Abstract
Introduction and importance
Impalement thoracoabdominal injuries are potentially life-threatening due to the associated bleeding and multiple visceral injuries. They are uncommon and often result in severe surgical complications, requiring prompt treatment and extensive care.
Case presentation
We present a 45-year-old male patient who fell from a 4.5-meter-high tree and landed on a Schulman iron rod stick, which pierced the patient's right midaxillary line, exiting from his epigastric region and leading to multiple intraabdominal injuries and right pneumothorax. The patient was resuscitated and immediately shifted to the operating theater. The main operative findings were moderate hemoperitoneum, gastric and jejunum perforations, and liver laceration. A right chest tube was inserted, and injuries were repaired with segmental resection, anastomosis, and colostomy procedure with uneventful post-operative recovery.
Clinical discussion
Providing efficient and prompt care is crucial for patient survival. This includes securing the airways, providing cardiopulmonary resuscitation, and aggressive shock therapy to stabilize the patient's hemodynamic status. The removal of impaled objects is strongly discouraged outside the operation theater.
Conclusion
Thoracoabdominal impalement injury is rarely reported in the literature; appropriate resuscitative care, prompt diagnosis, and early surgical intervention may minimize mortality and improve the patient's outcomes.
Keywords: Thoracoabdominal impalement injury, Rod injury, Case report
Highlights
-
•
Thoracoabdominal impalement injuries are a rare occurrence.
-
•
Progressive dyspnea is an important symptom in patients with penetrating chest injuries.
-
•
For penetrating trauma, resuscitative care, avoiding removal of penetrating objects, and early surgical intervention may minimize mortality.
1. Introduction
Impalement injuries are typically triggered by large blunt objects made of wood or metal. Such damages are most commonly seen in work-related or road accidents, which are more prevalent among adults [1]. Based on the mechanism, traumatic injuries are classified as either penetrating or blunt. The formers are categorized as stab wounds and gunshot wounds [2]. Impalement injuries are uncommon, with only a few cases documented in the medical literature [1], [3], [4]. Based on the available literature, managing these injuries is debatable, owing to the limited number of cases and the problematic surgical attitude [5], [6]. Here, we present a 45-year-old male patient with impalement thoracoabdominal injuries caused due to a fall from a tree on a Schulman iron rod. A senior general surgeon performed the surgery in a teaching university hospital (Al-Thora General Hospital, Ibb University, Ibb, Yemen). This case report has been reported in line with the SCARE Criteria [7].
2. Presentation of the case
2.1. Patient Information
A 45-year-old man presented to our emergency department in Al-Thora General Hospital, Ibb, Yemen, after 1 h of falling approximately 4.5 m from a tree and landing on a Schulman iron rod in June 2021 (Fig. 1).
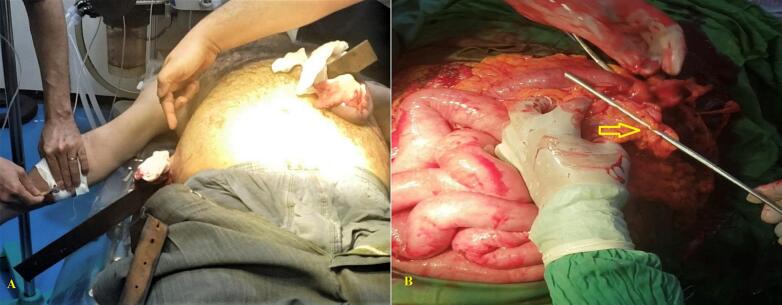
Fig. 1.

Photo showing the entry and exiting points of the penetrating Schulman iron rod.
The iron rod penetrated the patient from his right midaxillary line, exiting from his epigastric region and leading to multiple impalement injuries and minor damage to the right pleural space (right pneumothorax). At the exiting end, there was minimal bleeding and green, foul-smelling peritoneal contents. No attempts were made to remove the impaled rods to prevent further penetration of the rod inside the patient's abdominal cavity.
2.2. Clinical findings
Upon presentation, the patient was fully alert (GCS 14), and although his airway was intact, his breathing was difficult. The initial vital signs showed oxygen saturation of 88 % on room air, blood pressure: of 90/60 mm Hg, and heart rate of 90 beats/min. Reduced lung sounds were auscultated in the right lung. Abdominal examination revealed a tender abdomen with rigidity and guarding. The neurological examination was unremarkable, and the cervical collar was used to stabilize the cervical spine, which was indicated due to the concomitant distracting injury. Urinary catheterization with a 16 Fr catheter revealed 150 mL of gross clear urine.
2.3. Diagnostic assessment
Focused Assessment with Sonography in Trauma (FAST) scan showed moderate free fluid in the abdomen. Plain chest and abdominal radiography X-ray showed a right pneumothorax. A chest tube was inserted in the 5th intercostal space air bubble and noted an underwater seal with no bleeding. No further radiologic evaluation was performed, such as computed tomography (CT) scan.
2.4. Therapeutic interventions
Fluid resuscitation (2000 cc normal saline) via two wide-bore intravenous catheters, prophylactic antibiotics (Ceftriaxone 1 g and Metronidazole 500 mg intravenously), and tetanus vaccination prophylaxis were performed immediately. The iron rod was carefully cut using a rod cutter to facilitate his transfer to the operating room. Then, the patient was urgently transferred to the operating room after obtaining a consent. After general anesthesia with a supine position, the laparotomy was performed via a midline incision. Intraoperatively, an approximately 120-cm-long iron rod remained impaled in the body (Fig. 2A). The object caused a 2 cm gastric injury in length, transecting jejunum 35 cm from the duodenojejunal flexure [American Association for Surgery in Trauma (AAST- OIS Grade 5)], the right lobe of the liver was lacerated 2 cm depth [2]. Gastrointestinal (GI) contents spillage was noticed with a moderate hematoperitoneum with no vascular injury (Fig. 2B). An iron rod was retrieved and cautiously dissected from the damaged intra-abdominal structures. Then, the liver lacerations were repaired with Z-suturing using a 2-0 polydioxanone suture (PDS). Using a two-layered suturing, inner polyglactin, and outer silk, the gastric perforation was closed, and the jejunal perforation was repaired with resection and end-to-end jejunal anastomosis. Colostomy diverted at the right upper quadrant. Abdominal lavage was performed extensively with a two-liter of normal saline, and surgical drains were positioned in the subhepatic spaces bilaterally. The estimated blood loss was approximately 1000 mL. Intraoperatively, the patient had a brief episode of hypotension, which completely resolved with crystalloid and one unit of packed red blood transfusion. A senior general surgeon performed all surgical procedures.
Fig. 2.
Intraoperative photos.
A; Showing the entry and exiting points of the penetrating Schulman iron rod.
B; Showing the bowel perforation (arrow).
2.5. Follow-up and outcome
The patient was placed in the Intensive Care Unit (ICU) post-operatively. Based on the critical care and infectious disease team suggestions, broad-spectrum intravenous antibiotics were initiated, including; Meropenem (500 mg every 8 h) and clindamycin (300 mg every 6 h), given the severity of the injury and possible associated viscus contamination. On the 3rd day postoperatively, the patient was transferred to the surgical ward. On the 4th day post-operatively, a superficial surgical wound infection was noted and was managed by local dressings and topical antibiotics (Mupirocin). The chest tube was removed on the 5th postoperative day. A psychiatric assessment for post-traumatic stress disorder did not reveal any abnormality. The patient was released from the hospital after nine days and recuperated well with no neurological or functional abnormalities one month later. The one-month CT scan after surgery revealed a normal appearance with a minor right pneumothorax. The colostomy closure was performed after three months without complications. Within one year of follow-up, no signs of gastrointestinal problems.
3. Discussion
Penetrating thoracoabdominal injuries have been reported in the literature on occasion [1], [3], [4]. Several authors have reported penetration of various objects made of wood or metal, such as glass, knives, wooden blocks, blades, and so on [6], [8]. We encountered penetration of Schulman iron rod, penetrating the abdomen and thorax and causing multiple organ damage; such cases are rarely reported in the literature [9].
Most impalement injuries occur in automobile collisions, primarily at construction locations. In addition, these injuries can be seen with falls and sexually driven behaviors in the anogenital area [10]. According to a separate categorization, type 1 injuries occur when a body collides with object items (such as in construction site falls or car ejections), as seen in this case. In contrast, type 2 injuries occur when a moving object penetrates a standing body (e.g., an object enters a vehicle cabin) [2], [10].
The severity of penetrative thoracoabdominal injuries depends on the extent of blood loss and the concomitant organ damage, which can vary from minor to life-threatening injuries [3].
Providing efficient and prompt care is crucial for patient survival. This includes securing the airways, providing cardiopulmonary resuscitation, and aggressive shock therapy to stabilize the patient's hemodynamic status [1]. Furthermore, the trauma mechanism, severity, and concomitant injuries should be evaluated [5], including hemothorax and/or pneumothorax that may necessitate the placement of a thoracic drain, as was done in our patient [6].
In the presence of hypovolemia, adrenaline or inotropes are not recommended in early management stage. However, inotropes may be provided after fluid therapy and blood transfusion for refractory cases [11].
These injuries are difficult to manage due to their severity and concomitant hemodynamic instability, requiring multi-disciplinary care in a tertiary referral facility [6], [12], [13]. Due to the likelihood of serious organ and vascular damage impairing the normal physiology of breathing and circulation, adequate resuscitation and continuous monitoring are essential pre- and intra-optatively [9], [14]. However, the patient's condition limited us to transfer them to a tertiary referral center, and a general surgeon performed all management.
Radiologic investigations should be demanded depending on the medical findings and patient stability and must be restricted to those necessary for surgical planning [15]. We did not perform more radiologic investigations, such as CT scans, because the patient's condition was unstable and necessitated urgent exploration.
The removal of impaled objects is strongly discouraged outside the operation theater (OT) settings, as it occasionally serves as a buffer that prevents blood exsanguination [12]. Nevertheless, if the object is too long and obstructs the patient's transport, it can be cut short. A hydraulic pedal cutter is typically used in cases of metal impalement injury to minimize secondary damage caused by vibration [16]. In our patient, the iron rod was long and limited us from moving the patient. For that, it was first shortened then the patient was transferred to the OT.
The administration of broad-spectrum intravenous antibiotics and the tetanus vaccine is essential, given the high contamination risk associated with penetrative abdominal injuries, as was done in our patient [3], [8]. If not given preoperatively, tetanus prophylaxis must be administered post-operatively.
The prognosis is dictated by the location of the laceration, the extent of organ damage, and the presence of pollution [6]. The surgical approach should permit adequate exposure into the involved structures to allow vascular control and comprehensive anatomical identification along the route of the invading item and facilitate the removal, debridement, and reconstruction under direct visualization. Consequently, non-standard or non-conventional incisions may be necessary [14].
Impalement injuries are classically requiring immense force to be generated. Thus, structures routes traveled by the impaled item must also be assessed [4]. The impaled object should not be withdrawn until extensive examination, and vascular control have been performed. Organ-specific injuries must be treated according to the established individual trauma standards [17]. It is necessary to undertake a thorough debridement, including the lavage of wounds and structures along the object's course. Drains should often be used when there is severe contamination and a delayed primary or secondary intention is adequate, usually for wound closure, as was done in our patient [6].
Patients who survive severe injuries are at risk suffer from post-traumatic stress disorders and may need psychotherapy after surgery [4]. Our patient's surgical recovery was uncomplicated, except for a minor skin infection that was treated with an antibiotic ointment. In addition, we conducted a psychological evaluation which was unremarkable.
4. Conclusion
Thoracoabdominal impalement injuries are rarely reported in the literature. Providing immediate resuscitative care, a correct diagnosis, and appropriate surgical intervention may reduce mortality rates and improve patient outcomes.
Patient perspective
Throughout his course of treatment, the patient expressed satisfaction with the care he received.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Not required.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Guarantor
Faisal Ahmed is the guarantor of the work and accepts full responsibility.
Research registration number
N/a.
CRediT authorship contribution statement
Study concept and design: Menawar Dajenah and Faisal Ahmed
Data collection: Zaid Dajenah
Writing of paper: Anessa Thabet, and Faisal Ahmed
Critical revision for intellectual content: Khaled Ghaleb, Mohamed Badheeb, and Faisal Ahmed.
Declaration of competing interest
None of the authors have any conflict of interest to declare.
Acknowledgements
We appreciate our patient for his cooperation and allowing us to present his case for scientific community.
References
- 1.Kaur K., Singhal S.K., Bhardwaj M., Kumar P. Penetrating abdomino-thoracic injury with an iron rod: An anaesthetic challenge. Indian J Anaesth. 2014;58:742–745. doi: 10.4103/0019-5049.147172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ugoletti L., Zizzo M., Castro Ruiz C., Pavesi E., Biolchini F., Annessi V. Gluteal, abdominal, and thoracic multiple impalement injuries: A case report on management of a complex polytrauma. Medicine (Baltimore) 2019;98 doi: 10.1097/MD.0000000000015824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alsabek M.B., Badi M.N., Khatab M. Multiple impalement injuries of the torso with two metal bars: A case report. Ann Med Surg (Lond). 2021;63 doi: 10.1016/j.amsu.2021.102179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohan R., Ram D.U., Baba Y.S., Shetty A., Bhandary S. Transabdominal impalement: absence of visceral or vascular injury a rare possibility. J. Emerg. Med. 2011;41:495–498. doi: 10.1016/j.jemermed.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 5.Sankpal J., Rahul K., Phadke A., Sankpal S. Thoraco-abdominal impalement injury with two construction iron bars - A rare case report. Int J Surg Case Rep. 2020;67:80–81. doi: 10.1016/j.ijscr.2020.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eder F., Meyer F., Huth C., Halloul Z., Lippert H. Penetrating abdomino-thoracic injuries: report of four impressive, spectacular and representative cases as well as their challenging surgical management. Pol. Przegl. Chir. 2011;83:117–122. doi: 10.2478/v10035-011-0019-3. [DOI] [PubMed] [Google Scholar]
- 7.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 8.Barbois S., Abba J., Guigard S., Quesada J.L., Pirvu A., Waroquet P.A., et al. Management of penetrating abdominal and thoraco-abdominal wounds: A retrospective study of 186 patients. J Visc Surg. 2016;153:69–78. doi: 10.1016/j.jviscsurg.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Muhammad Afzal R., Armughan M., Javed M.W., Rizvi U.A., Naseem S. Thoracic impalement injury: a survivor with large metallic object in-situ. Chin. J. Traumatol. 2018;21:369–372. doi: 10.1016/j.cjtee.2018.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byard R.W. A forensic evaluation of impalement injuries. Med Sci Law. 2018;58:85–92. doi: 10.1177/0025802418755588. [DOI] [PubMed] [Google Scholar]
- 11.Shah H., Tiwari C., Jayaswal S., Murthy K. An unusual case of transorificial abdomino-thoracic impalement injury in a child. Bull. Emerg.Trauma. 2016;4:236–239. [PMC free article] [PubMed] [Google Scholar]
- 12.Ruano R.M., Pereira B.M., Biazzoto G., Bortoto J.B., Fraga G.P. Management of severe thoracic impalement trauma against two-wheeled horse carriage: a case report and literature review. Indian J. Surg. 2014;76:297–302. doi: 10.1007/s12262-013-0825-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pau L., Navez J., Cawich S.O., Dapri G. Laparoscopic Management of Blunt and Penetrating Abdominal Trauma: a single-center experience and review of the literature. J Laparoendosc Adv Surg Tech A. 2021;31:1262–1268. doi: 10.1089/lap.2020.0552. [DOI] [PubMed] [Google Scholar]
- 14.Sankpal J., Rahul K., Phadke A., Sankpal S. Thoraco-abdominal impalement injury with two construction ironbars - A rare case report.Int J Surg Case Rep. 2020;68:274–276. doi: 10.1016/j.ijscr.2020.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Govindaraju R.C., Munavalli J. Difficulties in the Management of Impalement Injuries Sustained in rural India. J emerg traumaShock. 2020;13:227–230. doi: 10.4103/JETS.JETS_163_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jawaid S., Cody D. Crowbar impalement: the PHEM perspective. BMJ Case Rep. 2018:11. doi: 10.1136/bcr-2018-227293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ketterhagen J.P., Wassermann D.H. Impalement injuries: the preferred approach. J. Trauma. 1983;23:258–259. [PubMed] [Google Scholar]