Abstract
This systematic review and meta-analysis aimed to examine more recent data to determine the extent of lingual nerve injury (LNI) following the surgical extraction of mandibular third molars (M3M). A systematic search of three databases [PubMed, Web of Science and OVID] was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The inclusion criteria encompassed studies on patients who underwent surgical M3M extraction using the buccal approach without lingual flap retraction (BA-), buccal approach with lingual flap retraction (BA+), and lingual split technique (LS). The outcome measures expressed in LNI count were converted to risk ratios (RR). Twenty-seven studies were included in the systematic review, nine were eligible for meta-analysis. Combined RR for LNI (BA+ versus BA-) was 4.80 [95% Confidence Interval:3.28–7.02; P<0.00001]. The prevalence of permanent LNI following BA-, BA+ and LS (mean%±SD%) was 0.18±0.38, 0.07±0.21, and 0.28±0.48 respectively. This study concluded that there was an increased risk of temporary LNI following M3M surgical extractions using BA+ and LS. There was insufficient evidence to determine whether there is a significant advantage of BA+ or LS in reducing permanent LNI risk. Operators should use lingual retraction with caution due to the increased temporary LNI risk.
Introduction
Lingual nerve injury (LNI) can have a detrimental effect on a patient’s quality of life (QoL) [1]. It can occur as a result of iatrogenic injury following oral and maxillofacial surgery (e.g. orthognathic surgery) [2] and the removal of mandibular third molars (M3M) [3]. LNI can lead to complications such as altered touch and taste sensation, neuralgia, as well as impaired swallowing and speech [4].
LNI following M3M removal is usually transient, with studies reporting the chance of spontaneous recovery to be 60% and 35% at three and six months respectively [4]. When LNI lasts more than six months, there is a significantly lower chance of spontaneous recovery and may be considered permanent [5]. Bagheri et al. found that patients with LNI lasting longer than nine months have less than 10% chance of recovery [4]. The incidence of permanent LNI following the removal of M3M is approximately 0.04–0.6% [6]. Though the incidence of LNI is low, the severity of the complications is deemed significant enough that patients should be informed of the risk of LNI before the procedure.
The lingual nerve (LN) is a branch of the mandibular division of the trigeminal nerve [7]. It provides somatosensory innervation such as pain, thermal, and pressure sensation to the mucous membrane. The LN innervates the anterior two-thirds of the tongue, lingual gingiva of the mandibular teeth, and the mucosa of the floor of the mouth [7]. Approximately 1 cm below where the inferior alveolar nerve and LN separates, the LN is joined by the chorda tympani nerve [8]. The path of the LN varies between individuals. A study by Pogrel et al. found that, in twenty cadaveric heads, the LN was in a range of 1 to 7 mm away from the lingual plate of the M3M [9]. This highlights the potential risk of LNI when a lingual flap is retracted due to varying locations of the LN.
The traditional approach to surgically removing the M3M is through raising a buccal flap and removing buccal bone, which can be done without (BA-) or with (BA+) lingual retraction [10]. An alternative approach is raising a lingual flap, placing a lingual retractor, and removing lingual bone, known as the lingual split technique (LS) [11]. The use of a lingual retractor has been associated with a higher incidence of LN paraesthesia [12]. The argument for this technique is that the incidence of recovery is higher, as severing the LN is avoided by protecting it with instruments and retractors. For example, the flap can be raised using Molt’s or Ward’s curved periosteal elevator and retracted using Walter’s lingual retractor [10]. Some also argue that lingual flap retraction provides improved access to the surgical site [10]. However, there are contrasting opinions. A systematic review, published in 2001, concluded that such retraction increased the tendency of temporary LNI [12]. However, this result was from analysing research performed pre-1999. Although there was a recent systematic review that was published [13], there is currently no published up-to-date study that quantitatively outlines the risks involved post-1999.
Therefore, this systematic review and meta-analysis aims to examine more recent data to determine the extent of LNI following the surgical removal of M3M. More specifically, comparing the incidence between three techniques: BA-, BA+, and LS.
Materials and methods
Ethical approval
The systematic review was registered on the PROSPERO database (Registration number: CRD42020181836).
Study selection
The systematic review was registered on the PROSPERO database (Registration number: CRD42020181836) and conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14]. Two authors (J.L. and B.F.) independently conducted a systematic search of the literature in June 2022. The digital databases PubMed, Web of Science, and OVID were utilised to assess published studies that reported on the incidence of LNI following the surgical removal of M3M. Multiple searches were conducted using the following keyword combination: Firstly, “lingual nerve” AND buccal flap, retraction, oral surgery, third molar, lingual split. Secondly, “lingual nerve injury” AND buccal flap, retraction, oral surgery, third molar, lingual split. The connecting word ‘AND’ was used as a combination between the key words “lingual nerve” and “lingual nerve injury” and the rest of the search words. A limit was placed on the time of publication, with only articles published between May 1999 to June 2022 selected, as the previous landmark systematic review by Pichler and Beirne investigated studies from 1983 to May 1999 [12]. Grey literature was not assessed. All studies not in English were excluded. All studies except for systematic reviews were included. In the screening stage, the title and abstracts of publications were reviewed, and the duplicated studies were excluded. Subsequently, full-text copies were reviewed for eligibility for a systematic review. The inclusion criteria consisted of all studies on patients who have undergone surgical M3M extractions with BA-, BA+, or LS. Studies that did not meet the inclusion criteria were excluded. We utilised the software EndNote X9 (Clarivate, PA, USA) to organise the references and articles retrieved in the search. A consensus was reached after thorough discussion and gaining a third opinion from another author (J.P) if any discrepancies arose between the two examiners.
Selection criteria
Population: The population for this systematic review is patients who underwent the surgical removal of M3M
Intervention/Comparison: The intervention was the extraction of M3M with or without lingual retraction or using the lingual split technique
Outcome: The outcome being measured within our study was the incidence of lingual nerve injury following the surgical extraction of M3M
Search outcome
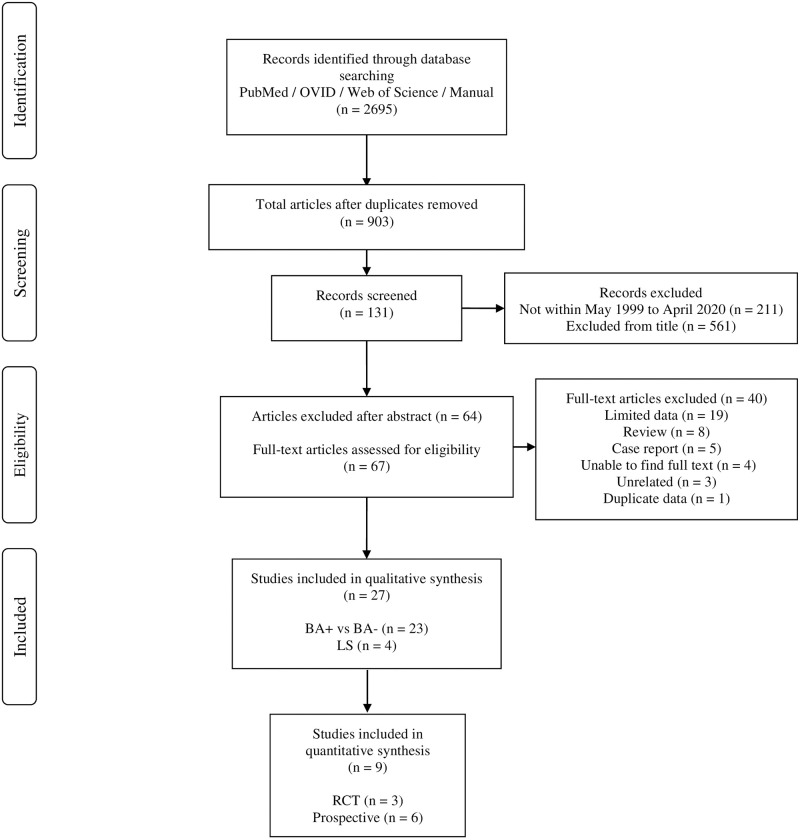
Fig 1 illustrates the outcomes of the search. From 2695 search results, 211 were excluded due to being outside the set time of publications, 1792 were removed due to being duplicates, 561 articles were excluded after analysing the title and a further 64 removed after analysing the abstract. Of the 67 potentially eligible studies, 40 citations were excluded. This left twenty-seven studies meeting the criteria and being suitable for inclusion in this systematic review [10, 15–40]. Of these, nine were suitable for quantitative synthesis and meta-analysis as information on LNI due to BA-, BA+, and LS was available [16, 17, 19, 21, 29, 32, 37, 38, 40].
Fig 1. Process of data collection in accordance with the PRISMA statement for systematic reviews.
Data extraction
The following were extracted: study design, prospective/retrospective design, number of patients, number of teeth, age of patients, location of study, intervention, types of lingual retractors used, comparison, outcomes, and quantitative data, which was the rate of lingual nerve injury, both permanent and temporary. The primary outcome was LNI. Within LNI, prevalence of temporary and permanent LNI was also calculated.
Data synthesis
The parameters for the meta-analysis consisted of analysing outcomes using the adopted risk ratio (RR) formula [41]:
a = Number of LNI cases after BA+
b = Number of LNI cases BA-
n1 = Total number of cases after BA+
n2 = Total number cases after BA-
After obtaining the necessary parameters, a meta-analysis was undertaken in accordance with Review Manager software (RevMan 5.0 for Windows, Last Update—2014). The level of significance was set at 95% (P< 0.05). Statistical heterogeneity was determined based on the Tau-squared test, with a threshold P-value of 0.1 and inconsistency (I2) test value greater than 50% indicating high heterogeneity [42].
Risk of bias
A critical appraisal tool to assess the quality of appropriate observation studies was utilised as per the checklist provided in the systematic review [43]. This included a series of questions with regards to the content of the Introduction, Methods, Results, Discussion, and Other sections. Furthermore, the cumulative count for these individual studies was tabulated.
Inter-agreement reliability
Inter-agreement reliability was calculated between the two independent reviewers, in the data extraction (identification, screening, eligibility, and inclusion) stage (%). In addition, kappa statistics as a measure to test the inter-agreement reliability amongst the reviewers was computed during the risk of bias stage [SPSS version 27.0 (IBM Company, Chicago, Il, USA)] [44].
Results
Study characteristics and study results
Table 1 highlights the characteristics of all studies included in the systematic review. Except for six studies [22, 30, 32, 33, 36, 37], all the studies were prospectively designed. Five of the prospective studies were randomised controlled trials [21, 23, 29, 35, 38]. There was a total number of 24,985 participants, aged between 12–89 years old, with 32,866 teeth analysed. Studies were undertaken in Australia, Brazil, China, Greece, Hong Kong, India, Jordan, Nigeria, Pakistan, Singapore, Spain, United Kingdom, and the United States. There was a total number of 388 cases of temporary LNI in the systematic review. In many studies the use of a lingual retractor was at the clinician’s discretion and the type of lingual retractor used varied (Table 2). Table 3 highlights the prevalence of temporary LNI as outlined by all studies [10, 15–40]. Temporary LNI accounted for an average prevalence of 2.64%±2.25% standard deviation (SD). Table 4 highlights the prevalence of permanent LNI as outlined by all studies [10, 15–40]. Permanent LNI accounted for an average prevalence of 0.24%±0.41%SD.
Table 1. Characteristics of the studies which utilised BA-, BA+ and LS technique.
| Author | Location | Prospective / Retrospective | Subjects | Teeth numbers | Age (Years) | Intervention | Comparison | Outcome (Primary and Secondary) | Quantitative data |
| Akadiri et al. 2009 | Nigeria | Prospective | 79 | - | - | Three-sided buccal flap with buccal guttering BA-: 79 |
- | Incidence and duration of complicating nerve injuries | LNI (BA-) cases total: 3 (4.0%) LNI (Day 14) cases total: 1 (1%) |
| Baqain et al. 2010 | Jordan | Prospective | 321 M: 92 F: 229 |
443 |
Mean 22 Range: 16–66 |
Buccal mucoperiosteal flap BA-: 299 Buccal mucoperiosteal flap + lingual retraction using a Howarth periosteal elevator. BA+: 110 No data: 34 |
- | Presence of postoperative lingual neurosensory deficit | LNI (BA-) cases total: 1 LNI (BA+) cases total: 10 Recovery within 6 months: 11 Permanent cases total: 0 Lingual flap retraction: OR = 22.821 (95% Confidence Intervals: 2.83–183.83; p = 0.003) |
| Bataineh et al. 2001 | Jordan | Prospective | 741 M: 417 F: 324 |
741 | <20: 61 20–30: 467 >30: 213 |
Buccal approach using a crestal incision extending to the distal of the second molar followed by a second incision extending downward and forward to the buccal sulcus BA-: 525 Buccal flap elevation + lingual retraction using a Howarth periosteal elevator BA+: 216 |
- | The rate and factors influencing sensory impairment of the inferior alveolar and lingual nerves after the removal of impacted mandibular third molars under local anaesthesia | LNI (BA-) cases total: 7 LNI (BA+) cases total: 12 Recovery within 12 months: 19 Permanent cases total: 0 |
| Bataineh and Batarseh 2016 | Jordan | Prospective | 53 M: 23 F: 30 |
66 | Mean: 23.3 Range: 16–43 |
Modified buccal flap without elevation of lingual flap BA-: 66 |
- | Evaluate a modified flap design for removal of lower third molars with avoidance of lingual flap elevation and its effect on postsurgical lingual nerve sensory impairment. | LNI cases total: 0 |
| Charan babu et al. 2013 | India | Prospective | 100 M: 69 F: 31 |
100 | 16–25: 49 26–35: 36 36–45: 9 46–55: 4 55–65: 2 |
Moore/Gillbe collar technique after placement of Ward’s incision by a single oral surgeon BA-: 92 Moore/Gillbe collar technique after placement of Ward’s incision + lingual retraction with unspecified periosteal elevator BA+: 8 |
- | To evaluate the incidence and various risk factors influencing the sensory deficit in case of lingual nerve injury (LNI) in individuals whose impacted mandibular third molars are surgically removed under local anaesthesia. | LNI (BA-) cases total: 1 LNI (BA+) cases total: 3 Recovery within 3 months: 4 Permanent cases total: 0 |
| Cheung et al. 2010 | Hong Kong | Prospective | 3595 M: 39% F: 61% |
4388 | Mean 27.2 Range 14–82 |
Extraction of 8s with or without raising of lingual flap Lingual flap raised: 1427 (33%) Attempt made to protect lingual tissue: 3477 (80%) |
- | To determine the incidence of subsequent neurosensory deficit due to inferior alveolar nerve (IAN) and lingual nerve (LN) injury, to examine possible contributing risk factors and to describe the pattern of recovery | LNI cases total: 30
Recovery after 24 months: 18/25 Permanent cases total: 7 (persist >2 years) (0.16%) |
| Gargallo-albiol et al. 2000 | Spain | Prospective (RCT) |
300 M: 140 F: 160 |
300 Totally impacted: 80 Partially erupted: 220 |
Mean: 27.4 Range: 14–59 |
Buccal mucoperiosteal flap BA-: 158 Buccal mucoperiosteal flap + lingual retraction with unspecified instrument BA+: 142 |
Comparison between protection of the lingual flap and without protection of the lingual flap | To evaluate the efficacy of protecting the lingual nerve by subperiosteal insertion of a retractor in 300 patients | LNI (BA-) cases total: 1 LNI (BA+) cases total: 3 Recovery after 21 days: 3 Recovery after 60 days: 1 Permanent cases total: 0 |
| Ge et al. 2016 | China | Retrospective |
89 M: 46 F: 43 |
110 Deeply impacted: 47 Fully impacted: 63 |
Mean 33.2 Range: 22–56 |
Lingual split technique using piezosurgery all by the same surgeon under LA LS: 110 |
- | Primary outcome: Evaluate the effect and safety of lingual split technique using piezosurgery for the extraction of lingually positioned impacted mandibular 3rd molars Success rate, operating time (from the 1st incision to the last suture), and the incidence of major complications Secondary outcome: Pain, swelling, restricted mouth opening, and the postoperative symptom severity (PoSSe) score at the postoperative 7-day |
LNI (LS) cases total: 6 (5.5%) Permanent cases total: 0 |
| Gomes et al. 2005 | Brazil | Prospective (RCT) |
55 | 110 |
- | Buccal flap with a buccal retractor BA-: 55 Buccal flap with buccal retractor + lingual flap retraction using Free’s elevator BA+: 55 Patients were randomly allotted to have 1 side operated with buccal flap only and the other side with buccal and lingual flap retraction |
Without lingual flap retraction Same patient, different technique for opposite side of mouth |
Primary outcome: To clinically evaluate the frequency, type, and risk factors for lingual nerve damage after mandibular third molar surgery with reference to lingual flap retraction. | LNI (BA-) cases total: 0 LNI (BA+) cases total: 5 Recovered within 3 months: 5 Permanent cases total: 0 |
| Janakiraman and Sanjay 2010 | India | Prospective | 119 | 119 | Mean 27 Range: 18–35 |
Standard buccal Ward’s mucoperiosteal flap BA-: 6 Standard buccal Ward’s mucoperiosteal flap + lingual flap retraction with unspecified periosteal elevator BA+: 113 |
- | To determine the incidence of injury to the inferior alveolar and lingual nerves following surgical removal of impacted mandibular third molars and to evaluate the various factors contributing to the same. | LNI (BA-) cases total: 0 LNI (BA+) cases total: 5 Recovery in 6 months: 2 Still under observation (permanent): 1 |
| Jerjes et al. 2006 | United Kingdom | Prospective | 1087 M: 505 F: 585 |
1087 Partially erupted: 857 |
Mean 23.3 Range 17–46 |
Envelope mucoperiosteal flap reflected and bone removal with a round bur in a straight hand- piece. Sectioning of tooth when needed. No lingual flap employed. BA-: 1087 |
- | The proportion of permanent sensory impairment of the inferior alveolar and lingual nerves and the factors influencing such prevalence after the removal of mandibular third molars under local anaesthesia. | LNI (BA-) cases total: 71 Permanent tongue paraesthesia 2 years after surgery: 11 |
| Jerjes et al. 2010 | United Kingdom | Prospective |
3236 M: 1445 F: 1791 |
3236 Partially impacted: 2572 Close to IAC: 2531 |
Mean: 24.2 Range: 17–36 17–20: 852 21–25: 49.2 26–30: 471 >30: 319 |
An envelope mucoperiosteal flap reflected and bone was removed bucco-distally. No lingual flap employed. No lingual split technique used. BA-: 3236 |
- | Earlier reports, including a preliminary study within our unit, have shown that the surgeon’s experience is one of the most influential factors in determining the likelihood of both permanent inferior alveolar nerve (IAN) and lingual nerve (LN) paraesthesia, following third molar surgery. The effect of this and other factors influencing such prevalence are assessed in this study. | LNI (BA-) cases total: 57 Recovery after 6 months: 5 Recovery after 6–18 months: 15 Cases present 18–24 months after surgery: 37 |
| Kale et al. 2014 | - | Prospective | 20 M: 13 F: 7 |
- | - | Standard Wards’ incision made in all cases. The tissue flap was reflected buccally, distally and lingually. The wide end of Howarth’s elevator was inserted adjacent to the lingual plate to protect the lingual nerve. Bone guttering on the buccal, distal and lingual side using straight fissure bur in low speed micrometre straight handpiece under copious irrigation. BA+: 20 |
- | To assess the clinical feasibility of lingual bone guttering technique for surgical extraction of mandibular third molars. | LNI (BA+) cases total: 0 |
| Lata and Tiwari 2011 | India | Prospective | 90 | - | - | Standard Terence Ward`s incision was made and after reflecting the buccal flap, a gutter in the disto-buccal bone was created. Bone removal done with motor-driven surgical bur under constant saline irrigation. Odontectomy or odontotomy procedure was done depending on the path of removal of the impacted tooth. No use of lingual retractor. BA-: 90 |
- | To determine the clinical incidence of lingual nerve injury following mandibular third molar removal and to analyse possible factors for the lingual nerve injury. | LNI (BA-) cases total: 6 LNI (6 months after surgery) cases total: 1 |
| Majeed et al. 2018 | Pakistan | Prospective (RCT) |
300 | 300 Right: 170 Left:130 |
Range: 21–50 21–30: 245 31–40: 40 41–50: 15 |
BA-: 200 BA+: 100 No other information provided |
- | To determine the incidence of lingual nerve injury and the effects of different variables on lingual nerve injury during mandibular third molars removal surgery. | LNI cases total: 18
|
| Malden and Maidment 2002 | United Kingdom | Retrospective | 260 | 260 | - | Mucoperiosteal flap raised buccal to the third molar. Distal relieving incision placed on retromolar pad to avoid all anatomical variants of the lingual nerve. Retracted with a Bowdler Henry rake retractor or Austin retractor. Lingual tissue retracted only to expose the occlusal aspect of the tooth or the superior aspect of mandibular bone covering the tooth or the crest of the lingual plate. No raising or elevating a lingual mucoperiosteal flap off the lingual aspect of the mandible. Tooth section with bone removal: 102 Bone removal without tooth section: 74 Soft tissue surgery: 84 BA-: 260 |
- | To determine if the incidence of lingual nerve damage differed to any significant extent from that reported elsewhere. To modify the operative technique, if indicated, to bring the incidence of nerve damage to within an accepted currently published standard. |
LNI (BA-) cases total: 1 Permanent cases total: 0. Returned to full sensation within 6 weeks |
| Mavrodi et al. 2015 | Greece | Prospective | - | 1210 Left: 47.3% Right: 52.7% |
Mean 48.5 Range: 15–82 |
Full thickness mucoperiosteal 3-cornered flap used in all cases 1. Classical bur technique: 470 2. Elevator placed on the buccal surface of the impacted molar to luxate the alveolar socket more easily: 740 Tooth sectioned 57.4% in group 1, 32.7% in group 2 BA-: 1210 |
- | To compare the efficacy and the postoperative complications of patients to whom two different surgical techniques were applied for impacted lower third molar extraction. | LNI cases total: 0 |
| Moss and Wake 1999 | United Kingdom | Retrospective | 1614 M: 605 F: 1009 |
2906 Removed with a lingual flap: 2088 |
Range: 12–89 | Buccal mucoperiosteal flap retraction BA-: 818 Buccal mucoperiosteal flap retraction + lingual flap retraction with the Hovell’s and Rowe retractors. BA+: 2088 |
- | To establish whether the deliberate raising of a lingual flap to allow the insertion of a broad lingual flap retractor in itself had any effect on lingual nerve morbidity. | LNI (BA-) cases total: 2 LNI (BA+) cases total: 16 Recovery within: 0–2 weeks: 8 3–6 weeks: 8 7–12 weeks: 1 13–25 weeks: 1 No permanent lingual sensory disturbance |
| Nguyen et al. 2014 | Australia | Retrospective | 6803 | 11599 | - | Buccal flap with bone removal and tooth division BA-: 11599 |
- | To assess the incidence of and risk factors for permanent neuro- logic injuries to the inferior alveolar nerve (IAN) or lingual nerve (LN) after the removal of third molars. |
LNI (BA-) cases total: 15 (0.15%) Temporary LNI cases total: 7 (0.069%) Permanent LNI cases total: 8 (0.079%) |
| Obiechina et al. 2001 | Nigeria | Prospective | 517 M: 297 F: 220 |
717 | >16 |
Bur technique with preservation of lingual plate BA-: 699 Lingual bone split technique LS: 18 |
- | To analyse the depth of impaction of mandibular third molars, the type of anaesthesia, the surgical method used and the outcome. | LNI (BA-) cases total: 3 (0.4%) LNI (LS) cases total: 6 (0.8%) Complete recovery of lingual/labial sensation within 10–21 days Permanent case totals: 0 |
| Pogrel and Goldman 2004 | United States | Prospective | 250 | - | - | Buccal flap raised and an appropriate buccal retractor placed (usually Minnesota-type retractor). Lingual flap then raised using Molt or Ward’s periosteal elevator. Walter’s lingual retractor was then placed Lingual flap + buccal flap with a specially designed lingual retractor BA+: 250 |
- | The traditional approach in the United States has been a buccal approach avoiding exposure or surgery on the lingual side of the crest of the ridge. An alternative technique is to deliberately expose the lingual tissues and retract the lingual nerve lingually before tooth removal. This study reports a trial of this technique. | LNI (BA+) cases total: 4 Recovery within 21 days: 3 Recovery within 60 days: 1 Permanent cases total: 0 |
| Praveen et al. 2007 | India | Prospective (RCT) |
90 | 90 | Mean: 38 Range: 14–62 |
Buccal mucoperiosteal flap with buccal bone removal and tooth division + lingual nerve protection using Howarth’s periosteal elevator: BA+: 30 Buccal mucoperiosteal flap + lingual nerve protection using Howarth’s periosteal flap + normal/modified lingual split technique using a chisel LS: 60 |
- | To compare the morbidity rates of the three different surgical techniques and their efficacy with regard to postoperative pain, swelling, labial and lingual sensation. | LNI (BA+) cases total: 0 LNI (LS) cases total: 3 Recovery after 7 days: 1 Recovery after 14 days: 1 Permanent cases total: 1 |
| Ramadorai et al. 2019 | Singapore | Retrospective | 1276 M: 458 F: 818 |
1276 | Mean: 30.5 Range: 15–80 |
Buccal bone removal without raising a lingual flap BA-: 1276 |
- | To ascertain the incidence of IAN and LN damage after mandibular third molar surgery in National Dental Centre Singapore. Secondary outcome: To identify the contributory factors for the risk of IAN and LN nerve injury on the basis of the data collected. |
LNI (BA-) cases total: 1 Recovery after 3 months: 1 Permanent cases total: 0 |
| Robinson et al. 1999 | United Kingdom | Retrospective | 200 | 200 | - | Buccal flap elevation without elevation of lingual mucoperiosteal flap: BA-: 110 Buccal flap elevation + Howarth periosteal elevator eased across the distal bone to the lingual side: BA+: 90 |
- | - | LNI (BA-) cases total: 1 LNI (BA+) cases total: 3 Complete recovery within 3 months Permanent cases total: 0 |
| Shad et al. 2015 | Pakistan | Prospective (RCT) |
380 M: 179 F: 201 |
380 | Mean: 25.6 Range: 18–38 |
Buccal flap elevation without elevation of lingual mucoperiosteal flap: BA-: 190 Buccal and lingual flap retraction + lingual flap retraction with Howarth’s periosteal elevator BA+: 190 |
- | - | LNI (BA-) cases total: 5 LNI (BA+) cases total: 17 Permanent cases total (BA-): 1 Although all showed signs of recovery within 3–6 months, 21 cases showed spontaneous recovery |
| Smith 2013 | United Kingdom | Prospective | 1000 | 1589 | Mean 33.9 Range: 13–87 |
Buccal envelope mucoperiosteal flap. Lingual retraction was not used electively unless a significant amount of distal or distolingual bone removal was anticipated. BA-: 1455 LS: 134 |
- | To identify the relative risk of damage to the inferior dental (ID) and lingual nerves in patients undergoing lower third molar removal. | LNI (BA-) cases total: 3 LNI (LS) cases total: 2 Permanent cases total (BA-): 1 (0.06%) |
| Yadav et al. 2014 | India | Prospective | 1200 | 1200 | Range: 18–45 | Buccal mucoperiosteal flap BA-: 576 Buccal mucoperiosteal flap + lingual retraction with Howarth’s periosteal elevator BA+: 624 |
- | Investigate the incidence of sensory impairment of the lingual nerves following lower third molar removal and to compare the outcome with various operative variables. | 1 week (Temporary) LNI (BA-) cases total: 10 LNI (BA+) cases total: 57 6 months (Permanent) LNI (BA-): 1 LNI (BA+): 3 |
BA+—Buccal approach with lingual flap retraction; BA-—Buccal approach without lingual flap retraction; F—Female; LNI—Lingual nerve injury; LS—Lingual split technique; M—Male; RCT—Randomised controlled trials
Table 2. Different types of lingual retractors used in M3M extraction.
| Purpose Built | Non-purpose built | No Lingual Retraction | Not specified |
|---|---|---|---|
| Moss and Wake 1999 | Baqain et al. 2010 | Akadiri et al. 2009 | Gargallo-albiol et al. 2000 |
| Pogrel and Goldman 2004 | Bataineh 2001 | Bataineh and Batarseh 2016 | Majeed et al. 2018 |
| Smith 2013 | Charan babu et al. 2013 | Lata and Tiwari 2011 | Obiechina et al. 2001 |
| Cheung et al. 2010 | Jerjes et al. 2006 | ||
| Ge et al. 2016 | Jerjes et al. 2010 | ||
| Gomes et al. 2005 | Malden and Maidment 2002 | ||
| Janakiraman and Sanjay 2010 | Mavrodi et al. 2015 | ||
| Kale et al. 2014 | Nguyen et al. 2014 | ||
| Praveen et al. 2007 | Ramadorai et al. 2019 | ||
| Robinson et al. 1999 | |||
| Shad et al. 2015 | |||
| Yadav et al. 2014 |
Non-purpose built = Freer, Molt, Obwegesser, Howarth
Purpose built = Hovell ’s, Walter’s lingual retractor, Rowe
Table 3. Prevalence of temporary LNI using BA-, BA+ and LS.
| Total Teeth | Temporary LNI due to: | Total Temporary LNI | Prevalence (BA-) | Prevalence (BA+) | Prevalence (LS) | Total Prevalence | |||
|---|---|---|---|---|---|---|---|---|---|
| BA- | BA+ | LS | |||||||
| Akadiri et al. 2009 | 79 | 3 | N/A | N/A | 3 | 3.80% | N/A | N/A | 3.80% |
| Baqain et al. 2010 | 443 | 1 | 10 | N/A | 11 | 0.23% | 2.26% | N/A | 2.48% |
| Bataineh 2001 | 741 | 7 | 12 | N/A | 19 | 0.94% | 1.62% | N/A | 2.56% |
| Bataineh and Batarseh 2016 | 66 | 0 | N/A | N/A | 0 | 0.00% | N/A | N/A | 0.00% |
| Charan babu et al. 2013 | 100 | 1 | 3 | N/A | 4 | 1.00% | 3.00% | N/A | 4.00% |
| Cheung et al. 2010 | 3595 | U | U | N/A | 30 | U | U | N/A | 0.83% |
| Gargallo-albiol et al. 2000 | 300 | 1 | 3 | N/A | 4 | 0.33% | 1.00% | N/A | 1.33% |
| Ge et al. 2016 | 110 | N/A | N/A | 6 | 6 | N/A | N/A | 5.45% | 5.45% |
| Gomes et al. 2005 | 110 | 0 | 5 | N/A | 5 | 0.00% | 4.55% | N/A | 4.55% |
| Janakiraman and Sanjay 2010 | 119 | 0 | 5 | N/A | 5 | 0.00% | 4.20% | N/A | 4.20% |
| Jerjes et al. 2006 | 1087 | 71 | N/A | N/A | 71 | 6.53% | N/A | N/A | 6.53% |
| Jerjes et al. 2010 | 3236 | 57 | N/A | N/A | 57 | 1.76% | N/A | N/A | 1.76% |
| Kale et al. 2014 | 20 | N/A | 0 | N/A | 0 | N/A | 0% | N/A | 0.00% |
| Lata and Tiwari 2011 | 90 | 6 | N/A | N/A | 6 | 6.67% | N/A | N/A | 6.67% |
| Majeed et al. 2018 | 300 | 6 | 12 | N/A | 18 | 2.00% | 4.00% | N/A | 6.00% |
| Malden and Maidment 2002 | 260 | 1 | N/A | N/A | 1 | 0.38% | N/A | N/A | 0.38% |
| Mavrodi et al. 2015 | 1210 | 0 | N/A | N/A | 0 | 0.00% | N/A | N/A | 0.00% |
| Moss and Wake 1999 | 2906 | 2 | 16 | N/A | 18 | 0.07% | 0.55% | N/A | 0.62% |
| Nguyen et al. 2014 | 11599 | 15 | N/A | N/A | 15 | 0.13% | N/A | N/A | 0.13% |
| Obiechina et al. 2001 | 717 | 3 | N/A | 6 | 9 | 0.42% | N/A | 0.84% | 1.26% |
| Pogrel and Goldman 2004 | 250 | N/A | 4 | N/A | 4 | N/A | 1.60% | N/A | 1.60% |
| Praveen et al. 2007 | 90 | N/A | 0 | 3 | 3 | N/A | 0.00% | 3.33% | 3.33% |
| Ramadorai et al. 2019 | 1276 | 1 | N/A | N/A | 1 | 0.08% | N/A | N/A | 0.08% |
| Robinson et al. 1999 | 200 | 1 | 3 | N/A | 4 | 0.50% | 1.50% | N/A | 2.00% |
| Shad et al. 2015 | 380 | 5 | 17 | N/A | 22 | 1.32% | 4.47% | N/A | 5.79% |
| Smith 2013 | 1589 | 3 | N/A | 2 | 5 | 0.19% | N/A | 0.13% | 0.31% |
| Yadav et al. 2014 | 1200 | 10 | 57 | N/A | 67 | 0.83% | 4.75% | N/A | 5.58% |
| 388 | Mean—1.24% ±1.91%SD | Mean—2.39% ±1.68%SD | Mean—2.44% ±2.11%SD | Mean—2.64% ±2.25%SD | |||||
SD—Standard deviation; N/A—Not applicable; U—Unspecified
Table 4. Prevalence of permanent LNI using BA-, BA+ and LS.
| Total Teeth | Permanent LNI due to: | Total Permanent LNI | Prevalence (BA-) | Prevalence (BA+) | Prevalence (LS) | Total Prevalence | |||
|---|---|---|---|---|---|---|---|---|---|
| BA- | BA+ | LS | |||||||
| Akadiri et al. 2009 | 79 | U | N/A | N/A | U (No follow up after 14 days) | U | N/A | N/A | U |
| Baqain et al. 2010 | 443 | 0 | 0 | N/A | 0 | 0.00% | 0.00% | N/A | 0.00% |
| Bataineh 2001 | 741 | 0 | 0 | N/A | 0 | 0.00% | 0.00% | N/A | 0.00% |
| Bataineh and Batarseh 2016 | 66 | 0 | N/A | N/A | 0 | 0.00% | N/A | N/A | 0.00% |
| Charan babu et al. 2013 | 100 | 0 | 0 | N/A | 0 | 0.00% | 0.00% | N/A | 0.00% |
| Cheung et al. 2010 | 3595 | U | U | N/A | 7 | U | U | N/A | 0.19% |
| Gargallo-albiol et al. 2000 | 300 | 0 | 0 | N/A | 0 | 0.00% | 0.00% | N/A | 0.00% |
| Ge et al. 2016 | 110 | N/A | N/A | 0 | 0 | N/A | N/A | 0.00% | 0.00% |
| Gomes et al. 2005 | 110 | 0 | 0 | N/A | 0 | 0.00% | 0.00% | N/A | 0.00% |
| Janakiraman and Sanjay 2010 | 119 | 0 | 1 | N/A | 1 | 0.00% | 0.84% | N/A | 0.84% |
| Jerjes et al. 2006 | 1087 | 11 | N/A | N/A | 11 | 1.01% | N/A | N/A | 1.01% |
| Jerjes et al. 2010 | 3236 | 37 | N/A | N/A | 37 | 1.14% | N/A | N/A | 1.14% |
| Kale et al. 2014 | 20 | N/A | 0 | N/A | 0 | N/A | 0.00% | N/A | 0.00% |
| Lata and Tiwari 2011 | 90 | 1 | N/A | N/A | 1 | 1.11% | N/A | N/A | 1.11% |
| Majeed et al. 2018 | 300 | 0 | 0 | N/A | 0 | 0.00% | 0.00% | N/A | 0.00% |
| Malden and Maidment 2002 | 260 | 0 | N/A | N/A | 0 | 0.00% | N/A | N/A | 0.00% |
| Mavrodi et al. 2015 | 1210 | 0 | N/A | N/A | 0 | 0.0% | N/A | N/A | 0.00% |
| Moss and Wake 1999 | 2906 | 0 | 0 | N/A | 0 | 0.00% | 0.00% | N/A | 0.00% |
| Nguyen et al. 2014 | 11599 | 8 | N/A | N/A | 8 | 0.07% | N/A | N/A | 0.07% |
| Obiechina et al. 2001 | 717 | 0 | N/A | 0 | 0 | 0.00% | 0.00% | 0.00% | 0.00% |
| Pogrel and Goldman 2004 | 250 | N/A | 0 | N/A | 0 | N/A | 0.00% | N/A | 0.00% |
| Praveen et al. 2007 | 90 | N/A | 0 | 1 | 1 | N/A | 0.00% | 1.11% | 1.11% |
| Ramadorai et al. 2019 | 1276 | 0 | N/A | N/A | 0 | 0.00% | N/A | N/A | 0.00% |
| Robinson et al. 1999 | 200 | 0 | 0 | N/A | 0 | 0.00% | 0.00% | N/A | 0.00% |
| Shad et al. 2015 | 380 | 1 | 0 | N/A | 1 | 0.26% | 0.00% | N/A | 0.26% |
| Smith 2013 | 1589 | 1 | N/A | 0 | 1 | 0.06% | N/A | 0.00% | 0.06% |
| Yadav et al. 2014 | 1200 | 1 | 3 | N/A | 4 | 0.08% | 0.25% | N/A | 0.33% |
| 72 | Mean—0.18% ±0.38%SD | Mean—0.07% ±0.21%SD | Mean—0.28% ±0.48%SD | Mean—0.24% ±0.41%SD | |||||
SD—Standard deviation; N/A—Not applicable; U—Unspecified
Meta-analysis
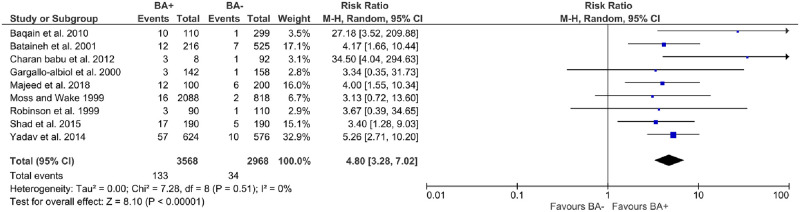
All studies that were included in the meta-analysis are outlined in Fig 2. Comparing BA+ vs BA-, the overall RR was 4.80 [95% Confidence Interval: 3.28–7.02; P < 0.00001], with a range of 3.13 to 34.50, and with negligible evidence of heterogeneity (I2 = 0%).
Fig 2. Forest plot outlining the risk of lingual nerve injury based on prospective clinical trials.
Risk of bias
Table 5 outlines the assessment of the studies included in the systematic review according to AXIS [45]. Individual studies were provided in Supplement 1. All of the studies had a clear aim, appropriate risk factors and outcome variables measured to the aims of the study, discussions and conclusions justified by the results. None of the studies justified their sample sizes. There were only two studies that addressed non-responders [28, 36], and only one study was internally consistent [20].
Table 5. Assessment of the studies included in the systematic review according to the appraisal tool for cross-sectional studies (AXIS).
| Questions | Yes | No | Uncertain | Not applicable |
|---|---|---|---|---|
| Introduction | ||||
| Were the aims/objectives of the study clear? | 27 | 0 | 0 | 0 |
| Methods | ||||
| Was the study design appropriate for the stated aim(s)? | 11 | 16 | 0 | 0 |
| Was the sample size justified? | 0 | 27 | 0 | 0 |
| Was the target/reference population clearly defined? | 19 | 8 | 0 | 0 |
| Was the sample frame taken from an appropriate population base so that it closely represented the target/reference population under investigation? | 19 | 0 | 8 | 0 |
| Was the selection process likely to select subjects/participants that were representative of the target/reference population under investigation? | 6 | 16 | 0 | 5 |
| Were measures undertaken to address and categorise non-responders? | 2 | 2 | 0 | 23 |
| Were the risk factor and outcome variables measured appropriate to the aims of the study? | 27 | 0 | 0 | 0 |
| Were the risk factor and outcome variables measured correctly using instruments/measurements that had been trialled, piloted or published previously? | 10 | 17 | 0 | 0 |
| Is it clear what was used to determine statistical significance and/or precision estimates? | 16 | 5 | 0 | 6 |
| Were the methods (including statistical methods) sufficiently described to enable them to be repeated? | 20 | 7 | 0 | 0 |
| Results | ||||
| Were the basic data adequately described? | 26 | 1 | 0 | 0 |
| Does the response rate raise concerns about non-response bias? | 0 | 27 | 0 | 0 |
| If appropriate, was information about non-responders described? | 2 | 2 | 0 | 23 |
| Were the results internally consistent? | 1 | 25 | 0 | 1 |
| Were the results presented for all the analyses described in the methods? | 22 | 5 | 0 | 0 |
| Discussion | ||||
| Were the authors’ discussions and conclusions justified by the results? | 27 | 0 | 0 | 0 |
| Were the limitations of the study discussed? | 18 | 9 | 0 | 0 |
| Other | ||||
| Were there any funding sources or conflicts of interest that may affect the authors’ interpretation of the results? | 0 | 9 | 18 | 0 |
| Was ethical approval or consent of participants attained? | 14 | 0 | 13 | 0 |
Inter-agreement reliability
The inter-agreement reliability between the two reviewers was 95.8% (Identification), 92.1% (Screening), 94.2% (Eligibility), and 100% (Inclusion). Each domain provided in AXIS tool had a strong to almost perfect inter-agreement reliability between the independent reviewers, with a kappa score of 0.835 (Introduction), 0.850 (Methods), 0.983 (Results), 0.900 (Discussion), and 0.911 (Other) respectively.
Discussion
To our knowledge, this is the most up-to-date study to quantitatively outline the possible risks involved in LNI following the surgical extraction of M3M. There was a statistically significant 4.80-fold increase in the risk of temporary LNI when BA+ was used compared to BA-. The incidence of permanent nerve injury was 0.28% with LS compared to 0.18% with BA- and 0.07% with BA+. Most of the articles did not provide sufficient information to develop a risk ratio for permanent injury. Zuniga et al. reported that the incidence of permanent LNI following the removal of M3M to be 0.04–0.60% regardless of the surgical technique [6]. Therefore, the findings in this study are not unusual. Further investigation to determine the incidence of permanent LNI is required so a meta-analysis can be conducted in the future.
Various factors also affected the incidence of LNI. The most commonly found statistically significant risk factors in the literature were angulation of the teeth [16, 19, 20, 26, 46], operator’s experience [17, 20, 25, 26, 29, 46, 47], and the difficulty of extraction (usually measured by the length of operation) [28, 29, 46, 47]. Obiechina and colleagues stated that operating under general anaesthesia may be a risk factor as the tissues can be retracted more, leading to increased stretching causing lingual paraesthesia [34]. Other factors such as sectioning the tooth and removing bone may also increase the risk of LNI [16, 26, 46, 47]. Age is also a suggested risk factor, however, whether or not this was statistically significant varied among the studies [16, 20, 24–26, 29, 36, 47]. The difficulty of extraction can be pre-operatively assessed by taking into account some of these identified risk factors, as well as the operator’s clinical judgement.
A previous systematic review investigated the incidence of LNI following the use of three different techniques, BA-, BA+, LS [12]. Pichler and Beirne found that the incidence of temporary LNI was higher when LS was used versus BA+ when they were compared to BA- (RR—13.3 and 8.8 respectively). Permanent LNI was found to be the lowest when LS was used (0.10%) versus BA+ (0.60%), and BA- (0.20%) [12]. Rapaport and Brown also examined the LNI risk but grouped together all procedures that used a lingual retractor [13]. They determined that when a purpose-built instrument was used to retract lingually, the percentage risk of temporary LNI was lower versus no lingual retraction [0.56% vs 0.60% respectively]. Interesting to note is that the percentage risk of temporary LNI was 7.78% when a non-purpose built instrument was used. The risk of permanent LNI was 0.00%, 0.08% and 0.41% for purpose-built lingual retraction, no lingual retraction and non-purpose built lingual retraction, respectively. Our study did not separate different types of retractors.
A previous Cochrane review was conducted in 2020 analysing techniques for the removal of M3M [48]. This study found that the Peto Odds Ratio of permanent lingual nerve injury was 0.14 [0.00, 6.82] when comparing using a lingual retractor compared to not using one. However, this result was based on 1 study. The Odds ratio in the same Cochrane review for temporary lingual nerve injury when comparing the use of a lingual retractor with no lingual retractor was 4.18 [1.75, 9.98]. However, this was also only based on the results of 3 studies [48].
Our study showed that there was a statistically significant increased risk of temporary LNI when using BA+ versus BA- (RR = 4.80). The prevalence of temporary LNI following BA-, BA+ and LS was found to be 1.24%, 2.39% and 2.44% respectively. This result was consistent with Pichler and Beirne. Their risk ratio when comparing BA+ and BA- was 8.8 and the prevalence of LNI was 0.60% (BA-), 6.40% (BA+), and 9.60% (LS). In both our results and Pichler and Beirne’s, LS had the highest incidence of temporary LNI followed by BA+ and then BA-. However, the prevalence of BA- found by Pichler and Beirne was lower while BA+ and LS were higher [12].
The prevalence of permanent LNI following BA-, BA+ and LS was 0.18%, 0.07%, and 0.28% respectively. There is an increased prevalence of permanent LNI following the use of LS compared to both BA- and BA+. These results were inconsistent with Pichler and Beirne who found that LS had the lowest prevalence of permanent LNI while BA+ had the highest [0.2% (BA-), 0.6% (BA+), 0.1% (LS)] [12]. This discrepancy may be due to insufficient data being available regarding permanent LNI.
Our study had negligible statistical heterogeneity. Quantifying statistical heterogeneity can only be validated if there is an unknown clinical heterogeneity [49]. According to the overall RR in this study, it is most likely that there was no evidence of clinical heterogeneity. Furthermore, according to our systematic review, clinical covariates across all studies (e.g. patient level, intervention level, outcome level) are shown to be similar. This was as a result of the stringent criterion placed to minimise heterogeneity [50]. Furthermore, during the derivation of the forest plot, implementing both fixed- and random- effects model made little difference to the I2 value.
Limitations
One of the major limitations of this systematic review and meta-analysis was that we were unable to calculate the risk ratio for permanent LNI due to the lack of published data. Furthermore, only the RR between BA+ versus BA- was calculated as there was insufficient data to calculate for LS to draw a statistically meaningful conclusion. Another limitation was the exclusion of grey literature from our study; however, the inclusion of grey literature may have further skewed our results due to the lack of peer review within these studies. In addition, many studies were not randomised controlled trials. In many studies, the use of a lingual retractor was used at the clinician’s discretion. This could introduce a level of bias as it may indicate that lingual retraction was used in more difficult cases that were at higher risk of LNI regardless of whether lingual retraction was used or not. Another limitation was that the type of lingual retractor used varied between the articles and some articles did not specify what was used (Table 2). This may introduce a level of bias as Rapaport and Brown found that the percentage risk of permanent LNI was lowest when purpose-built lingual retractors were used [13]. They also found that the use of repurposed lingual retractors had the highest risk of temporary and permanent LNI. Another limitation was the position and impaction of the M3M were not factored in when comparing the incidence of LNI. The position of the M3M has been noted to affect the risk of LNI [51]. However, we were unable to analyse this factor as the studies included in our systematic review did not outline the impaction of the M3M. This could be something that could potentially be explored in the future. Lastly, limitations were also present during data input. When papers did not list the number of subjects or teeth, we adopted a 1:1 ratio for subject:patient when inputting the data. This could potentially skew the results if studies had one patient undergoing two M3M surgical extractions.
Implication of practice
The global prevalence of impacted M3M is approximately 24% [52]. In 2008, an estimated number of hospitalisations for extraction of impacted M3M in Australia was 97,949 [15–34 years]. This resulted in the total cost of $531 million AUD [53]. In addition, in the United States, approximately 10 million M3M were extracted annually with costs approximating $3 billion USD [54]. One of the risks of M3M is LNI which can negatively impact a patient’s QoL [1], and therefore operators should attempt to minimise the risk as much as possible. Previous studies have used lingual retraction to protect the lingual nerve from injury. As there are limited studies that published the outcomes of permanent LNI, further research is required to assess and analyse the incidence of permanent LNI following these techniques (BA-, BA+, and LS).
Conclusion
This study has shown that there is a quantifiable increased risk of temporary LNI following the surgical extraction of M3M when BA+ and LS is used compared to BA-. The current literature showed that there was a lower incidence of permanent LNI after using BA+ compared to BA- and LS. LS had a higher temporary and permanent risk for LNI. There is insufficient evidence to determine whether there is a significant advantage of lingual nerve retraction for reducing the risk of permanent LNI despite the low incidence. Larger scale studies are needed to consolidate the findings. Operators should use BA+ and LS with caution due to the increased risk of temporary LNI.
Supporting information
(DOCX)
Acknowledgments
The authors would like to thank Winthrop Professor Marc Tennant from the University of Western Australia, for his support and guidance. J.L. and B.F. were part of the KASP programme of 2020.
Abbreviations
- BA-
Buccal approach without lingual flap retraction
- BA+
buccal approach with lingual flap retraction
- LN
Lingual nerve
- LNI
Lingual nerve injury
- LS
Lingual split technique
- M3M
Mandibular third molar
Data Availability
The data are all contained within the paper and its Supporting information file.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Patel N, Ali S, Yates JM. Quality of life following injury to the inferior dental or lingual nerve—A cross-sectional mixed-methods study. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 2018;11(1):9–16. doi: 10.1111/ors.12259 [DOI] [Google Scholar]
- 2.McLeod NM, Bowe DC. Nerve injury associated with orthognathic surgery. Part 3: lingual, infraorbital, and optic nerves. The British journal of oral & maxillofacial surgery. 2016;54(4):372–5. Epub 2016/02/28. doi: 10.1016/j.bjoms.2016.01.028 . [DOI] [PubMed] [Google Scholar]
- 3.Martos-Fernández M, de-Pablo-Garcia-Cuenca A, Bescós-Atín MS. Lingual nerve injury after third molar removal: Unilateral atrophy of fungiform papillae. Journal of clinical and experimental dentistry. 2014;6(2):e193–6. Epub 2014/05/03. doi: 10.4317/jced.51375 interest exist. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bagheri SC, Meyer RA, Khan HA, Kuhmichel A, Steed MB. Retrospective review of microsurgical repair of 222 lingual nerve injuries. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2010;68(4):715–23. Epub 2009/12/29. doi: 10.1016/j.joms.2009.09.111 . [DOI] [PubMed] [Google Scholar]
- 5.Coulthard P, Kushnerev E, Yates JM, Walsh T, Patel N, Bailey E, et al. Interventions for iatrogenic inferior alveolar and lingual nerve injury. The Cochrane database of systematic reviews. 2014;(4):CD005293. Epub 2014/04/18. doi: 10.1002/14651858.CD005293.pub2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zuniga JR. Management of third molar-related nerve injuries: observe or treat? The Alpha omegan. 2009;102(2):79–84. Epub 2009/07/14. doi: 10.1016/j.aodf.2009.04.014 . [DOI] [PubMed] [Google Scholar]
- 7.Ghabriel M, Takezawa K, Townsend G. The lingual nerve: overview and new insights into anatomical variability based on fine dissection using human cadavers. Odontology. 2019;107(1):1–9. Epub 2018/06/27. doi: 10.1007/s10266-018-0371-4 . [DOI] [PubMed] [Google Scholar]
- 8.Sittitavornwong S, Babston M, Denson D, Zehren S, Friend J. Clinical anatomy of the lingual nerve: A review. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2017;75(5):926.e1–.e9. Epub 2017/02/13. doi: 10.1016/j.joms.2017.01.009 . [DOI] [PubMed] [Google Scholar]
- 9.Pogrel MA, Renaut A, Schmidt B, Ammar A. The relationship of the lingual nerve to the mandibular third molar region: an anatomic study. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 1995;53(10):1178–81. Epub 1995/10/01. doi: 10.1016/0278-2391(95)90630-4 [DOI] [PubMed] [Google Scholar]
- 10.Pogrel MA, Goldman KE. Lingual flap retraction for third molar removal. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2004;62(9):1125–30. Epub 2004/09/04. doi: 10.1016/j.joms.2004.04.013 . [DOI] [PubMed] [Google Scholar]
- 11.Pippi R, Alvaro R. Piezosurgery for the lingual split technique in mandibular third molar removal: a suggestion. The Journal of craniofacial surgery. 2013;24(2):531–3. Epub 2013/03/26. doi: 10.1097/SCS.0b013e31826463f7 . [DOI] [PubMed] [Google Scholar]
- 12.Pichler JW, Beirne OR. Lingual flap retraction and prevention of lingual nerve damage associated with third molar surgery: a systematic review of the literature. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 2001;91(4):395–401. Epub 2001/04/20. doi: 10.1067/moe.2001.114154 . [DOI] [PubMed] [Google Scholar]
- 13.Rapaport BHJ, Brown JS. Systematic review of lingual nerve retraction during surgical mandibular third molar extractions. The British journal of oral & maxillofacial surgery. 2020;58(7):748–52. Epub 2020/07/06. doi: 10.1016/j.bjoms.2020.02.022 . [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6(7):e1000097. Epub 2009/07/22. doi: 10.1371/journal.pmed.1000097 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akadiri OA, Fasola AO, Arotiba JT. Incidence and risk factors for nerve injuries in mandibular third molar surgery. Nigerian journal of medicine: journal of the National Association of Resident Doctors of Nigeria. 2009;18(4):402–8. Epub 2010/02/03. doi: 10.4314/njm.v18i4.51252 . [DOI] [PubMed] [Google Scholar]
- 16.Baqain ZH, Abukaraky A, Hassoneh Y, Sawair F. Lingual nerve morbidity and mandibular third molar surgery: a prospective study. Medical principles and practice: international journal of the Kuwait University, Health Science Centre. 2010;19(1):28–32. Epub 2009/12/10. doi: 10.1159/000252831 . [DOI] [PubMed] [Google Scholar]
- 17.Bataineh AB. Sensory nerve impairment following mandibular third molar surgery. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2001;59(9):1012–7. Epub 2001/08/30. doi: 10.1053/joms.2001.25827 . [DOI] [PubMed] [Google Scholar]
- 18.Bataineh AB, Batarseh RA. The effect of modified surgical flap design for removal of lower third molars on lingual nerve injury. Clinical oral investigations. 2017;21(6):2091–9. Epub 2016/11/12. doi: 10.1007/s00784-016-1999-5 . [DOI] [PubMed] [Google Scholar]
- 19.Charan Babu HS, Reddy PB, Pattathan RK, Desai R, Shubha AB. Factors influencing lingual nerve paraesthesia following third molar surgery: a prospective clinical study. Journal of maxillofacial and oral surgery. 2013;12(2):168–72. Epub 2014/01/17. doi: 10.1007/s12663-012-0391-5 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheung LK, Leung YY, Chow LK, Wong MC, Chan EK, Fok YH. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. International journal of oral and maxillofacial surgery. 2010;39(4):320–6. Epub 2010/01/12. doi: 10.1016/j.ijom.2009.11.010 . [DOI] [PubMed] [Google Scholar]
- 21.Gargallo-Albiol J, Buenechea-Imaz R, Gay-Escoda C. Lingual nerve protection during surgical removal of lower third molars. a prospective randomised study. International journal of oral and maxillofacial surgery. 2000;29(4):268–71. Epub 2000/10/13. . [PubMed] [Google Scholar]
- 22.Ge J, Yang C, Zheng J, Qian W. Piezosurgery for the Lingual Split Technique in Lingual Positioned Impacted Mandibular Third Molar Removal: A Retrospective Study. Medicine. 2016;95(12):e3192. Epub 2016/03/26. doi: 10.1097/MD.0000000000003192 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gomes AC, Vasconcelos BC, de Oliveira e Silva ED, da Silva LC. Lingual nerve damage after mandibular third molar surgery: a randomized clinical trial. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2005;63(10):1443–6. Epub 2005/09/27. doi: 10.1016/j.joms.2005.06.012 . [DOI] [PubMed] [Google Scholar]
- 24.Janakiraman EN, Alexander M, Sanjay P. Prospective analysis of frequency and contributing factors of nerve injuries following third-molar surgery. The Journal of craniofacial surgery. 2010;21(3):784–6. Epub 2010/05/21. doi: 10.1097/SCS.0b013e3181d7f29a . [DOI] [PubMed] [Google Scholar]
- 25.Jerjes W, Swinson B, Moles DR, El-Maaytah M, Banu B, Upile T, et al. Permanent sensory nerve impairment following third molar surgery: a prospective study. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 2006;102(4):e1–7. Epub 2006/09/26. doi: 10.1016/j.tripleo.2006.01.016 . [DOI] [PubMed] [Google Scholar]
- 26.Jerjes W, Upile T, Nhembe F, Gudka D, Shah P, Abbas S, et al. Experience in third molar surgery: an update. British dental journal. 2010;209(1):E1. Epub 2010/07/03. doi: 10.1038/sj.bdj.2010.581 . [DOI] [PubMed] [Google Scholar]
- 27.Kale TP, Pandit VS, Patil S, Pawar V, Shetty N. Lingual guttering technique for removal of impacted mandibular third molars. Journal of international oral health: JIOH. 2014;6(4):9–11. Epub 2014/09/13. . [PMC free article] [PubMed] [Google Scholar]
- 28.Lata J, Tiwari AK. Incidence of lingual nerve paraesthesia following mandibular third molar surgery. National journal of maxillofacial surgery. 2011;2(2):137–40. Epub 2012/05/29. doi: 10.4103/0975-5950.94467 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Majeed F, Zahra A, Kanwal M, Majeed M, Izhar S. Revealing the various predisposing factors causing damage of lingual nerve during lower third molar surgery. Indo Am J Pharm Sci. 2018;5(12):16963–8. [Google Scholar]
- 30.Malden NJ, Maidment YG. Lingual nerve injury subsequent to wisdom teeth removal—a 5-year retrospective audit from a high street dental practice. British dental journal. 2002;193(4):203–5. Epub 2002/09/12. doi: 10.1038/sj.bdj.4801523 . [DOI] [PubMed] [Google Scholar]
- 31.Mavrodi A, Ohanyan A, Kechagias N, Tsekos A, Vahtsevanos K. Influence of two different surgical techniques on the difficulty of impacted lower third molar extraction and their post-operative complications. Medicina oral, patologia oral y cirugia bucal. 2015;20(5):e640–4. Epub 2015/06/28. doi: 10.4317/medoral.20605 interest exist. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moss CE, Wake MJ. Lingual access for third molar surgery: a 20-year retrospective audit. The British journal of oral & maxillofacial surgery. 1999;37(4):255–8. Epub 1999/09/04. doi: 10.1054/bjom.1999.0063 . [DOI] [PubMed] [Google Scholar]
- 33.Nguyen E, Grubor D, Chandu A. Risk factors for permanent injury of inferior alveolar and lingual nerves during third molar surgery. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2014;72(12):2394–401. Epub 2014/09/23. doi: 10.1016/j.joms.2014.06.451 . [DOI] [PubMed] [Google Scholar]
- 34.Obiechina AE, Oji C, Fasola AO. Impacted mandibular third molars: depth of impaction and surgical methods of extraction among Nigerians. Odonto-stomatologie tropicale = Tropical dental journal. 2001;24(94):33–6. Epub 2001/09/08. . [PubMed] [Google Scholar]
- 35.Praveen G, Rajesh P, Neelakandan RS, Nandagopal CM. Comparison of morbidity following the removal of mandibular third molar by lingual split, surgical bur and simplified split bone technique. Indian journal of dental research: official publication of Indian Society for Dental Research. 2007;18(1):15–8. Epub 2007/03/10. doi: 10.4103/0970-9290.30916 . [DOI] [PubMed] [Google Scholar]
- 36.Ramadorai A, Tay ABG, Vasanthakumar G, Lye WK. Nerve injury after surgical excision of mandibular third molars under local anesthesia: An audit. Journal of maxillofacial and oral surgery. 2019;18(2):307–13. Epub 2019/04/19. doi: 10.1007/s12663-018-1151-y . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robinson PP, Loescher AR, Smith KG. The effect of surgical technique on lingual nerve damage during lower 3rd molar removal by dental students. European journal of dental education: official journal of the Association for Dental Education in Europe. 1999;3(2):52–5. Epub 1999/10/26. doi: 10.1111/j.1600-0579.1999.tb00069.x . [DOI] [PubMed] [Google Scholar]
- 38.Shad S, Shah SM, Alamgir, Abbasi MM. Frequency of lingual nerve injury in mandibular third molar extraction: A comparison of two surgical techniques. Journal of Ayub Medical College, Abbottabad: JAMC. 2015;27(3):580–3. Epub 2016/01/02. . [PubMed] [Google Scholar]
- 39.Smith WP. The relative risk of neurosensory deficit following removal of mandibular third molar teeth: the influence of radiography and surgical technique. Oral surgery, oral medicine, oral pathology and oral radiology. 2013;115(1):18–24. Epub 2012/08/28. doi: 10.1016/j.oooo.2012.03.017 . [DOI] [PubMed] [Google Scholar]
- 40.Yadav S, Verma A, Sachdeva A. Assessment of lingual nerve injury using different surgical variables for mandibular third molar surgery: a clinical study. International journal of oral and maxillofacial surgery. 2014;43(7):889–93. Epub 2014/03/04. doi: 10.1016/j.ijom.2014.01.013 . [DOI] [PubMed] [Google Scholar]
- 41.Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving cross-over trials: methodological issues. International journal of epidemiology. 2002;31(1):140–9. Epub 2002/03/27. doi: 10.1093/ije/31.1.140 . [DOI] [PubMed] [Google Scholar]
- 42.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed). 2003;327(7414):557–60. Epub 2003/09/06. doi: 10.1136/bmj.327.7414.557 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Page MJ, McKenzie JE, Higgins JPT. Tools for assessing risk of reporting biases in studies and syntheses of studies: a systematic review. BMJ open. 2018;8(3):e019703. Epub 2018/03/16. doi: 10.1136/bmjopen-2017-019703 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McHugh ML. Interrater reliability: the kappa statistic. Biochemia medica. 2012;22(3):276–82. Epub 2012/10/25. doi: 10.1016/j.jocd.2012.03.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ open. 2016;6(12):e011458. Epub 2016/12/10. doi: 10.1136/bmjopen-2016-011458 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Lingual nerve damage after third lower molar surgical extraction. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics. 2000;90(5):567–73. Epub 2000/11/15. doi: 10.1067/moe.2000.110034 . [DOI] [PubMed] [Google Scholar]
- 47.Renton T, Smeeton N, McGurk M. Factors predictive of difficulty of mandibular third molar surgery. British dental journal. 2001;190(11):607–10. Epub 2001/07/10. doi: 10.1038/sj.bdj.4801052 . [DOI] [PubMed] [Google Scholar]
- 48.Bailey E, Kashbour W, Shah N, Worthington HV, Renton TF, Coulthard P. Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database Syst Rev. 2020;7(7):Cd004345. Epub 2020/07/28. doi: 10.1002/14651858.CD004345.pub3 Worthington: none known. Tara F Renton: I am an author of a study included in this review; however, I was not involved in ’Risk of bias’ assessment of this study. Paul Coulthard: none known. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Melsen WG, Bootsma MC, Rovers MM, Bonten MJ. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clinical microbiology and infection: the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2014;20(2):123–9. Epub 2013/12/11. doi: 10.1111/1469-0691.12494 . [DOI] [PubMed] [Google Scholar]
- 50.Gagnier JJ, Moher D, Boon H, Beyene J, Bombardier C. Investigating clinical heterogeneity in systematic reviews: a methodologic review of guidance in the literature. BMC medical research methodology. 2012;12:111. Epub 2012/08/01. doi: 10.1186/1471-2288-12-111 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tojyo I, Nakanishi T, Shintani Y, Okamoto K, Hiraishi Y, Fujita S. Risk of lingual nerve injuries in removal of mandibular third molars: a retrospective case-control study. Maxillofac Plast Reconstr Surg. 2019;41(1):40. Epub 2019/09/27. doi: 10.1186/s40902-019-0222-4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carter K, Worthington S. Predictors of third molar impaction: A systematic review and meta-analysis. Journal of dental research. 2016;95(3):267–76. Epub 2015/11/13. doi: 10.1177/0022034515615857 . [DOI] [PubMed] [Google Scholar]
- 53.Anjrini AA, Kruger E, Tennant M. Cost effectiveness modelling of a ’watchful monitoring strategy’ for impacted third molars vs prophylactic removal under GA: an Australian perspective. British dental journal. 2015;219(1):19–23. Epub 2015/07/15. doi: 10.1038/sj.bdj.2015.529 . [DOI] [PubMed] [Google Scholar]
- 54.Friedman JW. The prophylactic extraction of third molars: a public health hazard. American journal of public health. 2007;97(9):1554–9. Epub 2007/08/02. doi: 10.2105/AJPH.2006.100271 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
The data are all contained within the paper and its Supporting information file.