ABSTRACT
Novel COVID-19 variants continue to endanger global public health. Increasing COVID-19 vaccination, healthcare-related preventative behaviors, and general knowledge rates are all critical in halting COVID-19 spread. We evaluated Asian American COVID-19 healthcare-related behaviors and knowledge, due to the dearth of knowledge in this area and the unique social factor of COVID-19 related discrimination; discriminatory acts during the pandemic may play a role in COVID-19 related behavior adherence. Following PRISMA-P protocol, we conducted a systematic review. The search strategy combined synonyms of health-care behaviors and knowledge. Reviewers synthesized key themes across articles and assessed studies utilizing modified Newcastle–Ottawa criteria. Of the 2,518 articles, 32 were selected. Asian Americans reported greater COVID-19 vaccination willingness and decreased COVID-19 testing relative to other racial groups. Common COVID-19 vaccination concerns included vaccination side effects, long-term safety, and distrust of COVID-19 information sources. Asian Americans had high COVID-19 preventative behavior rates including mask-wearing, handwashing, and social isolation compared to other ethnic groups. Asian Americans, conversely, had lower COVID-19-related healthcare knowledge and telemedicine adoption levels relative to other participants. This systematic review informs public health officials and clinicians of COVID-19 related healthcare knowledge and behaviors in the Asian American population. Equipped with this knowledge, public health officials can better target messaging about vaccine safety concerns to the Asian American community and recognize the importance of tailoring COVID-19 educational materials to the heterogeneous Asian American subpopulations. This systematic review also provides insight into the unique telemedicine challenges physicians may face when engaging with Asian American patients.
KEYWORDS: COVID-19, Asian American, knowledge, behavior, vaccination
Introduction
Declared as a pandemic in March 2020, COVID-19 continues to endanger public health across the world [1]. The novel coronavirus responsible for the disease, SARS-CoV-2, was first identified in China’s Hubei Province after an outbreak of pneumonia at a seafood market in Wuhan [2]. Though mortality and morbidity have improved considerably since the introduction of vaccines and specific antivirals, the emergence of highly transmissible variants of concern – such as the Omicron variant – threatens to reverse this progress [3–5]. With spike protein mutations possibly enabling resistance to neutralizing antibodies, Omicron has caused official guidance to shift back to an emphasis on health practices that slow viral transmission, including hand-washing, proper mask-wearing, and physical distancing [6,7]. The practice of these health behaviors and knowledge of their rationale have both been strongly correlated with reduced COVID-19 infection and symptoms at all points of the pandemic [8–11].
The burden of infection and its complications have not been borne equally across American society. In the United States, the sequelae of COVID-19 have been severe enough to reduce life expectancies at birth by over a year in White populations and to a far greater extent in ethnic minorities, including Black and Latino populations [12]. Despite great emphasis on these two minority communities, the general population and groups such as health-care providers and high-risk adults, there is a dearth of research focusing on Asian American COVID-19 related knowledge and behaviors, who number over eighteen million in the United States [13–17]. This lack of data has serious implications for communities with sizable Asian American populations, including coastal cities in California, where public health officials must know the practices and knowledge levels of Asian Americans to accurately assess and mitigate the risk of SARS-CoV-2 transmission. Asian ethnicity has been associated with lower rates of COVID-19 testing [18–20]. Asian Americans have also faced inferior medical outcomes relative to other racial groups, partially due to difficulties in accessing needed care, and therefore relying on medical information from family members rather than medical professionals [21,22]. This information gap must be closed in order to properly target culturally sensitive and effective COVID-19 public health messaging to Asian Americans across the United States.
As a heterogeneous collection of national and ethnic subgroups differentially positioned in the American economy, Asian Americans offer a unique opportunity to understand COVID-19 vaccination, testing, preventative behavior uptake, and general COVID-19 knowledge in minority populations while stratifying by socioeconomic status (SES), nationality, and cultural heritage. For example, the Asian American population has the greatest income variance across U.S. racial and ethnic groups, which may impact health outcomes and inequalities across different Asian American communities [23]. This stratification may enhance our understanding of how these demographic factors affect adherence to COVID-19 preventative measures and knowledge, by informing specific COVID-19 preventative interventions. This racial population has also uniquely faced COVID-related racial discrimination during the pandemic [24,25]. The racist tendency to blame the Asian American community for COVID-19 transmission may have an impact on Asian American healthcare behavior, and allows for the impact of scapegoating on healthcare practice adherence to be examined. Given this context, our goal is to evaluate COVID-19 related healthcare knowledge and practice levels of the Asian American population.
Methods
Search strategy
Preliminary literature searches were conducted in accordance with the PRISMA-P protocol across four databases: PubMed, PsycInfo, Embase, and Web of Science [26]. Search terms were related to healthcare knowledge and behaviors, COVID-19, and the Asian American population and subgroups such as Chinese, Japanese, and Korean Americans. Selected South Asian American subgroups, including Bangladeshi, Pakistani, and Nepali Americans, were omitted due to a lack of articles focusing on these specific Asian American populations during the preliminary literature screen. Various synonyms and permutations were used; a complete list can be found in Online Resource 1. These results were filtered by language (English), availability (full text), subject type (human), and date (2/1/2020 – 10/20/2021) to ensure relevance. After an initial list of studies was compiled, the article selection process began.
Study selection
Selection took part in two phases: title and abstract screening followed by full-text assessment. Titles and abstracts were evaluated for pertinence to health-care behaviors and knowledge within the Asian American community. Studies identified as relevant based on abstracts and titles were housed in Endnote for later reference and preliminary deduplication [27]. Subsequently, this list was transferred to Rayyan for secondary deduplication and full-text assessment [28]. Two reviewers (SA and WG) conducted a full-text analysis to determine the final list of studies. Inclusion criteria were selected for observational studies with subjects self-identifying as Asian American and control groups with n > 10. These studies were pared down using exclusion criteria selected against non-peer reviewed studies, studies lacking quantitative data, animal research, opinions, abstracts, and literature reviews, as well as studies not relevant to Asian American COVID-19 related behavior and knowledge. The detailed PRISMA flow diagram process can be found in Figure 1.
Figure 1.
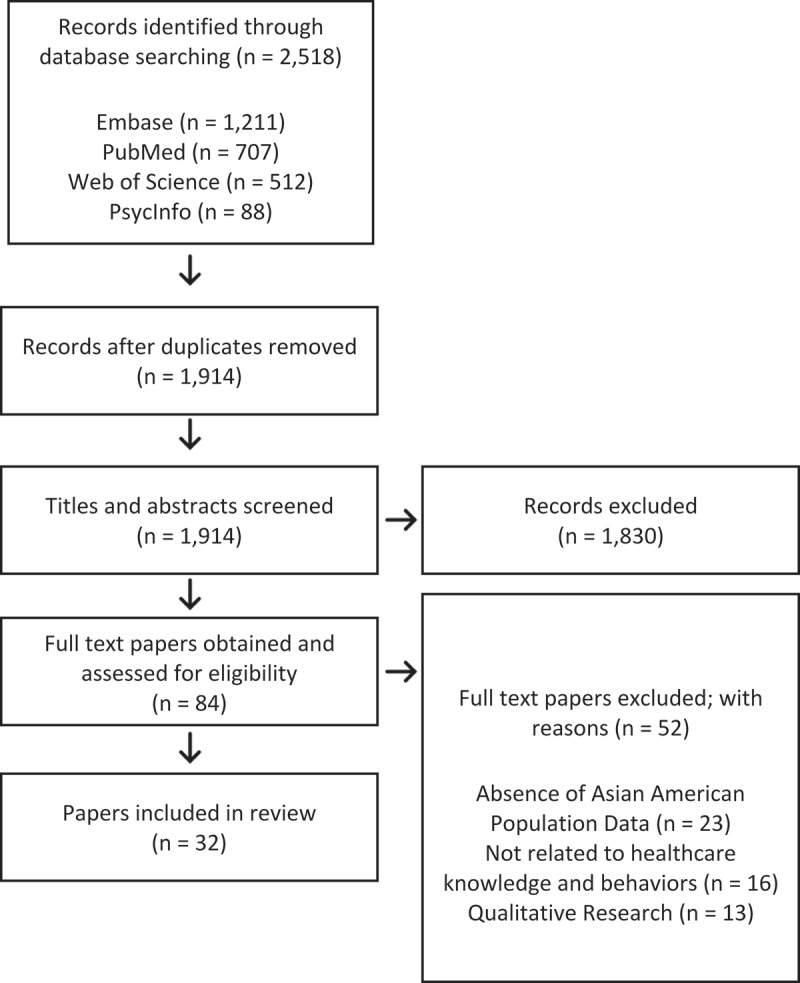
PRISMA flow diagram.
Quality assessment
After article selection was complete, quality assessment was performed by three reviewers (SA, EC, and RK) using modified versions of the Newcastle-Ottawa Scale developed for qualitative, cross-sectional, case-control, and cohort studies [29]. Based on scores calculated from these criteria, studies were assessed as good quality, fair quality, poor quality, or very poor quality.
Data extraction
Relevant data were extracted into two tables; Table 1 captures key study characteristics including author, overall study purpose, study design, and relevant study findings, whereas Online Resource 2 contains additional article information including population characteristics and relevant outcome measures used.
Table 1.
Study characteristics.
| Author (year) | Purpose | Study design | Key findings |
|---|---|---|---|
| Allen et al. (2021) [35] |
COVID-19 Vaccination Determines factors that affect COVID-19 vaccine uptake among women across racial/ethnic communities. |
Cross-sectional | Chinese and non-Latina White women had a greater likelihood of intent to receive the COVID-19 vaccine relative to other racial groups. Participants who were unemployed, were uninsured, or had decreased financial income or education levels were more likely to have decreased COVID-19 vaccination intentions. |
| Brandt et al. (2021) [36] |
COVID-19 Vaccination Understands impediments and facilitators that influence youth COVID-19 vaccination uptake. |
Cross-sectional | Asian American youth had a decreased probability of declining COVID-19 vaccination compared to White and Black youth participants. Common COVID-19 vaccination hesitation concerns included safety, potential for side effects, and general vaccine efficacy against COVID-19. |
| Dorman et al. (2021) [43] |
COVID-19 Vaccination Identifies attributes correlated with COVID-19 vaccination willingness levels. |
Cross-sectional | Asian Americans had greater COVID-19 vaccination willingness levels relative to other racial groups. Higher education levels and older age were correlated with greater COVID-19 vaccination willingness. |
| Ghaffari-Rafi et al. (2021) [42] |
COVID-19 Vaccination Determines factors correlated with COVID-19 vaccination hesitation for patients with neurological disorders. |
Cross-sectional | Body mass index (BMI) and insurance were both found to be statistically significant in predicting Asians American COVID-19 vaccination acceptance. A positive depression screen was correlated with decreased COVID-19 vaccination acceptance for Native Hawaiian and Pacific Islander Americans. Female Asian Americans and White participants were found to have COVID-19 vaccination safety concerns, including how vaccination could interact with other medical conditions. |
| Hagan et al. (2021) [40] |
COVID-19 Vaccination Assesses COVID-19 vaccine distribution and acceptance differences among staff and incarcerated individuals in the Federal Bureau of Prisons. |
Cross-sectional | Incarcerated Asian Americans and non-Hispanic Black Americans had reduced COVID-19 vaccination acceptance relative to other racial groups. |
| Kuter et al. (2021) [37] |
COVID-19 Vaccination Understands COVID-19 vaccine perceptions among health-care workers (HCWs). |
Cross-sectional | Asian and White HCWs had greater COVID-19 vaccination intention rates compared to other ethnic groups. COVID-19 vaccination hesitation concerns included newness of the COVID-19 vaccination and potential side effects. |
| Lang et al. (2021) [38] |
COVID-19 Vaccination Evaluates COVID-19 vaccine initiation and completion rates in the active component in the United States military population. |
Retrospective cohort | Asian Americans and Pacific Islanders had the greatest COVID-19 vaccination initiation rates relative to other racial groups. COVID-19 vaccination initiation increased with age, level of education, and higher rank. |
| Malik et al. (2020) [31] |
COVID-19 Vaccination Identifies factors that influence COVID-19 vaccine acceptance, risk perception, and trust in COVID-19-related information in the United States adult population. |
Cross-sectional | Asian Americans were more likely to report higher COVID-19 vaccine acceptance compared to other racial groups. Male gender, older age, and greater education levels were correlated with greater COVID-19 vaccination acceptance. |
| Momplaisir et al. (2021) [39] |
COVID-19 Vaccination Determines racial and ethnic differences in COVID-19 vaccine hesitancy among HCWs. |
Cross-sectional | Asian American and other minority HCWs reported greater vaccine hesitancy compared to White HCWs. Commonly cited vaccination concerns included side effects, novelty of vaccine, and a dearth of COVID-19 vaccination knowledge. |
| Niño et al. (2021) [30] |
COVID-19 Vaccination Assesses COVID-19 vaccination intentions over an extended period of time and across racial groups. |
Retrospective cohort | Asian Americans and Pacific Islanders were found to have greater COVID-19 vaccination intention rates relative to other participants. |
| Parente et al. (2021) [44] |
COVID-19 Vaccination Identifies factors that influence COVID-19 vaccination acceptance among health-care personnel. |
Cross-sectional | Greater COVID-19 vaccination acceptance was associated with increased education levels, male gender, prior influenza vaccination, and increased COVID-19 concern levels. Common concerns cited for COVID-19 vaccination hesitancy included cost, general efficacy, and vaccine safety. |
| Park et al. (2021) [41] |
COVID-19 Vaccination Assesses COVID-19 vaccination concerns across Asian American and Pacific Islander subethnic groups. |
Cross-sectional | Asian American subethnic group identity was associated with COVID-19 vaccination concern levels. COVID-19 vaccine side effects and overall safety were cited as common vaccination concerns. |
| Park et al. (2021) [32] |
COVID-19 Vaccination Examines COVID-19 vaccination willingness levels in Asian American and Pacific Islander populations. |
Cross-sectional | COVID-19 vaccination willingness levels were associated with gender, sexual orientation, and age. Native Hawaiians and Pacific Islanders had decreased COVID-19 vaccination willingness levels relative to Asian Americans. Vaccine willingness varied by subgroups within the Asian American and Pacific Islander populations. |
| Shaw et al. (2021) [33] |
COVID-19 Vaccination Understands COVID-19 vaccination willingness and concerns among health-care personnel. |
Cross-sectional | Asian American and White HCWs had a greater probability of becoming vaccinated against COVID-19 relative to other participant groups. Older age and male gender were associated with greater COVID-19 vaccine intention. |
| Sutton et al. (2021) [34] |
COVID-19 Vaccination Assesses COVID-19 vaccine acceptance in pregnant, breastfeeding, and nonpregnant women populations. |
Cross-sectional | Asian American respondents had the greatest COVID-19 vaccination acceptance rates compared to other racial and ethnic groups. |
| Bailey et al. (2020) [18] |
COVID-19 Testing Describes COVID-19 testing and infection rates among pediatric patients. |
Retrospective cohort | Asian Americans had a decreased probability of obtaining a COVID-19 test compared to White participants. |
| Ferguson et al. (2021) [19] |
COVID-19 Testing Assesses the relationship between COVID-19 testing rates and demographic factors in a military veteran population. |
Retrospective cohort | Asian Americans veterans were less likely to obtain a COVID-19 test compared to White veterans. Native Hawaiian and Pacific Islanders did not have greater COVID-19 testing rates relative to White veterans. |
| Quach et al. (2021) [20] |
COVID-19 Testing & Practices Understand the Asian American COVID-19 experience, including healthcare and social challenges faced. |
Cross-sectional | Asian Americans had low COVID-19 testing rates and reported inability to locate testing sites. Asian Americans had high-risk avoidant behavior rates, such as avoiding public spaces. |
| Stockman et al. (2021) [49] |
COVID-19 Testing & Practices Identify racial and ethnic disparities of COVID-19 outcome prevalence, stressors, fear, and preventive behaviors among U.S. adult women. |
Cross-sectional | Racial and ethnic minority women had a decreased likelihood of COVID-19 testing site awareness. Asian, Native Hawaiian, or other Pacific Islander women had a greater probability of engaging in preventative behaviors such as self-isolation when ill and handwashing with soap. |
| Chua et al. (2020) [45] |
COVID-19 Practices Identify factors correlated with parent/guardian COVID-19 schooling plans. |
Cross-sectional | Asian American and Black families had decreased intentions of selecting in-person learning compared to online forms of schooling during COVID-19. |
| Cohen et al. (2021) [46] |
COVID-19 Practices Examine factors correlated with mask-wearing adherence and physical distancing. |
Direct Observation Cross-sectional | Asian Americans were more likely to correctly wear masks relative to White participants. Female gender, older age, and living in high population density locations were associated with greater correct mask-wearing behaviors. |
| Hearne et al. (2020) [47] |
COVID-19 Practices Evaluate the impact of race, ethnicity, and gender on mask-wearing rates. |
Cross-sectional | Asian American participants had a greater likelihood of mask-wearing relative to White participants. |
| Jelliffe et al. (2021) [48] |
COVID-19 Practices Assess U.S. sick leave awareness and utilization, as well as demographical predictors of sick leave usage. |
Cross-sectional | Asian Americans were more likely to have awareness of and utilize paid sick leave. |
| Alobuia et al. (2020) [50] |
COVID-19 Knowledge Evaluates differences in COVID-19 knowledge, attitude, and practice levels across racial groups. |
Cross-sectional | Less than half of Asian American participants were reported to have high COVID-19 knowledge scores. Increased education and income levels were associated with greater COVID-19 knowledge scores. |
| Jones et al. (2020) [51] |
COVID-19 Knowledge Describes the variation of COVID-19 symptoms, knowledge, and beliefs across racial and ethnic groups. |
Cross-sectional | Asian Americans had a decreased likelihood of answering COVID-19 questions correctly relative to White participants. |
| O’Shea et al. (2021) [52] |
COVID-19 Knowledge Assesses the impact of demographic factors on COVID-19 expert trust levels. |
Cross-sectional | Asian Americans were found to have greater trust toward ordinary citizens than COVID-19 experts for coronavirus-related policy decisions. |
| Dennis et al. (2020) [57] |
COVID-19 Telemedicine Adoption Evaluates participant response after viewing COVID-19 screening chatbots. |
Experimental | Asian Americans perceived COVID-19 screening chatbots agents as having greater benevolence and ability relative to White participants. |
| Eberly et al. (2020) [56] |
COVID-19 Telemedicine Adoption Determines telemedicine and video utilization disparities during COVID-19. |
Retrospective cohort |
Asian American patients were less likely to use telemedicine visits compared to White patients. Older age, female, and lower income patients had a decreased probability of utilizing video-based telemedicine visits. |
| Hsiao et al. (2021) [55] |
COVID-19 Telemedicine Adoption Examines telemedicine disparities through analyzing COVID-19 patient telemedicine utilization patterns. |
Retrospective cross-sectional | Asian American, as well as Black/African American and Hispanic, patients significantly had a decreased likelihood of utilizing telemedicine appointments, including video-based visits. Older, rural, and uninsured or self-pay patients were less likely to have video-based telemedicine visits. |
| Meno et al. (2021) [54] |
COVID-19 Telemedicine Adoption Describes telemedicine perceptions of Asian American, Native Hawaiian, and Pacific Islander cancer patients. |
Cross-sectional | Asian American, Native Hawaiian, and Pacific Islander participants had a decreased likelihood of wanting future telemedicine appointments compared to White participants. |
| Wong et al. (2021) [53] |
COVID-19 Telemedicine Adoption Identifies factors that influence seizure clinic patient perceptions of telemedicine care. |
Retrospective and prospective cohort | Native Hawaiian patients were more likely to be seen in-person compared to White patients who had greater telemedicine utilization. |
| Yuan et al. (2021) [58] |
COVID-19 Telemedicine Adoption Evaluates the impact of shifting toward remote cardiology clinic visits on patient care access, medication prescription, and diagnostic ordering. |
Cross-sectional | Asian Americans, as well as Black and Hispanic participant groups, patients had increased utilization of remote clinic visits. Patients with private insurance, as well as patients with cardiovascular comorbidities, were associated with greater virtual clinic visits. |
Results
Study inclusion process and inclusion/exclusion criteria
Utilizing the search strategy, a total of 2,518 articles were retrieved across four databases. After deduplication efforts using Endnote and Rayyan software, 1,914 article titles and abstracts were initially screened for systematic review inclusion. Of the 1,914 studies, 84 full-text articles were retrieved, and two reviewers (SA and WG) independently assessed each article according to predetermined inclusion and exclusion criteria. Key reasons for exclusion included the absence of Asian American population data, lack of quantitative measures, and irrelevance to general healthcare knowledge and behaviors. Out of 84 studies, 32 articles were included within the systematic review.
Topic categories
We searched broadly across COVID-19 related health-care behaviors and knowledge and reported on the most commonly discussed. Major themes were divided into three categories: COVID-19 vaccination and testing; other COVID-19-related health-care practices, knowledge, and information gathering; and telemedicine adoption.
COVID-19 vaccination and testing
COVID-19 vaccination uptake and willingness
Fifteen articles reported on Asian American COVID-19 vaccination efforts, while two studies detailed COVID-19 testing rates. Out of the 15 studies, 9 disclosed that Asian Americans had greater overall vaccination uptake and willingness levels compared to other racial groups, across differing patient populations [30–38]. Sutton found that Asian American pregnant respondents had a greater likelihood of accepting COVID-19 vaccination than pregnant participants belonging to other racial groups [34]. Pregnant participants had an overall decreased likelihood of accepting COVID-19 vaccination when compared to nonpregnant and breastfeeding participants. Pregnant mothers expressed two main concerns: a dearth of COVID-19 vaccination research efforts and the possibility that their fetus could be harmed [34]. Shaw found that in a health-care worker population, being of White or Asian American racial background was associated with greater COVID-19 vaccination uptake [33]. Brandt reported that – within a youth (aged 14–24 years) population – racial background was the only vaccination willingness predictor, with Asian American youth being less likely to reject COVID-19 vaccination [36]. The majority of the youth population expressed being open to receiving a COVID-19 vaccination once they felt informed by scientific and medical experts that vaccination was safe and recommended, demonstrating a high level of youth trust in COVID-19 researchers and physicians [36]. Lang revealed in a study focused on understanding active military vaccination efforts that Asian Americans and Pacific Islanders had greater vaccine initiation rates compared to other ethnic groups [38]. Lang also details the unique characteristic of the U.S. active military population in that they are provided universal health-care eligibility, helping to eliminate access disparities – including vaccination availability, insurance co-payments, and transportation – that are common deterrents in nonmilitary populations [38].
Contrastingly, two studies disclosed that Asian Americans had greater COVID-19 vaccine hesitancy or lower vaccination acceptance. Momplaisir detailed how Asian American health-care workers had greater vaccination hesitancy compared to White participants. A potential explanation cited for increased hesitancy levels was the survey being conducted prior to COVID-19 vaccine authorization by the U.S. Food and Drug Administration; common reasons for vaccination hesitation included the newness of the COVID-19 vaccine and a dearth of knowledge related to the vaccine [39]. Similarly, Hagan detailed that – within the U.S. incarcerated population of the Federal Bureau of Prisons – decreased vaccination uptake was correlated with Asian American ethnicity [40]. One potential reason mentioned to explain decreased Asian American vaccination in the prison system is that incarcerated Asian Americans may hold the belief that they are less likely to contract COVID-19 infection [40].
COVID-19 Vaccination Concerns
While overall vaccination uptake was high for Asian American populations, there were still COVID-19 vaccination concerns detailed across studies. Four studies disclosed that the long-term safety and potential for side effects after COVID-19 vaccination were critical deterrents for Asian American vaccination uptake [32,33,41,42]. These concerns also included beliefs around the COVID-19 vaccine being experimental and novel, with not enough evidence to guarantee the safety of COVID-19 vaccine recipients [37]. Two articles detailed the distrust of COVID-19 vaccination information sources as a potential determinant of Asian American vaccination uptake and willingness [30,41]. Park reported that the active role of the government in vaccination trials may have contributed to vaccine distrust, while Niño described how a lack of trust in medical institutions and officials could also play a role in vaccine hesitation across racial groups, including Asian Americans [30,41]. One study revealed that Asian Americans also had concerns about the personal financial cost to receive a COVID-19 vaccine, lack of equal distribution, and general efficacy of the COVID-19 vaccine [41].
Factors associated with greater COVID-19 vaccination uptake and willingness
Demographic and social factors were also associated with greater COVID-19 vaccine uptake and willingness across racial groups, including Asian Americans. Seven articles disclosed that age was correlated with vaccination willingness, with the majority of studies detailing that older participants were more willing to be vaccinated [32,37,38,40–43]. Park, conversely, found that Asian Americans between the ages of 30–49 had greater COVID-19 vaccine hesitations, when compared to Asian Americans below the age of 30 [41]. Six studies have also revealed higher education levels to be a predictor of greater COVID-19 vaccine willingness [30,35,37,38,43,44]. Additionally, gender was also found to be a predictor of COVID-19 vaccination willingness, with males being more likely to have greater vaccination willingness and less concerns [32,37,40,41,44]. Increased perceived risks of COVID-19–including hospitalization and loss of life–had a positive association with vaccination willingness [30,44]. Interestingly, immigration status significantly predicted vaccine willingness levels, with foreign-born Asian Americans being more likely to accept COVID-19 vaccination when compared to U.S. born Asian Americans [30,32]. One study revealed that Asian American ethnic subgroup identity was associated with COVID-19 vaccination concern levels [41].
COVID-19 testing rates and associated factors
Even though Asian Americans were found to have greater willingness for accepting COVID-19 vaccination, multiple studies reported that Asian Americans had decreased COVID-19 testing rates and that Native Hawaiian/Other Pacific Islander American participants had no significant difference in testing compared to other racial groups [18,19]. Ferguson reported that Asian American military veterans were less likely to take a COVID-19 test, when compared to other racial groups; one potential reason cited for decreased COVID-19 testing is that Asian American veterans disclosed higher levels of income compared to veterans of other racial groups, which may impact their exposure to Coronavirus [19]. Native Hawaiian and Other Pacific Islander military veterans had a similar probability of obtaining a COVID-19 test when compared to White veterans [19]. Bailey, similarly, disclosed that Asian American pediatric patients were significantly less likely to take a COVID-19 test when compared to White patients [18]. Female gender, lower income, older age, and urban status were all correlated with greater COVID-19 testing rates [19].
Other COVID-19-related health-care practices, knowledge, and information gathering
Seven articles described additional COVID-19 related practices and behaviors of the Asian American population [20,45–50]. Asian Americans were more likely to wear masks, as well as wearing masks appropriately, in public spaces during COVID-19 [46,47]. Additional predictors of mask-wearing included female gender, older age, and being located in higher population density areas [46,47]. Additional studies focused on understanding Asian American COVID-19 quarantine and isolation practices [20,48,49]. Quach reported that 70.1% of Asian American participants had at least at one point during the pandemic avoided leaving the household for any public spaces including school, religious buildings, and grocery stores [20]. Stockman, similarly, found that Asian, Native Hawaiian, or other Pacific Islander (API) women had a greater probability of staying home, instead of engaging in any external activities. API women also had a greater likelihood of isolating themselves when sick than other racial groups [49]. Jeliffe, likewise, found that Asian Americans had significantly higher awareness and utilization of paid sick leave compared to other employees [48]. Stockman et al. also disclosed that API women were more likely to use soap when hand washing, another important COVID-19 preventative behavior, relative to other participants [49]. Chua et al. – focused on understanding familial preferences for in-person learning – detailed that Asian American families had a decreased probability of sending their children to schools for in-person learning during COVID-19 [45]. Overall, Asian Americans had high COVID-19 preventative behavior uptake relative to other racial groups.
Three articles reported on COVID-19 related knowledge and information sources for Asian American populations [50–52]. Two studies revealed that Asian Americans had less knowledge related to COVID-19 compared to other racial groups [50,51]. Alobuia disclosed that Asian American participants had lower levels of COVID-19 knowledge compared to White participants; Jones, likewise, demonstrated that Asian Americans had a decreased probability of answering COVID-19 questions correctly compared to a White participant group [50,51]. The question set gauged knowledge of COVID-19 preventative behaviors, transmission, and symptomatology [51]. Greater COVID-19 knowledge levels were correlated with higher levels of income and education [50]. O’Shea revealed that Asian Americans expressed greater trust toward ‘ordinary people’ than COVID-19 experts for COVID-19 related policy decisions [52].
COVID-19 telemedicine adoption
Six articles focused on Asian American telemedicine adoption levels during COVID-19 [53–58]. Four studies disclosed that Asian Americans and Native Hawaiian & Pacific Islanders expressed less acceptance of telemedicine or digital forms of medical communication compared to other racial groups [53–56]. Meno reported that Asian Americans and Native Hawaiians and Pacific Islanders had a decreased likelihood of having telehealth visits compared to White participants; while Hsiao disclosed a negative correlation between Asian American race and telemedicine video utilization for patient visits [54,55]. Wong and Eberly, likewise, disclosed that Asian American and Native Hawaiian patients had a decreased likelihood of telemedicine appointments compared to White patients at a seizure clinic and academic health system, respectively [53,56]. Greater provider bias and increasing COVID-19 racial discrimination for the Asian American population may help explain decreased telemedicine rates [56]. Decreased income, female gender, and older age were all associated with lower levels of video telemedicine utilization [56].
Interestingly, two studies revealed greater acceptance of technology-focused provider care and telemedicine usage in the Asian American population compared to other ethnic groups. Dennis et al. disclosed that Asian Americans had greater levels of trust and benevolence toward COVID-19 screening chatbots compared to other racial groups, while Yuan et al. reported that Asian Americans had a greater probability of engaging in remote COVID-19 cardiology ambulatory visits relative to White patients [57,58]. One potential rationale provided for increased chatbot satisfaction is that certain populations felt increased comfort when sharing information with an anonymous chatbot, compared to conversing with a health-care provider [57].
Study quality and risk of bias
Of the 32 studies incorporated for systematic review, 25 were cross-sectional studies, six were cohort studies, and one was a randomized trial. As appraised by the reviewers, studies were relatively homogenous in quality and risk of bias. Criteria and reviewer responses used in evaluating study quality and risk of bias are available in Figure 2.
Figure 2.
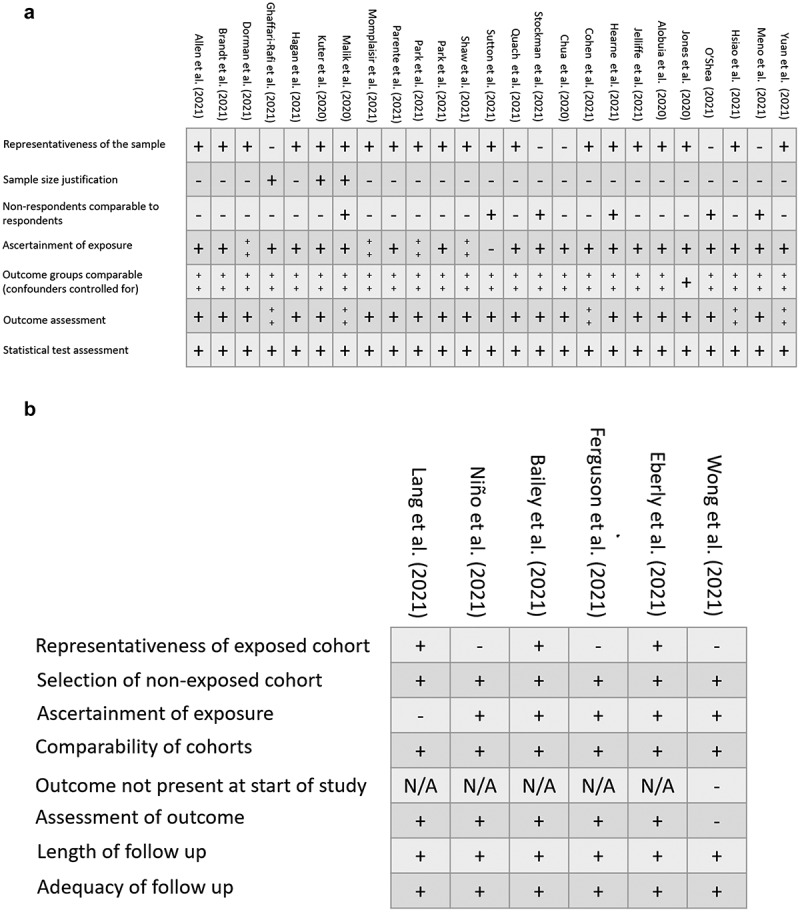
Study quality assessment. (a) Cross-sectional quality assessment. (b) Short quality assessment.
The cross-sectional quality assessment study scores ranged from 4/10 to 9/10 on the Newcastle-Ottawa Scale (NOS) variant used by Modesti et al., marking the studies selected as being poor to very good-quality overall [59]. Cohort studies assessed with the NOS incorporated by Wells et al., appraised qualities ranged from ‘fair’ to ‘good’ [29]. The one randomized controlled trial (RCT) assessed was found to have a low risk of bias overall, with a minimal risk of bias arising from lack of experimenter blinding. Thus, all the included studies were rated at low risk of bias: NOS score greater than or equal to 5 for cross sectional, at least ‘fair’ quality for cohort, and low risk of bias for RCTs.
Discussion
Our systematic review is the first of its kind to evaluate COVID-19 related practices and knowledge within the Asian American population. The majority of the studies reported greater COVID-19 vaccination willingness and decreased COVID-19 testing for Asian Americans relative to other racial groups. Common COVID-19 vaccination concerns among the Asian American population included vaccination side effects, long-term safety, and distrust of COVID-19 information sources. Higher education levels were found to be a key predictor in vaccine willingness; Asian Americans had the greatest percentage of adults with a college-level degree or higher across all U.S. racial groups [60]. Additionally, Asian Americans had high levels of COVID-19 preventative behaviors – including mask-wearing, hand washing, and social isolation – compared to other ethnic and racial groups. Contrastingly, Asian Americans had lower COVID-19 related healthcare knowledge and COVID-19 telemedicine adoption levels relative to other participants.
Subpopulation COVID-19 vaccination concerns
Asian Americans had increased COVID-19 vaccination willingness relative to other racial and ethnic groups. However, despite this overall trend, the female Asian American subpopulation reported high COVID-19 vaccine hesitancy levels. One possible explanation for greater vaccine hesitancy among Asian American females is side-effect concerns, especially potential implications of current and future pregnancy. Due to the relative novelty of the vaccine, there are limited data on short- and long-term effects of the vaccine on pregnancy; Van Spall reported that both pregnant and lactating females were excluded from COVID-19 vaccination clinical trials [34,61]. This theme is also seen in the broader U.S. population; compared to male counterparts, females were more likely to answer ‘no’ or ‘unsure’ when asked about COVID-19 vaccine intentions both within the U.S. and globally [62,63]. Another factor that may play a role in female vaccine hesitancy is the potential for adverse effects that could impact child caretaking ability [63]. The differences in COVID-19 vaccine willingness across Asian American subpopulations, including females, highlight the need to address specific vaccination concerns through targeted educational campaigns and government messaging.
Decreased Asian American COVID-19 testing
While Asian Americans showed greater acceptance of the COVID-19 vaccine, multiple studies reported that Asian Americans had lower COVID-19 testing rates relative to other racial groups [20,64,65]. Potential explanations include inaccessibility to testing sites and decreased concern rates of contracting Coronavirus [20]. Additionally, older Asian Americans with limited English proficiency (LEP) may face language challenges in trying to receive COVID-19 related care such as COVID-19 testing [66]. Specific to the veteran population, Tsai reported that Asian Americans had a greater probability of being permanently homebound relative to other racial groups, presenting a potential physical ability deterrent to receiving a COVID-19 test [67]. Additionally, decreased COVID-19 contraction concern may also be linked to high levels of Asian American COVID-19 preventative behavior uptake; Asian Americans may have felt safer due to reduced potential coronavirus exposure and therefore did not feel the need to get tested.
Internal and external cultural factors influencing COVID-19-related practices
Asian Americans were more likely to engage in appropriate preventive behaviors in curbing the spread of Coronavirus; behaviors including correct mask-wearing, handwashing, and self-isolation were more frequently observed in Asian American populations [20,46,47,49]. This difference in COVID-19 behaviors may stem from traditions and practices of preventing illness prevalent in Asian cultures. Before the COVID-19 pandemic, mask-wearing was commonly observed in East Asian countries such as China, Japan, Thailand, and Vietnam in response to prior outbreaks and pollution [68–70]. For example, Chinese mask-wearing policies trace back to the governmental response to the Manchurian Plague of 1910 [71]. Additionally, Chinese citizens were also regularly subject to government-imposed social quarantining during the 2004 SARS outbreak; universities and villages were placed under lockdown to prevent further disease spread [72,73]. Well-established preventative health behaviors present in Asia may have influenced the high levels of preventative practices of Asian Americans during COVID-19. An additional potential explanation of elevated COVID-19 preventative behaviors in the Asian American population may be due to the fact that Asian families tend to live in multigenerational households with older family members who are often at higher risk of COVID-19 related hospitalization and mortality [45,66,74,75]. Opting for virtual school or engaging in social quarantine would help reduce the possibility of infecting other family members.
The increase in COVID-19 related xenophobia and racial discrimination against Asian Americans may also contribute to the increased COVID-19 preventative behavior rates [76–78]. Multiple forms of racial discrimination increased during the COVID-19 pandemic, including vicarious and direct acts, contributing to adverse mental health outcomes in the Asian American population [79,80]. Examples of direct racially discriminatory experiences include physical violence and verbal abuse, while vicarious acts included hearing about racially discriminatory acts through media outlets and other individuals [81]. One study attributed increased Asian American stigmatization to the belief that Asian Americans had a greater likelihood of contracting COVID-19 [76]. Stockman et al. speak to the potential performative nature of engaging in COVID-19 preventative behaviors; Asian Americans may try to combat COVID-19 scapegoating by engaging in preventative behaviors to mitigate racial bias [49]. One example of this phenomenon was that Asian Americans had a greater likelihood of having fear to leave the household to purchase food products compared to other racial groups during the COVID-19 pandemic, citing increasing Asian American racialized hatred as one driver of these behavioral differences across groups [82].
Decreased COVID-19 knowledge
Multiple studies have reported that Asian Americans had low levels of COVID-19-related healthcare knowledge when compared to other racial groups [20,50]. Limited educational resources in a variety of Asian languages may influence the ability of these populations to learn about the COVID-19 pandemic. With greater than 33% of Asian Americans having LEP, there may be language barriers in accessing COVID-19 related resources; Bhutanese, Burmese, and Vietnamese Americans may be especially impacted due to high LEP levels [25,83]. While Asian Americans were more likely to receive the COVID-19 vaccine and engage in COVID-19 risk-avoidant behaviors, providing culturally appropriate resources and disseminating knowledge within Asian American communities are critical during the ongoing pandemic.
Telemedicine challenges
Asian Americans had less overall telemedicine acceptance compared to other racial and ethnic groups. Interestingly, Asian Americans have greater rates of general technology usage than other racial groups [84,85]. One potential explanation for these opposing trends is the perceived lower quality of medical care received through telemedicine by Asian Americans. Multiple studies reported that Asian Americans experienced lower patient satisfaction levels when interacting with health-care providers in-person, with potential reasons including inadequate listening and patient involvement in treatment decisions [86–88].
Telemedicine may further exacerbate these communication issues due to additional challenges in communicating effectively with patients, including the potential for health-care providers to miss nonverbal patient cues [89,90]. Indeed, Agha found that–for a veteran patient population attending pulmonary medicine appointments–telemedicine visits were more physician-focused, with the doctor driving the conversation, while the patient took a more passive role during the session compared to in-person appointments [91]. Liu, similarly, reported that internal medicine physicians spent less time with patients and utilized less empathetic behaviors toward patients in telemedicine appointments when compared to in-person visits; these behaviors were strongly correlated with better physician–patient interactions [92].
The lack of culturally-enhanced patient care experienced by Asian Americans in offline and online settings may also explain the Asian American telemedicine utilization discrepancy. In-person health-care provider–patient interactions already have a number of cultural challenges in providing effective physical and mental health care for Asian Americans that may become increasingly difficult in digital medical settings. Multiple studies cited the importance of family and familial dynamics in treating Asian American patients [93,94]. There may be greater familial expectations to be included in treatment discussion and options when compared to other racial groups [93]. Navigating this unique cultural context, health-care providers may find it challenging to balance the needs and desires of multiple stakeholders, in addition to the patient. Chesla et al., similarly, detailed how understanding the cultural context of food and diet in Chinese American culture was an important part of providing effective type 2 Diabetes treatment for Chinese Americans [94]. In both cases, the ability of health-care providers to take into account the cultural context of their Asian American patients is critical in providing the most effective form of medical care.
The technical challenges inherent to telehealth care may contribute to difficulties in providing culturally focused care to Asian American patients; Meno et al. described how the rapid switch to telehealth appointments may have led to greater challenges in providing culturally focused care [54]. LeRouge detailed the inherent challenges for a health-care provider in ensuring all technological quality requirements–System stability, environmental characteristics, and audio quality–are being met while also ensuring that the communication process with patients is effective [95]. The additional technological factors that influence telemedicine appointment quality may negatively impact health-care providers in attempting to have efficacious discussions with Asian American patients in trying to understand their unique cultural backgrounds and how they might inform patient treatment.
Limitations
There were limitations in conducting a systematic review. The ability to summarize data and outcomes across studies was challenging due to the disparate populations, outcome measures, and scales utilized across studies, preventing a meta-analysis from being conducted. The majority of studies being of a cross-sectional study design also serves as a limitation, in that the exposure and outcome are measured simultaneously, preventing a temporal relation from being established. Additionally, positive-result selection bias is a limitation; manuscripts that have positive outcomes–as opposed to inconclusive results–have a greater probability of being accepted for publication.
Future research opportunities
While our study focused narrowly on the Asian American population, future research efforts could concentrate on COVID-19 related knowledge and behavior levels of Asian populations in other locations, including in Asia and Europe. Additionally, greater research efforts should be conducted to understand COVID-19 healthcare-related behaviors and knowledge in the Pacific Islander population. Similarly, studies that focus on understanding sub-ethnic group COVID-19 related behavior and knowledge levels would be helpful in understanding the nuanced differences present across groups within the heterogeneous Asian American population; further literature on South Asian American origin groups is necessary. COVID-19 vaccination booster uptake research in Asian American and Pacific Islander populations should also be conducted. As immunity gained from a COVID-19 vaccination wanes within months, booster shots provide an additional protective layer against coronavirus during the pandemic [96,97].
Conclusion
This systematic review informs public health officials and clinicians of Asian American healthcare knowledge and behaviors that slow COVID-19 transmission, as well as telemedicine acceptance during the pandemic. By having a better understanding of common COVID-19 vaccination concerns and factors associated with greater vaccination uptake in the Asian American population, public health officials can better target messaging to address vaccine safety concerns and efficacy in minority populations. Likewise, the recognition of high levels of other COVID-19 preventative behaviors – including social quarantine, handwashing, and mask-wearing – and the cultural factors that may influence them may be useful in developing strategies to boost preventative behavior uptake in general and other minority populations. Identification of the COVID-19 knowledge gap within Asian American communities allows government and nonprofit organizations to recognize the importance of tailoring educational materials to the heterogeneous Asian American population. Lastly, this systematic review aids in understanding the unique barriers health-care providers may face when interacting with Asian American patients in telemedicine settings during and after COVID-19.
Acknowledgments
N/A
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Cucinotta D, Vanelli M.. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Xu S, Huang R, Sy LS, et al. COVID-19 vaccination and non-COVID-19 mortality risk – seven integrated health care organizations, United States, December 14, 2020-July 31, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(43):1520–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Johnson AG, Amin AB, and Ali AR, et al. COVID-19 incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of delta and omicron variant emergence – 25 U.S. Jurisdictions, April 4-December 25, 2021. MMWR Morb Mortal Wkly Rep. 2022;71(4):132–138. Accessed 10 Feb 2022. 10.15585/mmwr.mm7104e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Cohn BA, Cirillo PM, Murphy CC, et al. Wallace AW. SARS-CoV-2 vaccine protection and deaths among US veterans during 2021 TEST. Science. 2022;375(6578):331–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Science Brief : Omicron (B.1.1.529) Variant Atlanta (GA) 2020. Accessed 10 Feb 2022. Available from: https://www.ncbi.nlm.nih.gov/pubmed/34932278.
- [7].Riediker M, Briceno-Ayala L, Ichihara G, et al. Higher viral load and infectivity increase risk of aerosol transmission for Delta and Omicron variants of SARS-CoV-2. Swiss Med Wkly. 2022;152:w30133. [DOI] [PubMed] [Google Scholar]
- [8].Howard J, Huang A, Li Z, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci U S A. 2021;118(4):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Pradhan D, Biswasroy P, Kumar Naik P, et al. A review of current interventions for COVID-19 Prevention. Arch Med Res. 2020;51(5):363–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Goldust M, Abdelmaksoud A, Navarini AA. Hand disinfection in the combat against COVID-19. J Eur Acad Dermatol Venereol. 2020;34(9):e454–e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Do BN, Tran TV, Phan DT, et al. Health literacy, eHealth literacy, adherence to infection prevention and control procedures, lifestyle changes, and suspected COVID-19 symptoms among health care workers during lockdown: online survey. J Med Internet Res. 2020;22(11):e22894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Andrasfay T, Goldman N. Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the black and Latino populations. medRxiv. 2020. DOI: 10.1101/2020.07.12.20148387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rincon Uribe FA, Godinho RCS, Machado MAS, et al. Health knowledge, health behaviors and attitudes during pandemic emergencies: a systematic review. PLoS One. 2021;16(9):e0256731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Siddiquea BN, Shetty A, Bhattacharya O, et al. Global epidemiology of COVID-19 knowledge, attitude and practice: a systematic review and meta-analysis. BMJ Open. 2021;11(9):e051447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Tegegne GT, Kefale B, Engidaw MT, et al. Knowledge, attitude, and practice of healthcare providers toward novel coronavirus 19 during the first months of the pandemic: a systematic review. Front Public Health. 2021;9:606666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Clavel N, Badr J, Gautier L, et al. Risk perceptions, knowledge and behaviors of general and high-risk adult populations towards COVID-19: a systematic scoping review. Public Health Rev. 2021;42:1603979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Budiman A. RNG. Asian Americans are the fastest-growing racial or ethnic group in the U.S.2021. Accessed 15 Feb 2022. Available from: https://www.pewresearch.org/fact-tank/2021/04/09/asian-americans-are-the-fastest-growing-racial-or-ethnic-group-in-the-u-s/.
- [18].Bailey LC, Razzaghi H, Burrows EK, et al. Assessment of 135794 pediatric patients tested for severe acute respiratory syndrome coronavirus 2 across the United States. JAMA Pediatr. 2021;175(2):176–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ferguson JM, Abdel Magid HS, Purnell AL, et al. Differences in COVID-19 testing and test positivity among veterans, United States, 2020. 433021. 2021;136(4):483–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Quach T, Ethoan LN, Liou J, et al. A rapid assessment of the impact of COVID-19 on Asian Americans: cross-sectional survey study. JMIR Public Health Surveill. 2021;7(6):e23976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Jang Y, Park NS, Yoon H, et al. The risk typology of healthcare access and its association with unmet healthcare needs in Asian Americans. Health Soc Care Community. 2018;26(1):72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Jang Y, Yoon J, Park NS. Source of health information and unmet healthcare needs in Asian Americans. J Health Commun. 2018;23(7):652–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kochhar R. CA. income inequality in the U.S. is rising most rapidly among Asians 2018. Accessed 16 Feb 2022. Available from: https://www.pewresearch.org/social-trends/2018/07/12/income-inequality-in-the-u-s-is-rising-most-rapidly-among-asians/.
- [24].Devakumar D, Shannon G, Bhopal SS, et al. Racism and discrimination in COVID-19 responses. Lancet. 2020;395(10231):1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Wang D, Gee GC, Bahiru E, et al. Asian-Americans and Pacific Islanders in COVID-19: emerging disparities amid discrimination. J Gen Intern Med. 2020;35(12):3685–3688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Gotschall T. EndNote 20 desktop version. J Med Libr Assoc. 2021;109(3):520–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan – a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Wells G, Shea B, and O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses 2021. Accessed 3 Jan 2022. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- [30].Nino MD, Hearne BN, Cai T. Trajectories of COVID-19 vaccine intentions among U.S. adults: the role of race and ethnicity. SSM Popul Health. 2021;15:100824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Malik AA, McFadden SM, Elharake J, et al. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Ta Park VM, Dougan M, Meyer OL, et al. Vaccine willingness: findings from the COVID-19 effects on the mental and physical health of Asian Americans & Pacific Islanders survey study (COMPASS). Prev Med Rep. 2021;23:101480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Shaw J, Stewart T, Anderson KB, et al. Assessment of US healthcare personnel attitudes towards coronavirus disease 2019 (COVID-19) vaccination in a large university healthcare system. Clin Infect Dis. 2021;73(10):1776–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Sutton D, D’Alton M, Zhang Y, et al. COVID-19 vaccine acceptance among pregnant, breastfeeding, and nonpregnant reproductive-aged women. Am J Obstet Gynecol MFM. 2021;3(5):100403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Allen JD, Abuelezam NN, Rose R, et al. Factors associated with the intention to obtain a COVID-19 vaccine among a racially/ethnically diverse sample of women in the USA. Transl Behav Med. 2021;11(3):785–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Brandt EJ, Rosenberg J, Waselewski ME, et al. National study of youth opinions on vaccination for COVID-19 in the U.S. J Adolesc Health. 2021;68(5):869–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kuter BJ, Browne S, Momplaisir FM, et al. Perspectives on the receipt of a COVID-19 vaccine: a survey of employees in two large hospitals in Philadelphia. Vaccine. 2021;39(12):1693–1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Lang MA, Stahlman S, and Wells NY, et al. Disparities in COVID-19 vaccine initiation and completion among active component service members and health care personnel, 11 December 2020-12 march 2021. Msmr. Internet]. 2021. Available from.;284:2–9. Accessed 11 Nov 2021. https://www.ncbi.nlm.nih.gov/pubmed/33975434 [PubMed] [Google Scholar]
- [39].Momplaisir FM, Kuter BJ, Ghadimi F, et al. Racial/ethnic differences in COVID-19 vaccine hesitancy among health care workers in 2 Large academic hospitals. JAMA Network Open. 2021;4(8):e2121931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Hagan LM, Dusseau C, Crockett M, et al. COVID-19 vaccination in the federal bureau of prisons, December 2020-April 2021. Vaccine. 2021;39(40):5883–5890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Ta Park V, Dougan M, Meyer O, et al. Differences in COVID-19 vaccine concerns among Asian Americans and Pacific Islanders: the COMPASS survey. J Racial Ethn Health Disparities. 2021;9(3):979–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Ghaffari-Rafi A, Teehera KB, Higashihara TJ, et al. Variables associated with coronavirus disease 2019 vaccine hesitancy amongst patients with neurological disorders. Infect Dis Rep. 2021;13(3):763–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Dorman C, Perera A, Condon C, et al. Factors associated with willingness to be vaccinated against COVID-19 in a large convenience sample. J Community Health. 2021;46(5):1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Parente DJ, Ojo A, Gurley T, et al. Acceptance of COVID-19 vaccination among health system personnel. J Am Board Fam Med. 2021;34(3):498–508. [DOI] [PubMed] [Google Scholar]
- [45].Chua KP, DeJonckheere M, Reeves SL, et al. Factors associated with school attendance plans and support for COVID-19 risk mitigation measures among parents and guardians. Acad Pediatr. 2021;21(4):684–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Cohen DA, Talarowski M, Awomolo O, et al. Systematic observation of mask adherence and distancing (SOMAD): findings from Philadelphia. Prev Med Rep. 2021;23:101449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Hearne BN, Nino MD. Understanding how race, ethnicity, and gender shape mask-wearing adherence during the COVID-19 pandemic: evidence from the COVID impact survey. J Racial Ethn Health Disparities. 2022;9(1):176–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Jelliffe E, Pangburn P, Pichler S, et al. Awareness and use of (emergency) sick leave: US employees’ unaddressed sick leave needs in a global pandemic. Proc Natl Acad Sci U S A. 2021;118(29):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Stockman JK, Wood BA, Anderson KM. Racial and ethnic differences in COVID-19 outcomes, stressors, fear, and prevention behaviors among US women: web-based cross-sectional study. J Med Internet Res. 2021;23(7):e26296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Alobuia WM, Dalva-Baird NP, Forrester JD, et al. Racial disparities in knowledge, attitudes and practices related to COVID-19 in the USA. J Public Health (Oxf). 2020;42(3):470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Jones J, Sullivan PS, Sanchez TH, et al. Similarities and differences in COVID-19 awareness, concern, and symptoms by race and ethnicity in the United States: cross-sectional survey. J Med Internet Res. 2020;22(7):e20001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].O’Shea BA, Ueda M. Who is more likely to ignore experts’ advice related to COVID-19? Prev Med Rep. 2021;23:101470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Wong VSS, Williams MK, Akiona CK, et al. Demographic and technological factors influencing virtual seizure clinic visit satisfaction before and during the Covid-19 pandemic in rural Hawaii. Epilepsy Behav. 2021;124:108374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Meno M, Abe J, Fukui J, et al. Telehealth amid the COVID-19 pandemic: perception among Asian, native Hawaiian and Pacific Islander cancer patients. Future Oncol. 2021;17(23):3077–3085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Hsiao V, Chandereng T, Lankton RL, et al. Disparities in telemedicine access: a cross-sectional study of a newly established infrastructure during the COVID-19 pandemic. Appl Clin Inform. 2021;12(3):445–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Eberly LA, Kallan MJ, Julien HM, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Network Open. 2020;3(12):e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Dennis AR, Kim A, Rahimi M, et al. User reactions to COVID-19 screening chatbots from reputable providers. J Am Med Inform Assoc. 2020;27(11):1727–1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Yuan N, Pevnick JM, Botting PG, et al. Patient use and clinical practice patterns of remote cardiology clinic visits in the era of COVID-19. JAMA Network Open. 2021;4(4):e214157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Modesti PA, Reboldi G, Cappuccio FP, et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One. 2016;11(1):e0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Census Bureau Releases New Educational Attainment Data Census Bureau 2022. Accessed 9 June 2022. Available from: https://www.census.gov/newsroom/press-releases/2022/educational-attainment.html?fbclid=IwAR0fKQuV3PjJ2yA5IiRXi704pODi_Q1MYnT8irDhbMcmD-pBm0eEXRk747A.
- [61].Van Spall HGC. Exclusion of pregnant and lactating women from COVID-19 vaccine trials: a missed opportunity. Eur Heart J. 2021;42(28):2724–2726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Fisher KA, Bloomstone SJ, Walder J, et al. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173(12):964–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Khubchandani J, Sharma S, Price JH, et al. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46(2):270–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Yan BW, Hwang AL, Ng F, et al. Death toll of COVID-19 on Asian Americans: disparities revealed. J Gen Intern Med. 2021;36(11):3545–3549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Escobar GJ, Adams AS, Liu VX, et al. Racial disparities in COVID-19 testing and outcomes: retrospective cohort study in an integrated health system. Ann Intern Med. 2021;174(6):786–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Ma KPK, Bacong AM, Kwon SC, et al. The impact of structural inequities on older Asian Americans during COVID-19. Front Public Health. 2021;9:690014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Tsai J, Whealin JM, Pietrzak RH. Asian American and Pacific islander military veterans in the United States: health service use and perceived barriers to mental health services. Am J Public Health. 2014;104(Suppl S4):S538–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Burgess A, Horii M. Risk, ritual and health responsibilisation: Japan’s ‘safety blanket’ of surgical face mask-wearing. Sociol Health Illn. 2012;34(8):1184–1198. [DOI] [PubMed] [Google Scholar]
- [69].Feng S, Shen C, Xia N, et al. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8(5):434–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Greenhalgh T, Schmid MB, Czypionka T, et al. Face masks for the public during the covid-19 crisis. BMJ. 2020;369:m1435. [DOI] [PubMed] [Google Scholar]
- [71].Gong B, Genealogical A. Study of facemasks in China: from hygienic modernity to care. Fudan Journal of the Humanities and Social Sciences. 2022;15(2):189–206. [Google Scholar]
- [72].Huremović D. Social distancing, quarantine, and isolation. In: Huremović D, editor. Psychiatry of pandemics: a mental health response to infection outbreak. Cham: Springer International Publishing; 2019. p. 85–94. [Google Scholar]
- [73].Y. H . THE SARS epidemic and its aftermath in China: a political perspective. learning from SARS: preparing for the next disease outbreak: workshop summary. US: Institute of Medicine (US) Forum on Microbial Threats: National Academies Press; 2004. [PubMed] [Google Scholar]
- [74].Cohn D, and Passel JS. A record 64 million Americans live in multigenerational households 2018. Accessed 23 Feb 2022. Available from: https://www.pewresearch.org/fact-tank/2018/04/05/a-record-64-million-americans-live-in-multigenerational-households/.
- [75].CDC . COVID-19 mortality overview: National Center for Health Statistics; 2022. Accessed 27 Feb 2022. Available from: https://www.cdc.gov/nchs/covid19/mortality-overview.htm?fbclid=IwAR02eWas5TPno1IOz6zJqnkxeChoVXfJcBbJeHGiNIzMi6RBNshMLLlTj2g.
- [76].Pan S, Shen G, Liu C, et al. Coronavirus stigmatization and psychological distress among Asians in the United States. Ethn Health. 2021;26(1):110–125. [DOI] [PubMed] [Google Scholar]
- [77].Wu C, Qian Y, Wilkes R. Anti-Asian discrimination and the Asian-white mental health gap during COVID-19. Ethnic Racial Stud. 2020;44(5):819–835. [Google Scholar]
- [78].Trammell J, Joseph N, Harriger J. Racial and ethnic minority disparities in COVID-19 related health, health beliefs and behaviors, and well-being among students. J Am Coll Health. 2021;1–7. DOI: 10.1080/07448481.2021.1890606 [DOI] [PubMed] [Google Scholar]
- [79].Chae DH, Yip T, Martz CD, et al. Vicarious racism and vigilance during the COVID-19 pandemic: mental health implications Among Asian and black Americans. 433021. 2021;136(4):508–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Woo B, Jun J. COVID-19 racial discrimination and depressive symptoms among Asians Americans: does communication about the incident matter? J Immigr Minor Health. 2022;24(1):78–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Lee S, Waters SF. Asians and Asian Americans’ experiences of racial discrimination during the COVID-19 pandemic: impacts on health outcomes and the buffering role of social support. Stigma and Health. 2021;6(1):70–78. [Google Scholar]
- [82].Morales DX, Morales SA, Beltran TF. Racial/ethnic disparities in household food insecurity during the COVID-19 Pandemic: a nationally representative study. J Racial Ethn Health Disparities. 2021;8(5):1300–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Lee J, Ramakrishnan K, Wong J. Accurately counting Asian Americans is a civil rights issue. ANNALS Am Acad Political Social Sci. 2018;677(1):1. [Google Scholar]
- [84].Perrin A. English-speaking Asian Americans stand out for their technology use Washington, DC: pew research center; 2016. Accessed 25 Jan 2022. Available from: https://www.pewresearch.org/fact-tank/2016/02/18/english-speaking-asian-americans-stand-out-for-their-technology-use/.
- [85].Bender MS, Choi J, Arai S, et al. Digital technology ownership, usage, and factors predicting downloading health apps among caucasian, Filipino, Korean, and latino Americans: the digital link to health survey. JMIR Mhealth Uhealth. 2014;2(4):e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Liao L, Chung S, Altamirano J, et al. The association between Asian patient race/ethnicity and lower satisfaction scores. BMC Health Serv Res. 2020;20(1):678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Saha S, Hickam DH. Explaining low ratings of patient satisfaction among Asian-Americans. Am J Med Qual. 2003;18(6):256–264. [DOI] [PubMed] [Google Scholar]
- [88].Ngo-Metzger Q, Legedza AT, Phillips RS. Asian Americans’ reports of their health care experiences. Results of a national survey. J Gen Intern Med. 2004;19(2):111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Brown S. Preserving the human touch in medicine in a digital age. Cmaj. 2019;191(22):E622–E3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Toh N, Pawlovich J, Grzybowski S. Telehealth and patient-doctor relationships in rural and remote communities. Can Fam Physician. Internet]. 2016. Dec PMC5154642]; 62(12):[961–963 pp.]. Available from:. https://www.ncbi.nlm.nih.gov/pubmed/27965327 [PMC free article] [PubMed] [Google Scholar]
- [91].Agha Z, Roter DL, Schapira RM. An evaluation of patient-physician communication style during telemedicine consultations. J Med Internet Res. 2009;11(3):e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Liu X, Sawada Y, Takizawa T, et al. Doctor-patient communication: a comparison between telemedicine consultation and face-to-face consultation. Intern Med. 2007;46(5):227–232. [DOI] [PubMed] [Google Scholar]
- [93].Park M, Chesla CA, Rehm RS, et al. Working with culture: culturally appropriate mental health care for Asian Americans. J Adv Nurs. 2011;67(11):2373–2382. [DOI] [PubMed] [Google Scholar]
- [94].Chesla CA, Chun KM, Kwan CM. Cultural and family challenges to managing type 2 diabetes in immigrant Chinese Americans. Diabetes Care. 2009;32(10):1812–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].LeRouge CM, Garfield MJ, Hevner AR. Patient perspectives of telemedicine quality. Patient Prefer Adherence. 2015;9:25–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Goldberg Y, Mandel M, Bar-On YM, et al. Waning immunity after the BNT162b2 vaccine in Israel. N Engl J Med. 2021;385(24):e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Ferdinands JM, Rao S, Dixon BE, et al. Waning 2-dose and 3-dose effectiveness of mRNA vaccines against COVID-19-associated emergency department and urgent care encounters and hospitalizations among adults during periods of delta and omicron variant predominance – VISION network, 10 states, August 2021-January 2022. MMWR Morb Mortal Wkly Rep. 2022;71(7):255–263. [DOI] [PMC free article] [PubMed] [Google Scholar]


