Abstract
Introduction
Non-pharmacological pain management practices are very important for the successful treatment of pain. It has an impact on the patient’s quality of life and the family’s financial situation owing to missed workdays, direct medical expenses, and incapacity from pain.
Objective
Therefore, this study is intended to assess non-pharmacological pain management practice and associated factors among nurses working at comprehensive specialized hospitals in northwest, Ethiopia.
Methods
Institution-based cross-sectional study design was employed from May 30 to June 30, 2022. A stratified random sampling technique was used to select 322 study participants. A binary logistic regression model was used to identify factors associated with non-pharmacological pain management practice. Variables with a P-value less than .25 in the bi-variable analysis were entered into the multivariable logistic regression analysis and a P-value of less than .05 was considered as having a statistically significant association.
Results
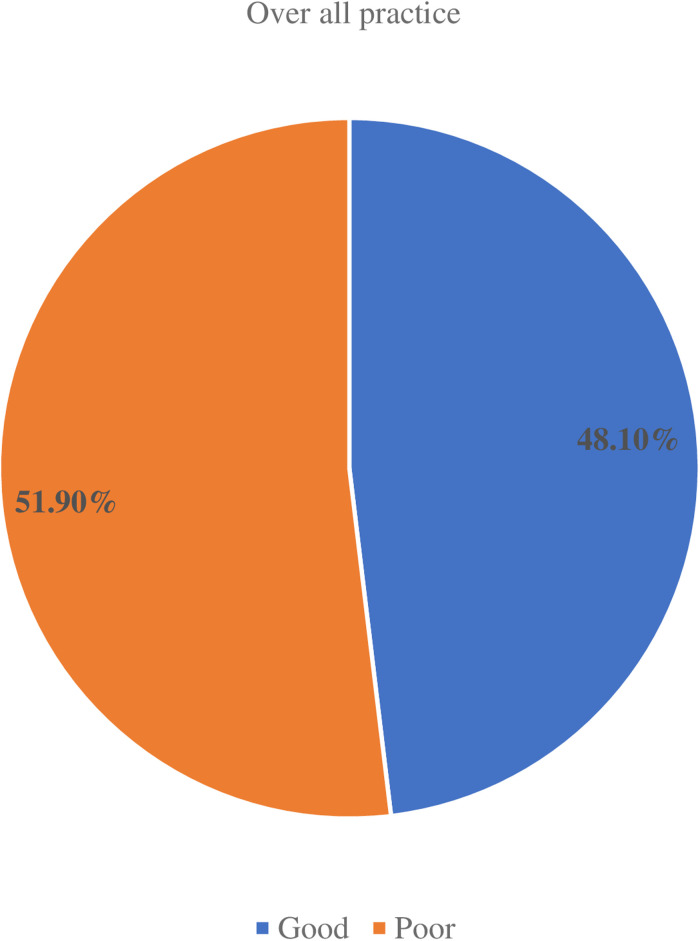
A total of 322 nurses participated, with a response rate of 98.8%. It was found that 48.1% (95% CI: 42.65, 53.62) of nurses had good practice in non-pharmacological pain management. Pain assessment tool availability (AOR = 1.68 [95% CI: 1.02, 2.75]) (P = .04), good pain assessment practice (AOR = 1.74 [95% CI: 1.03, 2.84]) (P = .03), favorable attitude (AOR = 1.71 [95% CI: 1.03, 2.95]) (P = .03), and age (26–35) (AOR = 4.46 [95% CI: 1.24, 16.18]) (P = .02) were factors significantly related to non-pharmacological pain management practice.
Conclusion
According to this work, the prevalence of non-pharmacological pain management practices was found to be low. Good pain assessment practices, availability of pain assessment tools, favorable attitude, and age (26–35) years were significant factors of non-pharmacological pain management practice. Hospitals are better give training on non-pharmacological pain management methods for nurses as they are important to treat pain holistically, increase patient satisfaction, and are cost-effective.
Keywords: nursing, pain management, practice, comprehensive specialized hospitals
Introduction
According to the International Association for the Study of Pain (IASP), pain is unpleasant sensory and emotional experiences associated with actual or potential tissue damage (Aydede, 2019). Pain is the most common health problem leading to seeking health care. About 4 out of 10 hospitalized adult patients suffer from pain. Pain management is a nursing activity comprising basic components of the nursing process; assessment, diagnosis, planning, intervention, and evaluation for patients in pain. The American Pain Society (APS) introduced the “pain as the 5th vital sign” concept in 1996 to lessen the burden of underassessing and treating pain (Araujo & Romero, 2015; Levy et al., 2018; Liyew et al., 2020). Various nursing tasks, including the application of efficient pain-relieving techniques, are involved in the treatment of pain. It has been indicated that pain management includes proper assessment and provision of relief for patients who suffer from pain (Association, 2011). Nurses are professionals who are closer to the patients than other professionals and devote most of their time to caring for patients. They play a crucial role and have the responsibility of assessing and managing patients’ pain (Awad & Hashem, 2019; Benimana, 2017).
Pain management involves pharmacological and non-pharmacological treatment approaches. Non-pharmacological pain management (NPPM) is an intervention without the use of medications (Conway, 2020). Non-pharmacological methods do not replace pharmacological treatments but are complementary to medication treatments. These strategies are worthwhile especially for managing mild to moderate pain (Mohamed Bayoumi et al., 2021). They are used along with medication for moderate to high-intensity pain control and alone for treatment of low-intensity pain. There are various NPPM practices that nurses can apply in nursing care. Physical methods such as massage, movement restriction/rest, repositioning, and cold and hot application have important pain-relieving effects (Demir, 2012). Cognitive behavioral and psychological therapies which include relaxations, patient education, breathing techniques, and attention distraction are important NPPM practices. Other NPPM practices include emotional support/reassurance, touching, and creating a comfortable environment (He et al., 2011; Kidanemariam et al., 2020).
Nurses can apply these methods easily with little resources (Funda Büyükyýlmaz, 2014; Gelinas et al., 2013).
NPPM practices are essential in that they promote comfort and patients can use to control their pain if they are provided appropriate information or education (Marie, 2013; Mohiuddin, 2019). Moreover, these methods have advantages over the conventional drug treatments that they treat cognitive, affective and socio-cultural aspects of pain. They increase feeling of control, diminish pain intensity, improve quality of life, lower required dosage of pain killers, and minimize cost (Demir, 2012; El Geziry et al., 2018).
Pain is a common health problem globally affecting many patients but often left undertreated (Tercan, 2017). More than 80% of surgical patients were affected by inadequately managed pain in the U.S. Evidence from the literature showed that unrelieved pain is associated with several detrimental consequences. It affects the quality of life, and economic status of the patient and families from work days lost, direct health costs, and disability due to pain (Mohiuddin, 2019). Among hospitalized patients, unrelieved pain lengthens the duration of recovery, and results in longer hospital stays leading to more cost and decreased patient satisfaction (Benimana, 2017; Swartzentruber, 2021). Due to this, incorporating NPPM practices into nursing care contributes to the effective management of patient’s pain (Nwaneri et al., 2018; Swartzentruber, 2021).
It has been identified that inadequate pain assessment, lack of knowledge, negative attitude, workload and absent/insufficient guidelines regarding NPPM (Seldon, 2017) are among several contributory factors to the low usage of NPPM practices that have been mentioned in the literature. Despite health professionals receiving training on pain assessment and management, patients are still suffering from poorly controlled pain. So, further training should be provided, along with training on nursing attitudes towards NPPM practice (Benimana, 2017). Educational program can improve knowledge and attitude of nurses regarding pain management (Germossa et al., 2018). In Ethiopia, despite the initiation of training on pain management and the development of national guidelines on the assessment and management of pain given high priority ever before, patients still suffer from undertreated pain. Nurses working at comprehensive specialized hospitals in Ethiopia, specifically in the study area did not take training regarding pain assessment, management and practice (Association, 2011; FMOH, 2014).
Review of Literature
Various studies had determined usage of different NPPM approaches for pain management in different countries. A study undertaken in Philippines to determine extent of nurses’ NPPM application for pain treatment showed that good number of nurses often use this practice (Antwi et al., 2019). Another study conducted in Turkey to examine knowledge and practice of nurses regarding NPPM practice had demonstrated that 62.4% of nurses apply NPPM practice (Tercan, 2017). In addition, a research was conducted in Iran to investigate extent of utilization in ICU nurses and found that 55.8% of nurses use NPPM practices. Another descriptive cross-sectional study undertaken in Nigeria and Cameroon to investigate nurses’ utilization of NPPM practice found that 65.2% and 56% of nurses use NPPM practice, respectively (Abimbola, 2021; Kimbi et al., 2016). Furthermore, descriptive exploratory study done in Egypt to determine critical nurses’ application of NPPM measures revealed that 67.3% of nurses’ practice was unsatisfactory (Khalil, 2018).
In Ethiopia, studies carried out at Tikur Anbessa and Debre Tabor hospitals and indicated that only 52.8% and 26% of nurses have good NPPM practice (Sisay, 2017; Zeleke et al., 2021).
Various studies carried out to examine practice of nurses on NPPM found that age, level of education and working experience were determinants of nurses’ NPPM practice (Ali et al., 2013; Mohamed et al., 2021; Seldon, 2017). Similarly, studies in Nigeria (Abimbola, 2021; Nwaneri et al., 2018), Egypt (Mohamed et al., 2021), Eritrea (Kidanemariam et al., 2020), and Ethiopia (Kerie et al., 2020; Sisay, 2017) demonstrated that increase in age, higher level of education and more working experience were associated with good practice on NPPM practices among nurses.
A research was conducted at Walden University and Turkey on nurses knowledge of NPPM practices and provision of holistic patient care for postoperative pain management. These studies demonstrated that nurses possess poor knowledge regarding NPPM practices which had led to low utilization of these practices in pain management (Arbuah, 2019; Şimşek & Gözen, 2021; Yaban, 2019). On the other hand, study in Makkah Al-Mukaramah had determined that nurses’ satisfactory knowledge on NPPM practices has contributed to satisfactory practice (Ali et al., 2013). Studies in Egypt (67.3%) (Mohamed et al., 2021) and Sudan (66%) (Elhusein et al., 2020) revealed that nurses had poor knowledge on NPPM practices. In Ethiopia, studies demonstrated that 52% of nurses had good knowledge regarding NPPM (Sisay, 2017).
A study in Philippines had proven that nurses’ good attitude towards NPPM and good pain assessment practice positively affects application of these practices (Antwi et al., 2019). Another research in Nigeria demonstrated that 65.7% of nurses’ attitude was positive towards these practices of pain treatment and has significant association with utilization of NPPM (Abimbola, 2021). Similarly, studies in Ethiopia had also indicated that attitude had significant difference on NPPM practice of nurses positively associated with good practice (Sisay, 2017; Zeleke et al., 2021).
Studies had proven that it is difficult to adequately alleviate pain without adequate assessment (Benimana, 2017). A study conducted in Egypt found that only 50.9% nurses had satisfactory pain assessment practice and most of them (56.4%) didn’t have education about pain assessment (Mohamed et al., 2022).
Multiple institutional-related factors invariably affect NPPM practice of nurses. Cross-sectional studies in Turkey (Gumus et al., 2020), Cameroon (Kimbi et al., 2016), Sudan (Elhusein et al., 2020), and Debre Tabor, Ethiopia (Zeleke et al., 2021) pointed out that in-service training was significant factor associated with NPPM practice. Lack of NPPM equipment's (e.g., special mattress, pillow) was also one of the significant factors with NPPM practice (Abimbola, 2021; Khalil, 2018; Nwaneri et al., 2018). Another cross-sectional study conducted in Eritrea showed that availability of pain measurement tools in the working unit had determined significant difference among nurses regarding their practice of NPPM (Kidanemariam et al., 2020). Studies had identified that workload was one of the reasons for low NPPM practice (Khalil, 2018; Kia et al., 2021; Kimbi et al., 2016).
A study in Ethiopia revealed that 70.3% of nurses said that patients’ preference to drugs was one of the reasons not to use NPPM practices for pain alleviation. But, absence of patients’ preference to drugs had positive effect on nurses’ NPPM practice (Sisay, 2017). It had also been identified that about 46.8% (Nwaneri et al., 2018) and 92.9% (Abimbola, 2021) nurses said patients’ severity of pain was one of the reasons in order not to apply NPPM practices. The aim of this study is intended to assess NPPM practice and associated factors among nurses working at comprehensive specialized hospitals in the northwest Ethiopia, 2022.
Conceptual Framework
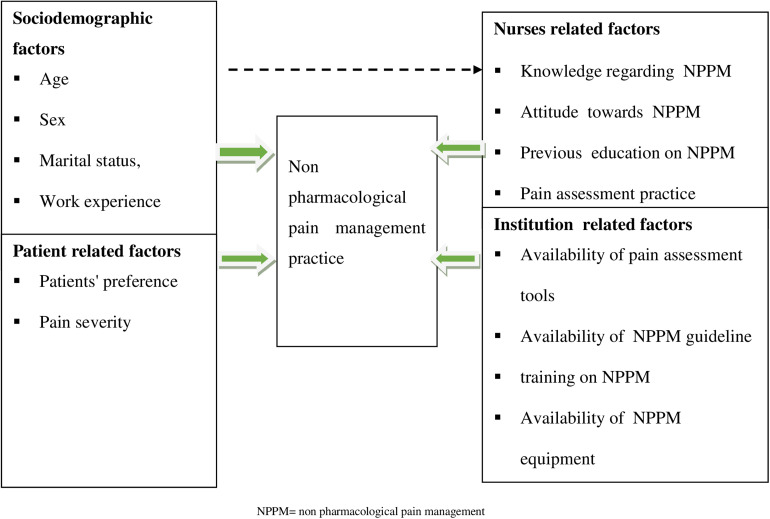
The nurse’s socio-demographic characteristics, institution-related factors, nurses-related factors, and patient-related factors directly affect NPPM practice (Abimbola, 2021; Ali et al., 2013; Antwi et al., 2019; Gumus et al., 2020; Kerie et al., 2020; Khalil, 2018; Kia et al., 2021; Sisay, 2017; Zeleke et al., 2021) (Figure 1).
Figure 1.
Schematic representation developed to show interactions between the dependent and the independent variables.
Methods
Study Design
Institution-based cross-sectional study design was employed.
Study Area and Period
The study was conducted in X, Y, and Z comprehensive specialty hospitals in northwest Ethiopia from May 30 to June 30, 2022. X Comprehensive Specialized Hospital is located in X Town, approximately 250 km from A, and 265 km from B, the capital city of the Amhara Regional State and Ethiopia, respectively. Two-hundred thirty-eight nurses were working in this hospital (Endawoke et al., 2021). Y and Z comprehensive specialty hospitals are located in A which is approximately 565 km away from Addis Ababa. These two university hospitals are public hospitals that provide care to more than five million residents in the catchment region. There were 430 and 310 nurses, respectively, in these hospitals (Belachew et al., 2021).
Population
The source populations were all nurses working at comprehensive specialty hospitals in the Northwest Ethiopia, and the study populations were all nurses working at the hospitals who were available during data collection period.
Eligibility Criteria
All nurses with more than 6 months of work experience at selected comprehensive specialty hospitals in Northwest Ethiopia were included. However, severely ill nurses and those on yearly or maternity leave at that time were excluded.
Variables of the Study
Dependent Variable
NPPM practice.
Independent Variables
Independent variables of the study were socio-demographic characteristics; age, sex, marital status, work experience, educational level, and working unit, institution-related factors; availability of pain assessment tools, availability of NPPM guidelines, availability of NPPM equipment, workload and in-service training on non-pharmacological methods, nurses-related factors; knowledge, attitude, nurses’ pain assessment practice and previous education on non-pharmacological methods and patient-related factors; patients’ preference and severity of pain.
Operational Definitions and Data Collection Tools and Procedures
Data were collected by using structured pretested self-administered questionnaires. The questionnaire has six parts. Part Ι: Socio-demographic variable questions developed by the researcher which include: age, sex, marital status, work experience, educational level, and working unit. Part ΙΙ: Knowledge-related questionnaire (NKASRP) assessing nurses’ knowledge regarding NPPM. It was adapted from previous studies after a literature review (Jira et al., 2020; Tekletsadik et al., 2021) and consists of 12 items of Yes or No type questions. Part ΙΙΙ: Attitude-related questionnaire (NKASRP) to assess nurses’ attitudes toward NPPM. It was adapted from previous studies after a literature review and consists of 12 items of Likert type ranging from 1 to 5 (Jira et al., 2020; Tekletsadik et al., 2021). Part ΙV: NPPM practice questionnaires. It was adapted from the validated tools after the literature review (Gumus et al., 2020; Khalil, 2018; Kia et al., 2021; Zeleke et al., 2021).
Part V: Pain assessment practice-related questionnaire, which was adopted from previous studies after the literature review and consists of 9 items with closed-ended Yes or No questions (Melile Mengesha et al., 2022). Part VI: contains questions to assess factors related to NPPM practice adapted after the literature review with closed-ended Yes or No questions (Ali et al., 2013; Mohamed Bayoumi et al., 2021; Nwaneri et al., 2018; Sisay, 2017).
Severe pain: is pain rating of 7 to 10 in the numerical pain rating scale; moderate pain is a pain rating of 4 to 6 in the numerical pain rating scale and mild pain is a pain rating of 1 to 3 in the numerical pain rating scale (Besufekad et al., 2021).
Workload: Participants who work >39 hours per week were considered as having a workload (Yazew et al., 2021).
Adequate knowledge: Study participants who scored points ≥65% out of prepared knowledge questions. Scoring system: correct answers were coded “1” and incorrectly coded “0.” Scores of each item were summed-up and the total was divided by the number of items (12 items) and changed to percentage. A score≥65% was considered adequate knowledge and ˂65% was considered inadequate knowledge (Mohamed et al., 2021).
Favorable attitude: Participants who scored points ≥60% out of the prepared attitude questions. Scoring system: for attitude items, scores were summed-up, and the total was divided by the possible maximum score (scores range from 12 to 60) and changed to percentage. A score ≥60% (i.e., 36 scores) was considered a favorable attitude and a score of ˂60% was considered an unfavorable attitude (Ali et al., 2013).
Good practice of NPPM: Participants who scored points ≥65% out of prepared NPPM practice questions. Scoring system: For practice items, scores are summed-up and total is divided by maximum (scores range from 13 to 52). Score ≥65% (i.e., 34 scores) was considered as good practice and score ˂65% considered as poor practice (Mohamed et al., 2021).
Good pain assessment practice: Participants who scored ≥70% to the questions assessing pain assessment practice. Scoring system: the correct answer was coded “1” and incorrect “0.” Scores of items were summed-up and the total score is divided by the number of items (9 items). Score ≥70% was considered good practice and ˂70% was considered poor practice (Melile Mengesha et al., 2022).
Sample Size Determination
The sample size was calculated for the first objective use a single population proportion formula, a 95% confidence interval, a 5% margin of error assumption, and a 26% P-value derived from other studies (Zeleke et al., 2021).
where n = desired sample size, p = 26% → 0.26, the proportion of nurses’ good practice in NPPM, d = 5%, margin of error, Z = 1.96 normal standard deviation for 95% confidence level
Then,
By adding 10% non-response rate, sample size was (296 * 0.1) + 296 = 326.
The sample size was also calculated for the second objective use double population formula using Epi 7 software for individual factors at 95% confidence level with 5% margin of error, 80% power, and 1:1 ratio of exposed to unexposed has been determined as follows (Table 1).
Table 1.
Determination of Sample Size by Associated Factors on Non-Pharmacological Pain Management Practice Among Nurses at Comprehensive Specialized Hospitals (N = 322).
| Variable | % Outcome among unexposed (p2) | % Outcome among exposed (p1) | AOR | Sample size | 10% non-response rate | Total | Reference |
|---|---|---|---|---|---|---|---|
| Workload | 22.1 | 50 | 2.61 | 114 | 12 | 126 | Zeleke et al. (2021) |
| Training on NPPM | 9.1 | 32 | 2.82 | 106 | 11 | 117 | Zeleke et al. (2021) |
| Knowledge | 7.6 | 42.2 | 7.27 | 58 | 6 | 64 | Zeleke et al. (2021) |
| Attitude | 5.5 | 73.3 | 2.68 | 20 | 2 | 22 | Zeleke et al. (2021) |
AOR = adjusted odd ratio, p1=exposed group, p2 unexposed group.
Therefore, the final sample size used for the study was the highest value n = 326 determined by the first objective.
Sampling Technique and Procedures
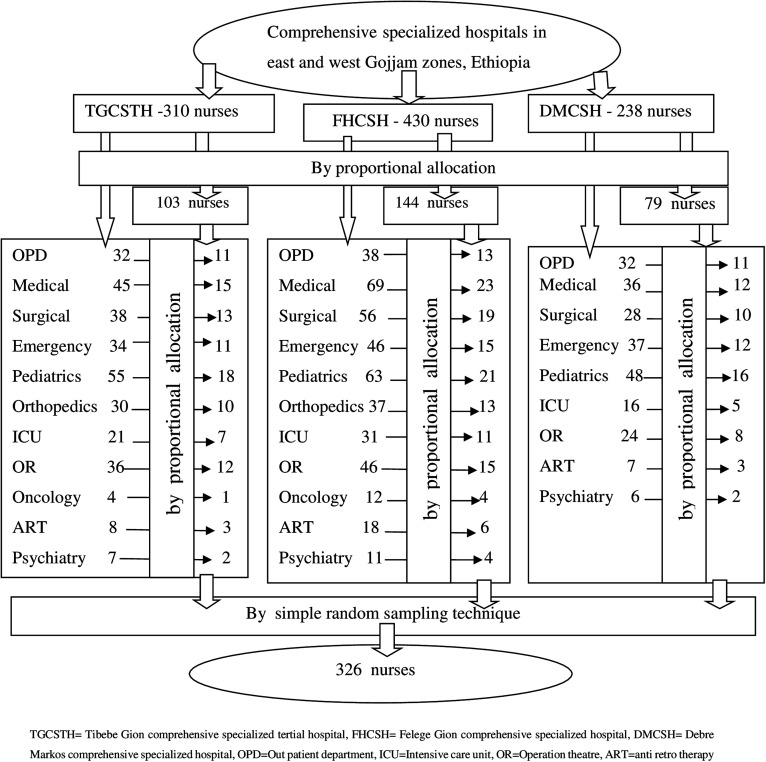
The study participants were chosen using a stratified random sampling technique. The human resource management office of the hospitals provided the total number of nurses from comprehensive specialty hospitals in the east and west Gojjam zones. The total sample size was proportionally distributed among the hospitals and nursing units. Finally, study participants were chosen from each unit using simple random sampling technique (Figure 2).
Figure 2.
Schematic presentation of sampling procedure on non-pharmacological pain management practice at comprehensive specialized hospitals in the east and west Gojjam zones, Ethiopia, 2022.
Data Quality Control
Before beginning the actual data collection, a pretest on 17 nurses (5% of the sample size) at Injibara General Hospital was conducted to ensure data quality. In previous studies, the tool was validated by a panel of experts. A reliability test was conducted, and the results showed that the knowledge, attitude, non-pharmacological pain treatment practice, and pain assessment practice items had corresponding Cronbach’s alpha values of 0.71, 0.70, 0.89, and 0.75, respectively. Supervisors and data collectors received training. Six nurses with bachelor degree and three supervisors with master’s degrees collected the data. The way that data were collected, the clarity of the questionnaire, the confidentiality of the information, the rights of the participants, and informed permission were all covered. Daily checks were made during data collection to ensure the accuracy. Data were collected using self-administered questionnaire and Epi Data was used for data entry to prevent data entry errors.
Data Processing and Analysis
The data were checked for completeness and consistency. Then it was coded and entered in EPI data version 3.02 Software. After that, data were exported to SPSS version 25 for analysis. Model fitness test (Goodness of fit was checked with Hosmer Lemeshow model of fit [P = .36] and assumption test for multicollinearity problem [VIF< 3.35] was done). Descriptive analysis using frequencies, proportions, and graphs was performed to describe the number and percentage of socio-demographic characteristics. The binary logistic regression analysis model was used to identify associated factors of NPPM practice. Variables with a P-value less than .25 in the bi-variable logistic regression were entered into the final multivariable logistic regression analysis to control possible confounding factors and to include more potential significant factors of NPPM practice. A P-value of less than .05 in multivariable regression analysis was considered statistically significant with NPPMP. The results were presented in text, tables, and graphs based on the types of data.
Ethical Considerations
Ethical clearance was obtained from X, the college of health sciences, ethical review committee. Then further permission letter was obtained from Amhara Public Health Institute’s research directorate and permission letters obtained from the institute's research directorate were distributed to X, Y, and Z hospitals. After obtaining permission from each hospital for preceding data collection, the purpose of the study, privacy issues, and participants’ right not to participate in the study or can withdraw from the study at any stage were explained to the study participants. Having obtained informed written consent from participants, data were collected and confidentiality was maintained with no name of the respondents written on the questionnaires.
Results
Distribution of Socio-Demographic Characteristics
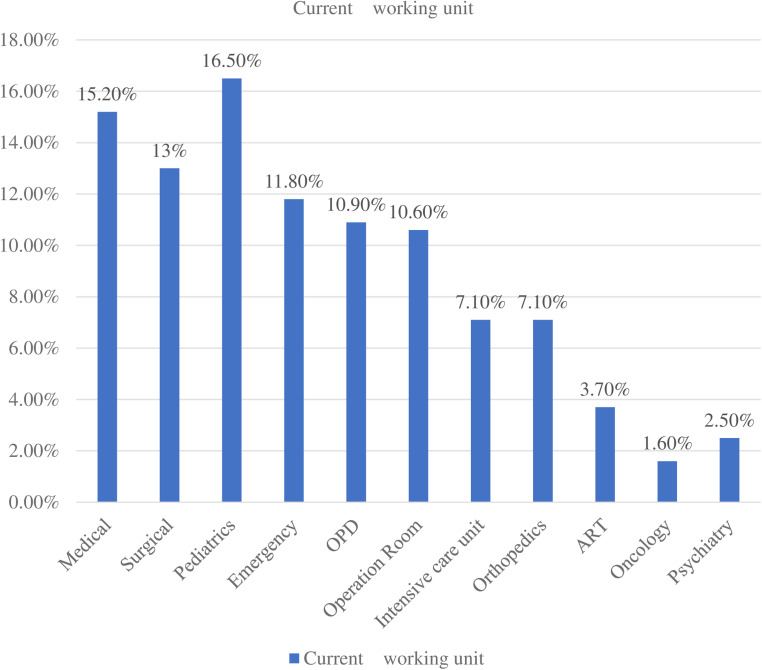
A total of 322 nurses participated in the study with a response rate of 98.8%. Of the total participants, 188 (55.9%) were male and 178 (55.3%) were married. Participants’ median age was 33 years with an interquartile range of 9 and the median work experience was 8 years with an interquartile range (IQR) of 6 (Table 2) (Figure 3).
Table 2.
Frequency Distribution of Nurses’ Socio-Demographic Characteristics at Comprehensive Specialized Hospitals (N = 322).
| Variables | Categories | Frequency | Percentage (100%) |
|---|---|---|---|
| Age | ≤25 | 13 | 4 |
| 26–35 | 175 | 54.3 | |
| 36–45 | 103 | 32 | |
| 46–55 | 31 | 9.6 | |
| Sex | Male | 188 | 55.9 |
| Female | 134 | 44.1 | |
| Marital status | Single | 142 | 44.1 |
| Married | 178 | 55.3 | |
| Divorced | 2 | 0.6 | |
| Level of education | Bachelor's degree | 278 | 86.3 |
| Diploma | 40 | 12.4 | |
| Masters | 4 | 1.2 | |
| Work experience | ≤9 | 202 | 62.7 |
| 10–19 | 94 | 29.2 | |
| 20–29 | 22 | 6.8 | |
| 30–39 | 4 | 1.2 |
Socio-demographic frequency distribution table.
Figure 3.
Current working unit of nurses’ socio-demographic characteristics at comprehensive specialized hospitals at oncology unit in the east and west Gojjam zones, Ethiopia, 2022 (N = 322).
Non-Pharmacological Pain Management Practices of Nurses
About 51.9% of nurses apply for position change routinely, 34.8% apply therapeutic communication often, and 43.8% of them use it to create a comfortable environment sometimes (Table 3).
Table 3.
Frequency Distribution of Nurses’ Non-Pharmacological Pain Management Practices at Comprehensive Specialized Hospitals (N = 322).
| Variables | Response | |||
|---|---|---|---|---|
| Never | Sometimes | Often | Routinely | |
| Frequency (%) | Frequency (%) | Frequency (%) | Frequency (%) | |
| Use cold application | 74 (23%) | 72 (22.4%) | 85 (26.4%) | 91 (28.3%) |
| Use hot application | 47 (14.6%) | 106 (32.9%) | 74 (23%) | 96 (29.8%) |
| Application of position changes | 48 (14.9%) | 76 (23.6%) | 31 (9.6%) | 167 (51.9%) |
| Apply breathing technique | 59 (18.3%) | 93 (28.9%) | 82 (25.5%) | 88 (27.3%) |
| Movement restriction/rest | 66 (20.5%) | 89 (27.6%) | 95 (29.5%) | 72 (22.4%) |
| Use therapeutic communication | 37 (11.5%) | 108 (33.5%) | 112 (34.8%) | 65 ( (20.2%) |
| Provide education to patient | 23 (7.1%) | 102 (31.7%) | 96 (29.8%) | 101 (31.4%) |
| Use comfort device | 114 (35.4%) | 107 (33.2%) | 39 (12.1%) | 62 (19.3%) |
| Create comfortable environment | 31 (9.6%) | 141 (43.8%) | 92 (28.6%) | 58 (18%) |
| Use relaxation | 82 (25.5%) | 132 (41%) | 88 (27.3%) | 20 (6.2%) |
| Use distraction | 96 (29.8%) | 131 (40.7%) | 75 (23.3%) | 20 (6.2%) |
| Apply massage | 170 (52.8%) | 115 (35.7%) | 34 (10.6%) | 3 (0.9%) |
| Use of therapeutic touch | 156 (48.4%) | 137 (42.5%) | 26 (8.1%) | 3 (0.9%) |
Frequency distribution table for nurses who practice non-pharmacological pain management.
Nurses-, Patients-, and Institutions-Related Factors
About 58.4%, 50.6%, 59%, and 32.9% of nurses had adequate knowledge, favorable attitude, good pain assessment practice, and received training on NPPM methods, respectively (Figure 4) (Table 4).
Figure 4.
Overall nursing practice of non-pharmacological pain management at comprehensive specialized hospitals in east and west Gojjam zones, Ethiopia, 2022 (N = 322).
Table 4.
Distribution of Factors on Non-Pharmacological Pain Management Practice of Nurses at Comprehensive Specialized Hospitals (N = 322).
| Variables | Response | Frequency | Percent (%) |
|---|---|---|---|
| Previous education on NPPM methods | Yes | 155 | 48.1 |
| No | 167 | 51.9 | |
| Availability of pain assessment tools in working unit | Yes | 192 | 59.6 |
| No | 130 | 40.4 | |
| Type of assessment tool available | Numeric scale | 83 | 25.8 |
| Verbal scale | 69 | 21.4 | |
| Face scale | 32 | 9.9 | |
| Othersa | 8 | 2.5 | |
| Availability of NPPM guidelines | Yes | 134 | 41.6 |
| No | 188 | 58.4 | |
| Availability of NPPM equipment | Yes | 191 | 59.3 |
| No | 131 | 40.7 | |
| Workload | Yes | 171 | 53.1 |
| No | 151 | 46.9 | |
| Pain severity | Yes | 220 | 68.3 |
| No | 102 | 31.7 | |
| Patient's preference | Yes | 217 | 67.4 |
| No | 105 | 32.6 |
Visual analog and FLACC scale.
Frequency distribution table for factors of non-pharmacological pain management practice.
Factors Associated with Non-Pharmacological Pain Management Practice
To identify factors associated with NPPM practice, binary logistic regression was done. In bivariate logistic regression analysis, age, educational level, training, nursing work load, attitude, pain assessment, patients’ preference, and availability of pain assessment tool had an association with NPPM practice. All variables that have an association with the outcome variables in bivariate logistic regression analyses were interred in the multivariate logistic regression analysis models by using backward likelihood ratio method. Then in multivariable logistic regression analysis factors that were significantly associated with NPPM practice were age (26–35), favorable attitude, good pain assessment practice and the presence of pain assessment tools.
The odds of NPPM practice is almost five times higher among nurses whose age were 26 to 35 than among nurses whose age were <25 years (AOR = 4.48 [95% CI: 1.24, 16.19]) (P = .04). Similarly the odds of NPPM practice is almost two times higher among nurses who had favorable attitude than among nurses who had not (AOR = 1.71 [95% CI: 1.03, 2.95]) (P = .03). Also nurses who had good pain assessment practice were practicing NPPM 1.74 times than who had not (AOR=1.74 [95% CI: 1.03, 2.84]) (P = .03). Finally nurses who had pain assessment tools in the working unit were practicing NPPM 1.68 times than nurses who had not (AOR = 1.68 [95% CI: 1.03, 2.76]) (P = .04) (Table 5).
Table 5.
Multivariable Logistic Regression Analysis of Factors Associated with Non-Pharmacological Pain Management Practice at Comprehensive Specialized Hospitals (N = 322).
| Variables | Poor practice (%) | Good practice (%) | COR (95% CI) | AOR (95% CI) | P-Value | |
|---|---|---|---|---|---|---|
| Age | ≤25 | 9 (5.4) | 4 (2.65) | 1 | 1 | |
| 26–35 | 75 (44.9) | 100 (64.5) | 3.00 (0.89,10.11) | 4.48 (1.24,16.19)* | .02 | |
| 36–45 | 63 (37.7) | 40 (25.8) | 1.43 (0.41,4.59) | 2.69 (0.71,10.28) | .14 | |
| 46–55 | 20 (12) | 11 (7.1) | 1.24 (0.31,4.96) | 2.65 (0.60,11.76) | .20 | |
| Attitude | Unfavorable | 97 (58.1) | 62 (40) | 1 | 1 | |
| Favorable | 70 (41.9) | 93 (60) | 2.08 (1.33,3.42)* | 1.71 (1.03,2.95)* | .03 | |
| Pain assessment | Poor | 83 (49.7) | 49 (31.6) | 1 | ||
| Good | 84 (50.3) | 106 (68.4) | 2.14 (1.36,3.37)* | 1.74 (1.03,2.84)* | .03 | |
| Available pain assessment tool | No | 80 (47.9) | 50 (32.3) | 1 | 1 | |
| Yes | 87 (67.7) | 105 (67.7) | 1.93 (1.23,3.04)* | 1.68 (1.03,2.76)* | .04 | |
*Statistically significant at P < .05, AOR = adjusted odd ratio, COR = crude odd ratio.
Logistic regression table.
Discussion
According to this study, 48.1% (95% CI: 42.65, 53.62) of nurses had a good practice on NPPM practice. This finding is in line with a study done in Addis Ababa (Sisay, 2017) in which 52.8% of nurses had good practice regarding NPPM. However, this study finding is incongruent with the study in Debre Tabor that only 26% of nurses had a good practice on NPPM (Zeleke et al., 2021). This discrepancy might be due to differences in sample size, training on NPPM methods, and scoring system used/operational definition.
However, the current study finding is higher than studies in Sudan (12%) (Elhusein et al., 2020), Turkey (29.1%) (Özveren1a et al., 2016), Egypt (26.7%) (Mohamed et al., 2022) and a study stated that most nurses did not use NPPM methods for pain management (Khalil, 2018). Possible reasons might be variations in the level of knowledge on NPPM methods, NPPM education, sampling technique, study design, and sample size difference. This means that when nurses are educated on NPPM practices, they become more knowledgeable which provides them confidence for practice. From the literature, it has been stated that evidence-based education on NPPM increases nurses’ knowledge and confidence, which helps nurses to apply these pain intervention methods in clinical practice (Arbuah, 2019). In these studies, convenient sampling was used and this non-probability sampling method might have affected the selection of participants, which in turn reduces accuracy.
On the other hand, this study result is lower than the studies in Nigeria (65.2%) (Abimbola, 2021), Iran (55.8%) (Kia et al., 2021), and Turkey (62.4%) (Tercan, 2017) of nurses used NPPM techniques for treatment of patients’ pain and the study (Gumus et al., 2020) that 92.6% of nurses used NPPM methods for pain management. The possible explanation might be variation in the level of knowledge on NPPM methods, training, sample size, level of education, and study setting. In these studies most of the study participants had received training and had a high level of education as compared to this study and training and a higher level of education are important in acquiring knowledge which is the foundation for practice. As well, in these studies, participants were from specific units (ICU, pediatrics, medical or surgical). From the literature, it has been stated that staying longer duration in specific clinical settings leads to more clinical exposure and more practice.
Nurses who had good pain assessment practice were nearly two times (AOR = 1.74 [95% CI: 1.03, 2.95]) (P = .03) more likely to practice NPPM than those who had poor practice on pain assessment. This implies that pain assessment has a positive effect on the NPPM practice of nurses. Pain assessment helps to determine the type of pain and effectiveness of pain management methods applied by reassessing after applying the methods and understanding the effectiveness of pain treatment methods helps to practice more. This finding is supported by the study (Antwi et al., 2019), which determined the statistically significant association between pain assessment practice and utilization of NPPM practices by nurses. This finding is also supported by studies done in Ethiopia (Ayenew et al., 2021; Melile Mengesha et al., 2022).
Nurses who reported that a pain assessment tool was available in their working unit were nearly two times (AOR = 1.68 [95% CI: 1.03, 2.76]) (P = .04) better to practice NPPM than those who said there was no pain measurement tool in their working unit. Pain assessment tools are necessary to measure pain before and after applying NPPM methods for patients in pain. Measuring pain helps to identify the type/level of pain which is important to plan appropriate and effective management methods. This may increase clinicians’ practice. This finding is supported by the study in Eritrea (Kidanemariam et al., 2020) that the availability of pain assessment tools showed statistically significant differences among nurses regarding NPPM utilization.
This study finding revealed that nurses with favorable attitudes were two times (AOR=1.71 [95% CI: 1.03, 2.84]) (P = .03) more likely to practice NPPM as compared to nurses whose attitude was unfavorable towards NPPM. This implies that nurses’ positive perceptions towards NPPM methods are the facilitator for good NPPM practice. This finding is congruent with the studies in Debre Tabor (Zeleke et al., 2021), Nigeria (Abimbola, 2021), and the Philippines (Antwi et al., 2019) that favorable attitude had a significantly positive association with good NPPM practice.
The last but not least, nurses aged 26 to 35 years were four times (AOR = [95% CI: 1.24,16.19]) (P = .04) more likely to practice NPPM than those whose age was 25 years and below. This finding is congruent with the study in west Gojjam (Kerie et al., 2020) and Egypt (Mohamed et al., 2022) that age had significant association with good NPPM practice of nurses (Figure 4).
Strength and Limitations
Cross-sectional study design makes it difficult to draw causal relationships between dependent and independent variables/factors. Research methodologies also involved self-reported measures that largely depend on individuals’ memory, and recall bias may exist. Nurses who were working in oncology unit are not included in the study.
Recommendations
Hospitals better give more emphasis on NPPM methods for nurses as they are important to treat pain holistically, increase patient satisfaction, and are cost-effective. The hospitals are also better to arrange training for nurses regarding NPPM practices, developing a decision algorithm or teaching which activities can reduce pain and avail pain assessment tool in each working units. It is better for nurses to emphasize and use NPPM methods in their nursing practice to reduce patients’ undesirable suffering from ineffectively treated pain and provide quality nursing care service since nurses have the responsibility to relieve patients’ pain. In addition, nurses better educate patients on NPPM methods to cope with and control their pain.
Implications for Practice
Considering the low practicability of NPPM, it is of great importance to provide in-service training, availing pain management tools, and decreasing work load of nurses to ensure the quality patient care. However, additional studies should be conducted to explore the long-term factor of the NPPM practice needed to improve quality nursing care.
Conclusion
According to the study, the overall NPPM practice of nurses in the study area was found to be poor. Good pain assessment practices, favorable attitude, the presence of pain assessment tools in the working unit, and age (26–35 years) were factors significantly associated with nurses’ NPPM practice. Hospitals are better give training on NPPM methods for nurses as they are important to treat pain holistically, increase patient satisfaction, and are cost-effective.
Abbreviations
- AOR
Adjusted Odds Ratio.
- ART
Anti-Retroviral Therapy.
- BSc
Bachelors Science.
- COR
Crude odds ratio.
- DMCSH
Debre Markos Comprehensive Specialized Hospital.
- FHCSH
Felegehiwot Comprehensive Specialized Hospital.
- ICU
Intensive Care Unit.
- NKASRP
Nurses’ Knowledge and Attitude Survey Regarding Pain.
- NPPM
Non-Pharmacological Pain Management.
- OPD
Outpatient Department.
- OR
Operation Room.
- TGCSTH
Tibebe Ghion Comprehensive Specialized and Teaching Hospital.
Footnotes
Author’s Contribution: All authors made a significant contribution to the work reported, whether to the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work. All authors read and approved the final draft of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Dejen Tsegaye https://orcid.org/0000-0002-3285-3855
Zemen Mengesha Yalew https://orcid.org/0000-0001-6341-5172
References
- Abimbola O. E. (2021). A survey of nurses knowledge and utilization of non-pharmacological methods of pain control at two selected hospitals in Ibadan, OYO State. International Journal of Medicine, Nursing & Health Sciences, 2(3), 5–19. https://doi.org/10.5281/zenodo.5029717 [Google Scholar]
- Ali H. S., Ibrahim Y., Mohamed E. (2013). Non-pharmacological pain management: Nurses’ knowledge, attitudes and practices in selected hospitals at Makkah El-Mukarramah. Life Science Journal, 2(10), 1327–1335. [Google Scholar]
- Antwi F. B., Osei S. A., Peprah W. K., Antwi E. (2019). Nurses’ attitude and pain assessment practices on non-pharmacologic pain management among patients with cephalalgia. Paper presented at the A paper presented at the 1st International Research Forum. On Fire: Excellence in Research, Adventist University of the Philippines, Putting Kahoy, Silang, Cavite, and April.
- Araujo L. C. d., Romero B. (2015). Pain: evaluation of the fifth vital sign. A theoretical reflection. Revista Dor, 16, 291–296. [Google Scholar]
- Arbuah N. (2019). Nonpharmacological techniques and pain management. Walden University. [Google Scholar]
- Association, Ethiopian Public Health. (2011). Baseline evaluation of pain management practices and teaching in health facilities and health training schools in Ethiopia: EPHA Addis Ababa.
- Awad W. H. A., Hashem E. S. (2019). In-service training program regarding nurses’ performance for non-pharmacological pain management among orthopedic patients. [Google Scholar]
- Aydede M. (2019). Does the IASP definition of pain need updating? Pain reports, 4(5). 10.1097/PR9.0000000000000777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayenew T., Melaku B., Gedfew M., Amha H., Bishaw K. A. (2021). Nurses’ knowledge, practice, and associated factors of pain assessment in critically ill adult patients at public hospitals, Addis Ababa, Ethiopia. International Journal of Africa Nursing Sciences, 15, 100361. 10.1016/j.ijans.2021.100361 [DOI] [Google Scholar]
- Belachew E. A., Tadess S., Alemayehu M. (2021). Health related quality of life and its associated factors among adults living with asthma attending at selected public hospitals in North-Western, Ethiopia: A multi-centered cross-sectional study. [Google Scholar]
- Benimana O. (2017). Knowledge, attitudes, practices and challenges faced by nurses in pain management among surgical patients, in one Referral Hospital in Rwanda. University of Rwanda. [DOI] [PubMed]
- Besufekad A., Admasu W., Fentie F., Mahmud S., Setot M., Shitemaw T. (2021). Assessment of pain severity and associated factors of post operative pain among adult patients in public hospitals of Addis Ababa, Ethiopia, 2021. [Google Scholar]
- Conway T. (2020). Noninvasive non-drug pain management: An alternative for treatment. https://minds.wisconsin.edu/bitstream/handle/1793/80821/Conway,%20Tajuan.pdf?sequence=1
- Demir Y. (2012). Non-pharmacological therapies in pain management. In Racz G. (Ed.), Current issues and opinions. InTech, ISBN: 978-953-307-813-7. http://www.intechopen.com/books/pain-management-current-issues-and-opinions/non-pharmacologicaltherapies-in-pain-management [Google Scholar]
- El Geziry A., Toble Y., Al Kadhi F., Pervaiz M., Al Nobani M. (2018). Non-pharmacological pain management. Pain Management in Special Circumstances, 1–14. [Google Scholar]
- Elhusein A., Mohamed H., Mariod A. A., Fadlalmola H., AbdElazim A. (2020). The nurses’ performance regarding non pharmacological pain management. Pak-Euro Journal of Medical and Life Sciences, 3(4), 176–186. [Google Scholar]
- Endawoke M., Alem G., Mulugeta H., Atinafu B. T., Nigussie F., Simachew A., Abiye M. (2021). Patients satisfaction and associated factors towards physiotherapy services in north west Ethiopia. Patient Preference and Adherence, 15, 2783. 10.2147/PPA.S337443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- FMOH. (2014). Standard treatment guidelines. http://www.fmhaca.gov.et/wp-content/uploads/2019/03/STG-General-Hospital.pdf
- Funda Büyükyýlmaz B. S. N. (2014). Non-pharmacological intervention in orthopedic pain: A systematic review. International Journal of Caring Sciences, 7(3), 718. [Google Scholar]
- Gelinas C., Arbour C., Michaud C., Robar L., Côté J. (2013). Patients and ICU nurses’ perspectives of non–pharmacological interventions for pain management. Nursing in Critical Care, 18(6), 307–318. 10.1111/j.1478-5153.2012.00531.x [DOI] [PubMed] [Google Scholar]
- Germossa G. N., Sjetne I. S., Hellesø R. (2018). The impact of an in-service educational program on nurses’ knowledge and attitudes regarding pain management in an Ethiopian university hospital. Frontiers in Public Health, 6, 229. 10.3389/fpubh.2018.00229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gumus K., Musuroglu S., Ozlu Z. K., Tasci O. (2020). Determining the use of nonpharmacologic methods by surgical nurses for postoperative pain management and the influencing professional factors: A multicenter study. Journal of PeriAnesthesia Nursing, 35(1), 75–79. 10.1016/j.jopan.2019.04.011 [DOI] [PubMed] [Google Scholar]
- He H., Lee T., Jahja R., Sinnappan R., Vehviläinen–Julkunen K., Pölkki T., Ang E. N. K. (2011). The use of nonpharmacological methods for children’s postoperative pain relief: Singapore nurses’ perspectives. Journal for Specialists in Pediatric Nursing, 16(1), 27–38. 10.1111/j.1744-6155.2010.00268.x [DOI] [PubMed] [Google Scholar]
- Jira L., Weyessa N., Mulatu S., Alemayehu A. (2020). Knowledge and attitude towards non-pharmacological pain management and associated factors among nurses working in Benishangul Gumuz regional state hospitals in Western Ethiopia, 2018. Journal of Pain Research, 13, 2917. 10.2147/JPR.S265544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerie S., Workineh Y., Menberu M. (2020). Nursing practice on non pharmacological pain management in Ethiopia, 2017. Journal of Community Medicine and Helth Education, 10(6), 5. [Google Scholar]
- Khalil N. S. (2018). Critical care nurses’ use of non-pharmacological pain management methods in Egypt. Applied Nursing Research, 44, 33–38. 10.1016/j.apnr.2018.09.001 [DOI] [PubMed] [Google Scholar]
- Kia Z., Allahbakhshian M., Ilkhani M., Nasiri M., Allahbakhshian A. (2021). Nurses’ use of non-pharmacological pain management methods in intensive care units: A descriptive cross-sectional study. Complementary Therapies in Medicine, 58, 102705. 10.1016/j.ctim.2021.102705 [DOI] [PubMed] [Google Scholar]
- Kidanemariam B. Y., Elsholz T., Simel L. L., Tesfamariam E. H., Andemeskel Y. M. (2020). Utilization of non-pharmacological methods and the perceived barriers for adult postoperative pain management by the nurses at selected national hospitals in Asmara, Eritrea. BMC Nursing, 19(1), 1–10. 10.1186/s12912-020-00492-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbi R. B., Ajong N. V., Tufon E. N. (2016). Non-pharmacological interventions for pain management used by Nurses at the Mezam Polyclinic Bamenda, Cameroon. Age, 21(9), 70.70. [Google Scholar]
- Levy N., Sturgess J., Mills P. (2018). “Pain as the fifth vital sign” and dependence on the “numerical pain scale” is being abandoned in the US: Why? British Journal of Anaesthesia, 120(3), 435–438. 10.1016/j.bja.2017.11.098 [DOI] [PubMed] [Google Scholar]
- Liyew B., Dejen Tilahun A., Habtie Bayu N. (2020). Knowledge and attitude towards pain management among nurses working at University of Gondar comprehensive specialized hospital, Northwest Ethiopia. Pain Research and Management, 2020. 10.1155/2020/6036575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marie B. S. (2013). Pain management in patients receiving palliative care. Oncology Nurse Advisor, 2013, e1. [PMC free article] [PubMed] [Google Scholar]
- Melile Mengesha B., Moga Lencha F., Ena Digesa L. (2022). Pain assessment practice and associated factors among nurses working at adult care units in public hospitals in Wolaita Zone, Southern Ethiopia, 2021. BMC nursing, 21(1), 1–7. 10.1186/s12912-022-00892-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamed Bayoumi M. M., Khonji L. M. A., Gabr W. F. M. (2021). Are nurses utilizing the non-pharmacological pain management techniques in surgical wards? PLoS ONE, 16(10), e0258668. 10.1371/journal.pone.0258668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamed R. M., Taha N. M., Moghazy N. A. E. K. (2021). Nursing performance regarding non-pharmacological pain management for patients with the cardiothoracic surgery at Zagazig University Hospitals. Annals of the Romanian Society for Cell Biology, 16952–16970. [Google Scholar]
- Mohamed R. M., Taha N. M., Moghazy N. A. E. K. (2022). Nursing practices regarding non-pharmacological pain management for patients with the cardiothoracic surgery at Zagazig University Hospitals. Zagazig Nursing Journal, 18(1), 16–28. [Google Scholar]
- Mohiuddin A. K. (2019). Non-drug pain management: Opportunities to explore. Lap Lambert Academic Publishing. [Google Scholar]
- Nwaneri A., Ndubuisi I., Anarodo A., Okoronkwo I., Offor E. (2018). Nurses’ knowledge and level of utilisation of non–pharmacological pain control for othorpaedic patients in Enugu Nigeria. International Journal of Nursing Science, 8(4), 61–66. [Google Scholar]
- Özveren1a H., Faydali S., Özdemir S. (2016). The knowledge and practices of nurses about pain management with non-pharmacological methods. Clinical Laboratory, 7(4), 99–105. [Google Scholar]
- Seldon L. A. (2017). Non-pharmacological methods in relieving children’s pain in hospital: A pilot study. https://ir.canterbury.ac.nz/handle/10092/13550
- Şimşek A., Gözen D. (2021). A study on pediatric nurses’ pain management knowledge and practices in Turkey. Trends in Pediatrics, 2(4), 159–164. [Google Scholar]
- Sisay S. (2017). Assessments of nurses knowledge, attitude and practice regarding non-pharmacological pain management and associated factors at Tikur Anbessa Hospital, in Addis Ababa, Ethiopia, 2017. Addis Ababa University.
- Swartzentruber M. (2021). The importance of providing multimodal analgesia: A literature review of nonpharmacologic pain treatments.
- Tekletsadik E. A., Desta A. A., Workneh B. S. (2021). Knowledge, attitude, and associated factors towards nonpharmacological pain management among nurses working at Amhara Region Comprehensive Specialized Hospitals, Ethiopia, 2021. Critical Care Research and Practice. 10.1155/2021/7374915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tercan B. (2017). Knowledge and practice situations of nurses on nonpharmacological methods and in pain management. New Trends and Issues Proceedings on Advances in Pure and Applied Sciences, 8, 98–105. [Google Scholar]
- Yaban Z. S. (2019). Usage of non-pharmacologic methods on postoperative pain management by nurses: Sample of Turkey. International Journal of Caring Sciences, 12(1), 529–541. [Google Scholar]
- Yazew K. G., Gebrie M. H., Aynalem Z. B. (2021). Nurses’ communication skills and determinant factors in Amhara region referral hospitals, northwest Ethiopia, 2019. International Journal of Africa Nursing Sciences, 14, 100310. 10.1016/j.ijans.2021.100310 [DOI] [Google Scholar]
- Zeleke S., Kassaw A., Eshetie Y. (2021). Non-pharmacological pain management practice and barriers among nurses working in Debre Tabor Comprehensive Specialized Hospital, Ethiopia. PLoS ONE, 16(6), e0253086. 10.1371/journal.pone.0253086 [DOI] [PMC free article] [PubMed] [Google Scholar]