Abstract
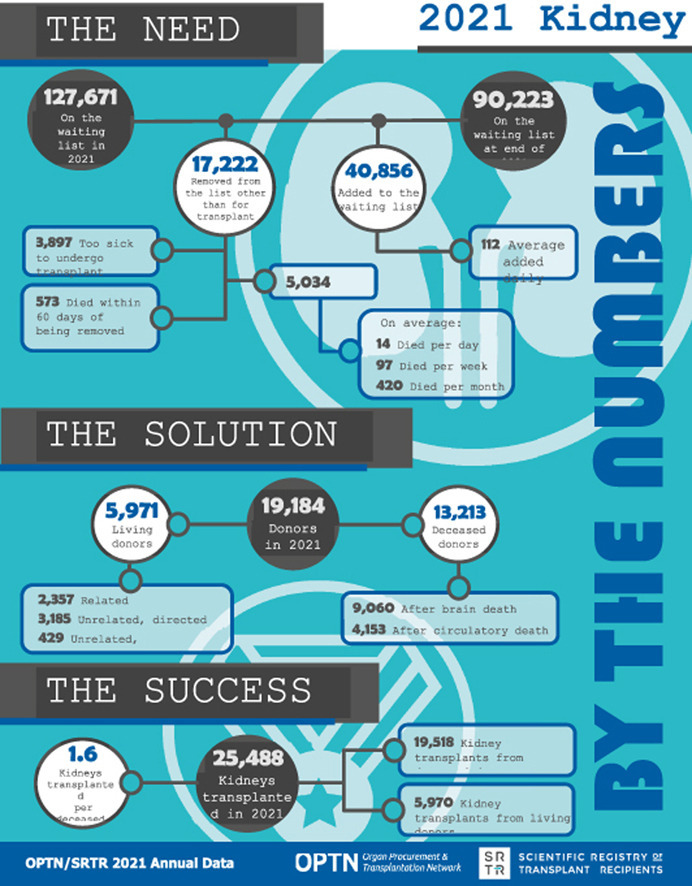
The year 2021 marked both successes and challenges for the field of kid- ney transplantation, in the context of the ongoing COVID-19 pandemic and broader geographic organ distribution. The total number of kidney transplants in the United States reached a record count of 25,487, driven by growth in deceased donor kidney transplants. The total number of candidates listed for deceased donor kidney transplant rose slightly in 2021 but remained below 2019 listing levels, with nearly 10% of candidates having been waiting 5 years or longer. Pretransplant mortality declined slightly among candidates of Black, Hispanic, and other races, in parallel with increasing numbers of Black and Hispanic transplant recipients. In the context of broader organ sharing, there is growing disparity in pretransplant mortality among non-metropolitan compared with metropolitan residents. The proportion of deceased donor kidneys recovered but not used for transplant (nonuse rate) rose to a high of 24.6% overall, with greater nonuse among biopsied kidneys (35.9%), kidneys from donors aged 55 years or older (51.1%), and kidneys with kidney donor profile index (KDPI) of 85% or greater (66.6%). Nonuse of kidneys from donors who are hepatitis C virus (HCV) anti- body positive only slightly exceeded that of HCV antibody–negative donors. Disparities in access to living donor kidney transplant persists, especially for non-White and publicly insured patients. Delayed graft function continues an upward trend and occurred in 24% of adult kidney transplants in 2021. Five-year graft survival after living compared with deceased donor transplant was 88.6% versus 80.7% for recipients aged 18-34 years, and 82.1% versus 68.0% for recipients aged 65 years or older. The total number of pediatric kidney transplants performed increased to 820 in 2021, the highest number since 2010. Despite numerous efforts, living donor kidney transplant re- mains low among pediatric recipients, with continued racial disparities. The rate of deceased donor transplants among pediatric candidates recovered in 2021 from a low in 2020. Congenital anomalies of the kidney and urinary tract remain the leading primary kidney disease diagnosis among pediatric candidates. Most pediatric deceased donor recipients receive a kidney from a donor with KDPI less than 35%. Graft survival continues to improve, with superior outcomes for living donor transplant recipients.
Keywords: Kidney transplant, transplant outcomes, waiting list outcomes
Graphical abstract
1. Introduction
Kidney transplant provides eligible patients with end-stage kidney disease the best op- portunity for long-term, dialysis-free survival at lowest cost to the health care system, but maximizing transplant access, reducing access disparities, and optimizing long-term allograft survival are ongoing challenges. A national urgency to increase access to kid- ney transplant received unprecedented attention from the federal government in the July 2019 Executive Order “Advancing American Kidney Health”1 and is an ongoing fo- cus area in regulatory and legislative actions and proposals. The COVID-19 pandemic profoundly affected kidney transplant practices since the declaration of a public health emergency in March 2020, including living donor transplant rates, organ use rates from deceased donors, and waitlist and posttransplant mortality rates. Changes in kidney distribution from locally prioritized allocation to broader geographic sharing in March 2021 (KAS250) were followed by notable increases in cold ischemia times and delayed graft function. The Annual Data Report is an opportunity to assess the state of kidney transplantation and examine successes along with concerning trends that warrant fur- ther monitoring and evaluation. Data on adult and pediatric kidney transplant waiting lists, deceased and living donation, transplants, and outcomes are provided.
2. Adult Kidney Transplant
2.1. Waiting List
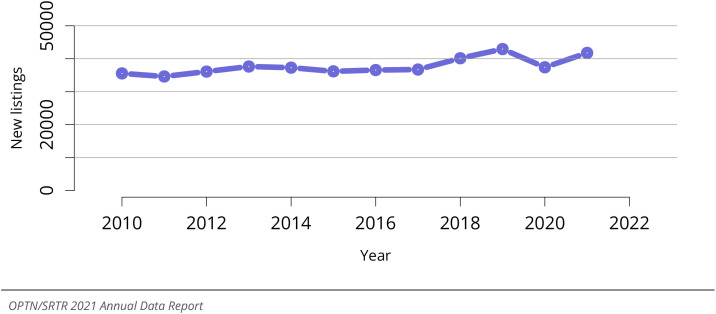
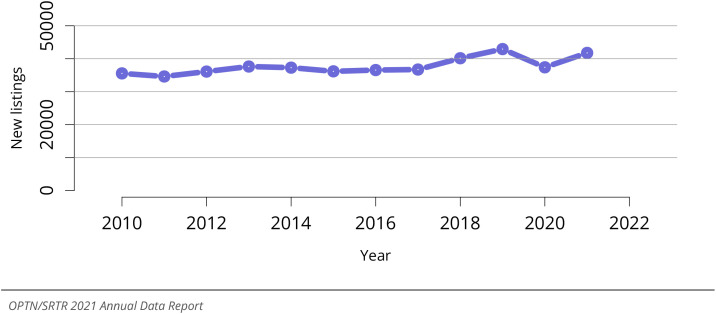
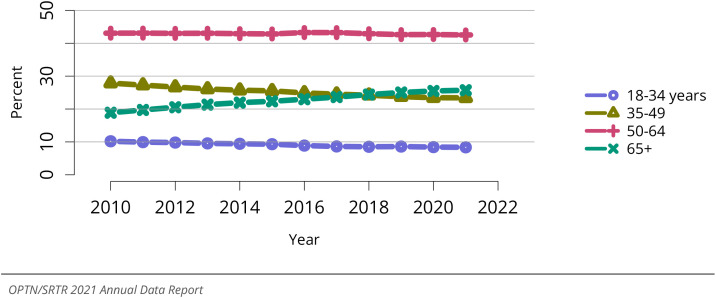
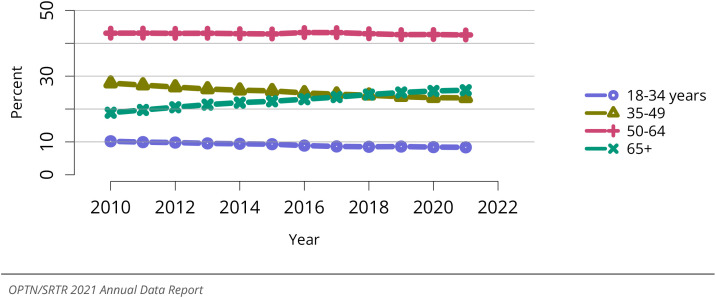
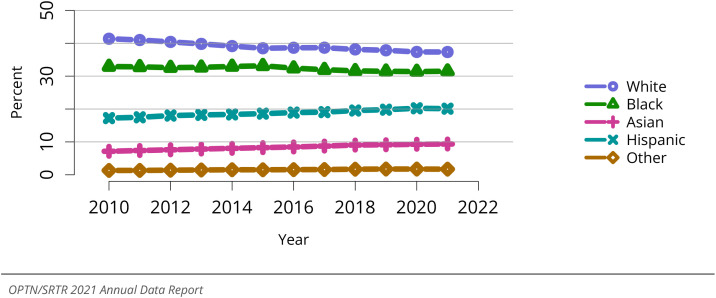
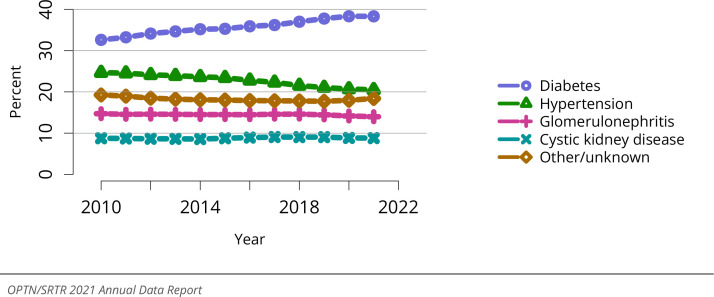
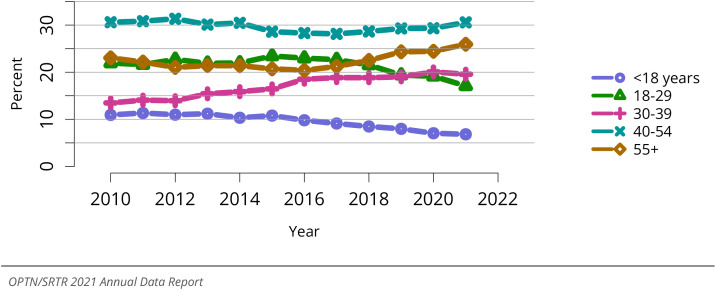
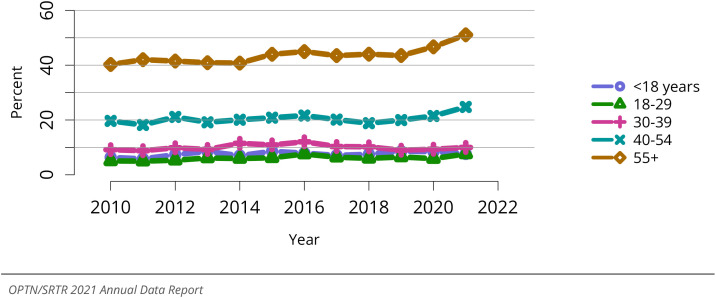
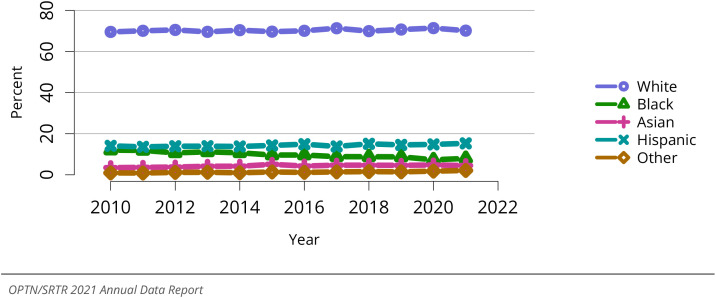
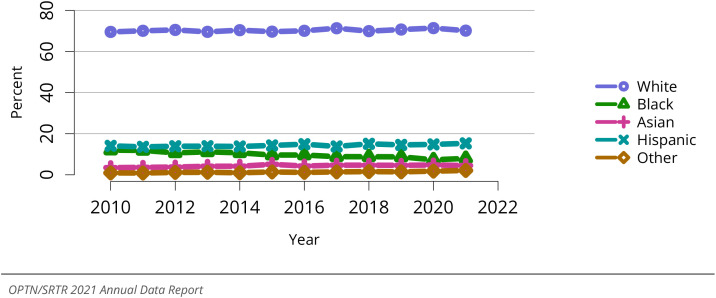
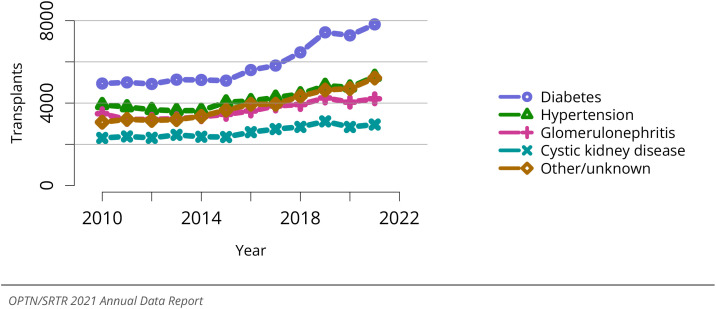
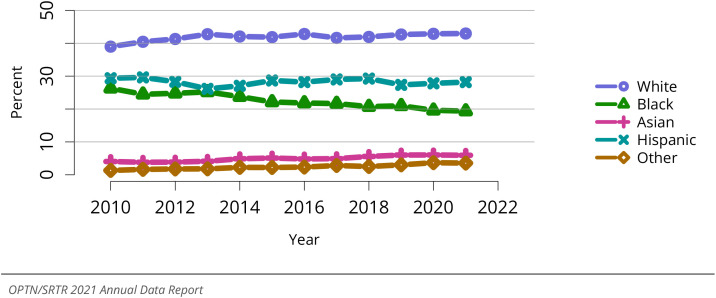
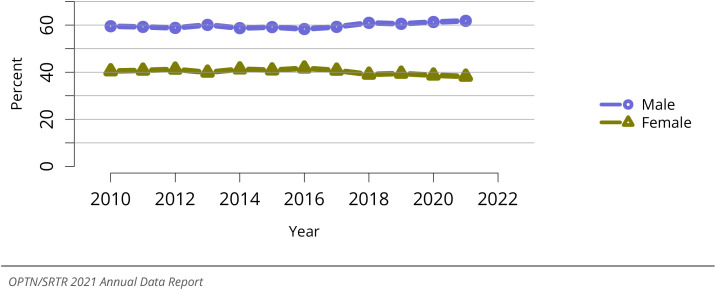
The number of adult candidates added to the kidney waiting list during the year 2021 rose to 41,765, recovering from the pandemic-related decline to 37,399 in 2020, and returning to waitlist addition rates similar to those in 2018-2019 (Figure KI 1). The total number of adult candidates listed for kidney transplant (including those listed at more than one center) rose slightly to 139,025, compared with 138,761 in 2020, but remained below the 144,060 candidates listed in 2019, prior to the COVID-19 pandemic (Figure KI 2). Amidst the ongoing COVID-19 pandemic, in 2021, there were 5,011 waitlist removals due to death, reflecting a slight decline from 5,105 removals due to death in 2020; however, the 4,056 waitlist removals due to being too sick for transplant in 2021 reflects a slight increase from 3,908 in 2020 (Table KI 5). The trend of a gradual increase in the age of candidates on the waiting list over the past 10 years persisted (Figure KI 3). Candidates aged 50-64 years at listing remained the largest age group (42.5% of listed candidates), while the proportion of candidates aged 65 years or older rose slightly to a high of 25.7% (Figure KI 3). The sex distribution of the waiting list was largely unchanged, with men making up 62.0% of kidney candidates (Figure KI 4). Since 2010, the proportion of Asian and Hispanic candidates on the kidney waiting list has gradually increased, accompanied by a decline in the proportion of White candidates, but the distribution in 2021 was stable compared with 2020 (Figure KI 5). The distribution of primary kidney failure diagnoses was stable in 2021, with diabetes (38.3%) and hypertension (20.5%) as the most common identified causes (Figure KI 6).
Figure KI 1.
New adult candidates added to the kidney transplant waiting list. A new candidate is one who first joined the list during the given year, without having been listed in a previous year. Previously listed candidates who underwent transplant and subsequently relisted are considered new. Active and inactive patients are included. Candidates listed at more than one center are counted once per listing. Includes kidney and kidney-pancreas listings.
Figure KI 2.
All adult candidates on the kidney transplant waiting list. Adult candidates on the list at any time during the year. Candidates listed at more than one center are counted once per listing. Includes kidney and kidney-pancreas candidates.
Table KI 5.
Removal reason among adult kidney transplant candidates. Removal reason as reported to the OPTN. Candidates with death dates that precede removal dates are assumed to have died waiting.
| Removal reason | 2019 | 2020 | 2021 |
|---|---|---|---|
| Removal reason | |||
| Deceased donor transplant | 16796 | 17848 | 18827 |
| Living donor transplant | 6605 | 4986 | 5714 |
| Transplant outside US | 64 | 47 | 39 |
| Patient died | 4060 | 5105 | 5011 |
| Patient refused transplant | 398 | 304 | 282 |
| Improved, transplant not needed | 205 | 180 | 217 |
| Too sick for transplant | 4302 | 3908 | 4056 |
| Other | 9933 | 8820 | 8269 |
| Changed to kidney-pancreas list | 242 | 198 | 242 |
| Still on waiting list | 38 | 74 | 238 |
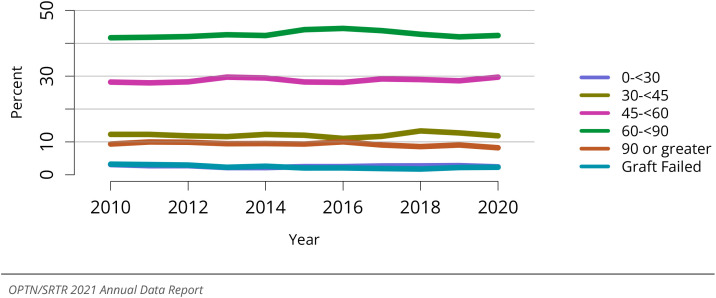
Figure KI 3.
Distribution of adults waiting for kidney transplant by age. Candidates waiting for trans- plant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive candidates are included. Age is determined at the earliest of transplant, death, removal, or December 31 of the year.
Figure KI 4.
Distribution of adults waiting for kidney transplant by sex. Candidates waiting for trans- plant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure KI 5.
Distribution of adults waiting for kidney transplant by race. Candidates waiting for trans- plant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure KI 6.
Distribution of adults waiting for kidney transplant by diagnosis. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
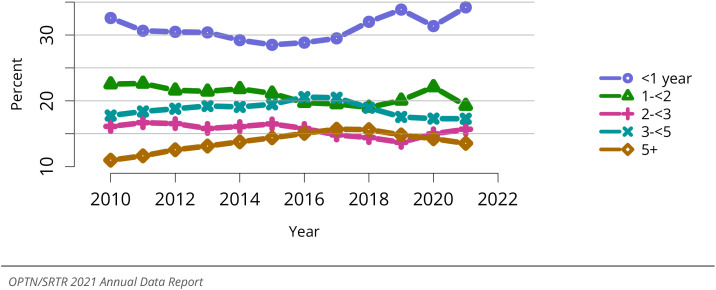
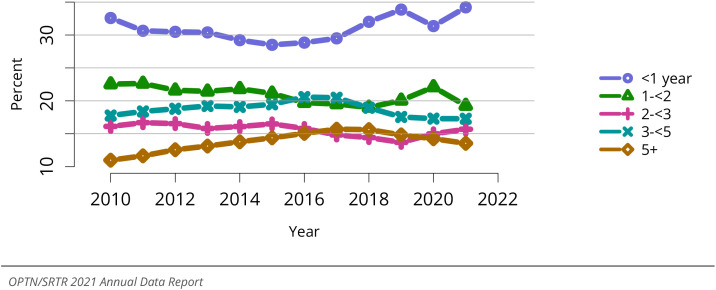
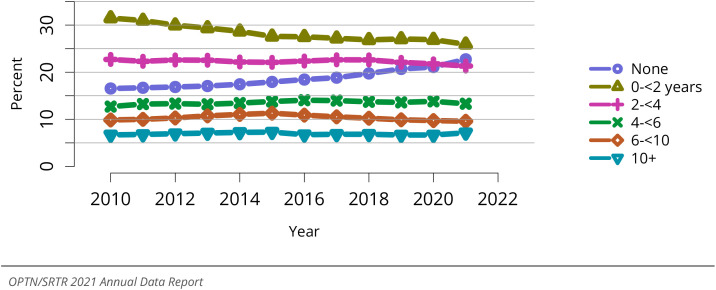
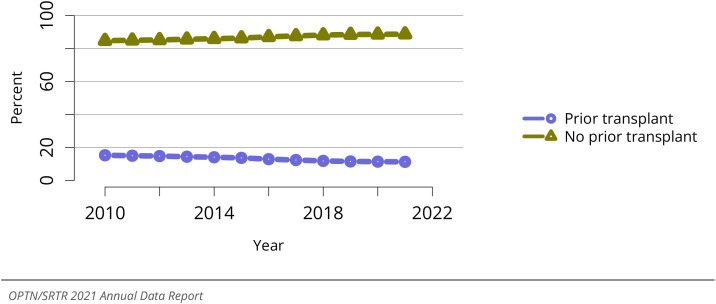
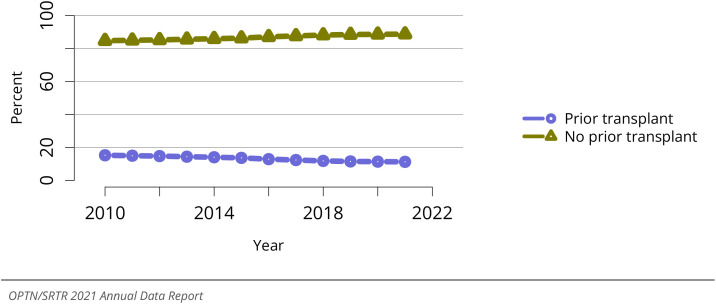
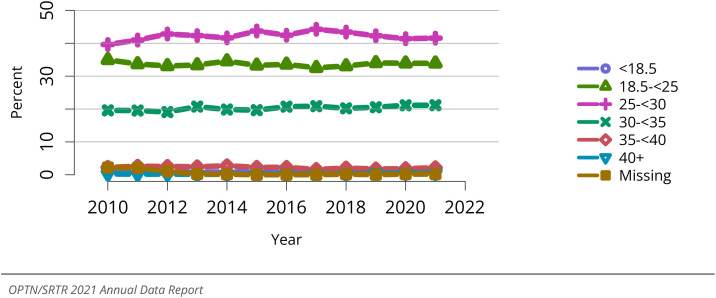
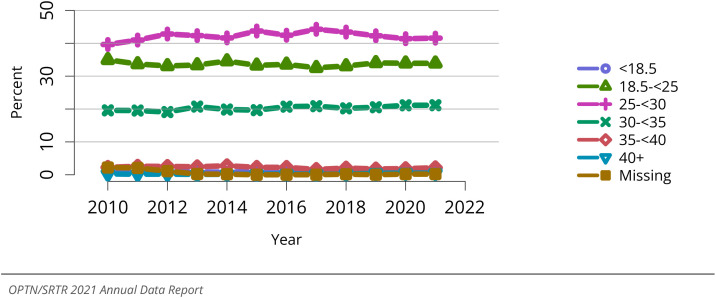
The proportion of candidates prevalent on the waiting list with waiting time less than 1 year rose to 34.2% in 2021 from 31.4% in 2020 and 33.9% in 2019, while 13.6% on the waiting list at some point in 2021 have been waiting 5 years or longer, a proportion that has been decreasing in recent years (Figure KI 7). The proportion of waitlisted candidates with high body mass index (BMI) also continued to increase slightly in 2021, with 27.6% having a BMI of 30-<35 kg/m2 and 18.4% having a BMI of 35 kg/m2 or greater (Figure KI 8). Encouragingly, the proportion of candidates waitlisted before starting dialysis continued to increase, reaching 22.7% in 2021, although 16.7% of those waitlisted had been on dialysis for 6 or more years (Figure KI 9). More than half of waitlisted kidney candidates had blood type O (Figure KI 10). The proportion of candidates with a previous transplant was 11.3% in 2021, reflecting a gradual decline from 15.3% in 2010 (Figure KI 11).
Figure KI 7.
Distribution of adults waiting for kidney transplant by waiting time (years). Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Time on the waiting list is determined at the earliest of transplant, death, removal, or December 31 of the year. Candidates listed in the given year are considered to have been listed less than 1 year. Active and inactive candidates are included.
Figure KI 8.
Distribution of adults waiting for kidney transplant by BMI. Candidates waiting for trans- plant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure KI 9.
Distribution of adults waiting for kidney transplant by years on dialysis. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Time on dialysis is computed as time from minimum of first ESRD service date or most recent graft failure to listing date or January 1 of the given year. Active and inactive candidates are included.
Figure KI 11.
Distribution of adults waiting for kidney transplant by prior transplant status. Candi- dates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
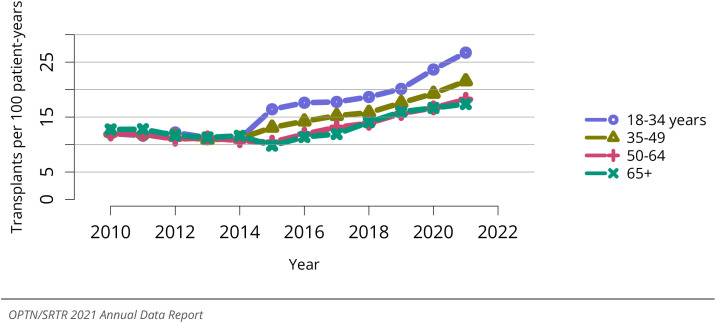
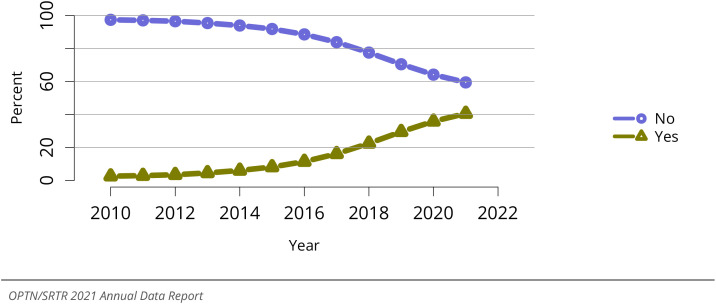
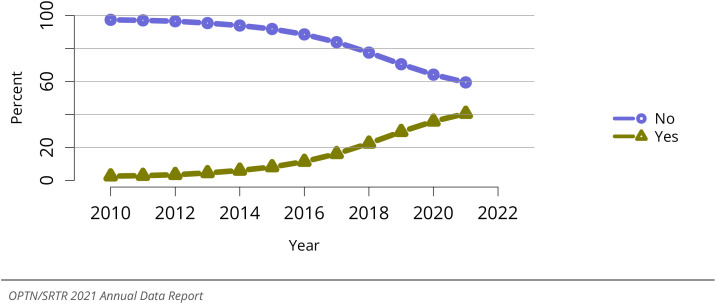
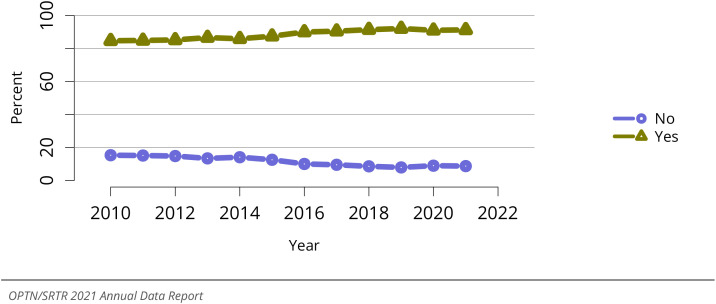
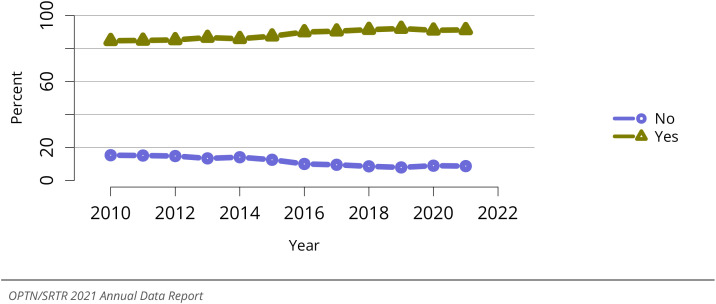
The proportion of candidates willing to accept a kidney with a high kidney donor profile index (KDPI) declined in all age groups in 2021 compared with 2020, continuing a decline after implementation of the revised kidney allocation system (KAS) in December 2014 (Figure KI 12). Half of candidates aged 50-64 years and less than two-thirds of candidates aged 65 years or older were willing to accept these kidneys (Figure KI 12), even though patients aged 50 years and older are less likely than younger patients to undergo kidney transplant under the current KAS (Figure KI 15). Conversely, the proportion of candidates willing to accept a kidney from a donor who is hepatitis C virus (HCV) antibody positive continues to increase sharply, to 40.6% in 2021, correlating with availability of highly effective direct-acting antiviral (DAA) agents and experience using DAA regimens to manage anticipated donor-derived infections (Figure KI 13). To date, the information on willingness to accept HCV-positive kidneys does not differentiate between donor HCV antibody (exposed) and nucleic acid (viremic) status.
Figure KI 12.
Adults willing to accept a kidney designated ECD or KDPI >= 85% by age. Adults waiting for kidney transplant on December 31 of the given year. Candidates listed at more than one center are counted once per listing. Willingness to accept ECD at time of listing or willingness to accept a local non- zero HLA mismatch KDPI >=85% kidney at the later of listing date or January 1 of the given year, beginning in 2014. ECD, expanded criteria donor.
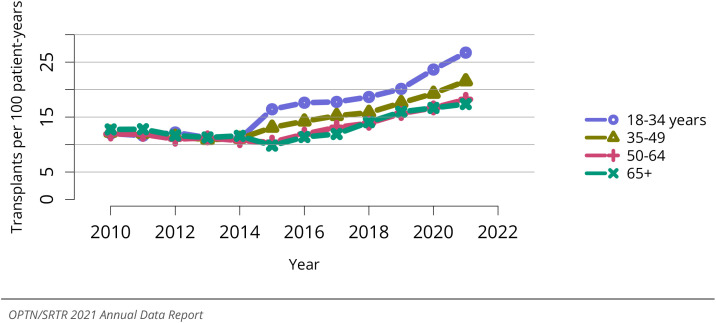
Figure KI 15.
Deceased donor kidney transplant rates among adult waitlist candidates by age. Trans- plant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately. Age is determined at the later of listing date or January 1 of the given year.
Figure KI 13.
Adults willing to accept kidney from HCV+ donor. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Willingness to accept HCV+ organ at time of listing. HCV, hepatitus C virus.
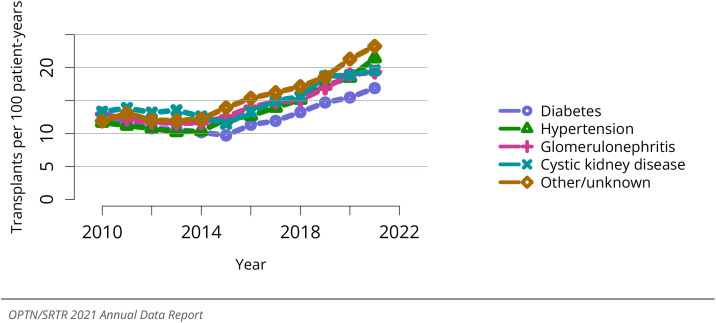
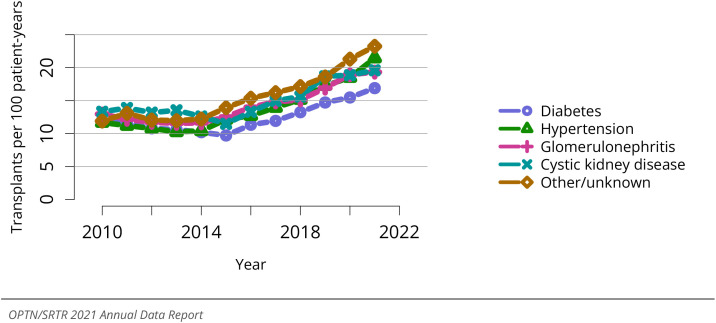
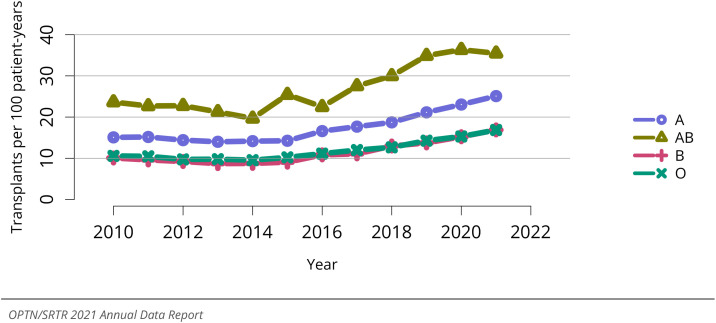
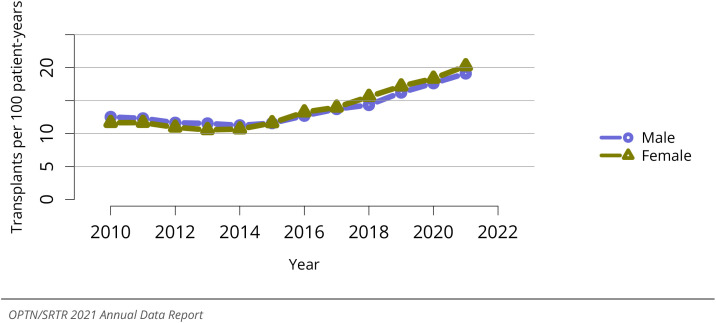
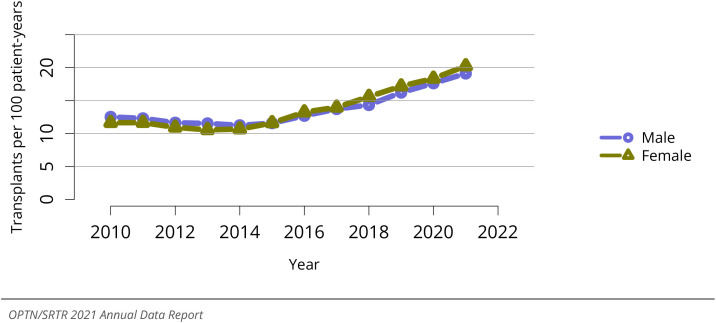
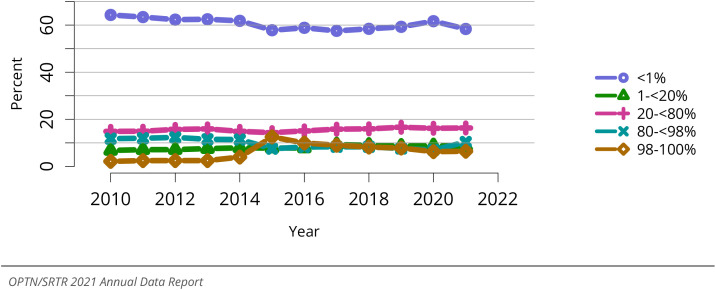
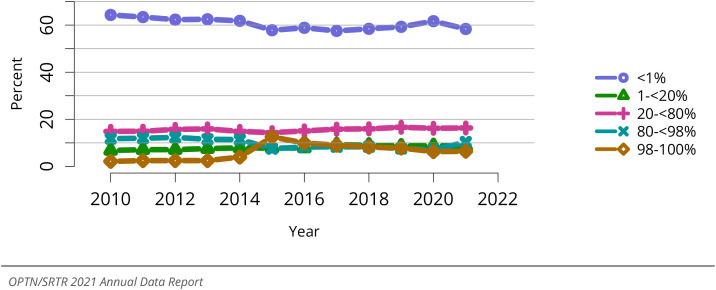
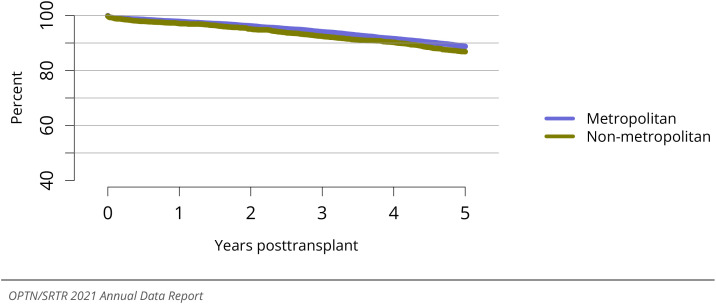
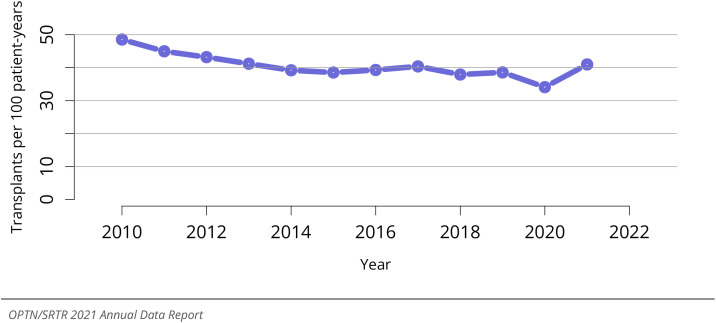
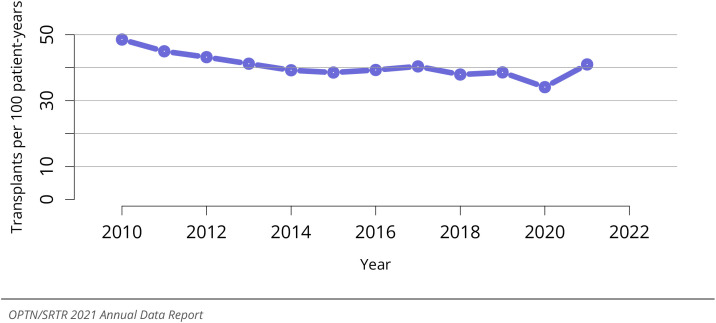
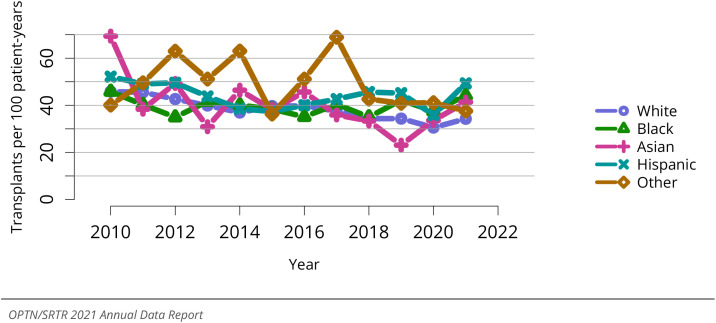
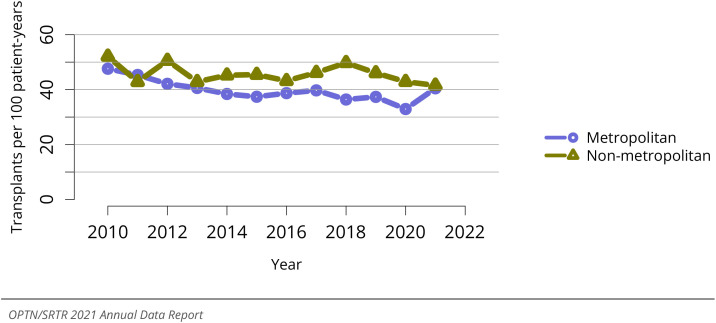
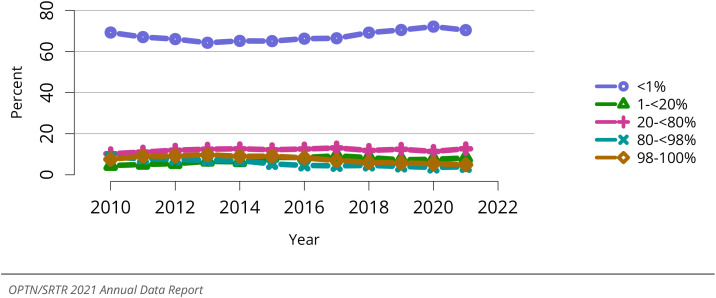
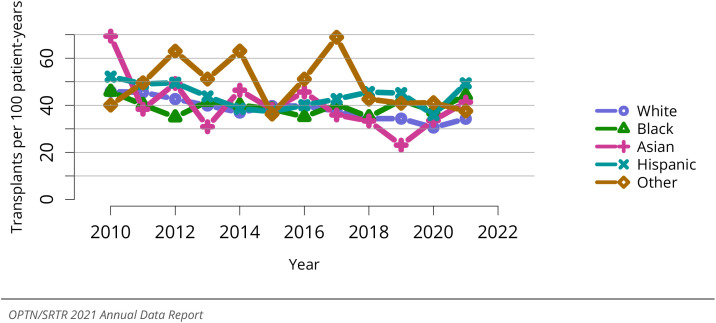
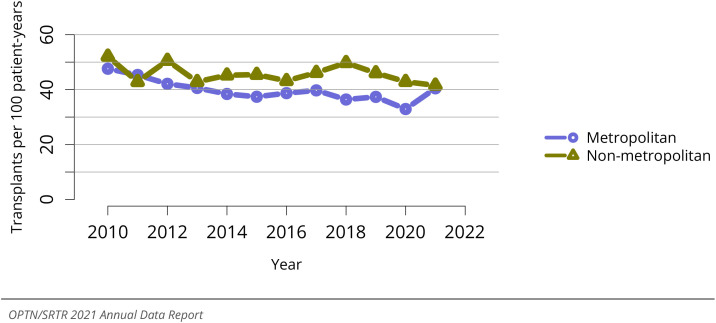
Deceased donor kidney transplant (DDKT) rates among adult waitlisted candidates continued to increase in 2021, after a nadir in 2014 (Figure KI 14). Increased rates were noted across all age groups (Figure KI 15) and primary kidney disease diagnosis groups (Figure KI 17). DDKT rates declined slightly among White candidates in 2021, but rose for all other racial and ethnic groups, especially among Black and Hispanic candidates, such that Black candidates had the highest DDKT rate among racial groups in 2021 (20.8 per 100 patient-years) (Figure KI 16). DDKT rates among patients with calculated panel-reactive antibody (cPRA) levels of 98%-100% rose slightly in 2021 compared with 2020, similar to the rate following the 2014 KAS revision (Figure KI 18). Following the March 2021 (KAS250) changes in organ distribution policy, the DDKT rate for patients with cPRA levels of 80%-<98% rose sharply in 2021 compared with 2020, to 31.0 transplants per 100 patient-years, compared with 16.1 to 19.8 DDKT per 100 patient-years in the other cPRA groups (Figure KI 18). While patients with type AB blood type continued to have the highest DDKT rate, the rate in this group declined slightly in 2021 while rising in other blood type groups (Figure KI 19); these patterns may in part reflect the 2014 revised KAS allowing allocation of A2 and A2B kidneys to B candidates. In 2021, DDKT rates increased across the range of waiting times, especially among those on the waiting list 5 years or longer (Figure KI 20). DDKT rates were similar between men and women in 2021 (Figure KI 21). After the March 2021 KAS250 changes in organ distribution policy and broader sharing, DDKT rates rose in residents of metropolitan areas but declined slightly among non-metropolitan residents, to reach similar rates of 19.4 and 20.4 per 100 patient-years, respectively (Figure KI 22).
Figure KI 14.
Overall deceased donor kidney transplant rates among adult waitlist candidates. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure KI 17.
Deceased donor kidney transplant rates among adult waitlist candidates by diagnosis. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure KI 16.
Deceased donor kidney transplant rates among adult waitlist candidates by race. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure KI 18.
Deceased donor kidney transplant rates among adult waitlist candidates by cPRA. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately. cPRA is determined at the later of listing date or January 1 of the given year.
Figure KI 19.
Deceased donor kidney transplant rates among adult waitlist candidates by blood type. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure KI 20.
Deceased donor kidney transplant rates among adult waitlist candidates by time on the waitlist. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure KI 21.
Deceased donor kidney transplant rates among adult waitlist candidates by sex. Trans- plant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately.
Figure KI 22.
Deceased donor kidney transplant rates among adult waitlist candidates by metropoli- tan vs. non-metropolitan residence. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of wait time in a given year. Individual listings are counted separately. Metropolitan/non-metropolitan determination is made using the RUCA (rural-urban commuting area) des- ignation of the candidate’s permanent zip code.
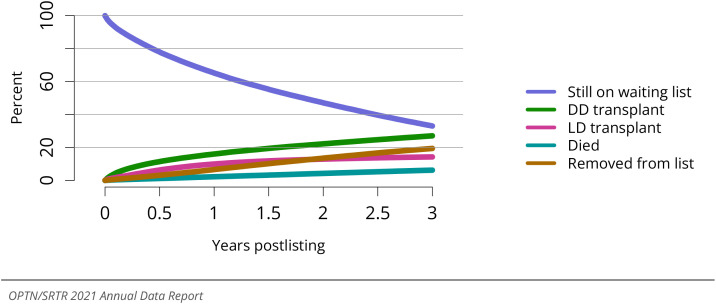
For patients waitlisted in 2016-2018, 33.0% were still waiting in 2021 (3 years after listing); 27.1% had undergone DDKT, 14.3% had undergone living donor kidney trans- plant (LDKT), 6.2% had died, and 19.4% were removed from the waiting list (Figure KI 23). The proportion of patients who underwent DDKT within 3 months rose to a high of 10.6% among those listed in 2020, while the percentage who underwent DDKT within 3 years also continued to rise (Figure KI 24).
Figure KI 23.
Three-year outcomes for adults waiting for kidney transplant, new listings in 2016- 2018. Candidates listed at more than one center are counted once per listing. Removed from list includes all reasons except transplant and death. DD, deceased donor; LD, living donor.
Figure KI 24.
Percentage of adults who underwent deceased donor kidney transplant within a given time period of listing. Candidates listed at more than one center are counted once per listing.
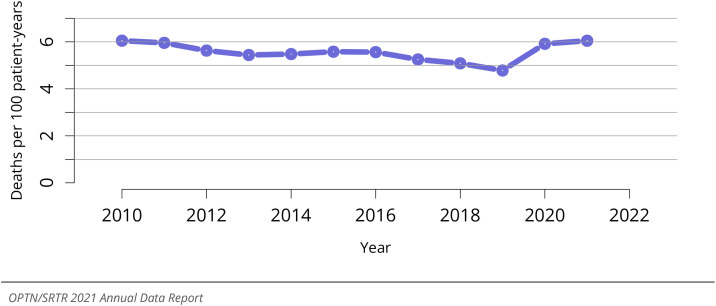
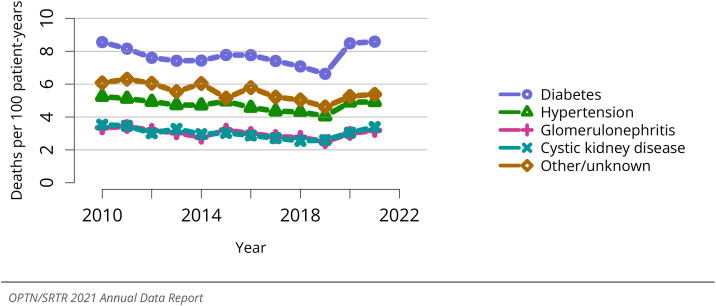
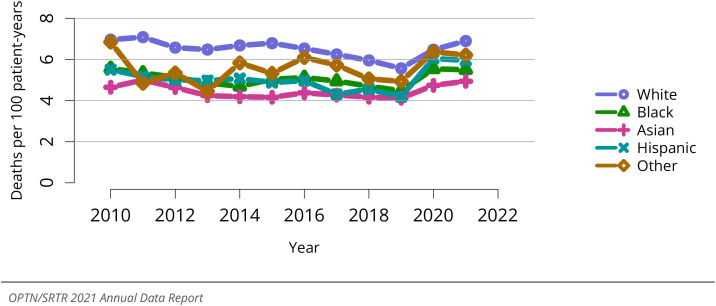
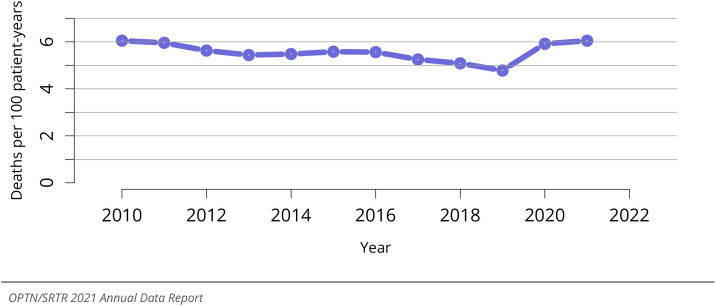
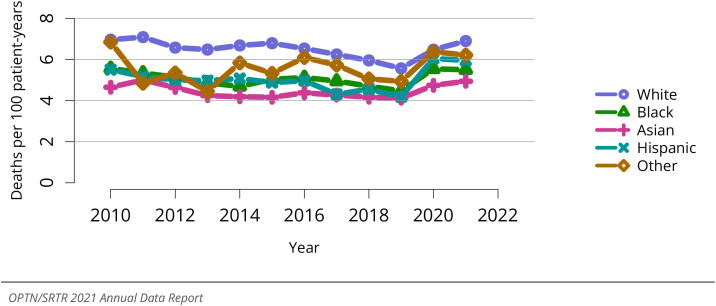
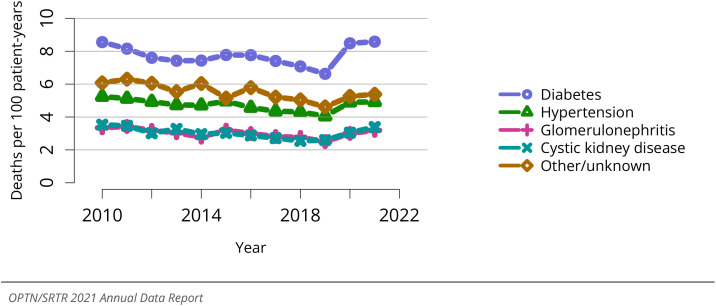
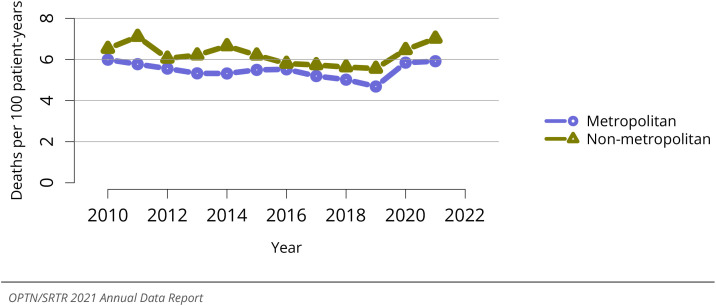
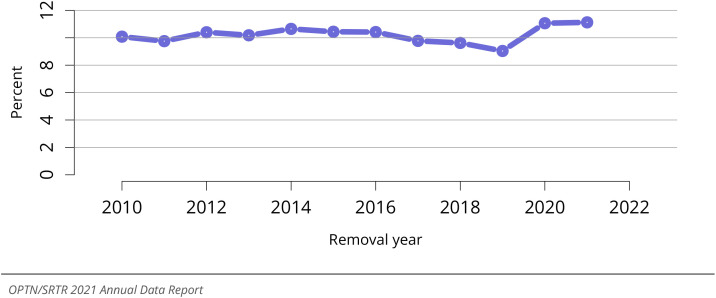
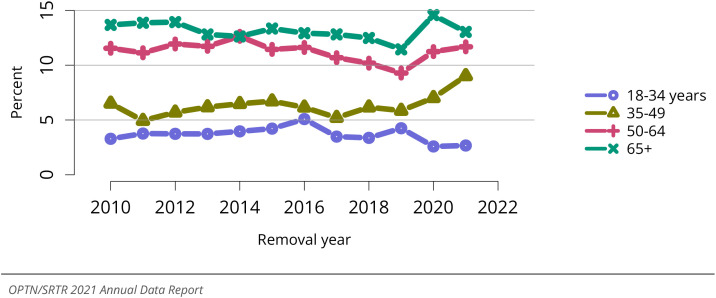
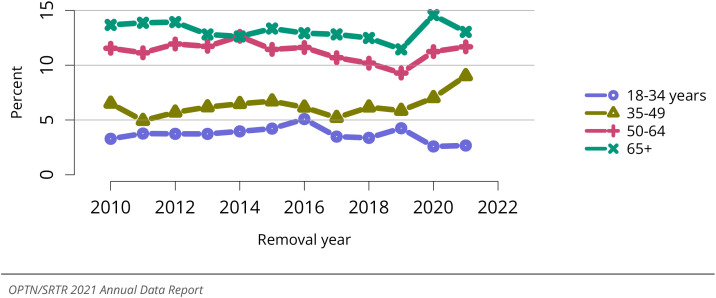
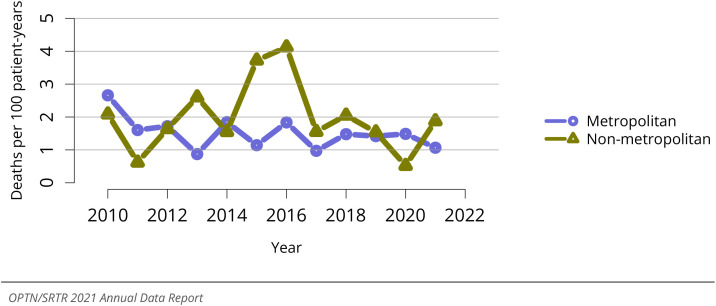
Pretransplant mortality rose slightly in 2021 to 6.0 deaths per 100 patient-years, the highest value since 2010 (Figure KI 25), with similar increases across diagnosis groups (Figure KI 29). Pretransplant mortality rose among men but declined slightly among women (Figure KI 28). Considered by candidate age, pretransplant mortality increased among candidates aged 18-34 years, but remained relatively stable in adults aged 35-64 years and older (Figure KI 26). While pretransplant mortality rates rose among White and Asian candidates in 2021, pretransplant mortality rates declined slightly among can- didates of Black, Hispanic, and other races (Figure KI 27). Considered by blood type, pretransplant mortality was lowest for those with type AB, the group with the highest DDKT rate (Figure KI 30). Pretransplant mortality continued to vary greatly by donation service area, from 3.0 to 8.5 deaths per 100 patient-years (Figure KI 32), and there was a growing disparity in pretransplant mortality among non-metropolitan compared with metropolitan residents (Figure KI 31).
Figure KI 25.
Overall pretransplant mortality rates among adults waitlisted for kidney transplant. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure KI 29.
Pretransplant mortality rates among adults waitlisted for kidney transplant by diag- nosis. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of im- proved condition, or end of cohort. Individual listings are counted separately.
Figure KI 28.
Pretransplant mortality rates among adults waitlisted for kidney transplant by sex. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure KI 26.
Pretransplant mortality rates among adults waitlisted for kidney transplant by age. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately. Age is determined at the later of listing date or January 1 of the given year.
Figure KI 27.
Pretransplant mortality rates among adults waitlisted for kidney transplant by race. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure KI 30.
Pretransplant mortality rates among adults waitlisted for kidney transplant by blood type. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure KI 32.
Pretransplant mortality rates among adults waitlisted for kidney transplant in 2021 by DSA. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
Figure KI 31.
Pretransplant mortality rates among adults waitlisted for kidney transplant by metropolitan vs. non-metropolitan residence. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, trans- fer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately. Urban/rural determination is made using the RUCA (rural-urban commuting area) designation of the candidate’s permanent zip code.
Death within 6 months of removal from the waiting list (for waitlist removal reasons other than transplant) was stable in 2021 compared with 2020 (Figure KI 33). Consid- ered by diagnosis group, mortality after waitlist removal increased for those with hy-pertension and other/unknown causes, was stable in those with diabetes, and declined in those with cystic kidney disease or glomerulonephritis (Figure KI 34). By age, death within 6 months of waitlist removal rose for candidates aged 35-64 years, while remain- ing stable in younger candidates and declining in older candidates (Figure KI 35).
Figure KI 33.
Deaths within six months after removal among adult kidney waitlist candidates, over- all. Denominator includes only candidates removed from the waiting list for reasons other than transplant or death while on the list.
Figure KI 34.
Deaths within six months after removal among adult kidney waitlist candidates, by diagnosis group at removal. Denominator includes only candidates removed from the waiting list for reasons other than transplant or death while on the list.
Figure KI 35.
Deaths within six months after removal among adult kidney waitlist candidates, by age. Denominator includes only candidates removed from the waiting list for reasons other than trans- plant or death while on the list. Age is determined at the later of listing date or January 1 of the given year.
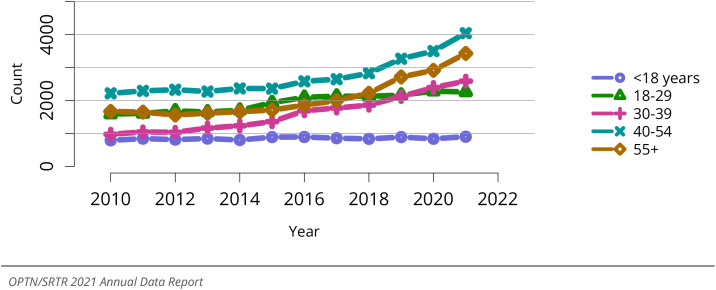
2.2. Deceased Donation
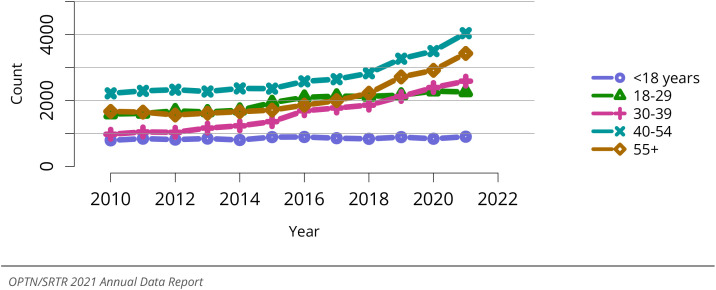
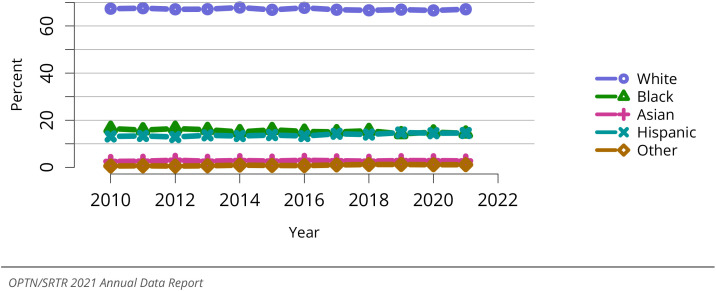
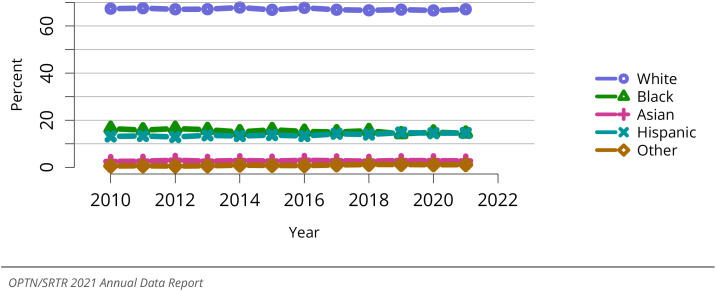
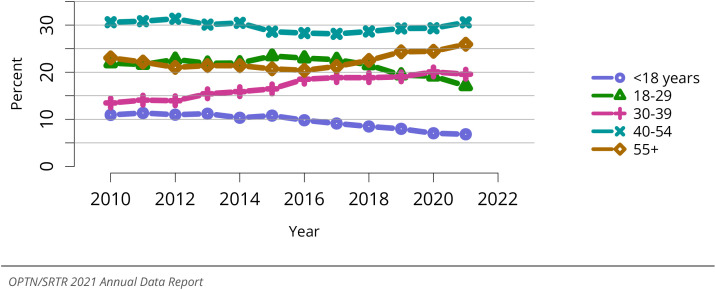
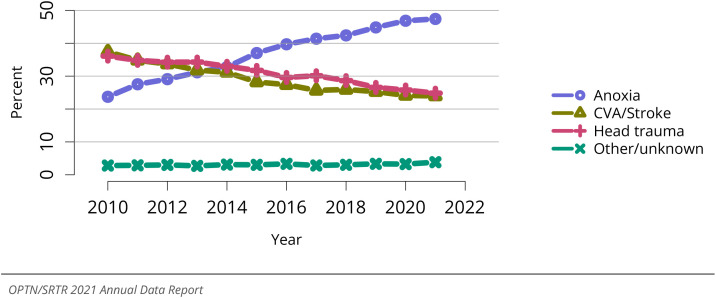
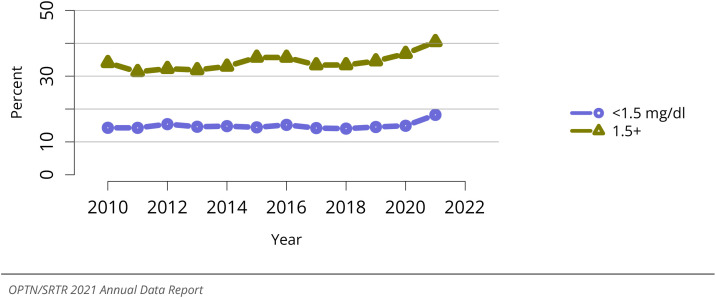
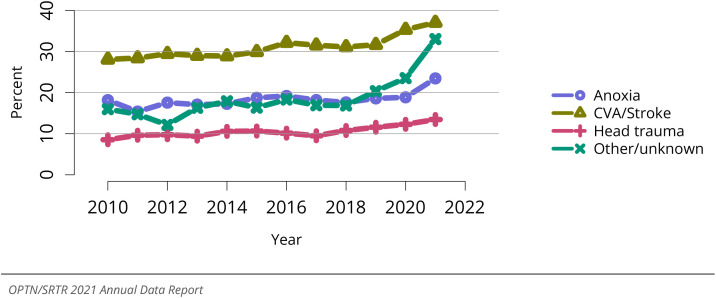
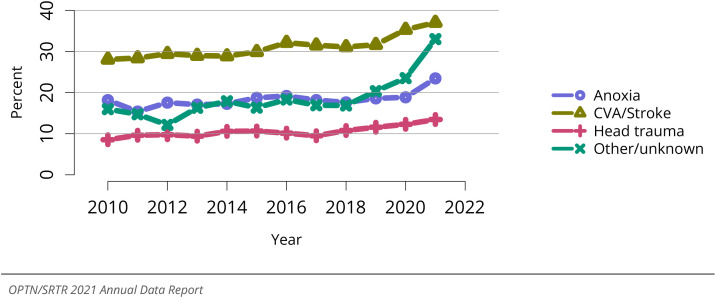
The counts of deceased donors from whom at least one kidney was recovered contin- ued to increase in 2021 (Figure KI 36), particularly among donors aged 30 years and older (Figure KI 37). The counts of HCV-positive deceased donors from whom kidneys were recovered also rose in 2021 (Figure KI 38), although the proportion was slightly lower compared to in 2020 at 10.2% (Figure KI 42). The racial and ethnic distribution of deceased kidney donors remained largely unchanged over the past decade (Figure KI 41), while the proportion of male deceased donors trended slightly higher over the past 2 years (Figure KI 40). In 2021, the proportion of deceased kidney donors aged 18-39 years declined slightly and those younger than 18 years remained stable, while deceased kid- ney donation rose for donors aged 40 years and older (Figure KI 39). The proportion of kidneys recovered from patients who died of anoxia continued to rise slightly in 2021 (Figure KI 43), amid the opioid epidemic.
Figure KI 36.
Overall deceased kidney donor count. Count of deceased donors from whom at least one kidney was recovered for transplant.
Figure KI 37.
Deceased kidney donor count by age. Count of deceased donors from whom at least one kidney was recovered for transplant.
Figure KI 38.
Deceased kidney donor count by HCV status. Count of deceased donors from whom at least one kidney was recovered for transplant. Donor HCV status was based on an antibody test.
Figure KI 42.
Distribution of deceased kidney donors by donor HCV status. Deceased donors from whom at least one kidney was recovered for transplant. Donor HCV status was based on an antibody test.
Figure KI 41.
Distribution of deceased kidney donors by race. Deceased donors from whom at least one kidney was recovered for transplant.
Figure KI 40.
Distribution of deceased kidney donors by sex. Deceased donors from whom at least one kidney was recovered for transplant.
Figure KI 39.
Distribution of deceased kidney donors by age. Deceased donors from whom at least one kidney was recovered for transplant.
Figure KI 43.
Cause of death among deceased kidney donors. Deceased donors with at least one kidney recovered for transplant. Each donor is counted once. CVA, cerebrovascular accident.
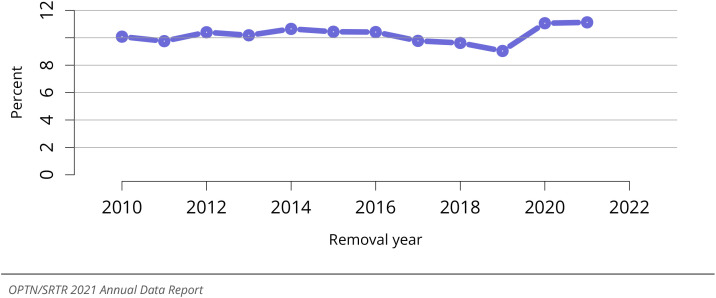
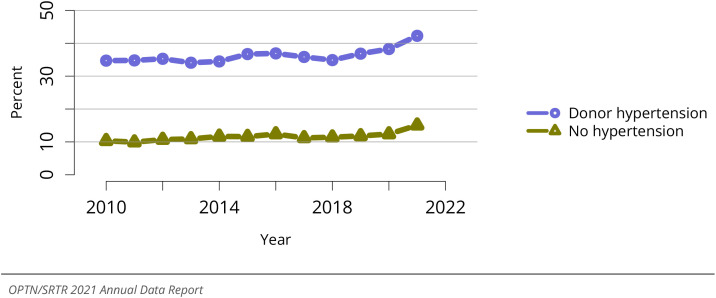
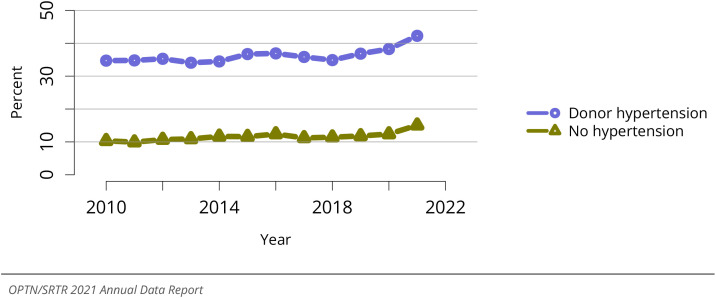
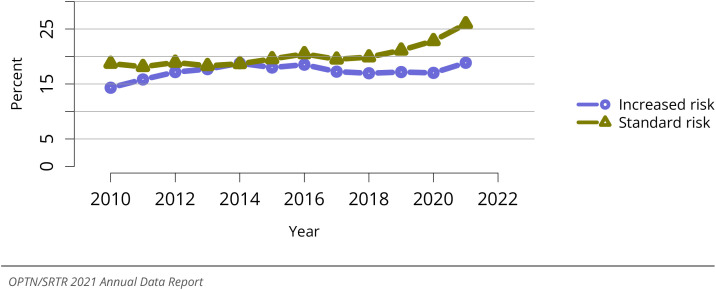
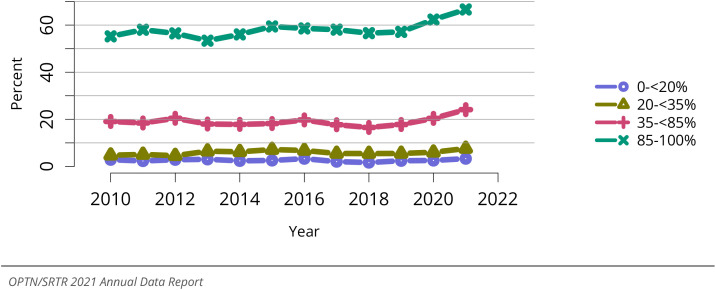
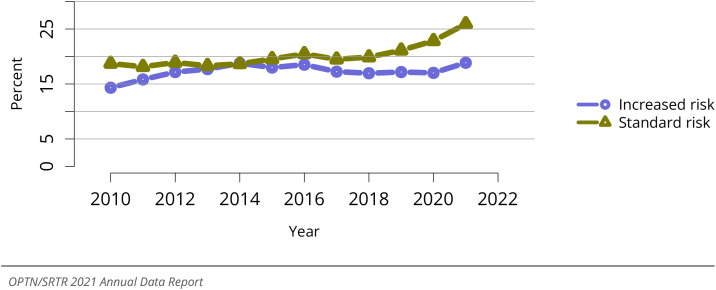
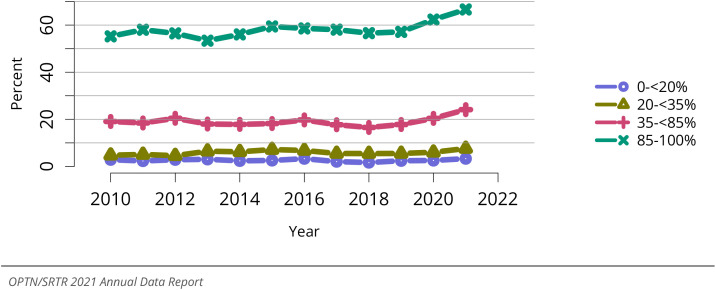
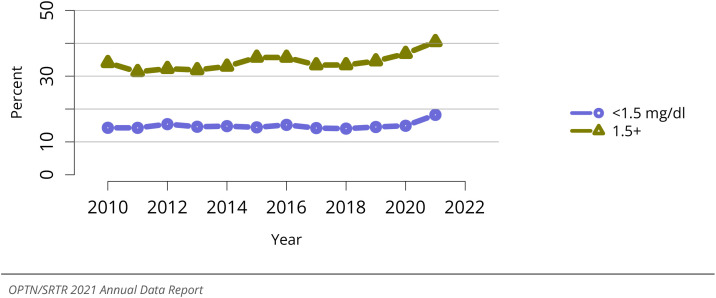
The proportion of deceased donor kidneys recovered but not transplanted (nonuse rate) rose to a high of 24.6% in 2021 compared with 17.9% in 2011, in the context of the COVID-19 pandemic and broader geographic organ distribution (Figure KI 44). Nonuse rates were highest for kidneys recovered from donors aged 55 years or older, reach- ing 51.1% in 2021 (Figure KI 45). The nonuse rate was also higher in kidneys recovered from donors with diabetes, hypertension, or elevated BMI (Figure KI 46, Figure KI 49, Figure KI 50). Racial disparity in kidney nonuse has diminished since 2016, although this is a result of increased nonuse of kidneys from White donors in 2021, rather than lower nonuse of kid- neys from non-White donors (Figure KI 48). Recovered kidneys from which biopsies were obtained continued to have rising nonuse rates, up to 35.9% in 2021 (Figure KI 52). The proportion of nonused kidneys recovered from HCV antibody–positive donors declined sharply from 2016 to 2020, but increased to 28.3% in 2021 (Figure KI 54). A lower pro- portion of kidneys from donors with increased infection risk as defined by the US Public Health Service guidelines were recovered for transplant but not transplanted than those from donors with standard infection risk in 2021 (18.9% vs 25.9%) (Figure KI 55), perhaps because kidneys with increased infection risk are often from younger donors, 2 and oth- erwise of high quality with low KDPI. In 2021, the nonuse rate of kidneys with KDPI of 85% or greater reached a high of 66.6% (Figure KI 57), while the nonuse rate of kidneys from donation after circulatory death (DCD) donors rose to 29.8% (Figure KI 56).
Figure KI 44.
Overall percent of kidneys recovered for transplant and not transplanted. Percentages of kidneys not transplanted out of all kidneys recovered for transplant.
Figure KI 45.
Percent of kidneys recovered for transplant and not transplanted by donor age. Per- centages of kidneys not transplanted out of all kidneys recovered for transplant.
Figure KI 46.
Percent of kidneys recovered for transplant and not transplanted by donor diabetes status. Percentages of kidneys not transplanted out of all kidneys recovered for transplant.
Figure KI 49.
Percent of kidneys recovered for transplant and not transplanted by donor hyperten- sion status. Percentages of kidneys not transplanted out of all kidneys recovered for transplant.
Figure KI 50.
Percent of kidneys recovered for transplant and not transplanted by donor BMI. Per- centages of kidneys not transplanted out of all kidneys recovered for transplant.
Figure KI 48.
Percent of kidneys recovered for transplant and not transplanted by donor race. Per- centages of kidneys not transplanted out of all kidneys recovered for transplant.
Figure KI 52.
Percent of kidneys recovered for transplant and not transplanted by donor biopsy status. Percentages of kidneys not transplanted out of all kidneys recovered for transplant. Kidneys are classified as biopsied if either of the donor’s kidneys was biopsied.
Figure KI 54.
Percent of kidneys recovered for transplant and not transplanted by donor HCV status. Percentages of kidneys not transplanted out of all kidneys recovered for transplant. Donor HCV status was based on an antibody test.
Figure KI 55.
Percent of kidneys recovered for transplant and not transplanted, by donor risk of dis- ease transmission. Percentages of kidneys not transplanted out of all kidneys recovered for transplant. “Increased risk” is defined by criteria from the US Public Health Service Guidelines for increased risk for HIV, hepatitis B, and hepatitis C transmission.
Figure KI 57.
Percent of kidneys recovered for transplant and not transplanted by KDPI. Percentages of kidneys not transplanted out of all kidneys recovered for transplant, by KDPI classification. Conversion of KDRI to KDPI is done using the OPTN KDPI Mapping Tables. For donors recovered January through May, the cohort 2 years prior was used to assign KDPI; for donors recovered June through December, the cohort 1 year prior was used to assign KDPI. KDPI, kidney donor profile index; KDRI, kidney donor risk index.
Figure KI 56.
Percent of kidneys recovered for transplant and not transplanted by DCD status. Per- centages of kidneys not transplanted out of all kidneys recovered for transplant. DBD, donation after brain death; DCD, donation after circulatory death.
2.3. Living Donation
Following a rise in the number of LDKTs from 2017 up to 6,855 in 2019, LKDTs decreased to 5,226 in 2020 during the COVID-19 pandemic, followed by partial recovery to 5,949 in 2021 with more widespread access to testing and use of vaccination (Figure KI 58). The largest increases in LDKT in 2021 compared with 2020 occurred among related and paired donors, while spousal donations declined (Figure KI 58). Of note, only a small pro- portion of the waiting list receives LDKTs each year, despite Health Resources and Ser- vices Administration initiatives to reduce financial barriers to living donation and Centers for Medicare & Medicaid Services initiatives to encourage early LDKT. 1 , 3 , 4
Figure KI 58.
Number of living kidney transplants by donor relation. As reported on the OPTN Living Donor Registration Form.
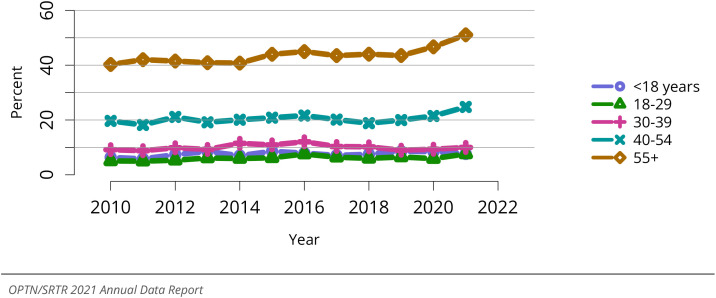
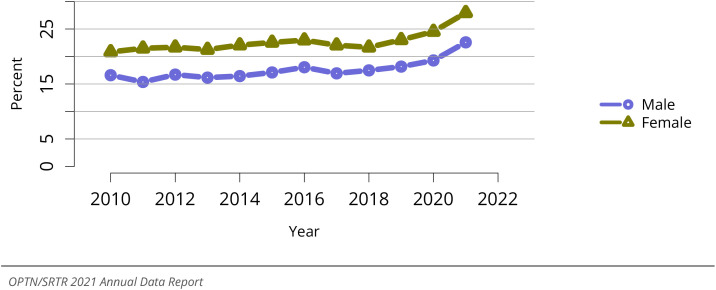
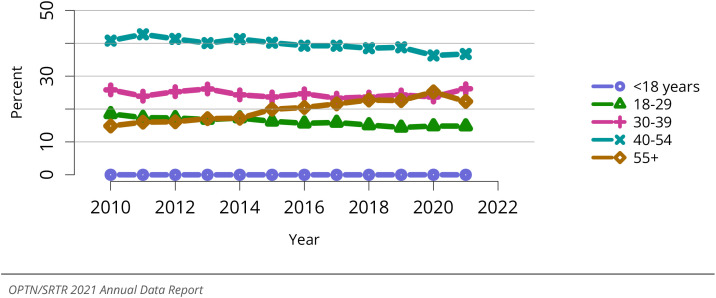
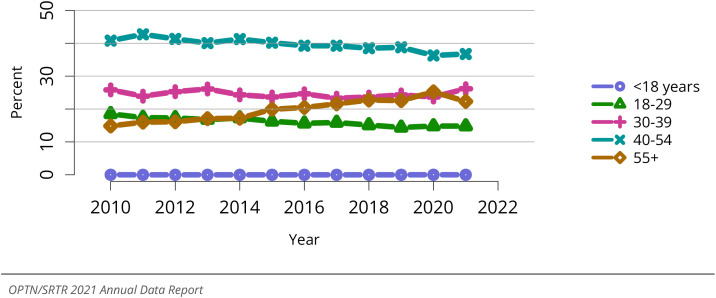
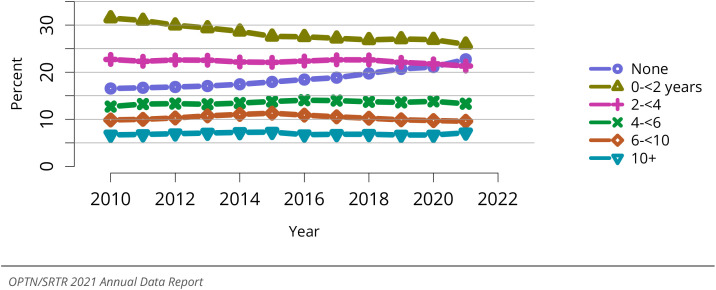
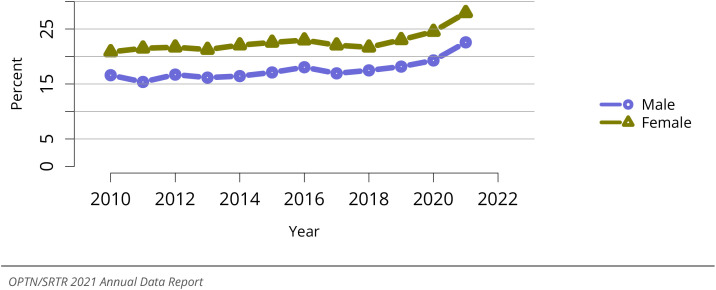
In 2021, the proportion of living donors aged 55 years or older declined slightly and the proportion aged 30-39 years rose slightly, while living donors aged 40-54 years con- tinued to make up the most common age group (Figure KI 59). In 2021, the proportion of living kidney donors who were women remained stably high, at 64.6% (Figure KI 60). The racial and ethnic composition of living donors in 2021 was relatively stable compared with 2020, with 70.1% White, 15.3% Hispanic, and 8.0% Black (Figure KI 61). Notably, this reflects a general decline in the proportion of Black living donors, from 12.0% in 2010 (Fig- ure KI 61). The proportion of living donors who were obese, based on BMI > 30 kg/m2, increased slightly to 23.8% (Figure KI 63). Most donation surgeries began as laparoscopic hand assisted (62.1%) or pure laparoscopy (36.8%) (Figure KI 62).
Figure KI 59.
Living kidney donors by age. As reported on the OPTN Living Donor Registration Form.
Figure KI 60.
Living kidney donors by sex. As reported on the OPTN Living Donor Registration Form.
Figure KI 61.
Living kidney donors by race. As reported on the OPTN Living Donor Registration Form.
Figure KI 63.
BMI among living kidney donors. Donor height and weight reported on the OPTN Living Donor Registration Form.
Figure KI 62.
Intended living kidney donor procedure type. As reported on the OPTN Living Donor Registration Form.
2.4. Transplants
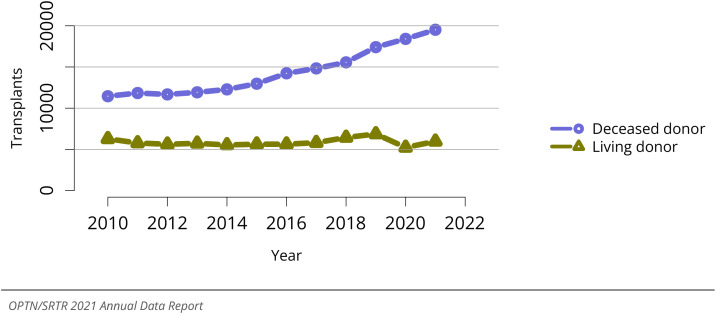
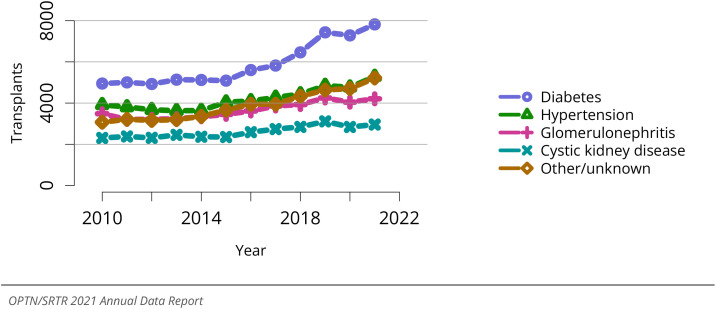
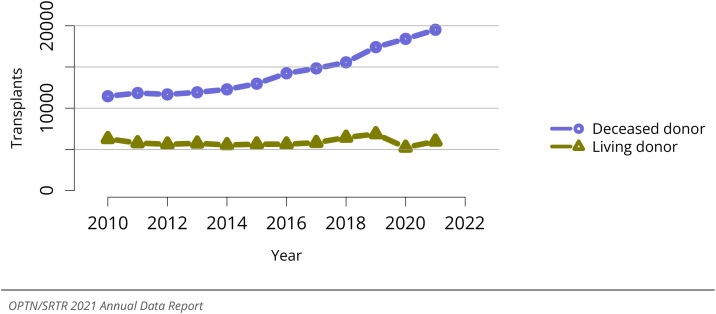
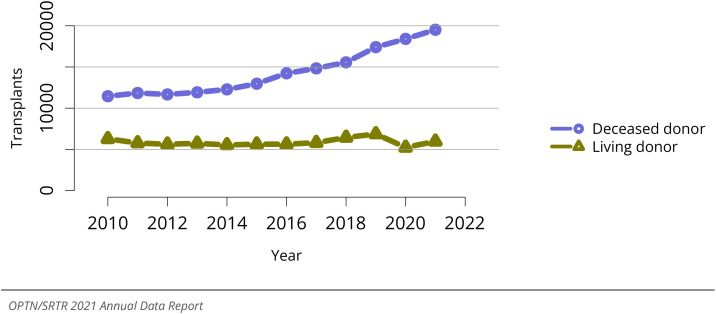
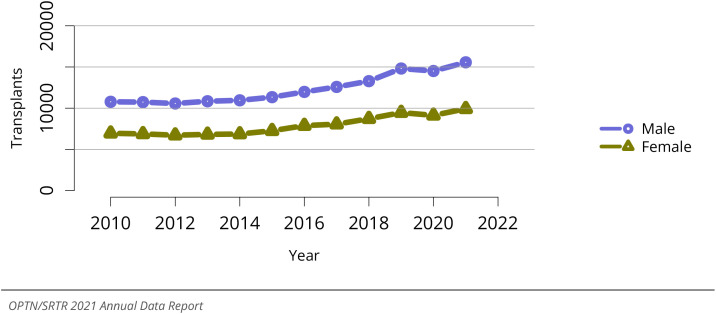
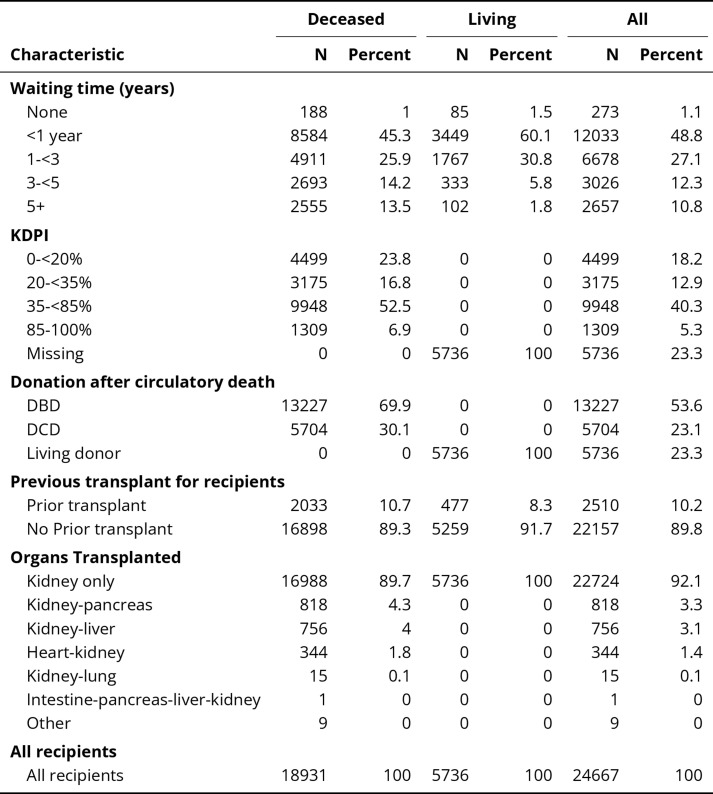
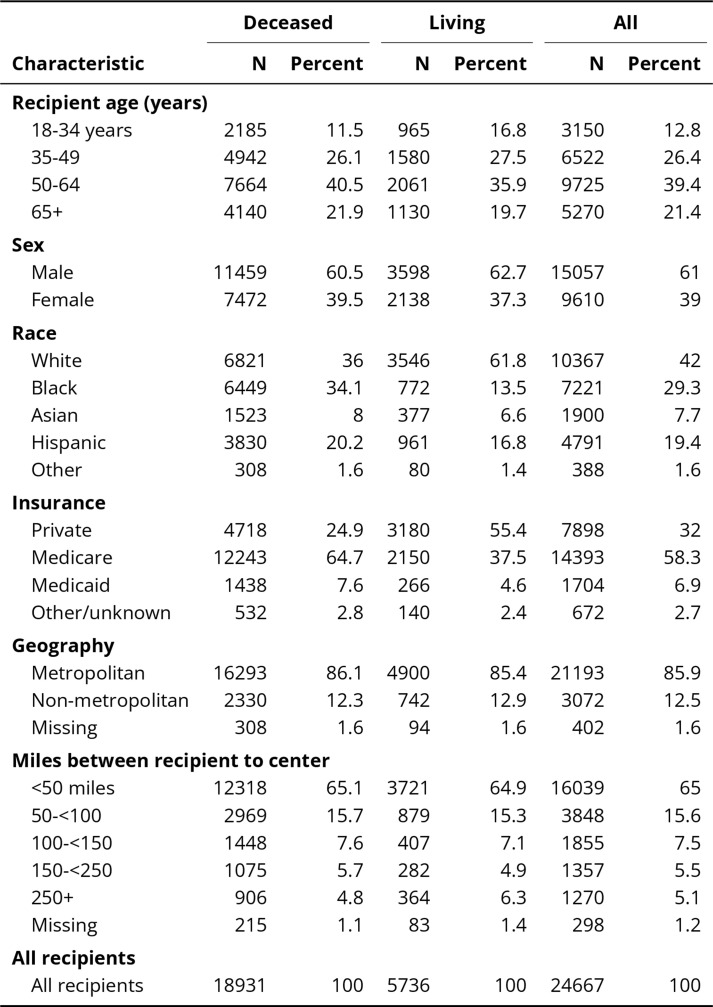
The upward trajectory in total kidney transplants was modestly slowed by the COVID-19 pandemic in 2020, then continued to rise in 2021, reaching a high of 25,487 (Figure KI 64). This trend was driven by growth in DDKT, which rose to 19,517 (Figure KI 65), pre- dominantly from donors with KDPI < 85%. In 2021, the proportion of DDKTs classified as KDPI <20% increased slightly to 23.8%, while proportions in other KDPI levels showed slight declines, with less than 7.0% of DDKTs from donors with KDPI of 85% or greater (Figure KI 70). Distributions of total kidney transplants in 2021 were similar to 2020 dis- tributions across recipient age, sex, and cause of kidney disease groups (Figure KI 66, Figure KI 67, Figure KI 69), while kidney transplant counts increased more among Black and Hispanic recipients compared with other racial and ethnic groups (Figure KI 68). In 2021, 89.3% of DDKTs and 91.7% of LDKTs were performed in first-time recipients (Table KI 8).
Figure KI 64.
Overall kidney transplants. All kidney transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Figure KI 65.
Total kidney transplants by donor type. All kidney transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Figure KI 70.
Kidney transplants by kidney donor profile index (KDPI). All adult recipients of deceased donor kidneys, including multiorgan transplants. Conversion of KDRI to KDPI is done using the OPTN KDPI Mapping Tables. For donors recovered January through May, the cohort 2 years prior was used to assign KDPI; for donors recovered June through December, the cohort 1 year prior was used to assign KDPI. Kidneys recovered en bloc are counted once. KDPI, kidney donor profile index; KDRI, kidney donor risk index.
Figure KI 66.
Total kidney transplants by age. All kidney transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Figure KI 67.
Total kidney transplants by sex. All kidney transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Figure KI 69.
Total kidney transplants by diagnosis. All kidney transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Figure KI 68.
Total kidney transplants by race. All kidney transplant recipients, including adult and pediatric, retransplant, and multiorgan recipients.
Table KI 8.
Transplant characteristics of adult kidney transplant recipients, 2021. Kidney transplant recipients, including retransplants. DBD, donation after brain death; DCD, donation after circulatory death; KDPI, kidney donor profile index. DCD status and KDPI scores apply to deceased donor transplants only.
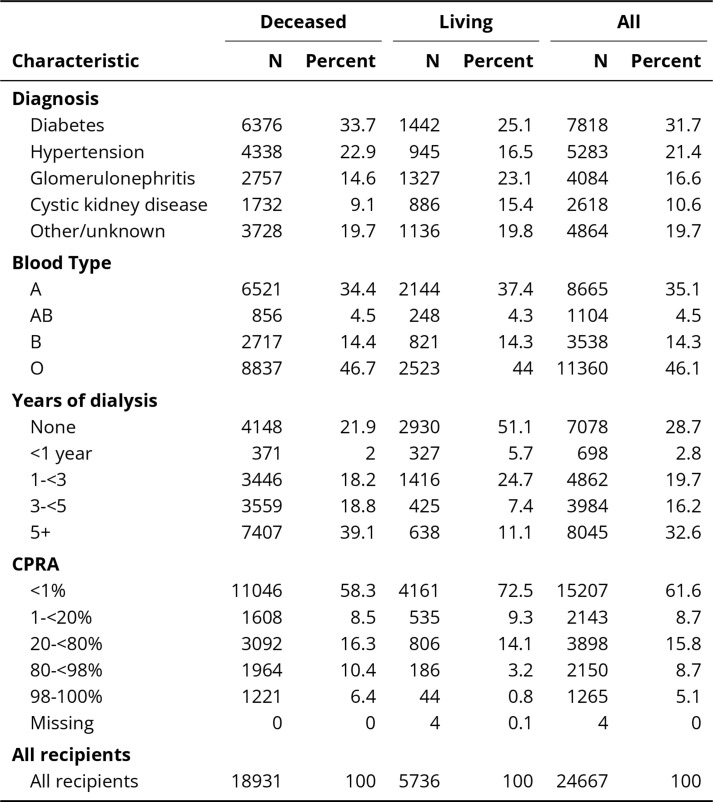
Disparities in access to LDKT persist. While 32.0% of waitlisted candidates as of De-cember 31, 2021, were Black (Table KI 1), Black patients constituted only 13.5% of LDKT recipients, versus 34.1% of DDKT recipients in 2021 (Table KI 6). White patients made up 35.8% of the waiting list (Table KI 1), while 61.8% of LDKT recipients and 36.0% of DDKT recipients were White (Table KI 6). Most LDKT recipients (55.4%) had private insurance at the time of transplant, compared with 24.9% of DDKT recipients (Table KI 6); 64.7% of DDKT recipients were Medicare beneficiaries (Table KI 6). LDKT recipients tended to have less dialysis time and lower cPRA levels than DDKT recipients (Table KI 7). Proportions of metropolitan and non-metropolitan place of residence and distance from transplant centers were similar among DDKT and LDKT recipients (Table KI 6) and similar to the pro- portions of these characteristics among waitlisted patients on December 31, 2021 (Table KI 1).
Table KI 1.
Demographic characteristics of adults on the kidney transplant waiting list on Decem- ber 31, 2011, December 31, 2016 and December 31, 2021. Candidates waiting for transplant on Decem- ber 31 of the given year, regardless of first listing date. Distance is computed from candidate’s home zip code to the transplant center. Age is determined on December 31 of the year.
| Characteristic | 2011 |
2016 |
2021 |
|||
|---|---|---|---|---|---|---|
| N | Percent | N | Percent | N | Percent | |
| Age (years) | ||||||
| 18-34 years | 9464 | 9.9 | 8841 | 8.5 | 7501 | 7.8 |
| 35-49 | 26429 | 27.7 | 26079 | 25 | 22415 | 23.3 |
| 50-64 | 41372 | 43.4 | 46099 | 44.2 | 41759 | 43.4 |
| 65+ | 18107 | 19 | 23310 | 22.3 | 24455 | 25.4 |
| Sex | ||||||
| Male | 56361 | 59.1 | 63583 | 60.9 | 59527 | 61.9 |
| Female | 39011 | 40.9 | 40746 | 39.1 | 36603 | 38.1 |
| Race | ||||||
| White | 36684 | 38.5 | 38273 | 36.7 | 34399 | 35.8 |
| Black | 32538 | 34.1 | 34772 | 33.3 | 30746 | 32 |
| Asian | 7400 | 7.8 | 9404 | 9 | 9566 | 10 |
| Hispanic | 17424 | 18.3 | 20246 | 19.4 | 19757 | 20.6 |
| Other | 1326 | 1.4 | 1634 | 1.6 | 1662 | 1.7 |
| Geography | ||||||
| Metropolitan | 81820 | 85.8 | 90668 | 86.9 | 83598 | 87 |
| Non-metropolitan | 12141 | 12.7 | 12494 | 12 | 11619 | 12.1 |
| Missing | 1411 | 1.5 | 1167 | 1.1 | 913 | 0.9 |
| Miles between candidate to center | ||||||
| <50 miles | 63494 | 66.6 | 68850 | 66 | 63318 | 65.9 |
| 50-<100 | 14226 | 14.9 | 15880 | 15.2 | 15250 | 15.9 |
| 100-<150 | 6822 | 7.2 | 7565 | 7.3 | 6565 | 6.8 |
| 150-<250 | 6234 | 6.5 | 6933 | 6.6 | 5785 | 6 |
| 250+ | 3784 | 4 | 4561 | 4.4 | 4766 | 5 |
| Missing | 812 | 0.9 | 540 | 0.5 | 446 | 0.5 |
| All candidates | ||||||
| All candidates | 95372 | 100 | 104329 | 100 | 96130 | 100 |
Table KI 6.
Demographic characteristics of adult kidney transplant recipients, 2021. Kidney trans- plant recipients, including retransplants. Distance is computed from recipient’s home zip code to the transplant center.
Table KI 7.
Clinical characteristics of adult kidney transplant recipients, 2021. Kidney transplant recipients, including retransplants.
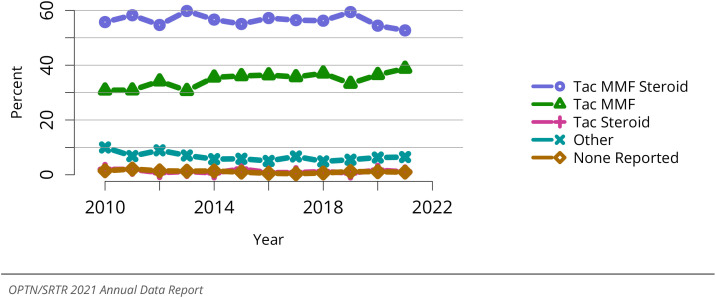
Induction immunosuppression was used in 91.3% of kidney transplants in 2021, a stable proportion compared with 2020 (Figure KI 71). Most patients received tacrolimus and mycophenolate mofetil (MMF)–based maintenance regimens at discharge, with triple therapy including steroids showing a slight increase to 67.5% in 2021, while use of tacrolimus-MMF (without reported steroid use) declined slightly to 25.6% (Figure KI 72). As noted previously, the proportion of DDKTs in recipients with peak cPRA levels of 98%-100% increased sharply after the 2014 KAS revision and then gradually declined, from 12.5% in 2015 to 6.3% in 2020, and remained stable at 6.4% in 2021 (Figure KI 73). Following the March 2021 KAS250 revision, there was an increase in the proportion of DDKTs in recipients with cPRA of 80%-98%, from 7.0% in 2020 to 10.4% in 2021 (Figure KI 73). By comparison, only 0.8% of LDKT recipients in 2021 had peak cPRA levels of 98%-100%, while most (72.5%) LDKT recipients had peak cPRA levels <1% (Figure KI 74).
Figure KI 71.
Induction agent use in adult kidney transplant recipients. Immunosuppression at trans- plant reported to the OPTN.
Figure KI 72.
Immunosuppression regimen use in adult kidney transplant recipients. Immunosup- pression regimen at transplant reported to the OPTN. Tac, tacrolimus. MMF, all mycophenolate agents.
Figure KI 73.
Peak cPRA at time of kidney transplant in adult deceased donor recipients. Peak cPRA is used.
Figure KI 74.
Peak cPRA at time of kidney transplant in adult living donor recipients. Peak cPRA is used.
2.5. Outcomes
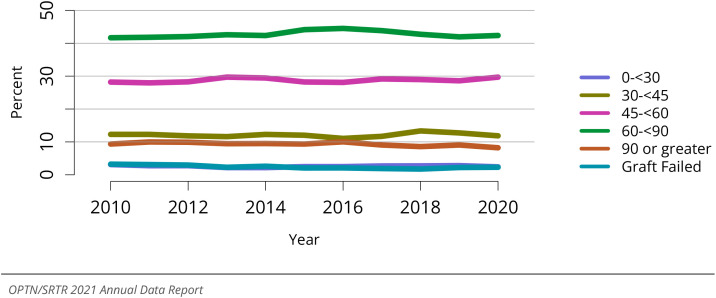
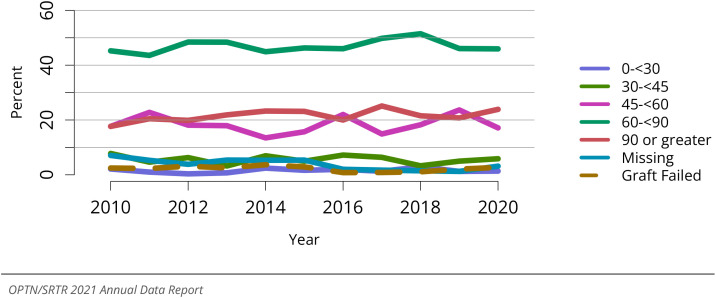
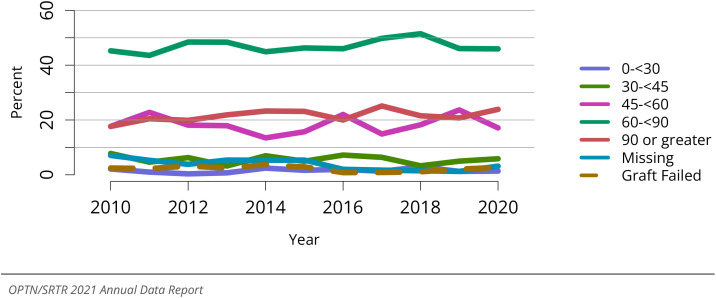
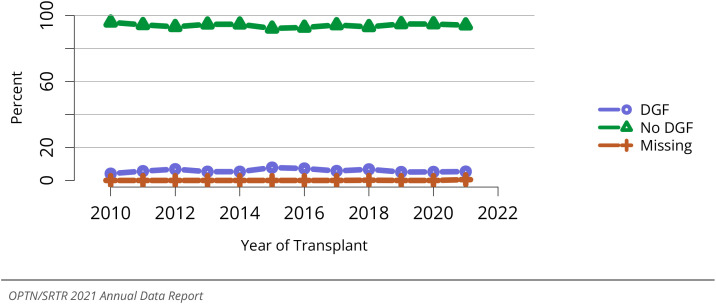
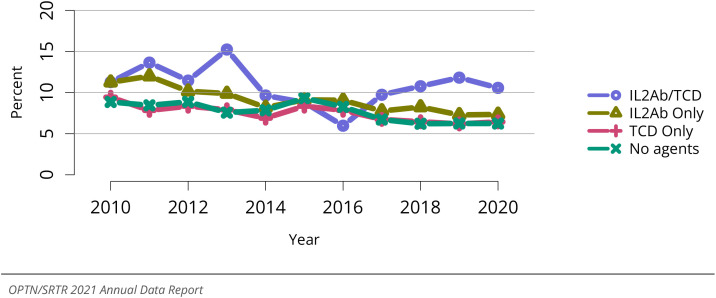
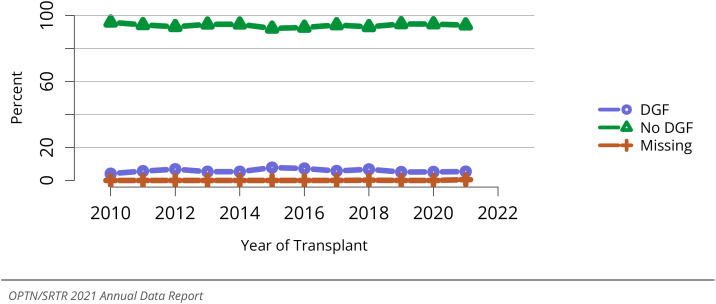
Delayed graft function, defined as dialysis within the first 7 days posttransplant, has trended up over the past decade, occurring in 24% of kidney recipients in 2021 (Figure KI 76). Estimated glomerular filtration rate (eGFR) at 12 months, calculated using the 2021 race-free Chronic Kidney Disease–Epidemiology Collaboration creatinine-based equation, an early surrogate allograft outcome, was 45 mL/min/1.73 m2 or higher for 64.1% of DDKT recipients in 2020, reflecting a downtrend from 67.8% in 2016 (Figure KI 88). Among LDKT recipients, 80.3% had 12-month eGFR of 45 mL/min/1.73 m2 or higher in 2020, a slight decline from 82.6% in 2016 (Figure KI 89). For transplants performed in 2020, acute rejection by 1 year was highest in recipients aged 18-34 years at 9.3% and lowest in recipients aged 65 years or older at 5.3% (Figure KI 90). Acute rejection at 1 year occurred in 10.6% of those who received combined interleukin 2 (IL-2) recep-tor antibody with T-cell–depleting induction, compared with 7.3% who received only IL-2 receptor antibody, 6.4% who received only T-cell–depleting induction, and 6.2% of the small subgroup whose transplants were managed without induction (Figure KI 91).
Figure KI 76.
Delayed graft function among adult kidney transplant recipients. All adult recipients of kidneys. Delayed graft function is defined as dialysis administered within the first seven days posttrans- plant.
Figure KI 88.
Distribution of eGFR at 12 months posttransplant among adult deceased donor kidney transplant recipients. GFR (mL/min/1.73 m2) estimated using the Chronic Kidney Disease Epidemiology Collaboration equation, and computed by SRTR for patients alive with graft function at 12 months post- transplant.
Figure KI 89.
Distribution of eGFR at 12 months posttransplant among adult living donor kidney transplant recipients. GFR (mL/min/1.73 m2) estimated using the Chronic Kidney Disease Epidemiology Collaboration equation, and computed by SRTR for patients alive with graft function at 12 months post- transplant.
Figure KI 90.
Incidence of acute rejection by 1 year posttransplant among adult kidney transplant recipients by age. Only the first reported rejection event is counted. Cumulative incidence is estimated using the Kaplan-Meier method.
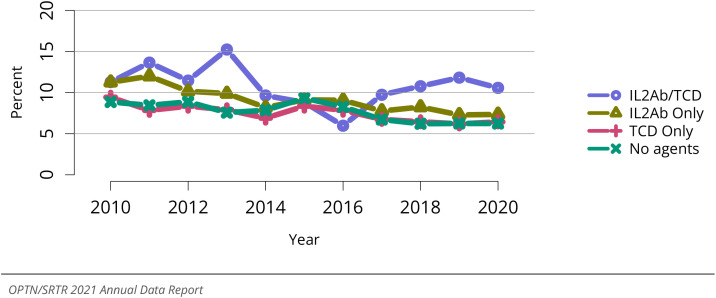
Figure KI 91.
Incidence of acute rejection by 1 year posttransplant among adult kidney transplant recipients by induction agent. Only the first reported rejection event is counted. Cumulative incidence is estimated using the Kaplan-Meier method. IL2Ab, interleukin 2 receptor antibody; TCD, T-cell depleting.
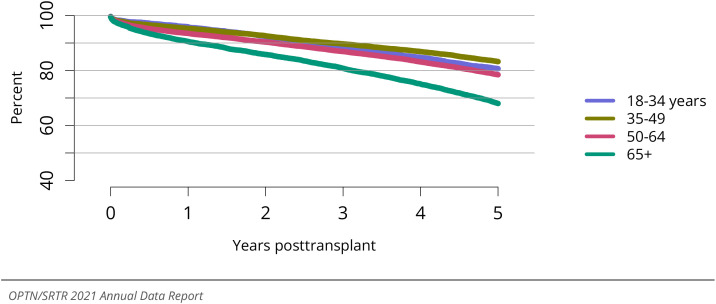
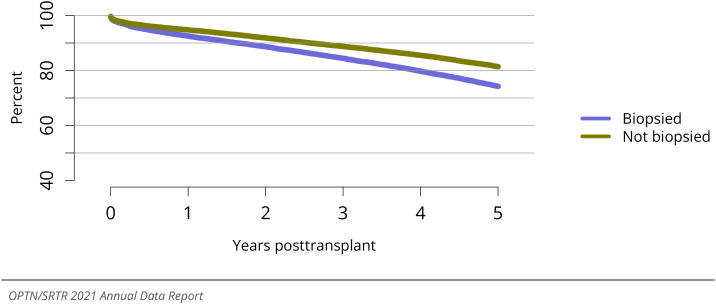
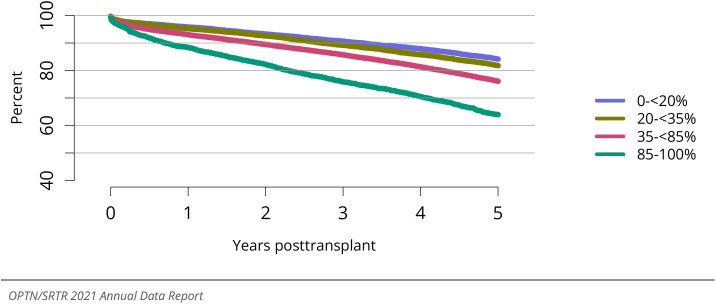
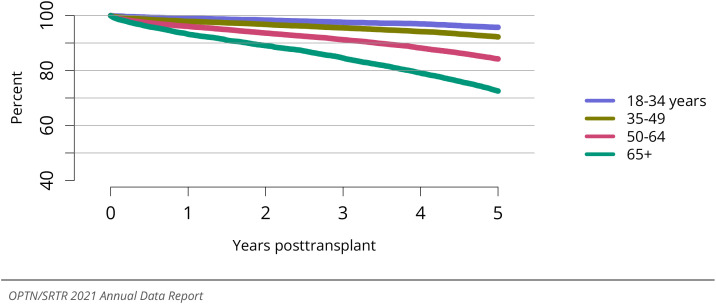
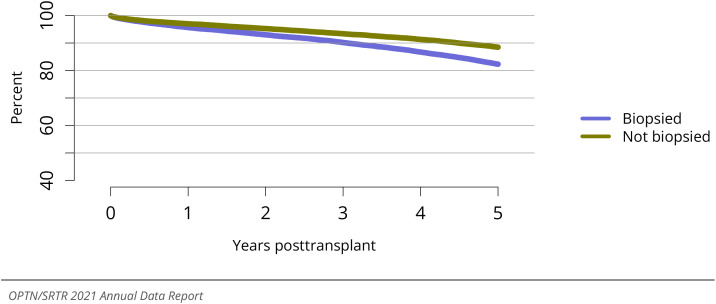
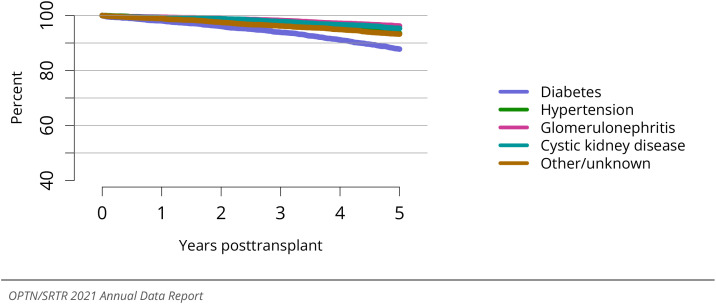
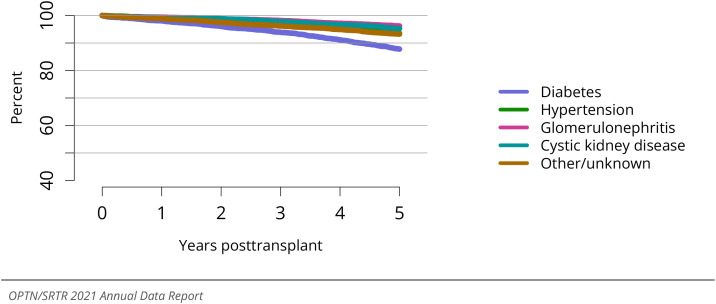
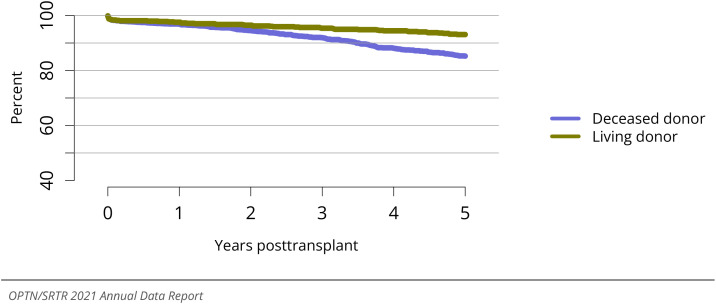
Among DDKTs, 5-year graft survival was lowest among older (vs younger) recipients, with 68.0% graft survival at 5 years among recipients aged 65 years and older compared with 80.7% graft survival at 5 years among recipients aged 18-34 years (Figure KI 77). Graft survival was also lower among recipients with diabetes as the cause of kidney fail- ure (vs other causes; Figure KI 78), and recipients with BMI of 35 kg/m2 or higher (vs BMI 18.5 to <25 kg/m2; Figure KI 82). Five-year DDKT graft survival was 64.0% for allo- grafts with KDPI of 85% or greater, compared with 84.2%, 81.8%, and 76.1% for those with KDPI <20%, KDPI 20%-35%, and KDPI 35%-<85%, respectively (Figure KI 79). Five- year graft survival did not differ for DCD transplants compared with donation after brain death transplants (Figure KI 80). Graft survival was lower after transplant of kidneys that underwent a procurement biopsy (Figure KI 81), although the utility of procurement biopsy in informing appropriate organ use warrants further consideration.5
Figure KI 77.
Graft survival among adult deceased donor kidney transplant recipients, 2014-2016, by age. Graft survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 78.
Graft survival among adult deceased donor kidney transplant recipients, 2014-2016, by diagnosis. Graft survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 82.
Graft survival among adult deceased donor kidney transplant recipients, 2014-2016, by BMI. Graft survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 79.
Graft survival among adult deceased donor kidney transplant recipients, 2014-2016, by KDPI. Graft survival estimated using unadjusted Kaplan-Meier methods. Conversion of KDRI to KDPI is done using the OPTN KDPI Mapping Tables. For donors recovered January through May, the cohort 2 years prior was used to assign KDPI; for donors recovered June through December, the cohort 1 year prior was used to assign KDPI. KDPI, kidney donor profile index.
Figure KI 80.
Graft survival among adult deceased donor kidney transplant recipients, 2014-2016, by DCD status. Graft survival estimated using unadjusted Kaplan-Meier methods. DCD, donation after circulatory death; DBD, donation after brain death.
Figure KI 81.
Graft survival among adult deceased donor kidney transplant recipients, 2014-2016, by biopsy status. Graft survival estimated using unadjusted Kaplan-Meier methods. Kidneys are classified as biopsied if either of the donor’s kidneys was biopsied.
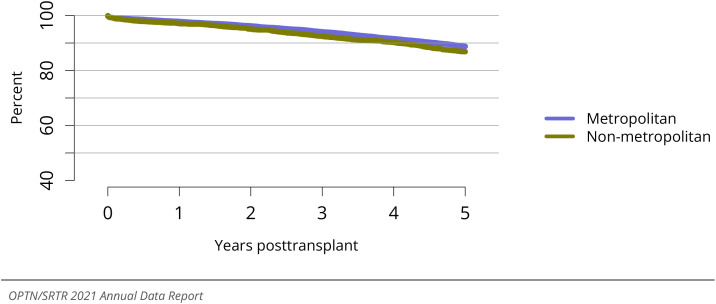
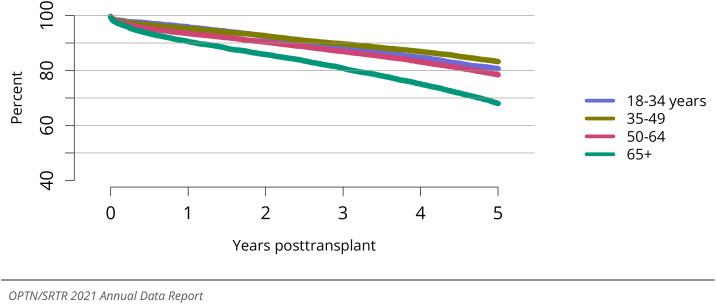
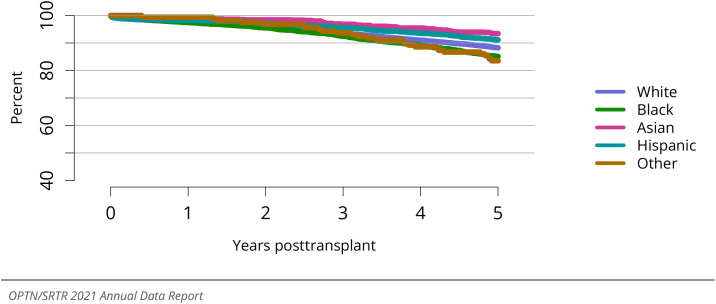
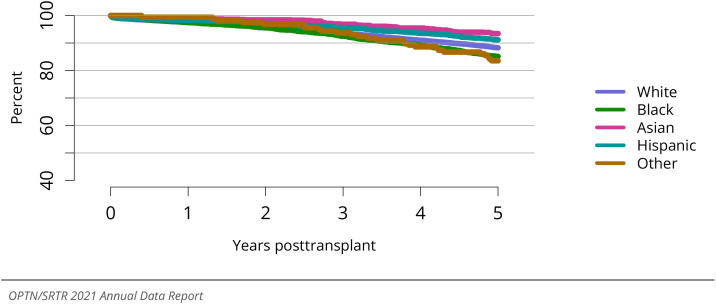
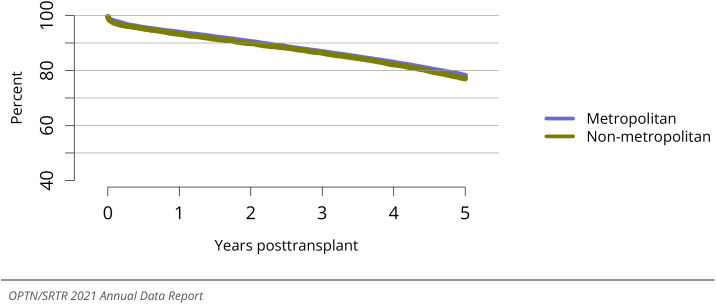
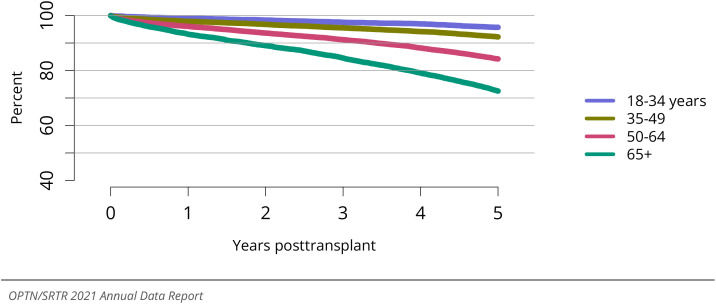
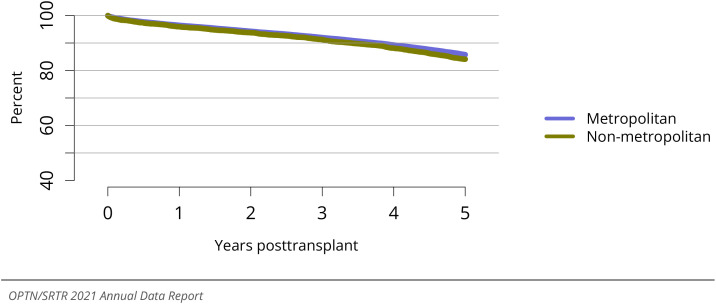
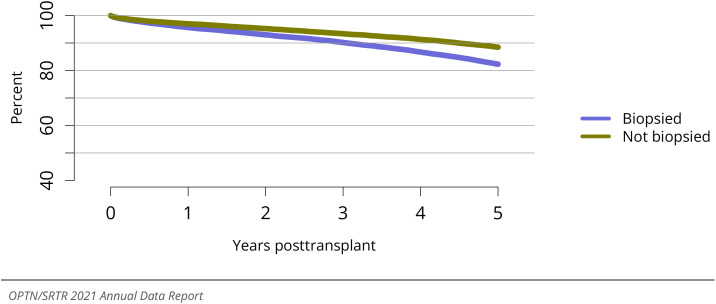
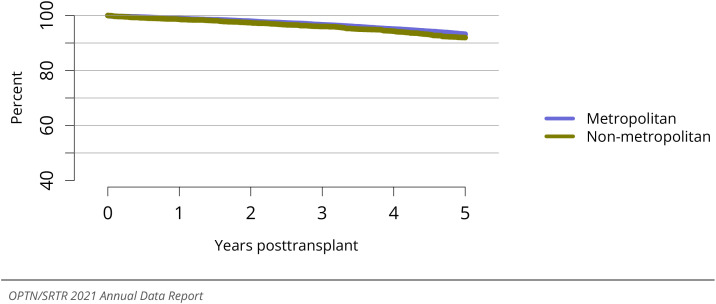
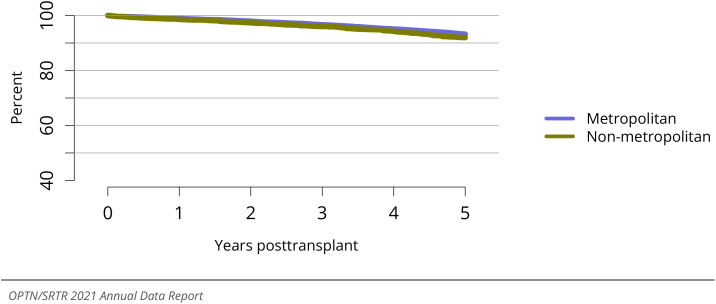
Among LDKTs, 5-year graft survival was 82.1% in recipients aged 65 years or older, compared with 88.6% in recipients aged 18-34 years (Figure KI 84), and was lower in recipients with diabetic kidney failure compared with those with other disease causes (Figure KI 86). Five-year LDKT survival was highest among Asian recipients and lowest among Black recipients and recipients of other races (Figure KI 85). Graft survival was slightly lower in recipients who resided in non-metropolitan compared with metropolitan zip codes (Figure KI 83, Figure KI 87).
Figure KI 84.
Graft survival among adult living donor kidney transplant recipients, 2014-2016, by age. Graft survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 86.
Graft survival among adult living donor kidney transplant recipients, 2014-2016, by diagnosis. Graft survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 85.
Graft survival among adult living donor kidney transplant recipients, 2014-2016, by race. Graft survival estimated using unadjusted Kaplan-Meier methods.
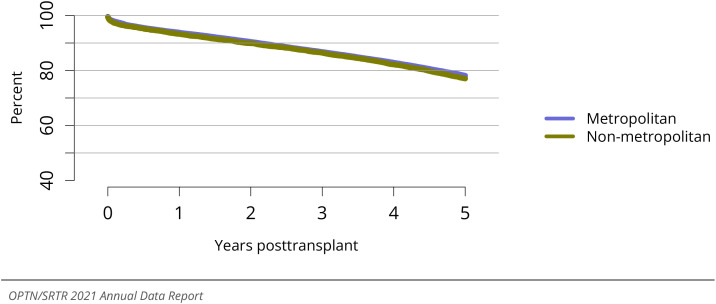
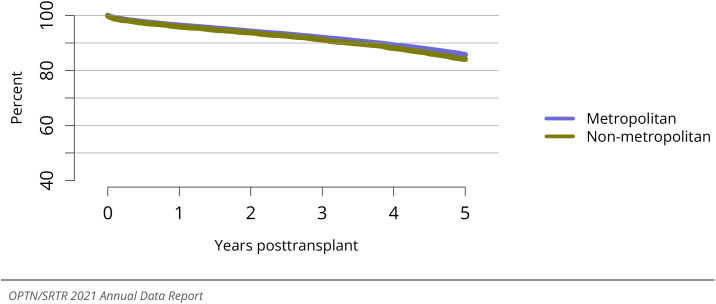
Figure KI 83.
Graft survival among adult deceased donor kidney transplant recipients, 2014-2016, by metropolitan vs. non-metropolitan recipient residence. Graft survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 87.
Graft survival among adult living donor kidney transplant recipients, 2014-2016, by metropolitan vs. non-metropolitan recipient residence. Graft survival estimated using unadjusted Kaplan-Meier methods.
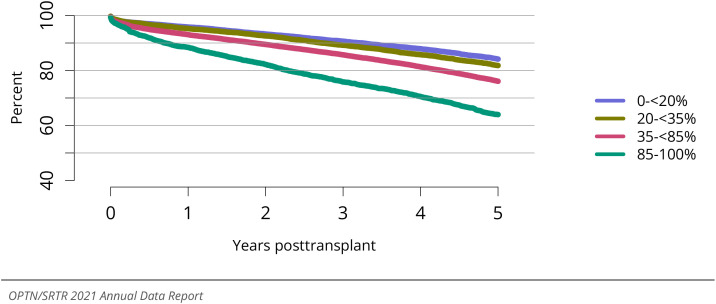
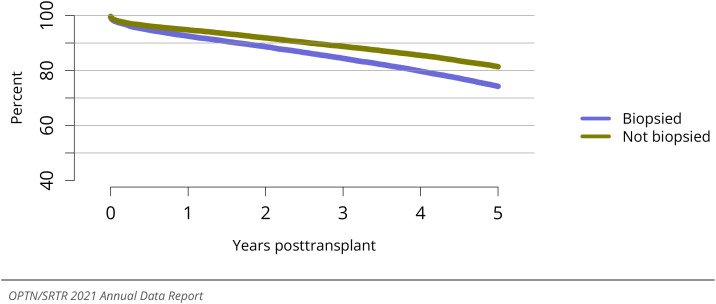
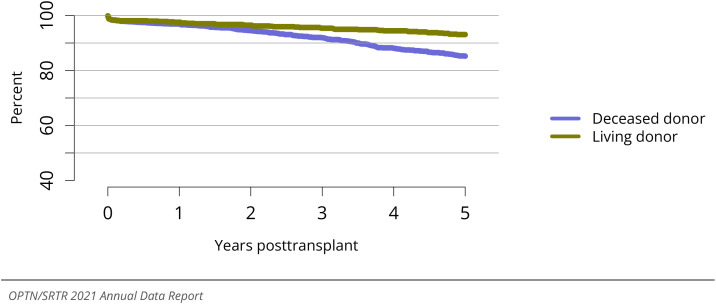
Trends in adult posttransplant patient survival generally paralleled patterns of graft survival (Figure KI 93, Figure KI 94, Figure KI 95, Figure KI 96, Figure KI 97, Figure KI 98, Figure KI 99, Figure KI 100, Figure KI 101). Five years posttransplant, 72.5% of DDKT recipients and 84.4% of LDKT recipients aged 65 years or older were alive, compared with 95.7% and 97.6% of those aged 18-34 years, respectively (Figure KI 93, Figure KI 98). Five-year patient survival was lowest among recipients with diabetes as the cause of kidney disease, at 79.5% for DDKT recipients with diabetes and 87.8% for LDKT recipients with diabetes (Figure KI 94, Figure KI 99). Patient survival was also lower among DDKT recipients who received kidneys with KPDI of 85% or greater and grafts that had undergone a procurement biopsy (Figure KI 96, Figure KI 97). Patient survival was slightly lower in recipients who resided in non-metropolitan compared with metropolitan zip codes (Figure KI 95, Figure KI 101).
Figure KI 93.
Patient survival among adult deceased donor kidney transplant recipients, 2014-2016, by age. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 94.
Patient survival among adult deceased donor kidney transplant recipients, 2014-2016, by diagnosis. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 95.
Patient survival among adult deceased donor kidney transplant recipients, 2014-2016, by metropolitan vs. non-metropolitan recipient residence. Patient survival estimated using unad- justed Kaplan-Meier methods.
Figure KI 96.
Patient survival among adult deceased donor kidney transplant recipients, 2014-2016, by KDPI. Patient survival estimated using unadjusted Kaplan-Meier methods. Conversion of KDRI to KDPI is done using the OPTN KDPI Mapping Tables. For donors recovered January through May, the cohort 2 years prior was used to assign KDPI; for donors recovered June through December, the cohort 1 year prior was used to assign KDPI. KDPI, kidney donor profile index.
Figure KI 97.
Patient survival among adult deceased donor kidney transplant recipients, 2014-2016, by biopsy status. Patient survival estimated using unadjusted Kaplan-Meier methods. Kidneys are clas- sified as biopsied if either of the donor’s kidneys was biopsied.
Figure KI 98.
Patient survival among adult living donor kidney transplant recipients, 2014-2016, by age. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 99.
Patient survival among adult living donor kidney transplant recipients, 2014-2016, by diagnosis. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 100.
Patient survival among adult living donor kidney transplant recipients, 2014-2016, by race. Patient survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 101.
Patient survival among adult living donor kidney transplant recipients, 2014-2016, by metropolitan vs. non-metropolitan recipient residence. Patient survival estimated using unadjusted Kaplan-Meier methods.
3. Pediatric Kidney Transplant
3.1. Waiting List
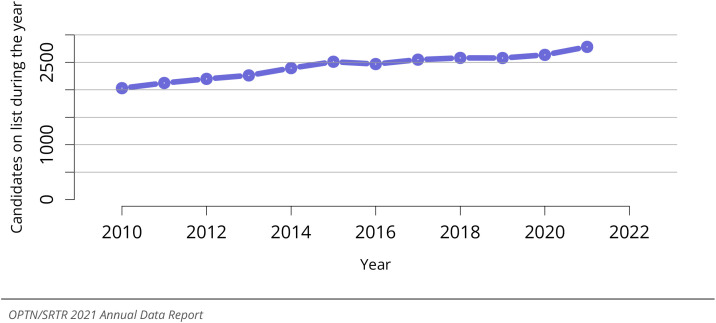
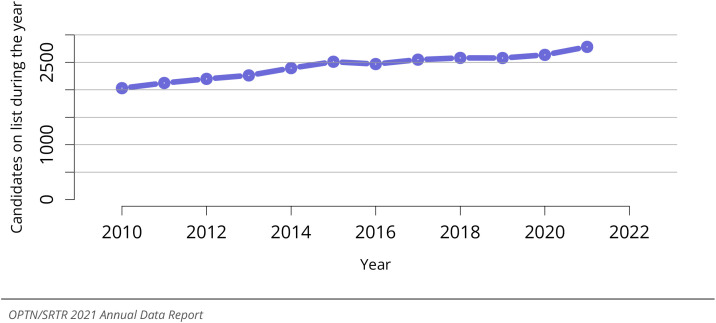
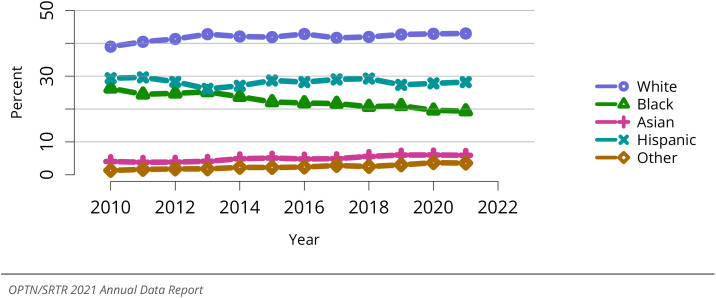
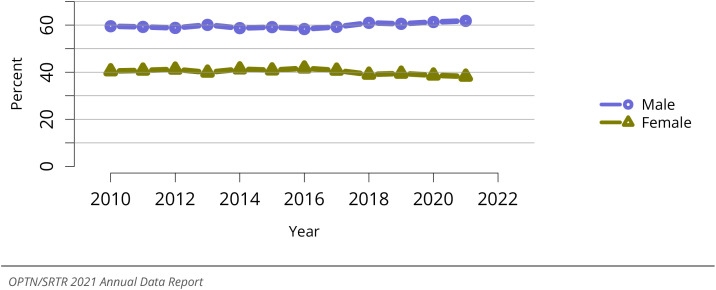
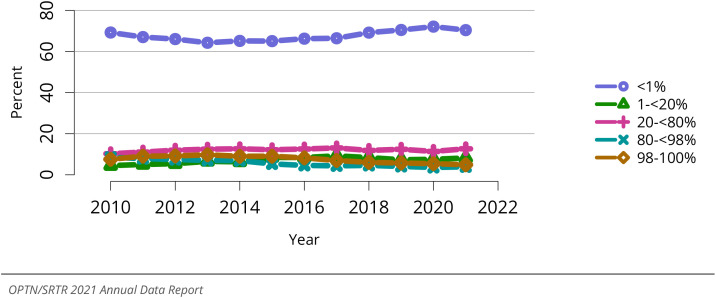
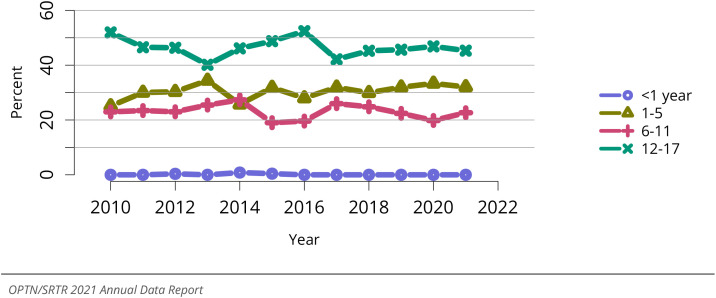
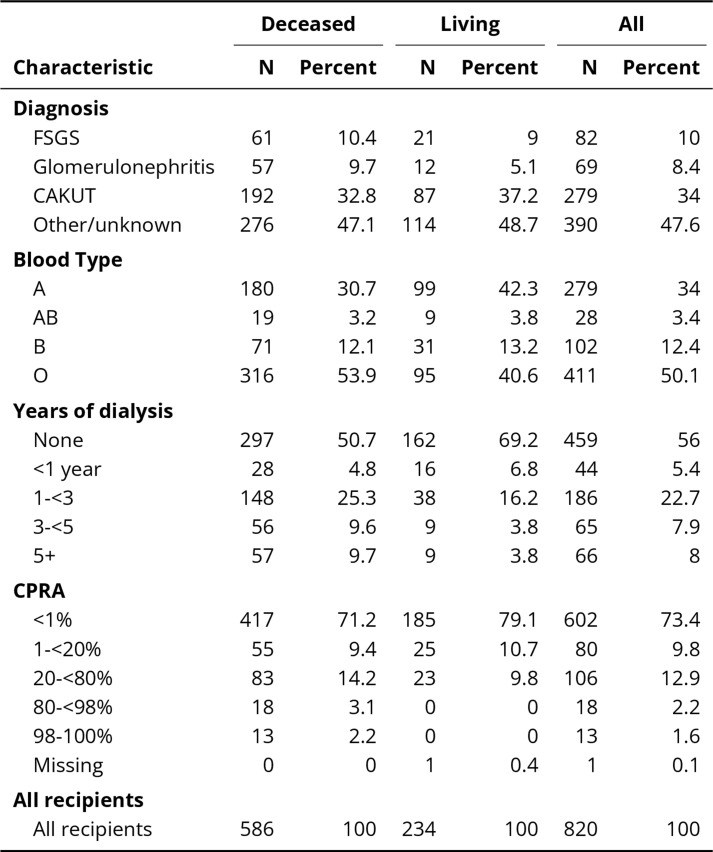
In 2021, 1,087 pediatric candidates were added to the kidney transplant waiting list (Fig- ure KI 102). The number of prevalent pediatric candidates (listed before age 18 years) continues to increase, reaching 2,782 in 2021 (Figure KI 103). By age, candidates aged 12 years and older accounted for the largest proportion of those waiting, at 67.3%, com- pared with those aged 6-11 years at 17.7%, 1-5 years at 14.9%, and younger than 1 year at 0.07% (Figure KI 104). In terms of race and ethnicity, White candidates accounted for the largest group (43.0%) on the kidney transplant waiting list followed by Hispanic (28.2%), Black (19.4%), and Asian candidates (5.9%) (Figure KI 105). Over the past decade, the age, sex, and geographic location of transplant candidates have remained largely un- changed (Table KI 11). The proportion of Black candidates decreased since 2011 (Table KI 11). The proportion of candidates with congenital anomalies of the kidney and urinary tract as primary cause of disease continues to increase, from 27.9% in 2011 to 35.9% in 2021, and the proportions with glomerulonephritis and focal segmental glomeruloscle- rosis decreased (Table KI 12). Most pediatric candidates (69.1%) waiting as of December 31, 2021, had a cPRA level less than 1% (Table KI 12). The proportion of pediatric can- didates waiting for retransplant decreased over the past decade from 32.5% in 2011 to 18.1% in 2021 (Table KI 13).
Figure KI 102.
New pediatric candidates added to the kidney transplant waiting list. A new candi- date is one who first joined the list during the given year, without having been listed in a previous year. Previously listed candidates who underwent transplant and subsequently relisted are considered new. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure KI 103.
All pediatric candidates on the kidney transplant waiting list. Candidates listed at more than one center are counted once per listing; age determined at first listing.
Figure KI 104.
Distribution of pediatric candidates waiting for kidney transplant by age. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive candidates are included. Age is determined at the earliest of transplant, death, removal, or December 31 of the year.
Figure KI 105.
Distribution of pediatric candidates waiting for kidney transplant by race. Candidates waiting for transplant any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive candidates are included.
Table KI 11.
Demographic characteristics of pediatric candidates on the kidney transplant waiting list on December 31, 2011, December 31, 2016, and December 31, 2021. Candidates aged younger than 18 years at listing waiting for transplant on December 31 of the given year, regardless of first listing date. Age is determined on December 31 of the year. Distance is computed from candidate’s home zip code to the transplant center.
| Characteristic | 2011 |
2016 |
2021 |
|||
|---|---|---|---|---|---|---|
| N | Percent | N | Percent | N | Percent | |
| Age (years) | ||||||
| 1-5 | 182 | 14.5 | 246 | 16.8 | 216 | 12.7 |
| 6-11 | 194 | 15.5 | 253 | 17.3 | 291 | 17.1 |
| 12-17 | 470 | 37.5 | 494 | 33.7 | 575 | 33.9 |
| 18+ | 409 | 32.6 | 472 | 32.2 | 614 | 36.2 |
| <1 year | 0 | 0 | 1 | 0.1 | 2 | 0.1 |
| Sex | ||||||
| Male | 741 | 59 | 880 | 60 | 1054 | 62.1 |
| Female | 514 | 41 | 586 | 40 | 644 | 37.9 |
| Race | ||||||
| White | 487 | 38.8 | 571 | 38.9 | 709 | 41.8 |
| Black | 329 | 26.2 | 350 | 23.9 | 353 | 20.8 |
| Asian | 45 | 3.6 | 72 | 4.9 | 108 | 6.4 |
| Hispanic | 375 | 29.9 | 438 | 29.9 | 467 | 27.5 |
| Other | 19 | 1.5 | 35 | 2.4 | 61 | 3.6 |
| Geography | ||||||
| Metropolitan | 1054 | 84 | 1259 | 85.9 | 1482 | 87.3 |
| Non-metropolitan | 181 | 14.4 | 191 | 13 | 204 | 12 |
| Missing | 20 | 1.6 | 16 | 1.1 | 12 | 0.7 |
| Miles between candidate to center | ||||||
| <50 miles | 786 | 62.6 | 935 | 63.8 | 1105 | 65.1 |
| 50-<100 | 217 | 17.3 | 227 | 15.5 | 278 | 16.4 |
| 100-<150 | 101 | 8 | 114 | 7.8 | 108 | 6.4 |
| 150-<250 | 86 | 6.9 | 109 | 7.4 | 114 | 6.7 |
| 250+ | 47 | 3.7 | 69 | 4.7 | 85 | 5 |
| Missing | 18 | 1.4 | 12 | 0.8 | 8 | 0.5 |
| All candidates | ||||||
| All candidates | 1255 | 100 | 1466 | 100 | 1698 | 100 |
Table KI 12.
Clinical characteristics of pediatric candidates on the kidney transplant waiting list on December 31, 2011, December 31, 2016, and December 31, 2021. Candidates aged younger than 18 years at listing waiting for transplant on December 31 of the given year, regardless of first listing date. FSGS, focal segmental glomerulosclerosis; GN, glomerulonephritis; CAKUT, congenital anomalies of the kidney and urinary tract.
| Characteristic | 2011 |
2016 |
2021 |
|||
|---|---|---|---|---|---|---|
| N | Percent | N | Percent | N | Percent | |
| Pediatric diagnosis | ||||||
| FSGS | 165 | 13.1 | 182 | 12.4 | 162 | 9.5 |
| Glomerulonephritis | 144 | 11.5 | 131 | 8.9 | 127 | 7.5 |
| CAKUT | 350 | 27.9 | 512 | 34.9 | 610 | 35.9 |
| Other/unknown | 596 | 47.5 | 640 | 43.7 | 799 | 47.1 |
| Blood Type | ||||||
| A | 384 | 30.6 | 421 | 28.7 | 572 | 33.7 |
| AB | 45 | 3.6 | 35 | 2.4 | 53 | 3.1 |
| B | 211 | 16.8 | 241 | 16.4 | 240 | 14.1 |
| O | 615 | 49 | 769 | 52.5 | 833 | 49.1 |
| CPRA | ||||||
| <1% | 784 | 62.5 | 926 | 63.2 | 1174 | 69.1 |
| 1-<20% | 44 | 3.5 | 126 | 8.6 | 133 | 7.8 |
| 20-<80% | 140 | 11.2 | 186 | 12.7 | 206 | 12.1 |
| 80-<98% | 123 | 9.8 | 79 | 5.4 | 80 | 4.7 |
| 98-100% | 164 | 13.1 | 149 | 10.2 | 105 | 6.2 |
| All candidates | ||||||
| All candidates | 1255 | 100 | 1466 | 100 | 1698 | 100 |
Table KI 13.
Listing characteristics of pediatric candidates on the kidney transplant waiting list on December 31, 2011, December 31, 2016, and December 31, 2021. Candidates aged younger than 18 years at listing waiting for transplant on December 31 of the given year, regardless of first listing date.
| Characteristic | 2011 |
2016 |
2021 |
|||
|---|---|---|---|---|---|---|
| N | Percent | N | Percent | N | Percent | |
| Waiting time (years) | ||||||
| <1 year | 577 | 46 | 607 | 41.4 | 679 | 40 |
| 1-<2 | 239 | 19 | 307 | 20.9 | 323 | 19 |
| 2-<3 | 117 | 9.3 | 192 | 13.1 | 195 | 11.5 |
| 3-<5 | 164 | 13.1 | 197 | 13.4 | 260 | 15.3 |
| 5+ | 158 | 12.6 | 163 | 11.1 | 241 | 14.2 |
| Previous transplant | ||||||
| No prior transplant | 847 | 67.5 | 1132 | 77.2 | 1390 | 81.9 |
| Prior transplant | 408 | 32.5 | 334 | 22.8 | 308 | 18.1 |
| All candidates | ||||||
| All candidates | 1255 | 100 | 1466 | 100 | 1698 | 100 |
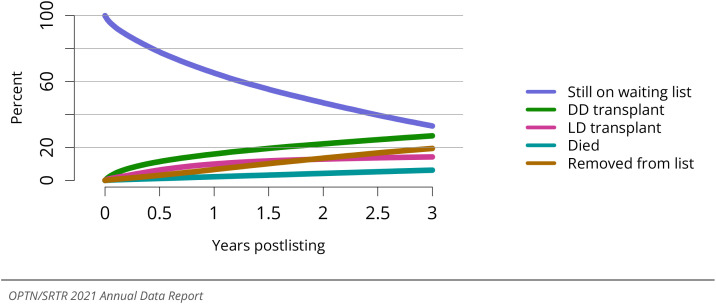
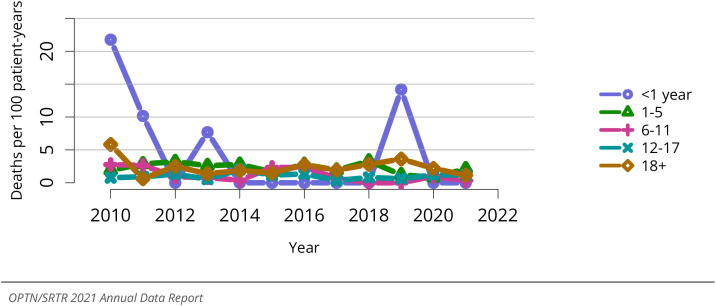
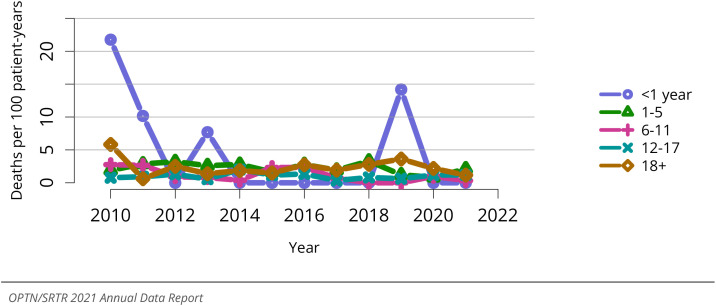
The distribution of waiting time among pediatric candidates on the waiting list has remained similar over the past decade, with almost 50% of pediatric candidates waiting for less than 1 year (Figure KI 108). Of the 1,084 candidates removed from the waiting list in 2021, 692 (63.8%) received a deceased donor kidney, 257 (23.7%) received a living donor kidney, 20 (1.8%) died, 4 (0.3%) were removed from the list because their condition improved, and 9 (0.8%) were considered too sick to undergo transplant (Table KI 14, Table KI 15). Among patients newly listed from 2016-2018, 50.5% underwent DDKT within 3 years, 25.6% underwent LDKT, 15.9% were still waiting, 7.1% were removed from the list for other reasons, and 0.9% died (Figure KI 110). After declining to its lowest point in 2020, the rate of DDKT among pediatric waitlisted candidates increased to 41.0 transplants per 100 patient-years in 2021 (Figure KI 111). In 2021, transplant rates were highest for candidates aged 12-17 years (56.1 per 100 patient-years), followed by candidates aged 1-5 years (49.9 per 100 patient-years), 6-11 years (43.9 per 100 patient-years), and younger than 1 year (19.1 per 100 patient-years) (Figure KI 112). Transplant rates vary by cPRA, with the highest rates among candidates 20%-<80% (46.7 transplants per 100 patient-years in 2021). The priority for highly sensitized candidates continued to result in higher transplant rates than pre-KAS, remaining steady at approximately 14 transplants per 100 patient-years since 2015 (Figure KI 114). Compared with pretransplant mortality of 6.0 deaths per 100 patient-years among adult kidney transplant candidates (Figure KI 25), pretransplant mortality among pediatric candidates was 1.2 deaths per 100 patient- years in 2021, with little variation by age or race (Figure KI 116, Figure KI 117, Figure KI 118).
Figure KI 108.
Distribution of pediatric candidates waiting for kidney transplant by waiting time. Candidates waiting for transplant any time in the given year. Candidates listed at more than one center are counted once per listing. Time on the waiting list is determined at the earliest of transplant, death, removal, or December 31 of the year. Candidates listed in the given year are considered to have been listed less than 1 year. Active and inactive candidates are included.
Table KI 14.
Kidney transplant waitlist activity among pediatric candidates. Candidates who are listed, undergo transplant, and are relisted are counted more than once. Candidates are not considered to be on the list on the day they are removed; counts on January 1 may differ from counts on December 31 of the prior year. Candidates listed for multiorgan transplants are included.
| Waiting list state |
2019 |
2020 |
2021 |
|---|---|---|---|
| Waiting list state | |||
| Patients at start of year | 1549 | 1553 | 1695 |
| Patients added during year | 1030 | 1083 | 1087 |
| Patients removed during year | 1025 | 941 | 1084 |
| Patients at end of year | 1554 | 1695 | 1698 |
Table KI 15.
Removal reason among pediatric kidney transplant candidates. Removal reason as reported to the OPTN. Candidates with death dates that precede removal dates are assumed to have died waiting.
| Removal reason |
2019 |
2020 |
2021 |
|---|---|---|---|
| Removal reason | |||
| Deceased donor transplant | 611 | 563 | 692 |
| Living donor transplant | 262 | 248 | 257 |
| Transplant outside US | 0 | 1 | 0 |
| Patient died | 18 | 20 | 20 |
| Patient refused transplant | 3 | 2 | 6 |
| Improved, transplant not needed | 6 | 5 | 4 |
| Too sick for transplant | 11 | 8 | 9 |
| Other | 114 | 92 | 96 |
| Changed to kidney-pancreas list | 0 | 1 | 0 |
| Still on waiting list | 0 | 1 | 0 |
Figure KI 110.
Three-year outcomes for newly listed pediatric candidates waiting for kidney trans- plant, 2016-2018. Pediatric candidates who joined the waitlist in 2016-2018. Candidates listed at more than one center are counted once per listing. DD, deceased donor; LD, living donor.
Figure KI 111.
Overall deceased donor kidney transplant rates among pediatric waitlist candidates. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of waiting in a given year. Individual listings are counted separately.
Figure KI 112.
Deceased donor kidney transplant rates among pediatric waitlist candidates by age. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of waiting in a given year. Individual listings are counted separately. Age is determined at the later of listing date or January 1 of the given year.
Figure KI 114.
Deceased donor kidney transplant rates among pediatric waitlist candidates by cPRA. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of waiting in a given year. Individual listings are counted separately. cPRA is determined at the earliest of transplant, death, removal, or December 31 of the year.
Figure KI 116.
Overall pretransplant mortality rates among pediatric candidates waitlisted for kid- ney. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of im- proved condition, or end of cohort. Individual listings are counted separately.
Figure KI 117.
Pretransplant mortality rates among pediatric candidates waitlisted for kidney trans- plant by age. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately. Age is determined at the later of listing date or January 1 of the given year.
Figure KI 118.
Pretransplant mortality rates among pediatric candidates waitlisted for kidney trans- plant by race. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately.
3.2. Transplant
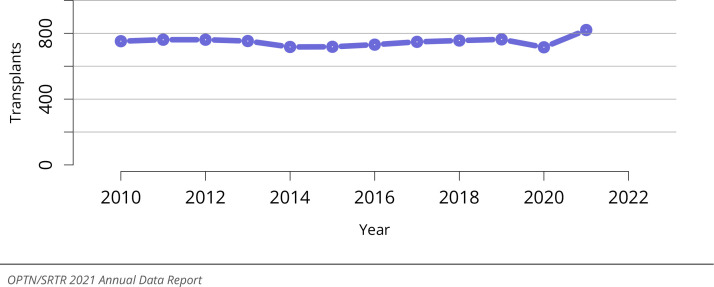
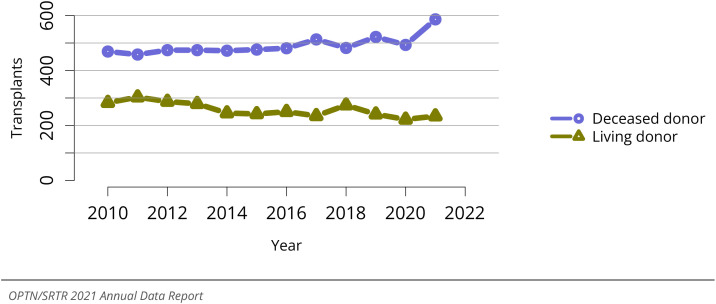
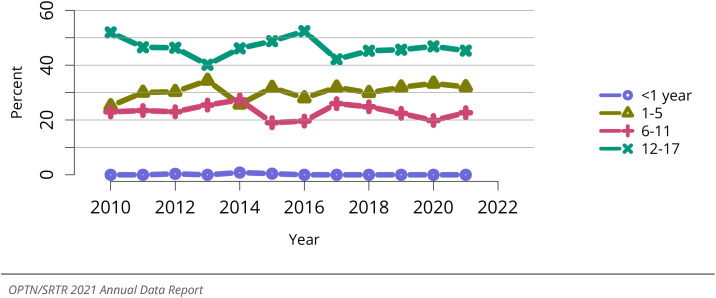
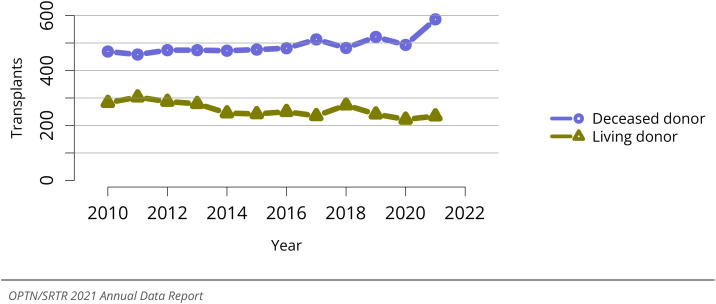
The total number of pediatric kidney transplants performed increased to its highest point in the past decade, at 820 transplants in 2021 (Figure KI 120). This increase was driven by an increase in the number of DDKTs as the number of LDKTs remains disappointingly low (Figure KI 121). In 2021, LDKTs accounted for only 28.5% of total transplants among pediatric recipients (Figure KI 121). Children aged 12-17 years made up the largest group of LDKT recipients (45.3%) (Figure KI 123).
Figure KI 120.
Overall pediatric kidney transplants. All pediatric kidney transplant recipients, including retransplant, and multiorgan recipients.
Figure KI 121.
Pediatric kidney transplants by donor type. All pediatric kidney transplant recipients, including retransplant, and multiorgan recipients.
Figure KI 123.
Percent of pediatric kidney transplants from living donors by recipient age. All pedi- atric living kidney transplant recipients, including retransplant, and multiorgan recipients.
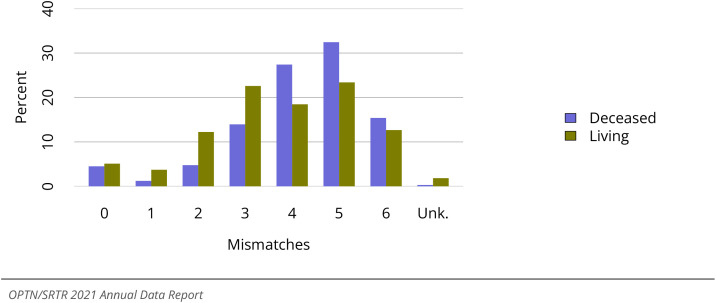
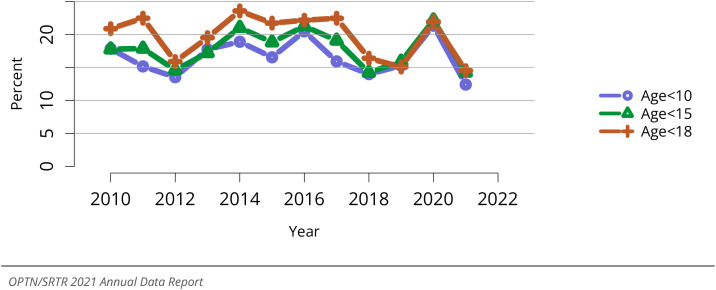
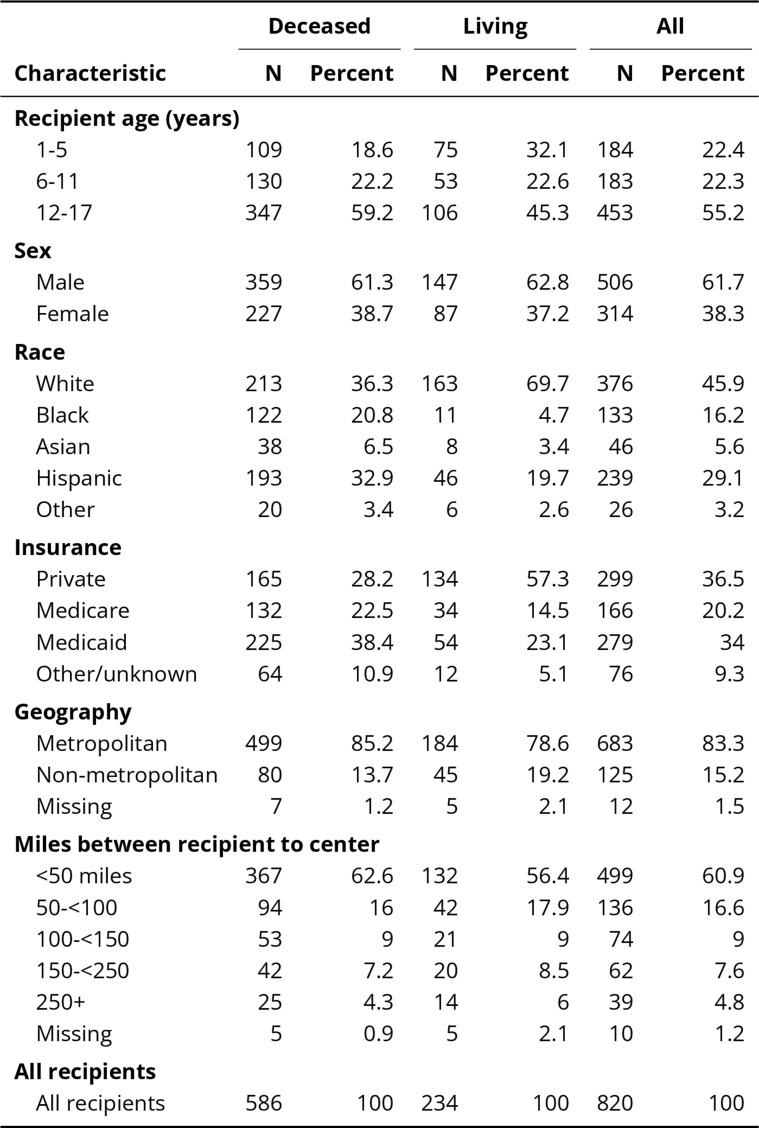
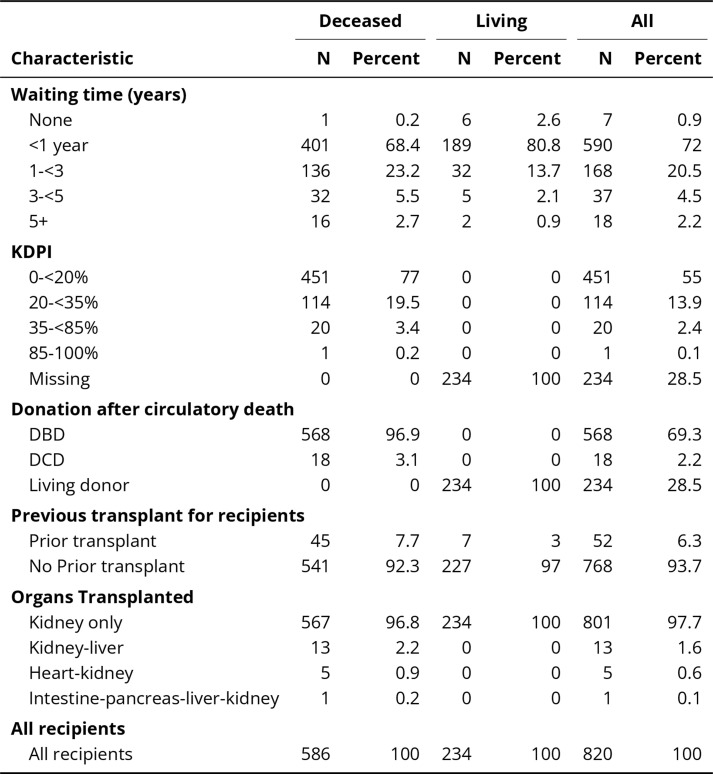
In 2021, 36 programs were performing only pediatric kidney transplants, compared with 136 performing only adult transplants and 54 performing transplants in both adults and children (Figure KI 124). Looking at transplant center volume, 14.5% of transplants in candidates aged younger than 18 years were performed at programs with volume of five or fewer pediatric transplants in 2021 (Figure KI 125). Most pediatric recipients who underwent transplant in 2021 were aged 12-17 years, 59.2% among DDKT recipients and, again, 45.3% among LDKT recipients (Table KI 16). The racial and ethnic distribution was notably different for DDKT and LDKT recipients. For LDKT recipients, 69.7% were White, 4.7% were Black, 19.7% were Hispanic, and 3.4% were Asian. In contrast, 36.3% of DDKT recipients were White, 20.8% were Black, 32.9% were Hispanic, and 6.5% were Asian (Table KI 16). Private insurance was more common among LDKT recipients (57.3%) and Medicare/Medicaid among DDKT recipients (60.9%) (Table KI 16). Most DDKT recipi- ents (96.4%) underwent transplant with a kidney from a donor with KDPI less than 35% (Table KI 18). Most pediatric DDKT recipients (82.9%) had four or more HLA mismatches compared with only 29.6% of LDKT recipients (Figure KI 128). Multiorgan transplant re- mained uncommon; only 2.3% of pediatric candidates received multiorgan transplant in 2021 (Table KI 18).
Figure KI 124.
Number of centers performing pediatric and adult kidney transplants by center age mix. Adult centers performed transplants only for recipients aged 18 years or older. Functionally adult centers performed transplants for 80% adults or more, and the remainder were children aged 15-17 years. Mixed included adults and children of any age groups. Pediatric centers performed transplants for recipi- ents aged 0-17 years, and a small number of adults up to age 21 years.
Figure KI 125.
Pediatric kidney recipients at programs that perform 5 or fewer pediatric transplants annually. Age groups are cumulative.
Table KI 16.
Demographic characteristics of pediatric kidney transplant recipients, 2021. Pediatric kidney transplant recipients, including retransplants. Distance is computed from recipient’s home zip code to the transplant center.
Table KI 18.
Transplant characteristics of pediatric kidney transplant recipients, 2021. Pediatric kidney transplant recipients, including retransplants. DBD, donation after brain death; DCD, donation after circulatory death; DGF, delayed graft function; KDPI, kidney donor profile index. DCD status and KDPI scores apply to deceased donor transplants only.
Figure KI 128.
Total HLA A, B, and DR mismatches among pediatric kidney transplant recipients, 2017-2021. Donor and recipient antigen matching is based on OPTN antigen values and split equivalences policy as of 2019.
The combination of a donor who was positive for cytomegalovirus and a pediatric recipient who was negative occurred in 36.7% of DDKTs (Table KI 19) and in 29.1% of LDKTs (Table KI 20). The combination of a donor who was positive for Epstein-Barr virus (EBV) and a pediatric recipient who was negative occurred in 37.6% (Table KI 19) of DDKTs and in 55.5% of LDKTs (Table KI 20).
Table KI 19.
Pediatric deceased donor kidney donor-recipient serology matching, 2019-2021. Donor serology is reported on the OPTN Donor Registration Form and recipient serology on the OPTN Trans- plant Recipient Registration Form. There may be multiple fields per serology. Any evidence for a positive serology is treated as positive for that serology. CMV, cytomegalovirus; EBV, Epstein-Barr virus.
| Donor | Recipient | CMV | EBV |
|---|---|---|---|
| Donor | |||
| D- | R- | 27.73 | 5.81 |
| D- | R+ | 12.87 | 7.56 |
| D- | R unk | 0.94 | 0.25 |
| D+ | R- | 36.66 | 37.6 |
| D+ | R+ | 20.55 | 47.16 |
| D+ | R unk | 0.31 | 1.31 |
| D unk | R- | 0.56 | 0.19 |
| D unk | R+ | 0.37 | 0.12 |
| D unk | R unk | 0 | 0 |
Table KI 20.
Pediatric living donor kidney donor-recipient serology matching, 2019-2021. Donor serology is reported on the OPTN Donor Registration Form and recipient serology on the OPTN Trans- plant Recipient Registration Form. There may be multiple fields per serology. Any evidence for a positive serology is treated as positive for that serology. CMV, cytomegalovirus; EBV, Epstein-Barr virus.
| Donor | Recipient | CMV | EBV |
|---|---|---|---|
| Donor | |||
| D- | R- | 38.59 | 6.74 |
| D- | R+ | 10.47 | 3.44 |
| D- | R unk | 0.57 | 0 |
| D+ | R- | 29.12 | 55.52 |
| D+ | R+ | 15.21 | 30.7 |
| D+ | R unk | 0.43 | 2.3 |
| D unk | R- | 4.02 | 0.43 |
| D unk | R+ | 1.43 | 0.86 |
| D unk | R unk | 0.14 | 0 |
3.3. Immunosuppressive Medication Use
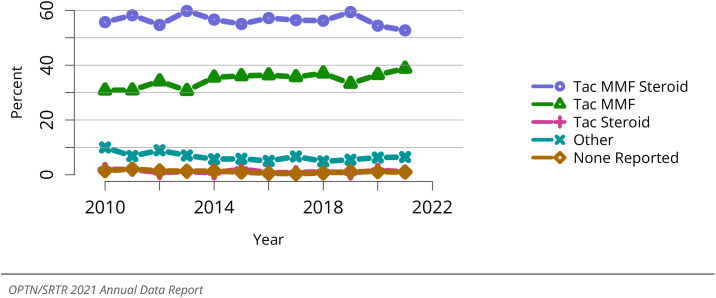
Almost all (94.0%) pediatric kidney transplant recipients reported some induction use in 2021 (Figure KI 126). The most common maintenance immunosuppression regimens at hospital discharge were tacrolimus, MMF, and steroids in 52.7% of recipients, followed by tacrolimus and MMF in 38.8% (Figure KI 127).
Figure KI 126.
Induction agent use in pediatric kidney transplant recipients. Immunosuppression at transplant reported to the OPTN.
Figure KI 127.
Immunosuppression regimen use in pediatric kidney transplant recipients. Immuno- suppression regimen at transplant reported to the OPTN. Tac, tacrolimus. MMF, all mycophenolate agents.
3.4. Outcomes
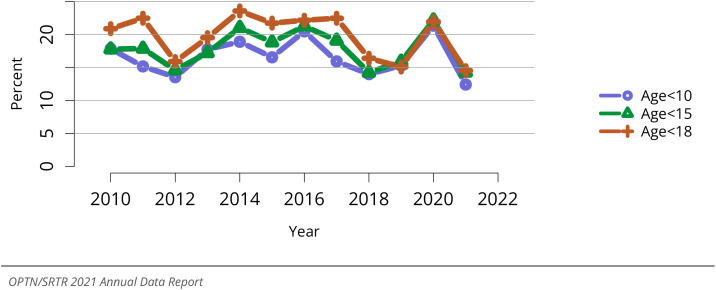
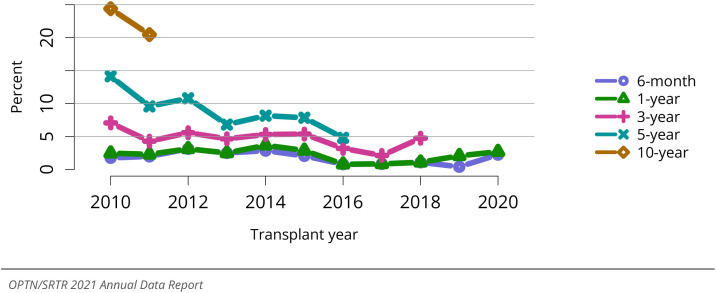
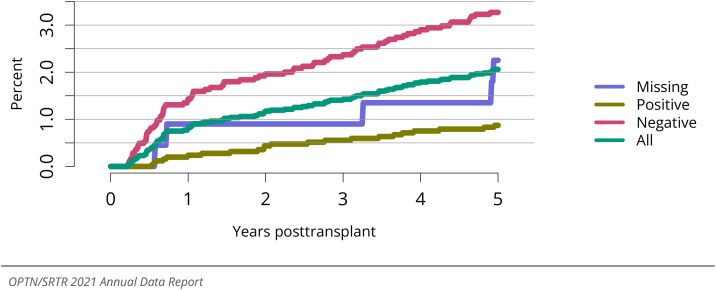
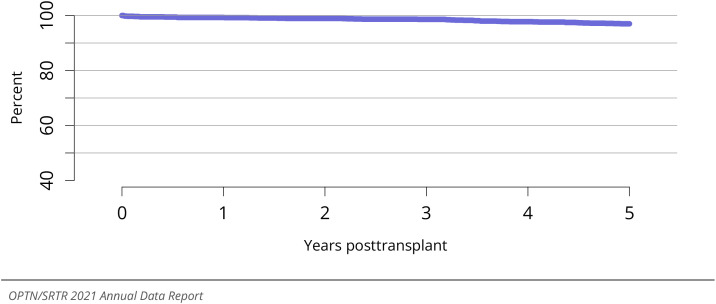
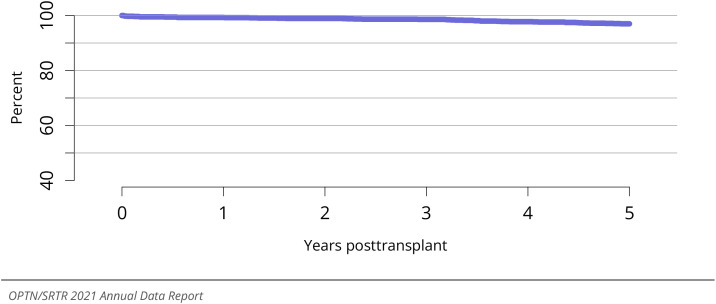
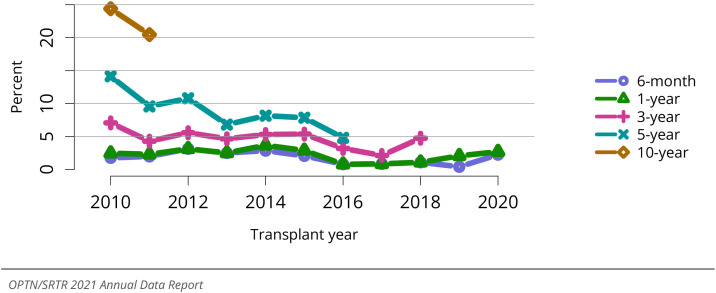
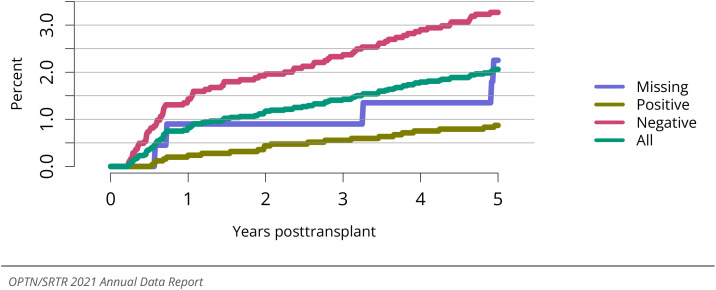
Graft failure after kidney-alone DDKT in pediatric recipients was 1.8% at 6 months and 2.4% at 1 year for transplants in 2020, 5.4% at 3 years for transplants in 2018, 13.9% at 5 years for transplants in 2016, and 31.9% at 10 years for transplants in 2011 (Figure KI 132). Corresponding graft failure after LDKT was 2.3% at 6 months and 2.7% at 1 year for transplants in 2020, 4.7% at 3 years for transplants in 2018, 4.8% at 5 years for trans- plants in 2016, and 20.5% at 10 years for transplants in 2011 (Figure KI 133). For the cohort of recipients who underwent transplant in 2014-2016, 1- and 5-year graft survival were 96.9% and 85.2% for DDKT recipients and 97.6% and 93.1% for LDKT recipients, respectively (Figure KI 135). In the 2020 cohort, the overall incidence of acute rejection within the first year ranged from 7.7% among patients aged 6-11 years to 11.3% among patients aged 12-17 years (Figure KI 136). Short-term renal function, measured by eGFR, has remained stable over the past decade. Proportions of LDKT and DDKT recipients from 2020 with eGFR of 60 mL/min/1.73 m2 or higher at 12 months posttransplant were 69.8% and 72.0%, respectively (Figures KI 131 and 130). Incidence of posttransplant lym- phoproliferative disorder among EBV-negative recipients from 2010-2016 was 3.5% at 5 years posttransplant, compared with 0.9% among EBV-positive recipients (Figure KI 137). Overall, 5-year patient survival among pediatric DDKT recipients in 2014-2016 was very high, at 97.0% (Figure KI 139), with little variability by age (Figure KI 140).
Figure KI 132.
Graft failure among pediatric deceased donor kidney transplant recipients. All pedi- atric recipients of deceased donor kidneys, including multiorgan transplants. Estimates are unadjusted, computed using Kaplan-Meier methods. Recipients are followed to the earliest of kidney graft failure; kid- ney retransplant; return to dialysis; death; or 6 months, 1, 3, 5, or 10 years posttransplant. All-cause graft failure is defined as any of the prior outcomes prior to 6 months, 1, 3, 5, or 10 years, respectively.
Figure KI 133.
Graft failure among pediatric living donor kidney transplant recipients. All pediatric recipients of living donor kidneys, including multiorgan transplants. Estimates are unadjusted, computed using Kaplan-Meier methods. Recipients are followed to the earliest of kidney graft failure; kidney retrans- plant; return to dialysis; death; or 6 months, 1, 3, 5, or 10 years posttransplant. All-cause graft failure is defined as any of the prior outcomes prior to 6 months, 1, 3, 5, or 10 years, respectively.
Figure KI 135.
Graft survival among pediatric kidney transplant recipients, 2014-2016, by donor type. Recipient survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 136.
Incidence of acute rejection by 1 year posttransplant among pediatric kidney trans- plant recipients by age. Only the first reported rejection event is counted. Cumulative incidence is esti- mated using the Kaplan-Meier method.
Figure KI 131.
Distribution of eGFR at 12 months posttransplant among pediatric living donor kidney-alone transplant recipients. GFR (mL/min/1.73 m2) estimated using the bedside Schwartz equa- tion, and computed by SRTR for patients alive with graft function at 12 months posttransplant. Equation: eGFR = 0.413*Height(cm)/Creatinine (mg/dL).
Figure KI 130.
Distribution of eGFR at 12 months posttransplant among pediatric deceased donor kidney-alone transplant recipients. GFR (mL/min/1.73 m2) estimated using the bedside Schwartz equa- tion, and computed by SRTR for patients alive with graft function at 12 months posttransplant. Equation: eGFR = 0.413*Height(cm)/Creatinine (mg/dL).
Figure KI 137.
Incidence of PTLD among pediatric kidney transplant recipients by recipient EBV sta- tus at transplant, 2010-2016. Cumulative incidence is estimated using the Kaplan-Meier method. PTLD is identified as a reported complication or cause of death on the OPTN Transplant Recipient Follow-up Form or on the Posttransplant Malignancy Form as polymorphic PTLD, monomorphic PTLD, or Hodgkin’s disease. Only the earliest date of PTLD diagnosis is considered. EBV, Epstein-Barr virus. PTLD, posttrans- plant lymphoproliferative disorder.
Figure KI 139.
Overall patient survival among pediatric deceased donor kidney transplant recipi- ents, 2014-2016. Recipient survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 140.
Patient survival among pediatric deceased donor kidney transplant recipients, 2014- 2016, by recipient age. Recipient survival estimated using unadjusted Kaplan-Meier methods.
This publication was produced for the U.S. Department of Health and Human Ser- vices (HHS), Health Resources and Services Administration (HRSA), by Hennepin Health- care Research Institute (HHRI) and the United Network for Organ Sharing (UNOS) under contracts HHSH75R60220C00011 and HHSH250201900001C, respectively.
This publication lists nonfederal resources in order to provide additional informa- tion to consumers. The views and content in these resources have not been formally approved by HHS or HRSA. Neither HHS nor HRSA endorses the products or services of the listed resources.
The OPTN/SRTR 2021 Annual Data Report is not copyrighted. Readers are free to du- plicate and use all or part of the information contained in this publication. Data are not copyrighted and may be used without permission if appropriate citation information is provided.
Pursuant to 42 U.S.C. §1320b-10, this publication may not be reproduced, reprinted, or redistributed for a fee without specific written authorization from HHS.
Suggested Citations:
Full citation: Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR). OPTN/SRTR 2021 Annual Data Report. U.S. De- partment of Health and Human Services, Health Resources and Services Administration; 2023. Accessed [insert date]. http://srtr.transplant.hrsa.gov/annual_reports/Default. aspx
Abbreviated citation: OPTN/SRTR 2021 Annual Data Report. HHS/HRSA; 2023. Accessed [insert date]. http://srtr.transplant.hrsa.gov/annual_reports/Default.aspx
Publications based on data in this report or supplied on request must include a ci- tation and the following statement: The data and analyses reported in the OPTN/SRTR 2021 Annual Data Report have been supplied by the United Network for Organ Sharing and Hennepin Healthcare Research Institute under contract with HHS/HRSA. The authors alone are responsible for reporting and interpreting these data; the views expressed herein are those of the authors and not necessarily those of the U.S. government.
This report is available at https://srtr.transplant.hrsa.gov. Individual chapters may be downloaded.
Figure KI 10.
Distribution of adults waiting for kidney transplant by blood type. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure KI 47: Percent of kidneys recovered for transplant and not transplanted by donor sex. Per- centages of kidneys not transplanted out of all kidneys recovered for transplant.
Figure KI 51: Percent of kidneys recovered for transplant and not transplanted by donor terminal creatinine. Percentages of kidneys not transplanted out of all kidneys recovered for transplant.
Figure KI 53: Percent of kidneys recovered for transplant and not transplanted by donor cause of death. Percentages of kidneys not transplanted out of all kidneys recovered for transplant. CVA, cere- brovascular accident.
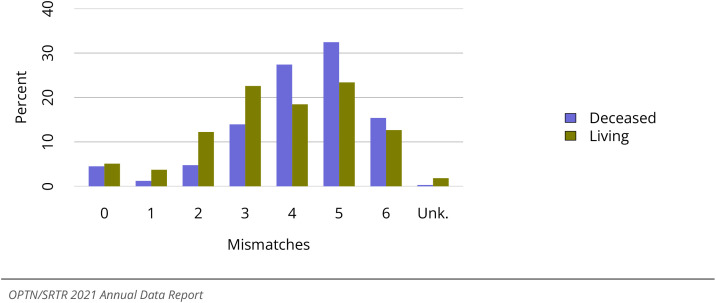
Figure KI 75: Total HLA A, B, and DR mismatches among adult kidney transplant recipients, 2017- 2021. Donor and recipient antigen matching is based on OPTN antigen values and split equivalences policy as of 2019.
Figure KI 92: Incidence of PTLD among adult kidney transplant recipients by recipient EBV status at transplant, 2010-2016. Cumulative incidence is estimated using the Kaplan-Meier method. PTLD is identified as a reported complication or cause of death on the OPTN Transplant Recipient Follow-up Form or the Posttransplant Malignancy Form as polymorphic PTLD, monomorphic PTLD, or Hodgkin’s disease. Only the earliest date of PTLD diagnosis is considered. EBV, Epstein-Barr virus; PTLD, posttransplant lym- phoproliferative disorder.
Figure KI 106: Distribution of pediatric candidates waiting for kidney transplant by diagnosis. Can- didates waiting for transplant any time in the given year. Candidates listed at more than one center are counted once per listing. Diagnosis categories follow North American Pediatric Renal Trials and Collab- orative Studies recommendations. Active and inactive candidates are included. FSGS, focal segmental glomerulosclerosis; CAKUT, congenital anomalies of the kidney and urinary tract.
Figure KI 107: Distribution of pediatric candidates waiting for kidney transplant by sex. Candidates waiting for transplant any time in the given year. Candidates listed at more than one center are counted once per listing. Active and inactive patients are included.
Figure KI 109: Distribution of pediatric candidates waiting for kidney transplant by cPRA. Candidates waiting for transplant at any time in the given year. Candidates listed at more than one center are counted once per listing. cPRA is determined at the earliest of transplant, death, removal, or December 31 of the year. Active and inactive candidates are included.
Figure KI 113: Deceased donor kidney transplant rates among pediatric waitlist candidates by race. Transplant rates are computed as the number of deceased donor transplants per 100 patient-years of waiting in a given year. Individual listings are counted separately.
Figure KI 115: Deceased donor kidney transplant rates among pediatric waitlist candidates by metropolitan vs. non-metropolitan residence. Transplant rates are computed as the number of de- ceased donor transplants per 100 patient-years of waiting in a given year. Individual listings are counted separately.
Figure KI 119: Pretransplant mortality rates among pediatric candidates waitlisted for kidney trans- plant by metropolitan vs. non-metropolitan residence. Mortality rates are computed as the number of deaths per 100 patient-years of waiting in the given year. Waiting time is censored at transplant, death, transfer to another program, removal because of improved condition, or end of cohort. Individual listings are counted separately. Urban/rural determination is made using the RUCA (rural-urban commuting area) designation of the candidate’s permanent zip code.
Figure KI 122: Pediatric kidney transplants by recipient age. All pediatric kidney transplant recipients, including retransplant, and multiorgan recipients.
Figure KI 129: Delayed graft function among pediatric kidney transplant recipients. All pediatric recipients of kidneys. Delayed graft function is defined as dialysis administered within the first seven days posttransplant.
Figure KI 134: Graft survival among pediatric deceased donor kidney transplant recipients, 2014- 2016, by age. Recipient survival estimated using unadjusted Kaplan-Meier methods.
Figure KI 138: Patient death among pediatric kidney transplant recipients. All pediatric recipients of deceased donor kidneys, including multiorgan transplants. Estimates are unadjusted, computed using unadjusted Kaplan-Meier methods.
Table KI 2: Clinical characteristics of adults on the kidney transplant waiting list on December 31, 2011, December 31, 2016 and December 31, 2021. Candidates waiting for transplant on December 31 of the given year, regardless of first listing date. *Diabetes status based on diagnosis and comorbid conditions.
| Characteristic | 2011 | 2016 | 2021 | |||
| N | Percent | N | Percent | N | Percent | |
| Diagnosis | ||||||
| Diabetes | 31796 | 33.3 | 37714 | 36.1 | 37162 | 38.7 |
| Hypertension | 23873 | 25 | 24272 | 23.3 | 19734 | 20.5 |
| Glomerulonephritis | 13946 | 14.6 | 15028 | 14.4 | 13513 | 14.1 |
| Cystic kidney disease | 8081 | 8.5 | 9202 | 8.8 | 8424 | 8.8 |
| Other/unknown | 17675 | 18.5 | 18112 | 17.4 | 17297 | 18 |
| NA | 1 | 0 | 1 | 0 | 0 | 0 |
| Blood Type | ||||||
| A | 27425 | 28.8 | 29011 | 27.8 | 25749 | 26.8 |
| AB | 2709 | 2.8 | 2735 | 2.6 | 2407 | 2.5 |
| B | 15369 | 16.1 | 17353 | 16.6 | 15985 | 16.6 |
| O | 49869 | 52.3 | 55230 | 52.9 | 51989 | 54.1 |
| CPRA | ||||||
| <1% | 60276 | 63.2 | 65371 | 62.7 | 59609 | 62 |
| 1-<20% | 6380 | 6.7 | 9160 | 8.8 | 9125 | 9.5 |
| 20-<80% | 13357 | 14 | 15835 | 15.2 | 16493 | 17.2 |
| 80-<98% | 6626 | 6.9 | 6231 | 6 | 5003 | 5.2 |
| 98-100% | 8733 | 9.2 | 7732 | 7.4 | 5900 | 6.1 |
| All candidates | ||||||
| All candidates | 95372 | 100 | 104329 | 100 | 96130 | 100 |
Table KI 3: Listing characteristics of adults on the kidney transplant waiting list on December 31, 2011, December 31, 2016 and December 31, 2021. Candidates waiting for transplant on December 31 of the given year, regardless of first listing date.
| Characteristic | 2011 |
2016 |
2021 |
|||
|---|---|---|---|---|---|---|
| N | Percent | N | Percent | N | Percent | |
| Waiting time (years) | ||||||
| year | 29311 | 30.7 | 29244 | 28 | 31622 | 32.9 |
| 1-<2 | 22336 | 23.4 | 21418 | 20.5 | 19210 | 20 |
| 2-<3 | 15806 | 16.6 | 16972 | 16.3 | 15925 | 16.6 |
| 3-<5 | 17034 | 17.9 | 21416 | 20.5 | 16979 | 17.7 |
| 5+ | 10885 | 11.4 | 15279 | 14.6 | 12394 | 12.9 |
| Previous transplant | ||||||
| No prior transplant | 80501 | 84.4 | 90844 | 87.1 | 85012 | 88.4 |
| Prior transplant | 14871 | 15.6 | 13485 | 12.9 | 11118 | 11.6 |
| All candidates | ||||||
| All candidates | 95372 | 100 | 104329 | 100 | 96130 | 100 |
Table KI 4: Kidney transplant waitlist activity among adults. Candidates listed at more than one center are counted once per listing. Candidates who are listed, undergo transplant, and are relisted are counted more than once. Candidates are not considered to be on the list on the day they are removed; counts on January 1 may differ from counts on December 31 of the prior year. Candidates listed for multiorgan transplants are included.
| Waiting list state | 2019 | 2020 | 2021 |
|---|---|---|---|
| Waiting list state | |||
| Patients at start of year | 101127 | 101362 | 97260 |
| Patients added during year | 42933 | 37399 | 41765 |
| Patients removed during year | 42643 | 41470 | 42895 |
| Patients at end of year | 101417 | 97291 | 96130 |
Table KI 9: Adult deceased donor kidney donor-recipient serology matching, 2018-2020. Donor serology is reported on the OPTN Donor Registration Form and recipient serology on the OPTN Trans- plant Recipient Registration Form. There may be multiple fields per serology. Any evidence for a positive serology is treated as positive for that serology. Donor HCV NAT data are shown by recipient HCV antibody status. CMV, cytomegalovirus; EBV, Epstein-Barr virus; HBsAg, hepatitis B surface antigen; HCV, hepatitis C virus; HIV, human immunodeficiency virus; NAT, nucleic acid test.
| Donor | Recipient | CMV | EBV | HBsAg | HCV antibody | HCV NAT |
|---|---|---|---|---|---|---|
| Donor | ||||||
| D- | R- | 13.43 | 0.63 | 97.33 | 84.98 | 88.57 |
| D- | R+ | 24.9 | 7.71 | 1.24 | 3.13 | 3.35 |
| D- | R unk | 0.46 | 0.23 | 1.21 | 1.56 | 1.63 |
| D+ | R- | 18.55 | 4.96 | 0.17 | 9.18 | 5.57 |
| D+ | R+ | 41.55 | 83.33 | 0.01 | 0.96 | 0.74 |
| D+ | R unk | 0.63 | 2.89 | 0 | 0.19 | 0.11 |
| D unk | R- | 0.15 | 0.01 | 0.04 | 0.01 | 0.02 |
| D unk | R+ | 0.32 | 0.22 | 0 | 0 | 0 |
| D unk | R unk | 0.01 | 0.01 | 0 | 0 | 0 |
Table KI 10: Adult living donor kidney donor-recipient serology matching, 2019-2021. Donor serology is reported on the OPTN Donor Registration Form and recipient serology on the OPTN Transplant Recipient Registration Form. There may be multiple fields per serology. Any evidence for a positive serology is treated as positive for that serology. Donor HCV NAT data are shown by recipient HCV antibody status. CMV, cytomegalovirus; EBV, Epstein-Barr virus; HBsAg, hepatitis B surface antigen; HCV, hepatitis C virus; HIV, human immunodeficiency virus; NAT, nucleic acid test.
| Donor | Recipient | CMV | EBV | HBsAg | HCV antibody | HCV NAT |
|---|---|---|---|---|---|---|
| Donor | ||||||
| D- | R- | 24.95 | 1.24 | 95.67 | 93.82 | 85.62 |
| D- | R+ | 20.76 | 6.99 | 0.85 | 1.81 | 1.67 |
| D- | R unk | 0.55 | 0.17 | 1.4 | 2.1 | 1.96 |
| D+ | R- | 17.46 | 6.01 | 0.31 | 0.76 | 0.07 |
| D+ | R+ | 32.03 | 82.08 | 0 | 0.03 | 0.01 |
| D+ | R unk | 0.67 | 1.77 | 0 | 0.01 | 0 |
| D unk | R- | 1.67 | 0.14 | 1.69 | 1.39 | 10.28 |
| D unk | R+ | 1.87 | 1.46 | 0.02 | 0.02 | 0.19 |
| D unk | R unk | 0.05 | 0.13 | 0.06 | 0.05 | 0.2 |
Table KI 17: Clinical characteristics of pediatric kidney transplant recipients, 2021. Pediatric kid- ney transplant recipients, including retransplants. Diagnosis categories follow North American Pediatric Renal Trials and Collaborative Studies recommendations. FSGS, focal segmental glomerulosclerosis; GN, glomerulonephritis; CAKUT, congenital anomalies of the kidney and urinary tract.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajt.2023.02.004
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Executive Office of the President Executive Order 13879 of July 10, 2019: Advancing American Kidney Health. 2019. https://www.federalregister.gov/documents/2019/07/15/2019-15159/ advancing-american-kidney-health
- 2.Abara W.E., Collier M.G., Moorman A., et al. Characteristics of Deceased Solid Organ Donors and Screening Results for Hepatitis B, C, and Human Im- munodeficiency Viruses — United States, 2010–2017. MMWR. 2019;68:61–66. doi: 10.15585/mmwr.mm6803a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services Health Resources and Services Ad- ministration. New Rule Expands the Scope of Reimbursable Expenses for Living Or- gan Donation. 2020. https://www.hrsa.gov/about/ news/press-releases/new-rule-expands-scope-living-organ-donation
- 4.Lentine K.L., Mannon R.B., Mandelbrot D. Understanding and Overcoming Finan- cial Risks for Living Organ Donors. Am J Kidney Dis. 2022 Feb;79(2):159–161. doi: 10.1053/j.ajkd.2021.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Stewart D.E., Foutz J., Kamal L., et al. The Independent Effects of Procurement Biopsy Findings on 10-Year Outcomes of Extended Criteria Donor Kidney Transplants. Kid- ney Int Rep. 2022;7(8):1850–1865. doi: 10.1016/j.ekir.2022.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.