Abstract
Objectives
Bio-psycho-social frailty is related to increased risk of death and utilization of health services. This paper reports the predictive validity of a 10-min multidimensional questionnaire on the risk of death, hospitalization and institutionalization.
Methods
A retrospective cohort study was performed based on data from the “Long Live the Elderly!” program, involving 8,561 community-dwelling Italian people >75, followed for an average of 516.6 days (Median = 448, P25–P75: 309–692). Mortality, hospitalization, and institutionalization rates according to frailty levels assessed by the Short Functional Geriatric Evaluation (SFGE) have been calculated.
Results
Compared with the robust, the pre-frail, frail, and very frail faced a statistically significant increase in the risk of mortality (RR = 1.40, 2.78 and 5.41), hospitalization (OR = 1.31, 1.67, and 2.08) and institutionalization (OR = 3.63, 9.52, and 10.62). Similar results were obtained in the sub-sample of those with only socio-economic issues. Frailty predicted mortality with an area under the ROC curve of 0.70 (95% CI 0.68–0.72) with sensitivity and specificity of 83.2% and 40.4%. Analyses of single determinants of these negative outcomes showed a multivariable pattern of determinants for all the events.
Conclusions
The SFGE predicts death, hospitalization and institutionalization by stratifying older people according to the levels of frailty. The short administration time, the socio-economic variables and the characteristics of personnel administering the questionnaire make it suitable for being used in public health as a screening tool for a large population, to put frailty at the core of the care for community-dwelling older adults. The difficulty in capturing the complexity of the frailty is witnessed by the moderate sensitivity and specificity of the questionnaire.
Keywords: Aged, Frailty, Geriatric assessment, Italy, Surveys and questionnaires
What is known?
-
•
Frailty is correlated with an increased risk of death, hospitalization, and institutionalization.
-
•
There is a large variety of frailty assessment tools, which differ in administration time, types of frailty investigated (psychophysical only or also social), and the personnel who can administer them.
-
•
The Short Functional Geriatric Evaluation (SFGE) is a multidimensional questionnaire that measures bio-psycho-social frailty and is administered in a maximum of 10 min, even by people with a high school diploma and on the phone.
What is new?
-
•
The SFGE has significant predictive validity for mortality, hospitalization, and institutionalization in both older adults with and without psycho-physical impairment.
-
•
The SFGE identifies older adults with a lack of socio-economic resources that are also associated with negative outcomes, namely mortality, hospitalization, and institutionalization.
-
•
The SFGE can be used on the community-dwelling older population as a screening tool to plan tailored interventions for people most at risk of death, hospitalization, and institutionalization.
1. Introduction
The Italian population is characterized by progressive aging; ISTAT (Istituto Nazionale di Statistica) showed that the old age index in 2011 and 2019 were respectively 148.7% and 180% [1] and that in 2019 people over 75 were approximately 6.9 million, including 2.5 million dependent in some functional activities [2]. That leads to a growing demand for social and health care services fuelled by the prevalence of Bio-Psycho-Social Frailty, which has been shown to be the most important determinant of care needs as well as the most synthetic and predictive indicator of negative events like death, hospitalization and institutionalization. Although the correlation between frailty and aging seems logical and obvious, quantitative data on the prevalence of frailty and its geographical distribution remain debated also because of its multiple definitions and measurement tools. A recent meta-analysis by O’Caoimh et al. carried out on people over 50 in 62 countries worldwide and taking all scales into account, showed that the prevalence of frailty and pre-frailty ranged between 12% (physical frailty) and 24% (deficit accumulation model) for frailty and between 46% (physical frailty) and 49% for pre-frailty [3]. This study showed a prevalence of frailty in Europe ranging from 8% (physical frailty) to 19% (deficit accumulation model). Concerning Italy, the values would seem to be higher; in fact, another work showed a prevalence of frailty and pre-frailty in the community-dwelling people over 65 of 23.0% and 45.6%, respectively (weighted proportion) [4]. In a study carried out in the Lazio Region on a population over 64, the prevalence of frailty was 13.9% [5].
Using the multidimensional bio-psycho-social approach, Gobbens et al. defined frailty as “a dynamic state affecting an individual who experiences losses in one or more domains of human functioning (physical, psychological and social), which is caused by the influence of a range of variables and increases the risk of adverse outcomes” [6] and recently many authors agreed with the multidimensional definition [7]. Assessing frailty is a key issue because it is very common among older adults [3], and it is associated with a lower survival rate [8], higher risk of functional decline [9], loss of independence at 12 months [10], death [11,12], institutionalization [13], hospitalization [14], higher frequency of emergency room access [15] and increased use of hospital services [16]. The increased risk of frail persons living at home to being hospitalized may be caused by the fact that any minor adverse event can alter their functional reserve; the consequence is that their hospitalization may contribute to an increase of both further negative events and increased healthcare costs. On the other hand, hospitalization often reveals the presence of a prodromal state of frailty (pre-frailty) that could be treated at home if it had been identified earlier through screening programs. Researching frailty through appropriate tools and implementing programs aimed at preventing frailty and taking care of the pre-frail and frail population through the implementation of individual care plans has a significant impact on social and health policies while also reducing the costs of social and health services. Then, frailty can be used as an indicator to plan Public Health interventions to prevent negative outcomes and reduce the hospital admission rate. WHO recently declared that health-related policies should operate considering the functional capacity of older people with a person-centered intervention [17] that, of course, involves social and health interventions. In these years, the need for health and social integrated care increased and many interventions have been proposed to promote out-of-hospital care [18] and to create multidimensional teams to act on integrated care [19].
Assessing frailty in older people living at home can allow health and social professionals to prevent frailty onset by planning preventive interventions [20] to preserve the functional and cognitive reserves [21] or to mitigate the impact of frailty on the health status of older people. Besides, the progression from non-frailty to frailty is associated with an increase in healthcare costs [22] that can be reduced by timely intervention led by the assessment of frailty. Finally, frailty can often be reversible [23]. The assessment of frailty needs a valid and reliable questionnaire, capable of accurately predicting negative outcomes such as hospital admission and mortality and of identifying people showing first signs of pre-frailty. To ideally reach all the population at higher risk of frailty, this questionnaire should have the following characteristics: to be simple, with few questions, multidimensional, quick to administer and should also be managed by non-specialist personnel. This holistic approach has to include the socio-economic aspect because factors such as social isolation are associated with mortality. Besides, this tool should also be validated on very large samples to be used in a Public Health setting. There are few available questionnaires with these characteristics.
This study aimed to examine the predictive validity of the Short Functional Geriatric Evaluation (SFGE) questionnaire to assess mortality, hospital admission, and institutionalization associated with frailty in a sample of community-dwelling older people aged>75.
The SFGE is a multidimensional, short, and simple scale that assesses frailty and stratifies the older population into 4 groups: robust, pre-frail, frail, and very frail [16,24,25]. The secondary outcome of this study is to ascertain whether the social issues assessed by SFGE are predictive of mortality, hospitalization, and institutionalization independently of the health aspects assessed by the same questionnaire. The construct validity of the questionnaire is under evaluation in a parallel paper to be published.
2. Methods
2.1. Study design
In this retrospective cohort study, we conducted a secondary analysis of data gathered from January 2016 to December 2020, on all the individuals’ records of community-dwelling people over 75 included in the “Long Live Elderly!” (LLE) program. The research was approved by the Independent Ethical Committee of our University (R.S. 60/17). After signing the informed consent, SFGE was administered on the phone by personnel with expertise in responding to a demand for protective and/or social care but not health care.
2.2. Long Live the Elderly!
The LLE program was instituted by the “Community of Sant’Egidio” and started in 2004 in Rome to prevent the consequences of heatwaves on the older population by reducing social isolation and increasing social capital at individual and community levels [26]. The LLE program’s protocol includes following all people over 75 in city areas chosen based on the availability of city municipalities to host the program and the funds available to implement it. The intervention starts with the telephone administration of SFGE [14]. After the first phone call, the participants were contacted a variable number of times, depending on the level of frailty detected (from once every 2 weeks to once every 3 months). The training of operators to administer the questionnaire was all done in Rome where inter-reliability and intra-reliability have been tested. The trained operators have been involved in recruiting participants with a proactive approach, including telephone calls, home visits and meetings through organized activities. Based on the frailty assessment, an individualised care plan is drafted to take care of frail individuals and periodically re-evaluated to meet the development of individuals’ social and health needs. Over the years, the program has been extended to some urban areas in the towns of Brindisi, Catania, Civitavecchia, Ferentino, Genoa, Naples, Novara, and Sassari.
2.3. Questionnaire
The SFGE is a multidimensional questionnaire to assess frailty in community-dwelling older people [25]. It is the short version of the Functional Geriatric Evaluation (FGE), a scale validated in Italy by Palombi et al. [8] derived from the GRAUER Functional Rating Scale [27]. SFGE showed a good correlation with FGE [24] and is characterized by good short-term sensitivity (90.4%) and specificity (78.3%) for the assessment of frailty (area under curve [AUC] 0.928; 95% CI 0.910–0.947) [16]. It consists of 13 questions about physical, functional, psychological, and socio-economic domains (see Appendix A). It is composed of 6 sections: Age and Education (items 1–2), Cohabitants (item 3), Informal/Formal Social Network (items 4–6 asks whether the person can count on someone in case of need, whether he/she is involved in social activities and whether he/she receives formal care services), Economic Situation (items 7–8 asks whether the pension is enough to get to the end of the month and the reason if not), Psychological Condition (item 9, that is about energy and motivation) and Health/Functional Status (items 10–13 asks whether the person can use the shower or bath independently, whether he/she can get out of the house, and whether he/she is bedridden or confused). SFGE can be administered by phone for a maximum of 10 min and can be managed by anyone with a secondary school diploma. Based on the results of this scale [16], older people can be stratified into 4 groups: robust (score ≤0), pre-frail (1–2), frail (3–9), and very frail (≥10).
2.4. Setting and participants
The setting involved community-dwelling people of the LLE program living in Brindisi, Catania, Civitavecchia, Ferentino, Genoa, Naples, Novara, Rome, and Sassari, all cities where the LLE program is active. The questionnaire has been administered over the phone by the non-health personnel trained in the Rome program headquarter to perform this task.
The recruited participants were all those residents in the Urban Areas included in the LLE program during the study period. The exclusion criteria were an age of fewer than 75 years and the refusal to sign the informed consent.
2.5. Data collection and statistical analysis
The data collection has been included in the software used, and the data have been analyzed from February 2021 to December 2021. Data entry has been done manually by one author and checked by another.
Through the statistical analysis, we studied the risk of hospitalization, institutionalization and mortality in the sample by comparing the pre-frail, frail, and very frail classes with the robust class considered as the reference. The average observation time was 516.6 days (Median 448, P25–P75: 309–692).
We used the Cox hazard regression model to compare the mortality of pre-frail, frail, and very frail persons to that of robust ones (reference category), including age and gender as covariates. We conducted the same analysis excluding all subjects with an impairment in Activities of Daily Living/Instrumental Activities of Daily Living (ADL/IADL) and/or psychological problems (those who showed no psycho-physical impairment, scoring zero to questions 9 to 13), to study the predictive validity of SFGE socio-economic issues in the sub-sample which did not show psycho-physical and/or functional impairment according to the questionnaire.
Binary logistic regression was used to study the relationship between hospitalization or institutionalization (dependent variable) and SFGE classes, gender, and age (covariates). Then we repeated the analysis as we had previously done for mortality, excluding subjects with physical, psychological, and functional impairment. The AUC by frailty score (the threshold for being defined frail≥1) for the occurrence of any of the three negative events and for each event separately has been also evaluated.
In all the analyses, a P-value <0.05 was considered statistically significant. Data entry and statistical analyses were performed using SPSS statistical software version 26 (SPSS Inc., Chicago, Illinois, United States).
3. Results
3.1. Baseline characteristics of all participants
This study sample was made up of 8,561 people over 75 years old, 2,834 males (33.1%) and 5,727 females (66.9%), monitored for 516.6 days on average. The mean age was 84.98 (SD = 5.17) and 84.31 (SD = 4.03) for females and males, respectively. People recruited in the study came mainly from Rome (4,204, 49.1%), Naples (1,808, 21.1%), Novara (1,197, 14.0%), and Genoa (653, 7.6%) (Table 1). There were no differences in the gender distribution of the sample among the cities; regarding age, Brindisi, Naples, and Sassari had a population of over 85, slightly greater than 40%. At the study baseline, the robust, pre-frail, frail and very frail were 3,319 (37.7%), 2,108 (24.0%), 2,577 (29.3%) and 796 (9.0%), respectively. Less than 5% of those contacted by telephone for the first time refused to answer the questionnaire. The final sample included a very large number of residents from various Italian cities and was therefore strongly representative of the older Italian population.
Table 1.
Distribution of the sample by the city of residence.
| City | Sample | Female | Aged over 85 |
|---|---|---|---|
| Rome | 4,204 (49.1) | 2,791 (66.4) | 1,774 (42.2) |
| Naples | 1,808 (21.1) | 1,205 (66.6) | 869 (48.1) |
| Novara | 1,197 (14.0) | 816 (68.2) | 511 (42.7) |
| Genoa | 653 (7.6) | 441 (67.5) | 292 (44.7) |
| Sassari | 298 (3.5) | 202 (67.8) | 142 (47.7) |
| Brindisi | 155 (1.8) | 99 (63.9) | 90 (58.1) |
| Catania | 148 (1.7) | 100 (67.6) | 63 (42.6) |
| Civitavecchia | 50 (0.6) | 36 (72.0) | 18 (36.1) |
| Ferentino | 48 (0.6) | 37 (77.1) | 23 (47.9) |
| Total | 8,561 (100) | 5,727 (66.9) | 3,782 (44.2) |
Note: Data are n (%).
During the observation, 55 people were lost at the follow-up about mortality data (0.6% of the total sample) and 1,566 people about both hospitalization and institutionalization information (18.3% of the total sample). These persons did not differ in age and sex from the people retained in the follow-up. During the same period, 941 persons died (11.0%), 785 were admitted to the hospital (9.2%) and 261 were institutionalized (3.0%). In the statistical analyses also, people without psychophysical impairments were considered. In this case, the sample was composed of 5,540 people of a mean age of 83.74 (SD = 4.31) years, 3,494 women (63.1%) and 2,046 men (36.9%), divided into 3 categories: robust (n = 3,069, 55.4%), pre-frail (n = 1,641, 29.6%) and frail (n = 830, 15.0%).
3.2. The predictive validity of SFGE for mortality (Cox regression analysis)
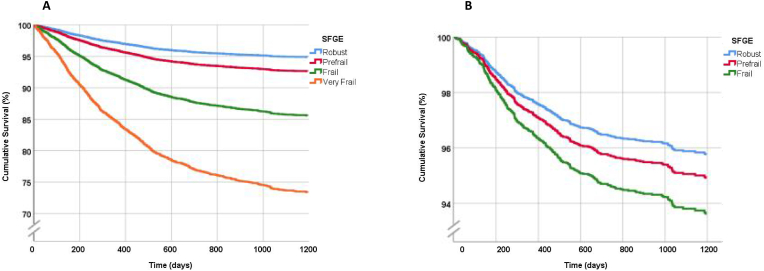
The Cox regression analysis showed that Survival Rate adjusted for age and gender was significantly associated with the frailty level identified by the administration of the SFGE. In fact, the risk of death compared with robust individuals increases progressively, through pre-frail (RR 1.40, 95% CI 1.11–1.76), frail (RR 2.78, 95% CI 2.29–3.38), and very frail individuals (RR 5.41, 95% CI 4.35–6.72), respectively. Besides, the risk of death was lower in women and increased with age (Table 2 – Model 1). The Cox regression analysis excluding individuals with psychophysical impairment showed a statistically significant increase in the risk of death for frail individuals compared with robust ones (RR 1.47, 95% CI 1.07–2.01) (Table 2 – Model 2). Pre-frail individuals showed an increased risk of death without statistical significance (Fig. 1). These results, therefore, showed that the SFGE could predict mortality associated with socio-economic frailty, in citizens who did not show any psycho-physical or functional impairment.
Table 2.
Multivariable Cox proportional hazard risk (death) and binary logistic regression (hospitalization and institutionalization).
| Variable | Model 1 (n = 8,561) |
Model 2 (n= 5,540) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| RR or OR | 95% CI |
RR or OR | 95% CI |
P | |||||
| Lower | Upper | Lower | Upper | ||||||
| Death | RR | P | RR | ||||||
| Age | 1.07 | 1.06 | 1.09 | <0.001 | 1.11 | 1.08 | 1.13 | <0.001 | |
| Gender (Male as Ref.) | Female | 0.53 | 0.46 | 0.60 | <0.001 | 0.48 | 0.38 | 0.61 | <0.001 |
| SFGE classes (Robust as Ref.) | Pre-frail | 1.40 | 1.11 | 1.76 | 0.003 | 1.19 | 0.91 | 1.56 | 0.200 |
| Frail | 2.78 | 2.29 | 3.38 | <0.001 | 1.47 | 1.07 | 2.01 | 0.017 | |
| Very frail | 5.41 | 4.35 | 6.72 | <0.001 | – | – | – | – | |
| Hospitalization | OR | OR | |||||||
| Age | 1.00 | 0.98 | 1.02 | 0.550 | 1.01 | 0.98 | 1.03 | 0.300 | |
| Gender (Male as Ref.) | Female | 0.83 | 0.71 | 0.98 | 0.029 | 0.90 | 0.73 | 1.12 | 0.370 |
| SFGE classes (Robust as Ref.) | Pre-frail | 1.31 | 1.06 | 1.63 | 0.011 | 1.34 | 1.06 | 1.70 | 0.014 |
| Frail | 1.67 | 1.37 | 2.03 | <0.001 | 1.34 | 1.01 | 1.79 | 0.041 | |
| Very frail | 2.08 | 1.59 | 2.72 | <0.001 | – | – | – | ||
| Institutionalization | OR | OR | |||||||
| Age | 1.08 | 1.05 | 1.10 | <0.001 | 1.07 | 1.02 | 1.13 | 0.007 | |
| Gender (Male as Ref.) | Female | 1.44 | 1.05 | 1.96 | 0.024 | 1.54 | 0.85 | 2.79 | 0.150 |
| SFGE classes (Robust as Ref.) | Pre-frail | 3.63 | 1.97 | 6.71 | <0.001 | 3.81 | 2.00 | 7.24 | <0.001 |
| Frail | 9.52 | 5.43 | 16.70 | <0.001 | 2.39 | 1.08 | 5.28 | 0.030 | |
| Very frail | 10.62 | 5.75 | 19.59 | <0.001 | – | – | – | – | |
Note: Model 1: for people with bio-psycho-socio-economic frailty, all the sample is considered. Model 2: for people with only socio-economic frailty. Gender and SFGE classes are treated as categorical in both models. SFGE = Short Functional Geriatric Evaluation.
Fig. 1.
Survival curves of the Model which includes all the sample (A) and of the Model which excludes individuals with psychophysical impairment (B).
3.3. The predictive validity of SFGE for hospitalization and institutionalization (logistic regression analysis)
Then, the predictive property of SFGE for hospitalization during the follow-up period was studied using a binary logistic regression to evaluate the correlation of this event with frailty assessed by SFGE, adjusted for age and gender. The logistic regression allowed to stratify of the risk of hospitalization according to the SFGE classes (pre-frail: OR 1.31, 95% CI 1.06–1.63; frail: OR 1.67, 95% CI 1.37–2.03; very frail: OR 2.08, 95% CI: 1.59–2.72), showing the predictive validity of the questionnaire, that was strongly associated to the increase of hospitalization risk (Table 2 – Model 1). In this analysis, the female gender was shown to be protective against the risk of hospitalization, too. The same analysis was carried out, excluding people with any psycho-physical or functional impairment (Table 2 – Model 2). In this case, hospital admission was associated with pre-frailty (OR 1.34, 95% CI 1.06–1.70) and frailty (OR 1.34, 95% CI 1.01–1.79) but not with age and sex, showing again the predictive validity for hospitalization of socio-economic issues included in the SFGE (Table 2).
Regarding institutionalization, the logistic regression carried out with the same model (SFGE classes, age, and gender as covariates) showed again that the more frail subjects were, the higher the institutionalization risk (Table 2). Results showed an OR of 3.63 (95% CI 1.96–6.71), 9.52 (95% CI 5.42–16.70) and 10.62 (95% CI 5.75–19.59) for pre-frail, frail and very frail individuals compared with the robust ones (Table 2 – Model 1). Besides, institutionalization increased with age and was associated with the female gender. Excluding people with any psychophysical impairment, results showed a significant correlation with institutionalization; Pre-frail individuals showed an OR even higher than frail ones (OR 3.81, 95% CI 2.00–7.24 vs. OR 2.39, 95% CI 1.08–5.28). In this analysis, older age was associated with a higher risk of institutionalization, but not gender (Table 2 – Model 2). Table 3 reports the risk of negative events according to every single item of the questionnaire, assessed by multivariable analysis.
Table 3.
Death, hospitalization and institutionalization according to every single item of the SFGE questionnaire (n = 8,561).
| Variable | OR | 95% CI | |
|---|---|---|---|
| Death | |||
| Gender | Female | 0.52 | 0.45–0.62 |
| Age | >85 | 2.15 | 1.85–2.50 |
| Living arrangement | Living with relatives or paid assistant | 1.26 | 1.01–1.58 |
| Social network | Not being involved in social activities | 1.25 | 1.01–1.55 |
| Energy and motivation | Hypoactive/hyperactive | 1.21 | 1.10–1.34 |
| Functional status | Not being able to bath/shower independently | 1.63 | 1.48–1.79 |
| Physical health | Not being able to get off from the house | 1.18 | 1.07–1.30 |
| Cognitive health | Severely confused | 1.05 | 1.02–1.08 |
| Hospitalization | |||
| Gender | Female | 0.82 | 0.68–0.99 |
| Age | >85 | 1.19 | 1.00–1.42 |
| Social network | Having someone to count on | 0.60 | 0.42–0.86 |
| Care services | Not Receiving formal home care | 0.73 | 0.57–0.94 |
| Functional status | Not being able to bath/shower independently | 1.32 | 1.17–1.47 |
| Institutionalization | |||
| Age | >85 | 1.79 | 1.31–2.44 |
| Education | None/Primary School | 2.66 | 1.68–4.19 |
| Living arrangement | Alone | 2.06 | 1.39–3.06 |
| Living with relatives or paid assistant | 1.85 | 1.23–2.78 | |
| Energy and motivation | Hypoactive/Hyperactive | 1.27 | 1.05–1.53 |
| Physical health | Not being able to get off from the house | 1.81 | 1.49–2.19 |
Note: Multivariable logistic regression, all variables are categorical. All P<0.05. SFGE = Short Functional Geriatric Evaluation.
The increased risks are also observed when we compare frail individuals with pre-frail ones (see Appendix B-Supplementary Table 1).
3.4. The ROC curve
The Receiver Operating Characteristic (ROC) curve for death showed an AUC of 0.70 (95% CI 0.68–0.72; Table 4 and Supplementary Fig. 1) with sensitivity and specificity of 83.2 and 40.4 respectively for the cut-off value ≥ 1, which is the threshold between robust and pre-frail individuals. The AUC values for several negative events are reported in Supplementary Table 2. The most predictable event based on the SFGE score seems to be institutionalization, and the least one is hospitalization. The AUC was also calculated for hospitalization and institutionalization (Table 4 and Appendix B-Supplementary Figs. 2–3), and all the values obtained were statistically significant.
Table 4.
AUC by death, hospitalization and institutionalization.
| Variables | AUC | 95% CI | P |
|---|---|---|---|
| Death | 0.70 | 0.68–0.72 | <0.001 |
| Hospitalization | 0.57 | 0.54–0.59 | <0.001 |
| Institutionalization | 0.75 | 0.73–0.78 | <0.001 |
Note: AUC = area under curve.
4. Discussion
4.1. Frailty in older people
Frailty in older people is one of the most important issues of Public Health [28]. Frailty onset is associated with increased mortality [20,29], hospitalization [30] and institutionalization [31], with repercussions on the quality of life and healthcare costs. Our study showed that frailty and pre-frailty assessed by SFGE correlate with mortality, hospitalization and institutionalization in a large Italian population composed of people aged more than 75 living at home. The stratification of frailty based on SFGE is associated with a progressive increase in the risk of developing these events. Since lack of social support may also be related to frailty [32], planning interventions, including social ones [26], when frailty is in its early stages could improve outcomes. These results are similar to those obtained with the Fried frailty phenotype in a population over 65, which was predictive of hospitalization and death over 3 years [12]. In this case, frailty was considered exclusively as a clinical syndrome, although it was found to be associated with social indicators such as low levels of education and income. About institutionalization, our results also confirmed the findings of other studies, i.e., that frailty, although considered in its multiple definitions, still correlates with this condition. For example, Viljanen et al. demonstrated an association between frailty measured using the Frailty Index (FI) in a population over 64 and a higher risk of institutionalization over ten years of follow-up. Also, the FI only included items investigating psycho-physical problems [13]. The peculiarity of SFGE is the predictive validity of the social items of the questionnaire which are associated with the increase in negative outcomes.
4.2. The use of SFGE in public health
SFGE is a questionnaire predictive of mortality and hospitalization, allowing for stratification of the population according to the level of risk. The study shows the relevance of information stemming from this 10-min-questionnaire administered by phone call, which would allow the periodical administration to a large portion of older people. This approach would put frailty at the core of the assessment of care needs both at population and individual levels. Screening for frailty in the older population allows planning in advance social and health interventions [16,33] so that health and social services are not put under pressure at the same time as reducing spending. The use of health and social services increases progressively with the level of frailty, and already the pre-frail older people often resort to primary and hospital care. Morbidity and disability increase the use of these services [16,34], as well as economic non-self-sufficiency and social isolation. Biopsychosocial frailty is a synthetic indicator of care needs that allows identifying people to target with care intervention. The use of screening tools such as the SFGE questionnaire identifies prefrail and frail individuals early, directing care services and reducing the use of social and health services by preventing individual crises due to unmet needs. Thus promoting healthier aging prevents and reduces mortality, decreases access to care, and ultimately also reduces pressure on healthcare systems [34]. Intervention plans must necessarily be tailored to the care needs of older people and can be identified in the social services of town halls and daycare centers dedicated to older people, while health care services consist of home care and dedicated pathways within health care facilities. The care planning in many European Union (EU)countries is still based more on the available human and economic resources than on a scientific assessment of the population’s care needs. The SFGE allows us a first assessment of frailty and represents an innovative approach to the risk stratification. A second step should be followed to clarify in which domain is/are the need(s) for care and to implement an individual care plan to improve individuals’ quality of life and decrease the demand for institutionalization and hospitalization [35]. The provision of services is also a powerful tool to overcome health inequalities which are determinants of negative health outcomes. In fact, economic differences can increase the risk of frailty. The stratification of the risk of frailty and the strengthening of assistance and social and health services allows to act promptly on care needs, thus preventing and/or limiting the worsening of frailty, and hopefully the use of hospitals and institutes.
The COVID-19 pandemic underlined the lack of preparedness of many EU countries to take care of old people who were requested to stay at home, thereby increasing social isolation. The lack of an effective community network due to several factors, including the reduction of households’ size and increasing social isolation [36], joined with the lack of effective community care services, contributed to the death rate.
Some studies highlighted that frailty could derive from problems of a social and economic nature [37]. Our study shows the predictiveness of SFGE concerning mortality, hospitalization, and institutionalization even for older people with only socio-economic problems, probably because the SFGE questionnaire score is made up of socio-economic issues for about 40%, which is not usual in similar tools. A recent review shows that short and multidimensional questionnaires to evaluate frailty in the older population are still not very widespread and have a low percentage of socio-economic items. Instead, SFGE stands out precisely for the high percentage of social items [6,38].
4.3. Comparison by ROC
The AUC for death is comparable to the ones reported by similar tools [39], such as the Tilburg Frailty Indicator (TFI). In the very recent study published regarding the prediction of mortality of the TFI, the authors highlight how the AUC for mortality is strongly associated with the whole questionnaire but not with the single domains of the Tilburg tool [39]. It indicates the robustness of the methodology to assess frailty based on a multidimensional approach. Even if psychophysical variables did not show any impairment, the mortality rate is still proportional to frailty level. However, the best AUC value in our study is observed in the AUC for institutionalization (0.81 in males and 0.73 in females), which leads us to conclude that SFGE has good predictivity for institutionalization, acceptable predictivity for mortality (0.69 in males and 0.72 in females), and low predictivity for hospitalization (0.59 in males and 0.56 in females). The reason for the difficulty in predicting hospitalization is intrinsic in the nature of this event because it is difficult to predict due to the multiple causes (including the iatrogenic ones) that can lead to hospitalization of a frail older individual. This result is slightly lower than that obtained for the predictive validity of the TFI with regard to hospital admission, which was also mediocre [6]. The value of AUC is shown for institutionalization that is related to the combination of social and health determinants and their impact on individuals’ quality of life as well as on their care needs. These results underscore the difficulty of capturing frailty, which cannot be diagnosed as a disease. Interestingly, the pre-frail level is associated without statistical significance with mortality among people without psychophysical impairment, while it is statistically significant for hospitalization and institutionalization, showing the different impact of socio-economic frailty. Because of the characteristic of the SFGE, which is very close to a screening tool, the possibility of assessing at the same time several risks in the same indicator is strongly advisable. Moreover, the analysis of single determinants of negative outcomes always showed a multivariable pattern of determinants for all of them.
4.4. Limitations
The main study limitation is the lack of information about diseases that are not included in the questionnaire. This is mainly the choice of involving also non-health professionals to administer SFGE to a very large population, which is a key to putting frailty at the core of the care process. Various authors show that comorbidity has been put concerning mortality, hospitalization, and institutionalization [40,41], which was not possible in this case. In addition, future research will be done to compare the SFGE to other established frailty instruments because in Public Health, it is crucial to choose a questionnaire simple and quick to administer, that can be used by different professional categories even without specific training [35], as a first step to select persons who need more attention by the services. Providing a first-level frailty assessment to be offered at least once a year to millions of people over 75 years of age is the main objective. Another limitation of our study is the age of the people involved, as the sample is composed of only persons over 75. Therefore it may be useful to carry out further studies involving the younger population.
5. Conclusion
In conclusion, the SFGE has significant predictive validity for mortality, hospitalization and institutionalization, not only in older adults with frailty associated with psychophysical problems but also in socially and economically frail older adults. Therefore, multidimensional questionnaires, which are short and easy to administer even in settings as diverse as SFGE, make it possible to assess a large sample of the older adults population, to stratify them according to frailty in order to undertake tailored interventions and pathways for those most at risk and thus reduce adverse events. Future researches need to be conducted to compare frailty assessment tools with the SFGE.
Ethical statement
The research was approved by the Independent Ethical Committee of the University of Rome Tor Vergata (R.S. 60/17) and people signed a written informed consent before taking part in the study. This survey was performed in accordance with the Declaration of Helsinki.
Funding
Nothing to declare.
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
CRediT authorship contribution statement
Giuseppe Liotta: term, Conceptualization, Methodology, Formal analysis, Resources, Writing – original draft, Project administration. Grazia Lorusso: Writing – original draft. Olga Madaro: Investigation, Data curation. Valeria Formosa: Formal analysis, Writing – original draft, Visualization. Susanna Gentili: Writing – original draft. Fabio Riccardi: Supervision, Validation. Stefano Orlando: Supervision, Formal analysis. Paola Scarcella: Supervision, Validation. Leonardo Palombi: Supervision.
Declaration of competing interest
The authors have declared no conflict of interest.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.12.019.
Appendices. Supplementary data
The following are the Supplementary data to this article.
References
- 1.Istituto Nazionale di Statistica (Istat). Il Censimento permanente della popolazione e delle abitazioni. Prima diffusione dei dati definitivi 2018 e 2019. [Accessed 8 November 2021]. https://www.istat.it/it/files/2020/12/REPORT_CENSIPOP_2020.pdf.
- 2.Istituto Nazionale di Statistica (Istat) 2019. Gli anziani e la loro domanda sociale e sanitaria anno.https://www.istat.it/it/files//2021/06/rapporto_commissione_anziani.pdf [Google Scholar]
- 3.O'Caoimh R., Sezgin D., O'Donovan M.R., Molloy D.W., Clegg A., Rockwood K., et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing. 2021;50(1):96–104. doi: 10.1093/ageing/afaa219. [DOI] [PubMed] [Google Scholar]
- 4.Santos-Eggimann B., Cuénoud P., Spagnoli J., Junod J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci. 2009;64(6):675–681. doi: 10.1093/gerona/glp012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liotta G., O'Caoimh R., Gilardi F., Proietti M.G., Rocco G., Alvaro R., et al. Assessment of frailty in community-dwelling older adults residents in the Lazio region (Italy):A model to plan regional community-based services. Arch Gerontol Geriatr. 2017;68:1–7. doi: 10.1016/j.archger.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Gobbens R.J.J., van Assen M.A.L.M., Luijkx K.G., Wijnen-Sponselee M.T., Schols J.M.G.A. The Tilburg frailty indicator: psychometric properties. J Am Med Dir Assoc. 2010;11(5):344–355. doi: 10.1016/j.jamda.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 7.van Oostrom S.H., van der A.D.L., Rietman M.L., Picavet H.S.J., Lette M., Verschuren W.M.M., et al. A four-domain approach of frailty explored in the Doetinchem Cohort Study. BMC Geriatr. 2017;17(1):196. doi: 10.1186/s12877-017-0595-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scarcella P., Liotta G., Marazzi M.C., Carbini R., Palombi L. Analysis of survival in a sample of elderly patients from Ragusa, Italy on the basis of a primary care level multidimensional evaluation. Arch Gerontol Geriatr. 2005;40(2):147–156. doi: 10.1016/j.archger.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Vermeiren S., Vella-Azzopardi R., Beckwée D., Habbig A.K., Scafoglieri A., Jansen B., et al. Frailty and the prediction of negative health outcomes: a meta-analysis. J Am Med Dir Assoc. 2016;17(12) doi: 10.1016/j.jamda.2016.09.010. 1163.e1-1163.e17. [DOI] [PubMed] [Google Scholar]
- 10.Oubaya N., Dramé M., Novella J.L., Quignard E., Cunin C., Jolly D., et al. Screening for frailty in community-dwelling elderly subjects: predictive validity of the modified SEGA instrument. Arch Gerontol Geriatr. 2017;73:177–181. doi: 10.1016/j.archger.2017.07.026. [DOI] [PubMed] [Google Scholar]
- 11.Schoenborn N.L., Blackford A.L., Joshu C.E., Boyd C.M., Varadhan R. Life expectancy estimates based on comorbidities and frailty to inform preventive care. J Am Geriatr Soc. 2022;70(1):99–109. doi: 10.1111/jgs.17468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fried L.P., Tangen C.M., Walston J., Newman A.B., Hirsch C., Gottdiener J., et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 13.Viljanen A., Salminen M., Irjala K., Korhonen P., Wuorela M., Isoaho R., et al. Frailty, walking ability and self-rated health in predicting institutionalization: an 18-year follow-up study among Finnish community-dwelling older people. Aging Clin Exp Res. 2021;33(3):547–554. doi: 10.1007/s40520-020-01551-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Terracciano E., Gentili S., Madaro O., Curti E., Inzerilli M.C., Albanese L., et al. The effect of community nurse on mortality and hospi- talization in a group of over-75 older adults: a nested case-control study. Ann Ig. 2021;33(5):487–498. doi: 10.7416/ai.2020.2398. [DOI] [PubMed] [Google Scholar]
- 15.Gentili S., Emberti Gialloreti L., Riccardi F., Scarcella P., Liotta G. Predictors of emergency room access and not urgent emergency room access by the frail older adults. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.721634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Capanna A., Scarcella P., Gilardi F., Mancinelli S., Palombi L., Marazzi M.C., et al. Sensitivity and specificity of a short questionnaire to screen frailty in the community-dwelling older population. Adv Aging Res. 2018;7(3):52–63. doi: 10.4236/aar.2018.73005. [DOI] [Google Scholar]
- 17.World Health Organization World report on ageing and health. https://www.who.int/publications/i/item/9789241565042
- 18.Billot L., Corcoran K., McDonald A., Powell-Davies G., Feyer A.M. Impact evaluation of a system-wide chronic disease management program on health service utilisation: a propensity-matched cohort study. PLoS Med. 2016;13(6) doi: 10.1371/journal.pmed.1002035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.GIMBE (Gruppo Italiano per la Medicina Basata sulle Evidenze) 4° Rapporto GIMBE sulla sostenibilità del SSN. https://www.salviamo-ssn.it/attivita/rapporto/4-rapporto-gimbe.it-IT.html
- 20.Clegg A., Young J., Iliffe S., Rikkert M.O., Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi: 10.1016/s0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Faller J.W., Pereira D.D.N., de Souza S., Nampo F.K., Orlandi F.S., Matumoto S. Instruments for the detection of frailty syndrome in older adults: a systematic review. PLoS One. 2019;14(4) doi: 10.1371/journal.pone.0216166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hajek A., Bock J.O., Saum K.U., Matschinger H., Brenner H., Holleczek B., et al. Frailty and healthcare costs-longitudinal results of a prospective cohort study. Age Ageing. 2018;47(2):233–241. doi: 10.1093/ageing/afx157. [DOI] [PubMed] [Google Scholar]
- 23.Calvillo-Arbizu J., Naranjo-Hernández D., Barbarov-Rostán G., Talaminos-Barroso A., Roa-Romero L.M., Reina-Tosina J. A sensor-based mHealth platform for remote monitoring and intervention of frailty patients at home. Int J Environ Res Publ Health. 2021;18(21) doi: 10.3390/ijerph182111730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liotta G., Orfila F., Vollenbroek-Hutten M., Roller-Winsberger R., Illario M., Musian D., et al. The European innovation partnership on active and healthy ageing synergies: protocol for a prospective observational study to measure the impact of a community-based program on prevention and mitigation of frailty (ICP - PMF) in community-dwelling older adults. Transl Med UniSa. 2016;15:53–66. [PMC free article] [PubMed] [Google Scholar]
- 25.Liotta G., Inzerilli M.C., Palombi L., Bianchini A., Di Gennaro L., Madaro O., et al. Impact of social care on Hospital Admissions in a sample of community-dwelling older adults: results of a quasi-experimental study. Ann Ig. 2018;30(5):378–386. doi: 10.7416/ai.2018.2237. [DOI] [PubMed] [Google Scholar]
- 26.Liotta G., Inzerilli M.C., Palombi L., Madaro O., Orlando S., Scarcella P., et al. Social interventions to prevent heat-related mortality in the older adult in Rome, Italy: a quasi-experimental study. Int J Environ Res Publ Health. 2018;15(4):715. doi: 10.3390/ijerph15040715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grauer H., Birnbom F. A geriatric functional rating scale to determine the need for institutional care. J Am Geriatr Soc. 1975;23(10):472–476. doi: 10.1111/j.1532-5415.1975.tb00933.x. [DOI] [PubMed] [Google Scholar]
- 28.Liotta G., Ussai S., Illario M., O'Caoimh R., Cano A., Holland C., et al. Frailty as the future core business of public health: report of the activities of the A3 action group of the European innovation partnership on active and healthy ageing (EIP on AHA) Int J Environ Res Publ Health. 2018;15(12):2843. doi: 10.3390/ijerph15122843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zaslavsky O., Zelber-Sagi S., Gray S.L., LaCroix A.Z., Brunner R.L., Wallace R.B., et al. Comparison of frailty phenotypes for prediction of mortality, incident falls, and hip fracture in older women. J Am Geriatr Soc. 2016;64(9):1858–1862. doi: 10.1111/jgs.14233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gilardi F., Scarcella P., Proietti M.G., Capobianco G., Rocco G., Capanna A., et al. Frailty as a predictor of mortality and hospital services use in older adults: a cluster analysis in a cohort study. Eur J Publ Health. 2018;28(5):842–846. doi: 10.1093/eurpub/cky006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rockwood K., Song X.W., MacKnight C., Bergman H., Hogan D.B., McDowell I., et al. A global clinical measure of fitness and frailty in elderly people. CMAJ (Can Med Assoc J) 2005;173(5):489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anantapong K., Wiwattanaworaset P., Sriplung H. Association between social support and frailty among older people with depressive disorders. Clin Gerontol. 2020;43(4):400–410. doi: 10.1080/07317115.2020.1728002. [DOI] [PubMed] [Google Scholar]
- 33.Cesari M., Prince M., Thiyagarajan J.A., De Carvalho I.A., Bernabei R., Chan P., et al. Frailty: an emerging public health priority. J Am Med Dir Assoc. 2016;17(3):188–192. doi: 10.1016/j.jamda.2015.12.016. [DOI] [PubMed] [Google Scholar]
- 34.Ilinca S., Calciolari S. The patterns of health care utilization by elderly Europeans: frailty and its implications for health systems. Health Serv Res. 2015;50(1):305–320. doi: 10.1111/1475-6773.12211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eurostat. Household composition statistics. [Accessed 20 March 2022]. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Household_composition_statistics#Increasing_number_of_households_consisting_of_adults_living_alone.
- 36.Sirven N., Dumontet M., Rapp T. The dynamics of frailty and change in socio-economic conditions: evidence for the 65+ in Europe. Eur J Publ Health. 2020;30(4):715–719. doi: 10.1093/eurpub/ckaa068. [DOI] [PubMed] [Google Scholar]
- 37.Formosa V, Lorusso G, Lentini G, Terracciano E, Gentili S, Liotta G. Multidimensional Short Tools to assess frailty: a narrative review. Ann Ig 2023;35(1):21-33. 10.7416/ai.2022.2516. [DOI] [PubMed]
- 38.Gobbens R.J.J., van Assen M.A.L.M., Augustijn H., Goumans M., van der Ploeg T. Prediction of mortality by the Tilburg frailty indicator (TFI) J Am Med Dir Assoc. 2021;22(3) doi: 10.1016/j.jamda.2020.07.033. 607.e1-607.e6. [DOI] [PubMed] [Google Scholar]
- 39.Liotta G., Madaro O., Scarcella P., Inzerilli M.C., Frattini B., Riccardi F., et al. Assessing the impact of A community-based pro-active monitoring program addressing the need for care of community-dwelling citizens aged more than 80:protocol for a prospective pragmatic trial and results of the baseline assessment. Transl Med UniSa. 2020;23:22–27. doi: 10.37825/2239-9747.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yarnall A.J., Sayer A.A., Clegg A., Rockwood K., Parker S., Hindle J.V. New horizons in multimorbidity in older adults. Age Ageing. 2017;46(6):882–888. doi: 10.1093/ageing/afx150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bottle A., Kim D., Hayhoe B., Majeed A., Aylin P., Clegg A., et al. Frailty and co-morbidity predict first hospitalisation after heart failure diagnosis in primary care: population-based observational study in England. Age Ageing. 2019;48(3):347–354. doi: 10.1093/ageing/afy194. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.