Abstract
Objective:
We sought to compare the incidence of adverse cardiovascular events in older adults with primary hyperparathyroidism (PHPT) treated with parathyroidectomy vs. non-operative management.
Summary of Background Data:
PHPT is a common endocrine disorder that is associated with increased cardiovascular mortality, but it is not known whether parathyroidectomy reduces the incidence of adverse cardiovascular events.
Methods:
We conducted a population-based, longitudinal cohort study of Medicare beneficiaries diagnosed with PHPT (2006–2017). Multivariable, inverse probability weighted Cox proportional hazards regression was used to determine the associations of parathyroidectomy with major adverse cardiovascular events (MACE), cardiovascular disease-related hospitalization, and cardiovascular hospitalization-associated mortality.
Results:
We identified 210,206 beneficiaries diagnosed with PHPT from 2006–2017. Among 63,136 (30.0%) treated with parathyroidectomy and 147,070 (70.0%) managed non-operatively within one year of diagnosis, the unadjusted incidence of MACE was 10.0% (mean follow-up 59.1 [SD 35.6] months) and 11.5% (mean follow-up 54.1 [SD 34.0] months), respectively. In multivariable analysis, parathyroidectomy was associated with a lower incidence of MACE (HR 0.92 [95%CI 0.90–0.94]), cardiovascular disease-related hospitalization (HR 0.89 [95%CI 0.87–0.91]), and cardiovascular hospitalization-associated mortality (HR 0.76 [95%CI 0.71–0.81]) compared to non-operative management. At 10 years, parathyroidectomy was associated with adjusted absolute risk reduction for MACE of 1.7% (95%CI 1.3%–2.1%), for cardiovascular disease-related hospitalization of 2.5% (95%CI 2.1%–2.9%), and for cardiovascular hospitalization-associated mortality of 1.4% (95%CI 1.2%–1.6%).
Conclusions:
In this large, population-based cohort study, parathyroidectomy was associated with a lower long-term incidence of adverse cardiovascular outcomes when compared with non-operative management for older adults with PHPT, which is relevant to surgical decision-making for patients with a long life expectancy.
Keywords: primary hyperparathyroidism, parathyroidectomy, geriatric surgery, cardiovascular outcomes
MINI ABSTRACT
This population-based study of 210,206 Medicare beneficiaries diagnosed with primary hyperparathyroidism from 2006–2017 evaluates the association of treatment with parathyroidectomy vs. non-operative management with major adverse cardiovascular (CV) events, CV disease-related hospitalization, and CV hospitalization-associated mortality.
INTRODUCTION
Primary hyperparathyroidism (PHPT) is a common endocrine disorder that primarily affects older adults and contributes to poor quality of life.1 While classically associated with morbidity due to osteoporotic fractures, kidney stones, and declining kidney function, PHPT is also associated with an increased incidence of hypertension, cardiovascular disease, stroke, and diabetes.2 In addition, large Scandinavian cohort studies have demonstrated increased 10-year all-cause and cardiovascular-associated mortality for patients with PHPT when compared to age- and sex-adjusted populations, including among patients with mild disease (i.e. those without metabolic complications of PHPT).2, 3 Primary hyperparathyroidism in older adults is undertreated, with only one in three affected patients receiving definitive management with parathyroidectomy.4 Given the high prevalence and associated morbidity of cardiovascular disease among older adults, it is imperative to determine if cardiovascular risk reduction should be considered when making treatment decisions for PHPT.
Despite data showing that PHPT is associated with a higher incidence of adverse cardiovascular outcomes, there is conflicting evidence on whether parathyroidectomy reduces this risk. Prior studies among hypertensive patients with PHPT have shown that parathyroidectomy is associated with a lower mean systolic and diastolic blood pressure and less need for antihypertensive medications on follow-up,5–9 although this association has not been consistent in all studies, including two small randomized clinical trials.10–12 Parathyroidectomy has also been associated with a lower risk of mortality secondary to cardiovascular events in cohorts of patients with symptomatic, severe PHPT, but there are no data to support this association in patient populations with mild disease. Smaller studies have demonstrated benefits of operative management for PHPT related to arterial stiffness,13–15 endothelial dysfunction,16, 17 and cardiac morphology, including left ventricular mass,18, 19 all of which may affect the risk of adverse cardiovascular outcomes. However, due to small sample sizes, heterogeneity of study design, and inconsistency of subpopulations studied, these findings have limited utility to inform treatment recommendations. Population-based, long-term data are needed to determine whether parathyroidectomy is associated with a reduction in adverse cardiovascular outcomes when compared to non-operative management.
The aim of this study was to determine if parathyroidectomy is independently associated with a lower risk of adverse cardiovascular events in older adults with PHPT, using contemporary methods to control for treatment selection bias and account for the competing risk of death. We also analyzed short- and long-term absolute cardiovascular risk reduction to understand the magnitude of treatment effect and the time to expected benefit. We hypothesized that parathyroidectomy would be associated with a lower risk of major adverse cardiovascular events (MACE), cardiovascular disease-related hospitalization, and cardiovascular hospitalization-associated mortality among older adults and that the time horizon to benefit from parathyroidectomy could be established to inform treatment decisions in this population.
METHODS
We conducted a population-based, longitudinal cohort study of all Medicare beneficiaries diagnosed with PHPT using 100% Medicare fee-for-service claims from 2006–2017. Outpatient claims, carrier claims, Medicare Provider Analysis and Review (MedPAR) files, and Master Beneficiary Summary File (MBSF) files were accessed through the Virtual Research Data Center housed on a secure Centers for Medicare & Medicaid Services (CMS) server for this analysis. The study was approved by the institutional review board at Stanford University, which waived the need for informed consent because of minimal risk. This study was performed and results documented in accordance with STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines for observational research.20
Population
The methods used to identify this patient cohort have been previously described in detail.4, 21 In summary, we included patients 66 years and older with an incident diagnosis of PHPT based on International Classification of Diseases, Ninth Revision (ICD-9) or Tenth Revision (ICD-10) diagnosis codes for PHPT (252.01, E21.0) on any claim during the study period. We excluded patients with: 1) diagnosis codes indicating possible secondary or tertiary hyperparathyroidism; 2) prior parathyroidectomy; 3) missing demographic information (age, sex, race/ethnicity); or 4) mailing zip codes outside of the U.S. or unavailable in U.S. Census or Area Deprivation Index (ADI) data. We required patients to have at least 12 months of continuous enrollment in Medicare Part A and Part B, without Part C enrollment, before and after PHPT diagnosis in order to allow identification of preexisting medical comorbidities or PHPT, to classify patients managed with parathyroidectomy within one year of diagnosis, and to allow access to comprehensive claims data,
Treatment
We divided patients into two PHPT treatment groups: those treated with parathyroidectomy within one year of diagnosis and those observed non-operatively. Patients who underwent delayed parathyroidectomy (more than one year after diagnosis) were included in the non-operatively managed group, with the goal of mimicking an intention-to-treat analysis. Patients who underwent parathyroidectomy were identified based on ICD-9/ICD-10 procedure codes (ICD-9: 06.81, 06.89, 06.99; and ICD-10: 0GBLxxx, 0GBMxxx, 0GBNxxx, 0GBPxxx, 0GBQxxx, 0GBRxxx) and Current Procedural Terminology (CPT) codes 60500, 60502, and 60505 from all settings of claims. In order to ensure similar time to follow up, time zero for our longitudinal, time-to-event analysis was the date of surgery in the parathyroidectomy group and a randomly generated “treatment date” in the non-operatively managed group, with the same overall distribution of treatment dates as those who underwent parathyroidectomy.
Outcomes
Our primary outcome was MACE, which was defined as non-fatal myocardial infarction (MI) or stroke; inpatient hospitalization for unstable angina, congestive heart failure, cardiac arrest, or cardiogenic shock; or procedure/surgery for coronary artery disease, which were based on ICD-9 and ICD-10 diagnosis and procedure codes, and CPT and diagnosis related group (DRG) codes (see eTable 1). Secondary outcomes included cardiovascular-disease related hospitalization (inpatient treatment for arrhythmia and other significant cerebrovascular and cardiovascular events) and cardiovascular hospitalization-associated mortality (any death within 30 days of MACE or cardiovascular disease-related hospitalization)(see eTable 1). Patients were followed from treatment date until censoring at death, Medicare disenrollment, or December 31, 2017.
Covariates
Covariates were based on clinical significance and included relevant demographic information (i.e. age, sex, race/ethnicity) and characteristics of place of residence (ADI, urban/rural inhabitance) assessed at the time of cohort entry (PHPT diagnosis). The Charlson-Deyo Comorbidity Index was used to measure comorbidity.22, 23 Frailty was assessed in the year prior to treatment using a validated deficit accumulation model, claims-based frailty index.24 We identified patients with sequelae of PHPT, including a history of osteoporosis, nephrolithiasis, or stage 3 chronic kidney disease (CKD), based on ICD-9 or ICD-10 codes from all available claims. Patients were considered to meet consensus guideline criteria for parathyroidectomy based on a history of one or more of these conditions at PHPT diagnosis.25, 26 Patients who received endocrinologist specialty care within 6 months of diagnosis were identified based on ≥1 outpatient or carrier claim with a CMS provider specialty code indicating subspecialty training in endocrinology and an associated diagnosis code for PHPT or related sequelae (e.g. hypercalcemia, osteoporosis). Risk factors for adverse cardiovascular outcomes included hypertension, diabetes, hyperlipidemia, coronary artery disease, prior MI, prior stroke, obesity, tobacco use, and alcohol use disorder, which were identified based on ICD-9 or ICD-10 codes and CMS Chronic Conditions Data Warehouse (CCW) indicator variables from claims in the year prior to treatment. The ADI, a validated measure of neighborhood disadvantage in the U.S., was used to estimate socioeconomic status based on mailing zip code.27, 28 Urban vs. rural inhabitance was determined using Census Bureau data, as previously described.4, 29
Statistical Analysis
Our analytic approach sought to determine if parathyroidectomy within one year of PHPT diagnosis was independently associated with adverse cardiovascular outcomes among older adults. Univariate comparisons were performed using chi-square and student’s t-tests. To account for treatment selection bias, we incorporated inverse probability weighting in our outcome analysis to estimate the average treatment effect. Covariates in the treatment and outcomes models included all variables described in the covariate section, all of which were associated with either treatment selection and/or development of the outcomes.30 We compared covariate balance between patients treated with parathyroidectomy and patients treated non-operatively using standardized mean differences (SMD) and considered SMD <10% to indicate adequate balance.31
We then calculated inverse probability weighted (IPW) cause-specific Cox proportional hazard time-to-event regression models to estimate the association between parathyroidectomy and time to primary and secondary outcomes, MACE, cardiovascular-associated hospitalization, and cardiovascular hospitalization-associated mortality. From the IPW Cox models, adjusted absolute risk reductions and numbers needed to treat at 2, 5, and 10 years were calculated for each outcome. In order to assess if parathyroidectomy is associated with a lower risk of adverse cardiovascular outcomes when accounting for the competing risk of death, IPW Fine-Gray competing risk regression models were calculated. We also included interaction terms to test for effect modification of treatment based on a history of cardiovascular disease or meeting guideline criteria for parathyroidectomy at PHPT diagnosis and generated hazard ratios (HRs) for parathyroidectomy vs. non-operative management within these subgroups. As sensitivity analyses to assess the likelihood of residual confounding, we calculated E-values for our primary and secondary outcomes.32, 33 In addition, we performed falsification endpoint analyses for two outcomes that we would not expect to have a direct causal association with parathyroidectomy (admission for gastrointestinal bleed and herpes zoster infection based on ICD-9 or ICD-10 codes in the primary position on inpatient claims within one year of treatment date). Statistical significance was assessed at the level of alpha=0.05. Statistical analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, NC).
RESULTS
A total of 210,206 Medicare beneficiaries were diagnosed with PHPT from January 1, 2006 to December 31, 2017 and met study criteria (Figure 1). The treatment within one year of diagnosis was parathyroidectomy for 63,136 (30.0%) patients and non-operative management for 147,070 (70.0%). Overall, the patients managed operatively were younger (mean age 73.5 vs. 76.0 years, p<.001) and healthier than their non-operatively managed counterparts, being more likely to be non-frail and have a lower comorbidity burden (eTable 2). In addition, patients treated with parathyroidectomy were less likely to have a history of cardiovascular risk factors. However, baseline characteristics were well-balanced between treatment groups after propensity score inverse probability weighting.
Figure 1.
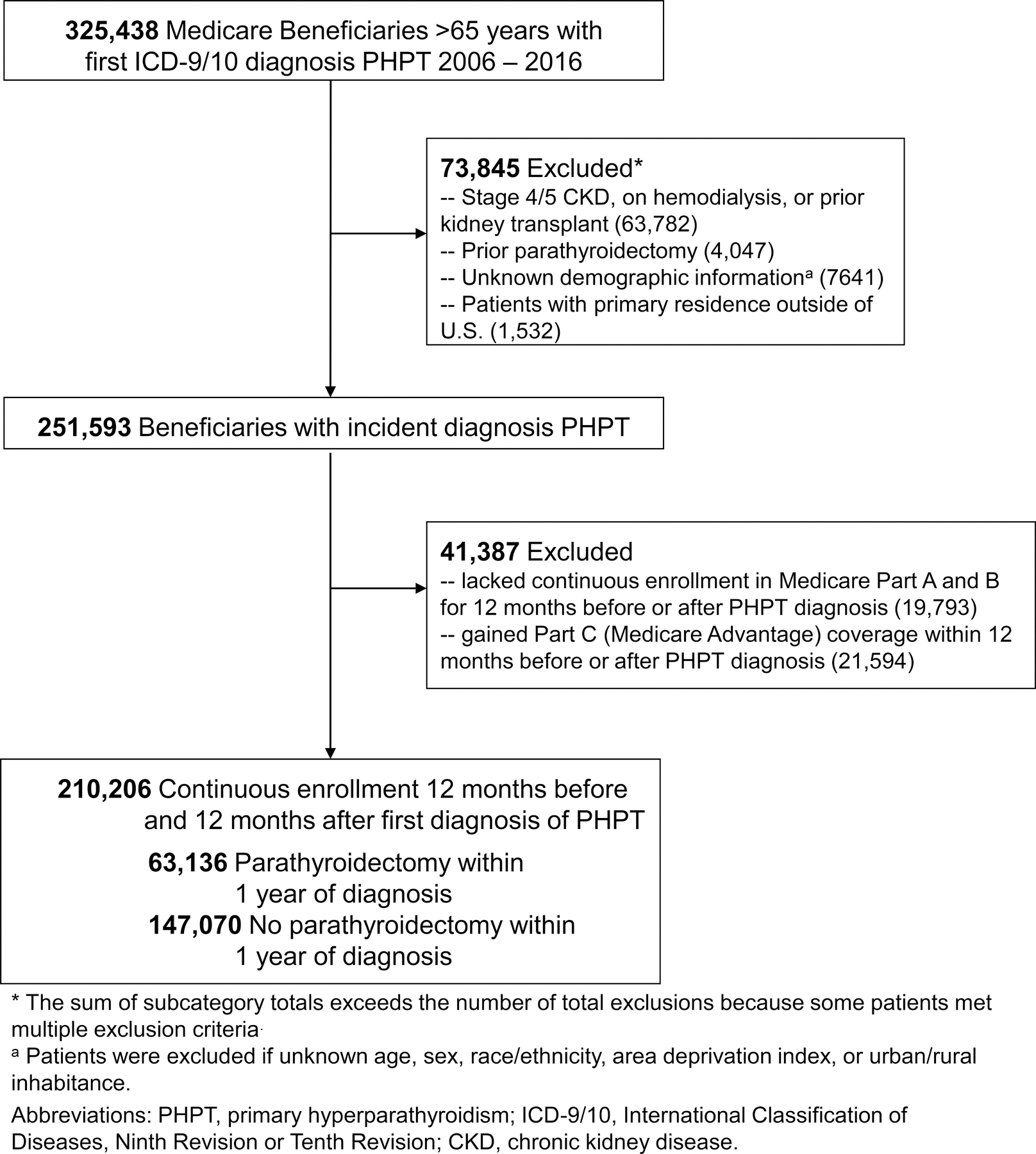
Consort diagram.
Among patients treated with parathyroidectomy, the unadjusted incidences of MACE, CV disease-related hospitalization, and cardiovascular hospitalization-associated mortality were 10.0% (mean follow-up 59.1 [SD 35.6] months), 12.1% (mean follow-up 57.8 [SD 35.4] months), and 1.4% (mean follow-up 62.1 [SD 35.7] months), respectively, compared to 11.5% (mean follow-up 54.0 [SD 34.0] months), 13.7% (mean follow-up 52.4 [SD 33.8] months), and 2.0% (mean follow-up 56.9 [SD 34.2] months), respectively, in those managed non-operatively. Figure 2 shows Kaplan-Meier curves demonstrating the unadjusted incidence of MACE, cardiovascular disease-related hospitalization, and cardiovascular hospitalization-associated mortality among the parathyroidectomy and non-operatively managed treatment groups.
Figure 2.
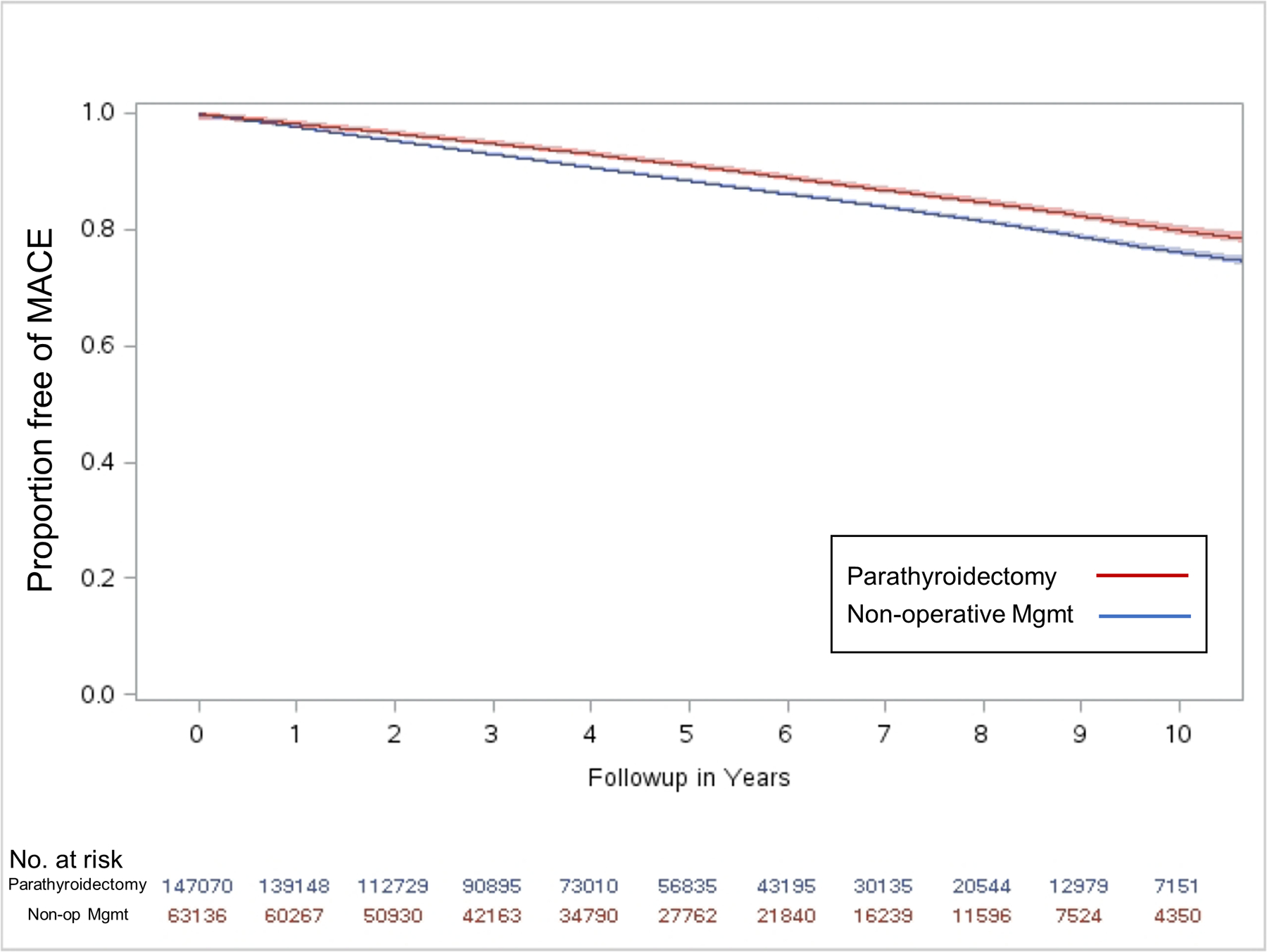
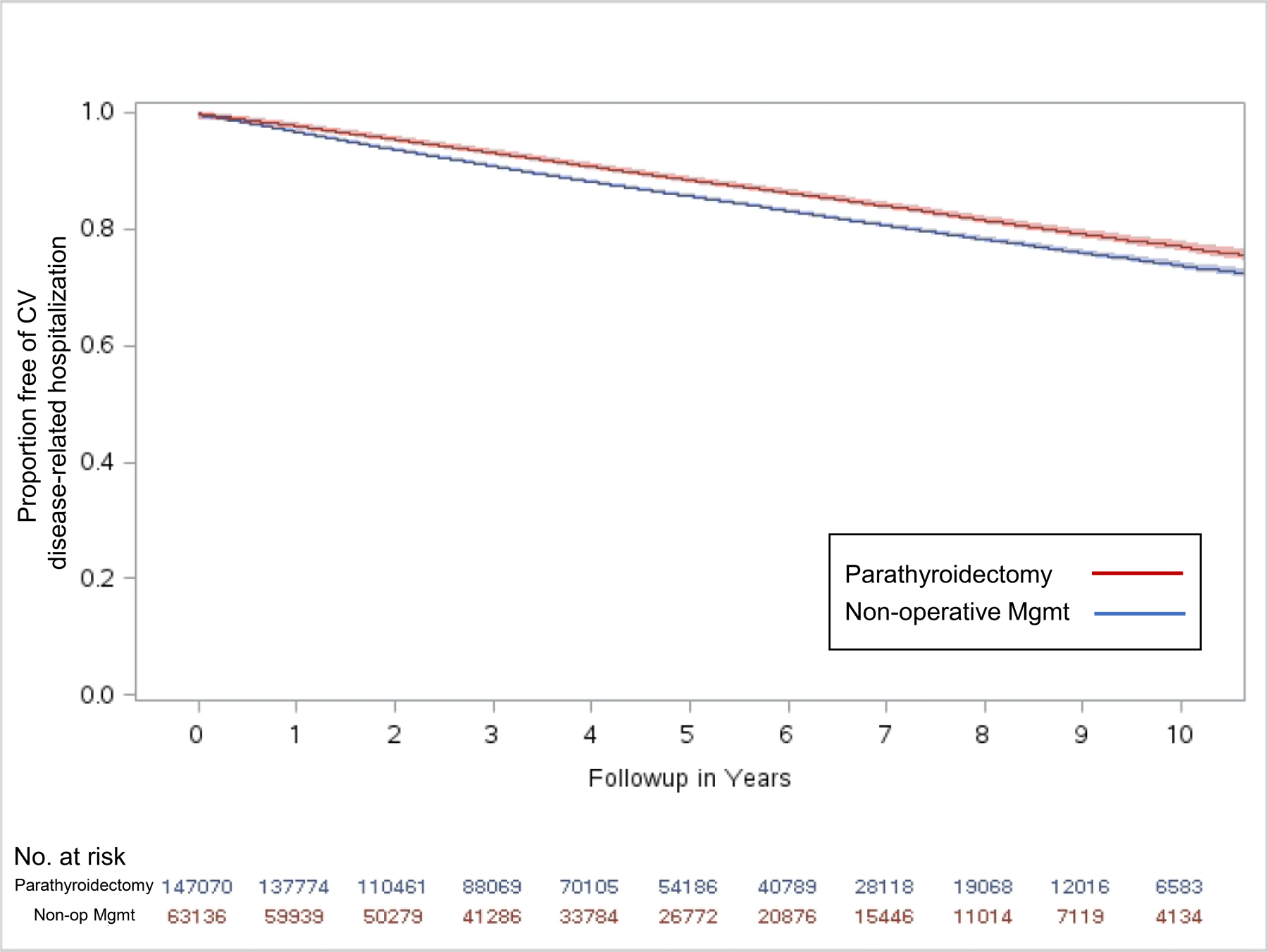
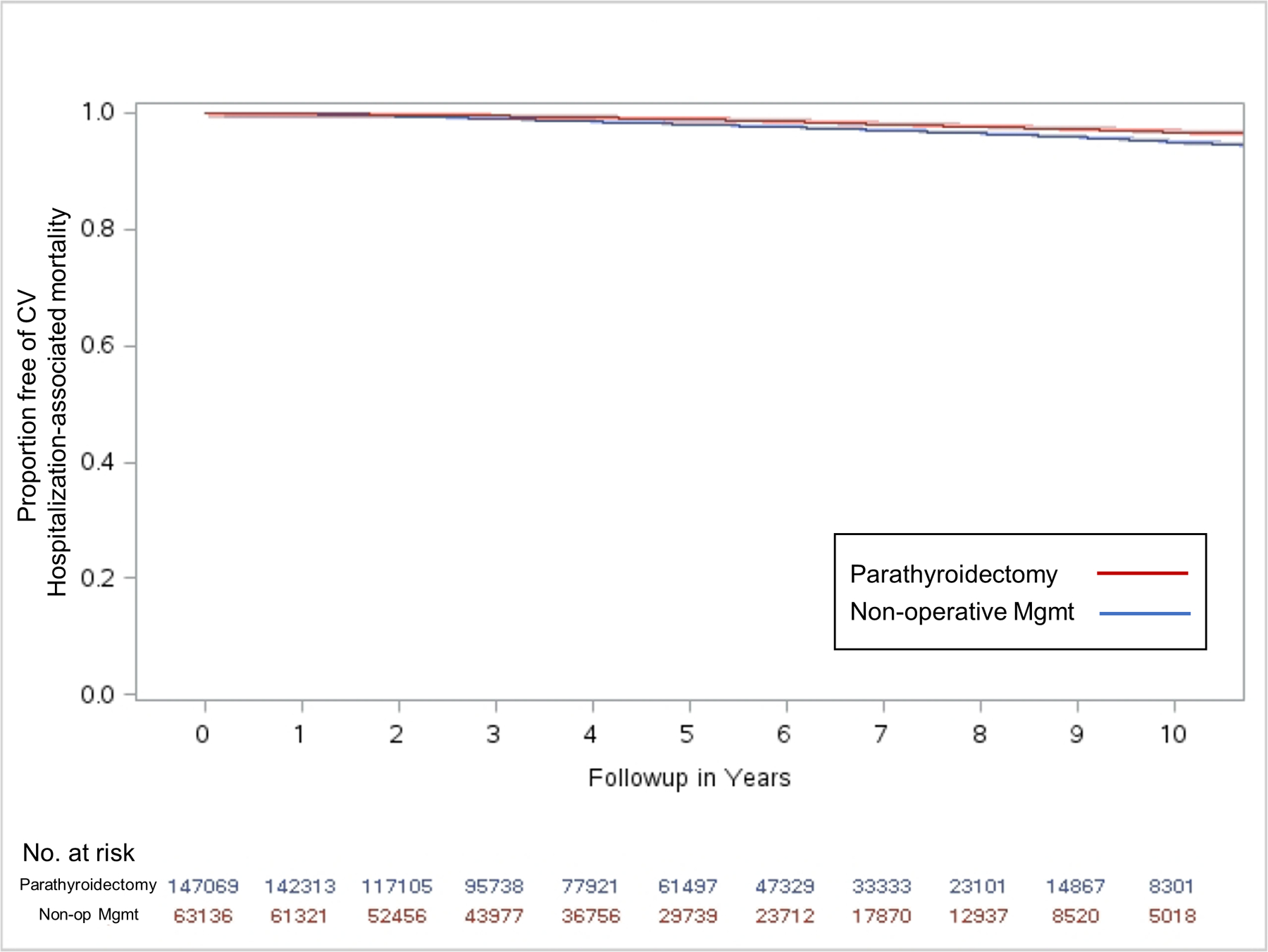
Kaplan-Meier curves showing unadjusted incidence of (a) major adverse cardiovascular events (MACE); (b) CV disease-related hospitalization; and (c) CV hospitalization-associated mortality among older adults with PHPT following parathyroidectomy vs. non-operative management.
In IPW-weighted multivariable Cox proportional hazards regression analysis, parathyroidectomy was associated with a lower adjusted hazard of MACE (HR 0.92 [95%CI 0.90–0.94]), cardiovascular disease-related hospitalization (HR 0.89 [95%CI 0.87–0.91]), and cardiovascular hospitalization-associated mortality (HR 0.76 [95%CI 0.71–0.81]) compared to non-operative management (eTable 3). This translated into parathyroidectomy being associated with statistically significant adjusted absolute MACE, cardiovascular disease-related hospitalization, and cardiovascular hospitalization-associated mortality risk reduction when compared to non-operative management at all time points, with 10-year adjusted absolute risk reduction of 1.66% (95%CI 1.26–2.06%), 2.48% (95%CI 2.07–2.89%), and 1.37% (95%CI 1.17–1.57%) and numbers needed to treat of 60, 40, and 73, respectively (Table 1). On stratified subgroup analyses, parathyroidectomy was associated with a lower incidence of cardiovascular disease-related hospitalization and cardiovascular hospitalization-associated mortality among patients with and without a history of cardiovascular disease, but parathyroidectomy was not associated with a statistically significant lower hazard of MACE among patients without a history of cardiovascular disease (Figure 3a). There were no significant differences in the association of parathyroidectomy with adverse cardiovascular event risk reduction based on meeting guideline criteria for parathyroidectomy (Figure 3b). Fine-Gray competing risk regression found that parathyroidectomy was associated with a lower incidence of cardiovascular disease-related hospitalization and cardiovascular hospitalization-associated mortality but not MACE when accounting for the competing risk of death (HR 0.95 [95%CI 0.93–0.96], HR 0.85 [95%CI 0.81–0.89], and HR 0.99 [95%CI 0.97–1.01], respectively) (eTable 4).
Table 1.
Adjusted* absolute risk reduction (ARR) and number needed to treat (NNT) for MACE, CV disease-related hospitalization, and CV hospitalization-associated mortality with parathyroidectomy at 2, 5, and 10 years following treatment.
| Adverse CV Outcome | Time Point | Adjusted Absolute Risk Reduction (ARR) | 95% CI | Number Needed to Treat (NNT) | |
|---|---|---|---|---|---|
| MACE | |||||
| 2 years | 0.35% | 0.16% | 0.54% | 288 | |
| 5 years | 0.84% | 0.55% | 1.13% | 119 | |
| 10 years | 1.66% | 1.26% | 2.06% | 60 | |
| CV Disease-Related Hospitalization | |||||
| 2 years | 0.63% | 0.41% | 0.84% | 159 | |
| 5 years | 1.42% | 1.10% | 1.74% | 70 | |
| 10 years | 2.48% | 2.07% | 2.89% | 40 | |
| CV Hospitalization-Associated Mortality | |||||
| 2 years | 0.11% | 0.06% | 0.17% | 884 | |
| 5 years | 0.46% | 0.34% | 0.57% | 220 | |
| 10 years | 1.37% | 1.17% | 1.57% | 73 | |
Inverse probability weighted and adjusted for sex, age group, race/ethnicity, ADI, urban/rural inhabitance, frailty, Charlson comorbidity index, operative indications for parathyroidectomy (history of osteoporosis, kidney stones, or stage 3 chronic kidney disease), endocrinologist care within 6 months of PHPT diagnosis, and history of prior myocardial infarction, prior stroke, coronary artery disease, hypertension, diabetes, obesity, tobacco use, and alcohol use disorder.
Figure 3.

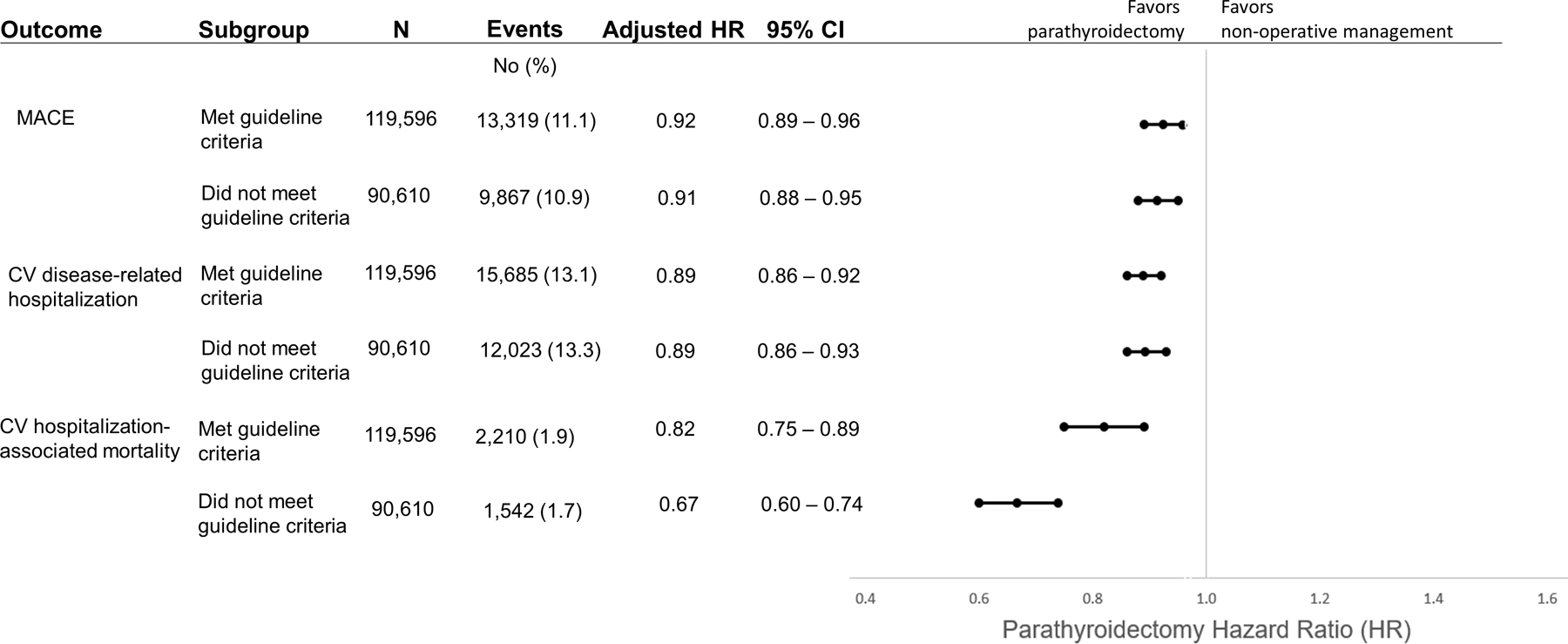
Adjusted hazard ratios (HR)* for the association between parathyroidectomy vs. non-operative management and MACE, CV disease-related hospitalization, and CV hospitalization-associated mortality in subgroups (a) with and without a history of CV disease; and (b) who did and did not meet consensus guideline criteria for parathyroidectomy.
*Inverse probability weighted and adjusted for sex, age group, race/ethnicity, ADI, urban/rural inhabitance, frailty, Charlson-Deyo comorbidity index, operative indications for parathyroidectomy (history of osteoporosis, kidney stones, or stage 3 chronic kidney disease), endocrinologist care within 6 months of PHPT diagnosis, and history of prior myocardial infarction, prior stroke, coronary artery disease, hypertension, diabetes, obesity, tobacco use, and alcohol use disorder.
E-value analyses demonstrated that the minimum association (HR) that an unmeasured confounder would need to have with both the treatment and outcome in the primary analysis, conditional on the measured covariates, in order to account for all of the association would be 1.39 (95%CI 1.32) for MACE, 1.5 (95%CI 1.43) for cardiovascular disease-related hospitalization, and 1.96 (95%CI 1.77) for cardiovascular hospitalization-associated mortality. Falsification end point analyses were not suggestive of residual confounding (eTable 5).
DISCUSSION
The results of this longitudinal cohort study showed that the treatment of PHPT with parathyroidectomy was associated with a lower adjusted rate of adverse cardiovascular events than non-operative management in a large, national population of older adults. However, the absolute risk reductions associated with parathyroidectomy were modest and more likely to be of clinical significance when extrapolated over long-term follow up. Among subgroups of interest, parathyroidectomy was not associated with a lower hazard of MACE in patients without a history of cardiovascular disease but was associated with a lower hazard of all adverse cardiovascular outcomes regardless of whether patients did or did not meet consensus guideline criteria for parathyroidectomy. When taking into account the competing risk of death, parathyroidectomy was associated with a lower risk of cardiovascular disease-related hospitalization and cardiovascular hospitalization-associated mortality but not MACE. Taken together, these results suggest parathyroidectomy is likely associated with a reduction in adverse cardiovascular outcomes among older adults with PHPT, but the absolute benefits are modest and more likely to be clinically meaningful to patients with a long life expectancy.
Historical, observational cohort studies from Europe in the late 20th century that demonstrated an increased risk of cardiovascular mortality in patients with PHPT that improved after parathyroidectomy have been discounted due to concerns that similar outcomes would not be observed in modern-day populations with predominantly mild disease.3, 34, 35 There are few contemporary population-based studies evaluating the risk of MACE or cardiovascular morbidity according to management strategy in patients with PHPT. A longitudinal cohort study of 3,213 Danish patients with PHPT diagnosed from 1989 to 1999 with a median 6.1 years follow-up found no difference in the hazard of MI, hypertension, heart failure, arrhythmia, or stroke between patients treated with parathyroidectomy vs. those managed non-operatively after adjusting for age, sex, and history of each event prior to PHPT diagnosis.36 A recently published population-based study of 16,374 patients with PHPT in Sweden showed a reduced risk of cardiovascular events in patients with PHPT who were treated with parathyroidectomy (HR 0.84, 95%CI 0.73–0.97), similar to our findings.37 Long-term follow up data from the 191-patient Scandinavian Investigation of Primary Hyperparathyroidism (SIPH) randomized controlled trial showed no statistically significant difference in the secondary outcome of cardiovascular events (HR 0.81, 95%CI 0.33–1.99) among adults with asymptomatic PHPT managed with parathyroidectomy vs. non-operatively, but this study was underpowered to detect differences in cardiovascular outcomes.38 Small, predominantly single-center studies have shown a beneficial effect of parathyroidectomy on surrogate cardiovascular end-points, including arterial stiffness, endothelial dysfunction, and left ventricular mass.13–19 These prior studies suggested that surgical cure with parathyroidectomy would alter the cardiovascular risk profile of patients with PHPT and lead to improved cardiovascular outcomes, consistent with our findings. However, it is important to note that the cardiovascular benefits of parathyroidectomy in our study and the recent Swedish cohort study37 were modest and most likely to be clinically meaningful on long-term follow-up (i.e. 5 to 10 years following surgery), which may not be relevant to patients with limited life expectancy. It is possible that more nuanced, short-term cardiovascular benefits are experienced by patients with PHPT treated operatively but that these are not as evident in the current analysis. Reassuringly, it does not appear that parathyroidectomy increases the short-term risk of adverse cardiovascular outcomes among this older patient population with a high prevalence of cardiovascular risk factors.
The findings of our study generally support current guideline recommendations related to the operative management of PHPT but also suggest a more nuanced approach to treatment decisions is warranted. Comprehensive guidelines published by the American Association of Endocrine Surgeons in 2016 suggested parathyroidectomy may be considered for patients with underlying cardiovascular disease based on the potential mitigation of adverse cardiovascular sequelae but acknowledged this was a weak recommendation based on low-quality evidence.26 In addition, the most recent consensus guidelines for the management of asymptomatic PHPT published in 2014 reported insufficient evidence to recommend parathyroidectomy to improve cardiovascular endpoints.39 Based on our documented absolute risk reduction and numbers needed to treat, 70 parathyroidectomies would be necessary to prevent one cardiovascular-associated hospitalization at 5 years, with larger numbers needed to prevent MACE or cardiovascular hospitalization-associated mortality. Although the numbers needed to treat decline with time, it is unlikely the potential cardiovascular benefits would outweigh the risks of surgery on a population level. However, it is notable that we found similar and statistically significant reductions in adverse cardiovascular outcomes among patients who did not meet guideline criteria for parathyroidectomy, many of whom likely had mild PHPT. Therefore, we recommend physicians participating in shared decision-making with patients with PHPT focus on the benefits of parathyroidectomy that are supported by strong evidence, including fracture risk-reduction21, 40 and improved quality of life,1 and counsel patients that potential cardiovascular benefits of surgical cure are relevant to patients who do and do not meet guideline criteria but are likely only clinically meaningful in the long-term.
This study is the first national, population-based study in the U.S. to compare the risk of adverse cardiovascular outcomes among patients with PHPT treated with parathyroidectomy vs. non-operative management and the largest study to-date evaluating cardiovascular outcomes among patients with PHPT. Strengths of our study include the large sample size, long-term follow up, and inclusion of a diverse, real-world population of older adults receiving treatment for PHPT. Limitations of our study are related to the use of administrative claims for our analyses, which lack laboratory data or granular information about the severity of PHPT, baseline cardiovascular disease, and other comorbidities that may influence both treatment decisions and outcomes. The use of claim codes to identify patients with PHPT may lead to underidentification of patients with a biochemical diagnosis of PHPT that is not identified by clinicians and be subject to coding errors, leading to misclassification of patients with hypercalcemia of other etiologies. The observational nature of our study leads to the possibility of residual confounding, which if present would likely be in the direction of favoring parathyroidectomy. Based on our secondary and sensitivity analyses, most notably our falsification endpoint analysis, it is not likely that residual confounding explains all the association between parathyroidectomy and cardiovascular disease-related hospitalization or cardiovascular hospitalization-associated mortality, but further evaluation with a prospective trial focused on long-term cardiovascular outcomes is indicated to confirm the effect sizes documented in our study and the clinical significance of this association.
CONCLUSION
In this longitudinal cohort study, parathyroidectomy was associated with a lower adjusted hazard of adverse cardiovascular outcomes, but the effect sizes were modest and the absolute benefits were most clinically meaningful when extrapolated over long-term follow up. When taking into account the competing risk of death, there was no difference in the incidence of MACE between patients treated with parathyroidectomy vs. non-operative management. These findings support current guidelines that do not recommend parathyroidectomy solely on the basis of cardiovascular risk reduction but suggest that the mitigation of adverse cardiovascular outcomes could be relevant for individual treatment decisions, especially among younger patients and those with a long life expectancy.
Supplementary Material
Acknowledgements:
Dr. Seib and Ms. Meng had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Source of Funding:
Dr. Seib reported prior consulting for Virtual Incision Corporation. Dr. Suh reported consulting for Medtronic, Prescient Surgical, and RPWB. Ms. Meng reports employment by Roche following completion of her work on this study. No other disclosures were reported. The authors acknowledge funding support from the National Institutes of Health, National Institute on Aging by awards R03AG060097 (Dr. Seib and Ms. Meng) and K76AG068526 (Dr. Seib) and the Department of Veterans Affairs Health Services Research & Development Service Research Career Scientist Award RCS 14–232 (Dr. Harris). Funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest
The authors have no conflicts of interest relevant to this project.
REFERENCES
- 1.Ambrogini E, Cetani F, Cianferotti L, et al. Surgery or surveillance for mild asymptomatic primary hyperparathyroidism: a prospective, randomized clinical trial. The Journal of Clinical Endocrinology & Metabolism 2007; 92(8):3114–3121. [DOI] [PubMed] [Google Scholar]
- 2.Yu N, Donnan PT, Flynn RWV, et al. Increased mortality and morbidity in mild primary hyperparathyroid patients. The Parathyroid Epidemiology and Audit Research Study (PEARS). Clinical endocrinology 2010; 73(1):30–34. [DOI] [PubMed] [Google Scholar]
- 3.Vestergaard P, Mollerup CL, Frøkjær VG, et al. Cardiovascular events before and after surgery for primary hyperparathyroidism. World journal of surgery 2003; 27(2):216–222. [DOI] [PubMed] [Google Scholar]
- 4.Seib C, Suh I, Meng T, et al. Patient Factors Associated with Parathyroidectomy in Older Adults with Primary Hyperparathyroidism. JAMA Surgery 2021; 156(4):334–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Broulik P, Brouliková A, Adámek S, et al. Improvement of hypertension after parathyroidectomy of patients suffering from primary hyperparathyroidism. International journal of endocrinology 2011; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farahnak P, Lärfars G, Sten-Linder M, et al. Mild primary hyperparathyroidism: vitamin D deficiency and cardiovascular risk markers. The Journal of Clinical Endocrinology & Metabolism 2011; 96(7):2112–2118. [DOI] [PubMed] [Google Scholar]
- 7.Heyliger A, Tangpricha V, Weber C, et al. Parathyroidectomy decreases systolic and diastolic blood pressure in hypertensive patients with primary hyperparathyroidism. Surgery 2009; 146(6):1042–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luigi P, Chiara FM, Laura Z, et al. Arterial hypertension, metabolic syndrome and subclinical cardiovascular organ damage in patients with asymptomatic primary hyperparathyroidism before and after parathyroidectomy: preliminary results. International journal of endocrinology 2012; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Graff-Baker AN, Bridges LT, Chen Q, et al. Parathyroidectomy for Patients With Primary Hyperparathyroidism and Associations With Hypertension. JAMA Surgery 2020; 155(1):32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ejlsmark-Svensson H, Rolighed L, Rejnmark L. Effect of Parathyroidectomy on Cardiovascular Risk Factors in Primary Hyperparathyroidism: A Randomized Clinical Trial. The Journal of Clinical Endocrinology & Metabolism 2019; 104(8):3223–3232. [DOI] [PubMed] [Google Scholar]
- 11.Rydberg E, Birgander M, Bondeson A-G, et al. Effect of successful parathyroidectomy on 24-hour ambulatory blood pressure in patients with primary hyperparathyroidism. International journal of cardiology 2010; 142(1):15–21. [DOI] [PubMed] [Google Scholar]
- 12.Bollerslev J, Rosen T, Mollerup CL, et al. Effect of surgery on cardiovascular risk factors in mild primary hyperparathyroidism. The Journal of Clinical Endocrinology & Metabolism 2009; 94(7):2255–2261. [DOI] [PubMed] [Google Scholar]
- 13.Cansu GB, Yılmaz N, Özdem S, et al. Parathyroidectomy in asymptomatic primary hyperparathyroidism reduces carotid intima-media thickness and arterial stiffness. Clinical Endocrinology 2016; 84(1):39–47. [DOI] [PubMed] [Google Scholar]
- 14.Walker M, Rundek T, Homma S, et al. Effect of parathyroidectomy on subclinical cardiovascular disease in mild primary hyperparathyroidism. European Journal of Endocrinology/European Federation of Endocrine Societies 2012; 167(2):277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schillaci G, Pucci G, Pirro M, et al. Large-artery stiffness: A reversible marker of cardiovascular risk in primary hyperparathyroidism. Atherosclerosis 2011; 218(1):96–101. [DOI] [PubMed] [Google Scholar]
- 16.Tuna MM, Doğan BA, Arduç A, et al. Impaired endothelial function in patients with mild primary hyperparathyroidism improves after parathyroidectomy. Clinical Endocrinology 2015; 83(6):951–956. [DOI] [PubMed] [Google Scholar]
- 17.Ekmekci A, Abaci N, Ozbey NC, et al. Endothelial function and endothelial nitric oxide synthase intron 4a/b polymorphism in primary hyperparathyroidism. Journal of endocrinological investigation 2009; 32(7):611–616. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal G, Nanda G, Kapoor A, et al. Cardiovascular dysfunction in symptomatic primary hyperparathyroidism and its reversal after curative parathyroidectomy: Results of a prospective case control study. Surgery 2013; 154(6):1394–1404. [DOI] [PubMed] [Google Scholar]
- 19.Nilsson I-L, Åberg J, Rastad J, et al. Maintained normalization of cardiovascular dysfunction 5 years after parathyroidectomy in primary hyperparathyroidism. Surgery 2005; 137(6):632–638. [DOI] [PubMed] [Google Scholar]
- 20.Ev Elm, Altman DG, Egger M, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007; 335(7624):806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seib CD, Meng T, Suh I, et al. Risk of Fracture Among Older Adults With Primary Hyperparathyroidism Receiving Parathyroidectomy vs Nonoperative Management. JAMA Internal Medicine 2022; 182(1):10–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of clinical epidemiology 1992; 45(6):613–619. [DOI] [PubMed] [Google Scholar]
- 23.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical care 2005:1130–1139. [DOI] [PubMed] [Google Scholar]
- 24.Kim DH, Glynn RJ, Avorn J, et al. Validation of a claims-based frailty index against physical performance and adverse health outcomes in the Health and Retirement Study. The Journals of Gerontology: Series A 2019; 74(8):1271–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bilezikian JP, Brandi ML, Eastell R, et al. Guidelines for the Management of Asymptomatic Primary Hyperparathyroidism: Summary Statement from the Fourth International Workshop. The Journal of Clinical Endocrinology & Metabolism 2014; 99(10):3561–3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA surgery 2016; 151(10):959–968. [DOI] [PubMed] [Google Scholar]
- 27.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible—the neighborhood atlas. The New England journal of medicine 2018; 378(26):2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hu J, Kind AJH, Nerenz D. Area deprivation index predicts readmission risk at an urban teaching hospital. American Journal of Medical Quality 2018; 33(5):493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Census Bureau Decennial Survery [database online]. Insert City of Publication Here see notes; 2010.
- 30.Bang H, Robins JM. Doubly robust estimation in missing data and causal inference models. Biometrics 2005; 61(4):962–973. [DOI] [PubMed] [Google Scholar]
- 31.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity‐score matched samples. Statistics in medicine 2009; 28(25):3083–3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mathur MB, Ding P, Riddell CA, et al. Website and R package for computing E-values. Epidemiology (Cambridge, Mass.) 2018; 29(5):e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Annals of internal medicine 2017; 167(4):268–274. [DOI] [PubMed] [Google Scholar]
- 34.Walker MD, Silverberg SJ. Primary hyperparathyroidism. Nature Reviews Endocrinology 2018; 14(2):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hedbäck G, Odén A, Tisell L-E. The influence of surgery on the risk of death in patients with primary hyperparathyroidism. World Journal of Surgery 1991; 15(3):399–405. [DOI] [PubMed] [Google Scholar]
- 36.Vestergaard P, Mosekilde L. Cohort study on effects of parathyroid surgery on multiple outcomes in primary hyperparathyroidism. Bmj 2003; 327(7414):530–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Axelsson KF, Wallander M, Johansson H, et al. Analysis of Comorbidities, Clinical Outcomes, and Parathyroidectomy in Adults With Primary Hyperparathyroidism. JAMA Network Open 2022; 5(6):e2215396–e2215396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pretorius M, Lundstam K, Hellström M, et al. Mortality and Morbidity in Mild Primary Hyperparathyroidism: Results from A 10 Year Prospective Randomised Controlled Trial Of Parathyroidectomy vs Observation. Annals of Internal Medicine 2022. [DOI] [PubMed] [Google Scholar]
- 39.Bilezikian JP, Khan AA, Potts JT Jr, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. The Journal of Clinical Endocrinology & Metabolism 2009; 94(2):335–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yeh MW, Zhou H, Adams AL, et al. The Relationship of Parathyroidectomy and Bisphosphonates With Fracture Risk in Primary Hyperparathyroidism: An Observational Study. Annals of Internal Medicine 2016; 164(11):715–723. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


