Abstract
While functional reconstruction of massive irreparable rotator cuff tears remains a challenge, current techniques aimed at recentering and preventing superior migration of the humeral head allow for clinical and biomechanical improvements in shoulder pain and function.
Recentering of the glenohumeral joint reduces the moment arm and helps the deltoid to recruit more fibers, which compensates for insufficient rotator cuff function and reduces joint pressure.
In the past, the concept of a superior capsular reconstruction with a patch secured by suture anchors has been used.
However, several innovative arthroscopic treatment options have also been developed.
The purpose of this article is to present an overview of new strategies and surgical techniques and if existing present initial clinical results.
Techniques that will be covered include rerouting the long head of the biceps tendon, utilization of the biceps tendon as an autograft to reconstruct the superior capsule, utilization of a semitendinosus tendon allograft to reconstruct the superior capsule, superior capsular reconstruction with dermal allografts, and subacromial spacers.
Keywords: massive irreparable rotator cuff tear, superior capsular reconstruction, margin convergence, orthobiologics, LHBT, BAR, SCR, InSpace balloon
Introduction
The prevalence of rotator cuff tears (RCT) in the literature is reported to be between 22.1% (1) and 34% (2), with one-third of the reported RCTs being symptomatic and approximately one-fourth of these RCTs being massive irreparable rotator cuff tears (MIRCTs) (1). There are numerous clinical presentations of MIRCTs, ranging from pain or decreased range of motion to debilitating pseudoparalysis. First-line therapy for MIRCTs can be either non-operative or operative and is dependent on age, rupture morphology, and patient expectations. Regardless, if non-operative treatment fails, surgical treatment should be considered.
Treatment of MIRCTs remains a challenging dilemma for surgeons. The intricate interaction between an aging population with associated sarcopenia and inferior tissue quality (3) in combination with increasing shoulder functional demands further complicates surgical management. Reverse total shoulder arthroplasty (RTSA) has traditionally been used in cases of MIRCTs, particularly in older patients (1, 2). The number of implanted RTSA has increased over the past years and continues to increase in the future. The number of primary shoulder replacements is set to increase significantly by 2040, reaching at least 37,000 procedures per year. Additionally, the age range of patients receiving RTSAs has expanded to include younger patients (4).
Despite the trend of rapidly increasing numbers of implanted RTSAs, alternative therapeutic options for MIRCTs have become available, as illustrated in the literature (5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17). The general concept of preventing the superior migration of the humeral head is to reduce the painful contact between the humeral head and the acromion and enable the remaining rotator cuff (RC) muscles and the deltoid muscle to be recruited for improved active range of motion. These techniques also seek to minimize glenohumeral joint pressures to reduce the risk of developing cuff arthropathy, reduce pain, and restore function.
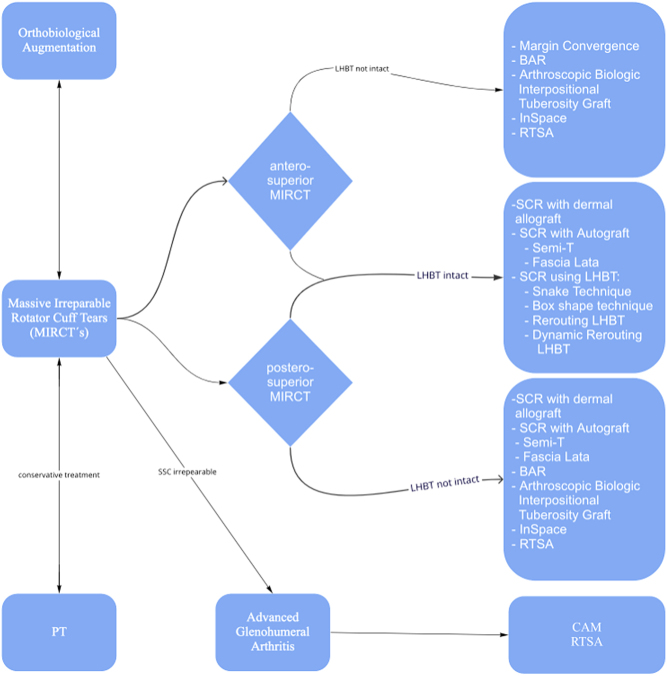
Recently, various autografts/allograft and surgical fixation techniques have been proposed including superior capsule reconstruction (SCR) with a dermal allograft (18), rerouting the long head of the biceps tendon (LHBT), utilization of the biceps as an autograft or the semitendinosus as a tendon allograft, and various subacromial spacers (Fig. 2). Clinically, SCR shows comparable results to RTSA (19) and may be preferable for certain patients. Recently, a consensus was reached on treatment for MIRCTs by the Neer Circle of the American Shoulder and Elbow Surgeons (Fig. 1) (24).
Figure 2.
Possible treatment options for massive irreparable rotator cuff tears. This flowchart gives an overview of novel arthroscopic as well as established techniques.
Figure 1.
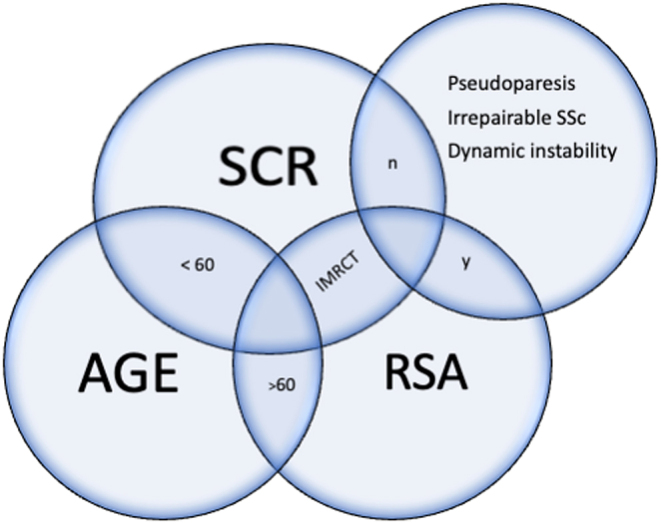
Neer Circle Consensus Paper on the treatment algorithm for MIRCTs: Displayed are the conditions in the patients where consensus was reached on treatment for MIRCTs (24). Starting with the patient’s age (bottom left bubble) and adding clinical findings (top right bubble), recommendations for treatment can be seen in this chart.
The purpose of this review is to present an overview of innovative surgical techniques for restoring native joint function in MIRCTs and to present available clinical results. A comprehensive search was performed using the PubMed (2019–2021) database. Keywords were as follows: massive rotator cuff tear; massive irreparable rotator cuff tear, superior capsular reconstruction. The queries were performed in October 2021. Inclusion criteria were techniques that provide a treatment option for MIRCTs. Articles involving RTSA, hemiarthroplasty, or muscle/tendon transfers were excluded.
Definition of tear size
If non-surgical treatment fails, preoperative MRI is necessary to assess tear size, degree of retraction, muscle atrophy, and fatty infiltration. Several classification systems with variable criteria for massive RCTs have been proposed. The Patte classification defines a massive RCT as retraction of tendons to the glenoid rim (20), Gerber et al. state that two tendons must be completely torn (6), Davidson and Burkhart define type 3 tears as a tear of at least 2 2 cm in the coronal and sagittal dimension (21), and lastly, DeOrio and Cofield define an anterior-posterior or medial-lateral dimension over 5 cm as massive (22). More recently, a Neer Circle Consensus statement determined that a massive RCT should be defined as the retraction of tendon(s) to the glenoid rim in either the coronal or axial plane and/or a tear with 67% of the greater tuberosity exposed measured in the sagittal plane (23). The measurement can be performed either with MRI or intraoperatively (24, 25, 26).
Indicators of irreparability of RCTs
Preoperative risk factors for irreparability help to anticipate the intraoperative risk of facing irreparable tears. Predictors of irreparability reported in the literature include the following:
Tear size and age (25).
Fatty degeneration: over 50% fatty infiltraion of the muscle belly (Goutailler grade 4) (27).
Muscle atrophy: Tangent sign in sagittal MRI (28) showing less supraspinatus muscle in the supraspinatus fossa.
Ultrasound assesment of tear size/MRI: anterosuperior (SSC + supraspinatus) or posterosuperior (infraspinatus + supraspinatus) massive tear > 5 cm (25, 29).
X-ray/CT scan: Moloney’s line: harmony arch of shoulder and glenoid, acromiohumeral distance distance less than < 6 mm (30).
Superior capsular reconstruction
The superior capsule is a thin structure from the labrum to the humeral head at the greater tuberosity that covers the footprint of the supraspinatus tendon and serves as a static stabilizer for the glenohumeral joint (31, 32, 33).
Mihata et al. studied the biomechanical properties of glenohumeral joints with irreparable supraspinatus tears. Compared to native joints, shoulders with large tears demonstrated superior humeral head translation, increased subacromial contact pressure, and decreased glenohumeral compression force (32, 34, 35). As a surgical solution, they invented the superior capsular reconstruction (SCR) using a facia lata autograft (32, 34, 35). The autograft is fixed onto the superior part of the scapular neck and the greater tuberosity of the humeral head, preventing the cranial migration of the humeral head (32, 34, 35, 36, 37).
The principle of the SCR is to restore superior capsular stability, which maintains the humeral head in its relocated, native position. This, in turn, allows the deltoid and remaining RC muscles to compensate for the deficient RC function and prevents painful bony contact between the humeral head and the acromion. Mihata et al. presented excellent clinical results in both the short-and mid-term follow-up periods. Preoperative compared to postoperative values showed American Shoulder and Elbow Surgeons score improvement from 29 to 83 and 92 at preop, 1-year, and 5-year time points, respectively. Forward elevation also improved from 85° preoperatively to 138° at 1-year and 151° at 5-year follow-up. Improvements in acromiohumeral distance (preoperative: 3.4 mm, 1-year follow-up: 9.1 mm, 5-year follow-up: 8.1 mm) and a decreased visual analog scale (preop: 6.9, 1-year follow-up: 1.3, 5-year follow-up: 0.9) were also seen (37).
Allogenic dermal allografts have been developed as an alternative to the fascia lata autograft, shortening procedure time and reducing donor site morbidity. These allografts have been shown biomechanically to restore the humeral head position after a posterosuperior RCT (38). Clinical 2-year results of 22 patients demonstrated significantly improved clinical scores (39). Postoperative MRI evaluations have shown 100% graft integrity at the tuberosity side, 76% at the midsubstance, and 81% on the glenoid side (39, 40). Table 1 summarizes the clinical and radiographic results of various study groups. Second-look case reports (41, 42) and animal rabbit models (43) have reported histological cell infiltration in the grafts. In these studies, retrieved graft tissue demonstrated a tendon-like structure, neovascularization, and various cell expressions (41, 42, 43).
Table 1.
Clinical and radiographic outcomes of superior capsular reconstruction.
| Year | Reference | Patients, n | Implant | Average follow-up (months) | Pre- to post-op clinical outcomes | Intact graft rate | Failure rate | |
|---|---|---|---|---|---|---|---|---|
| ASES | VAS | |||||||
| 2013 | Mihata et al.(64) | 23 | Fascia lata autograft | 34.1 | 23.5 → 92.9 | 83.3% | 4.3% | |
| 2017 | Denard et al.(65) | 59 | Dermal allograft† | 17.7 | 43.6 → 77.5 | 5.8 → 1.7 | 45% | 18.6% |
| 2017 | Hirahara et al.(66) | 8 | Dermal allograft† | 32.4 | 43.5 → 86.5 | 6.3 → 0.4 | 21.5% | |
| 2018 | Lee & Min (67) | 32 | Fascia lata autograft or allograft‡ | 24.8 | 50.3 → 84 | 5.8 → 1.34 | 63.9% | 36.1% |
| 2018 | Lim et al. (68) | 31 | Fascia lata allograft | 12.8 | 54.4 → 73.7 | 6 → 2.5 | 71% | 29% |
| 2018 | Mihata et al.(69) | |||||||
| No pseudoparalysis | 45 | Fascia lata allograft | 60 | 43.6 → 96.5 | 98% | 2% | ||
| Moderate pseudoparalysis | 28 | 29.2 → 92.2 | 96% | 4% | ||||
| Severe pseudoparalysis | 15 | 20.3 → 91.8 | 87% | 13% | ||||
| 2018 | Pennington et al. (70) | 86 | Dermal allograft† | Minimum 12 | 52.2 → 81.6 | 4.0 → 1.5 | 4.5% | |
| 2019 | Burkhart & Hartzler (71) | 10 | Dermal allograft† | 12.9 | 52 → 89 | 4.6 → 0.5 | ||
| 2019 | Burkhart et al. (40) | 41 | Dermal allograft† | 34 | 52 → 90 | 4.6 → 0.7 | 85% | 5% |
| 2020 | Lacheta et al. (39) | 22 | Dermal allograft† | 25.2 | 54.0 → 83.9 | 4 → 0 | Tuberosity: 100% Midsubstance: 76% Glenoid: 81% |
3.7% |
| 2021 | Okamura et al. (72) | Teflon§ | 42 | 13% | ||||
| 1 teflon layer | 15 | 42.4 → 63.2 | ||||||
| 3 teflon layers | 20 | 40.3 → 71.4 | 0% | |||||
†Arthroflex, Arthrex, Naples, FL, USA; ‡MegaDerm® allodermis, L&C BIO, Seoul, Korea; §Bard PTFE Felt, C.R. Bard, Inc., Murray Hill, NJ, USA.
ASES, American Shoulder and Elbow Surgeons score; VAS, visual analog score.
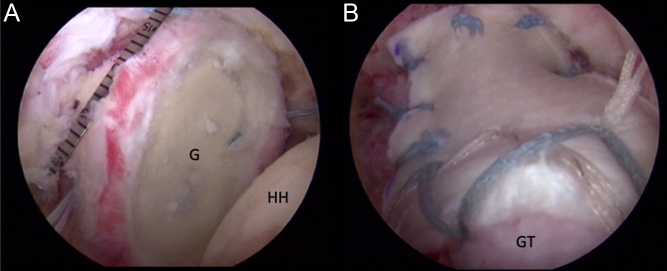
For the SCR technique (19, 31, 39), the shoulder is positioned in 30° to 40° of glenohumeral abduction. An arthroscopic measuring device is used to define the defect size in the anterior-posterior/medial-lateral directions (Fig. 4A). The 3-mm thick human cellular dermal allograft (Arthroflex, Arthrex, Naples, FL, USA) is sized and cut to include an additional 5–10 mm medially to allow for anchor placement and approximately 15 mm laterally to cover the anatomic footprint of the RC. Next, all four corners are armed with lasso loops ex vivo. The graft is then shuttled into the joint and fixed at the glenoid side and on the tuberosity side with a double-row reconstruction. Lastly, the graft is fixed with side-to-side sutures to the subscapularis and infraspinatus muscles, leaving the medial rotator interval open (Fig. 4B) (19, 44). The disadvantages of the SCR technique are the lack of restoration of active function of the supraspinatus muscle and relatively high costs (dermal allograft and multiple anchors). However, the procedure still serves as an effective surgical option to stave off the need for RTSA in patients that are young and/or do not wish to undergo shoulder arthroplasty.
Figure 4.
(A) Arthroscopic view of a right shoulder from the posterolateral portal demonstrating a massive irreparable tear of the supraspinatus and infraspinatus prior to capsular reconstruction. (B) Arthroscopic view of the right shoulder showing the completed capsular reconstruction with medial fixation to the superior glenoid and lateral fixation to the greater tuberosity (GT).
Alternative arthroscopic techniques for superior humeral head stabilization
Long head of the biceps tendon to reconstruct the superior capsule
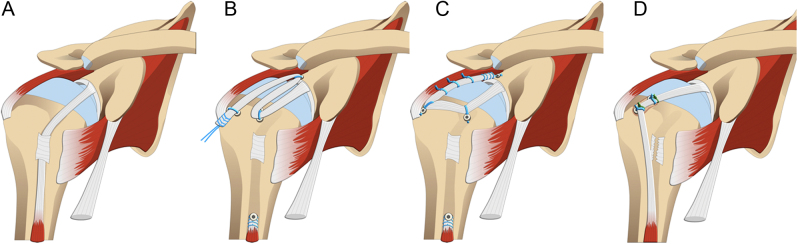
Recently, the LHBT has been utilized in numerous surgical techniques, often in combination with additional suprascapular nerve releases (11, 12, 15, 24, 33, 45, 46). These techniques can be divided into techniques rerouting the biceps tendon and techniques using the biceps tendon as an autograft (Fig. 3). All of these techniques take advantage of a viable and locally available autograft and require an intact LHBT. Successful clinical outcomes have been reported for these techniques in shoulders with intact LHBTs and intact glenohumeral cartilage.
Figure 3.
(A) Massive rotator cuff tear. (B) Snake technique by Kim et al. using the LHBT in a snake-like formation for SCR. (C) Box shape technique by Denard et al. using the LHBT in a box shape for SCR. (D) Biceps rerouting technique by Kim et al. using an intraarticular biceps tenodesis for SCR.
Rerouting biceps tendon
Kim et al. published a technique performing in situ SCR using the LHBT (16). In this technique, a mid-substance intraarticular biceps tenotomy is performed without detachment of the LHBT from the superior labral complex. The tendon is then fixated at the greater tuberosity with an anchor to reduce humeral head superior migration (Fig. 3D). Optional tenodesis at the distal aspect of the lateral anchor can be performed if needed (47, 48).
Fucai Han et al. analyzed the rerouting technique biomechanically in seven fresh frozen cadaveric shoulders in the following states: intact RC, artificially created massive RCT, and modified superior reconstruction using the LHBT. The LHBT was tenotomized at the entrance of the bicipital groove and attached with a transosseous wire suture repair at 30° of glenohumeral abduction. They found that this technique restored shoulder stability by recentering the humeral head with reduced subacromial peak contact pressure and improved range of motion (13). To further support this technique, Sang-Yup Han et al. tested eight cadaveric shoulders in unique testing conditions. They found decreased humeral head translation, reduced subacromial contact pressure, and no impairment in total rotational range after LHBT rerouting both with and without RC repair (45). Improved clinical outcomes and low retear rates have been reported for this technique used as an adjunct to arthroscopic RC repair (14, 49, 50). However, data for an isolated biceps rerouting for MIRC’s are not available yet (14, 49, 50).
A variation of the technique is the arthroscopic dynamic rerouting approach introduced by Tang and Zhao (15). In this technique, a new bicipital groove is shaped lateral to the native bicipital grove within the greater tuberosity without attaching the LHBT to the humeral head. Then, a side-to-side repair of the supraspinatus tendon is performed superior to the new groove carrying/containing the LHBT (15). Clinical or biomechanical data have not been presented yet.
In a systematic review comparing SCR techniques using LHBT, Kitridis et al. found the new techniques equal to the traditional techniques and describe them to be cost-effective, easy, and time-efficient (33).
SCR using the LHBT as an autograft
Denard et al. introduced a biceps tendon box configuration with a biomechanical study of eight cadaveric shoulders. The technique demonstrated decreased superior translation of the humeral head in massive RCTs but did not restore the translation to native levels (20). In this technique, the biceps tendon is cut at the lateral bicipital groove entrance and is fixed anteriorly at the humeral head with an anchor. The tendon is laid on the humeral head in a vertical orientation to the humeral axis and is then attached posteriorly to the greater tuberosity with a second anchor. Next, the tendon is secured to the upper margin of the infraspinatus as it continues toward the glenoid, where it is attached with a third anchor resulting in a box-shaped form (12). Clinical results for this technique are not available yet. (Fig. 3C)
A variant of this technique proposed by Kim et al. uses both the intraarticular and extraarticular portion of the LHBT for the superior capsular repair and is referred to as the Snake/Triple Bundle technique (11). In this approach, the study group used suture tape in addition to an open subpectoral tenodesis. The LHBT was arranged in a snake-like manner, meandering from the humeral head to the glenoid two to three times. This technique leaves the origin intact, and by performing a subpectoral biceps tenodesis in combination with a tenotomy at the incision site for the tenodesis, at least 14 cm of biceps tendon remain. The proximal part of the tendon is brought back to the greater tuberosity and secured with an anchor, then the loose end is brought back to the glenoid where it is fixed with another anchor (Fig. 3B). Once again, it is brought back to the humeral head at the posterior portion of the greater tuberosity. If necessary, a third bundle can be attached to the glenoid. No clinical data have been published so far.
SCR using the semitendinosus tendon as an allograft/autograft
Milano et al. published a surgical technique utilizing a semitendinosus tendon autograft. After tendon harvesting, the semitendinosus tendon is debrided and armed with non-absorbable sutures, leaving long suture tails for easier maneuvering. The greater tuberosity is cleaned, and then the graft is shuttled through the lateral portal and attached with anchors at the glenoid leaving either a box shape, V-shape, or reverse V-shape depending on the graft lengths (51, 52).
The pivot SCR fixation technique presented by Bader and Garcia in 2020 also uses a semitendinosus autograft that enters the joint through the posterior portal, shuttling the tendon through a predrilled hole in the scapular neck from posterior to anterior. The shuttling sutures of the armed autograft are utilized to pull the graft into the joint in an orientation that is parallel to the glenoid articular plane. Through a Neviaser portal, a K-wire is drilled into the upper part of the greater tuberosity, fixating the semitendinosus autograft with an interference screw (53). A biomechanical cadaver study by Berthold et al., published in 2021, showed that the V- shape and box-shape rerouting techniques significantly decreased glenohumeral superior translation and decreased maximum deltoid cumulative forces (54).
InSpace biodegradable implantable balloon (subacromial spacer)
In 2021, the US Food and Drug Administration approved the use of a subacromial spacer in MIRCTs. As described by Savarese and Romeo in 2012, the InSpace balloon gained interest due to its rather simple applicability (55). The InSpace balloon is a pre-shaped spacer consisting of poly-l-lactide-co-ɛ-caprolactone and is designed to be adsorbed in 12 months (55, 56, 57). After diagnostic arthroscopy and confirmation of the MIRCT, a lateral 1.5 cm arthroscopic portal is established parallel to the supraglenoid tubercle (55). After debridement and bursectomy in the usual fashion, the biodegradable spacer is positioned through the lateral portal and with the help of the application system 0.9% saline solution with a Luer-Lock syringe is inserted (55). The volume of saline solution utilized depends on the balloon size. Balloons are available in small (40 x 50 mm), medium (50 × 60 mm), and large (60 × 70 mm) sizes and are chosen based on shoulder and tear morphology or measurement with an arthroscopic probe (55). After inflating the InSpace Balloon, the application system is removed from the shoulder and the shoulder is moved through a full range of motion for correct implant placement (55).
After the preliminary technical description, Singh et al. provided a biomechanical analysis comparing the balloon to the SCR in irreparable RCTs based on superior humeral head migration in a cadaveric model (58). Both constructs showed comparable results at the time point zero regarding decreasing superior humeral head migration during various abduction states (0°, 30°, 60°, 90°). (58).
Since the balloon is biodegradable within 12 months, the mid- and long-term efficacy has been questioned (59). Familiari et al. prospectively investigated 51 patients with a mean age of 63 (range: 50–78) with a mean follow-up time of 36 months (range: 24–56 months) (56). The inclusion criteria were no prior shoulder surgery and a minimum of 6 months of physiotherapy preoperatively (56). This prospective study demonstrated total Constant Score (CS) improvement from 27 ± 7.4 to 77 ± 15 (P = <0.01), with 46 patients reporting good to excellent satisfaction scores and 5 reporting dissatisfaction with the results (56). A total of six patients needed revision surgery including five RTSAs and one latissimus dorsi transfer (56). Reasons for failure were not described in this study. Interestingly, the study group reported that a high postoperative acromiohumeral interval was associated with worse CS at follow-up, which is unexpected as the InSpace balloon is primarily designed to restore the humeral head position allowing for normal shoulder kinematics (56). Pieekar et al. reported similar clinical results as Familiari et al. in a cohort that included patients with partial repair. The study reported significant pre- to post-operative improvement in the Oxford Shoulder Score (21.32 to 34.39, range: 29.17–36.70), with an 82% satisfaction rate (57). In the current literature, there are no comparative studies between the InSpace Balloon and other treatment strategies for MIRCTs. Future comparative level 1 studies are needed to adequately compare these treatments.
Bursal acromial resurfacing
In addition to the InSpace balloon, Ravenscroft et al. presented another surgical technique based on the subacromial spacer concept. The bursal acromial resurfacing (BAR) technique utilizes an acellular dermal allograft as treatment for irreparable RCTs. The procedure is indicated for patients over the age of 70 with minimal to no osteoarthritic findings. According to the authors, BAR aims to combine the simplicity of the balloon and the longevity of the graft, with the goal of reducing pain and minimizing contact between the humeral head and the acromion. In addition, the procedure is proposed to be more cost-effective due to the reduced use of anchors and the durability of the construct. The BAR technique includes arthroscopic debridement with subacromial decompression to leave a bleeding bed for the autograft as well as a lateral acromioplasty. The graft is armed with six sutures using lasso loops and a cross link pattern. To place the graft, the medial sutures are shuttled into the joint and tied around the acromion, attaching the dermal allograft to the undersurface of the acromion. To date, no clinical outcomes have been presented (60).
Arthroscopic biologic interpositional tuberosity graft
Dermal allografts most commonly fail at the glenoid or in the midsubstance of the graft (39, 64). They rarely fail at the greater tuberosity (39, 64). Mirazayan et al. demonstrated in a clinical and imaging study that failed SCR with dermal allograft can still improve pain and function (67). Better coverage of the greater tuberosity resulted in better clinical outcomes, an observation described (67) as the ‘Biologic Tuberoplasty Effect’ (67). This led to the idea that an interpositional graft can be utilized to prevent painful contact between the acromion and greater tuberosity.
The biologic interpositional tuberosity graft technique presented by Griffin et al. and Mirzayan et al. (67, 84) uses an arthroscopic technique in which a dermal allograft is attached to the humeral head with anchors to cover the greater tuberosity. The graft acts like a biologic interpositional spacer between acromion and greater tuberosity preventing painful contact. Clinical results for this technique are not available yet.
Conclusion
There is a myriad of open and arthroscopic techniques to approach MIRCTs that have been developed in recent years. The development of these novel approaches has been driven by the technical challenges that surgeons experience when treating MIRCTs. Clinical results for the newer techniques are still lacking, so evidence-based recommendations cannot be made at this point. Biomechanically, all presented techniques have been shown to partially or fully restore native shoulder biomechanics. Improved shoulder function stems from the prevention of superior humeral head migration, which may stave off RCT arthropathy. This is particularly relevant for younger patients seeking to avoid RTSAs (19).
Despite lacking substantial clinical evidence, it is worth taking these new techniques into consideration as cost-effective alternative options for the treatment of MIRCTs. Future randomized, clinical, large multicenter trials are needed to determine which techniques are most suitable for different patient groups and pathologies.
ICMJE conflict of interest statement
P J Millett has received from Arthrex something of value (exceeding the equivalent of US$500) not related to this manuscript or research. He is a consultant and receives payments from Arthrex and owns stock in VuMedi with stock options in Game Ready. He received IP royalties from MedBridge. R-O Dey Hazra’s research fellowship position is supported by Arthrex, Inc. The remaining authors do not have any conflicts of interest to report.
References
- 1.Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T. Prevalence and risk factors of a rotator cuff tear in the general population. Journal of Shoulder and Elbow Surgery 201019116–120. ( 10.1016/j.jse.2009.04.006) [DOI] [PubMed] [Google Scholar]
- 2.Goodman RS.. Abnormal findings on magnetic resonance images of asymptomatic shoulders. Journal of Bone and Joint Surgery. American Volume 199678 633. [PubMed] [Google Scholar]
- 3.Chung SW, Yoon JP, Oh KS, Kim HS, Kim YG, Lee HJ, Jeong WJ, Kim DH, Lee JS, Yoon JW. Rotator cuff tear and sarcopenia: are these related? Journal of Shoulder and Elbow Surgery 201625e249–e255. ( 10.1016/j.jse.2016.02.008) [DOI] [PubMed] [Google Scholar]
- 4.Klug A, Herrmann E, Fischer S, Hoffmann R, Gramlich Y. Projections of primary and revision shoulder arthroplasty until 2040: facing a massive rise in fracture-related procedures. Journal of Clinical Medicine 202110. ( 10.3390/jcm10215123) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marigi EM, Johnson QJ, Dholakia R, Borah BJ, Sanchez-Sotelo J, Sperling JW. Cost comparison and complication profiles of superior capsular reconstruction, lower trapezius transfer, and reverse shoulder arthroplasty for irreparable rotator cuff tears. Journal of Shoulder and Elbow Surgery 202231847–854. ( 10.1016/j.jse.2021.08.027) [DOI] [PubMed] [Google Scholar]
- 6.Gerber C.. Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff. Clinical Orthopaedics and Related Research 1992275152–160. Available at: https://pubmed.ncbi.nlm.nih.gov/1735206/ [PubMed] [Google Scholar]
- 7.Waltenspül M, Jochum B, Filli L, Ernstbrunner L, Wieser K, Meyer D, Gerber C. Mid-term results of arthroscopically assisted latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. Journal of Shoulder and Elbow Surgery 202130e676–e688. ( 10.1016/j.jse.2021.03.149) [DOI] [PubMed] [Google Scholar]
- 8.Elhassan BT, Sanchez-Sotelo J, Wagner ER. Outcome of arthroscopically assisted lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tears. Journal of Shoulder and Elbow Surgery 2020292135–2142. ( 10.1016/j.jse.2020.02.018) [DOI] [PubMed] [Google Scholar]
- 9.Gerber C, Rahm SA, Catanzaro S, Farshad M, Moor BK. Latissimus dorsi tendon transfer for treatment of irreparable posterosuperior rotator cuff tears: long-term results at a minimum follow-up of ten years. Journal of Bone and Joint Surgery. American Volume 2013951920–1926. ( 10.2106/JBJS.M.00122) [DOI] [PubMed] [Google Scholar]
- 10.Samuelsen BT, Wagner ER, Houdek MT, Elhassan BT, Sánchez-Sotelo J, Cofield R, Sperling JW. Primary reverse shoulder arthroplasty in patients aged 65 years or younger. Journal of Shoulder and Elbow Surgery 201726e13–e17. ( 10.1016/j.jse.2016.05.026) [DOI] [PubMed] [Google Scholar]
- 11.Kim D, Jang Y, Park J, On M. Arthroscopic superior capsular reconstruction with biceps autograft: snake technique. Arthroscopy Techniques 20198e1085–e1092. ( 10.1016/j.eats.2019.05.023) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Denard PJ, Chae S, Chalmers C, Choi JH, McGarry MH, Adamson G, Park M, Lee TQ. Biceps box configuration for superior capsule reconstruction of the glenohumeral joint decreases superior translation but not to native levels in a biomechanical study. Arthroscopy, Sports Medicine, and Rehabilitation 20213e343–e350. ( 10.1016/j.asmr.2020.09.024) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han F, Kong CH, Hasan MY, Ramruttun AK, Kumar VP. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: a biomechanical study on cadavers. Orthopaedics and Traumatology, Surgery and Research 2019105257–263. ( 10.1016/j.otsr.2018.10.023) [DOI] [PubMed] [Google Scholar]
- 14.Rhee SM, Youn SM, Park JH, Rhee YG. Biceps rerouting for semirigid large-to-massive rotator cuff tears. Arthroscopy 2021372769–2779. ( 10.1016/j.arthro.2021.04.008) [DOI] [PubMed] [Google Scholar]
- 15.Tang J, Zhao J. Dynamic biceps rerouting for irreparable posterior-superior rotator cuff tear. Arthroscopy Techniques 20209e1709–e1714. ( 10.1016/j.eats.2020.07.014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim YS, Lee HJ, Park I, Sung GY, Kim DJ, Kim JH. Arthroscopic in situ superior capsular reconstruction using the long head of the biceps tendon. Arthroscopy Techniques 20187e97–e103. ( 10.1016/j.eats.2017.08.058) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Colbath G, Murray A, Siatkowski S, Pate T, Krussig M, Pill S, Hawkins R, Tokish J, Mercuri J. Autograft long head biceps tendon can be used as a scaffold for biologically augmenting rotator cuff repairs. Arthroscopy 20223838–48. ( 10.1016/j.arthro.2021.05.064) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zink TR, Schmidt CC, Papadopoulos DV, Blake RJ, Smolinski MP, Davidson AJ, Spicer CS, Miller MC, Smolinski PJ. Locating the rotator cable during subacromial arthroscopy: bursal- and articular-sided anatomy. Journal of Shoulder and Elbow Surgery 202130S57–S65. ( 10.1016/j.jse.2021.03.148) [DOI] [PubMed] [Google Scholar]
- 19.Lacheta L, Horan MP, Goldenberg BT, Dornan GJ, Higgins B, Millett PJ. Minimum 2-year clinical outcomes after superior capsule reconstruction compared with reverse total shoulder arthroplasty for the treatment of irreparable posterosuperior rotator cuff tears in patients younger than 70 years. Journal of Shoulder and Elbow Surgery 2020292514–2522. ( 10.1016/j.jse.2020.04.002) [DOI] [PubMed] [Google Scholar]
- 20.Patte D.. Classification of rotator cuff lesions. Clinical Orthopaedics and Related Research 199025481–86. ( 10.1097/00003086-199005000-00012) [DOI] [PubMed] [Google Scholar]
- 21.Davidson J, Burkhart SS. The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy 201026417–424. ( 10.1016/j.arthro.2009.07.009) [DOI] [PubMed] [Google Scholar]
- 22.DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. Journal of Bone and Joint Surgery. American Volume 198466563–567. ( 10.2106/00004623-198466040-00011) [DOI] [PubMed] [Google Scholar]
- 23.Schumaier A, Kovacevic D, Schmidt C, Green A, Rokito A, Jobin C, Yian E, Cuomo F, Koh J, Gilotra Met al. Defining massive rotator cuff tears: a Delphi consensus study. Journal of Shoulder and Elbow Surgery 202029674–680. ( 10.1016/j.jse.2019.10.024) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.St Pierre P, Millett PJ, Abboud JA, Cordasco FA, Cuff DJ, Dines DM, Dornan GJ, Duralde XA, Galatz LM, Jobin CMet al. Consensus statement on the treatment of massive irreparable rotator cuff tears: a Delphi approach by the Neer Circle of the American Shoulder and Elbow Surgeons. Journal of Shoulder and Elbow Surgery 2021301977–1989. ( 10.1016/j.jse.2021.05.012) [DOI] [PubMed] [Google Scholar]
- 25.Tse AK, Lam PH, Walton JR, Hackett L, Murrell GAC. Ultrasound determination of rotator cuff tear repairability. Shoulder and Elbow 2016814–21. ( 10.1177/1758573215585284) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frangiamore S, Dornan GJ, Horan MP, Mannava S, Fritz EM, Hussain ZB, Moatshe G, Godin JA, Pogorzelski J, Millett PJ. Predictive modeling to determine functional outcomes after arthroscopic rotator cuff repair. American Journal of Sports Medicine 2020481559–1567. ( 10.1177/0363546520914632) [DOI] [PubMed] [Google Scholar]
- 27.Melis B, Nemoz C, Walch G. Muscle fatty infiltration in rotator cuff tears: descriptive analysis of 1688 cases. Orthopaedics and Traumatology, Surgery and Research 200995319–324. ( 10.1016/j.otsr.2009.05.001) [DOI] [PubMed] [Google Scholar]
- 28.Khair MM, Gulotta LV. Treatment of irreparable rotator cuff tears. Current Reviews in Musculoskeletal Medicine 20114208–213. ( 10.1007/s12178-011-9098-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kovacevic D, Suriani RJ, Grawe BM, Yian EH, Gilotra MN, Hasan SA, Srikumaran U, Hasan SS, Cuomo F, Burks RTet al. Management of irreparable massive rotator cuff tears: a systematic review and meta-analysis of patient-reported outcomes, reoperation rates, and treatment response. Journal of Shoulder and Elbow Surgery 2020292459–2475. ( 10.1016/j.jse.2020.07.030) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kleim BD, Siebenlist S, Scheiderer B, Imhoff AB. Irreparable rotator cuff tear—reverse shoulder arthroplasty and alternative procedures. Der Unfallchirurg 2021124117–124. ( 10.1007/s00113-020-00922-3) [DOI] [PubMed] [Google Scholar]
- 31.Petri M, Greenspoon JA, Millett PJ. Arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy Techniques 20154e751–e755. ( 10.1016/j.eats.2015.07.018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical effect of thickness and tension of fascia Lata Graft on glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthroscopy 201632418–426. ( 10.1016/j.arthro.2015.08.024) [DOI] [PubMed] [Google Scholar]
- 33.Kitridis D, Yiannakopoulos C, Sinopidis C, Givissis P, Galanis N. Superior capsular reconstruction of the shoulder using the long head of the biceps tendon: a systematic review of surgical techniques and clinical outcomes. Medicina 2021571–12. ( 10.3390/medicina57030229) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. American Journal of Sports Medicine 2016441423–1430. ( 10.1177/0363546516631751) [DOI] [PubMed] [Google Scholar]
- 35.Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical effects of acromioplasty on superior capsule reconstruction for irreparable supraspinatus tendon tears. American Journal of Sports Medicine 201644191–197. ( 10.1177/0363546515608652) [DOI] [PubMed] [Google Scholar]
- 36.Greenspoon JA, Petri M, Warth RJ, Millett PJ. Massive rotator cuff tears: pathomechanics, current treatment options, and clinical outcomes. Journal of Shoulder and Elbow Surgery 2015241493–1505. ( 10.1016/j.jse.2015.04.005) [DOI] [PubMed] [Google Scholar]
- 37.Mihata T, Lee TQ, Hasegawa A, Fukunishi K, Kawakami T, Fujisawa Y, Ohue M, Neo M. Five-year follow-up of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Journal of Bone and Joint Surgery. American Volume 20191011921–1930. ( 10.2106/JBJS.19.00135) [DOI] [PubMed] [Google Scholar]
- 38.Lacheta L, Brady A, Rosenberg SI, Dekker TJ, Kashyap R, Zandiyeh P, Dornan GJ, Provencher MT, Millett PJ. Superior capsule reconstruction with a –thick dermal allograft partially restores glenohumeral stability in massive posterosuperior rotator cuff deficiency: a dynamic robotic shoulder model. American Journal of Sports Medicine 2021492056–2063. ( 10.1177/03635465211013364) [DOI] [PubMed] [Google Scholar]
- 39.Lacheta L, Horan MP, Schairer WW, Goldenberg BT, Dornan GJ, Pogorzelski J, Millett PJ. Clinical and imaging outcomes after arthroscopic superior capsule reconstruction with human dermal allograft for irreparable posterosuperior rotator cuff tears: a minimum 2-year follow-up. Arthroscopy 2020361011–1019. ( 10.1016/j.arthro.2019.12.024) [DOI] [PubMed] [Google Scholar]
- 40.Burkhart SS, Pranckun JJ, Hartzler RU. Superior capsular reconstruction for the operatively irreparable rotator cuff tear: clinical outcomes are maintained 2 years after surgery. Arthroscopy 202036373–380. ( 10.1016/j.arthro.2019.08.035) [DOI] [PubMed] [Google Scholar]
- 41.Hartzler RU, Softic D, Qin X, Dorfman A, Adams CR, Burkhart SS. The histology of a healed superior capsular reconstruction dermal allograft: a case report. Arthroscopy 2019352950–2958. ( 10.1016/j.arthro.2019.06.024) [DOI] [PubMed] [Google Scholar]
- 42.Altintas B, Scibetta AC, Storaci HW, Lacheta L, Anderson NL, Millett PJ. Biomechanical and histopathological analysis of a retrieved dermal allograft after superior capsule reconstruction: a case report. Arthroscopy 2019352959–2965. ( 10.1016/j.arthro.2019.07.006) [DOI] [PubMed] [Google Scholar]
- 43.Hasegawa A, Mihata T, Itami Y, Fukunishi K, Neo M. Histologic changes during healing with autologous fascia lata graft after superior capsule reconstruction in rabbit model. Journal of Shoulder and Elbow Surgery 2021302247–2259. ( 10.1016/j.jse.2021.02.019) [DOI] [PubMed] [Google Scholar]
- 44.Altintas B, Higgins B, Anderson N, Millett PJ. Superior capsule reconstruction for the treatment of irreparable rotator cuff tears. Operative Techniques in Orthopaedics 201828226–231. ( 10.1053/j.oto.2018.08.007) [DOI] [Google Scholar]
- 45.Han SY, Lee TQ, Wright DJ, Park IJ, Mauro M, McGarry MH, Lee HJ, Kim YS. Effect of biceps rerouting technique to restore glenohumeral joint stability for large irreparable rotator cuff tears: a cadaveric biomechanical study. Journal of Shoulder and Elbow Surgery 2020291425–1434. ( 10.1016/j.jse.2019.11.015) [DOI] [PubMed] [Google Scholar]
- 46.Sachinis NP, Papagiannopoulos S, Sarris I, Papadopoulos P. Outcomes of arthroscopic nerve release in patients treated for large or massive rotator cuff tears and associated suprascapular neuropathy: a prospective, randomized, double-blinded clinical trial. American Journal of Sports Medicine 2021492301–2308. doi:10.1177/03635465211021834) [DOI] [PubMed] [Google Scholar]
- 47.Boileau P, Bicknell RT, El Fegoun AB, Chuinard C. Arthroscopic Bristow procedure for anterior instability in shoulders with a stretched or deficient capsule: the “belt-and-suspenders” operative technique and preliminary results. Arthroscopy 200723593–601. ( 10.1016/j.arthro.2007.03.096) [DOI] [PubMed] [Google Scholar]
- 48.Garcia JC, Belchior RJ, Mello MBD, Cardoso AM. The long head of the biceps Bristow-Bankart procedure for anterior shoulder instability. Arthroscopy Techniques 20198e1185–e1191. ( 10.1016/j.eats.2019.06.005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Llinás PJ, Bailie DS, Sanchez DA, Chica J, Londono JF, Herrera GA. Partial superior capsular reconstruction to augment arthroscopic repair of massive rotator cuff tears using autogenous biceps tendon: effect on retear rate. American Journal of Sports Medicine 2022503064–3072. ( 10.1177/03635465221112659) [DOI] [PubMed] [Google Scholar]
- 50.Chiang CH, Shaw L, Chih WH, Yeh ML, Ting HH, Lin CH, Chen CP, Su WR. Modified superior capsule reconstruction using the long head of the biceps tendon as reinforcement to rotator cuff repair lowers retear rate in large to massive reparable rotator cuff tears. Arthroscopy 2021372420–2431. ( 10.1016/j.arthro.2021.04.003) [DOI] [PubMed] [Google Scholar]
- 51.Milano G, Saccomanno MF, Colosio A, Adriani M, Galli S, Scaini A, Marchi G. Arthroscopic superior capsule reconstruction with doubled autologous semitendinosus tendon graft. Arthroscopy Techniques 20209e1665–e1672. ( 10.1016/j.eats.2020.07.009) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rosales-Varo AP, Zafra M, García-Espona MA, Flores-Ruiz MA, Roda O. Superior capsular reconstruction of irreparable rotator cuff tear using autologous hamstring graft. Revista Española de Cirugía Ortopédica y Traumatología 2019631–6. ( 10.1016/j.recot.2018.08.004) [DOI] [PubMed] [Google Scholar]
- 53.Bader DAL, Garcia JC. Pivot superior capsular reconstruction of the shoulder. Arthroscopy Techniques 20209e697–e701. ( 10.1016/j.eats.2020.01.026) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Berthold DP, Muench LN, Dyrna F, Scheiderer B, Obopilwe E, Cote MP, Krifter MR, Milano G, Bell R, Voss Aet al. Comparison of different fixation techniques of the long head of the biceps tendon in superior capsule reconstruction for irreparable posterosuperior rotator cuff tears: a dynamic biomechanical evaluation. American Journal of Sports Medicine 202149305–313. ( 10.1177/0363546520981559) [DOI] [PubMed] [Google Scholar]
- 55.Savarese E, Romeo R. New solution for massive, irreparable rotator cuff tears: the subacromial “biodegradable spacer.” Arthroscopy Techniques 20121e69–e74. ( 10.1016/j.eats.2012.02.002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Familiari F, Nayar SK, Russo R, De Gori M, Ranuccio F, Mastroianni V, Giuzio E, Galasso O, Gasparini G, McFarland EGet al. Subacromial balloon spacer for massive, irreparable rotator cuff tears is associated with improved shoulder function and high patient satisfaction. Arthroscopy 202137480–486. ( 10.1016/j.arthro.2020.09.048) [DOI] [PubMed] [Google Scholar]
- 57.Piekaar RSM, Bouman ICE, van Kampen PM, van Eijk F, Huijsmans PE. The subacromial balloon spacer for massive irreparable rotator cuff tears: approximately 3 years of prospective follow-up. Musculoskeletal Surgery 2020104207–214. ( 10.1007/s12306-019-00614-1) [DOI] [PubMed] [Google Scholar]
- 58.Singh S, Reeves J, Langohr GDG, Johnson JA, Athwal GS. The subacromial balloon spacer versus superior capsular reconstruction in the treatment of irreparable rotator cuff tears: a biomechanical assessment. Arthroscopy 201935382–389. ( 10.1016/j.arthro.2018.09.016) [DOI] [PubMed] [Google Scholar]
- 59.Guevara BG.. Editorial commentary: balloons for rotator cuff tears: A viable treatment or just a bunch of hot air? Arthroscopy 202137487–488. ( 10.1016/j.arthro.2020.11.018) [DOI] [PubMed] [Google Scholar]
- 60.Ravenscroft M, Barnes MW, Muench LN, Mazzocca AD, Berthold DP. Bursal acromial reconstruction (BAR) using an acellular dermal allograft as a surgical solution for the treatment of massive irreparable rotator cuff tears. Arthroscopy Techniques 202110e877–e885. ( 10.1016/j.eats.2020.11.002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Emerson CP, Balazs GC, Lee SC, Dines JS, Jose J, Greditzer HG. Magnetic resonance imaging of the failed superior capsular reconstruction. Clinical Imaging 202060172–176. ( 10.1016/j.clinimag.2019.10.006) [DOI] [PubMed] [Google Scholar]
- 62.Mirzayan R, Bouz G. Biologic tuberoplasty with an acellular dermal allograft for massive rotator cuff tears. Arthroscopy Techniques 202110e1743–e1749. ( 10.1016/j.eats.2021.03.016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Griffin JW, Runzo D, Bonner KF. Arthroscopic biologic interpositional tuberosity graft for the treatment of irreparable rotator cuff tears. Arthroscopy Techniques 202110e1729–e1735. ( 10.1016/j.eats.2021.03.024) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mihata T Lee TQ Watanabe C Fukunishi K Ohue M Tsujimura T & Kinoshita M.. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy 2013 29459–470. ( 10.1016/j.arthro.2012.10.022) [DOI] [PubMed] [Google Scholar]
- 65.Denard PJ Brady PC Adams CR Tokish JM & Burkhart SS.. Preliminary Results of Arthroscopic Superior Capsule Reconstruction with Dermal Allograft. Arthroscopy 2018 3493–99. ( 10.1016/j.arthro.2017.08.265) [DOI] [PubMed] [Google Scholar]
- 66.Hirahara AM Andersen WJ & Panero AJ.. Superior Capsular Reconstruction: Clinical Outcomes After Minimum 2-Year Follow-Up. American Journal of Orthopedics (Belle Mead, NJ) 2017 46266–278. [PubMed] [Google Scholar]
- 67.SJ Lee & Min YK.. Can inadequate acromiohumeral distance improvement and poor posterior remnant tissue be the predictive factors of re-tear? Preliminary outcomes of arthroscopic superior capsular reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy 2018 262205–2213. ( 10.1007/s00167-018-4912-8) [DOI] [PubMed] [Google Scholar]
- 68.Lim S AlRamadhan H Kwak JM Hong H & Jeon IH.. Graft tears after arthroscopic superior capsule reconstruction (ASCR): pattern of failure and its correlation with clinical outcome. Archives of Orthopaedic and Trauma Surgery 2019 139231–239. ( 10.1007/s00402-018-3025-7) [DOI] [PubMed] [Google Scholar]
- 69.Mihata T Lee TQ Hasegawa A Kawakami T Fukunishi K Fujisawa Y Itami Y Ohue M & Neo M.. Arthroscopic Superior Capsule Reconstruction Can Eliminate Pseudoparalysis in Patients With Irreparable Rotator Cuff Tears. American Journal of Sports Medicine 2018 462707–2716. ( 10.1177/0363546518786489) [DOI] [PubMed] [Google Scholar]
- 70.Pennington WT Bartz BA Pauli JM Walker CE & Schmidt W.. Arthroscopic Superior Capsular Reconstruction With Acellular Dermal Allograft for the Treatment of Massive Irreparable Rotator Cuff Tears: Short-Term Clinical Outcomes and the Radiographic Parameter of Superior Capsular Distance. Arthroscopy 2018 341764–1773. ( 10.1016/j.arthro.2018.01.009) [DOI] [PubMed] [Google Scholar]
- 71.SS Burkhart & Hartzler RU.. Superior Capsular Reconstruction Reverses Profound Pseudoparalysis in Patients With Irreparable Rotator Cuff Tears and Minimal or No Glenohumeral Arthritis. Arthroscopy 2019 3522–28. ( 10.1016/j.arthro.2018.07.023) [DOI] [PubMed] [Google Scholar]
- 72.Okamura K Abe M Yamada Y Makihara T Yoshimizu T Sakaki Y Suzumori Y & Mihata T.. Arthroscopic superior capsule reconstruction with Teflon felt synthetic graft for irreparable massive rotator cuff tears: clinical and radiographic results at minimum 2-year follow-up. Journal of Shoulder and Elbow Surgery 202130625–634. ( 10.1016/j.jse.2020.06.022) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a