Abstract
Restorative sleep is an important component of quality of life. Disturbances in sleep after burn injury were reported but all based on uncontrolled or nonstandardized data. The occurrence and the effect of long-term sleep problems in young adult burn survivors have not been well defined. This 5-year (2003–2008) prospective multicenter longitudinal study included adults with burn injuries ages 19 to 30 years who completed the Young Adult Burn Outcome Questionnaire (YABOQ) up to 36 months after injury. The items measured 15 patient-reported outcomes including physical, psychological, and social statuses and symptoms such as itch and pain. Scores of these 15 YABOQ outcome domains were standardized to a mean of 50 and a SD of 10 based on an age-matched nonburned reference group of young adults. Sleep quality was assessed using the item "How satisfied are you now with your sleep," rated by a 5-point Likert scale. Patients responding with very and somewhat dissatisfied were classified as having sleep dissatisfaction and the remaining as less or not dissatisfied. The associations between sleep dissatisfaction (yes/no) and YABOQ outcome domains were analyzed longitudinally using mixed-effect generalized linear models, adjusted for %TBSA burned, age, gender, and race. Generalized estimating equations were used to take into account correlated error resulting from repeated surveys on each patient over time. One hundred and fifty-two burn survivors participated in the YABOQ survey at baseline and during the follow-up who had at least one survey with a response to the sleep item. Among them, sleep dissatisfaction was twice as prevalent (76/152, 50%) when compared with the nonburned reference group (29/112, 26%). The likelihood of a burn survivor being dissatisfied with sleep was reduced over time after the burn injury. Sleep dissatisfaction following burns was significantly associated, in a dose-dependent manner, with increasing burn size (P = .001). Better sleep was associated with better outcomes in all domains (P < .05) except Fine Motor Function, and this association was significantly more apparent in the longer term compared with the shorter term with the same domains (P < .05). Dissatisfaction with sleep is highly prevalent following burn injuries in young adults. Lower satisfaction with sleep is associated with poorer scores in nearly all quality of life measures. Satisfaction with sleep should be addressed during the long-term clinical follow-up of young adults with burn injuries. Further research should be undertaken to understand the components of sleep quality that are important to burn survivors and which ones might be modified and tested in future intervention studies.
Restorative sleep is an important component of quality of life, particularly for young adults.1 Sleep deprivation in young adults can affect well being, performance and even public safety, and impair executive function.2,3 In college students, lower performance in health-related physical fitness assessments is associated with poor sleep quality and decreased total sleep time.4 In young adults, sleep is also important for psychosocial function.5 Sleep restriction also can alter the body’s response to stress by promoting an inflammatory response including alterations in interleukin-6, tumor necrosis factor-α, and peak cortisol secretion.2,6 Conversely, improving sleep is associated with decreased inflammation.3
Sleep disturbance is almost universal in patients of every age group with medical and surgical problems in acute care settings. Severe symptoms of sleep deprivation occur in the burn intensive care unit.7,8 One week after discharge from their acute burn hospitalization, 73% adults studied reported a problem with sleep including frequent nighttime awakenings (87%), napping during the daytime (65%), sleeping alone (64%), experiencing pain during the night (62%), and difficulties with sleep onset (62%).9 Lawrence reported 40% of adults experienced continued sleep disturbance 2 months post discharge.10 Masoodi et al11 studied alterations in sleep architecture in 818 adults after burn injury at 1 year when compared with 600 nonburned adults using the Pittsburgh Sleep Quality Index Questionnaire and showed that 61% of burn survivors had poor sleep compared with 39% of a nonburned population. Sleep problems included difficulty falling asleep attributed to abnormal positions from contractures and pain, nightmares, sleep interrupted by frequent awakening, and difficulty breathing. These studies suggest that sleep disturbance is not only subsequent to an acute illness but, in the case of burns, continues long after acute recovery. In a retrospective study of burned children with acute stress disorder, 60% of subjects suffered from nightmares and 56% had difficulty falling asleep.12 In a prospective study, nightmares and/or difficulty falling asleep were reported by nearly all of the 25 participants.13 In young patients burned as children, Mayes et al14 found dramatic reductions in rapid eye movement sleep, slow wave sleep, and poorer sleep efficiency compared with nonburned controls, persisting for years after the burn. This has been attributed in part to symptoms related to posttraumatic stress disorder (PTSD) over the long term in childhood extending to young adulthood. Actigraphy has also shown dramatic reductions in overall total sleep time in teenage burn survivors, averaging 10.5 years post injury, and these data suggested an average total sleep time of only 5.25 hours.15
These studies in children and adults after burns suggest that poor sleep is a long-term problem. There are no controlled data on the occurrence and persistence of sleep disturbance in young adult burn survivors and the relationship of sleep with important domains of patient-centered outcomes. In this study, we use the Young Adult Burn Outcome Questionnaire (YABOQ) database16 to study self-reported sleep problems in burn injury. We explore the effect of sleep disruption on the multidimensional recovery of young adult burn survivors and compare this with an age-matched cohort without burn injuries. The hypothesis of this work is that young adult burn survivors experience greater dissatisfaction with sleep than their age-matched nonburned peers; that this problem permeates areas outside of their surgical and medical care settings and extends to the home, workplace, and affects other social aspects of their functioning. Furthermore, we hypothesize that sleep problems can persist for years after the injury. Following the course of recovery in young adult burn survivors with rich cohort data will pave the way to understanding the important points in the course of recovery where future clinical and social interventions can be implemented during the recovery process to impact on problems with sleep.
METHODS
The YABOQ Database
This 5-year (2003–2008) prospective multicenter study included 152 adults with burn injuries ages 19 to 30 years who completed the Young Adult Burn Outcome Questionnaire (YABOQ) from 0 to 36 months after traumatic burn injuries. Inclusion criteria for the burn group were all English speaking patients with burns that occurred on or after their 17th birthday. Burn subjects were approached in outpatient burn clinics after informed consent had been obtained. Questionnaires were administered on enrollment16 and repeated at 2 weeks, 6, 12, 24, and 36 months. Medical records were reviewed for clinical information. Subjects in the reference group were recruited from the community at each of the five study sites distributed across the country (California, Maryland, Massachusetts, Nebraska, and North Carolina). The YABOQ measured 15 domains including: pain, itch, fine motor function, physical function, social function limited by physical function, perceived appearance, social function limited by appearance, sexual function, emotion (persistent anger and sadness), family function, family concern, satisfaction with symptom relief, satisfaction with role, work reintegration, and religion (religion as source of strength and comfort, spiritually oriented, and feeling closeness to a supreme being). Domain scores were standardized to a mean of 50 and a SD of 10 based on an age-matched reference group without burn injuries. Higher scores denote better health, or a return toward or above the age-matched norm-based score for each domain.
The original study protocol was approved by each site’s institutional review board. Permission to review the deidentified YABOQ dataset was approved by the hospital institutional review board.
Assessment of Sleep Dysfunction
Sleep quality was assessed using the YABOQ item, “How satisfied are you now with your sleep,” rated by a 5-point Likert scale. This item is part of the original “satisfaction with symptom relief” domain of the YABOQ. Patients responding with “very” and “somewhat dissatisfied” were classified as those dissatisfied with sleep and the remaining as less or not dissatisfied. The original dataset also asked whether there were sleep problems before the burn injury, with a response of “yes” or “no.”
Association of Sleep Satisfaction with Demographic Characteristics and YABOQ Domains
Patients’ demographic and clinical characteristics and preexisting comorbidities before the burn injury were compared between subjects with sleep dissatisfaction and those without. P values for statistical comparisons were derived from the t-test of two means, the χ2 test or Fisher’s exact test of two proportions, whichever was appropriate. Prevalence rates using ratio and percentage of burn survivors who were dissatisfied with sleep were calculated for survivors with TBSA burned less than 20% (small burn) and those greater than or equal to 20% (large burn) by months since burn.
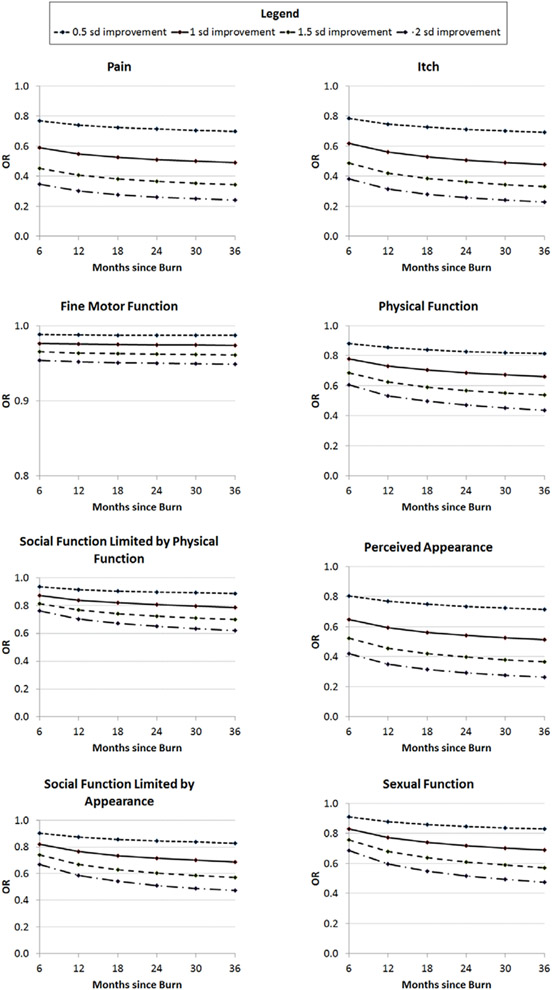
The associations between postburn sleep dissatisfaction (yes/no) and 14/15 YABOQ domains were analyzed longitudinally using mixed-effect generalized linear models (GENMOD) assuming a binomial distribution. Furthermore, the generalized estimating equation technique was used to take into account correlated error resulting from repeated surveys on each patient over time. The models were adjusted for %TBSA burned, age, gender, and race. The GENMOD results were presented as odds ratio (OR) of sleep dissatisfaction for each 1 SD (ie, 10 points) improvement in the YABOQ domain score. These ORs were tabulated at 6 and 36 months since burn injuries with 95% confidence intervals and P values. A significantly lower value of OR below 1 is an indication of positive association between satisfaction with sleep and the YABOQ domain scores. The domain “satisfaction with symptom relief” was not analyzed because the sleep item is part of this particular domain. Furthermore, detailed recovery patterns over time in the OR of sleep dissatisfaction were reported graphically.
RESULTS
One hundred and fifty-two burn survivors participated in the YABOQ surveys. Among them, 76 (50%) subjects showed sleep dissatisfaction at least once during the study period. It was almost twice of that reported by the age-matched, nonburned reference population (29/112, 26%). For the burn survivors who reported sleep dissatisfaction, the mean age at burn injury for these patients was 23.6 ± 3.5 years; mean TBSA burned was 12.5 ± 16%; 57 (75%) were male; 48 (64%) were white, 9 (12%) black, 7 (9%) Hispanic, and 11 (15%) others (Table 1). These compared with the rest of the burn survivor group who never reported dissatisfaction with sleep (N = 76; 50%): the mean age at burn injury, 24.8 ± 3.4 years; mean TBSA, 9.7 ± 11.4%; 54 (71%) male; 45 (60%) white, 9 (12%) black, 8 (11%) Hispanic, and 13 (17%) others. No significant differences resulted in these parameters other than age at burn (P = .04), indicating that the survivors who had sleep dissatisfaction were slightly younger. Medical conditions before burn were compared between those burn survivors with postburn dissatisfaction with sleep and those without (Table 2). Again, no significant differences were found except for epilepsy (P = .04). There was no significant association between those survivors who reported sleep problems before the injury and those with sleep dissatisfaction after the injury (P = .77).
Table 1.
Demographic and Clinical Characteristics of Young Adult Burn Survivors at Baseline by Sleep Problems (Total N = 152)
| Variable | Less or Not Dissatisfied With Sleep (N = 76) |
Dissatisfied With Sleep (N = 76) |
P |
|---|---|---|---|
| Age at burn, mean (SD) | 24.8 (3.4) | 23.6 (3.5) | .04 |
| Age at first survey, mean (SD) | 25.1 (3.5) | 24.2 (3.6) | .13 |
| Number of months from burn to first survey, mean (SD) | 5.5 (14.7) | 5.2 (15.0) | .90 |
| %TBSA, mean (SD) | 9.7 (11.4) | 12.5 (16.0) | .23 |
| Gender, N (%) | |||
| Male | 54 (71.1) | 57 (75.0) | .58 |
| Female | 22 (29.0) | 19 (25.0) | |
| Race, N (%) | |||
| White | 45 (60.0) | 48 (64.0) | .61 (white vs others) |
| Black | 9 (12.0) | 9 (12.0) | |
| Hispanic | 8 (10.7) | 7 (9.3) | |
| Others | 13 (17.3) | 11 (14.7) | |
| Inhalation injury, N (%) | 6 (8.0) | 6 (8.1) | .98 |
| Face involved, N (%) | 25 (32.9) | 22 (30.1) | .72 |
| Hands involved, N (%) | 44 (58.7) | 40 (55.6) | .70 |
| Genitals involved, N (%) | 2(2.7) | 2 (2.7) | 1.00 |
| Amputation required, N (%) | 1 (1.4) | 2 (3.0) | .61 |
P values were derived from t-test of two means, χ2 test or Fisher’s exact test of two proportions, whichever was appropriate.
For the age-matched nonburned reference group, 29 of 112 (25.9%) individuals reported sleep dissatisfaction in at least one survey.
Table 2.
Medical Conditions of Young Adult Burn Patients Before Burn Injury (N = 152)
| Medical Condition | Less or No Sleep Problem (N = 76), N (%) |
Had Sleep Problems (N = 76), N (%) |
P |
|---|---|---|---|
| Asthma | 9 (11.8) | 13 (17.1) | |
| Attention deficit hyperactivity disorder (ADHD) | 9 (11.8) | 9 (11.8) | |
| Chronic allergies or sinus trouble | 5 (6.6) | 10 (13.2) | |
| Diabetes | 5 (6.6) | 10 (13.2) | |
| Epilepsy (seizure disorder) | 3 (3.9) | 10 (13.2) | .04 |
| Hearing problem | 2 (2.6) | 3 (3.9) | |
| Heart problem | 9 (11.8) | 9 (11.8) | |
| Learning problem | 6 (7.9) | 5 (6.6) | |
| Sleep problem | 7 (9.2) | 6 (7.9) | |
| Speech problems | 5 (6.6) | 6 (7.9) | |
| Vision problems | 4 (5.3) | 5 (6.6) | |
| Depression | 5 (6.6) | 11 (14.5) | |
| Drug problem | 2 (2.6) | 7 (9.2) | |
| Alcohol problem | 2 (2.6) | 4 (5.3) | |
| Smoking habit | 6 (7.9) | 4 (5.3) | |
| Pregnancy (female only) | 3 (3.9) | 1 (1.3) | |
| Anemia | 1 (1.3) | 3 (3.9) | |
| High blood pressure | 4 (5.3) | 6 (7.9) | |
| Stomach problems (ulcer) | 2 (2.6) | 4 (5.3) | |
| Liver problems | 3 (3.9) | 7 (9.2) | |
| Kidney problems | 20 (26.3) | 16 (21.1) | |
| Other medical problem | 9 (11.8) | 7 (9.2) |
P values were derived from χ2 or Fisher’s exact test of two proportions, whichever was appropriate. All medical conditions were not significant with the exception of epilepsy P = .04.
The Effect of Burn Size on Sleep Dissatisfaction
The occurrence of sleep dissatisfaction was associated with increasing burn size (Table 3). During the baseline (0–6 months since burn injury), a total of 56 of 172 (33%) survey records showed sleep dissatisfaction, 32% of those with less than 20% TBSA and 43% of those with greater than or equal to 20% TBSA (P = .30; Table 3). During the next 6 months, however, the percent dissatisfaction with sleep showed significant disparity between these two TBSA groups: 9% vs 57% (P < .0001) for TBSA less than 20% vs greater than or equal to 20%, respectively. The disparity persisted after 12 months since burn injury in which 10% of surveys indicated sleep dissatisfaction among burn survivors with TBSA less than 20%, much lower than 38% of surveys among those with TBSA greater than or equal to 20% (P = .0148).
Table 3.
Ratio and Percentage of Burn Survivors Who Were Dissatisfied with Sleep Stratified by Burn Size
| Months Since Burn | All | TBSA Burned <20% | TBSA Burned ≥20% | P |
|---|---|---|---|---|
| 0 to ≤6 | 56/172 (33%) | 47/149 (32%) | 9/21 (43%) | .30 |
| >6 to ≤12 | 13/59 (22%) | 4/43 (9%) | 8/14 (57%) | <.0001 |
| >12 to ≤36 | 12/52 (23%) | 5/50 (10%) | 8/21 (38%) | .0148 |
| All | 82/302 (27%) | 56/242 (23%) | 25/56 (45%) | .0011 |
The unit of analysis was survey record, rather than unique patient.
In each cell, the ratio is the number of surveys that showed dissatisfaction with sleep divided by the total number of surveys for that cell.
Overall, 35 of 249 (14.1%) survey records by the age-matched nonburned reference group had sleep dissatisfaction, compared with 82 of 302 (27%) shown in the table for burned sample.
P values were derived from χ2 or Fisher’s exact test of two proportions, whichever was appropriate.
Associations Between Sleep Dissatisfaction and YABOQ Burn Outcome Domains at Baseline and Up to 6 Months After Burn Injury
Sleep dissatisfaction was associated with all YABOQ burn outcome domains except “fine motor function” during the first 6-month baseline period. More specifically, a score improvement in the associated domain resulted in a decreased odds for sleep dissatisfaction. For example, for the pain domain, a 1 SD better score yielded an OR of 0.59 (95% confidence limits, 0.48–0.72; P < .0001) of sleep dissatisfaction, representing a reduction of 0.41 (=1–0.59) in the odds of risk of sleep dissatisfaction (Table 4). It should be noted that 1 SD better score is equivalent to 10 points better in the standardized score as described in the Methods section. The OR of sleep dissatisfaction when the domain score is better by 1 SD varied from 0.49 (0.40–0.60, satisfaction with role) to 0.87 (0.82–0.93, social function limited by physical function) for all domains, with P value ranged from less than .05 to less than .0001, except fine motor function.
Table 4.
OR of Sleep Dissatisfaction Using Logistic Regression
| Months Since Burn | ||||||||
|---|---|---|---|---|---|---|---|---|
| 6 |
36 |
Reduction in OR |
||||||
| Domain | OR | 95% CL | P | OR | 95% CL | P | ΔOR | P |
| Pain | 0.59 | 0.48–0.72 | § | 0.49 | 0.38–0.63 | § | 0.1 | † |
| Itch | 0.62 | 0.52–0.74 | § | 0.48 | 0.36–0.63 | § | 0.14 | † |
| Fine motor | 0.98 | 0.95–1.01 | NS | 0.97 | 0.92–1.03 | NS | 0.003 | NS |
| Physical function | 0.78 | 0.7–0.86 | § | 0.66 | 0.56–0.79 | § | 0.12 | ‡ |
| Social function limited by physical function | 0.87 | 0.82–0.93 | § | 0.79 | 0.69–0.89 | § | 0.08 | * |
| Perceived appearance | 0.65 | 0.54–0.78 | § | 0.51 | 0.39–0.67 | § | 0.14 | † |
| Social function limited by appearance | 0.82 | 0.73–0.91 | ‡ | 0.69 | 0.58–0.81 | § | 0.13 | ‡ |
| Sexual function | 0.83 | 0.7–0.98 | * | 0.69 | 0.56–0.84 | ‡ | 0.14 | § |
| Emotion | 0.58 | 0.49–0.7 | § | 0.46 | 0.36–0.59 | § | 0.12 | § |
| Family function | 0.7 | 0.61–0.8 | § | 0.57 | 0.46–0.7 | § | 0.13 | § |
| Family concern | 0.63 | 0.53–0.76 | § | 0.49 | 0.37–0.64 | § | 0.15 | ‡ |
| Satisfaction with role | 0.49 | 0.4–0.6 | § | 0.4 | 0.3–0.53 | § | 0.09 | † |
| Work reintegration | 0.64 | 0.44–0.93 | * | 0.53 | 0.36–0.79 | † | 0.11 | ‡ |
| Religion | 0.84 | 0.76–0.92 | ‡ | 0.7 | 0.58–0.85 | ‡ | 0.14 | ‡ |
OR, odds ratio; CL, confidence limit.
Reduction in odds of sleep dissatisfaction if domain score is better by 1 SD (10 points).
Mixed-effect generalized linear models with generalized estimating equation were used for logistic regression.
Models were adjusted for %TBSA burned, age, gender, and race.
P < .05.
P < .01.
P < .001.
P < .0001.
Examining the Changes in Sleep Dissatisfaction After Burns Over Time
Table 4 displays the OR of sleep dissatisfaction if a domain score is better by 1 SD at the end of the study period: 36 months since the burn injury. As an example using the pain domain, the OR at the baseline was 0.59, which decreased to 0.49 (95% confidence limits, 0.38–0.63) at 36-month follow-up, a reduction of 0.1 in the OR (P < .01). The amount of OR reduction from 6 to 36 months post burn varied, ranging from 0.08 (P < .05, social function limited by physical function) to 0.15 (P < .001, family concern), excluding fine motor function. This indicates that the affect of improvement in sleep, related to better scores in each YABOQ domain was significantly more apparent in the longer term compared with the shorter term with the same domains (P < .05). Detailed recovery patterns over time in the OR of sleep dissatisfaction were reported graphically for 0.5, 1, 1.5, and 2 SDs better for a domain score (Figure 1). For example, the OR recovery curves for pain domain showed that a better domain score by 0.5, 1, 1.5, or 2 SDs was associated with the change in the OR of sleep dissatisfaction from 0.77 to 0.70, 0.59 to 0.49, 0.45 to 0.34, or 0.35 to 0.24 over the 36-month period, respectively.
Figure 1.
Recovery curves for the odds ratio (OR) of sleep dissatisfaction over time by changes in Young Adult Burn Outcome Questionnaire (YABOQ) domain scores. The impact of improvements in domain scores by 0.5, 1, 1.5, or 2 SD on the OR of sleep dissatisfaction is depicted. These curves show that the risk of sleep dissatisfaction decreases over time from burn, that improvements in all domain scores are associated with decreased risk of sleep dissatisfaction except fine motor function, and that the association of improvement in domain score with decreased risk of sleep dissatisfaction becomes more apparent with time.
DISCUSSION
Sleep dissatisfaction in young adults after burn injuries occurred in half of the population 36 months post injury, and this was twice that in the nonburned, age-matched reference group. The prevalence of a burn survivor being dissatisfied with sleep was reduced over time from when the burn injury occurred. Sleep dissatisfaction after burns was associated, in a dose-dependent manner, with increasing burn size. Better sleep was associated with better outcomes in all domains except fine motor function. Specifically, while controlling for demographics including age, sex, race, and burn size, significant associations were found between dissatisfaction with sleep and the domains of pain, itch, physical function, social function limited by physical function, perceived appearance, social function limited by appearance, sexual function, emotion (persistent anger and sadness), family function, family concern, satisfaction with role, work reintegration, and religion, indicating the pervasive nature of this symptom on a range of quality of life domains in young adult burn survivors. Improvements in domain scores were associated with improvement in sleep dissatisfaction, and this association became stronger with time. It is not possible to know from this work whether the sleep dissatisfaction was because of dysfunction occurring within a particular domain (such as increased pain, itch, or poor family function) or whether it was the poor sleep that made these functional domains worse. It is possible, perhaps likely, that these associations are bidirectional. It is also possible that multiple domains affect sleep at the same time, for example, pain, itch, and emotion. This is the first controlled study to show the multidimensional effect of sleep dissatisfaction over time from burn injury. Given the prevalence of sleep problems and the interaction with multiple other functional domains, sleep quality should be assessed as part of routine longitudinal care after burn injury.
Increasing burn size is known to have a profound negative effect on long-term multidimensional recovery from burn injuries in young adults.17 In this study, sleep disturbance was associated with multidimensional effects after accounting for the effects of burn size. Masoodi et al11 also found that burn size was a significant risk factor for poor sleep in adults at 1 year from acute hospital discharge as measured by the Pittsburg Sleep Quality Index. Further analysis of the Pittsburg Sleep Quality Index questionnaire results revealed that one of the most troublesome aspects of patients’ sleep was the inability to get to sleep because of abnormal positions due to contractures. Increasing burn size is associated with increasing odds of developing a major joint contracture.18 Although burn size itself is not a parameter that can be changed once the accident has happened, it is possible that reconstructive surgery addressing problematic contractures contributing to abnormal sleep positioning or severe neck contractures associated with sleep apnea19 could improve sleep quality.
Dissatisfaction with sleep was associated with worse scores in the domain of physical function. The presence of contractures makes physical activity more difficult and lack of physical activity can make resting difficult at night. In fact, vigorous exercise has been shown to be important in young adults and has mental health benefits beyond moderate physical activity. It is associated with less stress, pain, insomnia, and depression. Young adults who exercise vigorously reported fewer mental health problems if exposed to high stress.20 Again, the association of physical activity with sleep quality is likely bidirectional, and the fate of the symptoms of sleep and lack of physical activity are intermingled.
Increasing odds of sleep dissatisfaction was associated with pain and itch. There is some evidence in the literature that the association of sleep and pain are bidirectional.21 In a study on chronic pain and sleep, a bad pain day did not disrupt a night’s sleep, but once there was a poor night’s sleep, the pain was more difficult to treat the next day.22 Attention to sleep hygiene, timing of pain medications, and possibly medications supporting sleep would be an important component of the care plan, particularly, in regards to pain management. Neuropathic-like pain symptoms and itch in burn survivors23-25 are often evident at nighttime, where light touch, change in temperature, and absence of distractions might trigger the symptom, making it difficult to fall off to sleep. Use of pressure garments to decrease the exposure to light touch and changes in temperature might help reduce pain and improve sleep. Novel treatments, such as transcranial brain stimulation,26 laser treatment of scars,27 or the development of new medications for treating neuropathic-like pain and itch, if successful, should help promote better sleep. Given the difficulties in treating some burn patients for chronic pain and itch, treating sleep might be an important avenue to provide at least some symptomatic relief. In patients with chronic pain, better sleep promotes increased physical activity, which might assist in the ability of the patient’s to cope with the challenges facing burn survivors.
Poor sleep is strongly associated with depressive symptoms,28 yet the long-term association might not be bidirectional.29 Surely, nightmares and other symptoms of disruptive sleep accompany acute stress disorder and PTSD after burn injuries.30-32 One recent study of the Station Nightclub Fire showed that the incidence of PTSD was the same in people who escaped the fire without burn injury as those who sustained burns in the fire33 indicating that PTSD might be related to the circumstances of the accident and not just the burn. This is important to realize because even in survivors with smaller injuries, symptoms of PTSD can occur. In this study, the emotion or mental health domain generally refers to anger and sadness, and these were associated with sleep dissatisfaction in burn survivors. If these symptoms occur along with nightmares or other signs of PTSD, it is recommended that psychiatric evaluation be performed.34
Increased sleep dissatisfaction was associated with lower scores in all of the remaining domains, including social function limited by physical function, perceived appearance, social function limited by appearance, sexual function, family function, family concern, satisfaction with role, work reintegration, and religion. In many of these domains, there is evidence of sleep associations in other scenarios. For instance, there are visual cues of sleep deprivation on facial appearance that may carry social consequences, making the subject appear sadder than in those with normal sleep.35 In another example, impaired libido and insomnia are common symptoms of PTSD in general.36 Medications for depression can also interfere with libido. Improvement in sleep has been associated with improved erectile dysfunction in patients with sleep apnea who begin treatment with continuous positive airway pressure.37 Decreased family function and increased family concern were also associated with the subject’s increasing dissatisfaction with sleep. There is little information on the needs of families supporting a burn survivor through recovery, but a recent conceptual analysis found that the family members experienced emotional containment and vicarious suffering as a result of the family member’s injury.38 One could assume that poor sleep would be a recognizable symptom by families that could cause concern by the family members. For the domain work reintegration, cognitive changes associated with lack of sleep could be impairing relationships with coworkers.39 Further investigation is needed in the accommodations required for return to work after burn injury. Interestingly, higher scores in religion were associated with less sleep dissatisfaction than those with lower religiousity scores. The associations of religiosity and spirituality with quality of life and sleep have been recently studied, albeit in a very different situation. In Muslim women with breast cancer, increased religiosity measured by the spiritual well-being scale and the religious activities scale was associated with less sleep latency and less use of sleep medications.40 It is possible that higher religion scores, or a more open spiritual nature, provide an additional coping mechanism for the challenges faced by burn survivors. Much like the “higher power” aspect of the Alcoholics Anonymous 12-step program, or the spiritual focus of activities such as meditation and yoga, it can possibly attenuate some of the overwhelming aspects of those challenges burn survivors face.
Some caveats require discussion. A limitation of this study is that the assessment of sleep is based on a single item, “Due to the burn injury, how satisfied are you with your sleep?” Use of a single item introduces some error related to precision of the metric. However, given the sample size, this error was reduced somewhat. Second, potential causes and type of sleep problems experienced could not be elucidated. Nevertheless, the results demonstrated a large percentage of the subjects had dissatisfaction with their sleep. Third, sleep dissatisfaction was self-reported. Nevertheless, sleep quality is inherently subjective, and the results indicate a consistent and important relationship between sleep problems and a range of patient-centered YABOQ outcomes. These results also strongly suggest that future work can focus on patient-centered quality of life related to sleep problems in a burn survivor population.
Sleep problems are prevalent in young adults after burn injury, and these sleep effects are associated with many aspects of quality of life important to recovery from burns and community reintegration. Sleep should be addressed in clinical visits in young adults after burns and interventions should be tested to optimize sleep quality in long-term burn survivors.
Acknowledgments
This work is partially funded by the Fraser Family Fund of the Massachusetts General Hospital and grants from the National Institute on Disability, Independent Living, and Rehabilitation Research (H133A130023 and H133A120034), NIDILRR grant number 90DP0055 and 90DP0035. NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this article do not necessarily represent the policy of NIDILRR, ACL, HHS, and the reader should not assume endorsement by the Federal Government.
APPENDIX
The Multi-Center Benchmarking Study coinvestigators are as follows: Gabriel Shapiro, PhD (Department of Epidemiology, Biostatistics and Occupational Health, McGill University, Montreal, QC, Canada); Michael Peck, MD (Arizona Burn Center, Phoenix, AZ); Michelle Hinson, RN, and Helena Bauk, RN (Shriners Hospitals for Children Boston, Boston, MA); Richard Kagan, MD, and Glenn Warden, MD (Shriners Hospitals for Children Cincinnati, Cincinnati, OH); David Herndon, MD, Patricia Blakeney, PhD, and Robert McCauley, MD (Shriners Hospitals for Children Galveston, Galveston, TX); Grace Chan, RN, Karen Lenkus, RN, and Kate Nelson-Mooney, RN (Shriners Hospitals for Children Northern California, Sacramento, CA); David Wood, MD, MPH (University of Florida, Jacksonville, FL); Charlotte Phillips, RN MPH (New York Hospital for Special Surgery, New York, NY); Catherine Calvert, PhD (North Carolina Jaycee Burn Center, Chapel Hill, NC); Sylvia Garma, PhD (University of California at Davis, Sacramento, CA); Cleon Goodwin, MD (Western States Burn Center at North Colorado Medical Center, Greeley, CO); Mary Kessler, RN (North Carolina Jaycee Burn Center, University of North Carolina, Chapel Hill, ND); Kim Reiss, RA (Johns Hopkins Medical Center, Baltimore, MD); and Karen Taylor, RN (University of Nebraska Medical Center, Omaha, NE).
REFERENCES
- 1.Chen X, Gelaye B, Williams MA. Sleep characteristics and health-related quality of life among a national sample of American young adults: assessment of possible health disparities. Qual Life Res 2014;23:613–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vgontzas AN, Zoumakis E, Bixler EO, et al. Adverse effects of modest sleep restriction on sleepiness, performance, and inflammatory cytokines. J Clin Endocrinol Metab 2004;89:2119–26. [DOI] [PubMed] [Google Scholar]
- 3.Heinzelmann M, Lee H, Rak H, et al. Sleep restoration is associated with reduced plasma C-reactive protein and depression symptoms in military personnel with sleep disturbance after deployment. Sleep Med 2014;15:1565–70. [DOI] [PubMed] [Google Scholar]
- 4.Chang SP, Chen YH. Relationships between sleep quality, physical fitness and body mass index in college freshmen J Sports Med Phys Fitness. 2015;55:1234–41. [PubMed] [Google Scholar]
- 5.Tavernier R, Willoughby T. Bidirectional associations between sleep (quality and duration) and psychosocial functioning across the university years. Dev Psychol 2014;50:674–82. [DOI] [PubMed] [Google Scholar]
- 6.Vgontzas AN, Papanicolaou DA, Bixler EO, et al. Circadian interleukin-6 secretion and quantity and depth of sleep. J Clin Endocrinol Metab 1999;84:2603–7. [DOI] [PubMed] [Google Scholar]
- 7.Dotson CH, Kibbee E, Eland JM. Perception of sleep following burn injury. J Burn Care Rehabil 1986;7:105–8. [DOI] [PubMed] [Google Scholar]
- 8.Gottschlich MM, Jenkins ME, Mayes T, et al. The 1994 Clinical Research Award. A prospective clinical study of the polysomnographic stages of sleep after burn injury. J Burn Care Rehabil 1994;15:486–92. [PubMed] [Google Scholar]
- 9.Boeve SA, Aaron LA, Martin-Herz SP, et al. Sleep disturbance after burn injury. J Burn Care Rehabil 2002;23:32–8. [DOI] [PubMed] [Google Scholar]
- 10.Lawrence JW, Fauerbach J, Eudell E, Ware L, Munster A. The 1998 Clinical Research Award. Sleep disturbance after burn injury: a frequent yet understudied complication. J Burn Care Rehabil 1998;19:480–6. [DOI] [PubMed] [Google Scholar]
- 11.Masoodi Z, Ahmad I, Khurram F, Haq A. Changes in sleep architecture after burn injury: ‘Waking up’ to this unaddressed aspect of postburn rehabilitation in the developing world. Can J Plast Surg 2013;21:234–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Robert R, Meyer WJ 3rd, Villarreal C, Blakeney PE, Desai M, Herndon D. An approach to the timely treatment of acute stress disorder. J Burn Care Rehabil 1999;20:250–8. [DOI] [PubMed] [Google Scholar]
- 13.Robert R, Blakeney PE, Villarreal C, Rosenberg L, Meyer WJ 3rd. Imipramine treatment in pediatric burn patients with symptoms of acute stress disorder: a pilot study. J Am Acad Child Adolesc Psychiatry 1999;38:873–82. [DOI] [PubMed] [Google Scholar]
- 14.Mayes T, Gottschlich MM, Khoury J, McCall J, Simakajornboon N, Kagan RJ. A pilot review of the long-term impact of burn injury on sleep architecture in children. J Burn Care Res 2013;34:e15–21. [DOI] [PubMed] [Google Scholar]
- 15.Gottschlich MM, Mayes T, Khoury J, Simakajornboon N, Kagan RJ. Comparison of sleep parameters obtained from actigraphy and polysomnography during the rehabilitative phase after burn. J Burn Care Res 2013;34:183–90. [DOI] [PubMed] [Google Scholar]
- 16.Ryan CM, Schneider JC, Kazis LE, et al. ; Multi-Center Benchmarking Study Group. Benchmarks for multidimensional recovery after burn injury in young adults: the development, validation, and testing of the American Burn Association/Shriners Hospitals for Children young adult burn outcome questionnaire. J Burn Care Res 2013;34:e121–42. [DOI] [PubMed] [Google Scholar]
- 17.Ryan CM, Lee A, Kazis LE, et al. ; Multicenter Burn Outcome Group. Recovery trajectories after burn injury in young adults: does burn size matter? J Burn Care Res 2015;36:118–29. [DOI] [PubMed] [Google Scholar]
- 18.Schneider JC, Holavanahalli R, Helm P, Goldstein R, Kowalske K. Contractures in burn injury: defining the problem. J Burn Care Res 2006;27:508–14. [DOI] [PubMed] [Google Scholar]
- 19.Sheridan RL, Ryan DP, Fuzaylov G, Nimkin K, Martyn JA. Case records of the Massachusetts General Hospital. Case 2-2008. Case 5-2008. An 18-month-old girl with an advanced neck contracture after a burn. N Engl J Med 2008;358:729–35. [DOI] [PubMed] [Google Scholar]
- 20.Gerber M, Brand S, Herrmann C, Colledge F, Holsboer-Trachsler E, Pühse U. Increased objectively assessed vigorous-intensity exercise is associated with reduced stress, increased mental health and good objective and subjective sleep in young adults. Physiol Behav 2014;135:17–24. [DOI] [PubMed] [Google Scholar]
- 21.Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med 2015;38:427–49. [DOI] [PubMed] [Google Scholar]
- 22.McBeth J, Wilkie R, Bedson J, Chew-Graham C, Lacey RJ. Sleep disturbance and chronic widespread pain. Curr Rheumatol Rep 2015;17:469. [DOI] [PubMed] [Google Scholar]
- 23.Raymond I, Nielsen TA, Lavigne G, Manzini C, Choinière M. Quality of sleep and its daily relationship to pain intensity in hospitalized adult burn patients. Pain 2001;92:381–8. [DOI] [PubMed] [Google Scholar]
- 24.Schneider JC, Harris NL, El Shami A, et al. A descriptive review of neuropathic-like pain after burn injury. J Burn Care Res 2006;27:524–8. [DOI] [PubMed] [Google Scholar]
- 25.Gauffin E1, Oster C, Gerdin B, Ekselius L. Prevalence and prediction of prolonged pruritus after severe burns. J Burn Care Res. 2015;36:405–13. [DOI] [PubMed] [Google Scholar]
- 26.Carrougher GJ, Martinez EM, McMullen KS, et al. Pruritus in adult burn survivors: postburn prevalence and risk factors associated with increased intensity. J Burn Care Res 2013;34:94–101. [DOI] [PubMed] [Google Scholar]
- 27.Portilla AS, Bravo GL, Miraval FK, et al. A feasibility study assessing cortical plasticity in chronic neuropathic pain following burn injury. J Burn Care Res 2013;34:e48–52. [DOI] [PubMed] [Google Scholar]
- 28.Hultman CS, Friedstat JS, Edkins RE, Cairns BA, Meyer AA. Laser resurfacing and remodeling of hypertrophic burn scars: the results of a large, prospective, before-after cohort study, with long-term follow-up. Ann Surg 2014;260:519–29; discussion 529-32. [DOI] [PubMed] [Google Scholar]
- 29.Banack HR, Holly CD, Lowensteyn I, et al. The association between sleep disturbance, depressive symptoms, and health-related quality of life among cardiac rehabilitation participants. J Cardiopulm Rehabil Prev 2014;34:188–94. [DOI] [PubMed] [Google Scholar]
- 30.Skapinakis P, Rai D, Anagnostopoulos F, Harrison S, Araya R, Lewis G. Sleep disturbances and depressive symptoms: an investigation of their longitudinal association in a representative sample of the UK general population. Psychol Med 2013;43:329–39. [DOI] [PubMed] [Google Scholar]
- 31.El hamaoui Y, Yaalaoui S, Chihabeddine K, Boukind E, Moussaoui D. Post-traumatic stress disorder in burned patients. Burns 2002;28:647–50. [DOI] [PubMed] [Google Scholar]
- 32.Fukunishi I. Relationship of cosmetic disfigurement to the severity of posttraumatic stress disorder in burn injury or digital amputation. Psychother Psychosom 1999;68:82–6. [DOI] [PubMed] [Google Scholar]
- 33.Lawrence JW, Fauerbach JA. Personality, coping, chronic stress, social support and PTSD symptoms among adult burn survivors: a path analysis. J Burn Care Rehabil 2003;24:63–72; discussion 62. [DOI] [PubMed] [Google Scholar]
- 34.Schneider JC, Trinh NH, Selleck E, et al. The long-term impact of physical and emotional trauma: the station nightclub fire. PLoS One 2012;7:e47339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moore M, Fagan S, Nejad S, et al. The role of a dedicated staff psychiatrist in modern burn centers. Ann Burns Fire Disasters 2013;26:213–6. [PMC free article] [PubMed] [Google Scholar]
- 36.Sundelin T, Lekander M, Kecklund G, Van Someren EJ, Olsson A, Axelsson J. Cues of fatigue: effects of sleep deprivation on facial appearance. Sleep 2013;36:1355–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Green B. Post-traumatic stress disorder: symptom profiles in men and women. Curr Med Res Opin 2003;19:200–4. [DOI] [PubMed] [Google Scholar]
- 38.Budweiser S, Luigart R, Jörres RA, et al. Long-term changes of sexual function in men with obstructive sleep apnea after initiation of continuous positive airway pressure. J Sex Med 2013;10:524–31. [DOI] [PubMed] [Google Scholar]
- 39.Gullick JG, Taggart SB, Johnston RA, Ko N. The trauma bubble: patient and family experience of serious burn injury. J Burn Care Res 2014;35:e413–27. [DOI] [PubMed] [Google Scholar]
- 40.Shekleton JA, Flynn-Evans EE, Miller B, et al. Neurobehavioral performance impairment in insomnia: relationships with self-reported sleep and daytime functioning. Sleep 2014;37:107–16. [DOI] [PMC free article] [PubMed] [Google Scholar]