Abstract
There is some, but inconsistent, evidence to suggest that matching patient treatment preference enhances treatment engagement and outcome. The current study examined differential preferences and factors associated with treatment preference for 12-week group cognitive behavioral therapy (CBT), yoga, or stress education in 226 adults with generalized anxiety disorder (GAD; 70% female, Mean age=33±13.5). In a subsample of 165 patients who reported an intervention preference and were randomized to yoga or CBT, we further examined whether match to preferred intervention improved the primary treatment outcome (responder status on Clinical Global Impressions Scale) and engagement (dropout, homework compliance). Preferences for CBT (44%) and yoga (40%) were similar among patients. Women tended to prefer yoga (OR=2.75, p=.01) and CBT preference was associated with higher baseline perceived stress (OR=0.92, p=.04) and self-consciousness meta-cognitions (OR=0.90, p=.02). Among those not matched to their preference, treatment response was higher for those receiving CBT than yoga (OR=11.73, p=0.013); there were no group differences for those matched to their treatment preference. In yoga, those who received their preference were more likely to drop than those who did not (OR=3.02, 95% CI=[1.20, 7.58], p=0.037). This was not the case for CBT (OR=0.37, 95% CI=[0.13, 1.03], p=0.076). Preference match did not predict homework compliance. Overall, results suggest that treatment preference may be important to consider to optimize outcome and engagement; however, it may vary by treatment modality. Future research incorporating preference, especially with yoga for anxiety, is aligned with personalized medicine.
Trial Registration:
clinicaltrials.gov: NCT01912287; https://clinicaltrials.gov/ct2/show/NCT01912287
Keywords: generalized anxiety disorder, cognitive-behavioral therapy, yoga, preference, match, engagement
Introduction
Generalized anxiety disorder (GAD), characterized by chronic, persistent worry, is common, with a lifetime prevalence of 7.8% in the United States (Ruscio et al., 2017). GAD is associated with substantial psychological distress and functional impairment (Ruscio et al., 2017). Despite the existence of highly effective, evidence-based treatments, including cognitive behavioral therapy (CBT; Carpenter et al., 2018), less than 50% of affected individuals seek treatment (Ruscio et al., 2017; Young et al., 2001). To optimize treatment engagement and outcomes for patients with GAD, it is important to better understand factors that drive interest in care, including specific treatment preferences, and their impact on outcomes.
Better understanding patient treatment preferences and their impact aligns with the movement towards personalized medicine, promoted by the National Institutes of Health and the U.S. Food and Drug Administration, which aims to tailor treatment approaches to optimize engagement and outcomes (Ashley, 2015; Hamburg and Collins, 2010; Insel, 2009). Further, guidelines for evidence-based practice recommend the integration of the best research evidence with clinical expertise and patient preference in the selection and implementation of psychiatric treatment (American Psychological Association, 2005). Meta-analyses suggest a small but significant effect of receiving preferred as compared to non-preferred psychosocial intervention options on better treatment outcomes (effect sizes: d=0.17 to d=0.28), greater satisfaction (effect size: d=0.34) and lower dropout (Lindhiem et al., 2014; Swift et al., 2018). However, the majority of studies in these meta-analyses examined preference for evidence-based psychotherapy (e.g., CBT) and medication rather than mind-body and integrative interventions, such as yoga or mindfulness-based treatments. Mind-body interventions may circumvent common barriers to engagement in CBT, such as cost, time constraints, lack of access, and stigma (Goetter et al., 2020). Yoga, in particular, is very popular and growing rapidly in prevalence. The 2017 U.S. National Health Interview Survey (Clarke et al., 2018) showed that 14.3% of the adult population was practicing yoga, a substantial increase from 6.1% in 2007 and 9.5% in 2012 (Clarke et al., 2015). The 2016 Yoga in America Study identified 36.7 million yoga practitioners in the US, with 56% of participants reporting engaging in yoga for stress relief, the second most popular reason for yoga practice after flexibility (61%) (Yoga Alliance, 2016.). Nonetheless, little is known about whether patients with anxiety would choose yoga if given access to both yoga and an evidence-based psychotherapy, such as CBT. Given the popularity of yoga and growing evidence that yoga may be an efficacious intervention for anxiety (Cramer et al., 2018; Hofmann et al., 2016) as well as the movement towards personalized medicine, it is important to understand what patient factors are associated with specific preferences when offered a choice between CBT or yoga, and whether baseline preferences contribute to differential treatment outcome and engagement.
Primary analyses from a recent three-arm randomized controlled trial (RCT) comparing the efficacy of CBT, yoga, or stress education group interventions for patients with GAD found that treatment response rates were higher for both yoga and CBT as compared to stress education (SE). However, yoga was not found to be as effective as CBT (Simon et al., 2021). It remains unclear if preference for a gold-standard, evidence-based intervention (CBT) vs. a popular mind-body approach (yoga) may have played a role in outcome and engagement in this trial. The present study is a secondary analysis that aims to examine preference data from participants with GAD in the parent RCT (Simon et al., 2021) to: 1) quantify baseline preferences for each intervention as well as examine psychological and demographic predictors of preference; 2) assess the impact of receiving preferred vs. non-preferred treatment on treatment response; and 3) test the impact of receiving preferred vs. non-preferred treatment on engagement (dropout, homework compliance). These hypotheses were pre-registered: https://osf.io/eg4v3/. We hypothesized that comparable proportions of the sample would prefer CBT and yoga given the evidence base supporting CBT alongside the popularity and possible lower stigma of yoga, and that both would be preferred over SE. Although prior data guiding predictors of preference are limited, based on research supporting specific moderators of response (e.g., Schneider et al., 2015) and reasons for engaging in yoga practice (e.g., stress relief; Yoga Alliance, 2016), we hypothesized that higher baseline mindfulness and perceived stress would be associated with yoga preference, whereas those more focused on anxiety-related cognitions would consider CBT a better fit. Further, we hypothesized that those who received their treatment preference would be more likely to respond to treatment, show greater homework compliance, and be less likely to dropout than those receiving their non-preferred treatment, aligned with findings from prior meta-analyses (Lindhiem et al., 2014; Swift et al., 2018).
Material and Methods
Study Design
Detailed methods (Hofmann et al., 2015) and primary outcome (Simon et al., 2021) of the parent trial (Generalized Anxiety-A Treatment Evaluation [GATE]; clinicaltrials.gov identifier: NCT01912287) have been published elsewhere. Briefly, participants were randomized in a planned 2:2:1 allocation using permuted block randomization to one of three 12-week group interventions: 1) CBT (n=90), 2) yoga (n=93), or 3) stress education (n=43) with recruitment and enrollment occurring at two academic centers (Boston University and Massachusetts General Hospital) from December 2013 through October 2019. The study was approved by the local Institutional Review Boards and was carried out in accordance with the Declaration of Helsinki. After thorough explanation of study procedures, written informed consent was obtained.
Participants
Participants were 226 men and women (70% female, Mean age=33.4±13.5) with a primary DSM-5 diagnosis of GAD recruited by advertisement and clinical referral. Exclusion criteria included current posttraumatic stress disorder, substance use disorders, eating disorders, significant suicidal ideation, or mental disorder due to a medical or neurocognitive condition; and lifetime psychosis, bipolar disorder, or developmental disorders. Those who had completed more than five yoga or CBT sessions in the past five years were also excluded. Participants were required to be off psychotropic medication for at least two weeks prior to baseline or on a stable dose for at least six weeks prior to enrollment. All participants received medical clearance and were excluded if they had any physical conditions, injuries, or musculoskeletal problems that would interfere with participation in yoga.
Measures
Preference.
Participants were administered a single item prior to randomization asking, “If you had the choice, which intervention would you prefer to receive?” Options were yoga, CBT, SE, or no preference. Participants were allowed to choose only one option. These data were blinded from therapists and independent evaluators until the data analysis phase of the study. All intervention options were thoroughly described in the consent form. Every effort was made to ensure that each treatment option was presented as equally beneficial. Data from the Credibility and Expectancy questionnaire administered at baseline, after randomization, supports the idea that participants in each condition had similar ratings of the credibility and expectancy of their particular treatment on this 5-item credibility and expectancy questionnaire (for yoga, M=14.93 (4.85); for CBT, M=14.75 (4.77); for SE, M=15.38 (4.86), p=.794).
Treatment outcome.
The primary outcome, mirroring that of the parent trial (Simon et al., 2021), was responder status, defined as Clinical Global Impression of Improvement (CGI-I) score of ≤2 (“much improved” or “very much improved”) at post-treatment (Week 12). The CGI-I is a well validated measure that assesses symptom improvement or worsening on a Likert scale of 1-7 with lower scores indicating more improvement (Guy, 1976). CGI-I was measured biweekly beginning at Week 2 and was administered by trained independent evaluators, of at least a Masters level, blinded to intervention condition. Interrater reliability was assessed on 19% of assessments (n=91) and indicated strong rater agreement (Simon et al., 2021).
Engagement.
Treatment engagement was measured in two ways: 1) treatment completion (dropout); and 2) homework compliance. Treatment completion was defined as attending sessions through and including week 12, or if week 12 was not completed meeting the pre-specified definition of compliance (i.e., attending 10 or more sessions). Those who were not treatment completers were considered dropouts. Homework compliance was measured weekly. Participants kept a daily homework log and trained study staff reviewed homework completion with each participant weekly to complete a summary compliance rating on a Likert scale from 0-6 where 0=no homework completed, 3=moderate homework completion, and 6=completed all homework.
Baseline characteristics.
Baseline characteristics hypothesized to be associated with treatment preference were mindfulness, perceived stress, and meta-cognitions. The Five-Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006) measures trait-like aspects of mindfulness including observing experience, describing/labeling, non-judging of self-experience, and non-reacting to internal experience. Higher scores indicate better mindfulness skills. Perceived stress was assessed with the 10-item Perceived Stress Scale (PSS; Cohen et al., 1983), which measures the degree to which situations are appraised as stressful. The Meta-Cognitions Questionnaire (MCQ; Cartwright-Hatton and Wells, 1997) is a 65-item instrument used to assess beliefs people have about their thinking. It includes five subscales: 1) positive beliefs about worry, 2) negative beliefs about the uncontrollability of thoughts, 3) lack of cognitive confidence, 4) negative beliefs about thoughts in general, and 5) cognitive self-consciousness. Higher scores on the PSS and MCQ subscales indicate worse functioning. Participants also self-reported age, gender, race, and ethnicity.
Interventions
Details of the three interventions are published (Hofmann et al., 2020, 2015). Briefly, all interventions were conducted in a weekly group format over the course of 12 weeks and delivered in cohorts of 3 to 6 individuals. CBT consisted of seven modules: (1) goal setting, motivation, and psychoeducation, (2) progressive muscle relaxation, (3) cognitive restructuring, (4) meta-cognitive strategies, (5) worry exposures, (6) behavioral changes, and (7) goal evaluations and relapse prevention. The yoga intervention utilized Kundalini Yoga as taught by Yogi Bhajan, which employs physical postures, breathing techniques, relaxation exercises, and meditation practices. CBT was delivered by Masters or doctoral level psychologists who were trained and regularly supervised by a CBT expert (SGH). Yoga was overseen by a yoga expert (SBK), and a qualified doctoral-level supervisor oversaw SE, which included psychoeducational information about stress. For all interventions, participants were instructed to complete daily 20-minute home practice (homework).
Data Analysis
Baseline demographic and psychological characteristics of the full sample (n=226) were summarized using frequency and proportion for categorical variables, and mean and standard deviation for continuous variables. Differences in proportions of treatment preferences as well as differences in match vs. non-match between treatment preference and randomization were assessed using chi-squared tests. To assess the associations between baseline participant characteristics and treatment preference, a multivariable logistic regression model was used to predict yoga preference (versus CBT) among the subgroup of participants who endorsed a preference for either yoga or CBT (n=182). Participants who preferred SE were not included in this analysis given the few who preferred SE.(n=16). The logistic regression included the following predictors, per the preregistration: gender, age, FFMQ score, PSS score, and MCQ subscale scores (self-consciousness, uncontrollability, worry, competence, negative). Because treatment preference was not randomly assigned, characteristics that were significantly associated with treatment preference were included as covariates in the engagement analyses as outlined below, to adjust for potential confounding variables.
To examine the effect of treatment preference on treatment outcome, only participants randomly assigned to either yoga or CBT (not SE) who endorsed a preference for yoga, CBT, or SE were included in analyses (n=19 indicated no preference; these participants were not included in this analysis). The primary treatment outcome (responder status) was the pre-specified study primary outcome (https://clinicaltrials.gov/ct2/show/NCT01912287) at post-treatment (week 12), consistent with the primary paper (Simon et al., 2021). Hence, to assess the effect of preference match on responder status, we used a generalized linear mixed model (GLMM), employing a logistic linking function and binomial distribution. Repeated assessments of responder status through post-treatment (Week 12) were nested within participants, who were nested within treatment cohort. The GLMM model included treatment assignment, treatment preference match (match vs. non-match), the interaction of treatment assignment and treatment preference match, and time, with nested random effects of intercepts for participants within treatment cohorts. Time was centered at Week 12 (the post-treatment assessment) so that comparisons between treatment groups and between treatment preferences could be tested at the post-treatment assessment. Time was modeled as quadratic to match methods in the primary paper (Hofmann et al., 2015; Simon et al., 2021). Per the preregistration, the model also included interactions between the linear time component, treatment preference match, and treatment assignment, and the treatment assignment x treatment preference match interaction. Follow-up GLMM analyses examined the effects of preference match and non-match within each treatment group (CBT and yoga), as well as contrasts between treatment groups within preference match and non-match.
Treatment engagement was measured by dropout rates and homework compliance. Dropout (yes/no) was modeled using a multivariable logistic regression with the following predictors: preference match, treatment, preference match x treatment, and characteristics significantly associated with baseline preferences (i.e., participant gender, baseline MCQ-self-consciousness, and baseline PSS). For the analysis of weekly homework compliance scores (a continuous outcome), we used a multilevel model with repeated assessments nested within participants, who were nested within treatment cohort. The analysis included the same predictors that were in the dropout analysis, plus linear and quadratic time (to model the repeated measures over time). It also included the pairwise interactions between linear time and both treatment preference match, and treatment assignment, as well as with their interaction, and a random intercept for participants and for treatment cohorts.
All significance tests were two-tailed (p<0.05). Within each analysis, all contrasts between preference and treatment groups were adjusted for multiple comparisons using Benjamini-Hochberg criterion controlling for false discovery rate at 5%. Analyses used R 4.0.2 (library lme4) software.
Results
Treatment preference
The majority of participants in the full sample indicated a pre-randomization preference for either CBT (44%, n=97) or yoga (40%, n=87), with only 7% (n=16) preferring SE and 9% (n=19) indicating no preference. Preferences for CBT (χ2(1)=16.4, p<.001) and yoga (χ2(1)=13.4, p<.001) were significantly greater than preference for SE, but not different from each other (χ2(1)=0.54, p=.46). See Table 1 for baseline demographic and clinical characteristics by preference.
Table 1.
Baseline demographics and clinical characteristics by preference
| Cognitive behavioral therapy (n=97) |
Yoga (n=87) |
Stress education (n=16) |
No preference (n=19) |
|
|---|---|---|---|---|
| Age, mean (SD) | 33.4 (12.5) | 31.9 (12.8) | 37.6 (16.9) | 33.3 (14.9) |
| Male, n (%) | 36 (37.1%) | 17 (19.5%) | 8 (50%) | 5 (26.3%) |
| Race/ethnicity, n (%) | ||||
| White (non-Hispanic) | 74 (76.3%) | 61 (70.1%) | 11 (68.8%) | 10 (52.6%) |
| Hispanic | 9 (9.3%) | 9 (10.3%) | 4 (25%) | 5 (26.3%) |
| Black | 3 (3.1%) | 5 (5.8%) | 0 (0%) | 1 (5.3%) |
| Asian/Pacific Islander | 8 (8.3%) | 9 (10.3%) | 0 (0%) | 2 (10.5%) |
| Other | 3 (3.1%) | 3 (3.5%) | 1 (6.3%) | 1 (5.3%) |
| Educational level, n (%) | ||||
| High school, technical school, or some college | 14 (14.4%) | 15 (17.2%) | 4 (25%) | 3 (15.8%) |
| College graduate | 40 (41.2%) | 40 (46.0%) | 7 (43.8%) | 10 (52.6%) |
| Graduate or professional school (some or completed) | 43 (44.3%) | 31 (35.6%) | 4 (25%) | 6 (31.6%) |
| Comorbid psychiatric diagnoses (>5% prevalence) | ||||
| Social anxiety disorder | 47 (48.5%) | 34 (39.1%) | 6 (37.5%) | 10 (52.6%) |
| Major depressive disorder | 28 (28.9%) | 11 (12.6%) | 2 (12.5%) | 2 (10.5%) |
| Specific phobia | 18 (18.6%) | 15 (17.2%) | 5 (31.2%) | 2 (10.5%) |
| Panic disorder | 10 (10.3%) | 8 (9.2%) | 2 (12.5%) | 3 (15.8%) |
| Agoraphobia | 6 (6.2%) | 5 (5.8%) | 2 (12.5%) | 2 (10.5%) |
| Meta-cognitions Questionnaire, mean (SD) | ||||
| Positive beliefs about worry | 34.81 (10.70) | 35.73 (12.02) | 32.31 (9.82) | 36.21 (10.38) |
| Beliefs about uncontrollability and danger of worry | 47.93 (8.81) | 42.41 (10.07) | 32.94 (12.00) | 43.35 (9.13) |
| Meta-cognitive efficiency | 21.45 (6.57) | 20.46 (6.11) | 21.19 (7.32) | 20.19 (6.44) |
| General negative beliefs | 28.48 (7.53) | 25.99 (8.32) | 25.50 (9.22) | 26.65 (8.75) |
| Cognitive self-consciousness | 20.53 (4.26) | 18.58 (4.61) | 17.75 (4.52) | 20.47 (3.60) |
| Perceived Stress Scale, mean (SD) | 25.33 (4.89) | 22.57 (5.53) | 23.25 (5.21) | 21.47 (5.28) |
| Five Facet Mindfulness Questionnaire, mean (SD) | 113.18 (18.52) | 115.29 (15.53) | 111.38 (17.63) | 111.14 (17.20) |
Note. Data are missing for education level (n=2) and specific phobia comorbid diagnosis (n=1).
Forty-seven percent (n=41) of those who preferred yoga and 44% (n=43) who preferred CBT were randomized to their matched preference (“match”; those not randomized to their preference referred to as “non-match.”). These proportions were similar to the proportion randomly assigned to yoga (41%) and CBT (40%) across the study. The proportion of matched preference participants did not differ between CBT and yoga (χ2(4)=3.3, p=.51). As expected with randomization that was blind to preference, baseline demographic and clinical (i.e., FFMQ, PSS, MCQ subscales) characteristics did not significantly differ by preference match or non-match (all p>.17).
Characteristics associated with preference for yoga or CBT
In our sample of 182 participants who expressed a preference for either yoga or CBT, cognitive self-consciousness, a meta-cognitions subscale, was related to preference for CBT over yoga (OR=0.90, 95% CI=[0.83, 0.98], z=−2.39, p=.02). This result was consistent with our hypotheses. Higher baseline levels of perceived stress were also associated with preference for CBT over yoga, though we hypothesized the opposite (OR=0.92, 95% CI=[0.85, 1.00], z=−2.04, p=.04). Female gender was the only characteristic associated with greater preference for yoga over CBT (OR=2.75, 95% CI=[1.27, 5.94], z=2.56, p=.01). Contrary to hypotheses, baseline mindfulness was not significantly associated with preference for either yoga or CBT (OR=1.00, 95% CI=[0.97, 1.02], z=−0.24, p=.81). Other baseline characteristics, such as age (OR=0.99, 95% CI=[0.96, 1.02], z=−0.65, p=.52) and other MCQ subscales (all p>.09), were not significantly associated with preference.
Effect of preference match on treatment outcome and engagement
Treatment outcome.
There was a significant treatment assignment x treatment preference match interaction (OR=0.11, 95% CI=[0.02, 0.77], p=.026). Contrasts between preference match groups (matched vs. non-matched) within treatment group did not show an effect of preference match on post-treatment (Week 12) responder status within either yoga (OR=3.28, 95% CI=[0.70, 15.35], t=1.51, p=.26), or CBT (OR=0.38, 95% CI=[0.08, 1.79], t=−1.23, p=.29). Among preference matched participants, we detected no difference in the likelihood of treatment response between yoga and CBT (OR=1.35, 95% CI=[0.30, 6.03], t=0.30, p=.70). However, among non-matched participants, CBT was associated with higher odds of treatment response compared to yoga (OR=11.73, 95% CI=[2.27, 60.54], t=2.94, p=.01).
Treatment engagement.
In the match group, dropout was 26% for CBT versus 63% for yoga, whereas for the non-match group dropout rates were 40% for CBT versus 39% for yoga (Figure 2; Table 3). The odds of dropping out from yoga were higher for match compared to non-match participants (OR=3.02, 95% CI=[1.20, 7.58], z=2.35, p=.04), while this was not the case for CBT (OR=0.37, 95% CI=[0.13, 1.03], z=−1.90, p=.08). Further, in the match group, those randomized to CBT were less likely to drop compared to those randomized to yoga (OR=0.15, 95% CI=[0.06, 0.42], z=−3.62, p=.001). This difference was not found for the non-match group (OR=1.27, 95% CI=[0.49, 3.24], z=0.49, p=.62).
Figure 2:
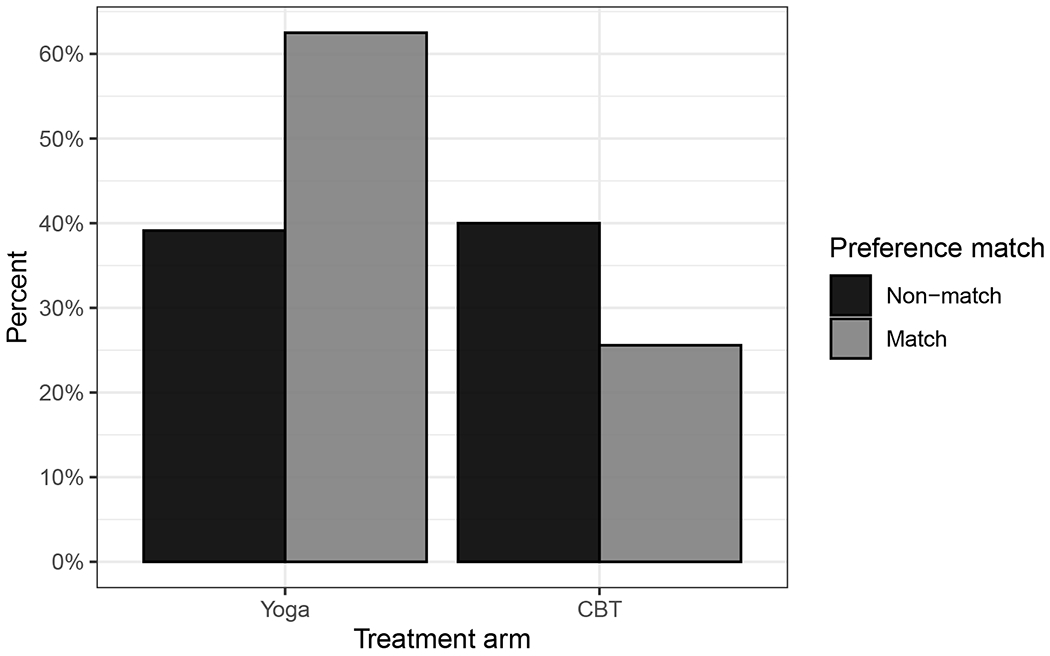
Observed dropout rate
Table 3:
Model results for treatment engagement: Dropout
| Odds ratio | 95% C.I. | p-value | |
|---|---|---|---|
| Intercept | 0.05 | [0.01, 0.53] | 0.013 |
| Treatment arm (CBT=1) | 1.27 | [0.49, 3.24] | 0.62 |
| Preference (match=1) | 3.02 | [1.20, 7.58] | 0.019 |
| Female=1 | 1.10 | [0.52, 2.34] | 0.80 |
| MCQ Self-conscious | 1.03 | [0.95, 1.11] | 0.46 |
| PSS Total Score | 1.08 | [1.01, 1.15] | 0.028 |
| Treatment arm x Preference | 0.12 | [0.03, 0.51] | 0.004 |
The overall mean for homework compliance was 3.79, with mean of 3.91 for match and 3.65 for non-match, indicating greater than moderate homework completion. There was no effect of preference match or treatment assignment on homework compliance (b(SE)=0.13 (0.25), p=.61 and (b(SE)=0.31 (0.30), p=.30), respectively) nor was there a significant match x treatment interaction (b(SE)=0.8 (0.36), p=.82).
Discussion
Mind-body and integrative approaches to anxiety and stress relief, such as yoga, are exploding in popularity in community settings; however, little is known about preference for these approaches versus gold-standard interventions for anxiety, such as CBT, in clinical settings or when both options are available. Integrating patient preferences into treatment planning and understanding factors associated with treatment preference are aligned with personalized medicine, which involves tailoring treatment approaches to optimize engagement, outcome, and safety (Ashley, 2015; Hamburg and Collins, 2010; Insel, 2009).
In our treatment-seeking sample, CBT and yoga had similar preference rates (44% preferring CBT and 40% yoga). These findings are consistent with a recent trial of 250 anxious older adults that found that CBT and yoga preferences were similarly dispersed with 48% preferring CBT and 52% yoga (Brenes et al., 2020). These data suggest that when both options are available, at least within a clinical trials framework, CBT and yoga are preferred at similar rates by patients with GAD.
Contrary to hypotheses, higher baseline levels of mindfulness did not predict preference for yoga, suggesting that individuals may be open to mind-body interventions regardless of their pre-existing mindful awareness of their thoughts. This may be aligned with beliefs that yoga offers general stress relief as well as benefits to overall health (Yoga Alliance, 2016). Other baseline demographic and clinical factors were associated with treatment preference. As hypothesized, those with higher levels of cognitive self-consciousness (heightened awareness of one’s thinking) were more likely to prefer CBT; those with higher levels of perceived stress also preferred CBT, though our initial hypothesis was they would prefer yoga. This may be due to perceived stress, as measured by the PSS, reflecting cognitions related to stress as opposed to bodily sensations related to stress. Of note, women were more likely to prefer yoga, aligned with recent surveys indicating women are twice as likely to practice yoga as men (Clarke et al., 2018). It may be helpful to take these factors into consideration when personalizing treatment approaches for patients and to examine them further as moderating factors of treatment outcome. Additionally, psychoeducation for men about the potential benefits of yoga may be helpful when it is an appropriate option.
Available meta-analyses offer conflicting evidence about the impact of preference match on treatment outcomes in general, although no studies included yoga or other mind-body interventions as options. For example, meta-analyses of 26 (Lindhiem et al., 2014) and 53 studies (Swift et al., 2018) on the effects of receiving preferred versus non-preferred interventions, a subset of which examined patients with anxiety, found small, significant effects indicating improvement in treatment outcomes for those receiving their preferred treatment (d=0.15-0.28). However, a recent meta-analysis did not find that preference match vs. non-match impacted anxiety or depression outcomes (n=16 studies, d=0.01), remission rates (n=5 studies, risk ratio=1.03), or global outcomes (e.g., Global Assessment Scale, CGI; n=4 studies, d=0.15), but sample sizes were limited (Windle et al., 2020).
Our study adds to this literature by examining the impact of preference match vs. non-match on treatment response in a rigorous, well-powered study that includes a popular mind-body intervention available in the community, yoga. We found that match to intervention preference (vs. non-match) did not generally improve GAD treatment outcome in terms of the primary pre-specified outcome, treatment response, nor was treatment match a determinant of outcome within either treatment group. However, that does not mean that treatment match had no effect on outcome. We did find a significant differential effect of treatment group among those who did not receive their preferred treatment: those in CBT counter to their preference were significantly more likely to respond to treatment (82% responding) than those in yoga counter to their preference (45.2% responding; OR=11.73). Although these results were not consistent with initial hypotheses about the impact of preference matching, they may still indicate the importance of taking preference into account in treatment selection. In the parent trial, CBT responses rates (70.8%) were marginally higher than yoga response rates (54.2%; Simon et al., 2021). Although preference match was not a predictor within groups, the rates of treatment response were similar in the match groups for both CBT and yoga, but not in the non-match groups. CBT may still demonstrate efficacy in non-matched groups, but yoga may be less effective or require additional pre-class work to enhance outcomes if there is not initial preference for participation. Our results should be interpreted with caution, however, as the higher dropout rates in the yoga matched-preference group may have biased outcomes.
Regarding dropout, existing meta-analyses (Lindhiem et al., 2014; Swift et al., 2018; Windle et al., 2020) offer stronger evidence for the impact of preference match for either psychotherapy or medication options, suggesting that preferred intervention match is associated with lower likelihood of treatment dropout (OR=1.37-1.79; pooled risk ratio=0.67) than non-match. In our sample, this trend was evident for CBT, as those matched to their CBT preference had a 26% dropout rate and those not matched had a 40% dropout rate (comparison not significantly different). However, contrary to our hypotheses, those matched to their yoga preference (63% dropout) were more likely to drop than those not matched to their preference (40% dropout). This counterintuitive result may be partially explained by expectancy effects related to the intervention itself as well as its potential benefits (Kazdin, 1979). Recent yoga practice surveys have shown differences in reasons for initiating and continuing practice suggesting that initial perceptions of yoga and its benefits are less accurate among novices and the general population (Cartwright et al., 2020; Park et al., 2019). In a large survey of 1,702 adults, Kundalini yoga was the 4th most commonly practiced yoga style (11%) after Sivananda (22%), Ashtanga (16%), and Hatha (14%), so novices to yoga, like our participants, may be more familiar with other yoga styles leading to different expectations about the yoga intervention (Park et al., 2019). To manage expectancy effects, even when yoga is preferred, it is possible that psychoeducation may be helpful to align expectations about content and enhance engagement to reduce dropout for patients with anxiety disorders. More research is needed to examine these possibilities, and suggest future studies of yoga outcomes for anxiety should include assessment of preferences as well as expectations about the intervention itself.
This study has some limitations. Our sample was predominantly White and well-educated; therefore, results may not generalize to underrepresented populations. Secondly, the form of yoga (Kundalini Yoga) implemented in this study may not fully generalize to all yoga types. Further, information in the public about yoga may differ from our structured class with homework. This may have contributed to higher dropout rates in the yoga preference match group, as expectations of the yoga style and class may not have matched with preconceived notions and/or been impacted by characteristics of GAD itself, although this possibility would need to be tested in future work. Though we were unable to detect differences between the response rates of those randomized to their CBT or yoga preference, the design of the study is a limitation as it did not allow differentiation between effects of preference versus the intervention itself within subjects, and required that participants be willing to be randomized to any of the three interventions. Doubly randomized preference control trials offer a strategy to assess these individual within subject effects and could be utilized in RCTs evaluating effects of preference in the future (e.g., Zoellner et al., 2018).
Conclusions
The current study contributes to the research examining the hypothesis that treatment preference is an important consideration to enhance engagement and optimize outcomes. Improving treatment engagement and retention is particularly important given the high dropout rates in patients receiving psychotherapy for GAD. In the context of RCTs, dropout rates for GAD patients are 17%, or one in six patients (Gersh et al., 2017). These rates are even higher in community samples, where up to 75% of those likely affected with GAD do not get appropriate treatment (Wang et al., 2005). In addition to accounting for preference, incorporating detailed psychoeducation regarding treatment options and expectations could maximize recruitment and retention (Mills et al., 2011), and is worthy of study with yoga for anxiety in particular. Overall, understanding treatment preference, its correlates, and its effects on engagement and outcome are the first steps towards thoughtful personalized medicine.
Figure 1:
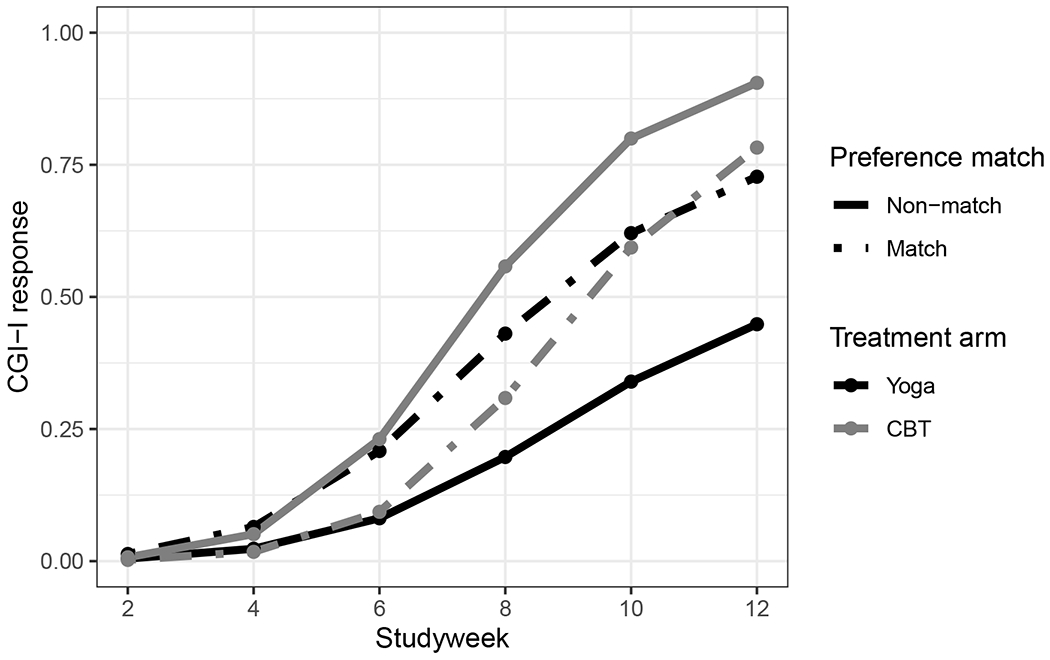
Model predicted CGI–I response
Table 2:
Model results for treatment outcome: CGI responder status
| Odds ratio | 95% C.I. | p-value | |
|---|---|---|---|
| Intercept | 0.81 | [0.26, 2.55] | 0.72 |
| Treatment arm (CBT=1) | 11.73 | [2.27 60.54] | 0.003 |
| Preference (match=1) | 3.28 | [0.70, 15.35] | 0.13 |
| Week (centered at week 12) | 1.17 | [0.87, 1.57] | 0.29 |
| Week (centered) squared | 0.97 | [0.94, 0.99] | 0.014 |
| Treatment arm x Pref. match | 0.11 | [0.02, 0.77] | 0.026 |
| Treatment arm x Week (centered) | 1.23 | [1.02, 1.48] | 0.030 |
| Preference x Week (centered) | 1.02 | [0.85, 1.22] | 0.86 |
References
- American Psychological Association, 2005. Policy statement on evidence-based practice in psychology. [Google Scholar]
- Ashley EA, 2015. The precision medicine initiative: a new national effort. JAMA 313, 2119–2120. 10.1001/jama.2015.3595 [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L, 2006. Using self-report assessment methods to explore facets of mindfulness. Assessment 13, 27–45. 10.1177/1073191105283504 [DOI] [PubMed] [Google Scholar]
- Brenes GA, Divers J, Miller ME, Anderson A, Hargis G, Danhauer SC, 2020. Comparison of cognitive-behavioral therapy and yoga for the treatment of late-life worry: A randomized preference trial. Depression and Anxiety 37, 1194–1207. 10.1002/da.23107 [DOI] [PubMed] [Google Scholar]
- Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JAJ, Hofmann SG, 2018. Cognitive behavioral therapy for anxiety and related disorders: A meta-analysis of randomized placebo-controlled trials. Depression and Anxiety 35, 502–514. 10.1002/da.22728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright T, Mason H, Porter A, Pilkington K, 2020. Yoga practice in the UK: a cross-sectional survey of motivation, health benefits and behaviours. BMJ Open 10, e031848. 10.1136/bmjopen-2019-031848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright-Hatton S, Wells A, 1997. Beliefs about Worry and Intrusions: The Meta-Cognitions Questionnaire and its Correlates. Journal of Anxiety Disorders 11, 279–296. 10.1016/S0887-6185(97)00011-X [DOI] [PubMed] [Google Scholar]
- Clarke TC, Barnes PM, Black LI, Stussman BJ, Nahin RL, 2018. Use of yoga, meditation, and chiropractors among US adults aged 18 and over. US Department of Health and Human Services, Centers for Disease Control and; …. [Google Scholar]
- Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL, 2015. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Report 1–16. [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R, 1983. A Global Measure of Perceived Stress. Journal of Health and Social Behavior 24, 385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cramer H, Lauche R, Anheyer D, Pilkington K, de Manincor M, Dobos G, Ward L, 2018. Yoga for anxiety: A systematic review and meta-analysis of randomized controlled trials. Depression and Anxiety 35, 830–843. 10.1002/da.22762 [DOI] [PubMed] [Google Scholar]
- Gersh E, Hallford DJ, Rice SM, Kazantzis N, Gersh H, Gersh B, McCarty CA, 2017. Systematic review and meta-analysis of dropout rates in individual psychotherapy for generalized anxiety disorder. Journal of Anxiety Disorders 52, 25–33. 10.1016/j.janxdis.2017.10.001 [DOI] [PubMed] [Google Scholar]
- Goetter EM, Frumkin MR, Palitz SA, Swee MB, Baker AW, Bui E, Simon NM, 2020. Barriers to mental health treatment among individuals with social anxiety disorder and generalized anxiety disorder. Psychological Services 17, 5–12. 10.1037/ser0000254 [DOI] [PubMed] [Google Scholar]
- Guy W, 1976. ECDEU assessment manual for psychopharmacology. US Department of Health, Education, and Welfare, Public Health Service [Google Scholar]
- Hamburg MA, Collins FS, 2010. The path to personalized medicine. N Engl J Med 363, 301–304. 10.1056/NEJMp1006304 [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Andreoli G, Carpenter JK, Curtiss J, 2016. Effect of Hatha yoga on anxiety: a meta-analysis. Journal of Evidence-Based Medicine 9, 116–124. 10.1111/jebm.12204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Baker AW, Carpenter JK, Curtiss J, Goetter EM, 2020. The anxiety skills workbook: Simple CBT and mindfulness strategies for overcoming anxiety, fear, and worry. New Harbinger Press, Oakland, CA. [Google Scholar]
- Hofmann SG, Curtiss J, Khalsa SBS, Hoge E, Rosenfield D, Bui E, Keshaviah A, Simon N, 2015. Yoga for generalized anxiety disorder: design of a randomized controlled clinical trial. Contemporary Clinical Trials 44, 70–76. 10.1016/j.cct.2015.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel TR, 2009. Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Archives of General Psychiatry 66, 128–133. 10.1001/archgenpsychiatry.2008.540 [DOI] [PubMed] [Google Scholar]
- Kazdin AE, 1979. Therapy outcome questions requiring control of credibility and treatment-generated expectancies. Behavior Therapy 10, 81–93. 10.1016/S0005-7894(79)80011-8 [DOI] [Google Scholar]
- Lindhiem O, Bennett CB, Trentacosta CJ, McLear C, 2014. Client preferences affect treatment satisfaction, completion, and clinical outcome: a meta-analysis. Clin Psychol Rev 34, 506–517. 10.1016/j.cpr.2014.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills N, Donovan JL, Wade J, Hamdy FC, Neal DE, Lane JA, 2011. Exploring treatment preferences facilitated recruitment to randomized controlled trials. J Clin Epidemiol 64, 1127–1136. 10.1016/j.jclinepi.2010.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL, Quinker D, Dobos G, Cramer H, 2019. Motivations for Adopting and Maintaining a Yoga Practice: A National Cross-Sectional Survey. The Journal of Alternative and Complementary Medicine 25, 1009–1014. 10.1089/acm.2019.0232 [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Hallion LS, Lim CCW, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Andrade LH, Borges G, Bromet EJ, Bunting B, Caldas de Almeida JM, Demyttenaere K, Florescu S, de Girolamo G, Gureje O, Haro JM, He Y, Hinkov H, Hu C, de Jonge P, Karam EG, Lee S, Lepine J-P, Levinson D, Mneimneh Z, Navarro-Mateu F, Posada-Villa J, Slade T, Stein DJ, Torres Y, Uda H, Wojtyniak B, Kessler RC, Chatterji S, Scott KM, 2017. Cross-sectional comparison of the epidemiology of dsm-5 generalized anxiety disorder across the globe. JAMA Psychiatry 74, 465–475. 10.1001/jamapsychiatry.2017.0056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider RL, Arch JJ, Wolitzky-Taylor KB, 2015. The state of personalized treatment for anxiety disorders: A systematic review of treatment moderators. Clinical Psychology Review 38, 39–54. 10.1016/j.cpr.2015.02.004 [DOI] [PubMed] [Google Scholar]
- Simon NM, Hofmann SG, Rosenfield D, Hoeppner SS, Hoge EA, Bui E, Khalsa SBS, 2021. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry 78, 13–20. 10.1001/jamapsychiatry.2020.2496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swift JK, Callahan JL, Cooper M, Parkin SR, 2018. The impact of accommodating client preference in psychotherapy: A meta-analysis. Journal of Clinical Psychology 74, 1924–1937. 10.1002/jclp.22680 [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC, 2005. Twelve-month use of mental health services in the united states: results from the national comorbidity survey replication. Archives of General Psychiatry 62, 629–640. 10.1001/archpsyc.62.6.629 [DOI] [PubMed] [Google Scholar]
- Windle E, Tee H, Sabitova A, Jovanovic N, Priebe S, Carr C, 2020. Association of patient treatment preference with dropout and clinical outcomes in adult psychosocial mental health interventions: a systematic review and meta-analysis. JAMA Psychiatry 77, 294–302. 10.1001/jamapsychiatry.2019.3750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alliance Yoga, 2016. Yoga in America Study. [Google Scholar]
- Young AS, Klap R, Sherbourne CD, Wells KB, 2001. The quality of care for depressive and anxiety disorders in the united states. Archives of General Psychiatry 58, 55–61. 10.1001/archpsyc.58.1.55 [DOI] [PubMed] [Google Scholar]
- Zoellner LA, Roy-Byrne PP, Mavissakalian M, Feeny NC, 2018. Doubly randomized preference trial of prolonged exposure versus sertraline for treatment of ptsd. AJP 176, 287–296. 10.1176/appi.ajp.2018.17090995 [DOI] [PubMed] [Google Scholar]


