Abstract
Ischemic priapism is a urologic emergency requiring urgent intervention to prevent tissue necrosis and preserve erectile function. Cases refractory to aspiration and intra-cavernosal sympathomimetic therapy requires timely surgical shunting. Corpus cavernosum abscess following penile shunts is an exceedingly rare complication, with as few as 2 previous reported cases.
We report our experience and outcome in the case of a 50-year-old patient who developed a corpora cavernosum abscess and concurrent corporoglanular fistula, following penile shunt procedures for ischemic priapism.
Keywords: Penile abscess, Corporal abscess, Corporoglanular fistula
1. Introduction
Ischemic priapism refractory to aspiration and intra-cavernosal sympathomimetic therapy requires timely surgical shunting to reduce long-term risks of chronic pain and erectile dysfunction. Corpus cavernosum abscess post-shunt procedure is an exceedingly rare pathology, with only two previous reported cases. In this report, we describe a case of corpora cavernosum abscess with concurrent corporoglanular fistula following the management of a complex case of stuttering priapism requiring multiple shunts for successful detumescence.
2. Case report
A 50-year-old patient presented to the emergency department following a 16-h episode of ischemic priapism.
Detumescence was achieved with intra-cavernosal injections of metaraminol (three aliquots of 0.1mg), following unsuccessful corporal aspiration. The patient was discharged the next morning.
The patient's urological background was significant for erectile dysfunction with intermittent use of phosphodiesterase type 5 inhibitors. Medical history included schizophrenia, bipolar disease, and hypertension. Regular medications consisted of amisulpride, sodium valproate, quetiapine, and prazosin.
The patient re-presented one month later with a 36-h episode of priapism. Cavernosal blood gas was diagnostic of ischemic priapism, with pH < 6.8, pO2 <6 mmHg and a lactate of 8.5mmol/L. Intra-cavernosal metaraminol was again utilised after unsuccessful aspiration. Partial detumescence was achieved following five aliquots of 0.2mg metaraminol. On serial review, priapism had recurred, and a Winter's shunt was successfully performed. Anti-platelet therapy (clopidogrel) was commenced to prevent premature shunt closure. Despite this, priapism recurred the following day. A T-shunt was successfully performed, and the patient was discharged the following day.
The patient re-presented 2 weeks later with increasing penile pain and erythema. On examination, a 3cm mid-penile shaft abscess was identified overlying the right corpora cavernosum, with a swollen prepuce (Fig. 1). Purulent discharge was expressible from within the prepuce, however due to the swelling and pain, retraction to assess the glans and urethra was not possible. Inflammatory markers were raised with a C Reactive Protein level of 100mg/L. Penile ultrasound revealed an abscess with extension and communication with the underlying right corpus cavernosum (Fig. 2). Additionally, reduced echogenicity and absent vascularity was noted bilaterally, consistent with ischemic changes.
Fig. 1.
Corporal Abscess (a) at presentation, (b) intra-operative findings with corporal defect, (c) 1-week post-operation.
Fig. 2.
Ultrasound images of Corporal Abscess (arrow delineating communication through Tunica Albuginea).
An incision and drainage was performed directly over the penile abscess revealing the corporal defect. 30mL of pus was expressed from the corpora. On assessment of the glans, pus was seen to drain from the site of the previous T-shunt. The wound was left open to allow for ongoing drainage and was managed with daily packing with normal saline soaked ribbon gauze. Intra-operative wound cultures were positive for heavy growth of prevotella bivia and scanty growth of streptococcus anginosus. The patient was discharged the following day with a 2-week course of oral amoxicillin and clavulanic acid.
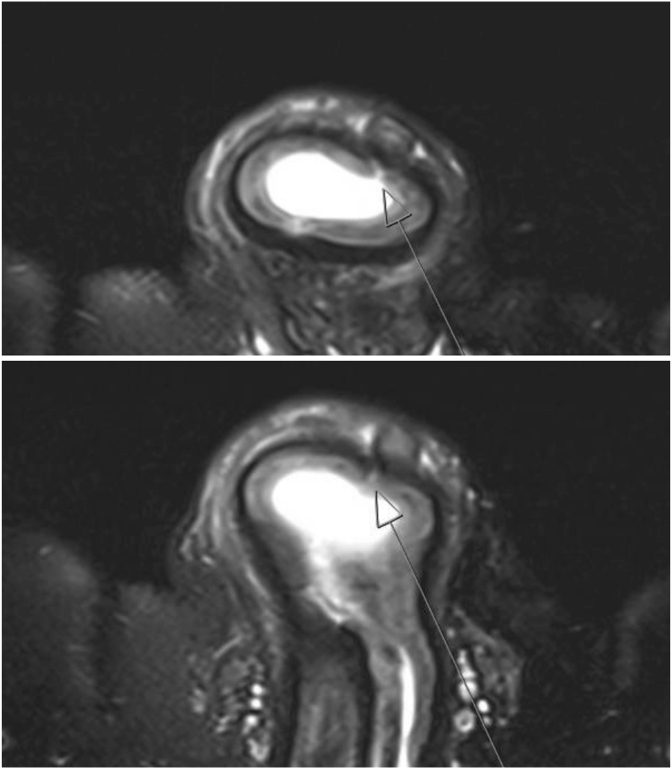
On review 1 week following incision and drainage, significant improvements in pain were reported, and inflammatory markers normalised. The corporal defect had closed, and granulation tissue was seen at the base of the wound. However, significant volumes of pus could still be expressed through the glans. Penile MRI was performed demonstrating residual abscess, and a tract consistent with a corporoglanular fistula (Fig. 3). As the patient was systemically well with significant symptomatic improvement, conservative management was continued with wound care, regular self-expression of pus and antibiotics.
Fig. 3.
Magnetic resonance imaging demonstrating corporoglanular fistula (arrow) with residual abscess.
On final review 2 months later, the penile wound had healed, purulent discharge had ceased and the corporoglanular fistula had closed. Penile ultrasound confirmed abscess resolution. However, both corpora demonstrated diffuse heterogenous loss of normal internal architecture and atrophy, consistent with sequelae from prolonged ischemia. Consistent with these ultrasound findings, the patient also reported complete erectile dysfunction.
3. Discussion
Ischemic priapism is a urologic emergency requiring urgent intervention to prevent tissue necrosis and preserve erectile function. Examination findings of rigid and tender corpora are suggestive of ischemic priapism. Cavernous blood gas analysis should be performed for confirmation.1 Goals of care relate to achieving rapid and complete detumescence while minimising complications from both disease and treatment. The American Urological Association guidelines recommend use of surgical shunts when aspiration and intra-cavernosal therapy is ineffective.1 Complications related to distal shunt procedures include premature shunt failure, damage to dorsal nerve branches and dorsal arteries.2
Corpora cavernosa abscesses are rare. They can occur spontaneously, as well as in the setting of trauma, tuberculosis, penile prosthesis placement, intra-cavernosal injections and fellatio.3 Incision and drainage represents the most common intervention. Singular cases of corporotomy and image guided aspiration have been reported. Outcomes range from complete resolution with normal anatomy to varying degrees of penile deviation, erectile dysfunction, corporal fibrosis and abscess recurrence. No clear benefit was evident from use of corporotomy compared to incision and drainage.3
From our literature review, only two cases of corporal abscesses have been reported following penile shunt procedures. Winter's shunt was used in both cases.4,5 These cases were successfully managed with surgical drainage and antibiotic therapy, with one case requiring a concurrent Al-Ghorab shunt and intra-cavernous tunnelling due to persistent penile rigidity. On long-term follow-up, erectile dysfunction was reported in both cases.4,5
To our knowledge, this is the first reported case of a corporoglanular fistula following penile shunting. The location of the corporal abscess was congruent with the needle insertion site during corporal aspiration. We hypothesise that the inciting bacteria was introduced at time of cavernosal aspiration. Additionally, the corporoglanular fistula was clinically consistent with the incision tract of the previous T-shunt. A history of recurrent priapism and prolonged ischemia resulting in devitalised tissue, as evidenced on ultrasound imaging, may have predisposed the patient to abscess development. While first-generation cephalosporins were used prior to shunt procedures, a course of antibiotic therapy may reduce the risk of abscess formation.
Drainage and antibiotic therapy successfully resolved both the corporal abscess and corporoglanular fistula. Erectile dysfunction was reported on long-term follow-up and should form part of the pre-operative risk discussion.
4. Conclusion
Corpora cavernosum abscesses following penile shunts for management of ischemic priapism is an exceedingly rare complication within the literature. In this report of a concurrent corpora cavernosum abscess and corporoglanular fistula following penile shunt procedures, we describe its successful management with antibiotic therapy, and incision and drainage.
Declarations of interest
None.
Section headings
Inflammation and Infection.
Consent
Consent was obtained for the publication of this case report.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors have no conflict of interest to declare.
Acknowledgements
The authors thank the Westmead Hospital Radiology Service.
Contributor Information
Henry Wang, Email: henry.wang@health.nsw.gov.au.
Ankur Dhar, Email: ankur.dhar@health.nsw.gov.au.
Audrey Wang, Email: audrey.wang@health.nsw.gov.au.
References
- 1.Bivalacqua T.J., Allen B.K., Brock G.B., et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J Urol. 2022;208(1):43–52. doi: 10.1097/JU.0000000000002767. [DOI] [PubMed] [Google Scholar]
- 2.Reed-Maldonado A.B., Kim J.S., Lue T.F. Avoiding complications: surgery for ischemic priapism. Transl Androl Urol. 2017;6(4):657–665. doi: 10.21037/tau.2017.07.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dugdale C.M., Tompkins A.J., Reece R.M., Gardner A.F. Cavernosal abscess due to Streptococcus anginosus: a case report and comprehensive review of the literature. Curr Urol. 2013;7(1):51–56. doi: 10.1159/000343555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paladino J.R., Jr., Nascimento F.J., Gromatsky C., Pompeo A.C. Corpus cavernosum abscess after Winter procedure performance. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-202089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kyoshi Hidaka A., Murata Hayashi R., Chahade Sibanto Simões G., Simões A.G.S., Paladino J.R., Jr. Corpus cavernosum abscess: a case report. Urol Case Rep. 2022;43 doi: 10.1016/j.eucr.2022.102118. [DOI] [PMC free article] [PubMed] [Google Scholar]