PURPOSE:
Patients with and survivors of hematologic malignancies are particularly vulnerable to COVID-19 disease and complications. This study examined patients' vaccination attitudes and behaviors and their correlates.
METHODS:
A two-wave survey was fielded in December 2020 and June 2021 among hematologic malignancy patients and survivors (N = 2,272). Demographic characteristics, intent to get vaccinated, vaccination status, attitudes toward vaccination, and level of trust in specific sources of information about COVID-19 vaccines were assessed. Descriptive statistics were calculated, and linear probability models were estimated to examine binary outcomes and their correlates.
RESULTS:
In December 2020, before COVID-19 vaccines were available, 73% stated they were likely or very likely to get vaccinated if an FDA-approved vaccine became available; however, in June 2021 over 90% reported being vaccinated. Being younger, unmarried, trusting local faith leaders, and not having a bachelor's degree or more were negatively associated with getting vaccinated. Among those hesitant in December 2020, those who expressed a distrust of vaccines in general were least likely to get vaccinated. Being vaccinated in June 2021 was positively associated with the degree to which respondents trust their oncologist, federal agencies, and pharmaceutical companies. Oncologists and primary care physicians were reported as the most trusted sources for information about vaccines.
DISCUSSION:
COVID-19 vaccine hesitancy remains a public policy concern even now, as additional boosters are recommended among vulnerable populations. Our findings suggest that patient trust in their treating physicians can play a critical role in promoting individual patient and public health goals.
INTRODUCTION
An estimated 1.5 million people in the United States are living with or in remission from a hematologic malignancy (blood cancer).1 Many patients with blood cancer and survivors are particularly vulnerable to COVID-19 disease and complications, as blood cancers can affect the bone marrow, blood cells, and lymphatic system,2 and most patients tend to be diagnosed in the sixth through ninth decades of life.3-6 Moreover, certain blood cancer treatments can be immunosuppressive.7 However, vaccination can reduce risks associated with COVID-19,8,9 and data have also shown that booster shots can help some patients significantly (depending on the type of cancer and treatment received).10,11
Although CDC guidelines prioritize patients with cancer in the 1c vaccine group,12 patients with cancer have expressed concerns related to the vaccine, in part because this group has faced inconsistent vaccine guidelines and because patients with cancer were excluded from COVID-19 vaccine trials, resulting in lack of data on vaccine safety and efficacy.13-16 Data on vaccine adoption among patients with cancer and other vulnerable subpopulations are scarce, although vaccines have become widely available in the United States. Little is known about how demographic factors and vaccine concerns relate to adoption and what sources of information about vaccination are most trusted among patients with cancer.
To better understand vaccination attitudes and behavior over time among patients with and survivors of a blood cancer, a nationwide two-wave survey was conducted. This study aimed to understand (1) the predictors of vaccination intentions in December 2020, prior the first vaccine approval; (2) the predictors of vaccination status in June 2021; (3) the extent to which different vaccination concerns predict later vaccine behavior among those who are hesitant in 2020; and (4) the association between trust in various sources of information about COVID-19 vaccines and vaccination status in June 2021. The goal of these efforts was to identify factors that may maximize vaccine adoption and adherence to evolving booster recommendations among this population.
METHODS
Study Design and Conduct
The first survey was launched in December 2020. Survey invitations were distributed via email to approximately 93,000 patients with and survivors of hematological malignancy (leukemia, lymphoma, myeloma, myeloproliferative neoplasms, and myelodysplastic syndromes [MDS]) in The Leukemia & Lymphoma Society's (LLS) constituent database. In total, 6,516 responses were obtained, for a response rate of 7%. The survey was distributed in English only.
Survey design was informed by the Health Beliefs Model.17,18 In the first survey, demographic information, cancer diagnosis, and treatment status were recorded, and participants were asked questions about their attitudes toward vaccination. Specifically, they were asked: “Imagine that your doctor offers you a COVID-19 vaccine for free in January 2021. How likely are you to choose to get the vaccine?” scored on a five-point Likert scale (very unlikely, unlikely, neither likely nor unlikely, likely, and very likely). Participants were also asked to indicate why they were likely/unlikely to get vaccinated (they could choose between 10 different options).
The second survey was fielded in June 2021 and was distributed to the same LLS constituent database. In total, 6,389 participants responded to the second wave (a response rate of 6.7%), and 2,272 individuals responded to both waves. As an aim of the study was to assess hesitancy and adoption over time, attention in this article is restricted to respondents who completed both waves.
In the second wave, demographic information was re-elicited, and participants were asked if they had received one or more vaccines, why they had or had not gotten vaccinated, and, if unvaccinated, if they are likely to get vaccinated in the future. Finally, participants were asked whether they trust different sources, such as their oncologist, pharmaceutical companies, and federal agencies, for information about COVID-19 vaccines.
This study was approved by the Institutional Review Board of Boston University (#A231602CD). Participants were not remunerated for their participation. Both surveys were administered via Qualtrics. In both waves, those who had not responded to the survey after one week received a reminder email, and participants had two weeks to complete the survey.
Statistical Analysis
Descriptive statistics were conducted regarding respondents' experiences with and attitudes toward COVID-19 vaccines. Multiple regression analyses were conducted that examine the four aims outlined above. All multiple regression analyses were conducted using linear probability models with binary outcomes, controlling for respondents' age, race/ethnicity, sex, marital status, educational attainment, residence, treatment status, and cancer diagnosis. Only results that are statistically significant at a 5% level are reported in the text. Statistical software Stata (version 16) was used to conduct the data analyses.
RESULTS
Sample Characteristics
The average age of respondents was 65.75 years; 61.1% were female. The majority identified as White (93%), 5.86% as African American/Black, and 1.04% as Asian; 4.26% identified as Hispanic or Latino/a. Most (58.7%) had a bachelor's degree or higher, and 87.24% reported living in urban zip codes. For comparison, the estimated overall population of patients with blood cancer in the United States is 87.1% White, 9.6% Black, 8.8% Hispanic, and 3% Asian, with the prevalence of blood cancer being greater among men than women and with most cases being diagnosed at age 65 years or older.19
Respondents could identify as both patients and survivors; 65% stated that they were patients, and 38.4% identified as survivors. Although leukemia was the most common reported diagnosis (40%), 32.7% had been diagnosed with lymphoma, 30.4% with myeloma, 8.36% with MDS, and 8.5% with myeloproliferative neoplasms. Furthermore, 61.8% stated that they were currently undergoing treatment, and 32.7% reported having had a stem-cell transplant.
Predictors of Vaccination Intentions in December 2020
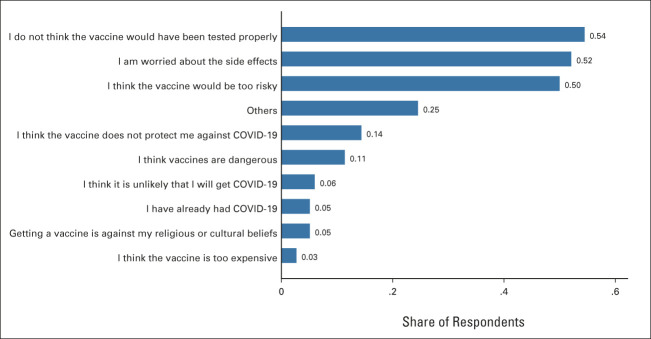
Figure 1 presents respondents' intentions to get vaccinated in December 2020, before emergency use authorization of any COVID-19 vaccine. The majority of respondents (52.8%) stated that they are very likely to get vaccinated, and 20% stated that they are likely to get vaccinated. However, 15.8% indicated that they are vaccine hesitant (ie, unlikely or very unlikely to get vaccinated).
FIG 1.
Intentions to get vaccinated in December 2020. Responses are from the survey conducted in December 2020. Sample size = 2,120.
Multiple regression analysis (n = 1,114) revealed that identifying as female was positively associated with vaccine hesitancy (b = 0.0511, P < .01), identifying as African American/Black was positively associated with vaccine hesitancy (b = 0.14, P < .05), age (in years) was negatively associated with being vaccine hesitant (b =–0.0045, P < .01), and having a bachelor's degree or more was also negatively associated with vaccine hesitancy (b = –0.0414, P < .05). There was no significant association between vaccine hesitancy and identifying as other race/ethnicities, whether the participant lived in a rural/urban zip code, cancer diagnosis, or treatment status.
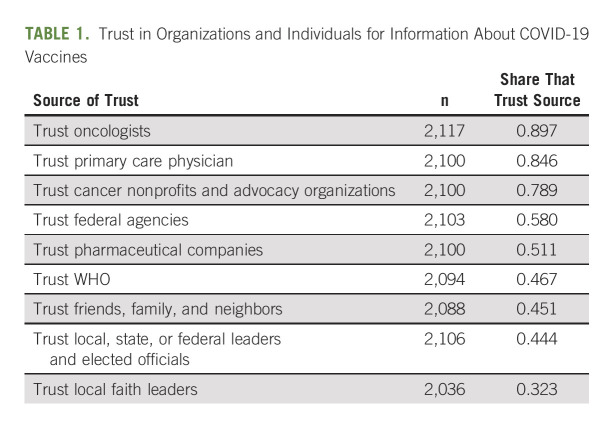
Among the 334 patients and survivors who stated that they were unlikely or very unlikely to get vaccinated, 54% reported concern that the vaccines were not tested properly (Fig 2). The second-most common concern was side effects (52%), followed by the vaccine would be too risky (50%). Fourteen percent of respondents believed that the vaccine would not protect them against COVID-19, and 11% expressed a general skepticism toward vaccines by stating that vaccines are dangerous. In total, 41.9% of those who stated that they were unlikely or very unlikely to get a vaccine cited having just one concern while 22.2% cited two concerns.
FIG 2.
Reasons for being unlikely to get a COVID-19 vaccine in December 2020 among those who stated that they were unlikely or very unlikely to get vaccinated. Sample size = 334.
Predictors of Vaccination Behavior in 2021
In the second survey (June 2021), 90.7% of respondents indicated that they had gotten one or more vaccines. Of those who were vaccinated, 52.2% had received a Pfizer-BioNTech vaccine, 44.2% had received a Moderna vaccine, and 3.4% had received a Johnson & Johnson (Janssen) vaccine. Furthermore, 97.9% of those who had received a two-dose vaccine (Pfizer-BioNTech or Moderna) had already received two doses. Most (68.5%) of those who remained unvaccinated in June 2021 stated that they were unlikely or very unlikely to take a COVID-19 vaccine in the future.
Those who stated that they were likely/very likely to get vaccinated in December 2020 were most likely to have gotten vaccinated by June 2021. However, 49.4% of those who stated that they were very unlikely to get vaccinated reported that they ended up receiving a vaccine, and 79.4% of those who stated they were unlikely to get vaccinated got vaccinated. Those who cited the most concerns about not getting vaccinated in December 2020 were, on average, the least likely to get vaccinated by June 2021. For example, 72% of those with one concern ended up getting vaccinated while only 55% of those with four concerns were vaccinated, and 33% of those with six concerns were vaccinated.
Among those who remained unvaccinated in June 2021, the majority were worried about the vaccine being too risky for their health (59%). Moreover, 53% of participants stated that my cancer care team does not recommend that I receive the vaccine at this time, and 49% reported worry about side effects.
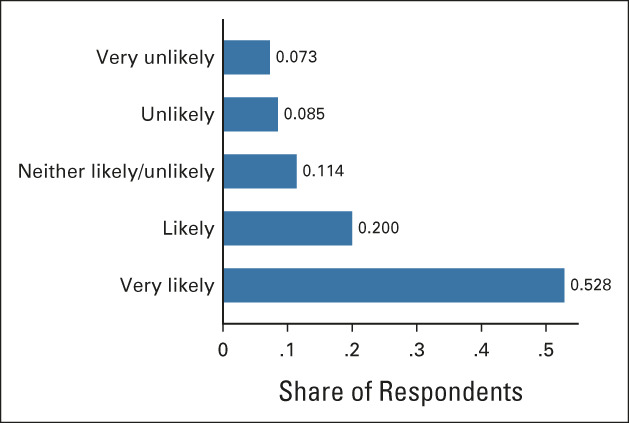
Multiple regression analysis was conducted (Appendix Table A1, online only) to examine the association between vaccination status in June 2021 and demographic variables as well as treatment status and cancer diagnosis (n = 1,114). It was found that age (measured in years) was positively associated with getting vaccinated (b = 0.003, P < .01). Being married was also positively associated vaccination status (b = 0.043, P < .05), as was having a bachelor's degree or more (b = 0.043, P < .05). Vaccination status in June 2021 was not found to be significantly associated with race/ethnicity, living in an urban/rural zip code, blood cancer diagnosis, or treatment status.
The Extent to Which Different Vaccine Concerns Predict Later Vaccination Behavior Among Those Who Were Hesitant in 2020
Multiple regression analysis was also conducted among those who stated that they were unlikely to get vaccinated in December 2020, where vaccine status in June 2021 was the dependent variable, and the concerns listed in Figure 2 were included as independent variables (n = 332). The regression showed that those who cited the vaccine being too risky as a concern were less likely to get vaccinated (b = –0.125, P < .05) and that those who thought that vaccines are dangerous in general were the least likely to get vaccinated (b = –0.421, P < .01).
The Association Between Trust in Various Sources of Information About COVID-19 Vaccines and Vaccine Status in June 2021
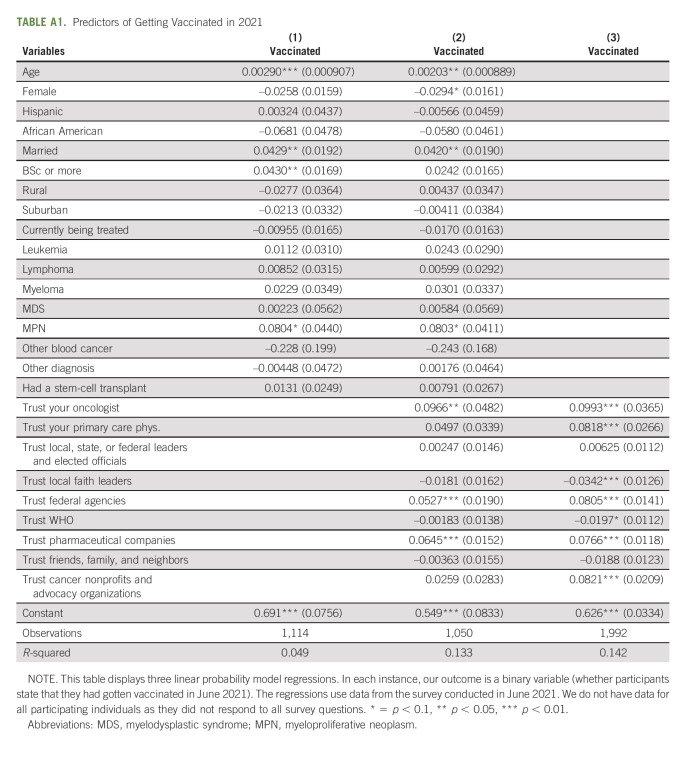
Organizations and individuals that respondents trust for information about COVID-19 vaccines were examined (Table 1). Oncologists are trusted by 89.7%, making them the most trusted source for information about COVID-19 vaccines. The second-most trusted source is primary care physicians (84.6%). The third-most trusted source is cancer nonprofits and advocacy organizations (78.9%). There is a sharp drop-off to fourth place, held by federal agencies (58%).
TABLE 1.
Trust in Organizations and Individuals for Information About COVID-19 Vaccines
Those who were unvaccinated in June 2021 were less likely to trust the sources listed in Table 1. Specifically, it was found that 65% of those unvaccinated trust their oncologist, 57% trust their primary care physician, and 48% trust cancer nonprofits. Few in this group trust pharmaceutical companies (11%), and only 16% trust federal agencies. Moreover, 29% of individuals in this group trust faith leaders, and 36% trust family and friends.
Finally, there is a strong association between whether participants trust different sources of information and whether they were vaccinated. Multiple regression analysis was conducted with vaccine status as the dependent variable and with trust in the sources listed in Table 1 as the independent variables (n = 1,992). This analysis shows that trusting your oncologist is positively associated with getting vaccinated (b = 0.099, P < .01). Trusting your primary care physician is also positively associated with getting vaccinated (b = 0.082, P < .01), as is trusting cancer nonprofits (b = 0.082, P < .01), federal agencies (b = 0.081, P < .01), and trusting pharmaceutical companies (b = 0.077, P < .01). Trusting local faith leaders was negatively associated with getting vaccinated (b = –0.034, P < .01).
DISCUSSION
In December 2020, which was before a vaccine becoming publicly available, those more likely to be vaccine hesitant identified as younger, female, and Black/African American and reported a lower level of education (less than a bachelor's degree). In June 2021, those most likely to be unvaccinated identified as younger, less educated (less than a bachelor's degree), and not married. Predictors of intent and vaccination found in this study are similar to those found by KFF and others.20 As found by KFF, race did not persist as a predictor of vaccination.21
Despite significant vaccine hesitancy in December 2020, most patients with hematological malignancy overcame concerns regarding COVID-19 vaccination and had received two doses by June 2021. This result may be as one would expect; as more information became available about the vaccine, patients and survivors were receiving the vaccine without serious side effects, vaccination became key to engaging with others and social activities, and many physicians were encouraging vaccination.22
Similar to others' findings, this study found a strong correlation between vaccine intention and eventual behavior, which is positive news for the large body of work that uses vaccine intentions as a proxy for actual vaccination behavior. The results suggest that it may be reasonable to use vaccine intentions as an outcome measure in experiments that evaluate the effects of various vaccine interventions and campaigns.23-27
Concerns among those who were hesitant in December 2020 predicted persistent hesitancy in 2021, specifically the vaccine being too risky and that vaccines are dangerous. This finding among a particularly vulnerable population is similar to others' findings in the general population—ie, overarching negative vaccine beliefs are a significant predictor of unwillingness to be vaccinated.28 The findings also suggest that blood cancer patients' vaccine behavior is predicted by trust in sources of information (again, these findings are similar KFF).29 Interestingly, the analyses show that relatively few respondents believed that the vaccines were ineffective (14%) and that many (53%) stated that their cancer care team advised them against taking the vaccine. The former is somewhat surprising given the information circulating about the vaccine being ineffective for certain groups, and the latter is surprising given the low prevalence of conditions, even among patients with blood cancer, that make the vaccines unsuitable. It must be acknowledged, however, that significantly less information about suitability was available in June 2021 than today.
The present study suggests that oncologists have an important role in discussing vaccination with patients and caregivers by answering questions and addressing concerns, uncertainty, misinformation, and misperceptions that are relevant to that particular patient and in the context of their values, with the recognition that beliefs evolve over time.30 Although the unvaccinated exhibited less trust overall, more than half of those who were unvaccinated at follow-up trust their oncologist for information about COVID-19 vaccines. The findings that vaccinated patients with cancer view health care providers and nonprofit organizations as trusted sources of COVID-19 information while both vaccinated and unvaccinated patients exhibit less trust in the government are similar to other studies on patients with cancer and the general population.31-33
These findings suggest important roles for government. First, public health officials can support oncologists and other trusted messengers by working to ensure that they have access to comprehensive and up-to-date information about vaccine safety and efficacy. Drawing on successful examples of community engagement, the findings from this study stress the importance of public health officials partnering with local healthcare providers and community organizations to develop tailored outreach programs to address questions and concerns of local populations.34 At the same time, it is vital that government officials avoid statements and actions that erode public confidence in the safety and value of vaccinations when systematic evidence meeting accepted scientific criteria demonstrates their value. Second, given the positive association between trust in federal agencies and vaccine uptake, public health officials should work to build trust in these agencies by remaining responsive to emerging data and by communicating transparently about regulatory decision- making, especially as it relates to the medical needs of vulnerable populations.
It is important to note that this study sample is not fully representative of the general population of patients with blood cancer and survivors, as the survey was conducted among a group that has previously engaged with an advocacy organization. In addition, the survey was administered only in English, which limits the generalizability of the results to non-English speaking patients and survivors. Moreover, although the response rate was consistent with past surveys conducted using the LLS constituent database, the rate was under 10%. It is unknown whether the results generalize to wider groups of patients with cancer or racial and ethnic populations underrepresented in the survey population. Moreover, self-reported political party affiliation and income level were not collected.
In conclusion, despite vaccine hesitancy in December 2020, most patients with and survivors of hematological malignancies overcame their concerns regarding COVID-19 vaccination and had received two doses by June 2021. Most patients and survivors who were hesitant later reported receiving the vaccine. Those hesitant were primarily concerned about the vaccine's safety, effectiveness, and development process. Lack of vaccination at follow-up was predicted by younger age, not being married, and not having a bachelor's degree or more. Vaccination status at follow-up was not significantly associated with race/ethnicity, living in an urban/rural zip code, blood cancer diagnosis, or treatment status. Those initially hesitant and who did not get vaccinated at follow-up were most likely to cite concerns that the vaccine is too risky and vaccines are dangerous in general. Moreover, although results indicate that physicians were most trusted when it comes to vaccine information, those unvaccinated were substantially less likely to trust physicians and all other sources of information. These results have important implications for efforts that can be undertaken by the medical community and advocacy organizations, as well as public health and other government officials, regarding vaccine decision-making support among this vulnerable population.
APPENDIX
TABLE A1.
Predictors of Getting Vaccinated in 2021
Elisa S. Weiss
Research Funding: AbbVie (Inst), AstraZeneca (Inst), Amgen (Inst), Bristol Myers Squibb/Celgene (Inst)
Maria Sae-Hau
Stock and Other Ownership Interests: Moderna Therapeutics (I), Acceleron Pharma (I), argenx (I), Beam Therapeutics (I), BridgeBio Pharma (I), Schrodinger (I), Applied DNA Sciences (I)
Research Funding: Bristol Myers Squibb/Celgene (Inst), AstraZeneca (Inst), Amgen (Inst), AbbVie (Inst)
No other potential conflicts of interest were reported.
SUPPORT
Supported by The Leukemia & Lymphoma Society.
AUTHOR CONTRIBUTIONS
Conception and design: Jesper Akesson, Elisa S. Weiss, Maria Sae-Hau, Gabriela Gracia, Marialanna Lee, Lucy Culp, Brian Connell, Rena M. Conti
Provision of study materials or patients: Elisa S. Weiss, Maria Sae-Hau
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
COVID-19 Vaccine–Related Beliefs and Behaviors Among Patients With and Survivors of Hematologic Malignancies
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Elisa S. Weiss
Research Funding: AbbVie (Inst), AstraZeneca (Inst), Amgen (Inst), Bristol Myers Squibb/Celgene (Inst)
Maria Sae-Hau
Stock and Other Ownership Interests: Moderna Therapeutics (I), Acceleron Pharma (I), argenx (I), Beam Therapeutics (I), BridgeBio Pharma (I), Schrodinger (I), Applied DNA Sciences (I)
Research Funding: Bristol Myers Squibb/Celgene (Inst), AstraZeneca (Inst), Amgen (Inst), AbbVie (Inst)
No other potential conflicts of interest were reported.
REFERENCES
- 1.Howlader N, Noone AM, Krapcho M, et al. (eds): SEER Cancer Statistics Review, 1975-2017. Bethesda, MD, National Cancer Institute, 2020. https://seer.cancer.gov/archive/csr/1975_2017/ [Google Scholar]
- 2.Hippisley-Cox J, Coupland CA, Mehta N, et al. : Risk prediction of covid-19 related death and hospital admission in adults after covid-19 vaccination: National prospective cohort study. BMJ 374:n2244, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bakouny Z, Hawley JE, Choueiri TK, et al. : COVID-19 and cancer: Current challenges and perspectives. Cancer Cell 38:629-646, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banks MA: COVID-19 More Deadly With Blood Than Solid Cancer: Study. The Scientist. 2021. https://www.the-scientist.com/news-opinion/covid-19-more-deadly-with-blood-than-solid-cancer-study-68459 [Google Scholar]
- 5.Vijenthira A, Gong IY, Fox TA, et al. : Outcomes of patients with hematologic malignancies and COVID-19: A systematic review and meta-analysis of 3377 patients. Blood 136:2881-2892, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmidt AL, Labaki C, Hsu CY, et al. : COVID-19 vaccination and breakthrough infections in patients with cancer. Ann Oncol 33:340-346, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boekel L, Wolbink GJ: Rituximab during the COVID-19 pandemic: Time to discuss treatment options with patients. Lancet Rheumatol 4:e154-e155, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Comprehensive Cancer Network : Preliminary Recommendations of the NCCN COVID-19 Vaccination Advisory Committee*, 2021. https://www.nccn.org/covid-19/pdf/COVID19_Vaccination_Guidance_V1.0.pdf [Google Scholar]
- 9.COVID-19 Vaccine & Patients with Cancer. American Society of Clinical Oncology. 2021. https://www.asco.org/ascocoronavirus-resources/covid-19-patient-care-information/covid-19-vaccine-patients-cancer [Google Scholar]
- 10.Greenberger L, Saltzman LA, Senefeld JW, et al. : Anti-spike antibody response to SARS-CoV-2 booster vaccination in patients with B cell-derived hematologic malignancies. Cancer Cell 39:1296-1299, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COVID-19 Vaccines and People with Cancer. National Cancer Institute. https://www.cancer.gov/about-cancer/coronavirus/covid-19-vaccines-people-with-cancer [Google Scholar]
- 12.Evidence used to update the list of underlying medical conditions that increase a person’s risk of severe illness from COVID-19. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html [PubMed] [Google Scholar]
- 13.Corti C, Crimini E, Tarantino P, et al. : SARS-CoV-2 vaccines for cancer patients: A call to action. Eur J Cancer 148:316-327, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mejri N, Berrazega Y, Ouertani E, et al. : Understanding COVID-19 vaccine hesitancy and resistance: Another challenge in cancer patients. Support Care Cancer 30:289-293, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chun JY, Kim SI, Park EY, et al. : Cancer patients’ willingness to take COVID-19 vaccination: A nationwide multicenter survey in korea. Cancers 13:3883, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brodziak A, Sigorski D, Osmola M, et al. : Attitudes of patients with cancer towards vaccinations–results of online survey with special focus on the vaccination against COVID-19. Vaccines (Basel) 9:411, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hochbaum GM: Public Participation in a Medical Screening Program: A Socio-Psychological Study. US Department of Health, Education, and Welfare, Public Health Service, Bureau of State Services, Division of Special Health Services, Tuberculosis Program, Washington DC, 1958 [Google Scholar]
- 18.Burke PF, Masters D, Massey G: Enablers and barriers to COVID-19 vaccine uptake: An international study of perceptions and intentions. Vaccine 39:5116-5128, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Updated Data on Blood Cancers. Leukemia & Lymphoma Society. 2020. https://www.lls.org/sites/default/files/2021-08/PS80%20FactsBook_2020_2021_FINAL.pdf [Google Scholar]
- 20.Hamel L, Kirzinger A, Munana C, Brodie M: KFF COVID-19 Vaccine Monitor: December 2020. Kaiser Family Foundation, 2020. https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december2020/ [Google Scholar]
- 21.KFF Covid-19 Vaccine Monitor. KFF. https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard/?utm_source=web&utm_medium=trending&utm_campaign=COVID-19-vaccine-monitor#uptake [Google Scholar]
- 22.KFF COVID-19 Vaccine Monitor: In Their Own Words, Six Months Later. KFF. 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-in-their-own-words-six-months-later/ [Google Scholar]
- 23.Palm R, Bolsen T, Kingsland J: The effect of frames on COVID-19 vaccine hesitancy. Front Polit Sci 3:661257, 2021 [Google Scholar]
- 24.Thunstrom L, Ashworth M, Finnoff D, et al. : Hesitancy Towards a COVID-19 Vaccine and Prospects for Herd Immunity. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3593098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Isler O, Isler B, Kopsacheilis O, Ferguson E: Limits of the social-benefit motive among high-risk patients: A field experiment on influenza vaccination behaviour. BMC Public Health 20:240, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Godinho C, Yardley L, Marcu A, et al. : Increasing the Intent to Receive a Pandemic Influenza Vaccination: Testing the Impact of Theory-Based Messages. https://www.semanticscholar.org/paper/Increasing-the-intent-to-receive-a-pandemic-Testing-Godinho-Yardley/f6ea8265a286d7eec77c73a03f016b9d9c999dae [DOI] [PubMed] [Google Scholar]
- 27.Guidry J: Framing and visual type: Effect on future Zika vaccine uptake intent. J Pub Health Res; 30:1162, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Sousa ÁFL, Teixeira JRB, Lua I, et al. : Determinants of COVID-19 vaccine hesitancy in Portuguese-speaking countries: A structural equations modeling approach. Vaccines 9:1167, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.KFF : KFF COVID-19 Vaccine Monitor: January 2021. https://www.kff.org/report-section/kff-covid-19-vaccine-monitor-january-2021-vaccine-hesitancy/ [Google Scholar]
- 30.Medical and Addictions Work Group of the Interdivisional Task Force on the Pandemic American Psychological Association : Rethinking Vaccine Hesitancy in a Pandemic, a Discussion 10, 2022 [Google Scholar]
- 31.Heyne S, Esser P, Werner A, et al. : Attitudes toward a COVID-19 vaccine and vaccination status in cancer patients: A cross-sectional survey. J Cancer Res Clin Oncol 148:1363-1374, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Latkin CA, Dayton L, Miller JR, et al. : Behavioral and attitudinal correlates of trusted sources of COVID-19 vaccine information in the US. Behav Sci 11:56, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kreps S, Prasad S, Brownstein JS, et al. : Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw Open 3:e2025594, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gorton L, Gorton MJ, Buol MR: Mayors on equity and COVID vaccines: Messaging, partnerships, and confidence. https://www.nlc.org/article/2021/02/19/mayors-on-equity-and-covid-vaccines-messaging-partnership-and-confidence/