus (HPV) viruses use human cellular proteins to reproduce and survive [52]. The virus genome consists of open reading frames [53] and long control regions (LCR) to regulate the replication and transcription of primary genes [54]. The main reservoir of HPV is inflamed gums, salivary gland epithelium, and cryptal epithelium of tonsils, oral border, and oropharynx. The most clinically important genus of HPV is the alpha genus of human papillomavirus [52]. In high-risk HPV, placing the virus genome in the host genome breaks the virus genome at the E1 and E2 sites, and losing E2, in turn, causes E6 and E7 to lose control that, inhibits the regular function of p53 and pRb, respectively, and interfere with the cell cycle [55].
3.1. Epidemiology
Owing to effective screening strategies, the incidence of HPV-caused cervical cancer has decreased; however, the oropharyngeal squamous cell carcinoma (OPSCC) cases have kept rising. In addition, the prevalence of HPV DNA has increased by between 24–45 percent from 1990 to 2005 [56]. In a study in the US, oral HPV rates in men were around 60 percent higher than in women. Additionally, their study evidenced the HPV is the leading cause of oropharyngeal carcinoma (OPC) in men, whereas smoking is the predominant cause in women [57].
3.2. Clinical Presentation
HPV infection can be transmitted from the mother’s cervix (sexual and non-sexual fomite transmission) and produces clinical or subclinical lesions. Oral HPV lesions include a range of benign oral lesions, lichen planus, fibroma, hyperplastic, papillomatous, verrucous, and carcinoma lesions. Generally, flat, exophytic, or wart-like white lesions in the oral mucosa, exophytic, wart-like, or papillary proliferations can be considered clinical manifestations of HPV [58]. Oral sex is the main transmission root in these diseases, and soft-circumscribed sessile nodular lesions and koilocytosis are some of their pathological and cellular manifestations [59]. The latent location of HPV in the mouth is usually in the gingival pocket because it is the only place where basal cells are in direct contact with the environment [60]. In about one-fourth of patients with periodontal disease in a clinical survey, the gingival samples have been associated with HPV [60]. Additionally, alveolar bone loss has been related to tumor-positive HPV [60,61].
3.3. Risk Factors
Risk factors for HPV infection include unsafe sexual behavior, smoking, periodontitis, and inflammation. These factors affect HPV infection by altering the oral environment. Cigarettes stimulate and suppress immune mechanisms in the mouth through the chemicals in tobacco. In women with oral HPV, the prevalence of HPV-infected cervixes is also higher, which may be a factor in increasing the risk of oral HPV [62].
3.4. Diagnosis
There are several diagnostic methods for HPV. Immunohistochemical analysis-specific antibodies (e.g., p16INK4A and p16 IHC) and HPV mRNA/DNA-detecting PCR are the sensitive and cost-effective diagnostic methods for HNSCC tumor specimens. However, studies have shown that mRNA tests are the best approach for confirming the diagnosis [63]. Serological biomarker tests cannot be used for detecting HPV infection in the oral cavity. Their examination in oral fluids is useful for identifying and examining the incidence and course of the disease as they are low-cost, non-invasive, and local-specific [64].
3.5. Treatment
Syrjänen discusses that HPV particles only get inactivated at temperatures 75–80 °C [62]. Preventive approaches such as vaccination and routine screening of HPV antibodies in the saliva are among the most effective ways to prevent HPV-associated head and neck diseases. Cold therapy, electrosurgery, surgical resection, laser therapy, and trichloroacetic acid are the usual treatments for papillomas/condyloma, verocroas, and FEH occurred by HPV [52]. The therapeutic developments in treating HPV infection are summarized in Table 1.
4. Candida albicans
More than 200 species of the genus Candida are usually non-pathogenic in humans. However, in immunocompromised individuals, Candida is the most frequent cause of oral mucosal infections, commonly due to antibiotics and the consequent change in the bacterial microbiota. In addition, suppressing the local or systemic immune system prepares the environment for infection. This group’s most common pathogen species is C. albicans, which accounts for more than 90% of oral lesions [65]. Morphological control between yeast and hyphae by C. albicans is involved in its pathogenesis. C. albicans co-adhesion with oral bacteria such as S. mutans helps it to colonize, persist, and grow by receiving a carbon supply. Vice versa, Candida reduces the bacteria’s oxygen stress, promotes better bacteria adhesion, and prepares stimulatory growth factors [66,67].
4.1. Epidemiology
The general prevalence of C. albicans is 20–75%, with 95% incidence in HIV patients, 90% in patients undergoing chemotherapy and acute leukemia, 88–65% in patients at long-term caring centers, 50–65% in people with detachable dentures, 45–30% in healthy adults, 65–45% in healthy children, and 45% in infants. In immunocompromised individuals, severe systemic exposure to Candida species increases mortality [68]. Oropharyngeal Candida is an opportunistic and recurrent fungal infection in more than 90% of patients with HIV [69]. The mortality rate of Candida bloodstream infection (candidemias) is more than 30% [68].
4.2. Clinical Presentation
Pseudomembranous, erythema, hyperplasticity, mucosal irritation, and edema are the symptoms of primary oral candidiasis [70,71]. In more severe cases, hemodynamic instability, positive blood cultures, fever, shock, and tachycardia may occur [70]. Pseudomembranous Candidiasis (thrush) is found on the white plaques, buccal mucosa, oropharynx, and junction of the hard and soft palate and is the most common form of candidiasis. Although some patients may experience a sour taste, burning sensation, and bleeding in the affected areas, most patients are asymptomatic [71]. Candidiasis may be hyperplastic or atrophic and occurs in either chronic or acute forms [70,72]. Different types of candidiasis can be asymptomatic or ulcerous [70]. Hyperplastic candidiasis resembles leukoplakia and may involve the labial commissures and become malignant [72]. Its chronic form is challenging to diagnose since the hyphae may hide in any rough surface in the oral cavity, such as papilloma, epithelial dysplasia, and squamous cell carcinoma [72]. Acute atrophic candidiasis is usually iatrogenic (such as antibiotic consumption) and especially common in HIV patients, whereas chronic atrophic candidiasis is iatrogenic mainly due to orthodontic retainers or dentures that do not adequately fit in place [70]. Chronic atrophic candidiasis and inflammatory papillary hyperplasia [73] may also accompany due to iatrogenic candidiasis because of taking biopsies from median rhomboid glossitis, smoking, and inhaled steroids, for instance [70]. Symptoms of esophageal candidiasis include ulceration, obstruction, narrowing of the esophagus, chest pain, nausea, and vomiting [70]. C. albicans, S. aureus, and β-hemolytic Streptococcus species are among the microorganisms present in angular cheilitis. The anterior region of the nostrils to the corners of the mouth is the source of staphylococci. Iron deficiency anemia, and vitamin B12 deficiency are among the etiological factors [74].
4.3. Risk Factors
IgA, mucins, and antifungal agents (e.g., histatin 5 and calprotectin) protect the oral environment from Candida infection. However, factors such as age, organ transplants, HIV, chemotherapy, poor oral hygiene, smoking, inhaled steroids, and radiotherapy increases its risk [75]. Then, in all patients with daily dental care, treatment of xerostomia, control of diabetes, restriction of corticosteroids and topical or systemic antibiotics, and elimination of underlying predisposing factors are very important [76]. The oral amount of Candida in HIV patients relates to their salivary flow [77]. The overgrowth of Candida species has no significant association with oral bacterial dysfunction [75].
4.4. Diagnosis
Candidiasis suspicion is based on examining mucosal changes, stained smears with Schiff’s reagent or KOH, and histopathological biopsies, searching for the hyphae or epithelial parakeratosis with polymorphonuclear leukocytes [78]. Transcribed internal distance sequencing [40] can be used to identify emerging candidate species and the historical course of candidiasis. For the rapid diagnosis of invasive candidiasis, serological biomarkers, including antibodies against mycelium, β-d-glucan (BDG), mannan antigen (Mannan-Ag), and mannan antibodies, are evaluated [79]. Endoscopy is also necessary for esophageal candidiasis suspicion patients [70].
4.5. Treatment
Polyenes and azoles are two types of antifungal drugs [80,81]. Polyenes (with conjugated double bonds) bind to sterols (mainly ergosterols) and change the cell membrane transfer temperature. Then, the leakage of monovalent ions (K+, Na+, H+, and Cl2) and small organic molecules lead to cell death [80]. On the other hand, azole stores α-methylase enosterol to prevent the lanosterol to ergosterol conversion. These topical drugs have no pharmacological systemic side effects since they have no systemic absorption. In cases where topical drugs do not respond, systemic drugs are used [81]. Studies have shown that probiotics may affect the toxicity of C. albicans. For example, Lactobacillus spp. and S. salivarius prevent the differentiation of C. albicans into hyphae or biofilm structure and decrease the salivary yeast level. Probiotics also increase the level of anti-Candida IgA and, consequently, the yeast level [82]. Recent developments for candida infection are shown in Table 2.
Table 2.
Recent developments in treating fungal infections.
| Species | Sample | Intervention | Outcomes | Ref. Year |
|---|---|---|---|---|
| C. albicans | Children under treatment with a removable maxillary appliance | NitrAdine tablets | The treatment had no significant effect on the salivary Candida load. | [83] 2011 |
| Aspergillus | Patients with allergic bronchopulmonary Aspergillosis | Omalizumab | The treatment was successful in preventing the exacerbation of the infection. | [84] 2014 |
| C. albicans | Adults living in nursing homes | Probiotics, including Lactobacillus reuteri (strains DSM 17938 and ATCC PTA 5289) | The probiotics significantly reduced the oral Candida counts. | [85] 2015 |
| C. albicans | In vitro study | Pomegranate peel extract (PomeGr) | The PomeGr treatment altered biofilm formation, fungal growth, and AI release. Moreover, fungal cells substantially reduced PomeGr’s phenolic content | [86] 2022 |
| Aspergillus | Patients with non-dermatophyte mold onychomycosis | Traconazole or terbinafine | Both treatment efficacy was non-statistically significant (clinical cure of 54–65%). | [87] 2016 |
| Aspergillus | Patients with suspected invasive mold infection | Intravenous injection of isavuconazonium sulfate or voriconazole followed by further oral administration | Isavuconazole efficacy was not worse than voriconazole. It was well tolerated with fewer adverse events. | [88] 2016 |
| C. albicans | Patients wearing dentures | Triphala churna and chlorhexidine gluconate | Triphala showed a more antifungal effect than conventional chlorhexidine. | [89] 2017 |
| C. albicans | Patients with denture stomatitis | Low-molecular-weight chitosan and nystatin | Chitosan solution showed a significant antifungal effect. | [90] 2017 |
| C. albicans | Patients wearing dentures | Two probiotics (Lactobacillus acidophilus or Lactobacillus rhamnosus) enriched into cheese | The enriched cheese with probiotics reduced oral Candida colonization. | [91] 2017 |
| Candida and Aspergillus | Patients with candidemia and invasive candidiasis | A member of echinocandins (CD101 IV) | The dosing of CD101 IV was safe, minimally accumulative, plasma-persistent, and well-tolerated with negligible renal excretion. | [92] 2017 |
| C. albicans | Patients with symptomatic oral lichen planus | Probiotics, including Lactobacilli reuteri | The probiotic used did not affect the Candida load. | [93] 2018 |
| Aspergillus and C. albicans | Patients with otomycosis | Topical betadine and clotrimazole | The agents showed similar antifungal potential for treating otomycosis. | [94] 2018 |
| Aspergillus | Patients in the acute stage of allergic bronchopulmonary Aspergillosis | Oral administration of itraconazole or prednisolone | Prednisolone induced a better immunologic response but more side effects. | [95] 2018 |
| C. albicans | Patients with denture stomatitis | Photodynamic inactivation using a diode laser and methylene blue | The inactivation operation reduced the fungal and inflammation levels. | [96] 2018 |
| C. albicans | Patients with candidemia or invasive candidiasis | Intravenous and oral isavuconazole comparedto caspofungin and voriconazole | Isavuconazole showed a lower minimal inhibitory concentration than caspofungin. | [97] 2019 |
| C. albicans | In vitro study | Tissue conditioner modified by chitosan or chitosan-oligosaccharide | Both formulations reduced the C. albicans density. | [98] 2019 |
| C. albicans | Patients wearing complete dentures with stomatitis | Photodynamic therapy using indocyanine green was added to the routine antifungal therapy with nystatin mouthwash alone | The combined therapy helped to improve the denture stomatitis showing no adverse effects. | [99] 2019 |
| S. mutans, C. albicans, C. glabrata, and C. parapsilosis | In vitro study | Propolis, saline, or alkaline peroxide solutions | The propolis solution had an antimicrobial effect against S. mutans and C. albicans, showing no immediate effect on denture biofilm. | [100] 2019 |
| C. albicans | Patients wearing removable dentures | Chitosan-curcuminoid/PEG mouthwash compared to chlorhexidine | The composite alcohol-free mouthwash was a safe topical therapeutic for treating candida-associated denture stomatitis. | [101] 2019 |
| Aspergillus | Patients with chronic pulmonary Aspergillosis | Intravenous followed by oral administration of itraconazole | The treatments with itraconazole were effective on chronic pulmonary Aspergillosis. | [102] 2019 |
| Aspergillus | Patients with invasive Aspergillosis | Single and multiple ascending intravenous doses of an antifungal drug (VL-2397) | The dosing of VL-2397 was safe, non-accumulative, and tolerable in both healthy subjects and patients. | [103] 2019 |
| C. albicans | Patients wearing dentures with stomatitis | Photodynamic inactivation by GaA1As diode laser in comparison with nystatin | Both treatments were equally effective in treating denture stomatitis. | [104] 2019 |
| C. albicans | Patients wearing maxillary dentures | Dettol and Lifebuoy liquid soaps compared to sodium hypochlorite and phosphate-buffered saline solution as positive and negative controls | The liquid soaps efficiently reduced the fungal biofilm. | [105] 2020 |
| C. albicans | Patients after head and neck radiotherapy | Probiotics, including L. acidophilus, B. longum, L. rhamnosus, and S. boulardii | The probiotic bacteria could effectively reduce the oral Candida load. | [106] 2020 |
| Aspergillus | Patients with otomycosis | Clotrimazole cream and tolnaftate solution | Clotrimazole improved otitis better. | [107] 2020 |
5. Aspergillus
Aspergillosis genus is the second most common opportunistic fungal infection in humans. Aspergillus fumigatus is an air-borne fungal pathogen causing many diseases [108,109]. This pathogen has a saprotrophic mycelial with an efficient spread through asexual spores and a life mostly on decaying organic matter secreting a wide range of enzymes (e.g., amylases, xylanases, pectinases, and elastase) [108]. However, some studies have evidence of heterothallism and a periodical sexual mating procedure [110]. All isolates of A. fumigatus are highly hydrophobic and fast-growing, but their virulence can vary based on indefinite factors such as the growth rate of isolates [109].
The main virulence factors of A. fumigatus are its cell wall containing polysaccharides (90%) and proteins and the glutotoxin from the epipolythiodioxopiperazines family [108]. Through the pathogenesis of Aspergilloma (noninvasive chronic pulmonary Aspergillosis), A. fumigatus hyphae form a biofilm in the extracellular matrix (ECM) with a different cell wall composition and structure [110].
5.1. Epidemiology
The epidemiological studies report that the prevalence of Aspergillus varies in a geographical-, regional-, seasonal-, and occupational-dependent manner [111]. Aspergillus spp. has been isolated from the respiratory tract of asymptomatic patients, and its DNA has been found in 37% of healthy individuals [112]. Its prevalence has been 30% in patients with chronic obstructive pulmonary disease (COPD), and 53% of patients with Aspergillus positive culture were conflicted with invasive Aspergillosis (IA) [112]. Distal–lateral subungual onychomycosis (DLSO) is an onychomycosis condition due to Aspergillus spp., with a prevalence of up to 35% on average and 71% in the diabetic population. It also accounts for 18–50% of all nail diseases and 30% of fungal skin infections [111].
5.2. Clinical Presentation
Aspergillus colonization function damages the epithelial cells and upregulation of ECM proteins by disrupting the expression of the ZNF77 transcription factor in bronchial epithelium and causing conidial adhesion. The immune system-survived and metabolically activated conidia grow, germinate, form hyphae, spread by attacking blood vessels, and invade the lung tissue [113]. Aspergillosis is divided into three categories: invasive (nonfulminant and fulminant), noninvasive, and noninvasive destructive. The nonfulminant invasive types are slowly progressive, and the fulminant invasive types are very aggressive. The non-invasive type can be locally destructive but has no tissue invasion and includes Aspergilloma, fungal ball, and Mycetoma [78,114]. Headache, fever, nasal congestion, swelling of the face, purulent or bloody nasal discharge, nasal pain, and epitaxy are the clinical symptoms of A. rhinosinusitis. This diagnosis should be considered in people with regular sinusitis or who are resistant to antibiotics. Oral lesions associated with Aspergillosis and other systemic mycoses can be considered dispersed diseases of the lungs. Irregular oral lesions may indicate the spread of an adjacent structure, such as the maxillary sinus, or a significant infection of the oral mucosa [115]. In the first stage of Aspergillosis, marginal growth areas appear to contain degraded epithelium and infiltrate fungal hyphae in the connective tissue. In the next stage, the previous lesions change to necrotic gray lesions and spread by attachment to the gums by ulceration and pseudomembrane. Invasion of the arteries is found at the base of these wounds. In the last stage, progressive damage to the alveolar bone and muscles is characterized by histopathological evidence of the penetration of fungal hyphae around the face [116]. Poor outcomes were associated with cases of older age, bone marrow transplantation, high sequential organ failure assessment (SOFA) score, and mechanical ventilation [112].
5.3. Diagnosis
To diagnose Aspergilloma, chest radiographs are still a suitable imaging technique that shows a round solid body enclosed in a radiolucent crescent in the upper part of the lung (bilateral and multiple). Thin-section chest computed tomography (MDCT), multiple incision (MSCT), spiral computed tomography (CT), and high-resolution CT at the optimal dose are suitable methods for patients at risk of IA. In the early stages of IA analysis, CT lung angiography can show vascular occlusion at the level of a suspected fungal lesion [117]. Additionally, microscopic examination and culture should be performed in patients at risk for IA. Culture is not a specific and appropriate diagnostic marker, while sputum culture is positive for Aspergillus in half of the patients with Aspergilloma. In the microscopic examination, it is essential to prove tissue attack by hyphae. The sensitivity of microscopic examination for IA is about 50% [118]. Evaluation of anti-Aspergillus antibodies by immunoblots and enzyme-linked immunosorbent assay (ELISA) methods is available as a robust and inexpensive method which is the reference method for serological diagnosis of chronic pulmonary Aspergillosis (CPA) [119].
5.4. Treatment
The standard doses of anti-fungi drugs recommended for treating IA may not be safe or effective for all patients. Then, high doses of drugs are commonly required in severe infectious diseases, treatment of difficult places, and infections caused by Aspergillus spp. with increased MIC. Patients with hematological malignancy at risk for IA are also managed by receiving initial prophylaxis or controlling biomarkers without receiving prophylaxis [120]. Oral-delivered Raziol treats CPA. All treatment instructions for the invasive Aspergillosis include using azoles, Amphotericin B (AmB), or echinocandin at appropriate doses with therapeutic evidence. However, in some regions, high rates of triazole resistance have been observed in A. fumigatus. In patients without previous exposure to antifungal therapies, a worrying resistance rate of 6% has been reported [108]. Recent developments in treating Aspergillosis are presented in Table 2.
6. Actinomyces
The genus Actinomyces spp. belongs to the typical human flora that can be found in the oropharynx, gastrointestinal tract, and urinary tract. It is one of the leading oral bacteria usually identifiable in healthy dental mucosa, dental plaque biofilm, periodontal lesions, and root rot. Actinomycosis resembles malignancy, tuberculosis, or nocardiosis in terms of its continuous and gradual spread [121]. The most common species in clinical conflicts is Actinomyces israelii. Actinomycosis infections can be associated with companion microbes inhibiting the host defense or reducing oxygen stress. The onset of Actinomycosis is likely to be multifactorial, and its association with mucosal cleavage is unpredictable. For example, minor trauma to the mucosa caused Actinomycosis in one patient, while no significant actinomycosis was observed in the large ruptures of the mouth [122].
6.1. Epidemiology
In 60% of all patients, Lmpy jaw syndrome (or action) is associated with odontogenic infection. The most common clinical form is cervicofacial Actinomycosis, and the most prevalent species are A. israeli and A. gerencseriae, A. naeslundii, A. viscosus, P. propionicum, A. gerencseriae, and A. odontolyticus [122]. Actinomycosis is more common in rural areas, men, and middle-aged people (50–30 years). The mortality rate is between 0 and 28% [123].
6.2. Risk Factors
Actinomycosis is associated with dental procedures. Diabetic patients are more likely to get infections because they have structural changes in their tissues and have impaired wound healing. Tumors, surgery, and radiation may also cause local tissue damage to spread into this infection [124].
6.3. Clinical Presentation
Complete vascularization of mucosal tissues and their replacement by weakly irritated tissue in actinomycetes supports its growth and provides adequate oxygen pressure. In necrotic foci, filamentous “sulfur” granules spread as a “sunburst radiation”. The ends of these granules can form extensions or rosettes due to the adhesion of neutrophils [123]. Cervicofacial clinical symptoms, which may last from 4 days to 1 year before diagnosis, include irregularly painful soft-tissue swelling of the submandibular or perimandibular area and emptying of the sinus ducts with sulfur granules, chewing problems, and recurrent and chronic infection [123]. In about 10% of patients, the bone is involved. Chronic infection can lead to osteomyelitis of the jawbone. Osteomyelitis due to cervicofacial Actinomycosis can spread to the lungs, gastrointestinal tract, tongue, sinuses, middle ear, larynx, ciliary tract, and thyroid gland [125].
6.4. Diagnosis
The best diagnoses are histological examination and bacterial culture of abscesses or suspected tissue. Staining sulfur granules with hematoxylin–eosin turns them into round basophil masses containing eosinophilic terminal clubs. Prescribing antimicrobial drugs leading to false negative culture results may cause anemia, mild leucocytosis, increased erythrocyte sedimentation rate, and increased C-reactive rutin value. Increased alkaline phosphatase concentrations may be seen in patients with hepatic Actinomycosis [126]. The blood test is a nonspecific diagnostic method for this disease. Imaging features are nonspecific and non-diagnostic in the early stages and may even be related to other inflammatory processes or neoplasms. Although cross-sectional imaging with CT or magnetic resonance imaging (MRI) does not provide accurate or diagnostic information, it can provide accurate anatomical information for sampling. Regional lymphadenopathy is rare in these patients. In later stages, infiltration of the surrounding tissues may be observed that is not diagnostic again. An aspiration biopsy should be performed in oscillating abscesses to examine the pus in the sulfur granules [127].
6.5. Treatment
Depending on the infection course, the course of antibiotics determines the clinical manifestations and response in Actinomycosis. The treatment is experimental because no similar success has been achieved with any antibiotic. The use of high doses of intravenous antibiotics for 2–6 weeks or 6–12 months orally is the primary treatment [128]. Acute lesions are often treated with tooth extractions, abscess drainage, and antibiotics for 2–3 weeks (penicillin). The penetration of antibiotics into the lesion may be delayed by weak vessels and solid capsules. Surgical interventions such as bone necrosis removal are performed for subacute or chronic voluminous lesions [129]. The recent treatments for Actinomycosis are summarized in Table 3.
Table 3.
Recent developments in treating bacterial infections.
| Species | Sample | Intervention | Outcomes | Ref. Year |
|---|---|---|---|---|
| S. mutans | Healthy subjects | Chlorhexidine and garlic extract mouthwash | Garlic extract inhibited S. mutans in both in vitro and in vivo studies. | [130] 2010 |
| A. gerencseriae | Patients with aggressive periodontitis | Systemic azithromycin | Azithromycin could slightly reduce the subgingival periodontal pathogens | [131] 2012 |
| Actinomyces spp. | Smoker and non-smoker subjects | Metronidazole and Amoxicillin | The non-smokers showed the lowest proportions of the orange complex and a meaningful increase in the proportions of Actinomyces species. | [132] 2013 |
| S. mutans | Children with decayed, missing, or filled teeth | Propolis and xylitol chewing gums | Both gums reduced the bacterial saliva load suggesting them an anti-cariogenic agent. | [133] 2014 |
|
Lactobacillus spp. Actinomyces naeslundii S. mutans |
Healthy adult subjects | Beverages containing apple fiber and polyphenols from boysenberry | The apple-boysenberry beverage exerted the most reduction on the colonization and biofilm adhesion. | [134] 2017 |
| S. mutans | Adolescent subjects with disabilities | Xylitol gum | The xylitol gum significantly reduced the caries rate. | [73] 2017 |
| S. mutans | Young subjects | Mouthwashes containing chlorhexidine, xylitol, and chlorhexidine + xylitol | All mouthwashes effectively reduced plaque, gingivitis, and bacterial saliva level. | [135] 2017 |
|
S. pseudopneumoniae
A. odontolyticus |
Adults with bronchiectasis | Erythromycin | The intervention significantly decreased the oropharyngeal microbiota composition. | [136] 2018 |
|
A. actinomycetemcomitans
A. naeslundii A. viscosus E. faecalis E. coli L. casei S. oralis S. sanguinis C. albicans |
In vitro study | Several flavonoids | Among the eight tested flavonoids, morin was the most effective; however other four flavonoids, including luteolin, naringin, quercetin, and rutin, could also decrease bacterial and fungal growth. | [137] 2019 |
|
A. israelii
E. faecium F. nucleatum L. gasseri S. mutans V. parvula |
In vitro study | Curcumin, protoporphyrin IX, resazurin, riboflavin, and light irradiation | All tested agents decreased the oral bacterial growth. | [138] 2019 |
|
E. faecalis
S. gordonii A. naeslundii L. acidophilus |
In vitro study | Dimethylaminododecyl methacrylate (DMADDM) and EndoREZ | The two tested sealers showed similar cytotoxicity, apical sealing ability, and solubility; however, DMADDM showed different properties at a mass fraction of 5%. | [139] 2019 |
|
S. oralis
A. naeslundii V. parvula F. nucleatum P. gingivalis A. actinomycetemcomitans |
In vitro study | Red wine, dealcoholized red wine, polyphenols-rich extracts from wine, and polyphenols-rich extracts from grape seeds | Conventional and dealcoholized red wine reduced the bacteria load within the biofilm, especially about P. gingivalis and A. actinomycetemcomitans. | [140] 2019 |
|
S. mutans
A. naeslundii |
In vitro study | Surface pre-reacted glass-ionomer filler in a resin-based composite incorporated with 2-methacryloyloxyethyl phosphorylcholine | The polymer added in the filler composite inhibited bacterial attachment and biofilm growth. | [141] 2019 |
|
A. naeslundii
E. faecalis |
Extracted single-rooted human mandibular first premolars | Platelet-rich fibrin scaffold with or without a 3-antibiotic mixture containing minocycline, metronidazole, and ciprofloxacin | The combination of scaffold and antibiotic mixture showed the highest antibacterial activity. | [142] 2020 |
|
S. mutans
L. casei A. naeslundii |
Human mandibular third molars | Diode laser and 2% chlorhexidine gluconate solution | All three cariogenic bacteria were affected by a diode. | [143] 2020 |
|
S. oralis
A. naeslundii V. parvula F. nucleatum P. gingivalis A. actinomycetemcomitans |
In vitro study in a subgingival biofilm model | Doxycycline, zinc, and calcium doped polymeric nanostructured membrane that is non-resorbable | The nanostructured membrane significantly reduced the biofilm growth dynamics and bacterial load. | [144] 2020 |
|
S. mutans
S. gordonii S. sobrinus A. naeslundii F. nucleatum A. actinomycetemcomitans P. gingivalis E. faecalis |
In vitro study in planktonic culture | Fruit juices derived from blackcurrant, redcurrant, cranberry, and raspberry | Blackcurrant, redcurrant, and cranberry juices had the most suppressing effect on bacterial growth, respectively, while raspberry only significantly suppressed the growth of P. gingivalis. | [53] 2020 |
| S. mutans | In vitro study on extracted teeth | A composite of nano-calcium fluoride and dimethylaminohexadecyl methacrylate | The composite showed promising fluoride release features and antibacterial functions. | [145] 2020 |
|
E. faecalis
S. mutans A. israelii |
In vitro study | Three licorice-derived polyphenols and cinnamon oil | The tested natural plant-derived compounds showed promising root canal disinfection properties. | [146] 2020 |
|
S. mutans
S. sobrinus A. viscosus L. acidophilus |
In vitro study | Caffeic acid phenethyl ester | The tested agent exerted high bactericidal and inhibitory activities against biofilms, cariogenic bacteria, and their virulence. | [147] 2020 |
|
S. mutans
A. naeslundii |
Human dentin blocks Periodontitis animal model |
Surface pre-reacted glass-ionomer nanofillers | The tested nanofiller coating showed antibacterial effects on the tooth surfaces and improved the clinical parameters of periodontitis. | [148] 2021 |
| S. sanguinis | In vitro study | The concentration of H2O2 | It has been shown that S. sanguinis evades neutrophil killing in vitro and counteracts innate immunity by the action of SpxB in collected blood | [149] 2017 |
| S. salivarius | Induced oral mucositis by experimental radiation in mice | The mouse oral cavity was treated daily with S. salivarius K12 | Cancer patients receiving radiotherapy may benefit from S. salivarius K12 as an adjuvant treatment. | [150] 2021 |
| S. salivarius | Primary human gingival fibroblasts | Pathogen-induced fibroblasts were treated with S. salivarius M18K12, K12, and fractions of its supernatant and whole-cell lysate | Periodontal disease pathogens were prevented from activating the immune system by S.salivarius M18 and K12. After chewing gum was administered with S. salivarius K12, the salivary microbiome and immune system did not change. | [151] 2021 |
| S. sanguinis | In vitro study | Measurement of SsaACB manganese transporter | In acidic conditions, SK36 mutants lacking SsaACB display reduced growth and manganese uptake. S. sanguinis may have a variety of manganese transporters due to the heterogeneity of its oral environment. | [152] 2022 |
| C. albicans, S. aureus and P. aeruginosa | In vitro study | Pomegranate (PomeGr) and microRepair (MicroR) | There were similarities in the effects of MicroR and PomeGr; however, the effectiveness of the two, given separately or in combination, varied based on which microbial agent was being treated. | [153] 2022 |
7. Streptococcus mutans
S. mutans lives in the mouth, specifically on dental plaque. Its importance is for involvement in the etiology of dental caries and its possible association with subacute infective endocarditis. Studies have shown that S. mutans is a major cause of tooth decay because of its ability to make large amounts of organic acids and activity at low pH compared to other species [154,155,156]. Through pathogenesis, S. mutans develop a biofilm starting by attachment of the initial pioneer species followed by colonization, co-adhesion, and co-aggregation of other species. Then, the bacteria produce extracellular polysaccharides, separate from the biofilm surface, and spread in the oral cavity environment [157]. S. mutans produces a sticky glucan by the action of glucosyltransferases (GTF) on sucrose that helps bacteria tight binding to the tooth surface. This binding allows bacteria to withstand rapid and frequent environmental fluctuations such as nutrient access, aerobic to anaerobic transfer, and pH changes. S. mutans also produces other virulence factors, including glucan-binding (Gbp) proteins and antigenic cell surface protein (PAc). PAc is in contact with salivary glands and plays an essential role in bacterial adhesion to tooth surfaces [158].
7.1. Epidemiology
Permanent tooth decay did not change according to age standards between 1990 and 2010 and peaked between 25 and 70, respectively. No significant differences were observed in terms of gender. Untreated tooth decay is the most common health condition worldwide. Studies have shown that the prevalence of early childhood caries is worrying in various regions worldwide [159].
7.2. Clinical Presentation
Tooth decay, the leading cause of tooth loss, is a multifactorial, infectious, and transmissible disease [160]. According to plaque-specific plaque (SPH) hypotheses, certain Gram-positive acidogenic and aciduric bacteria, including S. mutans and S. obrinus are typical infective dental plaques causing tooth decay as a biofilm-mediated disease in humans [161]. Environmental conditions such as regular daily sugar intake or salivary dysfunction increase the aciduric/acidogenic oral microbiome. As the lesions spread, the physiological balance between the tooth mineral and the biofilm fluid is disturbed, moving toward demineralization [162].
7.3. Diagnosis
Caries is diagnosed by visual and tactile dental examination. Alternative methods, including illumination-based methods such as optical coherence tomography [71], near-infrared [116], and fiber-optic technology, are also available [163]. In addition, the quantitative fluorescence light (QLF) devices, categorized by red, blue, and green labels based on the various wavelengths they generate, can be used in the early stages of caries [164]. Another method is an electronic caries monitor (ECM) that measures the bulk resistance of dental tissue. Material properties such as porosity, contact area, tissue thickness, enamel hydration, and ionic content of tooth fluids determine its electrical conductivity. Visual and radiographic assessments are used alongside other methods such as Diagnodent, ECM, or QLF. However, it is unclear whether such methods can be used as a standard tool in diagnosing tooth decay [165].
7.4. Treatment
First, biofilm management should be considered before tissue removal [166]. Patients are advised to consume less fermentable carbohydrates to correct the environmental pressures responsible for plaque biofilm dysbiosis [167]. Recent therapeutic advances are shown in Table 3.
8. Streptococcus sanguinis
S. sanguinis is a member of the Streptococcus family and a Gram-positive and facultative anaerobe. Similar to other streptococci, S. sanguinis divides along a single axis. According to reports, S.sanguinis is nonmotile. S.sanguinis use several carbohydrate sources to sustain itself. During the eruption of the first teeth of toddlers, S. sanguinis colonizes the oral cavity. Streptococcus species, however, have been reported to form biofilm during the first four to eight hours following biofilm formation. Their colonization of enamel is pioneering, particularly that of the mitis. As a result of refraining from using a toothbrush for some time, Streptococcus spp. colonizes the enamel more quickly, which could contribute to its cariogenic nature. S. sanguinis may colonize a mature biofilm at different rates, resulting in different cariogenic traits [168].
8.1. Epidemiology
Commensal bacteria such as S. sanguinis are common in the mouth. In human saliva, it can be found on tooth surfaces and the surface of the oral mucosa. In both supragingival and subgingival plaque, S. sanguinis thrives as an anaerobic species. Despite similar plaque mass, S. sanguinis biomass can differ substantially at different tooth locations. Teeth with lower incisors/canines have a high proportion of it, but upper molars with low proportions. Various dental implant surfaces have also been shown to form biofilms due to S. sanguinis [169].
8.2. Mechanism of Action
In general, S. sanguinis and S. gordonii are less acid-tolerant than S. mutans, but they contain arginine deiminases, which produce ammonia and provide ATP when exposed to acidic conditions. This system improves the survival and persistence of these organisms. Researchers have found that bacterial uptake and catabolism of specific carbohydrates can affect H2O2 and AD production by these commensals [170].
8.3. Clinical Importance
Dental caries has previously been shown to be prevented by S. sanguinis. For many years, S. mutans and humans have been antagonistic. There is a significant correlation between early S. sanguinis colonization and later S. mutans colonization. S. sanguinis levels decrease after S. mutans colonization. The inhibiting ability of S. sanguinis strains against Prevotella intermedia BS6 was found in at least one-third of the strains tested. As a result of hydrogen peroxide production by S. sanguinis, A. actinomycetemcomitans cannot grow in vitro [171]. Microbial and HSP epitope mimicry and microbial and HSP colonization of the oral mucosa have been proposed to elicit immunity and autoreactive T-cell clones. HSP stimulates adaptive and natural immune responses. Several autoimmune diseases, such as Behcet’s disease, have been linked to oral bacteria, including S. sanguinis [172].
8.4. Diagnosis
It has been primarily physiological and biochemical characteristics used to identify S. sanguinis in the past. Nevertheless, phenotypic identification methods and investigators differed in reliability and reproducibility. Previously, genotypic and phenotypic methods did not accurately identify clinical S. sanguinis isolates. To identify S. sanguinis and other oral bacteria, other methods, such as PCR with nucleic acid probes, are being investigated. [173].
9. Conclusions
Today, protecting and adequately repairing the tooth structure is the most critical approach to caries management. Successful clinical management of dental caries requires a good biological understanding of the disease process and the associated microbiome. Current approaches are based on the International Caries Consensus Collaboration (ICCC) recommendations, which state that tooth decay is a biofilm disease. In this regard, the literature states that biofilm management should be focused on before tissue removal to prevent the formation of new lesions and control the previous lesions [166]. Then, an understanding of microbiology, anatomy, pharmacology, wound healing, and oral surgery is required to manage acute dental infections. Today, the natural balance of the oral microbiome can be altered by lifestyle. The clinical goal in these patients is to establish this balance.
Despite treatment according to protocols, severe infections can be life-threatening. Therefore, using the idea of oral microbiome balance is essential for patients and healthcare professionals. The first approach is to maintain health rather than disease management. In preventing and diagnosing oral infections, healthcare providers can be very effective with activities such as controlling infections according to new protocols, educating patients, raising awareness about proper nutrition and uncontrolled sexual relationships, and motivating regular checkups. Early detection of infection and pathogens helps reduce oral or general infection. Identifying all aspects that cause antimicrobial resistance, immune system volatility profiles, potential mutations, and genotype differences should be examined in managing these infections. Timely management prevents complications in the patient and prevents the spread of the disease to others. In addition to their skills in treating these infections, clinicians need evidence-based knowledge about the pros and cons of any treatment.
10. Future Directions
It is suggested to study the mechanisms controlling the fate and function of infected tissues. Meta-analysis studies and robust trials with long follow-up periods should be performed, considering individual differences and other clinical limitations. Using the results of these studies, develop new treatments and approaches for tooth decay or damage to teeth and orofacial tissues. Several strategies have been used to prevent and manage oral infections in some not-yet-published current clinical trials. Genetics is also suggested as an important underlying factor that can affect the spread of infection and the immune response. Today, with the advancement of modern imaging systems and rigorous laboratory experiments, researchers can examine their treatment methods and disagreements in a shorter time.
Acknowledgments
The authors would like to acknowledge the valuable comments given by colleagues.
Author Contributions
E.T., A.K., M.A., K.A., S.R., F.N., M.Y., H.T., A.H. and G.V.O.F. were involved in the study design, collection of data, and Writing—original draft. E.T., A.K., M.A., K.A., S.R., F.N., M.Y., H.T., A.H. and G.V.O.F. were involved in helping in writing the review article and critically reviewing the data. All authors have reviewed and accepted the final draft and are in charge of the content and similarity index of the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This article is a review and does not contain any studies with humans or animals performed by any authors.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that they have no competing interests.
Funding Statement
There was no financial support.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Santosh A.B., Reddy B.V. Oral Mucosal Infections: Insights into Specimen Collection and Medication Management. Dent. Clin. N. Am. 2017;61:283–304. doi: 10.1016/j.cden.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Coll P.P., Lindsay A., Meng J., Gopalakrishna A., Raghavendra S., Bysani P., O’Brien D. The Prevention of Infections in Older Adults: Oral Health. J. Am. Geriatr. Soc. 2020;68:411–416. doi: 10.1111/jgs.16154. [DOI] [PubMed] [Google Scholar]
- 3.Gopalakrishnan U., Murthy R.T., Felicita A.S., Alshehri A., Awadh W., Almalki A., Vinothkumar T.S., Baeshen H.A., Bhandi S., Kathir A., et al. Sulfate-Reducing Bacteria in Patients Undergoing Fixed Orthodontic Treatment. Int. Dent. J. 2022 doi: 10.1016/j.identj.2022.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heboyan A., Avetisyan A., Skallevold H.E., Rokaya D., Marla V., Vardanyan A. Occurrence of Recurrent Aphthous Stomatitis (RAS) as a Rare Oral Manifestation in a Patient with Gilbert’s Syndrome. Case Rep. Dent. 2021;2021:6648729. doi: 10.1155/2021/6648729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heboyan A., Karobari M.I., Marya A. Possible oral manifestation after vaccination against COVID-19: A case report. Oxf. Med. Case Rep. 2022;2022:omac136. doi: 10.1093/omcr/omac136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heboyan A., Manrikyan M., Zafar M.S., Rokaya D., Nushikyan R., Vardanyan I., Vardanyan A., Khurshid Z. Bacteriological Evaluation of Gingival Crevicular Fluid in Teeth Restored Using Fixed Dental Prostheses: An In Vivo Study. Int. J. Mol. Sci. 2021;22:5463. doi: 10.3390/ijms22115463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abbasi K., Tavakolizadeh S., Hadi A., Hosseini M., Soufdoost R.S., Heboyan A., Alam M., Fani-Hanifeh S. The wound healing effect of collagen/adipose-derived stem cells (ADSCs) hydrogel: In vivo study. Vet. Med. Sci. 2022. online ahead of print . [DOI] [PMC free article] [PubMed]
- 8.Dahlén G. Bacterial infections of the oral mucosa. Periodontol. 2000. 2009;49:13–38. doi: 10.1111/j.1600-0757.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 9.Yazdanian M., Rahmani A., Tahmasebi E., Tebyanian H., Yazdanian A., Mosaddad S.A. Current and advanced nanomaterials in dentistry as regeneration agents: An update. Mini-Rev. Med. Chem. 2021;21:899–918. doi: 10.2174/1389557520666201124143449. [DOI] [PubMed] [Google Scholar]
- 10.Ogle O.E. Odontogenic Infections. Dent. Clin. N. Am. 2017;61:235–252. doi: 10.1016/j.cden.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Karobari M.I., Siddharthan S., Adil A.H., Khan M.M., Venugopal A., Rokaya D., Heboyan A., Marya C.M., Marya A. Modifiable and non-modifiable risk factors affecting oral and periodontal health and quality of life in south asia. Open Dent. J. 2022;16:e187421062209270. doi: 10.2174/18742106-v16-e2209270. [DOI] [Google Scholar]
- 12.Marya A., Rokaya D., Heboyan A., Fernandes G.V. Biomolecular and Biochemical Aspects of the Oral Cavity. Molecules. 2022;27:8676. doi: 10.3390/molecules27248676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hussain A., Tebyaniyan H., Khayatan D. The Role of Epigenetic in Dental and Oral Regenerative Medicine by Different Types of Dental Stem Cells: A Comprehensive Overview. Stem Cells Int. 2022;2022:5304860. doi: 10.1155/2022/5304860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramzan M., Karobari M.I., Heboyan A., Mohamed R.N., Mustafa M., Basheer S.N., Desai V., Batool S., Ahmed N., Zeshan B. Synthesis of Silver Nanoparticles from Extracts of Wild Ginger (Zingiber zerumbet) with Antibacterial Activity against Selective Multidrug Resistant Oral Bacteria. Molecules. 2022;27:2007. doi: 10.3390/molecules27062007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Srimaneepong V., Heboyan A., Zafar M.S., Khurshid Z., Marya A., Fernandes G.V.O., Rokaya D. Fixed Prosthetic Restorations and Periodontal Health: A Narrative Review. J. Funct. Biomater. 2022;13:15. doi: 10.3390/jfb13010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aurelius E., Franzen-Röhl E., Glimåker M., Akre O., Grillner L., Jorup-Rönström C., Studahl M., Group H.-M.S. Long-term valacyclovir suppressive treatment after herpes simplex virus type 2 meningitis: A double-blind, randomized controlled trial. Clin. Infect. Dis. 2012;54:1304–1313. doi: 10.1093/cid/cis031. [DOI] [PubMed] [Google Scholar]
- 17.Schang L.M. Timing Is Everything. mBio. 2018;9:e02140-17. doi: 10.1128/mBio.02140-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whitley R.J. Herpes Simplex Virus Infections of the Central Nervous System. Continuum. 2015;21:1704–1713. doi: 10.1212/con.0000000000000243. [DOI] [PubMed] [Google Scholar]
- 19.Kukhanova M.K., Korovina A.N., Kochetkov S.N. Human herpes simplex virus: Life cycle and development of inhibitors. Biochem. Biokhimiia. 2014;79:1635–1652. doi: 10.1134/S0006297914130124. [DOI] [PubMed] [Google Scholar]
- 20.Pires de Mello C.P., Bloom D.C., Paixão I.C. Herpes simplex virus type-1: Replication, latency, reactivation and its antiviral targets. Antivir. Ther. 2016;21:277–286. doi: 10.3851/IMP3018. [DOI] [PubMed] [Google Scholar]
- 21.Levin M.J., Weinberg A., Schmid D.S. Herpes Simplex Virus and Varicella-Zoster Virus. Microbiol. Spectr. 2016:4. doi: 10.1128/microbiolspec.DMIH2-0017-2015. [DOI] [PubMed] [Google Scholar]
- 22.Khadr L., Harfouche M., Omori R., Schwarzer G., Chemaitelly H., Abu-Raddad L.J. The Epidemiology of Herpes Simplex Virus Type 1 in Asia: Systematic Review, Meta-analyses, and Meta-regressions. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2019;68:757–772. doi: 10.1093/cid/ciy562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Betz D., Fane K. StatPearls. StatPearls Publishing LLC.; Treasure Island, FL, USA: 2021. Herpetic Whitlow. StatPearls Publishing Copyright © 2021. [PubMed] [Google Scholar]
- 24.Damour A., Garcia M., Seneschal J., Lévêque N., Bodet C. Eczema Herpeticum: Clinical and Pathophysiological Aspects. Clin. Rev. Allergy Immunol. 2020;59:1–18. doi: 10.1007/s12016-019-08768-3. [DOI] [PubMed] [Google Scholar]
- 25.Parra-Sánchez M. Genital ulcers caused by herpes simplex virus. Enferm. Infecc. Y Microbiol. Clin. 2019;37:260–264. doi: 10.1016/j.eimc.2018.10.020. [DOI] [PubMed] [Google Scholar]
- 26.Corstjens P.L., Abrams W.R., Malamud D. Saliva and viral infections. Periodontol. 2000. 2016;70:93–110. doi: 10.1111/prd.12112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Balasubramaniam R., Kuperstein A.S., Stoopler E.T. Update on oral herpes virus infections. Dent. Clin. N. Am. 2014;58:265–280. doi: 10.1016/j.cden.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 28.Samies N.L., James S.H. Prevention and treatment of neonatal herpes simplex virus infection. Antivir. Res. 2020;176:104721. doi: 10.1016/j.antiviral.2020.104721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schnitzler P. Essential Oils for the Treatment of Herpes Simplex Virus Infections. Chemotherapy. 2019;64:1–7. doi: 10.1159/000501062. [DOI] [PubMed] [Google Scholar]
- 30.Venturi C.R., Danielli L.J., Klein F., Apel M.A., Montanha J.A., Bordignon S.A., Roehe P.M., Fuentefria A.M., Henriques A.T. Chemical analysis and in vitro antiviral and antifungal activities of essential oils from Glechon spathulata and Glechon marifolia. Pharm. Biol. 2015;53:682–688. doi: 10.3109/13880209.2014.936944. [DOI] [PubMed] [Google Scholar]
- 31.Ang K.K., Harris J., Wheeler R., Weber R., Rosenthal D.I., Nguyen-Tân P.F., Westra W.H., Chung C.H., Jordan R.C., Lu C., et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N. Engl. J. Med. 2010;363:24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joura E.A., Garland S.M., Paavonen J., Ferris D.G., Perez G., Ault K.A., Huh W.K., Sings H.L., James M.K., Haupt R.M. Effect of the human papillomavirus (HPV) quadrivalent vaccine in a subgroup of women with cervical and vulvar disease: Retrospective pooled analysis of trial data. BMJ. 2012;344:e1401. doi: 10.1136/bmj.e1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perti T., Saracino M., Baeten J.M., Johnston C., Diem K., Ocbamichael N., Huang M.L., Selke S., Magaret A., Corey L., et al. High-dose valacyclovir decreases plasma HIV-1 RNA more than standard-dose acyclovir in persons coinfected with HIV-1 and HSV-2: A randomized crossover trial. J. Acquir. Immune Defic. Syndr. 2013;63:201–208. doi: 10.1097/QAI.0b013e3182928eea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Wagoner N., Geisler W.M., Bachmann L.H., Hook E.W. The effect of valacyclovir on HIV and HSV-2 in HIV-infected persons on antiretroviral therapy with previously unrecognised HSV-2. Int. J. STD AIDS. 2015;26:574–581. doi: 10.1177/0956462414546504. [DOI] [PubMed] [Google Scholar]
- 35.Le Cleach L., Trinquart L., Do G., Maruani A., Lebrun-Vignes B., Ravaud P., Chosidow O. Oral antiviral therapy for prevention of genital herpes outbreaks in immunocompetent and nonpregnant patients. Cochrane Database Syst. Rev. 2014;8:Cd009036. doi: 10.1002/14651858.CD009036.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Donatini B. Control of oral human papillomavirus (HPV) by medicinal mushrooms, Trametes versicolor and Ganoderma lucidum: A preliminary clinical trial. Int. J. Med. Mushrooms. 2014;16:497–498. doi: 10.1615/IntJMedMushrooms.v16.i5.80. [DOI] [PubMed] [Google Scholar]
- 37.Trimble C.L., Morrow M.P., Kraynyak K.A., Shen X., Dallas M., Yan J., Edwards L., Parker R.L., Denny L., Giffear M., et al. Safety, efficacy, and immunogenicity of VGX-3100, a therapeutic synthetic DNA vaccine targeting human papillomavirus 16 and 18 E6 and E7 proteins for cervical intraepithelial neoplasia 2/3: A randomised, double-blind, placebo-controlled phase 2b trial. Lancet. 2015;386:2078–2088. doi: 10.1016/S0140-6736(15)00239-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wald A., Timmler B., Magaret A., Warren T., Tyring S., Johnston C., Fife K., Selke S., Huang M.L., Stobernack H.P., et al. Effect of Pritelivir Compared With Valacyclovir on Genital HSV-2 Shedding in Patients With Frequent Recurrences: A Randomized Clinical Trial. JAMA. 2016;316:2495–2503. doi: 10.1001/jama.2016.18189. [DOI] [PubMed] [Google Scholar]
- 39.Guo X., Qiu L., Wang Y., Wang Y., Wang Q., Song L., Li Y., Huang K., Du X., Fan W., et al. A randomized open-label clinical trial of an anti-HPV biological dressing (JB01-BD) administered intravaginally to treat high-risk HPV infection. Microbes Infect. 2016;18:148–152. doi: 10.1016/j.micinf.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 40.Tyring S.K., Lee P., Hill G.T., Jr., Silverfield J.C., Moore A.Y., Matkovits T., Sullivan-Bolyai J. FV-100 versus valacyclovir for the prevention of post-herpetic neuralgia and the treatment of acute herpes zoster-associated pain: A randomized-controlled trial. J. Med. Virol. 2017;89:1255–1264. doi: 10.1002/jmv.24750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van Wagoner N., Fife K., Leone P.A., Bernstein D.I., Warren T., Panther L., Novak R.M., Beigi R., Kriesel J., Tyring S., et al. Effects of Different Doses of GEN-003, a Therapeutic Vaccine for Genital Herpes Simplex Virus-2, on Viral Shedding and Lesions: Results of a Randomized Placebo-Controlled Trial. J. Infect. Dis. 2018;218:1890–1899. doi: 10.1093/infdis/jiy415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mohseni A.H., Taghinezhad S.S., Keyvani H., Ghobadi N. Comparison of Acyclovir and Multistrain Lactobacillus brevis in Women with Recurrent Genital Herpes Infections: A Double-Blind, Randomized, Controlled Study. Probiotics Antimicrob. Proteins. 2018;10:740–747. doi: 10.1007/s12602-017-9320-8. [DOI] [PubMed] [Google Scholar]
- 43.Nofal A., Marei A., Ibrahim A.M., Nofal E., Nabil M. Intralesional versus intramuscular bivalent human papillomavirus vaccine in the treatment of recalcitrant common warts. J. Am. Acad. Dermatol. 2020;82:94–100. doi: 10.1016/j.jaad.2019.07.070. [DOI] [PubMed] [Google Scholar]
- 44.Peyman A., Nayebzadeh M., Peyman M., Afshari N.A., Pourazizi M. Topical cyclosporine-A versus prednisolone for herpetic stromal keratitis: A randomized controlled trial. Acta Ophthalmol. 2019;97:e194–e198. doi: 10.1111/aos.13913. [DOI] [PubMed] [Google Scholar]
- 45.De Rosa N., Giampaolino P., Lavitola G., Morra I., Formisano C., Nappi C., Bifulco G. Effect of Immunomodulatory Supplements Based on Echinacea Angustifolia and Echinacea Purpurea on the Posttreatment Relapse Incidence of Genital Condylomatosis: A Prospective Randomized Study. BioMed. Res. Int. 2019;2019:3548396. doi: 10.1155/2019/3548396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang Y., Meng Y.L., Duan S.M., Zhan S.B., Guan R.L., Yue T.F., Kong L.H., Zhou L., Deng L.H., Huang C., et al. REBACIN® as a noninvasive clinical intervention for high-risk human papillomavirus persistent infection. Int. J. Cancer. 2019;145:2712–2719. doi: 10.1002/ijc.32344. [DOI] [PubMed] [Google Scholar]
- 47.Tan D.H.S., Raboud J.M., Szadkowski L., Grinsztejn B., Madruga J.V., Figueroa M.I., Cahn P., Barton S.E., Clarke A., Fox J., et al. Effect of valaciclovir on CD4 count decline in untreated HIV: An international randomized controlled trial. J. Antimicrob. Chemother. 2019;74:480–488. doi: 10.1093/jac/dky433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Allen C.T., Lee S., Norberg S.M., Kovalovsky D., Ye H., Clavijo P.E., Hu-Lieskovan S., Schlegel R., Schlom J., Strauss J., et al. Safety and clinical activity of PD-L1 blockade in patients with aggressive recurrent respiratory papillomatosis. J. Immunother. Cancer. 2019;7:119. doi: 10.1186/s40425-019-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Breier A., Buchanan R.W., D’Souza D., Nuechterlein K., Marder S., Dunn W., Preskorn S., Macaluso M., Wurfel B., Maguire G., et al. Herpes simplex virus 1 infection and valacyclovir treatment in schizophrenia: Results from the VISTA study. Schizophr. Res. 2019;206:291–299. doi: 10.1016/j.schres.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 50.Luyt C.E., Forel J.M., Hajage D., Jaber S., Cayot-Constantin S., Rimmelé T., Coupez E., Lu Q., Diallo M.H., Penot-Ragon C., et al. Acyclovir for Mechanically Ventilated Patients With Herpes Simplex Virus Oropharyngeal Reactivation: A Randomized Clinical Trial. JAMA Intern. Med. 2020;180:263–272. doi: 10.1001/jamainternmed.2019.5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murray M.L., Meadows J., Doré C.J., Copas A.J., Haddow L.J., Lacey C., Jit M., Soldan K., Bennett K., Tetlow M., et al. Human papillomavirus infection: Protocol for a randomised controlled trial of imiquimod cream (5%) versus podophyllotoxin cream (0.15%), in combination with quadrivalent human papillomavirus or control vaccination in the treatment and prevention of recurrence of anogenital warts (HIPvac trial) BMC Med. Res. Methodol. 2018;18:125. doi: 10.1186/s12874-018-0581-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Syrjänen S. Oral manifestations of human papillomavirus infections. Eur. J. Oral Sci. 2018;126((Suppl. 1)):49–66. doi: 10.1111/eos.12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kranz S., Guellmar A., Olschowsky P., Tonndorf-Martini S., Heyder M., Pfister W., Reise M., Sigusch B. Antimicrobial Effect of Natural Berry Juices on Common Oral Pathogenic Bacteria. Antibiotics. 2020;9:533. doi: 10.3390/antibiotics9090533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crosbie E.J., Einstein M.H., Franceschi S., Kitchener H.C. Human papillomavirus and cervical cancer. Lancet. 2013;382:889–899. doi: 10.1016/S0140-6736(13)60022-7. [DOI] [PubMed] [Google Scholar]
- 55.Kumaraswamy K.L., Vidhya M. Human papilloma virus and oral infections: An update. J. Cancer Res. Ther. 2011;7:120–127. doi: 10.4103/0973-1482.82915. [DOI] [PubMed] [Google Scholar]
- 56.Rettig E.M., D’Souza G. Epidemiology of head and neck cancer. Surg. Oncol. Clin. N. Am. 2015;24:379–396. doi: 10.1016/j.soc.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 57.Gillison M.L., Chaturvedi A.K., Anderson W.F., Fakhry C. Epidemiology of Human Papillomavirus-Positive Head and Neck Squamous Cell Carcinoma. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015;33:3235–3242. doi: 10.1200/JCO.2015.61.6995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lerman M.A., Almazrooa S., Lindeman N., Hall D., Villa A., Woo S.B. HPV-16 in a distinct subset of oral epithelial dysplasia. Mod. Pathol. Off. J. U. S. Can. Acad. Pathol. Inc. 2017;30:1646–1654. doi: 10.1038/modpathol.2017.71. [DOI] [PubMed] [Google Scholar]
- 59.Antonsson A., Cornford M., Perry S., Davis M., Dunne M.P., Whiteman D.C. Prevalence and risk factors for oral HPV infection in young Australians. PLoS ONE. 2014;9:e91761. doi: 10.1371/journal.pone.0091761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Anderson K.S., Wong J., D’Souza G., Riemer A.B., Lorch J., Haddad R., Pai S.I., Longtine J., McClean M., LaBaer J., et al. Serum antibodies to the HPV16 proteome as biomarkers for head and neck cancer. Br. J. Cancer. 2011;104:1896–1905. doi: 10.1038/bjc.2011.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tezal M., Scannapieco F.A., Wactawski-Wende J., Hyland A., Marshall J.R., Rigual N.R., Stoler D.L. Local inflammation and human papillomavirus status of head and neck cancers. Arch. Otolaryngol. Head Neck Surg. 2012;138:669–675. doi: 10.1001/archoto.2012.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shipilova A., Dayakar M.M., Gupta D. High risk human papillomavirus in the periodontium: A case control study. J. Indian Soc. Periodontol. 2017;21:380–385. doi: 10.4103/jisp.jisp_56_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chai R.C., Lambie D., Verma M., Punyadeera C. Current trends in the etiology and diagnosis of HPV-related head and neck cancers. Cancer Med. 2015;4:596–607. doi: 10.1002/cam4.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pfaffe T., Cooper-White J., Beyerlein P., Kostner K., Punyadeera C. Diagnostic potential of saliva: Current state and future applications. Clin. Chem. 2011;57:675–687. doi: 10.1373/clinchem.2010.153767. [DOI] [PubMed] [Google Scholar]
- 65.Mayer F.L., Wilson D., Hube B. Candida albicans pathogenicity mechanisms. Virulence. 2013;4:119–128. doi: 10.4161/viru.22913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Metwalli K.H., Khan S.A., Krom B.P., Jabra-Rizk M.A. Streptococcus mutans, Candida albicans, and the human mouth: A sticky situation. PLoS Pathog. 2013;9:e1003616. doi: 10.1371/journal.ppat.1003616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Seifi Kafshgari H., Yazdanian M., Ranjbar R., Tahmasebi E., Mirsaeed S., Tebyanian H., Ebrahimzadeh M.A., Goli H.R. The effect of Citrullus colocynthis extracts on Streptococcus mutans, Candida albicans, normal gingival fibroblast and breast cancer cells. J. Biol. Res. 2019;92:8201. doi: 10.4081/jbr.2019.8201. [DOI] [Google Scholar]
- 68.Hellstein J.W., Marek C.L. Candidiasis: Red and white manifestations in the oral cavity. Head Neck Pathol. 2019;13:25–32. doi: 10.1007/s12105-019-01004-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hood S., Denning D. Treatment of fungal infection in AIDS. J. Antimicrob. Chemother. 1996;37:71–85. doi: 10.1093/jac/37.suppl_B.71. [DOI] [PubMed] [Google Scholar]
- 70.Reinhardt L., Nascente P., Ribeiro J., Guimarães V., Etges A., Lund R. Sensitivity to antifungals by Candida spp samples isolated from cases of chronic atrophic candidiasis (CAC) Braz. J. Biol. 2020;80:266–272. doi: 10.1590/1519-6984.190454. [DOI] [PubMed] [Google Scholar]
- 71.Benito-Cruz B., Aranda-Romo S., López-Esqueda F.J., de la Rosa-García E., Rosas-Hernández R., Sánchez-Vargas L.O. Oral Candida isolates and fluconazole susceptibility patterns in older Mexican women. Arch. Gerontol. Geriatr. 2016;65:204–210. doi: 10.1016/j.archger.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 72.Bhattacharya S., Sae-Tia S., Fries B.C. Candidiasis and mechanisms of antifungal resistance. Antibiotics. 2020;9:312. doi: 10.3390/antibiotics9060312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Watthanasaen S., Merchant A.T., Luengpailin S., Chansamak N., Pisek A., Pitiphat W. Xylitol-containing Chewing Gum for Caries Prevention in Students with Disabilities: A Randomised Trial. Oral Health Prev. Dent. 2017;15:519–527. doi: 10.3290/j.ohpd.a39668. [DOI] [PubMed] [Google Scholar]
- 74.Cabras M., Gambino A., Broccoletti R., Lodi G., Arduino P.G. Treatment of angular cheilitis: A narrative review and authors’ clinical experience. Oral Dis. 2020;26:1107–1115. doi: 10.1111/odi.13183. [DOI] [PubMed] [Google Scholar]
- 75.Alnuaimi A.D., Wiesenfeld D., O′Brien-Simpson N.M., Reynolds E.C., McCullough M.J. Oral Candida colonization in oral cancer patients and its relationship with traditional risk factors of oral cancer: A matched case-control study. Oral Oncol. 2015;51:139–145. doi: 10.1016/j.oraloncology.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 76.Awotiwon A.A., Johnson S., Rutherford G.W., Meintjes G., Eshun-Wilson I. Primary antifungal prophylaxis for cryptococcal disease in HIV-positive people. Cochrane Database Syst. Rev. 2018;8:Cd004773. doi: 10.1002/14651858.CD004773.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Patel M., Shackleton J.-A., Coogan M.M., Galpin J. Antifungal effect of mouth rinses on oral Candida counts and salivary flow in treatment-naïve HIV-infected patients. AIDS Patient Care STDs. 2008;22:613–618. doi: 10.1089/apc.2007.0160. [DOI] [PubMed] [Google Scholar]
- 78.Arya N.R., Rafiq N.B. StatPearls. StatPearls Publishing LLC.; Treasure Island, FL, USA: 2021. Candidiasis. StatPearls Publishing Copyright © 2021. [Google Scholar]
- 79.Custodio W., Silva W.J., Paes Leme A.F., Cury J.A., Del Bel Cury A.A. Plasma proteins in the acquired denture pellicle enhance substrate surface free energy and Candida albicans phospholipase and proteinase activities. J. Investig. Clin. Dent. 2015;6:273–281. doi: 10.1111/jicd.12101. [DOI] [PubMed] [Google Scholar]
- 80.Houšť J., Spížek J., Havlíček V. Antifungal drugs. Metabolites. 2020;10:106. doi: 10.3390/metabo10030106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gacon I., Loster J.E., Wieczorek A. Relationship between oral hygiene and fungal growth in patients: Users of an acrylic denture without signs of inflammatory process. Clin. Interv. Aging. 2019;14:1297–1302. doi: 10.2147/CIA.S193685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ishikawa K.H., Mayer M.P., Miyazima T.Y., Matsubara V.H., Silva E.G., Paula C.R., Campos T.T., Nakamae A.E. A multispecies probiotic reduces oral Candida colonization in denture wearers. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2015;24:194–199. doi: 10.1111/jopr.12198. [DOI] [PubMed] [Google Scholar]
- 83.Vento-Zahra E., De Wever B., Decelis S., Mallia K., Camilleri S. Randomized, double-blind, placebo-controlled trial to test the efficacy of nitradine tablets in maxillary removable orthodontic appliance patients. Quintessence Int. 2011;42:37–43. [PubMed] [Google Scholar]
- 84.Voskamp A.L., Gillman A., Symons K., Sandrini A., Rolland J.M., O’Hehir R.E., Douglass J.A. Clinical efficacy and immunologic effects of omalizumab in allergic bronchopulmonary aspergillosis. J. Allergy Clin. Immunol. Pract. 2015;3:192–199. doi: 10.1016/j.jaip.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 85.Kraft-Bodi E., Jørgensen M.R., Keller M.K., Kragelund C., Twetman S. Effect of Probiotic Bacteria on Oral Candida in Frail Elderly. J. Dent. Res. 2015;94:181s–186s. doi: 10.1177/0022034515595950. [DOI] [PubMed] [Google Scholar]
- 86.Colombari B., Tagliazucchi D., Odorici A., Pericolini E., Foltran I., Pinetti D., Meto A., Peppoloni S., Blasi E. Pomegranate Extract Affects Fungal Biofilm Production: Consumption of Phenolic Compounds and Alteration of Fungal Autoinducers Release. Int. J. Environ. Res. Public Health. 2022;19:4146. doi: 10.3390/ijerph192114146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ranawaka R.R., Nagahawatte A., Gunasekara T.A., Weerakoon H.S., de Silva S.H. Randomized, double-blind, comparative study on efficacy and safety of itraconazole pulse therapy and terbinafine pulse therapy on nondermatophyte mold onychomycosis: A study with 90 patients. J. Dermatol. Treat. 2016;27:364–372. doi: 10.3109/09546634.2015.1119781. [DOI] [PubMed] [Google Scholar]
- 88.Maertens J.A., Raad I.I., Marr K.A., Patterson T.F., Kontoyiannis D.P., Cornely O.A., Bow E.J., Rahav G., Neofytos D., Aoun M., et al. Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi (SECURE): A phase 3, randomised-controlled, non-inferiority trial. Lancet. 2016;387:760–769. doi: 10.1016/S0140-6736(15)01159-9. [DOI] [PubMed] [Google Scholar]
- 89.Sushma R., Sathe T.T., Farias A., Sanyal P.K., Kiran S. “Nature cures:” An alternative herbal formulation as a denture cleanser. Ann. Afr. Med. 2017;16:6–12. doi: 10.4103/aam.aam_43_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Atai Z., Atai M., Amini J., Salehi N. In vivo study of antifungal effects of low-molecular-weight chitosan against Candida albicans. J. Oral Sci. 2017;59:425–430. doi: 10.2334/josnusd.16-0295. [DOI] [PubMed] [Google Scholar]
- 91.Miyazima T.Y., Ishikawa K.H., Mayer M., Saad S., Nakamae A. Cheese supplemented with probiotics reduced the Candida levels in denture wearers-RCT. Oral. Dis. 2017;23:919–925. doi: 10.1111/odi.12669. [DOI] [PubMed] [Google Scholar]
- 92.Sandison T., Ong V., Lee J., Thye D. Safety and Pharmacokinetics of CD101 IV, a Novel Echinocandin, in Healthy Adults. Antimicrob. Agents Chemother. 2017;61:e01627-16. doi: 10.1128/AAC.01627-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Keller M.K., Kragelund C. Randomized pilot study on probiotic effects on recurrent candidiasis in oral lichen planus patients. Oral. Dis. 2018;24:1107–1114. doi: 10.1111/odi.12858. [DOI] [PubMed] [Google Scholar]
- 94.Mofatteh M.R., Naseripour Yazdi Z., Yousefi M., Namaei M.H. Comparison of the recovery rate of otomycosis using betadine and clotrimazole topical treatment. Braz. J. Otorhinolaryngol. 2018;84:404–409. doi: 10.1016/j.bjorl.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Agarwal R., Dhooria S., Singh Sehgal I., Aggarwal A.N., Garg M., Saikia B., Behera D., Chakrabarti A. A Randomized Trial of Itraconazole vs Prednisolone in Acute-Stage Allergic Bronchopulmonary Aspergillosis Complicating Asthma. Chest. 2018;153:656–664. doi: 10.1016/j.chest.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 96.de Senna A.M., Vieira M.M.F., Machado-de-Sena R.M., Bertolin A.O., Núñez S.C., Ribeiro M.S. Photodynamic inactivation of Candida ssp. on denture stomatitis. A clinical trial involving palatal mucosa and prosthesis disinfection. Photodiagnosis Photodyn. Ther. 2018;22:212–216. doi: 10.1016/j.pdpdt.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 97.Kullberg B.J., Viscoli C., Pappas P.G., Vazquez J., Ostrosky-Zeichner L., Rotstein C., Sobel J.D., Herbrecht R., Rahav G., Jaruratanasirikul S., et al. Isavuconazole Versus Caspofungin in the Treatment of Candidemia and Other Invasive Candida Infections: The ACTIVE Trial. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2019;68:1981–1989. doi: 10.1093/cid/ciy827. [DOI] [PubMed] [Google Scholar]
- 98.Saeed A., Haider A., Zahid S., Khan S.A., Faryal R., Kaleem M. In-vitro antifungal efficacy of tissue conditioner-chitosan composites as potential treatment therapy for denture stomatitis. Int. J. Biol. Macromol. 2019;125:761–766. doi: 10.1016/j.ijbiomac.2018.12.091. [DOI] [PubMed] [Google Scholar]
- 99.Afroozi B., Zomorodian K., Lavaee F., Zare Shahrabadi Z., Mardani M. Comparison of the efficacy of indocyanine green-mediated photodynamic therapy and nystatin therapy in treatment of denture stomatitis. Photodiagnosis Photodyn. Ther. 2019;27:193–197. doi: 10.1016/j.pdpdt.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 100.de Souza R.F., Silva-Lovato C.H., de Arruda C.N., Regis R.R., Zanini A.P., Longo D.L., Peracini A., de Andrade I.M., Watanabe E., Paranhos H.F. Efficacy of a propolis solution for cleaning complete dentures. Am. J. Dent. 2019;32:306–310. [PubMed] [Google Scholar]
- 101.Mustafa M.W., Ungphaiboon S., Phadoongsombut N., Pangsomboon K., Chelae S., Mahattanadul S. Effectiveness of an Alcohol-Free Chitosan-Curcuminoid Mouthwash Compared with Chlorhexidine Mouthwash in Denture Stomatitis Treatment: A Randomized Trial. J. Altern. Complement. Med. 2019;25:552–558. doi: 10.1089/acm.2018.0459. [DOI] [PubMed] [Google Scholar]
- 102.Tomioka H., Kaneda T., Kida Y., Kaneko M., Fujii H., Hayashi M., Tomii K., Tada K., Suzuki Y., Karino T. [An open, noncomparative multicenter study of the efficacy and safety of itraconazole injections and high dose capsules in chronic pulmonary aspergillosis] Kansenshogaku Zasshi J. Jpn. Assoc. Infect. Dis. 2011;85:644–651. doi: 10.11150/kansenshogakuzasshi.85.644. [DOI] [PubMed] [Google Scholar]
- 103.Mammen M.P., Armas D., Hughes F.H., Hopkins A.M., Fisher C.L., Resch P.A., Rusalov D., Sullivan S.M., Smith L.R. First-in-Human Phase 1 Study To Assess Safety, Tolerability, and Pharmacokinetics of a Novel Antifungal Drug, VL-2397, in Healthy Adults. Antimicrob. Agents Chemother. 2019;63:e00969-19. doi: 10.1128/AAC.00969-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Alrabiah M., Alsahhaf A., Alofi R.S., Al-Aali K.A., Abduljabbar T., Vohra F. Efficacy of photodynamic therapy versus local nystatin in the treatment of denture stomatitis: A randomized clinical study. Photodiagnosis Photodyn. Ther. 2019;28:98–101. doi: 10.1016/j.pdpdt.2019.08.028. [DOI] [PubMed] [Google Scholar]
- 105.Tasso C.O., de Oliveira Zoccolotti J., Ferrisse T.M., Malavolta I.F., Jorge J.H. Effectiveness of Disinfectant Liquid Soaps in the Reduction of Candida spp Present in Complete Dentures: A Crossover Randomized Clinical Trial. Int. J. Prosthodont. 2020;33:620–628. doi: 10.11607/ijp.6643. [DOI] [PubMed] [Google Scholar]
- 106.Doppalapudi R., Vundavalli S., Prabhat M.P. Effect of probiotic bacteria on oral Candida in head- and neck-radiotherapy patients: A randomized clinical trial. J. Cancer Res. Ther. 2020;16:470–477. doi: 10.4103/jcrt.JCRT_334_18. [DOI] [PubMed] [Google Scholar]
- 107.Jimenez-Garcia L., Celis-Aguilar E., Díaz-Pavón G., Muñoz Estrada V., Castro-Urquizo Á., Hernández-Castillo N., Amaro-Flores E. Efficacy of topical clotrimazole vs. topical tolnaftate in the treatment of otomycosis. A randomized controlled clinical trial. Braz. J. Otorhinolaryngol. 2020;86:300–307. doi: 10.1016/j.bjorl.2018.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Latgé J.-P., Chamilos G. Aspergillus fumigatus and Aspergillosis in 2019. Clin. Microbiol. Rev. 2019;33:e00140-18. doi: 10.1128/CMR.00140-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Obar J.J. Sensing the threat posed by Aspergillus infection. Curr. Opin. Microbiol. 2020;58:47–55. doi: 10.1016/j.mib.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Van De Veerdonk F.L., Gresnigt M.S., Romani L., Netea M.G., Latge J.-P. Aspergillus fumigatus morphology and dynamic host interactions. Nat. Rev. Microbiol. 2017;15:661. doi: 10.1038/nrmicro.2017.90. [DOI] [PubMed] [Google Scholar]
- 111.Bongomin F., Batac C., Richardson M.D., Denning D.W. A review of onychomycosis due to Aspergillus species. Mycopathologia. 2018;183:485–493. doi: 10.1007/s11046-017-0222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Heinekamp T., Schmidt H., Lapp K., Pähtz V., Shopova I., Köster-Eiserfunke N., Krüger T., Kniemeyer O., Brakhage A.A. Proceedings of Seminars in Immunopathology. Springer; Berlin/Heidelberg, Germany: 2015. Interference of Aspergillus fumigatus with the immune response; pp. 141–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Williams C., Rajendran R., Ramage G. Aspergillus biofilms in human disease. Fungal Biofilms Relat. Infect. 2016;931:1–11. doi: 10.1007/5584_2016_4. [DOI] [PubMed] [Google Scholar]
- 114.Rowe-Jones J.M., Moore-Gillon V. Destructive noninvasive paranasal sinus aspergillosis: Component of a spectrum of disease. J. Otolaryngol. 1994;23:92–96. [PubMed] [Google Scholar]
- 115.Chakrabarti A., Kaur H. Allergic aspergillus rhinosinusitis. J. Fungi. 2016;2:32. doi: 10.3390/jof2040032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Telles D.R., Karki N., Marshall M.W. Oral fungal infections: Diagnosis and management. Dent. Clin. 2017;61:319–349. doi: 10.1016/j.cden.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 117.Patterson T.F., Thompson G.R., III, Denning D.W., Fishman J.A., Hadley S., Herbrecht R., Kontoyiannis D.P., Marr K.A., Morrison V.A., Nguyen M.H. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016;63:e1–e60. doi: 10.1093/cid/ciw326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ullmann A.J., Aguado J.M., Arikan-Akdagli S., Denning D.W., Groll A.H., Lagrou K., Lass-Flörl C., Lewis R.E., Munoz P., Verweij P.E. Diagnosis and management of Aspergillus diseases: Executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin. Microbiol. Infect. 2018;24:e1–e38. doi: 10.1016/j.cmi.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 119.Page I.D., Richardson M.D., Denning D.W. Comparison of six Aspergillus-specific IgG assays for the diagnosis of chronic pulmonary aspergillosis (CPA) J. Infect. 2016;72:240–249. doi: 10.1016/j.jinf.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 120.Taccone F.S., Van den Abeele A.-M., Bulpa P., Misset B., Meersseman W., Cardoso T., Paiva J.-A., Blasco-Navalpotro M., De Laere E., Dimopoulos G. Epidemiology of invasive aspergillosis in critically ill patients: Clinical presentation, underlying conditions, and outcomes. Crit. Care. 2015;19:7. doi: 10.1186/s13054-014-0722-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kawashima J., Nakajo K., Washio J., Mayanagi G., Shimauchi H., Takahashi N. Fluoride-sensitivity of growth and acid production of oral Actinomyces: Comparison with oral Streptococcus. Microbiol. Immunol. 2013;57:797–804. doi: 10.1111/1348-0421.12098. [DOI] [PubMed] [Google Scholar]
- 122.Valour F., Sénéchal A., Dupieux C., Karsenty J., Lustig S., Breton P., Gleizal A., Boussel L., Laurent F., Braun E. Actinomycosis: Etiology, clinical features, diagnosis, treatment, and management. Infect. Drug Resist. 2014;7:183. doi: 10.2147/IDR.S39601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Boyanova L., Kolarov R., Mateva L., Markovska R., Mitov I. Actinomycosis: A frequently forgotten disease. Future Microbiol. 2015;10:613–628. doi: 10.2217/fmb.14.130. [DOI] [PubMed] [Google Scholar]
- 124.Wong V.K., Turmezei T., Weston V. Actinomycosis. BMJ. 2011;343:d6099. doi: 10.1136/bmj.d6099. [DOI] [PubMed] [Google Scholar]
- 125.Moghimi M., Salentijn E., Debets-Ossenkop Y., Karagozoglu K.H., Forouzanfar T. Treatment of cervicofacial actinomycosis: A report of 19 cases and review of literature. Med. Oral Patol. Oral Y Cir. Bucal. 2013;18:e627. doi: 10.4317/medoral.19124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Attaway A., Flynn T. Actinomyces meyeri: From “lumpy jaw” to empyema. Infection. 2013;41:1025–1027. doi: 10.1007/s15010-013-0453-8. [DOI] [PubMed] [Google Scholar]
- 127.Stájer A., Ibrahim B., Gajdács M., Urbán E., Baráth Z. Diagnosis and management of cervicofacial actinomycosis: Lessons from two distinct clinical cases. Antibiotics. 2020;9:139. doi: 10.3390/antibiotics9040139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Moturi K., Kaila V. Cervicofacial actinomycosis and its management. Ann. Maxillofac. Surg. 2018;8:361. doi: 10.4103/ams.ams_176_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Balbinot K.M., Sousa N.W.A., Pinheiro J.d.J.V., Ribeiro A.L.R. Surgical debridement as a treatment strategy for cervicofacial actinomycosis—Literature review and case report. Int. J. Surg. Case Rep. 2020;73:22–26. doi: 10.1016/j.ijscr.2020.06.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chavan S.D., Shetty N.L., Kanuri M. Comparative evaluation of garlic extract mouthwash and chlorhexidine mouthwash on salivary Streptococcus mutans count—An in vitro study. Oral Health Prev. Dent. 2010;8:369–374. [PubMed] [Google Scholar]
- 131.Haas A.N., Silva-Boghossian C.M., Colombo A.P., Susin C., Albandar J.M., Oppermann R.V., Rösing C.K. Adjunctive azithromycin in the treatment of aggressive periodontitis: Microbiological findings of a 12-month randomized clinical trial. J. Dent. 2012;40:556–563. doi: 10.1016/j.jdent.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 132.Faveri M., Rebello A., de Oliveira Dias R., Borges-Junior I., Duarte P.M., Figueiredo L.C., Feres M. Clinical and microbiologic effects of adjunctive metronidazole plus amoxicillin in the treatment of generalized chronic periodontitis: Smokers versus non-smokers. J. Periodontol. 2014;85:581–591. doi: 10.1902/jop.2013.130278. [DOI] [PubMed] [Google Scholar]
- 133.Tulsani S.G., Chikkanarasaiah N., Siddaiah S.B., Krishnamurthy N.H. The effect of Propolis and Xylitol chewing gums on salivary Streptococcus mutans count: A clinical trial. Indian J. Dent. Res. Off. Publ. Indian Soc. Dent. Res. 2014;25:737–741. doi: 10.4103/0970-9290.152182. [DOI] [PubMed] [Google Scholar]
- 134.Parkar S.G., Eady S., Cabecinha M., Skinner M.A. Consumption of apple-boysenberry beverage decreases salivary Actinomyces naeslundii and their adhesion in a multi-species biofilm model. Benef. Microbes. 2017;8:299–307. doi: 10.3920/BM2016.0061. [DOI] [PubMed] [Google Scholar]
- 135.Marya C.M., Taneja P., Nagpal R., Marya V., Oberoi S.S., Arora D. Efficacy of Chlorhexidine, Xylitol, and Chlorhexidine + Xylitol against Dental Plaque, Gingivitis, and Salivary Streptococcus mutans Load: A Randomised Controlled Trial. Oral Health Prev. Dent. 2017;15:529–536. doi: 10.3290/j.ohpd.a39669. [DOI] [PubMed] [Google Scholar]
- 136.Choo J.M., Abell G.C.J., Thomson R., Morgan L., Waterer G., Gordon D.L., Taylor S.L., Leong L.E.X., Wesselingh S.L., Burr L.D., et al. Impact of Long-Term Erythromycin Therapy on the Oropharyngeal Microbiome and Resistance Gene Reservoir in Non-Cystic Fibrosis Bronchiectasis. mSphere. 2018;3:e00103-18. doi: 10.1128/mSphere.00103-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gutiérrez-Venegas G., Gómez-Mora J.A., Meraz-Rodríguez M.A., Flores-Sánchez M.A., Ortiz-Miranda L.F. Effect of flavonoids on antimicrobial activity of microorganisms present in dental plaque. Heliyon. 2019;5:e03013. doi: 10.1016/j.heliyon.2019.e03013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kang S.M., Jung H.I., Kim B.I. Susceptibility of oral bacteria to antibacterial photodynamic therapy. J. Oral Microbiol. 2019;11:1644111. doi: 10.1080/20002297.2019.1644111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Liu D., Peng X., Wang S., Han Q., Li B., Zhou X., Ren B., Xu H.H.K., Weir M.D., Li M., et al. A novel antibacterial resin-based root canal sealer modified by Dimethylaminododecyl Methacrylate. Sci. Rep. 2019;9:10632. doi: 10.1038/s41598-019-47032-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sánchez M.C., Ribeiro-Vidal H., Esteban-Fernández A., Bartolomé B., Figuero E., Moreno-Arribas M.V., Sanz M., Herrera D. Antimicrobial activity of red wine and oenological extracts against periodontal pathogens in a validated oral biofilm model. BMC Complement. Altern. Med. 2019;19:145. doi: 10.1186/s12906-019-2533-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lee M.J., Kwon J.S., Kim J.Y., Ryu J.H., Seo J.Y., Jang S., Kim K.M., Hwang C.J., Choi S.H. Bioactive resin-based composite with surface pre-reacted glass-ionomer filler and zwitterionic material to prevent the formation of multi-species biofilm. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2019;35:1331–1341. doi: 10.1016/j.dental.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 142.Rafiee A., Memarpour M., Najibi Y., Khalvati B., Kianpour S., Morowvat M.H. Antimicrobial Efficacy of a Novel Antibiotic-Eluting Injectable Platelet-Rich Fibrin Scaffold against a Dual-Species Biofilm in an Infected Immature Root Canal Model. BioMed. Res. Int. 2020;2020:6623830. doi: 10.1155/2020/6623830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Vinothkumar T.S., Apathsakayan R., El-Shamy F.M.M., Homeida H.E., Hommedi A.I.M., Safhi M.Y.A., Alsalhi H.A.M. Antibacterial effect of diode laser on different cariogenic bacteria: An In-vitro study. Niger. J. Clin. Pract. 2020;23:1578–1582. doi: 10.4103/njcp.njcp_108_20. [DOI] [PubMed] [Google Scholar]
- 144.Bueno J., Sánchez M.C., Toledano-Osorio M., Figuero E., Toledano M., Medina-Castillo A.L., Osorio R., Herrera D., Sanz M. Antimicrobial effect of nanostructured membranes for guided tissue regeneration: An in vitro study. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2020;36:1566–1577. doi: 10.1016/j.dental.2020.09.011. [DOI] [PubMed] [Google Scholar]
- 145.Fei X., Li Y., Weir M.D., Baras B.H., Wang H., Wang S., Sun J., Melo M.A.S., Ruan J., Xu H.H.K. Novel pit and fissure sealant containing nano-CaF(2) and dimethylaminohexadecyl methacrylate with double benefits of fluoride release and antibacterial function. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2020;36:1241–1253. doi: 10.1016/j.dental.2020.05.010. [DOI] [PubMed] [Google Scholar]
- 146.Marcoux E., Lagha A.B., Gauthier P., Grenier D. Antimicrobial activities of natural plant compounds against endodontic pathogens and biocompatibility with human gingival fibroblasts. Arch. Oral Biol. 2020;116:104734. doi: 10.1016/j.archoralbio.2020.104734. [DOI] [PubMed] [Google Scholar]
- 147.Niu Y., Wang K., Zheng S., Wang Y., Ren Q., Li H., Ding L., Li W., Zhang L. Antibacterial Effect of Caffeic Acid Phenethyl Ester on Cariogenic Bacteria and Streptococcus mutans Biofilms. Antimicrob. Agents Chemother. 2020;64:e00251-20. doi: 10.1128/AAC.00251-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mayumi K., Miyaji H., Miyata S., Nishida E., Furihata T., Kanemoto Y., Sugaya T., Shitomi K., Akasaka T. Antibacterial coating of tooth surface with ion-releasing pre-reacted glass-ionomer (S-PRG) nanofillers. Heliyon. 2021;7:e06147. doi: 10.1016/j.heliyon.2021.e06147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Sumioka R., Nakata M., Okahashi N., Li Y., Wada S., Yamaguchi M., Sumitomo T., Hayashi M., Kawabata S. Streptococcus sanguinis induces neutrophil cell death by production of hydrogen peroxide. PLoS ONE. 2017;12:e0172223. doi: 10.1371/journal.pone.0172223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wang Y., Li J., Zhang H., Zheng X., Wang J., Jia X., Peng X., Xie Q., Zou J., Zheng L., et al. Probiotic Streptococcus salivarius K12 Alleviates Radiation-Induced Oral Mucositis in Mice. Front. Immunol. 2021;12:684824. doi: 10.3389/fimmu.2021.684824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.MacDonald K.W., Chanyi R.M., Macklaim J.M., Cadieux P.A., Reid G., Burton J.P. Streptococcus salivarius inhibits immune activation by periodontal disease pathogens. BMC Oral Health. 2021;21:245. doi: 10.1186/s12903-021-01606-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Puccio T., An S.S., Schultz A.C., Lizarraga C.A., Bryant A.S., Culp D.J., Burne R.A., Kitten T. Manganese transport by Streptococcus sanguinis in acidic conditions and its impact on growth in vitro and in vivo. Mol. Microbiol. 2022;117:375–393. doi: 10.1111/mmi.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Odorici A., Colombari B., Bellini P., Meto A., Venturelli I., Blasi E. Novel Options to Counteract Oral Biofilm Formation: In Vitro Evidence. Int. J. Environ. Res. Public Health. 2022;19:8056. doi: 10.3390/ijerph19138056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lemos J.A., Quivey R.G., Jr., Koo H., Abranches J. Streptococcus mutans: A new Gram-positive paradigm? Microbiology. 2013;159:436. doi: 10.1099/mic.0.066134-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Yazdanian M., Rostamzadeh P., Rahbar M., Alam M., Abbasi K., Tahmasebi E., Tebyaniyan H., Ranjbar R., Seifalian A., Yazdanian A. The Potential Application of Green-Synthesized Metal Nanoparticles in Dentistry: A Comprehensive Review. Bioinorg. Chem. Appl. 2022;2022:2311910. doi: 10.1155/2022/2311910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Yazdanian M., Rostamzadeh P., Alam M., Abbasi K., Tahmasebi E., Tebyaniyan H., Ranjbar R., Seifalian A., Moghaddam M.M., Kahnamoei M.B. Evaluation of antimicrobial and cytotoxic effects of Echinacea and Arctium extracts and Zataria essential oil. AMB Express. 2022;12:75. doi: 10.1186/s13568-022-01417-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Strużycka I. The oral microbiome in dental caries. Pol. J. Microbiol. 2014;63:127–135. doi: 10.33073/pjm-2014-018. [DOI] [PubMed] [Google Scholar]
- 158.Matsumoto-Nakano M. Role of Streptococcus mutans surface proteins for biofilm formation. Jpn. Dent. Sci. Rev. 2018;54:22–29. doi: 10.1016/j.jdsr.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Frencken J.E., Sharma P., Stenhouse L., Green D., Laverty D., Dietrich T. Global epidemiology of dental caries and severe periodontitis–a comprehensive review. J. Clin. Periodontol. 2017;44:S94–S105. doi: 10.1111/jcpe.12677. [DOI] [PubMed] [Google Scholar]
- 160.Pitts N.B., Zero D.T., Marsh P.D., Ekstrand K., Weintraub J.A., Ramos-Gomez F., Tagami J., Twetman S., Tsakos G., Ismail A. Dental caries. Nat. Rev. Dis. Prim. 2017;3:1–16. doi: 10.1038/nrdp.2017.30. [DOI] [PubMed] [Google Scholar]
- 161.Braga M.M., Mendes F.M., Ekstrand K.R. Detection activity assessment and diagnosis of dental caries lesions. Dent. Clin. 2010;54:479–493. doi: 10.1016/j.cden.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 162.Chen X., Daliri E.B.-M., Kim N., Kim J.-R., Yoo D., Oh D.-H. Microbial etiology and prevention of dental caries: Exploiting natural products to inhibit cariogenic biofilms. Pathogens. 2020;9:569. doi: 10.3390/pathogens9070569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Macey R., Walsh T., Riley P., Hogan R., Glenny A.-M., Worthington H.V., Clarkson J.E., Ricketts D. Transillumination and optical coherence tomography for the detection and diagnosis of enamel caries. Cochrane Database Syst. Rev. 2021;1:CD013855. doi: 10.1002/14651858.CD013855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Cochrane N., Walker G., Manton D., Reynolds E. Comparison of quantitative light-induced fluorescence, digital photography and transverse microradiography for quantification of enamel remineralization. Aust. Dent. J. 2012;57:271–276. doi: 10.1111/j.1834-7819.2012.01706.x. [DOI] [PubMed] [Google Scholar]
- 165.Gomez J. Detection and diagnosis of the early caries lesion. BMC Oral Health. 2015;15:1–7. doi: 10.1186/1472-6831-15-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Frencken J., Innes N., Schwendicke F. Managing Carious Lesions: Why Do We Need Consensus on Terminology and Clinical Recommendations on Carious Tissue Removal? SAGE Publications Sage CA; Los Angeles, CA, USA: 2016. [DOI] [PubMed] [Google Scholar]
- 167.Philip N., Suneja B., Walsh L. Beyond Streptococcus mutans: Clinical implications of the evolving dental caries aetiological paradigms and its associated microbiome. Br. Dent. J. 2018;224:219–225. doi: 10.1038/sj.bdj.2018.81. [DOI] [PubMed] [Google Scholar]
- 168.Zhu B., Macleod L.C., Kitten T., Xu P. Streptococcus sanguinis biofilm formation & interaction with oral pathogens. Future Microbiol. 2018;13:915–932. doi: 10.2217/fmb-2018-0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Stingu C.S., Eschrich K., Rodloff A.C., Schaumann R., Jentsch H. Periodontitis is associated with a loss of colonization by Streptococcus sanguinis. J. Med. Microbiol. 2008;57:495–499. doi: 10.1099/jmm.0.47649-0. [DOI] [PubMed] [Google Scholar]
- 170.Zeng L., Walker A.R., Lee K., Taylor Z.A., Burne R.A. Spontaneous Mutants of Streptococcus sanguinis with Defects in the Glucose-Phosphotransferase System Show Enhanced Post-Exponential-Phase Fitness. J. Bacteriol. 2021;203:e0037521. doi: 10.1128/JB.00375-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Dye B.A., Thornton-Evans G., Li X., Iafolla T.J. Dental caries and sealant prevalence in children and adolescents in the United States, 2011–2012. NCHS Data Brief. 2015;191:1–8. [PubMed] [Google Scholar]
- 172.Alpsoy E., Bozca B.C., Bilgic A. Behçet disease: An update for dermatologists. Am. J. Clin. Dermatol. 2021;22:477–502. doi: 10.1007/s40257-021-00609-4. [DOI] [PubMed] [Google Scholar]
- 173.Li Y., Pan Y., Qi F., Caufield P.W. Identification of Streptococcus sanguinis with a PCR-generated species-specific DNA probe. J. Clin. Microbiol. 2003;41:3481–3486. doi: 10.1128/JCM.41.8.3481-3486.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.