Abstract
This study aimed to evaluate the long-term clinical success of the use of mineral trioxide aggregate (MTA) as a sealant material in root perforation treatments. Therefore, the dental records of 53 patients were analyzed, and treatment data was collected (age, gender, tooth location, jaw, presence or absence of radiolucent lesion, fallow up time and final radiographic/clinical assessment). All procedures were performed by a single specialist. Two examiners analyzed three radiographs from the records of each patient and classified the treatments as successful or unsuccessful. Data was analyzed statistically using parametric chi-square (P≤0.05). The examiners classified 69.8% of the cases as successful, with a follow-up time of 1-16.25 years (average: 6 years). The presence of initial radiolucent lesion was observed in 79.2% of the teeth, with a higher index of treatment in maxillary teeth (62.3%). However, the majority of successful cases were located in the maxilla (73.0%), while most unsuccessful ones were located in the mandible (62.5%) (P=0.014). There was no statistically significant difference regarding presence of previous lesions in successful (75.7%) and unsuccessful cases (87.5%) (P=0.330). In the present study, root perforations sealed with MTA had a success rate of 69.8% within 1-16.25 years. The presence of initial injury did not influence the prognosis, and maxillary teeth presented a higher success rate.
Key Words: Mineral Trioxide Aggregate, Perforation, Endodontics
Introduction
Dental perforations, are communications between the pulp space and the periodontal structures [1]. It's etiology may have a pathological origin, such as tooth decay or root resorptive processes, or it may be iatrogenically induced, for example, during access surgery for endodontic therapy or even during the preparation procedures for prosthetic posts [2-5]. One of the main consequences of this injury is the infection of the periodontal tissues by bacteria that colonize the oral cavity or the root canal system. Thereby, an inflammatory response can be triggered and culminate in the lysis of the alveolar bone. In more advanced cases, it may even result in tooth loss [6-8].
In addition to occurring eventually in the daily practice of many professionals, root perforation is considered as one of the main complications leading to failure [9, 10]. Several studies have mentioned some of the main variables that influence the success of the perforation treatment, as follows: the level at which it occurred (above or below bone level), passed time since the occurrence, whether there was contamination, the amplitude of the perforation, operator ability, previous radiolucent lesion and the sealant material [4, 10-12]. However, few studies have verified the success of the treatment of root perforations sealed with mineral trioxide aggregate (MTA) in long-term. Most studies present an average of 1 year of follow-up, besides small sample sizes. Furthermore, there is a significant variety among the literature regarding different degree and number of professionals operating [7, 13-17].
Many materials for sealing root perforations have already been tested, including amalgam, Sealer 26®, Cavit®, gutta-percha, glass ionomer, calcium hydroxide, composite resins, and Super-EBA®. However, none of these meet all the criteria of an ideal repair material, which include sealing ability, biocompatibility, insolubility in the presence of tissue fluids, and the ability to induce osteogenesis and cementogenesis [2, 18-21]. MTA has been the material of choice for sealing perforations due to its biocompatibility, high sealing ability when used adequately, and induction of osteogenesis and cementogenesis [22-24]. Numerous studies have shown that MTA has superior features comparing to previous materials, although its long-term prognosis is still not consolidated in the literature [4, 7, 18, 25-28].
This study aimed to evaluate the long-term clinical success of using MTA as a sealant material in root perforation treatments, as well as to relate treatment success with preoperative factors such as the presence of initial injury and the location of the treated tooth.
Material and Methods
This study was approved by the ethics committee of Veiga de Almeida University. The dental records of patients with a history of root perforation were analyzed for iatrogenic and physiological etiology. All procedures were performed by the private practice of a single experienced specialist. The clinical examinations, as well as the treatments were conducted using an operating microscope (DFV, Valença, RJ, Brazil). MTA (Maillefer, Ballaigues, Switzerland) was used for all perforation treatments, all canals were sealed using sealer (Pulp Canal Sealer, Kerr, São Paulo, SP, Brazil) and calibrated gutta-percha (Endo Tanari Plus, Manacapuru, AM, Brazil).
The protocol for all cases was initially a coronal access followed by flatting of the perforation area with 1014 HL diamond spherical burrs (KG Sorensen, Brazil). A small curettage and irrigation with 5.25% sodium hypochlorite were promoted, as well as application of calcium hydroxide PA (Biodynamic, Brazil). Whitin the neutralization of inflammatory process, ProRoot MTA (Dentsply Tulsa, Tulsa, OK) was then manipulated with distilled water, inserted and condensed throughout the perforation. In a subsequent session, the MTA stabilization was confirmed and patient orientation was carried out for preservation.
Treatment cases monitored for less than 1 year, with incomplete medical records, with low-quality radiographic images, and patients with systemic or immune impairment were excluded from this study.
After analysis of the records and according to the previously mentioned exclusion criteria, 53 cases were selected in which the following data was pooled: age, gender, tooth location (anterior/posterior), jaw (mandible/maxilla), presence or absence of radiolucent lesion, follow up time and final radiographical/clinical assessment.
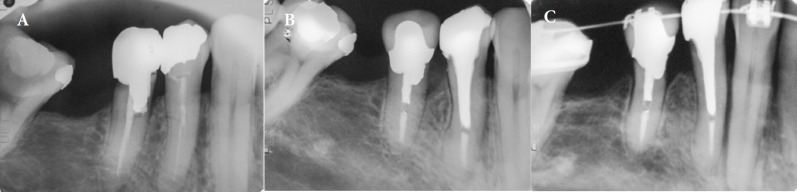
The clinical criteria of success included absence of pain, swelling, sinus tract or defects in the periodontal site of perforation. Radiographically, the criteria of healing was absence of periapical or adjacent to the perforation lesions [29]. Using Cohen’s kappa coefficient, two blinded examiners analyzed three radiographs from each patient’s record that were taken at three different times (Figures 1 to 10): initial radiograph (before treatment), final radiograph (immediately after treatment), and monitoring radiograph (the last radiograph of the case control contained in the dental record). On the initial radiograph, the examiners were asked to analyze the presence or absence of radiolucent injury adjacent to the perforation; in the final radiograph, they additionally confirmed the sealing of the perforation with MTA; and on the monitoring radiograph, they analyzed whether the treatment was successful by comparing it with the final radiograph. The evaluators considered repair as successful if there was new bone formation in the damaged area and increased radiopacity or absence of a pathological process; repairs were deemed unsuccessful if there was an increase or appearance of a radiolucent area in the dental root surrounding the tissues.
Figure 1.
Example of scanned radiographs of a successful case. A) Initial radiograph (05/08/1998) demonstrating a premolar with bone loss in the mesial of the cervical area; B) Final radiograph (02/09/1998) illustrating sealing of a perforation with MTA; C) Monitoring radiograph (10/05/2014) showing a radiopaque area adjacent to the perforation, indicating success because of the normal physiology of the environment, even after 15 years 4 months of treatment
Figure 10.
Example of scanned radiographs of an unsuccessful case. A) Initial radiograph (21/06/1999) illustrating an upper lateral incisor with perforation in the distal area; B) Final radiograph (08/10/1999) presenting complete filling of the injury with MTA; C) Monitoring radiograph (01/04/2002) showing development of radiolucent injury around the MTA, after 2 years 5 months of treatment
Statistical analysis
The data obtained from the records and from the evaluations made by the examiners was statistically analyzed with IBM SPSS Version 21.0 software (IBM Corporation, Armonk, NY, USA), using the nonparametric chi-square test suitable for crossing the categorical variables. The level of significance was set at P≤0.05.
Figure 2.
Example of scanned radiographs of a successful case. A) Initial radiograph (24/08/2001) demonstrating a left upper central incisor with root resorption and presence of initial injury; B) Final radiograph (15/11/2001) illustrating sealing of a perforation with MTA; C) Monitoring radiograph (15/04/2014) showing a radiopaque area where there was previously radiolucent lesion, indicating success, after 12 years 4 months of treatment
Figure 3.
Example of scanned radiographs of a successful case. A) Initial radiograph (19/12/2001) demonstrating a lower molar with furcal perforation and without radiolucent area; B) Final radiograph (27/02/2002) illustrating sealing of a perforation with MTA; C) Monitoring radiograph (04/04/2014) showing furcation region with absence of radiolucent area, indicating success of treatment, even after 12 years 1 month
Results
As shown in Table 1, 37 cases (69.8%) out of 53 were classified as successful by the examiners, with a monitoring time ranging from 1 to 16.25 years (average of six years). The presence of initial injury was observed in 42 (79.2%) teeth, with a higher percentage of treated teeth in the maxilla (n=33; 62.3%) than in the mandible. Most of the cases classified as successful (n=28, 75.7%) presented an initial injury, as did most of the cases classified as unsuccessful (n=14, 87.5%). There was no statistically significant difference (P=0.330). Most of the cases classified as successful (n=27, 73.0%) were located in the maxilla, while most of the cases classified as unsuccessful were located in the mandible (n=10, 62.5%). Therefore, the success of root perforation treatments with MTA presented a statistically significant difference when the location of the impacted tooth was considered (P=0.014). Table 2 shows the clinical findings.
Table 1.
Influence of the location (maxilla or mandible) and presence of initial injury in successful treatments
| Frequency | Successful | Unsuccessful | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Location | Maxilla | 27 | 73,0 | 6 | 37,5 |
| Mandible | 10 | 27,0 | 10 | 62,5 | |
| Total | 37 | 100,0 | 16 | 100,0 | |
| Initial injury | Yes | 28 | 75,7 | 14 | 87,5 |
| No | 9 | 24,3 | 2 | 12,5 | |
| Total | 37 | 100,0 | 16 | 100,0 | |
Table 2.
Demographic information of patients’
| Case | Age | Gender | Arch | Region | Presence of radiolucent lesion | Fallow up time (years) |
Final radiographic/
clinical assessment |
|---|---|---|---|---|---|---|---|
| 1 | 24 | Male | Maxilla | Anterior | Yes | 1.6 | Failure |
| 2 | 32 | Female | Maxilla | Anterior | Yes | 12.7 | Healing |
| 3 | 37 | Male | Maxilla | Anterior | Yes | 12.3 | Healing |
| 4 | 55 | Male | Mandible | Posterior | Yes | 1.25 | Healing |
| 5 | 43 | Female | Mandible | Posterior | Yes | 3.2 | Failure |
| 6 | 32 | Female | Mandible | Anterior | Yes | 1.3 | Healing |
| 7 | 37 | Female | Maxilla | Anterior | Yes | 1.4 | Healing |
| 8 | 28 | Female | Mandible | Posterior | Yes | 1.75 | Failure |
| 9 | 23 | Male | Maxilla | Anterior | Yes | 1.0 | Healing |
| 10 | 35 | Female | Mandible | Posterior | Yes | 6.0 | Healing |
| 11 | 49 | Male | Mandible | Posterior | Yes | 1.25 | Failure |
| 12 | 30 | Male | Mandible | Posterior | Yes | 1.5 | Failure |
| 13 | 56 | Female | Maxilla | Anterior | Yes | 1.8 | Healing |
| 14 | 48 | Female | Maxilla | Anterior | Yes | 1.5 | Healing |
| 15 | 50 | Female | Mandible | Anterior | Not | 1.3 | Healing |
| 16 | 51 | Female | Mandible | Posterior | Yes | 2.0 | Failure |
| 17 | 27 | Female | Mandible | Anterior | Yes | 1.2 | Failure |
| 18 | 49 | Female | Maxilla | Posterior | Yes | 2.2 | Healing |
| 19 | 42 | Female | Mandible | Posterior | Yes | 3.0 | Failure |
| 20 | 26 | Male | Maxilla | Anterior | Not | 2.4 | Failure |
| 21 | 29 | Female | Mandible | Posterior | Yes | 1.3 | Failure |
| 22 | 43 | Female | Maxilla | Anterior | Not | 1.3 | Healing |
| 23 | 36 | Male | Maxilla | Anterior | Not | 1.5 | Healing |
| 24 | 37 | Female | Maxilla | Anterior | Not | 2.7 | Healing |
| 25 | 29 | Female | Maxilla | Anterior | Yes | 2.8 | Healing |
| 26 | 46 | Female | Mandible | Anterior | Yes | 9.2 | Failure |
| 27 | 32 | Female | Maxilla | Posterior | Yes | 1.25 | Healing |
| 28 | 30 | Female | Mandible | Posterior | Yes | 15.3 | Healing |
| 29 | 25 | Male | Maxilla | Anterior | Not | 2.5 | Healing |
| 30 | 31 | Female | Maxilla | Anterior | Yes | 4.3 | Healing |
| 31 | 33 | Male | Maxilla | Anterior | Yes | 1.4 | Failure |
| 32 | 40 | Male | Maxilla | Anterior | Yes | 4.0 | Failure |
| 33 | 33 | Female | Mandible | Posterior | Yes | 1.7 | Healing |
| 34 | 42 | Female | Maxilla | Posterior | Not | 9.4 | Failure |
| 35 | 37 | Female | Maxilla | Posterior | Not | 13.5 | Healing |
| 36 | 38 | Female | Mandible | Posterior | Not | 12.1 | Healing |
| 37 | 35 | Male | Maxilla | Anterior | Yes | 13.8 | Failure |
| 38 | 26 | Female | Mandible | Posterior | Yes | 15.8 | Healing |
| 39 | 34 | Female | Maxilla | Posterior | Yes | 16.25 | Healing |
| 40 | 43 | Female | Maxilla | Anterior | Yes | 9.7 | Healing |
| 41 | 52 | Female | Maxilla | Anterior | Yes | 12.75 | Healing |
| 42 | 50 | Female | Maxilla | Anterior | Yes | 12.4 | Healing |
| 43 | 39 | Female | Maxilla | Anterior | Yes | 2.2 | Healing |
| 44 | 32 | Male | Mandible | Posterior | Yes | 12.7 | Healing |
| 45 | 35 | Female | Maxilla | Anterior | Yes | 2.7 | Healing |
| 46 | 27 | Female | Maxilla | Anterior | Yes | 16.1 | Healing |
| 47 | 38 | Female | Maxilla | Posterior | Yes | 12.6 | Healing |
| 48 | 46 | Female | Maxilla | Posterior | Not | 3.6 | Healing |
| 49 | 44 | Female | Mandible | Posterior | Yes | 8.9 | Healing |
| 50 | 45 | Male | Maxilla | Anterior | Not | 8.25 | Healing |
| 51 | 41 | Female | Mandible | Posterior | Yes | 13.75 | Failure |
| 52 | 35 | Female | Maxilla | Posterior | Yes | 9.6 | Healing |
| 53 | 38 | Female | Maxilla | Anterior | Yes | 6.7 | Healing |
Figure 4.
Example of scanned radiographs of a successful case. A) Initial radiograph (18/06/2001) demonstrating an upper central incisor with furcal perforation; B) Final radiograph (22/08/2001) illustrating sealing of a perforation with MTA; C) Monitoring radiograph (15/04/2014) showing the success after 12 years 8 months of treatment
Figure 5.
Example of scanned radiographs of a successful case. A) Initial radiograph (19/12/1997) demonstrating an upper first molar with furcal perforation; B) Final radiograph (29/01/1998) illustrating sealing of a perforation with MTA; C) Monitoring radiograph (01/04/2014) showing success after 16 years 3 months of treatment
Figure 6.
Example of scanned radiographs of an unsuccessful case. A) Initial radiograph (12/06/2000) illustrating a lower molar with perforation in the furcation area, with presence of initial injury; B) Final radiograph (26/06/2000) presenting complete filling of the injury with MTA; C) Monitoring radiograph (23/04/2014) showing development of radiolucent injury in the furcation area after 13 years 9 months of treatment
Figure 7.
Example of scanned radiographs of an unsuccessful case. A) Initial radiograph (16/04/2001) illustrating an upper first premolar with root perforation in the region of the apical third of the root, with presence of initial injury; B) Final radiograph (02/05/2001) presenting complete filling of the injury with MTA; C) Monitoring radiograph (28/03/2014) showing presence of radiolucent lesion after root end resection, after 13 years 10 months of treatment
Figure 8.
Example of scanned radiographs of an unsuccessful case. A) Initial radiograph (20/10/2000) illustrating an upper central incisor with mesial perforation and presence of initial injury; B) Final radiograph (20/11/2000) presenting complete filling of the injury with MTA; C) Monitoring radiograph (10/04/2002) showing the unsuccess after 1 year 5 months of treatment
Figure 9.
Example of scanned radiographs of an unsuccessful case. A) initial radiograph (14/12/1990) illustrating a lower first premolar with cervical perforation, with presence of initial injury; B) Final radiograph (15/01/1991) presenting complete filling of the injury with MTA; C) Monitoring radiograph (18/09/2000) showing bone loss at the mesial crest and discontinuity of the periodontal ligament hard blade in the apex region, after 9 years 2 months of treatment
Discussion
The presence of root perforation or failure in perforation sealing may cause a pathological process known as bone lysis, which can be identified on radiographic examination as a radiolucent area adjacent to the dental root [6, 8, 10, 17, 30]. Therefore, in this study, the evaluators considered a repair as successful if there was new bone formation in the damaged area and increased radiopacity or absence of a pathological process; repairs were deemed unsuccessful if there was an increase or appearance of a radiolucent area in the dental root surrounding the tissues. These parameters were also adopted in other retrospective studies [5, 7, 15, 31].
There are some divergences among studies regarding the influence of preoperative factors such as position (posterior or anterior teeth), location (maxilla or in the mandible), injury prior to treatment, size of the perforation, and others, in the treatment prognosis [10, 13-15, 31]. However, a meta-analysis published in 2015 made it possible to conclude that only two preoperative aspects influence the outcome of treatment of root perforations with MTA [7]. The first is the presence or absence of pretreatment injury; a radiolucent injury associated with root perforation may indicate greater contamination and, consequently, more advanced progression of the pathological process. The second is the location of the affected tooth (maxilla or mandible); better blood irrigation from more porous trabecular bone in the maxilla in relation to the mandible, which comprises very cortical bone tissue, may facilitate the process of tissue repair [7].
The success rate found in this study (69.8%) is in agreement with the average reported in the literature, according to a meta-analysis [7], in which averages ranged from 67.1% to 89.8%. Some studies [14, 15] reported a success rate of 86%; however, the monitoring time was relatively short, with an average of 33 months (2.75 years), and the longest case running for 8.9 years. Pontius et al. [16] reported a success rate of 90% for 50 treated teeth, yet several teeth were monitored for a short period of time; 20 of them for less than 2 years, and, some for less than 1 year. In studies in which the reevaluation time was longer [13], with an average follow-up of 3.4 years and the highest case being 10-year period, the success rate was reduced to 73.3%. Some authors [15], therefore, have speculated that the probability of success decreases over time, and that only after a period of 4 years the treatment of root perforations with MTA can be considered stable with clear signs of recovery of the periodontal structure. Siew et al. [7] reported that several treatments classified as “incomplete cure” were grouped into the “successful” group, especially in studies with short monitoring times, and this may influence the success rate. The average reevaluation time in the present study was 6.0 years, with a longer control time of 16.25 years, which may explain a lower success rate compared with other studies. The longest monitoring time found in the literature [7, 15] for the treatment of root perforations with MTA was 116 months (9.66 years) and an average of 37 months (3.08 years).
Some authors report the presence of an initial injury as a relevant preoperative factor in the prognosis of root perforation treatment, claiming that it is in communication with the mouth longer and, consequently, is more contaminated and has a greater likelihood of progressing to periodontal degradation [7, 13]. In this study, although the unsuccessful cases were more often observed in teeth with radiolucent injury associated with perforation (87.5%), a high success rate was also observed in treatment of teeth with initial injury (75.7%). Therefore, the presence or absence of initial injury was not statistically relevant, which contradicts other retrospective studies [14, 15, 31]. Endodontic treatment, in general, meets the disinfection and sealing premises, as does root perforation, provided that good cleaning and disinfection of the perforation is performed, followed by sealing with adequate materials, both to accomplish sealing and to stimulate the tissue repair. Preoperative factors, such as the time between occurrence and sealing, size of the injury, and the presence of injury associated with perforation, become irrelevant [7].
Another preoperative factor discussed in the literature as possibly influencing the successful sealing of root perforations is the location of the affected tooth. According to a meta-analysis, it was possible to find a larger number of successful cases in teeth located in the maxilla [7]. That result was corroborated by this study, in which the treatment of 73.0% of the maxillary teeth was successful, and a large percentage of unsuccessful cases involved teeth located in the mandible (62.5%).
Considering the divergent results in relation to the preoperative factors, current studies have attempted to correlate these factors with final result of sealing treatments of root perforations [7, 13, 15]. In this study, when correlating the presence of initial injury with success and location of the affected tooth, only the location of the tooth was statistically relevant. We emphasize that the better prognosis for maxillary teeth is likely because of better vascularization, enabling more effective periodontal repair. In addition, it is important to highlight that the presence of initial injury was not statistically relevant in this research. However, for this correlation to be valid in clinical practice, it is necessary that all perforations be adequately cleaned and disinfected, followed by effective sealing with MTA.
It is important to note that long-term retrospective studies correlating preoperative factors with the results of root perforation treatment with MTA are rare in the literature, and there are no studies that present an average monitoring time of more than 4 years. This 4-year period was established by Mente et al. [14] and Mente et al. [15] as the average period for the therapy to be considered successful/unsuccessful. Therefore, studies of root perforation treatments with longer monitoring times are required [32], bearing in mind that the survival of the dental element in the oral cavity depends on other factors such as periodontal conditions and prosthetic rehabilitations.
Conclusion
Considering the limitations and findings of this study, root perforations sealed with MTA achieved a success rate of 69.8% over a monitoring period of 1-16.25 years. The presence of initial injury did not influence the treatment prognosis; on the other hand, the location of the affected tooth influenced the result. It was also possible to conclude that root perforations in the maxilla had a higher success rate.
Conflict of Interest:
‘None declared’.
References
- 1.Maurice CG. An annotated glossary of terms used in endodontics American Association of Endodontists. Oral Surg Oral Med Oral Pathol. 1968;25(3):491–512. doi: 10.1016/0030-4220(68)90027-3. [DOI] [PubMed] [Google Scholar]
- 2.Alhadainy HA. Root perforations A review of literature. Oral Surg Oral Med Oral Pathol. 1994;78(3):368–74. doi: 10.1016/0030-4220(94)90070-1. [DOI] [PubMed] [Google Scholar]
- 3.Borkar S, de Noronha de Ataide I. Management of a massive resorptive lesion with multiple perforations in a molar: case report. J Endod. 2015;41(5):753–8. doi: 10.1016/j.joen.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 4.Tsesis I, Fuss Z. Diagnosis and treatment of accidental root perforations. Endod Topics. 2006;13(1):95–107. [Google Scholar]
- 5.Unal GC, Maden M, Isidan T. Repair of furcal iatrogenic perforation with mineral trioxide aggregate: two years follow-up of two cases. Eur J Dent. 2010;4(4):475–81. [PMC free article] [PubMed] [Google Scholar]
- 6.Saatchi M, Mohammadi G, Vali Sichani A, Moshkforoush S. Technical Quality of Root Canal Treatment Performed by Undergraduate Clinical Students of Isfahan Dental School. Iran Endod J. 2018;13(1):88–93. doi: 10.22037/iej.v13i1.18517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siew K, Lee AH, Cheung GS. Treatment outcome of repaired root perforation: a systematic review and meta-analysis. J Endod. 2015;41(11):1795–804. doi: 10.1016/j.joen.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Zambon da Silva P, Carlos Ribeiro F, Machado Barroso Xavier J, Pratte-Santos R, Demuner C. Radiographic Evaluation of Root Canal Treatment Performed by Undergraduate Students, Part I; Iatrogenic Errors. Iran Endod J. 2018;13(1):30–6. doi: 10.22037/iej.v13i1.16800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camilo do Carmo Monteiro J, Rodrigues Tonetto M, Coelho Bandeca M, Henrique Borges A, Claudio Martins Segalla J, Cristina Fagundes Jordao-Basso K, Fernando Sanchez-Puetate C, Carlos Kuga M. Repair of Iatrogenic Furcal Perforation with Mineral Trioxide Aggregate: A Seven-Year Follow-up. Iran Endod J. 2017;12(4):516–20. doi: 10.22037/iej.v12i4.16888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsesis I, Rosenberg E, Faivishevsky V, Kfir A, Katz M, Rosen E. Prevalence and associated periodontal status of teeth with root perforation: a retrospective study of 2,002 patients' medical records. J Endod. 2010;36(5):797–800. doi: 10.1016/j.joen.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Ingle JI. A standardized endodontic technique utilizing newly designed instruments and filling materials. Oral Surg Oral Med Oral Pathol. 1961;14(1):83–91. doi: 10.1016/0030-4220(61)90477-7. [DOI] [PubMed] [Google Scholar]
- 12.Seltzer S, Sinai I, August D. Periodontal effects of root perforations before and during endodontic procedures. J Dent Res. 1970;49(2):332–9. doi: 10.1177/00220345700490022301. [DOI] [PubMed] [Google Scholar]
- 13.Krupp C, Bargholz C, Brusehaber M, Hulsmann M. Treatment outcome after repair of root perforations with mineral trioxide aggregate: a retrospective evaluation of 90 teeth. J Endod. 2013;39(11):1364–8. doi: 10.1016/j.joen.2013.06.030. [DOI] [PubMed] [Google Scholar]
- 14.Mente J, Hage N, Pfefferle T, Koch MJ, Geletneky B, Dreyhaupt J, Martin N, Staehle HJ. Treatment outcome of mineral trioxide aggregate: repair of root perforations. J Endod. 2010;36(2):208–13. doi: 10.1016/j.joen.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 15.Mente J, Leo M, Panagidis D, Saure D, Pfefferle T. Treatment outcome of mineral trioxide aggregate: repair of root perforations-long-term results. J Endod. 2014;40(6):790–6. doi: 10.1016/j.joen.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Pontius V, Pontius O, Braun A, Frankenberger R, Roggendorf MJ. Retrospective evaluation of perforation repairs in 6 private practices. J Endod. 2013;39(11):1346–58. doi: 10.1016/j.joen.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Subay RK, Subay MO, Tuzcu SB. Endodontic management of root perforating internal replacement resorption. Eur J Dent. 2018;12(3):450–3. doi: 10.4103/ejd.ejd_31_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balla R, LoMonaco CJ, Skribner J, Lin LM. Histological study of furcation perforations treated with tricalcium phosphate, hydroxylapatite, amalgam, and Life. J Endod. 1991;17(5):234–8. doi: 10.1016/S0099-2399(06)81928-X. [DOI] [PubMed] [Google Scholar]
- 19.Bogaerts P. Treatment of root perforations with calcium hydroxide and SuperEBA cement: a clinical report. Int Endod J. 1997;30(3):210–9. doi: 10.1046/j.1365-2591.1997.00067.x. [DOI] [PubMed] [Google Scholar]
- 20.Fischer EJ, Arens DE, Miller CH. Bacterial leakage of mineral trioxide aggregate as compared with zinc-free amalgam, intermediate restorative material, and Super-EBA as a root-end filling material. J Endod. 1998;24(3):176–9. doi: 10.1016/S0099-2399(98)80178-7. [DOI] [PubMed] [Google Scholar]
- 21.Ramazani N, Sadeghi P. Bacterial Leakage of Mineral Trioxide Aggregate, Calcium-Enriched Mixture and Biodentine as Furcation Perforation Repair Materials in Primary Molars. Iran Endod J. 2016;11(3):214–8. doi: 10.7508/iej.2016.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altan H, Tosun G. The setting mechanism of mineral trioxide aggregate. J Istanb Univ Fac Dent. 2016;50(1):65–72. doi: 10.17096/jiufd.50128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torabinejad M, Parirokh M, Dummer PMH. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part II: other clinical applications and complications. Int Endod J. 2018;51(3):284–317. doi: 10.1111/iej.12843. [DOI] [PubMed] [Google Scholar]
- 24.Rahoma A, AlShwaimi E, Majeed A. Push-out bond strength of different types of mineral trioxide aggregate in root dentin. Int J Health Sci (Qassim) 2018;12(5):66–9. [PMC free article] [PubMed] [Google Scholar]
- 25.Katsamakis S, Slot DE, Van der Sluis LW, Van der Weijden F. Histological responses of the periodontium to MTA: a systematic review. J Clin Periodontol. 2013;40(4):334–44. doi: 10.1111/jcpe.12058. [DOI] [PubMed] [Google Scholar]
- 26.Kim JR, Nosrat A, Fouad AF. Interfacial characteristics of Biodentine and MTA with dentine in simulated body fluid. J Dent. 2015;43(2):241–7. doi: 10.1016/j.jdent.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 27.Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod. 1995;21(7):349–53. doi: 10.1016/S0099-2399(06)80967-2. [DOI] [PubMed] [Google Scholar]
- 28.Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod. 1993;19(12):591–5. doi: 10.1016/S0099-2399(06)80271-2. [DOI] [PubMed] [Google Scholar]
- 29.Pace R, Giuliani V, Pagavino G. Mineral trioxide aggregate as repair material for furcal perforation: case series. J Endod. 2008;34(9):1130–3. doi: 10.1016/j.joen.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 30.Guedes OA, da Costa MV, Dorileo MC, de Oliveira HF, Pedro FL, Bandeca MC, Borges AH. Detection of procedural errors during root canal instrumentation using cone beam computed tomography. J Int Oral Health. 2015;7(3):28–32. [PMC free article] [PubMed] [Google Scholar]
- 31.Main C, Mirzayan N, Shabahang S, Torabinejad M. Repair of root perforations using mineral trioxide aggregate: a long-term study. J Endod. 2004;30(2):80–3. doi: 10.1097/00004770-200402000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Cosme-Silva L, Carnevalli B, Sakai VT, Viola NV, Franco de Carvalho L, Franco de Carvalho EM. Radicular Perforation Repair with Mineral Trioxide Aggregate: A Case Report with 10-Year Follow-up. Open Dent J. 2016;10:733–8. doi: 10.2174/1874210601610010733. [DOI] [PMC free article] [PubMed] [Google Scholar]