Abstract
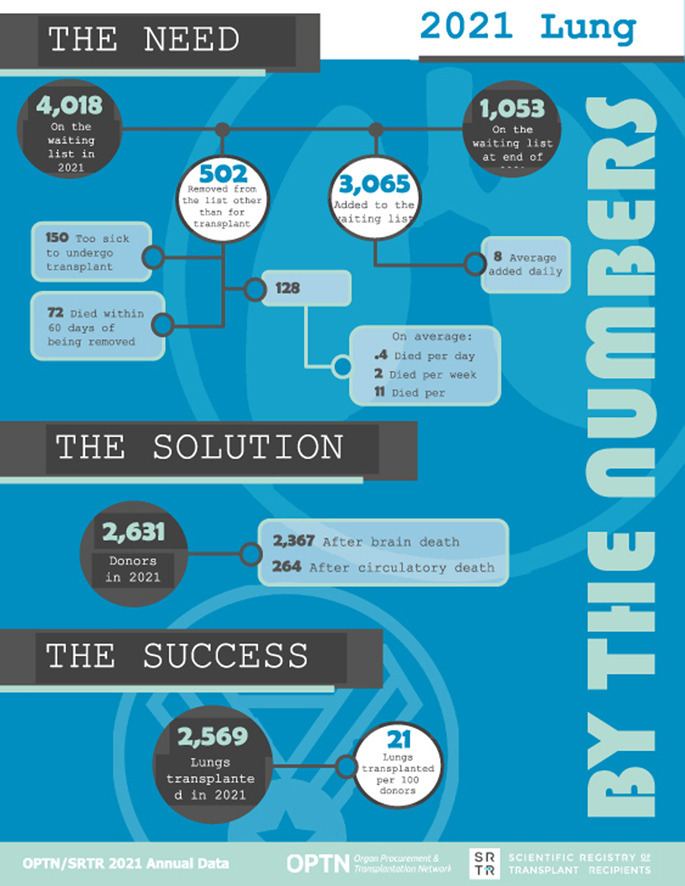
The number of lung transplants has continued to decline since 2020, a period that coincides with the onset of the COVID-19 pandemic. Lung allocation policy continues to undergo considerable change in preparation for adoption of the Composite Allocation Score system in 2023, beginning with multiple adaptations to the calculation of the Lung Allocation Score that occurred in 2021. The number of candidates added to the waiting list increased after a decline in 2020, while waitlist mortality has increased slightly with a decreased number of transplants. Time to transplant continues to improve, with 38.0% of candidates waiting fewer than 90 days for a transplant. Posttransplant survival remains stable, with 85.3% of transplant recipients surviving to 1 year; 67%, to 3 years; and 54.3%, to 5 years.
Keywords: End-stage lung disease, Lung Allocation Score, lung transplant, organ allocation, revised Lung Allocation Score, transplant outcomes
Graphical abstract
1. Introduction
The number of lung transplants has been declining since the peak noted in 2019, with 2,569 transplants occurring in 2021. This is a decrease of 28 transplants compared with 2020 and 190 transplants compared with 2019. New candidates added to the waiting list began to increase in 2021, with 415 more candidates added to the waiting list compared with 2020; but this still falls short of the number in 2019. COVID-19, and its complications, has emerged as a major indication for lung transplant, with 261 transplants performed for this indication in 2021. There have been only three cases of donor-derived transmission of COVID-19 to date (November 3, 2022), as a result of rigorous testing protocols used by the transplant community.
Major lung allocation policy changes occurred in 2021 in preparation for the implementation of the Composite Allocation Score (CAS) system, which is planned to go into effect in 2023. Changes to the Lung Allocation Score (LAS) were implemented on September 30, 2021, to reflect a more recent candidate and recipient cohort and improve the prediction of calculated waitlist and posttransplant survival models that are currently used in the LAS and will be used in the forthcoming CAS. This resulted in the removal of several previously significant variables from the survival models and parameter updates for multiple additional variables. Multiple variables were removed from the waitlist survival models, including diagnosis (obliterative bronchiolitis, lymphangioleiomyomatosis, and Eisenmenger syndrome), bilirubin increase of 50% or greater, diabetes, forced vital capacity, cardiac index, and central venous pressure. Variables removed from the posttransplant survival models include diagnosis (lymphangioleiomyomatosis, Eisenmenger syndrome, pulmonary fibrosis, and other), functional status, and serum creatinine increase of 150% or greater. Parameterizations on the remaining variables were updated to reflect the new cohort. The effect of these changes on the group LASs for the population has not yet been well studied, but readers should be cautioned that these changes make direct comparisons between LAS values pre- and post-policy difficult. Notably, the updated LAS still uses a 2:1 ratio of 1-year waitlist and 1-year posttransplant survival. The CAS will use a 1:1 ratio of 1-year waitlist and 5-year posttransplant survival.
The US lung allocation system will be the first to adopt a CAS system, with the goal of improving equity in organ allocation. The new CAS system will use the continuous distribution framework, whereby strict geographic cut points in concentric circles from the donor are no longer used to guide allocation. Work to develop the CAS system began with the Organ Procurement and Transplantation Network (OPTN) Lung Transplantation Committee in 2019, was open to public comment in 2019-2021, and was approved by the OPTN Board of Directors at the end of 2021. The CAS system includes five attributes: medical urgency, posttransplant survival, candidate biology, patient access, and placement efficiency. In this system, medical urgency (1 year) and posttransplant survival (5 years) will receive equal weighting. In the LAS system, the allocation process differs for those aged 12 years or younger and is governed by illness-based priority status, age, geography, blood-type compatibility, and waiting time. With adoption of the CAS system, persons aged 12 years or younger will receive a 20% weighting for pediatric status within the system, eliminating the need for separate adult and pediatric allocation systems.
With the LAS, transplant benefit is estimated by calculating a measure of waitlist and posttransplant mortality. Waitlist mortality receives twice the weight of posttransplant survival. Pulmonary diseases are characterized into four main diagnosis groups: group A, obstructive lung disease; group B, pulmonary vascular disease; group C, cystic fibrosis and immunodeficiency disorders; and group D, restrictive lung diseases. These groupings were derived to aggregate individuals based on disease pathophysiology and survival probability. Notable changes to the allocation system that might affect longitudinal results reported in this chapter include (1) the 2015 update including a more contemporary cohort and new variables for candidates in diagnosis group B; (2) the 2017 update replacing the donation service area with a 250–nautical-mile radius from the donor hospital as the first unit of allocation; and (3) the 2021 update including a more contemporary cohort, removed variables, and updated parameterizations.
In this report, results for the Adult Lung Transplantation section include all lung transplant candidates and recipients 18 years or older at the time of listing; those younger than 18 years are reported in the Pediatric Lung Transplantation section. Reports prior to 2020 separate pediatric and adult candidates at an age of 12 years because the LAS is calculated for candidates aged 12 years and older. This change in reporting was made to align with international reporting. This chapter includes information about both heart-lung and lung candidates and recipients.
2. Adult Lung Transplantation In The United States
2.1. Waiting List
2.1.1. Characteristics of adult candidates listed for lung transplant
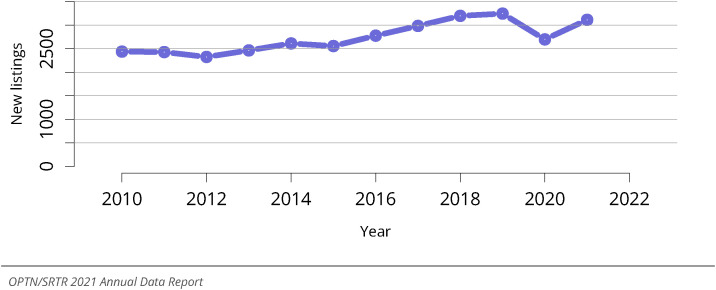
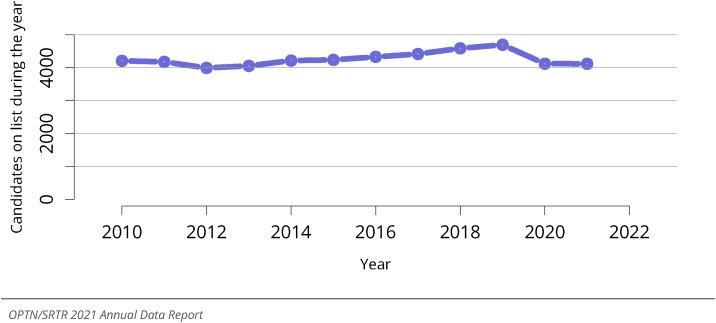
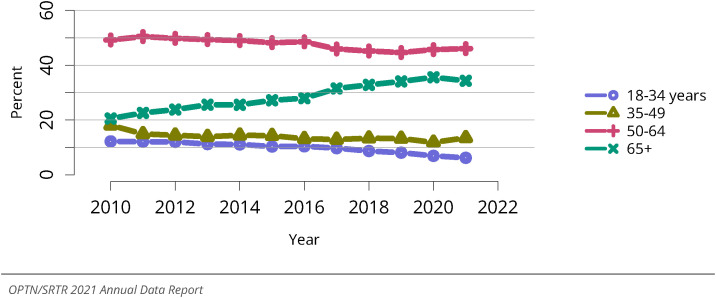
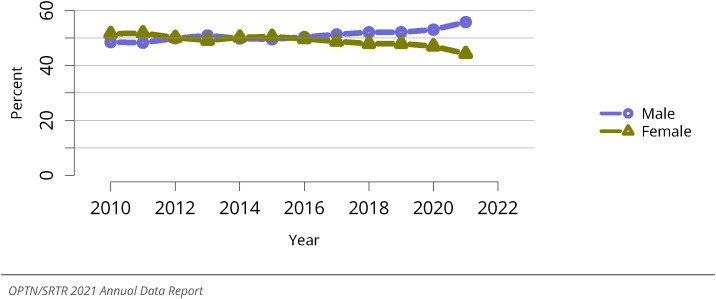
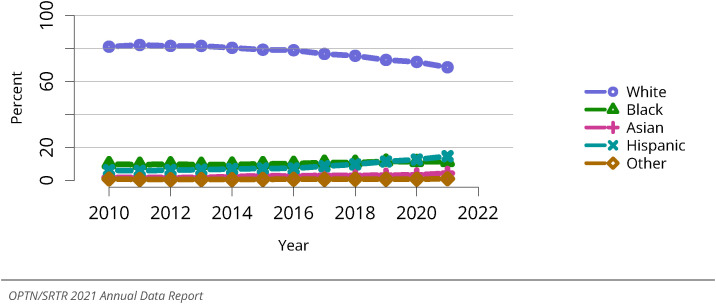
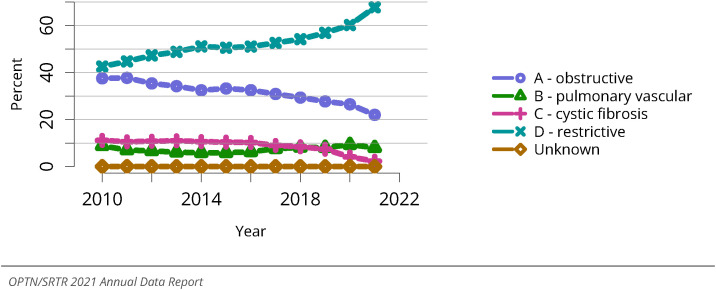
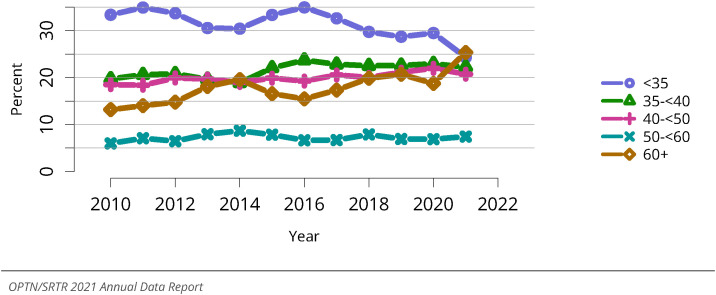
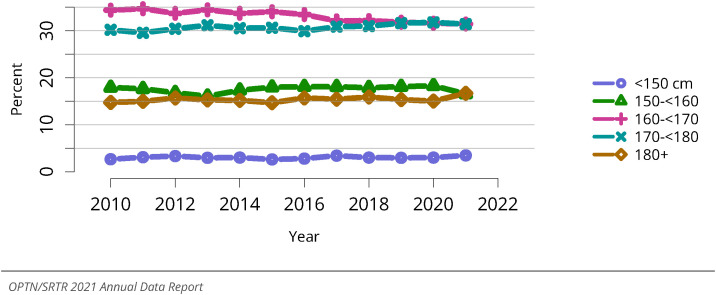
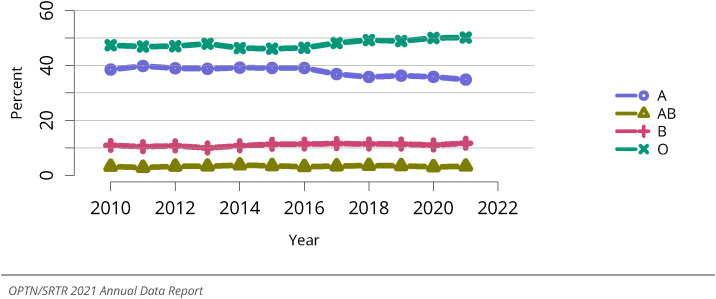
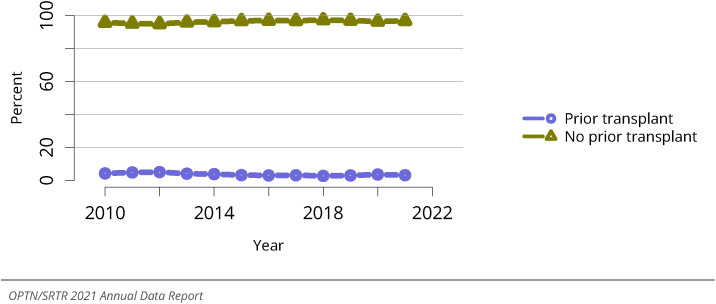
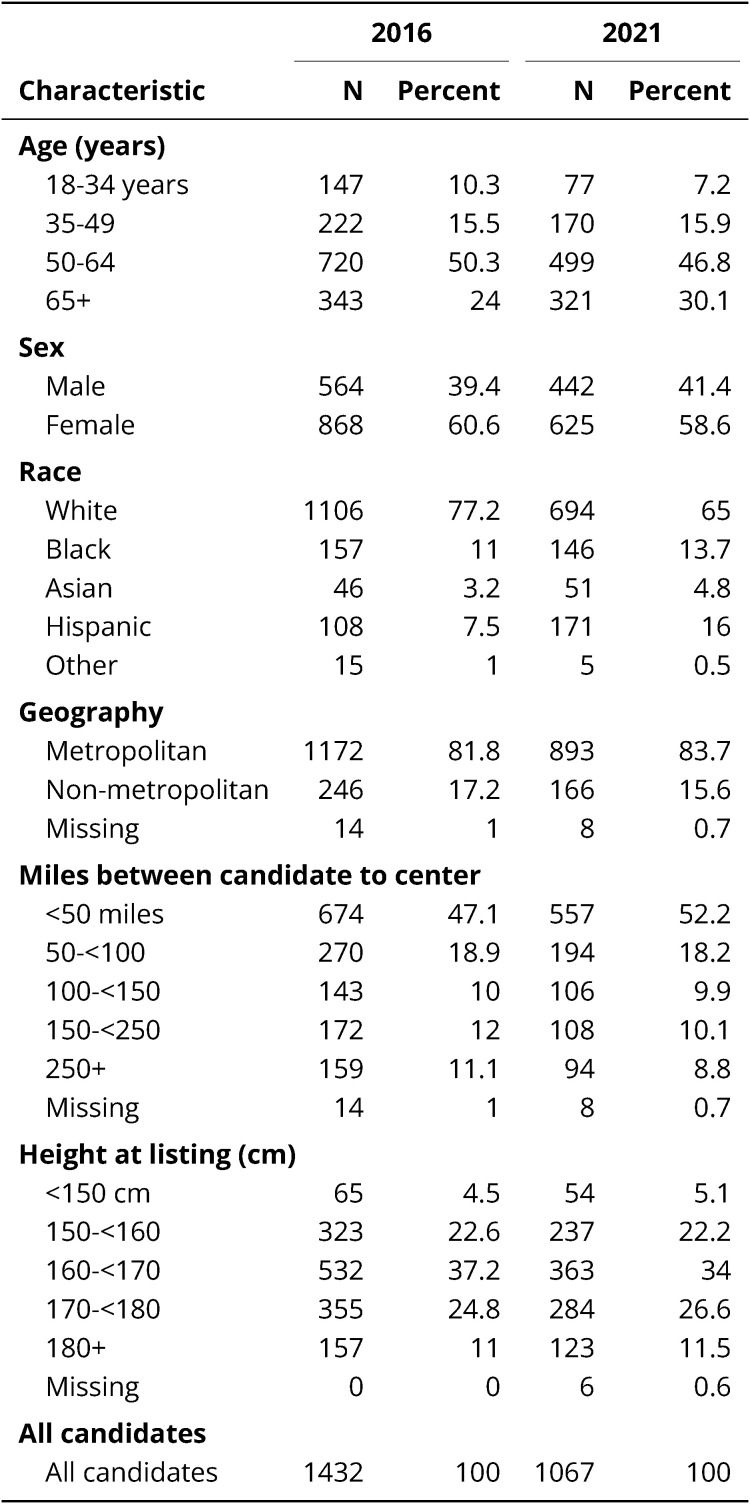
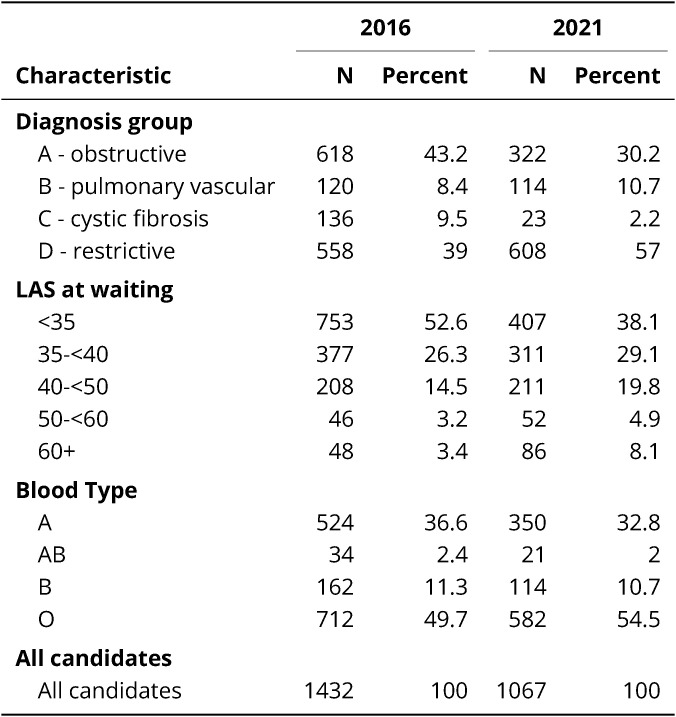
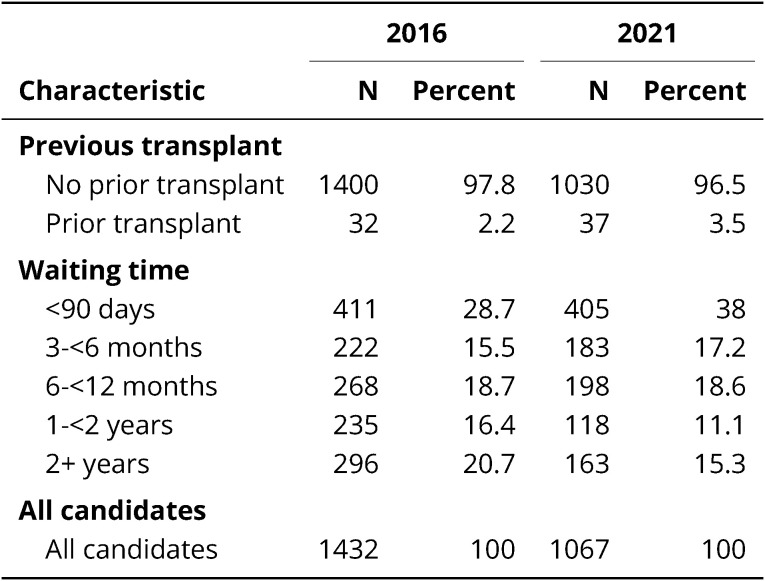
In 2021, there were 3,111 candidates added to the lung transplant waiting list. This represents a 27.7% increase compared with the past decade beginning in 2010 (Figure LU 1). The prevalent number of candidates on the waiting list remains stable at 4,117 (Figure LU 2). In 2021, 6.2% of candidates were aged 18-34 years, 13.5% were 35-49 years, 46.0% were 50-64 years, and 34.3% were 65 years or older. The candidates are older now compared with 2010. The proportion of individuals aged 18-34 years decreased by 49.2% and those aged 65 years or older increased by 67.0% compared with 2010 (Figure LU 3). The waiting list comprises a higher proportion of males at 55.7%, a 15% increase since 2010 (Figure LU 4). The proportion of candidates identifying as White race has declined to 68.6%, a 15.4% decline since 2010, whereas the proportion of candidates identifying as Black race has increased to 11.3% and Hispanic ethnicity to 14.7%, increases of 13.6% and 137.4%, respectively, over the same period (Figure LU 5). The proportion of individuals in group D continues to increase (67.7% of the waiting list), whereas those in group A have decreased to 22% and those in group C have decreased to 2.3%; the proportion of group B candidates on the list has remained stable (Figure LU 6). Distributions of LAS values changed slightly during the past 2 years, with a notable increase in individuals with an LAS of 60 or greater, who now make up 25.3% of the waitlist population. The proportion of candidates assigned an LAS less than 35 is converging to similar proportions for those assigned LAS values of 35-<40 and 40-<50 (Figure LU 8). Trends in height, blood type, and prior transplant status have remained stable over time (Figure LU 9, Figure LU 10, Figure LU 11). Geographic proximity to transplant centers is varied, with 52.2% of candidates living within 50 miles of the nearest transplant center and 8.8% of candidates living more than 250 miles from the nearest transplant center. The vast majority of candidates (83.7%) live in a designated metropolitan region (Table LU 1). Lung transplant candidates, as a whole, have not received a prior transplant, with only 3.5% listed for a retransplant (Table LU 3).
Figure LU 1.
New adult candidates added to the lung transplant waiting list. A new adult candidate is one who first joined the list during the given year, without having been listed in a previous year. Previously listed candidates who underwent transplant and subsequently relisted are considered new. Active and inactive patients are included.
Figure LU 2.
All adult candidates on the lung transplant waiting list. Adult candidates on the list at any time during the year. Candidates listed at more than one center are counted once per listing.
Figure LU 3.
Distribution of adults waiting for lung transplant by age. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive candidates are included. Age is determined at the earliest of transplant, death, removal, or December 31 of the year.
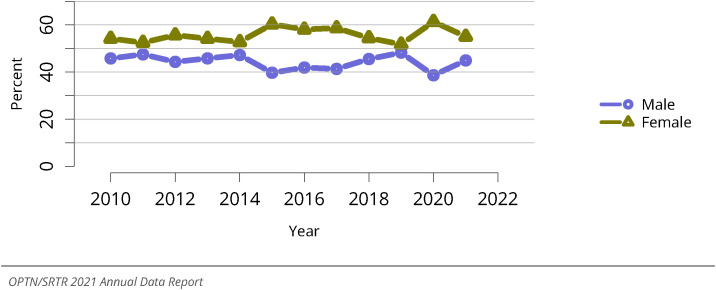
Figure LU 4.
Distribution of adults waiting for lung transplant by sex. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure LU 5.
Distribution of adults waiting for lung transplant by race. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure LU 6.
Distribution of adults waiting for lung transplant by diagnosis group. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included. The Other/unknown group includes a small number of heart-lung candidates prior to 2015 who did not have an A/B/C/D diagnosis group specified.
Figure LU 8.
Distribution of adult candidates waiting for lung transplant by LAS. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. LAS, lung allocation score. LAS is determined at the earliest of transplant, death, removal, or December 31 of the year.
Figure LU 9.
Distribution of adult candidates waiting for lung transplant by height. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure LU 10.
Distribution of adults waiting for lung transplant by blood type. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure LU 11.
Distribution of adults waiting for lung transplant by prior transplant status. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
With more attention being focused on addressing disparities in access to transplant, it is important to note that waitlist trends described herein can only be interpreted among candidates who are already listed. The US lung transplant registry only captures patients after listing and beyond; therefore, this report is unable to provide trends in the broader populations of individuals with end-stage lung disease. Research to evaluate disparities in access to transplant, an essential area of inquiry to promote equity in transplantation, is ongoing.
2.1.2. Outcomes of adult candidates listed for lung transplant
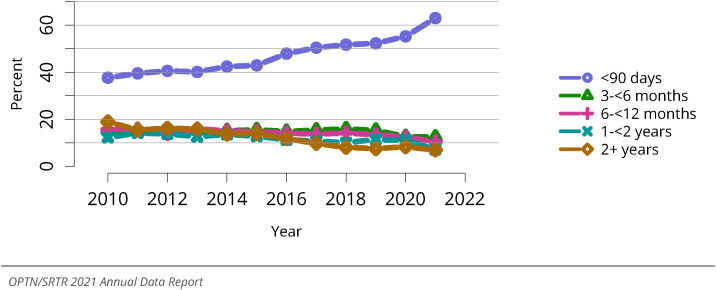
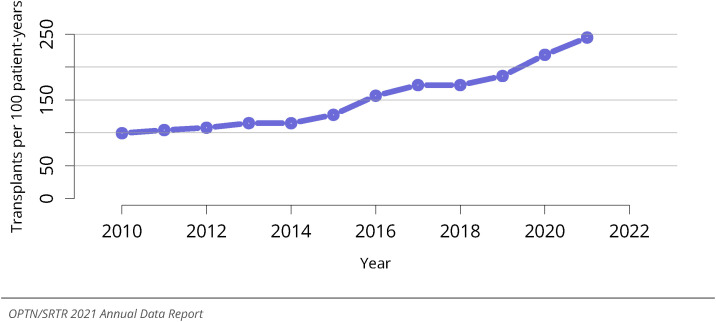
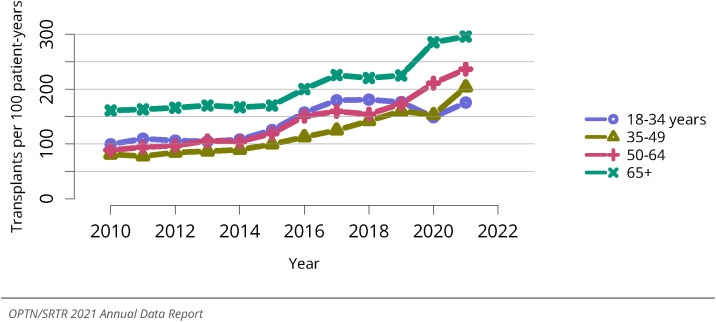
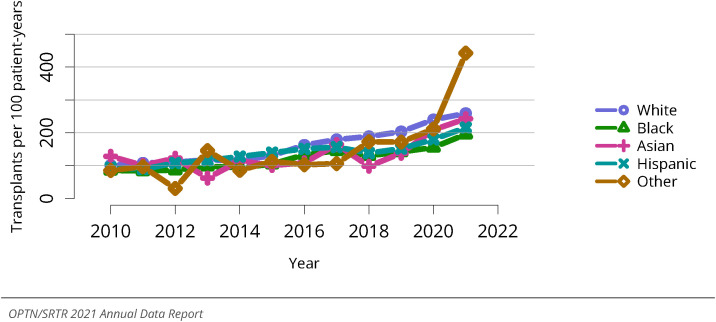
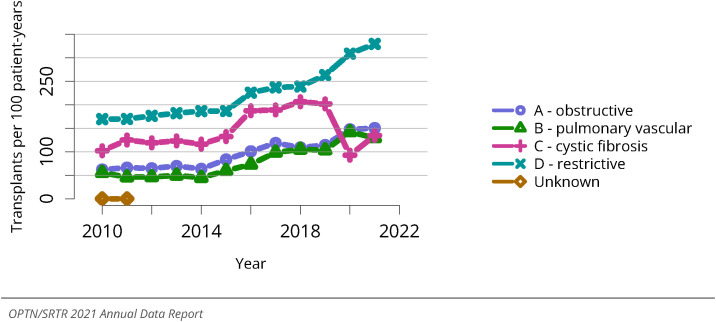
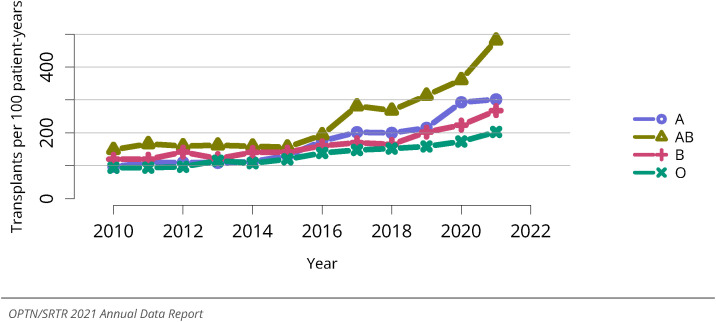
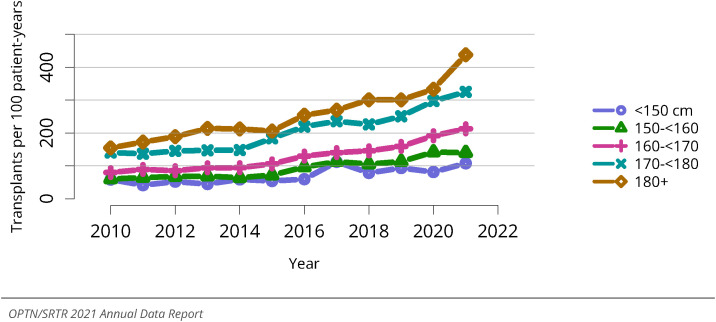
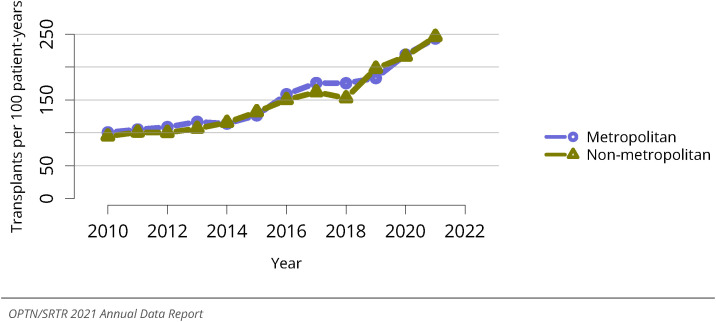
In 2021, 63.0% of candidates waited fewer than 90 days for a lung transplant, with only 24.6% of candidates waiting 6 months or more and 14.2% waiting 1 year or more (Figure LU 7). Transplant rates continue to increase annually, with 2021 having the highest transplant rate of 244.8 transplants per 100 patient-years (Figure LU 12). Deceased donor transplant rates were highest for individuals aged 65 years or older, followed by those aged 50-64, 35-49, and 18-34 years (Figure LU 13). Transplant rates varied slightly by race, with an outlier for “other” race due to small group numbers (Figure LU 14). Transplant rates were highest for individuals in group D, with clustering of transplant rates for diagnosis groups A, B, and C (129.5-150.3 transplants per 100 patient-years) (Figure LU 15). Transplant rates differed across blood type, most likely resulting from variability in numbers of candidates within each group (Figure LU 16). Transplant rates were highest for the tallest individuals (180 cm or greater), with decreasing transplant rates by height (Figure LU 17). Transplant candidates are accessing transplants faster, with 64% of individuals undergoing transplant within 3 months, a 56% increase from 2010 (Figure LU 19, Figure LU 20).
Figure LU 7.
Distribution of adults waiting for lung transplant by waiting time. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Time on the waiting list is determined at the earliest of transplant, death, removal, or December 31 of the year. Active and inactive candidates are included.
Figure LU 12.
Overall deceased donor lung transplant rates among adult waitlist candidates. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure LU 13.
Deceased donor lung transplant rates among adult waitlist candidates by age. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately. Age is determined at the later of listing date or January 1 of the given year.
Figure LU 14.
Deceased donor lung transplant rates among adult waitlist candidates by race. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure LU 15.
Deceased donor lung transplant rates among adult waitlist candidates by diagnosis group. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately. The Other/unknown group includes a small number of heart-lung candidates prior to 2015 who did not have an A/B/C/D diagnosis group specified.
Figure LU 16.
Deceased donor lung transplant rates among adult waitlist candidates by blood type. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure LU 17.
Deceased donor lung transplant rates among adult waitlist candidates by height. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure LU 19.
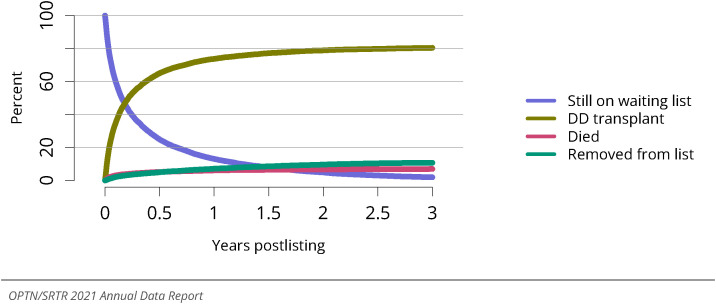
Three-year outcomes for adults waiting for lung transplant, new listings in 2016-2018. Candidates listed at more than one center are counted once per listing. Removed from list includes all reasons except transplant and death. DD, deceased donor.
Figure LU 20.
Percentage of adults who underwent deceased donor lung transplant within a given period of listing. Candidates listed at more than one center are counted once per listing.
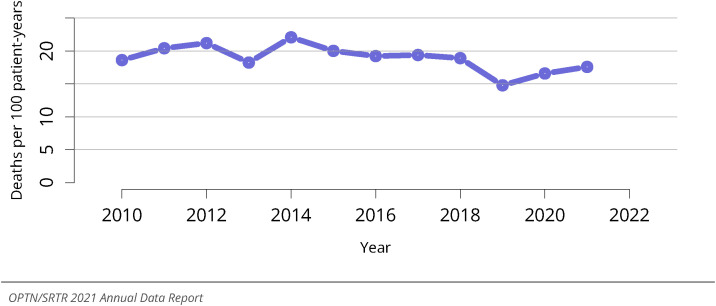
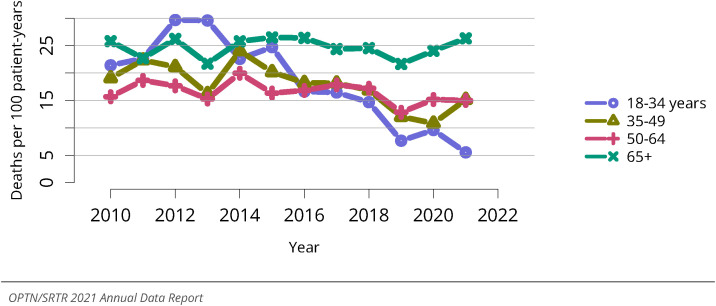
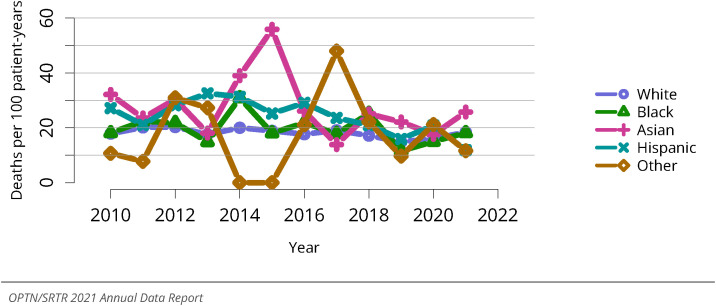
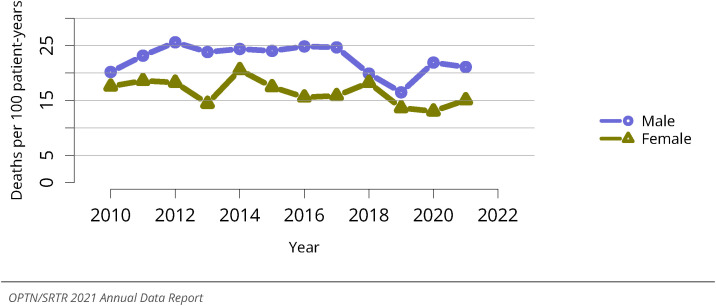
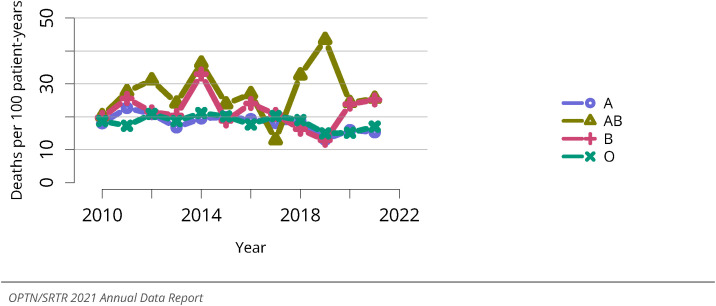
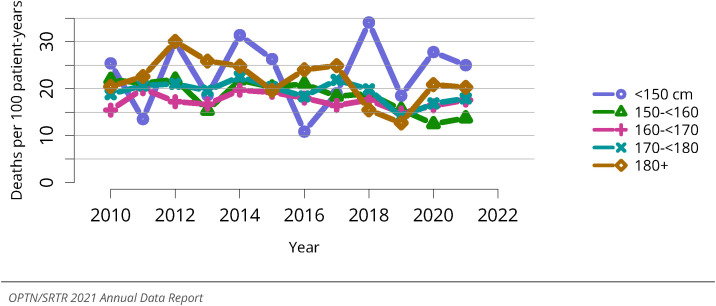
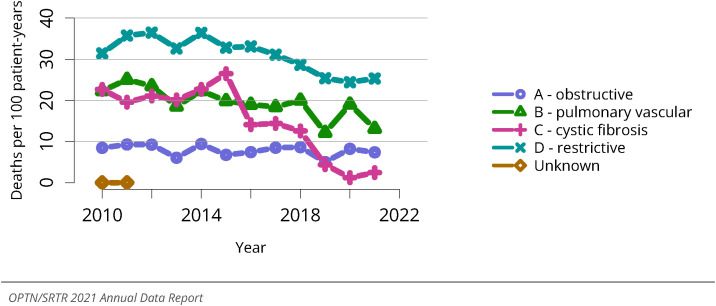
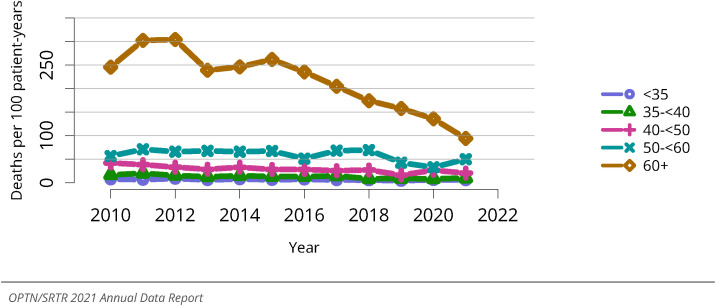
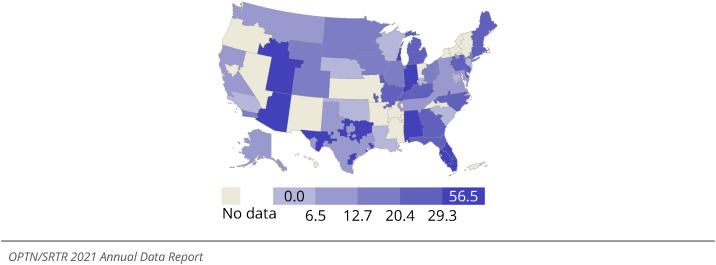
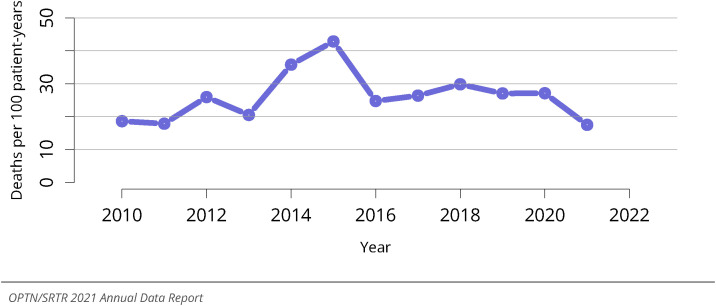
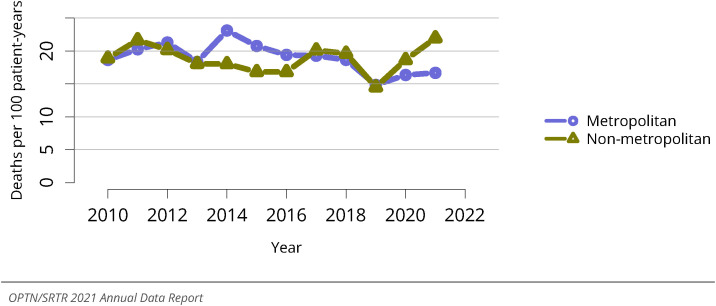
The waitlist mortality rate is 17.6 deaths per 100 patient-years, ranging from 14.8 to 21.2 since 2010 (Figure LU 21). Waitlist mortality has decreased markedly for individuals aged 18-34 years, a finding that may be subject to variability given small group numbers. Even with comparatively higher transplant rates, candidates aged 65 years or older have pretransplant mortality rates nearly two-fold those of persons aged 35-64 years and more than four-fold those of persons aged 18-34 years (Figure LU 22). Waitlist mortality rates vary by sex, with males having greater risk, and by race, blood type, and height, although these findings are influenced by small group numbers (Figure LU 23, Figure LU 24, Figure LU 27, Figure LU 28). Individuals in diagnosis group D have the highest mortality rate, followed by those in groups B, A, and C, respectively (Figure LU 25). Individuals with the highest LAS values have the highest waitlist mortality, and mortality rates increase by approximately two-fold moving from an LAS of 35-<40 to 40-<50, 40-<50 to 50-<60, and 50-<60 to 60 or greater (Figure LU 26). There is variability in waitlist mortality by geographic region (Figure LU 30). For individuals removed from the waiting list for reasons other than transplant or death, 23.3% died within 6 months of waitlist removal, with variability by diagnosis group and age (Figure LU 31, Figure LU 32, Figure LU 33). In 2021, there were 52 candidates who improved and were removed from the waiting list, 154 who became too sick for transplant, 132 who died, and 165 who were removed for other reasons (Table LU 5).
Figure LU 21.
Overall pretransplant mortality rates among adults waitlisted for lung transplant. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure LU 22.
Pretransplant mortality rates among adults waitlisted for lung transplant by age. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately. Age is determined at the later of listing date or January 1 of the given year.
Figure LU 23.
Pretransplant mortality rates among adults waitlisted for lung transplant by race. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure LU 24.
Pretransplant mortality rates among adults waitlisted for lung transplant by sex. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure LU 27.
Pretransplant mortality rates among adults waitlisted for lung transplant by blood type. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure LU 28.
Pretransplant mortality rates among adults waitlisted for lung transplant by height. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure LU 25.
Pretransplant mortality rates among adults waitlisted for lung transplant by diagnosis. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately. The Other/unknown group includes a small number of heart-lung candidates prior to 2015 who did not have an A/B/C/D diagnosis group specified.
Figure LU 26.
Pretransplant mortality rates among adults waitlisted for lung transplant by LAS. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately. LAS is determined at the later of listing date or January 1 of the given year.
Figure LU 30.
Pretransplant mortality rates among adults waitlisted for lung transplant in 2021 by DSA. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure LU 31.
Deaths within six months after removal among adult lung waitlist candidates, overall. Denominator includes only candidates removed from the waiting list for reasons other than transplant or death while on the list.
Figure LU 32.
Deaths within six months after removal among adult lung waitlist candidates, by diagnosis. Denominator includes only candidates removed from the waiting list for reasons other than transplant or death while on the list. The Other/unknown group includes a small number of heart-lung candidates prior to 2015 who did not have an A/B/C/D diagnosis group specified.
Figure LU 33.
Deaths within six months after removal among adult lung waitlist candidates, by age. Denominator includes only candidates removed from the waiting list for reasons other than transplant or death while on the list. Age is determined at removal.
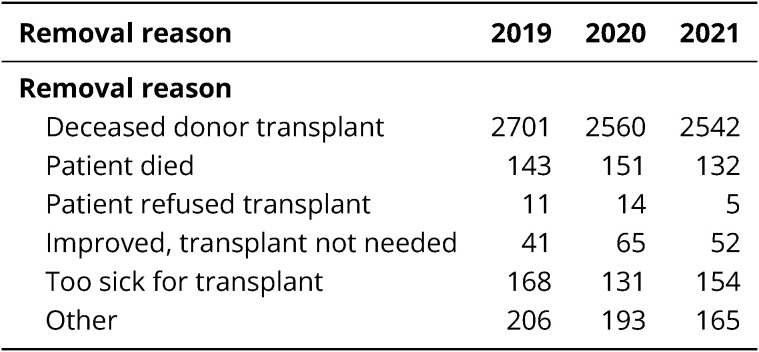
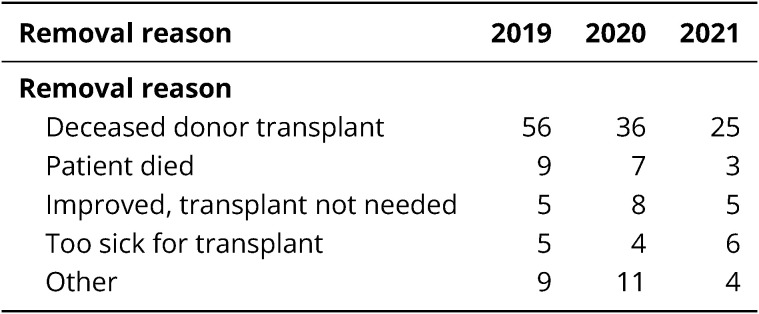
Table LU 5.
Removal reason among adult lung transplant candidates. Removal reason as reported to the OPTN. Candidates with death dates that precede removal dates are assumed to have died waiting.
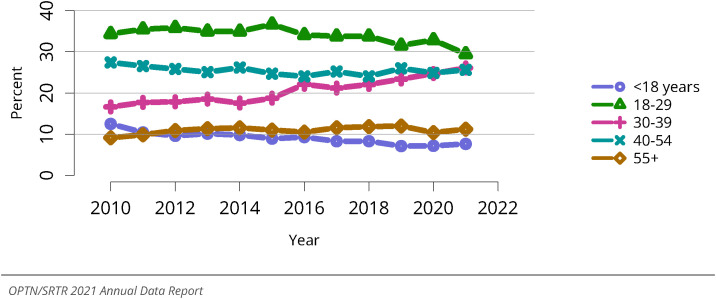
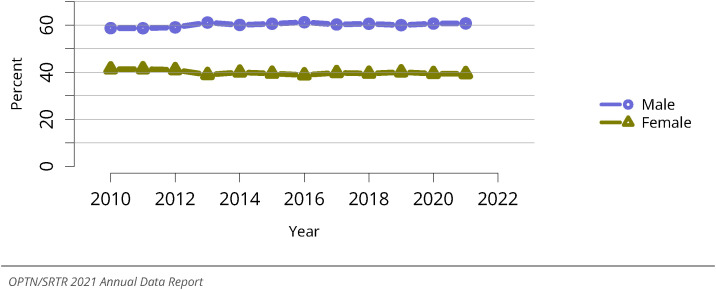
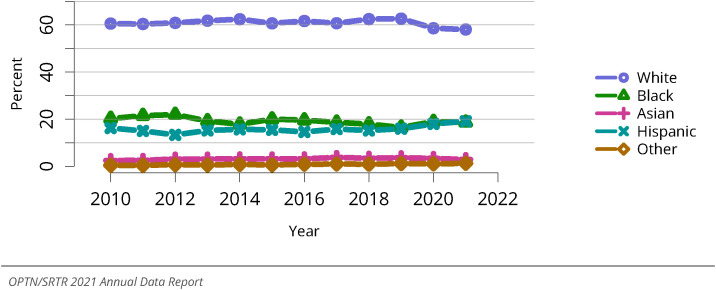
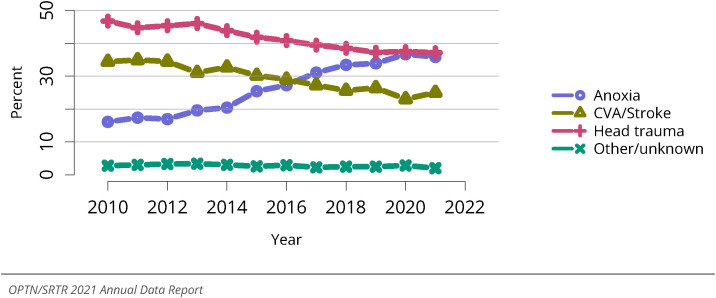
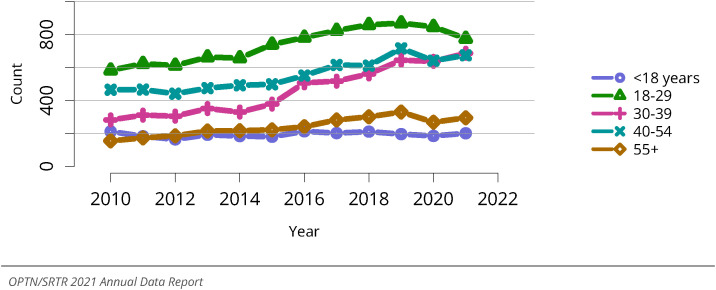
2.2. Donors
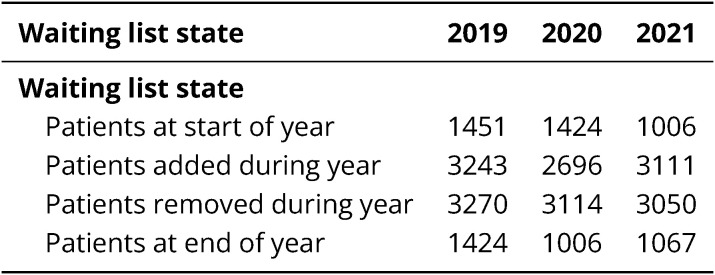
In 2021, there were 2,631 deceased lung donors, with 60.7% of donors male and 7.6% younger than 18 years, 29.5% aged 18-29 years, 26.1% aged 30-39 years, 25.6% aged 40-54 years, and 11.2% aged 55 years or older (Figure LU 34, Figure LU 36, Figure LU 37). Fifty-eight percent of donors were White; 19.1%, Hispanic; 18.7%, Black; and 2.9%, Asian (Figure LU 38). The overall rate of lungs recovered for transplant but not transplanted was 8.1%, with the highest rates for donors aged 55 years or older (Figure LU 39, Figure LU 40). The nonuse rates of recovered organs varied by donor cause of death but notably were similar among standard-risk and increased-risk donors (Figure LU 41, Figure LU 42). Head trauma was the leading cause of death at 37.1%, followed by anoxia (35.8%), cerebrovascular accident/stroke (25%), and other/unknown (2%) (Figure LU 43). Donation after circulatory death is becoming more common, accounting for 7.8% of transplants compared with 4% 5 years earlier (Table LU 8).
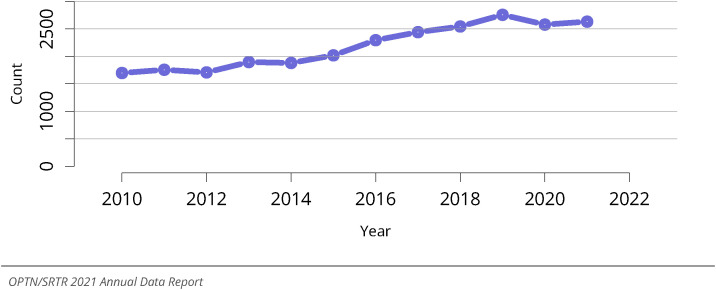
Figure LU 34.
Overall deceased lung donor count. Count of deceased donors with at least one lung recovered. Donors are counted once, regardless of the number of lungs recovered.
Figure LU 36.
Distribution of deceased lung donors by age. Deceased donors whose lungs were recovered for transplant. Donors are counted once, regardless of the number of lungs recovered.
Figure LU 37.
Distribution of deceased lung donors by sex. Deceased donors whose lungs were recovered for transplant. Donors are counted once, regardless of the number of lungs recovered.
Figure LU 38.
Distribution of deceased lung donors by race. Deceased donors whose lungs were recovered for transplant. Donors are counted once, regardless of the number of lungs recovered.
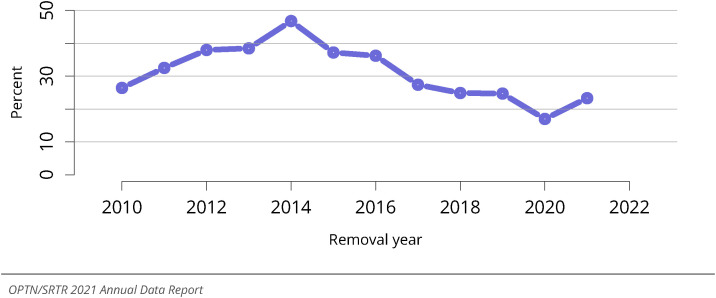
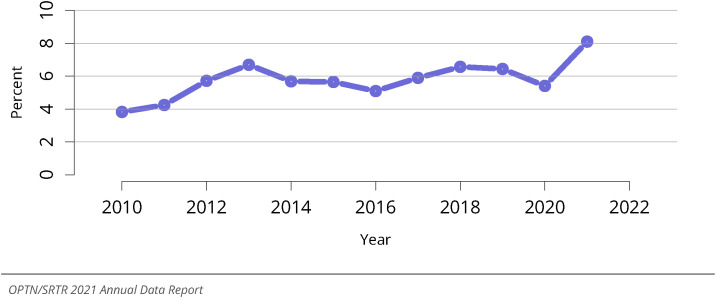
Figure LU 39.
Overall percent of lungs recovered for transplant and not transplanted. Percentages of lungs not transplanted out of all lungs recovered for transplant.
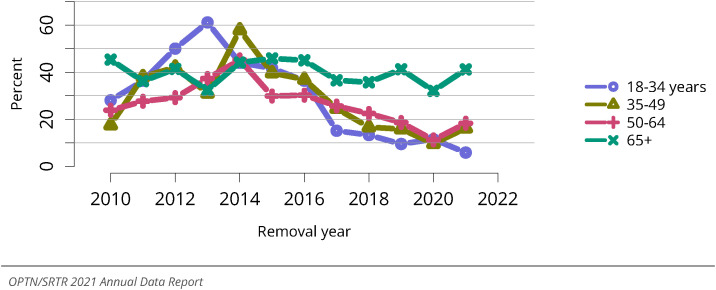
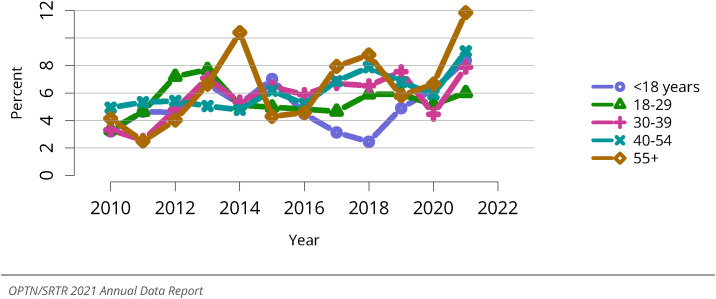
Figure LU 40.
Percent of lungs recovered for transplant and not transplanted by donor age. Percentages of lungs not transplanted out of all lungs recovered for transplant.
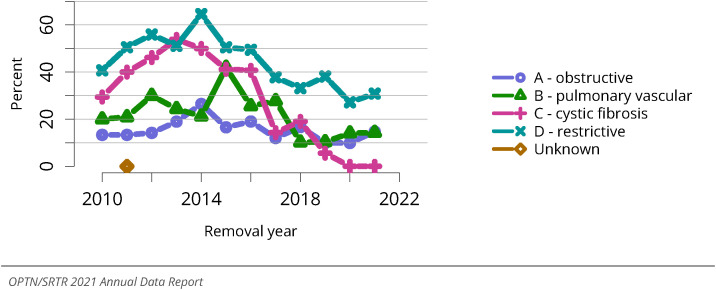
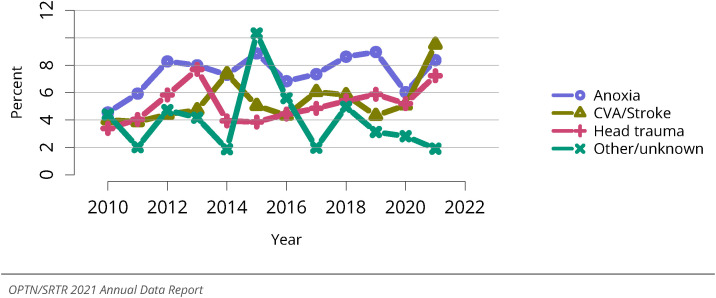
Figure LU 41.
Percent of lungs recovered for transplant and not transplanted by donor cause of death. Percentages of lungs not transplanted out of all lungs recovered for transplant. CVA, cerebrovascular accident.
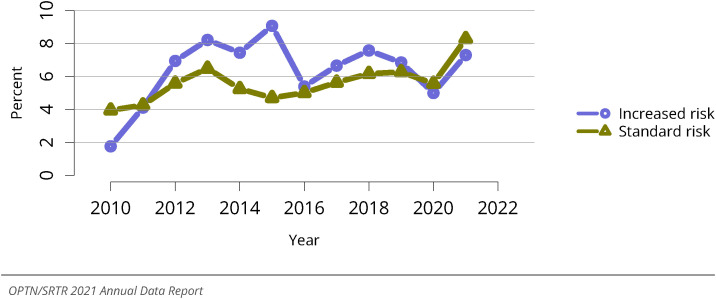
Figure LU 42.
Percent of lungs recovered for transplant and not transplanted, by donor risk of disease transmission. Percentages of lungs not transplanted out of all lungs recovered for transplant. “Increased risk” is defined by criteria from the US Public Health Service Guidelines for increased risk for HIV, hepatitis B, and hepatitis C transmission.
Figure LU 43.
Cause of death among deceased lung donors. Deceased donors with a lung recovered for the purposes of transplant. CVA, cerebrovascular accident.
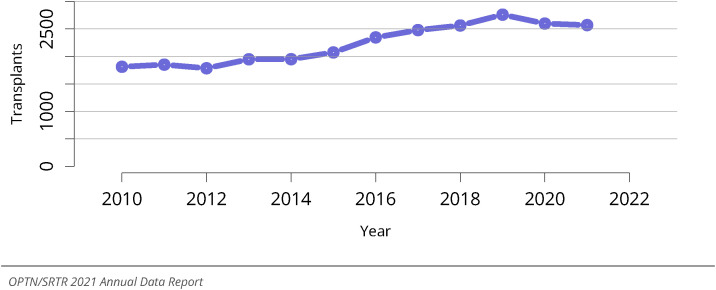
2.3. Transplant
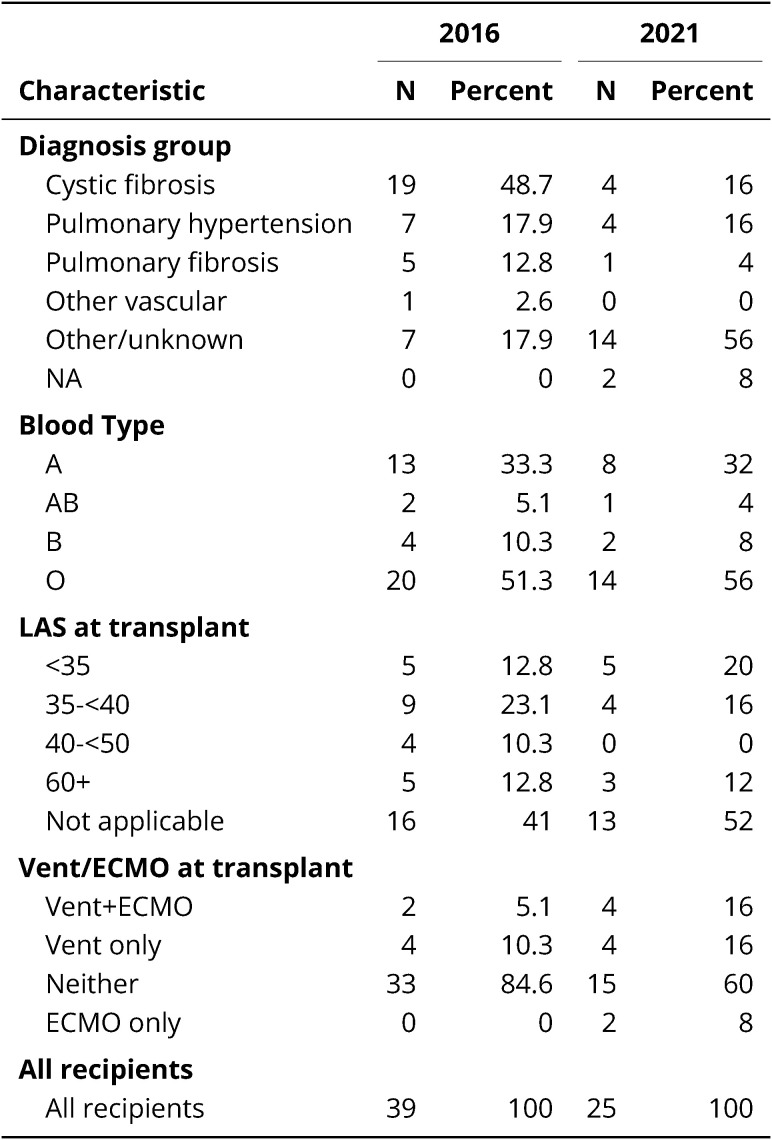
2.3.1. Characteristics of adult lung transplant recipients
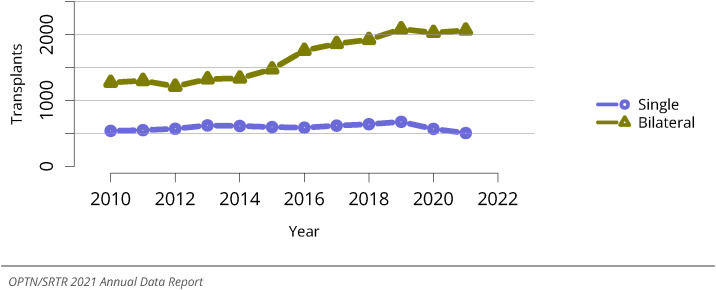
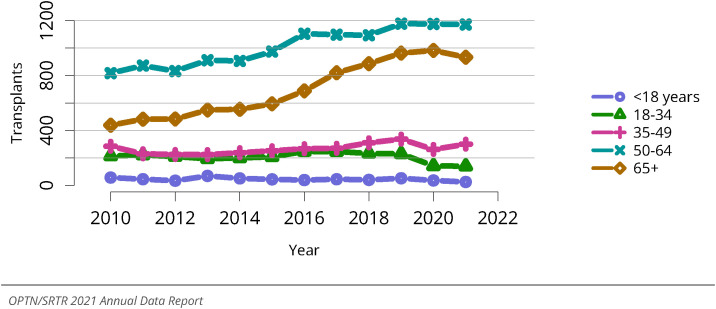
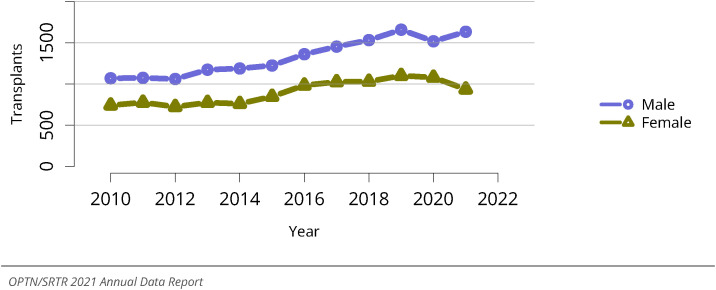
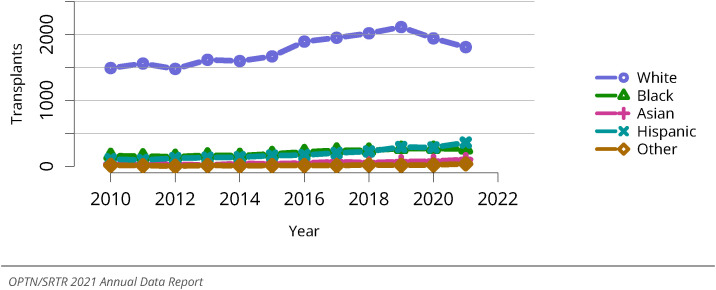
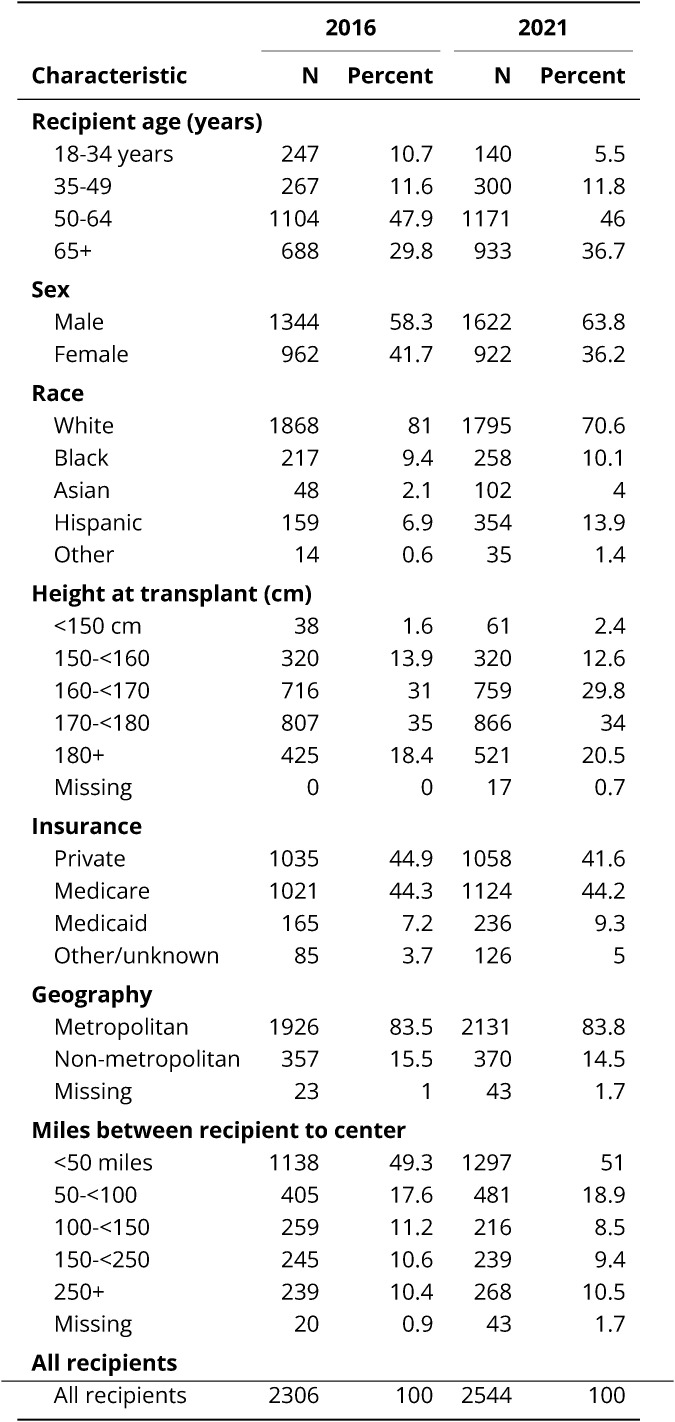
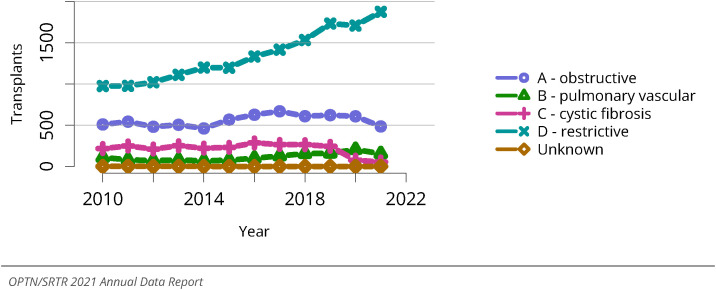
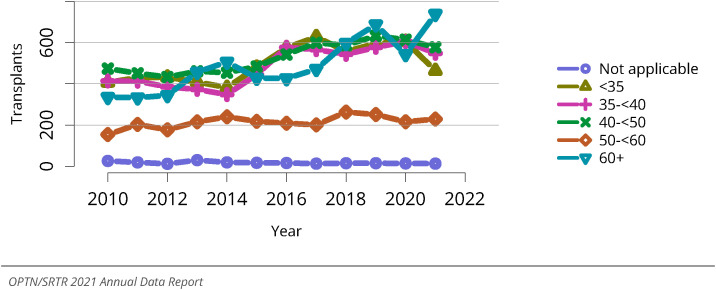
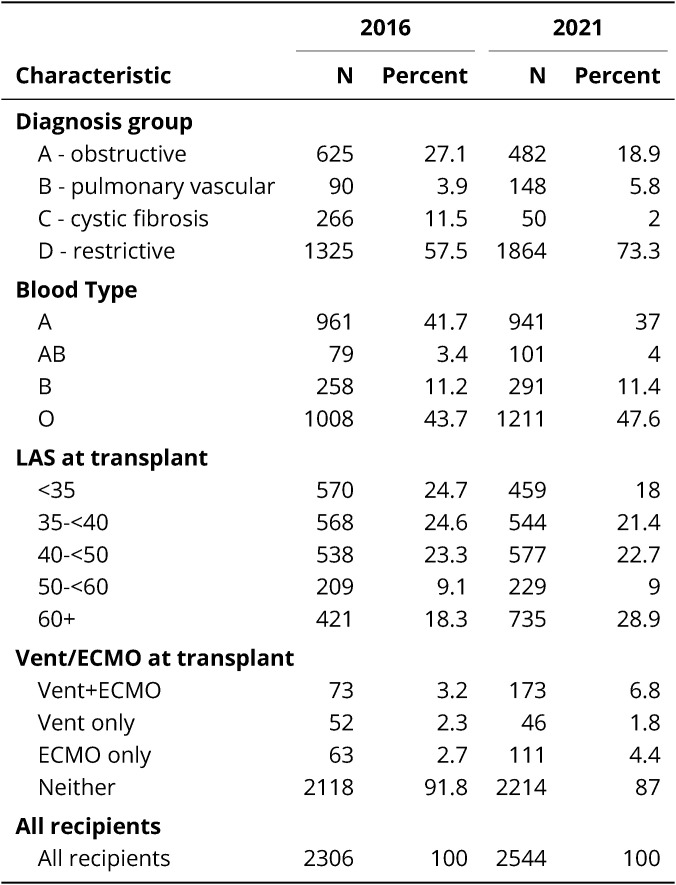
In 2021, there were 2,569 lung transplants, of which 2,063 were bilateral and 506 were single (Figure LU 44, Figure LU 45). The largest number of transplants (1,171) occurred in recipients aged 50-64 years, followed by 933 in those aged 65 years or older, with 440 transplants in recipients aged 18-49 years (Figure LU 46). More transplants occurred in males compared with females, in the context of a higher proportion of male candidates listed for transplant and a higher waitlist mortality compared with females (Figure LU 47). Fewer transplants occurred in White recipients, with small increases in transplants for Black, Hispanic, and Asian recipients (Figure LU 48). White recipients accounted for 70.6% of transplants; Hispanic, 13.9%; Black, 10.1%; and Asian, 4% (Table LU 6). Forty-four percent of recipients had Medicare insurance, followed by 41.6% with private insurance, 9.3% with Medicaid, and 5% unknown (Table LU 6). The number of transplants for recipients in group D continues to increase, with a 92% increase since 2010, while trends for groups A and B are relatively stable; transplants for group C have decreased by 75.1%, with most of that change occurring after approval of highly effective cystic fibrosis transmembrane conductance regulator modulator therapy (Figure LU 49). Trends by LAS have changed over time, with more transplants occurring for individuals with higher LAS values compared with 2010. There was a large increase in transplants for individuals with an LAS value of 60 or greater, a 36% increase compared with 2020 (Figure LU 50).
Figure LU 44.
Overall lung transplants. All lung transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Figure LU 45.
Total lung transplants by procedure type. All lung transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Figure LU 46.
Total lung transplants by age. All lung transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Figure LU 47.
Total lung transplants by sex. All lung transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Figure LU 48.
Total lung transplants by race. All lung transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Table LU 6.
Demographic characteristics of adult lung transplant recipients, 2016 and 2021. Lung transplant recipients, including retransplants. Distance is computed from recipient's home zip code to the transplant center.
Figure LU 49.
Total lung transplants by diagnosis. All lung transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients. The Other/unknown group includes a small number of heart-lung recipients prior to 2015 who did not have an A/B/C/D diagnosis group specified.
Figure LU 50.
Total lung transplants by LAS. All lung transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
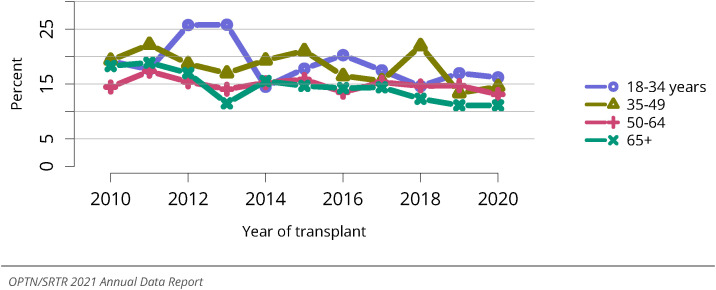
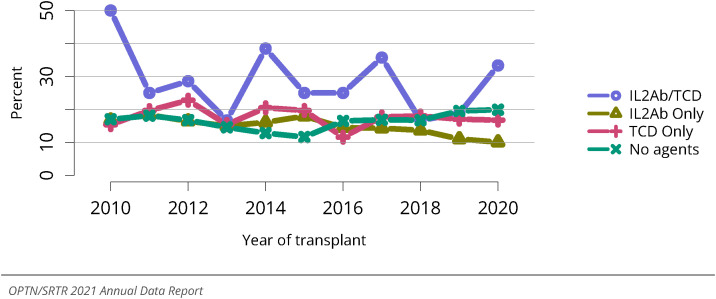
2.3.2. Outcomes of adult lung transplant recipients
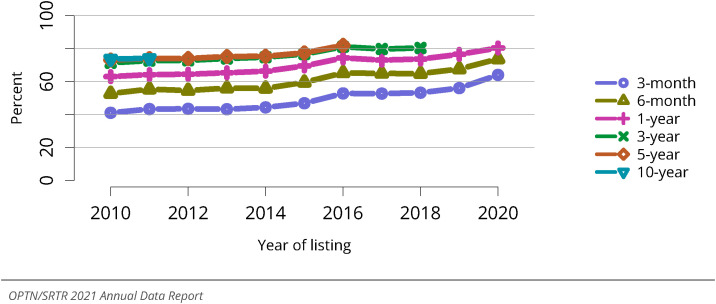
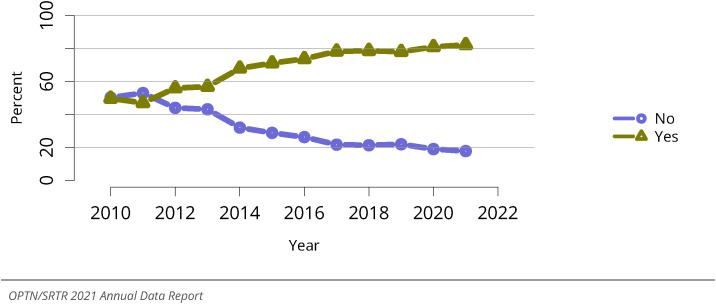
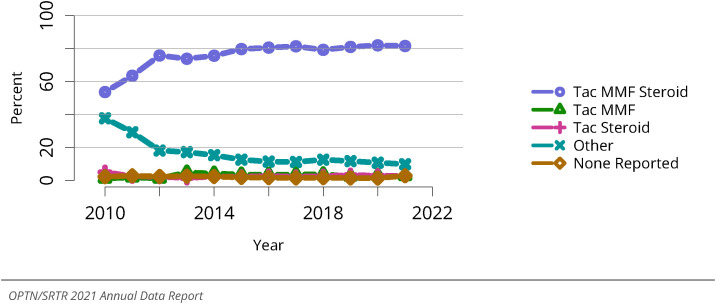
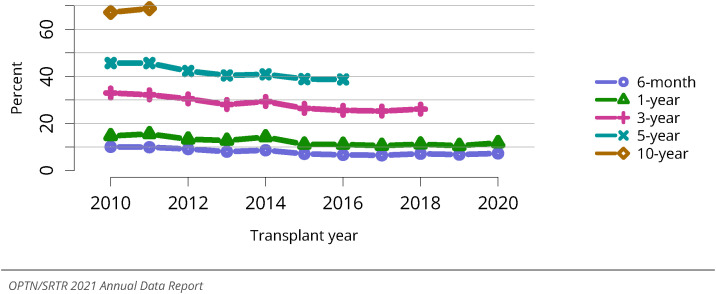
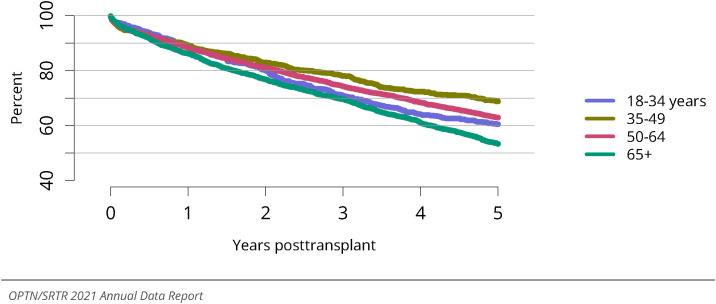
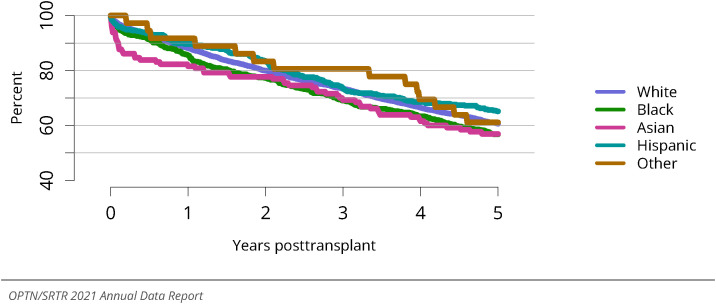
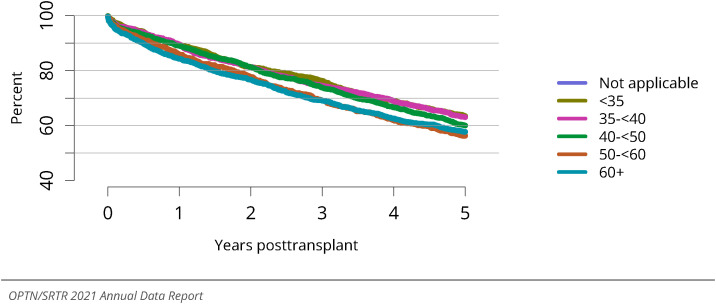
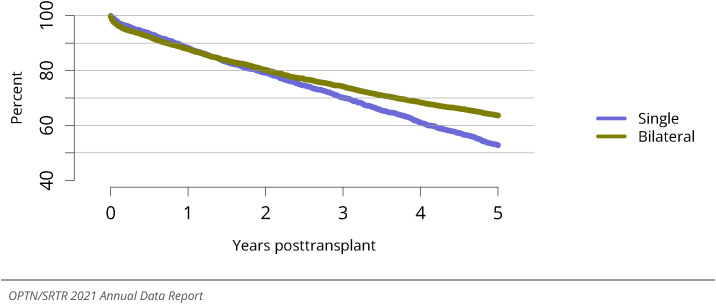
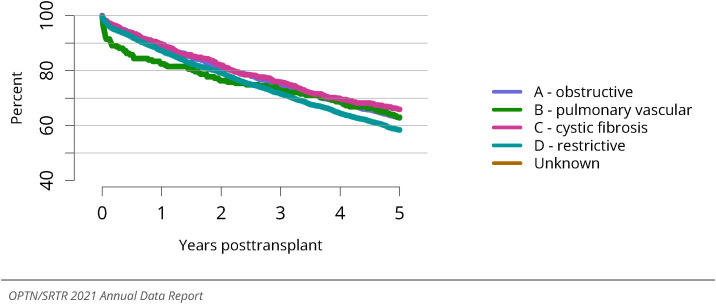
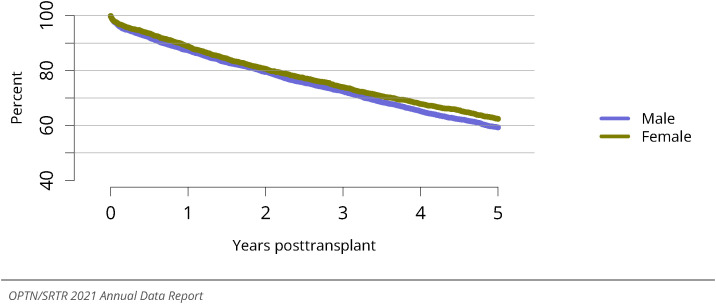
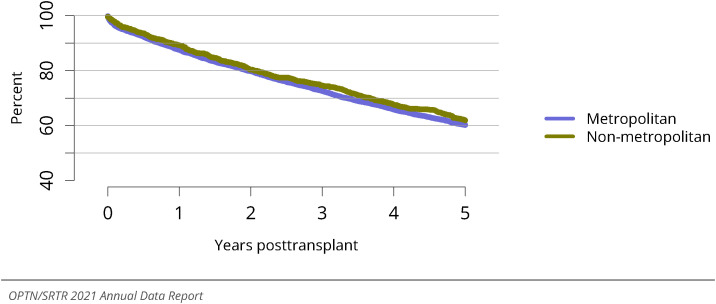
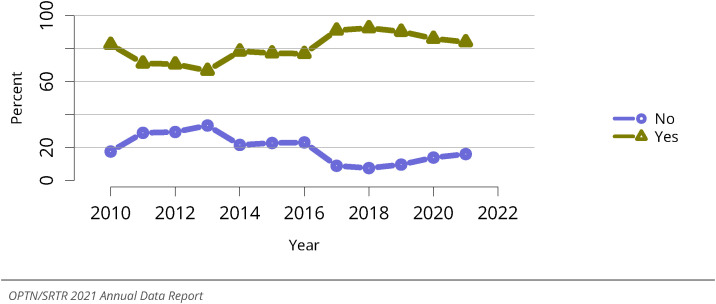
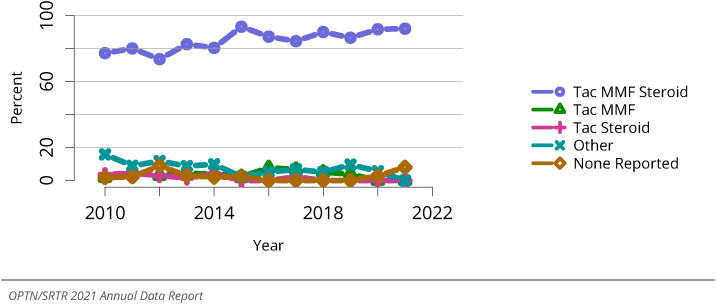
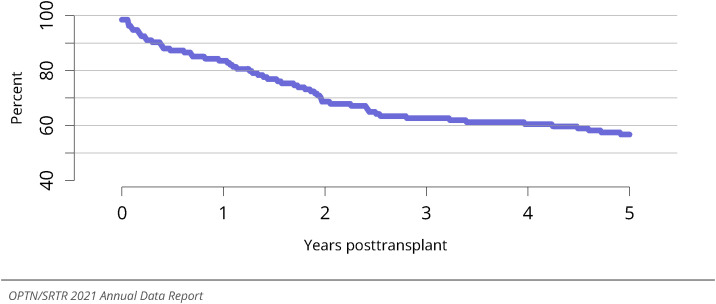
Most adult lung transplant recipients receive induction therapy, with only 17.8% not receiving it (Figure LU 51). The mainstay of posttransplant immunosuppression continues to be tacrolimus, mycophenolate mofetil, and prednisone, and this regimen is used for 81.6% of US adult lung transplant recipients (Figure LU 52). Short- and long-term posttransplant survival has not meaningfully changed since 2010 (Figure LU 53). In 2021, 85.3% of transplant recipients survive to 1 year; 67.0%, to 3 years; 54.3%, to 5 years; and 32.8%, to 10 years (Figure LU 53). Posttransplant survival varies by age, and this trend is accentuated with increased time from transplant. Persons aged 35-49 years have the best survival, followed by those aged 50-64 years, 18-34 years, and 65 years or older (Figure LU 54). Posttransplant survival differs by race, although trends vary with time from transplant (Figure LU 55). Individuals with LAS values of 50 or greater have lower posttransplant survival at all time points (Figure LU 56). Survival is equivalent between single and bilateral transplant recipients until approximately 2 years posttransplant, when survival for bilateral transplants is higher, possibly reflecting patient characteristics that drove the initial decision to perform the less surgically complex procedure of single lung transplant (Figure LU 57). Recipients in group B have the lowest early posttransplant survival but converge with other groups by 3 years posttransplant (Figure LU 58). Recipients in groups A and C have the highest posttransplant survival and group D the lowest after approximately 2.5 years (Figure LU 58). These posttransplant trends are unadjusted analyses, and trends may be confounded by additional recipient factors. Survival is similar between sexes and metropolitan and non-metropolitan inhabitants (Figure LU 59, Figure LU 60).
Figure LU 51.
Induction agent use in adult lung transplant recipients. Immunosuppression at transplant reported to the OPTN.
Figure LU 52.
Immunosuppression regimen use in adult lung transplant recipients. Immunosuppression regimen at transplant reported to the OPTN. Tac, tacrolimus. MMF, all mycophenolate agents.
Figure LU 53.
Patient death among adult lung transplant recipients. All adult recipients of deceased donor lungs, including multiorgan transplants.
Figure LU 54.
Patient survival among adult lung transplant recipients, 2014-2016, by age. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure LU 55.
Patient survival among adult lung transplant recipients, 2014-2016, by race. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure LU 56.
Patient survival among adult lung transplant recipients, 2014-2016, by LAS. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure LU 57.
Patient survival among adult lung transplant recipients, 2014-2016, by transplant type. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure LU 58.
Patient survival among adult lung transplant recipients, 2014-2016, by diagnosis group. Patient survival estimated using unadjusted Kaplan-Meier methods. The Other/unknown group includes a small number of heart-lung recipients prior to 2015 who did not have an A/B/C/D diagnosis group specified.
Figure LU 59.
Patient survival among adult lung transplant recipients, 2014-2016, by sex. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure LU 60.
Patient survival among adult lung transplant recipients, 2014-2016, by metropolitan vs. non-metropolitan recipient residence. Patient survival estimated using unadjusted Kaplan-Meier methods.
3. Pediatric Lung Transplantation In The United States
3.1. Waiting List
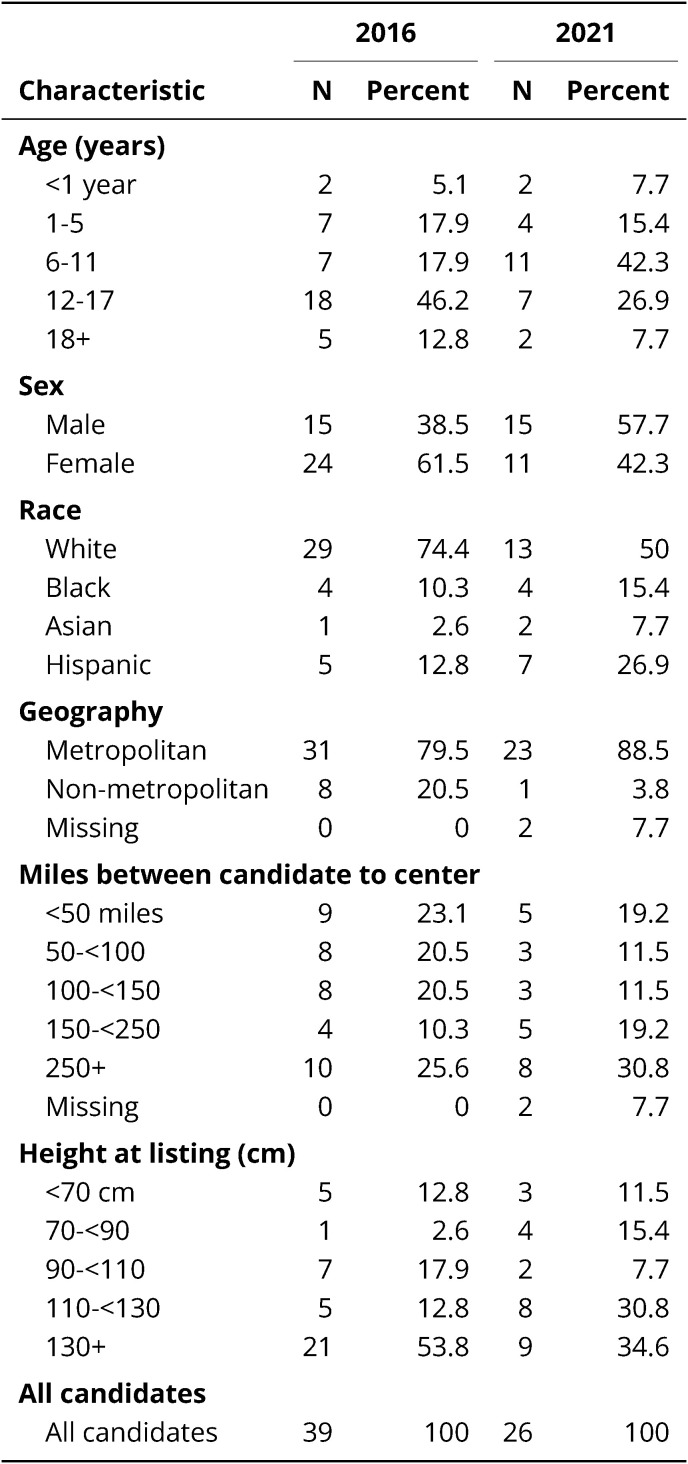
3.1.1. Characteristics of pediatric candidates listed for lung transplant
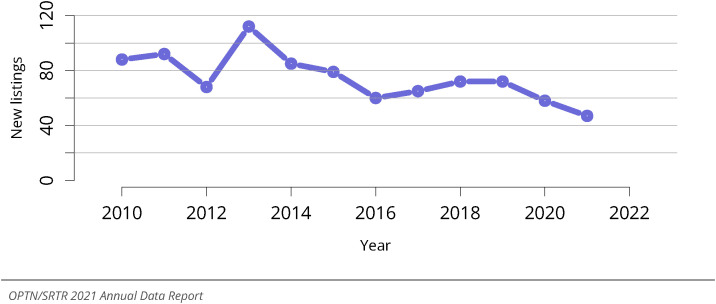
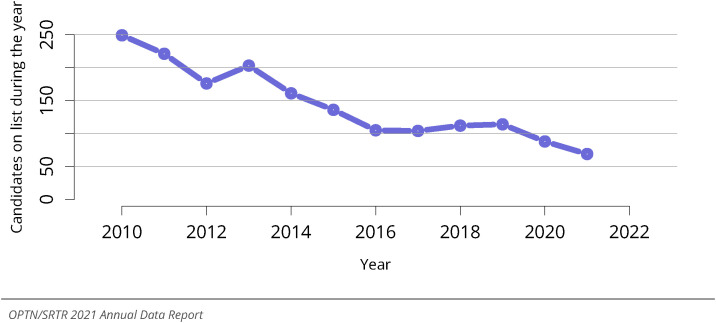
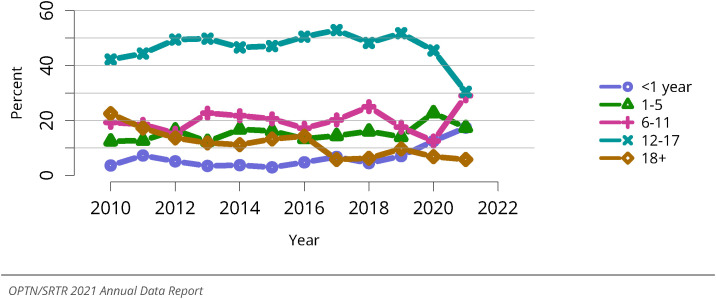
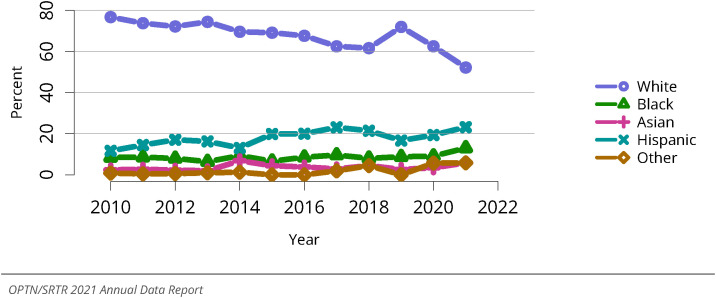
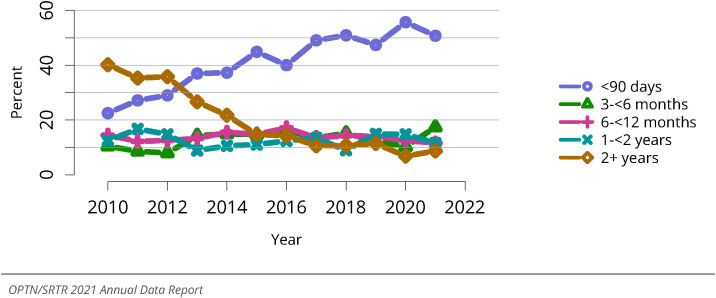
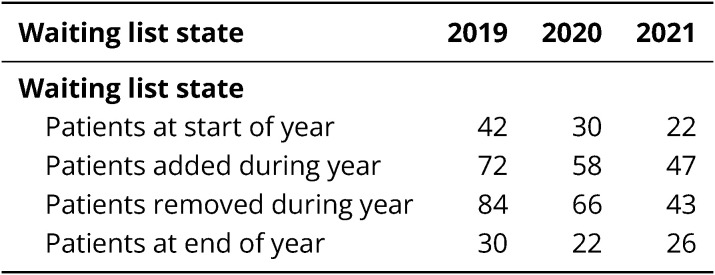
In 2021, 47 new pediatric candidates (younger than 18 years) were added to the lung transplant waiting list, a 47% decrease from 88 new listings in 2010 (Figure LU 64). The total number of pediatric waitlist candidates decreased by 72.3%, from 249 in 2010 to 69 in 2021 (Figure LU 65, Table LU 10). The largest age group of pediatric candidates on the waiting list in 2021 was 12-17 years (30.3%), followed by other age groups: 6-11 years, younger than 1 year, 1-5 years, and 18 years or older (Figure LU 66). Most pediatric lung transplant candidates were White (52.2%), followed by Hispanic (23.2%), Black (13.0%), and Asian (5.8%) (Figure LU 67). Most (50.7%) pediatric candidates on the waiting list in 2021 had been on the list fewer than 90 days (Figure LU 69).
Figure LU 64.
New pediatric candidates added to the lung transplant waiting list. A new candidate is one who first joined the list during the given year, without having been listed in a previous year. Previously listed candidates who underwent transplant and subsequently relisted are considered new. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure LU 65.
All pediatric candidates on the lung transplant waiting list. Pediatric candidates listed at any time during the year. Candidates listed at more than one center are counted once per listing.
Figure LU 66.
Distribution of pediatric candidates waiting for lung transplant by age. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive candidates are included. Age is determined at the earliest of transplant, death, removal, or December 31 of the year.
Figure LU 67.
Distribution of pediatric candidates waiting for lung transplant by race. Candidates waiting for transplant any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive candidates are included.
Figure LU 69.
Distribution of pediatric candidates waiting for lung transplant by waiting time. Candidates waiting for transplant any time in the given year. Candidates listed at more than one center are counted once per listing. Time on the waiting list is determined at the earliest of transplant, death, removal, or December 31 of the year. Active and inactive candidates are included.
3.1.2. Outcomes of pediatric candidates listed for lung transplant
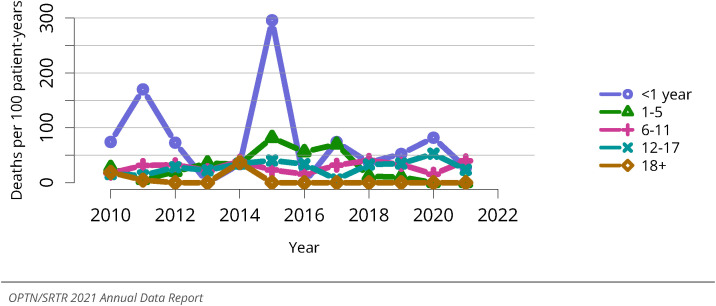
Of 43 candidates removed from the waiting list in 2021, 25 (58.1%) were removed after undergoing transplant, 6 (14.0%) due to becoming too sick to undergo transplant, 5 (11.6%) due to improved condition, and 3 (7.0%) due to patient death (Table LU 13). Among pediatric lung transplant candidates listed in 2016-2018, 62.4% underwent deceased donor transplant within 3 years, 18.8% were removed from the list for reasons other than transplant or death, 17.3% died waiting, and 1.5% were still waiting (Figure LU 70). The overall pediatric lung transplant rate has generally increased since 2010, but it has decreased in the past 3 years from 150.3 transplants per 100 patient-years in 2019 to 108.7 transplants per 100 patient-years in 2021 (Figure LU 71). Transplant rates varied with age and were highest for candidates aged 12-17 years (211.2 per 100 patient-years), followed by candidates younger than 1 year (207.4 per 100 patient-years), 6-11 years (61.1 per 100 patient-years), and 1-5 years (59.6 per 100 patient-years) (Figure LU 72). Transplant rates also varied by race, with the highest rates among those who reported their race as “other,” likely due to the small size of the group (471.0 per 100 patient-years), followed by Hispanic candidates (234.5 per 100 patient-years), Black candidates (117.6 per 100 patient-years), White candidates (83.9 per 100 patient-years), and Asian candidates (49.3 per 100 patient-years) (Figure LU 73). Pretransplant mortality decreased from a peak of 42.9 deaths per 100 patient-years in 2015 to 17.5 per 100 patient-years in 2021 (Figure LU 74). Pretransplant mortality varied by age, ranging from 31.7 deaths per 100 patient-years among candidates aged 12-17 years to 0 among candidates aged 1-5 years and 18 years or older (Figure LU 75).
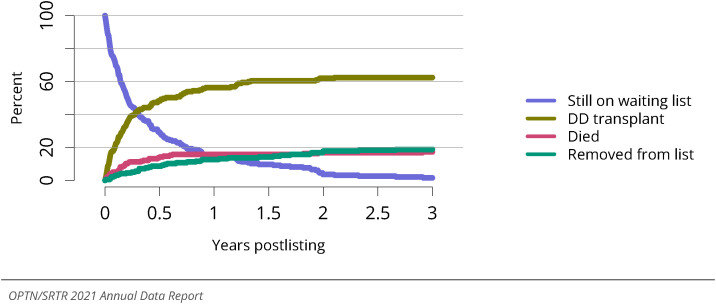
Figure LU 70.
Three-year outcomes for newly listed pediatric candidates waiting for lung transplant, 2016-2018. Pediatric candidates who joined the waiting list in 2016-2018. Pediatric candidates listed at more than one center are counted once per listing. Removed from list includes all reasons except transplant and death. DD, deceased donor.
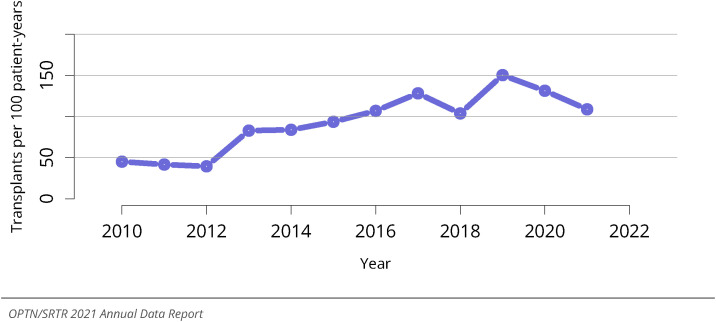
Figure LU 71.
Overall deceased donor lung transplant rates among pediatric waitlist candidates. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of waiting in a given year. Individual listings are counted separately.
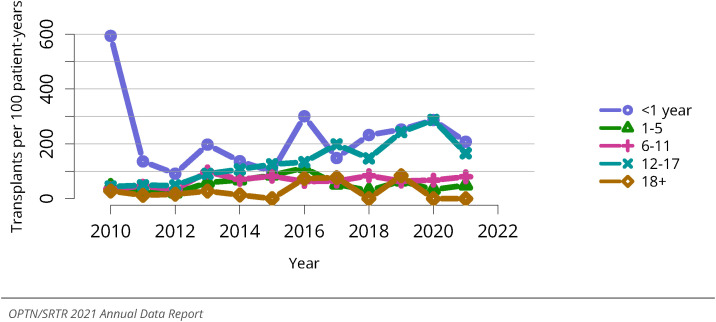
Figure LU 72.
Deceased donor lung transplant rates among pediatric waitlist candidates by age. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of waiting in a given year. Individual listings are counted separately. Age is determined at the later of listing date or January 1 of the given year.
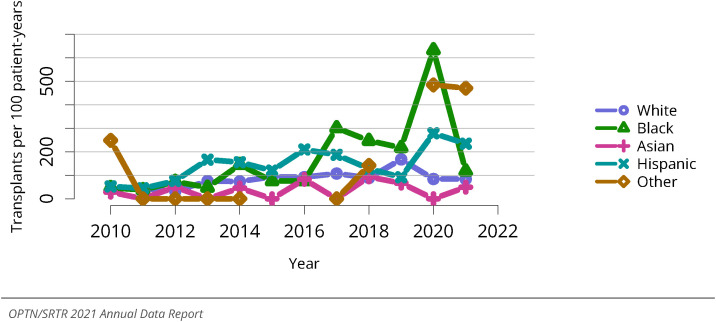
Figure LU 73.
Deceased donor lung transplant rates among pediatric waitlist candidates by race. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of waiting in a given year. Individual listings are counted separately.
Figure LU 74.
Overall pretransplant mortality rates among pediatric candidates waitlisted for lung. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure LU 75.
Pretransplant mortality rates among pediatric candidates waitlisted for lung transplant by age. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately. Age is determined at the later of listing date or January 1 of the given year.
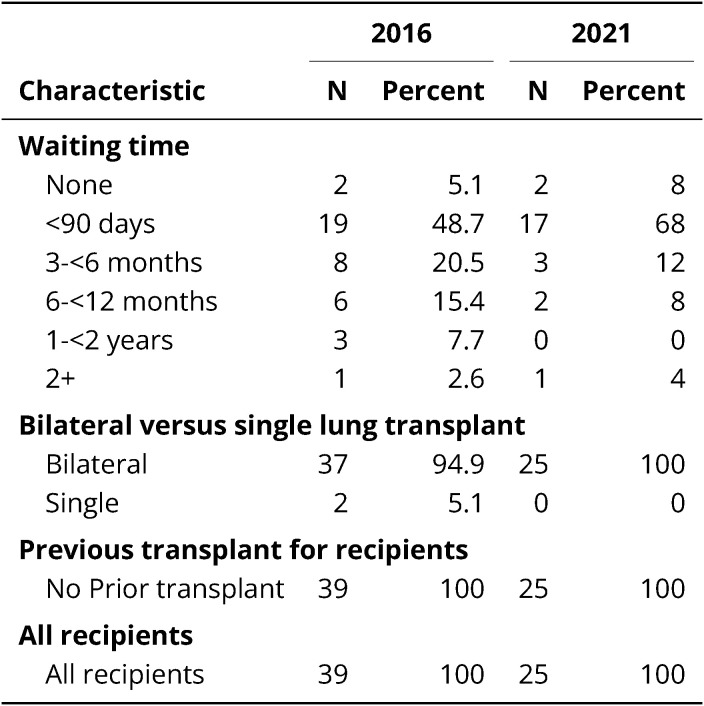
3.2. Transplant
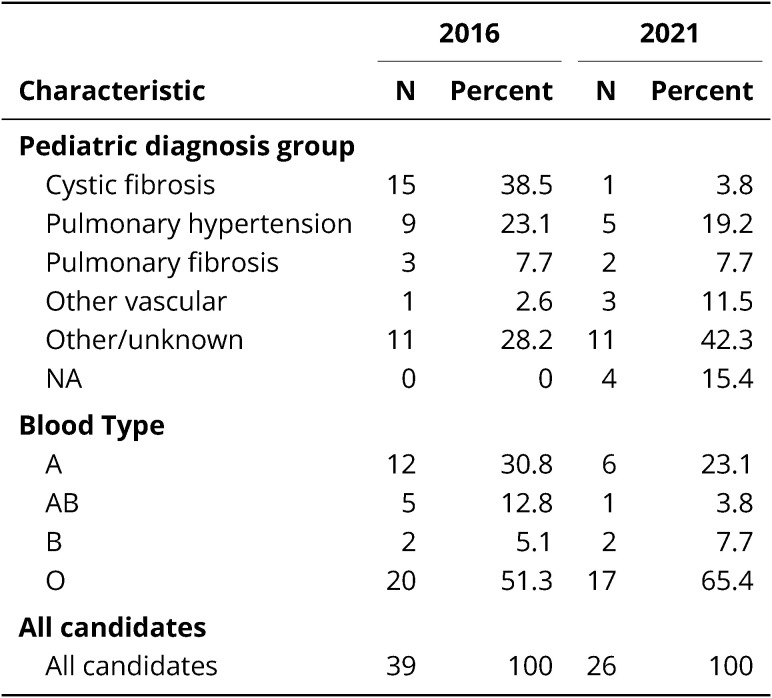
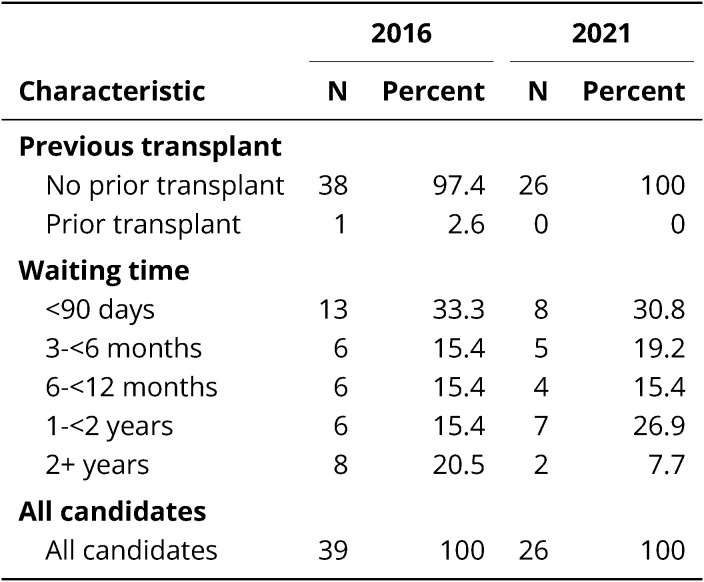
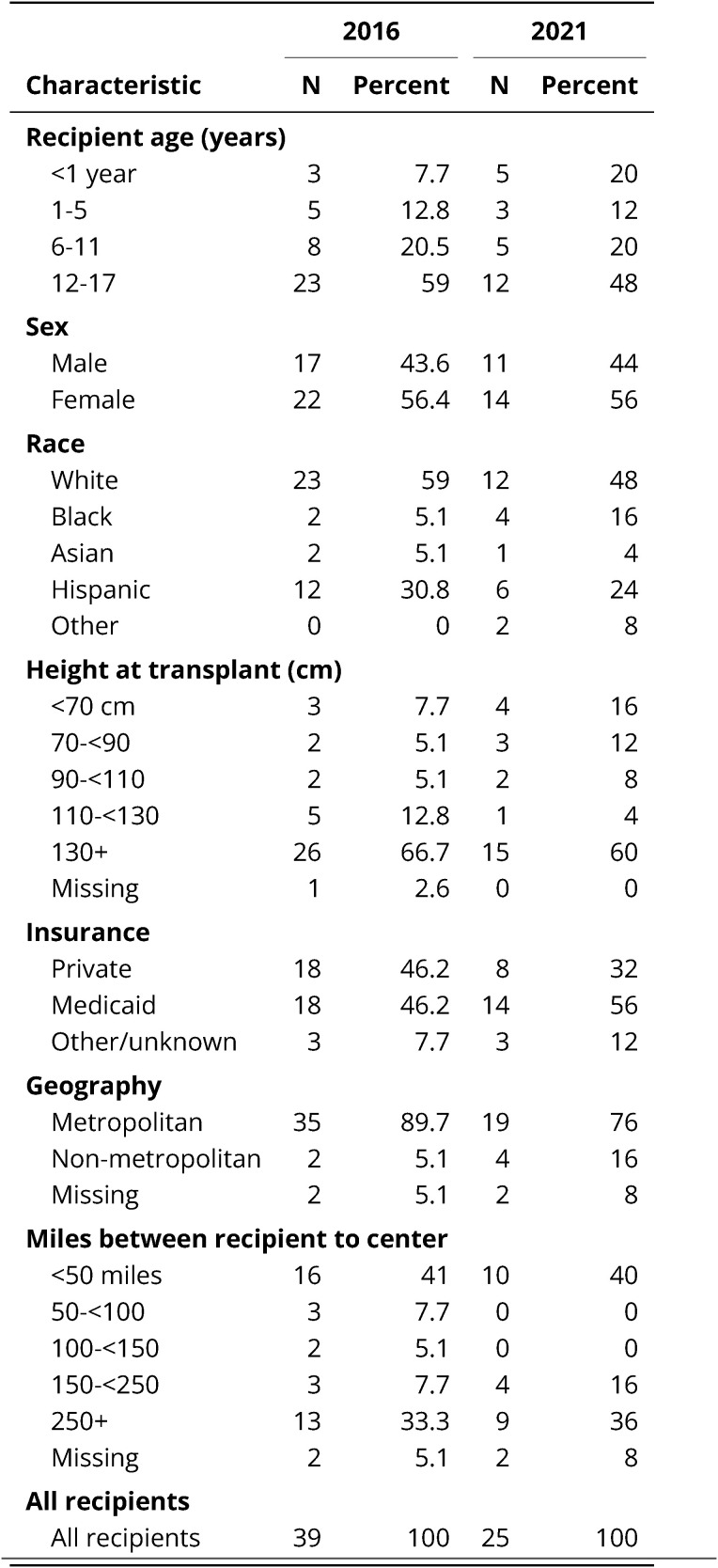
3.2.1. Characteristics of pediatric lung transplant recipients
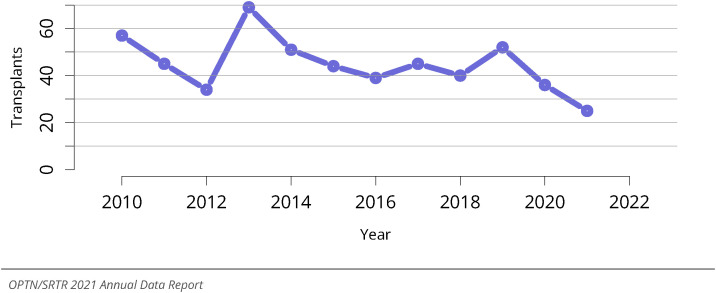
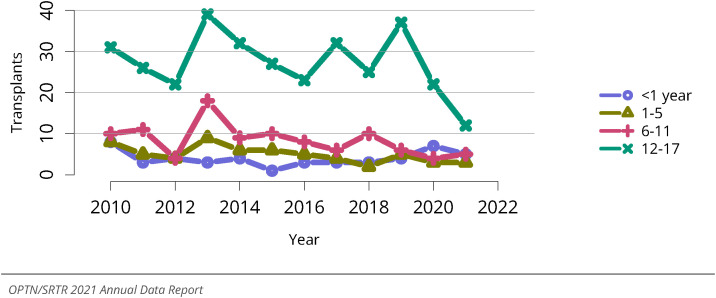
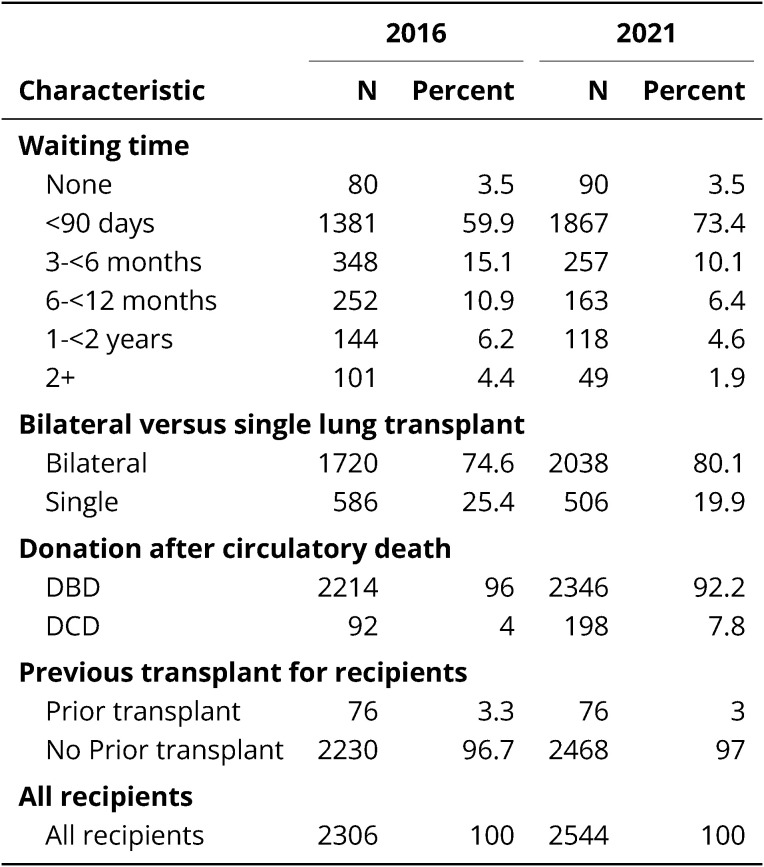
In 2021, 25 lung transplants were performed in pediatric recipients aged 0-17 years, a decrease of 56% since 2010 (Figure LU 76): five in those younger than 1 year, three in those aged 1-5 years, five in those aged 6-11 years, and twelve in those aged 11-17 years (Figure LU 77). An increasing proportion of candidates was bridged to transplant; 16.0% required mechanical ventilation and extracorporeal membrane oxygenation (ECMO), 16.0% mechanical ventilation only, and 8.0% ECMO only (Table LU 15). Time to transplant has changed over time, with 76% of recipients in 2021 with waiting times shorter than 90 days, compared with 53.8% in 2016 (Table LU 16). Induction therapy was reported in 84.0% of pediatric lung transplant recipients in 2021 (Figure LU 78). The most common initial immunosuppression regimen was tacrolimus, mycophenolate, and steroids, reported in 92.0% of pediatric lung recipients (Figure LU 79).
Figure LU 76.
Overall pediatric lung transplants. All pediatric lung transplant recipients, including retransplant, and multiorgan recipients.
Figure LU 77.
Pediatric lung transplants by recipient age. All pediatric lung transplant recipients, including retransplant, and multiorgan recipients.
Table LU 15.
Clinical characteristics of pediatric lung transplant recipients, 2016 and 2021. Pediatric lung transplant recipients, including retransplants. Pediatric priority was reported in 2010 and later. ECMO, extracorporeal membrane oxygenation.
Table LU 16.
Transplant characteristics of pediatric lung transplant recipients, 2016 and 2021. Pediatric lung transplant recipients, including retransplants.
Figure LU 78.
Induction agent use in pediatric lung transplant recipients. Immunosuppression at transplant reported to the OPTN.
Figure LU 79.
Immunosuppression regimen use in pediatric lung transplant recipients. Immunosuppression regimen at transplant reported to the OPTN. Tac, tacrolimus. MMF, all mycophenolate agents.
3.2.2. Outcomes of pediatric lung transplant recipients
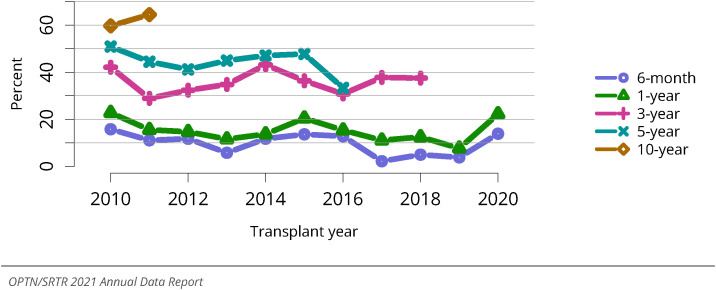
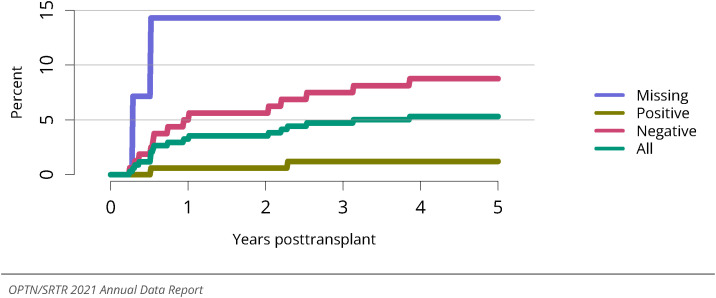
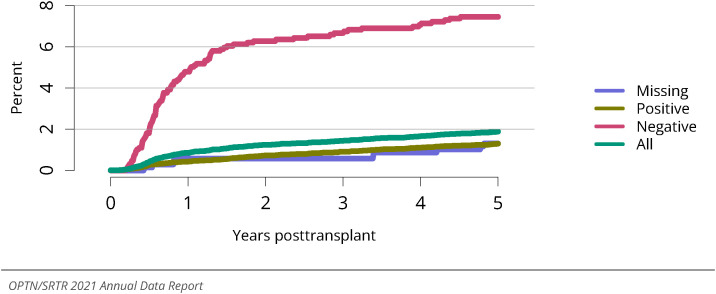
Across all pediatric recipients who underwent lung transplant in 2014-2016, 1-, 3-, and 5-year patient survival was 83.6%, 62.7%, and 56.7%, respectively (Figure LU 82). Incidence of death was 13.9% at 6 months and 22.2% at 1 year for transplants in 2020, 37.5% at 3 years for transplants in 2018, 33.3% at 5 years for transplants in 2016, and 64.4% at 10 years for transplants in 2011 (Figure LU 81). The incidence of posttransplant lymphoproliferative disorder among Epstein-Barr–negative recipients who underwent transplant in 2010-2016 was 8.8% at 5 years posttransplant, compared with 1.2% among Epstein-Barr–positive recipients (Figure LU 80).
Figure LU 82.
Overall patient survival among pediatric deceased donor lung transplant recipients, 2014-2016. Recipient survival estimated using unadjusted Kaplan-Meier methods.
Figure LU 81.
Patient death among pediatric lung transplant recipients. All pediatric recipients of deceased donor lungs, including multiorgan transplants. Estimates are unadjusted, computed using unadjusted Kaplan-Meier methods.
Figure LU 80.
Incidence of PTLD among pediatric lung transplant recipients by recipient EBV status at transplant, 2010-2016. Cumulative incidence is estimated using the Kaplan-Meier method. PTLD is identified as a reported complication or cause of death on the OPTN Transplant Recipient Follow-up Form or on the Posttransplant Malignancy Form as polymorphic PTLD, monomorphic PTLD, or Hodgkin’s disease. Only the earliest date of PTLD diagnosis is considered. EBV, Epstein-Barr virus. PTLD, posttransplant lymphoproliferative disorder.
This publication was produced for the U.S. Department of Health and Human Services (HHS), Health Resources and Services Administration (HRSA), by Hennepin Healthcare Research Institute (HHRI) and the United Network for Organ Sharing (UNOS) under contracts HHSH75R60220C00011 and HHSH250201900001C, respectively.
This publication lists nonfederal resources in order to provide additional information to consumers. The views and content in these resources have not been formally approved by HHS or HRSA. Neither HHS nor HRSA endorses the products or services of the listed resources.
The OPTN/SRTR 2021 Annual Data Report is not copyrighted. Readers are free to duplicate and use all or part of the information contained in this publication. Data are not copyrighted and may be used without permission if appropriate citation information is provided.
Pursuant to 42 U.S.C. 1320b-10, this publication may not be reproduced, reprinted, or redistributed for a fee without specific written authorization from HHS.
Suggested Citations:
Full citation: Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR). OPTN/SRTR 2021 Annual Data Report. U.S. Department of Health and Human Services, Health Resources and Services Administration; 2023. Accessed [insert date]. http://srtr.transplant.hrsa.gov/annual_reports/Default.aspx
Abbreviated citation: OPTN/SRTR 2021 Annual Data Report. HHS/HRSA; 2023. Accessed [insert date]. http://srtr.transplant.hrsa.gov/annual_reports/Default.aspx
Publications based on data in this report or supplied on request must include a citation and the following statement: The data and analyses reported in the OPTN/SRTR 2021 Annual Data Report have been supplied by the United Network for Organ Sharing and Hennepin Healthcare Research Institute under contract with HHS/HRSA. The authors alone are responsible for reporting and interpreting these data; the views expressed herein are those of the authors and not necessarily those of the U.S. government.
This report is available at https://srtr.transplant.hrsa.gov. Individual chapters may be downloaded.
Figure LU 18: Deceased donor lung transplant rates among adult waitlist candidates by metropolitan vs. non-metropolitan residence. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately. Urban/rural determination is made using the RUCA (rural-urban commuting area) designation of the candidate’s permanent zip code.
Figure LU 29: Pretransplant mortality rates among adults waitlisted for lung transplant by metropolitan vs. non-metropolitan residence. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately. Urban/rural determination is made using the RUCA (rural-urban commuting area) designation of the candidate’s permanent zip code.
Figure LU 35: Deceased lung donor count by age. Count of deceased donors with at least one lung recovered. Donors are counted once, regardless of the number of lungs recovered.
Figure LU 61: Incidence of acute rejection by 1 year posttransplant among adult lung transplant recipients by age. Only the first reported rejection event is counted. Cumulative incidence is estimated using the Kaplan-Meier method.
Figure LU 62: Incidence of acute rejection by 1 year posttransplant among adult lung transplant recipients by induction agent. Only the first reported rejection event is counted. Cumulative incidence is estimated using the Kaplan-Meier method. IL2Ab, interleukin-2 receptor antibody; TCD, T-cell depleting.
Figure LU 63: Incidence of PTLD among adult lung transplant recipients by recipient EBV status at transplant, 2010-2016. Cumulative incidence is estimated using the Kaplan-Meier method. PTLD is identified as a reported complication or cause of death on the OPTN Transplant Recipient Follow-up Form or the Posttransplant Malignancy Form as polymorphic PTLD, monomorphic PTLD, or Hodgkin’s disease. Only the earliest date of PTLD diagnosis is considered. EBV, Epstein-Barr virus; PTLD, posttransplant lymphoproliferative disorder.
Figure LU 68: Distribution of pediatric candidates waiting for lung transplant by sex. Candidates waiting for transplant any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Table LU 1.
Demographic characteristics of adults on the lung transplant waiting list on December 31, 2016, and December 31, 2021. Candidates waiting for transplant on December 31 of the given year, regardless of first listing date. Distance is computed from candidate's home zip code to the transplant center. Age is determined on December 31 of the year.
Table LU 2: Clinical characteristics of adults on the lung transplant waiting list on December 31, 2016, and December 31, 2021. Candidates waiting for transplant on December 31 of the given year, regardless of first listing date.
Table LU 3.
Listing characteristics of adults on the lung transplant waiting list on December 31, 2016, and December 31, 2021. Candidates waiting for transplant on December 31 of the given year, regardless of first listing date.
Table LU 4: Lung transplant waitlist activity among adults. Candidates listed at more than one center are counted once per listing. Candidates who are listed, undergo transplant, and are relisted are counted more than once. Candidates are not considered to be on the list on the day they are removed; counts on January 1 may differ from counts on December 31 of the prior year. Candidates listed for multiorgan transplants are included.
Table LU 7: Clinical characteristics of adult lung transplant recipients, 2016 and 2021. Lung transplant recipients, including retransplants. ECMO, extracorporeal membrane oxygenation.
Table LU 8.
Transplant characteristics of adult lung transplant recipients, 2016 and 2021. Lung transplant recipients, including retransplants. DBD, donation after brain death; DCD, donation after circulatory death.
Table LU 9: Demographic characteristics of pediatric candidates on the lung transplant waiting list on December 31, 2016, and December 31, 2021. Candidates younger than 18 years at listing waiting for transplant on December 31 of the given year, regardless of first listing date. Age is determined on December 31 of the year. Distance is computed from candidate's home zip code to the transplant center.
Table LU 10.
Clinical characteristics of pediatric candidates on the lung transplant waiting list on December 31, 2016, and December 31, 2021. Candidates younger than 18 years at listing waiting for transplant on December 31 of the given year, regardless of first listing date.
Table LU 11: Listing characteristics of pediatric candidates on the lung transplant waiting list on December 31, 2016, and December 31, 2021. Candidates younger than 18 years at listing waiting for transplant on December 31 of the given year, regardless of first listing date.
Table LU 12: Lung transplant waitlist activity among pediatric candidates. Candidates who are listed, undergo transplant, and are relisted are counted more than once. Candidates are not considered to be on the list on the day they are removed; counts on January 1 may differ from counts on December 31 of the prior year. Candidates listed for multiorgan transplants are included.
Table LU 13.
Removal reason among pediatric lung transplant candidates. Removal reason as reported to the OPTN. Candidates with death dates that precede removal dates are assumed to have died waiting.
Table LU 14: Demographic characteristics of pediatric lung transplant recipients, 2016 and 2021. Pediatric lung transplant recipients, including retransplants. Distance is computed from recipient's home zip code to the transplant center.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajt.2023.02.010.
Appendix A. Supplementary data
The following is the supplementary data to this article:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.