Abstract
A 38-year-old with Turner syndrome presented with acute myocardial infarction due to multivessel spontaneous coronary artery dissection (SCAD) complicated by left ventricular free wall rupture. Conservative management for SCAD was pursued. She underwent sutureless repair for an oozing-type left ventricular free wall rupture. SCAD has not been previously reported in Turner syndrome. (Level of Difficulty: Advanced.)
Key Words: acute coronary syndrome, cardiovascular disease, myocardial infarction
Abbreviations and Acronyms: ACS, acute coronary syndrome; CT, computed tomography; DAPT, dual antiplatelet therapy; DKA, diabetic ketoacidosis; ECG, electrocardiogram; LVFWR, left ventricular free wall rupture; PCI, percutaneous coronary intervention; PEA, pulseless electrical activity; SCAD, spontaneous coronary artery dissection; TS, Turner syndrome
Central Illustration
History of Presentation
A 38-year-old woman presented with nausea and vomiting and was diagnosed with diabetic ketoacidosis (DKA). She did not experience any chest pain. Laboratory work included serum glucose 353 mg/dL, anion gap 16 mmol/L, and 3+ urine ketones. Electrocardiogram (ECG) and cardiac enzymes were not obtained. She was treated with insulin and intravenous antibiotics for suspected aspiration pneumonia due to leukocytosis of 17,200/mm3 and left perihilar opacity on chest x-ray. The patient had recurrent episodes of emesis over the first 2 days. On hospital day 2, the patient experienced a pulseless electrical activity (PEA) cardiac arrest. Return of spontaneous circulation was promptly achieved with cardiopulmonary resuscitation that included chest compressions and epinephrine. A postarrest echocardiogram was not obtained. A chest computed tomography (CT) scan reported left ventricular aneurysm with hemopericardium concerning for left ventricular free wall rupture (LVFWR). The patient was transferred to our center intubated and neurologically intact. Vital signs were temperature 36°C, heart rate 92 beats/min, and blood pressure 90/61 mm Hg on norepinephrine infusion at 0.02 μg/kg/min. Physical examination findings included height 55 inches, weight 53 kg, thick neck, and low posterior hairline. Cardiovascular examination was notable for a regular rate and rhythm without murmur, rub, or gallop. Breath sounds were normal.
Learning Objectives
-
•
To understand the epidemiology, presentation, and management of SCAD.
-
•
To recognize the association of cardiovascular disease in TS.
-
•
To understand the epidemiology, presentation, and management of LVFWR.
Medical History
The patient had Turner syndrome (TS) without congenital heart disease or aortopathy, type 2 diabetes mellitus, hypertension, and hyperlipidemia.
Differential Diagnosis
The differential diagnosis for the etiology of LVFWR in our patient includes acute coronary syndrome (ACS), aortic dissection, and Takotsubo cardiomyopathy.1
Investigations
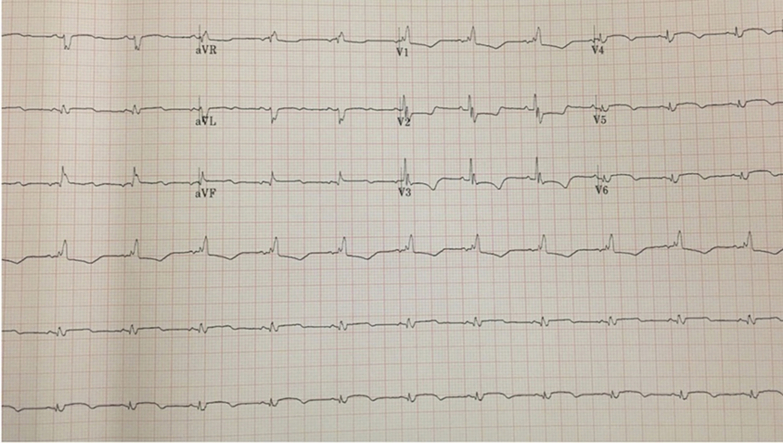
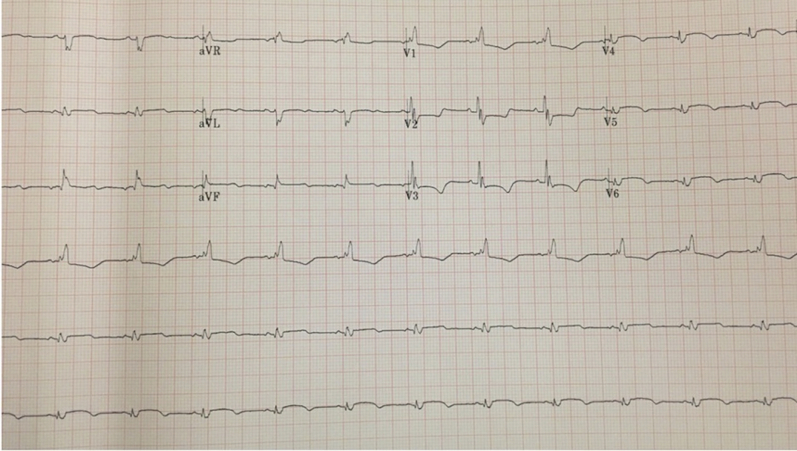
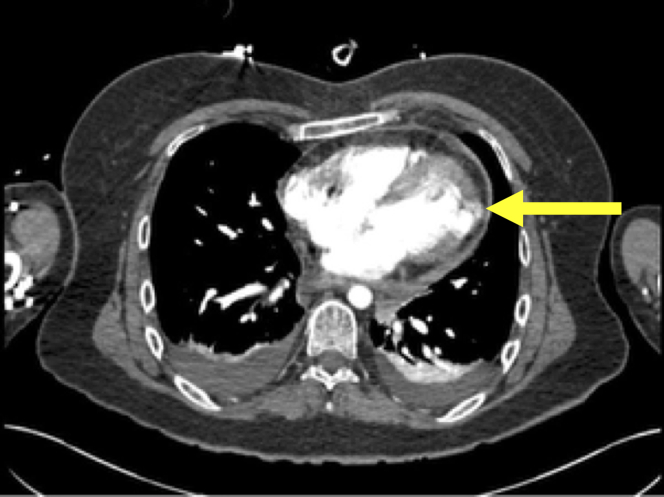
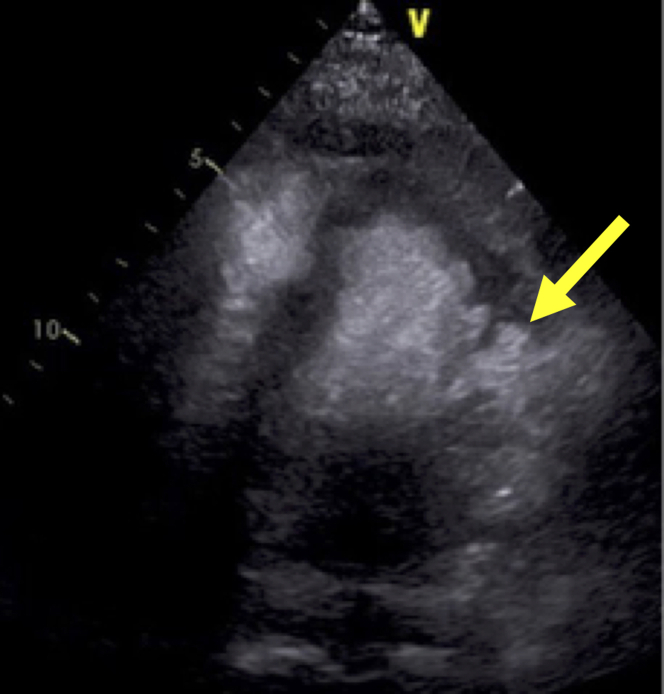
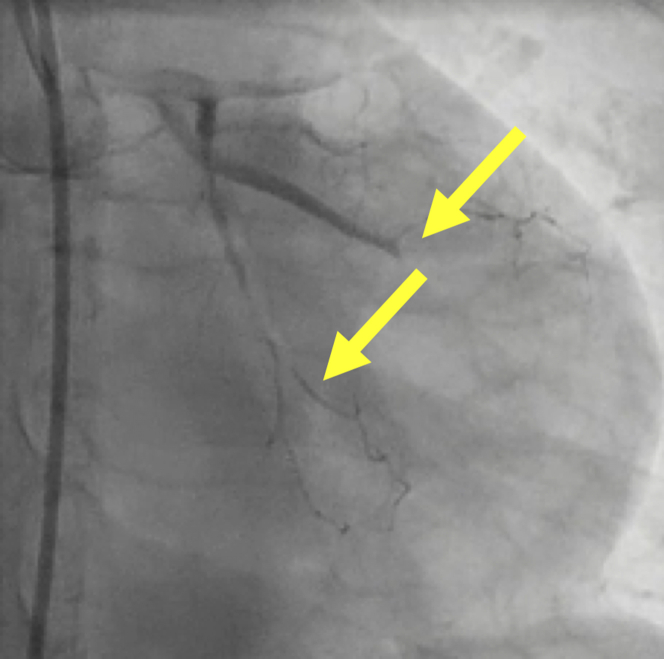
On arrival to our hospital an ECG was notable for a right bundle branch block, anterior Q-waves, small inferior Q-waves, and ST-segment elevation in the inferior and lateral leads consistent with an evolving anterior and inferior ST-segment elevation myocardial infarction (Figure 1). HS-troponin values during 2-h intervals were 5,889, 5,469, and 5,325 ng/L (normal ≤17 ng/L) consistent with a recent myocardial infarction. The outside chest CT scan was reviewed and demonstrated LVFWR (Figure 2). There was no aortic dilation or dissection. Contrast echocardiogram demonstrated an akinetic lateral wall with focal pseudoaneurysm and contrast extravasation consistent with a contained LVFWR (Figure 3). Within 3 h of admission to our hospital, the patient underwent coronary angiography demonstrating multivessel spontaneous coronary artery dissection (SCAD) with mid-left anterior descending and circumflex marginal branch occlusions and dissections in the diagonal branch and posterior descending artery (Figure 4, Videos 1 and 2).
Figure 1.
Electrocardiogram
Electrocardiogram on arrival to our tertiary referral medical center.
Figure 2.
Chest Computed Tomography
Chest computed tomography demonstrating left ventricular free wall rupture (arrow).
Figure 3.
Contrast Echocardiogram with Left Ventricular Pseudoaneurysm and Left Ventricular Free Wall Rupture
Arrow denotes the neck of the pseudoaneurysm.
Figure 4.
Left Coronary Angiogram Demonstrating Multivessel Spontaneous Coronary Artery Dissection
Top arrow highlights mid left anterior descending occlusion and bottom arrow points to dissections in circumflex and obtuse marginal branches.
Management
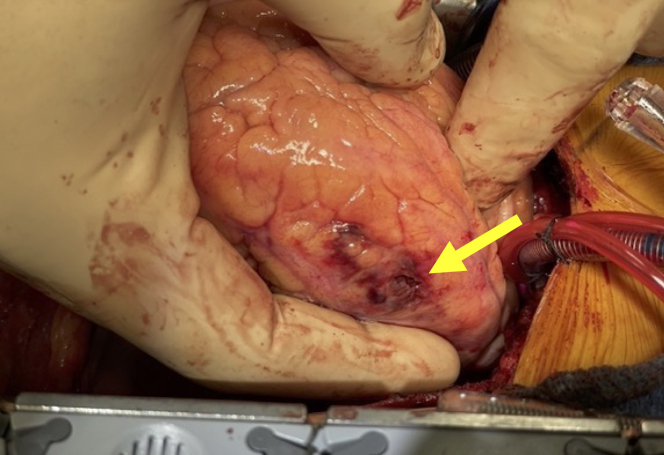
Our patient presented with an acute ST-segment elevation myocardial infarction due to multivessel SCAD masquerading as nausea and vomiting with DKA. The PEA arrest was due to LVFWR. The CT scan and echocardiogram confirmed the acute mechanical complication of myocardial infarction due to SCAD. Conservative management (without revascularization) for SCAD was pursued in our patient given poor targets for revascularization and stable hemodynamics. The patient underwent emergency open surgical sutureless repair using an EVARREST Fibrin Sealant Patch (Ethicon, Inc), fibrin glue (TISSEEL, Baxter Healthcare Corporation), and bovine pericardial patch (Edwards Lifesciences) for an oozing-type LVFWR (Figures 5 and 6). She was discharged home on postoperative day 16. Discharge medications included aspirin 81 mg daily, clopidogrel 75 mg daily, atorvastatin 80 mg daily, losartan 25 mg daily, and metoprolol tartrate 100 mg twice daily.
Figure 5.
Intraoperative Photograph
Intraoperative photograph of heart demonstrating the oozing-type left ventricular free wall rupture (arrow).
Figure 6.
Photograph of the Large Hematoma
Photograph of the large hematoma that was adherent to epicardial surface overlying the oozing-type left ventricular free wall rupture and removed at operative repair.
Discussion
SCAD is an important cause of acute myocardial infarction and is associated with 4% of all cases of ACS.2 SCAD may be responsible for up to 35% of all cases of ACS in women younger than 50 years of age.2 The etiology of SCAD is not fully understood with arteriopathy, estrogen hormones, and extracellular matrix dysfunction theorized as possible underlying factors.2,3
SCAD has not been previously reported to complicate TS. TS is associated with risk of underlying arteriopathy, including aortic dilation and dissection.4 Additionally, there are increased rates of premature ischemic heart disease in TS. Women with TS have hypergonadotropic hypogonadism and are often treated with hormone replacement therapy.5 Estrogen has been postulated to play a role in SCAD because the majority of affected patients are women, however, the exact mechanism is unknown.2 Our patient did not have aortopathy and was previously on estrogen replacement, but not at the time of SCAD.
A diagnosis of SCAD requires a high level of clinical suspicion because patients often lack traditional cardiovascular risk factors. Although the most common presenting complaint is chest pain, up to 27% of patients may have normal initial troponin levels.2 Our patient did not have chest pain and presented with DKA. Myocardial infarction may present with DKA and may have atypical presentations in women. Consideration of acute myocardial infarction with ECG and cardiac enzyme assays at time of presentation is recommended in DKA.6 Coronary angiography is the gold standard for diagnosis of SCAD. Conservative management for most patients with SCAD is preferred because SCAD typically heals spontaneously. However, when left main or proximal vessel SCAD leads to large areas of ischemia or hemodynamic compromise, revascularization (either percutaneous or surgical) is performed.2 Additionally, percutaneous coronary intervention (PCI) carries an elevated risk of complication in SCAD.2 Up to a third of PCIs will be complicated by dissection propagation, which may result in additional, unplanned stents.2
In SCAD managed conservatively, the use of dual antiplatelet therapy (DAPT) is controversial. There are no randomized controlled trials in SCAD and practice patterns vary considerably from aspirin monotherapy to DAPT at varying time intervals. A European registry reported that patients with SCAD managed conservatively had a higher rate of adverse cardiovascular events in follow-up when treated with DAPT than single antiplatelet therapy.7 Beta blocker therapy decreases recurrence rates of SCAD.2 For patients who undergo PCI or who have left ventricular systolic dysfunction, medical management is related to established guidelines.
LVFWR after SCAD is rarely reported.8 LVFWR may develop after a transmural infarction in which there is complete occlusion of a major proximal epicardial coronary vessel. SCAD more commonly involves branch vessels and distal vessels. LVFWR most often occurs on days 2-5 after myocardial infarction. LVFWR occurs in up to 0.5% of patients after acute myocardial infarction.9 Mortality rates have been reported to be 32%-92%9. A meta-analysis reported improved survival rates for patients with oozing-type LVFWR treated with a sutureless technique compared with a suture repair.9 Blowout-type LVFWR is often treated with a suture repair.10
Follow-Up
The patient is doing very well 18 months after hospital discharge. Transthoracic echocardiogram demonstrated mild anterior and inferior hypokinesis with a left ventricular ejection fraction of 65%.
Conclusions
We report the case of a woman with TS and diabetes presenting with DKA precipitated by an unrecognized myocardial infarction due to multivessel SCAD that was complicated by LVFWR. It is unclear if TS predisposed our patient to multivessel SCAD. Recognizing myocardial infarction as a precipitant of DKA is important and prompt treatment of LVFRW can be lifesaving.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Left Coronary Angiogram. Left coronary angiogram demonstrating multivessel SCAD with subtotal left anterior descending artery occlusion and complete occlusion distally and pruning of distal first and second diagonal arteries. The major obtuse marginal is completely occluded.
Right Coronary Angiogram. Right coronary artery demonstrating SCAD in right ventricular marginal branch, occlusion of posterior descending artery. and dissection involving the distal posterolateral vessel. Abbreviation as in Video 1.
References
- 1.Pujari S.H., Agasthi P. StatPearls [Internet] StatPearls Publishing; 2022. Left ventricular rupture. Accessed November 2022. https://www.ncbi.nlm.nih.gov/books/NBK559271/ [Google Scholar]
- 2.Hayes S.N., Tweet M.S., Adlam D., et al. Spontaneous coronary artery dissection: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76:961–984. doi: 10.1016/j.jacc.2020.05.084. [DOI] [PubMed] [Google Scholar]
- 3.Zekavat S.M., Chou E.L., Zekavat M., et al. Fibrillar collagen variants in spontaneous coronary artery dissection. JAMA Cardiol. 2022;7:396–406. doi: 10.1001/jamacardio.2022.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silberbach M., Roos-Hesselink J.W., Andersen N.H., et al. Cardiovascular health in Turner syndrome: a scientific statement from the American Heart Association. Circ Genom Precis Med. 2018;11 doi: 10.1161/HCG.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 5.Gravholt C.H., Viuff M.H., Brun S., Stochholm K., Andersen N.H. Turner syndrome: mechanisms and management. Nat Rev Endocrinol. 2019;15:601–614. doi: 10.1038/s41574-019-0224-4. [DOI] [PubMed] [Google Scholar]
- 6.Kaefer K., Botta I., Mugisha A., et al. Acute coronary syndrome and diabetic keto acidosis: the chicken or the egg? Ann Transl Med. 2019;7:397. doi: 10.21037/atm.2019.07.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cerrato E., Giacobbe F., Quadri G., et al. Antiplatelet therapy in patients with conservatively managed spontaneous coronary artery dissection from the multicentre DISCO registry (published correction appears in Eur Heart J. 2021;43:87. Eur Heart J. 2021;42:3161–3171. doi: 10.1093/eurheartj/ehab372. [DOI] [PubMed] [Google Scholar]
- 8.Alzayer H., Bossard M., Ahsan S., Tsang M., Whitlock R., Sheth T. A case of spontaneous coronary artery dissection complicated by free wall rupture. Can J Cardiol. 2017;33:1736.e13–1736.e15. doi: 10.1016/j.cjca.2017.09.021. [DOI] [PubMed] [Google Scholar]
- 9.Matteucci M., Formica F., Kowalewski M., et al. Meta-analysis of surgical treatment for postinfarction left ventricular free-wall rupture. J Card Surg. 2021;36:3326–3333. doi: 10.1111/jocs.15701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matteucci M., Fina D., Jiritano F., et al. Treatment strategies for post-infarction left ventricular free-wall rupture. Eur Heart J Acute Cardiovasc Care. 2019;8:379–387. doi: 10.1177/2048872619840876. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Left Coronary Angiogram. Left coronary angiogram demonstrating multivessel SCAD with subtotal left anterior descending artery occlusion and complete occlusion distally and pruning of distal first and second diagonal arteries. The major obtuse marginal is completely occluded.
Right Coronary Angiogram. Right coronary artery demonstrating SCAD in right ventricular marginal branch, occlusion of posterior descending artery. and dissection involving the distal posterolateral vessel. Abbreviation as in Video 1.