Summary
Background
Refugee children may be under-immunised against common vaccine-preventable diseases due to a myriad of factors related to their migration journey.
Methods
This retrospective cohort study explored the rates and determinants of enrolment on the National Immunisation Register (NIR) and measles, mumps and rubella (MMR) coverage among refugee children up to 18 years old who resettled in Aotearoa New Zealand (NZ) from 2006 to 2013. Univariate and multivariable logistic regression were conducted to determine associations.
Findings
Of the cohort (N = 2796), two thirds of the children (69%) were enrolled on the NIR. Among this sub-cohort (n = 1926), less than one third (30%) were age-appropriately vaccinated with MMR. MMR coverage was highest among younger children and improved over time. Logistic modelling revealed that visa category, year of arrival, and age group were significant factors that influenced NIR enrolment and MMR vaccine uptake. Those arriving via asylum seeking, family reunification and humanitarian pathways were less likely to be enrolled and vaccinated compared to refugees who entered under the national quota programme. More recent arrivals and younger children were more likely to be enrolled and vaccinated compared to children who arrived in NZ longer ago and were older.
Interpretation
Resettled refugee children have suboptimal NIR enrolment and MMR coverage rates which varied significantly by visa category, highlighting the need for immunisation services to better engage with all refugee families. These findings suggest that broad structural factors related to policy and immunisation service delivery may influence the differentials seen.
Funding
Health Research Council of New Zealand (18/586).
Keywords: Immunisation, Vaccine, Equity, Child, Data-linking, Refugee, New Zealand
Research in context.
Evidence before this study
We have conducted two scoping reviews of international literature to understand the burden of vaccine-preventable diseases (VPDs), immunisation coverage, and interventions to reduce VPD burden among migrants and refugees. The available evidence suggests that migrant populations generally experience higher VPD burden and lower immunisation rates compared to their host populations due to a myriad of factors. Our previous research in Aotearoa New Zealand (NZ) reported that more than half of overseas-born children with a migrant or refugee background (54%) were not enrolled on the National Immunisation Register (NIR). Of those enrolled on the NIR, they had lower reported age-appropriate vaccination rates by vaccine of interest, ethnicity and visa category compared to NZ-born children. Overseas-born children with refugee backgrounds who resettled in NZ had particularly low age-appropriate vaccination coverage rates, warranting further study into coverage rates and associated factors.
Added value of this study
Our study of measles, mumps and rubella (MMR) vaccine coverage in NZ from 2006 to 2013 provides population-level insights about vaccine uptake among overseas-born children of refugee backgrounds. Among the study cohort (N = 2796), two thirds of children (69%) were enrolled on the NIR. Of those children who were enrolled on the NIR, only 30% were age-appropriately vaccinated with MMR. However, protection was highest for younger children and had improved over time. Among this sub-cohort of children based on age group, 89% (258/291) of 0–<2 year olds, 47% (240/516) of 2–<6 year olds, and 8% (66/843) of 6–<19 years old were age-appropriately vaccinated against measles. This study explored the influence of numerous factors on NIR enrolment and coverage rates, including visa category, age, arrival year, United Nations region of nationality, ethnicity, number of dependent children, household income, parent's level of education, family type, and parent's ability to converse in English. This study showed that register enrolment and MMR coverage were significantly associated with visa category, year of arrival and age group.
Implications of all the available evidence
Despite a publicly funded national childhood schedule and comprehensive immunisation targets, this study demonstrates suboptimal register enrolment and MMR coverage among overseas-born refugee children. Whilst immunisation services have improved over time, there is still room for improvement with enrolment of refugees, particularly for older children and adolescents. The significant association of refugee visa category with both register enrolment and MMR coverage clearly demonstrate that policy- and service-level factors influence vaccine uptake among overseas-born children more than individual or family characteristics. Minimising epidemic risk in NZ requires engagement with all families with migrant and refugee backgrounds upon their arrival to ensure their health and immunisation needs are addressed. To meet the objectives of the World Health Organisation's new Immunisation Agenda 2030, tailored and targeted interventions to improve equitable access to vaccines for refugee children, particularly for older children and adolescents, are required.
Introduction
The number of refugees fleeing their homes has considerably increased over recent years due to ongoing conflict and political persecution.1 Disparities in vaccine-preventable disease (VPD) burden and immunisation coverage between migrants and refugees and their host populations have been reported globally.2 For instance, a review reported that migrants in Europe have been involved in VPD outbreaks with varying vulnerability based on disease, setting, and demographics.3 Moreover, a recent retrospective cross-sectional study of UK-bound refugees revealed suboptimal vaccination coverage that varied by age, nationality, country of health assessment, and by disease.4 A scoping review revealed that a complex myriad of factors influenced these inequities among migrants and refugees, including their nativity, country of origin, citizenship status, duration of residence, and language proficiency, to name a few.2 A recent systematic review further investigated the relative contribution of these factors on suboptimal vaccine uptake among migrants in Europe and identified 23 significant determinants, including geographic origin, recent migration, income, and being a refugee or asylum seeker.5
The World Health Organisation's new Immunisation Agenda 2030 (IA2030) sets out a global vision and strategic priorities for vaccines and immunisations.6 Underpinning the IA2030's strategy is “to leave no one behind” and recommends that migrants and other marginalised groups have equitable access to immunisation services.6 To meet the IA2030's vision, it is imperative that national immunisation policies and programmes are strengthened to better include the needs of migrants and refugees, particularly with improving access to catch-up vaccines across the life course.6
While a refugee is encompassed within the umbrella ‘migrant’ term as being a person who has left their country of origin, by definition, a refugee has been forced to flee their home because of a well-founded fear of persecution.7 There are three main pathways in which refugees arrive in Aotearoa New Zealand (NZ), including via the United Nations High Commissioner for Refugees (UNHCR)-mandated government-supported quota programme (quota refugees), the refugee family support category (family reunification refugees), or the refugee and protection status category (asylum seekers, who are then known as convention refugees if their claim is successful).8 NZ has a long-standing history of accepting refugees with recent increases in annual quotas up to 1500 quota refugees and 600 sponsored family members.8, 9, 10 Every year, approximately 300 claims for refugee status from asylum seekers are received with about a third to half of these being approved.9
In NZ, all children under the age of 18 years old are eligible to receive a series of publicly funded vaccinations according to the National Immunisation Schedule (NIS), regardless of their immigration and citizenship status.11 The newly designed national Health System Indicators aim for 92% of children being fully immunised by 24 months of age.12 Despite this target, national childhood immunisation coverage rates are suboptimal with marked inequities by ethnicity and geographic region.13 Moreover, the magnitude and global scale of disruption to routine immunisation services during the COVID-19 pandemic highlights the urgent need to improve immunisation coverage to prevent the resurgence of VPDs.14 Recent NZ data shows that fully immunised children aged 24 months old dropped from 91% before the pandemic (reporting period April 2019 to March 2020) to 84.4% (April 2021 to March 2022).13 The 2019/2020 measles outbreak in NZ and surrounding Pacific islands demonstrated the importance of achieving high immunisation coverage required to maintain herd immunity.15,16
National coverage rates may mask immunisation inequities among population sub-groups. A retrospective cohort study of migrant and non-migrant children reported relatively low coverage rates among migrant children, particularly those with refugee backgrounds.17 One of the health and wellbeing outcomes of NZ's Refugee Resettlement Strategy (RRS) is to increase the proportion of quota refugee children receiving age-appropriate immunisations.18 Data reports that the percent of quota refugee children receiving one or more schedules vaccines within 12 months of arrival has increased from 86% in 2015/16 to 99% in 2017/18.18 While this demonstrates high vaccine uptake that has improved over time, this data only represents quota refugee children and does not specify which vaccine(s) were received. Moreover, it is not currently known if refugee children entering NZ via different pathways adhere to catch-up immunisation schedules and sustain age-appropriate vaccinations post-resettlement. If we are to meet the goals of WHO's IA2030 from an equity perspective, it is imperative to investigate vaccine uptake among refugee children to inform improvements to immunisation programmes and to minimise epidemic risk in NZ. The presented retrospective cohort study explored factors influencing enrolment on the National Immunisation Register (NIR) and measles, mumps and rubella (MMR) coverage among overseas-born children of refugee backgrounds who resettled in NZ.
Methods
This study is part of a larger multimethod study19 comprising of a programme of quantitative and qualitative studies to explore factors associated with the access and uptake of immunisations and develop strategies to improve age-appropriate vaccinations among refugee children post-resettlement in NZ. Ethical approval to conduct this study was granted by the Auckland University of Technology Ethics Committee (AUTEC, ref: 18/322).
Study design and population
This retrospective cohort study focused on a cohort of children born overseas who arrived in NZ on a refugee visa prior to their 18th birthday from 1 January 2006 to 31 December 2018. These children were identified by selecting all individuals with a birth date between 1 January 1989 and 31 December 2018 whose first travel record was an arrival to NZ on a refugee (quota, convention, or family reunification), humanitarian, or overstayer visa. The humanitarian visa category primarily included visas related to asylum seekers, ministerial directions, and victims of domestic violence and human trafficking. The overstayer category refers to those who stayed in NZ after their visa expired and applied for a temporary or resident visa under Section 61 of the Immigration Act.20
Children were excluded if they stayed in NZ less than six months, died, opted off the NIR and/or had logical data inconsistencies (e.g., a birth date occurring after a travel date). To enable the use of variables associated with VPD burden and immunisation uptake among migrants and refugees, such as household income and language proficiency,2,5 children without data available in the 2013 Census were subsequently excluded.
Sources of data and variables
De-identified data were linked from multiple sources using Statistics New Zealand's Integrated Data Infrastructure (IDI). Data included were: Ministry of Health's National Health Index (NHI) for demographic data; Statistic New Zealand's Census 2013 for demographic data; Ministry of Business, Innovation and Employment (MBIE) and New Zealand Customs Journey datasets for immigration and travel data; Department of Internal Affairs for life event data; and the National Immunisation Register (NIR) for immunisation data. Refugee children who enter under the quota programme complete an orientation and health screening programme at the Mangere Refugee Resettlement Centre in which documented vaccination status is assessed and serology is undertaken to assess immunity for certain VPDs, including hepatitis B, rubella and measles; age-appropriate vaccines are offered to start any required catch-up immunisation schedule to align with the NIS.21,22 Quota refugees are also screened for tuberculosis.21,22 Refugee children who arrive from overseas via other pathways should have their documented history of vaccination assessed when they engage with a general practice to determine their immunisation catch-up schedule.11
Variables used or investigated included: month and year of birth, month and year of death (if applicable), sex, ethnicity, nationality (i.e., the country that issued their passport), visa category, time spent in NZ, number of dependent children, household income, parent's education level, family type, and parent's ability to converse in English. If an individual had multiple nationalities, the earliest recorded nationality was reported. Ethnicity was self-reported by parents and based on that recorded in the NHI dataset (as it provides more detail) and grouped according to Statistics New Zealand Level 1 ethnicity classifications.
The two outcome variables were enrolment on the NIR (yes/no) and MMR vaccination status (fully vaccinated or not for their age at the end of the study period). MMR was chosen since it is one of the most infectious VPDs and achieving high herd immunity is particularly important to prevent measles transmission.11 Previous NZ research noted that coverage amongst children with and without a migrant or refugee background was highest for MMR and pertussis-containing vaccines.17 Focusing on MMR coverage is important given the widespread misinformation about the link with autism and implications for vaccine uptake,23 particularly amongst certain refugee background communities (e.g., Somali Minnesotan community).24 To support our findings about MMR coverage, we also included supplementary descriptive analyses of children's pertussis-containing vaccination status.
Data linking and statistical analyses
A NHI number is allocated to overseas-born individuals the first time they access any health or disability support services in NZ. NHI numbers enabled deterministic linkage across health-related data sources. Linking the NIR with the NHI dataset was done using the encrypted NHI index (snz_moh_uid). Data that did not have a standard identifier, such as immigration and travel data, were linked to the health datasets and life events datasets using probabilistic linking originally by Statistics New Zealand, who assigned an encrypted identifier that was then used in this study (snz_uid) to link the data. The June 2020 refresh version of the IDI was used, noting that the NIR data within this dataset included all NIR registrations up to June 2019.
The cohort is described using counts and percentages, summarised according to each variable of interest and outcome variables. To explore MMR vaccine coverage, the recorded vaccination rates based on the child's age at the end of the study period are presented. Univariate logistic regression was conducted to determine associations between enrolment on the NIR and MMR vaccination status, and the included variables of interest. To identify significant associations, multivariable logistic regression was subsequently undertaken and presented. A p-value of <0.05 was considered significant. 95% confidence intervals for proportions are presented. Unadjusted and adjusted odds ratios (OR) are also presented. All analyses were performed using SAS.
Role of funding source
This work was supported by a grant from the Health Research Council of New Zealand (18/586). The funder had no role in the study design, collection and interpretation of the data, or the decision to submit the manuscript for publication. The authors are solely responsible for final content and interpretation. The authors received no financial support or other form of compensation related to the development of the manuscript.
Results
Description of cohort
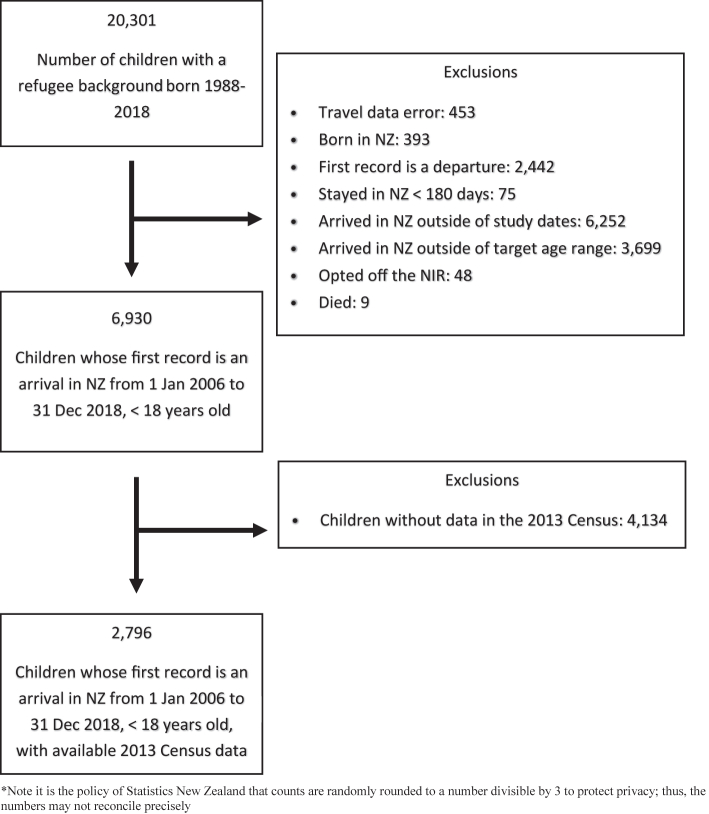
Fig. 1 shows the number of children included in the cohort after applying exclusions (N = 2796). Of the study population, the majority were quota refugees (n = 1815, 65%), followed by humanitarian (n = 504, 18%), convention refugees (n = 213, 8%), overstayers (people who overstayed their visa) (n = 150, 5%), and family reunification (n = 117, 4%). Just under half of the children were between six and under 14 years old (n = 1329, 48%) when they arrived in NZ. A relatively stable number of children arrived each year (noting limited data available for 2013 when the Census was conducted). Just over half of the children were of Asian (n = 1512, 54%) ethnicity and one third were of Middle Eastern, Latin American, or African (MELAA) ethnicity (n = 936, 33%). Accordingly, most children came from Asia (n = 1704, 61%) and African (n = 456, 16%) UN Regions. More specifically, children arrived from Myanmar (n = 681, 24%), Bhutan (n = 198, 7%), Afghanistan (n = 192, 7%), and Iraq (n = 174, 6%). Nearly half of the parents had an education qualification (n = 1269, 45%), more than half could converse in English (n = 1611, 58%), and two thirds represented low and medium household income brackets (n = 1848, 66%).
Fig. 1.
Participant flow chart with exclusions∗.
Enrolment on the National Immunisation Register
Almost two thirds of children (n = 1926, 69%) were enrolled on the NIR (Table 1). Of the different visa categories, children who arrived via the quota refugee pathway had the highest rates for being enrolled in the NIR (n = 1317, 73%) and the rest of the categories had similar rates (ranging from 59% to 62%). There was a decrease in the proportion of children who were on the NIR as age increased. For instance, most of the children under 2 years old were on the NIR (n = 291, 97%) compared to less than half of the children between 14 and under 19 years old (n = 276, 46%). The proportion of children enrolled in the NIR generally increased as arrival year increased, although noting particularly low rates in 2006 as the NIR first began recording information on children in 200511,25 and in 2013 when the Census data was collected. Among the ethnicities, almost three quarters of children of Asian (n = 1083, 72%) and MELAA (n = 630, 67%) ethnicities were enrolled on the NIR.
Table 1.
Demographic characteristics and enrolment on the National Immunisation Register of cohort of overseas-born refugee children (N = 2796) and age-appropriate measles, mumps and rubella vaccination status among a sub-cohort of children on the NIR (n = 1923).
| In the NIRa |
Total N | MMRb vaccination |
Total n | |
|---|---|---|---|---|
| Yesc (%) | Fully vaccinatedd, e (%) | |||
| Total number in the cohort | 1926 (69) | 2796 | 573 (30) | 1923 |
| Visa category | ||||
| Convention refugee | 132 (62) | 213 | 27 (21) | 132 |
| Family reunification | 69 (59) | 117 | 21 (30) | 69 |
| Humanitarian | 315 (63) | 504 | 66 (21) | 312 |
| Overstayer | 96 (64) | 150 | 36 (38) | 96 |
| Quota refugee | 1317 (73) | 1815 | 426 (32) | 1317 |
| Age group at arrival | ||||
| 0–<2 years | 291 (97) | 300 | 258 (89) | 291 |
| 2–<6 years | 513 (91) | 561 | 240 (47) | 516 |
| 6–<14 years | 843 (63) | 1329 | 66 (8) | 843 |
| 14–<19 years | 276 (46) | 606 | Added to 6–<14 years due to low numbers | |
| Arrival year | ||||
| 2006 | 243 (70) | 345 | 36 (15) | 243 |
| 2007 | 270 (63) | 432 | 57 (21) | 270 |
| 2008 | 291 (65) | 447 | 60 (20) | 294 |
| 2009 | 276 (69) | 402 | 87 (31) | 279 |
| 2010 | 234 (67) | 348 | 75 (32) | 234 |
| 2011 | 246 (77) | 321 | 84 (34) | 246 |
| 2012 | 300 (72) | 417 | 138 (46) | 300 |
| 2013 | 48 (76) | 63 | 24 (50) | 48 |
| United nations region | ||||
| Africa | 294 (65) | 456 | 72 (25) | 294 |
| America | 171 (76) | 225 | 39 (23) | 171 |
| Asia | 1203 (71) | 1704 | 390 (32) | 1203 |
| Europe | 60 (65) | 93 | 12 (20) | 60 |
| Oceania | 156 (61) | 258 | 42 (28) | 153 |
| Missing | 45 (71) | 63 | 15 (36) | 42 |
| Ethnicityf | ||||
| Asian | 1083 (72) | 1512 | 336 (31) | 1083 |
| Māori, European & Other | 108 (67) | 162 | 21 (20) | 105 |
| MELAAg | 630 (67) | 936 | 180 (29) | 630 |
| Pacific Peoples | 108 (59) | 183 | 36 (34) | 105 |
| Dependent children in family | ||||
| None | 60 (44) | 138 | S (S) | 60 |
| One | 366 (65) | 567 | 90 (25) | 366 |
| Two | 600 (71) | 849 | 207 (35) | 600 |
| Three | 450 (76) | 591 | 141 (31) | 450 |
| Four or more | 324 (69) | 468 | 108 (33) | 327 |
| Missing | 129 (68) | 189 | S (S) | 129 |
| Household incomeh | ||||
| Low | 672 (74) | 912 | 237 (35) | 672 |
| Medium | 645 (69) | 936 | 201 (31) | 645 |
| High | 132 (62) | 213 | 24 (18) | 132 |
| Missing | 474 (64) | 738 | 111 (23) | 474 |
| Parent education (usually mother) | ||||
| No reported qualification | 738 (68) | 1086 | 231 (31) | 738 |
| Overseas secondary qualification | 401 (69) | 579 | 132 (33) | 402 |
| NZ secondary qualification to diploma | 312 (69) | 453 | 78 (25) | 312 |
| Undergraduate degree | 138 (74) | 186 | 45 (33) | 138 |
| Postgraduate degree | 36 (71) | 51 | 12 (36) | 33 |
| Missing | 300 (68) | 444 | 75 (25) | 300 |
| Parent's ability to converse in English | ||||
| Yes | 1110 (69) | 1611 | 327 (30) | 1110 |
| No | 738 (69) | 1074 | 219 (30) | 738 |
| Missing | 78 (70) | 111 | 30 (39) | 78 |
| Family structure | ||||
| Couple | 1419 (71) | 2013 | 459 (32) | 1419 |
| Sole parent | 468 (64) | 726 | 102 (22) | 468 |
| Missing | 39 (5) | 783 | 12 (33) | 36 |
∗Note it is the policy of Statistics New Zealand that counts are randomly rounded to a number divisible by 3 to protect privacy; thus, the numbers may not reconcile precisely.
National Immunisation Register.
Measles, mumps and rubella vaccine.
Yes = child was enrolled on the National Immunisation Register by the end of the study period.
Vaccinated if child's age was ≥1 year and <5 years old and the child received at least one dose, or the child was ≥5 years and received two doses (MOH, 2020). Although children <1 year old are not eligible for MMR, we considered them to be age-appropriately vaccinated as they may have received a dose.
Vaccination status based on child's age at the end of the study period.
Ethnicity is self-reported by parents as per the National Health Index dataset and grouped according to Level 1 ethnic categories as per statistics New Zealand.
Middle Eastern, Latin American, or African.
Household income: Low (<$25,000), Medium ($25,001–$70,000), High ($70,001–$150,001 or more).
Recorded vaccination status for measles, mumps and rubella (MMR) vaccine
Among the sub-cohort of children who were enrolled on the NIR (n = 1926), less than one third of children (n = 573, 30%) were age-appropriately vaccinated with MMR at the end of the study period. Immunisation coverage steadily increased over time from 15% in 2006 to 50% in 2013. Younger children (0–<2 year olds) had the highest coverage rates. Age-appropriate vaccination status improved over time but remained better for younger children overall (Fig. 2). There were differences by visa category, ranging from 21% for convention refugees to 38% for overstayers. There were no trends noted between vaccination status and household income, parental education level or ability to converse in English. A similar pattern was noticeable for age-appropriate vaccination status of a pertussis-containing vaccine (Supplementary Table S1). At the end of the study period, 18% (n = 345) of children were age-appropriately vaccinated with a pertussis-containing vaccine, with coverage differences noted amongst age groups, arrival year, and visa groups.
Fig. 2.
Percent of overseas-born refugee children who are age-appropriately vaccinated with measles, mumps and rubella by age group and year of arrival.
Factors associated with enrolment on the National Immunisation Register (NIR) and measles, mumps and rubella (MMR) coverage
To explore factors that influenced enrolment on the NIR and MMR vaccination status, unadjusted and adjusted odds ratios are presented (Table 2). Univariate logistic regression showed that all variables were significantly associated with being enrolled on the NIR except for parental education level and their ability to converse in English. After adjusting for confounding, variables that remained significantly associated with being enrolled on the NIR were visa category, age group and arrival year in NZ. Those arriving via family reunification (p = 0.0021) and humanitarian (p = 0.024) pathways were less likely to be enrolled on the NIR compared to quota refugees. Children who arrived later in the study period (2011–2012) had approximately double the odds of being enrolled on the NIR compared to children who arrived in 2006. Younger children were more likely to be enrolled on the NIR compared to older children.
Table 2.
Univariate and multivariable logistic regression estimates for enrolment on the National Immunisation Register and age-appropriate measles, mumps and rubella vaccination status by demographic characteristics (n = 2796).
| In the NIRa, c |
Age appropriately received MMRb, d, e vaccine |
|||
|---|---|---|---|---|
| Unadjusted OR estimate (95% confidence range) | Adjusted OR estimate (95% confidence range) | Unadjusted OR estimate (95% confidence range) | Adjusted OR estimate (95% confidence range) | |
| Visa category | ||||
| Quota refugee | REF | REF | REF | REF |
| Convention refugee | 0.58 (0.42–0.79) | 0.63 (0.40–1.01) | 0.47 (0.31–0.73) | 0.30 (0.12–0.74)∗ |
| Humanitarian | 0.65 (0.52–0.81) | 0.62 (0.41–0.94)∗ | 0.5 (0.37–0.67) | 0.41 (0.21–0.80)∗ |
| Overstayer | 0.73 (0.49–1.08) | 0.68 (0.32–1.45) | 0.96 (0.63–1.48) | 0.61 (0.19–1.89) |
| Family reunification | 0.45 (0.30–0.67)∗ | 0.38 (0.20–0.70)∗ | 0.5 (0.29–0.87) | 0.26 (0.08–0.78)∗ |
| Age group at arrival | ||||
| 0–<2 years | 2.2 (0.88–5.53) | 2.11 (0.83–5.34) | 7.94 (4.97–12.69)∗ | 15.35 (8.59–27.4)∗ |
| 2–<6 years | REF | REF | REF | REF |
| 6–<14 years | 0.12 (0.08–0.19)∗ | 0.12 (0.08–0.19)∗ | 0.05 (0.04–0.08)∗ | 0.03 (0.02–0.05)∗ |
| 14–19 years | 0.05 (0.03–0.09)∗ | 0.05 (0.03–0.08)∗ | 0.009 (0.002–0.036)∗ | 0.005 (0.001–0.02)∗ |
| Arrival year | ||||
| 2006 | REF | REF | REF | REF |
| 2007 | 0.75 (0.54–1.05) | 0.64 (0.39–1.06) | 1.32 (0.84–2.1) | 0.83 (0.35–1.96) |
| 2008 | 0.81 (0.58–1.12) | 1.14 (0.70–1.85) | 1.2 (0.76–1.89) | 1.84 (0.77–4.36) |
| 2009 | 0.95 (0.68–1.34) | 1.08 (0.65–1.78) | 2.19 (1.43–3.37) | 4.58 (1.96–10.74)∗ |
| 2010 | 0.82 (0.58–1.16) | 1.00 (0.60–1.68) | 2.18 (1.41–3.37) | 8.03 (3.33–19.36)∗ |
| 2011 | 1.29 (0.90–1.86) | 2.11 (1.21–3.68)∗ | 2.67 (1.73–4.13) | 9.87 (4.07–23.93)∗ |
| 2012 | 1.07 (0.76–1.50) | 1.70 (1.01–2.84)∗ | 4.16 (2.76–6.27)∗ | 20.17 (8.60–47.30)∗ |
| 2013 | 1.40 (0.72–2.73) | 1.55 (0.62–3.86) | 4.43 (2.35–8.37)∗ | 6.71 (1.96–22.97)∗ |
| United Nations region | ||||
| Oceania | REF | REF | REF | REF |
| Africa | 1.13 (0.80–1.60) | 1.60 (0.66–3.88) | 0.89 (0.57–1.4) | 7.65 (1.46–40.12)∗ |
| America | 2.09 (1.36–3.21)∗ | 1.79 (0.69–4.64) | 1.06 (0.64–1.75) | 1.28 (0.23–7.10) |
| Asia | 1.57 (1.16–2.12) | 0.91 (0.41–2.00) | 1.54 (1.06–2.25)∗ | 2.61 (0.60–11.36) |
| Europe | 1.41 (0.82–2.44) | 1.79 (0.56–5.77) | 0.88 (0.44–1.75) | 11.69 (1.30–105.4)∗ |
| Ethnicityf | ||||
| Māori, European & Other | REF | REF | REF | REF |
| Pacific Peoples | 0.68 (0.42–1.11) | 1.23 (0.39–3.88) | 1.89 (0.99–3.60) | 5.35 (0.64–44.63) |
| Asian | 1.27 (0.87–1.87)∗ | 1.99 (0.88–4.52) | 2.21 (1.31–3.7)∗ | 2.76 (0.60–12.75) |
| MELAAg | 0.97 (0.66–1.43) | 0.95 (0.44–2.03) | 1.74 (1.02–2.98) | 2.04 (0.47–8.87) |
| Dependent children in familyh | ||||
| One | REF | REF | REF | REF |
| Two | 1.35 (1.07–1.69) | 0.95 (0.69–1.31) | 1.74 (1.31–2.29)∗ | 1.94 (1.10–3.43)∗ |
| Three | 1.77 (1.37–2.29)∗ | 1.32 (0.89–1.96) | 1.7 (1.26–2.29) | 1.94 (1.04–3.62)∗ |
| Four or more | 1.26 (0.97–1.64) | 0.83 (0.54–1.25) | 1.62 (1.18–2.22) | 1.47 (0.75–2.88) |
| Household incomei | ||||
| High | REF | REF | REF | REF |
| Low | 1.57 (1.12–2.20)∗ | 1.16 (0.71–1.90) | 2.58 (1.64–4.07)∗ | 1.60 (0.67–3.82) |
| Medium | 1.25 (0.90–1.76) | 0.92 (0.57–1.47) | 2.06 (1.3–3.26) | 1.80 (0.78–4.13) |
| Parent education (usually mother) | ||||
| No reported qualification | REF | REF | REF | REF |
| Undergraduate degree | 1.35 (0.93–1.96) | 1.53 (0.88–2.64) | 1.17 (0.81–1.71) | 0.92 (0.43–1.94) |
| NZ secondary qualification to diploma | 1.05 (0.81–1.36) | 1.32 (0.90–1.94) | 0.8 (0.6–1.08) | 1.40 (0.76–2.56) |
| Overseas secondary qualification | 1.11 (0.88–1.40) | 1.07 (0.75–1.54) | 1.13 (0.88–1.45) | 0.96 (0.57–1.60) |
| Postgraduate degree | 1.06 (0.55–2.05) | 0.87 (0.36–2.11) | 1.16 (0.57–2.33) | 2.81 (0.77–10.21) |
| Parent's ability to converse in English | ||||
| Yes | REF | REF | REF | REF |
| No | 0.94 (0.79–1.13) | 0.95 (0.70–1.31) | 1.03 (0.84–1.26) | 1.44 (0.90–2.32) |
| Family structure | ||||
| Sole parent | REF | REF | REF | REF |
| Couple | 1.33 (1.10–1.62)∗ | 1.14 (0.83–1.57) | 1.78 (1.4–2.26)∗ | 1.23 (0.72–2.11) |
∗p-value < 0.05.
National Immunisation Register.
Yes = child was enrolled on the National Immunisation Register by the end of the study period.
Measles, mumps and rubella vaccine.
Vaccinated if child's age was ≥1 year and <5 years old and the child received at least one dose, or the child was ≥5 years and received two doses (MOH, 2020). Although children <1 year old are not eligible for MMR, we considered them to be age-appropriately vaccinated as they may have received a dose.
Vaccination status based on child's age at the end of the study period.
Ethnicity is self-reported by parents as per the National Health Index dataset and grouped according to Level 1 ethnic categories as per Statistics New Zealand.
Middle Eastern, Latin American, or African.
The ‘none’ group has been removed from the modelling as they are likely to be young adults at the end of the study period who filled out the Census and thus are inconsistent with the rest of the cohort who were dependent children.
Household income: Low (<$25,000), Medium ($25,001–$70,000), High ($70,001–$150,001 or more).
A similar pattern was found for age-appropriate MMR vaccination status (Table 2). Univariate logistic regression showed that all variables were significantly associated with MMR status except for parental ability to converse in English. Multivariable logistic regression identified a significant association between MMR status and visa category, age group at arrival, and arrival year. Those arriving via asylum seeking (p = 0.0085), family reunification (p = 0.016) and humanitarian (p = 0.0087) pathways were less likely to be age-appropriately vaccinated compared to quota refugees. Children arriving later in the study period (2009–2013) were more likely to be age-appropriately vaccinated than children who arrived in NZ in 2006. As with enrolment on the NIR, the youngest age group (birth to less than 2 years old) had significantly higher odds of being age-appropriately vaccinated with MMR compared to older age groups. In addition, UN region and number of dependent children were significantly associated with MMR vaccination status. Children from African and European UN regions were significantly more likely to be age-appropriately vaccinated compared to children from the Oceania region. Lastly, families with two or three dependent children had twice the odds of being age-appropriately vaccinated compared to families with one child.
Discussion
This national retrospective cohort study revealed that immunisation register enrolment and receipt of the MMR vaccine are suboptimal for overseas-born refugee children. While less than 1% of NZ children opt-off the NIR,13 in this study, over one quarter (31%) of overseas-born refugee children did not have a record on the NIR, so their vaccination status is not able to be discerned. As mentioned, all refugees are encouraged to register with a general practice upon arrival for their vaccination status to be assessed and recorded on the NIR and be given an individualised immunisation catch-up programme.11 Thus, these results likely reflect failures of NZ health services to engage in a timely fashion with overseas refugee families upon their arrival in NZ and/or a failure of the services to enrol these children on the NIR on engagement.
Of those enrolled on the NIR, less than one third (30%) of overseas-born refugee children had recorded age-appropriate MMR vaccination status. MMR coverage rates were highest among younger children and steadily increased over time for all age groups. The majority (89%) of children in the youngest age group (under 2 years old) had received their two MMR vaccines, which is just below the required 95% of immune people in the population to prevent a measles outbreak.11 Amongst overseas-born children under 5 years old living in NZ with migrant or refugee backgrounds who were enrolled on the NIR, 69% were fully vaccinated on-time with two MMR vaccines.17 International studies have also reported suboptimal immunisation coverage for schedule vaccines among children with refugee backgrounds, including asylum-seeking26 and refugee children in Denmark,27 and refugee children in Greece,28 and UK-bound refugee children.4 Moreover, studies have reported the influence of nativity for children and their parents with lower vaccination coverage rates among those that are born overseas.2
These findings highlight that health providers must appropriately engage, enrol, and assess the immunisation needs of overseas-born refugee children immediately upon their arrival and provide catch-up immunisations based on their age to align with the NIS11 and provide optimal protection against VPDs. However, the suboptimal MMR coverage rates recorded in the NIR may underestimate actual coverage. Some overseas-born children may have received measles-containing vaccines in their country of origin or while transiting and these may not have been accurately recorded in the NIR because they are not a component of the NZ schedule. While the NIR data is generally accurate amongst the general NZ population, especially for schedule vaccines, the challenges of entering overseas vaccination records may account for some discrepancies.29
Determinants of NIR enrolment and MMR coverage
This study revealed that both NIR enrolment and MMR coverage rates were significantly associated with age, year of arrival, and visa category. Children who arrived later in the study period were more likely to be enrolled and be age-appropriately vaccinated with MMR than children who arrived at the start of the study. This likely reflects the concerted efforts that have been ongoing for the past two decades to improve immunisation coverage and reduce inequities in NZ.25
Older refugee children were less likely to be enrolled on the register and receive MMR vaccination. Similarly, a Danish study among asylum seeking children reported that younger children were more likely to be vaccinated compared to older children.26 Also, UK-bound refugee children were more likely to have recorded vaccinations compared to adolescent and adult refugees.4 There are notable barriers to improving vaccination coverage among adolescents, including lack of health provider recommendations, parental vaccine refusal, vaccine misinformation available on the Internet and social media platforms, and financial difficulties.30 A systematic review and meta-analysis noted that educational interventions, reminders, interventions for providers, financial incentives, and multilevel interventions may improve vaccination coverage for school-aged children and adolescents (5–19 years old) in high-income countries.31 Adolescent refugees who resettle in high-income countries have complex healthcare needs that reflect their migration journeys32; thus, future research is needed to understand which interventions are particularly feasible and effective for improving vaccination coverage among adolescent refugees. For optimum NZ wide protection against a measles epidemic, an integrated approach is likely needed to improve vaccination coverage for older children and adolescents with refugee backgrounds.
Children arriving on other refugee pathways were less likely to be enrolled and vaccinated compared to quota refugee children. A Danish study reported that quota refugees had lower vaccination uptake compared to asylum seeking children.27 This discrepancy may be explained by NZ's unique quota refugee programme that involves an orientation and health screening programme in which vaccination status is assessed and age-appropriate vaccines are offered at the Mangere Refugee Resettlement Centre.21,22 Moreover, only quota refugees are included in the RSS and receive support to register with primary care services in the community after leaving the Mangere Refugee Resettlement Centre.18 Given NZ's commitment to increase the quota, it is planned for this orientation programme to be reduced, and screening and immunisations will now be delivered offshore as part of the new refugee quota health service delivery model.18 Seamless flow of refugees' immunisation records from offshore to national databases will be essential, otherwise the apparent gains here from early engagement will be lost. Refugees entering via other pathways are not entitled to the same health screening and orientation programme and this has likely contributed to immunisation inequities and inadequate population protection against VPDs.
Previous literature has noted various factors that influence immunisation coverage among people with migrant backgrounds2,5; however, most of these were not significant factors in the presented study. For instance, although language has been identified as a barrier to accessing preventive health services, parent's ability to converse in English was not a significant factor influencing enrolment or MMR vaccination status. Thus, further research is needed to understand the complex interplay of factors underpinning former refugee families' engagement with immunisation services and vaccination coverage.
Implications for policy and practice
So long as there are immunisation inequities within a population, achieving population wide protection against VPDs will not be attainable. There is a continued need for providers to engage with refugee families upon their arrival to assess vaccination records and start catch-up immunisations. Tailored interventions to improve vaccine access and acceptance among refugees are needed that address commonly identified barriers and are sensitive to the heterogeneity within and between migrant and refugee populations.33 Barriers that contribute to migrants' and refugees' underutilisation of healthcare services are well documented in high-income countries34, 35, 36, 37; thus, as immunisation services are a part of primary healthcare services, concerted efforts to reduce these disparities are needed. High-income countries that welcome migrants and refugees, such as NZ, are becoming increasingly diverse and as such, health care systems and policies must be increasingly migrant-sensitive to address their health needs.38 Keeping in mind the WHO's IA2030 focus on equitable vaccination coverage across the life-course,6 approaches to improve engagement and coverage amongst refugee adolescents is imperative. There are clear immunisation inequities based on refugee visa category, which highlight the need for health services to be equitable for all refugees.17,39 The current RSS only applies to quota refugees although there is an intention that it will apply to all refugees in the future.18 An initial first step would be to honour this commitment and include all refugees in the RSS so that all refugees are entitled to the same health and support services. The proportion of overseas-born refugee children who were not enrolled on the NIR and the potential inaccurate recording of overseas vaccines warrants urgent attention. Accurate immunisation register data will be vital to identify and respond with appropriate and timely services.
Strengths and limitations
NZ's unique data collection and linking capabilities within the IDI enabled the presented analyses of NIR enrolment and vaccination coverage among refugee children. The presented findings may be relevant to other marginalised migrant groups resettled in high-income countries. However, as our findings demonstrate immunisation inequities by visa category, future studies should explore the role of different entry pathways and entitlement to health services on vaccination coverage amongst migrant groups. A few assumptions were made as the existing administrative data was used for a purpose other than its original one. It was not possible to control the variables or the value categories available, which may introduce some inaccuracies. Moreover, the analyses were limited to those that had completed the 2013 Census and some categories had small numbers that had to be suppressed thereby limiting the conclusion that can be made. Our cohort includes children from the same family and our logistic model did not adjust for clustering by family, so the confidence limits will slightly underestimate variability in our cohort. Whilst a large proportion of refugee children were missing Census 2013 data (60%) from the total cohort, there were still substantial numbers of children representing those in the outcome groups of interest (i.e., not in the NIR and not vaccinated with MMR) (Supplementary Table S2). We acknowledge that the drivers may be different for the children who were not recorded on the register and unvaccinated, and do not have Census 2013 data available. Lastly, our presented analyses focused on children with refugee backgrounds who had administrative data available in the IDI. Future research should focus on other groups of marginalised children, such as undocumented migrants, to ensure all children have equitable access to vaccines, no matter their migration background.
Conclusion
Despite the availability of publicly funded vaccines, overseas-born refugee children have suboptimal immunisation register enrolment and MMR vaccination coverage. Significant disparities were found between different groups of refugee-background children. Tailored and targeted interventions are required by immunisation service providers to engage with former refugee families post-resettlement to ensure age-appropriate vaccines are offered in a timely manner, particularly for older children and adolescents. A priority is to ensure all refugees are entitled to the same health and support services to reduce inequities between refugees who arrive on different pathways.
Contributors
All authors designed the study. NC did the initial literature reviews, and developed the study plan. JP linked and analysed the data. All authors contributed to the analysis and interpreted the results. NC drafted the initial manuscript, and JP and NT revised the manuscript critically for intellectual content and gave final approval.
Data sharing statement
Summary Statistics New Zealand Security Statement – This study is based on the integration of anonymised population census data from Statistics New Zealand and mortality data from the New Zealand Health Information Service. This project was approved by Statistics New Zealand as a Data Laboratory project under the Microdata Access Protocols in 1997. The datasets created by the integration process are covered by the Statistics Act 1975 and can be used for statistical purposes only. Only approved researchers who have signed Statistics New Zealand's declaration of secrecy can access the integrated data in the Data Laboratory. For further information about confidentiality matters in regard to this study please contact Statistics New Zealand.
Declaration of interests
The authors have no potential conflict of interest to report.
Acknowledgements
This study was conducted in collaboration with Statistics New Zealand and within the confines of the Statistics Act 1975. We would like to thank members of The Monarch Collaboration (http://monarchcollaboration.org/) for their support of this study.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100709.
Appendix A. Supplementary data
References
- 1.United Nations High Commissioner for Refugees . 2021. Global trends: forced displacement in 2020. [Google Scholar]
- 2.Charania N.A., Gaze N., Kung J.Y., Brooks S. Vaccine-preventable diseases and immunisation coverage among migrants and non-migrants worldwide: a scoping review of published literature, 2006–2016. Vaccine. 2019;37(20):2661–2669. doi: 10.1016/j.vaccine.2019.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Deal A., Halliday R., Crawshaw A.F., et al. Migration and outbreaks of vaccine-preventable disease in Europe: a systematic review. Lancet Infect Dis. 2021;21(12):e387–e398. doi: 10.1016/S1473-3099(21)00193-6. [DOI] [PubMed] [Google Scholar]
- 4.Deal A., Hayward S.E., Crawshaw A.F., et al. Immunisation status of UK-bound refugees between January, 2018, and October, 2019: a retrospective, population-based cross-sectional study. Lancet Public Health. 2022;7(7):e606–e615. doi: 10.1016/S2468-2667(22)00089-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crawshaw A.F., Farah Y., Deal A., et al. Defining the determinants of vaccine uptake and undervaccination in migrant populations in Europe to improve routine and COVID-19 vaccine uptake: a systematic review. Lancet Infect Dis. 2022;22:e254. doi: 10.1016/S1473-3099(22)00066-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation . 2020. Immunization agenda 2030: a global strategy to leave no one behind. [DOI] [PubMed] [Google Scholar]
- 7.International Organisation for Migration. Glossary on migration. 2019. https://publications.iom.int/system/files/pdf/iml_34_glossary.pdf Available from:
- 8.Immigration New Zealand Supporting refugees and asylum seekers. https://www.immigration.govt.nz/about-us/what-we-do/our-strategies-and-projects/supporting-refugees-and-asylum-seekers Available from: n.d.
- 9.Marlowe J., Elliott S. Global trends and refugee settlement in New Zealand. Kōtuitui New Zealand J Soc Sci Online. 2014;9(2):43–49. [Google Scholar]
- 10.Immigration New Zealand. Sponsoring family members if you are a refugee. 2022. https://www.immigration.govt.nz/new-zealand-visas/apply-for-a-visa/tools-and-information/general-information/sponsorship-refugee-family-support-category Available from:
- 11.Ministry of Health . Ministry of Health; Wellington: 2020. Immunisation handbook.https://www.health.govt.nz/publication/immunisation-handbook-2020 Available from: [Google Scholar]
- 12.Ministry of Health. Immunisation coverage. 2021. https://www.health.govt.nz/our-work/preventative-health-wellness/immunisation/immunisation-coverage Available from:
- 13.Ministry of Health. National and DHB immunisation data. 2022. https://www.health.govt.nz/our-work/preventative-health-wellness/immunisation/immunisation-coverage/national-and-dhb-immunisation-data Available from:
- 14.Shet A., Carr K., Danovaro-Holliday M.C., et al. Impact of the SARS-CoV-2 pandemic on routine immunisation services: evidence of disruption and recovery from 170 countries and territories. Lancet Glob Health. 2022;10(2):e186–e194. doi: 10.1016/S2214-109X(21)00512-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sonder G., Ryan D. Ministry of Health; Wellington: 2020. Health sector response to the 2019 measles outbreaks. [Google Scholar]
- 16.Craig A.T., Heywood A.E., Worth H. Measles epidemic in Samoa and other Pacific islands. Lancet Infect Dis. 2020;20(3):273–275. doi: 10.1016/S1473-3099(20)30053-0. [DOI] [PubMed] [Google Scholar]
- 17.Charania N.A., Paynter P., Lee A.C., Watson D.G., Turner N.M. Exploring immunisation inequities among migrant and refugee children in New Zealand. Hum Vaccin Immunother. 2018;14(12):3026–3033. doi: 10.1080/21645515.2018.1496769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Immigration New Zealand. New Zealand refugee resettlement strategy. 2022. https://www.immigration.govt.nz/about-us/what-we-do/our-strategies-and-projects/refugee-resettlement-strategy Available from:
- 19.Anguera M.T., Blanco-Villasenor A., Losada J.L., Sanchez-Algarra P., Onwuegbuzie A.J. Revisiting the difference between mixed methods and multimethods: is it all in the name? Qual Quant. 2018;52:2757–2770. [Google Scholar]
- 20.Immigration New Zealand If you do not leave New Zealand before your visa expires 2022. https://www.immigration.govt.nz/new-zealand-visas/already-have-a-visa/managing-your-visa-and-passport/if-you-do-not-leave-new-zealand-before-your-visa-expires Available from:
- 21.Rungan S., Reeve A.M., Reed P.W., Voss L. Health needs of refugee children younger than 5 years arriving in New Zealand. Pediatr Infect Dis J. 2013;32(12):e432–e436. doi: 10.1097/INF.0b013e3182a11526. [DOI] [PubMed] [Google Scholar]
- 22.McLeod A., Reeve M. The health status of quota refugees screened by New Zealand's Auckland public health service between 1995 and 2000. N Z Med J. 2005;118(1224):U1702. [PubMed] [Google Scholar]
- 23.DeStefano F., Shimabukuro T.T. The MMR vaccine and autism. Annu Rev Virol. 2019;6(1):585–600. doi: 10.1146/annurev-virology-092818-015515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gahr P., DeVries A.S., Wallace G., et al. An outbreak of measles in an undervaccinated community. Pediatrics. 2014;134(1):e220–e228. doi: 10.1542/peds.2013-4260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turner N.M. The challenge of improving immunization coverage: the New Zealand example. Expert Rev Vaccines. 2012;11(1):9–11. doi: 10.1586/erv.11.157. [DOI] [PubMed] [Google Scholar]
- 26.Nakken C.S., Skovdal M., Nellums L.B., Friedland J.S., Hargreaves S., Norredam M. Vaccination status and needs of asylum-seeking children in Denmark: a retrospective data analysis. Public Health. 2018;158:110–116. doi: 10.1016/j.puhe.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moller S.P., Hjern A., Andersen A.M., Norredam M. Differences in uptake of immunisations and health examinations among refugee children compared to Danish-born children: a cohort study. Eur J Pediatr. 2016;175(4):539–549. doi: 10.1007/s00431-015-2663-9. [DOI] [PubMed] [Google Scholar]
- 28.Mellou K., Silvestros C., Saranti-Papasaranti E., et al. Increasing childhood vaccination coverage of the refugee and migrant population in Greece through the European programme PHILOS, April 2017 to April 2018. Euro Surveill. 2019;24(27) doi: 10.2807/1560-7917.ES.2019.24.27.1800326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chisholm H., Paynter J., Willing E., Turner N., Howe A.S. Does the national immunisation register stack up? Quantifying accuracy when compared to parent-held health record books. N Z Med J. 2021;134(1541):22–32. [PubMed] [Google Scholar]
- 30.Bernstein H.H., Bocchini J.A., Jr., Committee on infectious Diseases The need to optimize adolescent immunization. Pediatrics. 2017;139(3) doi: 10.1542/peds.2016-4186. [DOI] [PubMed] [Google Scholar]
- 31.Siddiqui F.A., Padhani Z.A., Salam R.A., et al. Interventions to improve immunization coverage among children and adolescents: a meta-analysis. Pediatrics. 2022;149(Suppl 5) doi: 10.1542/peds.2021-053852D. e2021053852D. [DOI] [PubMed] [Google Scholar]
- 32.Hirani K., Payne D., Mutch R., Cherian S. Health of adolescent refugees resettling in high-income countries. Arch Dis Child. 2016;101(7):670–676. doi: 10.1136/archdischild-2014-307221. [DOI] [PubMed] [Google Scholar]
- 33.Charania N.A., Gaze N., Kung J.Y., Brooks S. Interventions to reduce the burden of vaccine-preventable diseases among migrants and refugees worldwide: a scoping review of published literature, 2006–2018. Vaccine. 2020;38(46):7217–7225. doi: 10.1016/j.vaccine.2020.09.054. [DOI] [PubMed] [Google Scholar]
- 34.Pandey M., Kamrul R., Michaels C.R., McCarron M. Identifying barriers to healthcare access for new immigrants: a qualitative study in Regina, Saskatchewan, Canada. J Immigr Minor Health. 2022;24(1):188–198. doi: 10.1007/s10903-021-01262-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lebano A., Hamed S., Bradby H., et al. Migrants' and refugees' health status and healthcare in Europe: a scoping literature review. BMC Public Health. 2020;20(1):1039. doi: 10.1186/s12889-020-08749-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morris M.D., Popper S.T., Rodwell T.C., Brodine S.K., Brouwer K.C. Healthcare barriers of refugees post-resettlement. J Community Health. 2009;34(6):529–538. doi: 10.1007/s10900-009-9175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morrison T.B., Wieland M.L., Cha S.S., Rahman A.S., Chaudhry R. Disparities in preventive health services among Somali immigrants and refugees. J Immigr Minor Health. 2012;14(6):968–974. doi: 10.1007/s10903-012-9632-4. [DOI] [PubMed] [Google Scholar]
- 38.Kanengoni B., Andajani-Sutjahjo S., Holroyd E. Setting the stage: reviewing current knowledge on the health of New Zealand immigrants-an integrative review. PeerJ. 2018;6:e5184. doi: 10.7717/peerj.5184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kennedy J.D., Moran S., Garrett S., Stanley J., Visser J., McKinlay E. Refugee-like migrants have similar health needs to refugees: a New Zealand post-settlement cohort study. BJGP Open. 2020;4(1) doi: 10.3399/bjgpopen20X101013. bjgpopen20X101013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.